Abstract
The World Health Organization recommends iron and folic acid (IFA) supplementation for pregnant women. The high prevalence of anaemia among pregnant women in Niger warrants better understanding of the utilization of antenatal care (ANC) and IFA. We aimed to assess the prevalence of and factors associated with ANC coverage and adherence to IFA recommendation among pregnant women. Pregnant women (n = 923) from 64 randomly selected villages within the catchment area of 12 health centres were interviewed during a baseline household survey in Zinder, Niger. ANC and IFA coverage were 60.1% and 43.6%, respectively. Only 71.7% of women who attended ANC received IFA. Of the 401 women who reportedly received any IFA supplements, 99.3% had attended any ANC during their current pregnancy and 68.6% reported adherence to recommended IFA supplementation (i.e., consumed IFA every day in the previous week). Women with gestational age ≥27 weeks were more likely to have attended ANC than women with gestational age <27 weeks (85.9% vs. 27.5%, odds ratio [OR]: 21.81, 95% confidence interval [CI]: 13.81, 34.45). Women who reportedly received husbands' advice about attending ANC were more likely to attend ANC (OR: 1.48, 95% CI [1.03, 2.11]) and adhere to IFA recommendations (OR: 1.80, 95% CI [1.04, 3.13]) compared to those who did not receive any advice. ANC attendance is crucial to ensure distribution of IFA supplementation among pregnant women in Zinder. Interventions to improve ANC and IFA adherence will require promotion of early ANC, ensure availability of IFA at ANC, and involve husbands in ANC.
Keywords: adherence, ANC, antenatal care, factors, IFA, iron folic acid, supplementation
1. INTRODUCTION
Antenatal care (ANC) improves maternal and perinatal health, contributes to newborn survival, promotes institutional birth (Carroli, Villar, et al., 2001; Fernandez Turienzo, Sandall, & Peacock, 2016; WHO & UNICEF, 2003), and reduces maternal mortality (Berhan & Berhan, 2014). The World Health Organization (WHO) until recently recommended “focused ANC” consisting of at least four visits for normal pregnancies with the first visit occurring before 12 weeks of pregnancy (WHO, 2002). Focused ANC provides an opportunity for early detection and management of any pregnancy‐related complications or pre‐existing diseases, distribution of preventive interventions and provision of treatment, and timely advice and counselling (WHO, 2002). Despite significant improvements in the coverage of ANC over the last two decades, about 40% of women globally still do not receive the recommended four routine ANC visits (WHO, 2015b), which may be due to interaction between potential factors such as rural residence, higher parity, low maternal education, and poverty across the region of sub‐Saharan Africa (WHO & UNICEF, 2003). Many women do not start ANC early enough to exploit all opportunities for ANC, possibly due to lack of understanding or ignorance or misconceptions of the purpose and value of ANC, the correct time to commence ANC, delayed recognition of pregnancy, and/or lack of support from husbands (Ebeigbe & Igberase, 2010; Gross, Alba, Glass, Schellenberg, & Obrist, 2012; Haddrill, Jones, Mitchell, & Anumba, 2014). Moreover, women who receive ANC often experience poor quality of care (WHO & UNICEF, 2003; WHO & World Bank, 2015; WHO, 2015b), and access to maternal health services is often affected by seasonality in sub‐Saharan Africa due to increased mother's workload during harvesting and planting season (O'Connell, Bedford, Thiede, & McIntyre, 2015) and substantial rainfall and flooding of roads during the wet season (Blanford, Kumar, Luo, & MacEachren, 2012).
Pregnant women are particularly vulnerable to iron deficiency anaemia because of increased iron demands for growth and maintenance of the maternal‐placental‐fetal unit (Balarajan, Ramakrishnan, Ozaltin, Shankar, & Subramanian, 2011) and physiological hemodilution (Goonewardene, Shehata, & Hamad, 2012), often aggravated by poor prepregnancy iron reserve (Breymann, 2015; Ronnenberg et al., 2004). A standard daily dose of oral iron and folic acid supplementation (30 to 60‐mg elemental iron with 400‐mcg folic acid) during pregnancy starting as early as possible as part of the ANC is currently recommended by the WHO to reduce the risk of low birth weight, maternal anaemia, and iron deficiency (WHO, 2012; WHO, 2016b). However, underutilization of recommended ANC may aggravate anaemia or iron deficiency during pregnancy due to delay in diagnosis and treatment of pre‐existing anaemia, inadequate access to prophylactic iron‐folic acid (IFA) supplementation, or lack of ANC counselling to adhere to IFA recommendations.
All countries in West Africa, including Niger, have an anaemia prevalence of ≥40% among pregnant women (Ayoya, Bendech, Zagre, & Tchibindat, 2012; WHO, 2015a) implying a severe public health concern (WHO, 2011). It has been estimated that the share of anaemia amenable to iron is >55% in pregnant women and children in low‐income regions of the world (Stevens et al., 2013). Iron deficiency contributes to maternal mortality (Black et al., 2008), and in Africa, 6.4% of maternal mortality is attributable to anaemia (Brabin, Hakimi, & Pelletier, 2001). Niger has a high maternal mortality rate (553 deaths/100,000 live births) (Central Intelligence Agency, 2015) and the world's highest fertility rate with an average of 7.6 children born per woman (The World Bank, 2015). The sustainable development goals target 3.1 aims to reduce the global maternal mortality ratio to <70 per 100,000 live births by 2030 (WHO, 2015b) and the World Health Assembly's second global nutrition target 2025 aims to reduce anaemia by 50% among women of reproductive age (WHO, 2014). Improvement in ANC seeking and adherence to IFA supplementation are expected to contribute to the reduction of maternal mortality and improve maternal and newborn health outcomes including reduction of maternal anaemia (Pena‐Rosas, De‐Regil, Garcia‐Casal, & Dowswell, 2015; WHO, 2015b).
Niger has adopted the policy of providing IFA supplementation during pregnancy through routine ANC (Wuehler & Biga Hassoumi, 2011). Despite significant improvements in the coverage of at least one ANC visit and distribution of IFA supplementation during pregnancy, coverage of the recommended four ANC visits (32.8%) and consumption of >90 IFA supplements (28.6%) remains low (INS & ICF International, 2013; WHO, 2016a). More importantly, the prevalence of anaemia in pregnant women is very high at 58.6% (WHO, 2016c).
The main objectives of the present study were to assess the prevalence of utilization of ANC and IFA and to identify the factors associated with utilization of ANC and adherence to recommended IFA supplementation among pregnant women in rural Zinder, Niger, using individual, household, and village level variables. Moreover, associations with seasonal variation were explored. Understanding the factors associated with ANC attendance and adherence to IFA supplementation during pregnancy will provide guidance for the development of sustainable intervention programmes to improve health and nutritional status of pregnant women in Niger.
Key messages.
ANC attendance and adherence to recommended IFA supplementation remains low in rural Zinder, Niger.
Longer gestational age (≥27 weeks) and previous health facility birth are positively associated with ANC attendance during current pregnancy in this population.
Women who reportedly received husbands' support are more likely to seek ANC and adhere to daily IFA supplementation.
ANC care seeking and adherence to recommended IFA supplementation may be improved through promotion of early ANC visits, ensuring availability and free distribution of IFA supplements at the health facility and involving husbands.
