Abstract
Objective:
To evaluate differences in body image distress (BID) scores between women with PCOS and controls and if BID mediates anxiety and depression.
Design:
Cross-sectional.
Setting:
Academic institution.
Patients:
Reproductive-aged women with PCOS (n=189) and controls (n=225).
Intervention:
Surveys (Multidimensional Body Self Relations-Appearance Subscale (MBSRQ-AS), Stunkard Figure Rating Scale (FRS), Hospital Anxiety and Depression Scale (HADS), PCOS quality of life survey (MPCOS-Q).
Main Outcome Measures:
BID, depression and anxiety scores and mediation of depression and anxiety scores by BID.
Results:
Women with PCOS had worse BID scores on all five MBSRQ-AS subscales (p<0.01) adjusted for age, BMI, race, pregnancy history, income and employment, and larger differences on the FRS (p<0.05) compared to controls. In multivariable regression models, the prevalence of depressive (28% vs 19.2%) and anxiety (76.5% vs 56.5%) symptoms were also significantly higher in women with PCOS compared to controls (p<0.001 for both). Most MBSRQ-AS subscale scores significantly correlated with depression, anxiety and quality of life scores (p<0.01). The association between PCOS/control status and higher anxiety and depression scores was completely mediated by the appearance evaluation and body areas satisfaction subscales and partially mediated by overweight preoccupation, appearance orientation and self-classified weight.
Conclusion:
Women with PCOS have increased body image distress, depressive and anxiety symptoms. In our study different aspects of body image distress either fully or partially mediated the association between PCOS/control status and depression and anxiety scores suggesting that therapeutic interventions targeted at improving body image may decrease depressive and anxiety symptoms.
Keywords: Anxiety, Body image distress, Depression, PCOS, Quality of life
Capsule:
Women with PCOS had higher body image distress scores compared to controls. Body image mediated the relationship between PCOS and anxiety/depressive scores and was correlated with lower quality of life.
Introduction
Polycystic ovary syndrome, or PCOS, is the most common endocrine disorder affecting reproductive aged woman.(1) It is characterized as a multi-system disorder, with affected women known to be at a higher risk of metabolic syndrome, diabetes, infertility and pregnancy-related complications.(2–6) Recently there has been increasing awareness of the association of PCOS with anxiety and depression.(7, 8) A recent systematic review and meta-analysis of 18 studies by Cooney et al. reported the prevalence of clinically significant depressive symptoms in women with PCOS to be 36.6% compared to 14.2% in controls, and the prevalence of anxiety symptoms to be 41.9% compared to 8.5% in controls.(9) Longitudinal studies have also demonstrated a higher risk of conversion to depression and/or depressive symptoms in women with PCOS.(10–12) The recently published international guidelines on PCOS and the Androgen Excess (AE-PCOS) society position statement therefore recommend screening all women with PCOS for anxiety and depression at their initial visit.(1, 13)
Certain physical characteristics are more prevalent in women with PCOS, such as acne, hirsutism and obesity.(14,15) Some studies suggest that these features are associated with higher depressive symptoms and contribute to lower health related quality of life (PCOSQ) scores in women with PCOS.(9, 16) Others have demonstrated that a higher body mass index (BMI), known to be independently associated with PCOS, is linked to greater body dissatisfaction.(17–19) Taken together, these findings suggest that women with PCOS could be at a higher risk of body image distress (BID). Body image is defined as an individual’s psychological experience of the appearance and function of his/her body.(17) Two central components of body image in general are body image evaluation and body image investment. It has been reported that 13–32% of women in the United States express dissatisfaction with their overall appearance.(20, 21) Understanding body image perceptions is particularly relevant when evaluating psychological distress especially in a condition such as PCOS.(22)
Very few studies have examined the association between PCOS and BID and the results have been mixed. In a cross-sectional study using a validated screening tool (MBSRQ), women with PCOS (n=177) had more negative body image compared to controls (n=109) and lower appearance evaluation was associated with depression independent of BMI.(23) Another study evaluating predictors of depression in women with PCOS (n=40) and fertile and infertile controls (n=100) reported significant differences in appearance orientation and body features satisfaction after controlling for BMI in women with PCOS.(24) However, a cross-sectional analysis of women with PCOS (n=96) and a comparison cohort (n=94) revealed similar body dissatisfaction, even within BMI strata, and body dissatisfaction was only associated with depressive symptoms in PCOS women who did not have obesity.(25) In another cross-sectional analysis of women without obesity, body image and self-esteem scores did not differ significantly between PCOS (n=83) and controls (n=64).(26) It is therefore unclear whether BID plays a role in the higher prevalence of depression and anxiety symptoms observed in PCOS as suggested in the general population.(17)
As the evidence for BID in women with PCOS is limited, the international PCOS guidelines drew upon clinical expertise and consensus and recommended that additional studies are needed to determine if clinically meaningful differences exist.(1) Given the lack of consistent findings and the potential impact BID can have on depression and anxiety symptoms, as well as lower quality of life in women already predisposed to these issues, we sought to determine the differences in BID scores in women with PCOS and controls, and then examine whether BID mediated the association between PCOS and depression and anxiety symptoms.
