Abstract
A large body of work links parental sick role reinforcement behavior to adolescent panic vulnerability. To date, however, little work has examined the role of the adolescent in this process. The current study addressed this gap in the literature, using a novel method to experimentally test the impact of adolescent anxiety during a straw-breathing task on parental propensity to engage in sick role reinforcement behavior. An unselected sample of 51 early adolescents (26 female, 10–14 years) and their parents participated in the study. Adolescents were trained to mimic a straw-breathing task, and adolescent reactions to the task were scripted. Parents were randomly assigned to watch their adolescent react either a) anxiously or b) non-anxiously to the straw-breathing task. Parents who viewed their adolescent react anxiously ended the task earlier, reported that they would reinforce more sick role behavior, and reported more negatively valenced reactions during the task than parents who viewed their adolescent react non-anxiously to the task. No group differences emerged in terms of parental self-reported or physiological arousal during the task. Results suggest that adolescent anxiety increases parental sick role reinforcement behavior. Findings are discussed in terms of future directions for reducing parenting behaviors thought to increase vulnerability for panic among adolescents.
Keywords: Adolescents, Bidirectional, Parenting, Anxiety, Panic, Sick role reinforcement
1. Introduction
Scholars have highlighted the need for constructing etiological models of panic disorder that include developmental factors that may increase risk for panic symptomology (e.g., Craske, 2003). This is a pressing concern, as panic and related complaints are associated with high societal costs and impairment (Lépine, 2002), begin early in life, and have a chronic course (Kessler, Alonso, Chatterji, & He, 2014). For example, evidence suggests that adults with panic disorder tend to unnecessarily utilize high-cost health care resources (e.g., a panic attack leads to a costly trip to the emergency room; Buccelletti et al., 2013; Lynch & Galbraith, 2003). Further, these processes begin early in life. Evidence from the Netherlands suggest that families with anxious offspring spend 21 times as much on healthcare as families with non-anxious offspring (Bodden, Dirksen, & Bogels, 2008). For this reason, it is critical to consider factors that may increase panic-related vulnerability early in life. The current paper seeks to better understand the link between adolescents’ description of their bodily experiences and parental responses that may engender panic vulnerability in offspring.
Adolescence is a core-risk period for the onset of panic attacks (Beesdo, Knappe, & Pine, 2009). This may be due, in part, to the onset of puberty. Although puberty itself is not a risk factor for psychopathology, as it is a normative developmental process, it is nonetheless a sensitive period during which there is an increased likelihood that anxiety and related symptoms will develop among vulnerable youth (Reardon, Leen-Feldner, & Hayward, 2009). Indeed, among youth vulnerable by virtue of anxiety sensitivity, advancing pubertal status predicts increased anxious reactivity to bodily arousal (Leen-Feldner et al., 2006). Primary and secondary sexual characteristics typically emerge in early-to mid-adolescence (i.e., between 10 and 14 years) with most youth in this age range experiencing the physiological and hormonal changes that characterize puberty (Herman-Giddens, 2007; Susman & Rogol, 2004). Consequently, the emergence of new, ambiguous bodily sensations is common during this developmental window, making it a fecund phase in which to examine panic-related processes.
Learning theories of panic suggest that the repeated pairing of bodily sensations (e.g., racing heart, sweating palms) with fear results in a classically conditioned association between somatic arousal and fear (Bouton, Mineka, & Barlow, 2001). Over time, bodily sensations come to elicit increasing anxious arousal and ultimately, for some, panic attacks. Operant contingencies maintain avoidance of bodily arousal and limit opportunities for extinction learning (Craske, Treanor, Conway, Zbozinek, & Vervliet, 2014; Mowrer, 1960). Key socializing agents, such as parents, are theorized to facilitate these learning processes among offspring (Watt, Stewart, & Cox, 1998). Consistent with this perspective, research suggests that parents can facilitate fear of bodily arousal among offspring, via vicarious conditioning, verbal transmission of information, as well as positive and negative reinforcement (Ehlers, 1993; Leen-Feldner, Blumenthal, Babson, Bunaciu, & Feldner, 2008; Stewart et al., 2001; Watt & Stewart, 2000; Watt et al., 1998). For instance, if a parent responds repeatedly to an adolescent female’s somatic complaints (e.g., gastrointestinal distress) by becoming visibly distressed, telling her the symptoms could be dangerous, or allowing her to skip an aversive after-school activity, she develops a learning history that may increase panic risk. Notably, adolescent reports of parental “sick role reinforcement” (i.e., rewarding behavior consistent with reporting/focusing on somatic perturbation) are associated with elevated psychological vulnerabilities for panic (anxiety sensitivity) and panic symptoms (Knapp, Frala, Blumenthal, Badour, & Leen-Feldner, 2013). Further, experimental evidence suggests parental modeling of anxious behavior in response to bodily arousal (vicarious conditioning) increases adolescent offspring escape behavior in response to bodily arousal (Bunaciu et al., 2014). Taken together, evidence converges to suggest that parental behavior in the context of somatic perturbation is important to consider as a factor that could increase adolescent panic-related vulnerability.
Few studies have examined the role of adolescents in influencing how parents respond to reports of bodily arousal. This relative neglect is unfortunate, because a large body of work suggests youth influence the parenting they receive (i.e., offspring-driven effects; O’Connor, 2002). Critically, adolescence is a developmental period characterized by a modest re-negotiation of the parent-child relationship (Laursen & Collins, 2009) in which youth seek to more directly influence the outcome of parent-child interactions (Wray-Lake, Croute, & McHale, 2010). Indeed, evidence suggests that adolescent anxiety influences parenting behavior. For example, experimental and behavioral genetic work indicates that mothers demonstrate more overinvolved behavior with anxious as compared to non-anxious children and early adolescents (Eley, Napolitano, Lau, & Gregory, 2010; Hudson, Doyle, & Gar, 2009). Given the profound bodily changes that characterize adolescence (Whitehead, Busch, Heller, & Costa, 1986), offspring-driven effects may be particularly relevant in the context of sick role reinforcement behavior. Specifically, adolescents’ descriptions of their somatic experiences may influence parenting behavior. For example, parents may be more inclined to encourage sick role behavior (e.g., staying home from school, providing special attention) if an adolescent describes benign somatic symptoms as anxiety provoking (e.g., “I feel lightheaded, and I’m worried that I am going to pass out.”) as compared to an adolescent who reports symptoms in a non-anxious manner (e.g., “I feel lightheaded …. But I doubt it’s anything to worry about.”). Indeed, in a recent study, when parents read a vignette in which they were asked to imagine their adolescent offspring describing ambiguous physical sensations anxiously, parents reported that they would reinforce significantly more sick role behavior than when they read a vignette in which they were asked to imagine that their offspring described ambiguous physical sensations non-anxiously (Bilsky, Feldner, Bynion, Rojas, & Leen-Feldner, 2018).
Finally, although a limited body of research has examined parental behavior in response to adolescent anxiety, no work has examined parental affect as a function of adolescent anxiety. This gap needs to be addressed; if offspring displays of anxiety increase parental distress, then aspects of the parent’s affective experience, such as distorted thinking and cognitive-behavioral efforts to manage the distress, may drive parental interactions with their child (e.g., Ginsburg, Silberman, & Kurtines, 1995). Indeed, theoretical work suggests that if parents become distressed in the presence of offspring anxiety, they may engage in maladaptive parenting behavior designed to improve their own affect (e.g., Moore, Whaley, & Sigman, 2004; Wood, McLeod, Piacentini, & Sigman, 2009). However, empirical support for this perspective has been modest. For instance, recent work suggests maternal anxiety disorder status does not influence parenting behavior (e.g., over-involvement or criticism) in the context of an adolescent social threat task (Gar & Hudson, 2008). Of note, the work to date has not examined real-time parental distress as a function of offspring display of anxiety where more subtle differences may be observed. Indeed, examining the impact of adolescent anxiety on real-time parental distress may help inform models of youth anxiety psychopathology in which shared genetic vulnerabilities and reciprocal parent-offspring influences shape the development and course of anxiety (Rapee, Schniering, & Hudson, 2009).
