ABSTRACT
Worldwide, the burden of morbidity and mortality from diet-related chronic diseases is increasing, driven by poor diet quality and overconsumption of calories. At the same time, the global food production system is draining our planet's resources, jeopardizing the environment and future food security. Personal, population, and planetary health are closely intertwined and will all continue to be vulnerable to these threats unless action is taken. Fortunately, shifting current global dietary patterns towards high-quality, plant-based diets could alleviate these health and environmental burdens. Compared with typical Western diets with high amounts of animal products, healthy plant-based diets are not only more sustainable, but have also been associated with lower risk of chronic diseases such as obesity, type 2 diabetes, cardiovascular disease, and some cancers. For personalized disease management and prevention, precision nutrition has the potential to offer more effective approaches tailored to individual characteristics such as the genome, metabolome, and microbiome. However, this area of research is in the early stages and is not yet ready for widespread clinical use. Therefore, it must not overshadow public health nutrition strategies, which have the power to improve health and sustainability on a larger scale. If widely implemented, interventions and policy changes that shift the globe towards healthy plant-based dietary patterns could be instrumental in ensuring future personal, population, and planetary health.
Keywords: plant-based diets, obesity, cardiovascular disease, type 2 diabetes, precision nutrition, public health nutrition, sustainable nutrition
Introduction
Diet-related chronic diseases such as obesity, type 2 diabetes (T2D), and cardiovascular disease (CVD) are serious public health threats. Worldwide, obesity rates have tripled since 1975 (1), driven by widespread diet and lifestyle changes which result in a positive energy balance (2). In 2016, 13% of the global adult population were obese and 39% were overweight (1). Obesity is a risk factor for numerous health problems including CVD, T2D, and some cancers (1). CVD, the leading cause of mortality worldwide, is responsible for 31% of all deaths (3). Diabetes is another major cause of death, directly responsible for 1.6 million deaths globally in 2015 (4). From 1980 to 2014, the overall global prevalence of diabetes rose from 4.7% to 8.5%, but has been rising more rapidly in low- and middle-income countries (4). In the United States, CVD and diabetes are both ranked in the top 10 causes of death. Of all the risk factors associated with the major causes of death in the United States, unhealthy diets are ranked as the most significant risk (5).
Diet-related chronic diseases are largely preventable through healthy diet and lifestyle. However, much of the world lives in obesogenic environments that promote unhealthy behaviors, causing weight gain and chronic diseases (2). For example, in the United States, processed, energy-dense foods are abundant, cheap, and convenient whereas unprocessed, healthier foods are often more expensive and less accessible in many areas (6). The food environment has the potential to affect dietary behaviors; one study found that adults living in neighborhoods with many fast-food restaurants were nearly twice as likely to be obese as adults living in areas with lower numbers of fast-food restaurants (6). This abundance of fast food is not only present in higher-income countries, but has spread globally; there are already 2500 branches of McDonald's in China, and the company plans to increase this to 4500 by 2022 (7). In conjunction with economic growth and urbanization, nearly all areas of the world have experienced an increased availability of low-cost food and beverages that are energy dense and nutritionally poor, which has led to negative dietary changes (2). Many low- and middle-income countries have experienced population-wide increases in consumption of animal products, refined grains, and added sugar, as well as a reduction in physical activity due to more mechanized lifestyles (2). Since 1963, global meat consumption has risen by 62%, driven by population growth and increasing wealth in developing countries (8). In addition to health implications, worldwide dietary changes also have environmental consequences. Animal food production is more environmentally damaging and resource intensive than plant food production. On average, producing animal protein (meat and dairy) requires 11 times more fossil fuel energy than grain-based protein. Red meat production is especially inefficient; the estimated ratio of kcal of energy expended to kcal of protein generated is 57:1 for lamb and 40:1 for beef (9). With increasing demand for animal products, especially meat, modern food-production systems have become unsustainable. Without drastic changes, these systems will not be able to support future populations, especially as climate change and population growth further threaten our environment and food supply (8). Large-scale interventions are necessary to change the food environment so that it is easy for the general population to make diet and lifestyle choices that are both healthy and sustainable. Encouraging populations to move towards healthy plant-based diets could be a potential target for interventions to prevent and manage diet-related chronic diseases and ensure future food security.
Plant-Based Diets for Chronic Disease Prevention
The term “plant-based diets” encompasses a wide range of dietary patterns that contain lower amounts of animal products and higher amounts of plant products such as vegetables, fruits, whole grains, legumes, nuts, and seeds (10). When making dietary recommendations, it is important to emphasize overall dietary patterns, rather than specific foods and nutrients, in order to account for the synergistic effects of the total diet on health (11). However, there is strong evidence and biological plausibility to support the roles of specific plant-based foods in preventing cardiometabolic diseases and premature mortality. Fruits and vegetables are rich sources of fiber, antioxidants, and various nutrients, and have been inversely associated with risk of chronic diseases and mortality. A meta-analysis of 95 cohort studies found that a 200-g/d increase in fruit and vegetable consumption was associated with a 16% lower risk of stroke, 8% lower risk of CVD, 3% lower risk of total cancer, and 10% lower risk of all-cause mortality (12). Whole grains also provide dietary fiber and contain numerous beneficial bioactive compounds (13). One meta-analysis found a strong dose-response relationship between whole-grain consumption and reduced total and cause-specific mortality. Consuming at least 70 g/d of whole grains was associated with a 22% lower risk of total mortality, 23% lower risk of CVD mortality, and 20% lower risk of cancer mortality, compared with consuming little or no whole grains (13). Nuts may also be useful for disease prevention due to their high content of unsaturated fat, fiber, protein, and minerals (14). Evidence from meta-analyses supports inverse associations between nut intake and ischemic heart disease, diabetes, overall CVD, and mortality from all causes (14, 15). Legumes may reduce the risk of chronic disease due to their high fiber, micronutrient, and protein content (15). One meta-analysis found that legume intake was associated with lower risk of ischemic heart disease (15). Another meta-analysis of 11 clinical trials found that without changing body weight, non-soy legume consumption lowered total cholesterol, LDL cholesterol, and triglycerides (16). Coffee and tea, which contain antioxidants and numerous other bioactive substances, can also contribute to a healthy plant-based diet (17). In healthy adults, consistent evidence shows that moderate coffee intake (3–5 cups/d or up to 400 mg caffeine/d) does not increase the risk of chronic diseases or mortality (11). In fact, coffee intake has been associated with lower risks of various neurologic diseases, liver diseases, T2D, CVD, some cancers, and mortality (17). Consuming 3 cups of tea per day has also been associated with lower chronic disease and mortality risk (18).
