Abstract
Background
Adults hospitalized with community-acquired pneumonia (CAP) are at high risk for short-term mortality. However, it is unclear whether improvements in in-hospital pneumonia care could substantially lower this risk. We extensively reviewed all in-hospital deaths in a large prospective CAP study to assess the cause of each death and assess the extent of potentially preventable mortality.
Methods
We enrolled adults hospitalized with CAP at five tertiary-care hospitals in the United States. Five physician investigators reviewed the medical record and study database for each patient who died to identify the cause of death, the contribution of CAP to death, and any preventable factors potentially contributing to death.
Results
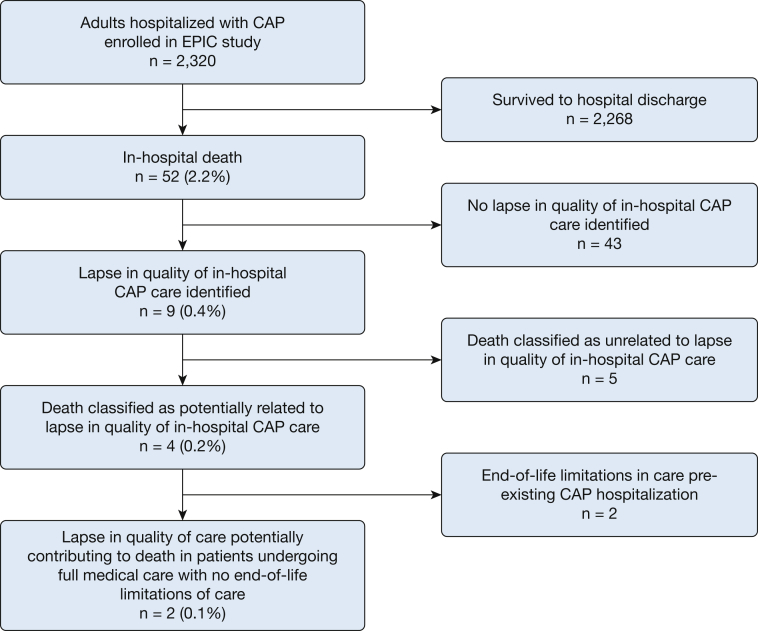
Among 2,320 enrolled patients, 52 (2.2%) died during initial hospitalization. Among these 52 patients, 33 (63.4%) were ≥ 65 years old, and 32 (61.5%) had ≥ two chronic comorbidities. CAP was judged to be the direct cause of death in 27 patients (51.9%). Ten patients (19.2%) had do-not-resuscitate orders prior to admission. Four patients were identified in whom a lapse in quality of care potentially contributed to death; preexisting end-of-life limitations were present in two of these patients. Two patients seeking full medical care experienced a lapse in in-hospital quality of pneumonia care that potentially contributed to death.
Conclusions
In this study of adults with CAP at tertiary-care hospitals with a low mortality rate, most in-hospital deaths did not appear to be preventable with improvements in in-hospital pneumonia care. Preexisting end-of-life limitations in care, advanced age, and high comorbidity burden were common among those who died.
Key Words: mortality, pneumonia, quality of care
Abbreviations: CAP, community-acquired pneumonia; DNR, do not resuscitate; EPIC, Etiology of Pneumonia in the Community; IRB, institutional review board
As a frequent cause of hospitalization and mortality, community-acquired pneumonia (CAP) has received significant attention from physicians, researchers, payers, and regulators.1, 2, 3, 4, 5, 6, 7 Understanding the circumstances in which patients with CAP die could facilitate improvements in the treatment of CAP by enabling future improvement efforts to focus on common preventable causes of death.
However, it is unclear whether improvements in in-hospital pneumonia care delivered to patients after they have received a diagnosis of CAP and been hospitalized could substantially reduce mortality in hospitals in the United States. Prior studies suggest that one-half of deaths among patients hospitalized with pneumonia are caused by nonpneumonia illnesses, and mortality is strongly associated with preexisting comorbid illnesses8, 9, 10, 11, 12, 13, 14, 15; hence, many of these deaths may not be preventable with improved adherence to current standards for acute pneumonia care. These prior studies were limited by small sample sizes, specific geographic regions, and retrospective designs.8, 9, 10, 11, 12, 13, 14, 15 Therefore, to further understand why patients admitted with CAP die in the hospital, we evaluated all in-hospital deaths in a large, population-based, prospective study of CAP in the United States to determine the cause of each death and the extent of preventable mortality.
