Abstract
Background:
Sleep is crucial to human's health and essential for a person's wellbeing. It is involved in multiple physiological mechanisms, such as metabolism, appetite regulation, immune and hormone function, and cardiovascular systems. The National Sleep Foundation recommends 7–9 h of sleep each night for adults. Short (<7 h) and long (<9 h) sleep duration has been reported to be associated with increased risk of morbidity and mortality.
Aim:
1) To assess the prevalence of short sleep durations among Saudi adult population. 2) To examine comorbid medical condition's association with short sleep duration.
Methods:
A nation-wide quantitative cross-sectional study using an online self-administered constructed questionnaire during the period from August to October 2018 was conducted. The questionnaire included demographic characters, such as age, gender, education level, height, and weight. As well as some of the participants’ habits such as consuming coffee and/or tea, smoking status, and other habits known to be associated with shorter sleep hours. The questionnaire also included self-reported duration of sleep and history of diagnosed medical illnesses.
Results:
The study included 805 adult Saudi participants with ages ranging from 15- to 60-year old and mean age of 21.8 ± 10.7-year old. About 63% of the participants were females. It was established that almost half 49.6% of the participants sleep for <7 h daily, and 39.3% of them sleep for 7–9 h.
Conclusion:
About half of Saudi adults do not get enough hours of sleep. Especially, people who are married, above 30-year old, students or tea drinkers (P < 0.05): furthermore, people with medical comorbidities such as anxiety, depression, and insomnia had a higher association with short sleep duration. Last, sleep deprivation adversely affects the physical wellbeing and quality of life of participants, demonstrated in bad mood, somnolence, and tiredness during the day time.
Keywords: Anxiety and insomnia, medical comorbidity, prevalence, short sleep
Background
Sleep is crucial to the human's health and essential for life.[1] It is involved in multiple systemic physiological mechanisms, such as metabolism, appetite regulation, immune and hormone function, and cardiovascular systems.[2] It is recommended by The National Sleep Foundation to get at least 7 h of sleep daily for adults. Short (<7 h) and long (>9 h) sleep duration has been reported to be associated with increased risk of morbidity and mortality.[3] Namely, cardiovascular and cerebrovascular disease, obesity, diabetes, cancer, and depression.[4]
However, nearly one-third of adults report short sleep duration.[5] Responsible factors that lead to increases in the prevalence of short sleep durations include bright environmental light during the night time, longer workdays, night shifts, and use of electronics, such as television, radio, and computers.[6] Studies suggest that short sleep duration may result in greater insulin resistance, along with decreased leptin and increased ghrelin through regulation of the hypothalamic-pituitary-adrenal axis. This possibly will lead to metabolic abnormalities and weight gain.[7] However, the mechanism of the relationship between sleep duration and chronic diseases is understudied and has not yet been explained.[8]
Studies reported that short sleep results in decreased glucose tolerance and increased insulin resistance, sympathetic tone, and blood pressure.[9] Experiments have established that short sleep results in elevations in C-reactive protein levels, an inflammatory marker that is related to cardiovascular disease[10] Furthermore, published studies confirmed that there is a link between short sleep duration and chances of developing hyperlipidemia, motor vehicle accident, and increased risk of coronary artery disease.[11]
Although the complications and adverse effects of inadequate sleep duration can be a detriment to a person's quality of life and daily living, affecting their mood, self-esteem, productivity, and potentially leading to more serious chronic morbidities such as hyperlipidemia, hypertension, and cardiac disease. They can be avoided and this behavioral issue can be effectively managed through preventive medicine at the primary care level where people can receive the most important keys to tackling this issue: health promotion and maintenance, medical counseling, and patient education.
The current study aimed to assess the prevalence of short sleep durations among Saudi adult population and its association with comorbid medical conditions.
As of writing this paper, there are very few population studies in Saudi Arabia that measure the prevalence of short sleep duration, its associated factors, and consequences of comorbidity on this unhealthy behavior. Thus, this study was conducted to further reinforce the literature knowledge in the region about the problem.