Taken together, there is emerging evidence to suggest adolescents influence parental behavior, including sick role reinforcement, as a function of how adolescent bodily sensations are reported. However, there is neither experimental nor correlational research evaluating the impact of real time adolescent descriptions of ambiguous bodily sensations on parental sick role reinforcement behavior and distress. The current study sought to address these limitations, by experimentally examining whether adolescents’ descriptions of bodily sensations elicited by a straw-breathing task affected these parenting outcomes. A novel experimental manipulation was employed in which adolescents were trained to mimic a straw-breathing task; then their reactions to the task were scripted (anxious or non-anxious) and presented to their parents. It was hypothesized that, parents who observed their adolescent react anxiously (c.f. non-anxiously) would evidence elevated parental sick role reinforcement operationalized as a) decreased latency to behaviorally intervene to address offspring concerns and b) self-reported endorsement of sick role reinforcement behavior (e.g., telling your child to go lay down). Further, in terms of parental distress during the task, it was hypothesized that parents would a) report progressively more negatively valenced affect, b) report progressively more affective arousal, and c) evidence progressively increased physiological responding in the presence of offspring anxious reactions than in the presence of offspring non-anxious reactions. Although the current study design (which allows parents to “escape” the task) precludes testing the full mediation model (i.e., parental distress mediating the relation between adolescent anxiety and sick role reinforcement behavior), measuring the effects of the experimental manipulation on a hypothesized intervening variable (e.g., parental distress) will provide initial evidence for parental distress as a putative link in the causal chain between adolescent anxiety and parental behavior (Kraemer, Stice, Kazdin, Offord, & Kupfer, 2001).
2. Method
2.1. Participants
Dyads consisting of parents with adolescents between the ages of 10 and 14 years old were recruited from the local community via radio-based advertising, flyers, and recruitment booths set up at various events. Other than offspring age, there were no other inclusion criteria. Exclusion criteria for offspring in the study were as follows: a) chronic cardiovascular illness (e.g. asthma); b) acute respiratory illness (e.g., bronchitis); c) possible pregnancy (by self-report); d) inability to read or write. Parental medical and psychological history was not included as exclusionary criteria, as parents would not be instructed to undergo a full voluntary hyperventilation. Consistent with previous work (Whaley, Pinto, & Sigman, 1999), if families had multiple children who were eligible for the study, the adolescent whose age was closest to the middle of the target range (i.e., 12 years old) was selected to participate in the study.
Fifty-three dyads completed the protocol. Two dyads were excluded from all analyses, due to the adolescents’ failure to comply with the experimental manipulation training. One dyad was excluded from the “latency to quit task” analyses due to experimenter error, in which the parent was allowed to quit the study due to boredom, rather than distress. The final sample was 51 parents (43 mothers) and their adolescent offspring (25 males) between the ages of 10 and 14 years (Mage = 12.20 years, SD = 1.19 years). Physiological data were missing for nine participants due to equipment malfunction or problematic levels of data artifacts resulting from participant movement. Data for these participants were included in the self-report analyses and excluded from analyses employing physiological data. Racial and ethnic composition of the sample reflected the local community (Southern Midwestern United State, U.S. Bureau of the Census, 2010): approximately 74.5% Caucasian, 5.9% Asian, 3.9% African American, 2.0% Native American, 11.8% more than one race, 2.0% “other.” In terms of ethnicity, 2 adolescents (3.9% of the sample) identified as Hispanic. Most parents (90.2%) identified as Caucasian and as being the primary caretaker for their offspring (n = 50, 98%). Notably, anxiety and depressive symptom levels in this sample were examined and found to be in the non-clinical range. Similarly, we evaluated parent-reported adolescent physical health problems and found this factor did not influence the pattern of results.
2.2. Parent measures
2.2.1. Demographics
Parents completed a series of standard demographic questions (i.e., age, gender, race/ethnicity, income, marital and caregiver status).
2.2.2. Anxiety Sensitivity Index-3 (ASI-3)
The ASI-3 is an 18-item questionnaire that measures fear of the consequences of anxiety (Taylor et al., 2007). Participants answer questions such as, “It scares me when my heart races,” on a five-point scale (0 = very little to 4 = very much). Items are summed with higher scores indicating higher global AS levels. The ASI-3 evidences strong psychometric properties (e.g., Cronbach α = 0.94, current study; Taylor et al., 2007).
2.2.3. Positive and Negative Affect Schedule (PANAS)
General negative affectivity was measured using the negative affect subscale of the PANAS (PANAS-NA; Watson, Clark, & Tellegen, 1988). Participants rate the extent to which they generally experience each of 10 descriptors (e.g., distressed, upset) on a 5-point scale (0 = Very Slightly to 4 = Extremely) over the past few weeks. Consistent with prior work supporting the psychometrics of the PANAS, excellent internal consistency was observed in the current study (α = 0.91).
2.2.4. Behavioral sick role reinforcement
Parent’s latency to end offspring participation in the straw-breathing task was utilized as a behavioral index of sick role reinforcement behavior. Parental latency to end the task was employed to reflect parental tendency to facilitate escape behavior in the presence of interoceptive arousal among adolescents, a behavior that might be maintained in the face of subsequent interoceptive arousal via negative reinforcement. It was operationally defined as the number of rounds of the straw-breathing task parents observed before ending the task. Scores ranged from 1 to 10, with lower scores reflecting shorter latencies and a swifter tendency to facilitate escape behavior/reinforce sick role behaviors in their offspring.
2.2.5. Self-reported sick role reinforcement
A self-report measure of sick role reinforcement was adapted for this study from a measure utilized in prior, published work (Bilsky et al., 2018). It is included in Appendix A. Immediately after parents observed their adolescent engage in a straw-breathing task, parental sick role reinforcement was measured by asking parents to rate how likely they would be to encourage sick role behavior. Parents rated each of 6 items (e.g., “tell them to go lay down,”) using a 5-point Likert-type scale (1 = Very Unlikely to 5 = Very Likely). A total score for sick role reinforcement behavior was computed by averaging the 6 items (scores ranged from 6 to 30; α = 0.80). Importantly, convergent validity of this measure is supported by a positive correlation with a conceptually-relevant index of parent’s negative beliefs about their child’s anxiety (e.g., “it scares me when my child is nervous,” r = 0.428, p = .002, PBA-Q; Francis & Chorpita, 2010).
2.2.6. Self Assessment Manikin (SAM)
The SAM (Lang, 1980) was used to measure parental affective responding to observing offspring complete the straw-breathing task. Factor analytic research indicates that the SAM measures two core features of affect: valence (scale 1) and arousal (scale 2; Lang, 1984). Each scale has five human-like figures. For example, the valence scale has five figures with different expressions of emotional valence, the figure on the farthest left has a “smile” while the figure on the farthest right has a “frown.” For the arousal scale, the figure on the farther left appears to be exploding, while the figure on the farthest right appears to be asleep. Each scale yields a rating of 0–9 by having participants mark on or between figures with lower scores representing more positive valence or higher levels of arousal. The SAM is a well-established measure with strong psychometric properties (Lang, 1984; Leen-Feldner et al., 2008; Olatunji, Wolitzky-Taylor, Babson, & Feldner, 2009).
2.2.7. Heart rate
In order to assess parental physiological response to observing their offspring complete the straw-breathing task, parental heart rate was collected continuously throughout the task. Heart rate was measured using a Biopac MP150 data acquisition system (Biopac Systems Inc, Goleta, CA). Heart rate was based on R-peaks that were collected by electrocardiogram (ECG) recordings from two Ag/AgCl electrodes placed on the upper right torso and below the left rib in a Lead II formation. Physiological data were visually inspected for problematic signals (e.g., poor signal due to excessive movement, recording noise, electrode connectivity problems), and problematic data were filtered prior to analyses. Nine recordings were completely removed from physiological analyses, in contrast; only small sections (e.g., 2 s or less) of data were removed from other recordings. Raw ECG data was used to calculate average heart rate across in 1-min increments across the experimental procedure. The 2-min of physiological data collected prior to the commencement of the procedure were averaged to compute baseline heart rate. During the baseline procedure, parents were seated in front of a computer and asked to wait quietly for the experiment to begin.
2.3. Offspring measures
2.3.1. Demographics
Adolescent offspring were asked to complete standard demographic questions (i.e., age, gender, race/ethnicity, grade).
2.3.2. Childhood Anxiety Sensitivity Index (CASI)
The 18-item CASI (Silverman, Fleisig, Rabian, & Peterson, 1991) was used to assess offspring anxiety sensitivity. The CASI is an 18-item measure on which participants use a 3-point scale (1 = None, 2 = Some, 3 = A lot) to answer questions such as “it scares me when my heart beats fast.” Items are summed to yield global AS level scores (Silverman et al., 1991; Wright, London, & Field, 2011). Prior work supports the validity and reliability of the CASI; the internal consistency estimate for the global factor from the current study also aligned with previously published work (α = 0.74; Graham & Weems, 2015; Knapp et al., 2013).
2.3.3. Positive and Negative Affect Schedule – child version (PANAS-C)
The negative affectivity subscale of the PANAS-C (PANAS-C-NA; Laurent et al., 1999) was used to measure general negative affect. For each of the 15 descriptors (e.g., upset, nervous, afraid), adolescents rated how often they had experienced each during the past several weeks using a 5-point scale ranging from 1 (very slightly or not at all) to 5 (extremely). The psychometrics of the PANAS-C are strong, and excellent internal consistency was obtained in the current study (α = 0.91).
