Abstract
Maternal and neonatal mortality are unacceptably high in developing countries. Essential nutrition interventions contribute to reducing this mortality burden, although nutrition is poorly integrated into health systems. Universal health coverage is an essential prerequisite to decreasing mortality indices. However, provision and utilization of nutrition and health services for pregnant women and their newborns are poor and the potential for improvement is limited where health systems are weak. The Community‐Based Maternal and Neonatal Health and Nutrition project was established as a set of demonstration projects in 4 countries in Africa with varied health system contexts where there were barriers to safe maternal health care at individual, community and facility levels. We selected project designs based on the need, context, and policies under consideration. A theory driven approach to programme implementation and evaluation was used involving developing of contextual project logic models that linked inputs to address gaps in quality and uptake of antenatal care; essential nutrition actions in antenatal care, delivery, and postnatal care; delivery with skilled and trained birth attendant; and postnatal care to outcomes related to improvements in maternal health service utilization and reduction in maternal and neonatal morbidity and mortality. Routine monitoring and impact evaluations were included in the design. The objective of this paper is to describe the rationale and methods used in setting up a multi‐country study that aimed at designing the key maternal and neonatal health interventions and identifying indicators related to inputs, outcomes, and impact that were measured to track change associated with our interventions.
Keywords: antenatal care, community‐based, health system strengthening, iron folic acid, nutrition, pregnant women
1. INTRODUCTION
Substantial progress was made towards achieving the Millennium Development Goals 4 and 5, nevertheless of all the goals, Millennium Development Goal 5 that sought a 75% reduction in every country's maternal mortality ratio by 2015 lagged the farthest behind (Gaffey, Das, & Bhutta, 2015). Maternal mortality remains a serious global problem especially in sub‐Saharan Africa. World Health Organization (WHO) estimates over 300,000 women died in 2015 during and following pregnancy and childbirth, the majority from preventable causes. Approximately 99% of these deaths occurred in low‐ or middle‐income countries (LMIC) with sub‐Saharan Africa alone accounting for about 66% (Alkema et al., 2016). Leading causes of maternal death include haemorrhage, hypertensive disorders, prolonged and obstructed labour, sepsis, and unsafe abortions (Say et al., 2014). Neonatal mortality, mainly due to preterm birth, severe infections, and asphyxia (UNICEF et al., 2011; UNICEF et al., 2015), is also excessive in these same regions and is inextricably linked with maternal mortality. A child's risk of dying is highest during the first 28 days of life when about 42% of all under‐five deaths take place, translating to about 2.6 million deaths annually (Wang et al., 2014). Undernutrition contributes significantly to these maternal and child deaths (Black et al., 2013).
The current global framework under the Sustainable Development Goals have set global targets for both maternal and neonatal mortality as well as targets that specifically address achieving universal health coverage, which is an essential prerequisite to change in the mortality indices (UN, 2015; WHO, 2013b). Aligned with this, experts currently propose that the main priority for reducing maternal mortality in developing countries should be to ensure that women have access to skilled birth attendants. The health sector however, faces several challenges and provision as well as utilization of services remains low. Health facilities tend towards curative and essential services, while preventive services—critical for nutrition—may be of lower priority (WHO, 2008). Actions to reduce maternal mortality for example, have focused attention on skilled attendant at birth and access to emergency obstetric care as crucial evidence‐based interventions (Campbell et al., 2006), despite the potential for reducing anaemia and pre‐eclampsia through nutrition interventions (Pena‐Rosas, De‐Regil, Dowswell, & Viteri, 2012; WHO, 2011; WHO, 2012a).
Demand barriers, such as the cost of health services, perceived lack of need for such services in “normal” pregnancy, and the long distances to reach health facilities are important limiting factors to improving health and health service utilization in many settings (Gabrysch & Campbell, 2009). Even if demand barriers can be overcome, access to universal health care coverage is threatened by a variety of factors including human resource constraints at the health facility (Shrimpton et al., 2016). Task shifting, which is a more rational distribution of tasks and responsibilities among health personnel, in these contexts has been proposed as a promising strategy for improving access to and utilization of health care and increasing cost effectiveness within the health system. Where appropriate, tasks are moved to less specialized health care providers including community workers (Lassi & Bhutta, 2015; WHO, 2012b). This approach seems ideal to ensure high coverage of nutrition interventions.
Nutrition International and its partners, developed a set of demonstration projects across four countries in Africa (Ethiopia, Kenya, Niger, and Senegal) with varied health system contexts where there were access, quality, and utilization barriers to safe maternal health care at individual, community, and facility levels. The objective of this paper is to describe the rationale and methods of the multi‐country study. These Community‐Based Maternal and Neonatal Health and Nutrition (CBMNH‐N) projects aimed to improve the quality and uptake of antenatal care (ANC); integrate essential nutrition actions into ANC and birth care; promote delivery with skilled and trained attendants; and promote postnatal care (PNC) in hard to reach populations. Promoted essential nutrition actions included early initiation of breastfeeding and promotion of exclusive breastfeeding, iron folic acid (IFA) supplementation in pregnancy, and delayed umbilical cord clamping at birth. Each project sought to demonstrate the feasibility and potential for impact of a modified care package that could be used for decision‐making and its potential for scale‐up in each country context.
Key messages.
It is possible to design contextually tailored intervention packages to address unique country gaps while incorporating components that had been proven elsewhere to be successful.
A theory driven approach to programme implementation and evaluation can be feasibly developed for different contexts to improve one or more of the functions of the health system.
There is potential of strengthening health systems in low‐ or middle‐income countries using the primary health care to deliver health and nutrition interventions.
Community, stakeholder, and political engagement and participation are invaluable in programme success
2. METHODS
We designed community‐based intervention packages to improve access, coverage, quality, and/or efficiency of maternal and neonatal health services, with emphasis on nutrition interventions, in four countries in Africa building on existing platforms. The methodological approach had four steps (Figure 1):
Figure 1.
