Summary
Islamic religious settings (IRS) may be useful places to implement obesity interventions for Muslims. However, little is known about the level and nature of such activity in these settings. We searched bibliographic databases and grey literature, and requested grey information from Muslim organizations, local councils, and mosques in 13 selected areas in the United Kingdom. Thirty‐five interventions were identified; most were poorly described and not evaluated. Twenty‐seven interventions focused on physical activity behaviours, four on diet behaviours, one on both behaviours, and seven addressed long‐term conditions associated with obesity. Most interventions were led by volunteers from the congregation/faith leaders and were funded through donations from congregants or charity organizations. The evidence suggests that health promotion interventions in IRS have a relatively high reach. Obesity interventions are commonly delivered in UK IRS. Most target physical activity behaviours, are instigated and led by volunteers from the congregation or faith leaders, receive no public funding, and are only recorded in people's memories. High‐quality evaluations of well‐specified interventions in this context are needed. We suggest that the methods used in this review, including the learning around positionality of researchers, could be adopted by other researchers as a way to locate opportunities for effective community‐level interventions.
Keywords: health promotion, interventions, Islamic religious settings, obesity
1. INTRODUCTION
Almost three million Muslims live in England and Wales and are a diverse population. The largest group of Muslims living in England and Wales are Asians (68%), primarily Pakistani (38%), and Bangladeshi (15%) Asians.1 The majority of Pakistanis and Bangladeshis living in the United Kingdom are Muslim, but not all. Pakistan and Bangladesh are two of the eight countries which make up South Asia; the others are Afghanistan, Bhutan, Sri Lanka, India, the Maldives, and Nepal. Much of the work in the scientific literature on health promotion in Muslims living in the United Kingdom refers to South Asians. Other ethnic groups with significant Muslim subpopulations include black African/Caribbean (10%), white (8%), and Arab (7%).
Although data on the prevalence of obesity by religious status (eg, Muslims) in the United Kingdom are not available, data on the prevalence of obesity by ethnicity are available. The same is true for data on dietary and physical activity behaviours. As such, we present data for South Asians and, where available, Pakistani and Bangladeshi populations, living in the United Kingdom. El‐Sayed et al found no consensus about obesity prevalence among South Asian children or South Asian adults relative to Caucasians in their systematic review of ethnic inequalities in the United Kingdom.2 However, their findings suggested a possible sexual dimorphism with regard to obesity risk. They found that South Asian boys may have higher risk for obesity relative to Caucasians, while South Asian girls may have lower risk for obesity relative to Caucasians. This dimorphism seems to shift among South Asian adults. Several of the studies suggest a sexual dimorphism in risk for obesity among South Asian adults relative to Caucasian adults that is opposite to the dimorphism observed among children. El‐Sayed et al also observed that the choice of obesity metrics may bias estimates of obesity prevalence among South Asian children and adults. The authors suggest that weight‐for‐height metrics, such as the BMI, may systematically underestimate obesity relative to adiposity metrics, such as DXA or skin‐fold measurements among South Asian children and adults in the United Kingdom. South Asian adults in the United Kingdom may accumulate more weight around the abdomen and have greater adiposity in general, than Caucasians, as all of the studies concerned with ethnic differences in obesity between South Asian adults and Caucasian adults in the United Kingdom which measured waist circumference or waist/hip ratio as metrics of obesity found that South Asian adults had significantly larger waists and higher waist/hip ratios than their Caucasian counterparts.
Muslims, in general, share many health beliefs, values, and experiences that impact on energy balance (dietary and physical activity) behaviours related to obesity across ethnic and racial lines.3 For example, one UK study found that after adjusting for deprivation and other sociodemographic characteristics, South Asian children were three times more likely to have an obesogenic lifestyle than white children.4 Research has shown substantial higher intakes of sugar and fat and greater levels of sedentary behaviour amongst Pakistani compared with white British Infants.5, 6 These obesogenic behaviours persist into childhood. For example, in the Child Heart Health Study in England, substantial differences in diet (higher total energy, fat, and protein intake) and physical activity (lower levels) were found in South Asian compared with white European children age 9 to 10, with particularly low levels of physical activity in South Asian girls.7 In adults, physical activity levels were consistently lower in UK South Asians than in white participants, when assessed from the Health Survey for England.8 Also in adults, the average consumption of fruit and vegetables, and fat intake, was lower among South Asian than in white participants, when assessed from this survey.9 Leung and Stanner provide a comprehensive and informative review of the limited data available on diets of South Asians in the United Kingdom and the challenges and opportunities for health promotion.9 Ethnic inequalities in health, including obesity, in the UK result from a combination of metabolic, socioeconomic, cultural, and implementation (of interventions) factors.10, 11 Deprivation is associated with inequalities in health, and in the United Kingdom, Muslim children and their families are over‐represented in such areas. A report from the Social Mobility Commission found that Muslims experience the greatest economic disadvantages of any group in UK society.12 They are more likely than non‐Muslims to experience neighbourhood deprivation, housing, educational and health disadvantage, and unemployment. The report concluded that there was a “broken social mobility promise” for young Muslims where educational success did not translate into good labour market outcomes.
There is also evidence that universal health promoting interventions are taken up more effectively by white compared with ethnic minority groups and therefore further widen ethnic inequalities in health.13 There is reasonable evidence that access and recruitment to universal interventions is a significant issue for some ethnic populations and can contribute to health inequalities.14 Bhopal also argues that approaches to, and characteristics of, the intervention itself can contribute to differential effectiveness.15 Differential effectiveness may arise at a number of points in the implementation of an intervention, including intervention efficacy, service provision or access, uptake, and compliance.16 A common assumption is that health promotion interventions found to be effective in the general population are also, if appropriately adapted, likely to prove effective when provided to ethnic minority populations, but there is limited evidence available to verify this claim.13
A UK government report published in 2007 acknowledged the possible role that places of worship could have in promoting health, listing faith groups as potentially important partners.17 In 2015, the Muslim Council of Britain stated that Muslim opinion makers such as mosque imams have a responsibility to promote health messages to their networks and congregations.18 A recent study by Maynard et al provides some evidence that health promotion interventions for children delivered in mosques may be more successful in terms of reach, compared with schools.19
Reasons why Islamic religious settings (IRS) may be particularly useful for targeted health promotion interventions for Muslims include (1) capitalizing upon the social support that the setting provides for adoption of healthy lifestyle behaviours20; (2) trust placed by the target population in religious leaders which may promote willingness to take part in advocated behaviours (such as physical activity) and to allay concerns relating to faith and cultural appropriateness21; (3) availability of tangible resources to support the delivery of an intervention (eg, a space to host an intervention, a volunteer base to facilitate and deliver an intervention)22; (4) the stable nature of IRS in the lives of the community they serve and frequent attendance,23 which facilitates sustainability of adopted behaviours; and (5) access to and opportunity to engage with hard‐to‐reach groups who may not access health services.24 In the current times of austerity where local authorities in the United Kingdom have sparse resources to direct towards pressing public health issues, it is timely to explore how community‐level settings, such as IRS, can contribute towards health promotion.
The aim of this scoping review and systematic mapping was to identify and describe the level and nature of health promotion interventions associated with obesity in IRS in the United Kingdom, and evaluations of them where available. From an initial search of bibliographic databases for relevant information, we identified only one intervention. However, in discussion with our project steering group, that included faith leaders, we understand that such interventions are common place in IRS in the United Kingdom.
The question of why research on health promotion interventions in IRS in the United Kingdom has been relatively uncommon compared with other settings is a potential cause for concern.25 Understanding reasons for the relative lack of research in this context could address a hidden area of generation and perpetuation of health inequalities and disparities. Sheikh asks those with the power to change the way in which research is conducted to translate the important insights around willingness to participate in research into significantly more invitations extended to minority ethnic and racial groups to participate.25 Thomas et al, in their paper entitled Toward a Fourth Generation of Disparities Research to Achieve Health Equity, suggest that the reductionist nature of randomized controlled trials as the gold standard for scientific evidence has advanced our mechanistic and biomedical understanding of obesity at the expense of understanding social and environmental determinants of the obesity epidemic.26 Paeratakul et al predict that the absence of evidence‐based studies and interventions for minority populations will perpetuate the problem of disproportionate burden of obesity among ethnic minorities compared with the white population.27 Thomas et al state that the opportunity is to recognize health disparities as an ethical issue of justice because specific groups were subjected to systematic racial discrimination and denied the basic benefits of society, a violation of the social contract.26 As Powers and Faden28 state,
One critical moral function of public health…is to monitor the health of those who are experiencing systematic disadvantage as a function of group membership, to be vigilant for evidence of inequities relative to those in privileged social groups and to intervene to reduce those inequalities. (p. 88)
Thomas et al argue that, because this situation places health disparities in a category of injustices deemed morally problematic, it demands achieving what we have thus far failed to do adequately, such as critically examine racism and race in a meaningful way and develop interventions that allow us to take direct action to eliminate health disparities.26
Given the relative lack of research on health promotion interventions in IRS in the United Kingdom that has been published in peer review journals and subject to systematic review, we used a broad approach to searching, and our inclusion criteria, for this review compared with a conventional systematic review. We did not aim to collate a comprehensive list of every relevant intervention in the United Kingdom at one point in time. Rather, we reviewed all available evidence that we could find through searching bibliographic databases and the grey literature and scoped for grey information from a targeted selection of Muslim organizations, local councils, mosques, and local health authorities and local councils.
2. METHODS
We undertook a scoping review and systematic mapping of the evidence, using methods adapted from previously published literature.29, 30 Ethical approval for our searching for relevant grey information was granted by the Research Ethics Panel, University of Bradford, UK (ethics application: E645 approved on 9 October 2017).