2.4. Procedure
The local institutional review board (IRB) approved the procedure prior to data collection. Interested parents and adolescents who contacted the laboratory were administered a brief phone screener to determine whether participants met initial study eligibility criteria. Eligible parents and adolescents were invited to attend a 2-h laboratory session. Written and verbal assent and consent were required for participation in the study, and were obtained prior to the commencement of data collection. During the consent and assent procedure, parents and adolescents were informed that the goal of the procedure was to examine associations between parent and adolescent response to a breathing task. Next, parents and adolescents were escorted to separate private rooms to complete baseline self-report measures then prepared for the experimental task.
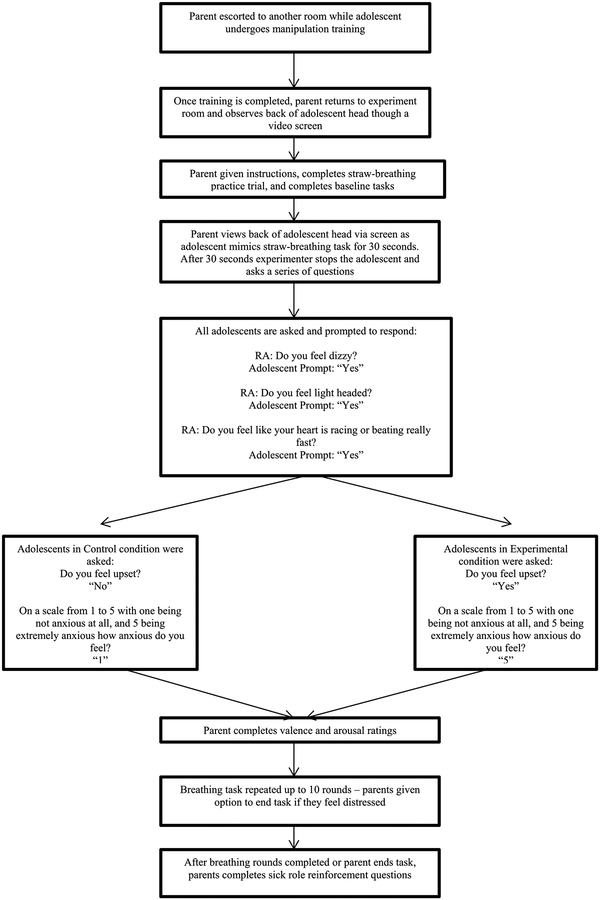
2.4.1. Experimental manipulation
Fig. 1 presents an overview of the study procedures. Without parents’ knowledge, a research assistant, blind to condition, administered a standardized instructional set to adolescents, in which adolescents were coached to mimic a straw-breathing task and instructed about how to respond to queries during the task (i.e., by reading answers that were written on a computer screen outside of parents’ view, holding a straw up to their mouth, maintaining a forward facing direction). A two-pronged approach was employed to assess the integrity of the experimental manipulation. First, prior to the commencement of the study, an experimenter who was blind to experimental condition administered a standardized training procedure in which participants were required to demonstrate their ability to adhere to the script presented on screen, and to maintain a forward-facing direction. All participants were then directly observed (via closed circuit television cameras) by experimenters during study procedures to ensure adherence to the protocol. In all cases, participants read the script as directed. Second, in terms of mimicking the straw breathing task, participants were trained in how to do this by being trained to hold the straw up to their mouths, and complete two successful practice rounds of the breathing task (including reading standardized scripts and maintaining a forward-facing direction) in front of the experimenter. This was done as part of the standardized training protocol described above, delivered by trained experimenters, blind to condition. The integrity of this aspect of the independent variable was checked during debriefing procedures, where parents were queried to see if they believed their child was actually completing the breathing task. Two parents reported that their child was not behaving believably during the conversation task, and their data was excluded from all analyses (as noted in the methods section).
Fig. 1.
Schematic describing study procedure.
Following training, adolescents were randomly assigned to one of two conditions. In the “anxious” condition, adolescents were instructed to read a set of anxious descriptors during the task, in the “non-anxious” (control) condition, adolescents were instructed to read a set of non-anxious descriptors during the task. Consistent with previous work (Bunaciu et al., 2014), in order to reduce possible cofounds that may have emerged as the adolescent mimicked the task (e.g., facial expressions, task compliance) adolescents faced away from their parents as they mimicked the breathing procedure. Adolescents completed up to 10 rounds of the straw-breathing task. After mimicking the task for 30 s, adolescents would pause and respond to the experimenter’s queries. Please see Appendix B for the script adolescents used during the experimental task. After five rounds, parents were given the option to have their child quit the task if the parent became distressed, although parents were permitted to end the task earlier due to distress if they requested to do so. Prior to watching the task, parents were asked to complete a brief (20 s) straw-breathing task, in order to allow parents to experience what their adolescent would be asked to do during the task. After instructions were given, parental physiological data was collected continuously throughout the task. Following completion of the study, parents and adolescents were debriefed separately. Consistent with recommended practices (Boynton, Portnoy, & Johnson, 2013), parents were fully debriefed about the nature of the study, with specific attention given to elements of deception included in the study. The experimenter revealed the nature of the deception, and why it was important to use deception in the experiment. The experimenter spent time discussing the experimental design with parents, and addressing any concerns parents may have had about the nature of the deception or the experiment broadly. Finally, the experimenter thanked the parents for their participation. Adolescents were also debriefed about the nature of the study, and thanked for their participation.
3. Results
3.1. Checks of the efficacy of random assignment
Conditions were compared in terms of theoretically relevant dichotomous (i.e., parent and offspring gender) and continuous (i.e., offspring: CASI, and PANAS-C; parents: ASI and PANAS) variables at baseline to check the efficacy of random assignment. Chi-square analyses indicated that there were no group differences in terms of offspring [χ2 (1) = 0.96, p = .404] or parent [χ2 (1) = 0.69, p = .465] gender. A series of independent samples t-tests were planned to examine group differences in continuous self-report measures. Inspection of continuous variables indicated that the normality assumption required for conducting parametric statistics was not met because the continuous variables were significantly skewed (i.e., Skew ranged from 0.52 to 2.66). Therefore, group differences on continuous variables were examined using non-parametric Mann-Whitney tests. Conditions did not differ in terms of offspring CASI scores (U = 278 z = −0.89, p = .374, r = −0.12) or PANAS-C scores (U = 267, z = −0.43, p = .664, r = −0.06). Similarly, conditions did not differ in terms of parent ASI scores (U = 302.50, z = −0.19, p = .846, r = −0.03) or PANAS scores (U = 231, z = −1.39, p = .166, r = −0.20). Accordingly, no covariates were included in the primary analyses described below.
3.2. Descriptive statistics and correlations
Descriptive statistics and correlations were computed. See Tables 1 and 2 for descriptive information and zero-order correlations (Table 3).
Table 1.
Descriptive data for parent and child demographic variables and theoretically relevant variables as a function of group.
| Group | ||
|---|---|---|
| Control | Anxious | |
| M or n (SD or %) n=26 | M or n (SD or %) n = 25 | |
| Child | ||
| Age | 12.32 (1.14) | 12.25 (1.26) |
| Gender (Male, n) | 11 (42.3%) | 14 (56%) |
| Grade | ||
| Fourth | 1 (3.8%) | 1 (4%) |
| Fifth | 2 (7.7%) | 4 (16%) |
| Sixth | 4 (15.4%) | 3 (12%) |
| Seventh | 11 (42.3%) | 9 (36%) |
| Eighth | 3 (11.5%) | 6 (24%) |
| Ninth | 5 (19.2%) | 2 (8%) |
| Race/Ethnicitya | ||
| Caucasian | 18 (69.2) | 20 (80%) |
| Asian | 2 (7.7) | 1 (4%) |
| African American | 2 (7.7) | - |
| Native American | 1 (3.8) | - |
| Multiple race | 3 (11.5) | 3 (12%) |
| Other | - | 1 (4%) |
| Parent | ||
| Age | 43.24 (5.62) | 42.29 (6.64) |
| Gender (Male, n) | 3 (11.5%) | 5 (20%) |
| Race/Ethnicitya | ||
| Caucasian | 22 (84.6%) | 24 (96%) |
| Asian | 4 (15.4%) | 1 (4%) |
| African American | - | - |
| Native American | 5 (19.2%) | - |
| Multiple race | - | - |
| Annual Household Income | ||
| < $20,000 | 3 (11.5%) | - |
| $20,001 - $40k | 8 (30.8%) | 3 (12%) |
| $40,001 - $60k | 2 (7.7%) | 6 (24%) |
| $60,001 - $70k | 2 (7.7%) | 3 (12%) |
| $70,001 - $90 | 3 (11.5%) | 2 (8%) |
| $90,001 - $100k | 2 (7.7%) | 2 (8%) |
| > $100k | 5 (19.2%) | 9 (36%) |
| Marital Status | ||
| Single | 3 (11.5%) | 1 (4%) |
| Married | 16 (61.5%) | 23 (92%) |
| Divorced | 5 (19.2%) | 1 (4%) |
| Separated | 1 (3.8%) | - |
| Child TheoreticaLly-Relevant Variables | ||
| CASI | 27.27 (4.84) | 26.04 (4.09) |
| PANASC-NA | 30.58 (12.78) | 27.33 (7.74) |
| Parent Theoretically-Relevant Variables | ||
| ASI | 28.36 (11.25) | 27.84 (13.25) |
| PANAS-NA | 19.16 (8.77) | 15.84 (5.23) |
Note. N = 51; CASI = Child Anxiety Sensitivity Index; PANASC-NA = Positive and Negative Affect Schedule for Children- Negative Affect Scale; ASI = Anxiety Sensitivity Index; PANAS-NA = Positive and Negative Affect Schedule- Negative Affect Scale.