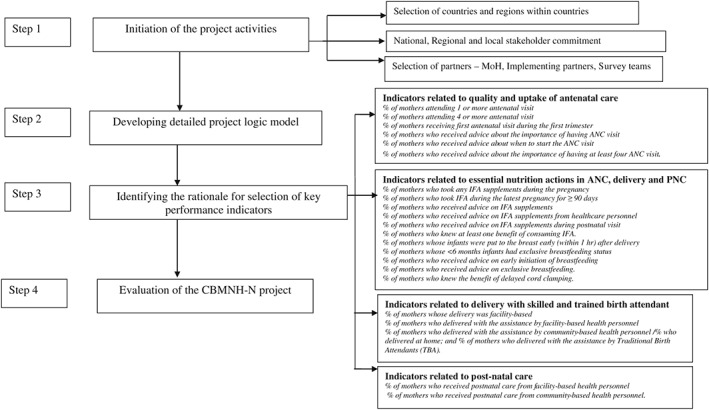
Summary of steps in designing Community‐Based Maternal and Neonatal Health and Nutrition (CBMNH‐N) projects in Ethiopia, Kenya, Niger, and Senegal. MoH = Ministry of Health; ANC = antenatal care; PNC = postnatal care; IFA = iron folic acid
2.1. Step 1: Initiation of the project activities
2.1.1. Selection of countries and regions within countries
The four countries; Ethiopia, Kenya, Niger, and Senegal were selected for the demonstration projects based on the following considerations: countries with high maternal mortality indices; countries where Nutrition International already had a presence and therefore ongoing collaboration with the Ministry of Health (MoH); political will to improve antenatal care and nutrition; countries with a cadre of community‐based personnel (Table 1) who would be the agents to deliver the community‐based intervention packages or equipped for tasks that are traditionally not in their domain. In all four countries, the interventions were at the primary health care level that is identified as the community, health post, health centre, and dispensary (Table 1).
Table 1.
Terminology used for health system and cadres of health workers in the four countries
| Country | Health infrastructure | Community or facility | Health personnel |
|---|---|---|---|
| Ethiopia | |||
| Community site | Community | CHWa/TBAb | |
| Health post | Community | HEWc | |
| Health centre | Facility | Nurse/midwife/health officer | |
| Primary hospital | Facility | Doctor/nurse/midwife/health officer | |
| Hospital | Facility | Doctor/nurse/midwife | |
| Kenya | |||
| Level 1 | Community | CHEWd/CHVe/TBA | |
| Level 2: Dispensary/health centre | Facility | Nurse/midwife/clinical officer | |
| Level 3: County referral hospital | Facility | Doctor/nurse/clinical officer | |
| Level 4: Teaching and referral | Facility | Doctor/nurse/specialists/clinical officer | |
| Niger | |||
| Community site | Community | CHW, matrone f, community relais g | |
| Level 1: Health centres Type 1 | Facility | Nurse, midwife, matrone, CHW | |
| Level 2: Health centres Type 2 | Facility | Doctor/nurse/midwife | |
| Level 3: Health district | Facility | Doctors/nurses/midwife | |
| Level 4: Regional hospitals | Facility | Doctors/nurses/midwife | |
| Level 5: National hospitals and national maternity | Facility | Doctors/nurses/midwife | |
| Senegal | |||
| Health hut | Community | CHW/matrone/relais/bajenou gox h /ASC i | |
| Community site | Community | CHW/relais/bajenou gox | |
| Health post/centre | Facility | Nurse/midwife/matrone/ relais/bajenou gox/ASC | |
| District hospitals | Facility | Doctor/nurse/midwife/ relais/bajenou gox/ASC | |
| Regional hospitals | Facility | Doctor/nurse/midwife | |
| National hospitals | Facility | Doctor/nurse/midwife | |
Note.
Community Health Worker (CHW): World Health Organization defines community health workers as members of the communities where they work, should be selected by the communities, should be answerable to the communities for their activities, should be supported by the health system but not necessarily a part of its organization, and have shorter training than professional workers.
Traditional Birth Attendant (TBA): World Health Organization defines a traditional birth attendant as a person who assists the mother during childbirth and who initially acquired her skills by delivering babies herself or through an apprenticeship to other TBAs.
Ethiopia's Health Extension Worker (HEW) cadre, modelled after the country's successful agricultural extension worker programmes, was launched in 2003 and includes young women with at least a grade 10 education recruited at the kebele and woreda levels to be trained as HEWs. They receive 1 year of didactic and practical training in 16 health care packages including maternal and child health and nutrition. Their primary charge is to promote health, including education, screening, prevention, and selective clinical interventions. HEWs are deployed in pairs, two for every kebele, and affiliated with each kebele's health post, part of the level one primary health care unit. HEWs receive mentoring and supervision from health officers stationed at the local health centre.
Community Health Extension Workers (CHEW): Are facility based personnel whose sole responsibility is to supervise CHWs and ensure appropriate services are delivered at the community level. Additionally, CHEWs are usually in charge of the community's Community Unit (CU). The CU is commonly referred to as the “link facility,” as it links CHV (formerly CHW) to the health system and community members to the formal health centres.
Community Health Volunteer (CHV) is the new terminology for community health workers in Kenya because it is a voluntary position.
A matrone is a community health worker. Involved in delivery of uncomplicated cases and referral of complicated cases to health facility.
Relais is a community health worker—they are volunteers who promote health and nutrition services at the community. Selected by the community, often men age between 18 and 50 years who reside in the community for at least 6 months.
Bajenou gox is a community health worker—they are volunteers who promote health and nutrition services at the community. Selected by the community, often women age between 18 and 50 years who reside in the community for at least 6 months.
Agent de Sante Communautaire (ASC) is a community health worker—Involved in delivery of uncomplicated cases and referral of complicated cases to health facility. Selected by the community, often men or women age between 18 and 50 years who reside in the community for at least 6 months.
The specific region within each country was selected in collaboration with each MoH based on a combination of factors including MoH priority based on documented or perceived need for additional services; and existence of a local partner with capacity to work in that region, including ability to ensure the safety of project implementation and evaluation teams. The four regions presented with different needs and contexts.
First, in Afar region of Ethiopia, the communities are pastoralists with an unsustainable food supply chain and a limited health workforce. The health care providers in this area are not necessarily from or familiar with the local customs of communities or ethnic groups where they serve, creating difficulties for developing trust in and demand for health care. The regional level MoH and the Maternal and Newborn Health in Ethiopia Partnership (MaNHEP) served as primary partners and facilitated access to communities.
Second, in Kakamega County Kenya, despite a national community health strategy, the availability of skilled health care providers and established health facilities, there was low utilization of services at the public health facilities, and high maternal morbidity rates. Amref Health Africa was already established in a nearby county and was given the mandate for the community interventions of the project in Kakamega.
Third, in Zinder region of Niger, local conflict had made it difficult for the MoH to maintain regular health care systems for women to receive the care required during pregnancy apart from established programmes such as through Hellen Keller International (HKI).
Fourth, in the Kolda region of Senegal, there were multiple partner agencies working to improve maternal and neonatal health, but without coordination and harmonized approaches there was continued low care‐seeking among pregnant women.
