Abstract
Anxiety is a major mental disorder in later life that impacts on activities of daily living and quality of life for adults living with dementia in nursing homes. The aim of this article was to systematically review nonpharmacological interventions for older adults living in nursing homes who experience comorbid anxiety and dementia.
Method
A systematic literature search was conducted across key databases (Cinahl, ASSIA, Cochrane reviews and trials, psycARTICLES, psycINFO, and PubMed) to identify studies measuring anxiety as an outcome for an intervention for older adults living with dementia in nursing homes, up to December 31, 2017.
Results
The search yielded a total of 1,925 articles with 45 articles accessed for full article review. A total of 13 articles were included in this review following quality appraisal based on Cochrane methodology with six different anxiety measures used. The studies included were moderate to high-quality randomized control trials although heterogeneity precluded a combined meta-analysis.
Clinical implications
The most common interventions used to address anxiety in this population were music therapy and activity-based interventions although there was limited evidence for the efficacy of either intervention. Little is known about effective nonpharmacological treatment for anxiety for people living with dementia in nursing homes. Further research using consistent measurement tools and time points is required to identify effective interventions to improve the quality of life for people living with both dementia and anxiety in nursing homes.
Keywords: Dementia, Anxiety, Nursing homes, Systematic review, Nonpharmacological treatment
Anxiety is a common neuropsychiatric condition in later life, significantly reducing quality of life for adults living with dementia (Hoe, Cooper, & Livingston, 2013; Selwood, Thorgrimsen, & Orrell, 2005) and increasing the likelihood of placement in residential environments such as nursing homes (Gibbons et al., 2002; Gibbons, Teri, Logsdon, & McCurry, 2006). Due to the overlap of symptoms of anxiety with medical illness, medication side effects, and other mental health conditions, such as depression, anxiety can be difficult to assess accurately in later life (Beattie, Pachana, & Franklin, 2010). Both assessment and management of anxiety in later life, particularly if it is comorbid with other conditions, including dementia, are challenging (Beattie et al., 2010). For example, adults with dementia who experience anxiety as a comorbidity exhibit a high level of psychological distress (Voyer, Verreault, Cappeliez, Holmes, & Mengue, 2005) and may have more difficulty with activities of daily living than people with dementia alone (Wancata, Benda, Meise, & Windhaber, 2003). However, the side effects of medication given to people living with dementia and anxiety further decrease their function and quality of life with current best practice recommending psychotherapeutic interventions as the first line of treatment (Bannerjee, 2009). Psychological therapies have been found to be useful for treating depression for people with dementia, but they were not effective in studies where self-rated or carer-rated anxiety were also measured with no included studies located in nursing homes (Orgeta, Qazi, Spector, & Orrell, 2014).
Anxiety has a major impact on functioning in activities of daily living and behavioral sequelae when left untreated (Hoe, Hancock, Livingston, & Orrell, 2006; McCurry, Gibbons, Logsdon, & Teri, 2004; Starkstein, Jorge, Petracca, & Robinson, 2007). People with dementia already face challenges in everyday activities, and untreated anxiety may further reduce their function or lead to Behaviors and Psychological Symptoms of Dementia (BPSD) that challenge those providing care (McCurry et al., 2004). Understanding anxiety in older adults is problematic as many assessment tools still lack a robust evidence base with a reliance on self-report (Therrien & Hunsley, 2012, 2013). Self-report is not always possible when adults with dementia experience difficulty with expressive language, which means that proxy reporting or behavioral observation is often used and these methods have their limitations when assessing anxiety (Seignourel, Kunik, Snow, Wilson, & Stanley, 2008). Although the majority of people with dementia reside in the community, BPSD is often a key factor leading to institutionalization (Sorensen, Duberstein, Gill, & Pinquart, 2006) with people living with dementia accounting for nearly half the population in nursing homes (Alzheimers Society, 2014). Although anxiety is often included in global assessments of behavioral symptoms for adults with dementia, this may compound the difficulties of differentiation between anxiety, symptoms of dementia, and depression (Gibbons et al., 2006). Symptoms such as agitation could, in fact, be ascribed to depression, anxiety, and/or dementia, with nursing home staff often faced with a daunting task of assessing the probable driver of the behavior (Teri, Logsdon, Uomoto, & McCurry, 1997). For example, in one study up to 75% of adults with dementia and diagnosed with generalized anxiety disorder also met the criteria for depression (Starkstein et al., 2007). This demonstrates how the measurement of a range of psychiatric and behavioral issues is problematic in nursing homes, due to the fact that persons in such institutions have multiple medical and/or psychiatric comorbidities, and measurement tools are often not designed to test such populations (Pachana et al., 2010). This may be further complicated by prior experience of anxiety where the person with dementia entering into the nursing home may require additional support (Hess, Williams, & Meeks, 2012). However, staff are often not trained to assess psychiatric conditions such as anxiety, which may confound diagnosis. For example, nursing home staff tend to confuse agitated behaviors with anxiety when compared with self-report of anxiety as experienced by the person with dementia (Williams, Hess, & Meeks, 2012). Seignourel and colleagues (2008) examined anxiety assessment measurement tools used for adults with dementia. From 13 empirical studies, four measurement tools were included that assessed anxiety in adults living with dementia: two for general neuropsychiatric assessment Behave-AD (Auer, Monteiro, & Reisberg, 1996) and Neuropsychiatric Inventory (NPI) (Cummings et al., 1994) and two specifically for anxiety Rating Anxiety in Dementia (RAID) (Shankar, Walker, Frost, & Orrell, 1999) and Worry Scale (LaBarge, 1993). Although there was limited quality assessment, Seignourel and colleagues (2008) concluded that all measurement tools were found to have good reliability but inadequate or undocumented construct validity; with the RAID being the only tool that used multiple sources of information for people with dementia providing both self and carer reporting (Seignourel et al., 2008). If anxiety is to be identified and subsequently treated in this population, staff require access to reliable methods of assessment and appropriate nonpharmacological interventions that can support people with comorbid dementia and anxiety. Therefore, this review aimed to assess the effectiveness of nonpharmacological interventions used for people with dementia living in Nursing Homes who had comorbid anxiety using a valid and reliable measurement tool. We asked the following questions:
Are nonpharmacological interventions effective in reducing anxiety symptoms in older adults with comorbid dementia?
If so, which nonpharmacological interventions demonstrate the greatest effectiveness in reducing anxiety symptoms in older adults with comorbid dementia?
Method
A protocol was developed and published (Arendt, Brown Wilson, Pachana, Neville, & Scott, 2016). The electronic databases CINAHL, ASSIA, Cochrane reviews and trials, psycARTICLES, psycINFO, and PubMed were searched for published journal articles that included the following search terms combined with Boolean phrases and associated meMESH terms: Anxiety AND Dementia OR Alzheimers OR Cognitive Impairment AND Elderly OR Geriatr* OR Older Adults OR Seniors AND Nursing Homes OR CareHomes Or Residential Aged Care. The search included all articles published up to December 31, 2017. There was no date before which articles were excluded. Inclusion/exclusion criteria (Table 1) were applied to all articles.
Table 1.