Materials and Methods
Subjects
We conducted a prospective cross-sectional study at the University of Pennsylvania’s Penn PCOS center and gynecology clinics. From January-October 2018, non-pregnant women aged 18–50 years presenting to these clinics were approached for participation in the study. Women with PCOS met the Rotterdam criteria, defined as 2 of the 3 following: elevated clinical or biochemical androgens (identified in this study by chart review for Ferriman-Gallwey (FG) scores and/or serum testosterone levels), irregular menses and polycystic appearing ovaries (identified by chart review for ultrasound report).(27) No restrictions were placed based on history of mood disorders, use of anti-depressants, hormonal contraception or presence of other medical comorbidities. In order to account for the possible impact of obesity on body image, enrollment of controls was targeted to balance the distribution of BMI to be similar to that observed in women with PCOS. Control subjects completed a screening questionnaire and were excluded if they reported both hirsutism and irregular menses. The University of Pennsylvania Institutional Review Board approved this study.
Surveys
Demographic questionnaires, containing items on socioeconomic status, psychiatric, menstrual and pregnancy history, the Multidimensional Body Self Relations-Appearance Subscale (MBSRQ-AS), Stunkard Figure Rating Scale (FRS) and Hospital Anxiety and Depression Scale (HADS) surveys were administered to both women with PCOS and controls whereas the modified-PCOSQ (MPCOSQ) survey was administered only to women with PCOS. The MBSRQ-AS is a 34-item questionnaire(28–30) validated in several languages across multiple populations to assess body image.(31–33) It includes the following 5 subscales: Appearance Evaluation (feelings about attractiveness and appearance), Appearance Orientation (extent of investment in and importance of one’s appearance), Overweight Preoccupation (degree of fat anxiety and weight vigilance), Self-Classified Weight (how a person perceives their weight), and Body Areas Satisfaction (degree of satisfaction with discrete aspects of one’s appearance). In this survey, higher scores on Appearance Evaluation and Body Areas Satisfaction indicate greater happiness with one’s appearance, whereas higher scores on Appearance Orientation, Overweight Preoccupation, and Self-Classified Weight indicate decreased happiness with one’s appearance. This suggests that higher scores on Appearance Orientation, Overweight Preoccupation and Self-Classified Weight and lower scores on Appearance Evaluation and Body Areas Satisfaction indicate more body image distress. As the MBSRQ-AS does not have cut-offs or thresholds to indicate dichotomous results (29), differences in continuous results between study groups were examined. The FRS scale is composed of nine numbered adult female silhouettes in increasing size from very thin (1) to obese (9)(34) and has been previously shown to be a reliable and valid tool for assessing body image satisfaction.(35, 36) For the FRS, women were asked to pick a silhouette in response to each of the following questions: Q1) Choose your ideal figure, Q2) Choose the figure that reflects how you think you look and Q3) Choose the figure that reflects how you feel most of the time. (Supplementary Figure 1) Score 1 was calculated as Q3–Q1, Score 2 as Q2–Q1 and Score 3 as Q3–Q2. Score values of 2 or more (in other words differences of 2 or more sizes) were considered indicative of body dissatisfaction, similar to methods described in other studies.(37, 38)
The HADS is a validated 14-item questionnaire with 7 questions dedicated to the assessment of anxiety and 7 to the assessment of depressive symptoms.(39, 40) HADS scores of 8 or above were considered abnormal, as previously described.(23, 40) The MPCOSQ is a 30-item questionnaire containing the following 6 domains: emotions, body hair, weight, infertility, menstruation and acne, with higher values indicating higher quality of life.(41)This is a modified version of the PCOSQ, which is reliable and validated in several languages as an instrument for measuring health-related quality of life in women with PCOS.(42–44) One of the drawbacks to the PCOSQ was lack of an acne dimension, rectified by the MPCOSQ, with authors noting very similar factor structure to that identified by previous research.(41) Each item of the MBSRQ-AS, HADS and MPCOSQ are scored on Likert scales. Study data were collected and managed using REDCap (Research Electronic Data Capture)(45) electronic data capture tools hosted at the University of Pennsylvania.
Outcomes and Statistical Analysis
The primary outcome was to determine the difference in BID scores between PCOS and control participants. Secondary outcomes included the association between BID scores and depression, anxiety and quality of life scores in the PCOS group. We also performed mediation analyses to assess to what extent BID mediated the association between PCOS/control status and depression or anxiety score differences. Continuous outcomes, including differences in MBSRQ-AS, HADS and FRS scores, were compared using either rank-sum or student t-test as dictated by normality assessments. Categorical outcomes such as prevalence of clinically significant depressive and anxiety symptoms were compared using Pearson chi-square tests. Multivariable linear regression modeling was used to examine differences in the continuous BID, depression and anxiety scores between women with PCOS and controls and associations between continuous depression, anxiety and BID scores while accounting for age, BMI, race, pregnancy history and socioeconomic status. Covariates included in the model were determined a-priori as well as after assessment of confounding variables using a backwards elimination strategy.
