Abstract
Introduction
Low and middle-income countries like South Africa are experiencing major increases in burden of non-communicable diseases such as diabetes and cardiovascular conditions. However, evidence-based interventions to address behavioural factors related to these diseases are lacking. Our study aims to adapt the CDC’s National Diabetes Prevention Program (DPP) within the context of an under-resourced urban community in Cape Town, South Africa.
Methods/analysis
The new intervention (Lifestyle Africa) consists of 17 weekly sessions delivered by trained community health workers (CHWs). In addition to educational and cultural adaptations of DPP content, the programme adds novel components of text messaging and CHW training in Motivational Interviewing. We will recruit overweight and obese participants (body mass index ≥25 kg/m2) who are members of 28 existing community health clubs served by CHWs. In a 2-year cluster randomised control trial, clubs will be randomly allocated to receive the intervention or usual care. After year 1, usual care participants will also receive the intervention and both groups will be followed for another year. The primary outcome analysis will compare percentage of baseline weight loss at year 1. Secondary outcomes will include diabetes and cardiovascular risk indicators (blood pressure, haemoglobin A1C, lipids), changes in self-reported medication use, diet (fat and fruit and vegetable intake), physical activity and health-related quality of life. We will also assess potential psychosocial mediators/moderators as well as cost-effectiveness of the programme.
Ethics/dissemination
Ethical approval was obtained from the University of Cape Town and Children’s Mercy. Results will be submitted for publication in peer-reviewed journals and training curricula will be disseminated to local stakeholders.
Trial registration number
Keywords: obesity, Diabetes Prevention Program, low and middle-income countries, community health workers
Strengths and limitations of this study.
Community-engaged development ensures the intervention fits the cultural context and existing models of care.
Broad participant inclusion criteria will help produce more relevant, generalisable findings.
Cluster-randomised design will lead to a rigorous evaluation of the intervention.
Biometric and biologic measures are rigorous outcome indicators.
Low-resource environment will make delivering the intervention reliably and with fidelity challenging.
Introduction
The WHO estimates that of the 56.4 million global deaths in 2015, almost 40 million (70%) were due to non-communicable diseases (NCDs).1 The leading causes were cardiovascular diseases (CVDs) with a substantial number also coming from diabetes mellitus (DM). Over three-quarters of deaths attributed to NCDs in 2015 occurred in low and middle-income countries, where the disproportionate burden of NCDs is expected to continue to increase.1 2
As a result of globalisation and economic advancement, countries like South Africa are experiencing an ‘epidemiological transition’ in which disease prevalence is shifting from primarily infectious disease and under-nutrition to primarily NCDs and over-nutrition.2 These trends have been attributed to rising incomes and urbanisation in low and middle-income countries, which lead to a shift from eating unrefined carbohydrates to a greater intake of fats, sweeteners, animal source foods, and highly-processed foods, sometimes referred to as a ‘nutrition transition’.3 4 The negative effects of this dietary change are compounded by reductions in physical activity associated with urban lifestyles.5 Contributing factors include the limited availability of affordable, healthy food in poorer areas, combined with the increased availability of fast foods and cheap snacks that are high in fats and sugar,6 sedentary employment,4 5 limited outdoor space, and high rates of street violence.7–9 Cultural beliefs and practices may also contribute. For example, obesity is less stigmatised, and even valued, in many African cultures because it is associated with dignity, wealth and being treated well by one’s husband, whereas weight loss is regarded as a source of stigma and a sign of disease, in particular HIV/AIDS.10
Although signs of epidemiological transition have been observed in many low and middle-income countries, studies suggest that the speed at which this transition appears to be occurring in South Africa is particularly striking.8 11–16 Fifty-four per cent of South African adults are overweight and 28.3% are obese—a statistic that has risen from 17.6% in 1996 and 22.9% in 2006.17 South African women have the highest prevalence of obesity in sub-Saharan Africa at 40%.18 Furthermore, hypertension affects 46% of women and 44% of men nationally.19
Considering the public health and economic impacts of NCDs, national and provincial health departments in South Africa have declared promotion of healthy lifestyles a public health priority.20 Despite the need for effective and affordable interventions for combating DM and CVD, there is a dearth of research devoted to developing and evaluating NCD interventions in low and middle-income settings, particularly in Africa. Globally, one of the most notable examples of effective interventions based on lifestyle change is the Diabetes Prevention Program (DPP), which the Centers for Disease Control has adopted and disseminated in the USA as the National DPP.21 Through 16 core sessions delivered by ‘lifestyle coaches’, the original DPP aimed for its participants to engage in at least 150 min of moderate physical activity per week and to reduce initial body weight by 7% over 6 months. Its original randomised control trial (RCT) among individuals with impaired glucose tolerance reported a 58% reduction in DM incidence.22 A more recent RCT examining long-term effects of a group-based version of the DPP among 5000 overweight and obese individuals with type 2 DM (the Look AHEAD trial) showed an average loss of 8.6% of initial body weight in the lifestyle intervention group (compared with 0.7% for controls) and 4.7% at the 4-year follow-up.23–25 In addition, there were significant improvements in glucose control as well as reductions in blood pressure, triglycerides, high-density lipoprotein cholesterol and medication use.
