Abstract
Introduction
Paediatric occupational therapy seeks to improve children's engagement and participation in life roles. A wide variety of intervention approaches exist. Our aim was to summarise the best‐available intervention evidence for children with disabilities, to assist families and therapists choose effective care.
Methods
We conducted a systematic review (SR) using the Cochrane methodology, and reported findings according to PRISMA. CINAHL, Cochrane Library, MEDLINE, OTSeeker, PEDro, PsycINFO were searched. Two independent reviewers: (i) determined whether studies met inclusion: SR or randomised controlled trial (RCT); an occupational therapy intervention for children with a disability; (ii) categorised interventions based on name, core components and diagnostic population; (iii) rated quality of evidence and determined the strength of recommendation using GRADE criteria; and (iv) made recommendations using the Evidence Alert Traffic Light System.
Results
129 articles met inclusion (n = 75 (58%) SRs; n = 54 (42%)) RCTs, measuring the effectiveness of 52 interventions, across 22 diagnoses, enabling analysis of 135 intervention indications. Thirty percent of the indications assessed (n = 40/135) were graded ‘do it’ (Green Go); 56% (75/135) ‘probably do it’ (Yellow Measure); 10% (n = 14/135) ‘probably don't do it’ (Yellow Measure); and 4% (n = 6/135) ‘don't do it’ (Red Stop). Green lights were: Behavioural Interventions; Bimanual; Coaching; Cognitive Cog‐Fun & CAPS; CO‐OP; CIMT; CIMT plus Bimanual; Context‐Focused; Ditto; Early Intervention (ABA, Developmental Care); Family Centred Care; Feeding interventions; Goal Directed Training; Handwriting Task‐Specific Practice; Home Programs; Joint Attention; Mental Health Interventions; occupational therapy after toxin; Kinesiotape; Pain Management; Parent Education; PECS; Positioning; Pressure Care; Social Skills Training; Treadmill Training and Weight Loss ‘Mighty Moves’.
Conclusion
Evidence supports 40 intervention indications, with the greatest number at the activities‐level of the International Classification of Function. Yellow light interventions should be accompanied by a sensitive outcome measure to monitor progress and red light interventions could be discontinued because effective alternatives existed.
Keywords: disability, intervention and service provision, occupational therapy, paediatric, systematic review
Introduction
Occupational therapy intervention for children promotes engagement and participation in children's daily life roles (Mandich & Rodger, 2006). Children's roles include, developing personal independence, becoming productive and participating in play or leisure pursuits (Roger et al.). Inability to participate because of disease, disability or skill deficits, can cause marginalisation, social isolation and lowered self‐esteem (Mandich & Rodger, 2006). Occupational therapists select interventions for children based upon an analysis of the child's performance of daily life roles, how their performance is affected by their disability, and how their environment supports or constrains their performance (Mandich & Rodger, 2006).
The practices of paediatric occupational therapists have evolved and changed based on research and theory (Rodger, Brown & Brown, 2005), such as family centred care and the World Health Organisation's (WHO) International Classification of Functioning, Disability and Health (ICF; World Health Organisation, 2001). These frameworks have led many occupational therapists to move away from impairment‐based interventions at the body structures and functions level aimed at remediating the child's deficits (known as ‘bottom‐up’ interventions), and instead to focus on improving functional activity performance and participation (‘top‐down’ interventions) (Weinstock‐Zlotnick & Hinojosa, 2004), as well as partnering with parents to deliver therapy embedded within daily life.
Clinicians will always have different expertise and preferences, but there are financial and ethical ramifications of delivering interventions. Ensuring the latest research findings are easily accessible to families and clinicians is vital. Occupational therapists positively embrace evidence‐based practice, but on the ground, implementation can lag (Flores‐Mateo & Argimon, 2007; Upton, Stephens, Williams & Scurlock‐Evans, 2014). Systematic reviews (SR) indicate that the translation of the latest evidence into routine clinical care lags 10–20 years in all countries and specialities (Flores‐Mateo & Argimon), which for paediatric patients is an entire childhood. Multiple paediatric occupational therapy interventions exist to address children's specific goals. In partnership with parents, it is the therapist's role to choose and tailor the intervention choices to match the child and parent's goals, preferences and potential for improvement based upon their diagnosis. Staying up‐to‐date is time‐consuming. Furthermore, appraising evidence and up skilling in new interventions requires reallocation of time and resources.
The aim of this paper is to systematically describe current intervention options available to paediatric occupational therapists across different child diagnostic populations, rating the quality and recommendations for use of each intervention, using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system (Guyatt et al., 2008) and the Evidence Alert Traffic Light System (Novak & McIntyre, 2010). The purpose of reviewing and rating the entire evidence‐base is to provide a ‘one‐stop’ access guide for clinicians and policy‐makers, allow for the easy comparison of interventions, encourage the uptake of evidence‐based interventions, to confer better outcomes for children. We sought to answer the following ‘PICOs’ question: What is the effectiveness of occupational therapy intervention for children with disabilities? Population = children with a disability (including arthrogyposis OR attention deficit hyperactivity disorder OR autism spectrum disorder OR behaviour disorders OR brachial plexus OR brain injury OR burns OR cerebral palsy OR cancer OR chronic pain OR developmental coordination disorder OR developmental disability OR down syndrome OR fetal alcohol spectrum disorder OR learning disability OR mental health OR muscle diseases; OR intellectual disability OR obesity OR preterm infants OR physical disability OR rheumatoid arthritis OR spina bifida); Intervention = occupational therapy (including all specific named occupational therapy techniques); Comparison = none specified; Outcome = all outcomes accepted; and Study Design = SR OR randomised controlled trials (RCTs).
Methods
Study design
A SR of reviews was conducted, to provide an overview of the best available evidence. RCTs not included within the SRs were also appraised.
Search strategy
This review was carried out according to the Cochrane Collaboration methodology (Higgins & Green, 2011), incorporating the recommended quality features for conducting SRs of reviews (Smith, Devane, Begley & Clarke, 2011), and is reported according to the PRISMA statement (Moher, Liberati, Tetzlaff & Altman, 2010). Relevant articles were identified by searching: CINAHL (1983–2016); Cochrane Database of Systematic Reviews (http://www.cochrane.org); Database of Reviews of Effectiveness (DARE); EMBASE (1980–2016); ERIC; Google Scholar; MEDLINE (1956–2014); OTSeeker (http://www.otseeker.com); and PsycINFO (1935–2016). Searches were supplemented by hand searching and retrieval of any additional articles meeting eligibility criteria that were cited in reference lists. The search of all published studies was performed in March 2014 and updated in August 2018. Interventions and keywords for investigation were identified using the contributing authors’ knowledge.
Inclusion criteria
Published studies fulfilling the following criteria were included: (i) Type of study: All SRs and RCTs meeting inclusion criteria were appraised. SRs were preferentially sought since they provide a summary of large bodies of evidence and help to explain differences amongst studies. Plus, SRs limit bias. We also included RCTs not included within the SRs, because they are the gold standard design for measuring the effectiveness of interventions. Lower levels of evidence were only included if: the SR reviewed lower levels of evidence; (ii) Types of interventions: Studies that involved the provision of any type of occupational therapy intervention; and (iii) Types of participants: Studies that explicitly involved humans in which 100% of the participants were children of any childhood disability diagnosis.
Exclusion criteria
(i) Studies about typically developing children or adults; (ii) diagnostic studies OR prognostic studies OR about outcome measure psychometrics OR about theoretical frameworks NOT intervention; (iii) interventions that primarily fall under the skillset of another profession, for example pharmacotherapies, psychotherapy, speech therapies, etc. (iv) a second publication of the same study (Note: RCTs that met inclusion criteria but were also cited within included SRs, were treated as duplicates and not reported on twice); (v) studies were unpublished or non‐peer reviewed; and (vi) full‐text was not available in English.
Data abstraction
A data abstraction form was devised based on the Cochrane's recommendations (Higgins & Green, 2011). Abstracts identified from searches were screened by two independent raters. Both independent raters reviewed full‐text versions of the articles and articles were retained if they met inclusion criteria. Agreement on inclusion and exclusion assignment was unanimous. Data extracted from included studies comprised: authors and date of study; type of intervention (if named), core components and diagnostic population; who delivered the intervention; location of where the intervention was carried out; intensity of the intervention; study design and original authors’ conclusions about efficacy across study outcomes (Table S1). In addition, based on intervention description and ICF definitions, reviewers assigned an ICF domain to each intervention outcome sought by study authors (World Health Organisation, 2001). Where multiple SRs or RCTs existed, we noted when the older research was superseded by newer evidence. Interventions with the same name and/or similar core components, and that were administered to the same diagnostic populations, were grouped together. All data required to answer the study questions were published within the papers, so no contact with authors was necessary. All the supporting data are included with Table S1.
Quality of the evidence
Quality ratings were assigned by two independent raters for each publication using GRADE (Guyatt et al., 2008), which is endorsed by the World Health Organization. Within GRADE randomised trials are initially rated high, observational studies low; and other levels of evidence very low. However, high quality evidence is downgraded if methodological flaws exist, and low quality evidence is upgraded when high rigor and large effect sizes exist (Guyatt et al. ). Ultimately, a high score indicates ‘further research is unlikely to change our confidence in the estimate of effect’; moderate scores indicate ‘further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate’; low scores indicate ‘further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate’; and very low scores indicate ‘any estimate of effect is very uncertain’ (Guyatt et al.).
Strength of recommendation
Unlike SR frameworks, the GRADE framework does not solely examine effect size to determine efficacy of intervention. Instead, effect size makes up just one component when weighing up the benefits and harms of each intervention. In line with the GRADE framework, the following factors were considered by both independent raters when evaluating the body of evidence for the intervention and arriving at a strength of recommendation for each diagnostic group: (i) methodological quality regarding likely benefits vs. likely risks; (ii) inconvenience; (iii) importance of the outcome that the intervention prevents; (iv) magnitude of intervention effect (effect size); (v) precision of estimate of effect; (vi) burdens; (vii) costs; and (viii) varying clinician and family values (Guyatt et al., 2008).
The Evidence Alert Traffic Light System (Novak & McIntyre, 2010) was then applied based on the strength of recommendations by both independent raters. The Evidence Alert Traffic Light System is a GRADE‐complementary knowledge translation tool designed to assist clinicians and families to obtain easily readable, clinically useful answers within minutes (Campbell, Novak, McIntyre & Lord, 2013), because the alert uses a simple, three‐level colour coding that recommends a course of action. Green signifies ‘go’ because high quality evidence indicates effectiveness; red signifies ‘stop’ because high quality evidence indicates harm or ineffectiveness; and yellow signifies ‘measure’ because insufficient evidence exists to be certain about whether the child will benefit. Yellow can be assigned in three scenarios: (i) promising evidence (weak positive), (ii) unknown effectiveness because no research exists, or (iii) evidence suggests possibly no effect (weak negative).
Ethics and data
The study did not involve contact with humans, so the need for ethical approval was waived by the Cerebral Palsy Alliance's National Health and Medical Council Human Research Ethics Committee. This SR was not registered.
Results
3138 citations were identified using the search strategy, of which 129 articles met the inclusion criteria for review. Of the 129 included articles, 58% (n = 75/129) were SRs; 42% (n = 54/129) were RCTs. Note, more than 54 RCTs exist in the paediatric occupational therapy evidence base, but we treated any RCT that was cited within an included SR as a duplicate. Flow of information is presented in the PRISMA diagram (Fig. 1).
