Abstract
Background
Despite their high prevalence and advances in the field of neurogastroenterology, there remain few effective treatment options for functional gastrointestinal disorders (FGIDs). It is recognized that approximately 25% of sufferers will have symptoms refractory to existing therapies, causing significant adverse effects on quality of life and increased healthcare utilization and morbidity. Gut‐focused hypnotherapy, when delivered by trained therapists, has been shown to be highly effective in severe refractory FGIDs. However, hypnotherapy continues to be surrounded by much misunderstanding and skepticism.
Purpose
The purpose of this review is to provide a contemporary overview of the principles of gut‐focused hypnotherapy, its effects on gut‐brain interactions, and the evidence‐base for its efficacy in severe FGIDs. As supplementary material, we have included a hypnotherapy protocol, providing the reader with an insight into the practical aspects of delivery, and as a guide, an example of a script of a gut‐focused hypnotherapy session.
Keywords: functional gastrointestinal disorders, hypnotherapy, irritable bowel syndrome
Short abstract
The purpose of this review is to provide a contemporary overview of the principles of gut‐focused hypnotherapy, its effects on gut‐brain interactions, and the evidence‐base for its efficacy in severe FGIDs. As supplementary material, we have included a hypnotherapy protocol, providing the reader with an insight into the practical aspects of delivery, and as a guide, an example of a script of a gut‐focused hypnotherapy session.
Key Points.
Gut‐focused hypnotherapy is highly effective in functional gastrointestinal disorders when conventional treatments have failed.
While the exact mechanisms remain elusive, hypnotherapy appears to modulate brain‐gut pain pathways and sensorimotor function.
Hypnotherapy significantly improves symptoms in up to 76% of patients with durable effects and important socioeconomic benefits.
1. INTRODUCTION
Functional gastrointestinal disorders (FGIDs) are the most common diagnoses in gastroenterology1, 2 with a reported population prevalence of 35%.3 Based on advances in the understanding of FGIDs and their pathophysiology over the past two decades, these are now defined as disorders of 'Gut‐brain interaction'.4 The hallmark of these conditions is gastrointestinal symptoms related to any combination of: motility disturbance, visceral hypersensitivity, altered mucosal and immune function, altered gut microbiota, and altered central nervous system processing.1 While the recent Rome IV classification for FGIDs has described 33 separate entities covering six different anatomical regions,1 it is recognized that there is significant overlap between these disorders.3, 5 Unfortunately, despite progress in making positive diagnoses,6 physiological testing7 and understanding of gut‐brain interactions, treatment remains challenging8. Moreover, patient satisfaction with medical treatment is disappointingly low,9 with many patients failing to improve despite being prescribed a wide variety of conventional therapies. It is estimated that around a quarter of patients have severe, refractory symptoms, with significant impairment of quality of life (QoL), detrimental effects on daily functioning, personal and social relationships, workplace productivity, and psychological well‐being including suicidal ideation.10, 11, 12, 13, 14, 15, 16, 17 These patients are also vulnerable to iatrogenic harm including repeatedly negative investigations, opiate analgesia, and unnecessary surgical interventions,18, 19, 20 not to mention the associated spiraling healthcare costs.21 Perhaps unsurprisingly, when we consider the current pathophysiological understanding of FGIDs, among all the heterogeneous treatment options available, approaches targeting 'gut‐brain interactions' including centrally acting neuromodulators22, 23 and behavioral approaches such as gut‐focused hypnotherapy24 have shown the most promise. Indeed, mounting evidence and clinical experience from tertiary centers, including our own center in Manchester over the past 35 years, have shown that gut‐focused hypnotherapy can improve symptoms, even in severe, refractory cases, by modulating some of the key pathophysiological processes including visceral pain sensitivity and motility25 and can improve coping, resilience, self‐regulation skills26 and reduce healthcare utilization.27, 28 Despite initial skepticism, there is now increased interest in the role of hypnotherapy in the area of FGIDs. However, the literature on the subject remains relatively sparse with only 384 peer‐reviewed papers being identified in a PubMed search in November 2018 using the search terms 'functional gastrointestinal disorders' and 'hypnotherapy’ with the 'AND' operator. Despite this, there are now several high‐quality systematic reviews,24, 29, 30 demonstrating that it is an effective option for refractory/severe symptoms in patients with FGIDs. Moreover, the pivotal role of the gastroenterologist in making a strong and compelling recommendation for appropriate patients to have this effective therapy has recently been highlighted.31 In this context, the aim of this review article is to provide a state of the art overview of the evidence‐base and practical aspects of gut‐focused hypnotherapy as a primer for gastroenterologists looking after patients with severe FGIDs.
2. THE HISTORY AND PRINCIPLES OF GUT‐FOCUSED HYPNOTHERAPY
2.1. Myths and misperceptions
Gut‐focused hypnotherapy has been used as a treatment for refractory, severe FGIDs since the early 1980 s.32 Unfortunately, uptake among some clinicians and patients has been hindered by the common misperception of hypnosis, which carries an erroneous legacy of mystery and coercive influence over people from popular media and stage shows.33 Indeed, recent data from our own unit has shown that over half of patients referred for gut‐focused hypnotherapy have negative perceptions about treatment before, but not after, treatment.34 Fortunately, negative perceptions pretreatment did not appear to influence the chances of a clinical response.34
2.2. The aims and principles of gut‐focused hypnotherapy
Hypnotherapy is usually carried out on an individualized basis by a trained therapist during 30‐60 minute sessions, at weekly intervals, for 6‐12 weeks. Clinical hypnosis is a verbal intervention that utilizes a special mental state of enhanced receptivity to suggestion, to facilitate therapeutic psychological and physiological changes.35 Broadly, the aims of gut‐focused hypnotherapy are to induce a deep state of relaxation to guide the patient to learn how to control their gut function. The first session is typically an introductory session. One of the fundamental aspects of delivering a gut‐focused hypnotherapy package for a functional disorder is educating the patient regarding the basic anatomy and physiology of the gut. This is provided in a way that is easily understandable at the outset. The patient is then provided with explanations about how disturbance of this normal gastrointestinal 'function' can produce their specific symptoms. Previous studies have shown the benefits of optimizing gut‐focused hypnotherapy based on patients’ personal visual imagery of their functional disorder,36 using color,37, 38 illustrations and anatomical diagrams39, 40 to enhance the treatment experience (Figure 1). During subsequent hypnotherapy sessions, the patient is taught a series of approaches to enable them to gain control of their gut function. The approach is adapted to the patients’ symptom profile and own personal imagery using metaphors. For example, patients with a functional bowel disorder could be asked to imagine their gut as a river and modify its flow according to their needs depending on whether they have predominant diarrhea or constipation.25 For abdominal pain, the tactile approach of the patient placing their hand on their abdomen, feeling warmth, and using this to alleviate pain can be useful.25 Similarly, an inflated balloon being slowly deflated can be used as a metaphor to reduce abdominal bloating. This is also sometimes combined with other helpful techniques such as teaching the patient diaphragmatic breathing.
Figure 1.
Examples of illustrations and visual imagery to represent functional gastrointestinal symptoms to enhance the hypnotherapy experience (Reproduced and adapted with permission from Carruthers HR, Morris J, Tarrier N, Whorwell PJ. Reactivity to images in health and irritable bowel syndrome. Aliment Pharmacol Ther 2010; 31:131–142)
During hypnotherapy sessions, great emphasis is placed on the patient having control of their gut, rather than their gut having control over them, a mantra which is reinforced repeatedly.25 While the content of sessions is similar, therapists often introduce suggestions and strategies on how to overcome tendencies to anxiety or fear of imminent catastrophe and developing the ability to gain control over other coincidental problems.25 Patients are encouraged to practice hypnotherapy at home in between sessions using audio recordings.
For further information on the practical delivery of gut‐focused hypnotherapy, please find our hypnotherapy protocol, with an example of a hypnotherapy script, in the supplementary file linked to this paper (Data S1).
