Abstract
Background
Young adult drug use and law breaking behaviors often have roots in adolescence. These behaviors are predicted by early drug use, parental substance use disorders, and disrupted and conflict-ridden family environments.
Aim
To examine long-term outcomes of Brief Strategic Family Therapy (BSFT) compared to treatment as usual (TAU) in the rates of drug use, number of arrests and externalizing behaviors in young adults who were randomized into treatment conditions as adolescents.
Design
261 of 480 adolescents who had been randomized to BSFT or TAU in the BSFT effectiveness study were assessed at a single time, 3–7 years post randomization
Methods
Assessments of drug use, externalizing behaviors, arrests and incarcerations were conducted using Timeline Follow Back, Adult Self Report and self-report, respectively. Drug use, arrests and incarcerations were examined using negative binomial models and externalizing behaviors were examined using linear regression.
Results
When compared with TAU, BSFT youth reported lower incidence of lifetime (IRR = 0.68, 95% CI [0.57, 0.81]) and past year (IRR = 0.54, 95% CI [0.40, 0.71]) arrests; lower rates of lifetime (IRR=0.63, 95% CI [0.49, 0.81]) and past year (IRR = 0.70, 95% CI [0.53, 0.92]) incarcerations; and lower scores on externalizing behaviors at follow-up (B = −0.42, SE = .15, p = .005). There were no differences in drug use.
Conclusion
BSFT may have long term effects in reducing the number of arrests, incarcerations and externalizing problems. These effects could be explained by the improvements in family functioning that occurred during the effectiveness study.
Keywords: young adulthood, family therapy, Brief Strategic Family Therapy, substance abuse, substance abuse treatment, arrests, incarcerations, externalizing behaviors
1. Introduction
Young adulthood is the peak age period for binge drinking, illegal drug use, risky sexual behavior and delinquent acts.1,2Adult substance use and law-breaking behaviors often have their roots in adolescence. Adolescents most at risk for these substance abuse trajectories are those who initiate substance use at young ages (usually before age 14 or 15), whose involvement is especially severe, who have experienced traumatic events, and who come from dysfunctional families.3 Substance use and externalizing behaviors are likely linked because they share common risk factors such as parental substance use disorders, disrupted and conflict-ridden family environments, and dispositional risk factors.4,5 Family-based interventions such as Multisystemic Therapy, Multi-dimensional Family Therapy, Functional Family Therapy, and Brief Strategic Family Therapy have been shown to be particularly promising in treating adolescent drug use and related behavior problems.6–8 To date, very few studies have examined the long-term effects of family therapy during adolescence on outcomes during young adulthood.6,8 Two randomized clinical trials of Multisystemic Therapy have established long term effects in reducing marijuana use and aggressive criminal activity9,10 and arrests and incarcerations.11,12
Brief Strategic Family Therapy® (BSFT®)3,13,14 is an empirically supported family approach that has been shown to be efficacious in the prevention15 and treatment16–18 of adolescent drug use and associated externalizing behavior problems. BSFT considers adolescent symptoms to be rooted in maladaptive family interactions and it operates according to the assumption that transforming family interactions directly linked to the problem behaviors and improving family functioning will correct these problems. A recent clinical trial that randomized 480 adolescents and their families to BSFT or treatment as usual (TAU)19 in community settings demonstrated that BSFT was more effective in engaging and retaining adolescents and family members into treatment and improving family functioning.20 In addition, median treatment differences in adolescent drug use appeared one year post randomization with youth in BSFT demonstrating significantly less use than youth in TAU.
Building on these outcomes, this study conducted a cross-sectional follow-up to examine whether young adults who received either BSFT or TAU as adolescents in the BSFT effectiveness study, differed in drug use, externalizing behaviors and rates of arrests and incarcerations.
2. Methods
The methods and research strategies of the BSFT effectiveness study are summarized here, and are described in more detail in Robbins et al.21,20
2.1. Participants and design
The effectiveness study randomized 480 drug using adolescents and their family members to BSFT or TAU in 8 outpatient community treatment providers (CTPs) across the country.21,20 To enroll, adolescents ages 12–17, had to self-report illicit drug use in the 30-day period preceding the baseline assessment or had to be referred from an institution (e.g., detention, residential treatment, court, etc.) for drug abuse outpatient treatment. Adolescents were excluded if they were expected to reside in a halfway house, institution, independent or assisted living, foster care, or outside of the agency’s geographical area. Adolescents with current/pending severe criminal offenses (e.g. murder, aggravated assault, and sexual assault) that could have resulted in incarceration were excluded. All exclusionary criteria were intended to maximize availability of families and adolescents for the BSFT intervention and for follow-up assessments. Finally, adolescents had to assent and a parent or legal guardian had to consent to participate in the study.
