Abstract
Metastases from melanoma, lung and breast cancer are among the most common causes of intracranial malignancy. Standard of care for brain metastases include a combination of surgical resection, stereotactic radiosurgery, and whole-brain radiation. However, evidence continues to accumulate regarding the efficacy of molecularly-targeted systemic treatments and immunotherapy. For non-small cell lung cancer (NSCLC), numerous clinical trials have demonstrated intracranial activity for inhibitors of EGFR and ALK. Patients with melanoma brain metastases may benefit from systemic therapy using BRAF-inhibitors with and without trametinib. Several targeted options are available for breast cancer brain metastases that overexpress HER2, although agents with intracranial activity are still needed for other molecular subtypes. Immune checkpoint inhibitors including anti-CTLA-4 and anti-PD-1/PD-L1 antibodies are yielding impressive responses in intracranial manifestations of metastatic melanoma and NSCLC. Given the promising early results with these emerging therapies, management of eligible patients will require increased multidisciplinary discussion incorporating novel systemic treatment approaches prior or in addition to local therapy.
Keywords: brain metastases, targeted therapy, precision medicine, immunotherapy, systemic therapy
INTRODUCTION
Metastases from systemic cancers are the most common type of intracranial malignancy, and the most common cancers that lead to brain metastases (BM) are lung (16.3% 5-year cumulative incidence), renal (9.8%), melanoma (7.4%), and breast (5.0%) [1]. The incidence of BM is likely increasing because patients are living longer due to more effective systemic therapies, as well as increasing use of screening neuroimaging. Traditionally, standard therapy for BM has focused on local treatment including craniotomy for resection and/or stereotactic radiosurgery (SRS), with whole-brain radiation therapy (WBRT) reserved for more disseminated intracranial disease [2]. A recent set of guidelines produced by the Congress of Neurological Surgeons (CNS) and the American Association of Neurological Surgeons/CNS Section on Tumors provides updated recommendations regarding the roles of surgery, SRS, and WBRT but concluded that there is insufficient evidence to make recommendations regarding molecularly targeted agents [3, 4].
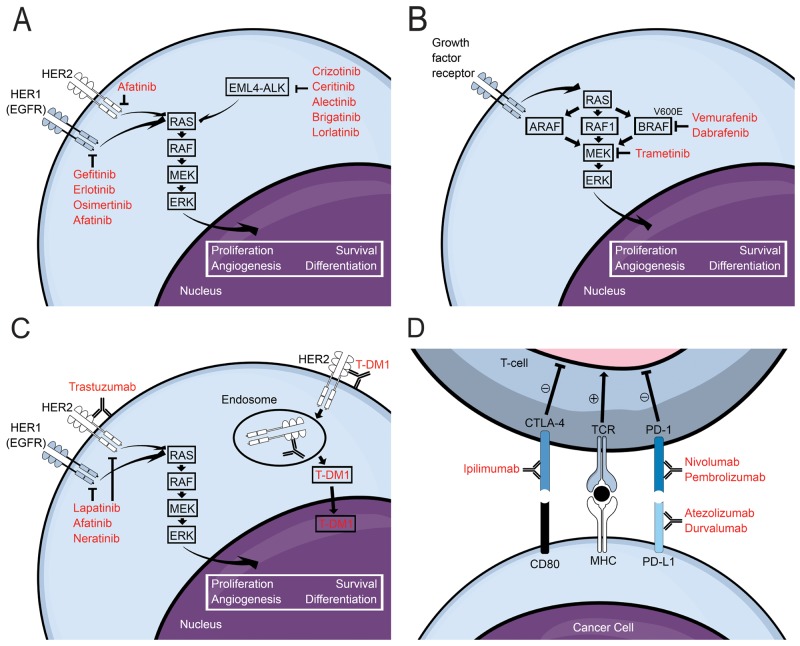
Although attractive in many cases, the utility of conventional systemic therapy in the treatment of BM has historically been limited due to poor penetration across the blood-brain (BBB) and blood-tumor barrier [5]. Traditional clinical trials for systemic therapies have excluded patients with symptomatic or uncontrolled BM due to these challenges with central nervous system (CNS) penetration [1]. More recently, targeted systemic therapies have demonstrated improved extracranial disease control and survival in molecularly defined subpopulations, and the ability of these medications to complement or even replace local treatment of BM is under intense investigation [6]. In fact, a series of recent studies have importantly suggested that many targeted agents are able to achieve therapeutic concentrations in the brain, including EGFR- and ALK- inhibitors for non-small cell lung cancer, BRAF- and MEK- inhibitors for melanoma, and HER2-directed therapies for breast cancer. In addition, systemically delivered immune therapies such as checkpoint blockade have also demonstrated efficacy in the CNS [7]. Furthermore, while earlier trials were difficult to interpret due to variations in response and progression criteria, the Response Assessment in Neuro-Oncology Brain Metastases (RANO-BM) provided standardization in study assessments [8]. This review summarizes emerging evidence for targeted systemic therapies for the most common sources of BM, which are illustrated in Figure 1.