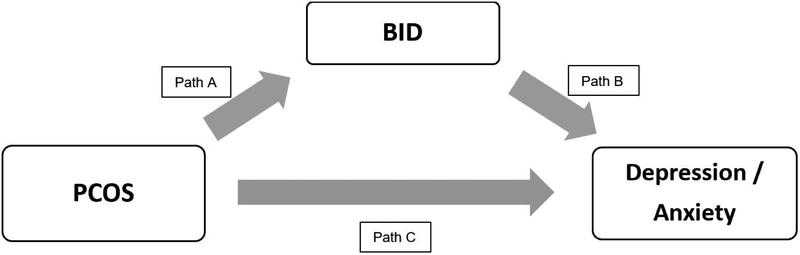
Linear regression and joint regression models were used to evaluate whether identified associations between PCOS/control status and continuous depression and anxiety scores were mediated by MBSRQ-AS subscales, while controlling for the covariates mentioned above. In order to conduct mediation analyses, the mediator (BID) must show an association with the predictor variable of interest: PCOS (See Path A of Figure 1A) and outcome: depression/anxiety (See Path B of Figure 1A). There must also be an established association between PCOS and depression/anxiety scores (See Path C of Figure 1A). Then, mediation analyses can evaluate to what extent the association between PCOS and depression/anxiety is accounted for, or in other words mediated by, BID.(46, 47) Finally, univariate linear regression models were used to identify associations between each MBSRQ-AS subscale and FG score and BMI in women with PCOS. All analyses were conducted using STATA v14.2 (Stata-Corp).
Figure 1A:
Mediation analysis framework
Results
Demographic characteristics
One hundred eighty-nine women with PCOS and 225 controls were included in the study (Table 1). Women with PCOS were significantly younger, more likely to be Caucasian, less likely to have been pregnant previously and of a higher socio-economic status as defined by highest degree obtained, income and employment status. There were no significant differences between the two study groups in terms of BMI or marital status. (See Table 1)
Table 1:
Demographic characteristics of women with PCOS and controls
| PCOS (n=189) | Controls (n=225) | p-value | |
|---|---|---|---|
| Median age in years (range) | 29.3 (18.1–47.4) | 32.1 (19.7–49.8) | <0.001 |
| Median BMI in kg/m2 (range) | 32.1 (17.8–57.1) | 30.9 (17.3–54.4) | 0.175 |
| Race, n (%) | <0.001 | ||
| Caucasian | 123 (65) | 58 (26) | |
| African American | 38 (20) | 140 (63) | |
| Asian | 13 (7) | 10 (4) | |
| Other | 14 (8) | 15 (7) | |
| Highest degree, n (%) | <0.001 | ||
| Some high school | 2 (1) | 13 (6) | |
| High school | 15 (8) | 53 (24) | |
| Some college | 43 (23) | 52 (24) | |
| College | 67 (36) | 49 (22) | |
| Some professional | 9 (5) | 9 (4) | |
| Professional | 51 (27) | 44 (20) | |
| Employment, n (%) | 0.010 | ||
| Full time | 141 (76) | 153 (70) | |
| Part time | 30 (16) | 23 (10) | |
| Unemployed, not looking for job | 8 (4) | 19 (9) | |
| Unemployed, looking for job | 8 (4) | 24 (11) | |
| Income in dollars, n (%) | <0.001 | ||
| <20,000 | 28 (15) | 58 (27) | |
| 20,001–50,000 | 38 (21) | 80 (37) | |
| 50,001–100,000 | 61 (33) | 44 (20) | |
| 100,001–150,000 | 29 (16) | 19 (9) | |
| >150,000 | 28 (15) | 14 (7) | |
| Marital status, n (%) | 0.217 | ||
| Single, never married | 122 (65) | 151 (68) | |
| Married or domestic partnership | 64 (34) | 64 (29) | |
| Divorced or separated | 2 (1) | 7 (3) | |
| Previously pregnant, n (%) | 46 (24) | 164 (73) | <0.001 |
| Depression medication use, n (%) | 32 (17) | 32 (14) | 0.448 |
| Hormonal contraceptive use, n (%) | 96 (51) | 106 (47) | 0.424 |
Body image survey scores
Table 2 shows body image survey scores using the MBSRQ-AS and Stunkard FRS surveys. All assessed areas of the MBSRQ-AS showed significant differences between PCOS and controls suggestive of BID. In multivariable regression models adjusted for age, BMI, race, pregnancy history, income and employment, BID scores for Appearance Evaluation and Body Areas Satisfaction were significantly lower whereas Appearance Orientation, Overweight Preoccupation and Self-Classified Weight were significantly higher in women with PCOS compared to controls. On the Stunkard FRS survey, women with PCOS had larger differences compared to controls for Stunkard Score 1 (p=0.020) and Score 2 (p=0.011) but not Score 3 (p=0.276). For both Score 1 and Score 2, the values were noted to be 2 or greater, indicative of BID as described in the Methods.
Table 2:
Path A: Body image survey scores (mean ± SD) in women with PCOS compared to controls
| BID measure | PCOS (n=189) | Controls (n=225) | p-valuec |
|---|---|---|---|
| MBSRQ-ASa Appearance Evaluation | 2.6 ± 0.9 | 3.4 ± 0.9 | <0.001 |
| MBSRQ-AS Overweight Preoccupation | 3.4 ± 0.9 | 2.8 ± 1.0 | <0.001 |
| MBSRQ-AS Appearance Orientation | 3.8 ± 0.6 | 3.6 ± 0.7 | 0.002 |
| MBSRQ-AS Body Areas Satisfaction | 2.8 ±0.7 | 3.3 ± 0.7 | <0.001 |
| MBSRQ-AS Weight Classification | 4.0 ± 0.7 | 3.6 ± 0.9 | 0.013 |
| Stunkardb Score 1: Q3-Q1 | 2.6 ± 1.6 | 1.5 ± 1.8 | 0.020 |
| Stunkard Score 2: Q2-Q1 | 2.0 ± 1.2 | 1.2 ± 1.4 | 0.011 |
| Stunkard Score 3: Q3-Q2 | 0.6 ± 0.9 | 0.3 ±1.0 | 0.276 |
Multidimensional Body Self Relations-Appearance Subscale
Stunkard scores are generated from the Stunkard Figure Rating Scale
Multivariable regression analysis controlling for age, BMI, race, pregnancy history, income and employment
Depression and anxiety scores
In multivariable logistic regression models, after adjusting for age, BMI, race, pregnancy history and income, the prevalence, as measured by percentage of women scoring 8 or greater on the HADS, of abnormal depression scores (28% vs 19.2%, p<0.001) and anxiety scores (76.5% vs 56.5%, P<0.001) were significantly higher in women with PCOS compared to controls. In multivariable linear regression models examining continuous depression and anxiety scores and adjusting for age, BMI, race, pregnancy history and income, women with PCOS were significantly more likely to have higher depression scores (mean score 5.1 vs 4.5, p=0.01) and anxiety scores (mean score 10.1 vs 8.4, p=0.02) compared to controls.