Figure 1.
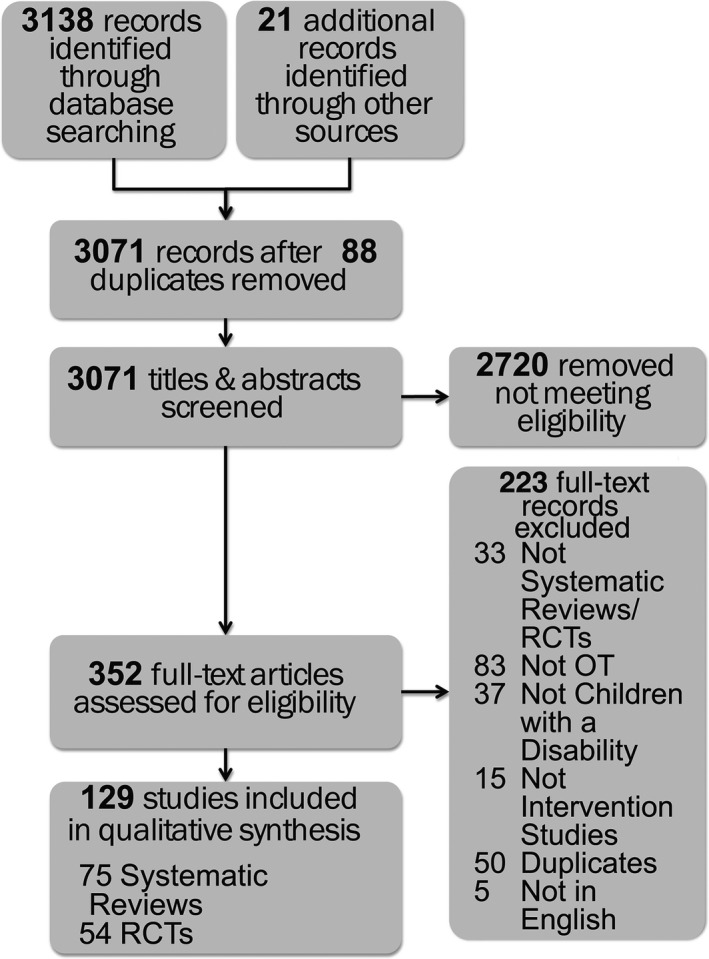
PRISMA Flow Diagram
The results are now presented using PICO question format headings.
Population (Participants)
Included studies were across the following childhood disability diagnoses: arthrogyposis; attention deficit hyperactivity disorder (ADHD); autism spectrum disorder (ASD); behaviour disorders; brachial plexus injury; brain injury (BI); burns; cerebral palsy (CP); cancer; chronic pain; developmental coordination disorder (DCD); developmental disability (DD); Down syndrome; foetal alcohol spectrum disorder; learning disability (LD); mental health; intellectual disability (ID); obesity; preterm infants; physical disability; rheumatoid arthritis; and spina bifida. Some studies included samples from a variety of the aforementioned diagnoses. Consistent with childhood disability population incidence data, more research existed about ASD (n = 32/135; 24%), ADHD (n = 8/135; 6%), CP (n = 38/135; 28%) and DCD (n = 9/135; 7%), than other conditions.
Paediatric occupational therapy involves working with the child, the parent and the family unit: The child was the primary client for 87% (n = 45/52) of the interventions, i.e. therapy focussed on improving the child outcomes (e.g. an orthotic worn by the child to improve hand function), whereas the parent was the primary client for 13% (n = 7/52) for the interventions (e.g. parent education, aiming to improve knowledge, skills and confidence).
Interventions
Included studies, researched the effectiveness of 52 occupational therapy intervention groups: (1) Acupuncture; (2) Assistive Devices; (3) Assistive Technology; (4) Behavioural Interventions including Applied Behavioural Analysis (ABA) and Positive Parenting Program (Triple P); (5) Bimanual Training; (6) Biofeedback; (7) Coaching; (8) Cognitive Interventions including CogFun, CogMed, (9) Cognitive Orientation to Occupational Performance (CO‐OP); (10) Conductive Education; (11) Constraint Induced Movement Therapy (CIMT); (12) CIMT &/or Bimanual; (13) Context Focused; (14) Ditto™ (hand held education & distraction device for burns patients); (15) Early Intervention, including a Developmental Approach, Neurodevelopmental Therapy (NDT) and Goals Activity and Motor Enrichment (GAME); (16) Electrical Stimulation (ES); (17) Family Centred Care; (18) Feeding Interventions; (19) Goal Directed Training, including Task Specific Training, Functional Training, Neuromotor Task Training (NTT) and Motor Imagery; (20) Handwriting Interventions; (21) Hippotherapy [Therapeutic Horse Riding]; (22) Home Programs; (23) Joint Attention; (24) Massage; (25) Meditation and/or Mindfulness; (26) Mental Health Interventions; (27) Neuro‐Developmental Therapy (NDT); (28) Occupational Therapy after BoNT; (29) Orthotics; (30) Pain Management; (31) Parent Counselling; (32) Parent Education/Parent Training; (33) Picture Exchange Communication System (PECS); (34) Play Therapy; (35) Positioning; (36) Pressure Care; (37) School Therapy; (38) Self‐Management; (39) Sensation Training; (40) Sensory Approach, including brushing, therapy balls, weighted vests, warm‐ups, sensory stimulation; (41) Sensory Integration, including sensory diets, swinging, brushing, therapy balls, weighted vests, body socks; (42) Skills Training via Mental Imagery; (43) Sleep Interventions; (44) Social Skills Training; (45) Stretching, including passive: self‐administered, therapist‐administered and device‐administered; (46) Treatment and Education of Autistic and Communication Handicapped Children (TEACCH); (47) Therapeutic Listening; (48) Treadmill Training; (49) Visual Motor Interventions; (50) Weight Loss; (51) Whole Body Vibration; and (52) Yoga.
Outcomes
Of the 12 included articles, authors measured the effectiveness of 52 occupational therapy interventions, across 22 diagnoses. From this, 136 intervention outcome indicators were identified, whereby an intervention, with an individual target outcome was administered to specific diagnostic groups. Insufficient data was available for analysis on one of these outcome indicators (number 74 in Table S1, where the SR authors found no publish data examining the effectiveness of hand orthotics in children with brain injury and therefore no recommendations could be made), (Jackman, Novak & Lannin, 2014) resulting in 135/136 intervention outcome indicators available for analysis.
Of the 135 intervention outcome indications: 30% (n = 40/135) were graded ‘do it’ (Green Go) (Arbesman, Bazyk & Nochajski, 2013; Bellows et al., 2011; Bleyenheuft, Arnould, Brandao, Bleyenheuft & Gordon, 2015; Brown, Kimble, Rodger, Ware & Cuttle, 2014; Chang & Yu, 2014; Chen, Pope, Tyler & Warren, 2014c; Chen et al., 2014b; Christmas, Sackley, Feltham & Cummins, 2018; Crompton et al., 2007; Estes et al., 2014; Fehlings et al., 2010; Frolek Clark & Schlabach, 2013; Hechler et al., 2014; Heinrichs, Kliem & Hahlweg, 2014; Hoare & Imms, 2004; Hoare, Imms, Carey & Wasiak, 2007; Hoare et al., 2010; Hoy, Egan & Feder, 2011; Huang, Fetters, Hale & McBride, 2009; Inguaggiato, Sgandurra, Perazza, Guzzetta & Cioni, 2013; Kamps et al., 2015; Kasari et al., 2016; Kaya Kara et al., 2015; Kurowski et al., 2014; Lannin, Scheinberg & Clark, 2006; Lidman, Nachemson, Peny‐Dahlstrand & Himmelmann, 2015; Lin & Wuang, 2012; Madlinger‐Lewis et al., 2014; Maeir et al., 2014; Novak, 2014a; Park, Maitra, Achon, Loyola & Rincón, 2014; Speth et al., 2015; Spittle, Orton, Anderson, Boyd & Doyle, 2012; Spittle, Orton, Doyle & Boyd, 2007; Stavness, 2006; Stickles Goods, Ishijima, Chang & Kasari, 2013; Vroland‐Nordstrand, Eliasson, Jacobsson, Johansson & Krumlinde‐Sundholm, 2016; Zwaigenbaum et al., 2015); 56% (75/135) were graded ‘probably do it’ (Yellow Measure) (Armstrong, 2012; Au et al., 2014; Auld, Russo, Moseley & Johnston, 2014; Bialocerkowski, Kurlowicz, Vladusic & Grimmer, 2005; Bodison & Parham, 2018; Cameron et al., 2017a, 2017b; Chacko et al., 2014; Chantry & Dunford, 2010; Chen, Lee & Howard, 2014a; Chiu, Ada & Lee, 2014; Cole, Harris, Eland & Mills, 1989; Copeland et al., 2014; Dagenais et al., 2009; De Vries, Beck, Stacey, Winslow & Meines, 2015; Duncan et al., 2012; Fedewa, Davis & Ahn, 2015; Grynszpan, Weiss, Perez‐Diaz & Gal, 2014; Hahn‐Markowitz, Berger, Manor & Maeir, 2017; Hammond, Jones, Hill, Green & Male, 2014; Huang et al., 2014; Jackman et al., 2018; James, Ziviani, Ware & Boyd, 2015; Janeslätt, Kottorp & Granlund, 2014; Jones et al., 2014; Krisanaprakornkit, Ngamjarus, Witoonchart & Piyavhatkul, 2010; Lannin, Novak & Cusick, 2007; Malow et al., 2014; Maskell, Newcombe, Martin & Kimble, 2014; Mast et al., 2014; Matute‐Llorente, González‐Agüero, Gómez‐Cabello, Vicente‐Rodríguez & Mallén, 2014; McLean et al., 2017; Meany‐Walen, Bratton & Kottman, 2014; Miller‐Kuhaneck & Watling, 2018; Montero & Gómez‐Conesa, 2014; Morgan, Novak, Dale & Badawi, 2015; Morgan et al., 2016a; Morgan, Novak, Dale, Guzzetta & Badawi, 2016b; Pfeiffer B & Arbesman, 2018; Polatajko & Cantin, 2010; Reeuwijk, van Schie, Becher & Kwakkel, 2006; Schaaf, Dumont, Arbesman & May‐Benson, 2018; Smith et al., 2014; Snider, Majnemer & Darsaklis, 2010; Storebø et al., 2011; Tatla et al., 2013; Tatla, Sauve, Jarus, Virji‐Babul & Holsti, 2014; Vargas & Lucker, 2016; Westendorp et al., 2014; Whalen & Case‐Smith, 2012; Xu, He, Mai, Yan & Chen, 2015; Zadnikar & Kastrin, 2011; Ziviani, Feeney, Rodger & Watter, 2010; Zwicker & Mayson, 2010); 10% (n = 14/130) were graded ‘probably don't do it’ (Yellow Measure) (Wallen & Gillies, 2006; Wells, Marquez & Wakely, 2018); and 4% (n = 6/135) were graded ‘don't do it’ (Red Stop) (Gringras et al., 2014; Katalinic et al., 2010).