2. MATERIALS AND METHODS
2.1. Study design and participants
This study was a community‐based cross‐sectional survey of pregnant women carried out in two health districts in the Zinder region of Niger using a continuous enrollment schedule over a period of 12 months to account for seasonality (Mar 2014–Feb 2015). The survey was part of the baseline evaluation of the Niger Maternal Nutrition (NiMaNu) Project, which was registered with the U.S. National Institutes of Health (http://www.ClinicalTrials.gov, http://clinicaltrials.gov/ct2/show/NCT01832688?term=NCT01832688&rank=1). Households with potentially eligible pregnant women within the catchment areas of 12 integrated health centres (CSIs) were identified for the baseline survey employing a multistage clustered sampling design. Briefly, 12 CSIs (seven from Mirriah Health District and five from Zinder Health District) were initially selected by convenience sampling and were randomized to the order of participation. Within the catchment area of each CSI, five to eight villages were selected per CSI resulting in a total of 64 villages. The village in which the sampled CSI was located (CSI containing village) was automatically included in the study. One village with a health post (CS) was randomly selected per CSI (CS containing village) among all CS containing villages in the catchment area of that particular CSI. The remaining 3–6 villages per CSI were randomly selected from among the remaining villages (not containing any CSI or CS) after stratification by population size and distance to the health facility. To explore the impact of seasonality, we targeted enrollment of ~77 pregnant women per CSI to enroll of 923 women over 12 months. Pregnant women were identified and interviewed using the random walk method (United Nations, 2008), with a starting point randomly selected for each village (market, primary school, or mosque). Particpant enrollment continued until the desired sample size was reached (16–20 women per village) or until there were no more eligible pregnant women in the village.
Women of any age were eligible to participate in the survey if they reported being currently pregnant, had resided in the village for the six previous months, and planned to stay for at least two additional months. Those who presented with a severe illness warranting immediate hospital referral or were unable to provide consent due to mental disabilities were excluded from the study. All eligible pregnant women were interviewed through household visits using pretested structured questionnaires. Interviews were conducted by eight trained local female interviewers in Hausa, the predominant local language. Data were collected on sociodemographic characteristics of the households, anthropometric measurements, household food insecurity, dietary diversity, and knowledge, attitude, and practices of the women about ANC and IFA. To obtain village level information on village characteristics, infrastructures and services (Table S1), health centre personnel, and/or heads of villages were interviewed. In cases where respondents were not able to provide all village level information, we asked the interviewee to refer us to additional village representatives with relevant knowledge.
2.2. Ethical consideration
The study protocol and consenting procedures were approved by the National Consultative Ethical Committee of Niger and the Institutional Review Board of the University of California, Davis, USA. In case the pregnant woman was illiterate, an impartial witness was present during the consent process, who confirmed that the information in the consent document was accurately explained, and that consent was freely given. Informed consent was documented with a signature or a fingerprint.
2.3. Measures
2.3.1. Outcome variables
We constructed two primary dichotomous outcome variables. The first outcome was utilization of ANC, and the second outcome was adherence to recommended IFA supplementation. ANC use was defined as whether the woman participated in any ANC visit to any health facilities including CSI or CS during her current pregnancy regardless of her estimated gestational age. Adherence to recommended IFA supplementation was defined as whether the woman consumed IFA supplement daily in the previous 7 days if she had reported receiving any IFA supplement during her current pregnancy.
2.3.2. Independent variables
The independent variables examined are listed in the Table S1, and some additional explanations are provided below.
Gestational age and pregnancy trimester
A weighted average of gestational age was created in which reported measures for last menstrual period (LMP; LMP by months, LMP by lunar cycle, and LMP by proximity to a religious or cultural event), time elapsed since first quickening was felt and two fundal height measures together received each one third of the weight, as described in more detail elsewhere (Hess & Ouédraogo, 2016). We defined first trimester: <13 weeks, second trimester: ≥13 to <27 weeks, and third trimester: ≥27 weeks.
Nutritional status of pregnant woman
Low mid‐upper‐arm circumference was defined as <23 cm (Ververs, Antierens, Sackl, Staderini, & Captier, 2013). Women's dietary diversity was constructed from a food frequency questionnaire based on a woman's food intake in the past 24 hours. After an initial open recall, during which women were asked to list all foods consumed in the past 24 hours, a list‐based method was used to ask the woman if she had consumed any foods during the past 24 hours from each of the food groups (FAO & FHI 360, 2016). Consuming ≥5 food groups (out of 10) in the past 24 hours was considered as meeting the minimum dietary diversity for women (MDD‐W) (FAO & FHI 360, 2016).
Household socio‐economic status and food insecurity
Socio‐economic status of the household was estimated using three proxy indicators. Housing quality index was constructed based on whether the household had an improved roof, improved walls, or improved floors. It was a continuous scale from 0 to 1 where 1 was the highest possible score corresponding to the best housing quality. A household asset index was based on ownership of a set of assets including a radio, a mobile phone, a battery, a bicycle, a moped/motorcycle, and a car/truck. The household livestock index was a standardized composite measure of household small animals including goats, sheep, and poultry including a conversion factor for feed requirements (FAO, 2003). Household food insecurity was assessed using the Household Food Insecurity Access Scale of the Food and Nutrition Technical Assistance/USAID (Coates, Swindale, & Bilinsky, 2007). A household was categorized as food secure, or mildly, moderately or severely food insecure.
2.3.3. Statistical analyses
Data analyses were performed using Stata version 12.1 (Stata Corporation, College Station, TX, USA). A statistical analysis plan was created prior to analysis (Hess & Ouédraogo, 2016). For our two outcomes (utilization of ANC and adherence to recommended IFA supplementation), we considered two sample sizes. All 923 pregnant women who were interviewed during the household visits were included in the ANC coverage analyses. Women who received IFA (n = 401) provided information on adherence to recommended IFA supplementation (Figure 1).
Figure 1.
