Abstract
Background
Sleep-related disorders are a group of illnesses with marked effects on patients’ quality of life and functional ability. Their diagnosis and treatment is a matter of common interest to multiple medical disciplines.
Methods
This review is based on relevant publications retrieved by a selective search in PubMed (Medline) and on the guidelines of the German Society for Sleep Medicine, the German Neurological Society, and the German Association for Psychiatry, Psychotherapy and Psychosomatics.
Results
A pragmatic classification of sleep disorders by their three chief complaints—insomnia, daytime somnolence, and sleep-associated motor phenomena—enables tentative diagnoses that are often highly accurate. Some of these disorders can be treated by primary care physicians, while others call for referral to a neurologist or psychiatrist with special experience in sleep medicine. For patients suffering from insomnia as a primary sleep disorder, rather than a symptom of another disease, meta-analyses have shown the efficacy of cognitive behavioral therapy, with high average effect sizes. These patients, like those suffering from secondary sleep disorders, can also benefit from drug treatment for a limited time. Studies have shown marked improvement of sleep latency and sleep duration from short-term treatment with benzodiazepines and Z-drugs (non-benzodiazepine agonists such as zolpidem and zopiclone), but not without a risk of tolerance and dependence. For sleep disorders with the other two main manifestations, specific drug therapy has been found to be beneficial.
Conclusion
Sleep disorders in neurology and psychiatry are a heterogeneous group of disorders with diverse manifestations. Their proper diagnosis and treatment can help prevent secondary diseases and the worsening of concomitant conditions. Care structures for the treatment of sleep disorders should be further developed.
Sleep is essential for a person’s health and wellbeing. Disturbed sleep reduces the quality of life and restfulness of sleep, is a risk factor for secondary diseases and may be caused by other medical conditions. Sleep is a dynamic and complex behavioral process. Sleep disturbances may occur in this complexity. The International Classification of Sleep Disorders pragmatically groups disorders into six major categories (table 1) (1). Patients reporting sleeping problems, typically do not follow the structure of the classification, but describe the following 3 cardinal symptoms:
Table 1. Classification of sleep disorders according to ICSD-3 with typical examples and symptoms*.
| ICSD-3 major category | Exemplary diagnosis | Typical symptoms |
| Insomnias | Chronic insomnia | Disorder of initiating and maintaining sleep |
| Sleep-related breathing disorders | Obstructive sleep apnea syndrome (OSAS) | Excessive daytime sleepiness |
| Central disorders of hypersomnolence | Narcolepsy | Excessive daytime sleepiness, cataplexy (with narcolepsy) |
| Parasomnias | Somnambulism | Nighttime movements, getting up |
| Sleep-related movement disorders | Restless legs syndrome | Urge to move legs, disorder of initiating sleep |
| Circadian rhythm sleep disorders | Shift work, jetlag | Disorders of initiating and maintaining sleep, early awakening, excessive daytime sleepiness, indigestion |
* ICSD-3, International Classification of Sleep Disorders (1). The new ICD-11 classification (scheduled to be effective from 1 January 2022) will feature a separate chapter dedicated to sleep disorders (chapter 7 “sleep-wake disorders“) to highlight the clinical relevance of sleep disorders. The classification of disorders will be partially regrouped, the pragmatic strategy of a symptom-oriented approach will be emphasized.
The inability to fall asleep or sleep through the night
Excessive daytime sleepiness; or
Sleep-related movement phenomena.
The diversity of sleep-related disorders is reflected in the variety of specialties involved in the care of these patients—ranging from respiratory medicine to otorhinolaryngology to dentistry. The aim of this review is to describe the sleep-related disorders directly linked to neurology and psychiatry and present these according to their chief complaints (table 1).
Methods
This review includes original articles, reviews, and meta-analyses. It is based on pertinent publications retrieved by a selective search in PubMed (Medline), while also taking secondary literature into account. The guidelines of the German Society of Sleep Medicine (DGSM, Deutsche Gesellschaft für Schlafmedizin), the German Society of Neurology (DGN, Deutsche Gesellschaft für Neurologie) and the German Association for Psychiatry, Psychotherapy and Psychosomatics (DGPPN, Deutsche Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde) were also included in this review. The levels of evidence were determined following the recommendations of the Association of the Scientific Medical Societies in Germany (AWMF).
Cardinal symptom: Disorders of initiating and maintaining sleep
Disorders of initiating and maintaining sleep are collectively referred to as insomnias (Box 1). They represent the typical cardinal symptom of “poor sleep”. Transient (acute, short-term) insomnia has a 1-year prevalence of up to 30%, but does not necessarily require treatment due to its short duration. If it persists for more than 4 weeks, is of high intensity or associated with other signs and symptoms, a comprehensive work-up is indicated (2). Insomnia may be a symptom of an underlying disease or a distinct entity.
BOX 1. 5 tips for good sleep.
The bedroom should be a quiet space reserved for sleeping.
Regular habits of going to bed and falling asleep improve sleep.
Keeping a regular sleep schedule improves sleep.
Alcohol is not a suitable sleeping aid.
Relaxation exercises help to switch to sleep.
Insomnia as a primary disorder
Disorders of initiating and maintaining sleep, which have a negative impact on performance or daytime wellbeing and which cannot be explained by other underlying medical issues, are referred to as nonorganic insomnia, a common condition, affecting 6% of the population in Western industrialized countries (3). Nonorganic insomnia takes a chronic course, with more than 70% of persons with insomnia still meeting the diagnostic criteria after one year (e1). Women are one and a half times as likely to be affected as men and the condition is more prevalent among older people. Insomnia results in reduced quality of life (e2) and limitations in performance (e3). In addition, longitudinal studies have shown that insomnia is a risk factor for cardiovascular disease (risk ratio [RR]: 1.3–1.5), diabetes (RR: 1.5–1.8), depression (odds ratio [OR]: 2.1), and suicidality (RR: 1.9–3.0) (e4– e7). It is likely that insomnia is also a risk factor for dementia (e8), anxiety disorders (e9), and alcohol dependence (e10). Hence, sleep disorders and health are closely related in a bidirectional fashion. Insomnia is associated with a significant increase in consumption of health services, along with higher levels of absence from work and reduced work performance (4)
Epidemiological studies have found that sleep disorders are increasing in prevalence (e11). The guidelines recommend psychotherapy specifically designed for sleep problems, so-called cognitive behavioral therapy for insomnia (CBT-I, core modules in Table 2), for which, on average, large effect sizes have been found (5– 6; e11), as demonstrated in meta-analyses with large effect sizes (improvement of the measured values by 0.5 to 1 standard deviation) and level Ia evidence (e12). Studies have been conducted to determine how many patients actually receive treatment; according to expert estimates, it is only a minority of those affected (5, 7). By contrast, sleeping pills are not recommended as the primary treatment option for insomnia (6, 7). Medications can be used for short-term support; in this case, they are similar to those used to treat symptomatic insomnia (table 3).