With evidence of its effectiveness among adults with pre-diabetes as well as adults with diabetes, the DPP has also been adapted for several real-world settings within the USA including YMCAs,26 27 African American churches,28 community hospitals,29 community healthcare facilities,30 as well as through online social networks and mobile phone platforms.31 Adaptations of the DPP designed to be delivered by lay community health workers (CHWs) have also been successful32 33—some achieving weight loss in the range of 6%–7%,27 33 comparable with the 8.6% observed in the original trial23 and consistent with recommended weight loss goals for diabetes risk reduction.34
Although the DPP has shown strong outcomes when adapted for community settings in the USA, adaptation has not yet been extended to low and middle-income settings. For example, the mode of delivery in the USA has been through trained health or allied health professionals with post-graduate training and backgrounds in nutrition or behaviour change.22 This is not feasible in most low-resource environments due to costs and/or the lack of trained public health professionals. Delivering services at medical facilities may also hinder attendance because of the time loss and cost of local travel. Furthermore, the content of sessions needs adaptation to be suitable for the prevailing literacy and numeracy levels of both providers and recipients of the programme and to take into account the unique food preferences, cooking and shopping patterns of the region. Cultural norms that affect food preferences or attitudes about body weight or weight loss, as well as environmental barriers that affect access to food or ability to exercise, need to be addressed. For example, many individuals in South Africa live in crowded informal (shack) settlements that may lack reliable electricity, space, access to affordable produce, cold storage of fresh food and places that are safe to exercise. In addition to barriers, there may be unique facilitators that can support intervention delivery in low and middle-income countries. For example, many countries currently provide community-based care using CHWs, offering opportunities to tap existing social support networks and a community-based health infrastructure.35 Also, cell phone use is high, offering the opportunity to deliver supportive text messages, which have been shown to enhance the effectiveness of behaviour change interventions.36 37
The purpose of our study is to use a community-engaged adaptation process to develop and test a new version of the DPP (‘Lifestyle Africa’) tailored to overweight and obese adults in low-income, urban areas of sub-Saharan Africa. The key adaptation is to design the programme for delivery by CHWs. In South Africa, CHWs are typically drawn from the local community and have similar levels of education as the target population. Evaluation of Lifestyle Africa is based on a community-based cluster RCT conducted in partnership with two non-governmental organisations (NGOs) that provide chronic disease care to individuals with DM and/or CVD using CHWs. CHWs are used to provide medication delivery and health monitoring to individuals who are members of ‘support groups’ or ‘health clubs’. Care is provided from approximately February through November each calendar year due to the year-end holiday season during which most community members travel to their rural homes for an extended period. CHWs and their associated support groups are randomised to receive Lifestyle Africa or to serve as a treatment-as-usual control. The primary outcome analysis will compare percentage weight loss from baseline to follow-up at the end of the year between Lifestyle Africa and usual care participants. Secondary outcomes are DM and cardiovascular risk indicators (blood pressure, haemoglobin A1C [HbA1C], lipids), changes in medication use, diet (fat, fruit and vegetable intake), physical activity and health-related quality of life (HRQOL).
Methods and analysis
Setting
This study is being conducted in the area of Khayelitsha, a fast-growing urban township of Cape Town, South Africa. Khayelitsha residents are 99% Black African and 97% Xhosa speaking.38 Poverty is extremely high, with 38% of individuals unemployed and 89% earning less than R6400 (approximately 475 USD) per month. More than half of the residents are rural to urban migrants and 64% of adults have not completed high school.38 There is a high prevalence of overweight and obesity39 and prevalence of DM among Black Africans is approximately 13%, having increased to more than 50% over 20 years.40
Patient and public involvement
Community partners
Project implementation is conducted in partnership with two well-established NGOs that use CHWs from the community to support the health of over 9,000 individuals in Khayelitsha and surrounding communities. Our intervention is delivered through adaptation of the NGO’s existing programme that use CHWs to provide health-related services to small community groups or ‘clubs’ of approximately 10–50 individuals who meet in homes or community facilities. CHWs provide such services as health monitoring, medication delivery, education, physical activity, meals, wellness programming and income generating activities. NGOs work collaboratively with local health clinics to both refer patients and receive referrals of patients many of whom have diabetes and CVD. CHWs meet regularly (varying by NGO and club from daily to monthly) with their designated groups. Many groups also function independently providing meals and social activities to members on a regular basis.
Involvement in study design
Our team’s preliminary work involved extensive formative research with club members, CHWs and community leaders to better understand cultural norms, barriers and facilitators surrounding physical activity, diet and body image.10 In partnership with CHWs, a training manual and pilot programme was developed, which demonstrated the feasibility of using health clubs to encourage walking.41 Additional pilot work included development and evaluation of three intervention sessions based on the DPP. Two pairs of CHWs were trained to deliver three DPP pilot sessions to participants, and both CHW and participant feedback were incorporated into the development of the complete programme. To develop the complete Lifestyle Africa programme for the present study, we formed two community advisory boards (CABs) in two Khayelitsha area neighbourhoods to guide the development of a culturally appropriate and sustainable programme. Members included CHWs, community residents with DM and/or CVD, local experts in DM and CVD, and community leaders capable of guiding and supporting dissemination (eg, a neighbourhood elder and a representative of the provincial Department of Health). The CABs provide input and assistance with all aspects of the project including naming the intervention programme, assisting with programme development, reviewing intervention content and materials, and providing input on programme logistics. Members attend quarterly meetings as well as participate in work groups focused on specific tasks (eg, adapting the DPP manual, reviewing or trying out suggested adaptations of the DPP, or reviewing text messages).
Trial design
This is a two-arm parallel group cluster RCT with balanced randomisation (1:1) and a cross-over of the control arm after the main outcome assessment (figure 1). CHWs mostly work individually or in pairs with a particular group, but in some cases CHWs work as trios or work with more than one group. For this reason, the unit of randomisation is CHW ‘team’ (individual, pair or trio). CHW teams randomised to intervention receive training and provide the intervention to their support groups. CHW teams randomised to control provide treatment as usual to their support groups. After approximately 1 year of intervention, control CHW teams are also trained in the intervention and their support groups are crossed over to the intervention arm. Participants in both arms are assessed at the end of the first and second year.