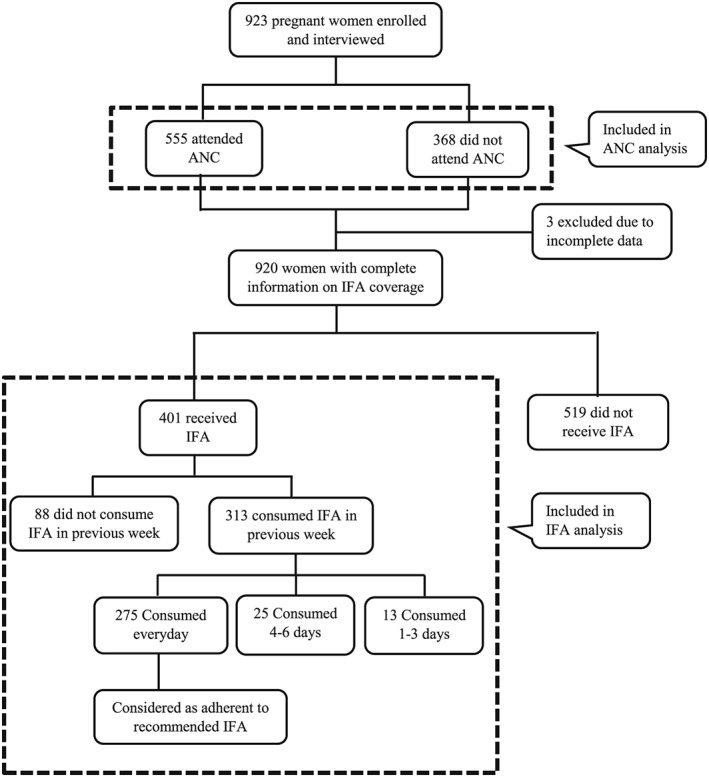
Flow chart of the pregnant women included in the ANC and IFA analyses. ANC = antenatal care; IFA = iron‐folic acid supplement
Descriptive analyses were used to assess the characteristics of women and villages. If a characteristic contained a homogenous response and less than 3% of respondents were in any category, we attempted to combine categories in logical ways to have each category contain at least 3% of respondents. The prevalence of outcome by categories of independent variables was measured taking into account the cluster design nature of the survey. To test for multicollinearity among independent variables, we ran collinearity diagnostics to calculate variance inflation factor and tolerance for each of the variables. We used variance inflation factor ≥2 (or equivalently, tolerances ≤0.50) as cut‐off values to minimize the possibility of multicollinearity within the variables. Bivariate logistic regression analyses were carried out to evaluate the unadjusted associations between dependent variables and each of the independent variables. All these bivariate models were adjusted to assess whether any of the significant associations in the bivariate models are attributable to variation in seasonality (i.e, time of year interview was conducted), estimated pregnancy trimester, or household socio‐economic status. For the purpose of analyses, we classified the seasons as (a) dry hot (Mar–May), (b) wet or lean (Jun–Sep), and (c) dry cool, harvest season (Oct–Feb; USAID & FEWS Net, 2011). Multivariable logistic regression models were constructed to identify the factors associated with ANC attendance and adherence to recommended IFA supplementation when controlling for the effect of other covariates. The decision of which covariates to include was based on public health significance and plausibility instead of any statistical criteria. In order to identify the women at risk of inadequate utilization of ANC, pregnancy‐related covariates that are meaningful and targetable in public health practices were included in the multivariable model. All models were adjusted for women's education as a variable of particular interest and relevance, because education has been found to be less associated with ANC use in sub‐Saharan Africa than in other regions of Africa and Asia (WHO & UNICEF, 2003). All models were constructed using mixed effect logistic regression procedure where CSI was considered as cluster nested within the health district as a fixed effect and village nested within CSI as a random effect. Results were considered significant at p < .05 and the final models present the results as odds ratios (ORs) with 95% confidence intervals (95% CI).
3. RESULTS
3.1. Participants' characteristics
All pregnant woman who were identified using the random walk method and invited to participate in the study, agreed to participation and provided written consent. Nine hundred twenty‐three pregnant women were enrolled from two health districts of Zinder (532 from Mirriah and 391 from Zinder). Seventy‐three to 82 women were enrolled within the catchment area of each of the 12 CSIs. Over half of the women were enrolled during the dry cool, harvest season (50.6%), and the rest during the dry hot season (19.1%) and lean season (30.3%).
The mean age ± standard deviation of the women was 26.1 ± 6.3 years (range 14–45 years; Table 1). All women were Muslim, 99.0% were married and 67.7% lived in a monogamous marriage. At the time of interview, 48.3% of the women were estimated to be in their third trimester of pregnancy, 40.5% were estimated to be in their second trimester, and only 2.4% were in their first trimester. Gestational age could not be estimated for 8.8% of the women. The median population of the 64 villages was 1,067 (range 42–7,397). Other village level characteristics are presented in Table 2.
Table 1.
Characteristics of participating pregnant women in Zinder, Niger
| Variables | % (n)a |
|---|---|
| Characteristics of the woman | |
| Age, years (mean ± SD) | 26.1 ± 6.3 |
| Ethnicity | |
| Hausa | 82.9 (765) |
| Tuareg | 12.5 (115) |
| Other minorities | 4.7 (43) |
| Education | |
| No education or literacy training only | 61.4 (567) |
| Koranic school | 20.3 (187) |
| Some primary education/completed 6th level | 12.9 (119) |
| Any type of secondary education | 5.4 (50) |
| Nutritional status of the woman | |
| MUAC <23 cm | 26.4 (244) |
| Adequate MDD‐W | 20.2 (186) |
| Woman's current pregnancy status | |
| Experienced nausea/vomiting in the past week because of pregnancy | 30.2 (279) |
| Any danger sign during current pregnancy | 60.4 (554) |
| Obstetric history of the woman | |
| Age at first pregnancy (median, min, max) | 17.0 (12.0, 30.0) |
| Gravidity (primigravida) | 12.9 (119) |
| Last pregnancy outcome | |
| Child born alive, still living | 83.8 (674) |
| Child born alive, had since died | 11.7 (94) |
| Still birth, miscarriage, abortion | 4.5 (36) |
| Attended ANC during last pregnancy | 89.9 (723) |
| Had at least four ANC during last pregnancy | 37.4 (300) |
| Health facility delivery during last pregnancy | 33.0 (264) |
| Woman's knowledge, attitudes and practices | |
| Knew about anaemia | 47.1 (435) |
| Knew about IFA supplements | 93.0 (854) |
| Knew about how to prevent or treat anaemia | 57.6 (250) |
| Had adequate knowledge of danger signs of pregnancy | 53.6 (493) |
| Mentioned IFA as one of the important practices for her and her child's wellbeing | 4.6 (42) |
| Mentioned ANC as one of the important practices for her and her child's wellbeing | 24.8 (229) |
| Support and advice received during current pregnancy | |
| Husband provided advice to go to ANC and woman followed advice | 22.5 (207) |
| Husband provided advice about consuming IFA and woman followed advice | 3.4 (31) |
| Aside from husband, pregnant woman received advice about her pregnancy from others | 39.6 (365) |
| Household level characteristics | |
| Number of houses in the household (median, min, max) | 1.0 (1.0, 6.0) |
| Principal occupation of the household head | |
| Farming related occupation | 39.9 (366) |
| Nonfarming related occupation | 50.2 (460) |
| Migrant/foreign remittance | 9.9 (91) |
| Levels of household food insecurity | |
| Food secure | 29.0 (267) |
| Mildly food insecure | 9.4 (86) |
| Moderately food insecure | 26.1 (240) |
| Severely food insecure | 35.5 (327) |
ANC = antenatal care; IFA = iron folic acid supplement; MDD‐W = minimum dietary diversity‐Women; MUAC = mid‐upper arm circumference.
Values are % (n), if not mentioned otherwise; number of observations associated with percentage are not always 923 because of missing values or skip pattern of the specific question asked.
Table 2.