Table 2. Core modules of cognitive behavioral therapy for insomnia (CBT-I).
| Module | Description |
| Psychoeducation | Information about “sleep hygiene rules“ and basic information about sleep and sleep disorders |
| Relaxation techniques | Methods of physical and mental relaxation (e.g. progressive muscle relaxation; guided visualization) |
| Bedtime restriction | Temporary significant restriction of the amount of time spent in bed during the night to the average amount of sleep with subsequent adjustment of the amount of time spent in bed in the weekly rhythm. To this end, the average sleep efficiency (sleeping time/bed time) is calculated for one week; in case of high values (e.g. >90%), the bedtime for the following week is extended by e.g. 30 min, while in case of low values (e.g. <80%) the bedtime for the following week is shortened by e.g. 30 min |
| Stimulus-control therapy | Reassociation of the sleeping environment with the behavior “sleep” by asking the patient not to engage in any activities other than sleep in bed and to get out of bed if unable to fall asleep in 15–30 minutes. |
| Cognitive techniques | Psychological methods to reduce worrying or to challenge and change dysfunctional sleep- and insomnia-related cognitions (e.g. the dysfunctional cognitions “The sleep before midnight is the healthiest sleep“, “everyone needs 8 hours of sleep“ or “If I don’t get enough sleep, I will not be able to function tomorrow“) |
Table 3. Symptomatic drug therapy of insomnias*.
| Substance (and dose) |
Effect depending on the study population |
Notes |
| Benzodiazepines and Z-drugs | Zopiclone: Sleep latency − 12 min Sleep duration + 28 min (LoE Ia; e17) (9) |
Approved for the treatment of primary insomnia; typically, it is not used longer than 4 weeks. Warning: development of tolerance and dependence |
| Melatonin | Sleep latency − 5 min Sleep duration n.s. (LoE Ia; e18) |
Approved in prolonged-release dosage form for the treatment of insomnia in patients over 55 years of age |
| Mirtazapine (3.75–15 mg) | Sleep latency − 2 min Sleep duration + 9 min (LoE IIb; e19–e20) |
Primarily for symptomatic sleep disorder associated with depression, not approved for the treatment of primary insomnia (“off-label“ use) |
| Doxepin (1–50 mg) | Sleep latency − 3 min Sleep duration + 24 min (LoE Ib; e21–e22) |
Primarily for symptomatic sleep disorder associated with depression; in some cases, very low doses (drops) highly effective; not approved for the treatment of primary insomnia (“off-label“ use) |
| Quetiapine (25–75 mg) | Sleep latency − 2 min Sleep duration + 14 min (LoE IIb; e20) |
Primarily for symptomatic sleep disorder associated with depression and psychotic disorders; not approved for the treatment of primary insomnia (“off-label“ use) |
| Trimipramine (50–100 mg) | Sleep efficiency + 7% Sleep duration + 18 min (LoE IIb; e23) |
Often used with good clinical response; improves sleep efficiency, but not overall sleep time. |
| Melperone/Pipamperone | No controlled trials (LoE V) | Older butyrophenones, used primarily in gerontopsychiatry („off label“ use) |
Secondary insomnias
Insomnia may be caused by other medical conditions (box 2). With more than 50% of disorders of initiating and maintaining sleep being caused by psychiatric illnesses (including addiction), psychiatric examination plays a key role in the assessment of insomnia (7). Similarly, diseases of the central and peripheral nervous system, such as restless legs syndrome (RLS), are among the most common causes of insomnia; thus, neurological evaluation is conducive to diagnosing important underlying problems. In patients with abnormal breathing during sleep, the chief complaint of excessive daytime tiredness is very prominent; therefore, the often present disorder of initiating and maintaining sleep should be explicitly addressed during history taking (10).
BOX 2. Secondary causes of disorders of initiating and maintaining sleep*.
Psychiatric disorders (e.g. depression, anxiety disorders, alcohol dependence)
Disorders of the central nervous system
(e.g. neurodegenerative, inflammatory, tumor)
Disorders of the peripheral nervous system
(e.g. polyneuropathies)
Restless legs syndrome
Sleep-related breathing disorders (e.g. obstructive sleep apnea syndrome)
Cardiac disease (e.g. heart failure)
Endocrine disorders (e.g. hyperthyroidism)
External factors (e.g. noise, light, shift work)
*also refer to (7)
Treatment should be directed at the cause. While basic treatment can be provided by general practitioners, more complex constellations require the involvement of a specialized physician or sleep specialist. Pharmacological intervention should be specific, e.g. a sedating antidepressant should be used to treat patients with depression-related sleep disorder. Symptomatic treatment with traditional sleeping pills and other GABA (?-aminobutyric acid)ergic substances (Z-drugs such as zolpidem and zopiclone) should typically be short term (up to 4 weeks) (5, e13) (table 3). The behavioral treatment strategies for nonorganic insomnia described above have been proven beneficial for symptomatic sleep disorders as well, if the condition causing insomnia cannot be completely eliminated. This is supported by evidence from, for example, meta-analyses on the use of CBT-I to treat insomnia in patients with posttraumatic stress disorder (e14), cancer (e15), or chronic pain (e16); here, again, moderate to large effect sizes were achieved.
Circadian rhythm disorders
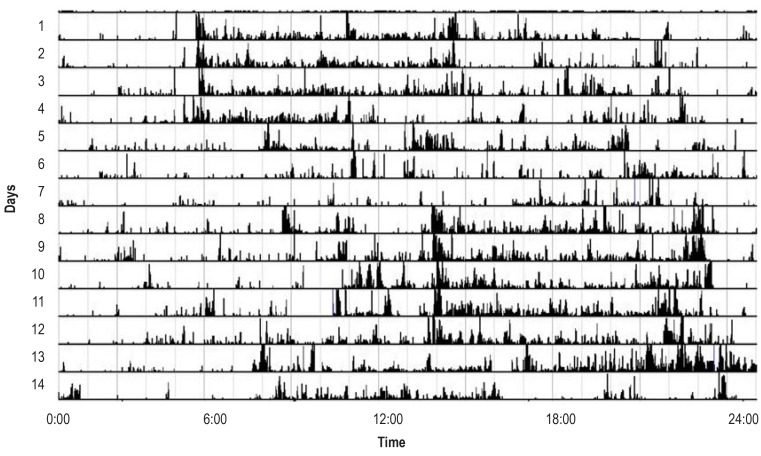
A distinct cause of insomnia are disturbances of the internal (“body”) clock. Circadian rhythm abnormalities are characterized by deviation of the internal body rhythm (e.g. sleep, digestion) from the external time of the day, e.g. being awake at night or sleeping during the day. A broad spectrum of related disorders illustrates the effect of the internal clock, influencing the activity of every system of the body throughout the day. Shift work (in Germany 10.8% night work, 13.5% rotating shift work, and 35.3% evening work, Figure 1) (e24) and jetlag (traveling to different time zones) are among the most common reasons for disturbances of the internal clock. They can have a massive negative impact on sleep (e25, e26).