Note that race/ethnicity percentages do not sum to 100 because race/ethnicity categories were not mutually exclusive.
Table 2.
Descriptive data and zero-order correlations between relevant continuous variables.
| M (SD) | 1 | 2 | 3 | 4 | |
|---|---|---|---|---|---|
| 1. CASI | 26.67 (4.48) | −.02 | .28 | −.04 | |
| 2. ASI | 28.1 (12.16) | .12 | .61** | ||
| 3. PANASC-NA | 28.96 (10.58) | .033 | |||
| 4. PANAS-NA | 17.47 (7.31) |
Note: CASI = Child Anxiety Sensitivity Index; PANASC-NA = Positive and Negative Affect Schedule for Children-Negative Affect Scale; ASI = Anxiety Sensitivity Index; PANAS-NA = Positive and Negative Affect Schedule -Negative Affect Scale.
p < .001 (two-tailed).
Table 3.
Descriptive data for parental distress and arousal during the experimental procedure.
| Baseline M (SD) | Round 1 M (SD) | Round 2 M (SD) | Round 3 M (SD) | Round 4 M (SD) | Round 5 M (SD) | Round 6 M (SD) | Round 7 M (SD) | Round 8 M (SD) | Round 9 M (SD) | Round 10 M (SD) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Control Group Valence | 3.04 (1.48) | 3.15 (1.54) | 3.23 (1.53) | 3.38 (1.65) | 3.46 (1.73) | 3.46 (1.77) | 3.46 (1.79) | 3.38 (1.77) | 3.54 (1.90) | 3.64 (1.82) | 3.50 (1.98) |
| Anxiety Group Valence | 2.88 (1.20) | 3.96 (2.01) | 4.30 (2.18) | 4.39 (1.88) | 4.43 (1.78) | 4.68 (2.10) | 4.71 (1.93) | 4.71 (2.03) | 4.83 (1.72) | 4.78 (1.87) | 4.63 (2.28) |
| Control Group Arousal | 7.19 (1.65) | 6.96 (1.91) | 7.04 (1.93) | 7.12 (1.63) | 7.00 (1.79) | 7.00 (1.83) | 7.15 (1.76) | 7.31 (1.62) | 7.35 (1.67) | 7.36 (1.63) | 7.38 (1.80) |
| Anxiety Group Arousal | 6.33 (2.04) | 5.84 (2.15) | 5.91 (2.26) | 5.91 (1.78) | 6.00 (1.93) | 5.86 (2.10) | 5.57 (1.83) | 5.62 (2.20) | 5.89 (1.88) | 6.06 (1.83) | 6.00 (1.86) |
| Baseline | Experiment | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| M (SD) | M (SD) | |||||||||
| Control Group Heart Rate | 65.62 (25.77) | 71.97 (8.95) | ||||||||
| Anxiety Group Heart Rate | 66.35 (27.22) | 74.00 (11.74) |
Note: Valence and Arousal assessed by the Self Assessment Manikin. Parents’ average heart rate over the experimental procedure is presented due to the large number of heart rate measurements obtained in 1-min increments over the course of the experiment. As noted in Table 6, there was no significant effect of time or experimental condition on parental heart rate as measured in 1-min increments over the course of the experiment.
3.3. Sick role reinforcement
3.3.1. Behavioral sick role reinforcement
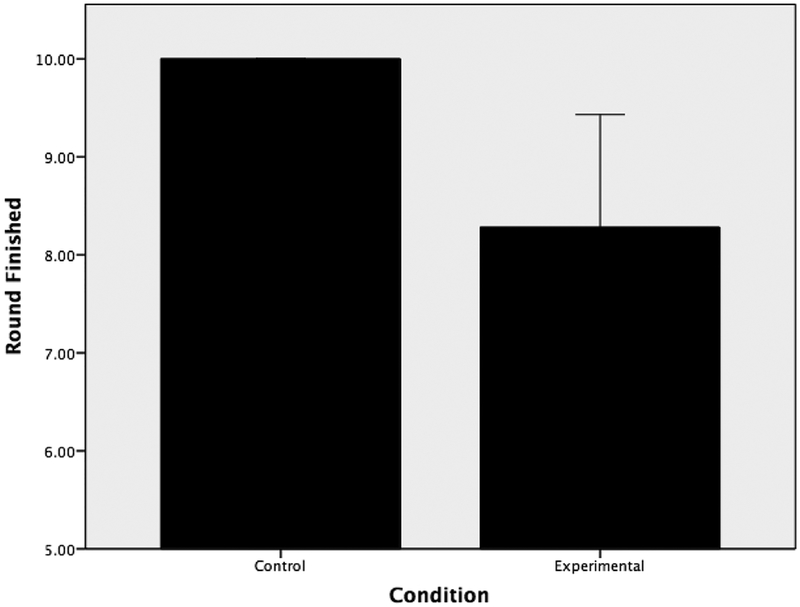
A one-way ANOVA was run to examine the effect of experimental condition on parental latency to end the task. A Levene’s test revealed significant group differences in variance with regards to parental latency to end the straw-breathing task, F (1,48) = 41.71, p < .001. Given that the assumption of the homogeneity of variance required for conducting parametric statistics were not met, non-parametric statistics, specifically the Mann-Whitney tests, were utilized to examine group differences in latency to end the straw-breathing task. For the purposes of this investigation, Pearson’s r was selected as the index of effect size (Cohen, 1988) with small, medium, and large effect sizes being represented by r-values of 0.10, 0.30, and 0.50, respectively. Ten parents in the anxious condition ended their offspring’s straw-breathing task early due to distress, whereas no parents in the control condition did so. Results of the Mann-Whitney task indicated that parents in the anxious condition (Mean Rank = 20.50) ended the straw-breathing task faster than parents in the control condition (Mean Rank = 30.50), (U = 187.50, z = −3.47, p = .001, r = −0.49). This effect was medium-large in magnitude. See Fig. 2.
Fig. 2.
Mean number of mimicked straw-breathing rounds completed. Error bars reflect 95% confidence intervals. No parents in control condition ended the task early therefore, error bars are not included.
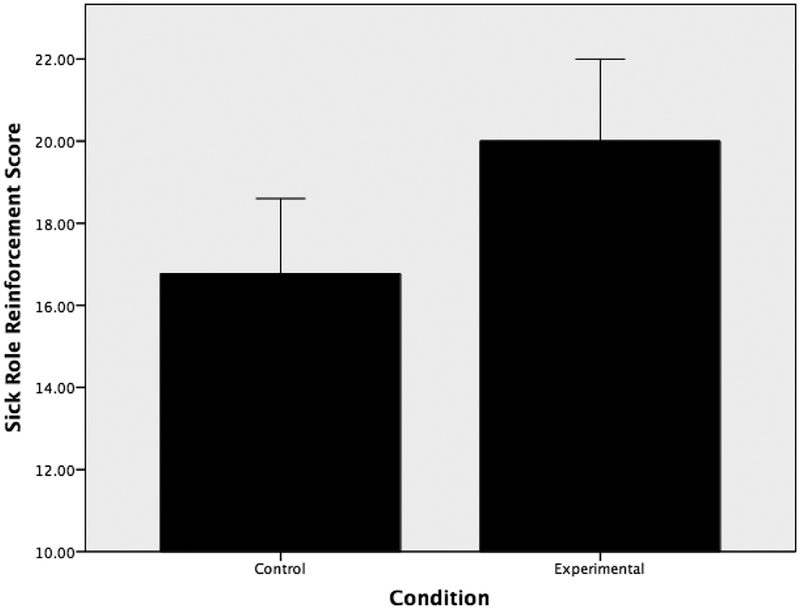
3.3.2. Self-reported sick role reinforcement
An ANOVA was run to examine the effect of experimental condition on parental self-reported sick role reinforcement behavior. Results indicated that there was a significant effect of condition on parental sick role reinforcement, (F (1,49) = 6.06, p = .017, r = 0.33), such that parents in the anxious condition reported that they would reinforce more sick role behavior (M = 20.00, SD = 4.84) than parents in the control condition (M = 16.77, SD = 4.54). This effect was medium in magnitude. See Fig. 3.