2.1. Inclusion criteria
This review was part of a larger research project, funded by the National Health Research Institute (UK) [Programme Development Grant award RP‐DG‐1215‐10002], which aimed to assess the feasibility of developing interventions to tackle obesity in IRS. At the protocol development stage, and in discussion with the project steering group31 which included Muslim faith leaders, it was agreed to broaden the search for evidence for our scoping review to include any health promotion intervention in IRS for two reasons: first, to gain learning and understanding of factors relating to health promotion intervention development and implementation in IRS, which could potentially be translated for interventions which aim to tackle obesity in these settings and second, to ensure that we included interventions which may help tackle obesity but are not labelled as such. An example was project number 53's stated aim, which was to promote healthy living, but the intervention content specifically focused on promoting physical activity and an awareness of obesity.
We defined IRS to include mosques (predominately attended by men), madrasas (Islamic schools where children are taught daily), halaqas (group meetings to study Islam, also sometimes called women's circles when these meetings are exclusively for females), Muslim charity organizations, and Muslim sports or physical activity groups. We also included in our definition those interventions that were organised by local Islamic religious communities but were delivered beyond the mosque, madrassa, or halaqas (eg, physical activity interventions which took place in public spaces such as local parks and leisure centres). Quantitative and qualitative evidence was considered. Evidence in the context of this scoping review was defined as published research, grey literature, and grey information (which included written and spoken word, evidence not available online).
2.2. Searching for evidence
A search was conducted using the methods described by Adams et al.29 This approach is particularly useful when searching for information around public health interventions, which have traditionally not been subject to scientific study, but are relatively common in practice. It includes searching for (1) published research (bibliographic databases), (2) grey literature (websites), and (3) grey information (contacting relevant organizations and individuals for information which is recorded only on paper or in a person's memory).
Published research was searched using bibliographic databases (Assia, CINAHL, Embase, MEDLINE, PsycInfo, SSCI, and The Cochrane Library). We did not restrict our search of bibliographic databases to interventions in IRS in the United Kingdom, but we did restrict our search for such evidence to the United Kingdom when searching the grey literature and grey information. Grey literature was searched using Google, the NIHR portfolio and website, and health websites (NICE and Public Health England (PHE)). These searches were initially conducted in October 2017 and updated in October 2018 so that we could include the most up‐to‐date evidence. The combination of keywords used for these searches can be found in Table S1.
For the bibliographic databases, one reviewer (KR) screened all search results on titles and abstracts and subsequently the full‐text articles of those search results which were considered candidates for inclusion. For the grey literature, one reviewer (KR) screened for IRS from the first 100 results from each website searched. A shortlist of interventions was independently assessed by another reviewer (CS), and the list of interventions included in this review was agreed on by KR and CS. Evidence included in this scoping review was extracted by KR using an agreed upon data extraction form.
For the grey information, one reviewer (SD) conducted the majority of information requests. KR conducted a few information requests in Birmingham. As suggested by one of the journal reviewers for this paper, we here describe the positionality of these researchers relative to the religious, ethnic, and linguistic status of the UK communities we attempted to contact. SD is male, Muslim, Pakistani, of Punjabi origins, and is fluent in Punjabi, Urdu, Arabic, Farsi, and English. KR is female, Sikh, British Indian, and is fluent in Punjabi and English. First, relevant Muslim charity organizations and Muslim community organizations that operate in the UK were contacted (by email initially and then by phone if they did not reply to the email) for information on any relevant local or national interventions in the United Kingdom. Details for persons and/or organizations to be contacted were initially scoped from the expert knowledge of members of the project steering group and also a simple Google search. A snowballing approach to identifying information was used, by requesting details of other relevant organizations from initially identified Muslim charity and community organizations.
We also directly contacted local councils, mosques, and local health authorities (by email initially and then by phone if they did not reply to the email). When contacting local councils, we requested to speak with Muslim councillors where possible. Given that the aim of our research was to primarily identify and describe health promotion interventions in IRS in the United Kingdom, rather than collate a comprehensive list of every relevant intervention in the United Kingdom at one point in time, we used a targeted approach and focused our efforts only on areas in the United Kingdom with the highest Muslim populations (extracted from the most recent UK census data on ethnicity32). At the protocol development stage, we decided to target only the top 10 areas in the United Kingdom. However, we found that all of these areas were in England. In order to include information from across the United Kingdom, in discussion with the project steering group, we agreed to additionally include the area with the highest Muslim populations in Scotland, Northern Ireland, and Wales (Table S2). One reviewer (SD) assessed all grey information received for relevance. A shortlist of interventions was independently assessed by another reviewer (KR), and any queries discussed with CS. The final list of interventions included in this review was agreed on by SD, KR, and CS. Literature included in this scoping review was extracted by SD using an agreed‐upon data extraction form and checked by KR.
We acknowledge that, for information found in grey literature and grey information, there is a potential risk of bias and thus value of that information. As suggested by Adams et al,29 we assumed that the risk of bias relating to the description of interventions was low—there is little reason why such information would be misrecorded. In contrast, we assumed that the risk of bias of evaluations of interventions was high, due to methodological weakness and conflicts of interest.
2.3. Data extraction
Data were extracted for each intervention using standardised forms, which were pilot tested using five (randomly selected) of the included interventions identified from five different sources (bibliographic databases, Google search, website search, email information request, and telephone call information request). The format of the forms was then revised, in discussion with KR, SD, and CS. An example of a revision we made to the form was the inclusion of the collection of information for impetus of the intervention. [The data extraction form can be requested from the authors.] Information extracted included:
The funding source for the intervention
The aim(s) of the intervention
The impetus for the intervention
Target population and recruitment methods
Topic/area focus of the intervention
Intervention content
Intervention setting
Intervention duration and frequency
Intervention delivery team (and any training and support they had or received).
Evaluation of the intervention.
2.4. Systematic mapping
We define systematic mapping in this context as checking for any duplicate interventions identified by more than one method of searching. As we anticipated, some of the included interventions were identified by more than one method of searching. All interventions were systematically mapped by KR and SD, and duplicates removed. Results of the scoping review and systematic mapping were synthesized narratively.
3. RESULTS
Thirty‐five health promotion interventions that were directly associated with obesity were identified from the systematic search and mapping process (Figure 1). Interventions were categorised as being directly associated with obesity where they aimed to specifically improve physical activity and/or dietary intake behaviours, or improve long‐term conditions associated with obesity. The stated aim of most of the 35 interventions was to simply increase physical activity, promote healthy eating, or both. However, for 7 of the 35 interventions, the stated aim was to improve long‐term chronic conditions associated with obesity (project numbers 6, 27, 31, 34, 38, 51, and 52). After deduplication, 1 of these 35 interventions was identified from bibliographic databases, 9 from grey literature (seven of which were also identified from grey information), and 25 from only grey information. Brief details of these 35 interventions can be found in Table 1, and a concise description of these interventions can be found in Table 2.
Figure 1.
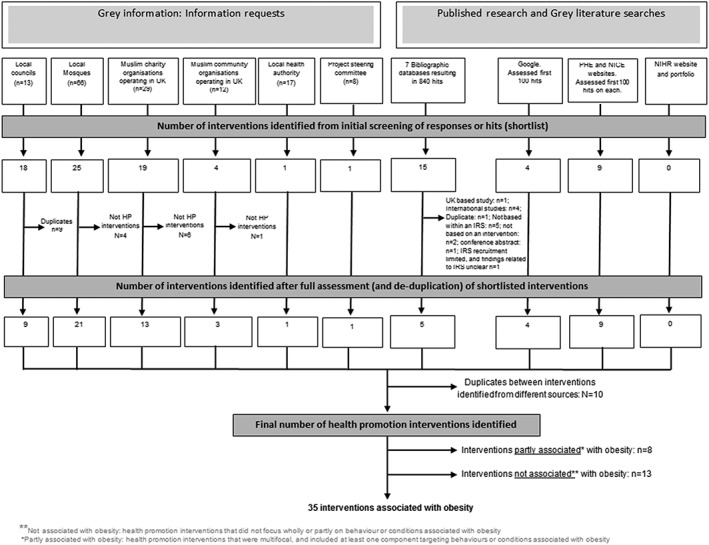
Systematic search and mapping of interventions of health promotion interventions within Islamic religious settings
Table 1.