2.1.2. National, regional, and local stakeholder commitment
To get the commitment of stakeholders to the CBMNH‐N model at national, regional, and local levels, a series of meetings were held at different levels to explain the project objectives in the different countries. Nutrition International coordinated these meetings with the objective of getting stakeholder engagement and ownership through an iterative and collaborative process of project design and implementation.
The process of project leadership and stakeholder involvement growing into aligned stakeholder commitment also involved establishment of project coordination committees or teams that would provide administrative, management, technical, and supportive supervision roles at all levels. In some cases, these teams met at a scheduled regular basis throughout the project life and were vital in providing quality assurance of the implementation process and ensuring that the project plans and implementation approaches were of technically high quality and in line with national technical guidelines. These teams also ensured that all relevant implementing partners' work was well coordinated and they resolved project challenges throughout the project life. We anticipate that these teams will also have the responsibility of synthesizing the impact analysis results at country level and advising the MoH on the adoption for scale up of the components of the CBMNH‐N model.
2.1.3. Selection of partners
In all four countries, the MoH was considered the main implementing partner supported by other partners responsible for specific components. We selected partners already successfully engaged in components of the CBMNH‐N package that was proposed in each country context. The survey teams were composed of competent researchers in various disciplines relevant to maternal health and nutrition with experience in designing and conducting epidemiological studies and a track record for publications. Nutrition International was responsible for coordination and synergy among partners.
2.2. Step 2: Developing detailed project logic model
Embedding theory driven approaches to programme implementation and evaluation is well described in public health literature (Loechl et al., 2009; Rawat et al., 2013). To track how the CBMNH‐N project would achieve impact, it was important to develop an overall logic model (De‐Regil, Pena‐Rosas, Flores‐Ayala, & Del Socorro Jefferds, 2014; Figure 2) and detailed country logic models (Figures 3, 4, 5, 6) that explain the specific country context and how components of the interventions are linked with each other and with the ultimate outcome of reducing maternal and neonatal morbidity and mortality. Approaches described in CBMNH‐N logic models were hypothesized to ultimately reduce maternal and neonatal morbidity and mortality in the four countries. We identified ways to bridge gaps in the provision and utilization of maternal and neonatal health services. Quantitative key performance indicators along with frequency of collection of the indicators were defined to match the different levels of the key components of the logic model and were measured to track progress and change associated with the project interventions. Qualitative approaches included formative assessments that were used to design culturally appropriate behaviour change interventions. Behaviour change communication (BCC) strategies within our CBMNH‐N projects included social mobilization, interpersonal communication, branding, and use of promotional materials, dramas, scripts, and skits. The duration and intensity of the strategies used were not identical across the countries but depended on the type of behaviour being changed, the barriers and enablers identified through formative research and the social and cultural context. The formative research will be reported elsewhere.
Figure 2.
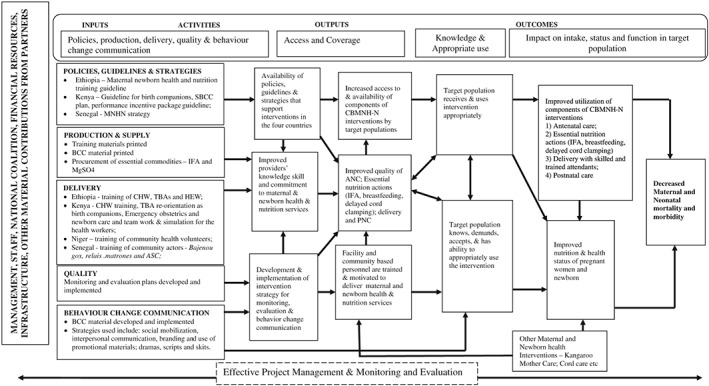
Overall Community‐Based Maternal and Neonatal Health and Nutrition (CBMNH‐N) programme theory using CDC/WHO generic logic model. CDC = Centers for Disease Control and Prevention; WHO = World Health Organization; SBCC = Social and Behavior Change Communication; MNHN = Maternal Neonatal Health and Nutrition; BCC = behaviour change communication; IFA = iron folic acid; CHW = community health workers; TBA = Traditional Birth Attendant; HEW = Health Extension Worker; ASC = Agent de Sante Communautaire; ANC = antenatal care; PNC = postnatal care
Figure 3.
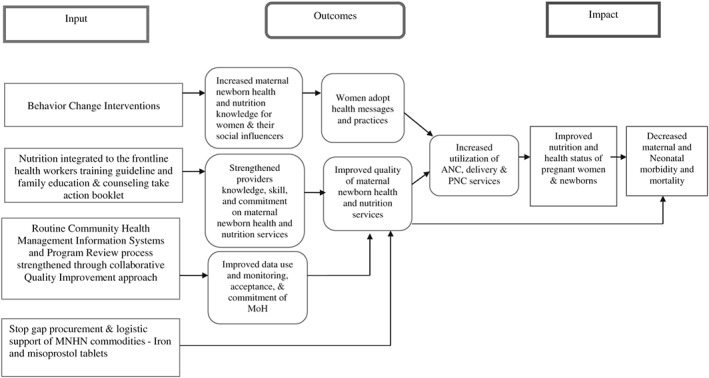
Ethiopia: Reducing maternal and neonatal morbidity and mortality through supporting Ethiopia's health extension programme to increase access to quality maternal, neonatal, and nutrition services. MNHN = Maternal Newborn Health and Nutrition; MoH = Ministry of Health; ANC = antenatal care; PNC = postnatal care
Figure 4.
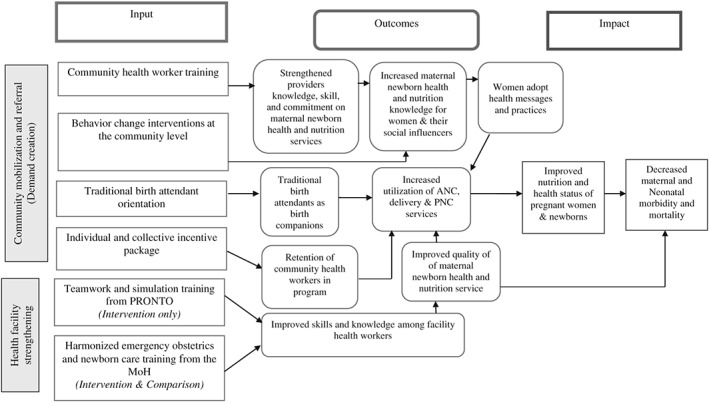
Kenya: Reduce maternal and neonatal morbidity and mortality in Kenya through improving care and nutrition for women at risk during pregnancy through a novel community–facility linkage programme. PRONTO = Programa de Rescate Obstétrico y Neonatal: Tratamiento Óptimo y Oportuno; MoH = Ministry of Health; ANC = antenatal care; PNC = postnatal care
Figure 5.