Adolescents were predominately male (78.45%; N=377) with a mean age of 16.01 (SD = 1.8). The sample included 213 (44.3%) Hispanic/Latino, 148 (30.8%) non-Hispanic White, and 110 (22.9%) Black/African Americans. Most families were biological one-parent (N=224 46.6%) or two-parent (N=120 25%) households, and approximately half of the families reported a household income of less than $25,000. Seventy two percent of the participants were referred for drug treatment by the juvenile justice system. At baseline, 69% of adolescents met criteria for substance abuse or dependence criteria (DSM-IV-TR), 50% of adolescents reported at least one externalizing disorder (such as aggressive or rule-breaking behavior) and 52% reported at least one internalizing disorder (such as anxiety/depression or being withdrawn). Only 378 of the 480 adolescents that participated in the BSFT effectiveness study agreed to be contacted for future studies, and of those 261 were successfully assessed in this study.
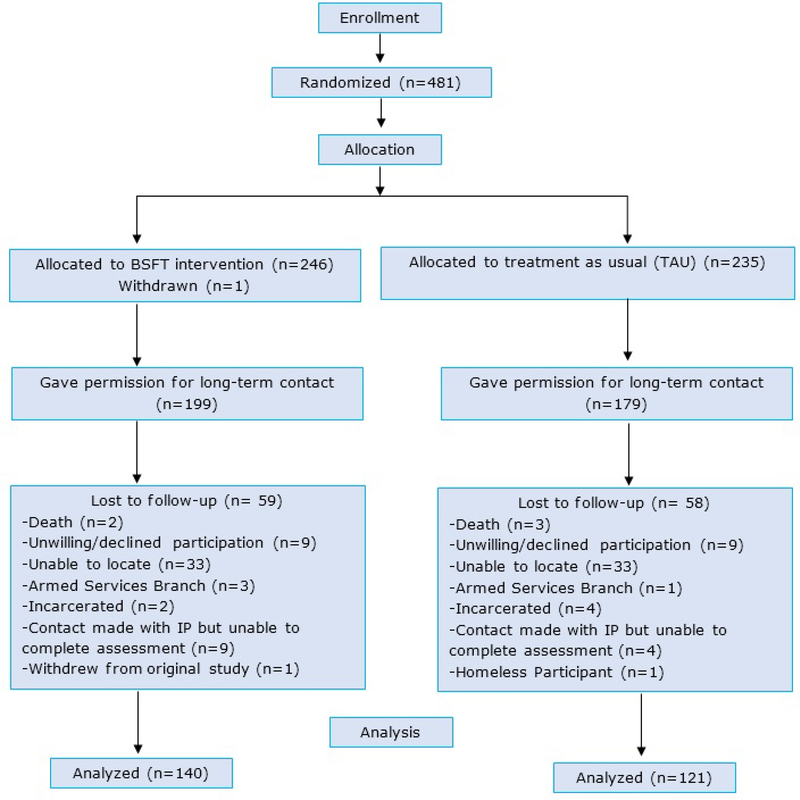
Outreach and assessments for this study were conducted from June 2010 to July 2011 by site research staff who had participated in the effectiveness study. A variety of IRB approved outreach procedures were used to contact participants including relying on the locator information they had provided, accessing public, local offender and court record databases and social media. Because this study was funded independently and after the completion of the effectiveness study, long term follow up assessments occurred on average, 4.7 years post randomization (range 3–7 years). The study was approved by the University of Miami IRB, University of Arizona IRB, University of Cincinnati IRB, UCLA IRB and Universidad Central del Caribe IRB. Participants in the final study sample were not significantly different from those in the original sample (N=480) in demographics nor in outcome variables (see Table 1 under results). A consort flow diagram listing, by treatment condition, the reasons participants were lost to follow up is presented in figure 1.
Table 1.
Baseline characteristics of the study sample that participated in the extended follow up, compared to those that did not.
| Variable | “In study” group1 (n=2613) | “Not in study” group1 (n=2194) | p-value2 |
|---|---|---|---|
| Gender | 0.657 | ||
| Male | 207 (79.3%) | 170 (77.6) | |
| Female | 54 (20.7%) | 49 (22.4) | |
| Race/Ethnicity | 0.544 | ||
| Hispanic | 119 (45.6) | 94 (42.9) | |
| Non-Hispanic White | 84 (32.2) | 64 (29.2) | |
| Non-Hispanic Black | 54 (20.7) | 56 (25.6) | |
| Other | 4 (1.5) | 5 (2.3) | |
| Age (at baseline) | 16 (15, 17) | 16 (15, 17) | 0.310 |
| % drug days | 11 (0, 40) | 7 (0, 27) | 0.253 |
| Externalizing Behavior5 | 0.078 (3.183) | −0.128 (3.043) | 0.470 |
| Number of Arrests | 1 (0, 2) | 1 (0, 2) | 0.431 |
| Number of Juvenile Detentions | 1 (0, 1) | 1 (0, 1) | 0.967 |
| Family Functioning6 | −0.196 (5.806) | 0.071 (5.475) | 0.604 |
For categorical variables, N (%). For continuous variables, Means (SD) for approximately normal variables and Median (Q1, Q3) otherwise.
For categorical variables, Fisher’s exact test p-values. For continuous variables, T-tests p-values for approximately normal variables and Wilcoxon two sample p-values otherwise.
Except for % drug days (n=258), number of arrests (n=260), and number of juvenile detentions (n=207).
Except for % drug days (n=218) and number of juvenile detentions (n=170).