Association of depression and anxiety scores with MBSRQ-AS scores
In multivariable linear regression models accounting for PCOS status, age, BMI, race, pregnancy history and income, HADS depression scores were significantly associated with the MBSRQ-AS appearance evaluation (p<0.001), body areas satisfaction (p<0.001), overweight preoccupation (p=0.001) and self-classified weight (p<0.001) subscales. When examining HADS anxiety scores, models accounting for the same covariates were significantly associated with the MBSRQ-AS appearance evaluation (p<0.001), appearance orientation (p=0.001), overweight preoccupation (p<0.001), self-classified weight (p=0.008) and body areas satisfaction (p<0.001) subscales. (See Table 3)
Table 3:
Path B: Association of depression and anxiety scores with MBSRQ-AS scores
| HADSa Depression | HADS Anxiety | |||
|---|---|---|---|---|
| Coefficient | p-valueb | Coefficient | p-valueb | |
| Appearance Evaluation | −2.30 | <0.001 | −2.43 | <0.001 |
| Appearance Orientation | 0.07 | 0.808 | 1.66 | 0.001 |
| Overweight Preoccupation | 0.66 | 0.001 | 1.09 | <0.001 |
| Self-Classified Weight | 1.17 | <0.001 | 0.979 | 0.008 |
| Body Areas Satisfaction | −2.92 | <0.001 | −3.36 | <0.001 |
Hospital Anxiety and Depression Scale
Multivariable regression analysis controlling for PCOS, age, BMI, race, pregnancy history and income
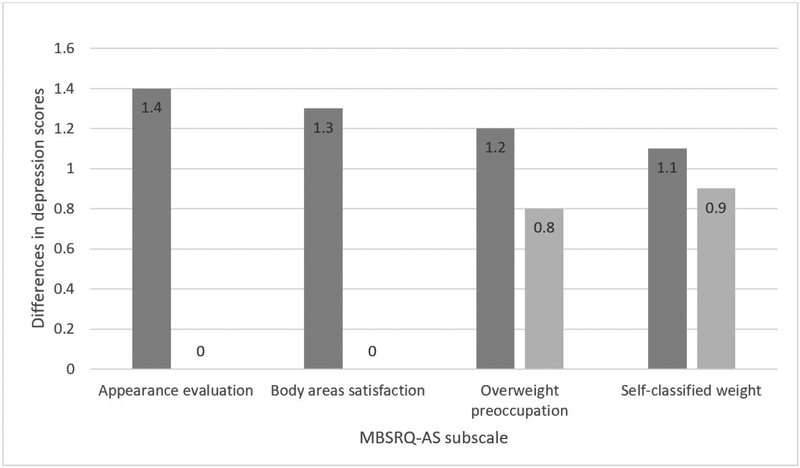
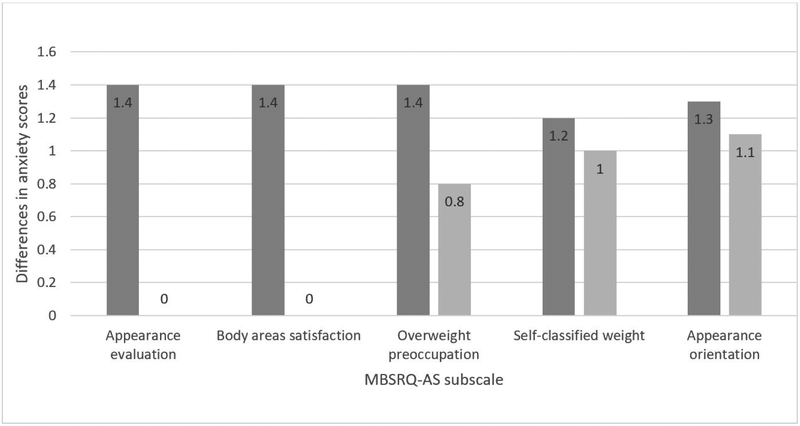
Depressive and anxiety symptom mediation by body image
After establishing the independent associations between PCOS, BID and depression/anxiety, we examined if the differences in anxiety and depression scores between women with PCOS and controls were mediated by MBSRQ subscales. The association between PCOS/control status and depressive symptoms was completely mediated (100%) by appearance evaluation and body areas satisfaction. For example, in models adjusted for age, BMI, race, pregnancy history and income, the differences between PCOS and controls in depressive symptom score went from being a score difference of 1.4 to becoming a score difference of 0 from mediation by appearance evaluation. It was partially mediated by Overweight Preoccupation (33%) and Weight Classification (20%) (Figure 1B). The association between PCOS/control status and higher anxiety scores was completely mediated (100%) by both appearance evaluation and body areas satisfaction, whereas it was partially mediated by the other subscales: Overweight Preoccupation (43%), Appearance Orientation (16.5%) and Self-Classified Weight (15%) (Figure 1C).