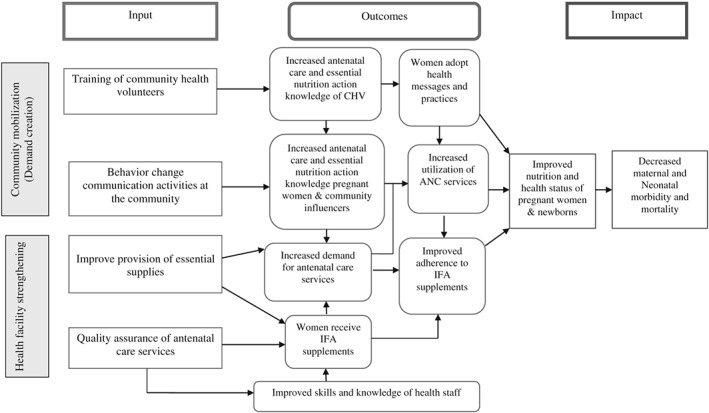
Niger: Reducing maternal and neonatal morbidity through health facility strengthening and community mobilization. CHV = Community Health Volunteer; IFA = iron folic acid; ANC = antenatal care
Figure 6.
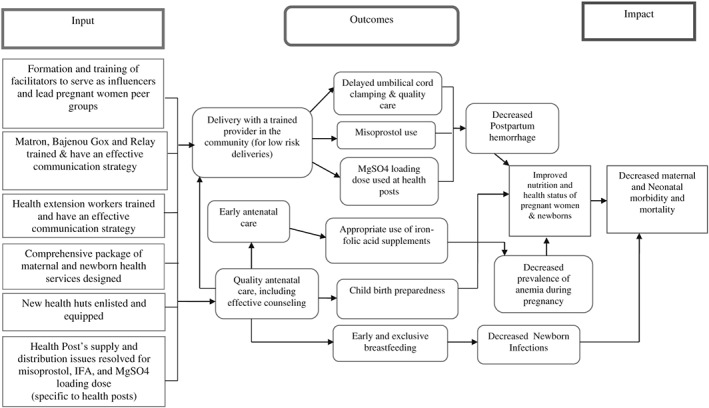
Senegal: Reducing maternal and neonatal morbidity and mortality through the development and piloting of a comprehensive maternal and newborn community health policy for Senegal. IFA = iron folic acid
2.3. Step 3: Identifying the rationale for selection of key performance indicators
A key characteristic of the CBMNH‐N project was a rigorous monitoring and evaluation system as part of the design of the project. In order to measure improvements in inputs and outcomes along the implementation pathway as outlined in the project logic models, we highlight in this section what we identified as the rationale for selection of key performance indicators based on an evidence informed programme model using proven interventions (Bhutta et al., 2013). Uptake of the interventions is described as utilization of one or more components of the CBMNH‐N package and was assessed by measuring changes in key performance indicators.
2.3.1. Quality and uptake of antenatal care
It is well known that ANC is more beneficial in preventing adverse pregnancy outcomes when received early in the pregnancy and continued through delivery (Klemm et al., 2011). WHO recommends that a woman without complications should have at least four ANC visits, the first of which should take place during the first trimester (Lincetto, Mothebesoane‐Anoh, Gomez, & Munjanja, 2013). Quality and uptake of ANC were key components in each of the projects and we developed indicators to capture the status of these components. These include percentage of mothers attending one or more antenatal visit; percentage of mothers attending four or more antenatal visit; percentage of mothers receiving first antenatal visit during the first trimester; percentage of mothers who received advice about the importance of having ANC visit; percentage of mothers who received advice about when to start the ANC visit; and percentage of mothers who received advice about the importance of having at least four ANC visits.
2.3.2. Essential nutrition actions in ANC, delivery, and PNC—IFA supplementation; initiation of breastfeeding and exclusive breastfeeding; delayed umbilical cord clamping
IFA supplementation
Daily oral IFA supplementation is recommended as part of the ANC to reduce the risk of iron deficiency, maternal anaemia, and low birthweight. Pregnant women are advised to take IFA supplements during pregnancy for at least 90 days to prevent anaemia and other complications (WHO, 2012a). Through formative assessments in each of the four countries, we identified barriers to IFA supplementation and developed country‐specific BCC material that was used by the relevant implementing partner in each country to educate women at both health facility and informal and formal community encounters. We also ensured there was adequate IFA supplements after facility supply chain assessments identified shortages by including stop gap procurement as part of our package to ensure no stock outs during the project life. Indicators measured include percentage of mothers who took any IFA supplements during the pregnancy; percentage of mothers who took IFA supplement during the latest pregnancy for ≥ 90 days; percentage of mothers who received advice on IFA supplements; percentage of mothers who received advice on IFA supplements from health care personnel; percentage of mothers who received advice on IFA supplements during postnatal visit; and percentage of mothers who knew at least one benefit of consuming IFA supplement.
Breastfeeding
It is recommended that children be put to the breast within an hour of birth and should be exclusively breastfed for the first 6 months of life to achieve optimal growth, development, and health (WHO, 2014). Through formative research, we identified key influencers of the mother in each country context, who we then involved in BCC relating to protecting, promoting, and supporting breastfeeding. Indicators measured included percentage of mothers whose infants were put to the breast early (within 1 hr) after delivery; percentage of mothers whose < 6 months infants had exclusive breastfeeding status; percentage of mothers who received advice on early initiation of breastfeeding; and percentage of mothers who received advice on exclusive breastfeeding.
Delayed cord clamping
WHO recommends that delayed umbilical cord clamping (not earlier than 1 min after birth) should be performed during the provision of essential neonatal care for improved maternal and infant health and nutrition outcomes (WHO, 2014). Delayed umbilical cord clamping was incorporated into the training curriculum of health workers in Ethiopia, Kenya, and Senegal. The indicator we measured was the percentage of mothers who knew the benefit of delayed cord clamping.