The reported value for externalizing is the mean of the square root of the raw score.
The reported value for family functioning is the mean of the composite created for this outcome.
Figure 1.
Consort Flow diagram
Most (N=252) of the assessments were conducted in person. Telephone assessments were conducted for those unable to attend in person (N=9). The urine drug screening was not completed by those who participated by phone (N=9), those in jail (N=9), and one other who refused. Research assistants were trained to competence in the administration study measures and research procedures.
2.2. Measures
Drug Use
The Timeline Follow Back interview (TLFB)22 uses a calendar and memory prompts to stimulate recall for retrospective reports of daily substance use for the 90 days preceding the assessment. The TLFB yields consistently high test–retest correlations.23 Assessments of the presence of 10 different drugs, but not levels of toxicity, were conducted using Sure Step 10 urine drug screens and urine cups. These tests include temperature verification and detection of adulterants. Urine drug screens were administered immediately prior to the TLFB to improve veracity of drug use report.
Externalizing behaviors
Externalizing behaviors were assessed using the externalizing scale of the Adult Self Report,24 a 123 item self-report scale designed for 18- to 59-year-olds. Items are on a 3-point Likert-type scale (0 = not true, 1 = somewhat or sometimes true, 2 = very true or often true). The externalizing scale is comprised by the aggressive, rule breaking, and intrusive syndromes. The problem syndromes have been normed on a nationally representative sample of 2,020 United States adults.24 Scores were square-root transformed to more closely approximate a normal distribution; therefore, those participants with greater severity show greater reductions than those with a lower severity.
Criminal Justice Involvement
Participants were asked, “How many times have you been arrested in your life?” (lifetime) and “How many times have you been arrested in the past year?” (current). Similarly worded questions were asked for “incarceration.” Because many arrests do not lead to incarceration for youth we included both variables in our analyses.
Family Functioning
The family functioning measure was a composite of parent report of family cohesion, family conflict, positive parenting, discipline effectiveness, avoidance of discipline, and monitoring25 subscales. These were measured at baseline, 4, 8 and 12 months post-randomization during the effectiveness trial.20
2.3. Interventions
Treatment as Usual (TAU)
TAU varied depending on the treatment programs at 8 participating CTPs. TAU included one or more of the following: individual and/or group therapy, parent training groups, non-manualized family therapy, and case management. A pre-requisite for participation was that the CTP’s TAU had to include at least 12–16 planned sessions to ensure same planned dose opportunity as in BSFT. Most CTPs provided treatment opportunities well beyond 16 sessions, with unlimited booster sessions.
Brief Strategic Family Therapy (BSFT)13,3
BSFT is a present-oriented, problem-focused, directive, and practical approach. It focuses on improving family functioning by identifying and altering patterns of family interaction that are directly related to adolescent’s substance abuse and related behavioral problems. BSFT aims to improve parental leadership, parent involvement, and positive parenting practices, all of which have been shown to serve as protective factors against adolescents’ later substance use and the negative effects of deviant friends, neighborhood crime, and underperforming schools.26–29BSFT therapeutic strategies are organized into four theoretically and empirically supported domains: Joining, tracking and diagnostic enactments, reframing and restructuring 30,13 BSFT had a planned dose of 12 to 16 sessions, which occurred over an 8- month period. The majority (97%) of the BSFT sessions involved multiple family members.
2.4. Therapy Dose
Dose in both conditions was tracked through monthly therapists’ interviews. Therapists also reported on any additional treatment services that their cases received. Total dose was constructed as the sum of all therapy sessions conducted by any therapist (not just the study-therapist) at the agency. Retention was defined as attendance to 8 or more sessions.
Therapist demographic characteristics, BSFT training, supervision, and adherence to BSFT was reported in Robbins et al.20 Therapists achieved a mean of 3.49 (SD = .52) out of 5, with a 3 as the minimally accepted level of adherence. The relationship between BSFT therapeutic strategies and outcomes was reported in Robbins et al.30 .
2.5. Analysis Plan
The plan was to first determine whether participants in this study differed from the original study participants on important baseline characteristics. Second, we examined whether any of our outcome variables or demographic characteristics differed by condition at the time of randomization. For our primary analyses, we examined differences by treatment assignment in drug use, externalizing, arrests and incarcerations at the long-term follow-up. Because drug use, arrests and incarcerations were count variables, Poisson and negative binomial distributions were examined. The negative binomial showed a better fit to the data so this analytical approach was used. We present the incidence rate ratio associated with these analyses as an effect size for these variables. Externalizing was analyzed using linear regression. For each of these outcomes a series of regression models were tested. Model 1 tested the main effect of treatment condition on these outcomes. Model 2 tested the main effects of treatment condition and retention. Model 3 tested the interaction between treatment condition and retention, controlling for the main effects. All analyses were estimated as generalized estimating equations which controlled for dependencies in the data resulting from different participants working with the same therapist and included fixed effects for recruitment site and time since randomization into the main study. Analyses were conducted using SAS 9.3.