The 40 green light ‘do it’ interventions indications included: (1) Behavioural Intervention using ABA for children with ASD; (2) Behavioural Intervention using Triple P for children behaviour disorders; (3) Behavioural Intervention using token economy contracts for children with a brain injury; (4) Bimanual Training for children with hemiplegic CP; (5) Coaching for parents of children at risk of disability to promote development; (6) Coaching for parents of children with ASD to promote function and behaviour; (7) CAPS cognitive intervention for children with brain injury to improve long term executive function; (8) Cog‐Fun intervention for children with attention deficit disorder to improve executive function; (9) CO‐OP for children with DCD for functional motor task performance; (10) CIMT for children with CP to improve hand function; (11) CIMT plus Bimanual for children with CP to improve hand function; (12) Context Focused intervention for children with CP for functional motor task performance; (13) Ditto hand held devices for children with burns to provide procedural distraction and self‐management education; (14) Early Intervention using ABA for children with ASD; (15) Early Intervention using Developmental Care for preterm infants; (16) Family Centred Care for children with brain injury or CP, to improve children's function; (17) Parent education feeding intervention for children with disability to improve feeding competency and growth; (18) Physiological feeding intervention for children with disability; (19) Goal Directed Training for children with CP, to improve functional task performance; (20) Goal Directed Training for children with DCD, to improve functional task performance; (21) Handwriting Task‐Specific Practice for children with DCD; (22) Home Programs for children with CP, to improve functional task performance; (23) Home Programs for children with ID, to improve functional task performance; (24) Joint Attention for children with ASD to improve social interactions; (25) Mental Health interventions for children with ASD; (26) Mental Health interventions for children with developmental delay; (27) Mental Health interventions for children with mental health disorders; (28) Occupational therapy after botulinum toxin injections for children with CP to promote hand function; (29) Kinesiotape for children with CP to improve hand function; (30) Pain Management for children with chronic pain secondary to physical disability and or chronic health conditions; (31) Parent Education using mindfulness for parents of children with ASD to reduce parental stress; (32) Parent Education using problem solving for parents of children with ASD to reduce parental stress; (33) Parent Education for children with disabilities to promote parenting confidence; (34) Parent Education for children with behaviour disorders to improve parent well‐being; (35) PECS for children with ASD to promote communication; (36) Positioning in NICU for preterm infants to promote normal movement development; (37) Pressure Care for children with CP using mattresses and cushions; (38) Social Skills Training mediated by peers for children with ASD; (39) Treadmill training for children with Down Syndrome to accelerate the onset of independent walking; (40) Weight loss using a family education and activity program called ‘Mighty Moves’ for children with obesity.
We assigned an ICF category to the primary and secondary intervention outcome of each intervention. Using the primary ICF level code, we mapped the profile of the paediatric OT evidence base to the ICF framework (Fig. 2). Green light effective interventions existed at the body structures and function ICF level (n = 14/74 indications (19%)), the activity level (n = 14/27 indications (52%)) and the environment level (n = 12/34 indications (35%)). When we compared the proportions of green light to yellow light to red light interventions by ICF levels, the activity level contained the largest number of green lights. At the activity level where there was 27 indications, green lights outweighed the number of yellow and red lights (Gree n = 14/27; Yellow = 13/27; Red = 0/27), meaning the most common traffic code at the activity level was green, which we illustrated by green shading in Figure 2. At the body structures and function ICF level, the most common traffic code was yellow, which we illustrated by yellow shading in Figure 2. All the red lights within the evidence base existed at the body structures and function level. At the environmental level, the most common traffic code was also yellow, which we illustrated by yellow shading in Figure 2. Two intervention's primary ICF code was at the participation level (Willis et al., 2010) and none at the personal level, indicating gaps in the occupational therapy evidence base, which we illustrated using grey shading in Figure 2. The two participation codes were weak positive, but these were based on trials that used activity‐based interventions and assumed an upstream participation gain, which was not well‐supported.
Figure 2.

Occupational Therapy Interventions and the International Classification of Function
Comparisons
In the included papers, consistent with conventional beliefs about it being unethical to withhold early intervention from children, rarely did researchers design studies where the control group received no intervention. In most studies, the controlled comparison was usual care. Some researchers carried out short duration studies using a wait‐list control design, where the control group received the experimental intervention after study completion.
CIMT for children with CP, was the only intervention comprehensively and empirically compared to other intervention options, using head‐to‐head RCT comparisons identified in our search strategy. CIMT was: (i) compared head‐to‐head with Bimanual Training showing no difference between the approaches (Sakzewski et al., 2015; Tervahauta, Girolami & Øberg, 2017); and (ii) combined with Bimanual Training and/or Botulinum toxin A, showing no additive benefits occurred from a combined intervention approach (Hoare et al., 2013). These researcher's concluded ‘intensity’ of practice was the key ingredient of these effective CP approaches (Sakzewski et al.; Tervahauta et al., 2017).
A meta‐analysis of intervention options for children with DCD compared the relative effect of DCD motor interventions by calculating and comparing effect sizes (Smits‐Engelsman et al., 2013). The authors calculated that ‘top‐down’ approaches (effect size = 0.89) were more effective than ‘bottom‐up’ approaches (effect size = 0.12).
To assist with comparative clinical decision‐making across the paediatric occupational therapy evidence base, we created bubble charts. We mapped the 52 identified paediatric occupational therapy interventions, across 22 diagnoses, spanning 135 intervention indications, which sought to provide analogous outcomes, by diagnosis, into separate bubbles. In the bubble charts, the size of the bubble indicated the volume of published evidence, which was calculated by counting the number of published studies on the topic. The location of the bubble on the y‐axis of the graph corresponded to the GRADE system rating. The colour of the bubble denoted the Traffic Light Evidence Alert System rating (Fig. 3).
Figure 3.
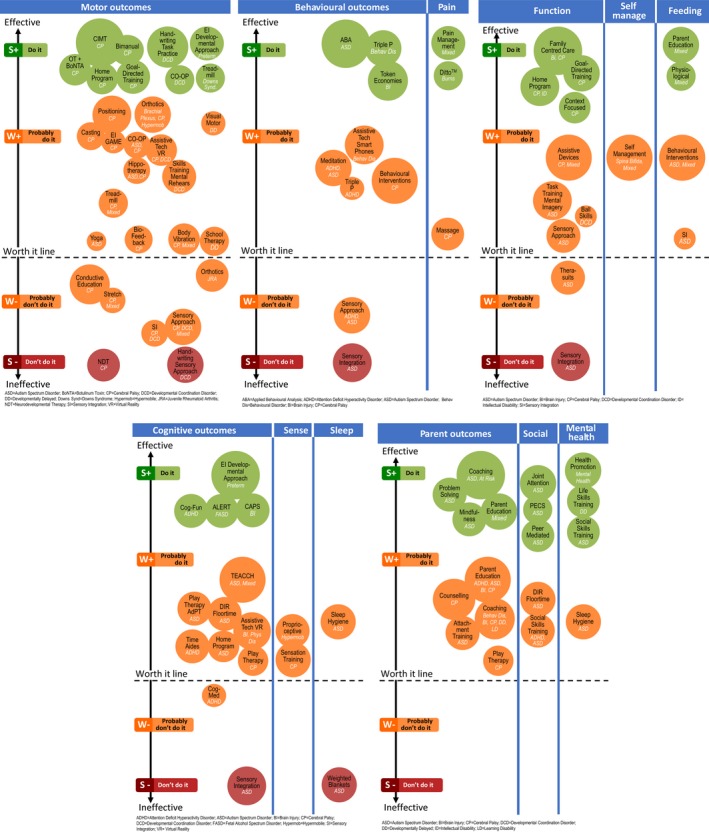
Bubble Charts Comparing the Effectiveness of Different Occupational Therapy Indications for Different Diagnoses
Discussion
We set out to systematically summarise the current intervention options available to paediatric occupational therapists across different childhood disability populations. We found 40 interventions that received a ‘strong’ recommendation for use, indicating a high‐quality evidence base with more benefits than harms. These ‘green light’ interventions included: Behavioural Interventions (including ABA, Triple P and Token Economies); Bimanual; Coaching; Cognitive Cog‐Fun and CAPS; CO‐OP; CIMT; CIMT plus Bimanual; Context‐Focused; Ditto; Early Intervention (including ABA and Developmental Care); Family Centred Care; Feeding interventions (including coaching and physiologic); Goal Directed Training; Handwriting Task‐Specific Practice; Home Programs; Joint Attention; Mental Health Interventions; occupational therapy after BoNT; Kinesiotape; Pain Management; Parent Education; PECS; Positioning in NICU; Pressure Care; Social Skills Training Peer Mediated; Treadmill training and Weight loss ‘Mighty Moves’.
The paediatric occupational therapy evidence base is under immense growth and expansion. The SRs and trials greater than 10 years old were predominantly about CP with one study about Brachial Plexus and DD. Almost always these older studies showed that the ‘bottom‐up’ interventions were ineffective with no difference between the experimental and control groups.
Clinical Implications
Occupational therapists working with children and their parents have several evidence based interventions to choose from. The strength of this paper is that it provides a systematic, clear and concise summary of all the available interventions by diagnosis with an easy to interpret summary of efficacy. There are some important learnings:
A. Parent partnership within occupational therapist intervention is effective and worthwhile
Occupational Therapists embrace the principles of family centred care (Hanna & Rodger, 2002) where the parent is the decision‐maker and the expert in knowing their child and the therapist is a technical resource to the family. We found that 13% of paediatric occupational therapy interventions are directed at the parent, so parents can deliver intervention at home within daily parenting. Evidence suggests that parent‐delivered intervention is equally effective to therapist‐delivered intervention (Baker et al., 2012), which is not surprising given parent's knowledge of their children's preferences and engagement style, and the volume of caregiving they carryout (Smith, Cheater & Bekker, 2015). In the diagnoses studied (ADHD, ASD, At risk, Behavioural Disorders, BI, CP, DD, LD, obesity), it was very clear that parents respond well to parent education and training (Antonini et al., 2014; Barlow, Smailagic, Huband, Roloff & Bennett, 2012; Case‐Smith & Arbesman, 2008; Dykens, Fisher, Taylor, Lambert & Miodrag, 2014; Feinberg et al., 2014; Hanna & Rodger, 2002; Howe & Wang, 2013; Kuhaneck, Madonna, Novak & Pearson, 2015; Lawler, Taylor & Shields, 2013; Tanner, Hand, O'toole & Lane, 2015; Zwi, Jones, Thorgaard, York & Dennis, 2011), consistent with family centred philosophy about parents’ aspirations of parenting well, to help their children (Hanna & Rodger, 2002). Moreover, parents and children carry out intervention effectively at home, and therefore home programs (Novak & Berry, 2014b; Novak et al., 2013; Sakzewski, Ziviani & Boyd, 2013; Sakzewski et al., 2015; Wuang, Ho & Su, 2013) and self‐management programs (Lindsay, Kingsnorth, Mcdougall & Keating, 2014; Moola, Faulkner, White & Kirsh, 2014) are an effective method for increasing the intensity of therapy.
When carrying out parent education, literature tells us that parents need and want: knowledge of the condition and intervention options; help accessing support services; and advice about coping strategies, via a collaborative partnership (Smith et al., 2015). Even though family centred practice has existed since the 1990s, parents still experience some resistance to their input from health professionals (Smith et al.). Unclear expectations about roles further elevate parental stress (Coyne, 2015). Occupational therapists therefore need to be mindful of parent's experiences and aim to clearly communicate information and coach parents to guide care, to optimise family outcomes (Coyne).