2.3.3. Delivery with skilled and trained birth attendant
Proper medical attention and hygienic conditions during delivery can reduce the risk of complications and infection that can cause morbidity and mortality to either the mother or the baby. Increasing the number of deliveries in the health facilities is an important factor in reducing health risks to both the mother and the child; the specific mechanism to reduce risks of delivery was adapted to the policy of each country. In Kenya, where the policy advocates for facility based deliveries, one major component of the CBMNH‐N project was redefining the roles of Traditional Birth Attendants (TBAs) to birth companions. TBAs who originally delivered women at home were motivated through the CBMNH‐N interventions to accompany women to the health facility for delivery. In Afar region of Ethiopia, where the health system context allowed, the project equipped heath care providers at the health posts by training them as birth attendants to deliver women at the health post. Bridging the personnel gaps in health facilities is in line with the WHO guidance on optimizing health workers roles through task shifting (WHO, 2012b). In Senegal, community health workers (CHWs) were trained to conduct delivery for low risk deliveries; while in Niger, no specific intervention was specified. Indicators measured included percentage of mothers whose delivery was facility‐based; percentage of mothers who delivered with the assistance by facility‐based health personnel; percentage of mothers who delivered with the assistance by community‐based health personnel/who delivered at home; and percentage of mothers who delivered with the assistance by TBAs.
2.3.4. PNC
Appropriate care during the postnatal period is an important determinant of the well‐being of mothers and their newborns. WHO has provided recommendations on timing of discharge from a health facility after birth, number and timing of postnatal contacts, home visits for PNC, and content of PNC for newborn (assessment of the baby, exclusive breastfeeding, and cord care; WHO, 2013a). Indicators measured included percentage of mothers who received PNC from facility‐based health personnel; and percentage of mothers who received PNC from community‐based health personnel.
2.4. Step 4: Evaluation of the CBMNH‐N project
Strengthening the evidence base on how to effectively deliver maternal and neonatal health and nutrition interventions requires programmes or complex public health interventions that are well designed, implemented, and evaluated. The CBMNH‐N project engaged rigorous plausibility evaluation designs (Habicht, Victora, & Vaughan, 1999). All countries implemented quasi‐experimental pre–post non‐randomized intervention studies with comparison groups. It was not logistically feasible to conduct randomized controlled trials; nonetheless, these less robust yet rigorous designs were implemented to maximize our ability to evaluate the impact of the various components of the CBMNH‐N project on knowledge and practices related to maternal and neonatal care and to inform scale‐up (Kung'u et al., 2018). Routine monitoring and evaluations were implemented in each country with the intent of estimating the overall public health impact of the project and facilitating the compilation of evidence and lessons learnt for potential of similar programmes in other regions of the country or other countries.
3. RESULTS
This CBMNH‐N multi‐country project logic models focus on pregnant women and their newborns. Each country's logic model uniquely addresses the gaps identified, though there are a few cross cutting themes that touch all four countries as described in Figure 2, the overall programme theory. Each county's package of interventions is unique and therefore could not be described in detail here; however, we provide a brief explanation of each country's project and logic model as a key result of the setting up of the CBMNH‐N project.
3.1. Ethiopia
Nutrition International's objective in Ethiopia was to improve the coverage and quality of care for women and newborns by improving ANC, delivery, and PNC through a strong focus on training community‐level providers and quality improvement (QI). The project also focused on strengthening essential nutrition actions in ANC, delivery, and PNC. The project targeted 13,000 pregnant women and newborns, and over 700 health providers in the pastoralist region of Afar, Ethiopia.
3.1.1. Partners
Nutrition International partnered with Emory University, MaNHEP for implementation, the Federal and Regional MoH for Policy and Advocacy, and the University of Addis Ababa and Jimma University for the baseline and end line surveys, respectively. The MaNHEP model was developed specifically for Ethiopia and had been successfully implemented in rural Amhara and Oromiya regions of Ethiopia. This model integrates specific maternal and neonatal nutrition actions into their basic package of essential services through a three pronged intervention approach: (a) community‐ and facility‐based maternal and newborn health training, (b) continuous QI, and (c) BCC for demand creation.
3.1.2. Key project interventions
The CBMNH‐N project in Ethiopia trained TBAs to identify pregnant women, provide home visits to these women, give group family counselling, refer women to facilities for the ANC package, and make referrals to facilities in the cases where complications arose prior to or during delivery. Community leaders, elders, and religious leaders formed QI teams to monitor the work of the TBAs and health extension workers providing ANC, delivery, and PNC. TBAs and QI teams worked together to develop “change ideas” utilized to improve uptake and quality of ANC, delivery, and PNC services in their communities. Facility‐based health providers were trained in emergency obstetrics and newborn care and participated in facility‐QI teams in order to monitor the quality of services provided. Furthermore, regularly facilitated community learning sessions were held to review coverage data, evaluate change ideas, and plan activities.
Health care providers were encouraged to use misoprostol to prevent maternal mortality due to post‐partum haemorrhage and were taught about detecting danger signs during pregnancy. TBAs and health extension workers provided pregnant women with IFA supplements during ANC at the health posts. Health workers were trained on birth planning and taught this to pregnant women. These women were also educated on the importance of early initiation of breastfeeding and exclusive breastfeeding for infants 0–6 months of age. Pregnant women were also provided with nutrition counselling through various providers throughout pregnancy (Figure 3).
3.2. Kenya
The objective of the CBMNH‐N project in Kenya was to improve maternal health outcomes by building community–facility linkages that focused on increasing the demand for ANC, delivery, and PNC services by pregnant women as well as improving the skills of health workers in team work and emergency obstetrics via the PRONTO (Programa de Rescate Obstétrico y Neonatal: Tratamiento Óptimo y Oportuno) model. The project also focused on strengthening essential nutrition actions in ANC, delivery, and PNC. CBMNH‐N targeted 58,000 pregnant women and newborns, and 3,750 health care workers in Kenya's Kakamega County.
3.2.1. Partners
Nutrition International partnered with Amref Health Africa as implementing partner at the community level, PRONTO as implementing partner at the facility level, the MoH for policy and advocacy, and University of Nairobi and Kenyatta University for the baseline and end line surveys respectively. Amref Health Africa's mission is to improve the health of people in Africa by partnering with and empowering communities, and strengthening health systems. Amref was responsible for creating demand for maternal and newborn health services through community mobilization and referral in Kenya. They established and strengthened community units; implemented behaviour change interventions; and redefined the roles of TBAs to birth companions among other interventions at the community. PRONTO aims to optimize care during birth by providing a novel approach to emergency obstetrics and perinatal training for health and non‐health workers present at the health facility to foster teamwork and ensure they respond more effectively (within their institutional limitations) to emergencies involving women and newborns. PRONTO uses a high fidelity, low‐tech in‐situ simulation based team training programme that was developed by University of Washington and other collaborators (http://prontointernational.org) and has been used elsewhere and shown to have impact (Walker et al., 2014; Walker et al., 2015). Building on their existing relationship with the University of Nairobi, where they were setting up a regional training hub, PRONTO was made responsible for training facility based personnel in teamwork and simulation training using the PRONTO model in Kenya. The PRONTO intervention and its impact on participant teamwork skills, obstetric, and neonatal knowledge and self‐efficacy is described in another manuscript that will be printed in this supplement (Dettinger et al., 2018).