Inclusion/Exclusion Criteria
| Inclusion | Exclusion |
|---|---|
| Older people with dementia Parkinson’s disease with dementia Residential aged care Assisted living Specialist dementia unit Psychotherapeutic intervention RCTs Use of a validated tool that measures anxiety |
People without dementia People with MCI Caregivers Other mental health issues Population-based studies Home care/primary care/memory clinic Inpatient or outpatient of a hospital Community-dwelling Drug intervention Individual case studies/case reports Prevalence studies Case–control studies RCT protocol Narrative reviews or systematic reviews Opinion pieces or commentary Global or subjective assessment of anxiety Cognitive assessment only |
Two members of the team (L. Arendt and C. Brown Wilson) reviewed all titles and abstracts independently with a third member (T. L. Scott) being available if an agreement was not reached. Articles that met the inclusion/exclusion criteria were retrieved for quality appraisal using the Cochrane Risk of Bias tool (Higgins, 2011). Members of the team working in pairs (N. A. Pachana, L. Arendt, T. L. Scott, C. C. Neville) appraised each article before data extraction and reached agreement on the quality, with a third assessor involved if there was disagreement (C. Brown Wilson). Data were then extracted systematically (C. Brown Wilson and M. Nguyen) and summarized in Table 2 (author, year, methods, sample, intervention, measurement tools used, fidelity, and outcomes).
Table 2.
Summary of Articles Included in This Review
| Reference | Methods | Participants | Intervention | Tools used | Fidelity | Outcomes |
|---|---|---|---|---|---|---|
| Cooke and colleagues (2010) | RCT—crossover with interactive reading group | 47 people with mild-moderate dementia from two nursing homes in Australia | Music therapy conducted by musician three times/week for 8 weeks with 5-week washout period before interactive reading group conducted by group reader | RAID | Standardized procedure manual; musician and group reader training provided; a practice music session in a facility not involved in the research and four random spot checks made by research team | No statistically significant effects found for anxiety. 11/47 participants had scores over 11 indicating anxiety. |
| Eggermont, Knol, Hol, Swaab, and Scherder (2009) | Cluster RCT with read aloud group as control | 66 people with dementia from 10 nursing homes in the Netherlands | Guided hand exercises conducted 30 min for 5 days per week for 6 weeks or a read aloud program followed by casual conversation for same time. Groups conducted by recreational therapist or trained Masters Psychology students. | The Dutch version of the subscale Anxiety from the Symptom Check List (SCL-90) | Instruction by Primary investigator. Recreational therapists or Masters Psychology students followed by instructional video. |
Mood domain was assessed combining anxiety and depression—no improvements found in intention to treat analysis. Medication use was controlled for. |
| Guetin and colleagues (2009) | Single center RCT with reading control | 30 people with mild-moderate dementia from one nursing home in France | Weekly sessions of receptive individual music using validated U technique using a computerized system based on person’s music preferences. therapy for 16 weeks with follow-up at 24 weeks. Interventionist not identified. | Hamilton Scale | Not discussed | All participants had anxiety with scores ranging between 12 and 25 and were on stable medication therapy. Significant improvements in Anxiety (p < .01) as primary outcome. |
| Husebo, Ballard, Fritze, Sandvik, and Aarsland (2014) | Cluster RCT | 352 people with moderate to severe dementia from 18 nursing homes in western Norway | Daily treatment for 8 weeks with follow up at 12 weeks of a stepwise protocol of treating pain compared with usual management. Interventionist not identified. | NPI-NH | Not discussed | High prevalence of anxiety in the group before intervention. No statistically significant effects found for anxiety (p = 0.125). |
| Hutson, Orrell, Dugmore, and Spector (2014) | RCT | 39 people with moderate to severe dementia from four nursing homes in the UK | 14 sessions of SONAS: multisensory stimulation using music lasting 45 min over 7- to 8-week period. Compared with usual care control. Intervention delivered by trained nursing home staff. | RAID | Standardized SONAS manual; care home staff trained in intervention; prearranged schedule of sessions agreed with researcher | Range of RAID scores at baseline: 0–21 (11 suggests anxiety). No statistically significant effects found for anxiety. |
| Kolanowski, Litaker, Buettner, Moeller, and Costa (2011) | RCT—double-blind | 128 people with mild to severe dementia from nine community-based nursing homes, Pennsylvania, United States | Activities adjusted to a functional level (FL) or personality style of interest (PSI) or FL +PSI provided up to 20 min twice daily for 3 weeks. Follow-up 1 week later. Compared with active control. Interventionists not specified. |
Philadelphia Geriatric Centre Affect Rating Scale | Treatment Fidelity plan with treatment fidelity checks on 10% of all interventions sessions with retraining if intervention not delivered according to protocol—one deviation noted | Anxiety improved during the intervention irrespective of which group the person was assigned to. One week after the intervention, anxiety improved in the PSI group. over baseline one week after the intervention. Anxiety as a secondary outcome. |