Finally, we examined whether our previously reported increase in family functioning over the course of the effectiveness study mediated the impact of BSFT on the long-term follow-up outcomes. This required replicating the model test for the impact of BSFT on family functioning from the previous report on this study sample (i.e. those that completed the long term follow up assessment). The test for mediation was done in a single model including all long-term differential outcomes between conditions (Figure 1). The presence of mediation was assessed by testing the significance of the product of the coefficient of family functioning (measured independently as linear change in family functioning, and level of family functioning at 12 months) with the coefficient of family functioning on the long-term outcomes using the model constraint option in Mplus 7.
In post-hoc analyses, we explored whether there were any differences in outcomes across race/ethnicity, in particular whether race/ethnicity moderated effects of the intervention.
3. Results
Demographics
Participants in the follow-up study (N=261) did not differ from those who did not participate in the follow-up study (N=219) on any of the key baseline variables. These variables included age, race/ethnicity, gender, percent of drug use days (of the last 90 days), externalizing behaviors (such as rule-breaking and aggression), arrests, incarcerations and family functioning (see Table 1). The outcome variables, drug use days, externalizing, arrests and incarcerations did not differ significantly by treatment condition at baseline in either the full sample from the effectiveness study (N=480) or the follow-up study sample (N=261). There were no differences between treatment conditions in the numbers of years from randomization to completion of the follow-up assessment (BSFT Mean=4.82, SD=0.66; TAU Mean =4.71, SD=0.70, t(259)=1.25, p<.21).
Substance Use
A small percentage of individuals (N=7, 5.3%) indicated that they were currently receiving drug or alcohol treatment at the follow-up assessment, and this did not differ by treatment condition. More than one-third of the participants (N= 94, 36%) reported using both marijuana and alcohol in the 90 days preceding the follow-up assessment. About one-quarter (N=66, 25.2%) indicated using alcohol, marijuana and other drugs. Smaller percentages were using marijuana only (N=30, 11.4%) and alcohol only (N=29 11.1%). Very few participants reported using alcohol and drugs other than marijuana (N=5, 1.9%) or marijuana and other drugs (N=5, 1.9%). Few participants (N=32, 12.2%) reported no substance use. No statistical differences were observed between conditions in any of these categories (See Table 2). Fewer than 10% of adolescents in the study (N = 20) indicated no drug use in the past 30 days, but had a positive urine screen.
Table 2:
Long term Outcomes by treatment condition.
| BSFT | TAU | Significance | |
|---|---|---|---|
| In Drug or alcohol Treatment | N=7 5.0% | N=7 5.8% 55.8%555.8% | χ2(1) = 0.07, p =.79 |
| Substance use in last 90 days | |||
| Alcohol, marijuana and other drugs | N=31 22.1% | N=35 28.9% | χ2(1) = 1.58, p =.21 |
| Marijuana and alcohol | N=54 38.6% | N=40 33.1 % | χ2(1) = 0.86, p = .35 |
| Marijuana only | N=17 12.1% | N=13 10.7% | χ2(1) = 0.12, p = .72 |
| Alcohol only | N=14 10.0% | N=15 12.4% | χ2(1) = 0.38, p =.54 |
| Alcohol and drugs other than | N=2 1.4% | N=3 2.5% | χ2(1) = 0.38, p =.54 |
| Marijuana and other drugs | N=2 1.4% | N=3 2.5% | χ2(1) = 0.38, p = .54 |
| No substance Use | N=20 14.3% | N=12 9.9% | χ2(1) = 1.15, p =.28 |
| Mean drug use days* | 38.2 SE= 2.9 | 40.4 SE= 2.4 | χ2(1) = 0.67, p =.41 |
| Employment | |||
| Current employment | N=52 37.4% | N=48 39.7% | χ2(1) = 0.14, p=.71 |
| Lifetime employment | N=64 73.6% | N=61 83.6% | χ2(1) = 2.32, p=.13 |
| Number of times living arrangements changed | 1.2 SE=.15 | 2.2 SE=.26 | χ2(1) = 12.29, p = 0.0005 |
| Externalizing** | 3.11 SE=.10 | 3.53 SE=.13 | χ2(1) = 8.07, p = 0.005 |
| Arrests*** | |||
| Lifetime | 4.0 SE = .25 | 5.9 SE =.55 | χ2(1) = 17.81, p <.001 |
| Last year | .37 SE=.05 | .70 SE=.12 | χ2(1) = 18.24, p <.001 |
| Incarcerations**** | |||
| Lifetime | 2.1 SE = .20 | 3.3 SE =.42 | χ2(1) = 12.89, p <.001 |
| Last year | .40 SE=.03 | .57 SE=.07 | χ2(1) = 6.71, p =.01 |
no differences in means at baseline BSFT Mean = 6.3, SE = .52; TAU Mean = 6.4, SE = .50 χ2(1) = 0.01, p = .92
no differences in means at baseline BSFT Mean = 19.4, SE = .55; TAU Mean = 19.6, SE = .85 χ2(1) = 0.04, p = .84
no differences in means at baseline BSFT Mean = 1.1, SE = .11; TAU Mean = 1.2, SE = .15 2(1) = 0.12, p = .73
no differences in means at baseline BSFT Mean = 0.6 (SE=.08), TAU Mean = 0.6, SE=.09 χ2(1) = 0.04, p < .84
There was not a significant difference in number of drug use days by treatment condition (IRR = 0.95, 95% CI[0.81,1.10]). The estimated means for drug use days over the prior 90 days were 38.2 (SE= 2.9) in BSFT and 40.4 (SE= 2.4) in TAU (χ2(1) = 0.67, p= 0.41). The estimated means for drug use days over the prior 30 days were 12.1 (SE= 0.4) in BSFT and 13.8 (SE= 0.8) in TAU. There were also not a significant difference across treatment condition in drug use measured by urine screen (χ2(1) = 0.30 p = .59). Retention in treatment (attending 8+ sessions) was related to reduced drug use at follow-up across treatments (IRR = 0.75, 95% CI[0.58, 0.97]). There was not a treatment condition by retention interaction for drug use (χ2(1) = 1.32, p = .25).