3.2.2. Key project interventions
Project interventions included having CHWs promote ANC, delivery, and PNC services through home visits, community dialogue days, and peer support groups. In tandem, health facility providers received training on the government's recently developed but not scaled up harmonized emergency neonatal and obstetric care curriculum; and were engaged in simulation and team‐based training for additional emergency neonatal and obstetric care skills. TBAs were trained and transitioned to new roles as Birth Companions and received a fixed rate transport reimbursement equivalent to $2.5 for every pregnant woman directed to deliver at a health facility. In conjunction with MoH, we developed a guideline for reorienting TBAs as birth companions that describes the reorientation process, implementation of new roles, and recognition of TBAs. A manuscript describing the community perceptions towards the new role of TBAs as Birth Companions and Nutrition Advocates in Kakamega County, Kenya will be printed in this journal supplement (Anono et al., 2018). The programme utilized WHO's “Near Miss” form to monitor quality of delivery services. The Near Miss form was completed for every pregnant woman who visited the health facility for delivery or those up to 48 hours post‐partum who were admitted to the facility or referred immediately. Embedded within the health facility strengthening component was a monitoring system that ensured effective stock management of essential maternal and newborn health and nutrition commodities.
Community‐based and facility‐based health care personnel were trained on maternal and newborn health solutions. These solutions included the promotion of and referral to ANC, including both IFA supplements and PNC. Personnel learned to detect danger signs during pregnancy and when to refer pregnant women to health facility for delivery. The promotion of delayed umbilical cord clamping was also taught to health care providers as one of the essential nutrition actions. Pregnant women received nutrition counselling throughout pregnancy and were trained on the importance of immediate and exclusive breastfeeding for 6 months and encouraged to practice these essential nutrition actions. They also utilized the services of TBAs as birth companions to the health facility for delivery (Figure 4).
During the initiation of the project activities, national, regional, and local stakeholder meetings resulted in tweaking of the approach; the partners had developed the CBMNH‐N approach with the assumption that all facility health workers had minimum training in emergency obstetrics. Through these initiation consultations, we found that the training and capabilities of public facility health workers were varied and MoH strongly suggested that we retrain them on a harmonized emergency obstetrics curriculum as a component of the CBMNH‐N package in the project area.
3.3. Niger
Unlike the other three countries, which had targets of programme delivery in addition to evidence generation, the project in Niger was an in‐depth study to inform how to strengthen uptake, quality of care and access to ANC in rural Niger. The project targeted over 900 pregnant women in the Zinder region of Niger.
3.3.1. Partners
Nutrition International's partners in conducting this research project included HKI for the implementation, University of California Davis for the evaluation, and the MoH for policy and advocacy. The project in Niger focused on assessment of the Nutritional Status of Pregnant Women in Zinder, Niger and optimization of prenatal care services, as such, it had an elaborate research component, hence the choice of University of California Davis who had extensive research experience in West Africa. HKI, the implementing partner, started its programmes in 1987, and assists the government's efforts in prevention and treatment of malnutrition, strengthening health services, and community networks for promoting essential nutrition actions among other programmes.
3.3.2. Key project interventions
The project included a baseline survey to assess the stage of pregnancy and the nutritional status (weight, height, presence of anaemia, and biomarkers for iron and vitamin A status) of pregnant women. A qualitative assessment was also conducted on beliefs, barriers, and enabling factors for ANC and pregnancy outcomes. We also evaluated the quality of PNC services at the health centre. Based on the qualitative research, we developed an optimization strategy to improve ANC uptake and quality in the project districts. The strategy included ensuring a full supply of materials and essential commodities for ANC at health facilities; training health facility providers on improved counselling skills; and training community volunteers on dissemination of the BCC messages for improved uptake of ANC to pregnant women, their families, and community influencers. A rigorous evaluation of the strategy was undertaken, which involved an assessment of the nutritional status of pregnant women using anthropometric measures. Other components of the model included nutrition counselling and gestational weight monitoring and malaria prevention for pregnant women (Figure 5). A manuscript detailing the CBMNH‐N project in Niger has been submitted for publication in this supplement. (Begum et al., 2018).
3.4. Senegal
The objective of the CBMNH‐N project in Senegal was to increase the uptake and improve the quality of maternal and newborn health services through the development and implementation of a comprehensive maternal and newborn health policy for Senegal. These interventions targeted 46,000 pregnant women and newborns, and 650 community‐based and facility‐based health personnel in Kolda, Senegal.
3.4.1. Partners
Nutrition International partnered with Santé Plus for the situation assessment, Child Fund for implementation of the CBMNH‐N model, the MoH for policy and advocacy, and the Institut de Santé & Développement for the baseline and end line surveys. Child fund was already at work in Kolda region. Their activities included carrying out community sensitization workshops and strengthening the community based health platform by training of community health volunteers and developing BCC and community‐based health information systems.
3.4.2. Key project interventions
CBMNH‐N project in Senegal was implemented through a three step process: Step 1 involved validation of the CBMNH‐N concept note through a series of iterative workshops to agree on key relevant interventions for the country and to approve the CBMNH‐N proposed strategy; Step 2 involved conducting a national situation assessment. The situation assessment served as a baseline contextual analysis and included formative research to understand the maternal and newborn health situation from both the beneficiaries' and the stakeholders' perspectives. The findings from the situation assessment were analysed and incorporated into the development of the maternal and newborn health and nutrition package of interventions, and were brought into alignment with the National Maternal Health Policy; Step 3 involved the developing of a national operational plan and detailed implementation plan for Kolda region. National workshops were conducted to validate the plan; a regional workshop in Kolda to finalize and validate the essential package of services to be implemented; and a community sensitization workshop before onset of implementation.
The package of interventions was then defined as the CBMNH‐N model (Figure 6). The components of the model included training CHWs, TBAs, nurses, and midwives on essential nutrition actions. Peer support groups were also created to promote ANC, delivery, and PNC services. The model also included improving the referral system from health huts to higher‐level health facilities for complications detected during pregnancy and delivery. Additionally, the model ensured that all health huts and health posts in the project area had adequate equipment and supplies of essential commodities (Figure 6).
Various cadres of health workers were trained on specific topics, which included the promotion of ANC, IFA consumption, birth assistance, and PNC. Health care workers were encouraged to use misoprostol to prevent maternal mortality due to post‐partum haemorrhage. Health workers and pregnant women were taught about the benefits of delaying their first pregnancy and birth spacing. Pregnant women were also educated on the importance of initiation of breastfeeding and exclusive breastfeeding as critical essential nutrition actions. The project also included nutrition counselling and monitoring of gestational weight gain.