| Moyle and colleagues (2013) | RCT crossover with an interactive reading group (pilot) | 18 residents with mild to severe dementia in one nursing home in Australia | Companion robot: Paro Seal for 45 min three times a week for 5 weeks with 3-week washout period before interactive reading group. Activity therapist conducted both groups. | RAID | Protocol manual; training of the activity therapist by researchers | Small to moderate effects found for RAID with participants in PARO group exhibiting less anxiety symptoms confirmed on video analysis |
| Raglio and colleagues (2008) | RCT (pilot) | 59 significantly impaired people with dementia in three nursing homes in Italy | 30 Active music therapy sessions using instruments over 16 weeks with control as educational support or entertainment activities. Music therapists with 5 years training and experience of working with people with dementia. | NPI | Each music therapy session was video recorded and assessed using two observers using Music Therapy Coding Scheme | Anxiety symptoms significantly improved (p < .0001) as a secondary outcome |
| Raglio and colleagues (2015) | Multicentre three armed RCT | 120 people with moderate to severe dementia from nine institutions in Italy | 20 Active music therapy sessions with instruments for 30 min twice a week for 10 weeks and standard care or individualized listening to music sessions for the same duration and standard care compared with standard care alone. Music therapy and listening to music performed by specifically trained music therapist. | NPI | Four independent observers (music therapists with specific training and not involved in the process) assessed the music therapy sessions using the Music Therapy Checklist—Dementia. | NPI global score reduced significantly (p < .0001). Anxiety not reported individually. |
| Rodriguez-Mansilla and colleagues (2015) | Three armed RCT (pilot) | 120 people with mild-severe dementia | Comparison of ear acupressure, massage and no therapy over 3 months with 2 months follow-up. Ear acupressure undertaken by qualified therapist. Massage was undertaken by qualified physiotherapist 20 min on a daily basis. |
Campbell scale | All participants had tape placed over ear to blind acupressure intervention | Improvement in anxiety in both interventions arms (acupressure and massage therapy) was noted in last month of intervention [9.63 (5.00) with 95% CI: 8.02, 11.23]. It was not possible to distinguish between interventions. |
| Serrani Azcurra (2012) | Single blind, parallel groups RCT | 135 residents with mild impairment from two nursing homes (country not specified) | 24 bi-weekly sessions Reminiscence using life story approach more than 12 weeks compared with unstructured social contact for same period (one comparison group) and control (no intervention) group delivered by psychologists | RAID | Protocols for intervention; Specific training provided to three psychologists responsible for intervention, comparison and control groups; videotaped records were assessed by two experts using a process validation model; inter rater reliability high for measures. | No statistically significant effects found for anxiety. Some participants were taking psychotropic medication. |
| Sung, Lee, Li, and Watson (2012) | RCT | 55 people with mild to moderate dementia in a single facility in Taiwan | 30-min group music intervention using percussion instruments twice weekly for 6 weeks delivered by trained research assistants compared with usual care | RAID | Not discussed | Significantly lower anxiety score in intervention group (p < .004) |
| Wenborn and colleagues (2013) | Cluster RCT with matched pair design | 210 people across 16 facilities in London, UK | 16-week occupational therapy intervention through training and coaching care home staff | RAID | Training manual for delivery of education and coaching developed. Limited compliance. | No statistically significant effects found for anxiety |
The validity and reliability of the assessment tools used were assessed using Hunsley and Mash (2008) criteria. Hunsley and Mash (2008) developed criteria from empirical studies of anxiety in older adults and compared these criteria against a meta-analysis of the same measurement tools to determine the minimum evidence required to make the judgment for clinical and research use (Therrien & Hunsley, 2013). From this study, nine categories: norms, internal consistency, inter-rater reliability, test–retest reliability, content validity, construct validity, validity generalization, sensitivity to treatment change, and clinical utility were identified with four rating scales: less than adequate, adequate, good, and excellent. Using the guide produced by Hunsley and Mash (2008), each criteria was judged as either “adequate” when the instrument met a minimal level of scientific rigor with psychometric properties undertaken as part of tool development, “good” signaled that the instrument would mostly be seen as acquiring solid scientific support as it had been developed and used for similar populations, and “excellent” signaled that there was extensive, high quality supporting evidence with psychometric data being reported as part of the same study or over multiple studies with similar populations. When a criterion was left blank, it indicated that there was “less than adequate” information available. “Not applicable” indicated that the psychometric property under consideration was not relevant to the instrument. If there were disagreements about the rating, a third member of the team (C. C. Neville) was consulted.