B. Activities‐based, ‘top‐down’ interventions deliver bigger gains
Numerous occupational therapy interventions exist, aiming to improve motor, behavioural and functional outcomes (Fig. 3), affording a lot of choice to families and clinicians. The greatest number of effective green light interventions was at the activity level of the ICF, indicating that daily life skills training using a ‘top‐down’ approach is a strength of the occupational therapy profession. Examples include: Bimanual Training; CIMT; CO‐OP; GAME; Goal‐Directed Training; Handwriting Task Training; Home Programs using Goal‐Directed Training; Social Skills Training; and Task Training. Consistent with current knowledge about the conditions for inducing neuroplasticity (Kleim & Jones, 2008), the green light, ‘top‐down’, activity level interventions all have the following key ingredients in common: (i) begin with the child's goal, to optimise motivation and saliency of practice; (ii) practice of real‐life activities in natural environments to optimise the child's learning and the variability of the practice; (iii) intense repetitions to activate plasticity, including home‐based practice; and (iv) scaffolded practice to the ‘just right challenge’ to enable success under self‐generated problem‐solving conditions, to optimise enjoyment.
In contrast, some of the most established paediatric occupational therapy interventions NDT/Bobath and SI were originally developed as ‘bottom‐up’ interventions. NDT/Bobath and SI originated in an era of medicine when intervention aimed to remediate the child's body structural deficits, thinking function would emerge (Rodger et al., 2005; Rodger et al., 2006). However, over time the NDT/Bobath and SI approaches have been broadened to also accommodate use of ‘top‐down’ functional training approaches. Fidelity to the original NDT/Bobath and SI approach therefore varies greatly (Mayston, 2016), and as such, a leading Bobath expert has recently stated that Bobath ‘no longer stands for a valid universal therapy approach’ (Mayston, 2016, p. 994). This means that interpreting the meaning of historical NDT/Bobath and SI research evidence about efficacy within the context of contemporaneous clinical practice is challenging. The efficacy of both NDT/Bobath and SI have been critiqued within SRs (Boyd & Hays, 2001; Brown & Burns, 2001; Case‐Smith & Arbesman, 2008; Case‐Smith, Clark & Schlabach, 2013; Case‐Smith, Weaver & Fristad, 2015; Lang et al., 2012; May‐Benson & Koomar, 2010; Novak et al., 2013; Sakzewski, Ziviani & Boyd, 2009; Sakzewski et al., 2013; Steultjens et al., 2004; Watling & Hauer, 2015; Weaver, 2015) and these data mostly relate to older trials. SR authors have concluded that NDT/Bobath and SI rarely confer motor gains superior to no intervention, but the RCTs contain so many methodological flaws that recommendations for use or discontinuation of use within practice cannot be made with certainty (Boyd & Hays, 2001; Brown & Burns, 2001; Case‐Smith & Arbesman, 2008; Case‐Smith et al., 2013; Case‐Smith et al., 2014; Lang et al., 2012; May‐Benson & Koomar, 2010; Novak et al., 2013; Sakzewski et al., 2009, 2013; Steultjens et al., 2004; Watling & Hauer, 2015; Weaver, 2015). Some therapists have interpreted the uncertainty of the NDT/Bobath and SI systematic evidence as justification of continuance, whereas others in the profession recommend discontinuance because of the growing body of ‘top‐down’ evidence that offer effective alternatives (Rodger et al., 2006). A Bobath expert has recommended that the common‐sense way forward for the profession is to choose interventions that promote activity and participation outcomes (Mayston, 2016) and to use consistent language to describe intervention options. For example, describing interventions by clear uniform terminology (i.e. ‘splitting’) might be more helpful than ‘clumping’ interventions into expanded NDT/Bobath umbrella terms.
We analysed the breakdown of the effectiveness of motor interventions, above and below the worth it line (Fig. 3), in terms of ‘bottom‐up’ vs. ‘top‐down’, and a trend favouring ‘top‐down’ emerged. Of the seven motor intervention indications below the ‘worth it line’, coded on GRADE as weak negative or strong negative (red), 7/7 (100%) were ‘bottom‐up’ approaches. Of the 22 motor intervention indications above the ‘worth it line’ eight were green and 14 were yellow: 8/8 (100%) green indications (strong positive) were ‘top‐down’. A similar trend emerged in the comparative effectiveness analysis of functional interventions. Of the seven functional intervention indications above the ‘worth it line’, coded on GRADE as strong positive (green), 4/4 (100%) were ‘top‐down’. There were a small number of studies using SI and the sensory approach to improve function coded on GRADE as weak positive, but the studies had a high risk of bias and SR authors recommended interpreting the positive results with caution (Case‐Smith et al., 2014; Case‐Smith et al., 2015; Watling & Hauer, 2015).
Research Implications
The following areas of the evidence‐base would benefit from more research: (i) Parent Education: None of the parent education approaches were ineffective. Thus, more research is worthwhile exploring parent's preferred learning styles and levels of support required to manage the stress of raising a child with a disability. There are potential financial gains to the health system by thoroughly understanding effective parent interventions, because parent‐delivered intervention is equally effective and less expensive; (ii) Head‐to‐head comparisons: Head‐to‐head comparisons of different interventions aiming to achieve the same outcomes, in well‐controlled trials with cost‐effectiveness data, would enable determinations about best practice to be made from good evidence, and thus inform parent and policy‐maker's decision‐making; (iii) ‘Dose’ comparison studies: ‘Dose’ comparison studies using well controlled intensity trials would enable occupational therapists to better inform parents about ‘how much’ intervention is enough; and (iv) Participation Interventions: There is a clear gap in the evidence‐base about interventions that directly improve a child's participation in life and should be the focus of future RCTs and other rigorous methodologies. CIMT, Bimanual and Home Program occupational therapy interventions were measured to confirm whether or not they conferred participation gains, and the clinical trials demonstrated no between group differences (Adair, Ullenhag, Keen, Granlund & Imms, 2015). These results indicate that there is a clear need to develop interventions that specifically target participation, rather than anticipating activities‐based interventions will confer upstream participation gains. Changes in participation are multifactorial and involve individual factors, contextual factors, the nature of the participation activity and the environment in which the activity is being performed (Imms et al., 2017). Any new participation intervention invented, will need to address all of these factors to be successful.
Limitations
Our review has several limitations. First, we only included SRs and RCTs because we aimed to analyse best‐available evidence, but means some intervention approaches will have been excluded and overlooked because no trials or reviews existed. Second, this was an analysis of secondary data sources and reporting bias and publication bias may be in operation, because positive findings have a higher chance of being published. This evidence may exist suggesting some interventions are ineffective which we were unable to review. Third, our search terms included ‘occupational therapy’ and thus will have excluded other effective interventions used by occupational therapists, but not invented or published by occupational therapists e.g. ‘Triple P’ for children with CP. Fourth, our paper was designed to provide an overview for clinicians indicating which interventions are effective, however, it does not provide enough detail about any one intervention to guide administration or training in any specific intervention. Clinicians need to refer directly to the cited article and more widely in the published literature for this information. Our findings must be interpreted within the context of our study limitations.
Conclusions
This review provides a high‐level summary of effective paediatric occupational therapy interventions. Thirty‐nine effective intervention indications exist, offering both families and clinicians many choices to match their preferences and expertise. The paediatric occupational therapy evidence base suggests a growing trend towards activities‐level, ‘top‐down’ approaches and parent education, over and above ‘bottom‐up’ approaches. There are important ethical implications of translating these effective evidence‐based occupational therapy intervention options into clinical practice to give children the best chance at achieving their goals.
Key points for occupational therapy
Collaboration with parents is effective and worthwhile.
Activities‐based, top‐down interventions confer larger clinical gains, than bottom‐up approaches, when aiming to improve a child's function.
Authorship
All authors declare that this is original work and that they meet the criteria for authorship. Iona Novak designed the study, extracted the data, conducted the analyses and wrote the manuscript. Ingrid Honan conducted the analyses and wrote the manuscript. All authors read and approved the final manuscript.
Funding
The study was unfunded and there are no competing financial disclosures.
Conflict of interest
The authors have no conflicts of interest to disclose.
Supporting information
Table S1. Main results table.
Conflict of interest
The authors have no conflicts of interest to disclose.