Methodology
A nation-wide quantitative cross-sectional study using an online self-administered structured questionnaire during the period from August to October 2018 was conducted. The sample size was decided relying on this established formula n = (z2 × p × q)/d2,[12] where n is the minimum sample size, z = 1.96, P = 0.5, and q = (1 − p) =0.86. After doing the calculations, we found that the minimum sample size to achieve a precision of ±4% with a 95% confidence interval (CI) is 601 after accounting for on-response and incomplete data we set our goal to 805 participants. All participants aged 15–60 years, Saudis, who completed all the required questions of the survey were included in the study.
Exclusion criteria apply to non-Saudis, below 15-year old and those who are currently using any sleep medication. The researchers distributed the questionnaire randomly in known social media platforms through the use of Google form. Participants were requested to give their consent before filling the questionnaire. The questionnaire was developed by the researchers after intensive literature review and it was reviewed by medical experts for modifications. The questionnaire included demographic characters, such as age, gender, education level, height, and weight. There are questions about the participants’ habits like consuming coffee and/or tea, and whether they are smokers or not. The questionnaire also included self-reported duration of sleep and history of diagnosed diseases, such as diabetes mellitus (DM), hypertension (HTN), hyperlipidemia, asthma, and chronic obstructive pulmonary disease (COPD). The ethical approval to conduct this study was obtained from the research ethics committee of Shaqra University.
Data analysis
After data collection, it was revised, entered into a computer and analyzed with statistical software IBM SPSS version 20. The given graphs were constructed using Microsoft excel software. Statistical analysis was performed using two-tailed tests and alpha error of 0.05. P value ≤0.05 was deemed statistically significant. Chi-square/Mont Carlo exact test and Fisher's exact test were used to test for the association between different patients’ factors and sleep duration. Exact tests were used if there are small frequencies where chi square is invalid. Multiple logistic regression model was used to identify the most important predictors for short sleep duration after adjusting all confounders.
Results
The study included 805 adult Saudi participants with ages that ranged from 15- to 60-year old and mean age of 21.8 ± 10.7-year old. About 63% of the participants were females and 61% were unmarried. University level of education was recorded among 77% of the sampled adults and 50% were students.
With regard to sleeping duration, 49.6% of the participants sleep for <7 h daily and 39.3% of them sleep for 7–9 h daily [Figure 1].
Figure 1.
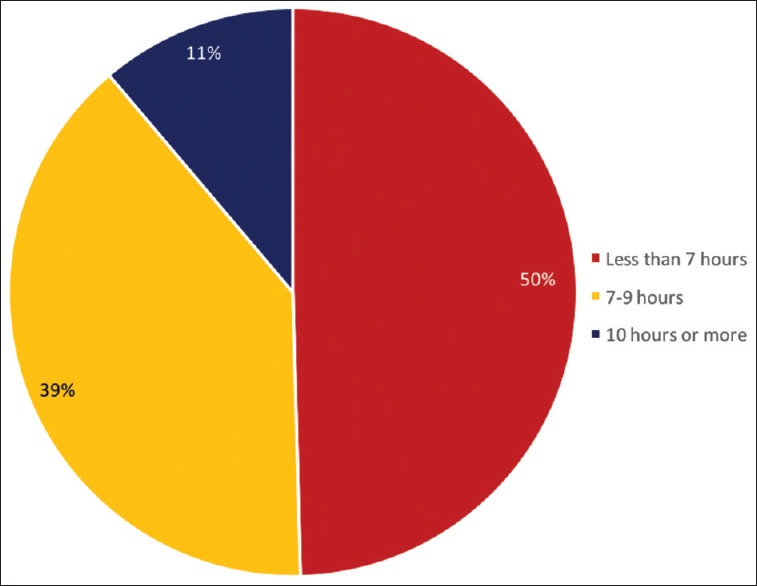
Prevalence of sleep duration among Saudi adult population in 2018
On relating sleeping duration with participants’ personal characteristics [Table 1], it was clear that about half of both males and females (49%) sleep for <7 h daily. With regard to age, 24.4% of those who aged <18 years sleep for <7 h daily compared with 64.5% of those who were >30 years with recorded statistical significance (P < 0.05). Considering marital status, 59.8% of married participants sleep for <7 h daily compared with 43.7% of unmarried adults and this difference was found to be statistically significant (P < 0.05). As for educational level, 80% of those who had primary educational level sleep for <7 h daily compared with 51.4% of university graduated participants with statically significance (P < 0.05). Also, 80.8% of retired population sleep for <7 h daily compared with 44.1% of students. Considering number of coffee cups per day, 57.4% of those who had three cups of coffee per day or more sleep for <7 h compared with 46.8% of those who did not drink coffee with borderline statistical significance (P = 0.066). As for tea drinking, 54.5% of those who had three cups of tea per day or more sleep for <7 h compared with 46.4% of those who did not had tea at all with significant difference (P < 0.05).