3. GUT‐FOCUSED HYPNOTHERAPY AND EFFECTS ON GUT‐BRAIN INTERACTIONS
3.1. Effects of hypnosis on gastrointestinal motility and function
While the exact mechanisms of gut‐focused hypnotherapy in functional FGIDs are not fully understood, a number of studies have demonstrated its ability to induce changes in gastrointestinal function and physiology. For example, in the upper gastrointestinal tract, hypnotherapy has been shown to be able to modulate gastric acid secretion,41 accelerate gastric emptying,42 and alter orocecal transit time measured using the lactulose hydrogen breath test,43 in controlled studies in healthy participants. Similarly, in the lower gastrointestinal tract, some studies conducted in patients with Irritable Bowel Syndrome (IBS) have shown appreciable differences in colonic sensory and motor function before and immediately after hypnotherapy, demonstrating modulation of postprandial gastrocolic reflex activity,44 colonic motility,45 and visceral hypersensitivity.44, 46, 47, 48 In an interesting study of the effects of hypnotherapy on gastrointestinal motility in a heterogeneous group of IBS patients, Lindfors et al did not detect any significant long‐term differences in gastric emptying, small intestinal transit time, antroduodenal manometry or colonic transit time before and after hypnotherapy.49 However, the inclusion of patients with both constipation and diarrhea predominant IBS in this study49 makes the motility and transit data difficult to interpret, given the differing therapeutic approaches to gut‐focused hypnotherapy between the two IBS subtypes and the potential opposing effects on these metrics that the differing approaches to hypnotherapy may have.
3.2. Putative mechanisms of action of gut‐focused hypnotherapy
As alluded to earlier, while the exact mechanisms of action of gut‐focused hypnotherapy remain unclear, a number of studies using functional brain imaging techniques have given some plausible explanations which suggest that hypnotherapy can induce changes in neuroplasticity. For example, several studies have investigated brain activity in response to painful visceral stimuli in IBS.50 Based on this work, and other studies, current understanding is that patients with painful FGIDs have abnormal signaling in visceral afferent pathways and central pain amplification.51 Interestingly, the anterior cingulate cortex, one of the brain regions most consistently enhanced by painful visceral stimuli in IBS,52, 53, 54 has been shown to be an area which can be modulated by hypnotherapy during treatment focused on altering the response to a noxious painful stimulus (Figure 2).55 Studies of hypnotherapy in the chronic pain literature have shown that hypnotic suggestions for pain modulation also impact the prefrontal, insular, and somatosensory regions, and there is evidence for differing brain activations depending on whether the hypnotic suggestion is related to pain affect or pain intensity.56 Moreover, a recent, well‐designed, controlled study has shown that responders to hypnotherapy with moderate to severe IBS had attenuation of brain activity in the posterior insula and that improvement in symptoms was associated with normalization of evoked brain responses to painful visceral stimuli (Figure 3).57 These data suggest that the use of gut‐focused metaphors, hypnotic suggestions for physiological improvement, and imagery used during hypnotherapy, may select specific related peripheral and central gut‐brain neuronal pathways, leading to favorable neuroplastic changes induced by practice and further re‐enforcement during, and in between hypnotherapy sessions. This would perhaps explain the functional, physiological and clinically relevant benefits that have been observed following hypnotherapy, which may drive such neuroplastic changes to restore 'normal' processing of painful visceral stimuli in patients with FGIDs.
Figure 2.
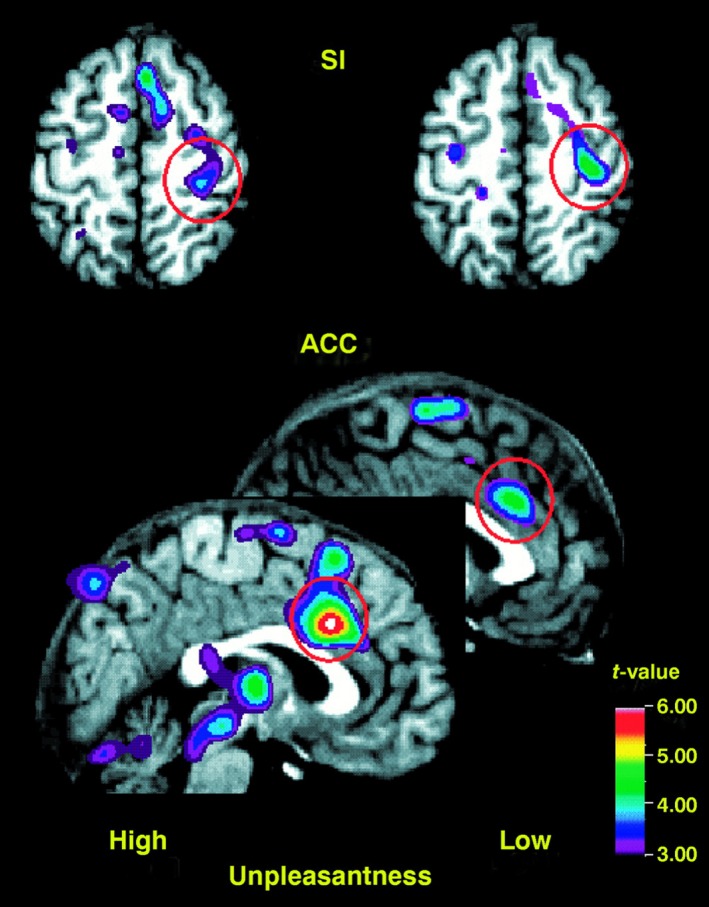
Hypnotherapy induced changes in pain‐related brain activation in the Anterior Cingulate Cortex (ACC) seen on Positron Emission Topography. Hypnotic suggestions of low unpleasantness of pain evoke less activity in ACC compared to highly unpleasant hypnotic suggestions of pain (Reproduced with permission from Rainville P, Duncan GH, Price DD, Carrier Bt, Bushnell MC. Pain Affect Encoded in Human Anterior Cingulate But Not Somatosensory Cortex. Science 1997; 277:968–971)
Figure 3.
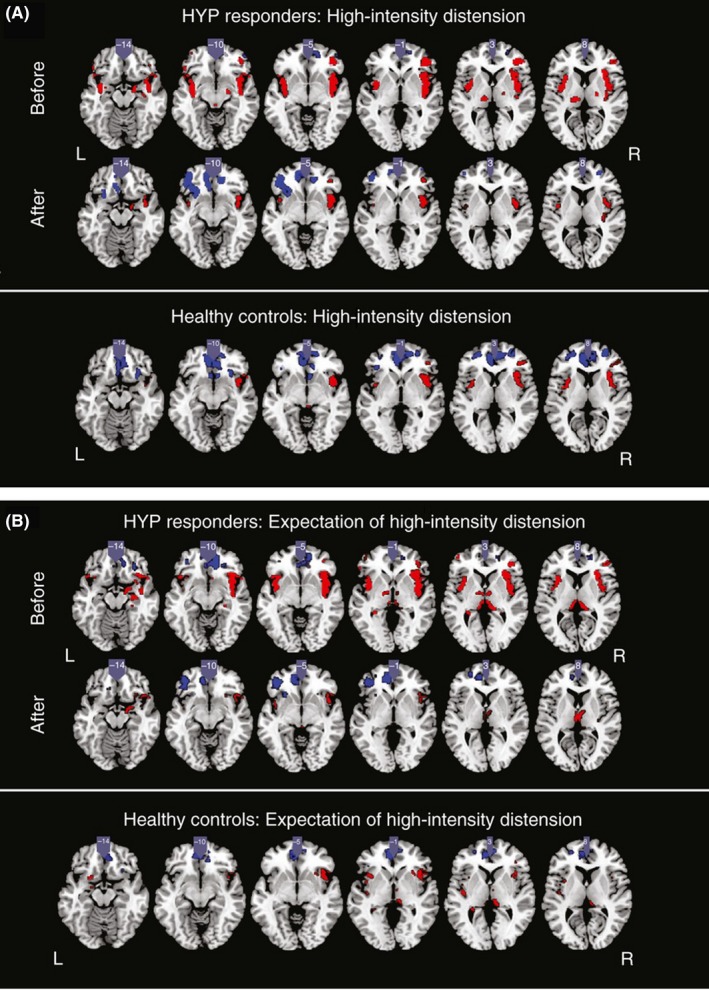
Hypnotherapy restores a normal pattern of brain activity evoked by high‐intensity rectal distension in IBS patients (Reproduced with permission from Lowén, A. ME, et al Effect of hypnotherapy and educational intervention on brain response to visceral stimulus in the irritable bowel syndrome. Alimentary Pharmacology & Therapeutics 2013; 37:1184–1197)
4. HYPNOTHERAPY IN IRRITABLE BOWEL SYNDROME: A MODEL FOR OTHER FUNCTIONAL DISORDERS
IBS, the most common FGID,3 is defined by recurrent abdominal pain associated with defecation or a change in bowel habit and abdominal bloating/distension.58 Unsurprisingly, given its high prevalence, it has been the subject of the most research since gut‐focused hypnotherapy was introduced for FGIDs in the 1980 s.59 Given the common, overlapping features and characteristics of FGIDs, IBS has proved to be an ideal model for understanding how hypnotherapy can be applied to the investigation and management of other functional disorders.