Figure 1.
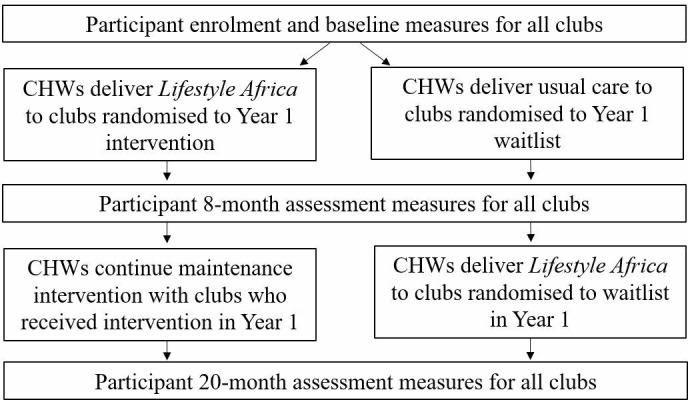
Flowchart of study procedures (repeated for each of two waves of participants). CHWs, community health workers.
Participants/recruitment
To recruit participants, two initial sessions were developed to introduce and explain the purpose and nature of the Lifestyle Africa programme. CHWs are trained to deliver these sessions, which follow a similar format to the main Lifestyle Africa sessions. At the introductory sessions, interested club members are invited to return for an eligibility screening and enrolment session. To serve our NGO partners and to be sensitive to community wishes, our goal is to invite all eligible members of 28 clubs (~18 members each) served by our partner NGOs to participate in the intervention and to enrol as many as feasible in the study. The eligibility criteria were therefore designed to be as inclusive of club members as possible. The inclusion criterion for support group members is being overweight or obese (body mass index [BMI] ≥25 kg/m2). Exclusion criteria are as follows: (1) having an unsafe level of blood pressure (>=160 [systolic] and/or >=100 mm [diastolic])42; (2) elevated blood sugar (HbA1C>11)42; (3) being pregnant, breast feeding or planning pregnancy within 2 years; (4) chronic use of oral steroid medication (which may affect weight loss); (5) not intending to stay in the group over the next 2 years; and/or had apparent intellectual disabilities that would prevent them from understanding the program.
Randomisation
Randomisation of support groups was conducted by the project statistician using a numbered list of the CHW teams and their associated groups. CHW teams are stratified within NGO. A computerised random number generator was used to create the allocation scheme. CHW groups have been randomised prior to enrolment of participants and launch of the intervention in order to know which CHWs need to be ready to deliver the intervention. It is therefore not feasible to blind CHWs or participants.
Interventions
Lifestyle Africa
Adaptation of the DPP
In developing Lifestyle Africa, we aimed to retain key elements from the CDC National DPP22 43 while making necessary cultural, educational and language adaptations relevant to the community. CDC’s National DPP consists of 16 ‘core’ sessions delivered over 6 months and 15 ‘post-core’ sessions focused on maintaining participants’ engagement in the programme. Participants are encouraged to lose 7% of body weight and exercise 150 min/week. Central components of the programme include self-monitoring of caloric intake and physical activity along with other social-cognitive and problem-solving theory elements.43
The primary adaptation was to eliminate the need for a high-level health professional (such a nutritionist or dietitian) to deliver the core sessions of the programme by providing session content on video (Katula et al 44, 2011). With expert content provided via video, the role of CHWs is to show the video, serve as group facilitators and ensure engagement with the video material. Videos were developed in Xhosa and use a presenter/narrator in conjunction with photographs and animation. Frequent pauses are built into the video session during which CHWs prompt participants with interactive questions and activities such as completing worksheets that reinforce and personalise video content. Activities are designed to minimise writing and allow for participants to engage orally if needed (eg, through discussion with a partner). Participants receive a programme book in Xhosa (or English if preferred) with educationally and culturally adapted handouts and forms needed for each session (eg, physical activity tracking sheets, goal setting forms). The visual elements of the video were designed to be culturally sensitive, for example, by depicting the individuals and scenes representative of the target community. To aid CHWs, each video has an accompanying session guide that provides step-by-step guidance on materials, procedures and the verbal prompts and questions needed to facilitate the session. To avoid excessive session length, the Lifestyle Africa programme consists of 17 rather than 16 core sessions.
Other key adaptations included those made because, unlike the original DPP, participants in Lifestyle Africa are not actively seeking treatment in the form of lifestyle behaviour change. Therefore, in addition to the 17 core sessions, we created two additional ‘recruitment sessions’ that follow the same format (ie, video delivered with pauses for discussion) to provide information on the rationale for participating in a diet and exercise programme. To account for participants’ levels of health literacy and numeracy, we expanded educational content (eg, explained the physiology of diabetes and CVD; explained the meaning of a kilojoule), simplified explanations, reduced calculations and ‘chunked’ information by interspersing it with discussion and related activities. We also bolstered motivational aspects of the DPP through the addition of elements of Motivational Interviewing, a method of counselling designed to strengthen motivation by fostering participant’s own reasons for change (eg, exploring personal values, asking participants to express their own reasons for change). According to Motivational Interviewing principles, the counsellor’s style or manner of counselling is also important (eg, person-centred and autonomy supportive rather than directive or persuasive; use of reflective listening rather and open questions rather than closed questions and confrontation). For this reason, a Motivational Interviewing and group facilitation skills training curriculum was also developed for CHWs to provide the skills necessary for delivering the sessions in a Motivational Interviewing consistent manner.45
A final adaptation capitalises on the widespread use of cell phones in the developing world and increasing evidence of the potential benefit of text messaging to help promote behaviour change.37 A empirically based text message system was developed in which participants are provided with two messages per day (morning and lunch time) to provide reminders, foster motivation and self-efficacy, affirm ongoing efforts and help with implementation planning (ie, behaviour change tips). The same messages are delivered to all participants, but weekly message content refers to each of the core sessions and is timed to match the participant’s session progress.
