Abstract
Introduction:
Traumatic brain injury (TBI) is of the most challenging public health problems.
Aim:
The aim of this study was to investigate the epidemiology of mild TBI, frequency of clinically important head injuries identifiable on computed tomography (CT) scans and also short-time outcomes of mild TBI in elderly population in north of Iran.
Patients and Methods:
A prospective epidemiological study was conducted at the Emergency department of Imam Khomeini general hospital, Mazandaran, Iran. Inclusion criteria were age older than 60, Glasgow coma scale (GCS) score of 13-15, and a single head trauma. Data were collected by retrospective chart review, interview with patients or their caregivers and contact with them after a week from time of discharge or transferring to another wards.
Results:
Response rate was estimated at 67.8% (n: 122/180). Mean age of patients was 65.54±6.42 years. 82% of patients were younger than 70. Mean time from head trauma to hospital admission was 270 minutes. In majority of patients, mechanism of trauma was fall (28%) and then interpersonal violence (25%). 6.6% (95% CI: 2.87 to 12.5%) of patients suffered from important radiologically head injuries and 2.5% (95% CI: 0.5-7.00) were readmitted to hospital within a week.
Conclusion:
Time to admission for minor TBI in elderly patients was too long and could be of clinical concern. Considering the lower prevalence of important radiologically head injury among elderly population, using any clinical guideline for indication of CT scan may be more cost-effective than routine use of CT scan. Although short term outcomes of minor TBI were less threatening and not lethal but these patients need follow-up.
Keywords: Craniocerebral Trauma, Aged, Tomography, X-Ray Computed, Iran
1. INTRODUCTION
Traumatic brain injury (TBI) is one of the most challenging public health problems, world-wide. Despite medical and pharmacological advances, more effective interventions are needed to improve TBI outcomes, especially in older adults (1, 2). There are egregious discrepancies regarding epidemiology of TBI in the world (1). These discrepancies could be explained mainly by cultural context of different societies (3, 4). Age and gender distribution, and also prevalence of interpersonal violence may be of main explanation of these discrepancies (1, 3). Although motor vehicle collision has been indicated as the most common cause of the TBI in the developing countries (5), several studies reported high differences across different world regions, which are not recognizable through such a holistic statement (4, 6). Accordingly, epidemiological studies are essential to provide necessary information related to TBI in order to develop proper strategies and programs for better TBI control and prevention and also clinically manage the patients in an evidence-based approach (1, 3, 6). Reports from Iran, have shown that incidence rate of head trauma had been less than the most of other countries (7–9). Some of these had reported that fall is the most common cause of TBI but the most others had shown that traffic collision is the most cause of TBI in Iran. The most of studies from Iran had been focused on the younger age groups and adults, and moderate to severe TBI due to traffic collision. They have paid less attention or even ignored mild TBI and elder patients (8–9). Additionally, older adults with TBI are at greater risk of morbidity and mortality compared to the younger patients (10).
The most of previous epidemiological studies had reported that more than 65% of the TBI patients could be categorized as mild TBI, according to Glasgow comma scale (GCS) score (6, 11–12). Despite of less lethal outcome of mild TBI, its incidence rate is very high. Additionally, due to the high incidence of TBI in patients who referred to the emergency departments (ED), this higher number of patients lead to a higher work load in the ED, increase health system expenditures, and, even with a lower risk of lethal outcomes, can result in a considerable number of patients with long time disability (13–14).
2. AIM
Considering the importance and limited evidence regarding TBI in older adults, the aim of this study was to investigate the epidemiology of mild TBI, frequency of clinically important head injuries identifiable on computed tomography (CT) scans and also short-time outcomes of mild TBI in elderly population in north of Iran.
3. PATIENTS AND METHODS
This prospective epidemiological study was conducted at the ED of Imam Khomeini hospital, a most known public hospital in Mazandaran province, north of Iran. Our hospital is an educational hospital and the referral center for head trauma in the Mazandaran University of Medical Science. Sampling population was defined as the almost all of consecutive eligible minor head trauma cases referred to our ED from March 20, 2016 to March 18, 2017. Inclusion criteria were age≥60 years and admission to the ED with head trauma and GSC score of 13-15. Patients with multiple injuries were not included. After approved of the study by the Ethics Committee of Mazandaran University of Medical Science, objectives of the study and procedures were explained to all eligible patients or their closed caregivers in details. Then they asked to sign the informed consent form. In some cases, and with the approval of the ethical committee of Mazandaran University of Medical Sciences, informed consent was taken verbally, considering cultural issues (16).