References
- Adair, B. , Ullenhag, A. , Keen, D. , Granlund, M. & Imms, C. (2015). The effect of interventions aimed at improving participation outcomes for children with disabilities: A systematic review. Developmental Medicine & Child Neurology, 57 (12), 1093–1104. 10.1111/dmcn.12809. [DOI] [PubMed] [Google Scholar]
- Antonini, T. N. , Raj, S. P. , Oberjohn, K. S. , Cassedy, A. , Makoroff, K. L. , Fouladi, M. et al (2014). A pilot randomized trial of an online parenting skills program for pediatric traumatic brain injury: Improvements in parenting and child behavior. Behavior Therapy, 45 (4), 455–468. 10.1016/j.beth.2014.02.003. [DOI] [PubMed] [Google Scholar]
- Arbesman, M. , Bazyk, S. & Nochajski, S. M. (2013). Systematic review of occupational therapy and mental health promotion, prevention, and intervention for children and youth. American Journal of Occupational Therapy, 67 (6), e120–e130. 10.5014/ajot.2013.008359. [DOI] [PubMed] [Google Scholar]
- Armstrong, D. (2012). Examining the evidence for interventions with children with developmental coordination disorder. British Journal of Occupational Therapy, 75 (12), 532–540. 10.4276/030802212X13548955545413. [DOI] [Google Scholar]
- Au, A. , Lau, K. M. , Wong, A. H. C. , Lam, C. , Leung, C. , Lau, J. et al (2014). The efficacy of a group Triple P (Positive Parenting Program) for Chinese parents with a child diagnosed with ADHD in Hong Kong: A pilot randomised controlled study. Australian Psychologist, 49 (3), 151–162. 10.1111/ap.12053. [DOI] [Google Scholar]
- Auld, M. L. , Russo, R. , Moseley, G. L. & Johnston, L. M. (2014). Determination of interventions for upper extremity tactile impairment in children with cerebral palsy: A systematic review. Developmental Medicine & Child Neurology, 56 (9), 815–832. 10.1111/dmcn.12439. [DOI] [PubMed] [Google Scholar]
- Baker, T. , Haines, S. , Yost, J. , DiClaudio, S. , Braun, C. & Holt, S. (2012). The role of family‐centered therapy when used with physical or occupational therapy in children with congenital or acquired disorders. Physical Therapy Reviews, 17 (1), 29–36. 10.1179/1743288X11Y.0000000049. [DOI] [Google Scholar]
- Barlow, J. , Smailagic, N. , Huband, N. , Roloff, V. & Bennett, C . (2012). Group‐based parent training programmes for improving parental psychosocial health. Cochrane Database of Systematic Reviews, 6, CD002020 10.1002/14651858.cd002020.pub4 [DOI] [PubMed] [Google Scholar]
- Bellows, L. , Silvernail, S. , Caldwell, L. , Bryant, A. , Kennedy, C. , Davies, P. et al (2011). Parental perception on the efficacy of a physical activity program for preschoolers. Journal of Community Health, 36 (2), 231–237. 10.1007/s10900-010-9302-1. [DOI] [PubMed] [Google Scholar]
- Bialocerkowski, A. , Kurlowicz, K. , Vladusic, S. & Grimmer, K. (2005). Effectiveness of primary conservative management for infants with obstetric brachial plexus palsy. International Journal of Evidence‐Based Healthcare, 3 (2), 27–44. 10.1111/j.1479-6988.2005.00020.x. [DOI] [PubMed] [Google Scholar]
- Bleyenheuft, Y. , Arnould, C. , Brandao, M. B. , Bleyenheuft, C. & Gordon, A. M. (2015). Hand and Arm Bimanual Intensive Therapy Including Lower Extremity (HABIT‐ILE) in children with unilateral spastic cerebral palsy: A randomized trial. Neurorehabilitation and Neural Repair, 29 (7), 645–657. 10.1177/1545968314562109. [DOI] [PubMed] [Google Scholar]
- Bodison, S. C. & Parham, L. D. (2018). Specific sensory techniques and sensory environmental modifications for children and youth with sensory integration difficulties: A systematic review. American Journal of Occupational Therapy, 72 (1), 7201190040p1–7201190040p11. 10.5014/ajot.2018.029413 [DOI] [PubMed] [Google Scholar]
- Bonnechere, B. , Jansen, B. , Omelina, L. , Degelaen, M. , Wermenbol, V. , Rooze, M. et al (2014). Can serious games be incorporated with conventional treatment of children with cerebral palsy? A review. Research in Developmental Disabilities, 35 (8), 1899–1913. 10.1016/j.ridd.2014.04.016. [DOI] [PubMed] [Google Scholar]
- Boyd, R. N. & Hays, R. M. (2001). Current evidence for the use of botulinum toxin type A in the management of children with cerebral palsy: A systematic review. European Journal of Neurology, 8, 1–20. 10.1046/j.1468-1331.2001.00034.x. [DOI] [PubMed] [Google Scholar]
- Brown, G. T. & Burns, S. A. (2001). The efficacy of neurodevelopmental treatment in paediatrics: A systematic review. British Journal of Occupational Therapy, 64 (5), 235–244. 10.1177/030802260106400505. [DOI] [Google Scholar]
- Brown, N. J. , Kimble, R. M. , Rodger, S. , Ware, R. S. & Cuttle, L. (2014). Play and heal: Randomized controlled trial of Ditto™ intervention efficacy on improving re‐epithelialization in pediatric burns. Burns, 40 (2), 204–213. 10.1016/j.burns.2013.11.024. [DOI] [PubMed] [Google Scholar]
- Cameron, D. , Craig, T. , Edwards, B. , Missiuna, C. , Schwellnus, H. & Polatajko, H. J. (2017). Cognitive Orientation to daily Occupational Performance (CO‐OP): A new approach for children with cerebral palsy. Physical & Occupational Therapy in Pediatrics, 37 (2), 183–198. 10.1080/01942638.2016.1185500. [DOI] [PubMed] [Google Scholar]
- Campbell, L. , Novak, I. , McIntyre, S. & Lord, S. (2013). A KT intervention including the evidence alert system to improve clinician's evidence‐based practice behavior—A cluster randomized controlled trial. Implementation Science, 8 (1), 132 10.1186/1748-5908-8-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case‐Smith, J. & Arbesman, M. (2008). Evidence‐based review of interventions for autism used in or of relevance to occupational therapy. The American Journal of Occupational Therapy, 62 (4), 416 10.5014/ajot.62.4.416. [DOI] [PubMed] [Google Scholar]
- Case‐Smith, J. , Clark, G. J. F. & Schlabach, T. L. (2013). Systematic review of interventions used in occupational therapy to promote motor performance for children ages birth–5 years. American Journal of Occupational Therapy, 67 (4), 413–424. 10.5014/ajot.2013.005959. [DOI] [PubMed] [Google Scholar]
- Case‐Smith, J. , Weaver, L. L. & Fristad, M. A. (2015). A systematic review of sensory processing interventions for children with autism spectrum disorders. Autism, 19 (2), 133–148. https://doi.org/10.1177%2F1362361313517762. [DOI] [PubMed] [Google Scholar]
- Chacko, A. , Bedard, A. C. , Marks, D. J. , Feirsen, N. , Uderman, J. Z. , Chimiklis, A. et al (2014). A randomized clinical trial of Cogmed Working Memory Training in school‐age children with ADHD: A replication in a diverse sample using a control condition. Journal of Child Psychology and Psychiatry, 55 (3), 247–255. 10.1111/jcpp.12146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang, S. H. & Yu, N. Y. (2014). The effect of computer‐assisted therapeutic practice for children with handwriting deficit: A comparison with the effect of the traditional sensorimotor approach. Research in Developmental Disabilities, 35 (7), 1648–1657. 10.1016/j.ridd.2014.03.024. [DOI] [PubMed] [Google Scholar]
- Chantry, J. & Dunford, C. (2010). How do computer assistive technologies enhance participation in childhood occupations for children with multiple and complex disabilities? A review of the current literature. British Journal of Occupational Therapy, 73 (8), 351–365. https://doi.org/10.4276%2F030802210X12813483277107 [Google Scholar]
- Chen, Y. P. , Lee, S. Y. & Howard, A. M. (2014a). Effect of virtual reality on upper extremity function in children with cerebral palsy: A meta‐analysis. Pediatric Physical Therapy, 26 (3), 289–300. 10.1097/PEP.0000000000000046. [DOI] [PubMed] [Google Scholar]
- Chen, H. C. , Chen, C. L. , Kang, L. J. , Wu, C. Y. , Chen, F. C. & Hong, W. H. (2014b). Improvement of upper extremity motor control and function after home‐based constraint induced therapy in children with unilateral cerebral palsy: Immediate and long‐term effects. Archives of Physical Medicine and Rehabilitation, 95 (8), 1423–1432. 10.1016/j.apmr.2014.03.025. [DOI] [PubMed] [Google Scholar]
- Chen, Y. P. , Pope, S. , Tyler, D. & Warren, G. L. (2014c). Effectiveness of constraint‐induced movement therapy on upper‐extremity function in children with cerebral palsy: A systematic review and meta‐analysis of randomized controlled trials. Clinical Rehabilitation, 28(10), 939–953. https://doi.org/10.1177%2F0269215514544982 [DOI] [PubMed] [Google Scholar]
- Chiu, H. C. , Ada, L. & Lee, H. M. (2014). Upper limb training using Wii Sports Resort™ for children with hemiplegic cerebral palsy: A randomized, single‐blind trial. Clinical Rehabilitation, 28(10), 1015–1024. https://doi.org/10.1177%2F0269215514533709 [DOI] [PubMed] [Google Scholar]
- Christmas, P. M. , Sackley, C. , Feltham, M. G. & Cummins, C. (2018). A randomized controlled trial to compare two methods of constraint‐induced movement therapy to improve functional ability in the affected upper limb in pre‐school children with hemiplegic cerebral palsy: CATCH TRIAL. Clinical Rehabilitation, 32(7), 909–918. https://doi.org/10.1177%2F0269215518763512 [DOI] [PubMed] [Google Scholar]
- Cole, K. N. , Harris, S. R. , Eland, S. F. & Mills, P. E. (1989). Comparison of two service delivery models: In‐class and out‐of‐class therapy approaches. Pediatric Physical Therapy, 1 (2), 49–54. [Google Scholar]
- Copeland, L. , Edwards, P. , Thorley, M. , Donaghey, S. , Gascoigne‐Pees, L. , Kentish, M. et al (2014). Botulinum toxin A for nonambulatory children with cerebral palsy: A double blind randomized controlled trial. The Journal of Pediatrics, 165 (1), 140–146. 10.1016/j.jpeds.2014.01.050 [DOI] [PubMed] [Google Scholar]
- Coyne, I. (2015). Families and health‐care professionals’ perspectives and expectations of family‐centred care: Hidden expectations and unclear roles. Health Expectations, 18 (5), 796–808. 10.1111/hex.12104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crompton, J. , Imms, C. , McCoy, A. T. , Randall, M. , Eldridge, B. , Scoullar, B. et al (2007). Group‐based task‐related training for children with cerebral palsy: A pilot study. Physical & Occupational Therapy in Pediatrics, 27 (4), 43–65. 10.1080/J006v27n04_04. [DOI] [PubMed] [Google Scholar]
- Dagenais, L. M. , Lahay, E. R. , Stueck, K. A. , White, E. , Williams, L. & Harris, S. R. (2009). Effects of electrical stimulation, exercise training and motor skills training on strength of children with meningomyelocele: A systematic review. Physical & Occupational Therapy in Pediatrics, 29 (4), 445–463. 10.3109/01942630903246018. [DOI] [PubMed] [Google Scholar]
- De Vries, D. , Beck, T. , Stacey, B. , Winslow, K. & Meines, K. (2015). Music as a therapeutic intervention with autism: A systematic review of the literature. Therapeutic Recreation Journal, 49 (3), 220. [Google Scholar]
- Duncan, B. , Shen, K. , Zou, L. P. , Han, T. L. , Lu, Z. L. , Zheng, H. et al (2012). Evaluating intense rehabilitative therapies with and without acupuncture for children with cerebral palsy: A randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 93 (5), 808–815. 10.1016/j.apmr.2011.12.009. [DOI] [PubMed] [Google Scholar]