Methods
This analysis was a secondary analysis of the Etiology of Pneumonia in the Community (EPIC) study funded by the Centers for Disease Control and Prevention.16 Adults hospitalized with CAP between January 2010 and June 2012 were enrolled at five tertiary-care hospitals, including three in Chicago (John H. Stroger, Jr. Hospital of Cook County, Northwestern Memorial Hospital, Rush University Medical Center) and two in Nashville (University of Tennessee Health Science Center-Saint Thomas Health, Vanderbilt University Medical Center). Institutional review board (IRB) approval was obtained at each site. IRB protocol numbers were as follows: Cook County, #09-163; Northwestern, #STU00019685; Rush, #09102105; Sterling IRB for Saint Thomas Health, #3476-001; and Vanderbilt, #091422. Written informed consent for study participation was obtained from each patient or an authorized representative.
Patient inclusion and exclusion criteria for the EPIC study have been described previously.16 Major inclusion criteria included clinical features of acute respiratory infection on hospital presentation, a chest radiograph or CT scan consistent with pneumonia, and hospital admission. Major exclusion criteria included recent hospitalization (< 28 days for immunocompetent patients and < 90 days for immunosuppressed patients), tracheotomy, gastric tube, cystic fibrosis, cancer with neutropenia, solid organ or stem cell transplantation in the prior 90 days, active graft-vs-host disease, bronchiolitis obliterans, and HIV infection with a CD4 cell count < 200/mm3. The EPIC study had no interventional component. Additional blood, urine, and respiratory specimens were collected to perform microbiologic diagnostic testing for research purposes; these results were not available to treating physicians. All patient treatment decisions were at the discretion of the treating physicians.
Using the EPIC study data set, we first assessed the clinical characteristics of patients who died in the hospital, and compared them with those of patients who survived to hospital discharge. For these comparisons, the following comorbidities were considered severe chronic comorbidities based on their association with increased mortality and ICU admission in previously developed CAP severity scores17, 18: chronic heart failure, COPD, coronary artery disease, chronic kidney disease, chronic liver disease, cerebrovascular disease, cancer (not including skin cancer), and diabetes mellitus. The rank-sum test and χ2 test were used for comparisons of continuous and dichotomous data, respectively.
In addition, the medical record and EPIC study database of each patient who died during the index CAP hospitalization were reviewed by a panel of five physician investigators at each study city with subspecialty expertise in pulmonary, critical care, infectious disease, and emergency medicine. Cause of death was assigned by the review panel according to criteria developed a priori on the basis of previously published trials.8, 19, 20 Each panelist reviewed cases with a standardized case report form that included these criteria (e-Appendix 1).
The following causes of death were considered directly related to CAP: septic shock, respiratory failure, multisystem organ failure, cardiopulmonary arrest prior to stabilization of CAP, and endocarditis (e-Appendix 1). The following causes of death were considered indirectly related to CAP: acute cardiovascular disease, stroke, acute renal failure, and secondary infections that developed after hospitalization. Causes of death indirectly related to CAP were further classified as CAP having a major or minor contribution to death. A major contribution indicated death would likely not have occurred without pneumonia, for example, a patient admitted with CAP who developed a myocardial infarction during the acute inflammatory phase of pneumonia and subsequently died of cardiac ischemia. A minor contribution indicated CAP was the primary reason for initial hospitalization but death was due to a cardiovascular, renal, or infectious event not immediately related to pneumonia, for example, a patient admitted with CAP who had a urinary catheter placed and then subsequently developed a catheter-associated urinary tract infection and died of urosepsis. Other causes of death, such as cancer, cirrhosis, and chronic neurologic conditions, were considered unrelated to CAP (e-Appendix 1).
Patient medical records were also systematically examined to determine whether treatment was consistent with current recommendations in quality-of-care metrics, including antibiotics consistent with the guidelines published by the Infectious Diseases Society of America (IDSA) and American Thoracic Society (ATS),21 antibiotics delivered within 6 h of presentation in the absence of shock and within 1 h in the presence of shock, and assessment of oxygenation by pulse oximetry or arterial blood gas analysis.