Except for a follow up at a week after the time of discharge or disposition from the ED, they were managed in a routine manner and according to the Iranian standards of practice for minor head trauma patients. Primary outcome was readmission to hospital due to current minor head trauma within a week after leaving the ED. Secondary outcome was any symptoms within follow-up period which was related to the current trauma. Data were collected by three trained and competent emergency nurses, one in each working shift. They were responsible to fill study data collection form for patients who were admitted during their shift by retrospective chart review, interview with patients or their caregivers and also contact with them after a week from time of discharge or disposition.
Data collection form was designed by research team and its validity was confirmed using content validity. Considering applicability of data collection in our setting, routine data gathered during patients’ admission and what is available by chart review were considered. Data form was used in a primary study and some corrections were made according to unavoidable field limitations. Final data form was consist of age, gender, habitation (rural/urban), time from trauma to admission (minutes), length of stay (LOS) in the ED, mechanism of head trauma (fall, interpersonal violence, objects striking the head, during traffic collision, and sport-related, work-related), GCS score at admission time, number of vomiting or convulsion from time of trauma to admission, loss of consciousness (Yes/No; its duration if applicable), drowsiness (Yes/ No), vertigo (Yes/ No), headache (Yes/ No), restlessness (Yes/ No), vital signs (systolic and diastolic blood pressure, heart rate, and body temperature), important head injures identifiable on cranial CT scan (Yes/ No; its type if applicable) according to the report of radiologist, need neurosurgical intervention (Yes/ No), readmission after discharge or disposition from the ED, any symptoms within follow-up period which was related to the current trauma (headache, convulsion, restlessness, disorientation, lack of consciousness and others), and interviewee’s phone number (for future contacts and follow-up).
Statistical analysis
Data cleaning and preparation procedures were performed using available statistical procedures (17). Data were described using absolute and relative frequencies, mean, median and standard deviation (SD). Univariate associations were tested applying Chi square, independent sample t test, one-way analysis of variance and Mann-Whitney U tests. 95% confidence intervals were estimated assuming binomial distribution. A two-sided P-value of less than 0.05 was considered as statistical significant level. Statistical analysis was done using Stata version 11.2.
RESULTS
Out of 180 minor head trauma patients admitted to our ED, 122 patients accept to participate in the study. Accordingly, response rate was estimated at 67.8%. Seventy-two patients were male. There was a statistically significant deference between proportion of male (57.38, 95% CI: 48.60-66.16) and female (42.62, 95% CI: 33.84-51.39) patients (P-value= 0.021). Out of study participants, 67.21 of patients were referred from urban and 32.79 of them come from rural areas. Mean±SD and median of age of male and female patients were 65.54±6.42 and 63.00 years, respectively. Around 82% of all patients and in both genders were younger than 70 years (Figure 1). Mean±SD and median of time from trauma to admission were 314.75±169.57 and 270 minutes, respectively. This time was not statistically different between males (mean±SD: 322.78±169.45) and females (mean ± SD: 303.94±170.77, P=0.424).
Figure 1.
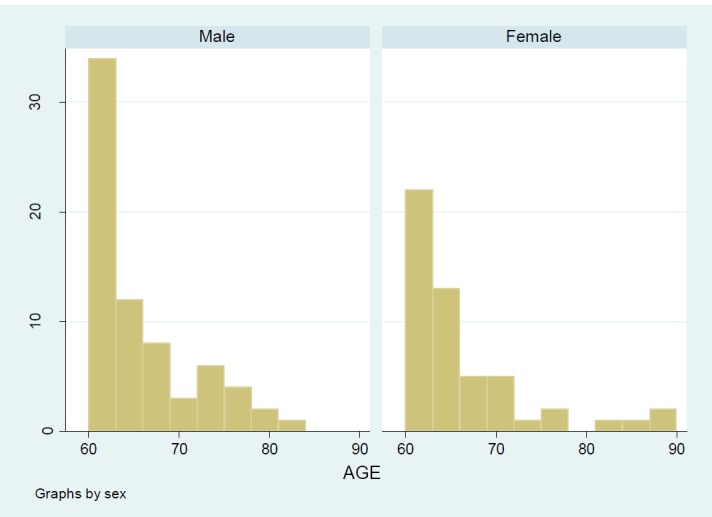
Age and gender distribution of elderly (60 years and older) minor head trauma patients referred to the ED
Longest time from trauma to admission was reported for trauma due to interpersonal violence with a mean± SD and median of 342.72±193.26 and 305 minutes, respectively. Shortest time to admission was reported for trauma due to traffic collision with a mean± SD and median of 288±159.60 and 270 minutes, respectively. For a majority of patients, mechanism of trauma was reported to be fall and then interpersonal violence. Proportion of trauma from interpersonal violence was higher among males than females (Table 1).