- Dykens, E. M. , Fisher, M. H. , Taylor, J. L. , Lambert, W. & Miodrag, N. (2014). Reducing distress in mothers of children with autism and other disabilities: A randomized trial. Pediatrics, 134, e454–e463. 10.1542/peds.2013-3164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes, A. , Vismara, L. , Mercado, C. , Fitzpatrick, A. , Elder, L. , Greenson, J. et al (2014). The impact of parent‐delivered intervention on parents of very young children with autism. Journal of Autism and Developmental Disorders, 44 (2), 353–365. 10.1007/s10803-013-1874-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fedewa, A. , Davis, M. A. & Ahn, S. (2015). Effects of stability balls on children's on‐task behavior, academic achievement, and discipline referrals: A randomized controlled trial. American Journal of Occupational Therapy, 69, 6902220020p1–p9. 10.5014/ajot.2015.014829 [DOI] [PubMed] [Google Scholar]
- Fehlings, D. , Novak, I. , Berweck, S. , Hoare, B. , Stott, N. S. & Russo, R. N. (2010). Botulinum toxin assessment, intervention and follow‐up for paediatric upper limb hypertonicity: International consensus statement. European Journal of Neurology, 17, 38–56. 10.1111/j.1468-1331.2010.03127.x. [DOI] [PubMed] [Google Scholar]
- Feinberg, E. , Augustyn, M. , Fitzgerald, E. , Sandler, J. , Suarez, Z. F. C. , Chen, N. et al (2014). Improving maternal mental health after a child's diagnosis of autism spectrum disorder: Results from a randomized clinical trial. JAMA Pediatrics, 168 (1), 40–46. 10.1001/jamapediatrics.2013.3445. [DOI] [PubMed] [Google Scholar]
- Flores‐Mateo, G. & Argimon, J. M. (2007). Evidence based practice in postgraduate healthcare education: A systematic review. BMC Health Services Research, 7 (1), 119 10.1186/1472-6963-7-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frolek Clark, G. J. & Schlabach, T. L. (2013). Systematic review of occupational therapy interventions to improve cognitive development in children ages birth–5 years. American Journal of Occupational Therapy, 67 (4), 425–430. 10.1186/1472-6963-7-119. [DOI] [PubMed] [Google Scholar]
- Gringras, P. , Green, D. , Wright, B. , Rush, C. , Sparrowhawk, M. , Pratt, K. et al (2014). Weighted blankets and sleep in autistic children—A randomized controlled trial. Pediatrics, 134, 298–306. 10.1542/peds.2013-4285. [DOI] [PubMed] [Google Scholar]
- Grynszpan, O. , Weiss, P. L. , Perez‐Diaz, F. & Gal, E. (2014). Innovative technology‐based interventions for autism spectrum disorders: A meta‐analysis. Autism, 18(4), 346–361. https://doi.org/10.1177%2F1362361313476767 [DOI] [PubMed] [Google Scholar]
- Guyatt, G. H. , Oxman, A. D. , Vist, G. E. , Kunz, R. , Falck‐Ytter, Y. , Alonso‐Coello, P. et al (2008). GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ, 336, 924–926. 10.1136/bmj.39489.470347.ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn‐Markowitz, J. , Berger, I. , Manor, I. & Maeir, A. (2017). Impact of the Cognitive–Functional (Cog–Fun) intervention on executive functions and participation among children with attention deficit hyperactivity disorder: A randomized controlled trial. American Journal of Occupational Therapy, 71(5), 7105220010p1–9. 10.5014/ajot.2017.022053 [DOI] [PubMed] [Google Scholar]
- Hammond, J. , Jones, V. , Hill, E. L. , Green, D. & Male, I. (2014). An investigation of the impact of regular use of the WiiFit to improve motor and psychosocial outcomes in children with movement difficulties: A pilot study. Child: Care, Health and Development, 40(2), 165–175. 10.1111/cch.12029 [DOI] [PubMed] [Google Scholar]
- Hanna, K. & Rodger, S. (2002). Towards family‐centred practice in paediatric occupational therapy: A review of the literature on parent–therapist collaboration. Australian Occupational Therapy Journal, 49 (1), 14–24. 10.1046/j.0045-0766.2001.00273.x. [DOI] [Google Scholar]
- Hechler, T. , Ruhe, A. K. , Schmidt, P. , Hirsch, J. , Wager, J. , Dobe, M. et al (2014). Inpatient‐based intensive interdisciplinary pain treatment for highly impaired children with severe chronic pain: Randomized controlled trial of efficacy and economic effects. Pain, 155, 118–128. 10.1016/j.pain.2013.09.015. [DOI] [PubMed] [Google Scholar]
- Heinrichs, N. , Kliem, S. & Hahlweg, K. (2014). Four‐year follow‐up of a randomized controlled trial of Triple P group for parent and child outcomes. Prevention Science, 15 (2), 233–245. 10.1007/s11121-012-0358-2. [DOI] [PubMed] [Google Scholar]
- Higgins J. & Green S. (Eds.). (2011). Cochrane handbook for systematic reviews of interventions. 5th ed West Sussex: John Wiley & Sons Ltd. [Google Scholar]
- Hoare, B. J. & Imms, C. (2004). Upper‐limb injections of botulinum toxin‐A in children with cerebral palsy: A critical review of the literature and clinical implications for occupational therapists. American Journal of Occupational Therapy, 58 (4), 389–397. 10.5014/ajot.58.4.389. [DOI] [PubMed] [Google Scholar]
- Hoare, B. , Imms, C. , Carey, L. & Wasiak, J. (2007). Constraint‐induced movement therapy in the treatment of the upper limb in children with hemiplegic cerebral palsy: A Cochrane systematic review. Clinical Rehabilitation, 21 (8), 675–685. 10.1002/14651858.cd004149.pub2. [DOI] [PubMed] [Google Scholar]
- Hoare, B. , Imms, C. , Villanueva, E. , Rawicki, H. B. , Matyas, T. & Carey, L. (2013). Intensive therapy following upper limb botulinum toxin A injection in young children with unilateral cerebral palsy: A randomized trial. Developmental Medicine & Child Neurology, 55 (3), 238–247. 10.1111/dmcn.12054. [DOI] [PubMed] [Google Scholar]
- Hoare, B. J. , Wallen, M. A. , Imms, C. , Villanueva, E. , Rawicki, H. B. & Carey, L. (2010). Botulinum toxin A as an adjunct to treatment in the management of the upper limb in children with spastic cerebral palsy (UPDATE). Cochrane Database of Systematic Reviews, 1, CD003469 10.1002/14651858.cd003469.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe, T. H. & Wang, T. N. (2013). Systematic review of interventions used in or relevant to occupational therapy for children with feeding difficulties ages birth–5 years. American Journal of Occupational Therapy, 67 (4), 405–412. 10.5014/ajot.2013.004564. [DOI] [PubMed] [Google Scholar]
- Hoy, M. M. , Egan, M. Y. & Feder, K. P. (2011). A systematic review of interventions to improve handwriting. Canadian Journal of Occupational Therapy, 78 (1), 13–25. 10.2182/cjot.2011.78.1.3. [DOI] [PubMed] [Google Scholar]
- Huang, H. H. , Fetters, L. , Hale, J. & McBride, A. (2009). Bound for success: A systematic review of constraint‐induced movement therapy in children with cerebral palsy supports improved arm and hand use. Physical Therapy, 89 (11), 1126–1141. 10.2522/ptj.20080111. [DOI] [PubMed] [Google Scholar]
- Huang, J. S. , Dillon, L. , Terrones, L. , Schubert, L. , Roberts, W. , Finklestein, J. et al (2014). Fit4Life: A weight loss intervention for children who have survived childhood leukemia. Pediatric Blood & Cancer, 61 (5), 894–900. 10.1002/pbc.24937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imms, C. , Granlund, M. , Wilson, P. H. , Steenbergen, B. , Rosenbaum, P. L. & Gordon, A. M. (2017). Participation, both a means and an end: A conceptual analysis of processes and outcomes in childhood disability. Developmental Medicine & Child Neurology, 59, 16–25. 10.1111/dmcn.13237. [DOI] [PubMed] [Google Scholar]
- Inguaggiato, E. , Sgandurra, G. , Perazza, S. , Guzzetta, A. & Cioni, G. (2013). Brain reorganization following intervention in children with congenital hemiplegia: A systematic review. Neural Plasticity. 10.1155/2013/356275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackman, M. , Novak, I. & Lannin, N. (2014). Effectiveness of hand splints in children with cerebral palsy: A systematic review with meta‐analysis. Developmental Medicine & Child Neurology, 56 (2), 138–147. 10.1111/dmcn.12205. [DOI] [PubMed] [Google Scholar]
- Jackman, M. , Novak, I. , Lannin, N. , Froude, E. , Miller, L. & Galea, C. (2018). Effectiveness of Cognitive Orientation to daily Occupational Performance over and above functional hand splints for children with cerebral palsy or brain injury: A randomized controlled trial. BMC Pediatrics, 18 (1), 248 10.1186/s12887-018-1213-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James, S. , Ziviani, J. , Ware, R. S. & Boyd, R. N. (2015). Randomized controlled trial of web‐based multimodal therapy for unilateral cerebral palsy to improve occupational performance. Developmental Medicine & Child Neurology, 57 (6), 530–538. 10.1111/dmcn.12705. [DOI] [PubMed] [Google Scholar]
- Janeslätt, G. , Kottorp, A. & Granlund, M. (2014). Evaluating intervention using time aids in children with disabilities. Scandinavian Journal of Occupational Therapy, 21 (3), 181–190. 10.3109/11038128.2013.870225. [DOI] [PubMed] [Google Scholar]
- Jones, D. J. , Forehand, R. , Cuellar, J. , Parent, J. , Honeycutt, A. , Khavjou, O. et al (2014). Technology‐enhanced program for child disruptive behavior disorders: Development and pilot randomized control trial. Journal of Clinical Child & Adolescent Psychology, 43 (1), 88–101. 10.1080/15374416.2013.822308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamps, D. , Thiemann‐Bourque, K. , Heitzman‐Powell, L. , Schwartz, I. , Rosenberg, N. , Mason, R. et al (2015). A comprehensive peer network intervention to improve social communication of children with autism spectrum disorders: A randomized trial in kindergarten and first grade. Journal of Autism and Developmental Disorders, 45 (6), 1809–1824. 10.1007/s10803-014-2340-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasari, C. , Dean, M. , Kretzmann, M. , Shih, W. , Orlich, F. , Whitney, R. et al (2016). Children with autism spectrum disorder and social skills groups at school: A randomized trial comparing intervention approach and peer composition. Journal of Child Psychology and Psychiatry, 57 (2), 171–179. 10.1111/jcpp.12460. [DOI] [PubMed] [Google Scholar]
- Katalinic, O. M. , Harvey, L. A. , Herbert, R. D. , Moseley, A. M. , Lannin, N. A. & Schurr, K. (2010). Stretch for the treatment and prevention of contractures. Cochrane Database of Systematic Reviews, 9(9). 10.1002/14651858.cd007455.pub2 [DOI] [PubMed] [Google Scholar]
- Kaya Kara, O. , Atasavun Uysal, S. , Turker, D. , Karayazgan, S. , Gunel, M. K. & Baltaci, G. (2015). The effects of Kinesio Taping on body functions and activity in unilateral spastic cerebral palsy: a single‐blind randomized controlled trial. Developmental Medicine & Child Neurology, 57 (1), 81–88. 10.1111/dmcn.12583. [DOI] [PubMed] [Google Scholar]
- Kleim, J. A. & Jones, T. A. (2008). Principles of experience‐dependent neural plasticity: Implications for rehabilitation after brain damage. Journal of Speech, Language, and Hearing Research, 51 (1), S225–S239. 10.1044/1092-4388(2008/018). [DOI] [PubMed] [Google Scholar]
- Krisanaprakornkit, T. , Ngamjarus, C. , Witoonchart, C. & Piyavhatkul, N. (2010). Meditation therapies for attention‐deficit/hyperactivity disorder (ADHD). Cochrane Database of Systematic Reviews, 6, CD006507 10.1002/14651858.cd006507.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhaneck, H. M. , Madonna, S. , Novak, A. & Pearson, E . (2015). Effectiveness of interventions for children with autism spectrum disorder and their parents: A systematic review of family outcomes. American Journal of Occupational Therapy, 69(5), 6905180040p1–6905180040p14. 10.5014/ajot.2015.017855 [DOI] [PubMed] [Google Scholar]