4.1. Patient selection and clinical indications
It is important to ensure a firm clinical diagnosis of IBS is established prior to considering hypnotherapy. Hypnotherapy is indicated for patients with severe symptoms refractory to 12 months of pharmacological treatment.60, 61 In recent years, dietary interventions have been shown to play a significant role in treating FGIDs. There is now a strong body of evidence for exclusion diets and the low fermentable oligo‐, di‐, and monosaccharides and polyols (FODMAPs) diet, which have been shown to improve symptoms in 40%‐50% of patients.62, 63, 64 These dietary interventions are recommended as first‐line therapy for IBS.60, 65 Indeed, a small randomized study from Australia compared outcomes from first‐line therapy with six weeks of hypnotherapy versus a low‐FODMAPs diet, and a combination of the two approaches, and found all three to be equally effective in improving symptoms.66 These data support current recommendations to use dietary interventions such as the low‐FODMAPs diet as first‐line and reserving gut‐focused hypnotherapy for more severe, refractory cases, where all conventional measures have failed. In practice, most patients referred for hypnotherapy for IBS have, therefore, usually tried the low‐FODMAPs diet. It is important that hypnotherapy is not considered a standalone treatment, and the package of care offered should include dietary modifications to improve the chances of a successful outcome.65
Patient age appears to account for very little of the variance in clinical outcomes to gut‐focused hypnotherapy67 and therefore should not be a barrier to accessing gut‐focused hypnotherapy. Indeed, there is evidence showing that the efficacy of gut‐focused hypnotherapy in children and adolescents with IBS is similar to that in adults,68, 69, 70, 71, 72 with long‐term benefits.73 While our experience suggests that the magnitude of clinical response in those over 50 years of age is less than that seen in younger patients,71, 74 74% of those above the age of 50 still achieve a clinically meaningful improvement (50 point reduction in IBS symptom severity scores);74 therefore, hypnotherapy is certainly still worth considering in this group, particularly in refractory cases where other conventional treatments have failed.
However, it is important to note that hypnotherapy is not appropriate in all patients and caution should be exercised in patients with significant psychopathologies.
4.2. Clinical efficacy in Irritable Bowel Syndrome
The earliest randomized study of hypnotherapy for IBS demonstrated significant improvement in abdominal pain, abdominal bloating, and bowel function following hypnosis, compared to supportive therapy with a placebo medication.59 Subsequent studies have not only replicated this,59, 67, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83 but several have demonstrated that gut‐focused hypnotherapy has potential wider socioeconomic benefits including improving general well‐being, reduction in healthcare utilization,75, 84, 85 improved QoL67, 83, 85, 86 and presenteeism at work.75 Moreover, in addition to bowel symptoms, patients with IBS are known to suffer from multiple extra‐intestinal symptoms including: nausea, thigh pain, low backache, lethargy, and a range of urinary and gynecological symptoms.87 These symptoms are notoriously difficult to treat and seldom respond to conventional treatments for IBS. However, these extra‐intestinal symptoms have also been shown to improve with gut‐focused hypnotherapy67, 74, 75 and improvement in anxiety and depression levels67, 74, 79, 85, 86 and cognitive function.88 Furthermore, the effects of hypnotherapy are long lasting,84, 85 associated with high levels of patient satisfaction86 and reduced medication use.85, 89 In a recent, large cohort study of 1000 adult patients with refractory IBS, 76% of patients achieved a response (defined as a 50 point improvement in the IBS symptom severity score) following gut‐focused hypnotherapy (Figure 4), with higher response rates in females 80% compared to 62% in males.74
Figure 4.
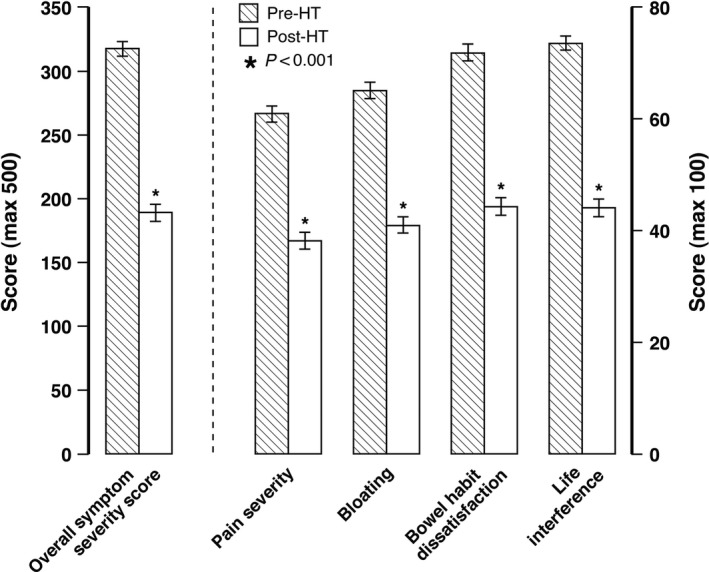
IBS Symptom Severity Scores before and after gut‐focused hypnotherapy in the largest cohort to date (n = 1,000) (Reproduced with permission from Miller V, Carruthers HR, Morris J, Hasan SS, Archbold S, Whorwell PJ. Hypnotherapy for irritable bowel syndrome: an audit of one thousand adult patients. Aliment Pharmacol Ther 2015; 41:844–855)
5. GUT‐FOCUSED HYPNOTHERAPY IN FUNCTIONAL UPPER GASTROINTESTINAL DISORDERS
As described earlier in this paper, there is considerable overlap in the pathophysiology of FGIDs, with studies in both upper and lower FGIDs consistently demonstrating visceral hypersensitivity to mechanical or chemical stimuli.90, 91 Indeed, there is emerging evidence that 'esophagus‐focused hypnotherapy' is both feasible and acceptable to patients with functional esophageal disorders.92, 93 Importantly, the recently updated diagnostic criteria for this group of disorders reflect advances in motility diagnostics.94 These robust criteria, therefore, ensure that all patients, by definition, will have had all the necessary structural endoscopic/radiological, pH/impedance monitoring and motility investigations where appropriate. Similar to findings in IBS patients, patients with normal esophageal physiology and refractory functional esophageal symptoms have recently been shown to have impaired quality of life and high levels of psychosocial distress.95 The principles of esophageal‐focused hypnotherapy in this group of patients mirror the approaches used in IBS, but specifically target esophageal hypervigilance and esophageal hypersensitivity.90 This is usually achieved using visual imagery around esophageal physiology and metaphoric imagery related to esophageal symptoms using structured, scripted protocols.90 In globus pharyngeus, 7 sessions of this type of hypnotherapy significantly reduced globus symptoms with response in 9 out of 10 patients without altering upper esophageal sphincter pressures.93 Similarly, in functional heartburn, 9 patients who completed 7 weekly sessions of hypnosis, all reported symptomatic improvement including visceral anxiety and QoL.92 Functional chest pain, defined as recurring, unexplained retrosternal pain of presumed esophageal origin, requires prior exclusion of coronary artery disease with appropriate cardiological investigations,94 is a particularly debilitating condition associated with high psychological morbidity. Hypnotherapy in a randomized controlled study in non‐cardiac chest pain patients with normal coronary angiography (n = 28) demonstrated reduction of global pain scores in 12/15 patients (80%) compared to only 23% response in controls (supportive treatment plus placebo medication).96 Twelve sessions of hypnotherapy also improved well‐being, QoL, reduced pain intensity, and medication use, with long‐lasting effects maintained at 2 years posthypnotherapy (Figure 5).96, 97
Figure 5.