Figure 1.
Schematic diagrams illustrating mechanisms of action for (A) EGFR- and ALK- inhibitors for non-small cell lung cancer, (B) BRAF- and MEK- inhibitors for metastatic melanoma, (C) HER2-targeted therapies for breast cancer, and (D) immune checkpoint inhibitors. For additional information regarding PD-L1 inhibitors please see article by O’Kane and Leighl [83]. Abbreviations: HER: human epidermal growth factor receptor; EGFR: epidermal growth factor receptor; EML4: echinoderm microtubule-associated protein-like 4; ALK: anaplastic lymphoma kinase; T-DM1: trastuzumab emtansine; CTLA-4: cytotoxic T-lymphocyte-associated protein 4; CD80: cluster of differentiation 80; TCR: T-cell receptor; MHC: major histocompatibility complex; PD-1: programmed cell death protein 1; PD-L1: programmed death-ligand 1.
LUNG CANCER BRAIN METASTASES
Lung cancer is the leading cause of cancer death overall, and 13-44% of patients with lung cancer ultimately develop BM [9–11]. Although BM are more common in small cell lung cancer, most studies have focused on the targeted treatment of metastases from non-small cell lung cancer (NSCLC) because the latter represents a greater proportion (80-85%) of total lung cancer cases [9]. NSCLC comprises a heterogeneous group of cancers including squamous cell carcinoma, large cell carcinoma, and adenocarcinoma. Several molecular driver mutations have been identified within NSCLC including mutation of epidermal growth factor receptor (EGFR), as well as fusion of anaplastic lymphoma kinase (ALK) and echinoderm microtubule-associated protein-like 4 (EML4) genes [1]. Targeted therapies for NSCLC BM have focused on inhibitors of these subclasses of tumors (Table 1).
Table 1. Selected clinical studies of targeted treatments for non-small cell lung cancer brain metastases.