Figure 1.
Actimetry of a shift worker over a 2-week period. Four days of morning shift are followed by three days off work and then five days of late shift, identified by the significantly higher level of activity (height of the black bars) on the way to work at the beginning and end of the working day. The sleep is disturbed by frequent awakenings, no consolidated circadian activity–rest rhythm can be identified.
The lack of daily circadian adaption (typically, the rhythm is slightly longer than 24 hours) results in a constantly shifting, non-synchronous periodicity compared to the day–night rhythm (e27). Frequently, blind people are affected, because light as a timer does not get through to their internal clock. In periods of significant divergence between internal and external time, sleep disorders (the internal clock triggers activity at nighttime) and daytime tiredness (due to sleep deprivation and the internal clock demanding rest) can occur. These disorders are diagnosed based on the medical history, actimetry findings and sleep diary records (e28). Actimetry shows the shift of the rhythm compared to the day–night rhythm. Treatment is based on behavioral interventions and melatoninergic drugs which restore normal rhythm in 40–57% of cases (level Ib evidence; e29, e30). The melatonin receptor agonist tasimelteon has recently been approved for non-24-hour sleep–wake disorder in blind individuals (e31, e32).
Chief complaint: excessive daytime sleepiness
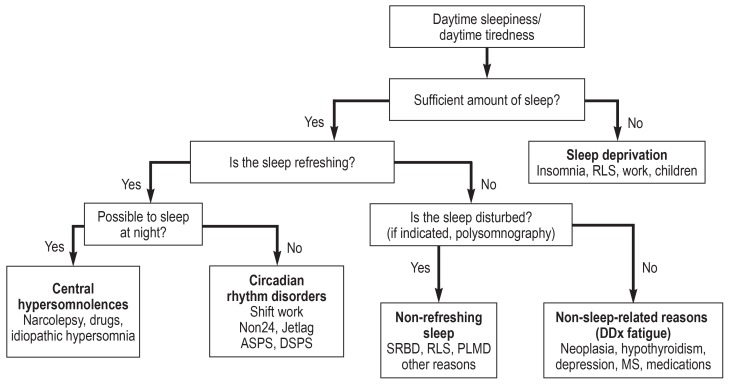
Sleepiness and sudden sleep attacks during the daytime have a negative impact on performance and may be indicative of abnormal sleep regulation or disturbed sleep at night. Sleepiness can be measured using the Epworth Sleepiness Scale (ESS) (e33) and be objectively determined after a night in the sleep laboratory using the Multiple Sleep Latency Test (MSLT) (figure 2). Especially in patients with comorbidities such as cancer or multiple sclerosis, it can be difficult to distinguish it from daytime tiredness and/or fatigue (reduced performance and feeling of exhaustion) (11).
Figure 2.
Diagnostic flowchart for daytime sleepiness/daytime tiredness. The diagnoses are only examples, comorbid causes may be present. ASPS/DSPS, advanced/delayed sleep phase syndrome; DDx, differential diagnosis; MS, multiple sclerosis; Non24, non–24-hour sleep–wake disorder; PLMD, periodic leg movement disorder; RLS, restless legs syndrome; SRBD, sleep-related breathing disorders
Central disorders of hypersomnolence
Narcolepsy and idiopathic hypersomnia are disorders typically associated with excessive daytime tiredness (tiredness without falling asleep in monotonous situations) and fall into the category of “central disorders of hypersomnolence“. The primary symptom is always excessive daytime sleepiness (uncontrollable episodes of falling asleep during the daytime) and/or prolonged sleep not explained by other sleep disorders or other medical conditions. Another central symptom, which is also used to distinguish between two types of narcolepsy, is cataplexy (type I narcolepsy with cataplexy; type 2 narcolepsy without cataplexy). Facultative symptoms include hypnagogic/hypnopompic hallucinations, sleep paralysis, automatic behaviors, and fragmented sleep at night (12).
The overall prevalence of narcolepsy is 25–50 per 100 000 population, with an incidence of 0.8/100 000 (e34). The pathogenesis of the two types of narcolepsy is not fully understood. Given the strong HLA association (the HLA marker DQB1*0602 is present in 98% of patients with type 1 narcolepsy, but only in 23% of healthy controls [e35]), autoimmunity is assumed to be involved in the pathogenesis; however, the diagnostic significance of typing is limited to a supporting role, due to the prevalence of the marker in the general population (e35). Pathophysiologically, there is a disturbance of the hypocretin/orexin system (controlling wakefulness) and the histamine system. Reduced hypocretin levels in cerebrospinal fluid (CSF) were found in over 80% of patients with type 1 narcolepsy (e36). CFS hypocretin-1 levels below 110 pg/mL are considered diagnostic of type 1 narcolepsy. This may be a starting point for the development of future biological treatments (13).
The multiple sleep latency test (MSLT) is the key technical investigation. The test consists of five scheduled naps during the daytime in a sleep laboratory setting. Here, daytime sleep latency (threshold: <8 minute) and the occurrence of REM sleep periods are key diagnostic requirements (e37). The test is performed to rule out rare (about 7%), but treatment-relevant symptomatic types of narcolepsy, such as anti-Ma2–associated encephalitis (e38).
In many cases, the various narcolepsy symptom complexes respond well to treatment. Table 4 summarizes selected medications; the reader is referred to the DGSM guideline for more information (11).
Table 4. Selected medications for the treatment of narcolepsy.
| Agent | Indication | Posology |
| Modafinil | EDS (LoE Ia; e39–e40) | 200–400 mg/d, max. 600 mg |
| Methylphenidate (controlled substance prescription required) | EDS (LoE II; e39) | 10–60 mg/d |
| Pitolisant | EDS (LoE Ib; e41) cataplexy (LoE Ib; e41) | 4.5–36 mg |
| Sodium oxybate (controlled substance ‧prescription required) | EDS, cataplexy (reduced by 90%) Improvement of nighttime sleep (LoE for both Ib; e39, e42) |
4.5–9 g/d |
| Clomipramine | Cataplexy (LoE III; e39, e43) | 10–150 mg/d |
| Venlafaxine | Cataplexy (LoE IV; e39, e44) | 37.5–300 mg/d not approved |
EDS, excessive daytime sleepiness; LoE, level of evidence
Idiopathic hypersomnia
Idiopathic hypersomnia is an important differential diagnosis of narcolepsy (14). It is characterized by excessive daytime sleepiness without the REM-associated symptoms, such as sleep paralysis or cataplexy. The condition is diagnosed in the presence of clinical symptoms of daytime sleepiness without REM-associated symptoms and a daytime sleep latency of less than 8 minutes in the MSLT (14). While modafinil has proved effective in the treatment of idiopathic hypersomnia (e45), it is not approved for this indication so that reimbursement of costs can be problematic.