Characteristics (study design, intervention description, method of identification, data source, and outcome measures) of health promotion interventions associated with obesity (n = 35)
| Project Reference Number | Authors or Organization Which Provided Information | Study Design (If Applicable), Name or Description of Intervention and Location | Method of Identification | Participant Characteristics, Description of Outcome Measure and Data Source (If Applicable) |
|---|---|---|---|---|
| 3 | Banerjee et ala | Pre and post intervention study Mosque‐based physical activity intervention Canada | Bibliographic databases |
Characteristics N = 28 Female (%): 100 Mean age (SD): 51.0 (12.0) Ethnicity (%): Indian: 82.0% Pakistani: 18% Outcome measures
|
| 6 | East London Mosque, London Muslim Centre and NHS Tower Hamletsb |
Faith in health East London |
|
Website address: http://www.eastlondonmosque.org.uk/content/faith-health |
| 8 |
Streatham mosquec |
No specific name, physical activity classes Streatham |
Website address: http://www.streathammosque.org/ | |
| 9 | Ipswich mosqued |
No specific name, physical activity classes Ipswich |
Website address: http://www.ipswichmosque.org/our_aims.php | |
| 10 | KSIMC Birmingham Mosquee |
Community salad for Iftar Birmingham |
|
Website address: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/619891/Guide_to_Healthy_Living_Mosques.PDF |
| 11 | Ghamkol Sharif Central Jamia Mosquee |
Children's healthy eating and sports Birmingham |
|
Website address: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/619891/Guide_to_Healthy_Living_Mosques.PDF |
| 12 | KSIMC Birmingham Mosquee |
Health and well‐being champion Birmingham |
|
Website address: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/619891/Guide_to_Healthy_Living_Mosques.PDF |
| 13 | KSIMC Birmingham Mosquee |
Volunteer sports committee Birmingham |
|
Website address: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/619891/Guide_to_Healthy_Living_Mosques.PDF |
| 14 | Ghamkol Sharif Central Jamia Mosquee |
Park walks in‐between prayers Birmingham |
|
Website address: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/619891/Guide_to_Healthy_Living_Mosques.PDF |
| 17 | Birmingham Central Mosquee |
Health‐exchange signposting Birmingham |
|
Website address: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/619891/Guide_to_Healthy_Living_Mosques.PDF |
| 19 | Bikeworks |
Bikeworks Tower Hamlets, London |
Community organization | Personal communication (telephone) |
| 20 | East London Mosque |
Muslim charity run London |
Mosque | Personal communication (telephone) |
| 23 | Jamiyat Tabligh‐ul‐Islam Mosque |
No specific name, group walking Bradford |
Mosque | Personal communication (telephone) |
| 24 | Madni Masjid |
No specific name, education on healthy eating Bradford |
Mosque | Personal communication (telephone) |
| 27 | Luton Central Mosque |
No specific name, education on long‐term conditions,health assessments, advice and signposting to services Luton |
Mosque | Personal communication (telephone) |
| 30 | Active Luton |
Active Luton Luton |
Community organization | Personal communication (telephone) |
| 31 | Bury Park Masjid |
Bury Park Masjid Luton |
Mosque | Personal communication (telephone) |
| 32 |
Unknown |
The Big Iftaar Luton |
Muslim charity organization | Personal communication (telephone) |
| 34 | Jamea Masjid and Islamic Centre |
Bowel cancer screening project Slough |
Mosque | Personal communication (telephone) |
| 35 | Jamea Masjid and Islamic Centre |
No specific name, various physical activities Slough |
Mosque | Personal communication (telephone) |
| 38 | Oldham Central Mosque |
No specific name, education on chronic disease Greater Manchester |
Mosque | Personal communication (telephone) |
| 39 | Oldham Central Mosque |
No specific name, education on healthy eating Greater Manchester |
Mosque | Personal communication (telephone) |
| 41 | Social Justice Charity |
No specific name, physical activity Newport |
Muslim charity organization | Personal communication (telephone) |
| 42 | Belfast Islamic Centre |
No specific name, physical activity Belfast, Northern Ireland |
Mosque | Personal communication (email) |
| 43 | Belfast Islamic Centre |
No specific name, physical activity Belfast, Northern Ireland |
Mosque | Personal communication (email) |
| 46 | Ilford Central Mosque |
No specific name, physical activity Redbridge |
Mosque | Personal communication (telephone) |
| 47 | Seven Kings Mosque |
No specific name, physical activity Redbridge |
Mosque | Personal communication (telephone) |
| 48 | Muslim Youth Community Centre |
Muslim Youth Foundation Manchester |
Muslim charity organization | Personal communication (telephone) |
| 49 | Ashton Central Mosque |
No specific name, physical activity Manchester |
Mosque | Personal communication (telephone) |
| 50 | Active Sisters |
Active sisters London |
Muslim charity organization | Personal communication (telephone) |
| 51 | Birmingham Central Mosque |
No specific name, increasing awareness of chronic conditions and screening programme Birmingham |
Mosque | Personal communication (telephone) |
| 52 | Sufi Trust |
No specific name, education on chronic conditions Birmingham |
Muslim charity organization | Personal communication (telephone) |
| 53 | Sufi Trust |
Active weekends Birmingham |
Muslim charity organization | Personal communication (telephone) |
| 54 | Association of Muslim Schools |
Interfaith games Birmingham |
Muslim charity organization | Personal communication (email) |
| 55 | Ghausia Mosque |
No specific name, physical activity Pendle, Lancashire |
Mosque | Personal communication (telephone) |
Banerjee ET, Landry M, Zawi M, Childerhose D, Stephens N, Shafique A, et al. A pilot examination of a mosque‐based physical activity intervention for South Asian Muslim women in Ontario, Canada. Journal of Immigrant and Minority Health. 2017;19 (2):349–57.
East London Mosque, London Muslim Centre. Faith in Health 2017. Available from: http://www.eastlondonmosque.org.uk/content/faith-health.
Streatham Mosque. Daily activities at Masjid 2017. Available from: http://www.streathammosque.org/.
Ipswich mosque. Activities 2017. Available from: http://www.ipswichmosque.org/our_aims.php.
Public Health England. Guide to Healthy Living: Mosques 2017. Available from: http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/619891/Guide_to_Healthy_Living_Mosques.PDF.
Table 2.
Aim and characteristics of health promotion interventions associated with obesity, and their evaluation where available (n = 35)
| Project Reference, Dates of Projectf, and Funding Source | Aim | Target Population and Recruitment Methods | Intervention | Evaluation Results | ||||
|---|---|---|---|---|---|---|---|---|
| Topic/Area | Intervention Content | Setting | Intervention Duration and Frequency | Intervention Delivery Team (and Training) | ||||
|
3a Year: 2014 Funding: part funded by a research grant.
One author working at the Women's Xchange (research centre) at Women's College Hospital was supported by a research funding body (Canadian Institute for Health Research) via a postdoctoral fellowship award. |
To assess the feasibility, acceptability, and effectiveness of a mosque‐based physical activity program for South Asian women The Women's Xchange (research centre) at Women's College Hospital. One author was supported by a research funding body (Canadian Institute for Health Research) via a postdoctoral fellowship award. |
South Asian women in Ontario, Canada.
Inclusion criteria: South Asian (originated from India, Sri Lanka, Pakistan or Bangladesh), member of the Islamic faith and mosque community and ≥18 years. |
Physical activity | The intervention involved:
|
Mosque in Ontario, Canada.
Activities were carried out in the women's' prayer area |
Intervention was carried out between June and December 2014. The 24‐wk program was offered to three times a week (evenings only) to the participants. Duration of the session: 1 h |
Health professionals/workers Kinesiologists delivered the intervention alongside a female community member. Kinesiologists were trained by physiotherapists, a kinesiologist, and a nurse practitioner. Study investigators observed the sessions on a number of occasions to assess the delivery of the program |
Feasibility Class attendance: Average number attending each session (range): 13 (3‐28) Average number of classes attended (range): 20 (1‐51) Acceptability median readiness towards exercise score (IQR): Pre: 80 (60‐100) Post: 100 (70‐100) P value: .29
Median importance of participating in exercise score (IQR): Pre: 90 (50‐100) Post: 100 (90‐100) P value: .004
Median confidence related to exercise participation score (IQR): Pre: 90 (70‐100) Post: 100 (80‐100) P value: .013
Overall experience: Participants completed 12 questions (5‐point Likert scale) which indicated participants had a positive experience of the program: convenient, easy to follow, educational, helpful, and supportive. International Physical Activity Questionnaire (IPAQ) score (n, %): 1. Inactive pre: n = 8 (42%); post: n = 2 (10%) 2. Meet the Canadian Physical Activity Guidelines (CPAG) pre: n = 10 (53%); post: n = 10 (53%) 3. Exceed the CPAG pre: n = 1 (5%); post: n = 7 (37%) P value: .006
Duke Activity Status Index (DASI) mean score (SD) pre: 39.2 (12.1) post: 44.6 (10.9) P value: .06 |
|
6b Project dates unclear Funding: unknown |
To increase awareness in the community of the available health services |
Those living in Tower Hamlets Recruitment methods unclear |
Health promotion related to long‐term conditions | Unclear. However, some information on
|
Mosques (n = 45) and GP surgeries (? N = unclear) in Tower Hamlets | Unclear. | Unclear |
No evaluation reported |
|
8c
Project dates unclear Funding: unknown |
Unclear (not stated) |
Those attending Streatham mosque Recruitment methods unclear |
Physical activity |
|
Streatham mosque | Unclear | Unclear |
No evaluation reported |
|
9d Project dates unclear Funding: unknown |
Unclear (not stated) |
Those attending Ipswich mosque Recruitment methods are unclear |
Physical activity |
|
At Ipswich mosque or another location(s) | Unclear | Unclear |
No evaluation reported |
|
10e Project dates unclear Funding: unknown |
Unclear (not stated) |
Mosque attendees Recruitment methods are unclear |
Diet |
|
KSIMC Birmingham Mosque | Limited details, but appears to be during the month of Ramadhan. | Unclear |
No evaluation reported |
|
11e Project dates unclear Funding: unknown |
Unclear (not stated) |
Children attending the madrassa classes at the mosque Recruitment methods are unclear |
|
Limited details provided. Healthy eating and sports initiative mentioned. | Unclear where the physical activity sessions are carried out. | Unclear |
Unclear Sports initiative run by youth volunteers, but no detail of where these volunteers were drawn from. |
No evaluation reported |
|
12e Project dates unclear Funding: unknown |
Unclear (not stated) | Unclear |
Limited details. Physical activity mentioned. |
Limited details.