In addition to specific plant-based foods, overall plant-based dietary patterns have been associated with lower risk of chronic diseases such as T2D and CVD. Evidence from randomized controlled trials indicates that compared to nonvegetarian diets, vegetarian diets can lower CVD risk factors such as total cholesterol and blood pressure, enhance weight loss, and improve glycemic control (10). However, plant-based diets do not need to be vegetarian. A variety of different plant-based diets may reduce chronic disease risk, many of which include meat in moderate amounts. Martínez-González et al. (19) created a provegetarian score based on repeated dietary measures in omnivorous Spanish adults at high CVD risk, with animal foods weighted negatively and plant foods weighted positively. Participants with higher scores had lower risk of mortality from all causes, as well as lower risk of mortality from CVD. Compared to individuals with very low scores, those with low (HR: 0.76; 95% CI: 0.53, 1.10), moderate (HR: 0.79; 95% CI: 0.55, 1.13), and high provegetarian scores (HR: 0.59; 95% CI: 0.39, 0.89; P-trend < 0.05) had a lower risk of mortality over a median of 5 y of follow-up (19), illustrating that health benefits from plant-based diets can still be achieved even with inclusion of animal products.
When considering overall plant-based dietary patterns, it is crucial to examine the types of foods included because not all plant-based diets are healthy. Among >200,000 female and male health professionals, an overall plant-based diet index (created by positively scoring plant foods and negatively scoring animal foods) was associated with lower risk of coronary heart disease (HR comparing extreme deciles: 0.92; 95% CI: 0.83, 1.01; HR per 10-unit increase: 0.93; 95% CI: 0.90, 0.97; P-trend < 0.05) (20). However, the association changed significantly when the index was broken down into a healthy plant-based diet (emphasizing foods such as whole grains, fruits, vegetables, nuts, legumes, oils, tea, and coffee) and an unhealthy plant-based diet including higher amounts of juices/sweetened beverages, refined grains, potatoes/fries, and sweets. For participants with higher healthy plant-based diet scores, coronary heart disease risk was significantly reduced (HR comparing extreme deciles: 0.75; 95% CI: 0.68, 0.83; HR per 10-unit increase: 0.88; 95% CI: 0.85, 0.91; P-trend < 0.001). For those with higher unhealthy plant-based diet scores, the association with coronary heart disease risk became positive (HR comparing extreme deciles: 1.32; 95% CI: 1.20, 1.46; HR per 10-unit increase: 1.10; 95% CI: 1.06, 1.14; P-trend < 0.001) (20). In a similar analysis, the overall plant-based diet score was associated with a moderately lower risk of T2D (HR comparing extreme deciles: 0.80; 95% CI: 0.74, 0.87; HR per 10-unit increase: 0.88; 95% CI: 0.86, 0.91; P-trend < 0.001), whereas the healthy plant-based diet score was more strongly associated with reduced T2D risk (HR comparing extreme deciles: 0.66; 95% CI: 0.61, 0.72; HR per 10-unit increase: 0.83; 95% CI: 0.80, 0.85; P-trend < 0.001) and the unhealthy plant-based diet score was associated with an increased T2D risk (HR comparing extreme deciles: 1.16; 95% CI: 1.08, 1.25; P-trend < 0.001) (21).
Relationship between Types of Dietary Fats and Health Outcomes
There is strong evidence that intakes of saturated fat (found mostly in animal-based foods) and unsaturated fat (found predominantly in plant-based foods) have divergent effects on health outcomes. In a study of 126,000 health professionals, PUFA and MUFA intake were associated with lower mortality risk (HRs comparing extreme quintiles: 0.81; 95% CI: 0.78, 0.84 for PUFA; 0.89; 95% CI: 0.84, 0.94 for MUFA; P-trend < 0.001 for both) (Figure 1) (22). Trans fat intake was positively associated with mortality risk, (HR: 1.13; 95% CI: 1.07, 1.18) as was saturated fat intake (HR: 1.08; 95% CI: 1.03, 1.14; P-trend < 0.001 for both). However, when interpreting these associations, it is necessary to consider substitution effects. In the above study, replacing 5% of energy from saturated fat with the same amount of energy from MUFAs and PUFAs was associated with a 27% and 15% reduced risk of mortality, respectively (22). In another study (23), exchanging 5% of calories from saturated fat with PUFA, MUFA, or whole grains was associated with a 25%, 15%, and 9% lower risk of coronary heart disease, respectively. However, replacing saturated fat with carbohydrates from refined starches and added sugars did not change coronary heart disease risk. The source of fat (plant or animal) may also affect health outcomes, even when considering the same type of fat. A recent study suggested that replacing 5% of energy intake from saturated fat, trans fat, and refined carbohydrates with MUFA intake from plant sources was associated with lower risk of coronary heart disease, whereas the same substitution with MUFA from animal sources was not beneficial (24).
FIGURE 1.