End-of-life limitations in care were also gathered by medical records review. An end-of-life limitation in care was defined as decisions by the patient and/or family to forego full medical treatment; this included do-not-resuscitate (DNR) orders, do-not-intubate (DNI) orders, as well as decisions to forego ICU admission or transfer, invasive procedures, or antibiotics.
After each panelist performed his/her reviews, all five panelists at each site participated in an in-person meeting to attribute the cause of death and identify potential lapses in quality of care for each case. Cases were discussed with the entire medical record available for review until a consensus of at least four of five panelists was reached.
Results
During the EPIC study, 3,634 eligible adults were identified, 2,488 (68%) were enrolled, and 2,320 (93% of enrolled) were confirmed to have radiographically confirmed CAP. Among all 2,320 adults in the final study population, 52 (2.2%) died during the CAP hospitalization. Among the 832 included patients ≥ 65 years old, 33 (4.0%) died during the hospitalization. Compared with patients who survived to hospital discharge, those who died were older and had more chronic comorbidities (Table 1). Among the 52 patients who died, 15 (28.9%) were between 65 and 79 years old, and 18 (34.6%) were ≥ 80 years old; 14 (26.9%) had two severe comorbidities, and 18 (34.6%) had ≥ three severe comorbidities. Most deaths (80.8%) occurred in patients with high-risk pneumonia severity index (PSI) scores (risk classes IV and V), but 10 deaths (19.2%) occurred in patients with low-to-moderate PSI scores (risk classes I-III).
Table 1.
Clinical Characteristics of Patients Who Died and Those Who Survived the Index Community-Acquired Pneumonia Hospitalization
| Characteristics | Died During Index Hospitalization (n = 52) | Survived Index Hospitalization (n = 2,268) | P Value |
|---|---|---|---|
| Female sex, No. (%) | 23 (44.2) | 1,167 (51.5) | .30 |
| Age, median (IQR), y | 71 (58-82) | 57 (46-71) | < .01 |
| Age group, No. (%), y | < .01 | ||
| 18-49 | 7 (13.5) | 694 (30.6) | |
| 50-64 | 12 (23.1) | 775 (34.2) | |
| 65-79 | 15 (28.9) | 502 (22.1) | |
| ≥ 80 | 18 (34.6) | 297 (13.1) | |
| Comorbidity, No. (%) | |||
| Chronic heart failure | 14 (26.9) | 426 (18.8) | .14 |
| COPD | 11 (21.1) | 518 (22.8) | .77 |
| Coronary artery disease | 25 (48.4) | 654 (28.8) | < .01 |
| Chronic kidney disease | 14 (26.9) | 352 (15.5) | .03 |
| Chronic liver disease | 5 (9.6) | 125 (5.5) | .20 |
| Cerebrovascular disease | 9 (17.3) | 129 (5.7) | < .01 |
| Cancer | 15 (28.9) | 401 (17.7) | .04 |
| Diabetes mellitus | 12 (23.1) | 585 (25.8) | .66 |
| No. of above comorbidities, No. (%) | .012 | ||
| 0 | 9 (17.3) | 778 (34.3) | |
| 1 | 11 (21.2) | 591 (26.1) | |
| 2 | 14 (26.9) | 408 (18.0) | |
| ≥ 3 | 18 (34.6) | 491 (21.6) | |
| Patient report of seasonal influenza vaccination, No. (%) | 30 (57.7) | 1,161 (51.2) | .35 |
| Patient report of pneumococcal vaccination in adults ≥ 65 y old, vaccinated/total (%) | 20/33 (60.6) | 482/799 (60.3) | .97 |
| CURB-65 score | < .01 | ||
| 0 | 9 (17.3) | 901 (39.7) | |
| 1 | 9 (17.3) | 695 (30.6) | |
| 2 | 12 (23.1) | 432 (19.1) | |
| 3 | 16 (30.8) | 211 (9.3) | |
| 4 | 6 (11.5) | 28 (1.2) | |
| 5 | 0 (0) | 1 (< 0.1) | |
| PSI risk class | < .01 | ||
| I | 3 (5.8) | 426 (18.8) | |
| II | 3 (5.8) | 614 (27.1) | |
| III | 4 (7.7) | 460 (20.3) | |
| IV | 25 (48.1) | 581 (25.6) | |
| V | 17 (32.7) | 187 (8.3) |
CURB-65 = confusion, urea nitrogen, respiratory rate, blood pressure, 65 years of age and older; IQR = interquartile range; PSI = pneumonia severity index.