In addition to the video-based core sessions, 12 post-core sessions were developed. These are reduced in length but follow the same format (weigh-in, review and discussion of progress toward goal(s) from the prior session, delivery and discussion of new content, goal setting for the next session). New content is brief and delivered by the CHW using scripted language and straightforward handouts.
CHW training
CHWs working for our partner NGOs are not required to have any specific educational background but must have basic reading, writing and arithmetic skills sufficient to maintain attendance registers, medication logs and assess and record weight, height, etc. CHWs also have received basic training as part of their employment as CHWs (eg, in home-based care, chronic disease management and wellness). Training for Lifestyle Africa facilitators consists of 5.5 days of didactic training and 8 weekly half day sessions of experiential training as mock Lifestyle Africa participants conducted in Xhosa by local research team members. Didactic training includes basic training in diabetes and diabetes management, behaviour change principles, Motivational Interviewing and group facilitation. CHWs are also trained in use of the video projectors and logistical and study-related safety procedures. Content of motivational interview training was also adapted to limit jargon and to adapt concepts and experiential learning activities to CHW cultural values, language and educational level. For example, ‘Motivational Interviewing Spirit’ was distilled as ‘What is effective counselling?’ and focused on the need to listen and reflect before giving advice. Experiential training involved CHWs discussing their own experiences with making behaviour change. ‘Evocation and eliciting change talk’ was described in terms of building ‘motivation’ or ‘a strong why’. Experiential training involved exploring goals and values related to behaviour change. Content was adapted to be culturally relevant (eg, use of values such as ‘at peace with ancestors’). With regard to core skills in Motivational Interviewing, training and practice emphasised the use of open-ended questions and reflections.
CHWs reviewed and practised key activities after each session (eg, conduct weigh-in, conduct opening facilitation, provide feedback on food logs) during their training. In subsequent mock sessions (where these activities were repeated), they were asked on a rotational basis to act as facilitators (eg, lead the opening facilitation, facilitate goal-setting and action planning). A checklist was used to confirm all CHWs had satisfactorily conducted all key elements of the programme.
Delivery
To avoid disruption of the study during the widely-observed year-end holiday season, enrolment takes place in February and March following the break and intervention begins immediately after each club is enrolled. Control group clubs begin the intervention one year after the intervention arm begins. CHWs are asked to deliver the programme weekly (or biweekly if needed to fit the schedule of the group) but adjustments are made to allow for days when club members do not meet (eg, on days when many members collect pension payments or days of neighbourhood disruptions due to protests). Session attendance, weight and activity minutes are tracked by CHWs using standardised forms. After clubs complete the 17 core sessions, they continue with monthly sessions until the final assessment.
Fidelity monitoring
Research staff will observe at least the first 10 sessions for each CHW team and taper observations over time to at least one session every 5–8 weeks. Checklists are used to verify adherence to key session protocol elements (eg, completed weigh-in, followed verbal prompts, used projector correctly). Adherence to Motivational Interviewing principles and group facilitation behaviours is evaluated using rating scales (poor/never to excellent/always) adapted from the OnePass measure for Motivational Interviewing competence.46
Usual care (wait list)
For clubs randomised to usual care, CHWs continue to lead clubs in their usual activities (eg, approximately monthly monitoring of weight, blood pressure and blood glucose, delivery of medication). Although usual care may include education and health monitoring, there is no systematic, structured means by which lifestyle change is facilitated on an ongoing basis.
Data collection
Clubs are enrolled in two waves separated by 12 months. Each wave follows the same procedure for enrolment and assessment (see figure 1). Recruitment and enrolment of each wave take approximately 2 months over February and March of the calendar year. Enrolment for wave 1 began in February of 2018. The baseline assessment is conducted at enrolment. Follow-up assessments occur at the end of the enrolment year (approximately 8 months after enrolment) and the end of the second year (approximately 20 months after enrolment). Although the goal was to conduct assessments 12 and 24 months after enrolment, the timing of the enrolment and follow-up assessments had to be adjusted to avoid the holiday season break when most participants leave their neighbourhoods to return to their rural homes. To minimise attrition and interference in programme participation due to holiday travel, we therefore enrol participants and begin the programme as early as possible in the calendar year (immediately after participants return from their holiday break) and conduct our year 1 follow-up assessment as late as possible in the calendar year (just before participants leave for their holiday break). For similar reasons, the year 2 assessment is conducted 12 months after the year 1 assessment, just before participants leave for their holiday break.
The follow-up assessment at the end of year 1 is the main outcome time point. The follow-up assessment at the end of year 2 is used to evaluate long-term outcomes for the intervention arm as well as the effects of the control arm receiving the intervention. Consistent with local norms, participants receive a R150 (approximately $12USD) gift voucher for completing each assessment.