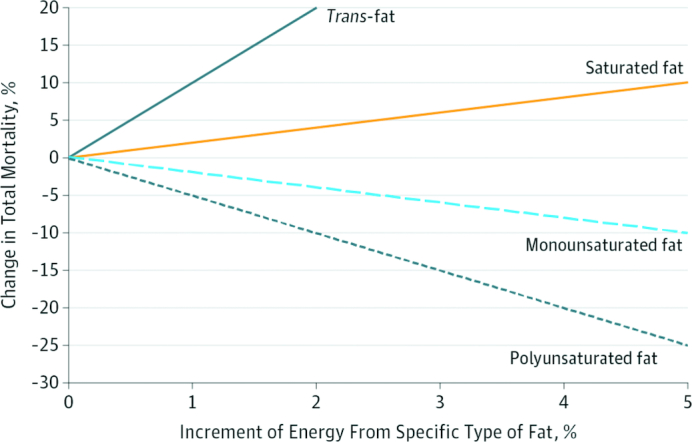
Change in total mortality risk associated with increments of calorie intake from specific types of fat in the Nurses’ Health Study and Health Professionals Follow-Up Study. Multivariable HRs are shown for total mortality associated with replacing the percentage of energy from total carbohydrates with the same energy from specific types of fat (P-trend < 0.001 for all), adjusted for age, race, marital status, BMI, physical activity, smoking status, alcohol consumption, multivitamin use, vitamin E supplement use, current aspirin use, family history of myocardial infarction, family history of diabetes, family history of cancer, history of hypertension, history of hypercholesterolemia, intakes of total energy and dietary cholesterol, percentage of energy intake from dietary protein, menopausal status and hormone use in women, and percentage of energy from the remaining specific types of fat. Reproduced with permission from reference 22.
Types of Protein, Red Meat Consumption and Health Outcomes
In addition to type of fat, there is evidence that type of protein consumed is important for health. Among US health professionals with at least 1 unhealthy risk factor (smoking, alcohol intake, overweight or obesity, or physical inactivity), animal protein intake was linked to a higher risk of death from CVD, whereas plant protein consumption was associated with a lower risk of death from all causes (25). In the same study, replacing 3% of animal protein sources with plant protein sources was associated with significantly lower risks of all-cause mortality for processed red meat (HR: 0.66; 95% CI: 0.59, 0.75), unprocessed red meat (HR: 0.88; 95% CI: 0.84, 0.92), and egg (HR: 0.81; 95% CI: 0.75, 0.88) (25).
Of all the animal-based foods, red meat appears to be especially detrimental to health, and has been linked to premature mortality and T2D. Among men in the Health Professionals Follow-Up Study (followed for ≤22 y) and women in the Nurses’ Health Study (followed for ≤28 y), an increase in 1 serving of processed and unprocessed red meat per day was linked to a 13% and 20% increased risk of mortality, respectively (26). Replacing 1 serving of red meat per day with other foods such as fish, poultry, legumes, nuts, low-fat dairy, or whole grains was associated with a 7–19% lower risk of premature death. The authors estimated that if all study participants had consumed less than a half serving of red meat (42 g) per day, 9.3% of deaths in men and 7.6% in women could have been prevented (26). Pan et al. (27) found that processed, unprocessed, and total red meat intakes were associated with a 12%, 32%, and 14% increased T2D risk, respectively, in the Nurses’ Health Study and Health Professionals Follow Up Study cohorts and confirmed these results with a meta-analysis of 442,000 individuals. In the cohorts, replacing 1 serving of red meat per day with nuts, low-fat dairy, or whole grains was associated with a 16–35% lower T2D risk (27). An additional analysis in these cohorts found that individuals who increased their red meat consumption by more than a half serving per day over 4 y had a 30% increased risk of developing T2D in the next 4 y, even after adjusting for BMI and concurrent weight gain (28).
The cooking methods used for red meat also appear to influence health. Liu et al. (29) found that independent of total red meat consumption, a higher frequency of open-flame and higher-temperature cooking methods was significantly associated with T2D risk. Those who broiled or barbecued red meat ≥2 times/wk had an increased T2D risk (HR for broiling: 1.29; 95% CI: 1.19, 1.40, P-trend < 0.001; HR for barbecuing: 1.23; 95% CI: 1.11, 1.38; P-trend < 0.001), compared with those who used these cooking methods <1 time/mo. Red meat broiling and barbecuing were also associated with a significantly greater risk of obesity and weight gain. Another analysis found a similar association between T2D risk and high-temperature and open-flame cooking of chicken, further indicating that meat cooking methods may play a role in the development of T2D (30).
Precision Nutrition for Personal Health
Evidence-based dietary recommendations are often created based on population averages, which is effective for promoting health in populations, but may not be optimal for specific individuals (31). Precision nutrition is an emerging field that aims to use individualized information, such as data from the genome, microbiome, and metabolome, to prescribe personalized diets and lifestyles for chronic disease prevention and management (Figure 2) (32).
FIGURE 2.
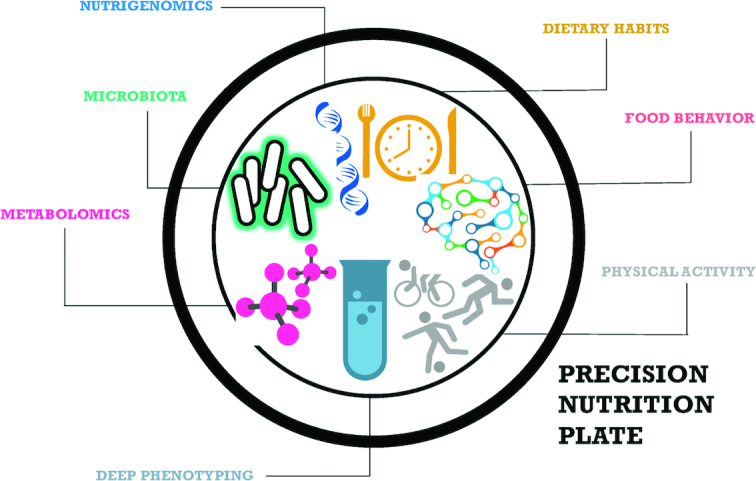
The precision nutrition plate: types of individual data that are important to consider in precision nutrition research. Reproduced with permission from reference 32.
Nutrigenomics studies are advancing the field of precision nutrition by discovering how genetic differences affect dietary intakes and chronic disease risk (31). Genome-wide association studies have identified genetic variants that are associated with different dietary factors such as consumption of specific macronutrients (33). Studies have also identified numerous genetic variants associated with obesity and coronary heart disease. There is increasing evidence that healthy diets may be able to mitigate the adverse effects of these variants (31). However, for obesity, unhealthy diets have been found to increase the genetic effects (31). Additional evidence suggests that healthy diets such as the Mediterranean and prudent dietary patterns may have an effect on gene expression (34, 35). However, due to the small sample sizes of these studies and high potential for confounding by other lifestyle factors, further research is needed to confirm these results.