Other disorders associated with excessive daytime tiredness
Sleep-related breathing disorders are one of the most important and most common conditions requiring sleep medical care; as distinct entities, these conditions are outside the scope of this review. About 2% to 7% of adults suffer from obstructive sleep apnea (OSAS); prevalence rates have not yet become available for Germany (10).
Besides excessive daytime sleepiness, OSAS has clinically relevant associations with neurological and psychiatric conditions. The prevalence of OSAS is found significantly increased in psychiatric patients. If left untreated, OSAS can complicate the treatment of depression (e46); on the other hand, excessive daytime tiredness in patients with OSAS is an important differential diagnosis of reduced drive and symptoms of fatigue in patients with depression (e47). Patients with neurological disorders also have relevant comorbidities. Today, OSAS is recognized as an independent risk factor for cardiovascular disease (hazard ratio [HR]: 2.23 for stroke) (e48, e49). It is also a relevant risk factor for the development of atrial fibrillation (HR: 1.55–2.18) (e50) and has a negative impact on survival after stroke (HR: 1.76 for premature mortality) (49). If patients with epilepsy suffer from obstructive sleep apnea, seizure control with medication is significantly more difficult to achieve (e51).
Chief complaint: involuntary sleep-related movements
Involuntary individual movements or movement patterns during sleep are only partially perceived by the patient; in the majority of cases with sleep-related movement disorders, the condition is detected by injuries of the patient or the bedpartner, or by reports of the bed partner. Diagnoses typically associated with motor symptoms are parasomnias (e.g. sleepwalking) and restless legs syndrome. Parasomnias are classified into rapid eye movement (REM) sleep and non–rapid eye movement (NREM) sleep parasomnias. Nocturnal seizures—typically requiring examination in a sleep laboratory or seizure monitoring unit—are the main differential diagnosis of parasomnias (15).
NREM parasomnias
NREM parasomnias, such as sleep (night) terrors (sudden awakening from sleep, frequently associated with crying or screaming) and somnambulism are common (up to 35% and 17%, respectively, depending on age group) (16, e52) and reason to visit a doctor at the time of first manifestation. It can be effectively treated. In this context, protection against self-injury should be ensured (sleepwalkers do not avoid danger with “somnambulistic confidence“) and the sleepers and their families adequately counseled (e53, e54). Commonly, NREM parasomnias start in childhood or adolescence and become less intense or stop in adulthood. Prevalence increases again in the elderly (also drug-induced); such potential drug side effects should be taken into consideration (table 5) (16, 17, e55).
Table 5. Medications with somnambulism as a potential side effect (17)*.
| GABAergic substances | Psychotropic drugs | Antipsychotics | Other medications |
| Zolpidem | Amitriptyline | Olanzapine | Propranolol, metoprolol |
| Zopiclone | Paroxetine, fluoxetine | Quetiapine | Ciprofloxacin |
| Zaleplon | Mirtazapine, reboxetine | Chlorprothixene | |
| Bupropion | |||
| Lithium |
* “Somnambulism“ is a well described side effect of the two common Z-drugs (zolpidem and zopiclone); for the other medications (italics), the available information comes from anecdotic reports. Nighttime eating attacks may also be a symptom.
REM sleep behavior disorder
REM-sleep behavior disorder (RBD) is characterized by movements during REM sleep, at times associated with vocalizations (talking, shouting, or screaming). Simultaneously, complex movements may be displayed which are associated with significant risk of injury to self or others. The existing questionnaires on RBD (REM Sleep Behavior Questionnaire, RBDSQ) (18) are not very sensitive, since patients typically miss (“oversleep”) their symptoms (e56). Therefore, a third-party medical history and examination in a sleep laboratory are required for a definite diagnosis of RBD. The latter demonstrates the characteristic increase in muscle tone during REM sleep (1). A fact that increases the relevance of RBD is that it is thought to be a precursor to neurodegenerative disease, such as Parkinson’s disease or multiple system atrophy (45–81%, depending on the observational period) (19, e57); therefore, it will be of special significance to future treatment studies as a specific early symptom of neurodegeneration (e58). More than 50% of all patients with Parkinson’s disease experience RBD, albeit of various severity; treatment should comprise prevention of injuries and pharmacotherapy with clonazepam (0.5–2 mg) or melatonin (2–10 mg).
Restless legs syndrome (RLS)
RLS is one of the most common neurological diseases, but despite its typical symptoms diagnosis is often delayed. With a prevalence of 6% to 9% (female: male 1.5–2 : 1, [e59]), 0.5 to 1% of the general population require pharmacological treatment (e60), especially older and multimorbid patients (e61).
Clinically, RLS is diagnosed based on “four essential criteria“ (20):
Unpleasant sensations (paresthesia, pain, formication) accompanied by an urge to move, usually of the legs
Typically occurring during periods of rest
Partially or totally relieved by movement
Circadian rhythm with worsening in the evening or at night, causing sleep disturbance.
A new fifth criterion (“The symptoms are not explained by another condition”) makes the diagnosis more specific. Supportive criteria include response to dopaminergic medication, positive family history, and detection of periodic limb movement during sleep (PLMS); these criteria are unspecific, but occur in up to 80% of patients and can cause the patient to wake up. Many RLS patients primarily complain of disorders of initiating and maintaining sleep and only report the essential criteria when specifically asked about them.
The validity of the commonly used classification into “primary“ and “secondary“ RLS is contestable (e62), because the RLS phenotype manifests as the result of an interaction between genetic factors and comorbidities, such as iron deficiency in women as well as chronic kidney disease, heart disease, diabetes, and Parkinson’s disease (21). Medications, such as antipsychotics, antidepressants of the selective serotonin reuptake inhibitor (SSRI) type, and possibly steroids and ß-adrenergic agonists (asthma treatment) can trigger symptoms of RLS. Typically, exacerbation of RLS is observed with mirtazapine, which is often used as a sleep-promoting treatment by patients with insomnia (e63).
Polysomnography may be required to rule out other sleep disorders or if the diagnosis cannot be established based on the medical history. Moderate to severe RLS should be treated with medication after stopping treatment with any RLS-aggravating drugs. Iron deficiency should be corrected with iron supplementation (level of evidence [LoE] Ia; e64–e65). RLS is treated with dopamine agonists (pramipexole, ropinirole, or rotigotine, LoE Ia) (22), administered in the respective lowest approved doses; alternatively, gabapentin or pregabalin can be used (effective, but not approved for this indication; LoE Ia) (22, 23). Second-line treatments for severe RLS are low-dose prolonged-release opioids; prolonged-release oxycodone/naloxone is approved as a second-line treatment (level Ib evidence) (22, 24, e66).