Externalizing behaviors
When compared to TAU, participants in BSFT reported significantly lower externalizing behaviors (B = −0.42, SE = .15, p = .005). This represents a standardized difference between the treatments of −0.26 which is between a small (0.1) and medium (0.5) effect size.31 There was not a statistically significant impact of retention in treatment on externalizing behaviors (B = −0.11, SE = 0.10, χ2(1) = 0.32, p < .57) and the interaction of treatment condition and retention was not significant (B = −0.03, SE = 0.39, χ2(1) = 0.01, p < .94).
Arrests
The rate of lifetime and last year arrests in BSFT was significantly lower than in TAU (IRR = 0.68, 95% CI [0.57, 0.81]; IRR = 0.54, 95% CI [0.40, 0.71]). The mean number of lifetime arrests in BSFT was 4.0 (SE = .25) and in TAU was 5.9 (SE = 0.55). There was a main effect of retention in treatment on lifetime (IRR = 0.76, 95% CI [0.61, 0.95]) and last year (IRR=0.61, 95% CI [0.45, 0.84]) arrests. There was not a significant interaction of treatment and retention for lifetime arrests (B = .11, SE = 0.22, χ2(1) = 0.26, p < .61) or last year arrests (B = .23, SE = .33, χ2(1) = 0.49, p = .48).
Incarcerations
Relative to TAU, BSFT had significantly lower rates of lifetime incarcerations (IRR=0.63, 95% CI [0.49, 0.81]) and last year incarcerations (IRR = 0.70, 95% CI [0.53, 0.92]). The mean number of lifetime incarcerations at follow-up in BSFT was 2.1 (SE = .20) and in TAU was 3.3 (SE = .42). Participants who were retained in treatment showed significantly different rates of last year incarcerations (IRR = 0.65, 95% CI [0.45, 0.93]) than those not retained, but there were no differences for lifetime incarcerations (IRR = 0.84, 95% CI [0.58, 1.22]). There was no evidence of a retention by treatment condition interaction on lifetime (b = −0.13, SE = 0.35, χ2(1) = 0.14, p = .71) or last year (b = 0.26, SE = 0.24, χ2(1) = 0.71, p < .40) incarcerations.
Mediation analyses
Whereas in the effectiveness study20, there was a significant effect of BSFT on the trajectory of family functioning, this relationship was weak in the long-term follow-up sample. In this sample, the pathway from BSFT to the linear rate of change in family functioning was a=.25 (SE = .13, χ2(1) = 3.74, p = .053) and for the level of family functioning at month 12 (the intercept was centered at month 12) of the main study was a=.20 (SE = .10, χ2(1) = 3.58, p = .058). As shown in Table 3, both linear change in family functioning and level of family functioning at 12 months were significant predictors of externalizing, last year arrests, lifetime arrests, and lifetime incarcerations at the long-term follow-up. Linear change in family functioning was also a significant predictor of last year incarcerations, but 12 month level of family functioning was not. None of the mediating effects were statistically significant.
Table 3.