4. DISCUSSION
Provision of services (supply) and utilization of services (demand) are important pillars in the attainment of the overall goal of reducing maternal and neonatal morbidity and mortality. To achieve this goal, various models are used by programmers and researchers to better understand the causes and associated contextual factors of maternal and neonatal health and nutrition. Recommended models are generally composed of addressing barriers in demand for services and deciding to seek care, barriers in accessing the health facility and barriers in encounter with a skilled service provider, and barriers in receiving quality care once at the health facility (Thaddeus & Maine, 1994). Use of community based personnel and outreach services are important components for such models because they mitigate some of these barriers. We did not systematically implement any specific model, rather we worked through available health systems in the four countries and identified gaps and barriers to address through improved programme designs based on a theory driven approach. Therefore, one strength of the CBMNH‐N project was that each intervention package was tailored to the uniquely identified gaps in each country while incorporating components that had been proven elsewhere to be successful.
Another strength of the CBMNH‐N projects was the focus on the primary health care approach that emphasizes promotion of preventive services. Various levels of the health system are skewed towards curative rather than preventive services. Health and nutrition interventions that focus on prevention have for the most part been on the sidelines, yet they are critical for the same outcomes that curative services seek to manage and treat. The potential of strengthening health systems in LMIC using primary health care to deliver health and nutrition interventions is well documented (WHO, 2008; WHO, 2013b). We anticipate that to some extent with CBMNH‐N, we have addressed the core principles of primary health care: universal coverage; people centred services; health public polices; and leadership (WHO, 2008).
Another critical component of all our CBMNH‐N country projects was the focus on strengthening essential nutrition actions in ANC, delivery, and PNC. Overall, assessing effective functioning of essential nutrition actions within ANC, delivery, and PNC has been infrequent with focus mainly being on IFA supplementation programmes within ANC (Klemm et al., 2011; Stoltzfus, 2011). Indeed, to be successful, IFA supplementation programmes need to be well integrated into the programmatic agendas for reducing morbidity and mortality of pregnant women and neonates (Stoltzfus, 2011). Policy options informed by scientific evidence and accompanied with best practices can help countries make appropriate choices for their contexts and increase likelihood of achieving these essential nutrition actions. Because LMIC have limited resources to address their health and nutrition challenges, evidence‐informed decisions will assist in prioritizing the use of those resources efficiently in actions proven to be effective in other contexts, yet adapting to their specific needs with project such as this CBMNH‐N.
CBMNH‐N projects were set up to generate evidence relevant to designing and implementing contextually tailored maternal and neonatal health packages integrating nutrition into health programmes at the community level in different countries. The impact of the projects has been demonstrated and will be reported in this supplement (Kung'u et al., 2018). Efforts to replicate and scale up components of the projects in similar contexts based on the demonstrated impact evidence of the interventions are currently underway. That notwithstanding, invaluable other lessons were learned in setting up the projects that set them up for success and have implications for others setting up health and nutrition programmes. These factors are fundamental building blocks that underpin, enable, and drive change in nutrition programmes and can proactively be made to happen in other settings (Gillespie & van den Bold, 2017). These included building commitment, coherence, accountability, capacity, and leadership by community sensitization and engagement of community leaders as part of stakeholder dialogue; stakeholders' participation and agreement on common results' framework; and early dialogue and engagement of political and community leadership.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
JKK, BN, RP, LN, JM, HHD, MD, and MD participated in the conception and design of the study. The first draft of the work was by JKK. All authors revised the manuscript critically for important intellectual content. All authors reviewed the manuscript and approved the final version to be published. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved by all authors.
ACKNOWLEDGEMENTS
The authors thank the MoH in Kenya, Ethiopia, Senegal, and Niger for consenting to have the demonstration projects in their countries and all partners involved in the intervention delivery. We thank Ali MacLean for her contribution in setting up CBMNH‐N projects in the four countries; Henock Gezahegn and Chris Wanyoike—country directors in Ethiopia and Kenya respectively who held initial discussions with MoH and partners in each country. Funding for this research was provided by the Nutrition International (formerly Micronutrient Initiative).
Kung'u JK, Ndiaye B, Ndedda C, et al. Design and implementation of a health systems strengthening approach to improve health and nutrition of pregnant women and newborns in Ethiopia, Kenya, Niger, and Senegal. Matern Child Nutr. 2018;14(S1):e12533 10.1111/mcn.12533
REFERENCES
- Alkema, L. , Chou, D. , Hogan, D. , Zhang, S. , Moller, A. B. , Gemmill, A. , … Technical Advisory, G (2016). Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario‐based projections to 2030: A systematic analysis by the UN Maternal Mortality Estimation Inter‐Agency Group. Lancet, 387, 462–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anono, E. L. , Ochola, S. , Wawire, S. , Ogada, I. , Ndedda, C. , & Kung'u, J. K. (2018). Community perceptions towards the new role of traditional birth attendants as birth companions and nutrition advocates in Kakamega County, Kenya. Maternal & Child Nutrition, 14(Suppl 1): e12578 10.1111/mcn.12578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begum, K. , Ouédraogo, C. T. , Wessells, K. R. , Young, R. R. , Faye, M. T. , Wuehler, S. E. , & Hess, S. Y. (2018). Prevalence of and factors associated with antenatal care seeking and adherence to recommended iron-folic acid supplementation among pregnant women in Zinder, Niger. Maternal & Child Nutrition, 14(Suppl 1): e12466 10.1111/mcn.12466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhutta, Z. A. , Das, J. K. , Rizvi, A. , Gaffey, M. F. , Walker, N. , Horton, S. , … Maternal & Child Nutrition Study, G . (2013). Evidence‐based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet, 382, 452–477. [DOI] [PubMed] [Google Scholar]
- Black, R. E. , Victora, C. G. , Walker, S. P. , Bhutta, Z. A. , Christian, P. , De Onis, M. , … Maternal & Child Nutrition Study, G . (2013). Maternal and child undernutrition and overweight in low‐income and middle‐income countries. Lancet, 382, 427–451. [DOI] [PubMed] [Google Scholar]
- Campbell, O. M. , Graham, W. J. , & Lancet Maternal Survival Series Steering, G (2006). Strategies for reducing maternal mortality: Getting on with what works. Lancet, 368, 1284–1299. [DOI] [PubMed] [Google Scholar]
- De‐Regil, L. M. , Pena‐Rosas, J. P. , Flores‐Ayala, R. , & Del Socorro Jefferds, M. E. (2014). Development and use of the generic WHO/CDC logic model for vitamin and mineral interventions in public health programmes. Public Health Nutrition, 17, 634–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dettinger, J. C. , Kamau, S. , Calkins, K. , Cohen, S. R. , Cranmer, J. , Kibore, M. , … Walker, D. (2018). Quality improvement: Measuring movement towards improved emergency obstetric care in rural Kenya with implementation of the PRONTO simulation and team training program. Maternal & Child Nutrition, 14(Suppl 1): e12465 10.1111/mcn.12465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabrysch, S. , & Campbell, O. M. (2009). Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy and Childbirth, 9, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaffey, M. F. , Das, J. K. , & Bhutta, Z. A. (2015). Millennium development goals 4 and 5: Past and future progress. Seminars in Fetal & Neonatal Medicine, 20, 285–292. [DOI] [PubMed] [Google Scholar]
- Gillespie, S. , & van den Bold, M. (2017). Stories of change in nutrition: An overview. Global Food Security, 13, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habicht, J. P. , Victora, C. G. , & Vaughan, J. P. (1999). Evaluation designs for adequacy, plausibility and probability of public health programme performance and impact. International Journal of Epidemiology, 28, 10–18. [DOI] [PubMed] [Google Scholar]
- Klemm, R. , Sommerfelt, A. , Boyo, A. , Barba, C. , Kotecha, P. , Steffen, M. & Franklin, N. (2011). Are we making progress on reducing anemia in women? Cross‐country comparison of anemia prevalence, reach, and use of antenatal care and anemia reduction interventions. A2Z: The USAID Micronutrient and Child Blindness Project. AED.