|
Unclear Mentions community setting. |
Unclear | Unclear |
No evaluation reported |
|
13e Project dates unclear Funding: unknown |
Unclear (not stated) | Unclear | Physical activity |
|
Some sessions held at Bordesley Green school, Birmingham | Unclear | Unclear |
No evaluation reported |
|
14e Project dates unclear Funding: unknown |
Unclear (not stated) |
Mosque attendees Recruitment methods unclear |
Physical activity |
|
Local park in Birmingham | Unclear | Unclear |
No evaluation reported |
|
17e Project dates unclear Funding: unknown |
Improve the health and well‐being of the community |
Unclear (presume mosque community) Recruitment via announcements during Friday sermons |
Mental health Physical health Raising awareness of diabetes |
Limited details but included physical activity | Mosque in Birmingham | Unclear |
Health professionals/workers Health trainer Limited details, about other members involved in this intervention. |
No evaluation reported |
| Project reference, dates of project and funding source | Aims and (where information forthcoming) impetus for intervention | Population and recruitment | Intervention | Evaluation results | ||||
|---|---|---|---|---|---|---|---|---|
| Topic or area | Intervention description | Setting | Intervention duration | Details of intervention team | ||||
|
19 Project name: Bikeworks Dates: Unknown Funding: Bikeworks is a social enterprise funded by a number of organizations (eg, Barclays Bank [primary funder], local authorities, businesses) |
To encourage cycling within the community and improve physical health |
Project recruited those living within Tower Hamlets Recruitment: volunteers and/or activists within mosques recruited those who attend the mosques(s) |
Physical activity |
|
Cycling outdoors within Tower Hamlets. Exact location (eg, cycling routes or parks) was unclear |
|
Social enterprise Bikeworks delivered intervention |
Evaluation of process or implementation only: Project team mentioned Muslim males attended in groups, whereas Muslim females took part in the individual cycling sessions |
|
20 Project name: Muslim charity run Dates: annual event (start date unknown) Funding: Muslim charity organizations (eg, Islamic Relief Worldwide, Muslim Aid, Muslim Hands) |
To promote healthier lifestyles and help with fundraising for other Muslim charities |
Open to all those within the UK; however, majority of participants included Muslims living within Tower Hamlets Recruitment methods unclear |
Physical activity |
|
Victoria Park, London |
|
Islamic faith leaders
|
No evaluation reported |
|
23 Project name: no name available Dates: ongoing project (start date unknown) Funding: donations from mosque attendees |
Improve physical fitness |
Those attending Jamiyat Tabligh‐ul‐Islam Mosque, Bradford Recruitment methods unclear |
Physical activity |
|
|
Sessions took place once a day and length of session were 15 to 30 min, but unclear whether participants were expected at all sessions. |
Islamic faith leaders
|
No evaluation reported. |
|
24 Project name: no name available Dates: 2007 (one‐off event) Funding: donations from mosque attendees |
Promote healthy eating during Ramadhan |
Mosque attendees at Madni Masjid, Bradford Recruitment methods unclear |
|
Specific details about the intervention were unavailable. Some components included:
|
Madni Masjid, Bradford | Education provided daily during the month of Ramadhan in 2007. However, frequency and lengths of the sessions were unclear. | Islamic faith leader
|
No evaluation reported. |
|
27 Project name: no name available Dates: ongoing (start date unknown) Funding: no funding, intervention carried out on a voluntary basis by a mosque attendee |
To promote general health and well‐being among those who attend the mosque |
Those who attend Luton Central Mosque, Luton
Recruitment: mosque attendees informed by mosque volunteers about the GP drop‐in clinics. Congregation informed by announcement after prayer; however, the frequency of these announcements is unknown |
|
General practitioner (GP) drop‐in clinic: Trained GP provides regular drop‐in clinics at the mosque, and the following services: (a) education on long‐term conditions, (b) medical check‐up (for example, blood pressure measurements), and (c) health advice |
The clinics are held at Luton Central Mosque, Luton |
|
Combination
|
No evaluation reported. |
|
30 Project name: active Luton Dates: ongoing (start date unknown) Funding: charity organizations (Team Beds and Luton, Sports England, and The British Lung Foundation) |
To promote physical activity |
Project recruits those living within Luton Recruitment: The Council of Mosques in Luton encourages mosques within Luton to inform mosque attendees about this programme. Mosque volunteers are also involved in recruiting people to take part |
Physical activity |
|
The interventions are carried out in various venues within Luton. Details about these venues are unknown. |
|
Health professionals/workers
|
No evaluation reported. |
|
31 Project name: Bury Park Masjid Dates: started 2016 and ongoing Funding: donations from mosque attendees and voluntary support from health professionals |
To improve the health and well‐being of those who attend the mosque |
Those who attend the mosque (Bury Park Masjid, Luton) Recruitment: congregation are informed about the sessions through announcement after prayer. However, the frequency of the announcements and when they are delivered are unknown. |
|
Qualified doctors provide the following services to those attending the mosque:
|
Bury Park Masjid | Frequency and duration of sessions are unknown. |
Combination
|
No evaluation reported. |
|
32 Project name: The Big Iftaar Dates: started 2015, and held once a year Funding: voluntary support from health professional and charity organizations (eg, Luton foodbank) |
To encourage social cohesion amongst the community Impetus: a qualified doctor (mosque attendee) raised the importance of educating the community about healthy eating with the mosque management committee |
Those who live within Luton Recruitment methods unclear |
Dietary education |
Qualified doctors provided group education on healthy dietary practices for the month of Ramadhan. Details about the educational session (eg, content or topics covered) are unknown. |
Education delivered in a public space outdoors, within city Centre Luton | Length of group education session unknown. | Islamic faith leaders
|
No evaluation reported. |
|
34 Project name: Bowel cancer screening project Dates: 3 June 2016 (one‐off event) Funding: Slough CCG and Macmillan Cancer Support |
To increase the awareness of bowel cancer and bowel cancer screening programmes |
Those living within Slough. However, the majority of participants included mosque attendees (Jamea Masjid and Islamic Centre, Slough) Recruitment methods unclear |
|
|
Jamea Masjid and Islamic Centre, Slough |
One off‐event: 1400 to 1700. Unclear about the frequency and length of the educational sessions provided by the doctors. |
Combination
|
No evaluation reported |
|
35 Project name: no name available Dates: ongoing (start date unknown) Funding: donations from mosque attendees |
Promote outdoor physical activity |
Children who attend the madrassa (Jamea Masjid and Islamic Centre, Slough) Recruitment methods unclear |
Physical activity |
Weekly outdoor activity club, which includes the following components:
Limited details about the exercise sessions (eg, content and equipment) and other sports activities. |
Unclear | Activity club occurs every Sunday, after mosque attendance. Duration: 2 h |
Islamic faith leaders
|
No evaluation reported. |
|
38 Project name: no name available Dates: started 2015 and ongoing Funding: no funding, intervention carried out on a voluntary basis |
Enhanced management of those with chronic disease posthospitalization |
Recruitment: Mosque volunteers involved in recruiting participants to the programme |
|
|
Education session within Oldham Central Mosque, Greater Manchester |
Duration of the education session: unknown. Advised frequency of hospital visits: unknown. |
Islamic faith leaders
|
No evaluation reported. |
|
39 Project name: no name available Dates: ongoing (start date unknown) Funding: donations from mosque attendees |
Promote good dietary practices |
Children attending madrassa at Oldham Central Mosque, Greater Manchester (Age undefined) Recruitment methods unclear |
Dietary education |
|
Madrassa at Oldham Central Mosque, Greater Manchester | Education sessions occur once weekly. |
Islamic faith leaders
|
No evaluation reported. |
|
41 Project name: no name available Dates: January 1991‐ongoing Funding: Sports Wales |
To improve access to sports activities and highlight its association with better physical health |
Aimed at various populations living in Wales (ethnic minority, asylum seekers, survivors of sexual violence, disabled, travellers, and those who have experienced hate crimes) Charity working with various mosques in Newport, Wales, to encourage the uptake among the Welsh Muslim population Recruitment: Mosque volunteers involved in recruiting participants to the programme |
|
Physical activity
Increasing awareness of physical activity
|
Physical activity This is carried out outside of the mosque, however the venues are unknown Increasing awareness of physical activity Various mosques within Newport, Wales. |
Physical activity Unclear: whether the activities happen over a particular period, sports activities frequency and duration. Increasing awareness of physical activity It is unclear how often the imams and volunteers carry out their sessions to raise awareness |
Islamic faith leaders
|
No evaluation reported. |
|
42 Project name: no name available Dates: ongoing (start date unknown) Funding: donations from mosque attendees |
To promote physical activity among toddlers (age undefined by mosque) |
Children of mosque attendees at Belfast Islamic Centre, Northern Ireland Recruitment: imam and mosque volunteers raise awareness of the session and recruit participants |
Physical activity |
|
Belfast Islamic Centre, Northern Ireland | Sessions occur every Monday, between 1030 and 1200 |
Islamic faith leaders
|
No evaluation reported. |
|
43 Project name: football coaching Dates: ongoing (start date unknown) Funding: donations from mosque attendees |
To promote physical activity among children aged 7 to 16 years |
Children (7 to 16 years) attending Belfast Islamic Centre, Northern Ireland Recruitment methods unclear |
Physical activity |
|
Outdoor pitches at the QUB Sports Centre, Northern Ireland | Sessions occur every Sunday, between 1200 and 1300 |
Islamic faith leaders
|
No evaluation reported. |
|
46 Project name: no name available Dates: ongoing (start date unknown) Funding: donations from mosque attendees |
To promote physical fitness |
Children attending Ilford Central Mosque, Redbridge. Recruitment methods unclear |
Physical activity | Boxing classes held for two groups:
|
Classes held at a pre‐arranged sport venue (specific location unknown) | Classes held once a week (Sundays), for 1 h. |
Islamic faith leaders Mosque volunteers arrange and conduct the sessions |
No evaluation reported. |
|
47 Project name: no name available Dates: September 2013 and ongoing Funding: donations from mosque attendees |
To promote physical fitness |
Children (6 to 16 years) attending Seven Kings Mosque, Redbridge. Recruitment methods unclear |
Physical activity |
|
Local park (specific area unknown) | Training sessions occur once a week (Sundays), for 2 h (1000‐1200) |
Islamic faith leaders Mosque volunteers arrange and conduct the sessions |
No evaluation reported. |
|
48 Project name: Muslim Youth Foundation Dates: ongoing (start date unknown) Funding: donations from mosque attendees |
To promote physical activity |
Muslims attending Muslim Youth Community Centre, Manchester. Recruitment methods unclear |