Figure 1B:
Path C: Mean depression score (HADS) differences between the PCOS and control groups before and after accounting for mediation by BID subscales.

Figure 1C:
Path C: Mean anxiety score (HADS) differences between the PCOS and control groups before and after accounting for mediation by BID subscales.

Association of FG score and BMI with MBSRQ-AS subscales in women with PCOS
When evaluating factors affecting body image distress in women with PCOS, we found that higher FG scores were significantly associated with lower appearance evaluation (p=0.04), lower body areas satisfaction (p=0.03) and higher overweight preoccupation (p=0.02). Higher BMI was significantly associated with lower appearance evaluation (p<0.01), lower body areas satisfaction (p<0.01), higher overweight preoccupation (p=0.03) and higher self-classified weight (p<0.01). The magnitudes of these associations were weak, (regression coefficients ranging from 0.02–0.06).
Discussion
The significant association of PCOS with psychological disorders,(14) led us to evaluate whether body image scores were different in women with PCOS and if body image distress mediated the relationship between depression, anxiety and PCOS. This is the largest study to date showing worse body image scores on all subscales of the MBSRQ-AS survey independent of known mediators such as obesity and race.(48) In addition, we report for the first time in the PCOS population greater differences between ideal and perceived images using the FRS survey, also indicative of body image distress. While women with PCOS were more likely to have abnormal depression and anxiety scores compared to controls, our study found that both depressive and anxiety symptoms were mediated in full by the appearance evaluation and body areas satisfaction subscales of the MBSRQ-AS. They were also partially mediated by the other three subscales, indicating a need to screen for BID in women with PCOS.
Although other studies have evaluated the relationship between PCOS and body image, they have been limited by several factors. Some lack comparative or control groups,(49, 50) others did not confirm the diagnosis of PCOS or used subject report of PCOS diagnosis which could result in misclassification bias, and others relied on self-report of BMI, which could result in reporting bias.(24, 25, 51) Our results for the MBSRQ-AS scales are similar to another large but primarily Caucasian cohort, although they reported significant differences in BMI between the PCOS and control groups.(23) Two previous studies described associations between body image and depression scores but they did not examine the extent to which aspects of body image mediate differences in anxiety and depression scores between the two groups.(23, 24)
The etiology for higher depression and anxiety scores in women with PCOS is unclear although a role for hyperandrogenemia and hyperinsulinemia has been suggested. In a meta-regression evaluating pooled standardized mean differences (SMDs) between groups, women with PCOS and concurrent depression had higher mean values of BMI and hirsutism scores, while women with PCOS and concurrent anxiety had higher mean values of BMI, hirsutism scores and free testosterone, although the effect size was small.(9) In a prospective cohort study of women with PCOS, multivariable logistic regression models demonstrated that women who had obesity at baseline had an increased depression risk at follow-up (OR 5.07; 95% Cl: 1.07, 24.0) compared to women with normal body weight.(52) A secondary analysis of a randomized controlled trial demonstrated that insulin resistance, which is more common in obesity and PCOS, was associated with increased odds of depression, after controlling for age and BMI.(53) In our study, FG score and BMI were weakly associated with lower body image scores as well. Given that physical features such as hirsutism and obesity impact body image, it is not surprising that body image distress also appears to correlate with anxiety and depression scores, as seen in our study and that by Deeks et al.(23) We found that negative appearance evaluation and body areas satisfaction mediated both anxiety and depression in women with PCOS.
Our study has several strengths. We confirmed use of Rotterdam criteria to establish the diagnosis of PCOS in all participants and used a prescreening questionnaire and chart review to confirm that controls did not have undiagnosed PCOS. There was no difference in the mean BMI between the two groups, and our study population included a racially and socio-economically diverse women allowing our findings to be generalizable. We also utilized previously validated surveys for body image, depression and anxiety that were analyzed in conjunction with a psychologist (KA). For example, the FRS has been validated in different languages(54) and has been used previously to examine body image distress in women of different races(55), with aging(37) and longitudinally(56). This survey has been used in one previous study of lean women with no significant FRS score differences found between PCOS women and controls.(57) We also attempted to account for possible medication effect on depression; for example, the percentages of women reporting depression medication or hormonal contraception use, which can both affect mood, were not different in the two groups.
However, our study has a few limitations as we only included a clinic based population of adult women. Controls reporting both hirsutism and irregular menses were excluded. As ultrasound and biochemical androgens are not routinely assessed in the control group, it is possible that some controls could have PCOS phenotypes C or D. The impact of this misclassification would be to bias results toward the null; therefore, our current results would be more conservative estimates. In addition, while we controlled for sociocultural variables including race, income and employment it is possible that there could be residual confounding due to unmeasured confounding factors as is possible with any observational study. We chose to frame the analysis as presented, i.e. assuming body image dissatisfaction as a predictor of depressive symptoms given previous evidence of its role as a significant mediator of depression among adolescent girls and adult women in both prospective and cross-sectional studies.(58–60) However, the cross-sectional design limits our ability to determine the temporality in the associations between BID and depression or anxiety scores.