- Kurowski, B. G. , Wade, S. L. , Kirkwood, M. W. , Brown, T. M. , Stancin, T. & Taylor, H. G. (2014). Long‐term benefits of an early online problem‐solving intervention for executive dysfunction after traumatic brain injury in children: A randomized clinical trial. JAMA Pediatrics, 168 (6), 523–531. 10.1001/jamapediatrics.2013.5070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang, R. , O'Reilly, M. , Healy, O. , Rispoli, M. , Lydon, H. , Streusand, W. et al (2012). Sensory integration therapy for autism spectrum disorders: A systematic review. Research in Autism Spectrum Disorders, 6 (3), 1004–1018. 10.1016/j.rasd.2012.01.006. [DOI] [Google Scholar]
- Lannin, N. , Scheinberg, A. & Clark, K. (2006). AACPDM systematic review of the effectiveness of therapy for children with cerebral palsy after botulinum toxin A injections. Developmental Medicine and Child Neurology, 48 (6), 533–539. 10.1111/j.1469-8749.2006.tb01309.x. [DOI] [PubMed] [Google Scholar]
- Lannin, N. A. , Novak, I. & Cusick, A. (2007). A systematic review of upper extremity casting for children and adults with central nervous system motor disorders. Clinical Rehabilitation, 21 (11), 963–976. 10.1177/0269215507079141. [DOI] [PubMed] [Google Scholar]
- Lawler, K. , Taylor, N. F. & Shields, N. (2013). Outcomes after caregiver‐provided speech and language or other allied health therapy: A systematic review. Archives of Physical Medicine and Rehabilitation, 94 (6), 1139–1160. 10.1016/j.apmr.2012.11.022. [DOI] [PubMed] [Google Scholar]
- Lidman, G. , Nachemson, A. , Peny‐Dahlstrand, M. & Himmelmann, K. (2015). Botulinum toxin A injections and occupational therapy in children with unilateral spastic cerebral palsy: a randomized controlled trial. Developmental Medicine & Child Neurology, 57 (8), 754–761. 10.1111/dmcn.12739. [DOI] [PubMed] [Google Scholar]
- Lin, H. C. & Wuang, Y. P. (2012). Strength and agility training in adolescents with Down syndrome: A randomized controlled trial. Research in Developmental Disabilities, 33 (6), 2236–2244. 10.1016/j.ridd.2012.06.017. [DOI] [PubMed] [Google Scholar]
- Lindsay, S. , Kingsnorth, S. , Mcdougall, C. & Keating, H. (2014). A systematic review of self‐management interventions for children and youth with physical disabilities. Disability and Rehabilitation, 36 (4), 276–288. 10.3109/09638288.2013.785605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madlinger‐Lewis, L. , Reynolds, L. , Zarem, C. , Crapnell, T. , Inder, T. & Pineda, R. (2014). The effects of alternative positioning on preterm infants in the neonatal intensive care unit: A randomized clinical trial. Research in Developmental Disabilities, 35 (2), 490–497. 10.1016/j.ridd.2013.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeir, A. , Fisher, O. , Bar‐Ilan, R. T. , Boas, N. , Berger, I. & Landau, Y. E. (2014). Effectiveness of Cognitive‐Functional (Cog–Fun) occupational therapy intervention for young children with attention deficit hyperactivity disorder: A controlled study. American Journal of Occupational Therapy, 68 (3), 260–267. 10.5014/ajot.2014.011700. [DOI] [PubMed] [Google Scholar]
- Malow, B. A. , Adkins, K. W. , Reynolds, A. , Weiss, S. K. , Loh, A. , Fawkes, D. et al (2014). Parent‐based sleep education for children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 44 (1), 216–228. 10.1007/s10803-013-1866-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandich, A. & Rodger, S. (2006). Doing, being and becoming: their importance for children. Occupational therapy with children: understanding children's occupations and enabling participation. Oxford, UK: Blackwell Publishing Ltd, 123–125. [Google Scholar]
- Maskell, J. , Newcombe, P. , Martin, G. & Kimble, R. (2014). Psychological and psychosocial functioning of children with burn scarring using cosmetic camouflage: A multi‐centre prospective randomised controlled trial. Burns, 40 (1), 135–149. 10.1016/j.burns.2013.04.025. [DOI] [PubMed] [Google Scholar]
- Mast, J. E. , Antonini, T. N. , Raj, S. P. , Oberjohn, K. S. , Cassedy, A. , Makoroff, K. L. et al (2014). Web‐based parenting skills to reduce behavior problems following abusive head trauma: A pilot study. Child Abuse & Neglect, 38 (9), 1487–1495. 10.1016/j.chiabu.2014.04.012. [DOI] [PubMed] [Google Scholar]
- Matute‐Llorente, Á. , González‐Agüero, A. , Gómez‐Cabello, A. , Vicente‐Rodríguez, G. & Mallén, J. A. C. (2014). Effect of whole‐body vibration therapy on health‐related physical fitness in children and adolescents with disabilities: A systematic review. Journal of Adolescent Health, 54 (4), 385–396. 10.1016/j.jadohealth.2013.11.001. [DOI] [PubMed] [Google Scholar]
- May‐Benson, T. A. & Koomar, J. A. (2010). Systematic review of the research evidence examining the effectiveness of interventions using a sensory integrative approach for children. American Journal of Occupational Therapy, 64 (3), 403–414. 10.5014/ajot.2010.09071. [DOI] [PubMed] [Google Scholar]
- Mayston, M. (2016). Bobath and neurodevelopmental therapy: What is the future? Developmental Medicine & Child Neurology, 58 (10), 994 10.1111/dmcn.13221. [DOI] [PubMed] [Google Scholar]
- McLean, B. , Taylor, S. , Blair, E. , Valentine, J. , Carey, L. & Elliott, C. (2017). Somatosensory discrimination intervention improves body position sense and motor performance in children with hemiplegic cerebral palsy. American Journal of Occupational Therapy, 71(3), 7103190060p1–9. 10.5014/ajot.2016.024968 [DOI] [PubMed] [Google Scholar]
- Meany‐Walen, K. K. , Bratton, S. C. & Kottman, T. (2014). Effects of Adlerian play therapy on reducing students’ disruptive behaviors. Journal of Counseling & Development, 92 (1), 47–56. 10.1002/j.1556-6676.2014.00129.x. [DOI] [Google Scholar]
- Miller‐Kuhaneck, H. & Watling, R. (2018). Parental or teacher education and coaching to support function and participation of children and youth with sensory processing and sensory integration challenges: A systematic review. American Journal of Occupational Therapy, 72(1), 7201190030p1–11. 10.5014/ajot.2018.029017 [DOI] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. & Altman, D. G. (2010). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. International Journal of Surgery, 8 (5), 336–341. 10.1371/journal.pmed.1000097. [DOI] [PubMed] [Google Scholar]
- Montero, S. M. & Gómez‐Conesa, A. (2014). Technical devices in children with motor disabilities: A review. Disability and Rehabilitation: Assistive Technology, 9 (1), 3–11. 10.3109/17483107.2013.785034. [DOI] [PubMed] [Google Scholar]
- Moola, F. J. , Faulkner, G. E. J. , White, L. & Kirsh, J. A . (2014). The psychological and social impact of camp for children with chronic illnesses: A systematic review update. Child: Care, Health and Development, 40(5), 615–631. 10.1111/cch.12114 [DOI] [PubMed] [Google Scholar]
- Morgan, C. , Novak, I. , Dale, R. C. & Badawi, N. (2015). Optimising motor learning in infants at high risk of cerebral palsy: A pilot study. BMC Pediatrics, 15 (1), 30 10.1186/s12887-015-0347-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan, C. , Darrah, J. , Gordon, A. M. , Harbourne, R. , Spittle, A. , Johnson, R. et al (2016a). Effectiveness of motor interventions in infants with cerebral palsy: A systematic review. Developmental Medicine & Child Neurology, 58 (9), 900–909. 10.1111/j.1365-2214.2008.00921_2.x. [DOI] [PubMed] [Google Scholar]
- Morgan, C. , Novak, I. , Dale, R. C. , Guzzetta, A. & Badawi, N. (2016b). Single blind randomised controlled trial of GAME (Goals‐Activity‐Motor Enrichment) in infants at high risk of cerebral palsy. Research in Developmental Disabilities, 55, 256–267. 10.1186/s12883-014-0203-2. [DOI] [PubMed] [Google Scholar]
- Novak, I. (2014a). Evidence to practice commentary new evidence in coaching interventions. Physical & Occupational Therapy in Pediatrics, 34 (2), 132–137. 10.3109/01942638.2014.903060. [DOI] [PubMed] [Google Scholar]
- Novak, I. & Berry, J. (2014b). Home program intervention effectiveness evidence. Physical & Occupational Therapy in Pediatrics, 34 (4), 384–389. 10.3109/01942638.2014.964020. [DOI] [PubMed] [Google Scholar]
- Novak, I. & McIntyre, S. (2010). The effect of education with workplace supports on practitioners’ evidence‐based practice knowledge and implementation behaviours. Australian Occupational Therapy Journal, 57 (6), 386–393. 10.1111/j.1440-1630.2010.00861.x. [DOI] [PubMed] [Google Scholar]
- Novak, I. , Mcintyre, S. , Morgan, C. , Campbell, L. , Dark, L. , Morton, N. et al (2013). A systematic review of interventions for children with cerebral palsy: State of the evidence. Developmental Medicine & Child Neurology, 55 (10), 885–910. 10.1111/dmcn.12246. [DOI] [PubMed] [Google Scholar]
- Park, H. Y. , Maitra, K. , Achon, J. , Loyola, E. & Rincón, M. (2014). Effects of early intervention on mental or neuromusculoskeletal and movement‐related functions in children born low birthweight or preterm: A meta‐analysis. American Journal of Occupational Therapy, 68 (3), 268–276. 10.5014/ajot.2014.010371. [DOI] [PubMed] [Google Scholar]
- Pfeiffer B, Clark GF & Arbesman, M. (2018). Effectiveness of cognitive and occupation‐based interventions for children with challenges in sensory processing and integration: A systematic review. American Journal of Occupational Therapy, 72(1), 7201190020p1–7201190020p9. 10.5014/ajot.2018.028233 [DOI] [PubMed] [Google Scholar]
- Polatajko, H. J. & Cantin, N. (2010). Exploring the effectiveness of occupational therapy interventions, other than the sensory integration approach, with children and adolescents experiencing difficulty processing and integrating sensory information. American Journal of Occupational Therapy, 64 (3), 415–429. 10.5014/ajot.2010.09072. [DOI] [PubMed] [Google Scholar]
- Reeuwijk, A. , van Schie, P. E. , Becher, J. G. & Kwakkel, G. (2006). Effects of botulinum toxin type A on upper limb function in children with cerebral palsy: A systematic review. Clinical Rehabilitation, 20 (5), 375–387. 10.1191/0269215506cr956oa. [DOI] [PubMed] [Google Scholar]
- Rodger, S. , Brown, G. T. & Brown, A. (2005). Profile of paediatric occupational therapy practice in Australia. Australian Occupational Therapy Journal, 52 (4), 311–325. 10.1111/j.1440-1630.2005.00487.x. [DOI] [Google Scholar]
- Sakzewski, L. , Ziviani, J. & Boyd, R. (2009). Systematic review and meta‐analysis of therapeutic management of upper‐limb dysfunction in children with congenital hemiplegia. Pediatrics, 123 (6), e1111–e1122. 10.1542/peds.2008-3335. [DOI] [PubMed] [Google Scholar]
- Sakzewski, L. , Ziviani, J. & Boyd, R. N. (2013). Efficacy of upper limb therapies for unilateral cerebral palsy: A meta‐analysis. Pediatrics, 133, e175–e204. 10.1542/peds.2013-0675. [DOI] [PubMed] [Google Scholar]