Physical activity | Various physical activity sessions are held by the volunteers from the community centre. These include the following:
|
Muslim Youth Community Centre, Manchester |
Four times a week (Monday to Thursday), 2000‐2100
Once a week (Wednesday), 2000‐2100
Every day, 1200‐onwards (specific timings unknown)
Once a week (Sunday), 2000‐2100 |
Islamic faith leaders Community centre volunteers arrange and conduct the sessions |
No evaluation reported. |
|
49 Project name: no name available Dates: ongoing (start date unknown) Funding: donations from mosque attendees |
To promote physical fitness |
Those who attend Ashton Central Mosque, Greater Manchester. Recruitment methods unclear |
Physical activity |
|
Exercise held in a premises owned by Ashton central Mosque in greater Manchester | Twice a week (Monday and Wednesday), 1300‐1430 |
Islamic faith leaders
|
No evaluation reported. |
|
50 Project name: active sisters (a Muslim charity) Dates: ongoing (start date unknown) Funding: sporting equal |
To improve physical fitness |
Muslim women living within London Muslim charity organizations and active sisters are involved in raising awareness of the project and recruiting participants. Recruitment methods unclear |
Physical activity | Organization has a number of premises/venues in London (number unknown). Physical activity equipment available at venue as well as various physical activity classes:
|
Various venues throughout London | Daily/weekly classes, duration of 1 to 2 h each. Specific session details are unknown |
Muslim charity
|
No evaluation reported. |
|
51 Project name: no name available Dates: since 2007 and onwards Funding: NHS |
Promote health awareness |
Those who attend Birmingham Central Mosque, Birmingham
Recruitment: mosque volunteers are involved with recruitment |
|
|
Birmingham Central Mosque, Birmingham | These sessions are held a few times a year (exact number unknown), and for a few hours during the day. |
Health professionals/workers
|
No evaluation reported. |
|
52 Project name: no name available Dates: 2002 to 2005 Funding: Public Health England |
To enable members of the mosque to become active health champions and educate mosque attendees |
Volunteers from the Sufi Trust, Birmingham, were approached to take part in the training programme. Volunteers delivered education to those who attended Birmingham Central Mosque, Birmingham. Recruitment methods to the education sessions were unclear. |
|
|
It is unclear where the volunteers were trained. The education sessions were either delivered in the mosque, or in the home of those who have a family member with a chronic condition. |
Six‐week training programme for volunteers. Details about the education session(s) length and frequency are unknown. |
Combination
|
Evaluation of process or implementation only: Number of volunteers trained: n = 6 Number of people who received education from volunteers trained: n = 400 |
|
53 Project name: Active weekends Dates: since 1998 and ongoing Funding: Sufi Trust (a Muslim charity) |
To promote healthy living |
Muslim mothers and children who live in Birmingham Recruitment methods unclear |
|
|
The location of these residential weekends is unknown. | Sessions are carried out over 2 days (Saturday and Sunday), however the frequency of these residential weekends is unknown. |
Muslim charity
|
No evaluation reported. |
|
54 Project name: Interfaith games Dates: since 2015 and ongoing Funding: Football Association of England, Islamic relief worldwide |
Promoting fitness and physical activity in children |
Children who attend a Muslim school—predominantly those in Birmingham Recruitment methods unclear |
Physical activity |
|
Sports halls and play grounds at various locations in Birmingham |
Sports gala occurs once a year. Duration of football training/practice unknown. Football match length: 50 min |
Islamic faith leaders Muslim schools, in collaboration with the with the England Schools Football Association (ESFA) |
No evaluation reported. |
|
55 Project name: Youth project Dates: ongoing (start date unknown) Funding: donations from mosque attendees |
Unknown |
Mosque attendees at Ghausia Mosque, Pendle, Lancashire. Recruitment methods unclear. |
Physical activity |
|
A venue owned by the mosque, located close to Ghausia Mosque, Pendle. | Duration and frequency of classes/sessions are unknown. |
Islamic faith leaders Mosque volunteers |
No evaluation reported. |
Banerjee ET, Landry M, Zawi M, Childerhose D, Stephens N, Shafique A, et al. A pilot examination of a Mosque‐based physical activity intervention for South Asian Muslim women in Ontario, Canada. J Immigr Minor Health 2017;19(2):349–357.
East London Mosque, London Muslim Centre. Faith in Health 2017. Available from: http://www.eastlondonmosque.org.uk/content/faith-health.
Streatham Mosque. Daily activities at Masjid 2017. Available from: http://www.streathammosque.org/.
Ipswich mosque. Activities 2017. Available from: http://www.ipswichmosque.org/our_aims.php.
Public Health England. Guide to Healthy Living: Mosques 2017. Available from: http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/619891/Guide_to_Healthy_Living_Mosques.PDF.
“Ongoing” at the time of data collection.
In addition, the systematic search and mapping process identified 8 health promotion interventions which were partly associated with obesity and 13 which were not associated with obesity. Brief details and a concise description of these interventions are provided in Tables S3 to S6.
In total, 137 grey information requests for relevant information were made to local councils, local mosques, Muslim charity organizations operating in the United Kingdom, Muslim community organizations operating in the United Kingdom, and local health authorities and eight requests to the project steering group. Only three (2%) of the email requests resulted in a response: One local health authority and one Muslim charity organization provided information on one intervention each (project numbers 40, 54), and one mosque provided information on two interventions (project numbers 42, 43). Due to this low response rate, a follow‐up telephone call (by SD) was made to those who did not respond. This method of searching for grey information was more successful, and 33 additional interventions were identified: 19 from mosques (one mosque provided information on four different interventions, and another mosque provided information on three interventions), 11 from Muslim charity organizations (one of these organizations provided information on two interventions), 3 from Muslim community groups, and 1 from a project steering group member. One telephone call request to a Muslim charity organization resulted in a request from them for SD to visit them face to face for a conversation, and this resulted in the identification of one additional intervention.
4. DESCRIPTION OF INTERVENTIONS
We first describe the specific content, duration, and frequency for those interventions which were directly associated with obesity (n = 35).
4.1. Content of obesity interventions
The majority of the 35 interventions focused on changing physical activity behaviours (n = 23). Most of these interventions included group sessions around sport, exercise, or physical activity. Sporting activities included many different types of sports, but football was particularly popular, and also boxing and kick boxing. Football and boxing sessions for adults and children, and males and females, were common. Other sports included swimming, badminton, netball, cycling, table tennis, and golf. Exercise sessions included aerobic, strength, self‐defence, walking, resistance training, relaxation, chair, Jiu‐Jitsu, Zanga Zanga, and general sessions in a commercial gym. Seven of the 23 physical activity interventions were targeted at children (including one in toddlers) and three at women. The remaining 13 interventions focused specifically on physical activity for all the community, but often included separate classes for women and separate classes and age‐appropriate exercises for children.
Four interventions specifically focused on diet (including one targeting children). Two of these interventions simply focused on health eating, and one focussed on healthy eating practices during Ramadhan. The other diet intervention focused on women preparing salads at home and bringing them to the mosque for informal “salad of the month” competitions. One intervention specifically focused on diet plus physical activity, where the diet component was simply healthy eating. The intervention content of the remaining seven obesity interventions was unclear.
Our main interest in collecting data on content of obesity interventions was to assess for any themes or examples of differences in content compared with what might normally be contained in interventions aimed at the general public in the United Kingdom. From the information available, the content of the interventions appeared to be similar to those contained in health promotion interventions for the general public in the United Kingdom.
4.2. Duration and frequency of obesity interventions
Some of the obesity interventions we identified took the form of a one‐off health fair/event (project number 34), an annual event (annual run, project number 20; annual sports gala, project number 54), a residential active weekend for Muslim mothers and children (project number 53), or a regular drop in clinic (held every 2 weeks, project number 27). Two projects (numbers 10 and 24), which focused on healthy eating, took place during Ramadhan.
Eight projects (35, 39, 42, 43, 46, 48, 49, 50) ran one or more weekly sessions, and these focused on physical activity and exercise; it was unclear for how many weeks these ran and some projects appeared to be ongoing (at the point of writing this manuscript). Three of these eight projects ran sessions to coincide with prayer attendance at the mosque or madrassa. For example, project number 35 aimed to promote outdoor physical activity in children through a weekly activity club every Sunday after mosque services. Project number 39 aimed to promote a healthy diet in children through a weekly activity club for children attending a madrassa. Project number 42 aimed to promote physical activity among toddlers during a weekly session for mothers in an Islamic centre.
Next, we describe a variety of generic intervention development and implementation factors for all of the health promotion interventions we identified (n = 56): funding source, impetus, target population and recruitment methods, intervention setting, intervention delivery team (and any training and support they received), and evidence for intervention content being embedded in religious teaching. Factors which appear to increase the acceptability and impact of a health promotion intervention in IRS may be usefully translated for interventions which aim to tackle obesity in these settings.
4.3. Funding source for the intervention
Information on funding source was available for 40 of the 56 interventions. All five studies identified by searching the bibliographic databases were funded through, at least in part, research funding bodies. Interventions which were identified from grey literature or grey information were funded by donations from congregants (n = 12) or by volunteering to organize and run the intervention (n = 3), and one intervention was funded by the mosque. Nine interventions were funded by charity organizations (often a combination of charities, including Muslim charity organizations), and a further nine interventions were primarily funded by local health authorities or local councils. One intervention was funded by a number of organizations including a bank, local health authority, and local businesses. The funding source for the remaining interventions was unclear.