Our study suggests the need for screening and counseling women with PCOS regarding the higher predisposition for BID and its association with other anxiety and depressive symptoms. Treatments for negative body image include cognitive behavioral therapy (CBT)(61), psychoeducation, stress management training, guided imagery, exposure exercises where positive thoughts about one’s body are accompanied by the feeling that the respective thoughts are true, and size-estimate exercises, where one estimates the size of the body part followed by objective measurement of that body part.(62) Given the known association of BID with obesity in the general population(58), treatment may need to also include lifestyle changes for weight management. In a pilot RCT in women with PCOS, an 8 week trial of CBT with lifestyle interventions was shown to result in improved weight loss and quality of life compared to lifestyle interventions alone(63), suggesting the benefit of combining various therapies. Care of women with PCOS must thus adopt a holistic approach and collaboration with nutritionists, endocrinologists and behavioral health specialists is essential in order to provide comprehensive care.
In summary, our study shows an increased prevalence of body image distress in a diverse population of women with PCOS. Moreover, BID was associated with depression and anxiety scores after accounting for multiple potential confounders including age, BMI, race and socioeconomic status. A significant finding of our study was that some aspects of body image distress either fully or partially mediated the differences in depression and anxiety scores between the two groups. Future studies should evaluate adolescents to better understand how early body image issues arise and follow subjects longitudinally to assess if early interventions to address body image issues decrease depressive and anxiety symptoms and improves quality of life in this population.
Supplementary Material
Supplementary Figure 1: Stunkard Figure Rating Scale and Questions
Funding:
Snigdha Alur-Gupta is supported by the NIH T32 Training Grant: HD007440. This source did not play any role in study design; in the analysis or interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Conflicts of interest: Dr. Allison reports personal fees from Weight Watchers International, grants from Novo Nordisk, outside the submitted work.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertil Steril 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Leo V, Musacchio MC, Cappelli V, Massaro MG, Morgante G, Petraglia F. Genetic, hormonal and metabolic aspects of PCOS: an update. Reprod Biol Endocrinol 2016; 14:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Franks S, McCarthy MI, Hardy K. Development of polycystic ovary syndrome: involvement of genetic and environmental factors. Int J Androl 2006;29:278–85; discussion 86–90. [DOI] [PubMed] [Google Scholar]
- 4.Palomba S, de Wilde MA, Falbo A, Koster MP, La Sala GB, Fauser BC. Pregnancy complications in women with polycystic ovary syndrome. Hum Reprod Update 2015;21:575–92. [DOI] [PubMed] [Google Scholar]
- 5.de Groot PC, Dekkers OM, Romijn JA, Dieben SW, Helmerhorst FM. PCOS, coronary heart disease, stroke and the influence of obesity: a systematic review and meta-analysis. Hum Reprod Update 2011; 17:495–500. [DOI] [PubMed] [Google Scholar]
- 6.Okoroh EM, Boulet SL, George MG, Craig Hooper W. Assessing the intersection of cardiovascular disease, venous thromboembolism, and polycystic ovary syndrome. Thromb Res 2015;136:1165–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dokras A, Clifton S, Futterweit W, Wild R. Increased risk for abnormal depression scores in women with polycystic ovary syndrome: a systematic review and meta-analysis. Obstet Gynecol 2011;117:145–52. [DOI] [PubMed] [Google Scholar]
- 8.Dokras A, Clifton S, Futterweit W, Wild R. Increased prevalence of anxiety symptoms in women with polycystic ovary syndrome: systematic review and meta-analysis. Fertil Steril 2012;97:225–30.e2. [DOI] [PubMed] [Google Scholar]
- 9.Cooney LG, Lee I, Sammel MD, Dokras A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod 2017;32:1075–91. [DOI] [PubMed] [Google Scholar]
- 10.Rowlands IJ, Teede H, Lucke J, Dobson AJ, Mishra GD. Young women’s psychological distress after a diagnosis of polycystic ovary syndrome or endometriosis. Hum Reprod 2016;31:2072–81. [DOI] [PubMed] [Google Scholar]
- 11.Hung JH, Hu LY, Tsai SJ, Yang AC, Huang MW, Chen PM et al. Risk of psychiatric disorders following polycystic ovary syndrome: a nationwide population-based cohort study. PLoS One 2014;9:e97041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kerchner A, Lester W, Stuart SP, Dokras A. Risk of depression and other mental health disorders in women with polycystic ovary syndrome: a longitudinal study. Fertil Steril 2009;91:207–12. [DOI] [PubMed] [Google Scholar]
- 13.Dokras A, Stener-Victorin E, Yildiz BO, Li R, Ottey S, Shah D et al. Androgen Excess-Polycystic Ovary Syndrome Society: position statement on depression, anxiety, quality of life, and eating disorders in polycystic ovary syndrome. Fertil Steril 2018;109:888–99. [DOI] [PubMed] [Google Scholar]
- 14.Dumesic DA, Oberfield SE, Stener-Victorin E, Marshall JC, Laven JS, Legro RS. Scientific Statement on the Diagnostic Criteria, Epidemiology, Pathophysiology, and Molecular Genetics of Polycystic Ovary Syndrome. Endocr Rev 2015;36:487–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dokras A Cardiovascular disease risk in women with PCOS. Steroids 2013;78:773–6. [DOI] [PubMed] [Google Scholar]
- 16.Bazarganipour F, Taghavi SA, Montazeri A, Ahmadi F, Chaman R, Khosravi A. The impact of polycystic ovary syndrome on the health-related quality of life: A systematic review and meta-analysis. Iranian journal of reproductive medicine 2015;13:61–70. [PMC free article] [PubMed] [Google Scholar]