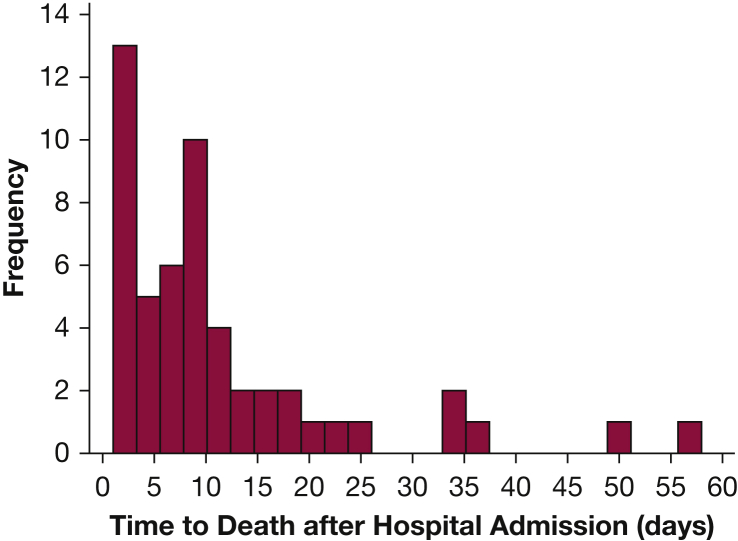
Among the 52 deaths, hypoxemic respiratory failure (25.0%) and septic shock (23.1%) were the most common causes of death (Table 2). The physician review panel classified 27 deaths (51.9%) to be directly from CAP, 10 (19.2%) with CAP having an indirect role with major contribution, nine (17.3%) with CAP having an indirect role with minor contribution, and six (11.5%) with CAP having no role in death (Table 3). DNR orders were present at the time of death for 21 patients (40.4%), including 10 with DNR orders entered before admission, eight after admission but more than 48 h prior to death, and three within 48 h of death. Most of the in-hospital deaths occurred early in the hospitalization, with 35 (67.3%) occurring within the first 10 days of admission, but five deaths (9.6%) occurred after 30 days in the hospital (Fig 1).
Table 2.
Causes of Death Among 52 Adults Hospitalized With Community-Acquired Pneumonia
| Cause of Death | No. (%) |
|---|---|
| Hypoxemic respiratory failure | 13 (25.0) |
| Septic shock | 12 (23.1) |
| Cancer | 5 (9.6) |
| Combined respiratory and cardiac failure | 5 (9.6) |
| Sudden death (cardiac arrest) | 5 (9.6) |
| Nosocomial pneumonia | 3 (5.8) |
| Cardiogenic shock | 2 (3.8) |
| Multisystem organ failure | 2 (3.8) |
| Stroke | 2 (3.8) |
| Chronic neuromuscular disorder | 1 (1.9) |
| Endocarditis | 1 (1.9) |
| Nosocomial sepsis (other than pneumonia) | 1 (1.9) |
Table 3.
Contribution of Pneumonia to Death Among 52 Adults Who Died During the Index Community-Acquired Pneumonia Hospitalization
| Contribution of Community-Acquired Pneumonia to Death | No. (%) |
|---|---|
| Direct cause of death | 27 (51.9) |
| Indirect cause of death with major contribution | 10 (19.2) |
| Indirect cause of death with minor contribution | 9 (17.3) |
| Unrelated to cause of death | 6 (11.5) |
Figure 1.
Timing of in-hospital death among 52 adults who died during the index hospitalization for community-acquired pneumonia.
Of the 52 patients who died in-hospital, 45 (86.5%) were admitted to an ICU, with 37 dying in the ICU and eight dying on the ward after transfer out of the ICU; all eight patients who died after transfer out of the ICU had end-of-life limitations of care in place. All seven patients not treated at all in an ICU and who died also had end-of-life limitations of care in place.