4.4. Impetus for the intervention
The impetus for the five interventions identified by the bibliographic databases was clear and is detailed in the published research papers. For all but five interventions identified by the grey literature search or information requests for grey information, the impetus for the intervention (ie, why was this particular intervention chosen, rather than a different intervention) was unclear.
For one intervention (project number 22), Islamic leaders, mosque volunteers, and the Council of Mosques wanted mosques to be viewed by Muslims as being involved in important activities other than prayer. For another intervention (project number 28), the suicide of three community members led an imam to voluntarily undergo counselling training and provide counselling services for all mosque attendees. The impetus for projects 32 and 37 came from a physician congregant who raised the importance of educating the community about healthy eating, and sexual health and pregnancy, respectively, with the mosque management committee. The impetus for project 40 came from Public Health Wales that included a strategy to approach and educate mosque Imams in their Screening for Life programme.
4.5. Target population and recruitment methods
The target population and recruitment methods for the five interventions identified by the bibliographic databases were clear and are detailed in the published research papers. For health promotion interventions that were relevant to the whole community, the target population was the congregation of the IRS (usually the mosque). Potential participants were recruited using posters and leaflets which were distributed in the IRS setting by faith leaders (and sometimes researchers directly), and announcements after communal prayers. The addiction recovery service intervention specifically targeted Muslims on a methadone treatment waiting list at a local hospital, and the awareness raising training programme on family health for Islamic religious leaders appeared to randomly select participants.
For interventions identified by the grey literature search or information requests for grey information, the target population and recruitment methods were generally unclear or not stated. However, where information was provided for health promotion interventions that were relevant to the whole community, the target population was the congregation of the IRS (usually the mosque). The most commonly reported method of recruitment was via an announcement after communal prayers. However, information about who carried out the announcement, its frequency, and whether it was carried out after a specific prayer was unavailable for most of the interventions. Potential participants were also recruited using posters and leaflets, which were distributed in the IRS by members of the mosque (and sometimes researchers directly). Various types of members of the mosque were reported as being involved, including mosque volunteers, a imam, religious teacher, or religious leader. One intervention (project number 37), which aimed to increase awareness of sexual health and which targeted women, also used an existing social media group (WhatsApp instant messaging) and approached mosque attendees in person during their visit to the mosque. A few of the interventions targeting children stated that they recruited participants through madrassa classes at the mosque, and one intervention targeted children attending an Islamic school.
4.6. Intervention setting
Most interventions (n = 34) were reported to be carried out in either a mosque (or a site owned by the mosque), madrassa, mens' or womens' halaqas, a Muslim youth centre, or a combination of these settings.
Thirteen interventions (mainly physical activity interventions) were reported to take place in a range of local outdoor (eg, parks) or indoor (eg, leisure centre, school) public spaces. For nine interventions, the exact setting was unclear.
4.7. Intervention delivery team (and any training and support they received)
Where stated (n = 45 in total), interventions were delivered by Islamic faith leaders (n = 20), health professionals/workers (n = 7), Muslim charities (n = 2), nonreligious charities or social enterprises (n = 2), or by a combination of these individuals and organizations (n = 14). No detailed information was provided about any training for nonhealth professionals/workers who were responsible for delivering the interventions.
The 20 interventions that were delivered by Islamic faith leaders were delivered by a range of members of the mosque community, including mosque volunteers, an imam, religious teacher, or religious leader. Four of these 19 interventions were delivered by an Islamic faith leader within the mosque community who was also a health professional/worker (project numbers 24, 37, 38, 49). One of these 19 interventions (project number 54) was delivered by teachers at Muslim schools in collaboration with the Football Association of England. Two interventions were delivered by Muslim charities (project numbers 50, 53).
The seven interventions that were delivered by health professionals/workers focused mostly on medical conditions or mental health. The two interventions that were delivered by nonreligious charities or social enterprises included one intervention which aimed to promote cycling and physical activity (project number 19) and one which aimed to promote health and well‐being for people with disabilities (project number 45).
Fourteen interventions were delivered by a combination of Islamic faith leaders, Muslim charities, health professionals/workers, and nonreligious charities or social enterprises.
4.8. Evidence for intervention content being embedded in religious teaching
Where stated, interventions were usually delivered during or after prayers, halaqas meetings, Quran, or madrassa classes. One intervention (project number 1) assessed the acceptability and feasibility of using a tailored sermon that included theologically framed health messaging. Another intervention (on addiction treatment, project number 4) included a brief spiritual component of prayer and discussion on the Islamic view on addiction and how to use faith in manage addiction, delivered by an Imam. Another intervention, a training programme for religious leaders on family health (project number 5), was guided by the Religious Leaders' Training Manual on Family Health.33 An intervention (project number 21) to improve the health and fitness of Muslim women included advice on issues relating to cultural and religious barriers to increasing physical activity levels. Project number 26 “Smile with the Prophet” included a session delivered by the imam on the importance of dental hygiene linked to Islamic teaching.
4.9. Evaluation of the 56 health promotion interventions
Four evaluations (project numbers 2, 3, 4, 5) included preintervention and postintervention outcome assessments: two controlled trials and two pre and post studies. These four interventions were published in research journals and identified from bibliographic databases. All four of these interventions received research funding and included some process and outcome evaluation. For the purposes of this review, we were most interested in process evaluations and information which could be usefully translated to inform the design of interventions to tackle (prevent or treat) obesity in IRS. We were particularly interested in any information on the reach of interventions.
Only one of the four evaluations reported recruitment and retention rates, which appeared to be relatively high in IRS. In project number 2, conducted in the United Kingdom, 79% of IRS agreed to take part in the study, and 74% of households invited to participate agreed; 100% of IRS remained in the study throughout, as did 81% of households. From this one study (which was a smoke‐free home intervention), recruitment and retention rates appear to be relatively high in IRS.
All four of the evaluations reported on some aspect of acceptability of the intervention, but the results from three of the evaluations were general and did not provide any useful information for the purposes of this review. One study (project number 2) conducted a separate qualitative study and highlighted a number of facilitators and barriers to the delivery of the intervention. The reported facilitators included the importance of flexibility in session delivery, having systems in place which involve women and children (if the intervention is targeted at these groups), independence of religious teachers and support of the mosque chair, and the correct personal characteristics (skills and motivation) of the religious leader to engage the mosque community with the intervention. Barriers to the delivery of the intervention included the diverse settings (eg, the culture/ethos or organizational structure of the setting), which led to difficulties in delivering a standardized intervention in the participating settings.
Another five interventions which included an evaluation (project numbers 7, 19, 22, 37, 52) were identified in the grey literature or grey information and reported very limited information on one or more of the following: numbers of participants taking part in the intervention, response or retention rates, numbers of measurements taken in total, and/or the acceptability of the intervention(s) to the participants. The data reported were not deemed to be of sufficient quality (and at high risk of bias) to provide any useful evidence that could be used to help inform intervention development or delivery.
5. DISCUSSION
We found evidence of a variety of health promotion interventions associated with obesity in IRS in all areas of the United Kingdom that were targeted for study. The majority of interventions were only identified in the grey literature and grey information, sometimes in locally produced reports that were not available on websites or the internet, but more often only in people's memories. We asked those people who had provided us with grey information if they thought it would be useful to record a detailed description of the content and delivery of their intervention, so that others could find it through searching the internet. Their view was that this was not a priority. Our findings support those of Adams et al,29 who concluded that information on the nature and range of public health interventions, and evaluations of them, may be predominantly, or only, held in grey information.
The most successful approaches to organizations or individuals for relevant grey information were through telephone calls or face‐to‐face conversations, rather than emails. Using personal contacts (ie, knowing the name of the person being contacted and using their name when making a call or sending an e‐mail) and exploiting existing connections were deemed to contribute to success. In addition, the positionality of the researchers relative to the ethnic, linguistic, and religious status of the UK communities we attempted to contact for this study was deemed to contribute to success. Using researchers who could be considered community insiders, who have a meaningful personal understanding of the culture and faith associated with IRS and the communities they serve, was deemed to contribute to success. SD was responsible for making most of the requests for information, and KR made a few requests in Birmingham. SD is male, Muslim, Pakistani, of Punjabi origins, and is fluent in Punjabi, Urdu, Arabic, Farsi and English. KR is female, Sikh, British Indian, and is fluent in Punjabi and English. It appeared to be the case that there was more success if the approach for information was made by a man rather than a woman. KR found that, on some occasions, she was required to have a male colleague with her to facilitate discussions or access.
The fact that we encountered significant difficulties in gaining access to the Muslim community, even as community insiders, has implications for the time, cost, and relevant skills and characteristics of project researchers. Our findings support those of others and underscore the importance of the positionality of researchers who are responsible for gaining access to mosque communities and in turn promoting and delivering projects for the Muslim community.34, 35
We found that most interventions identified through the grey literature and grey information were poorly described and rarely evaluated. We appreciate that the Template for Intervention Description and Replication (TIDieR) framework is a very useful method for standardizing intervention description36 and should be used where resource and skills are available. Where these are not available and/or those delivering the intervention do not consider this effort a priority, we suggest that researchers work alongside the delivery team to capture (for example, through conversation, as we did) the detail required. Individuals in IRS that we spoke to were, without exception, willing to provide as much detail as they could through conversation.
The majority of health promotion interventions associated with obesity in IRS included at least some advice on physical activity and/or diet, with around half focusing specifically on these behaviours. Some, particularly those with a physical activity component, included separate classes and age‐appropriate exercises for children, and separate sessions and sex‐appropriate exercises for women. Most physical activity interventions were group based and many involved walking groups or informal (rather than competitive) team games. Indeed, Jepson and colleagues37 found that Muslims living in Scotland described the main motivators for taking part in physical activity were external motivators (ie, undertaking physical activity as a means to an end, which included the opportunities that physical activity provided for social activity and enjoyment). Cross‐Bardell and colleagues38 reported similar findings from their qualitative study of Muslims living in East Midlands, UK; respondents emphasised using a social approach for potential physical activity and diet interventions, undertaking activity with family or friends and with bilingual community peers to facilitate engagement, motivation and support.