Characteristics of the sampled villages in Zinder, Niger
| Variables | % (n)a |
|---|---|
| Distance of the village from the paved road | |
| Situated on the paved road | 21.9 (14) |
| ≤10 km from the paved road | 37.5 (24) |
| >10 km from the paved road | 40.6 (26) |
| Distance of the village from CSI/CS | |
| 0–1 km | 17.2 (11) |
| 2–10 km | 50.0 (32) |
| >10 km | 32.8 (21) |
| Number of TBA serving the village | |
| None | 7.9 (5) |
| One | 17.5 (11) |
| Two | 50.8 (32) |
| Three or more | 23.8 (15) |
| Number of community health agents serving the village | |
| None | 29.7 (19) |
| One | 20.3 (13) |
| Two | 21.9 (14) |
| Three or more | 28.1 (18) |
| Number of CSI serving the village | |
| One | 84.4 (54) |
| Two or more | 15.6 (10) |
| Number of CS serving the village | |
| None | 39.1 (25) |
| One | 40.6 (26) |
| Two or more | 20.3 (13) |
| Any pharmacy in the village | 20.3 (13) |
| Any market in the village | 21.9 (14) |
| Any electricity in the village | 17.5 (11) |
| Any microcredit organization in the village | 25.0 (16) |
| Any health organization in the village | 18.8 (12) |
| Any women's organization in the village | 40.6 (26) |
| Any husbands' group in the village | 12.5 (8) |
| Any food aid in the previous 6 months | 14.1 (9) |
CS = Centre de santé (health post); CSI = Centre de santé intégré (integrated health centre); TBA = traditional birth attendant.
Number of observations associated with percentage are not always 64 because of missing values.
3.2. Prevalence of attendance to any ANC visit and adherence to recommended IFA supplementation
Of the 923 women, 60.1% (n = 555) reported attending any ANC visit during the current pregnancy, 43.6% (n = 401) reported receiving any IFA supplement, 33.9% (n = 313) consumed any number of IFA supplements in the previous week, and 29.8% (n = 275) consumed the recommended number of IFA supplements in the previous week. There was no difference in ANC attendance and IFA adherence by age group (Table S2).
Of the 555 women who attended any ANC in the current pregnancy, 69.9% mentioned that they had chosen the facility because of their proximity to the facility, 88.5% reported attending ANC visits by walking, and 82.6% reported spending less than half a day for each ANC visit (Table S3). Although 93.2% reported not incurring any cost for any medication prescribed during the ANC visit, 19.5% reported paying for ANC exams. Only 4.8% of the women who attended ANC reported doing so in their first trimester of pregnancy (<13 weeks). Among women who did not attend ANC (n = 368), 74.5% stated that their pregnancies had not advanced enough to attend an ANC. Among those who mentioned that their pregnancy had not advanced enough to attend an ANC, 8.5% were estimated to be in the first trimester, 81.4% in the second trimester, and 10.1% in the third trimester of their pregnancy, respectively.
Of the 401 women who reportedly received any IFA supplements, 99.3% (n = 398) had attended at least one ANC during their current pregnancy. However, only 77.1% of women who attended ANC reported receiving IFA supplements. Seventy‐eight percent of women who had received IFA reported consuming any IFA in the previous week, and 68.6% reported adherence to IFA supplementation as recommended (i.e., consumed IFA every day in the previous week; Table S4). Of the 257 women who were asked about the sources of their last batch of IFA, 88.3% received IFA supplements free from the CSI and the remaining 11.7% purchased or otherwise acquired IFA. Common reasons for not adhering to IFA recommendations were that they had run out of supplements (40.2%), forgot (23.1%), and had experienced side effects (16.2%; Table S4).
3.3. Factors associated with of ANC attendance
Women who were interviewed in their third trimester of pregnancy (≥27 weeks) had significantly higher odds of ANC attendance in comparison to those interviewed before 27 weeks (OR: 19.19, 95% CI [12.81, 28.75]; Table S5). Women with adequate minimum dietary diversity (vs. inadequate MDD‐W) were more likely to report ANC attendance (OR: 1.77, 95% CI [1.21, 2.60]). Women who mentioned that they knew about IFA supplements or how to prevent and treat anaemia during pregnancy reported higher ANC attendance in comparison to those who reported not being aware of IFA or anaemia. Women who reportedly received and followed husbands' advice about going to ANC or consuming IFA were more likely to attend ANC in comparison to those who did not receive any advice (OR: 1.48, 95% CI [1.03, 2.11] and OR: 8.84, 95% CI [2.01, 38.94], respectively). All these unadjusted bivariate associations reported above remained significant when adjusted individually for seasonality, estimated pregnancy trimester, or housing quality index with the exception that women who received and followed husband's advice about going to ANC did not have significantly higher odds of ANC attendance when controlling for estimated pregnancy trimester (OR: 1.41, 95% CI [0.89, 2.23]; Table S5). Women who reported receiving advice about her pregnancy from other family members aside from husband were more likely to attend ANC in comparison to those who did not receive any advice (OR: 1.72, 95% CI [1.27, 2.33]), and this association remained significant when adjusted individually for pregnancy trimester, seasonality, and housing quality index (Table S5). There were no significant associations between ANC attendance and any of the sociodemographic characteristics, household food security, or other household characteristics evaluated, with the exception of the housing quality index (median vs. higher housing quality than the median OR: 1.48, 95% CI [1.02, 2.14]).
Women who delivered their last child in a health facility (vs. home) reported greater ANC attendance (OR: 2.25, 95% CI [1.55, 3.27]). In contrast, women who reported the death of a child born alive as the outcome of their last pregnancy (vs. child born alive and still living) had significantly lower odds of ANC attendance in the current pregnancy, and the overall association between ANC attendance and last pregnancy outcome was marginally significant (p = .06). Presence of any danger sign during the current pregnancy was positively associated with ANC attendance but was not significant when adjusted for pregnancy trimester (p = .21). Our multivariable analyses confirmed gestational age ≥27 weeks (vs. <27 weeks; OR: 21.81, 95% CI [13.81, 34.45]) and health facility birth during the last pregnancy (vs. home birth; OR: 2.38, 95% CI [1.45, 3.91]) as significant factors positively associated with ANC coverage (Table 3).
Table 3.
Factors associated with ANC attendance: multivariable analyses with pregnancy related variables as potential confounders and adjusted for women's education as a variable of particular interest and relevance
| Variables | OR (95% CI)a | p * | OR (95% CI)b | p * | OR (95% CI)c | p * |
|---|---|---|---|---|---|---|
| Woman's education | ||||||
| No education/literacy training only | ||||||
| Koranic school | 1.03 (0.70–1.52) | . | . | 1.51 (0.90–2.54) | ||
| Some primary education/completed 6th level | 0.75 (0.48–1.19) | . | . | 1.11 (0.56–2.18) | ||
| Any type of secondary education | 0.90 (0.45–1.81) | .639 | . | . | 0.99 (0.35–2.76) | .472 |
| Period of gestation by trimester at the time of survey | ||||||
| First and second trimester (<27 weeks) | ||||||
| Third trimester(≥27 weekks) | 19.19 (12.81–28.75) | .000 | 21.13 (13.43–33.25) | .000 | 21.81 (13.81–34.45) | .000 |
| Woman had any danger sign during current pregnancy | ||||||
| No | ||||||
| Yes | 1.44 (1.07–1.95) | .017 | 1.15 (0.76–1.74) | .522 | 1.13 (0.74–1.71) | .581 |
| Woman attended ANC during last pregnancy | ||||||
| No | ||||||
| Yes | 1.52 (0.92–2.52) | .104 | 1.41 (0.70–2.85) | .334 | 1.38 (0.69–2.78) | .366 |
| Woman's last pregnancy outcome | ||||||
| Child born alive, still living | ||||||
| Child born alive, had since died | 0.57 (0.36–0.91) | 0.54 (0.29–1.00) | 0.52 (0.28–0.97) | |||
| Still birth, miscarriage, abortion | 0.89 (0.42–1.86) | .059 | 1.21 (0.43–3.38) | .059 | 1.13 (0.40–3.17) | .110 |
| Place of delivery during last pregnancy | ||||||
| Home | ||||||
| Heath facility | 2.25 (1.55–3.27) | .000 | 2.44 (1.50–3.98) | .000 | 2.38 (1.45–3.91) | .001 |
ANC = antenatal care; CI = confidence interval; OR = odds ratio.