Metabolomics is another important precision nutrition tool and can help to identify biomarkers or metabolic signatures of chronic diseases or dietary intakes. A recent meta-analysis reported significant positive associations between T2D and plasma concentrations of tyrosine, phenylalanine, and branched-chain amino acids (leucine, isoleucine, and valine) and inverse associations with glycine and glutamine (36). These findings offer the potential to use dietary modifications to target these metabolites to prevent or treat T2D (31). Many recent studies have also focused on discovering metabolomic signatures of specific foods and dietary patterns to provide more accurate assessment of dietary intake in free-living populations. For example, plasma and urinary anserine has been associated with chicken consumption, and urinary trimethylamine-N-oxide and carnitines have been associated with red meat and fish intake (31). However, metabolomics is not yet able to accurately distinguish between most dietary patterns and specific foods. Therefore, it can be used in conjunction with existing dietary assessment methods to measure dietary intake and assess compliance to dietary interventions, but should not replace the established dietary assessment methods (31).
Microbiome research is another rapidly developing area of precision nutrition. Gut microbiota composition varies significantly between individuals, and likely plays a role in the development of chronic diseases (31). Ley et al. (37) observed that obese participants had less Bacteroidetes and more Firmicutes bacteria compared with lean controls, but their proportion of Bacteroidetes compared with Firmicutes bacteria increased with weight loss. Studies have also observed that gut microbiota composition can be influenced by short-term dietary changes and long-term usual diets (31). Characteristics of a long-term Western-style dietary pattern, including high energy intake and snacking, as well as sugar-sweetened beverage (SSB) and whole-milk consumption, have been associated with lower microbiota diversity. Other dietary factors, such as habitual consumption of coffee and tea, have been associated with higher diversity (31). There is evidence that plant-based foods may favorably alter gut microbiota as they are high in dietary fiber, prebiotics, fermentable carbohydrates, and polyphenols, which fuel gut microbiota activity (38). However, microbiome research is still in the early stages and future large prospective studies are necessary to uncover the complex relationships between diet, the microbiome, and disease.
A study by Zeevi et al. (39) highlights the value of precision nutrition and potential impact of personalized diets. The authors integrated microbiome, physical activity, sleep, anthropometric, dietary, and biochemical parameter data from 800 participants to create a machine learning algorithm that could prescribe personalized diets. When given as an intervention, the personalized diets were more effective at reducing individual postprandial glucose than traditional dietary advice provided by a dietitian. Although this study illustrates the potential benefits of precision nutrition, the findings are preliminary, and more research is needed to evaluate the compliance with and effects of the personalized diets long term. It is also currently unclear if these results could be generalized to other populations and health outcomes. Even so, it would be enormously expensive to use this method in a clinical setting due to the large amount of data collection and analysis required.
With the continuing advances in omics technologies and big data analytics, the field of precision nutrition is developing rapidly. Although precision nutrition will likely become important for improving personal health in the future, currently there is insufficient evidence to support its widespread use in clinical settings (31). To improve human health, population-wide approaches remain fundamental. Therefore, it is crucial to avoid the hype surrounding precision nutrition and ensure that the available resources are balanced between investing in precision nutrition research and public health strategies (31).
Public Health Nutrition Strategies for Population Health
Public health nutrition strategies aim to improve health in populations. These approaches often include education, policies, or interventions, all of which could be utilized to promote healthy plant-based diets. Policies, when based on consistent scientific evidence, can be especially effective because they have the power to shape food environments and encourage the general population to make healthy choices. For example, many countries across the globe have enacted policies to limit trans fats in food products based on extensive evidence linking them to CVD (40, 41). Denmark was the first country in the world to regulate trans fats, nearly eliminating them from the Danish food supply (42). In the 3 y after the regulation was implemented, CVD mortality decreased in the Danish population by 14.2 deaths per 100,000, compared with similar countries without trans fat policies (42). Between 2007 and 2011, New York State restricted trans fat in 11 counties in all public eateries such as restaurants, vending machines and concessions. Three years after implementation, compared with the nonrestricted counties, the counties with the restriction had an additional 6.2% decline in hospital admissions for myocardial infarction and stroke events, beyond temporal trends (43). In 2006, the FDA mandated trans fat labeling on all food products, which resulted in many companies reformulating products to reduce trans fat content (41). By June 2018, partially hydrogenated oils, the primary source of artificial dietary trans fats, were banned from the US food supply, marking an important step in creating a healthy food environment (41).
SSB taxes are another case in which scientific evidence has successfully informed nutrition policy. There is strong evidence that regular consumption of SSBs increases risk of obesity, T2D, and other chronic diseases (44–46). In 2014, Mexico implemented an SSB tax, which was followed by a 7.6% sales reduction in taxed beverages and 2.1% increase in untaxed beverages over the next 2 y (47). In the United States, several cities including Seattle, Oakland, Berkeley, San Francisco, Boulder, and Philadelphia have implemented similar taxes (48). In Berkeley, there was a 9.6% reduction in SSB sales 1 y after implementation of a 1 cent per ounce tax (49). If expanded throughout the entire United States, it was estimated that in the second year of implementation, the tax could reduce mean BMI by an average of 0.08 kg/m2 (95% CI: 0.03, 0.20 kg/m2) among adults and 0.16 kg/m2 (95% CI: 0.06, 0.37 kg/m2) among youth, resulting in a 0.99% and 1.38% decrease in obesity prevalence among adults and children, respectively (50). The tax could also save an estimated US$23.6 billion in healthcare costs for the period 2015–2025 (50).