| Authors & Year | Regimen | Target (gen.) | N | cRR (%) | PFS (mo) | OS (mo) |
|---|---|---|---|---|---|---|
| Kim et al., 2009 | Gefitinib or erlotinib | EGFR (I) | 23 | 73.9 | 7.1 | 18.8 |
| Iuchi et al., 2013 | Gefitinib | EGFR (I) | 41 | 87.8 | 14.5 | 21.9 |
| Welsh et al., 2013 | Erlotinib + WBRT | EGFR (I) | 40 | 86 | 8.0 | 11.8 |
| Hoffknecht et al., 2015 | Afatinib | EGFR (II) | 100 | 35 | 3.6 | 9.8 |
| Kim et al., 2016 (ASCEND-1) | Ceritinib | ALK (II) | 94 | 68 | -- | -- |
| Crino et al., 2016 (ASCEND-2) | Ceritinib | ALK (II) | 100 | 45 | 5.4 | -- |
| Soria et al., 2017 (ASCEND-4) | Ceritinib | ALK (II) | 121 | 46.3 | 10.7 | -- |
| Shaw et al., 2017 (ASCEND-5) | Ceritinib | ALK (II) | 66 | 35 | 4.4 | -- |
| Gadgeel et al., 2014 | Alectinib | ALK (II) | 21 | 52 | -- | -- |
| Gadgeel et al., 2016 | Alectinib | ALK (II) | 136 | 42.6 | 11.1 | -- |
| Novello et al., 2018 (ALUR) | Alectinib | ALK (II) | 40 | 54.2 | -- | -- |
| Camidge et al, 2018 (ALTA) | Brigatinib | ALK (II) | 59 | 46-67 | 14.6-18.4 | -- |
| Shaw et al., 2017 | Lorlatinib | ALK/ROS1 (III) | 24 | 46 | -- | -- |
| Solomon et al., 2018 | Lorlatinib | ALK/ROS1 (III) | 165 | 53.1-87.0 | -- | -- |
Abbreviations: cRR: CNS response rate; gen: generation; mo: months; N: # patients; OS: overall survival; PFS: progression free survival; WBRT: whole-brain radiation therapy.
EGFR inhibitors
Mutation of EGFR increases its kinase activity thereby promoting tumor cell survival in 10-35% of NSCLC [12]. First generation EGFR inhibitors bind reversibly to the tyrosine kinase of EGFR, whereas second-generation agents bind irreversibly and are therefore more potent. Third generation EGFR inhibitors have less adverse effects and are active against tumors with acquired EGFRT790M mutations [8]. The two first-generation EGFR inhibitors, erlotinib and gefitinib, have shown potent activity within the CNS. However, most prospective studies evaluating the efficacy of erlotinib or gefitinib for NSCLC BM have used them as second-line agents in patients who had been previously treated with radiotherapy or chemotherapy [13, 14].
Two published phase II trials have evaluated first-generation EGFR inhibitors (gefitinib or erlotinib) as first-line therapy in patients with EGFR-mutant NSCLC with BM [15, 16]. None of the patients in these trials had received prior treatment with chemotherapy or radiotherapy. Both studies showed favorable response of BM to either gefitinib or erlotinib with progression free survival (PFS) between 7.1 and 14.5 months and overall survival (OS) between 18.8 and 21.9 months. Additional studies have evaluated the efficacy of radiotherapy combined with EGFR inhibitors in radiotherapy-naïve patients with EGFR-mutated NSCLC BM [17–19]. One clinical trial using erlotinib concurrently with WBRT showed improved PFS (12.3 versus 5.2 months) and OS (19.1 versus 9.3 months) in patients with EGFR mutations compared to those without [20]. Intracranial response rate within the study cohort was 86%, including 31% who experienced complete response. Overall, the first-generation EGFR inhibitors, gefitinib and erlotinib, appear to be effective in controlling BM both with and without concurrent radiation in patients with EGFR-mutant NSCLC.
At present, data are sparse regarding the second and third-generation EGFR inhibitors, afatinib and osimertinib, respectively, in treatment of NSCLC BM. One prospective study assessed the efficacy of afatinib in 100 patients with NSCLC BM [21]. These patients had all failed at least one prior platinum-based chemotherapy as well as a first-generation EGFR inhibitor. PFS in patients treated with afatinib was 3.6 months, and cerebral response rate was 35%. Further clinical trials on the efficacy of afatinib for the treatment of NSCLC BM are underway (NCT02768337). The third-generation EGFR inhibitor, osimertinib, has been approved for patients with a specific EGFR mutation (T790M) who have failed prior tyrosine kinase inhibitor treatment [22]. Preclinical studies have shown good CNS penetration and activity of third-generation EGFR inhibitors [23], and additional clinical trials are underway (NCT02972333, NCT02736513, NCT02971501). The efficacy of second and third-generation EGFR inhibitors for the management of NSCLC BM requires further study before they can be recommended for clinical use.