Bivariate.
Unadjusted multivariable.
Adjusted multivariable.
Bold indicates significant p‐value (p < 0.05).
The village characteristics that had significant positive association with ANC attendance in bivariate analyses were larger village population, having electricity in the village, presence of any secondary schools, existence of any agricultural or microcredit organizations, husbands' school or World Food Programme activities in the village. These relationships remained significant when the analyses were adjusted individually for seasonality, pregnancy trimester, or housing quality index (Table S5) but were not significant (data not shown) when adjusted for distance to the health facility. Greater distance of the village from a paved road or from the CSI were significantly negatively associated with ANC attendance.
3.4. Factors associated with adherence to recommended IFA supplementation
Adherence to recommended IFA supplementation was lower among women who used other means of transportation instead of walking (OR: 0.39, 95% CI [0.18, 0.85]), incurred expenses for roundtrip ANC transportation (vs. no expenses; OR: 0.39, 95% CI [0.16, 0.98]) and paid out of pocket payment for ANC examination (vs. no payment; OR: 0.51, 95% CI [0.26, 0.98]; S7). This significant negative association between IFA adherence and cost of ANC transportation (p = .02) persisted when adjusted for pregnancy trimester (p < .01) or maternal education (p = .02) or housing quality index (p = .02) but became only marginally significant when adjusted for seasonality (p = .06). Women who reportedly received husbands' advice about attending ANC and followed this advice were more likely to adhere to IFA recommendations compared to those who did not receive any advice or did not follow the advice received (OR: 1.80, 95% CI [1.04, 3.13]), and this association remained significant when adjusted individually for pregnancy trimester, seasonality, housing quality index, or maternal education. However, we did not find any association between advice received from other family members (aside from husband) and adherence to recommended IFA. Women who were interviewed during the dry hot or lean seasons were more likely to adhere to recommended IFA when compared to the women enrolled in the dry cool, harvest season, and this relationship persisted when adjusted for housing quality index but not for pregnancy trimester. No significant associations were found between adherence to recommended IFA supplementation and any of the sociodemographic, nutritional or past obstetric characteristics of the women, pregnancy trimester, or any household characteristics. Among the village characteristics, presence of any pharmacy in the village had significant positive association and presence of any market in the village had significant negative association with recommended IFA adherence. The negative association with existence of market in the village was not significant when the analysis was adjusted for seasonality.
To characterize the women at risk of poor adherence to recommended IFA supplementation, we built two multivariable models: one with pregnancy related variables and the other with ANC related variables since IFA receipt is directly associated with ANC attendance. Multivariable analyses with pregnancy variables confirmed that pregnancy‐related variables including pregnancy trimester were not significantly related to recommended IFA adherence with or without adjustment for women's education (data not shown). The multivariable model with ANC‐related variables confirmed that the cost of transportation for ANC attendance (vs. no cost), expenses incurred for any examination recommended during ANC (vs. no expenses), and out‐of‐pocket payment for any ANC medication (vs. no payment) were significantly negatively associated with adherence to IFA recommendations (p value .03, .05, and .03, respectively; Table 4).
Table 4.
Factors associated with adherence to recommended IFA supplements: multivariable analyses with ANC related variables adjusted for pregnancy trimester as potential confounders and women's education as a variable of particular interest and relevance
| Variables | OR (95% CI)a | p * | OR (95% CI)b | p * | OR (95% CI)c | p * |
|---|---|---|---|---|---|---|
| Woman's education | ||||||
| No education/literacy training only | ||||||
| Koranic school | 0.93 (0.51–1.69) | . | . | 0.93 (0.47–1.81) | ||
| Some primary education/completed 6th level | 1.98 (0.90–4.32) | 2.05 (0.85–4.94) | ||||
| Any type of secondary education | 0.52 (0.22–1.24) | .105 | . | . | 0.55 (0.20–1.53) | 0.189 |
| Period of gestation by trimester at the time of survey (n = 358) | ||||||
| First and second trimester (<27 weeks) | ||||||
| Third trimester(≥27 weeks) | 0.74 (0.39–1.41) | 0.362 | . | . | 0.86 (0.44–1.68) | 0.651 |
| Place of ANC visit (n = 397) | ||||||
| Health centre or higher level facility | ||||||
| Health post | 1.06 (0.53–2.12) | 0.862 | 0.59 (0.27–1.29) | 0.187 | 0.62 (0.26–1.48) | 0.287 |
| Cost of roundtrip transportation for attending ANC (n = 396) | ||||||
| No cost incurred | ||||||
| 100–2,500 West African CFA franc | 0.39 (0.16–0.98) | 0.045 | 0.49 (0.18–1.32) | 0.157 | 0.28 (0.09–0.86) | 0.027 |
| Did the woman pay for ANC exam fee (n = 397) | ||||||
| No | ||||||
| Yes | 0.51 (0.26–0.98) | 0.044 | 0.47 (0.23–0.97) | 0.042 | 0.44 (0.19–1.01) | 0.053 |
| Did the woman pay for ANC medication (n = 386) | ||||||
| No | ||||||
| Yes | 0.48 (0.20–1.18) | 0.109 | 0.40 (0.16–1.03) | 0.056 | 0.30 (0.11–0.86) | 0.025 |
| Time spent for each ANC visit (n = 396) | ||||||
| Less than half day | ||||||
| Half day | 0.48 (0.23–1.00) | 0.45 (0.21–0.96) | 0.49 (0.22–1.12) | |||
| More than half day | 1.25 (0.47–3.31) | 0.116 | 1.22 (0.46–3.21) | 0.098 | 1.53 (0.51–4.56) | 0.151 |
ANC = antenatal care; CI = confidence interval; IFA = iron‐folic acid supplement; OR, odds ratio.
Bivariate.
Unadjusted multivariable.
Adjusted multivariable.
Bold indicates significant p‐value (p < 0.05).
4. DISCUSSION
Using baseline cross‐sectional data from the NiMaNu project, our analyses showed that ANC and IFA coverage is low in rural Zinder, Niger. ANC coverage was particularly low in early pregnancy as women tended to attend ANC later in pregnancy. Besides trimester, we identified previous health facility birth and adequate dietary diversity as important positive factors associated with any ANC attendance during the current pregnancy. In contrast, we did not demonstrate any significant effect of seasonality on ANC attendance. Factors negatively associated with adherence to IFA recommendations included cost of roundtrip ANC transportation and out‐of‐pocket payment for any examination or any medication recommended during ANC visits, and husband's encouragement regarding ANC was positively associated with both ANC attendance and IFA adherence.