Table 1.
Distribution of sleep hours among Saudi adults population according to their personal characteristics
| Personal data | Sleep hours | P | ||||||
|---|---|---|---|---|---|---|---|---|
| <7 h | 7-9 h | >10 h | ||||||
| n | % | n | % | n | % | |||
| Gender | Male | 149 | 49.8 | 116 | 38.8 | 34 | 11.4 | 0.976 |
| Female | 250 | 49.4 | 200 | 39.5 | 56 | 11.1 | ||
| Age in years | <18 | 11 | 24.4 | 22 | 48.9 | 12 | 26.7 | 0.001* |
| 19-30 | 223 | 44.2 | 210 | 41.7 | 71 | 14.1 | ||
| 31-60 | 165 | 64.5 | 84 | 32.8 | 7 | 2.7 | ||
| Marital status | Married | 171 | 59.8 | 99 | 34.6 | 16 | 5.6 | 0.001* |
| Unmarried | 217 | 43.7 | 208 | 41.9 | 72 | 14.5 | ||
| Divorced | 11 | 50.0 | 9 | 40.9 | 2 | 9.1 | ||
| Educational level | Primary | 4 | 80.0 | 1 | 20.0 | 0 | 0.0 | 0.045* |
| Intermediate | 3 | 30.0 | 5 | 50.0 | 2 | 20.0 | ||
| Secondary | 72 | 42.9 | 67 | 39.9 | 29 | 17.3 | ||
| University/more | 320 | 51.4 | 243 | 39.1 | 59 | 9.5 | ||
| Job | Student | 179 | 44.1 | 169 | 41.6 | 58 | 14.3 | 0.001* |
| Employee | 115 | 55.3 | 78 | 37.5 | 15 | 7.2 | ||
| Not working | 84 | 50.9 | 64 | 38.8 | 17 | 10.3 | ||
| Retired | 21 | 80.8 | 5 | 19.2 | 0 | 0.0 | ||
| Coffee cups per day | None | 73 | 46.8 | 57 | 36.5 | 26 | 16.7 | 0.066 |
| One | 180 | 46.9 | 162 | 42.2 | 42 | 10.9 | ||
| Two | 84 | 53.5 | 62 | 39.5 | 11 | 7.0 | ||
| Three or more | 62 | 57.4 | 35 | 32.4 | 11 | 10.2 | ||
| Tea cups per day | None | 83 | 46.4 | 73 | 40.8 | 23 | 12.8 | 0.016* |
| One | 205 | 47.8 | 184 | 42.9 | 40 | 9.3 | ||
| Two | 69 | 57.5 | 39 | 32.5 | 12 | 10.0 | ||
| Three or more | 42 | 54.5 | 20 | 26.0 | 15 | 19.5 | ||
P=Pearson χ2 test, *P<0.05 (significant)
On relating sleeping duration with comorbidities [Table 2], 56.1% of those who complained of anxiety sleep for <7 h daily and also 54% of those who had late insomnia and 48% of participants with early insomnia. About 36% of participants who were overweight sleep for <7 h daily, whereas those who reported diagnosis of depression were found to be 14.5%. About 41% of participants who had interrupted sleeping also sleep for <7 h daily. Tiredness during the day time was recorded among 60.7% of those who sleep for < 7 h daily, whereas 77.9% had unpleasant mood.