The level of detail of the content and delivery of the interventions that were identified from the grey literature and grey information was unclear or limited. It was not clear, for example, whether the participants received any written advice in hard copy, by email, or internet site. However, evidence suggests that Muslims living in the United Kingdom favour spoken content and delivery of physical activity and diet interventions, including personal stories, within local informal rather than provider settings.38 It is reasonable to assume that interventions delivered in this way are less likely to be described in detail in writing.
We found some evidence to suggest that the promotion of the intervention by religious leaders was done in the context of the Islamic faith. Indeed, references advocating physical activity can be inferred from the Qur'an and Prophetic tradition/saying (Hadiths), which share the common theme of maintaining respect for the body. The following Hadith narrated by Aisha, wife of the Prophet Muhammad, not only serves to promote walking and running as physical exercise but also shows that this benefit relates to women and men equally.
“I raced with the Prophet (p.b.u.h.) and beat him in the race.
Later, when I had put on some weight, we raced again and he won.”
[Noumani,39 quoting Abu Dawud, Hadith number 2572]
One study, which assessed the feasibility of developing (in coproduction with resident imams) and delivering tailored sermons (included theologically framed health messaging), found that the intervention was well received by all members of the mosque community.3 These findings support those of recent studies that suggest that strategies for leveraging religious concepts to promote health among Muslims have value.40, 41
Most of the interventions we identified were inspired and run by members of the mosque community or Muslim organizations, the impetus being the personal experience of a member of the congregation or instruction from Mosque leaders. The most common recruitment method was via announcements after prayers, and faith leaders appear supportive of health promotion interventions. This method of recruitment appears to promote a relatively high reach (recruitment and retention rate), which in turn may militate against intervention‐generated inequalities.42 Indeed, Jepson and colleagues37 found that role models were seen by South Asians living in Scotland as important for inspiring and motivating people to undertake physical activity interventions that they may otherwise lack confidence in. Findings from an ongoing systematic review conducted by Mustafa and colleagues,43 which aims to elucidate the role and effectiveness of imams and mosques in health promotion in Western societies, may highlight more insights for intervening in these settings.
It is clear that most health promotion interventions in IRS are not associated with any public funding. Most activities are volunteer‐led (often members of the congregation who are health professionals) and funded by congregant donations and/or Muslim organizations. We did not hear, in our conversations with people, that this approach was a result of the fact that they had applied for public funding and had been rejected. The approach of volunteering their own time and resources was not something that any of the people we talked to complained about, or found unusual. As for many other religious faiths, it is central to the Muslim identity to feel care and compassion for one's fellow human beings. As well as the indisputable benefits for those receiving charity, Islam also highlights the spiritual need of those with wealth to give some of it away selflessly. In the Qur'an, Allah emphasises that charity should be given in “prosperity or adversity” (Al‐Quran, 3:134). Indeed, one of the five central pillars of Islam is zakat, or almsgiving—the obligatory tax due on an adult Muslim's wealth every year, making charity an undeniable cornerstone of the faith.
A number of national and international organizations and agencies have suggested that faith‐based organizations and groups, including IRS, should be the focus of greater efforts to promote health. Recently, the World Health Organization published their Global Action Plan on Physical Activity, in which action 3.3 is to “enhance provision of, and opportunities for, more physical activity programmes and promotion in … faith‐based centres, to support participation in physical activity, by all people of diverse abilities”.44 We suggest that health promotion in IRS should be supported by public funding, health professional, and academic researcher input, where that is welcome, and researchers should work in coproduction with faith leaders in IRS. Such support should be informed and sensitive to the Islamic norms and culture in these settings, which highly value health and the benefits of physical activity and a healthy diet. We suggest that this support should focus on working in partnership with faith leaders in IRS to help them develop, deliver, and evaluate health promotion interventions. Where relevant, this should include training programmes (train the trainer) to upskill those delivering the intervention in IRS.
Previous studies have indicated that faith‐based organizations and settings are natural partners for the delivery of health promotion programs due to a number of factors.45, 46, 47, 48 These factors include their role as community centres; access to large segments of the population, especially underserved groups; supportive infrastructure (eg, health ministries, communication channels, regularity of contact); presence of support networks (eg, prayer groups); and personnel resources (eg, volunteers, lay leaders, and champions). Although the majority of the existing evidence base comes from church‐based organizations in America, and particularly the black African‐American community, we suggest that the learning from research in these settings could be translated for IRS in the United Kingdom. In particular, we suggest that the learning around barriers to access and intervention implementation that were addressed in these projects by partnering with established community‐based religious organizations are highly relevant to health promotion in IRS in the United Kingdom. An excellent example of good practice and potential learning is emerging from The Racial and Ethnic Approaches to Community Health for Asian Americans (REACH FAR) project, that is implementing a multilevel and evidence‐based health promotion in faith‐based organizations serving Asian American communities (Bangladeshi, Filipino, Korean, Asian Indian) across multiple denominations (Christian, Muslim, and Sikh) in New York/New Jersey.49
6. CONCLUSION
The current review suggests that IRS are an appropriate setting for health promotion interventions associated with obesity, which may reach a high proportion of the community and reduce inequalities in health. However, it was clear from this scoping review that this is an area severely lacking in evidence. In order to ascertain the potential effectiveness of interventions in this setting, future research should first focus on developing interventions with a sound theory of change and clear specification of key components. This should be done in partnership with IRS and faith leaders to learn from their existing, albeit informal, expertise in this area. Second, high‐quality evaluations are needed to evidence the impact of these interventions on health outcomes.
We also suggest that the methods used in this review, including the learning around positionality of researchers, could be adopted by other researchers as a way to best locate opportunities and partners for effective community‐level interventions.
CONFLICT OF INTEREST
No conflict of interest was declared.
FUNDING SOURCE
This study was funded by the National Institute for Health Research (NIHR) [Programme Development Grant (RP‐DG‐1215‐10002)/Bradford Institute for Health Research]. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Supporting information
Table S1. Bibliographic and grey literature searches and search terms used to identify public health interventions delivered in Islamic religious settings in the UK.
Table S2. Geographical areas1 with the highest Pakistani and Bangladeshi populations within England, Wales, Scotland and Northern Ireland (assessed August 20172)
Table S3. Name, location and source of identification of health promotion interventions partly associated with obesity (n = 8)
Table S4. Author, study design, outcome measures (where applicable), project name, location and source of identification of health promotion interventions not associated with obesity (n = 13)
Table S5. Aim and characteristics of health promotion interventions partly associated with obesity, and their evaluation where available (n = 8)
Table S6. Aim and characteristics of health promotion interventions not associated with obesity, and their evaluation where available (n = 13)
ACKNOWLEDGEMENTS
We are thankful to the Muslim leaders, managers, volunteers, workers, and attendants of all the Islamic religious settings (IRS) in the United Kingdom who provided us information about health promotion activities in IRS and their selfless work to use IRS for health promotion interventions. We are thankful to the members of project steering group who provided their input on some projects of health promotion in IRS and gave feedback during meetings. We are thankful to Faye Dobbin, Abigail Dawson, and Harry Bennett, the Industrial Placement Students at Born in Bradford study, for making some inquiring about health promotion in IRS throughout the United Kingdom. We are thankful to NIHR for funding this pioneering research.
Rai KK, Abid Dogra S, Barber S, Adab P, Summerbell C, on behalf of the “Childhood Obesity Prevention in Islamic Religious Settings' Programme Management Group” . A scoping review and systematic mapping of health promotion interventions associated with obesity in Islamic religious settings in the UK. Obesity Reviews. 2019;20:1231–1261. 10.1111/obr.12874
The “Childhood Obesity Prevention in Islamic Religious Settings” Programme Management Group includes Mohammed Arshad, Rosie McEachan, Emma Frew, Catherine Hewitt, Laura Sheard, Kamran Siddiqi, Judith Watson, and John Wright.
Footnotes
To improve the completeness of reporting, and ultimately the replicability, of interventions, an international group of experts and stakeholders developed the Template for Intervention Description and Replication (TIDieR) checklist and guide. The resultant 12‐item TIDieR checklist and guide provides, for each item, an explanation, elaboration, and examples of good reporting.
REFERENCES
- 1. Office for National Statistics . Ethnic group by religion 2015. Available from: https://www.ons.gov.uk/aboutus/transparencyandgovernance/freedomofinformationfoi/ethnicityandreligionbyage.
- 2. El‐Sayed AM, Scarborough P, Galea S. Ethnic inequalities in obesity among children and adults in the UK: a systematic review of the literature. Obes Rev. 2011;12(5):e516‐e534. [DOI] [PubMed] [Google Scholar]
- 3. Padela AI, Malik S, Ahmed N. Acceptability of Friday sermons as a modality for health promotion and education. J Immigr Minor Health. 2018;20(5):1075‐1084. [DOI] [PubMed] [Google Scholar]
- 4. Falconer CL, Park MH, Croker H, et al. Can the relationship between ethnicity and obesity‐related behaviours among school‐aged children be explained by deprivation? A cross‐sectional study. BMJ Open. 2014;4(1):e003949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sahota P, Gatenby LA, Greenwood DC, Bryant M, Robinson S, Wright J. Ethnic differences in dietary intake at age 12 and 18 months: the born in Bradford 1000 study. Public Health Nutr. 2016;19(1):114‐122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nagy LC, Horne M, Bingham DD, Kelly B, Clemes S, Mohammed MA, Barber SE, Cultural and economic differences in television viewing in early childhood 2015. Available from: https://bradscholars.brad.ac.uk/bitstream/handle/10454/7367/ISBNPA2_LC.pdf?sequence=1&isAllo.