- Sakzewski, L. , Miller, L. , Ziviani, J. , Abbott, D. F. , Rose, S. , Macdonell, R. A. et al (2015). Randomized comparison trial of density and context of upper limb intensive group versus individualized occupational therapy for children with unilateral cerebral palsy. Developmental Medicine & Child Neurology, 57 (6), 539–547. 10.1111/dmcn.12702. [DOI] [PubMed] [Google Scholar]
- Schaaf, R. C. , Dumont, R. L. , Arbesman, M. & May‐Benson, T. A. (2018). Efficacy of occupational therapy using Ayres Sensory Integration®: A systematic review. American Journal of Occupational Therapy, 72(1), 7201190010p1–10. 10.5014/ajot.2018.028431 [DOI] [PubMed] [Google Scholar]
- Smith, V. , Devane, D. , Begley, C. M. & Clarke, M. (2011). Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Medical Research Methodology, 11 (1), 15 10.1186/1471-2288-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, T. O. , Bacon, H. , Jerman, E. , Easton, V. , Armon, K. , Poland, F. et al (2014). Physiotherapy and occupational therapy interventions for people with benign joint hypermobility syndrome: A systematic review of clinical trials. Disability and Rehabilitation, 36 (10), 797–803. 10.3109/09638288.2013.819388. [DOI] [PubMed] [Google Scholar]
- Smith, J. , Cheater, F. & Bekker, H. (2015). Parents’ experiences of living with a child with a long‐term condition: A rapid structured review of the literature. Health Expectations, 18 (4), 452–474. 10.1111/hex.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits‐Engelsman, B. C. , Blank, R. , van der Kaay, A. C. , Mosterd‐Van Der Meijs, R. , Vlugt‐Van Den Brand, E. , Polatajko, H. J. et al (2013). Efficacy of interventions to improve motor performance in children with developmental coordination disorder: A combined systematic review and meta‐analysis. Developmental Medicine & Child Neurology, 55 (3), 229–237. 10.1111/dmcn.12008. [DOI] [PubMed] [Google Scholar]
- Snider, L. , Majnemer, A. & Darsaklis, V. (2010). Virtual reality as a therapeutic modality for children with cerebral palsy. Developmental Neurorehabilitation, 13 (2), 120–128. 10.3109/17518420903357753. [DOI] [PubMed] [Google Scholar]
- Speth, L. , Janssen‐Potten, Y. , Rameckers, E. , Defesche, A. , Winkens, B. , Becher, J. et al (2015). Effects of botulinum toxin A and/or bimanual task‐oriented therapy on upper extremity activities in unilateral cerebral palsy: A clinical trial. BMC Neurology, 15 (1), 143 10.1186/s12883-015-0404-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spittle, A. , Orton, J. , Doyle, L. W. & Boyd, R. (2007). Early developmental intervention programs post hospital discharge to prevent motor and cognitive impairments in preterm infants. Cochrane Database of Systematic Reviews, (2), CD005495 10.1002/14651858.cd005495.pub2 [DOI] [PubMed] [Google Scholar]
- Spittle, A. , Orton, J. , Anderson, P. , Boyd, R. & Doyle, L. W. (2012). Early developmental intervention programmes post‐hospital discharge to prevent motor and cognitive impairments in preterm infants. Cochrane Database of Systematic Reviews, (12), CD005495 10.1002/14651858.cd005495.pub3 [DOI] [PubMed] [Google Scholar]
- Stavness, C. (2006). The effect of positioning for children with cerebral palsy on upper‐extremity function: A review of the evidence. Physical & Occupational Therapy in Pediatrics, 26 (3), 39–53. 10.1300/j006v26n03_04. [DOI] [PubMed] [Google Scholar]
- Steultjens, E. M. , Dekker, J. , Bouter, L. M. , Van De Nes, J. C. , Lambregts, B. L. & van den Ende, C. H. (2004). Occupational therapy for children with cerebral palsy: A systematic review. Clinical Rehabilitation, 18 (1), 1–14. 10.1002/14651858.cd004490. [DOI] [PubMed] [Google Scholar]
- Stickles Goods, K. , Ishijima, E. , Chang, Y. C. & Kasari, C. (2013). Preschool based JASPER intervention in minimally verbal children with autism: Pilot RCT. Journal of Autism and Developmental Disorders, 43 (5), 1050–1056. 10.1007/s10803-012-1644-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storebø, O. J. , Skoog, M. , Damm, D. , Thomsen, P. H. , Simonsen, E. & Gluud, C. (2011). Social skills training for Attention Deficit Hyperactivity Disorder (ADHD) in children aged 5 to 18 years. Cochrane Database of Systematic Reviews, 12, CD008223 10.1002/14651858.cd008223.pub2 [DOI] [PubMed] [Google Scholar]
- Tanner, K. , Hand, B. N. , O'toole, G. & Lane, A. E . (2015). Effectiveness of interventions to improve social participation, play, leisure, and restricted and repetitive behaviors in people with autism spectrum disorder: A systematic review. American Journal of Occupational Therapy, 69(5), 6905180010p1–6905180010p12. 10.5014/ajot.2015.017806 [DOI] [PubMed] [Google Scholar]
- Tatla, S. K. , Sauve, K. , Virji‐Babul, N. , Holsti, L. , Butler, C. & Van Der Loos, H. F. M. (2013). Evidence for outcomes of motivational rehabilitation interventions for children and adolescents with cerebral palsy: An American Academy for Cerebral Palsy and Developmental Medicine systematic review. Developmental Medicine & Child Neurology, 55 (7), 593–601. 10.1111/dmcn.12147. [DOI] [PubMed] [Google Scholar]
- Tatla, S. K. , Sauve, K. , Jarus, T. , Virji‐Babul, N. & Holsti, L. (2014). The effects of motivating interventions on rehabilitation outcomes in children and youth with acquired brain injuries: A systematic review. Brain Injury, 28 (8), 1022–1035. 10.3109/02699052.2014.890747. [DOI] [PubMed] [Google Scholar]
- Tervahauta, M. H. , Girolami, G. L. & Øberg, G. K. (2017). Efficacy of constraint‐induced movement therapy compared with bimanual intensive training in children with unilateral cerebral palsy: A systematic review. Clinical Rehabilitation, 31 (11), 1445–1456. 10.1177/0269215517698834. [DOI] [PubMed] [Google Scholar]
- Upton, D. , Stephens, D. , Williams, B. & Scurlock‐Evans, L. (2014). Occupational therapists’ attitudes, knowledge, and implementation of evidence‐based practice: A systematic review of published research. British Journal of Occupational Therapy, 77 (1), 24–38. 10.4276/030802214x13887685335544. [DOI] [Google Scholar]
- Vargas, S. & Lucker, J. R. (2016). A quantitative summary of The Listening Program (TLP) efficacy studies: What areas were found to improve by TLP intervention? Occupational Therapy International, 23 (2), 206–217. 10.1002/oti.1425. [DOI] [PubMed] [Google Scholar]
- Vroland‐Nordstrand, K. , Eliasson, A. C. , Jacobsson, H. , Johansson, U. & Krumlinde‐Sundholm, L. (2016). Can children identify and achieve goals for intervention? A randomized trial comparing two goal‐setting approaches. Developmental Medicine & Child Neurology, 58 (6), 589–596. 10.1111/dmcn.12925. [DOI] [PubMed] [Google Scholar]
- Wallen, M. M. & Gillies, D. (2006). Intra‐articular steroids and splints/rest for children with juvenile idiopathic arthritis and adults with rheumatoid arthritis. Cochrane Database of Systematic Reviews, 1, CD002824 10.1002/14651858.cd002824.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watling, R. & Hauer, S. (2015). Effectiveness of Ayres Sensory Integration® and sensory‐based interventions for people with autism spectrum disorder: A systematic review. American Journal of Occupational Therapy, 69 (5), 1–12. 10.5014/ajot.2015.018051. [DOI] [PubMed] [Google Scholar]
- Weaver, L. L . (2015). Effectiveness of work, activities of daily living, education, and sleep interventions for people with autism spectrum disorder: A systematic review. American Journal of Occupational Therapy, 69(5), 6905180020p1–6905180020p11. 10.5014/ajot.2015.017962 [DOI] [PubMed] [Google Scholar]
- Weinstock‐Zlotnick, G. & Hinojosa, J. (2004). Bottom‐up or top‐down evaluation: Is one better than the other? American Journal of Occupational Therapy, 58 (5), 594–599. 10.5014/ajot.58.5.594. [DOI] [PubMed] [Google Scholar]
- Wells, H. , Marquez, J. & Wakely, L. (2018). Garment therapy does not improve function in children with cerebral palsy: A systematic review. Physical & Occupational Therapy in Pediatrics, 38, 395–416. 10.1080/01942638.2017.1365323. [DOI] [PubMed] [Google Scholar]
- Westendorp, M. , Houwen, S. , Hartman, E. , Mombarg, R. , Smith, J. & Visscher, C. (2014). Effect of a ball skill intervention on children's ball skills and cognitive functions. Medicine and Science in Sports and Exercise, 46, 414–422. 10.1249/mss.0b013e3182a532b3. [DOI] [PubMed] [Google Scholar]
- Whalen, C. N. & Case‐Smith, J. (2012). Therapeutic effects of horseback riding therapy on gross motor function in children with cerebral palsy: A systematic review. Physical & Occupational Therapy in Pediatrics, 32 (3), 229–242. 10.3109/01942638.2011.619251. [DOI] [PubMed] [Google Scholar]
- Willis, C. , Nyquist, A. , Girdler, S. , Jahnsen, R. , Reid, S. , Rosenberg, M. et al (2016). Identifying and operationalising the active ingredients of a participation intervention for children with disabilities: Staff perspectives. Developmental Medicine & Child Neurology, 58, 42–43. [Google Scholar]
- World Health Organisation . (2001). ICF: International classification of functioning, disability and health (9241545429). Geneva, Switzerland: World Health Organisation; 10.4135/9781412950510.n454. [DOI] [Google Scholar]
- Wuang, Y. P. , Ho, G. S. & Su, C. Y. (2013). Occupational therapy home program for children with intellectual disabilities: A randomized, controlled trial. Research in Developmental Disabilities, 34 (1), 528–537. 10.1016/j.ridd.2012.09.008. [DOI] [PubMed] [Google Scholar]
- Xu, K. , He, L. , Mai, J. , Yan, X. & Chen, Y. (2015). Muscle recruitment and coordination following constraint‐induced movement therapy with electrical stimulation on children with hemiplegic cerebral palsy: A randomized controlled trial. PLoS ONE, 10 (10), e0138608 10.1371/journal.pone.0138608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zadnikar, M. & Kastrin, A. (2011). Effects of hippotherapy and therapeutic horseback riding on postural control or balance in children with cerebral palsy: A meta‐analysis. Developmental Medicine & Child Neurology, 53 (8), 684–691. 10.1111/j.1469-8749.2011.03951.x. [DOI] [PubMed] [Google Scholar]
- Ziviani, J. , Feeney, R. , Rodger, S. & Watter, P. (2010). Systematic review of early intervention programmes for children from birth to nine years who have a physical disability. Australian Occupational Therapy Journal, 57 (4), 210–223. 10.1111/j.1440-1630.2010.00850.x. [DOI] [PubMed] [Google Scholar]
- Zwaigenbaum, L. , Bauman, M. L. , Choueiri, R. , Kasari, C. , Carter, A. , Granpeesheh, D. et al (2015). Early intervention for children with autism spectrum disorder under 3 years of age: Recommendations for practice and research. Pediatrics, 136 (Suppl 1), S60–S81. 10.1542/peds.2014-3667E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwi, M. , Jones, H. , Thorgaard, C. , York, A. & Dennis, J. A . (2011). Parent training interventions for Attention Deficit Hyperactivity Disorder (ADHD) in children aged 5 to 18 years. Cochrane Database of Systematic Reviews, 12, CD003018 10.4073/csr.2012.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwicker, J. G. & Mayson, T. A. (2010). Effectiveness of treadmill training in children with motor impairments: An overview of systematic reviews. Pediatric Physical Therapy, 22 (4), 361–377. 10.1097/pep.0b013e3181f92e54. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Main results table.