Results
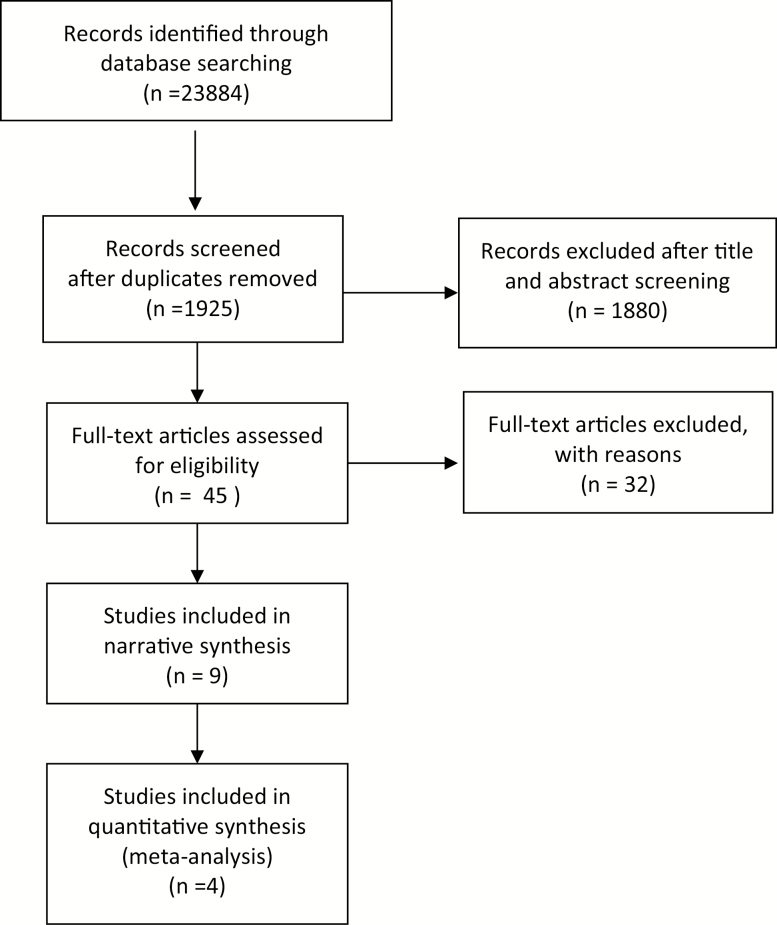
The search yielded a total of 1,925 articles with 45 articles retrieved for a full review following title/abstract check (Figure 1). Articles excluded at this point were those that: did not identify anxiety as a measurable outcome in the study; focused on cognitively intact residents in nursing homes; were not in English, did not use an assessment instrument, did not report an intervention or did not have a randomized control group. A total of 13 articles are included in this review (Table 2).
Figure 1.
Study selection flow diagram.
Quality Assessment
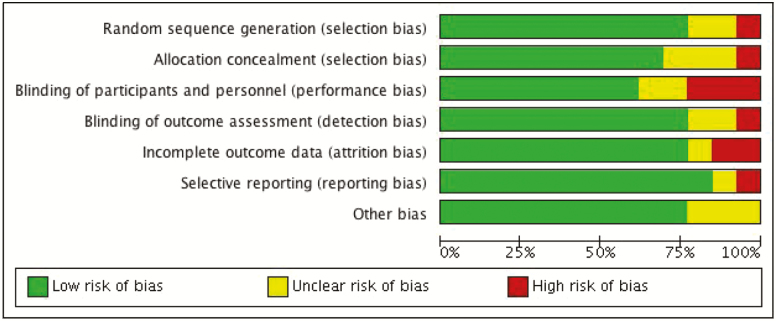
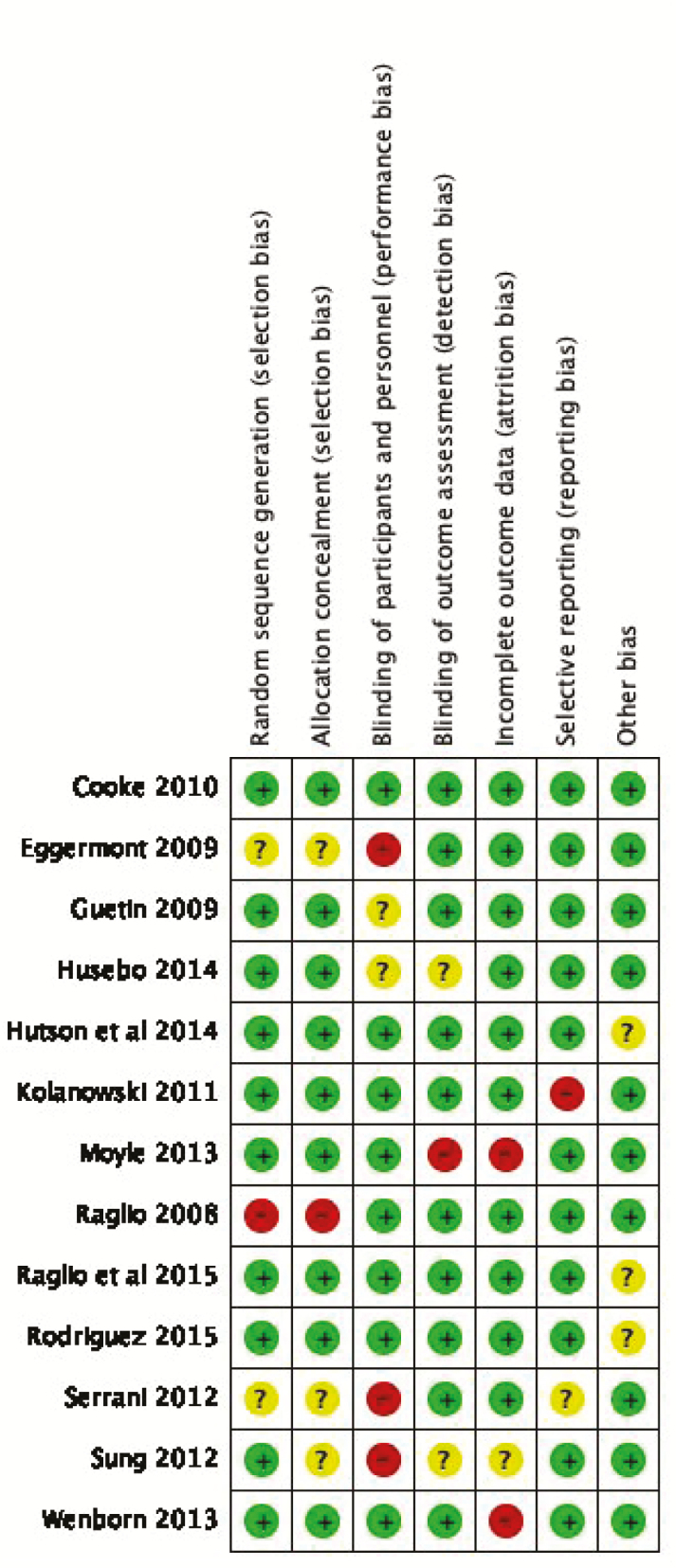
The 13 studies in this review were randomized controlled trials (RCTs) assessed for quality using CONSORT 2010 guidelines (Schulz, Altman, & Moher, 2010) and risk of bias (Higgins, 2011). All studies conformed to the consort guidelines for publication of RCTs. Risk of bias results are displayed in tabular format (Figure 2). We did not exclude any studies based on quality.
Figure 2.
Review authors’ judgments on the risk of bias per article.
Most studies described blinded allocation alongside an automated randomization process, suggesting a low risk of selection bias. It was unclear how Serrani Azcurra (2012) and Eggermont and colleagues (2009) undertook allocation or randomization. Sung and colleagues (2012) had a clear randomization process but did not report the allocation procedures, and Raglio and colleagues (2008) used nonstandardized randomization criteria with a high risk of selection bias. Three studies (Eggermont et al., 2009; Serrani Azcurra, 2012; Sung et al., 2012) were unable to blind participants to allocation to the intervention condition resulting in performance bias, but each of these studies did blind outcome assessors, reducing the risk of detection bias. Blinding of participants in Guetin and colleagues (2009) was unclear although outcome assessors were blinded. Blinding at both levels was unclear in Husebo and colleagues (2014), and there was no blinding of the outcome assessor in Moyle and colleagues (2013). There was incomplete outcome data for Moyle and colleagues (2013) and Wenborn and colleagues (2013) where data were not missing at random, resulting in attrition bias. Reporting bias was only identified in one article, where not all outcome measures were reported (Kolanowski et al., 2011). Cooke, Moyle, Shum, Harrison, and Murfield (2010), Hutson, Orrell, Dugmore, and Spector (2014), Raglio and colleagues (2015) and Rodríguez-Mansilla and colleagues (2015), had no risk of bias for each of the reported items. Overall there was a low—moderate risk of bias across studies resulting in the judgment that the RCTs reported in this review were of moderate quality (Figure 3).
Figure 3.
Risk of bias summary.
Assessment Tools
Not all articles included information on the psychometric properties of the instruments used. Three articles used data reported elsewhere (Husebo et al., 2014; Hutson et al., 2014; Sung et al., 2012) with only three articles reporting reliability and validity coefficient from data analyzed in the article (Eggermont et al., 2009; Kolanowski et al., 2007; Cooke et al., 2010). Only Cooke and colleagues (2010) reported psychometric data of the RAID in the population they were testing.
The Rating Anxiety in Dementia (RAID) (Shankar et al., 1999) was the most used instrument in this review, used in 6 out of 13 studies, with the Neuropsychiatric Inventory NPI or NPI—Nursing Home (Cummings et al., 1994) used in three studies. This is not surprising given that the RAID was specifically designed for measuring anxiety symptoms in adults with dementia. The RAID has been shown to possess very good psychometric properties (Seignourel et al., 2008) with scale items showing fair to excellent inter-rater and test–retest reliability, satisfactory internal consistency (alpha = .83), and significant correlations with other anxiety scales (Shankar et al., 1999). The six studies using the RAID reported adequate to good validity generalization, adequate treatment sensitivity, and excellent clinical utility. Therefore, this review supports previous recommendations that the RAID is a valid instrument for assessing anxiety (Sansoni, 2007; Seignourel et al. (2008).
Interventions for Managing Anxiety
Thirteen articles in this review considered six different interventions where anxiety was a measurable outcome for people with dementia living in nursing homes. The most common interventions were music therapy (Cooke et al., 2010; Guetin et al., 2009; Hutson et al., 2014; Raglio et al., 2008; Raglio et al., 2015; Sung et al., 2012) and activity therapy (Kolanowski et al., 2011; Wenborn et al., 2013) with more diverse interventions including acupressure (Rodríguez-Mansilla et al., 2015), companion robots (Moyle et al., 2013), exercise (Eggermont et al., 2009), and pain control (Husebo et al., 2014).