Among the 52 patients who died in-hospital, the physician review panel identified nine (17.3%) who had a lapse in quality of in-hospital CAP care (Table 4). Five of these nine deaths were judged as unrelated to the lapse in quality of care (Fig 2). Three of these five patients received antipneumococcal antibiotics but did not receive empiric antibiotics for atypical pathogens; none had an atypical pathogen identified by study protocol testing, and the review panel judged that these deaths were likely unrelated to the lack of atypical coverage. The other two patients had at least a 6-h delay between hospital presentation and the first dose of antibiotics in the absence of shock; both of these patients were receiving palliative care at the time of hospital presentation for conditions unrelated to pneumonia (stroke and advance chronic heart failure) and died of their underlying chronic comorbidity.
Table 4.
Lapses in Quality of In-Hospital Community-Acquired Pneumonia Care Among 52 Patients Who Died During the Index Hospitalization
| Quality Measure | Not Fulfilled: No. (%) |
|---|---|
| Empiric antibiotics consistent with IDSA/ATS CAP guidelines | 4 (7.7%) |
| First dose of antibiotics in < 6 h in the absence of shock | 2 (3.8%) |
| First dose of antibiotics in < 1 h in the presence of shock | 3 (5.7%) |
| Assessment of oxygenation on presentation | 0 (0%) |
ATS = American Thoracic Society; CAP = community-acquired pneumonia; IDSA = Infectious Diseases Society of America.
Figure 2.
Flow diagram outlining in-hospital deaths and lapses in quality of in-hospital care for adults hospitalized with community-acquired pneumonia. CAP = community-acquired pneumonia; EPIC = Etiology of Pneumonia in the Community study.
Among the nine patients with in-hospital death and a lapse in quality of in-hospital CAP care, the review panel identified four in whom a lapse could potentially have contributed to death (Fig 2). This included two patients with end-of-life limitations of care who presented with shock and had a delay to antibiotics greater than 1 h; both of these patients had metastatic cancer and decisions were made not to pursue ICU care at the time of admission. Thus, only two patients undergoing full medical treatment without end-of-life limitations of care had an identified lapse in quality of in-hospital pneumonia care potentially contributing to in-hospital death, including one with a delay in antibiotics for more than 1 h in the presence of shock and one with initial antibiotics not consistent with IDSA/ATS guidelines. In the first patient, pneumonia and shock were promptly identified, but IV access was delayed approximately 4 h from hospital presentation because of difficulties establishing a peripheral IV line, and antibiotics were not administered until a peripherally inserted central catheter was placed. In the second patient, the clinical team initially thought the patient had an intraabdominal source of infection and ciprofloxacin was the only antibiotic administered in the first 24 h of care; a chest radiograph at admission did not demonstrate signs of pneumonia, but a CT scan the next day was consistent with pneumonia.
Discussion
In a comprehensive review of all 52 in-hospital deaths in a prospective multicenter study of 2,320 adults hospitalized with CAP in five tertiary-care medical centers in the United States, we identified only two patients with a lapse in in-hospital pneumonia care potentially contributing to death. Consistent with other published reports,8, 22 we found that most in-hospital deaths among adult patients admitted with CAP in this study would not have been preventable with higher quality in-hospital pneumonia care. Many of the in-hospital deaths among patients admitted with CAP occurred in older patients with severe comorbidities and end-of-life limitations in care.
The influence of end-of-life limitations on care short of full palliation is an important finding in our study, with all patients who died outside the ICU having end-of-life limitations in care. Current Diagnosis-Related Group (DRG) and International Classification of Diseases (ICD) coding systems do not have the necessary nuances to capture these limitations of care, yet they are clearly important factors in determining whether patients experience in-hospital death. In many of these cases with limitations of care in place, the goal is not to prevent death, but to provide compassionate end-of-life care without subjecting patients to unwanted critical care. Although comparisons of mortality among different institutions and health care systems are commonly performed,23, 24 our study suggests that such comparisons are likely to be misleading if end-of-life limitations of care and preventability of death are not considered.