Other nations and cities have utilized public institutions, such as schools or government-owned buildings, to improve nutrition by setting mandatory standards or encouraging provision of healthy foods (51). Through an SSB ban, Boston was able to nearly eliminate sales of SSBs in public schools, which was followed by a significant decline in SSB consumption among Boston high school students (52). The USDA Fresh Fruit and Vegetable Program (FFVP), which provides funding to qualifying schools to distribute free fruits and vegetables to students, has also seen promising results. An evaluation of the program found that students in FFVP schools consumed approximately one-third of a cup more fresh fruit and vegetables than students in comparable schools not participating in the program (53). Although there is evidence that policies such as taxes, bans, or school programs may be able to change purchasing and consumption behavior, additional studies are needed to evaluate the impact of these policies on health outcomes and provide support for future legislation.
In addition to the approaches used for trans fats and SSBs, numerous other public health strategies have the capability to encourage healthy and sustainable lifestyle choices and improve the obesogenic environment. Evidence supports the efficacy of a variety of approaches aimed at influencing behavior, such as well-designed media and education campaigns (54). Economic incentives have also been successful, including subsidies to increase the availability and affordability of healthy food, and taxes to increase prices of less healthy foods and beverages (54). Nutrition labeling on food products and menus not only provides information for individuals to make healthy choices, but in some cases has also led the food industry to reformulate products to reduce unhealthy ingredients such as sodium, added sugar, and trans fat (54). Increasing availability of supermarkets and enacting restrictions on marketing unhealthy foods to children can also help to improve food environments and diets (54). Additional opportunities to improve both public health and sustainability exist at the level of the food supply chain. A few US states have been successful in passing legislation to set nutrition standards for public food procurement, and other nations have enacted policies to support local food production and urban agriculture (51). Although public health nutrition approaches have been successful in many cases, much work is needed to evaluate the policies and interventions that currently exist, formulate new strategies based on existing research, and generate evidence to support public health initiatives (54). The strong evidence supporting the health and environmental benefits of plant-based diets could be used to inform public health nutrition strategies to shift populations towards diets higher in healthy plant-based foods and lower in animal-based foods.
Dietary Patterns and Planetary Health
In addition to their associated health benefits, plant-based diets also tend to have less environmental impact than animal-based diets (55). Globally, food production is the largest contributor to biodiversity loss and is responsible for 80% of deforestation, >70% of fresh water use, and 30% of human-generated greenhouse gas (GHG) emissions (55). Meat has been identified as the food that has the greatest impact on GHG emissions and land use (55). Producing 1000 kcal of lamb or beef generates 14 and 10 kg of GHG emissions, respectively, compared with just 1 and 3 kg for 1000 kcal of lentils or tofu (56). Producing 1 serving of beef or pork requires 1211 and 469 L of water, respectively, compared with 220, 57, and 30 L required to produce 1 serving of dry beans, tofu, or tomatoes (56). Multiple studies have shown that decreasing meat consumption could reduce GHG emissions as well as land, water, and energy usage, while simultaneously improving health outcomes (55). However, it is not necessary to completely eliminate meat to consume a healthy and sustainable diet. A systematic review by Nelson et al. (55) showed that it is possible to achieve a sustainable diet that meets nutritional requirements without eliminating meat or dairy and without increasing cost. Multiple plant-based diets such as the Dietary Approaches to Stop Hypertension, Mediterranean, Healthy US-Style, and Healthy Vegetarian patterns have been shown to reduce the risk of chronic diseases such as obesity, CVD, T2D, and some cancers. All of these dietary patterns can include animal products such as dairy and some even allow red meat in moderate quantities, but they have all been shown to be healthier and associated with less environmental impact than the average US diet (55).
It is also important to note that just because a diet is sustainable, does not mean it is healthy. Vegan and vegetarian diets typically have less environmental impact than diets containing meat (57), but a vegan eating many refined carbohydrates and added sugars could be at greater risk for weight gain and chronic diseases than an omnivore consuming meat and a variety of healthy plant-based foods. Although it is possible to achieve a healthy and sustainable diet without becoming vegan or vegetarian, these dietary patterns, if comprised of high-quality plant foods and appropriately planned to avoid deficiencies, can be nutritionally adequate for all stages of the life cycle (including infancy, pregnancy, and older adulthood) and can reduce chronic disease risk (57). The 2015–2020 US Dietary Guidelines provide detailed meal plans for the Healthy Vegetarian Pattern, and an adaptation for vegans, that satisfy nutritional requirements at varying levels of energy intake (58).
In addition to the types of foods included in dietary patterns, it is also necessary to consider calorie intake. Very-high-calorie diets are common in many high-income countries and not only can lead to poor health outcomes but also have been shown to have higher carbon dioxide emissions than lower-calorie diets (55). After an extensive review of the current evidence, scientists on the 2015 United States Dietary Guidelines Scientific Advisory Committee concluded that in order to improve population and planetary health, the US population should eat more plant-based foods and less meat, and decrease its total calorie intake (11). These recommendations are applicable to other high-income countries beyond the United States and could be evaluated and adapted for other global contexts.
A recent study modeled the effects of different diet scenarios in 150 countries in all regions of the world, and found that 4 different energy-balanced, low-meat diets in line with current evidence-based dietary recommendations could reduce global environmental impact, nutrient deficiencies, and diet-related mortality (59). Designed to meet global public health objectives and adapted to fit national food preferences for each country, these dietary patterns were all predominantly plant-based, including abundant fruits, vegetables, nuts, and legumes, and limiting sugar and processed meat. The 4 dietary patterns were: flexitarian (limited red meat, moderate animal-source foods); pescatarian (meat replaced with fish, moderate animal-source foods); vegetarian (no meat, moderate animal-source foods); and vegan (no animal-source foods). Worldwide, it was estimated that large-scale adoption of any of these diets could provide an adequate nutrient supply (although vitamin B-12, riboflavin, and calcium may need to be supplemented in some vegetarian/vegan diets); reduce premature mortality by ∼20% (predominantly due to CVD-, cancer-, and T2D-related causes); and reduce GHGs, nitrogen application, phosphorus application, cropland use, and freshwater use in high- and middle-income countries. The authors also modeled dietary patterns focused only on environmental or food security priorities (59), and found that although these patterns had benefits, they did not simultaneously address environmental, nutrient deficiency, and diet-related mortality challenges as effectively as the 4 diets based on public health objectives. As demonstrated by this study, adherence to evidence-based dietary recommendations, through a variety of different plant-based dietary patterns, can itself have beneficial environmental impacts. The potential health and environmental benefits of shifting global consumption patterns towards plant-based diets are substantial. Encouraging plant-based diets globally will become increasingly important as population growth and climate change continue, straining our planet's food production capacity and threatening future food security (55).