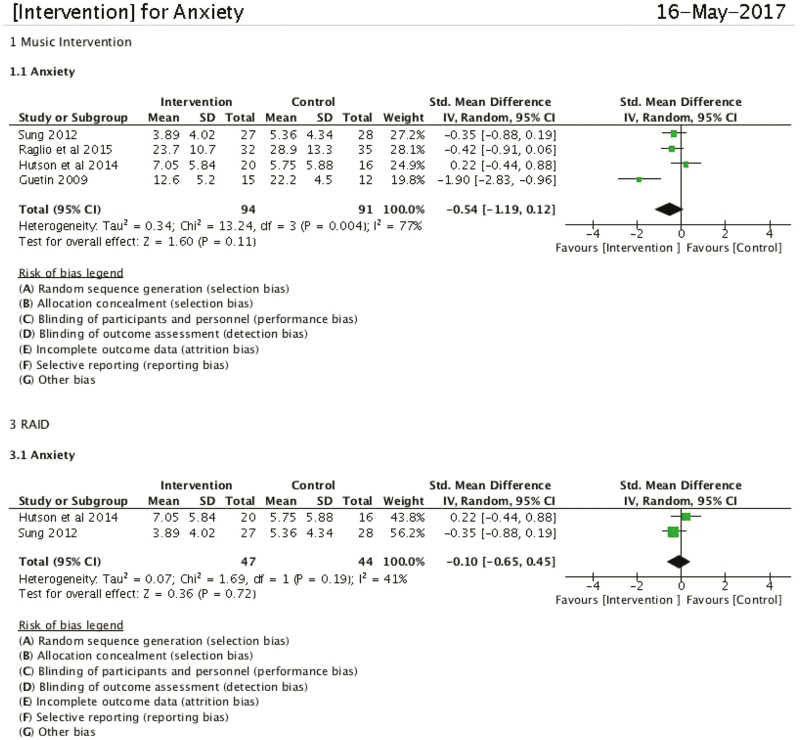
Music therapy fell into two groups: group therapy with a trained music therapist (Cooke et al., 2010; Hutson et al., 2014; Raglio et al., 2008; Sung et al., 2012) or listening to music of choice independently (Guetin et al., 2009; Sung et al., 2012), with Raglio and colleagues (2015) comparing both forms of music therapy. Active music therapy seeks to engage the participants in music making that enables expressions of emotions in relation to the music therapist (Raglio et al., 2008) whereas receptive music therapy is undertaken by listening to music in isolation with the music therapist only involved in supporting the choice of music (Raglio et al., 2015). Different tools were used across the studies with the most common being NPI and RAID. Many music therapy studies are hampered by small sample sizes whereas the studies included in this review ranged from 30 to 120 residents in well-designed randomized control trials. Interventions lasted from 6 to 16 weeks usually for 30 min per week. Most studies used multiple measurement time points, at baseline, midpoint and postintervention with the longest study duration of 24 weeks using five time points (Guetin et al., 2009). The results of the receptive music studies were positive, with Guetin and colleagues (2009; 15 residents in intervention arm assessed with the Hamilton Scale) finding a statistically significant effect on anxiety sustained up to 8 weeks postintervention. Studies using active music groups were mixed with Raglio and colleagues (2008; 30 residents assessed with the NPI) and Sung and colleagues (2012; 27 residents assessed with the RAID) finding a statistically significant effect on anxiety between control and intervention groups. Similarly to Guetin and colleagues (2009), Raglio and colleagues (2008) also found positive effects up to one month following the completion of the music therapy. Cooke and colleagues (2010) used a cross over the trial where 47 residents attended a music group using a reading group as control, and demonstrated no statistical effect on anxiety using the RAID. Hutson and colleagues (2014) used an active music therapy session across four care homes resulting in 20 residents completing the intervention and found no statistically significant effects between intervention and control (n = 16). Raglio and colleagues (2015) undertook multi center three-arm trial of 120 residents to compare receptive and active music therapies with usual care, and although they found an improvement across NPI global scores, there were no significant effects when compared with the control group. This may have been due to the large dropout rate and using the NPI global score as the outcome measure (Raglio et al., 2015). When the results of these studies were pooled for meta-analysis, the heterogeneity of these studies suggest it is difficult to demonstrate a statically significant outcome for either the effect or the most commonly used measurement tool, the RAID (Figure 4). Means and standard deviations were extracted from four articles and entered into RevMan for meta-anlaysis demonstrating insufficient evidence to show whether music interventions have an effect on anxiety (standardized mean difference = −0.54; 95% CI = −1.19 to 0.12), I2 = 77%, tau = 0.34). Where possible, missing data were accessed directly from the authors.
Figure 4.
Meta-analysis of music interventions with use of RAID.
Activity therapy in the studies reviewed was generally defined as an occupational activity or pleasant events where the activity was adjusted for the person with dementia either based on function and/or preferences or personality. The length of intervention ranged from twice daily specialized, individualized support for the person with dementia more than 3 weeks (Kolanowski et al., 2011) to the delivery of an occupational therapy intervention more than 12 weeks (Wenborn et al., 2013). To assess the changes in anxiety, the RAID was used in Wenborn and colleagues (2013) with 210 residents across 16 homes in a cluster RCT. Kolanowski and colleagues (2011) used the Philadelphia Geriatric Center Affect Rating Scale (ARS) for 129 residents where anxiety was a subscale. Both studies measured three to four time points. Kolanowski and colleagues considered the impact of customizing activities to the personality of the person and found this was the only factor that accounted for a change in scores when all other factors were controlled. Furthermore, Kolanowski and colleagues also found that anxiety did not improve over the 3-week intervention but improved 1 week after completion, suggesting it might take longer to demonstrate improvement in anxiety. However, Wenborn and colleagues (2013) who undertook the longer intervention with postintervention follow-up found no difference for anxiety between controls and the intervention groups. This finding may be a result of the lack of fidelity as this study was reliant on nursing home staff delivering the intervention. The heterogeneity of these interventions precluded a meta-analysis for activity-based interventions.
The remainder of the interventions was diverse with none of the included studies considering anxiety as the primary outcome. Rodríguez-Mansilla and colleagues (2015) conducted a three-arm trial with 111 residents more than 3 months finding that both acupressure and massage improved anxiety toward the end of the treatment and one-month posttreatment. Exercise interventions are known to affect mood, and Eggermont and colleagues (2009) undertook a hand movement program exercise tailored to the frailty of the nursing home population, finding a combined reduction of depression and anxiety in the intervention group on completion of the program. Husebo and colleagues (2014) conducted a cluster RCT measuring the impact of using the Stepwise Protocol of Treating Pain in persons with dementia using NPI-NH. This approach to pain control conferred significant benefit in the treatment of the NPI-NH mood cluster although the effects on anxiety did not reach statistical significance (Husebo et al., 2014).
Companion robots are becoming a feature of dementia care although these studies are hampered by small sample sizes and low quality (Bemelmans, Gelderblom, Jonker, & de Witte, 2012). In the current review, only one pilot study (with 18 residents) was located that involved a robotic baby seal known as “Paro” that considered anxiety as an outcome using RAID instrument over a 10-week intervention period (Moyle et al., 2013). Although no clinically significant effects were seen on anxiety, a small to moderate effect was seen using a standardized difference in means, suggesting a larger study is warranted (Moyle et al., 2013). Although it is difficult to generalize based on the heterogeneity of these studies, these findings suggest that where improvements in anxiety are achieved, they tend to be demonstrated after the midpoint of a treatment and may last for about 1 month after the treatment concludes.
Discussion
Anxiety in adults is generally considered to be as disabling as severe depression and should be considered a major health concern (Hunot, Churchill, Teixeira, & Silva de Lima, 2007). A systematic review suggests that cognitive behavioral therapy (CBT) is more effective than other psychotherapeutic interventions in treating anxiety in older adults (Hunot et al., 2007). However, CBT may not always be viable for people living with advanced dementia, particularly in nursing homes. Psychotherapeutic interventions have been used to treat anxiety and depression in people with dementia. However, the latest Cochrane systematic review of psychotherapeutic interventions found no difference in self-rated or carer-rated anxiety with none of the included studies examining people with dementia living in nursing homes (Orgeta et al., 2014). An examination of the relationship between depression, anxiety, and agitation in one facility in the United States for a doctoral thesis suggests that significant relationships exist between these three conditions, with a history of anxiety being a significant predictor of current anxiety in the nursing home (Hess, 2012). Hess (2012) concluded that it is not always possible to separate anxiety from other issues such as agitation and depression and that this might contribute to a more global construct of distress in the person with dementia living in nursing homes. This may account for the dearth of studies considering anxiety as the primary outcome for people living with dementia in nursing homes. The aim of this review was to consider if nonpharmacological interventions used to alleviate anxiety in this population were effective and if so, which interventions demonstrate the greatest effectiveness in reducing anxiety symptoms in older adults with comorbid dementia.