Assessments are conducted by study staff who travel to club sites or nearby suitable locations. At enrolment, club members complete informed consent, eligibility screening and baseline assessment. All participants are assessed on demographics, eligibility criteria and key outcome measures (ie, BMI, blood pressure and HbA1C). At the end of assessments, study staff give each participant a feedback form with their biometric data and explain their results. Due to resource limitations and logistics, only a randomly selected subsample of 12 participants per club complete the lipids and self-report survey assessments described below. All survey measures were translated to Xhosa and back-translated to English. During this process, we applied some minor cultural adaptations to increase relevance and comprehensibility of certain items and also harmonised some response scales across instruments to reduce complexity for respondents. All data are collected by trained Xhosa-speaking interviewers using tablets and the REDCap data management system.47
Measures
The primary outcome will be percentage of weight lost between baseline and the first follow-up assessment. Weight is measured to the half kilogram with a standard electronic scale. Participants are asked to wear light clothing and to fast the morning of enrolment. They are asked to remove footwear, heavy clothing/accessories prior before being weighed. Height is measured in order to calculate BMI to determine eligibility. Height is measured to the nearest millimetre with the participant standing straight against a standard stadiometer. BMI is calculated as weight in kilograms divided by the square of height in metres.
Blood pressure is assessed by staff with calibrated portable automated instruments (Omrons HBP1300), averaging two or three independent measurements according to American Heart Association Council on High Blood Pressure Research Methods.48 Non-fasting HbA1C, triglycerides and low-density lipoprotein cholesterol are measured via automated assay from a capillary sample using an Afinion AS100 Analyzer.49 Medication use is assessed by asking participants to bring all their medications to the enrolment session. Interviewers recorded the medication name and dose including use of HIV antiretroviral medications.
Demographic measures are assessed via participant survey and include age, gender, education level, income level and housing type. Dietary intake focuses on intake of whole grains, fruits and vegetables, fibre and sugar, measured with an adaptation of the National Health and Nutrition Evaluation Survey (NHANES) Dietary Screener Questionnaire.50 Physical activity is measured using the International Physical Activity Questionnaire-Short Form,51 and HRQOL is measured with the Veterans RAND 12-item Health Survey.52 53
Data analysis
Power analysis
Power analyses were conducted using the Optimal Design software for cluster-randomised trials with person-level outcomes. Prior studies of lifestyle interventions have indicated that the intra-class correlation coefficient (ICC) of the main outcome (per cent weight loss) will likely be small (eg, 0.01). Therefore, values of 0.01 and 0.05 were considered in the power analysis for conservative estimation. Because of the community-based nature of the trial, the study committed to enrol as many eligible and interested club members as possible. The power analysis was therefore used to determine the adequacy of the anticipated sample size. At the time of conducting our power analysis, we had one NGO partner and anticipated a sample of 54 clusters averaging approximately 10 participants each for a total N of 540. However, government changes in NGO-designated areas of responsibility and withdrawal from participation in the trial of one branch of our NGO partner changed our plans. After recruiting a second NGO partner, we anticipate 28 total clusters averaging 18–19 participants for a total N of 518. In order to allow for up to 25% attrition, cluster sizes of 19 and 15 were included in the power analysis. Assuming an ICC of 0.01, we projected that we would have 0.80 power to detect even small effect sizes of 0.28 and 0.31 with cluster sample sizes of 19 and 15, respectively. If we conservatively assume an ICC of 0.05, we projected we would still have 0.80 power to detect effect sizes of 0.35 and 0.37 with sample sizes of 19 and 15 per cluster. Using the pooled standard deviation from Look AHEAD (5.8), the largest trial of overweight/obese type 2 diabetic patients24 and a conservative estimate of a 3.15% weight loss for the treatment group and a 1% loss for the control group, a conservative estimated effect size for weight loss in the current study would be 0.37. This estimate is larger than the effect we will be able to detect with 0.80 power as we will be able to detect a per cent weight loss difference of 1.6%–1.7% between groups.
Planned analytic strategy
To accommodate the cluster randomised design, all analyses will be conducted with a multilevel modelling framework using SAS PROC MIXED (version 9.4). In this design, participants (level 1 units) will be nested within CHW pairs (level 2 units). Primary analyses will use an intention-to-treat strategy. Exploratory analyses will also examine low versus high dose (ie, sessions attended) effects. Unconditional models will be examined with each dependent variable to determine the amount of between-cluster and within-cluster variance. Some questions involve comparison of effects between conditions and some involve change within a condition.
Preliminary analyses will examine baseline equivalence across the two treatment conditions on variables that may impact outcome (eg, medication use) to identify covariates for the main analyses. If groups differ at baseline, baseline values will be added to the models as covariates. To address the primary research question regarding differences in per cent weight loss at the end of year 1, per cent weight loss from baseline to the end of year 1 will be the dependent variable in the multilevel model described above. The significance of the fixed effect for treatment group will indicate if there are differences in overall outcomes across groups. Anticipated effects are directional, in that Lifestyle Africa participants should respond better than control participants. Similar models will be evaluated for each of the secondary outcomes. Relevant covariates will be added to the models as appropriate (eg, use of diabetic medications for weight loss).
To determine if the Lifestyle Africa intervention group maintains its response to the intervention over the second year, scores at the year 1 assessment will be compared with those at the year 2 assessment. Random intercepts for health club and participant nested within health club will be included in the model. The significance of the fixed effect for time will indicate whether or not participants were able to maintain their response. This type of maintenance model will be evaluated for each of the outcomes of interest individually. Similar models will be used to examine intervention response within each of the study arms to determine if intervention effectiveness is replicated in the control group. If there are no differences between groups in the assessments taken just prior to participating in the Lifestyle Africa intervention, we will combine the groups and examine potential predictors of treatment effectiveness such as fidelity at level 2 and attendance at level 1.