Relationship Between Variables in the Mediation Model
| Family Functioning Trajectory B (SE) | Family Functioning at 12 months B (SE) | Externalizing B (SE) | Lifetime Arrests B (SE) | Last Year Arrests B (SE) | Lifetime Incarcerations B (SE) | Last Year Incarcerations B (SE) | |
|---|---|---|---|---|---|---|---|
| Intervention Condition | 0.25 (0.13) p = .05 | 0.20 (0.10) p = .06 | 2.13 (1.64) p = .20 | 5.39 (3.80) p = .16 | 5.00 (3.73) p = .18 | 7.14 (4.96) p = .15 | 5.92 (4.29) p = .17 |
| Family Functioning Trajectory | X | X | −12.47 (4.04) p < .01 | −28.5 (9.60) p < .01 | −27.43 (10.33) p < .01 | −37.40, (12.40) p < .01 | −31.00 (11.23) p < .01 |
| Family Functioning at 12 months | X | X | −0.39 (0.13) p < .001 | −0.28 (0.12) p < .01 | −0.32 (0.12) p < .01 | −0.33 (0.14) p = .02 | −0.20 (0.18) p = .25 |
|
Tests of
Mediation | |||||||
| Intervention → Family Functioning Trajectory → Externalizing | a*b2 = −3.10 | SE = 1.80 | p = .09 | ||||
| Intervention → Family Functioning at 12 Months → Externalizing | a*b2 = −0.96 | SE = 0.06 | p = .11 | ||||
| Intervention → Family Functioning Trajectory → Lifetime Arrests | a*b3 = −7.10 | SE = 4.20 | p = .10 | ||||
| Intervention → Family Functioning at 12 Months → Last Year Arrests | a*b3 = −0.07 | SE = 0.05 | p = .14 | ||||
| Intervention → Family Functioning Trajectory → Lifetime Incarcerations | a*b4 = −9.30 | SE = 5.50 | p = .09 | ||||
| Intervention → Family Functioning at 12 Months → Last Year Incarcerations | a*b4 = −0.08 | SE = 0.05 | p = .13 | ||||
Post-Hoc Analyses
Post-hoc analyses suggested there were no significant moderations of the effect of BSFT by race/ethnicity on drug use outcomes (X2(3) = 2.80, p = .42), externalizing outcomes (X2(3) = 1.23, p = .75), lifetime (X2(3) = 0.15, p = .99) or past year arrests(X2(3) = 1.13, p = .60), or lifetime (X2(3) = 3.12, p = .37) or past year incarcerations (X2(3) = 0.09, p = .96).
4. Discussion
The purpose of this study was to evaluate drug use, externalizing behavior and criminal outcomes on young adults that had been randomized to BSFT or TAU as part of the BSFT effectiveness study. Encouragingly, retention in treatment (attending 8+ sessions) during the original study was associated with lower levels of drug use across treatment conditions in the long term follow- up. However, remarkably, 76 % of the young adults were using drugs in the 90 days that preceded the follow up assessment. The estimated mean of drug use days at the long term follow up was higher than at baseline (12.1 vs 2.5 for BSFT, and 13.8vs 2.7 for TAU). In spite of this, only 5% were receiving treatment. Research has shown that adolescents and young adults may relapse into drug use or continue to use as a result of a constellation of personal and treatment factors.32 Continued care has consistently shown to reduce relapse and enhance the maintenance of treatment gains.
In the BSFT effectiveness study, 12 month follow-up results revealed a significantly higher median level of drug use days in TAU than in BSFT. In this present study, there were no differences in median drug use days between conditions. It is possible that differences that were not observed between conditions were present at some time between the effectiveness study and the present study. Also, the fact that differences observed at the last time point of the original study were not sustained could suggest the need for booster sessions to maintain the effect of the BSFT intervention.
In this long term follow-up, differences emerged in arrests, incarceration and externalizing behaviors. Participants randomized to BSFT had significantly fewer externalizing behaviors at the cross sectional assessment than TAU participants. BSFT also had lower incidence rates of both lifetime and last year arrests and incarcerations when compared to TAU. Improvements in family functioning during the main study did not mediate the effects of BSFT in the long term follow up. It is possible that the ability to detect a finding was hindered by the smaller sample size and therefore insufficient power to detect mediating effects. Nonetheless, it is noteworthy that the rate of change in family functioning and family functioning at 12 months post randomization in BSFT during the effectiveness study was significantly related to externalizing behaviors, arrests and incarceration at the long term follow up.
A key predictor of the trajectories of adolescent to young adult substance use and criminal behavior is family functioning, as manifested in parental monitoring, family bonding and family support. Adolescent externalizing behavior is also a predictor of both substance use and behavioral problems in young adulthood.29 Treatments that target adolescent substance use and behavior problems, particularly at the family level, may prove especially effective at reducing later trouble with the law and can have salubrious consequences for both youth and society. BSFT and other family-based adolescent treatments, found to be less expensive that juvenile justice interventions,33 may be construed as cost-beneficial interventions that prevent further penetrance in the justice system. In this study, retention in adolescent substance abuse treatment (both in BSFT and in TAU) was associated with lower rates of drug use, arrests and incarcerations in the last year.
Perhaps the most severe limitation of the study is that of the original sample of 480 participants, only 378 agreed to be re-contacted for later studies. Of these, we were only able to reach and assess 261. Nevertheless, a comparison between the original sample and those who agreed to participate did not show any significant differences at baseline in any of the variables examined. Similarly, there were no significant differences between those who agreed to participate and those who participated in the final assessment. A second limitation is that there was variability in length of time between participation in the study and the long term assessment time point. The average number of years between randomization in the original study and the final follow up was 4.7 years, but there were no differences in length of time from randomization between conditions. Third, relying on self-reports may have resulted in underreporting when assessing substance use and criminal history. Finally, it is not possible in a long term follow up such as this one to rule out factors other than intervention condition that could have affected its outcomes therefore, no direct causal influences could be concluded.
Future Directions
One way future studies can overcome the sample limitations of this study in evaluating justice system involvement is by using public records of justice involvement. Official records could also facilitate longer time follow-ups and provide more regular time-point assessments. Longitudinal approaches are needed to understand the trajectories of adolescent substance users as they become adults. Findings from the original study pointed to the importance of implementation strategies that appear critical for the model to succeed. Future implementation studies should evaluate the impact of BSFT implementation strategies34 on short term and long term outcomes for adolescents and young adults.