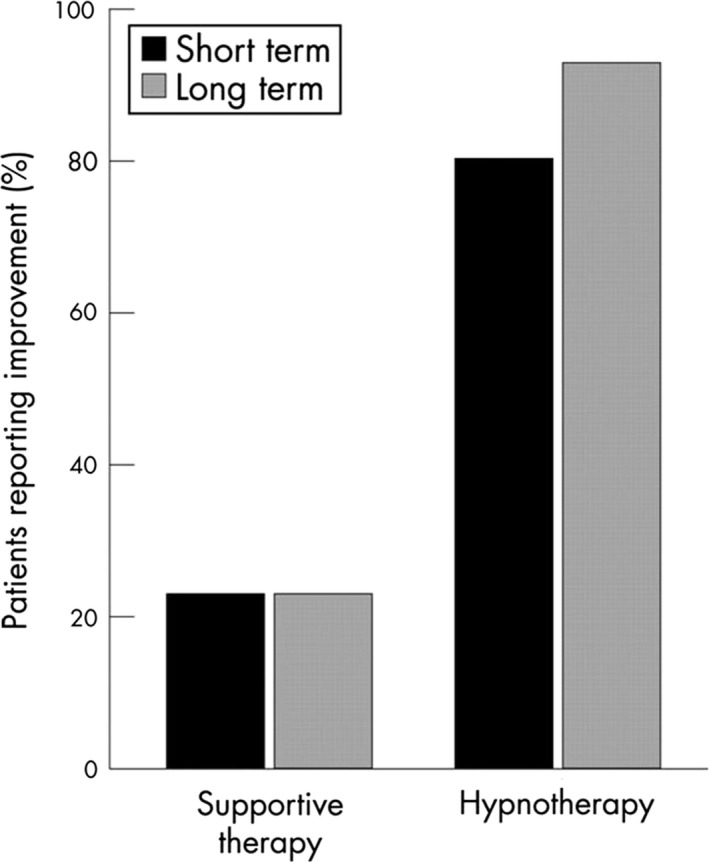
Short‐ and long‐term benefits of gut‐focused hypnotherapy in non‐cardiac chest pain compared to supportive therapy (Reproduced with permission from Miller V, Jones H, Whorwell PJ. Hypnotherapy for non‐cardiac chest pain: long‐term follow‐up. Gut 2007; 56:1643)
Functional Dyspepsia (FD), another relatively common FGID which significantly impacts activities of daily living, is defined by one or more of the following symptoms: postprandial fullness, early satiation, epigastric pain, and burning, in the absence of structural abnormalities.98 Gut‐focused hypnotherapy can also be customized for FD by targeting gastroduodenal function and symptoms. This can involve both tactile and imagery techniques with suggestions of positive changes in motor activity, sensitivity, and secretion of acid. This approach has been shown to be highly effective in a randomized controlled trial which demonstrated that 16 weeks of hypnotherapy was superior to both supportive care and medical therapy, with 73% response rates at 12 months (Figure 6) and wider socioeconomic benefits including reduced consultation rates and lower medication use when compared to both the control groups.99
Figure 6.
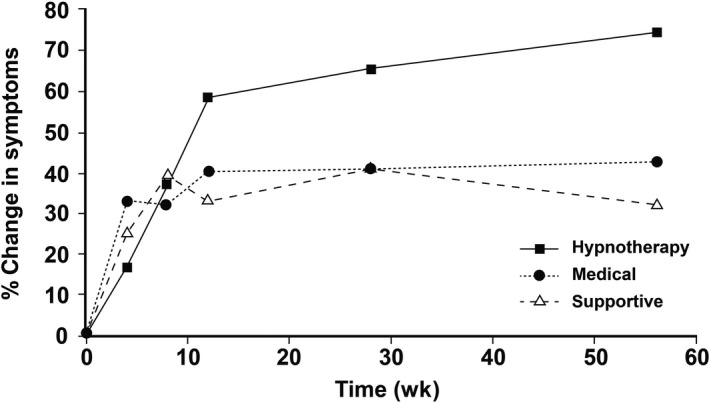
The efficacy of gut‐focused hypnotherapy compared to medical therapy and supportive care in Functional Dyspepsia (Reproduced with permission from Calvert EL, Houghton LA, Cooper P, Morris J, Whorwell PJ. Long‐term improvement in functional dyspepsia using hypnotherapy. Gastroenterology 2002; 123:1778–1785)
6. CENTRALLY MEDIATED ABDOMINAL PAIN
Centrally mediated abdominal pain syndrome (CAPS) is a recently redefined, relatively rare but severe FGID, which is defined as chronic continuous abdominal pain that is minimally related to the physiological events of eating, defecation, and menses and results in a loss of day‐to‐day functioning.100 While poorly understood, the mechanism of pain in these disorders is postulated to be due to central sensitization.51, 101 CAPS is a challenging condition to treat with patients often presenting repeatedly with significant psychological comorbidity, multiple repeated negative investigations, and heavy socioeconomic costs including healthcare utilization and the burden of loss of working days due to illness.100 Hence, patients with CAPS often exhibit consequences of fear avoidance and characteristics including pain catastrophizing, hypervigilance, and attentional bias and psychological inflexibility, factors which make a compelling case for treatment of CAPS with gut‐focused hypnotherapy.102 While specific evidence for hypnotherapy in CAPS is lacking in the adult literature, it has been shown to be effective in children.70
7. AREAS FOR FUTURE RESEARCH AND DEVELOPMENT
In this paper, we have already presented the compelling case for hypnotherapy and have summarized its benefits and limitations in Table 1. Despite the mounting evidence for hypnotherapy in FGIDs, one of the challenges is optimizing access to services in already resource‐stretched healthcare systems. To address some of these challenges, it is recognized that there is a need to trial novel platforms of delivery, in order to provide wider‐scale access to this highly effective treatment. Group delivery of gut‐focused hypnotherapy is one potential way of achieving this aim. In a randomized controlled trial of the group approach compared to standard medical treatment, group hypnotherapy has been shown to be effective (61% vs. 41%), with durable effects being maintained over a year posttreatment. Moreover, while preliminary data from two recently completed randomized head to head trials have shown marginally better response rates in individualized vs. group hypnotherapy, both trials found that group therapy was not significantly inferior to individualized therapy,103, 104 suggesting that group hypnotherapy may be a way of improving access. One of the drawbacks of group hypnotherapy is that the package has to be generic, whereas for the more severe, refractory cases seen in tertiary care, who have more complex needs, treatment needs to be individualized. Consequently, group hypnotherapy would be ideal for primary care where a visiting hypnotherapist could treat large numbers of patients at a number of different practices. Furthermore, this would have the added advantage that the group, who would all come from one locality, could potentially support each other. Another challenge facing tertiary services is that the outcomes for gut‐focused hypnosis appear to be better in highly specialized research centers rather than in smaller community settings.106 The exact reasons for these differences are unclear but may be due to differences in the training of therapists.107 Another reason for apparent differences in outcomes may be due to differences in symptom severity and patient characteristics between tertiary patients treated in highly specialized centers and those treated in non‐specialized centers. For example, there is reasonably good evidence to suggest that hypnotherapy is effective in the refractory group of IBS patients seen in tertiary care and the UK National Institute for Health and Care Excellence (NICE) recommends this form of treatment in patients not responding to pharmacological and dietary interventions. Within this group of tertiary care patients, those with higher symptom severity scores tend to respond better and this is probably because such patients have a much more complex form of the disorder with additional psychological factors contributing. Furthermore, these patients are more likely to fully engage in this time‐consuming form of treatment, which is often perceived as their last chance to improve. Nonetheless, given that there are relatively few highly specialized centers, there is now an acute need for specialist centers to be able to provide effective hypnotherapy to patients further afield. Telemedicine is an emerging concept as a result of recent technological advances and is an attractive potential solution for this problem. Indeed, Skype gut‐focused hypnotherapy has been recently trialed in Manchester with some success. This approach resulted in a clinically significant reduction in IBS symptoms in 65% of twenty IBS patients treated with 12 sessions of hypnotherapy which included only one face to face, introductory session.108 These results are promising and only slightly less effective (65% vs. 76%) than traditional face to face hypnotherapy outcomes from 1,000 consecutive patients at the same center.74, 108 A particular advantage of Skype hypnotherapy was that it did ensure that patients, who would otherwise have been unable to attend for face to face hypnotherapy, were able to access effective treatment within the comfort of their own home.