In the current systematic review, few studies considered anxiety as the primary outcome for people with dementia residing in nursing homes. Some studies considered anxiety as part of the construct for mood (Husebo et al., 2014; Kolanowski et al., 2011) or BPSD (Raglio et al., 2008; Raglio et al., 2015). Anxiety was only a primary outcome in studies focused on music (Guetin et al., 2009; Sung et al., 2012) as the intervention. Thus, the findings for the effectiveness of many of the interventions were limited. Music therapy, either interacting with a therapist or using a therapist to support the choice of music, was the most consistent approach to reducing anxiety for people living with dementia in nursing homes in 6 out of the 13 articles reviewed. The findings for the reduction of anxiety in this population using music therapy were mixed with limited findings for an active music therapy group demonstrating statistically significant findings in two small groups with larger studies demonstrating no effect when compared with other activities (Cooke et al., 2010) or integrated with usual care (Raglio et al., 2015). Not all results for music therapy were able to be used in the meta-analysis, but the results show that overall music therapy has some promise in reducing anxiety for people with dementia living in nursing homes. Music therapy interventions that demonstrated improvement were group based, but when two group interventions were compared, no difference was found in anxiety (Cooke et al., 2010) suggesting it might be the group interaction rather than the music therapy having the effect.
Activity tends to be a multifactorial intervention with differing approaches being adopted across different studies. Two studies included a choice of activities known as pleasant events or activities that the person with dementia chose to be involved in (Kolanowski et al., 2011; Wenborn et al., 2013). Both studies implemented staff education as part of the intervention, aimed at increasing activity or pleasant events but found limited or no improvement in anxiety between groups (Kolanowski et al., 2011; Wenborn et al., 2013). Wenborn and colleagues (2013) acknowledged the limitations of care home staff being able to deliver the activity intervention resulting in variability of compliance across care homes. This may have accounted for the lack of changes between control and intervention groups. This study underlines the complexity of care home staff engaging with interventions to increase activity for care homes residents in nursing homes. There was no information provided about the cost-effectiveness of the intervention in any of the studies reviewed. Wenborn and colleagues (2013) was the only study that calculated the cost of the professional delivering the intervention across nursing homes. Limited conclusions can be drawn about the other interventions due to the heterogeneity of the interventions and small sample sizes within each of the studies. Jutkowitz and colleagues (2016) raised similar concerns in a systematic review and meta-analysis of nonpharmacological interventions to manage agitation and aggression in dementia in nursing homes and assisted living facilities. These authors similarly concluded that the heterogeneity of interventions, different measures being used alongside small sample sizes all reduced the methodological rigor required to identify the efficacy of nonpharmacological interventions.
In a state of the science review for behavioral and psychological symptoms of dementia, Kales, Gitlin, and Lyketsos (2015) suggest that the underlying cause of the behavior needs to be assessed and an intervention designed for that person implemented and evaluated. There were only two studies that identified participants with clinical anxiety in advance of the intervention (Cooke et al., 2010; Guetin et al., 2009). This suggests a need for a more systematic screening of anxiety in nursing home populations, particularly with dementia (Hess et al., 2012) with interventions implemented when assessed symptoms are more prevalent (Cooke et al., 2010).
Limitations of This Review
It was possible that not all studies reporting on anxiety were captured in the search as only articles in English were included. To capture as many articles as possible, we kept the search terms very broad. The heterogeneity of the studies meant it was not feasible to undertake a meta-analysis on all but a few of the studies, which limits the generalizability of this review. A limitation across many of the studies was the lack of identification of anxiety as a clinical problem in the sample population (Cooke et al., 2010; Guetin et al., 2009 were the notable exceptions), which may account for the lack of efficacy of the interventions.
To develop effective treatments, appropriate measurement tools for assessment must be available, particularly to enable the effectiveness of treatment to be determined (Hunsley & Mash, 2008). A challenge in this review was the heterogeneity in assessment tools used. The lack of reported reliability or validity information in the majority of the articles suggests a lack of understanding of the importance of psychometric analysis when using measurement tools in different populations. These findings are similar to a systematic review of assessment measurement tools for anxiety in older adults (Therrien & Hunsley, 2012) where only 16% of published studies provided reliability coefficients from the data analyzed and less than one quarter provided information about the population that the instrument was designed for (Therrien & Hunsley, 2012). However, the three studies that considered psychometric data as part of their study used three different instruments (RAID, Philadelphia ARS and a Dutch subscale of SCL-90) with each reporting adequate treatment sensitivity and clinical utility. Across this review, the RAID was the most utilized instrument for the nursing home population (six articles) using a dyadic scale, thus overcoming the limitation of self-report with adults experiencing impaired expressive and comprehension abilities.
Conclusions
Anxiety in later life is known to reduce the quality of life and impact on activities of daily living. Little is known about the experience of people with dementia living with anxiety as a comorbid condition in nursing homes as anxiety in adults living with dementia is often unrecognized by clinicians and so remains untreated. Many older adults with anxiety report having had anxiety throughout their lives, suggesting that older adults with dementia who have a history of anxiety may continue to experience anxiety as their dementia progresses (Hess, 2012). However, there was a dearth of studies that considered anxiety as a primary outcome or identified if participants had clinical anxiety at baseline. Furthermore, a key finding from this review is that there remain limited interventions known to reduce anxiety for people living with dementia. It has been recommended that interventions should be implemented when assessed symptoms are more prevalent (Cooke et al., 2010) or take into account the individualized preferences of the person with dementia (Kales et al., 2015; Kolanowski et al., 2011). Therefore, to develop effective interventions, further research is needed to understand the lived experience of anxiety from the perspective of the person with dementia living in nursing homes. The quality of the included RCTs was of moderate to high quality however the difference in time points and use of anxiety measures makes it difficult to combine data and so identify interventions that may be effective. A key contribution of this review is to identify that interventions lasting between 4 and 12 weeks are more likely to demonstrate an impact on anxiety and that the RAID instrument is the most commonly used instrument. This suggests the RAID is an effective tool for assessing anxiety for people with dementia and could be used more widely in nursing homes to understand the experience of anxiety as a comorbid condition with dementia. Further research is needed taking these factors into account into how common and cost-effective activities undertaken in nursing homes might be used to reduce anxiety in this population.
Funding
This study was supported by an Alzheimer’s Association Pioneer Grant P10-1999-1800 (L Teri, P.I.) and the National Institutes of Health (5 P50 AG05136-17).
Conflict of Interest
None reported.