Monitoring
A Data Safety Monitoring Board (DSMB) oversees the study and approved the stopping rules. The DSMB operates independently from the study investigators and the funder and comprises members based in the USA and South Africa and includes a psychologist, a physician, a doctor of public health and a statistician with expertise relevant to the trial. Details of the DSMB operating procedures are described in the DSMB charter. The DSMB may require termination (stopping rules) or modification of the study: (1) for any perceived safety concern including concerns related to adverse events or (2) because of severe failure to recruit or retain participants. There is no interim analysis or related stopping rule because the intervention involves minimal risk to participants and even in the absence of indications of weight loss, the intervention may yield other educational or psychological benefits. In addition, stopping for reasons other than safety could be negatively perceived by community partners, CHWs and club members. As part of usual care, CHWs and supervising nurses monitor the health of participants and refer patients to their physician, or local health clinic, or emergency service as needed. Study staff continuously monitor unanticipated problems or serious adverse events, which can be identified by CHWs, NGO staff, participants, participants’ families, participants’ physicians or other health professionals. Events are investigated, documented and reported to the principal investigators who report to the DSMB in accord with their regulations and to the Institutional Review Board (IRB) and the funder if appropriate.
Ethics and dissemination
Any amendments are approved by the IRB. Protocol modifications are communicated to study staff during regular meetings and, when relevant, to CHWs and participants through personal outreach and through regular meetings with NGO partners. Written informed consent is collected from all participants prior to eligibility screening and enrolment. Multiple protections for participant confidentiality are in place. Participant identifiers (name and contact information) are marked as an identifier in REDCap and are then censored when the database is downloaded for analysis. Only trained study staff have access to REDCap databases during data collection. All identifying information will be removed with the deletion of the REDCap project at the end of the study. Consent forms and signature logs for reimbursements will be secured in a locked file cabinet within a locked office on a secured floor.
A full data package will be maintained by the investigators for at least 7 years after data collection is complete. Third-party access to the full data package will be addressed by the investigators on a case-by-case basis. Results will be disseminated through publication in peer-reviewed journals and conference presentations. Lifestyle Africa curricula will be made available to local stakeholders such as Universities and the Department of Health. Study progress and findings will also be updated on clinicaltrails.gov.
Discussion
The growing burden of NCDs in low and middle-income countries presents a critical need for evidence-based interventions that address behavioural contributors to the prevention and management of CVD and DM. Our study aims to adapt one of the strongest existing evidence-based lifestyle behaviour change interventions to the context of low-income, under-resourced urban areas of sub-Saharan Africa and rigorously assesses its impact in a cluster RCT. Results will inform both the feasibility and the effectiveness of an intervention delivery model that uses CHWs as facilitators, video as the primary medium for delivering content and enhancement of the DPP with Motivational Interviewing principles and a text message system. This will be an important addition to similar efforts that have targeted more educated and resourced populations in India.54
Successful outcomes will hinge on both successful programme delivery as well as participant engagement and retention. The main outcomes will therefore need to be interpreted in the context of key aspects of study implementation including the success of training CHWs, the reliability and fidelity with which sessions are delivered and the engagement of participants. On completion of the study, a process evaluation is planned to enhance understanding of the outcomes by assessing CHW and participant perspectives on the strengths and weaknesses of the programme. Through training and technical support, the project also aims to build capacity in partner NGOs to continue the programme after the study has been completed.
Strengths of the study include its community-engaged development process that has led to an intervention design that fits with the existing models of care of our partner NGOs and may be transferable to programme aimed at other NCDs. The study’s pragmatic design, including broad inclusion criteria, should also lead to findings that are relevant and generalisable to many communities in low and middle-income countries. Although the study is pragmatic and the result of a community-engaged process, it uses a rigorous cluster randomised design with objective measurements of key biometric and biologic outcomes related to diabetes and CVD. Chief among the challenges of the trial will be to achieve adequate reliability and fidelity in the delivery of the intervention in the context of an impoverished environment where resources are limited, residents are taxed trying to meet their basic needs and social disruptions (eg, strikes, protests, crime) are frequent. Limitations include low precision of measures like dietary and physical activity recalls as well as limitations of measure breadth due to low literacy.
Regardless of the efficacy findings of the study, results should provide an important first step in understanding how lifestyle interventions such as the DPP might be disseminated in similar communities with few resources and low levels of education and literacy. Studies evaluating lifestyle behaviour change interventions in low and middle-income countries are vital for addressing the epidemic of diabetes and CVD.
Supplementary Material
Acknowledgments
The authors acknowledge the contributions made by our Community Advisory Board in designing this study.
Footnotes
Contributors: All authors made substantial contributions to the design of the study. DC led the study design, with other authors collaborating on the design of specific aspects (TP/LT/KR/MZV/EVL/NSL—DPP intervention content; EAH/KR/KG/TP/LT—measures and outcomes; JMS—text message component; KR/KG—Motivational Interviewing content). KF contributed to the research design and led the development of the statistical analysis plan. DC and EAH drafted the manuscript and all others contributed to revising it critically for important intellectual content. All authors reviewed and approved of the final version submitted for publication and agree to be accountable for all aspects of the work in ensuing that questions related to accuracy and integrity are appropriately investigated and resolved.