The ANC coverage in currently pregnant women in our study was 60.1%, which is much lower than the 2012 national estimates of 82.8% (INS & ICF International, 2013). This difference was likely due to methodological differences as women in the present survey, who were mostly in the second and third trimester, were asked about ANC attendance during the present pregnancy, whereas the Demographic and Health Survey asked women about their most recent pregnancy in the past 5 years. In fact, when asked about their most recent previous pregnancy, 89.9% of the women in our survey reported that they had attended ANC. Thus, our findings are comparable with the nationally representative ANC coverage derived from the Demographic and Health Survey 2012. However, only about half of the women in our survey reported attending at least four ANC visits in the previous pregnancy, and none of the 22 women who were currently in their first trimester (<13 weeks) of pregnancy reported yet attending any ANC visits in the present pregnancy. This is of concern, as failure to attend ANC early in pregnancy prevents timely detection and treatment of pregnancy‐related complications and leaves women at increased risk of morbidity and mortality during pregnancy, labour, and puerperium (Carroli, Rooney & Villar, 2001).
Unlike a systematic review on factors affecting the utilization of ANC in developing countries (Simkhada, Teijlingen, Porter, & Simkhada, 2008), our study did not demonstrate any significant association between ANC and sociodemographic variables such as age, ethnicity, education or occupation of the women, or any of the obstetric variables considered such as gravidity, previous history of fetal loss, last pregnancy outcome, or spacing between births. However, we identified health facility birth during the previous pregnancy as an independent predictor of ANC seeking during the current pregnancy. It is not clear whether this was due to health concerns during the previous pregnancy or positive experiences during the health facility birth or any other unidentified factors (e.g., financial security) that may link women who give birth at health centres and attend ANC. However, this cannot explain the negative association between the death of a child born alive during last pregnancy and ANC attendance because we do not know whether the last pregnancy outcome happened due to reasons related to health facility birth. Further research is needed to explore whether interactions with health staff, counselling received, and/or quality of postnatal appointments following previous health facility births have any impact on improving ANC attendance in subsequent pregnancies.
Geographic or physical access of the population to health facilities impacts availability of adequate health services (Feikin et al., 2009; Muller, Smith, Mellor, Rare, & Genton, 1998; Stock, 1983). In Niger, vaccination rates in children were strongly correlated with distance to health centre, with children living in closely located clusters having higher odds of complete vaccinations compared to those living in clusters further from a health centre (Blanford et al., 2012). Similarly, our study also provided evidence that greater distance between the village and a paved road or between the village and the health centre decrease ANC utilization. Access to ANC may potentially be improved by providing outreach services in inaccessible remote locations. ANC attendance was also positively associated with the presence of community‐level activities, such as husbands' school, through which health practices and ANC utilization may be promoted. Overall, all of the above findings highlight the importance of considering local context while designing public health interventions to increase ANC attendance and IFA compliance.
Consumption of recommended IFA supplementation by our study population (29.8%) was nearly similar to the national average (28.6%) although the parameter was defined differently in the national survey (percentage of women who reportedly consumed at least 90 IFA supplements in previous pregnancy in national survey vs. every day in the previous week of current pregnancy for the current survey; INS & ICF International, 2013). These findings are alarmingly low, and efforts are needed to increase both ANC and IFA coverage.
In many resource‐poor settings, ANC is considered as the main access point to the health care system for pregnant women (WHO & World Bank, 2015) and may be the only means of distribution of IFA. This is the case in our study area in Zinder, Niger. However, 28% of women who attended ANC did not receive any IFA supplementation. Moreover, 40% of those who had received IFA supplementation at some point during their pregnancy cited running out of IFA supplements as the reason for noncompliance. The lack of IFA supplements at home could be due to irregular ANC visits to refill IFA supplements or inadequate supply at the facility. Together, these highlight the importance of timely ANC visits and ensuring adequate supply and distribution of IFA throughout all ANC visits.
Our multivariable model confirmed cost of roundtrip ANC transportation and out‐of‐pocket payment for any examination or medication recommended during ANC visit as risk factors of poor adherence to daily IFA supplement consumption in comparison to those who did not incur any such cost or payment. We did not collect data to clarify why this may be the case. One possible explanation is that those who incurred any such costs did not revisit the facility to refill their IFA and hence ran out of supply. Alternatively, a woman who paid for transportation or medication may have had an illness along with her pregnancy, thus opting to pay for transportation because walking would have been more difficult; the care she sought could have been more focused on the illness than to IFA for her pregnancy, and when choosing what to consume, she could have been more concerned about the purchased medication than the IFA.
Evidence suggests that male involvement is associated with improved maternal health outcomes in developing countries including seeking ANC (Wai et al., 2015; Yargawa & Leonardi‐Bee, 2015). Consistent with this, we identified a positive association between husband's support and important maternal health outcomes such as ANC seeking and adherence to recommended IFA supplementation. We also found that presence of a husbands' school in the village was positively associated with ANC attendance by women in the study area. Thus, involving husbands in prenatal health care and recommended practices seems a promising strategy. One communication tool that builds on this is the Essential Nutrition Actions (Guyon & Quinn, 2011) providing specific messages for husbands to increase their participation and support in their wives' health care and nutrition during pregnancy and lactation.
An important strength of our study is the large sample size and the availability of a wide range of variables at the individual, household, and village level. The design of the survey consisting of continuous enrollment schedule over a period of 12 months allowed us to account for seasonality throughout the whole year. We minimized the sampling error by appropriate adjustment for cluster sampling design where both CSI and village were included as randomization structure covariates. Unlike other surveys, we interviewed currently pregnant women about their ANC attendance and IFA adherence, which minimized the possibility of longer recall bias. The major limitation of the study is that the data are only representative of a limited portion of the population, thus have limited generalizability to Niger as a whole. The analyses were also performed on cross‐sectional data, which restricted the establishment of causal association between the independent and outcome variables. Because of concerns of increased probability of false positives among all significant results during simultaneous multiple hypotheses testing, we limited the number of multivariable analyses and included only key covariates based on potential public health significance and plausibility instead of any statistical criteria into those multivariate models. Despite these limitations, the results of these analyses contribute to our understanding of the prevalence of and factors associated with inadequate ANC seeking and adherence to recommended IFA supplementation in a high‐risk rural population of Niger. In our analyses, sociodemographic variables did not appear to influence ANC and IFA. This suggests that the factors identified in this study may well be causal rather than explained by confounding with sociodemographic factors.
In summary, our study identified four falter points (USAID, 2014) related to access, distribution, and adherence to IFA supplementation: (a) did not attend at least one ANC visit: Many women failed to attend ANC during current pregnancy, and among those who attended, many missed early ANC and, thus, did not have access to adequate IFA supplementation throughout the duration of the pregnancy; (b) did not receive IFA supplements: Even among women who attended ANC, some did not receive IFA supplements during the ANC visit, possibly indicating insufficient supply or inappropriate distribution of IFA at the facility; (c) did not consume any IFA: Some women reportedly did not consume the IFA supplements they received; and (d) did not consume IFA everyday: Some women who reported consuming IFA did not consume daily as recommended. Public health interventions for pregnant women should address these falter points to ensure adequate access, distribution, and compliance to recommended IFA supplementation.