References
- Alzheimer’s Society (2014). Dementia UK 2nd ed. London. Retrieved from https://www.alzheimers.org.uk/sites/default/files/migrate/downloads/dementia_uk_update.pdf
- Arendt L., Brown Wilson C., Pachana N. A., Neville C., & Scott T (2016). A systematic review of nonpharmacological interventions for older adults with comorbid dementia and anxiety living in residential aged care. (Protocol). PROSPERO 2016:CRD42016034043 Retrieved from http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016034043
- Auer S. R., Monteiro I. M., & Reisberg B (1996). The Empirical Behavioral Pathology in Alzheimer’s Disease (E-BEHAVE-AD) Rating Scale. International Psychogeriatrics, 8, 247–266. doi:10.1017/S1041610296002621 [DOI] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare (AIHW) (2012). Dementia in Australia Canberra. Retrieved from https://www.aihw.gov.au/getmedia/199796bc-34bf-4c49-a046-7e83c24968f1/13995.pdf.aspx?inline=true
- Bannerjee S. (2009).The use of antipsychotic medication for people with dementia: Time for action. A report for the Minister of State London. Retrieved fromhttps://webarchive.nationalarchives.gov.uk/20130104165557/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_108303
- Beattie E., Pachana N. A., & Fanklin S. J (2010). Double Jeapoardy: Comorbid anxiety and depression in late life. Research in Gerontological Nursing, 3(3), 2019–2020. doi:10.3928/19404921-20100528-99 [DOI] [PubMed] [Google Scholar]
- Bemelmans R., Gelderblom G. J., Jonker P., & de Witte L (2012). Socially assistive robots in elderly care: A systematic review into effects and effectiveness. Journal of the American Medical Directors Association, 13(2), 114.e1–120.e1. doi: 10.1016/j.jamda.2010.10.002 [DOI] [PubMed] [Google Scholar]
- Cooke M. L., Moyle W., Shum D. H., Harrison S. D., & Murfield J. E (2010). A randomized controlled trial exploring the effect of music on agitated behaviours and anxiety in older people with dementia. Aging & Mental Health, 14, 905–916. doi: 10.1080/13607861003713190 [DOI] [PubMed] [Google Scholar]
- Cummings J. L., Mega M., Gray K., Rosenberg-Thompson S., Carusi D. A., & Gornbein J (1994). The Neuropsychiatric Inventory: Comprehensive assessment of psychopathology in dementia. Neurology, 44, 2308–2314. doi:10.1212/WNL.44.12.2308 [DOI] [PubMed] [Google Scholar]
- Eggermont L. H., Knol D. L., Hol E. M., Swaab D. F., & Scherder E. J (2009). Hand motor activity, cognition, mood, and the rest-activity rhythm in dementia: A clustered RCT. Behavioural Brain Research, 196, 271–278. doi: 10.1016/j.bbr.2008.09.012 [DOI] [PubMed] [Google Scholar]
- Gibbons L. E., Teri L., Logsdon R. G., & McCurry S. M (2006). Assessment of anxiety in dementia: An investigation into the association of different methods of measurement. Journal of Geriatric Psychiatry and Neurology, 4, 202–208. doi: 10.1177/0891988706292758 [DOI] [PubMed] [Google Scholar]
- Gibbons L. E., Teri L., Logsdon R., McCurry S. M., Kukull W., Bowen J., & Larson E (2002). Anxiety symptoms as predictors of nursing home placement in patients with Alzheimer’s disease. Journal of Clinical Geropsychology, 8(4), 335–342. doi: 10.1023/a:1019635525375 [Google Scholar]
- Guétin S., Portet F., Picot M. C., Pommié C., Messaoudi M., Djabelkir L.,…Touchon J (2009). Effect of music therapy on anxiety and depression in patients with alzheimer’s type dementia: Randomised, controlled study. Dementia and Geriatric Cognitive Disorders, 28(1), 36–46. doi: 10.1159/000229024 [DOI] [PubMed] [Google Scholar]
- Hess L. S. (2012). Anxiety in older adults with dementia residing in long-term care facilities. Electronic theses and dissertations. Paper 611. doi: 10.18297/etd/611 University of Louisville. Retrieved from https://ir.library.louisville.edu/etd/611/ [DOI] [Google Scholar]
- Hess L. S., Williams J. C., & Meeks S (2012). Mental health history predicts anxiety in long-term care residents with dementia. The Gerontologist, 52(Suppl. 1), 156. [Google Scholar]
- Higgins J. P. T., & Green S. (Eds.). (2011). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] The Cochrane Collaboration. Retrieved from www.cochrane-handbook.org
- Hoe J., Cooper C., & Livingston G (2013). An overview of the LASER-AD study: A longitudinal epidemiological study of people with Alzheimer’s disease. International Review of Psychiatry (Abingdon, England), 25, 659–672. doi: 10.3109/09540261.2013.838152 [DOI] [PubMed] [Google Scholar]
- Hoe J., Hancock G., Livingston G., & Orrell M (2006). Quality of life of people with dementia in residential care homes. The British Journal of Psychiatry: The Journal of Mental Science, 188, 460–464. doi: 10.1192/bjp.bp.104.007658 [DOI] [PubMed] [Google Scholar]
- Hunot V., Churchill R., Teixeira V., & Silva de Lima M (2007). Psychological therapies for generalised anxiety disorder. Cochrane Database of Systematic Reviews, 1: CD001848. doi: 10.1002/14651858.CD001848.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunsley J., & Mash E. J (2008). A guide to assessments that work. New York: Oxford University Press. [Google Scholar]
- Husebo B. S., Ballard C., Fritze F., Sandvik R. K., & Aarsland D (2014). Efficacy of pain treatment on mood syndrome in patients with dementia: A randomized clinical trial. International Journal of Geriatric Psychiatry, 29(8), 828–836. doi: 10.1002/gps.4063 [DOI] [PubMed] [Google Scholar]
- Hutson C., Orrell M., Dugmore O., & Spector A (2014). Sonas: A pilot study investigating the effectiveness of an intervention for people with moderate to severe dementia. American Journal of Alzheimer’s Disease & Other Dementias, 29(8), 696–703. doi: 10.1177/1533317514534756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jutkowitz E., Brasure M., Fuchs E., Shippee T., Kane R. A., Fink H.,…Kane R. L (2016). Care-delivery interventions to manage agitation and aggression in dementia nursing home and assisted living residents: A systematic review and meta-analysis. Journal of the American Geriatrics Society, 64(3), 477–488. doi:10.1111/jgs.13936 [DOI] [PubMed] [Google Scholar]
- Kales H., Gitlin L. N., & Lyketsos C. G (2015). Assessment and management of behavioural and psychological symptoms of dementia. British Medical Journal, 350, h369 doi: 10.1136/bmj.h369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolanowski A., Litaker M., Buettner L., Moeller J., & Costa P. T (2011). A randomized clinical trial of theory-based activities for the behavioral symptoms of dementia in nursing home residents. Journal of the American Geriatrics Society, 59(6), 1032–1041. doi: 10.1111/j.1532-5415.2011.03449.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBarge E. (1993). A preliminary scale to measure the degree of worry among mildly demented Alzheimer disease patients. Physical & Occupational Therapy in Geriatrics, 11(3), 43–57. doi: 10.1080/J148v11n03_04 [DOI] [Google Scholar]