Conclusions
Personal, population, and planetary health are closely intertwined and are all threatened by low-quality diets and environmental degradation (Figure 3). Current evidence clearly indicates that dietary patterns higher in healthy plant-based foods and lower in animal-based foods, especially meat, are associated with less environmental impact and lower risk of diet-related chronic diseases. Shifting global populations towards healthy plant-based dietary patterns could alleviate the current diet-related chronic disease epidemics as well as future environmental and food security crises that will likely occur if we continue to consume our planet's resources at the current rates. To make this shift, public health policies and interventions are necessary to encourage healthy behavior and change current food environments. It is also important to consider strategies to reduce food waste, which will greatly benefit the environment, and to reduce caloric intake, which will benefit both the environment and human health. Precision nutrition will likely play a role in optimizing personal health in the future, but much more research is needed before it can be widely applied to disease prevention. Therefore, when allocating resources, it is crucial to balance investment in precision nutrition and public health strategies. If the current chronic disease and environmental degradation trends continue, we will overwhelm global healthcare and food production systems, jeopardizing personal, population, and planetary health. Transitioning global diets towards healthy plant-based dietary patterns would require large-scale public health efforts, but could be instrumental in ensuring future human and planetary health.
FIGURE 3.
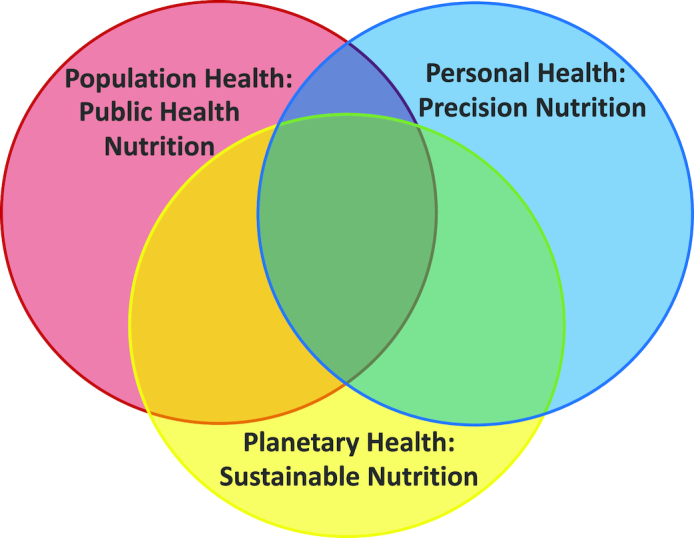
The intersection between population, personal, and planetary health and relation to public health nutrition, precision nutrition, and sustainable nutrition.
Acknowledgments
All authors contributed to the conceptual development, writing, and revision of the manuscript, and read and approved the final manuscript.
Notes
Published in a supplement to Advances in Nutrition. This supplement was sponsored by the Harding-Buller Foundation of Ohio. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the sponsors. Publication costs for this supplement were defrayed in part by the payment of page charges. The opinions expressed in this publication are those of the authors and are not attributable to the sponsors or the publisher, Editor, or Editorial Board of Advances in Nutrition.
FBH's research is supported by NIH grants HL60712, HL118264, and DK112940.
Author disclosures: ECH report no conflicts of interest. FBH reported receiving research support from the California Walnut Commission and personal fees from Standard Process, Diet Quality Photo Navigation, and Metagenics, outside the submitted work.
Abbreviations used: CVD, cardiovascular disease; FFVP, Fresh Fruit and Vegetable Program; GHG, greenhouse gas; MUFA, monounsaturated fatty acid; PUFA, polyunsaturated fatty acid; SSB, sugar-sweetened beverage; T2D, type 2 diabetes.
References
- 1. World Health Organization. Obesity and overweight fact sheet. [updated October; cited 27 November, 2017] WHO; 2017.; Available from: http://www.who.int/mediacentre/factsheets/fs311/en/. [Google Scholar]
- 2. Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications. Nat Rev Endocrinol. 2013;9(1):13–27. [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization. Cardiovascular diseases. [cited 17 November 2017] WHO; 2017.; Available from: http://www.who.int/cardiovascular_diseases/en/. [Google Scholar]
- 4. World Health Organization. Diabetes. [updated November, cited 17 November 2017] WHO; 2017.; Available from: http://www.who.int/mediacentre/factsheets/fs312/en/. [Google Scholar]
- 5. Marczak L, O'Rourke K, Shepard D, for the Institute for Health Metrics and Evaluation . When and why people die in the United States, 1990–2013. JAMA. 2016;315(3):241. [Google Scholar]
- 6. Bhupathiraju SN, Hu FB. Epidemiology of obesity and diabetes and their cardiovascular complications. Circ Res. 2016;118(11):1723–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. The Carlyle Group. McDonald's Announces Growth Plan for China Following Completion of Strategic Partnership with CITIC and Carlyle. The Carlyle Group; 2017. Available from: https://carlyle.com/media-room/news-release-archive/mcdonald's-announces-growth-plan-china-following-completion. [Google Scholar]
- 8. Sabate J, Soret S. Sustainability of plant-based diets: back to the future. Am J Clin Nutr. 2014;100(Suppl 1):S476–82. [DOI] [PubMed] [Google Scholar]
- 9. Pimentel D, Pimentel M. Sustainability of meat-based and plant-based diets and the environment. Am J Clin Nutr. 2003;78(3 Suppl):S660–3. [DOI] [PubMed] [Google Scholar]
- 10. Satija A, Hu FB. Plant-based diets and cardiovascular health. Trends Cardiovasc Med. 2018;28(7):437–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dietary Guidelines Advisory Committee. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. Washington, DC: US Department of Agriculture and US Department of Health and Human Services; 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Aune D, Giovannucci E, Boffetta P, Fadnes LT, Keum N, Norat T, Greenwood DC, Riboli E, Vatten LJ, Tonstad S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—a systematic review and dose-response meta-analysis of prospective studies. Int J Epidemiol. 2017;46(3):1029–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zong G, Gao A, Hu FB, Sun Q. Whole grain intake and mortality from all causes, cardiovascular disease, and cancer: a meta-analysis of prospective cohort studies. Circulation. 2016;133(24):2370–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Luo C, Zhang Y, Ding Y, Shan Z, Chen S, Yu M, Hu FB, Liu L. Nut consumption and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a systematic review and meta-analysis. Am J Clin Nutr. 2014;100(1):256–69. [DOI] [PubMed] [Google Scholar]