ALK inhibitors
ALK-positive NSCLC make up approximately 5% of patients with NSCLC metastases and are characterized by a fusion of ALK and EML4 genes. These patients are of particular interest because they comprise primarily younger patients with little or no smoking history and for which EGFR inhibitors do not work [24, 25]. BM appear to be more common in patients with ALK-positive NSCLC compared to unselected NSCLC [9, 26]. Several notable ALK inhibitors have been studied with positive effects in ALK-positive NSCLC BM [27].
The first-generation ALK inhibitor, crizotinib, was approved in 2011 for treatment of patients with locally advanced or metastatic ALK-positive NSCLC. A retrospective analysis of two randomized clinical trials (PROFILE 1005 and 1007) examined the intracranial response to crizotinib in patients with ALK-positive NSCLC BM, and found intracranial disease control rates of 56-62% [28]. However, several studies have found CNS disease progression resulting from acquired resistance to crizotinib [29–31].
Subsequently, two second-generation ALK inhibitors, ceritinib and alectinib, were found to have improved CNS penetration and are now approved for the treatment of ALK-positive metastatic NSCLC in patients who previously failed crizotinib [9]. An open-label phase I trial assessed the safety of ceritinib in 246 patients (ASCEND-1), and efficacy was determined in post-hoc analysis [32]. In this trial, 94 (38%) patients had confirmed BM and follow-up neuroimaging. Intracranial disease control with ceritinib was 79% and 65% in ALK-inhibitor naïve and previously ALK-inhibitor treated patients, respectively. Intracranial activity of ceritinib has been confirmed in several follow-up phase II/III studies (ASCEND 2-5) [33–35]. An open-label, multicenter phase II trial is ongoing to assess the safety and efficacy of ceritinib in patients with ALK-positive NSCLC and brain or leptomeningeal metastases (NCT02336451). At present, ceritinib appears to be effective in controlling BM from ALK-positive NSCLC and may be more beneficial when used prior to crizotinib.
Following the phase I trial for alectinib in patients with ALK-positive NSCLC, a multi-center, single-group, open-label phase II trial was undertaken in North America [36, 37]. All 87 patients in this trial had baseline CNS imaging with MRI or CT, and 16 (18%) had measurable CNS disease at baseline. Of these, 11 (69%) had received prior brain radiation therapy. Complete CNS response was reported in 4 of the 16 patients, and partial response in an additional 8 of 16. Median duration of CNS response was 11.1 months. A global phase II trial assessing 138 patients with ALK-positive NSCLC who were treated with second-line alectinib after failing crizotinib showed similar results [38]. A pooled analysis of these two trials included 225 total patients, 136 (60%) of which had CNS metastases at baseline (50 measurable, 86 unmeasurable) [39]. All patients had been previously treated with crizotinib and 95 (70%) had already undergone radiation therapy. Complete CNS response was seen in 37 (27.2%) patients, partial response in 21 (15.4%), and 58 (42.6%) patients had stable CNS disease. Median CNS duration of response was 11.1 months.
Following the success of phase I and II trials for alectinib in ALK-positive NSCLC, several phase III studies focused on CNS disease [40–42]. The ALEX study included 122 patients with ALK-positive NSCLC and baseline BM who received either alectinib or crizonitib [43]. CNS response rate was 85.7% with alectinib versus 71.4% with crizonitib in patients with prior radiotherapy and 78.6% versus 40.0%, respectively, in those without prior radiotherapy. The ALUR study randomized a total of 107 patients with advanced ALK-positive NSCLC who were previously treated with crizotinib to receive either alectinib or chemotherapy [40]. Out of the 40 patients with baseline measurable CNS disease (24 alectinib, 16 chemotherapy), CNS response rate was higher with alectinib (54.2%) versus chemotherapy (0%). Together, these studies suggest robust response of ALK-positive NSCLC BM to alectinib both as initial and secondary ALK inhibitor therapy.