Table 2.
Distribution of comorbidities among Saudi adults population according to their sleep duration
| Comorbidities | Sleep hours | P | |||||
|---|---|---|---|---|---|---|---|
| <7 h | 7-9 h | >10 h | |||||
| n | % | n | % | n | % | ||
| DM | 17 | 4.3 | 6 | 1.9 | 3 | 3.3 | 0.207 |
| HTN | 21 | 5.3 | 11 | 3.5 | 4 | 4.4 | 0.519 |
| Depression | 58 | 14.5 | 34 | 10.8 | 23 | 25.6 | 0.002* |
| Asthma | 25 | 6.3 | 15 | 4.7 | 6 | 6.7 | 0.630 |
| Hypercholesterolemia | 41 | 10.3 | 28 | 8.9 | 6 | 6.7 | 0.533 |
| Overweight | 145 | 36.3 | 115 | 36.4 | 27 | 30.0 | 0.494 |
| Anxiety | 224 | 56.1 | 104 | 32.9 | 28 | 31.1 | 0.001* |
| Early insomnia | 192 | 48.1 | 107 | 33.9 | 34 | 37.8 | 0.001* |
| Interrupted sleep | 163 | 40.9 | 95 | 30.1 | 33 | 36.7 | 0.012* |
| Late insomnia | 217 | 54.4 | 162 | 51.3 | 28 | 31.1 | 0.001* |
| Tiredness during day time | 242 | 60.7 | 126 | 39.9 | 44 | 48.9 | 0.001* |
| Insufficient sleeping affect mode | 311 | 77.9 | 260 | 82.3 | 73 | 81.1 | 0.342 |
DM=diabetes mellitus; HTN=hypertension; P=Pearson χ2 test. *P<0.05 (significant)
Finally, multiple logistic regression model for predictors of short duration sleep revealed that among all included determinants, age, coffee drinking, and marital status were the most significant determinants [Table 3]. As for age, the increased age by 1 year was associated with increase in the likelihood of short duration sleep by about 72% (OR = 1.72; 95% CI: 1.3-2.3). Considering marital status, married participants recorded 24% more likelihood for short duration sleep than unmarried (OR = 1.24; 95% CI: 1.12–1.79). With regard to coffee drinking, the increased intake by one more cup per day was associated with increased likelihood for short-duration sleeping by about 18% (OR = 1.18; 95% CI: 1.10–1.69) keeping all other factors constant.
Table 3.
Multiple logistic regression model for determinants of short sleep duration among Saudi adult population
| Determinant | B | SE | P | OR | 95% CI for OR | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Gender | −0.031 | 0.157 | 0.846 | 0.970 | 0.712 | 1.320 |
| Age | 0.546 | 0.139 | 0.001 | 1.727* | 1.315 | 2.269 |
| Marital status | 0.216 | 0.054 | 0.045 | 1.240* | 1.120 | 1.790 |
| Education | 0.111 | 0.154 | 0.472 | 1.117 | 0.826 | 1.510 |
| Job | 0.009 | 0.100 | 0.930 | 1.009 | 0.830 | 1.226 |
| Coffee | 0.170 | 0.009 | 0.044 | 1.180* | 1.10 | 1.690 |
| Tea | 0.053 | 0.089 | 0.551 | 1.054 | 0.886 | 1.255 |
| Constant | −1.830 | 0.709 | 0.010 | 0.160 | ||
| Pseudo R2: Model significance | 26%; 0.026* | |||||
| Model accuracy | 59.9% | |||||
SE=standard error; OR=odds ratio; CI=confidence interval
Discussion
Sleep deprivation is a very common problem worldwide, and in Saudi Arabia in particular as evident by this study's results, affecting the productivity of the participants and causing low mood. Also, it was found to have a statistically significant association with multiple comorbidities as demonstrated by the results of this study.