- 17.Friedman KE, Reichmann SK, Costanzo PR, Musante GJ. Body image partially mediates the relationship between obesity and psychological distress. Obes Res 2002;10:33–41. [DOI] [PubMed] [Google Scholar]
- 18.Son N Assessment of body perception, psychological distress, and subjective quality of life among obese and nonobese subjects in Turkey. Niger J Clin Pract 2017;20:1302–8. [DOI] [PubMed] [Google Scholar]
- 19.Weinberger NA, Kersting A, Riedel-Heller SG, Luck-Sikorski C. Body Dissatisfaction in Individuals with Obesity Compared to Normal-Weight Individuals: A Systematic Review and Meta-Analysis. Obesity facts 2016;9:424–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sarwer DB, Thompson JK, Cash TF. Body image and obesity in adulthood. Psychiatr Clin North Am 2005;28:69–87, viii. [DOI] [PubMed] [Google Scholar]
- 21.Fallon EA, Harris BS, Johnson P. Prevalence of body dissatisfaction among a United States adult sample. Eating behaviors 2014;15:151–8. [DOI] [PubMed] [Google Scholar]
- 22.Sarwer DB, Cash TF. Body image: interfacing behavioral and medical sciences. Aesthet Surg J 2008;28:357–8. [DOI] [PubMed] [Google Scholar]
- 23.Deeks AA, Gibson-Helm ME, Paul E, Teede HJ. Is having polycystic ovary syndrome a predictor of poor psychological function including anxiety and depression? Hum Reprod 2011;26:1399–407. [DOI] [PubMed] [Google Scholar]
- 24.Himelein MJ, Thatcher SS. Depression and body image among women with polycystic ovary syndrome. J Health Psychol 2006; 11:613–25. [DOI] [PubMed] [Google Scholar]
- 25.Pastore LM, Patrie JT, Morris WL, Dalai P, Bray MJ. Depression symptoms and body dissatisfaction association among polycystic ovary syndrome women. J Psychosom Res 2011;71:270–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Annagur BB, Tazegul A, Akbaba N. Body Image, Self-Esteem and Depressive Symptomatology in Women with Polycystic Ovary Syndrome. Noro Psikiyatr Ars 2014;51:129–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. .Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril 2004;81:19–25. [DOI] [PubMed] [Google Scholar]
- 28.Brown TA, Cash TF, Mikulka PJ. Attitudinal body-image assessment: factor analysis of the Body-Self Relations Questionnaire. J Pers Assess 1990;55:135–44. [DOI] [PubMed] [Google Scholar]
- 29.Cash T The Multidimensional Body-Self Relations Questionnaire users’ manual, 2000. Available from the author at www.body-images.com 2016.
- 30.Cash TF. The great American shape-up: Body-image survey report. Psychol Today 1986;20:30–7. [Google Scholar]
- 31.Marco JH, Perpina C, Roncero M, Botella C. Confirmatory factor analysis and psychometric properties of the Spanish version of the Multidimensional Body-Self Relations Questionnaire-Appearance Scales in early adolescents. Body image 2017;21:15–8. [DOI] [PubMed] [Google Scholar]
- 32.Roncero M, Perpina C, Marco JH, Sanchez-Reales S. Confirmatory factor analysis and psychometric properties of the Spanish version of the Multidimensional Body-Self Relations Questionnaire-Appearance Scales. Body image 2015;14:47–53. [DOI] [PubMed] [Google Scholar]
- 33.Vossbeck-Elsebusch AN, Waldorf M, Legenbauer T, Bauer A, Cordes M, Vocks S. German version of the Multidimensional Body-Self Relations Questionnaire - Appearance Scales (MBSRQ-AS): confirmatory factor analysis and validation. Body image 2014;11:191–200. [DOI] [PubMed] [Google Scholar]
- 34.Stunkard AJ, Sorensen T, Schulsinger F. Use of the Danish Adoption Register for the study of obesity and thinness. Res Publ Assoc Res Nerv Ment Dis 1983;60:115–20. [PubMed] [Google Scholar]
- 35.Bulik CM, Wade TD, Heath AC, Martin NG, Stunkard AJ, Eaves LJ. Relating body mass index to figurai stimuli: population-based normative data for Caucasians. Int J Obes Relat Metab Disord 2001;25:1517–24. [DOI] [PubMed] [Google Scholar]
- 36.Thompson JK, Altabe MN. Psychometric qualities of the figure rating scale. Int J Eat Disord 1991;10:615–9. [Google Scholar]
- 37.Jackson KL, Janssen I, Appelhans BM, Kazlauskaite R, Karavolos K, Dugan SA et al. Body image satisfaction and depression in midlife women: the Study of Women’s Health Across the Nation (SWAN). Archives of women’s mental health 2014;17:177–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paans NPG, Bot M, Brouwer IA, Visser M, Penninx B. Contributions of depression and body mass index to body image. J Psychiatr Res 2018;103:18–25. [DOI] [PubMed] [Google Scholar]
- 39.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. [DOI] [PubMed] [Google Scholar]
- 40.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69–77. [DOI] [PubMed] [Google Scholar]
- 41.Barnard L, Ferriday D, Guenther N, Strauss B, Balen AH, Dye L. Quality of life and psychological well being in polycystic ovary syndrome. Hum Reprod 2007;22:2279–86. [DOI] [PubMed] [Google Scholar]
- 42.Lin CY, Ou HT, Wu MH, Chen PC. Validation of Chinese Version of Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (Chi-PCOSQ). PLoS One 2016;11:e0154343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Böttcher B, Fessier S, Friedl F, Toth B, Walter MH, Wildt L et al. Health-related quality of life in patients with polycystic ovary syndrome: validation of the German PCOSQ-G. Arch Gynecol Obstet 2018;297:1027–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jones GL, Benes K, Clark TL, Denham R, Holder MG, Haynes TJ et al. The Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ): a validation. Hum Reprod 2004;19:371–7. [DOI] [PubMed] [Google Scholar]
- 45.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Valente MJ, Pelham WE, Smyth H, MacKinnon DP. Confounding in statistical mediation analysis: What it is and how to address it. J Couns Psychol 2017;64:659–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Frazier P,P Tix A, Barron K. Testing Moderator and Mediator Effects in Counseling Psychology Research, 2004.