Table 1. Frequency (relative frequency, 95% CI) of minor head trauma among 60 years and older population, according to mechanism of trauma and gender. Abbreviation: CI, confidence interval.
| Mechanism | Males | Females | P-value |
|---|---|---|---|
| Fall | 27(0.39,0.27-0.51) | 29(0.56,0.41-0.70) | 0.063 |
| Interpersonal violence | 30(0.43,0.31-0.55) | 16(0.31,0.19-0.45) | 0.177 |
| Traffic collision | 4(0.06, 0.02-0.14) | 1(0.02, 0.00-0.10) | 0.075 |
| Others | 9(0.13, 0.06-0.23) | 6(0.12, 0.04-0.23) | 0.869 |
| Total | 70(0.57, 0.48-0.66) | 52(0.43, 0.34-0.52) | 0.021 |
Two of the most common symptoms at admission were vertigo (31.15%) and vomiting (18.85%), respectively. 14.75% of patients were unconsciousness and 2.4% were drowsiness and 3.8% reported restlessness at the time of admission. Mechanism of trauma and gender were not statistically associated with type of symptoms at admission. Mean ±SD, median and 25th and 75th percentile of systolic and diastolic blood pressure, heart rate and body temperature are presented in Table 2. According to the radiologist’s report, there were only eight case with important head injures identified on CT scans which is equal with 6.6% of study participant with a 95% confidence interval of 2.87 to 12.5%. Out of eight patients with important head injury, three had brain contusion (2.46%, 95% CI: 0.5-7.00) and five had skull fracture (4.10%, 95% CI: 1.34-9.30). No other injury was identified on CT scans. Only one case need neurosurgical intervention. According to follow-up data, three patients (2.5%, 95% CI: 0.5-7.00) were readmitted to hospital within a week from discharge or disposition from the ED. In addition, 6.56% (95% CI, 2.87-12.51) had headache and 7.34 (95% CI: 3.43-13.54) had vertigo within follow-up period.
Table 2. Vital sings at admission in elderly patient admitted to the ED due to minor head trauma. Abbreviation: SD, standard deviation .
| Sing at admission | Mean ±SD | Median | 25th percentile | 75th percentile |
|---|---|---|---|---|
| Systolic blood pressure | 127.30±16.35 | 130 | 120 | 135 |
| Diastolic bloodpressure | 78.99±9.18 | 80 | 70 | 80 |
| Heart rate | 80.91±7.76 | 80 | 78 | 88 |
| Body temperature | 36.67±3.35 | 37 | 37 | 37 |
5. DISCUSSION
In this epidemiological study it has been shown that more than half of elder patients with mild TBI referred to the ED at least with four hours delay from the time of trauma. The most common cause of TBI was different between males and females. However, fall was the most selfreported common cause of mild TBI. Rate of radiological important head injuries and rate of readmission during a week of disposition from the ED were at 6.6% and 2.5%, respectively. We also have shown that frequency of elder males and younger elders are higher than other patients with TBI who referred to out referral ED.
Rate of abnormal findings which were identified on CT scans were meaningfully less than previous studies. Despite of reasons of this difference, it probably could be interpreted as overuse of CT scan in such cases. Overuse of CT scan may be due to tenacity of patients’ caregivers or absence of a universal indication guideline accepted in Iranian EDs and even ignorance of available international indication guidelines (18, 19). According to the study findings, less serious short time outcomes were observed within a week after disposition of patient. It may be a result of high quality care provided for these patients in our department as well as less serious TBI in elderly population in north of Iran. We could not able to find any previous study from Iran which had reported outcomes of mild TBI. Studies from other regions but have reported. Considering timely care as an influential determinant of the outcome TBI, at least four hours delay to admission may be of clinical concerns. Delayed admission was more concerning in cases due to interpersonal violence and less serious in cases due to traffic collision. This issue has to be investigated in future studies to provide more timely emergency care to mild TBI patients.