Another second-generation ALK-inhibitor, brigatinib, has shown promising intracranial disease activity in clinical trials [44, 45]. ALTA was a randomized phase II trial in which patients with ALK-positive NSCLC with baseline BM received varying doses of brigatinib [44]. Intracranial response rate among patients with measurable BM was 46-67% (total 59 patients). Median intracranial PFS was 14.6 to 18.4 months. Another open-label, randomized, phase III trial enrolled 275 patients with advanced ALK-positive NSCLC who were ALK-inhibitor naïve to receive brigatinib or crizotinib [45]. Among 39 patients with measurable brain lesions, intracranial response rate was 14 out of 18 (78%) with brigatinib versus 6 out of 21 (29%) with crizotinib. Therefore, brigatinib has improved intracranial activity compared to crizotinib and is efficacious in the treatment of ALK-positive NSCLC BM.
Finally, promising data are emerging regarding a third-generation dual-inhibitor of ALK and ROS proto-oncogene 1 (ROS1) with CNS penetrance, lorlatinib. An international multicenter, open-label phase I study enrolled 54 patients with advanced ALK-positive or ROS1-positive NSCLC to receive lorlatinib at varying doses, including 24 with baseline measurable BM [46]. Of these, 11 of 24 had intracranial objective response to the treatment drug (7 complete, 4 partial). This was followed by a phase II study which included 276 patients with ALK- or ROS1-positive NSCLC who underwent treatment with lorlatinib [47]. Study patients were divided into 6 cohorts on the basis of ALK and ROS1 status and previous therapy with crizotinib, other ALK-inhibitors, or chemotherapy. In patients with measurable baseline BM, objective intracranial responses were noted in 53.1-87.0% of patients with ALK-positive NSCLC. Lorlatinib is currently undergoing a phase III trial comparing its efficacy against crizotinib as first-line treatment for ALK-positive NSCLC (NCT02927340 and NCT03052608). Overall, lorlatinib demonstrates strong activity against ALK-positive NSCLC BM and may also be efficacious for ROS1-positive NSCLC.
MELANOMA BRAIN METASTASES
The prevalence of BM in patients with malignant melanoma is as high as 50-75%, and survival of patients with multiple BM is generally 6 months or less [48–50]. Because patients with melanoma BM frequently have multiple small metastases, systemic targeted therapy is an attractive treatment option (Table 2) [9, 51, 52].
Table 2. Selected clinical studies of targeted treatments for melanoma brain metastases.
| Authors & Year | Regimen | Target | N | cRR (%) | PFS (mo) | OS (mo) |
|---|---|---|---|---|---|---|
| Dummer et al., 2014 | Vemurafenib | BRAF | 24 | 84 | 3.9 | 5.3 |
| McArthur et al., 2017 | Vemurafenib | BRAF | 146 | 18 | 3.7-4.0 | 8.9-9.6 |
| Falchook et al., 2012 | Dabrafenib | BRAF | 10 | 90 | 4.2 | -- |
| Long et al., 2012 (BREAK-MB) | Dabrafenib | BRAFV600E | 139 | 30.8-39.2 | 16.1-16.6 | 31.4-33.1 |
| Davies et al., 2017 (COMBI-MB) | Dabrafenib + trametinib | BRAFV600E/MEK | 76 | 58 | 5.6 | 10.8 |
Abbreviations: cRR: CNS response rate; mo: months; N: # patients; OS: overall survival; PFS: progression free survival
BRAF-inhibitors
The proto-oncogene BRAF is mutated in approximately 50% of malignant melanomas [53], and BRAF-mutant melanoma is associated with a higher rate of CNS involvement (24%) compared with BRAF wild type melanomas (12%) [54]. At present, two BRAF-inhibitors, vemurafenib and dabrafenib, are approved for the treatment of advanced malignant melanoma. An open-label phase II trial treated 24 patients with nonresectable, previously treated BRAF-mutated melanoma BM using vemurafenib [55]. In this cohort, median OS was 5.3 months and PFS was 3.9 months. Among 19 patients with measurable intracranial disease at baseline, 3 (16%) experienced partial response and 13 (68%) had stable intracranial disease. Another multicenter, open-label phase II trial examined the response of BM from BRAF-mutated melanoma to vemurafenib [56]. The study included 90 patients with previously untreated BM (cohort 1), and 56 patients who had received prior treatment for their BM (cohort 2). Overall intracranial response rate was 16 out of 90 (18%) in cohort 1, including two complete responses and 14 partial responses. Median OS and PFS were 8.9 and 3.7 months in cohort 1, respectively, and 9.6 and 4.0 months in cohort 2, respectively. Together, these studies suggest a modest response of intracranial disease to vemurafenib in BRAF-mutant melanoma.