Table 1.
The benefits and limitations of gut‐focused hypnotherapy for functional gastrointestinal disorders
| Benefits | Limitations |
|---|---|
|
|
Furthermore, in order to manage finite resources such as gut‐focused hypnotherapy clinics, there is a need for a randomized dose‐response study, which is currently lacking, to help determine the optimal number of sessions. Current practice varies in terms of the number of sessions being offered in different centers. This is usually somewhere between 6 and 12 weekly sessions. Interestingly, while one study has shown that response at week 6 is predictive of a favorable response at week 12,109 outcomes from a trial of 6 sessions of hypnotherapy have not shown the same long‐term effects seen with 12 sessions, suggesting that the effects of shorter courses of hypnotherapy may wear off over time.85, 89 However, from experience in other behavioral neurogastroenterology interventions such as pelvic floor biofeedback therapy, it is likely that one size will not fit all when it comes to follow‐up. Male patients in particular and those with the most severe symptoms are likely to require more sessions, whereas highly motivated individuals including those who spend longer doing self practice at home may achieve better outcomes after fewer sessions.110, 111 Further studies to better understand predictive factors to successful hypnotherapy outcomes112 will, therefore, help customize the intensity of treatment, reduce dropout rates and improve resource management. In addition to gut‐focused hypnotherapy, there are several other promising behavioral treatments such as cognitive behavioral therapy with level 1 evidence in FGIDs.24 These techniques, while beyond the scope of this article, are worthy of consideration, especially when hypnotherapy is not available. Unfortunately, to date, there are no published comparative studies between these other behavioral treatments and hypnotherapy, which should be the subject of future research. Finally, as detailed in this review, gut‐focused hypnotherapy has only been evaluated in several of the 33 described FGIDs, and therefore, future studies may explore its efficacy in other rarer FGIDs with overlapping pathophysiology.
8. CONCLUSIONS
Gut‐focused hypnotherapy is a highly adaptable and effective treatment for refractory FGIDs which can be customized to the patient's symptoms. Not only has it consistently been shown to be superior to standard medical care, hypnosis has the added advantages of improving extra‐intestinal symptoms of FGIDs, improving psychological, cognitive function, and quality of life, and reducing healthcare utilization. Gastroenterologists should, therefore, seriously consider referral for hypnotherapy in patients with refractory FGIDs.
DISCLOSURES
Over the last 3 years, DHV has acted as a consultant for Allergan and Shire and PJW has acted as a consultant or received research funding from Danone, Allergan Pharma, Ironwood Pharma, and Salix Pharma, but it is not felt that the contents of this paper have been influenced at all by any of these relationships.
AUTHOR CONTRIBUTIONS
DHV developed and wrote the manuscript, and PJW reviewed the manuscript and provided critical intellectual input.
Supporting information
ACKNOWLEDGMENTS
The authors are extremely grateful to Mrs. Vivien Miller who proofread the final version of the manuscript and Helen Carruthers PhD (medical illustrations manager), and Kelly Shennan (Graphic Designer) at Wythenshawe Hospital who helped optimise the figures.
Vasant DH, Whorwell PJ. Gut‐focused hypnotherapy for Functional Gastrointestinal Disorders: Evidence‐base, practical aspects, and the Manchester Protocol. Neurogastroenterol Motil. 2019;31:e13573 10.1111/nmo.13573
REFERENCES
- 1. Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology 2016;150(6):1262‐1279. [DOI] [PubMed] [Google Scholar]
- 2. Agrawal A, Whorwell PJ. Irritable bowel syndrome: diagnosis and management. BMJ. 2006;332(7536):280‐283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Aziz I, et al. The prevalence and impact of overlapping Rome IV‐diagnosed functional gastrointestinal disorders on somatization, quality of life, and healthcare utilization: a cross‐sectional general population study in three countries. Am J Gastroenterol. 2018;113(1):86‐96. [DOI] [PubMed] [Google Scholar]
- 4. Drossman DA, Hasler WL. Rome IV‐functional GI disorders: disorders of gut‐brain interaction. Gastroenterology. 2016;150(6):1257‐1261. [DOI] [PubMed] [Google Scholar]
- 5. Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: one or many? Lancet. 1999;354(9182):936‐939. [DOI] [PubMed] [Google Scholar]
- 6. Moayyedi P, Mearin F, Azpiroz F, et al. Irritable bowel syndrome diagnosis and management: A simplified algorithm for clinical practice. United European Gastroenterol J. 2017;5(6):773‐788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fox MR, Kahrilas PJ, Roman S, et al. Clinical measurement of gastrointestinal motility and function: who, when and which test? Nat Rev Gastroenterol Hepatol. 2018;1. [DOI] [PubMed] [Google Scholar]
- 8. Corsetti M, Whorwell P. Novel pharmacological therapies for irritable bowel syndrome. Expert Rev Gastroenterol Hepatol. 2016;10(7):807‐815. [DOI] [PubMed] [Google Scholar]
- 9. Hungin A, Whorwell PJ, Tack J, Mearin F. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40,000 subjects. Aliment Pharmacol Ther. 2003;17(5):643‐650. [DOI] [PubMed] [Google Scholar]
- 10. Drossman DA, Chang L, Bellamy N, et al. Severity in irritable bowel syndrome: a Rome Foundation working team report. Am J Gastroenterol. 2011;106:1749. [DOI] [PubMed] [Google Scholar]
- 11. Drossman DA, Li Z, Andruzzi E, et al. US householder survey of functional gastrointestinal disorders. Dig Dis Sci. 1993;38(9):1569‐1580. [DOI] [PubMed] [Google Scholar]
- 12. Lea R, Whorwell PJ. Quality of life in irritable bowel syndrome. Pharmacoeconomics. 2001;19(6):643‐653. [DOI] [PubMed] [Google Scholar]
- 13. El‐Serag HB. Impact of irritable bowel syndrome: prevalence and effect on health‐related quality of life. Rev Gastroenterol Disord. 2003;3(Suppl 2):S3‐S11. [PubMed] [Google Scholar]
- 14. Gralnek IM, Hays RD, Kilbourne A, Naliboff B, Mayer EA. The impact of irritable bowel syndrome on health‐related quality of life. Gastroenterology. 2000;119(3):654‐660. [DOI] [PubMed] [Google Scholar]
- 15. Miller V, Hopkins L, Whorwell PJ. Suicidal ideation in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2004;2(12):1064‐1068. [DOI] [PubMed] [Google Scholar]
- 16. Ballou S, Keefer L. The impact of irritable bowel syndrome on daily functioning: Characterizing and understanding daily consequences of IBS. Neurogastroenterol Motil. 2017;29(4):e12982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Frändemark Å, Törnblom H, Jakobsson S, Simrén M. Work productivity and activity impairment in irritable bowel syndrome (IBS): a multifaceted problem. Am J Gastroenterol. 2018;113:1540‐1549. [DOI] [PubMed] [Google Scholar]