In line with some previous studies in elderly populations (20) the most common cause of minor head trauma among males and females were interpersonal violence and fall, respectively. Bordignon et al. (21) had also reported that interpersonal aggression, fall and automobile accidents were respectively the most common causes of minor head trauma in their study. This agreement was in spite of different age groups of studied populations in our study (60 years and older) versus other studies (all age groups). On the other hand, two systematic reviews from Europe have reported that fall and then traffic collision were the first two cause of TBI (4, 6). Another population-based study from New Zealand reported a different pattern of the cause of mild TBI (22). Cultural contexts may be the best explanation for variation of cause of TBI in different countries (3, 5, 13).
Male: Female ratio was estimated at 1.4:1. It is meaning fully less than previous reports by Iranian authors ranged from 2:1 to 4.5:1 (7-9). It may be mainly due to different populations which were previously studied compare with our study population. In this study we focused on the elderly population which are less affected by gender related socioeconomic factors (22–24). Higher risk of younger males compared with younger females may be a major cause of greater male/female ratios in previous studies (24–25). In this study, characteristics and short-term outcome of a representative sample of minor TBI among elderly population of north of Iran were epidemiologically reviewed. Accordingly, we hope our results were generalizable to at least other parts of Iran and culturally similar countries. However, due to restricted number of elder patients with minor TBI, statistical power of our study was moderate. Future studies with a higher statistical power may be valuable.
6. CONCLUSION
Time to admission for minor TBI in elderly patients was too long and could be of clinical concern. Considering the lower prevalence of important radiologically head injury among elderly population, using any clinical guideline for indication of CT scan may be more cost-effective than routine use of CT scan. Although short term outcomes of minor TBI were less threatening and not lethal but these patients need follow-up.
Acknowledgments:
We thank to Mazandaran university of Medical Sciences for financial support.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent forms.
Author’s contributions:
Study conception and design: SMH and FJ. Acquisition of data: SMH, FJ, IGK, AA and SMT. Statistical analysis and interpretation of data: SMH and SMT. Drafting of the manuscript: SMH, FJ, IGK and SMT. Critical revision of the manuscript for important intellectual content: SMH, FJ, IGK, AA and SMT.
Conflict of interest:
The authors declare no conflicts of interest.
Financial support:
This study has been financially supported by the deputy of research and technology, Mazandaran University of Medical Sciences, Sari, Iran.
REFERENCES
- 1.Roozenbeek B, Maas AI, Menon DK. Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol. 2013;9(4):231–236. doi: 10.1038/nrneurol.2013.22. [DOI] [PubMed] [Google Scholar]
- 2.Frost RB, Farrer TJ, Primosch M, Hedges DW. Prevalence of traumatic brain injury in the general adult population: a meta-analysis. Neuroepidemiology. 2013;40(3):154–159. doi: 10.1159/000343275. [DOI] [PubMed] [Google Scholar]
- 3.Andelic N. The epidemiology of traumatic brain injury. Lancet Neurol. 2013;12(1):28–29. doi: 10.1016/S1474-4422(12)70294-6. [DOI] [PubMed] [Google Scholar]
- 4.Peeters W, van den Brande R, Polinder S, Brazinova A, Steyerberg EW, Lingsma HF, et al. Epidemiology of traumatic brain injury in Europe. Acta Neurochir (Wien) 2015;157(10):1683–1696. doi: 10.1007/s00701-015-2512-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galgano M, Toshkezi G, Qiu X, Russell T, Chin L, Zhao LR. Traumatic Brain Injury: Current Treatment Strategies and Future Endeavors. Cell Transplant. 2017;26(7):1118–1130. doi: 10.1177/0963689717714102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faul M, Coronado V. Epidemiology of traumatic brain injury. Handb Clin Neurol. 2015;127:3–13. doi: 10.1016/B978-0-444-52892-6.00001-5. [DOI] [PubMed] [Google Scholar]
- 7.Rahimi-Movaghar V, Rasouli MR, Ghahramani M. The incidence of traumatic brain injury in Tehran, Iran: a population based study. Am Surg. 2011;77(6):e112–114. [PubMed] [Google Scholar]