Both genders were found to have similar percentages of sleep deprivation with a slight increase in males 149 (49.8%) compared with females 250 (49.4%), which is in accordance with another study done in Saudi Arabia which showed that there is no difference in sleep duration between males and females.[13]
It was found that the majority of the participants (49.6%) sleep <7 h a day, which is considered a higher percentage compared with a study conducted in America on 444,306 adults[14] as well as other studies worldwide.[15,16]
The age factor played a significant role in the association between increasing in age and short sleep duration, for instance, 165 (64.5%) of participants aged >30-year old sleep <7 h/day. Which is a result replicated in other studies.[17]
Furthermore, married participants were found to suffer from short sleep duration 171 (59.8%) when compared to unmarried participants 217 (43.7%), which is an expected result due to the increase in daily life duties and responsibilities married people are usually facing, including the potential of being parents which makes it harder to gain the appropriate amount of sleep daily. Educational level in this study showed a statistically significant association to short sleep duration, especially in university students of which 320 (51.4%) were found to sleep <7 h a day.
Participants who are currently employed 115 (55.3%) have shown a higher number of short sleep duration in contrast to unemployed participants 84 (50.9%). It is predictable that students are likely affected by late-night activities and early morning school manifesting in a high percentage of short sleep in this population 179 (44.1%), which is a shared problem students face worldwide as shown in a study conducted on Chinese university students in 2017.[18]
We can also see that retired people are showing higher percentages of short sleep 21 (80.8%) and this is most likely goes with the fact that retired people are mainly from the old age population which is a factor of its own.
Coffee can affect sleep duration, for instance, those who drink three or more cups of coffee have a higher percentage of short sleep duration 62 (57.4%), which goes with a previous study done in Taiwan.[19]
Contributors who drink tea frequently were found to have a statistically significant relation with short sleep duration 42 (54.5%), which also goes with another study done in the USA in 2013.[20]
Furthermore, there is a statistical relation between short sleep duration and participants who suffer from depression 58 (14.5%). The same is observed for people with anxiety 224 (56.1%), which is similar to other study done in the Netherlands on 2,619 participants in 2013.[21]
A high percentage of people who reported sleeping <7 h had early insomnia 192 (48.1%), and an even a higher percentage reported suffering from late insomnia 217 (54.4%). In accordance with a study done in 2010 measuring short sleep duration, insomnia and mortality.[22]
Another high percentage 163 (40.9%) of participants with short sleep duration reported suffering from interrupted sleep, and 311 (77.9%) reported affected mood.
In this study, we could not find a statistically significant relation between short sleep duration and asthma, BMI, DM, and HTN. However, such associations were present in other studies that discussed the relationship between short sleep and asthma,[23] BMI,[24,25] DM,[26] and HTN.[27]
When comparing the study results to very recent literature, we find multiple similarities in regards to significant associations of short sleep to the multitude of factors found in this study, namely, a study conducted in New Zealand in 2019 showed the relation between short sleep duration and participant's psychological wellbeing demonstrated in the presence of bad mood, dissatisfaction and low self-esteem in people who sleep less than 7 h a day.[28] Other studies showed the relation to physical and social factors,[29] and lastly, depression.[30] On the other hand, some result did not align with commonly found and documented relations: hypertension, diabetes mellitus, and hyperlipidemia to name a few. This can be seen in a recent study conducted in Taiwan on 26,016 volunteers in 2019 which evidently shows that sleep duration is associated with metabolic syndrome components.[31] We postulate that the reason for this discrepancy is the small sample size. Furthermore, when assessing the medical history of participants and checking for comorbidities, self-reports were relied upon to gain the data rather than professional medical diagnosis.
Conclusions
After analyzing the results of this research, it was concluded that about half of Saudi adults do not get enough hours of sleep, especially people who are married, >30-year old, students and tea drinkers. People with medical comorbidities such as anxiety, depression, and insomnia had a higher association with short sleep duration. Sleep deprivation adversely affects the physical wellbeing of participants demonstrated in bad mood and tiredness during the day.