Conclusion and Implications
Overall, this study found that while there were no differences in drug use by treatment type (BSFT vs TAU) at a long-term follow-up, there were significant differences in the rates of arrests, incarcerations, and externalizing behaviors favoring those who received BSFT. These effects could be explained by the improvements in family functioning that occurred during the effectiveness study. Additional research is needed to help identify how treatments like BSFT can be better implemented to maximize beneficial outcomes.
5. Acknowledgements
This work was supported by NIDA grant U10 DA 13720, José Szapocznik, Principal Investigator, and NIDA grant RC2 DA028864-02 José Szapocznik and Michael Robbins Principal Investigators. This study is registered in Clinical Trials.gov, registration number . The sponsor had no role in the design, collection, analyses, interpretation of the data, in the writing of the report and in the decision to submit the article for publication.
Footnotes
Declaration of Interest
The authors alone are responsible for the content and writing of this paper. Author Jose Szapocznik is the developer of the BSFT model and has copyrighted the intervention. He is also the director for the BSFT training institute. The sponsor that supported this work is not affiliated with the model.
References
- 1.Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE Monitoring the Future national survey results on drug use, 1975–2013: 2014 Volume II, College students and adults ages 19–50. Ann Arbor: Institute for Social Research, The University of Michigan; 2014. [Google Scholar]
- 2.Brook DW, Brook JS, Rubenstone E, Zhang C, & Saar NS Developmental associations between externalizing behaviors, peer delinquency, drug use, perceived neighborhood crime, and violent behavior in urban communities. Aggress Behav, 2011;37(4):349–361. doi: 10.1002/ab.20397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horigian VE, & Szapocznik J Brief Strategic Family Therapy: Thirty-five years of interplay among theory, research and practice in adolescent behavior problems and drug abuse In: Scheier LM ed. APA Handbook of Drug Prevention. Washington, DC, US: American Psychological Association; 2015:249–265 [Google Scholar]
- 4.Young SE, Stallings MC, Corley RP, Krauter KS, & Hewitt JK Genetic and environmental influences on behavioral disinhibition. Am J Med Genet, 2000;96(5):684–695. doi: [DOI] [PubMed] [Google Scholar]
- 5.Schulden JD, Thomas YF, & Compton WM Substance abuse in the United States: Findings from recent epidemiologic studies. Curr Psychiatry Rep, 2009;11(5):353–359. doi: 10.1007/s11920-009-0053-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hogue A, Henderson CE, Ozechowski TJ, & Robbins MS Evidence base on outpatient behavioral treatments for adolescent substance use: updates and recommendations 2007–2013. J Clin Child Adolesc Psychol, 2014;43(5):695–720. doi: 10.1080/15374416.2014.915550 [DOI] [PubMed] [Google Scholar]
- 7.Tanner-Smith EE, Wilson SJ, & Lipsey MW The comparative effectiveness of outpatient treatment for adolescent substance abuse: A meta-analysis. J Subst Abuse Treat, 2013;44,145–158. doi: 10.1016/j.jsat.2012.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waldron HB, & Turner CW Evidence-based psychosocial treatments for adolescent substance abuse. J Clin Child Adolesc Psychol, American Psychological Association, Division, 2008;37(1):238–261. doi: 10.1080/15374410701820133 [DOI] [PubMed] [Google Scholar]
- 9.Henggeler SW, & Sheidow AJ Empirically supported family-based treatments for conduct disorder and delinquency in adolescents. J Marital Fam Ther, 2012;38(1):30–58. doi: 10.1111/j.1752-0606.2011.00244.x; 10.1111/j.1752–0606.2011.00244.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henggeler SW, Clingempeel WG, Brondino MJ, & Pickrel SG Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. J Am Acad Child Adolesc Psychiatry, 2002;41(7):868–874. doi: 10.1097/00004583-200207000-00021 [DOI] [PubMed] [Google Scholar]
- 11.Schaeffer CM, & Borduin CM Long-term follow-up to a randomized clinical trial of multisystemic therapy with serious and violent juvenile offenders. J Consult Clin Psychol, 2005;73(3):445–453. doi: 10.1037/0022-006X.73.3.445 [DOI] [PubMed] [Google Scholar]
- 12.Sawyer AM & Borduin CM Effects of multisystemic therapy through midlife: A 21.9-year follow-up to a randomized clinical trial with serious and violent juvenile offenders. J Consult Clin Psychol, 2011;79(5):643–652. doi: 10.1037/a0024862. [DOI] [PubMed] [Google Scholar]
- 13.Szapocznik J, Hervis OE, & Schwartz S Brief strategic family therapy for adolescent drug abuse, 2003; (NIH publication no. 03–4751). (NIDA Therapy Manuals for Drug Addiction ed.). Rockville, MD: National Institute on Drug Abuse. [Google Scholar]
- 14.Szapocznik J, & Kurtines W Breakthroughs in family therapy with drug abusing and problem youth. New York, NY: Springer; 1989. [Google Scholar]