- 8.Farzaneh E, Fattahzadeh-Ardalani G, Abbasi V, Kahnamouei-Aghdam F, Molaei B, Iziy E, et al. The epidemiology of hospital-referred head injury in Ardabil City. Emerg Med Int. 2017;2017:1439486. doi: 10.1155/2017/1439486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aghakhani N, Azami M, Jasemi M, Khoshsima M, Eghtedar S, Rahbar N. Epidemiology of traumatic brain injury in urmia, iran. Iran Red Crescent Med J. 2013;15(2):173–174. doi: 10.5812/ircmj.2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: epidemiology, outcomes, and future implications. J Am Geriatr Soc. 2006 Oct;54(10):1590–1595. doi: 10.1111/j.1532-5415.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rickels E, von Wild K, Wenzlaff P. Head injury in Germany: a population-based prospective study on epidemiology, causes, treatment and outcome of all degrees of head-injury severity in two distinct areas. Brain Inj. 2010;24(12):1491–1504. doi: 10.3109/02699052.2010.498006. [DOI] [PubMed] [Google Scholar]
- 12.Styrke J, Stålnacke B-M, Sojka P, Björnstig U. Traumatic brain injuries in a well-defined population: epidemiological aspects and severity. J Neurotrauma. 2007;24(9):1425–1436. doi: 10.1089/neu.2007.0266. [DOI] [PubMed] [Google Scholar]
- 13.Tagliaferri F, Compagnone C, Korsic M, Servadei F, Kraus J. A systematic review of brain injury epidemiology in Europe. Acta Neurochir (Wien) 2006;148(3):255–268. doi: 10.1007/s00701-005-0651-y. [DOI] [PubMed] [Google Scholar]
- 14.Corrigan JD, Selassie AW, Orman JAL. The epidemiology of traumatic brain injury. J Head Trauma Rehabil. 2010;25(2):72–80. doi: 10.1097/HTR.0b013e3181ccc8b4. [DOI] [PubMed] [Google Scholar]
- 15.Humphreys I, Wood RL, Phillips CJ, Macey S. The costs of traumatic brain injury: a literature review. Clinicoecon Outcomes Res. 2013;5:281–287. doi: 10.2147/CEOR.S44625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vardanjani HM, Baneshi MR, Haghdoost A. Cancer Visibility among Iranian Familial Networks: To What Extent Can We Rely on Family History Reports? PLoS One. 2015;10(8):e0136038. doi: 10.1371/journal.pone.0136038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Molavi Vardajani H, Haghdoost AA, Shahravan A, Rad M. Cleansing and preparation of data for statistical analysis: A step necessary in oral health sciences research. J Oral Health Oral Epid. 2016;5(4):171–185. [Google Scholar]
- 18.Smits M, Dippel DW, de Haan GG, Dekker HM, Vos PE, Kool DR, et al. External validation of the Canadian CT Head Rule and the New Orleans Criteria for CT scanning in patients with minor head injury. JAMA. 2005;294(12):1519–1525. doi: 10.1001/jama.294.12.1519. [DOI] [PubMed] [Google Scholar]
- 19.Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357(9266):1391–1396. doi: 10.1016/s0140-6736(00)04561-x. [DOI] [PubMed] [Google Scholar]
- 20.Harvey LA, Close JC. Traumatic brain injury in older adults: characteristics, causes and consequences. Injury. 2012;43(11):1821–1826. doi: 10.1016/j.injury.2012.07.188. [DOI] [PubMed] [Google Scholar]
- 21.Bordignon KC, Arruda WO. CT scan findings in mild head trauma: a series of 2,000 patients. Arq Neuropsiquiatr. 2002;60(2-A):204–210. doi: 10.1590/s0004-282x2002000200004. [DOI] [PubMed] [Google Scholar]
- 22.Feigin VL, Theadom A, Barker-Collo S, Starkey NJ, McPherson K, Kahan M, et al. Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet Neurol. 2013;12(1):53–64. doi: 10.1016/S1474-4422(12)70262-4. [DOI] [PubMed] [Google Scholar]
- 23.Stevens JA, Sogolow ED. Gender differences for non-fatal unintentional fall related injuries among older adults. Injury Prevention. 2005;11(2):115–119. doi: 10.1136/ip.2004.005835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peloso PM, Von Holst H, Borg J. Mild traumatic brain injuries presenting to Swedish hospitals in 1987-2000. J Rehabil Med. 2004;(43 Suppl):22–27. doi: 10.1080/16501960410023714. [DOI] [PubMed] [Google Scholar]
- 25.Gholipour Baradari A, Sharifi H, Firouzian A, Daneshiyan M, Aarabi M, Talebiyan Kiakolaye Y, et al. Comparison of Proposed Modified and Original Sequential Organ Failure Assessment Scores in Predicting ICU Mortality: A Prospective, Observational, Follow-Up Study. Scientifica (Cairo) 2016;2016:7379325. doi: 10.1155/2016/7379325. [DOI] [PMC free article] [PubMed] [Google Scholar]