The greatest challenge in the treatment of RLS is augmentation, an increase in RLS symptoms after an initially good response to dopaminergic medication. Dopaminergic augmentation is characterized by a worsening of the RLS symptoms (after increasing the dose of dopaminergic treatment) which start to occur earlier in the day and spread to other body parts (arms). Augmentation is treated by rigorously reducing the dose of the dopaminergic medication and starting the patient on a combination therapy with other substances (e66).
Conclusion
Due to their significant negative impact on quality of life, sleep-related disorders in neurology and psychiatry are highly relevant to patients (25, e2). Their presentation is more complex than the symptom of “poor sleep” reported by a patient; thus, when taking the patient’s history, specific questions should be asked to reveal symptoms of sleep-related disorders and associated illnesses, such as depression. Properly diagnosed sleep-related disorders respond well to treatment, but require a differentiated therapeutic strategy. However, in Germany, the current structures for healthcare provision do not cover all patients; depending on the diagnosis, some patients (e.g. with insomnia) may miss out as only few specialized centers for the treatment of patients with sleep-related neurological and psychiatric disorders exist in Germany. Thus, it is critical to establish new treatment structures, complementing the existing offering, in the future.
Key Messages.
Healthy and disturbed sleep both influence quality of life.
Disturbed sleep has a significant impact on other conditions.
The subjective complaints can be classified into insomnia, increased daytime sleepiness, and abnormal behavior during sleep.
Treatment should address any underlying condition and not be primarily based on the use of sleeping pills.
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Footnotes
Conflict of interest statement Prof. Trenkwalder received consultancy fees from Benevolent, Roche, and Novartis. For the preparation of scientific seminars, she received funds from UCB, Grünenthal, and Otsuka. For a research project that she initiated, she received funds from Mundipharma. For the conduct of clinical studies, she received funds from Vifor Pharma.
PD Rémi received fees for Advisory Board activities as well as lecture fees from Vanda. He received lecture fees from Vanda and bioproject. For carrying out clinical trials on a contract basis, he received funds from Kappa Saute.
Prof. Young received lecture fees from Adboard, Medice, Vanda, and Sanofi-Genzyme. He received reimbursement of meeting participation fees for congresses as well as travel and accommodation expenses from Medice and Vanda. He received fees for preparing continuing medical education events from Medice and Vanda.
Prof. Pollmächer and Prof. Spiegelhalder declare that no conflict of interests exists.
References
- 1.American Academy of Sleep Medicine. The International Classification of Sleep Disorders - Third Edition (ICSD-3) Darien, Il, Il: American Academy of Sleep Medicine. 2014 [Google Scholar]
- 2.Pollmächer T, Wetter TC, Happe S, Richter K, Acker J, Riemann D. Schlafmedizinische Differenzialdiagnostik in Psychiatrie und Psychotherapie. Nervenarzt. 2014;85:57–66. doi: 10.1007/s00115-013-3895-4. [DOI] [PubMed] [Google Scholar]
- 3.Morin CM, Drake CL, Harvey AG, et al. Insomnia disorder. Nat Rev Dis Prim. 2015;1 doi: 10.1038/nrdp.2015.26. [DOI] [PubMed] [Google Scholar]
- 4.Kucharczyk ER, Morgan K, Hall AP. The occupational impact of sleep quality and insomnia symptoms. Sleep Med Rev. 2012;16:547–559. doi: 10.1016/j.smrv.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Riemann D, Baum E, Cohrs S, et al. S3-Leitlinie Nicht erholsamer Schlaf/Schlafstörungen Kapitel „Insomnie bei Erwachsenen“. Somnologie. 2017;21:2–44. [Google Scholar]
- 6.Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26:675–700. doi: 10.1111/jsr.12594. [DOI] [PubMed] [Google Scholar]
- 7.Pollmächer T, Wetter TC. Schlafstörungen und psychische Erkrankungen. Stuttgart: Kohlhammer; 2017 [Google Scholar]
- 8.Everitt H, Baldwin DS, Stuart B, et al. Antidepressants for insomnia in adults. Cochrane Database Syst Rev. 2018;5 doi: 10.1002/14651858.CD010753.pub2. CD010753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rösner S, Englbrecht C, Wehrle R, Hajak G, Soyka M. Eszopiclone for insomnia. Cochrane Database Syst Rev. 2018;10 doi: 10.1002/14651858.CD010703.pub2. CD010703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayer G, Arzt M, Braumann B, et al. S3-Leitlinie Nicht erholsamer Schlaf/Schlafstörungen Kapitel „Schlafbezogene Atmungsstörungen bei Erwachsenen“. Somnologie. 2017;20(Suppl s2) S97-180. [Google Scholar]
- 11.DGSM. S3-Leitlinie. Somnologie - Schlafforsch und Schlafmedizin. 2009;13 (S1):1–160. [Google Scholar]
- 12.Ruoff C, Rye D. The ICSD-3 and DSM-5 guidelines for diagnosing narcolepsy: clinical relevance and practicality. Curr Med Res Opin. 2016;32:1–12. doi: 10.1080/03007995.2016.1208643. [DOI] [PubMed] [Google Scholar]
- 13.Mahoney CE, Cogswell A, Koralnik IJ, Scammell TE. The neurobiological basis of narcolepsy. Nat Rev Neurosci. 2019;20:83–93. doi: 10.1038/s41583-018-0097-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Billiard M, Sonka K. Idiopathic hypersomnia. Sleep Med Rev. 2016;29:23–33. doi: 10.1016/j.smrv.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 15.Derry CP, Davey M, Johns M, et al. Distinguishing sleep disorders from seizures: diagnosing bumps in the night. Arch Neurol. 2006;63:705–709. doi: 10.1001/archneur.63.5.705. [DOI] [PubMed] [Google Scholar]