It was also notable that most (86.5%) of the patients who died in our study were admitted to an ICU, in contrast to European studies where most patients died without ICU care.25, 26 This discrepancy likely reflects cultural differences between the United States and Europe in the role of intensive care for patients with advanced age and/or advanced comorbid conditions, with patients in Europe being less likely to be admitted to an ICU during the final stages of fatal, chronic illnesses.27
Compared with earlier published data on the cause of death among patients admitted with pneumonia,8 we more frequently classified pneumonia as a direct or major contributor to death (71.2%). For example, using the Pneumonia Patient Outcomes Research Team (PORT) cohort from the 1990s, Mortensen et al8 reported that 53% of deaths were pneumonia-related among patients who died within 90 days of receiving a CAP diagnosis. A higher proportion of deaths in our study were judged as pneumonia-related, which likely reflects the shorter follow-up interval in our study (in-hospital vs 90 days) and an expanding view of how acute pneumonia can lead to cardiovascular complications due to systemic inflammation.28
The published literature, including this study, evaluating the association between the quality of in-hospital pneumonia care and mortality may be subject to publication bias. Hospitals with frequent lapses in the quality of pneumonia care may be less likely to publish mortality data. The five hospitals that participated in this study were all academic, urban US hospitals with extensive training programs and physician investigators specifically dedicated to studying CAP and providing high-quality pneumonia care.16 The low mortality rate and high compliance with pneumonia guidelines in this study may reflect specific expertise at these hospitals. The study’s findings may not be generalizable to other settings, such as other hospitals, other countries, or settings with higher CAP mortality rates. Additional research into pneumonia care and mortality in diverse settings is needed.
Our study also has additional limitations. In our review for deaths related to lapses in quality of in-hospital care, we did not consider new interventions that have not gathered enough supporting evidence to be adopted into pneumonia guidelines, such as antiplatelet therapy to prevent cardiovascular complications, corticosteroids as adjunctive therapy, and early mobilization.1 The 2.2% mortality rate in our study is low compared with some other studies and with mortality estimates outside of prospective studies.29, 30 A requirement for informed consent for participation in our prospective study may have led to nonenrollment of some patients at high risk of death. Finally, determining which deaths may have been preventable can be subjective. To minimize this concern, we used a standardized case report form for records review, a multidisciplinary panel of five experienced physicians to review cases together, and adjudicated cases by consensus.
In summary, in our study of CAP at five US hospitals with expertise in pneumonia care and a relatively low mortality rate, we found that most in-hospital deaths were likely not preventable with current medical therapy after admission. Preexisting end-of-life limitations in care, advanced age, and a high comorbidity burden were common in patients who died in our study. To more fully understand how and why patients with CAP die, we suggest future studies in diverse settings that carefully note whether death was due to pneumonia or other causes, whether care delivered was consistent with international guidelines, the presence and severity of comorbidities, and whether end-of-life limitations of care were in place at the time of CAP admission.
Acknowledgments
Author contributions: G. W. W. takes responsibility for the manuscript as a whole. Study concept and design: G. W. W., W. H. S., R. G. W.; acquisition of data: G. W. W., W. H. S., D. M. C., C. G. G., R. A. B., T. D. G., S. S. F., C. T., P. McN., E. J. A., D. J. W., K. M. E., R. G. W.; statistical analysis: G. W. W., W. H. S.; interpretation of data: G. W. W., W. H. S., D. M. C., C. G. G., R. A. B., T. D. G., S. S. F., C. T., P. McN., E. J. A., D. J. W., A. M. B., S. J., K. M. E., R. G. W.; drafting of the initial manuscript: G. W. W., W. H. S.; critical revision of manuscript: all authors; obtained funding: K. M. E., R. G. W.; study supervision: G. W. W., W. H. S., S. J., K. M. E., R. G. W.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: W. H. S. reports consulting fees from Abbott Point of Care, Ferring Pharmaceuticals, Cempra Pharmaceuticals, and BioTest AG. E. J. A. reports a consulting fee from AbbVie and research funding from MedImmune, Regeneron, and Novavax. None declared (G. W. W., D. M. C., C. G. G., R. A.B., T. D. G., S. S. F., C. T., P. McN., D. J. W., A. M. B., S. J., K. M. E., R. G. W.).
Role of sponsors: The sponsors had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Other contributions: The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Additional information: The e-Appendix can be found in the Supplemental Materials section of the online article.