Fig. 3.
Mean parental sick role reinforcement scores. Error bars reflect 95% confidence intervals.
3.4. Parental distress during task
Two separate multilevel models were employed to examine the effects of experimental condition on parental affective arousal and valence during the task. Separate linear mixed models with maximum likelihood estimation were used to examine changes in parental affective valence and arousal over the course of the experiment in response to offspring reactions to the task. Linear mixed models were employed due to their ability to handle missing data (Field & Wright, 2011). Critically, missing data was not an issue for most analyses included in the current data (i.e., self-reported sick role reinforcement, behavioral sick role reinforcement). However, because parents were allowed to end the breathing task early if they became distressed, some parents were missing some data from the parental distress during the task analyses (i.e., parental valence and arousal during the breathing task). For example, the average round completed for parents in the anxious condition was round 8 of 10 (scores ranged from 1 round to 10 rounds), suggesting that many parents were missing minimal data for the majority of analyses (the average number of rounds completed for the control condition was a full 10 rounds). Unstructured covariance matrices were employed in all models. The Control condition was coded as 1, while the Anxious condition was coded as 2 for primary analyses. To facilitate interpretation, baseline levels of affective valence and arousal, as well as time, were centered at their means. A number of models were run to determine the model of best fit. Individual participants were considered level 2 predictors. First, intercept was entered as a random effect, followed by the fixed main effects of baseline affective valence/arousal, time, and experimental condition, as well as the interaction between experimental condition and time. Second, a model identical to the model above was run, but the slope across time was allowed to vary randomly. Criterion variables for the response through the experimental period were comprised of the repeated assessments of the SAM valence and arousal scores. Significant interactions were examined using post-hoc probing as recommended by Holmbeck (2002). Control condition was re-coded as 0, while anxious condition was re-coded as 1 in post-hoc analyses.
3.4.1. Arousal ratings
Chi square tests indicated that the best fitting model for arousal scores, χ2 (9) = 168.81, p < .001, was a random intercepts model, with the slope of time allowed to vary randomly. In terms of random effects, the relation between experimental condition and parent arousal showed significant variance in intercepts across participants, SD = 1.13 (95% CI: 0.91, 1.40), χ2 = 623.56, p < .0001. Similarly, the slopes, SD = 0.18 (95% CI: 0.15, 0.23), χ2 = 168.62, p < .0001, varied significantly across participants. Finally, the slopes and intercepts were not significantly correlated, r = 0.22, (−0.11, 0.50).
As detailed in Table 4, in terms of fixed effects, there was a significant, positive relation between parental baseline self-reported arousal and self-reported arousal during the task. In contrast, after accounting for the association with baseline arousal, there was not a significant relation between time and arousal. There also was not an effect of condition on arousal. The interaction between time and condition was not significant.
Table 4.
Parental self-reported arousal as a function of experimental condition.
| b | SEb | 95% CI | p | ||
|---|---|---|---|---|---|
| Fixed Effects | Baseline Arousal | 0.69 | 0.09 | 0.52, 0.87 | < .001 |
| Time | 0.04 | 0.04 | −0.04, 0.12 | .300 | |
| 1Experimental Condition | −0.46 | 0.34 | −1.13, 0.22 | .186 | |
| Experimental Condition X | −0.02 | 0.06 | −0.13, 0.09 | .742 | |
| Time | |||||
| Variance Components | Intercept | 1.13 | |||
| Time | 0.19 |
Note.
Control condition coded as 1, Anxious Condition coded as 2, therefore negative b estimates reflect greater arousal in the Control Condition and positive estimates reflect greater arousal in the Anxious Condition.
Lower scores indicate higher levels of arousal.
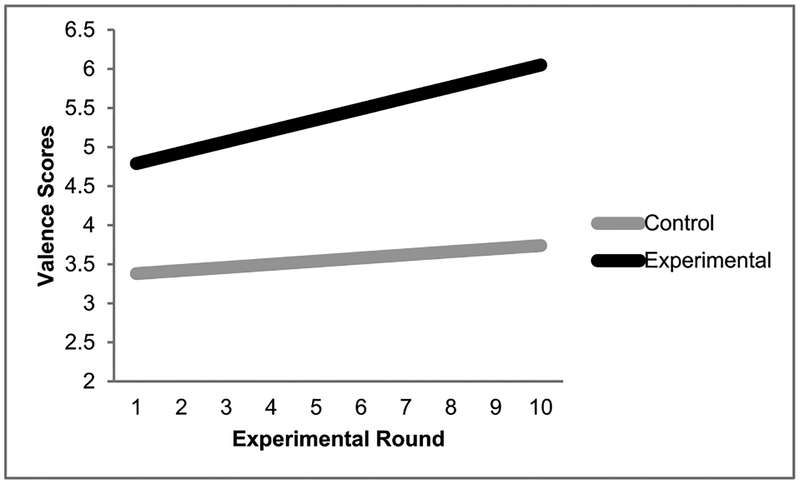
3.4.2. Affective valence ratings
Chi square tests indicated that the best fit for the affective valence scores, χ2 (9) = 70.23, p < .001, was a random intercepts model with the slope of time varying randomly. In terms of random effects, parent affective valence showed significant variance in intercepts across participants, SD = 1.37 (95% CI: 1.21, 1.67), χ2 = 721.15, p < .001. Similarly, the slopes, SD = 0.12 (95% CI: 0.09, 0.15), χ2 = 70.23, p < .001, varied significantly across participants. Finally, the slopes and intercepts were not significantly correlated, r = 0.29 (−0.05, 0.57).
As detailed in Table 5, in terms of fixed effects, there was a statistically significant, positive relation between parental baseline self-reported affective valence and self-reported affective valence during the experimental task. In contrast, there was not a relation between time and parental valence during the task. There was, however, a significant effect of condition, such that parents in the anxious condition reported more negatively valenced affect over the course of the procedure than parents in the control condition. Finally, there was a significant interaction between time and condition such that in the control condition, valence scores did not change significantly over time (B = 0.05, t = 1.90, p = .058), while for the anxious condition, valence scores increased over time, indicating that parents’ valence showed steeper increases in negative valence over time (B = 0.14, t = 4.82, p < .001). Fig. 4 graphically depicts the interaction.
Table 5.
Parental self-reported affective valence as a function of experimental condition.
| b | SEb | 95% CI | p | ||
|---|---|---|---|---|---|
| Fixed Effects | Baseline Valence | 0.74 | 0.14 | 0.45, 1.02 | < .001 |
| Time | 0.05 | 0.03 | −0.00, 0.10 | .057 | |
| 1Experimental Condition | 1.40 | 0.39 | 0.62, 2.19 | < .001 | |
| Experimental Condition X | 0.09 | 0.04 | 0.14, 0.17 | .021 | |
| Time | |||||
| Variance Components | Intercept | 1.37 | |||
| Time | 0.12 |
Note.
Control condition coded as 1, Anxious Condition coded as 2, therefore negative b estimates reflect greater valence in the Control Condition and positive estimates reflect greater valence in the Anxious Condition.
Higher scores indicate more negative affective valence.
Fig. 4.
Interaction of Experimental Condition × Time in predicting SAM Valence Scores.
3.4.3. Heart rate during task
Chi square tests indicated that the best fit for the heart rate averages, χ2 (12) = 56.15, p < .001, was a random intercepts model with the slope of time varying randomly. In terms of random effects, parent heart rate showed significant variance in intercepts across participants, SD = 2.81 (95% CI: 2.25, 3.51), χ2 = 1884.94, p < .001. Similarly, the slopes, SD = 0.18 (95% CI: 0.13, 0.24), χ2 = 56.15, p < .001, varied significantly across participants. Finally, the slopes and intercepts were significantly correlated, r = 0.70 (0.42, 0.86).
As detailed in Table 6, in terms of fixed effects, there was a significant, positive relation between parental baseline self-reported arousal and self-reported arousal during the task. In contrast, after accounting for the association with baseline arousal, there was not a significant relation between time and arousal. There also was not an effect of condition on arousal. The interaction between time and condition was not significant.
Table 6.
Parental heart rate as a function of experimental condition.
| b | SEb | 95% CI | p | |
|---|---|---|---|---|
| Baseline Heart Rate | 0.90 | 0.70 | 0.45, 1.02 | < .001 |
| Time | 0.05 | 0.06 | −0.00, 0.10 | .425 |
| 1Experimental Condition | 0.12 | 1.16 | 0.62, 2.19 | .918 |
| Experimental Condition X Time | 0.01 | 0.09 | 0.14, 0.17 | .871 |
| Intercept | 2.81 | |||
| Time | 0.18 |
Note.