Adequate and timely ANC is crucial for reducing maternal and newborn morbidity and mortality through identifying and managing any complications during pregnancy early, providing supply of essential medications, counselling and support, and promoting health facility birth. In countries such as Niger where the ANC visit is the main access point for IFA distribution, promotion of at least four ANC visits, as recommended until recently by WHO, is crucial to ensure pregnant women's access to these supplements. At the health facility level, health care providers should maintain adequate supply and free distribution of IFA supplements through ANC visits and provide relevant information and counselling on the benefits, potential side effects, and proper dosage of IFA supplementation. At the community and family level, behaviour change communication strategies should include husbands to gain their support and involvement in their wives' prenatal health practices, ANC, and intake of recommended IFA supplementation.
CONFLICTS OF INTEREST
SEW works for Nutrition International (formerly the Micronutrient Initiative). All other authors declare that they have no conflicts of interest.
CONTRIBUTIONS
SYH, KB, KRW, RRY, and CTO conceived and designed the study. KB, RRY, and KRW analysed the data. KB, KRW, RRY, CTO, SEW, and SYH interpreted the results. KB and SYH prepared a first draft of the paper. All co‐authors critically reviewed the manuscript. All authors read and approved the final manuscript.
Supporting information
Table S1: List of independent variables
Table S2: Percent distribution of reported attendance at any ANC visit during current pregnancy and adherence to daily IFA consumption in the previous week, by characteristics of the women and village in which they live
Table S3: Reported utilization of antenatal care (ANC) among currently pregnant women in Zinder, Niger
Table S4: Reported utilization of iron‐folic acid (IFA) supplement among currently pregnant women in Zinder, Niger
Table S5: Associations between independent variables and reported ANC attendance among 923 currently pregnant women in Zinder, Niger: bivariate and adjusted bivariate analyses (adjusted individually for seasonality, pregnancy trimester and housing quality index)
Table S6: Associations between independent variables and reported daily IFA consumption in previous 7 days among 401 currently pregnant women in Zinder, Niger who received any IFA during pregnancy: bivariate and adjusted bivariate analyses (adjusted individually for seasonality, pregnancy trimester and housing quality index)
ACKNOWLEDGEMENTS
We thank the entire NiMaNu study staff. Special thanks go to Salamatou Mahamane and Adèle Bienvenu (Helen Keller International, Niger). Finally, we sincerely appreciate the support of the participants, the local communities and the staff of the Health Districts of Zinder and Mirriah, and the national steering committee. Charles Arnold, statistician at the University of California, Davis, provided statistical advice.
Begum K, Ouédraogo CT, Wessells KR, et al. Prevalence of and factors associated with antenatal care seeking and adherence to recommended iron‐folic acid supplementation among pregnant women in Zinder, Niger. Matern Child Nutr. 2018;14(S1):e12466 10.1111/mcn.12466
REFERENCES
- Ayoya, M. A. , Bendech, M. A. , Zagre, N. M. , & Tchibindat, F. (2012). Maternal anaemia in West and Central Africa: Time for urgent action. Public Health Nutrition, 15, 916–927. [DOI] [PubMed] [Google Scholar]
- Balarajan, Y. , Ramakrishnan, U. , Ozaltin, E. , Shankar, A. H. , & Subramanian, S. V. (2011). Anaemia in low‐income and middle‐income countries. Lancet, 378, 2123–2135. [DOI] [PubMed] [Google Scholar]
- Berhan, Y. , & Berhan, A. (2014). Antenatal care as a means of increasing birth in the health facility and reducing maternal mortality: A systematic review. Ethiopian Journal Health Science, 24(Suppl), 93–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black, R. E. , Allen, L. H. , Bhutta, Z. A. , Caulfield, L. E. , de Onis, M. , Ezzati, M. , … Rivera, J. (2008). Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet, 371, 243–260. [DOI] [PubMed] [Google Scholar]
- Blanford, J. I. , Kumar, S. , Luo, W. , & MacEachren, A. M. (2012). It's a long, long walk: accessibility to hospitals, maternity and integrated health centers in Niger. International Journal of Health Geographics, 11, 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brabin, B. J. , Hakimi, M. , & Pelletier, D. (2001). An analysis of anemia and pregnancy‐related maternal mortality. The Journal of Nutrition, 131, 604S–614S discussion 614S‐615S. [DOI] [PubMed] [Google Scholar]
- Breymann, C. (2015). Iron Deficiency Anemia in Pregnancy. Seminars in Hematology, 52, 339–347. [DOI] [PubMed] [Google Scholar]
- Carroli, G. , Rooney, C. , & Villar, J. (2001). How effective is antenatal care in preventing maternal mortality and serious morbidity? An overview of the evidence. Paediatric and Perinatal Epidemiology, 15(Suppl 1), 1–42. [DOI] [PubMed] [Google Scholar]
- Carroli, G. , Villar, J. , Piaggio, G. , Khan‐Neelofur, D. , Gulmezoglu, M. , Mugford, M. , … Bersgjø, P. (2001). WHO systematic review of randomised controlled trials of routine antenatal care. Lancet, 357, 1565–1570. [DOI] [PubMed] [Google Scholar]
- Central Intelligence Agency (2015). The world fact book: Niger. Accessed Retrieved from https://www.cia.gov/library/publications/the-world-factbook/geos/ng.html [Google Scholar]
- Coates, J. , Swindale, A. , & Bilinsky, P. (2007). Household Food Insecurity Access Scale (HFIAS) for Measurement of Household Food Access: Indicator Guide (v.3). Washington, D.C.: FHI 360/FANTA.
- Ebeigbe, P. N. , & Igberase, G. O. (2010). Reasons given by pregnant women for late initiation of antenatal care in the niger delta, Nigeria. Ghana Medical Journal, 44(2), 47–51. [PMC free article] [PubMed] [Google Scholar]
- FAO (2003) Compendium of Agricultural‐Environmental Indicators 1989‐91 to 2000. Statistics Analysis Service, Statistics Division, Food and Agriculture Organization of the United Nations, Rome.
- FAO and FHI 360 (2016). Minimum dietary diversity for women: A guide for measurement. Rome: Food and Agricultural Organizations (FAO) of the United Nations Washington, DC. [Google Scholar]
- Feikin, D. R. , Nguyen, L. M. , Adazu, K. , Ombok, M. , Audi, A. , Slutsker, L. , & Lindblade, K. A. (2009). The impact of distance of residence from a peripheral health facility on pediatric health utilisation in rural western Kenya. Tropical Medicine & International Health, 14, 54–61. [DOI] [PubMed] [Google Scholar]
- Fernandez Turienzo, C. , Sandall, J. , & Peacock, J. L. (2016). Models of antenatal care to reduce and prevent preterm birth: A systematic review and meta‐analysis. BMJ Open, 6, e009044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goonewardene, M. , Shehata, M. , & Hamad, A. (2012). Anaemia in pregnancy. Best Practice & Research. Clinical Obstetrics & Gynaecology, 26, 3–24. [DOI] [PubMed] [Google Scholar]
- Gross, K. , Alba, S. , Glass, T. R. , Schellenberg, J. A. , & Obrist, B. (2012). Timing of antenatal care for adolescent and adult pregnant women in south‐eastern Tanzania. BMC Pregnancy and Childbirth, 12, 16 10.1186/1471-2393-12-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyon, A. B. , & Quinn, V. J. (2011). Essential nutrition action frame work. Training guide for health workers. Washington DC: Core Group. [Google Scholar]
- Haddrill, R. , Jones, G. L. , Mitchell, C. A. , & Anumba, D. O. (2014). Understanding delayed access to antenatal care: A qualitative interview study. BMC Pregnancy and Childbirth, 14, 207 10.1186/1471-2393-14-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hess, S. Y. , & Ouédraogo, C. T. (2016). NiMaNu project. Open Science Framework. osf.io/4cenf.