- 16.Stallman HM, Kohler M. Prevalence of sleepwalking: a systematic review and meta-analysis. Arez AP, editor. PLoS One. 2016;11 doi: 10.1371/journal.pone.0164769. e0164769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stallman HM, Kohler M, White J. Medication induced sleepwalking: a systematic review. Sleep Med Rev. 2018;37:105–113. doi: 10.1016/j.smrv.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 18.Stiasny-Kolster K, Mayer G, Schäfer S, Möller JC, Heinzel-Gutenbrunner M, Oertel WH. The REM sleep behavior disorder screening questionnaire—a new diagnostic instrument. Mov Disord. 2007;22:2386–2393. doi: 10.1002/mds.21740. [DOI] [PubMed] [Google Scholar]
- 19.Schenck CH, Boeve BF, Mahowald MW. Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series. Sleep Med. 2013;14:744–748. doi: 10.1016/j.sleep.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 20.Allen RP, Picchietti D, Hening WA, et al. Restless legs syndrome: Diagnostic criteria, special considerations, and epidemiology A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003;4:101–119. doi: 10.1016/s1389-9457(03)00010-8. [DOI] [PubMed] [Google Scholar]
- 21.Bartl M, Winkelmann J, Högl B, Paulus W, Trenkwalder C. Häufige neurologische Erkrankungen assoziiert mit dem Restless-legs-Syndrom. Nervenarzt. 2018;89:1156–1164. doi: 10.1007/s00115-018-0528-y. [DOI] [PubMed] [Google Scholar]
- 22.Winkelmann J, Allen RP, Högl B, et al. Treatment of restless legs syndrome: Evidence-based review and implications for clinical practice (Revised 2017) Mov Disord. 2018;33:1077–1091. doi: 10.1002/mds.27260. [DOI] [PubMed] [Google Scholar]
- 23.Allen RP, Chen C, Garcia-Borreguero D, et al. Comparison of pregabalin with pramipexole for restless legs syndrome. N Engl J Med. 2014;370:621–631. doi: 10.1056/NEJMoa1303646. [DOI] [PubMed] [Google Scholar]
- 24.de Oliveira CO, Carvalho LB, Carlos K, et al. Opioids for restless legs syndrome. Cochrane Database Syst Rev. 2016;6 doi: 10.1002/14651858.CD006941.pub2. CD006941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buysse DJ. Insomnia. JAMA. 2013;309 doi: 10.1001/jama.2013.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.Morin CM, Bélanger L, LeBlanc M, et al. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med. 2009;169:447–453. doi: 10.1001/archinternmed.2008.610. [DOI] [PubMed] [Google Scholar]
- E2.Kyle SD, Morgan K, Espie CA. Insomnia and health-related quality of life. Sleep Med Rev. 2010;14:69–82. doi: 10.1016/j.smrv.2009.07.004. [DOI] [PubMed] [Google Scholar]
- E3.Fortier-Brochu E, Beaulieu-Bonneau S, Ivers H, Morin CM. Insomnia and daytime cognitive performance: a meta-analysis. Sleep Med Rev. 2012;16:83–94. doi: 10.1016/j.smrv.2011.03.008. [DOI] [PubMed] [Google Scholar]
- E4.Li M, Zhang X-W, Hou W-S, Tang Z-Y. Insomnia and risk of cardiovascular disease: a meta-analysis of cohort studies. Int J Cardiol. 2014;176:1044–1047. doi: 10.1016/j.ijcard.2014.07.284. [DOI] [PubMed] [Google Scholar]
- E5.Anothaisintawee T, Reutrakul S, Van Cauter E, Thakkinstian A. Sleep disturbances compared to traditional risk factors for diabetes development: Systematic review and meta-analysis. Sleep Med Rev. 2016;30:11–24. doi: 10.1016/j.smrv.2015.10.002. [DOI] [PubMed] [Google Scholar]
- E6.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- E7.Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. 2012;73:e1160–e1167. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- E8.Shi L, Chen S-J, Ma M-Y, et al. Sleep disturbances increase the risk of dementia: a systematic review and meta-analysis. Sleep Med Rev. 2018;40:4–16. doi: 10.1016/j.smrv.2017.06.010. [DOI] [PubMed] [Google Scholar]
- E9.Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30:274–280. [PubMed] [Google Scholar]
- E10.Weissman MM, Greenwald S, Niño-Murcia G, Dement WC. The morbidity of insomnia uncomplicated by psychiatric disorders. Gen Hosp Psychiatry. 1997;19:245–250. doi: 10.1016/s0163-8343(97)00056-x. [DOI] [PubMed] [Google Scholar]
- E11.Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Clinical Guidelines Committee of the American College of Physicians Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165:125–133. doi: 10.7326/M15-2175. [DOI] [PubMed] [Google Scholar]
- E12.van Straten A, van der Zweerde T, Kleiboer A, Cuijpers P, Morin C, Lancee J. Cognitive and behavioral therapies in the treatment of insomnia: a meta-analysis. Sleep. 2018;38:3–16. doi: 10.1016/j.smrv.2017.02.001. [DOI] [PubMed] [Google Scholar]
- E13.Nissen C, Frase L, Hajak G, Wetter TC. Hypnotika - Stand der Forschung. Nervenarzt. 2014;85:67–76. doi: 10.1007/s00115-013-3893-6. [DOI] [PubMed] [Google Scholar]
- E14.Ho FYY, Chan CS, Tang KNS. Cognitive-behavioral therapy for sleep disturbances in treating posttraumatic stress disorder symptoms: a meta-analysis of randomized controlled trials. Clin Psychol Rev. 2016;43:90–102. doi: 10.1016/j.cpr.2015.09.005. [DOI] [PubMed] [Google Scholar]
- E15.Johnson JA, Rash JA, Campbell TS, et al. A systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy for insomnia (CBT-I) in cancer survivors. Sleep Med Rev. 2016;27:20–28. doi: 10.1016/j.smrv.2015.07.001. [DOI] [PubMed] [Google Scholar]
- E16.Tang NKY, Lereya ST, Boulton H, Miller MA, Wolke D, Cappuccio FP. Nonpharmacological treatments of insomnia for long-term painful conditions: a systematic review and meta-analysis of patient-reported outcomes in randomized controlled trials. Sleep. 2015;38:1751–1764. doi: 10.5665/sleep.5158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E17.Rösner S, Englbrecht C, Wehrle R, Hajak G, Soyka M. Eszopiclone for insomnia. Cochrane Database Syst Rev. 2018;10 doi: 10.1002/14651858.CD010703.pub2. CD010703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E18.Auld F, Maschauer EL, Morrison I, Skene DJ, Riha RL. Evidence for the efficacy of melatonin in the treatment of primary adult sleep disorders. Sleep Med Rev. 2017;34:10–22. doi: 10.1016/j.smrv.2016.06.005. [DOI] [PubMed] [Google Scholar]