Control condition coded as 1, Anxious Condition coded as 2.
4. Discussion
It is critical to improve our understanding of factors that may enhance panic vulnerability among adolescents. A large self-report literature suggests that parents can enhance fear of bodily arousal among offspring via sick role reinforcement behavior (Ehlers, 1993; Leen-Feldner et al., 2008; Stewart et al., 2001; Watt & Stewart, 2000; Watt et al., 1998). Notably, few studies have examined the dyadic process of parents and adolescents in real-time. This relative degree of neglect is unfortunate, given adolescents influence the parenting behavior they receive (O’Connor, 2002). The current study used a novel method to experimentally test if experimentally manipulated adolescent reactions to a straw-breathing task influenced parental propensity to engage in sick role reinforcement behavior and distress. Results were partially consistent with hypotheses. Conditions differed in terms of parental self-reported and behavioral indices of sick role reinforcement behavior, and affective valence during the task. No condition differences emerged in terms of parental self-reported or directly measured physiological arousal during the task.
First, consistent with hypotheses, parents ended the task significantly earlier following anxious, as compared to non-anxious, adolescent descriptions. In fact, 10 out of 25 parents in the anxious condition opted to discontinue their offspring’s participation in the straw-breathing task, whereas none of the parents in the control condition ended the experiment early. This effect was medium-large in magnitude (r = − 0.49). Second, and also consistent with expectations, parents whose adolescent described an anxious response to the straw-breathing task reported that they would reinforce significantly more sick role behavior than parents whose adolescent described a non-anxious reaction. This effect was medium in magnitude (r = 0.33). Critically, there were no significant differences between conditions in terms of demographic variables (e.g., offspring or parent gender) or theoretically relevant covariates (e.g., AS), so it is unlikely that these variables accounted for differences in parental behavior. These findings suggest an important role of offspring descriptions of ambiguous bodily sensations in eliciting parenting behavior thought to increase adolescent vulnerability for panic. They also extend previous vignette-based work suggesting offspring factors influence parental propensity to engage in sick role reinforcement behavior (Bilsky et al., 2018). Such behavior may account, in part, for elevated healthcare utilization within families with anxious youth (Bodden et al., 2008), and may enhance offspring panic vulnerability by preventing opportunities for extinction learning (Bouton et al., 2001). Furthermore, the observed pattern of findings here are consistent with evidence demonstrating that adolescent anxiety elicits controlling parenting behavior (e.g., Eley et al., 2010; Hudson et al., 2009), adding to a growing body of work suggesting that adolescent anxious behavior elicits specific, maladaptive parenting behaviors. These findings also highlight the transactional nature of parent-adolescent interactions (Sameroff, 2010), and lend insight into the complex processes that confer risk for panic vulnerability among adolescents. An intriguing next step would be to clarify specific classical and operant contingencies involved in this process. For instance, it is currently unclear the extent to which youth are differentially susceptible to particular fear acquisition processes (e.g., direct conditioning, vicarious conditioning, information transmission; Rachmann, 1977) and the degree to which they influence parental reinforcement or punishment of displays of anxiety in the context of somatic arousal. This is a potentially fruitful area for future research aimed at refining our knowledge of factors that may increase adolescent panic vulnerability.
Also consistent with hypotheses, parents who viewed their adolescent react anxiously to the straw-breathing task reported progressively more negatively valenced affect over the course of the experiment. In contrast, parents who viewed their offspring react non-anxiously self-reported more positively valenced affect that did not change significantly over the course of the experiment. These findings correspond with theory suggesting that parents become affectively distressed in the presence of offspring anxiety, and set the stage for evaluating whether such distress prompts parents to reinforce adolescent sick role behavior (e.g., Wood et al., 2009). These results complement the findings that adolescent anxiety was related to increased self-reported and behavioral indices of sick role reinforcement behavior. A logical next step would be to examine if parental distress elicited by adolescent anxiety about somatic perturbation mediates the relation between adolescent anxiety and parental sick role reinforcement. As noted previously, the behavioral index of sick-role reinforcement in this study was parental latency to end the straw-breathing task. This behavioral index was selected to provide a real-life proxy for the degree to which parents would behaviorally facilitate escape behavior on behalf of their adolescents. Unfortunately, the “differential drop-out” across cells made a mediation analysis difficult to interpret. This remains a critical next step, as the identification of such mediators would facilitate the development of sequential interventions designed to target multiple links in a causal chain that increases adolescent vulnerability for panic (Kraemer et al., 2001). If parental distress mediates the relation between adolescent anxiety and parental sick role reinforcement, teaching parents strategies to manage their own affect in response to offspring anxiety could be a helpful tool to reduce sick role reinforcement behavior. For instance, if, in the context of exposure-based treatments for adolescents who fear bodily arousal (e.g., Panic Control Treatment for Adolescents; Pincus, May, Whitton, Mattis, & Barlow, 2010), parents facilitate adolescent escape behavior, then providing parents with tools to manage their own affective reactions, and encourage their children to finish exposure exercises may further enhance the efficacy of these treatments. Although this remains to be tested, this could represent a relatively simple way to enhance current treatments for adolescent anxiety.
Surprisingly, and contrary to hypotheses, there were no group differences in terms of parental self-reported or physiological arousal as a function of group. There are a number of factors that may explain this pattern. First, in terms of the manipulation employed, adolescents were instructed to face away from their parents, thereby obscuring parents’ view of their adolescent’s facial expressions. Drawing from prior experimental work examining the effect of adolescent anxiety on parenting behaviors in which parents and adolescents interact directly (e.g., Hudson et al., 2009; Moore et al., 2004), parental perception of their child’s emotional expressions may be important in eliciting parental arousal. Second, the current hypotheses were examined among a community-recruited sample of parents and adolescents, which likely limited upper level variability in parental self-reported and physiological arousal. Future work could usefully build on the current findings by sampling parent-adolescent dyads experiencing clinically-significant levels of anxiety (e.g., Silverman, Kurtines, Jaccard, & Pina, 2009). Significant effects of offspring anxiety on parental arousal may emerge within a sample of parents and adolescents with disorders characterized by elevated fear and anxious arousal (e.g., panic disorder, social anxiety disorder; Naragon-Gainey, Prenoveau, Brown, & Zinbarg, 2016). Finally, it is also possible that the manipulation employed in the current study was strong enough to increase negativity, but not strong enough to elicit parental arousal. The fact that parents observed offspring engage in a laboratory-based task under controlled conditions likely reassured parents that their offspring were safe, thereby reducing affective arousal. It is possible that less predictable and more uncontrollable experiences (such as those occurring naturalistically) would elicit parental arousal, potentially enhancing the effects observed here. While this level of intensity may be difficult to safely and ethically model in a laboratory, naturalistic investigations of the relation between adolescent reports of anxiety focused on bodily arousal and parental self-reported arousal would be valuable in further elucidating these possible links. Future research should integrate laboratory and naturalistic, prospective methods (e.g., ecological momentary assessment, EMA; Oppenheimer et al., 2016), to provide a more complete picture of the relation between adolescent anxiety and parental sick role reinforcement behavior.
A number of limitations warrant mention. First, this sample consisted of primarily healthy, middle class, Caucasian participants. In light of evidence that parenting varies significantly as a function of race and ethnicity (e.g., Kwak, 2003; Lansford, Deater-Deckard, Dodge, Bates, & Pettit, 2004), a critical next step will be to examine the generalizability of the current findings by extending this work to a more heterogeneous sample. Second, the self-report sick role reinforcement measure utilized in this study was developed for the current project. A number of factors speak to the self-report measure’s validity; first the measure was based on items from a well-validated measure (i.e., the LHQ-III; Stewart et al., 2001) and it was adapted for this study from a measure utilized in prior, published work (Bilsky et al., 2018). Further, preliminary data supported its construct validity. Nonetheless, the psychometric properties of the measure are not well-established, which decreases confidence in the observed pattern of findings. Further examinations of the measures validity remain an important objective for future research in this area. In addition, this sample was comprised primarily of mothers. Given the unique and important role that fathers may play in the development and etiology of adolescent anxiety, future work should endeavor to examine the impact of adolescent anxiety on a larger sample of fathers (Bögels & Phares, 2008). Finally and relatedly, because this sample was comprised primarily of mothers and their adolescents, this study did not examine how parent and offspring gender may affect these processes. In light of compelling evidence suggesting that there may be “cross-gender” effects (i.e., fathers influence on daughters, and mothers influence on sons) in the relation between parenting behavior and offspring psychopathology generally (e.g., Stolz, Barber, & Olsen, 2005), and anxiety specifically (Burstein & Ginsburg, 2010), future work should examine if these effects differ as a function of parent and offspring gender. Finally, parents were queried about adolescent physical and mental health symptoms prior to taking part in laboratory procedures. This may have impacted their decision about whether to intervene. Although this effect was equated across groups, future work may benefit from having a longer time interval between the assessment of symptomatology and examination of sick role behavior.