- 15.Szapocznik J, Santisteban D, Rio A, Perez-Vidal A, Santisteban D, & Kurtines WM Family effectiveness training: An intervention to prevent drug abuse and problem behaviors in Hispanic adolescents. Hispanic Journal of Behavioral Sciences, 1989; 11(1):4–27. doi: 10.1177/07399863890111002 [DOI] [Google Scholar]
- 16.Santisteban DA, Coatsworth JD, Perez-Vidal A et al. Efficacy of brief strategic family therapy in modifying Hispanic adolescent behavior problems and substance use. J Fam Psychol, 2003; 17(1):121–33. 10.1037/0893-3200.17.1.121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Szapocznik J, Kurtines WM, Foote FH, Perez-Vidal A, & Hervis O Conjoint versus one-person family therapy: Further evidence for the effectiveness of conducting family therapy through one person with drug-abusing adolescents. J Consult Clin Psychol, 1986;54(3):395–397. doi: 10.1037/0022-006X.54.3.395 [DOI] [PubMed] [Google Scholar]
- 18.Szapocznik J, Perez-Vidal A, Brickman AL et al. Engaging adolescent drug abusers and their families in treatment: A strategic structural systems approach. J Consult Clin Psychol, 1988;56(4):552–557. 10.1037/0022-006X.56.4.552 [DOI] [PubMed] [Google Scholar]
- 19.Winters KC, Tanner-Smith EE, Bresani E, & Myers K Current advances in the treatment of adolescent drug use. Adolescent Health, Medicine and Therapeutics, 2014;20(5):199–210. doi: 10.2147/AHMT.S48053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robbins MS, Feaster DJ, Horigian VE et al. Brief strategic family therapy versus treatment as usual: Results of a multisite randomized trial for substance using adolescents. J Consult Clin Psychol, 2011;79(6):713–727. doi: 10.1037/a0025477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Robbins MS, Szapocznik J, Horigian VE et al. Brief strategic family therapy for adolescent drug abusers: A multi-site effectiveness study. Contemp Clin Trials, 2009;30(3):269–278. doi: 10.1016/j.cct.2009.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sobell LC, & Sobell MB Timeline follow-back: a technique for assessing self-reported alcohol consumption In: Litten RZ & Allen JP, eds. Measuring Alcohol Consumption Totowa, NJ: Humana Press; 1992:41–72. [Google Scholar]
- 23.Carey KB Reliability and validity of the time-line follow-back interview among psychiatric outpatients: A preliminary report. Psychol Addict Behav, 1997;11:26–33. doi: 10.1037/0893-164X.11.1.26 [DOI] [Google Scholar]
- 24.Achenbach TM, & Rescorla LA Manual for the ASEBA Adult Forms & Profiles, Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2003. [Google Scholar]
- 25.Feaster DJ, Robbins MS, Henderson C et al. Equivalence of family functioning and externalizing behaviors in adolescent substance users of different race/ethnicity. Journal J Subst Abuse Treat, 2010;38(Suppl. 1):S113–S124. doi: 10.1016/j.jsat.2010.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hawkins JD, Catalano RF, & Miller JY Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull, 1992;112(1):64–105 doi: 10.1037/0033-2909.112.1.64 [DOI] [PubMed] [Google Scholar]
- 27.Hemovich V, Lac A, & Crano WD Understanding early-onset drug and alcohol outcomes among youth: the role of family structure, social factors, and interpersonal perceptions of use. Psychol Health Med, 2011;16(3):249–267 doi: 10.1080/13548506.2010.532560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kodjo CM, & Klein JD Prevention and risk of adolescent substance abuse – the role of adolescents, families and communities. Pediatr Clin North Am, 2002;49(2):257–268. doi: 10.1016/S0031-3955(01)00003-7 [DOI] [PubMed] [Google Scholar]
- 29.Stone AL, Becker LG, Huber AM, & Catalano RF Review of risk and protective factors of substance use and problem use in emerging adulthood. Addict Behav, 2012;37(7),747–775. doi: 10.1016/j.addbeh.2012.02.014 [DOI] [PubMed] [Google Scholar]
- 30.Robbins MS, Feaster DJ, Horigian VE, Puccinelli M, Henderson C, & Szapocznik J Therapist adherence in brief strategic family therapy for adolescent drug abusers. J Consult Clin Psychol, 2011;79(6):43–53. doi: 10.1037/a0022146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen J Statistical Power Analysis for the Behavioral Sciences, 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 32.Winters KC, Botzet AM, & Fahnhorst T Advances in adolescent substance abuse treatment. Curr Psychiatry Rep, 2011;13(5):416–421. doi: 10.1007/s11920-011-0214-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Evidence Based Associates. Redirection Quarterly Update Report. Oviedo, FL: Evidence Based Associates; 2012. http://www.evidencebasedassociates.com/featured_projects/redirectionQ3_12.pdf. Accessed December 2012. [Google Scholar]
- 34.Szapocznik J, Schwartz S, Muir J, & Brown CH Brief Strategic Family Therapy: An intervention to reduce adolescent risk behavior. Couple Family Psychology, 2012;1(2):134–145. doi: 10.1037/a0029002 [DOI] [PMC free article] [PubMed] [Google Scholar]