Footnotes
FUNDING/SUPPORT: This work was supported by a cooperative agreement with the Centers for Disease Control and Prevention [Grant U18 IP000299]. W. H. S. was supported in part by the National Institute of General Medical Sciences [Grant K23GM110469]. C. G. G. was supported in part by the National Institute on Aging [Grant R01AG043471].
Supplementary Data
References
- 1.Waterer G., Bennett L. Improving outcomes from community-acquired pneumonia. Curr Opin Pulm Med. 2015;21(3):219–225. doi: 10.1097/MCP.0000000000000155. [DOI] [PubMed] [Google Scholar]
- 2.Australian Commission on Safety and Quality in Health Care (ACSQHC) ACSQHC; Sydney, Australia: 2014. Using Hospital Mortality Indicators to Improve Patient Care: A Guide for Boards and Chief Executives.https://www.safetyandquality.gov.au/wp-content/uploads/2015/03/Using-hospital-mortality-indicators-to-improve-patient-care-A-guide-for-Boards-and-Chief-Executives.pdf Accessed April 3, 2018. [Google Scholar]
- 3.Clinical Indicators Team, NHS Digital. Summary Hospital Level Mortality Indicator (SHMI)—Deaths Associated With Hospitalisation, England, April 2016-March 2017: Background Quality Report. Published September 21, 2017. https://files.digital.nhs.uk/21/E79BD7/SHMI%20background%20quality%20report%2C%20Apr16-Mar17.pdf. Accessed April 3, 2018.
- 4.Johnstone J., Mandell L. Guidelines and quality measures: do they improve outcomes of patients with community-acquired pneumonia? Infect Dis Clin North Am. 2013;27(1):71–86. doi: 10.1016/j.idc.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Joint Commission on Accreditation of Healthcare Organization A Comprehensive Review of Development and Testing for National Implementation of Hospital Core Measures. https://www.jointcommission.org/assets/1/18/A_Comprehensive_Review_of_Development_for_Core_Measures.pdf Accessed November 26, 2017.
- 6.Alexandrescu R., Bottle A., Hua Jen M., Jarman B., Aylin P. The US hospital standardised mortality ratio: retrospective database study of Massachusetts hospitals. JRSM Open. 2015;6(1) doi: 10.1177/2054270414559083. 2054270414559083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jarman B., Bottle A., Aylin P., Browne M. Monitoring changes in hospital standardised mortality ratios. BMJ. 2005;330(7487):329. doi: 10.1136/bmj.330.7487.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mortensen E.M., Coley C.M., Singer D.E. Causes of death for patients with community-acquired pneumonia: results from the Pneumonia Patient Outcomes Research Team cohort study. Arch Intern Med. 2002;162(9):1059–1064. doi: 10.1001/archinte.162.9.1059. [DOI] [PubMed] [Google Scholar]
- 9.Soto-Gomez N., Anzueto A., Waterer G.W., Restrepo M.I., Mortensen E.M. Pneumonia: an arrhythmogenic disease? Am J Med. 2013;126(1):43–48. doi: 10.1016/j.amjmed.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perry T.W., Pugh M.J., Waterer G.W. Incidence of cardiovascular events after hospital admission for pneumonia. Am J Med. 2011;124(3):244–251. doi: 10.1016/j.amjmed.2010.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramirez J., Aliberti S., Mirsaeidi M. Acute myocardial infarction in hospitalized patients with community-acquired pneumonia. Clin Infect Dis. 2008;47(2):182–187. doi: 10.1086/589246. [DOI] [PubMed] [Google Scholar]
- 12.Musher D.M., Rueda A.M., Kaka A.S., Mapara S.M. The association between pneumococcal pneumonia and acute cardiac events. Clin Infect Dis. 2007;45(2):158–165. doi: 10.1086/518849. [DOI] [PubMed] [Google Scholar]
- 13.Carr G.E., Yuen T.C., McConville J.F., American Heart Association’s Get With the Guidelines-Resuscitation (National Registry of CPR) Investigators Early cardiac arrest in patients hospitalized with pneumonia: a report from the American Heart Association’s Get With the Guidelines-Resuscitation Program. Chest. 2012;141(6):1528–1536. doi: 10.1378/chest.11-1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simpson J.C., Macfarlane J.T., Watson J., Woodhead M.A., British Thoracic Society Research Committee and Public Health Laboratory Service A national confidential enquiry into community acquired pneumonia deaths in young adults in England and Wales. Thorax. 2000;55(12):1040–1045. doi: 10.1136/thorax.55.12.1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marrie T.J. Deaths in risk classes I-III: a measure of quality of care in patients hospitalised with CAP? Eur Respir J. 2004;23(1):103–105. doi: 10.1183/09031936.03.00072803. [DOI] [PubMed] [Google Scholar]