- 48.Kronenfeld LW, Reba-Harrelson L, Von Holle A, Reyes ML, Bulik CM. Ethnic and racial differences in body size perception and satisfaction. Body image 2010;7:131–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bazarganipour F, Ziaei S, Montazeri A, Foroozanfard F, Kazemnejad A, Faghihzadeh S. Predictive factors of health-related quality of life in patients with polycystic ovary syndrome: a structural equation modeling approach. Fertil Steril 2013;100:1389–96. [DOI] [PubMed] [Google Scholar]
- 50.Bazarganipour F, Ziaei S, Montazeri A, Foroozanfard F, Kazemnejad A, Faghihzadeh S. Body image satisfaction and self-esteem status among the patients with polycystic ovary syndrome. Iranian journal of reproductive medicine 2013; 11:829–36. [PMC free article] [PubMed] [Google Scholar]
- 51.Karacan E, Caglar GS, Gursoy AY, Yilmaz MB. Body satisfaction and eating attitudes among girls and young women with and without polycystic ovary syndrome. J Pediatr Adolesc Gynecol 2014;27:72–7. [DOI] [PubMed] [Google Scholar]
- 52.Greenwood EA, Pasch LA, Shinkai K, Cedars MI, Huddleston HG. Clinical course of depression symptoms and predictors of enduring depression risk in women with polycystic ovary syndrome: Results of a longitudinal study. Fertil Steril 2018. [DOI] [PubMed] [Google Scholar]
- 53.Greenwood EA, Pasch LA, Cedars MI, Legro RS, Eisenberg E, Huddleston HG. Insulin resistance is associated with depression risk in polycystic ovary syndrome. Fertil Steril 2018;110:27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Scagliusi FB, Alvarenga M, Polacow VO, Cordas TA, de Oliveira Queiroz GK, Coelho D et al. Concurrent and discriminant validity of the Stunkard’s figure rating scale adapted into Portuguese. Appetite 2006;47:77–82. [DOI] [PubMed] [Google Scholar]
- 55.Fitzgibbon ML, Blackman LR, Avellone ME. The relationship between body image discrepancy and body mass index across ethnic groups. Obes Res 2000;8:582–9. [DOI] [PubMed] [Google Scholar]
- 56.Lynch E, Liu K, Wei GS, Spring B, Kiefe C, Greenland P. The relation between body size perception and change in body mass index over 13 years: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Epidemiol 2009;169:857–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Morotti E, Persico N, Battaglia B, Fabbri R, Meriggiola MC, Venturoli S et al. Body imaging and sexual behavior in lean women with polycystic ovary syndrome. J Sex Med 2013;10:2752–60. [DOI] [PubMed] [Google Scholar]
- 58.Weinberger NA, Kersting A, Riedel-Heller SG, Luck-Sikorski C. The Relationship between Weight Status and Depressive Symptoms in a Population Sample with Obesity: The Mediating Role of Appearance Evaluation. Obesity facts 2018; 11:514–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bearman SK, Stice E. Testing a gender additive model: the role of body image in adolescent depression. J Abnorm Child Psychol 2008;36:1251–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Silveira ML, Ertel KA, Dole N, Chasan-Taber L. The role of body image in prenatal and postpartum depression: a critical review of the literature. Archives of women’s mental health 2015;18:409–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Butters JW, Cash TF. Cognitive-behavioral treatment of women’s body-image dissatisfaction. J Consult Clin Psychol 1987;55:889–97. [DOI] [PubMed] [Google Scholar]
- 62.Alleva JM, Sheeran P, Webb TL, Martijn C, Miles E. A Meta-Analytic Review of Stand-Alone Interventions to Improve Body Image. PLoS One 2015;10:e0139177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cooney LG, Milman LW, Hantsoo L, Kornfield S, Sammel MD, Allison KC et al. Cognitive-behavioral therapy improves weight loss and quality of life in women with polycystic ovary syndrome: a pilot randomized clinical trial. Fertil Steril 2018;110:161–71.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1: Stunkard Figure Rating Scale and Questions