- Kung'u, J. K. , Pendame, R. , Ndiaye, M. B. , Gerbaba, M. , Ochola, S. , Faye, A. , … De‐Regil, L. M. (2018). Integrating nutrition into health systems at community level: Impact evaluation of the community‐based maternal and neonatal health and nutrition projects in Ethiopia, Kenya, and Senegal. Maternal & Child Nutrition, 14(Suppl 1): e12577 10.1111/mcn.12577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassi, Z. S. , & Bhutta, Z. A. (2015). Community‐based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database of Systematic Reviews. CD007754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lincetto, O. , Mothebesoane‐Anoh, S. , Gomez, P. & Munjanja, S. (2013). Antenatal Care.
- Loechl, C. U. , Menon, P. , Arimond, M. , Ruel, M. T. , Pelto, G. , Habicht, J. P. , & Michaud, L. (2009). Using programme theory to assess the feasibility of delivering micronutrient Sprinkles through a food‐assisted maternal and child health and nutrition programme in rural Haiti. Maternal & Child Nutrition, 5, 33–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pena‐Rosas, J. P. , De‐Regil, L. M. , Dowswell, T. , & Viteri, F. E. (2012). Daily oral iron supplementation during pregnancy. Cochrane Database of Systematic Reviews, 12. CD004736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawat, R. , Nguyen, P. H. , Ali, D. , Saha, K. , Alayon, S. , Kim, S. S. , … Menon, P. (2013). Learning how programs achieve their impact: Embedding theory‐driven process evaluation and other program learning mechanisms in alive & thrive. Food and Nutrition Bulletin, 34, S212–S225. [DOI] [PubMed] [Google Scholar]
- Say, L. , Chou, D. , Gemmill, A. , Tuncalp, O. , Moller, A. B. , Daniels, J. , … Alkema, L. (2014). Global causes of maternal death: AWHO systematic analysis. The Lancet Global Health, 2, e323–e333. [DOI] [PubMed] [Google Scholar]
- Shrimpton, R. , Du Plessis, L. M. , Delisle, H. , Blaney, S. , Atwood, S. J. , Sanders, D. , … Hughes, R. (2016). Public health nutrition capacity: assuring the quality of workforce preparation for scaling up nutrition programmes. Public Health Nutrition, 19, 2090–2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoltzfus, R. J. (2011). Iron interventions for women and children in low‐income countries. The Journal of Nutrition, 141, 756S–762S. [DOI] [PubMed] [Google Scholar]
- Thaddeus, S. , & Maine, D. (1994). Too far to walk: Maternal mortality in context. Social Science & Medicine, 38, 1091–1110. [DOI] [PubMed] [Google Scholar]
- UN (2015). Sustainable development goals. United Nations.
- UNICEF , WHO , BANK, T. W . & DIVISION, U. N. D. P . (2011). Levels and trends in child mortality. Report 2011 Estimates Developed by the UN Inter‐agency Group for Child Mortality Estimation. UNICEF Headquarters.
- UNICEF , WHO , BANK, T. W . & DIVISION, U. N. D. P . (2015). Levels and trends in child mortality. Report 2015 Estimates Developed by the UN Inter‐agency Group for Child Mortality Estimation.
- Walker, D. , Cohen, S. , Fritz, J. , Olvera, M. , Lamadrid‐Figueroa, H. , Cowan, J. G. , … Fahey, J. O. (2014). Team training in obstetric and neonatal emergencies using highly realistic simulation in Mexico: Impact on process indicators. BMC Pregnancy and Childbirth, 14, 367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker, D. M. , Holme, F. , Zelek, S. T. , Olvera‐Garcia, M. , Montoya‐Rodriguez, A. , Fritz, J. , … Kestler, E. (2015). A process evaluation of PRONTO simulation training for obstetric and neonatal emergency response teams in Guatemala. BMC Medical Education, 15, 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, H. , Liddell, C. A. , Coates, M. M. , Mooney, M. D. , Levitz, C. E. , Schumacher, A. E. , & Al, E. (2014). Global, regional, and national levels of neonatal, infant, and under‐5 mortality during 1990‐2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet, 384, 957–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . (2008). The World Health Report 2008. Primary Health Care – Now More Than Ever.
- WHO . (2011). WHO recommendations for prevention and treatment of pre‐eclampsia and eclampsia. Geneva. [PubMed]
- WHO . (2012a). Guideline: Daily iron and folic acid supplementation in pregnant women. Geneva. [PubMed]
- WHO . (2012b). WHO recommendations: Optimizing health worker roles to improve access to key maternal and newborn health interventions through task shifting. Geneva. [PubMed]
- WHO . (2013a). WHO recommendations on postnatal care of the mother and newborn. Geneva. [PubMed] [Google Scholar]
- WHO . (2013b). The World Health Report 2013. Research for Universal Health Coverage. World Health Organization.
- WHO . (2014). Guideline: Delayed umbilical cord clamping for improved maternal and infant health and nutrition outcomes. Geneva. [PubMed]