These limitations notwithstanding, the current study extends the literature by utilizing a novel method to examine the role that adolescent displays of anxiety in response to bodily arousal play in eliciting parenting behavior thought to increase vulnerability for panic. These findings are the first to experimentally demonstrate that real time adolescent anxiety in response to somatic perturbation increases behavioral and self-reported indicators of parental sick role reinforcement behavior as well as parental negative affective valence. These results lay the groundwork for future studies targeted at improving our understanding of the impact of adolescent anxiety on parenting behavior, including those focused on the complex interplay between adolescent and parent characteristics in increasing vulnerability for the development of panic.
Acknowledgements
This project was supported by a National Science Foundation Graduate Research Fellowship Award (Grant No. 2015179871) awarded to Sarah A. Bilsky, and a National Institute of Drug Abuse research grant (1F31 DA041105) awarded to Renee M. Cloutier.
S.A. Bilsky drafted the manuscript with crucial revision from authors R.M. Cloutier, T.R. Bynion, M.T. Feldner, and E.W. Leen-Feldner. T.R. Bynion created tables. All authors contributed to, edited, and approved the final manuscript. S.A. Bilsky conducted the statistical analysis and R.M. Cloutier consulted on the statistical analysis.
Appendix A
Questions following the experimental procedure:
If you child displayed these symptoms, how likely would you be to:
Tell them to go lay down (1–5)
Let them stay home from school (1–5)
Excuse your child from chores (1–5)
Take them to the doctor (1–5)
Tell them to observe their symptoms carefully (1–5)
Give them medicine (1–5)
Appendix B
Research Assistant: “OK, are you ready to start the breathing task we practiced earlier? After the breathing task, I am going to ask you if you are experiencing a number of symptoms. I will also ask you how anxious you are feeling on a scale of 1 to 5, with 1 being not anxious at all, 2 being a little, 3 being moderately, 4 being quite a bit, and 5 being extremely anxious. Do you have any questions about this? Ok, when I say go, please begin breathing into the straw. Go.”
Adolescent mimics straw-breathing procedure for 30 s.
Then all adolescents are asked and prompted to respond:
Research Assistant: “Do you feel dizzy?”
Adolescent Prompt: “Yes”.
Research Assistant: “Do you feel light headed?”
Adolescent Prompt: “Yes”
Research Assistant: “Do you feel like your heart is racing or beating really fast”?
Adolescent Prompt: “Yes”
Anxious Condition
Research Assistant: “Do you feel upset?”
Adolescent: “Yes”
Research Assistant: “On a scale from 1 to 5 with one being not anxious at all, and 5 being extremely anxious how anxious do you feel?”
Adolescent: “5”
Control Condition
Research Assistant: “Do you feel upset?”
Adolescent: “No”
Research Assistant: “On a scale from 1 to 5 with one being not anxious at all, and 5 being extremely anxious how anxious do you feel?”
Adolescent: “1”
References
- Beesdo K, Knappe S, & Pine DS (2009). Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America, 32, 483–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilsky SA, Feldner MT, Bynion T, Rojas SR, & Leen-Feldner EW (2018). Child anxiety and parental anxiety sensitivity are related to parent sick role reinforcement. Parenting, 18(2), 110–125. 10.1080/15295192.2018.1444132. [DOI] [Google Scholar]
- Bodden DM, Dirksen CD, & Bogels SM (2008). Societal burden of clinically anxious youth referred for treatment: A cost-of-illness study. Journal of Abnormal Child Psychology, 36(4), 487–497. 10.1007/s10802-007-9194-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bögels S, & Phares V (2008). Fathers’ role in the etiology, prevention and treatment of child anxiety: A review and new model. Clinical Psychology Review, 28(4), 539–558. 10.1016/j.cpr.2007.07.011. [DOI] [PubMed] [Google Scholar]
- Bouton ME, Mineka S, & Barlow DH (2001). A modern learning theory perspective on the etiology of panic disorder. Psychological Review, 108, 4–32. 10.1037/0033-295X.108.1. [DOI] [PubMed] [Google Scholar]
- Boynton MH, Portnoy DB, & Johnson BT (2013). Exploring the ethics and psychological impact of deception in psychological research. IRB: Ethics & Human Research, 35(2), 7–13. [PMC free article] [PubMed] [Google Scholar]
- Buccelletti F, Ojetti V, Merra G, Carroccia A, Marsiliani D, Mangiola F, … Franceschi F (2013). Recurrent use of the Emergency Department in patients with anxiety disorder. European Review for Medical and Pharmacological Sciences, 17(1), 100–106. [PubMed] [Google Scholar]
- Bunaciu L, Leen-Feldner EW, Blumenthal H, Knapp AA, Badour CL, & Feldner MT (2014). An experimental test of the effects of parental modeling on panic-relevant escape and avoidance among early adolescents. Behavior Therapy, 45(4), 517–529. 10.1016/j.beth.2014.02.01. [DOI] [PubMed] [Google Scholar]
- Burstein M, & Ginsburg GS (2010). The effect of parental modeling of anxious behaviors and cognitions in school-aged children: An experimental pilot study. Behaviour Research and Therapy, 48(6), 506–515. 10.1016/j.brat.2010.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Craske MG (2003). Origins of phobias and anxiety disorders: Why more women than men? New York: Elsevier. [Google Scholar]
- Craske MG, Treanor M, Conway CC, Zbozinek T, & Vervliet B (2014). Maximizing exposure therapy: An inhibitory learning approach. Behaviour Research and Therapy, 58, 10–23. 10.1016/j.brat.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A (1993). Somatic symptoms and panic attacks: A retrospective study of learning experiences. Behaviour Research and Therapy, 31, 269–278. 10.1016/0005-7967(93)90025-P. [DOI] [PubMed] [Google Scholar]
- Eley TC, Napolitano M, Lau JY, & Gregory AM (2010). Does childhood anxiety evoke maternal control? A genetically informed study. Journal of Child Psychology and Psychiatry, 51(7), 772–779. 10.1111/j.1469-7610.2010.02227.x. [DOI] [PubMed] [Google Scholar]
- Field AP, & Wright DB (2011). A primer on using multilevel models in clinical and experimental psychopathology research. Journal of Experimental Psychopathology, 2(2), 271–293. 10.5127/jep.013711. [DOI] [Google Scholar]
- Francis SE, & Chorpita BF (2010). Development and evaluation of the parental beliefs about anxiety questionnaire. Journal of Psychopathology and Behavioral Assessment, 32(1), 138–149. 10.1007/s10862-009-9133-5. [DOI] [Google Scholar]
- Gar NS, & Hudson JL (2008). An examination of the interactions between mothers and children with anxiety disorders. Behaviour Research and Therapy, 46(12), 1266–1274. 10.1016/j.brat.2008.08.006. [DOI] [PubMed] [Google Scholar]
- Ginsburg GS, Silverman WK, & Kurtines WK (1995). Family involvement in treating children with phobic and anxiety disorders: A look ahead. Clinical Psychology Review, 15(5), 457–473. 10.1016/0272-7358(95)00026-L. [DOI] [Google Scholar]
- Graham RA, & Weems CF (2015). Identifying moderators of the link between parent and child anxiety sensitivity: The roles of gender, positive parenting, and corporal punishment. Journal of Abnormal Child Psychology, 43(5), 885–893. 10.1007/s10802-014-9945-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman-Giddens ME (2007). The decline in the age of menarche in the United States: Should we be concerned? Journal of Adolescent Health, 40(3), 201–203. 10.1016/j.jadohealth.2006.12.019. [DOI] [PubMed] [Google Scholar]
- Holmbeck G (2002). Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology, 27, 87–96. 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Hudson JL, Doyle AM, & Gar N (2009). Child and maternal influence on parenting behavior in clinically anxious children. Journal of Clinical Child and Adolescent Psychology, 38(2), 256–262. 10.1080/15374410802698438. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Alonso J, Chatterji S, & He Y (2014). Disability and costs In Emmelkamp P, & Ehring T (Eds.). The Wiley handbook of anxiety disorders, Volume I: Theory and research; Volume II: Clinical assessment and treatment (pp. 47–57). Chichester, UK: Wiley-Blackwell. [Google Scholar]
- Knapp AA, Frala J, Blumenthal H, Badour CL, & Leen-Feldner EW (2013). Anxiety sensitivity and childhood learning experiences: Impacts on panic symptoms among adolescents. Cognitive Therapy and Research, 37(6), 1151–1159. 10.1007/s10608-013-9558-8. [DOI] [Google Scholar]