- Institut National de la Statistique (INS) et ICF International (2013). Enquête Démographique et de Santé et à Indicateurs Multiples du Niger 2012. Calverton, Maryland, USA: INS et ICF International. [Google Scholar]
- Muller, I. , Smith, T. , Mellor, S. , Rare, L. , & Genton, B. (1998). The effect of distance from home on attendance at a small rural health centre in Papua New Guinea. International Journal of Epidemiology, 27, 878–884. [DOI] [PubMed] [Google Scholar]
- O'Connell, T. S. , Bedford, K. J. , Thiede, M. , & McIntyre, D. (2015). Synthesizing qualitative and quantitative evidence on non‐financial access barriers: Implications for assessment at the district level. International Journal for Equity in Health, 14, 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pena‐Rosas, J. P. , De‐Regil, L. M. , Garcia‐Casal, M. N. , & Dowswell, T. (2015). Daily oral iron supplementation during pregnancy. Cochrane Database of Systematic Reviews, 7, CD004736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronnenberg, A. G. , Wood, R. J. , Wang, X. , Xing, H. , Chen, C. , Chen, D. , … Xu, X. (2004). Preconception hemoglobin and ferritin concentrations are associated with pregnancy outcome in a prospective cohort of Chinese women. The Journal of Nutrition, 134, 2586–2591. [DOI] [PubMed] [Google Scholar]
- Simkhada, B. , Teijlingen, E. R. , Porter, M. , & Simkhada, P. (2008). Factors affecting the utilization of antenatal care in developing countries: Systematic review of the literature. Journal of Advanced Nursing, 61, 244–260. [DOI] [PubMed] [Google Scholar]
- Stevens, G. A. , Finucane, M. M. , De‐Regil, L. M. , Paciorek, C. J. , Flaxman, S. R. , Branca, F. , … Ezzati, M. (2013). Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non‐pregnant women for 1995‐2011: A systematic analysis of population‐representative data. The Lancet Global Health, 1, e16–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stock, R. (1983). Distance and the utilization of health facilities in rural Nigeria. Social Science and Medicine, 17, 563–570. [DOI] [PubMed] [Google Scholar]
- The World Bank (2015) World development indicators: Reproductive health.
- United Nations (2008). Designing household survey samples: Pactical guidelines. Department of Economic and Social Affairs, Statistics Division, United Nations Publication. [Google Scholar]
- USAID (2014) SPRING nutrition technical brief: A rapid assessment of the distribution and consumption of iron‐folic acid tablets through antenatal care in Niger, Accessed on July 05, 2016. Retrieved from https://www.spring-nutrition.org/sites/default/files/publications/briefs/spring_ifa_brief_niger.pdf
- USAID & FEWS Net (2011) Livelihoods zoning plus activity in Niger. A special report by the Famine Early Warning Systems Network (FEWS Net). Niamey, Niger.
- Ververs, M. T. , Antierens, A. , Sackl, A. , Staderini, N. , & Captier, V. (2013). Which anthropometric indicators identify a pregnant woman as acutely malnourished and predict adverse birth outcomes in the humanitarian context? PLoS Currents Disasters, Edition 1. 10.1371/currents.dis.54a8b618c1bc031ea140e3f2934599c8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wai, K. M. , Shibanuma, A. , Oo, N. N. , Fillman, T. J. , Saw, Y. M. , & Jimba, M. (2015). Are husbands involving in their spouses' utilization of maternal care services?: A cross‐sectional study in Yangon, Myanmar. PloS One, 10, e0144135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2002). WHO antenatal care randomized trial: Manual for the implementation of the new model. Geneva, Switzerland: World Health Organization. [Google Scholar]
- WHO (2011). Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity, vitamin and mineral nutrition information system. Geneva: World Health Organization. [Google Scholar]
- WHO (2012). Guideline: Daily iron and folic acid supplementation in pregnant women. Geneva: World Health Organization. [PubMed] [Google Scholar]
- WHO (2014). Comprehensive implementation plan on maternal, infant and young child nutrition. World Health Organization. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2015a). The global prevalence of anemia in 2011. Geneva: World Health Organization. [Google Scholar]
- WHO (2015b). Health in 2015: From MDGs, Millenium development goals to SDGs. World Health Organization, Geneva, Switzerland: Sustainable Development Goals. [Google Scholar]
- WHO (2016a) Global Health Observatory Data Repository: Antenatal Care Coverage Data by Country, Accessed Retrieved from http://apps.who.int/gho/data/view.main.321
- WHO (2016b). Guideline: Daily iron suplementation in adult women and adolescent girls. Geneva: World Health Organization. [PubMed] [Google Scholar]
- WHO (2016c) Maternal, newborn, child and adolescent health: Country profiles on maternal and perinatal health, Accessed Retrieved from http://www.who.int/maternal_child_adolescent/epidemiology/profiles/maternal/ner.pdf?ua=1
- WHO & UNICEF (2003). Antenatal care in developing countries: Promises, achievements and missed opportunities. Geneva, Switzerland: World Health Organization. [Google Scholar]
- WHO & World Bank (2015). Tracking universal health coverage: First global monitoring report. Geneva and Washington DC: World Health Organization and World Bank. [Google Scholar]
- Wuehler, S. E. , & Biga Hassoumi, A. (2011). Situational analysis of infant and young child nutrition policies and programmatic activities in Niger. Maternal & Child Nutrition, 7, 133–156. 10.1111/j.1740-8709.2010.00307.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yargawa, J. , & Leonardi‐Bee, J. (2015). Male involvement and maternal health outcomes: Systematic review and meta‐analysis. Journal of Epidemiology and Community Health, 69, 604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: List of independent variables
Table S2: Percent distribution of reported attendance at any ANC visit during current pregnancy and adherence to daily IFA consumption in the previous week, by characteristics of the women and village in which they live
Table S3: Reported utilization of antenatal care (ANC) among currently pregnant women in Zinder, Niger
Table S4: Reported utilization of iron‐folic acid (IFA) supplement among currently pregnant women in Zinder, Niger
Table S5: Associations between independent variables and reported ANC attendance among 923 currently pregnant women in Zinder, Niger: bivariate and adjusted bivariate analyses (adjusted individually for seasonality, pregnancy trimester and housing quality index)
Table S6: Associations between independent variables and reported daily IFA consumption in previous 7 days among 401 currently pregnant women in Zinder, Niger who received any IFA during pregnancy: bivariate and adjusted bivariate analyses (adjusted individually for seasonality, pregnancy trimester and housing quality index)