- 18. Whorwell P. preventing unnecessary investigation and surgery in the irritable bowel syndrome—the critical role of the general practitioner. Aliment Pharmacol Ther. 2018;47(11):1558‐1559. [DOI] [PubMed] [Google Scholar]
- 19. Longstreth GF, Yao JF. Irritable bowel syndrome and surgery: A multivariable analysis. Gastroenterology. 2004;126(7):1665‐1673. [DOI] [PubMed] [Google Scholar]
- 20. Sayuk GS, Kanuri N, Gyawali CP, Gott BM, Nix BD, Rosenheck RA. Opioid medication use in patients with gastrointestinal diagnoses vs unexplained gastrointestinal symptoms in the US Veterans Health Administration. Aliment Pharmacol Ther. 2018;47(6):784‐791. [DOI] [PubMed] [Google Scholar]
- 21. Inadomi JM, Fennerty MB, Bjorkman D. Systematic review: the economic impact of irritable bowel syndrome. Aliment Pharmacol Ther. 2003;18(7):671‐682. [DOI] [PubMed] [Google Scholar]
- 22. Drossman DA, Tack J, Ford AC, Szigethy E, Törnblom H, VanOudenhove L. Neuromodulators for functional gastrointestinal disorders (Disorders of gut‐brain interaction): a rome foundation working team report. Gastroenterology. 2018;154(4):1140‐1171.e1 [DOI] [PubMed] [Google Scholar]
- 23. Sobin WH, Heinrich TW, Drossman DA. Central neuromodulators for treating functional gi disorders: a primer. Am J Gastroenterol. 2017;112(5):693‐702. [DOI] [PubMed] [Google Scholar]
- 24. Ford AC, Quigley E, Lacy BE, et al. Effect of antidepressants and psychological therapies, including hypnotherapy, in irritable bowel syndrome: systematic review and meta‐analysis. Am J Gastroenterol. 2014;109(9):1350‐1365. [DOI] [PubMed] [Google Scholar]
- 25. Miller V, Whorwell PJ. Hypnotherapy for functional gastrointestinal disorders: a review. Int J Clin Exp Hypn. 2009;57(3):279‐292. [DOI] [PubMed] [Google Scholar]
- 26. Ballou S, Keefer L. Psychological interventions for irritable bowel syndrome and inflammatory bowel diseases. Clin Transl Gastroenterol. 2017;8(1):e214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kinsinger SW, Ballou S, Keefer L. Snapshot of an integrated psychosocial gastroenterology service. World J Gastroenterol. 2015;21(6):1893‐1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. VanOudenhove L, Crowell MD, Drossman DA, et al. Biopsychosocial aspects of functional gastrointestinal disorders. Gastroenterology. 2016;150(6):1355‐1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Peters SL, Muir JG, Gibson PR. Review article: gut‐directed hypnotherapy in the management of irritable bowel syndrome and inflammatory bowel disease. Aliment Pharmacol Ther. 2015;41(11):1104‐1115. [DOI] [PubMed] [Google Scholar]
- 30. Häuser W, Hagl M, Schmierer A, Hansen E. The efficacy, safety and applications of medical hypnosis. Dtsch Arztebl Int. 2016;113(17):289‐296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Keefer L, Palsson OS, Pandolfino JE. Best practice update: incorporating psycho‐gastroenterology into management of digestive disorders. Gastroenterology. 2018;154:1249‐1257. [DOI] [PubMed] [Google Scholar]
- 32. Gonsalkorale WM. Gut‐directed hypnotherapy: the Manchester approach for treatment of irritable bowel syndrome. Int J Clin Exp Hypn. 2006;54(1):27‐50. [DOI] [PubMed] [Google Scholar]
- 33. Palsson OS, Whitehead WE. The growing case for hypnosis as adjunctive therapy for functional gastrointestinal disorders. Gastroenterology. 2002;123(6):2132‐2135. [DOI] [PubMed] [Google Scholar]
- 34. Donnet A‐S, Hasan S, Miller V. PWE‐128 Hypnotherapy for irritable bowel syndrome: the patient’s perception. Gut. 2018;67(Suppl 1):A211‐A212. [Google Scholar]
- 35. Palsson OS, Whitehead WE. Psychological treatments in functional gastrointestinal disorders: a primer for the gastroenterologist. Clin Gastroenterol Hepatol. 2013;11(3):208‐216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Carruthers HR, Miller V, Morris J, Evans R, Tarrier N, Whorwell PJ. Using art to help understand the imagery of irritable bowel syndrome and its response to hypnotherapy. Int J Clin Exp Hypn. 2009;57(2):162‐173. [DOI] [PubMed] [Google Scholar]
- 37. Carruthers HR, Morris J, Tarrier N, Whorwell PJ. The manchester color wheel: development of a novel way of identifying color choice and its validation in healthy, anxious and depressed individuals. BMC Med Res Methodol. 2010;10:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Carruthers HR, Morris J, Tarrier N, Whorwell PJ. Mood color choice helps to predict response to hypnotherapy in patients with irritable bowel syndrome. BMC Complement Altern Med. 2010;10(1):75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Carruthers HR, Morris J, Tarrier N, Whorwell PJ. Reactivity to images in health and irritable bowel syndrome. Aliment Pharmacol Ther. 2010;31(1):131‐142. [DOI] [PubMed] [Google Scholar]
- 40. Carruthers HR, Whorwell PJ. Using pictures to improve communication between doctor and patient in functional gastrointestinal disorders. Aliment Pharmacol Ther. 2014;40(11–12):1364. [DOI] [PubMed] [Google Scholar]
- 41. Klein KB, Spiegel D. Modulation of gastric acid secretion by hypnosis. Gastroenterology. 1989;96(6):1383‐1387. [DOI] [PubMed] [Google Scholar]
- 42. Chiarioni G, Vantini I, De iorio F, Benini L. Prokinetic effect of gut‐oriented hypnosis on gastric emptying. Aliment Pharmacol Ther. 2006;23(8):1241‐1249. [DOI] [PubMed] [Google Scholar]
- 43. Beaugerie L, Burger AJ, Cadranel JF, Lamy P, Gendre JP, Le Quintrec Y. Modulation of orocaecal transit time by hypnosis. Gut. 1991;32(4):393‐394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Simrén M, Ringström G, Björnsson ES, Abrahamsson H. Treatment with hypnotherapy reduces the sensory and motor component of the gastrocolonic response in irritable bowel syndrome. Psychosom Med. 2004;66(2):233‐238. [DOI] [PubMed] [Google Scholar]
- 45. Whorwell PJ, Houghton LA, Taylor EE, Maxton DG. Physiological effects of emotion: assessment via hypnosis. Lancet. 1992;340(8811):69‐72. [DOI] [PubMed] [Google Scholar]
- 46. Lea R, Houghton LA, Calvert El, et al. Gut‐focused hypnotherapy normalizes disordered rectal sensitivity in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2003;17(5):635‐642. [DOI] [PubMed] [Google Scholar]
- 47. Prior A, Colgan SM, Whorwell PJ. Changes in rectal sensitivity after hypnotherapy in patients with irritable bowel syndrome. Gut. 1990;31(8):896‐898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Houghton LA, Calvert EL, Jackson NA, Cooper P, Whorwell PJ. Visceral sensation and emotion: a study using hypnosis. Gut. 2002;51(5):701‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lindfors P, Törnblom H, Sadik R, Björnsson ES, Abrahamsson H, Simrén M. Effects on gastrointestinal transit and antroduodenojejunal manometry after gut‐directed hypnotherapy in irritable bowel syndrome (IBS). Scand J Gastroenterol. 2012;47(12):1480‐1487. [DOI] [PubMed] [Google Scholar]