- McCurry S. M., Gibbons L. E., Logsdon R. G., & Teri L (2004). Anxiety and nighttime behavioral disturbances. Awakenings in patients with Alzheimer’s disease. Journal of Gerontological Nursing, 30, 12–20. doi:10.3928/0098-9134-20040101-05 [DOI] [PubMed] [Google Scholar]
- Moyle W., Cooke M., Beattie E., Jones C., Klein B., Cook G., & Gray C (2013). Exploring the effect of Companion Robots on emotional expression in older adults with dementia: A pilot randomized controlled trial. Journal of Gerontological Nursing, 39(5), 46–53. doi: 10.3928/00989134-20130313-03 [DOI] [PubMed] [Google Scholar]
- Orgeta V., Qazi A., Spector A. E., & Orrell M (2014). Psychological treatments for depression and anxiety in dementia and mild cognitive impairment. Cochrane Database of Systematic Reviews, 1, CD009125. doi: 10.1002/14651858.CD009125.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachana N. A., Helmes E., Byrne G. J. A., Edelstein B. A., Konnert C. A., Pot A. M.,…Stanley M (2010). Screening for mental disorders in residential aged care facilities. International Psychogeriatrics, 22, 1107–1120. doi: 10.1017/S1041610210000128 [DOI] [PubMed] [Google Scholar]
- Raglio A., Bellandi D., Baiardi P., Gianotti M., Chiara Ubezio M., Zanacchi E.,…Stramba-Badiale M (2015). Effect of active music therapy and individualized listening to music on dementia: A multicenter randomized controlled trial. Journal of the American Geriatrics Society, 63(8), 1534–1539. doi: 10.1111/jgs.13558 [DOI] [PubMed] [Google Scholar]
- Raglio A., Bellelli G., Traficante D., Gianotti M., Chiara Ubezio M., Villani D., & Trabucchi M (2008). Efficacy of music therapy in the treatment of behavioral and psychiatric symptoms of dementia. Alzheimer Disease & Associated Disorders, 22(2), 158–162. doi: 10.1097/WAD.0b013e3181630b6f [DOI] [PubMed] [Google Scholar]
- Rodríguez-Mansilla J., López-Arza M. V. G., Varela-Donoso E., Montanero-Fernández J., Sánchez B. G., & Garrido-Ardila E. M (2015). The effects of ear acupressure, massage therapy and no therapy on symptoms of dementia: A randomized controlled trial. Clinical Rehabilitation, 29(7), 683–693. doi: 10.1177/0269215514554240 [DOI] [PubMed] [Google Scholar]
- Sansoni J., Marosszeky N., Jeon Y.-H., Chenoweth L., Hawthorne G., King M.,…Low L.-F (2007). Final report: Dementia outcomes measurement suite project. Retrieved from University of Wollongong Retrieved from https://ahsri.uow.edu.au/content/groups/public/@web/@chsd/documents/doc/uow217365.pdf
- Schulz K. F., Altman D. G., Moher D., & for the CONSORT group. (2010). Consort 2010 Statement: Updated guidance on reporting parallel group randomised trials. British Medical Journal, 340, c332 doi: 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seignourel P. J., Kunik M. E., Snow L., Wilson N., & Stanley M (2008). Anxiety in dementia: A critical review. Clinical Psychology Review, 28, 1071–1082. doi: 10.1016/j.cpr.2008.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selwood A., Thorgrimsen L., & Orrell M (2005). Quality of life in dementia—A one-year follow-up study. International Journal of Geriatric Psychiatry, 20, 232–237. doi: 10.1002/gps.1271 [DOI] [PubMed] [Google Scholar]
- Serrani Azcurra D. J. L. (2012). A reminiscence program intervention to improve the quality of life of long-term care residents with Alzheimer’s disease. A randomized controlled trial. Revista Brasileira de Psiquiatria, 34(4), 422–433. doi: 10.1016/j.rbp.2012.05.008 [DOI] [PubMed] [Google Scholar]
- Shankar K. K., Walker M., Frost D., & Orrell M. W (1999). The development of a valid and reliable scale for rating anxiety in dementia (RAID). Aging & Mental Health, 3(1), 39–49. doi: 10.1080/13607869956424 [DOI] [Google Scholar]
- Sorensen S., Duberstein P., Gill D., & Pinquart M. (2006). Dementia care: Mental health effects, intervention strategies, and clinical implications. The Lancet. Neurolology, 5, 961–973. doi:10.1016/S1474-4422(06)70599-3 [DOI] [PubMed] [Google Scholar]
- Starkstein S. E., Jorge R., Petracca G., & Robinson R. G (2007). The construct of generalized anxiety disorder in Alzheimer disease. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 15, 42–49. doi: 10.1097/01.JGP.0000229664.11306.b9 [DOI] [PubMed] [Google Scholar]
- Sung H.-C., Lee W.-L., Li T.-L., & Watson R. (2012). A group music intervention using percussion Instruments with familiar music to reduce anxiety and agitation of institutionalized older adults with dementia. International Journal of Geriatric Psychiatry, 27(6), 621–627.doi: 10.1002/gps.2761 [DOI] [PubMed] [Google Scholar]
- Teri L., Logsdon R. G., Uomoto J., & McCurry S (1997). Behavioral treatment of depression in dementia patients: A controlled clinical trial. The Journal of Gerontology, Series B: Psychological Sciences, 52, 159–166. [DOI] [PubMed] [Google Scholar]
- Therrien Z., & Hunsley J (2012). Assessment of anxiety in older adults: A systematic review of commonly used measures. Aging & Mental Health, 16, 1–16. doi: 10.1080/13607863.2011.602960 [DOI] [PubMed] [Google Scholar]
- Therrien Z., & Hunsley J (2013). Assessment of anxiety in older adults: A reliability generalization meta-analysis of commonly used measures. Clinical Gerontologist, 36(3), 171–194. doi: 10.1080/07317115.2013.767871 [DOI] [Google Scholar]
- Voyer P., Verreault R., Cappeliez P., Holmes D., & Mengue P. N (2005). Symptoms of psychological distress among older adults in Canadian long-term care centres. Aging & Mental Health, 9, 542–554. doi: 10.1080/13607860500193336 [DOI] [PubMed] [Google Scholar]
- Wancata J., Benda N., Meise U., & Windhaber J (2003). Non-cognitive symptoms of dementia in nursing homes: Frequency, course and consequences. Social Psychiatry and Psychiatric Epidemiology, 38(11),637–643. doi: 10.1007/s00127-003-0683-7 [DOI] [PubMed] [Google Scholar]
- Wenborn J., Challis D., Head J., Miranda-Castillo C., Popham C., Thakur R.,…Martin Orrell M (2013). Providing activity for people with dementia in care homes: A cluster randomised controlled trial. International Journal of Geriatric Psychiatry, 28(12), 1296–1304. doi: 10.1002/gps.3960 [DOI] [PubMed] [Google Scholar]
- Williams J. C., Hess L. S., & Meeks S (2012). Informants’ perspectives on anxiety and agitation in nursing home residents with dementia. The Gerontologist, 52(Suppl. 1), 155. [Google Scholar]