- 15. Afshin A, Micha R, Khatibzadeh S, Mozaffarian D. Consumption of nuts and legumes and risk of incident ischemic heart disease, stroke, and diabetes: a systematic review and meta-analysis. Am J Clin Nutr. 2014;100(1):278–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Anderson JW, Major AW. Pulses and lipaemia, short- and long-term effect: potential in the prevention of cardiovascular disease. Br J Nutr. 2002;88(Suppl 3):S263–71. [DOI] [PubMed] [Google Scholar]
- 17. Poole R, Kennedy OJ, Roderick P, Fallowfield JA, Hayes PC, Parkes J. Coffee consumption and health: umbrella review of meta-analyses of multiple health outcomes. BMJ. 2017;359:j5024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhang C, Qin YY, Wei X, Yu FF, Zhou YH, He J. Tea consumption and risk of cardiovascular outcomes and total mortality: a systematic review and meta-analysis of prospective observational studies. Eur J Epidemiol. 2015;30(2):103–13. [DOI] [PubMed] [Google Scholar]
- 19. Martínez-González MA, Sánchez-Tainta A, Corella D, Salas-Salvad J, Ros E, Arós F, Gómez-Gracia E, Fiol M, Lamuela-Raventós RM, Schröder H et al.. A provegetarian food pattern and reduction in total mortality in the Prevencion con Dieta Mediterranea (PREDIMED) study. Am J Clin Nutr. 2014;100(Suppl 1):320s–8s. [DOI] [PubMed] [Google Scholar]
- 20. Satija A, Bhupathiraju SN, Spiegelman D, Chiuve SE, Manson JE, Willett W, Rexrode KM, Rimm EB, Hu FB. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J Am Coll Cardiol. 2017;70(4):411–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Satija A, Bhupathiraju SN, Rimm EB, Spiegelman D, Chiuve SE, Borgi L, Willett WC, Manson JE, Sun Q, Hu FB. Plant-based dietary patterns and incidence of type 2 diabetes in US men and women: results from three prospective cohort studies. PLoS Med. 2016;13(6):e1002039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wang DD, Li Y, Chiuve SE, Stampfer MJ, Manson JE, Rimm EB, Willett WC, Hu FB. Association of specific dietary fats with total and cause-specific mortality. JAMA Intern Med. 2016;176(8):1134–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Li Y, Hruby A, Bernstein AM, Ley SH, Wang DD, Chiuve SE, Sampson L, Rexrode KM, Rimm EB, Willett WC et al.. Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease: a prospective cohort study. J Am Coll Cardiol. 2015;66(14):1538–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zong G, Li Y, Sampson L, Dougherty LW, Willett WC, Wanders AJ, Alssema M, Zock PL, Hu FB, Sun Q. Monounsaturated fats from plant and animal sources in relation to risk of coronary heart disease among US men and women. Am J Clin Nutr. 2018;107(3):445–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Song M, Fung TT, Hu FB, Willett WC, Longo VD, Chan AT, Giovannucci EL. Association of animal and plant protein intake with all-cause and cause-specific mortality. JAMA Intern Med. 2016;176(10):1453–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Stampfer MJ, Willett WC, Hu FB. Red meat consumption and mortality: results from 2 prospective cohort studies. Arch Intern Med. 2012;172(7):555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pan A, Sun Q, Bernstein AM, Schulze MB, Manson JE, Willett WC, Hu FB. Red meat consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. Am J Clin Nutr. 2011;94(4):1088–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pan A, Sun Q, Bernstein AM, Manson JE, Willett WC, Hu FB. Changes in red meat consumption and subsequent risk of type 2 diabetes mellitus: three cohorts of US men and women. JAMA Intern Med. 2013;173(14):1328–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Liu G, Zong G, Hu FB, Willett WC, Eisenberg DM, Sun Q. Cooking methods for red meats and risk of type 2 diabetes: a prospective study of U.S. women. Diabetes Care. 2017;40(8):1041–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Liu G, Zong G, Wu K, Hu Y, Li Y, Willett WC, Eisenberg DM, Hu FB, Sun Q. Meat cooking methods and risk of type 2 diabetes: results from three prospective cohort studies. Diabetes Care. 2018;41(5):1049–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wang DD, Hu FB. Precision nutrition for prevention and management of type 2 diabetes. Lancet Diabetes Endocrinol. 2018;6(5):416–26. [DOI] [PubMed] [Google Scholar]
- 32. de Toro-Martín J, Arsenault BJ, Després JP, Vohl MC. Precision nutrition: a review of personalized nutritional approaches for the prevention and management of metabolic syndrome. Nutrients. 2017;9(8):913. doi:10.3390/nu9080913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Tanaka T, Ngwa JS, van Rooij FJ, Zillikens MC, Wojczynski MK, Frazier-Wood AC, Houston DK, Kanoni S, Lemaitre RN, Luan J et al.. Genome-wide meta-analysis of observational studies shows common genetic variants associated with macronutrient intake. Am J Clin Nutr. 2013;97(6):1395–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Castañer O, Corella D, Covas MI, Sorlí JV, Subirana I, Flores-Mateo G, Nonell L, Bulló M, de la Torre R, Portolés O et al.. In vivo transcriptomic profile after a Mediterranean diet in high-cardiovascular risk patients: a randomized controlled trial. Am J Clin Nutr. 2013;98(3):845–53. [DOI] [PubMed] [Google Scholar]