Funding: This work was supported by National Heart Lung and Blood Institute of the National Institutes of Health under award number R01HL126099.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Our study protocol has been approved by the IRBs at the University of Cape Town (the primary IRB) and Children’s Mercy Kansas City and the University of the Western Cape.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
References
- 1. World Health Organization Global health estimates 2015: deaths by cause, age, sex, by country and by region. Geneva: World Health Organization, 2016. http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html [Google Scholar]
- 2. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006;3:e442–30. 10.1371/journal.pmed.0030442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Drewnowski A, Popkin BM. The nutrition transition: new trends in the global diet. Nutr Rev 1997;55:31–43. 10.1111/j.1753-4887.1997.tb01593.x [DOI] [PubMed] [Google Scholar]
- 4. Popkin BM. The nutrition transition in the developing world. Dev Policy Rev 2003;21:581–97. 10.1111/j.1467-8659.2003.00225.x [DOI] [Google Scholar]
- 5. Kruger HS, Venter CS, Vorster HH. Physical inactivity as a risk factor for cardiovascular disease in communities undergoing rural to urban transition: the THUSA study. Cardiovasc J South Africa 2003;14:16–23. [PubMed] [Google Scholar]
- 6. Beaglehole R, Yach D. Globalisation and the prevention and control of non-communicable disease: the neglected chronic diseases of adults. The Lancet 2003;362:903–8. 10.1016/S0140-6736(03)14335-8 [DOI] [PubMed] [Google Scholar]
- 7. Bradley HA, Puoane T. Prevention of hypertension and diabetes in an urban setting in South Africa: participatory action research with community health workers. Ethn Dis 2007;17:49–54. [PubMed] [Google Scholar]
- 8. Bourne LT, Lambert EV, Steyn K. Where does the black population of South Africa stand on the nutrition transition? Public Health Nutr 2002;5:157–62. 10.1079/PHN2001288 [DOI] [PubMed] [Google Scholar]
- 9. Friel S, Chopra M, Satcher D. Unequal weight: equity oriented policy responses to the global obesity epidemic. BMJ 2007;335:1241–3. 10.1136/bmj.39377.622882.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Puoane T, Bradley H, Hughes G. Community intervention for the emerging epidemic of non-communicable diseases. South Afr J Clin Nutr 2006;19:56–62. 10.1080/16070658.2006.11734094 [DOI] [Google Scholar]
- 11. Reddy SP, Resnicow K, James S, et al. Underweight, overweight and obesity among South African adolescents: results of the 2002 national youth risk behaviour survey. Public Health Nutr 2009;12:203–7. 10.1017/S1368980008002656 [DOI] [PubMed] [Google Scholar]
- 12. Steyn K, Kazenellenbogen JM, Lombard CJ, et al. Urbanization and the risk for chronic diseases of lifestyle in the black population of the Cape Peninsula, South Africa. J Cardiovasc Risk 1997;4:135–42. 10.1097/00043798-199704000-00010 [DOI] [PubMed] [Google Scholar]
- 13. Sliwa K, Wilkinson D, Hansen C, et al. Spectrum of heart disease and risk factors in a black urban population in South Africa (the heart of Soweto study): a cohort study. The Lancet 2008;371:915–22. 10.1016/S0140-6736(08)60417-1 [DOI] [PubMed] [Google Scholar]
- 14. Steyn K, Sliwa K, Hawken S, et al. Risk factors associated with myocardial infarction in Africa: the INTERHEART Africa study. Circulation 2005;112:3554–61. [DOI] [PubMed] [Google Scholar]
- 15. Tibazarwa K, Ntyintyane L, Sliwa K, et al. A time bomb of cardiovascular risk factors in South Africa: Results from the Heart of Soweto Study “Heart Awareness Days”. Int J Cardiol 2009;132:233–9. 10.1016/j.ijcard.2007.11.067 [DOI] [PubMed] [Google Scholar]
- 16. Steyn NP, Bradshaw D, Norman R, et al. Dietary changes and the health transition in South Africa: implications for health policy. In: The double burden of malnutrition: Case Studies from six developing countries, 2006: 259–303. http://www.fao.org/docrep/009/a0442e/a0442e00.HTM [Google Scholar]
- 17. World Health Organization Prevalence of obesity among adults, BMI ≥ 30, age-standardized: estimates by country. Glob. Heal. Obs. Data Repos 2017. http://apps.who.int/gho/data/node.main.A900A?lang=en [Google Scholar]
- 18. Marie N, Flemming T, Robinson M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet 2013;384:766–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. National Department of Health (NDoH), Statistics South Africa (Stats SA), (SAMRC) SAMRC . South Africa demographic and health survey 2016: key indicators. Pretoria, South Africa, and Rockville, Maryland, USA, 2017. [Google Scholar]
- 20. Republic of South Africa department of health. strategy for the prevention and control of obesity in South Africa 2015-2020. Pretoria 2016. [Google Scholar]
- 21. DPP Research Group National diabetes prevention program. Available: http://www.cdc.gov/diabetes/prevention/
- 22. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pi-Sunyer X, Blackburn G, Brancati FL, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look ahead trial. Diabetes Care 2007;30:1374–83. 10.2337/dc07-0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wadden TA, West DS, Neiberg RH, et al. One-Year weight losses in the look ahead study: factors associated with success. Obesity 2009;17:713–22. 10.1038/oby.2008.637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wadden TA, Neiberg RH, Wing RR, et al. Four-Year weight losses in the look ahead study: factors associated with long-term success. Obesity 2011;19:1987–98. 10.1038/oby.2011.230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ackermann RT, Marrero DG. Adapting the diabetes prevention program lifestyle intervention for delivery in the community: the YMCA model. Diabetes Educ 2007;33:69–78. 10.1177/0145721706297743 [DOI] [PubMed] [Google Scholar]