- E19.Winokur A, DeMartinis NA, McNally DP, Gary EM, Cormier JL, Gary KA. Comparative effects of mirtazapine and fluoxetine on sleep physiology measures in patients with major depression and insomnia. J Clin Psychiatry. 2003;64:1224–1229. doi: 10.4088/jcp.v64n1013. [DOI] [PubMed] [Google Scholar]
- E20.Karsten J, Hagenauw LA, Kamphuis J, Lancel M. Low doses of mirtazapine or quetiapine for transient insomnia: a randomised, double-blind, cross-over, placebo-controlled trial. J Psychopharmacol. 2017;31:327–337. doi: 10.1177/0269881116681399. [DOI] [PubMed] [Google Scholar]
- E21.Hajak G, Rodenbeck A, Voderholzer U, et al. Doxepin in the treatment of primary insomnia: a placebo-controlled, double-blind, polysomnographic study. J Clin Psychiatry. 2001;62:453–463. doi: 10.4088/jcp.v62n0609. [DOI] [PubMed] [Google Scholar]
- E22.Krystal AD, Durrence HH, Scharf M, et al. Efficacy and safety of Doxepin 1 mg and 3 mg in a 12-week sleep laboratory and outpatient trial of elderly subjects with chronic primary insomnia. Sleep. 2010;33:1553–1561. doi: 10.1093/sleep/33.11.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E23.Riemann D, Voderholzer U, Cohrs S, et al. Trimipramine in primary insomnia: results of a polysomnographic double-blind controlled study. Pharmacopsychiatry. 2002;35:165–174. doi: 10.1055/s-2002-34119. [DOI] [PubMed] [Google Scholar]
- E24.Statistisches Bundesamt. Mikrozensus. www.destatis.de (last accessed on 9 April 2019) 2017 [Google Scholar]
- E25.Reid KJ, Abbott SM. Jet lag and shift work disorder. Sleep Med Clin. 2015;10:523–535. doi: 10.1016/j.jsmc.2015.08.006. [DOI] [PubMed] [Google Scholar]
- E26.Morgenthaler TI, Lee-Chiong T, Alessi C, et al. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An american academy of sleep medicine report. Sleep. 2007;30:1445–1459. doi: 10.1093/sleep/30.11.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E27.Emens JS, Laurie AL, Songer JB, Lewy AJ. Non-24-hour disorder in blind individuals revisited: variability and the influence of environmental time cues. Sleep. 2013;36:1091–1100. doi: 10.5665/sleep.2818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E28.Emens JS, Eastman CI. Diagnosis and treatment of non-24-h sleep-wake disorder in the blind. Drugs. 2017;77:637–650. doi: 10.1007/s40265-017-0707-3. [DOI] [PubMed] [Google Scholar]
- E29.Li T, Jiang S, Han M, et al. Exogenous melatonin as a treatment for secondary sleep disorders: a systematic review and meta-analysis. Front Neuroendocrinol. 2018;52:22–28. doi: 10.1016/j.yfrne.2018.06.004. [DOI] [PubMed] [Google Scholar]
- E30.Quera Salva MA, Hartley S, Léger D, Dauvilliers YA. Non-24-hour sleep-wake rhythm disorder in the totally blind: diagnosis and management. Front Neurol. 2017;8 doi: 10.3389/fneur.2017.00686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E31.Keating GM. Tasimelteon: a review in non-24-hour sleep-wake disorder in totally blind individuals. CNS Drugs. 2016;30:461–468. doi: 10.1007/s40263-016-0330-y. [DOI] [PubMed] [Google Scholar]
- E32.Lockley SW, Dressman MA, Licamele L, et al. Tasimelteon for non-24-hour sleep-wake disorder in totally blind people (SET and RESET): two multicentre, randomised, double-masked, placebo-controlled phase 3 trials. Lancet. 2015;386:1754–1764. doi: 10.1016/S0140-6736(15)60031-9. [DOI] [PubMed] [Google Scholar]
- E33.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- E34.Khatami R, Luca G, Baumann CR, et al. The European Narcolepsy Network (EU-NN) database. J Sleep Res. 2016;25:356–364. doi: 10.1111/jsr.12374. [DOI] [PubMed] [Google Scholar]
- E35.Coelho FMS, Pradella-Hallinan M, Predazzoli Neto M, Bittencourt LRA, Tufik S. Prevalence of the HLA-DQB1*0602 allele in narcolepsy and idiopathic hypersomnia patients seen at a sleep disorders outpatient unit in São Paulo. Rev Bras Psiquiatr. 2009;31:10–14. doi: 10.1590/s1516-44462009000100004. [DOI] [PubMed] [Google Scholar]
- E36.Liblau RS, Vassalli A, Seifinejad A, Tafti M. Hypocretin (orexin) biology and the pathophysiology of narcolepsy with cataplexy. Lancet Neurol. 2015;14:318–328. doi: 10.1016/S1474-4422(14)70218-2. [DOI] [PubMed] [Google Scholar]
- E37.Murer T, Imbach LL, Hackius M, et al. Optimizing MSLT specificity in narcolepsy with cataplexy. Sleep. 2017;40 doi: 10.1093/sleep/zsx173. [DOI] [PubMed] [Google Scholar]
- E38.Kritikou I, Vgontzas AN, Rapp MA, Bixler EO. Anti-Ma1- and Anti-Ma2-associated encephalitis manifesting with rapid eye movement sleep disorder and narcolepsy with cataplexy: a case report. Biol Psychiatry. 2018;83:e39–e40. doi: 10.1016/j.biopsych.2016.12.014. [DOI] [PubMed] [Google Scholar]
- E39.Billiard M, Bassetti C, Dauvilliers Y, et al. EFNS guidelines on management of narcolepsy. Eur J Neurol. 2006;13:1035–1048. doi: 10.1111/j.1468-1331.2006.01473.x. [DOI] [PubMed] [Google Scholar]
- E40.US Narcolepsy Multicentre Study. Randomized trial of modafinil for the treatment of pathological somnolence in narcolepsy. US Modafinil in Narcolepsy Multicenter Study Group. Ann Neurol. 1998;43:88–97. doi: 10.1002/ana.410430115. [DOI] [PubMed] [Google Scholar]
- E41.Kollb-Sielecka M, Demolis P, Emmerich J, Markey G, Salmonson T, Haas M. The European Medicines Agency review of pitolisant for treatment of narcolepsy: summary of the scientific assessment by the Committee for Medicinal Products for Human Use. Sleep Med. 2017;33:125–129. doi: 10.1016/j.sleep.2017.01.002. [DOI] [PubMed] [Google Scholar]
- E42.The U.S. Xyrem Multicenter Study Group. A randomized, double-blind, placebo-controlled multicenter trial comparing the effects of three doses of orally administered sodium oxybate with placebo for the treatment of narcolepsy. Sleep. 2002;25:42–49. [PubMed] [Google Scholar]
- E43.Schachter M, Parkes JD. Fluvoxamine and clomipramine in the treatment of cataplexy. J Neurol Neurosurg Psychiatry. 1980;43:171–174. doi: 10.1136/jnnp.43.2.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E44.Smith M, Parkes J, Dahlitz M. Venlafaxine in the treatment of the narcoleptic syndrome. J Sleep Res. 1996;5 [Google Scholar]