- Kraemer HC, Stice E, Kazdin A, Offord D, & Kupfer D (2001). How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry, 158(6), 848–856. 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- Kwak K (2003). Adolescents and their parents: A review of intergenerational family relations for immigrant and non-immigrant families. Human Development, 46(2–3), 115–136. 10.1159/000068581. [DOI] [Google Scholar]
- Lang PJ (1980). Behavioral treatment and bio-behavioral assessment: Computer applications In Sidowski JB, Johnson JH, & Williams TA (Eds.). Technology in the health care delivery system (pp. 119–137). Norwood, NJ: Ablex. [Google Scholar]
- Lang PJ (1984). Cognition in emotion: Concept and action In Izard CE, Kagan J, & Zajonc RB (Eds.). Emotions, cognitions, and behavior (pp. 192–228). New York: Cambridge. [Google Scholar]
- Lansford JE, Deater-Deckard K, Dodge KA, Bates JE, & Pettit GS (2004). Ethnic differences in the link between physical discipline and later adolescent externalizing behaviors. Journal of Child Psychology and Psychiatry, 45(4), 801–812. 10.1111/j.1469-7610.2004.00273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurent J, Catanzaro SJ, Joiner TJ, Rudolph KD, Potter KI, Lambert S, … Gathright T (1999). A measure of positive and negative affect for children: scale development and preliminary validation. Psychological Assessment, 11(3), 326–338. 10.1037/1040-3590.11.3.326. [DOI] [Google Scholar]
- Laursen B, & Collins WA (2009). Parent-child relationships during adolescence In (3rd ed.). Lerner RM, & Steinberg L (Vol. Eds.), Handbook of adolescent psychology: Contextual influences on adolescent development: Vol. 2, (pp. 3–42). Hoboken, NJ, US: John Wiley & Sons Inc. [Google Scholar]
- Leen-Feldner EW, Blumenthal H, Babson K, Bunaciu L, & Feldner MT (2008). Parenting-related childhood learning history and panic vulnerability: A test using a laboratory-based biological challenge procedure. Behaviour Research and Therapy, 46(9), 1009–1016. 10.1016/j.brat.2008.06.00. [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Reardon LE, McKee LG, Feldner MT, Babson KA, & Zvolensky MJ (2006). The interactive role of anxiety sensitivity and pubertal status in predicting anxious responding to bodily sensations among adolescents. Journal of Abnormal Child Psychology, 34(6), 799–812. 10.1007/s10802-006-9079-y. [DOI] [PubMed] [Google Scholar]
- Lépine J (2002). The epidemiology of anxiety disorders: prevalence and societal costs. The Journal of Clinical Psychiatry, 63, 4–8. [PubMed] [Google Scholar]
- Lynch P, & Galbraith K (2003). Panic in the emergency room. Canadian Journal of Psychiatry, 48(6), 361–366. [DOI] [PubMed] [Google Scholar]
- Moore PS, Whaley SE, & Sigman M (2004). Interactions between mothers and children: Impacts of maternal and child anxiety. Journal of Abnormal Psychology, 113(3), 471–476. 10.1037/0021-843X.113.3.471. [DOI] [PubMed] [Google Scholar]
- Mowrer OH (1960). Learning theory and behavior. New York: Wiley. [Google Scholar]
- Naragon-Gainey K, Prenoveau JM, Brown TA, & Zinbarg RE (2016). A comparison and integration of structural models of depression and anxiety in a clinical sample: Support for and validation of the tri-level model. Journal of Abnormal Psychology, 125(7), 853–867. 10.1037/abn000019z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olatunji BO, Wolitzky-Taylor KB, Babson KA, & Feldner MT (2009). Anxiety sensitivity and CO2 challenge anxiety during recovery: Differential correspondence of arousal and perceived control. Journal of Anxiety Disorders, 23(4), 420–428. 10.1016/j.janxdis.2008.08.006. [DOI] [PubMed] [Google Scholar]
- Oppenheimer CW, Ladouceur CD, Waller JM, Ryan ND, Allen KB, Sheeber L, … Silk JS (2016). Emotion socialization in anxious youth: Parenting buffers emotional reactivity to peer negative events. Journal of Abnormal Child Psychology, 44(7), 1267–1278. 10.1007/s10802-015-0125-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor TG (2002). Annotation: The ‘effects’ of parenting reconsidered: Findings, challenges, and applications. Journal of Child Psychology and Psychiatry, 43, 555–572. 10.1111/1469-7610.00046. [DOI] [PubMed] [Google Scholar]
- Pincus DB, May JE, Whitton SW, Mattis SG, & Barlow DH (2010). Cognitive–behavioral treatment of panic disorder in adolescence. Journal of Clinical Child and Adolescent Psychology, 39(5), 638–649. 10.1080/15374416.2010.501288. [DOI] [PubMed] [Google Scholar]
- Rachmann S (1977). The conditioning theory of fear-acquisition: a critical examination. Behaviour Research and Therapy, 15(5), 375–387. 10.1016/0005-7967(77)90041-9. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Schniering CA, & Hudson JL (2009). Anxiety disorders during childhood and adolescence: Origins and treatment. Annual Review of Clinical Psychology, 5, 311–341. 10.1146/annurev.clinpsy.032408.153628. [DOI] [PubMed] [Google Scholar]
- Reardon LE, Leen-Feldner EW, & Hayward C (2009). A critical review of the empirical literature on the relation between anxiety and puberty. Clinical Psychology Review, 29, 1–23. 10.1016/j.cpr.2008.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sameroff A (2010). A unified theory of development: A dialectic integration of nature and nurture. Child Development, 81(1), 6–22. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Fleisig W, Rabian B, & Peterson RA (1991). Child anxiety sensitivity index. Journal of Clinical Child Psychology, 20(2), 162–168. 10.1207/s15374424jccp2002_7. [DOI] [Google Scholar]
- Silverman WK, Kurtines WM, Jaccard J, & Pina AA (2009). Directionality of change in youth anxiety treatment involving parents: An initial examination. Journal of Consulting and Clinical Psychology, 77(3), 474–485. 10.1037/a0015761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH, Taylor S, Jang KL, Cox BJ, Watt MC, Fedoroff IC, et al. (2001). Causal modeling of relations among learning history, anxiety sensitivity, and panic attacks. Behaviour Research and Therapy, 39, 443–456. 10.1016/S0005-7967(00)00023-1. [DOI] [PubMed] [Google Scholar]
- Stolz HE, Barber BK, & Olsen JA (2005). Toward disentangling fathering and mothering: An assessment of relative importance. Journal of Marriage and Family, 67(4), 1076–1092. 10.1111/j.1741-3737.2005.00195.x. [DOI] [Google Scholar]
- Susman EJ, & Rogol A (2004). Puberty and psychological development In Lerner RM, & Steinberg L (Eds.). Handbook of adolescent psychology (pp. 15–44). Hoboken, NJ, US: John Wiley & Sons Inc. [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, … Cardenas SJ (2007). Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment, 19, 176–188. 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- U.S. Bureau of the Census (2010). State and county quick facts. Retrieved from: http://quickfacts.census.gov/qfd/states/05/05143.html.
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. 10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watt MC, & Stewart SH (2000). Anxiety sensitivity mediates the relationships between childhood learning experiences and elevated hypochondriacal concerns in young adulthood. Journal of Psychosomatic Research, 49, 107–118. 10.1016/S0022-3999(00)00097-0. [DOI] [PubMed] [Google Scholar]
- Watt MC, Stewart SH, & Cox BJ (1998). A retrospective study of the learning history origins of anxiety sensitivity. Behaviour Research and Therapy, 36(5), 505–525. 10.1016/S0005-7967(97)10029-8. [DOI] [PubMed] [Google Scholar]
- Whaley SE, Pinto A, & Sigman M (1999). Characterizing interactions between anxious mothers and their children. Journal of Consulting and Clinical Psychology, 67(6), 826–836. 10.1037/0022-006X.67.6.826. [DOI] [PubMed] [Google Scholar]
- Whitehead WE, Busch CM, Heller BR, & Costa PT (1986). Social learning influences on menstrual symptoms and illness behavior. Health Psychology, 5, 13–23. 10.1037/0278-6133.5.1.1. [DOI] [PubMed] [Google Scholar]
- Wood JJ, McLeod BD, Piacentini JC, & Sigman M (2009). One-year follow-up of family versus child CBT for anxiety disorders: Exploring the roles of child age and parental intrusiveness. Child Psychiatry and Human Development, 40(2), 301–316. 10.1007/s10578-009-0127-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray-Lake L, Crouter AC, & McHale SM (2010). Developmental patterns in decision making autonomy across middle childhood and adolescence: European American parents perspectives. Child Development, 81(2), 636–651. 10.1111/j.1467-8624.2009.01420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright DB, London K, & Field AP (2011). Using bootstrap estimation and the plugin principle for clinical psychology data. Journal of Experimental Psychopathology, 2(2), 252e270 10.5127/jep.013611. [DOI] [Google Scholar]