- 50. Tillisch K, Mayer EA, Labus JS. Quantitative meta‐analysis identifies brain regions activated during rectal distension in irritable bowel syndrome. Gastroenterology. 2011;140(1):91‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mayer EA, Tillisch K. The brain‐gut axis in abdominal pain syndromes. Annu Rev Med. 2011;62:381‐396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Chang L, Berman S, Mayer EA, et al. Brain responses to visceral and somatic stimuli in patients with irritable bowel syndrome with and without fibromyalgia. Am J Gastroenterol. 2003;98(6):1354‐1361. [DOI] [PubMed] [Google Scholar]
- 53. Mertz H, Morgan V, Tanner G, et al. Regional cerebral activation in irritable bowel syndrome and control subjects with painful and nonpainful rectal distention. Gastroenterology. 2000;118(5):842‐848. [DOI] [PubMed] [Google Scholar]
- 54. Naliboff BD, Derbyshire S, Munakata J, et al. Cerebral activation in patients with irritable bowel syndrome and control subjects during rectosigmoid stimulation. Psychosom Med. 2001;63(3):365‐375. [DOI] [PubMed] [Google Scholar]
- 55. Rainville P, Duncan GH, Price DD, Carrier B, Bushnell MC. Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science. 1997l;277(5328):968‐971. [DOI] [PubMed] [Google Scholar]
- 56. Gill M. Anatomy and pathophysiology of chronic pain and the impact of hypnotherapy. Sleep and Hypnosis. 2018l;20(2):85‐90. [Google Scholar]
- 57. Lowén M, Mayer EA, Sjöberg M, et al. Effect of hypnotherapy and educational intervention on brain response to visceral stimulus in the irritable bowel syndrome. Aliment Pharmacol Ther. 2013;37(12):1184‐1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology. 2016;150(6):1393‐1407. [DOI] [PubMed] [Google Scholar]
- 59. Whorwell PJ, Prior A, Faragher EB. Controlled trial of hypnotherapy in the treatment of severe refractory irritable‐bowel syndrome. Lancet. 1984;2(8414):1232‐1234. [DOI] [PubMed] [Google Scholar]
- 60. NICE . Irritable bowel syndrome in adults: diagnosis and management National Institute for Healthcare and Excellence guidelines, 2008; CG61. [PubMed]
- 61. Spiller R, Aziz Q, Creed F, et al. Guidelines on the irritable bowel syndrome: mechanisms and practical management. Gut. 2007;56(12):1770‐1798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Eswaran SL, Chey WD, Han‐Markey T, et al. A randomized controlled trial comparing the low FODMAP diet vs. modified NICE guidelines in US adults with IBS‐D. Am J Gastroenterol. 2016;111(12):1824. [DOI] [PubMed] [Google Scholar]
- 63. Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology. 2014;146(1):67‐75.e5. [DOI] [PubMed] [Google Scholar]
- 64. Böhn L, Störsrud S, Liljebo T, et al. Diet low in FODMAPs reduces symptoms of irritable bowel syndrome as well as traditional dietary advice: a randomized controlled trial. Gastroenterology. 2015;149(6):1399‐1407.e2. [DOI] [PubMed] [Google Scholar]
- 65. McKenzie YA, Bowyer RK, Leach H, et al. British Dietetic Association systematic review and evidence‐based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). J Hum Nutr Diet. 2016;29(5):549‐575. [DOI] [PubMed] [Google Scholar]
- 66. Peters Sl, Yao CK, Philpott H, et al. Randomised clinical trial: the efficacy of gut‐directed hypnotherapy is similar to that of the low FODMAP diet for the treatment of irritable bowel syndrome. Aliment Pharmacol Ther. 2016;44(5):447‐459. [DOI] [PubMed] [Google Scholar]
- 67. Gonsalkorale WM, Houghton LA, Whorwell PJ. Hypnotherapy in irritable bowel syndrome: a large‐scale audit of a clinical service with examination of factors influencing responsiveness. Am J Gastroenterol. 2002;97(4):954‐961. [DOI] [PubMed] [Google Scholar]
- 68. Rutten J, Reitsma JB, Vlieger AM, Benninga MA. Gut‐directed hypnotherapy for functional abdominal pain or irritable bowel syndrome in children: a systematic review. Arch Dis Child. 2013;98(4):252‐257. [DOI] [PubMed] [Google Scholar]
- 69. Rutten J, Vlieger AM, Frankenhuis C, et al. Gut‐directed hypnotherapy in children with irritable bowel syndrome or functional abdominal pain (syndrome): a randomized controlled trial on self exercises at home using CD versus individual therapy by qualified therapists. BMC Pediatr. 2014;14(1):140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Vlieger AM, Menko–Frankenhuis C, Wolfkamp S, et al. Hypnotherapy for children with functional abdominal pain or irritable bowel syndrome: a randomized controlled trial. Gastroenterology. 2007;133(5):1430‐1436. [DOI] [PubMed] [Google Scholar]
- 71. Whorwell PJ. Hypnotherapy: first line treatment for children with irritable bowel syndrome? Arch Dis Child. 2013;98(4):243‐244. [DOI] [PubMed] [Google Scholar]
- 72. Gupta S, Schaffer G, Saps M. Pediatric irritable bowel syndrome and other functional abdominal pain disorders: an update of non‐pharmacological treatments. Expert Rev Gastroenterol Hepatol. 2018;12(5):447‐456. [DOI] [PubMed] [Google Scholar]
- 73. Vlieger AM, Rutten J, Govers A, et al. Long‐term follow‐up of gut‐directed hypnotherapy vs. standard care in children with functional abdominal pain or irritable bowel syndrome. Am J Gastroenterol. 2012;107(4):627‐631. [DOI] [PubMed] [Google Scholar]
- 74. Miller V, Carruthers HR, Morris J, Hasan SS, Archbold S, Whorwell PJ. Hypnotherapy for irritable bowel syndrome: an audit of one thousand adult patients. Aliment Pharmacol Ther. 2015;41(9):844‐855. [DOI] [PubMed] [Google Scholar]
- 75. Houghton LA, Heyman DJ, Whorwell PJ. Symptomatology, quality of life and economic features of irritable bowel syndrome–the effect of hypnotherapy. Aliment Pharmacol Ther. 1996;10(1):91‐95. [DOI] [PubMed] [Google Scholar]
- 76. Forbes A, MacAuley S, Chiotakakou‐Faliakou E. Hypnotherapy and therapeutic audiotape: effective in previously unsuccessfully treated irritable bowel syndrome? Int J Colorectal Dis. 2000;15(5–6):328‐334. [DOI] [PubMed] [Google Scholar]
- 77. Galovski TE, Blanchard EB. The treatment of irritable bowel syndrome with hypnotherapy. Appl Psychophysiol Biofeedback. 1998;23(4):219‐232. [DOI] [PubMed] [Google Scholar]
- 78. Harvey RF, Gunary RM, Hinton RA, Barry RE. Individual and group hypnotherapy in treatment of refractory irritable bowel syndrome. The Lancet. 1989;333(8635):424‐425. [DOI] [PubMed] [Google Scholar]
- 79. Palsson OS, Turner MJ, Johnson DA, Burnett CK, Whitehead WE. Hypnosis treatment for severe irritable bowel syndrome: investigation of mechanism and effects on symptoms. Dig Dis Sci. 2002;47(11):2605‐2614. [DOI] [PubMed] [Google Scholar]
- 80. Vidakovic‐Vukic M. Hypnotherapy in the treatment of irritable bowel syndrome: methods and results in amsterdam. Scand J Gastroenterol. 1999;34(230):49‐51. [DOI] [PubMed] [Google Scholar]
- 81. Lindfors P, Unge P, Arvidsson P, et al. Effects of gut‐directed hypnotherapy on IBS in different clinical settings—results from two randomized, controlled trials. Am J Gastroenterol. 2012;107(2):276. [DOI] [PubMed] [Google Scholar]