Thus, it is recommended to express the importance of adequate sleep duration during health education sessions in primary healthcare centers and implement campaigns for the benefit of the general population regarding the adverse effects of short sleep.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Li X, Yu F, Guo A. Sleep deprivation specifically impairs short-term olfactory memory in drosophila. Sleep. 2009;32:1417–24. doi: 10.1093/sleep/32.11.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fernandez-Mendoza J, Vgontzas AN, Kritikou I, Calhoun SL, Liao D, Bixler EO. Natural history of excessive daytime sleepiness: Role of obesity, weight loss, depression, and sleep propensity. Sleep. 2015;38:351–60. doi: 10.5665/sleep.4488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Broussard JL, Kilkus JM, Delebecque F, Abraham V, Day A, Whitmore HR, et al. Elevated ghrelin predicts food intake during experimental sleep restriction. Obesity (Silver Spring) 2016;24:132–8. doi: 10.1002/oby.21321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khanijow V, Prakash P, Emsellem HA, Borum ML, Doman DB. Sleep dysfunction and gastrointestinal diseases. Gastroenterol Hepatol (N Y) 2015;11:817–25. [PMC free article] [PubMed] [Google Scholar]
- 5.Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004;43:678–83. doi: 10.1016/j.jacc.2003.07.050. [DOI] [PubMed] [Google Scholar]
- 6.Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American academy of sleep medicine and sleep research society. Sleep. 2015;38:843–4. doi: 10.5665/sleep.4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ge B, Guo X. Short and long sleep durations are both associated with increased risk of stroke: A meta-analysis of observational studies. Int J Stroke. 2015;10:177–84. doi: 10.1111/ijs.12398. [DOI] [PubMed] [Google Scholar]
- 8.Ren H, Liu Z, Zhou X, Yuan G. Association of sleep duration with apolipoproteins and the apolipoprotein B/A1 ratio: The China health and nutrition survey. Nutr Metab (Lond) 2018;15:1. doi: 10.1186/s12986-017-0237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rizzi M, Barrella M, Kotzalidis GD, Bevilacqua M. Periodic limbic movement disorder during sleep as diabetes-related syndrome? A polysomnographic study. ISRN Endocrinol. 2011;2011:246157. doi: 10.5402/2011/246157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma S, Kavuru M. Sleep and metabolism: An overview. Int J Endocrinol. 2010;2010:270832. doi: 10.1155/2010/270832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Leeuwen WM, Lehto M, Karisola P, Lindholm H, Luukkonen R, Sallinen M, et al. Sleep restriction increases the risk of developing cardiovascular diseases by augmenting proinflammatory responses through IL-17 and CRP. PLoS One. 2009;4:e4589. doi: 10.1371/journal.pone.0004589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang W. Vol. 101. Beijing: Higher Education Press; 2012. Clinical Epidemiology-Basic Principles and Practical Applications. [Google Scholar]
- 13.Al-Hazzaa HM, Musaiger AO, Abahussain NA, Al-Sobayel HI, Qahwaji DM. Prevalence of short sleep duration and its association with obesity among adolescents 15- to 19-year olds: A cross-sectional study from three major cities in Saudi Arabia. Ann Thorac Med. 2012;7:133–9. doi: 10.4103/1817-1737.98845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of healthy sleep duration among Adults--United States 2014. MMWR Morb Mortal Wkly Rep. 2016;65:137–41. doi: 10.15585/mmwr.mm6506a1. [DOI] [PubMed] [Google Scholar]
- 15.Luckhaupt SE, Tak S, Calvert GM. The prevalence of short sleep duration by industry and occupation in the National health interview survey. Sleep. 2010;33:149–59. doi: 10.1093/sleep/33.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tuomilehto H, Peltonen M, Partinen M, Seppa J, Saaristo T, Korpi-Hyovalti E, et al. Sleep duration is associated with an increased risk for the prevalence of type 2 diabetes in middle-aged women-The FIN-D2D survey. Sleep Med. 2008;9:221–7. doi: 10.1016/j.sleep.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 17.Schubert CR, Cruickshanks KJ, Dalton DS, Klein BE, Klein R, Nondahl DM. Prevalence of sleep problems and quality of life in an older population. Sleep. 2002;25:889–93. [PubMed] [Google Scholar]