- 27. Ackermann RT, Finch EA, Brizendine E, et al. Translating the diabetes prevention program into the community. The DEPLOY pilot study. Am J Prev Med 2008;35:357–63. 10.1016/j.amepre.2008.06.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Boltri JM, Davis-Smith YM, Seale JP, et al. Diabetes prevention in a faith-based setting: results of translational research. J Public Heal Manag Pract 2008;14:29–32. [DOI] [PubMed] [Google Scholar]
- 29. McTigue KM, Conroy MB, Bigi L, et al. Weight loss through living well: translating an effective lifestyle intervention into clinical practice. Diabetes Educ 2009;35:199–208. 10.1177/0145721709332815 [DOI] [PubMed] [Google Scholar]
- 30. Amundson HA, Butcher MK, Gohdes D, et al. Translating the diabetes prevention program into practice in the general community: findings from the montana cardiovascular disease and diabetes prevention program. Diabetes Educ 2009;35:209–23. [DOI] [PubMed] [Google Scholar]
- 31. Joiner KL, Nam S, Whittemore R. Lifestyle interventions based on the diabetes prevention program delivered via eHealth: a systematic review and meta-analysis. Prev Med 2017;100:194–207. 10.1016/j.ypmed.2017.04.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ali MK, Echouffo-Tcheugui JB, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the diabetes prevention program? Health Aff 2012;31:67–75. 10.1377/hlthaff.2011.1009 [DOI] [PubMed] [Google Scholar]
- 33. Ruggiero L, Castillo A, Quinn L, et al. Translation of the diabetes prevention program's lifestyle intervention: role of community health workers. Curr Diab Rep 2012;12:127–37. 10.1007/s11892-012-0254-y [DOI] [PubMed] [Google Scholar]
- 34. Klein S, Sheard NF, Pi-Sunyer X, et al. Weight management through lifestyle modification for the prevention and management of type 2 diabetes: rationale and strategies. A statement of the American diabetes association, the North American association for the study of obesity, and the American Society for clinical nutrition. Am J Clin Nutr 2004;80:257–63. 10.1093/ajcn/80.2.257 [DOI] [PubMed] [Google Scholar]
- 35. Bangdiwala SI, Fonn S, Okoye O, et al. Workforce resources for health in developing countries. Public Health Rev 2010;32:296–318. 10.1007/BF03391604 [DOI] [Google Scholar]
- 36. Lester RT, Gelmon L, Plummer FA. Cell phones: tightening the communication gap in resource-limited antiretroviral programmes? AIDS 2006;20:2242–4. 10.1097/QAD.0b013e3280108508 [DOI] [PubMed] [Google Scholar]
- 37. Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 2010;32:56–69. 10.1093/epirev/mxq004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Statistics South Africa (Stats SA) Census 2011 statistical release. Pretoria 2012.
- 39. Malhotra R, Hoyo C, Østbye T, et al. Determinants of obesity in an urban township of South Africa. South Afr J Clin Nutr 2008;21:315–20. 10.1080/16070658.2008.11734173 [DOI] [Google Scholar]
- 40. Peer N, Steyn K, Lombard C, et al. Rising diabetes prevalence among urban-dwelling black South Africans. PLoS One 2012;7:e43336 10.1371/journal.pone.0043336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Puoane TR, Tsolekile L, Igumbor EU, et al. Experiences in developing and implementing health clubs to reduce hypertension risk among adults in a South African population in transition. Int J Hypertens 2012;2012:1–6. 10.1155/2012/913960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bray G, Gregg E, Haffner S, et al. Baseline characteristics of the randomised cohort from the look ahead (action for health in diabetes) study. Diab Vasc Dis Res 2006;3:202–15. 10.3132/dvdr.2006.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Venditti EM, Kramer MK. Necessary components for lifestyle modification interventions to reduce diabetes risk. Curr Diab Rep 2012;12:138–46. 10.1007/s11892-012-0256-9 [DOI] [PubMed] [Google Scholar]
- 44. Katula JA, Vitolins MZ, Rosenberger EL, et al. One-Year results of a community-based translation of the diabetes prevention program: Healthy-Living partnerships to prevent diabetes (help PD) project. Diabetes Care 2011;34:1451–7. 10.2337/dc10-2115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Miller WR, Rollnick S. Motivational interviewing: helping people change. 3rd edn, 2012. [Google Scholar]
- 46. McMaster F, Resnicow K. Validation of the one pass measure for motivational interviewing competence. Patient Educ Couns 2015;98:499–505. 10.1016/j.pec.2014.12.014 [DOI] [PubMed] [Google Scholar]
- 47. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of professional and public education of the American heart association Council on high blood pressure research. Circulation 2005;111:697–716. 10.1161/01.CIR.0000154900.76284.F6 [DOI] [PubMed] [Google Scholar]
- 49. Arabadjief M, Nichols JH. Evaluation of the afinion AS100 point-of-care analyzer for hemoglobin A1c. Point Care 2009;8:11–15. 10.1097/POC.0b013e3181971cef [DOI] [Google Scholar]
- 50. Thompson FE, Midthune D, Kahle L, et al. Development and evaluation of the National cancer Institute's dietary screener questionnaire scoring algorithms. J Nutr 2017;147:1226–33. 10.3945/jn.116.246058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381–95. 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 52. Jones D, Kazis L, Lee A, et al. Health status assessments using the Veterans SF-12 and SF-36: methods for evaluating outcomes in the Veterans health administration. J Ambul Care Manage 2001;24:68–86. 10.1097/00004479-200107000-00011 [DOI] [PubMed] [Google Scholar]
- 53. Selim AJ, Rogers W, Fleishman JA, et al. Updated U.S. population standard for the Veterans Rand 12-Item health survey (VR-12). Qual Life Res 2009;18:43–52. 10.1007/s11136-008-9418-2 [DOI] [PubMed] [Google Scholar]
- 54. Sathish T, Williams ED, Pasricha N, et al. Cluster randomised controlled trial of a peer-led lifestyle intervention program: study protocol for the Kerala diabetes prevention program. BMC Public Health 2013;13 10.1186/1471-2458-13-1035 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