- E45.Mayer G, Benes H, Young P, Bitterlich M, Rodenbeck A. Modafinil in the treatment of idiopathic hypersomnia without long sleep time—a randomized, double-blind, placebo-controlled study. J Sleep Res. 2015;24:74–81. doi: 10.1111/jsr.12201. [DOI] [PubMed] [Google Scholar]
- E46.Stubbs B, Vancampfort D, Veronese N, et al. The prevalence and predictors of obstructive sleep apnea in major depressive disorder, bipolar disorder and schizophrenia: a systematic review and meta-analysis. J Affect Disord. 2016;197:259–267. doi: 10.1016/j.jad.2016.02.060. [DOI] [PubMed] [Google Scholar]
- E47.Guichard K, Marti-Soler H, Micoulaud-Franchi JA, et al. The NoSAS score: a new and simple screening tool for obstructive sleep apnea syndrome in depressive disorder. J Affect Disord. 2017;227:136–140. doi: 10.1016/j.jad.2017.10.015. [DOI] [PubMed] [Google Scholar]
- E48.Hermann DM, Bassetti CL. Role of sleep-disordered breathing and sleep-wake disturbances for stroke and stroke recovery. Neurology. 2016;87:1407–1416. doi: 10.1212/WNL.0000000000003037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E49.Sahlin C, Sandberg O, Gustafson Y, et al. Obstructive sleep apnea is a risk factor for death in patients with stroke. Arch Intern Med. 2008;168 doi: 10.1001/archinternmed.2007.70. [DOI] [PubMed] [Google Scholar]
- E50.Gorenek (chair) B, Pelliccia (co-chair) A, Benjamin EJ, et al. European Heart Rhythm Association (EHRA)/European Association of Cardiovascular Prevention and Rehabilitation (EACPR) position paper on how to prevent atrial fibrillation endorsed by the Heart Rhythm Society (HRS) and Asia Pacific Heart Rhythm Society. Eur J Prev Cardiol. 2017;24:4–40. doi: 10.1177/2047487316676037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E51.Chihorek AM, Abou-Khalil B, Malow BA. Obstructive sleep apnea is associated with seizure occurrence in older adults with epilepsy. Neurology. 2007;69:1823–1827. doi: 10.1212/01.wnl.0000279334.78298.d5. [DOI] [PubMed] [Google Scholar]
- E52.Petit D, Pennestri M-H, Paquet J, et al. Childhood sleepwalking and sleep terrors. JAMA Pediatr. 2015;169 doi: 10.1001/jamapediatrics.2015.127. [DOI] [PubMed] [Google Scholar]
- E53.Schenck CH, Boyd JL, Mahowald MW. A parasomnia overlap disorder involving sleepwalking, sleep terrors, and REM sleep behavior disorder in 33 polysomnographically confirmed cases. Sleep. 1997;20:972–981. doi: 10.1093/sleep/20.11.972. [DOI] [PubMed] [Google Scholar]
- E54.Hwang T-J, Ni H-C, Chen H-C, Lin Y-T, Liao S-C. Risk predictors for hypnosedative-related complex sleep behaviors: a retrospective, cross-sectional pilot study. J Clin Psychiatry. 2010;71:1331–1335. doi: 10.4088/JCP.09m05083bro. [DOI] [PubMed] [Google Scholar]
- E55.Hoque R, Chesson AL. Zolpidem-induced sleepwalking, sleep related eating disorder, and sleep-driving: fluorine-18-flourodeoxyglucose positron emission tomography analysis, and a literature review of other unexpected clinical effects of zolpidem. J Clin Sleep Med. 2009;5:471–476. [PMC free article] [PubMed] [Google Scholar]
- E56.Halsband C, Zapf A, Sixel-Döring F, Trenkwalder C, Mollenhauer B. The REM sleep behavior disorder screening questionnaire is not valid in de novo parkinson’s disease. Mov Disord Clin Pract. 2018;5:171–176. doi: 10.1002/mdc3.12591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E57.Iranzo A, Molinuevo JL, Santamaria J, et al. Rapid-eye-movement sleep behaviour disorder as an early marker for a neurodegenerative disorder: a descriptive study. Lancet Neurol. 2006;5:572–577. doi: 10.1016/S1474-4422(06)70476-8. [DOI] [PubMed] [Google Scholar]
- E58.Iranzo A, Santamaría J, Valldeoriola F, et al. Dopamine transporter imaging deficit predicts early transition to synucleinopathy in idiopathic rapid eye movement sleep behavior disorder. Ann Neurol. 2017;82:419–428. doi: 10.1002/ana.25026. [DOI] [PubMed] [Google Scholar]
- E59.Berger K, Luedemann J, Trenkwalder C, John U, Kessler C. Sex and the risk of restless legs syndrome in the general population. Arch Intern Med. 2004;164:196–202. doi: 10.1001/archinte.164.2.196. [DOI] [PubMed] [Google Scholar]
- E60.Happe S, Vennemann M, Evers S, Berger K. Treatment wish of individuals with known and unknown restless legs syndrome in the community. J Neurol. 2008;255:1365–1371. doi: 10.1007/s00415-008-0922-7. [DOI] [PubMed] [Google Scholar]
- E61.Szentkirályi A, Völzke H, Hoffmann W, Trenkwalder C, Berger K. Multimorbidity and the risk of restless legs syndrome in 2 prospective cohort studies. Neurology. 2014;82:2026–2033. doi: 10.1212/WNL.0000000000000470. [DOI] [PubMed] [Google Scholar]
- E62.Trenkwalder C, Allen R, Högl B, Paulus W, Winkelmann J. Restless legs syndrome associated with major diseases: a systematic review and new concept. Neurology. 2016;86:1336–1343. doi: 10.1212/WNL.0000000000002542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E63.Kolla BP, Mansukhani MP, Bostwick JM. The influence of antidepressants on restless legs syndrome and periodic limb movements: a systematic review. Sleep Med Rev. 2018;38:131–140. doi: 10.1016/j.smrv.2017.06.002. [DOI] [PubMed] [Google Scholar]
- E64.Trenkwalder C, Allen R, Högl B, et al. Comorbidities, treatment, and pathophysiology in restless legs syndrome. Lancet Neurol. 2018;17:994–1005. doi: 10.1016/S1474-4422(18)30311-9. [DOI] [PubMed] [Google Scholar]
- E65.Trotti LM, Bhadriraju S, Becker LA. Iron for restless legs syndrome. Cochrane Database Syst Rev. 2012;5 doi: 10.1002/14651858.CD007834.pub2. CD007834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E66.Walters AS, Wagner ML, Hening WA, et al. Successful treatment of the idiopathic restless legs syndrome in a randomized double-blind trial of oxycodone versus placebo. Sleep. 1993;16:327–332. doi: 10.1093/sleep/16.4.327. [DOI] [PubMed] [Google Scholar]