- 16.Jain S., Self W.H., Wunderink R.G. Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med. 2015;373(5):415–427. doi: 10.1056/NEJMoa1500245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fine M.J., Auble T.E., Yealy D.M. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336(4):243–250. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 18.Renaud B., Labarere J., Coma E. Risk stratification of early admission to the intensive care unit of patients with no major criteria of severe community-acquired pneumonia: development of an international prediction rule. Crit Care. 2009;13(2):R54. doi: 10.1186/cc7781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ranieri V.M., Thompson B.T., Barie P.S. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366(22):2055–2064. doi: 10.1056/NEJMoa1202290. [DOI] [PubMed] [Google Scholar]
- 20.Crouch Brewer S., Wunderink R.G., Jones C.B., Leeper K.V., Jr. Ventilator-associated pneumonia due to. Pseudomonas aeruginosa. Chest. 1996;109(4):1019–1029. doi: 10.1378/chest.109.4.1019. [DOI] [PubMed] [Google Scholar]
- 21.Mandell L.A., Wunderink R.G., Anzueto A. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–S72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stefan M.S., Jaber R., Lindenauer P.K., Garb J.L., Fitzgerald J., Rothberg M.B. Death among patients hospitalized with pneumonia: implications for hospital outcome measures. JAMA Intern Med. 2015;175(5):851–853. doi: 10.1001/jamainternmed.2015.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Medicare and Medicaid Services. Hospital Compare.https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalCompare.html. Last updated October 19, 2016. Accessed June 13, 2017.
- 24.Drye E.E., Normand S.L., Wang Y. Comparison of hospital risk–standardized mortality rates calculated by using in-hospital and 30-day models: an observational study with implications for hospital profiling. Ann Intern Med. 2012;156(1 part 1):19–26. doi: 10.1059/0003-4819-156-1-201201030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chalmers J.D., Taylor J.K., Mandal P. Validation of the Infectious Diseases Society of America/American Thoracic Society minor criteria for intensive care unit admission in community-acquired pneumonia patients without major criteria or contraindications to intensive care unit care. Clin Infect Dis. 2011;53(6):503–511. doi: 10.1093/cid/cir463. [DOI] [PubMed] [Google Scholar]
- 26.Kolditz M., Bauer T., Konig T., Rohde G., Ewig S. 3-day mortality in hospitalised community-acquired pneumonia: frequency and risk factors. Eur Respir J. 2016;47(5):1572–1574. doi: 10.1183/13993003.00113-2016. [DOI] [PubMed] [Google Scholar]
- 27.Bekelman J.E., Halpern S.D., Blankart C.R. Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA. 2016;315(3):272–283. doi: 10.1001/jama.2015.18603. [DOI] [PubMed] [Google Scholar]
- 28.Singanayagam A., Singanayagam A., Elder D.H., Chalmers J.D. Is community acquired pneumonia an independent risk factor for cardiovascular disease? Eur Respir J. 2012;39(1):187–196. doi: 10.1183/09031936.00049111. [DOI] [PubMed] [Google Scholar]
- 29.Ramirez J.A., Wiemken T.L., Peyrani P. Adults hospitalized with pneumonia in the United States: incidence, epidemiology, and mortality. Clin Infect Dis. 2017;65(11):1806–1812. doi: 10.1093/cid/cix647. [DOI] [PubMed] [Google Scholar]
- 30.Valley T.S., Sjoding M.W., Ryan A.M., Iwashyna T.J., Cooke C.R. Association of intensive care unit admission with mortality among older patients with pneumonia. JAMA. 2015;314(12):1272–1279. doi: 10.1001/jama.2015.11068. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.