- 35. Bouchard-Mercier A, Paradis AM, Rudkowska I, Lemieux S, Couture P, Vohl MC. Associations between dietary patterns and gene expression profiles of healthy men and women: a cross-sectional study. Nutr J. 2013;12:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Guasch-Ferré M, Hruby A, Toledo E, Clish CB, Martínez-González MA, Salas-Salvadó J, Hu FB. Metabolomics in prediabetes and diabetes: a systematic review and meta-analysis. Diabetes Care. 2016;39(5):833–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ley RE, Turnbaugh PJ, Klein S, Gordon JI. Microbial ecology: human gut microbes associated with obesity. Nature. 2006;444(7122):1022–3. [DOI] [PubMed] [Google Scholar]
- 38. Wong JM. Gut microbiota and cardiometabolic outcomes: influence of dietary patterns and their associated components. Am J Clin Nutr. 2014;100(Suppl 1):369s–77s. [DOI] [PubMed] [Google Scholar]
- 39. Zeevi D, Korem T, Zmora N, Israeli D, Rothschild D, Weinberger A, Ben-Yacov O, Lador D, Avnit-Sagi T, Lotan-Pompan M et al.. Personalized nutrition by prediction of glycemic responses. Cell. 2015;163(5):1079–94. [DOI] [PubMed] [Google Scholar]
- 40. Coombes R. Trans fats: chasing a global ban. BMJ. 2011;343:d5567. [DOI] [PubMed] [Google Scholar]
- 41. Brownell KD, Pomeranz JL. The trans-fat ban—food regulation and long-term health. N Engl J Med. 2014;370(19):1773–5. [DOI] [PubMed] [Google Scholar]
- 42. Restrepo BJ, Rieger M. Denmark's policy on artificial trans fat and cardiovascular disease. Am J Prev Med. 2016;50(1):69–76. [DOI] [PubMed] [Google Scholar]
- 43. Brandt EJ, Myerson R, Perraillon MC, Polonsky TS. Hospital admissions for myocardial infarction and stroke before and after the trans-fatty acid restrictions in New York. JAMA Cardiol. 2017;2(6):627–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Fung TT, Malik V, Rexrode KM, Manson JE, Willett WC, Hu FB. Sweetened beverage consumption and risk of coronary heart disease in women. Am J Clin Nutr. 2009;89(4):1037–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, Willett WC, Hu FB. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA. 2004;292(8):927–34. [DOI] [PubMed] [Google Scholar]
- 46. de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med. 2012;367(15):1397–406. [DOI] [PubMed] [Google Scholar]
- 47. Colchero MA, Rivera-Dommarco J, Popkin BM, Ng SW. In Mexico, evidence of sustained consumer response two years after implementing a sugar-sweetened beverage tax. Health Aff (Millwood). 2017;36(3):564–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Center for Science in the Public Interest. Local Sugary Drink Taxes Voted on 2014–2017. Washington, DC; January2018. Available from: https://cspinet.org/sites/default/files/attachment/localsugarydrinks3.pdf. [Google Scholar]
- 49. Silver LD, Ng SW, Ryan-Ibarra S, Taillie LS, Induni M, Miles DR, Poti JM, Popkin BM. Changes in prices, sales, consumer spending, and beverage consumption one year after a tax on sugar-sweetened beverages in Berkeley, California, US: a before-and-after study. PLoS Med. 2017;14(4):e1002283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Long MW, Gortmaker SL, Ward ZJ, Resch SC, Moodie ML, Sacks G, Swinburn BA, Carter RC, Claire Wang Y. Cost effectiveness of a sugar-sweetened beverage excise tax in the U.S. Am J Prev Med. 2015;49(1):112–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. World Cancer Research Fund International. NOURISHING Database, 2018; [updated 24 October, 2018; cited 24 October, 2018]. Available from: https://www.wcrf.org/int/policy/nourishing-database. [Google Scholar]
- 52. Mozaffarian RS, Gortmaker SL, Kenney EL, Carter JE, Howe MC, Reiner JF, Cradock AL. Assessment of a districtwide policy on availability of competitive beverages in Boston public schools, Massachusetts, 2013. Prev Chronic Dis. 2016;13:E32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Bartlett S OL, Klerman J, Patlan KL, Blocklin M, Connor P, Webb K, Ritchie L, Wakimoto P, Crawford P. Evaluation of the Fresh Fruit and Vegetable Program (FFVP): Final Evaluation Report. Alexandria, VA: US Department of Agriculture, Food and Nutrition Service; 2013. [Google Scholar]
- 54. Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, Franch HA, Jacobs DR Jr, Kraus WE, Kris-Etherton PM, Krummel DA et al.. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126(12):1514–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Nelson ME, Hamm MW, Hu FB, Abrams SA, Griffin TS. Alignment of healthy dietary patterns and environmental sustainability: a systematic review. Adv Nutr. 2016;7(6):1005–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Culinary Institute of America and President and Fellows of Harvard College. Menus of Change 2018 Annual Report. Culinary Institute of America and Harvard TH Chan School of Public Health; 2018. [Google Scholar]
- 57. Melina V, Craig W, Levin S. Position of the Academy of Nutrition and Dietetics: vegetarian diets. J Acad Nutr Diet. 2016;116(12):1970–80. [DOI] [PubMed] [Google Scholar]
- 58. U.S. Department of Health and Human Services and U.S. Department of Agriculture . 2015–2020 Dietary Guidelines for Americans. 8th Edition. pp. 86–8. December 2015. Available at http://health.gov/dietaryguidelines/2015/guidelines/. [Google Scholar]
- 59. Springmann M, Wiebe K, Mason-D'Croz D, Sulser TB, Rayner M, Scarborough P. Health and nutritional aspects of sustainable diet strategies and their association with environmental impacts: a global modelling analysis with country-level detail. Lancet Planet Health. 2018;2(10):e451–61. [DOI] [PMC free article] [PubMed] [Google Scholar]