- 7. Owen CG, Nightingale CM, Rudnicka AR, et al. Physical activity, obesity and cardiometabolic risk factors in 9‐ to 10‐year‐old UK children of white European, south Asian and black African‐Caribbean origin: the child heart and health study in England (CHASE). Diabetologia. 2010;53(8):1620‐1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Williams E, Stamatakis E, Chandola T, Hamer M. Asessment of physical activity levels in south Asians in the UK: findings from the health survey England. J Epidemiol Community Health. 2010;65(6):517‐521. [DOI] [PubMed] [Google Scholar]
- 9. Leung G, Stanner S. Diets of minority ethnic groups in the UK: influence on chronic disease risk and implications for prevention. Nutr Bull. 2011;36(2):161‐198. [Google Scholar]
- 10. Whincup P, Gilg JA, Papacosta O, et al. Early evidence of ethnic differences in cardiovascular risk: cross sectional comparison of British south Asian and white children. Br Med J. 2002;324(7338):635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bhopal R, Unwin N, White M, et al. Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: cross sectional. Br Med J. 1999;319(7204):215‐220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Social Mobility Commission . The Social Mobility Challenges Faced by Young Muslims. London: Social Mobility Commission; 2017. [Google Scholar]
- 13. Liu J, Davidson E, Bhopal R, et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed‐methods evidence synthesis. Health Technol Assess. 2012;16(44):1‐469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Smith GD, Chaturvedi N, Harding S, Nazroo JY, Williams R. Ethnic inequalities in health: a review of UK epidemiological evidence. Crit Public Health. 2000;10(4):375‐408. [Google Scholar]
- 15. Bhopal R. Health education and ethnic minorities. Br Med J. 1991;302(6788):1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. White M, Adams J, Heywood P. How and why do interventions that increase health overall widen inequalities within populations? In: Babones S, ed. Health, inequality and society. Bristol: Policy Press; 2009. [Google Scholar]
- 17. National Heart Forum , Faculty of Public Health, Department of Health. Lightening the Load. Tackling Overweight and Obesity. London; 2007.
- 18. The Muslim Council of Britain . British Muslims in Numbers. A demographic, socio‐economic and health profile of Muslims in Britain drawing on the 2011 Census London; 2015.
- 19. Maynard M, Baker G, Harding S. Exploring childhood obesity prevention among diverse ethnic groups in schools and places of worship: recruitment, acceptability and feasibility of data collection and intervention components. Prev Med Rep. 2017;6:130‐136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bagby I, Perl PM, Froehle BT. The mosque in America: a national portrait. A report from the mosque study project 2001. Available from: http://icnl.com/files/Masjid_Study_Project_2000_Report.pdf.
- 21. Padela AI, Killawi A, Heisler M, Demonner S, Fetters MD. The role of imams in American Muslim health: perspectives of Muslim community leaders in Southeast Michigan. J Relig Health. 2011;50(2):359‐373. [DOI] [PubMed] [Google Scholar]
- 22. Public Health England . Tackling health inequalities through enhancing the wellbeing role of mosques 2017. Available from: https://publichealthmatters.blog.gov.uk/2017/08/23/tackling-health-inequalities-through-enhancing-the-wellbeing-role-of-mosques/.
- 23. Pallan M, Parry J, Adab P. Contextual influences on the development of obesity in children: a case study of UK south Asian communities. Prev Med. 2012;54(3–4):205‐211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tomalin E, Sadgrove J, Russell A. Places of worship as minority ethnic public health settings in Leeds 2015. Available from: https://www.leeds.gov.uk/docs/Places%20of%20Worship%20as%20Minority%20Public%20Health%20Settings%20in%20Leeds.pdf. [DOI] [PubMed]
- 25. Sheikh A. Why are ethnic minorities under‐represented in US research studies? PLoS Med. 2006;3(2):e49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Thomas SB, Quinn SC, Butler J, Fryer CS, Garza MS. Toward a fourth generation of disparities research to achieve health equity. Annu Rev Public Health. 2011;32(1):399‐416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Paeratakul S, Lovejoy JC, Ryan DH, Bray GA. The relation of gender, race and socioeconomic status to obesity and obesity comorbidities in a sample of US adults. Int J Obes Relat Metab Disord. 2002;26(9):1205‐1210. [DOI] [PubMed] [Google Scholar]
- 28. Powers M, Faden R. Social Justice: Moral Foundations of Public Health and Health Policy. New York: Oxford University Press; 2006. [Google Scholar]
- 29. Adams J, Hillier‐Brown FC, Moore HJ, et al. Searching and synthesising ‘grey literature’ and ‘grey information’ in public health: critical reflections on three case studies. Syst Rev. 2016;5(1):164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hillier‐Brown FC, Summerbell CD, Moore HJ, et al. A description of interventions promoting healthier ready‐to‐eat meals (to eat in, to take away, or to be delivered) sold by specific food outlets in England: a systematic mapping and evidence synthesis. BMC Public Health. 2017;17(1):93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Born in Bradford . Using Islamic religious settings to prevent childhood obesity among South Asian children in the UK 2017. Available from: https://borninbradford.nhs.uk/research/grants/using-islamic-religious-settings-prevent-childhood-obesity-among-south-asian-children-uk.
- 32. Office for National Statistics . 2011. Census: ethnic group, local authorities in the United Kingdom 2011. Available from: https://www.ons.gov.uk/file?uri=/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/2011censuskeystatisticsquickstatsticsforlocalauthoritiesintheunitedkingdompart1/r21ukrttableks201ukladv1_tcm77-330436.xls.
- 33. The Health Compass . Religious Leaders' Training Manual on Family Health 2011. Available from: https://www.thehealthcompass.org/project-examples/religious-leaders-training-manual-family-health.
- 34. Muhammad M, Wallertein N, Sussman AL, Avila M, Belone L, Duran B. Reflections on researcher identity and power: the impact of positionality on community based participatory research (CBPR) processes and outcomes. Crit Socio. 2014;41(7–8):1045‐1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ryan L, Kofman E, Aaron P. Insiders and outsiders: working with peer researchers in researching Muslim communities. Int J Soc Res Methodol. 2010;14(1):49‐60. [Google Scholar]
- 36. Hoffman TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348(mar07 3). [DOI] [PubMed] [Google Scholar]
- 37. Jepson R, Harris FM, Bowes A, Robertson R, Avan G, Sheikh A. Physical activity in south Asians: an in‐depth qualitative study to explore motivations and facilitators. Plos One. 2012;7(10):e45333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cross‐Bardell L, George T, Bhoday M, Tuomainen H, Qureshi N, Kai J. Perspectives on enhancing physical activity and diet for health promotion among at‐risk urban UK south Asian communities: a qualitative study. BMJ Open. 2015;5(2):e007317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Noumani M. Ma'ariful Hadith: Quoting Sunan Abu Dawood, Hadith Number 2572. Karachi: Darul Ishaat Publishers; 2002. [Google Scholar]
- 40. Maziha ZA, Imran A, Azlina I, Harmy MY. Randomized controlled trial on the effect of Al‐Quran recitation vs counseling on smoking intensity among Muslim men who are trying to quit smoking. Malays Fam Physician. 2018;13(2):19‐25. [PMC free article] [PubMed] [Google Scholar]
- 41. Vu M, Muhammad H, Peek ME, Padela AI. Muslim women's perspectives on designing mosque‐based women's health interventions—an exploratory qualitative study. Women Health. 2018;58(3):334‐346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health. 2013;67(2):190‐193. [DOI] [PubMed] [Google Scholar]
- 43. Mustafa Y, Baker D, Puligari P, Melody T, Yeung J, Gao‐Smith F. The role of imams and mosques in health promotion in Western societies‐a systematic review protocol. Syst Rev. 2017;6(1):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. World Health Organization. Global action plan on physical activity 2018–2030: more active people for a healthier world. Geneva; 2018. [Google Scholar]
- 45. Baskin ML, Resnicow K, Campbell MK. Conducting health interventions in black churches: a model for building effective partnerships. Ethnic Divers. 2001;11(4):823‐833. [PubMed] [Google Scholar]
- 46. Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin ML. Church‐based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28(1):213‐234. [DOI] [PubMed] [Google Scholar]
- 47. Bopp M, Fallon EA. Health and wellness programming in faith‐based organizations: a description of a nationwide sample. Health Promot Pract. 2013;14(1):122‐131. [DOI] [PubMed] [Google Scholar]
- 48. Peterson J, Atwood JR, Yates B. Key elements for church‐based health promotion programs: outcome‐based literature review. Public Health Nurs. 2002;19(6):401‐411. [DOI] [PubMed] [Google Scholar]
- 49. Kwon SC, Patel S, Choy C, et al. Implementing health promotion activities using community‐engaged approaches in Asian American faith‐based organizations in new York City and New Jersey. Transl Behav Med. 2017;7(3):444‐466. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Bibliographic and grey literature searches and search terms used to identify public health interventions delivered in Islamic religious settings in the UK.
Table S2. Geographical areas1 with the highest Pakistani and Bangladeshi populations within England, Wales, Scotland and Northern Ireland (assessed August 20172)
Table S3. Name, location and source of identification of health promotion interventions partly associated with obesity (n = 8)
Table S4. Author, study design, outcome measures (where applicable), project name, location and source of identification of health promotion interventions not associated with obesity (n = 13)
Table S5. Aim and characteristics of health promotion interventions partly associated with obesity, and their evaluation where available (n = 8)
Table S6. Aim and characteristics of health promotion interventions not associated with obesity, and their evaluation where available (n = 13)