- 82. Moser G, Trägner S, Gajowniczek EE, et al. Long‐term success of GUT‐directed group hypnosis for patients with refractory irritable bowel syndrome: a randomized controlled trial. Am J Gastroenterol. 2013;108(4):602. [DOI] [PubMed] [Google Scholar]
- 83. Smith GD. Effect of nurse‐led gut‐directed hypnotherapy upon health‐related quality of life in patients with irritable bowel syndrome. J Clin Nurs. 2006;15(6):678‐684. [DOI] [PubMed] [Google Scholar]
- 84. Lindfors P, Unge P, Nyhlin H, et al. Long‐term effects of hypnotherapy in patients with refractory irritable bowel syndrome. Scand J Gastroenterol. 2012;47(4):414‐420. [DOI] [PubMed] [Google Scholar]
- 85. Gonsalkorale WM, Miller V, Afzal A, Whorwell PJ Long term benefits of hypnotherapy for irritable bowel syndrome. Gut. 2003;52(11):1623‐1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Lindfors P, Ljótsson B, Bjornsson E, Abrahamsson H, Simrén M. Patient satisfaction after gut‐directed hypnotherapy in irritable bowel syndrome. Neurogastroenterol Motil. 2013;25(2):169‐e86. [DOI] [PubMed] [Google Scholar]
- 87. Whorwell PJ, McCallum M, Creed FH, Roberts CT. Non‐colonic features of irritable bowel syndrome. Gut. 1986;27(1):37‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Gonsalkorale WM, Toner BB, Whorwell PJ. Cognitive change in patients undergoing hypnotherapy for irritable bowel syndrome. J Psychosom Res. 2004;56(3):271‐278. [DOI] [PubMed] [Google Scholar]
- 89. Roberts L, Wilson S, Singh S, Roalfe A, Greenfield S. Gut‐directed hypnotherapy for irritable bowel syndrome: piloting a primary care‐based randomised controlled trial. Br J Gen Pract. 2006;56(523):115‐121. [PMC free article] [PubMed] [Google Scholar]
- 90. Riehl ME, Keefer L. Hypnotherapy for esophageal disorders. Am J Clin Hypn. 2015;58(1):22‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Farmer AD, Ruffle JK, Aziz Q. The role of esophageal hypersensitivity in functional esophageal disorders. J Clin Gastroenterol. 2017;51(2):91‐99. [DOI] [PubMed] [Google Scholar]
- 92. Riehl ME, Pandolfino JE, Palsson OS, Keefer L. Feasibility and acceptability of esophageal‐directed hypnotherapy for functional heartburn. Dis Esophagus. 2016;29(5):490‐496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Kiebles Jl, Kwiatek MA, Pandolfino JE, Kahrilas PJ, Keefer L. Do patients with globus sensation respond to hypnotically assisted relaxation therapy? A case series report. Dis Esophagus. 2010;23(7):545‐553. [DOI] [PubMed] [Google Scholar]
- 94. Aziz Q, Fass R, Gyawali CP, Miwa H, Pandolfino JE, Zerbib F. Functional esophageal disorders. Gastroenterology. 2016;150(6):1368‐1379. [DOI] [PubMed] [Google Scholar]
- 95. Yadlapati R, Tye M, Keefer L, Kahrilas PJ, Pandolfino JE. Psychosocial distress and quality of life impairment are associated with symptom severity in PPI non‐responders with normal impedance‐pH profiles. Am J Gastroenterol. 2018;113(1):31‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Jones H, Cooper P, Miller V, Brooks N, Whorwell PJ. Treatment of non‐cardiac chest pain: a controlled trial of hypnotherapy. Gut. 2006;55(10):1403‐1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Miller V, Jones H, Whorwell PJ. Hypnotherapy for non‐cardiac chest pain: long‐term follow‐up. Gut. 2007;56(11):1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Stanghellini V, Chan F, Hasler WL. Gastroduodenal disorders. Gastroenterology. 2016;150(6):1380‐1392. [DOI] [PubMed] [Google Scholar]
- 99. Calvert EL, Houghton LA, Cooper P, Morris J, Whorwell PJ. Long‐term improvement in functional dyspepsia using hypnotherapy. Gastroenterology. 2002;123(6):1778‐1785. [DOI] [PubMed] [Google Scholar]
- 100. Keefer L, Drossman DA, Guthrie E, et al. Centrally mediated disorders of gastrointestinal pain. Gastroenterology. 2016;150(6):1408‐1419. [DOI] [PubMed] [Google Scholar]
- 101. Nozu T, Kudaira M. Altered rectal sensory response induced by balloon distention in patients with functional abdominal pain syndrome. Biopsychosoc Med. 2009;3:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Keefer L, Mandal S. The potential role of behavioral therapies in the management of centrally mediated abdominal pain. Neurogastroenterol Motil. 2015;27(3):313‐323. [DOI] [PubMed] [Google Scholar]
- 103. Flik CE, Laan W, Zuithoff N, et al. Efficacy of individual and group hypnotherapy in irritable bowel syndrome (IMAGINE): a multicentre randomised controlled trial. Lancet Gastroenterol Hepatol. 2019;4(1):20‐31. [DOI] [PubMed] [Google Scholar]
- 104. Flik CE, van Rood YR, Laan W, et al. A randomised controlled trial on hypnotherapy for irritable bowel syndrome: design and methodological challenges (the IMAGINE study). BMC Gastroenterol. 2011;11:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Lövdahl J, Palsson OS, Ringström G, Törnblom H, Simrén M. OP282 Individual versus group hypnotherapy for IBS: A Randomized Controlled Trial. United European Gastroenterol J. 2017;5(Supplement 1):A120. [Google Scholar]
- 106. Lindfors P, Unge P, Arvidsson P, et al. Effects of gut‐directed hypnotherapy on IBS in different clinical settings‐results from two randomized, controlled trials. Am J Gastroenterol. 2012;107(2):276‐285. [DOI] [PubMed] [Google Scholar]
- 107. Miller V, Carruthers H, Morris J, Hasan SS, Archbold S, Whorwell PJ. Letter: efficacy of hypnotherapy in one thousand patients with irritable bowel syndrome–authors' reply. Aliment Pharmacol Ther. 2015;41(11):1223‐1224. [DOI] [PubMed] [Google Scholar]
- 108. Hasan SS, Pearson JS, Morris J, Whorwell PJ. Skype hypnotherapy for irritable bowel syndrome: effectiveness and comparison with face to face treatment. Int J Clin Exp Hypn. 2019;67:69‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Lövdahl J, Ringström G, Agerforz P, Törnblom H, Simrén M. Nurse‐administered, gut‐directed hypnotherapy in IBS: efficacy and factors predicting a positive response. Am J Clin Hypn. 2015;58(1):100‐114. [DOI] [PubMed] [Google Scholar]
- 110. Vasant DH, Solanki K, Balakrishnan S, Radhakrishnan NV. Integrated low‐intensity biofeedback therapy in fecal incontinence: evidence that "good" in‐home anal sphincter exercise practice makes perfect. Neurogastroenterol Motil. 2017;29(1);e12912. [DOI] [PubMed] [Google Scholar]
- 111. Vasant DH, Solanki K, Radhakrishnan NV. Rectal digital maneuvers may predict outcomes and help customize treatment intensity of biofeedback in chronic constipation and dyssynergic defecation. Dis Colon Rectum. 2017;60(1):e2. [DOI] [PubMed] [Google Scholar]
- 112. Krouwel M, Greenfield S, Farley A, Ismail T, Jolly K. Factors which affect the efficacy of hypnotherapy for IBS: Protocol for a systematic review and meta‐regression. Eur J Integr Med. 2018;21:58‐62. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