- 18.Li L, Wang YY, Wang SB, Li L, Lu L, Ng CH, et al. Sleep duration and sleep patterns in Chinese university students: A comprehensive meta-analysis. J Clin Sleep Med. 2017;13:1153–62. doi: 10.5664/jcsm.6760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yen CF, Ko CH, Yen JY, Cheng CP. The multidimensional correlates associated with short nocturnal sleep duration and subjective insomnia among Taiwanese adolescents. Sleep. 2008;31:1515–25. doi: 10.1093/sleep/31.11.1515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drake C, Roehrs T, Shambroom J, Roth T. Caffeine effects on sleep taken 0, 3, or 6 hours before going to bed. J Clin Sleep Med. 2013;9:1195–200. doi: 10.5664/jcsm.3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Mill JG, Hoogendijk WJ, Vogelzangs N, van Dyck R, Penninx BW. Insomnia and sleep duration in a large cohort of patients with major depressive disorder and anxiety disorders. J Clin Psychiatry. 2010;71:239–46. doi: 10.4088/JCP.09m05218gry. [DOI] [PubMed] [Google Scholar]
- 22.Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Basta M, et al. Insomnia with short sleep duration and mortality: The Penn state cohort. Sleep. 2010;33:1159–64. doi: 10.1093/sleep/33.9.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jensen ME, Gibson PG, Collins CE, Hilton JM, Latham-Smith F, Wood LG. Increased sleep latency and reduced sleep duration in children with asthma. Sleep Breath. 2013;17:281–7. doi: 10.1007/s11325-012-0687-1. [DOI] [PubMed] [Google Scholar]
- 24.Sabanayagam C, Shankar A. Sleep duration and hypercholesterolaemia: Results from the National health interview survey 2008. Sleep Med. 2012;13:145–50. doi: 10.1016/j.sleep.2011.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: A meta-analysis of prospective studies. Sleep Med. 2014;15:1456–62. doi: 10.1016/j.sleep.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 26.Lou P, Zhang P, Zhang L, Chen P, Chang G, Zhang N, et al. Effects of sleep duration and sleep quality on prevalence of type 2 diabetes mellitus: A 5-year follow-up study in China. Diabetes Res Clin Pract. 2015;109:178–84. doi: 10.1016/j.diabres.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 27.Tsai TC, Wu JS, Yang YC, Huang YH, Lu FH, Chang CJ. Long sleep duration associated with a higher risk of increased arterial stiffness in males. Sleep. 2014;37:1315–20. doi: 10.5665/sleep.3920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee CH, Sibley CG. Sleep duration and psychological well-being among New Zealanders. Sleep Health. 2019 doi: 10.1016/j.sleh.2019.06.008. Dpii: S2352-7218 (19) 30120-2. doi: 10.1016/j.sleh.2019.06.008. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 29.Lallukka T, Sivertsen B, Kronholm E, Bin YS, Øverland S, Glozier N. Association of sleep duration and sleep quality with the physical, social, and emotional functioning among Australian adults. Sleep Health. 2018;4:194–200. doi: 10.1016/j.sleh.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 30.Gupta P, Sagar R, Mehta M. Subjective sleep problems and sleep hygiene among adolescents having depression: A case-control study. Asian J Psychiatr. 2019;44:150–5. doi: 10.1016/j.ajp.2019.07.034. [DOI] [PubMed] [Google Scholar]
- 31.Syauqy A, Hsu CY, Rau HH, Kurniawan AL, Chao JC. Association of sleep duration and insomnia symptoms with components of metabolic syndrome and inflammation in middle-aged and older adults with metabolic syndrome in Taiwan. Nutrients. 2019;11 doi: 10.3390/nu11081848. pii: E1848. doi: 10.3390/nu1108184.8. [DOI] [PMC free article] [PubMed] [Google Scholar]