Use of dabrafenib to treat melanoma BM has been explored in a phase I trial involving 184 patients who received the drug for incurable solid tumors [57]. Out of 10 patients who had asymptomatic, untreated BM, 9 had decrease in size of their BM, and 4 had complete resolution. Median PFS was 4.2 months in this subset of patients. A subsequent multicenter, open-label phase II trial included 172 patients with melanoma BM who were treated with dabrafenib [58]. Patients were divided by prior local treatment status and by type of BRAF-mutation (BRAFV600E or BRAFV600K). Out of 74 patients with previously untreated BM and BRAFV600E mutations, 29 (39.2%) had an overall intracranial response. Out of 65 patients who had undergone prior local treatment for BM and had BRAFV600E mutations, 20 (30.8%) achieved overall intracranial response. OS and PFS were 33.1 and 16.1 months, respectively, for untreated patients, and 31.4 and 16.6 months, respectively, for previously treated patients. Response rates, OS, and PFS were lower in patients with BRAFV600K-mutant melanoma. Overall, dabrafenib has activity against BRAFV600E-mutant melanoma BM regardless of prior local treatment status.
BRAF- and MEK-inhibitor combination therapy
One major challenge in treating metastatic melanoma with BRAF-inhibitors is the 13 development of resistance secondary to upregulation of other proteins in the Ras-Raf-MEK14 MAPK pathway, such as RAF1 (C-RAF) or RAS. This can lead to increased tumor cell 15 proliferation and even to the development of secondary skin tumors such as squamous cell 16 carcinomas [59–62]. This finding has led to trials combining treatment with BRAF-inhibitors and 17 the MEK-inhibitor, trametinib. An open-label phase III trial investigated the efficacy of 18 dabrafenib and trametinib combination treatment in 704 patients with BRAF-mutated metastatic 19 melanoma [63]. The study found that first-line combination dabrafenib-trametinib led to 20 improved 12 months OS (72% versus 65%) and longer median PFS (11.4 versus 7.3 months) 21 compared to vemurafenib monotherapy. This was followed by a multicenter, open-label, phase II 22 trial (COMBI-MB) that examined intracranial response to combination dabrafenib-trametinib in 23 patients with BRAF-mutant melanoma BM [64]. The study found intracranial response in 44 of 1376 (58%) patients, OS of 10.8 months, and PFS of 5.6 1 months in patients with BRAFV600E-2 mutant, asymptomatic BM with no prior local treatment. Overall, patients appear to benefit 3 clinically from dabrafenib-trametinib as evidenced by median OS of 10.1-24.3 versus 3.4 months 4 in historical controls treated with WBRT alone.
BREAST CANCER BRAIN METASTASES
Breast cancer is the most common cancer in women, and 10-20% of breast cancer patients have BM [65, 66]. Breast cancers can be classified on the basis of estrogen receptor, progesterone receptor, and human epidermal growth factor receptor 2 (HER2) status. HER2 overexpression is present in approximately 25-30% of breast cancers, and these are 2-4 times more likely to result in BM [9]. Thus far, only HER2-positive breast cancers have found success in targeted therapy for BM (Table 3) [67, 68].
Table 3. Selected clinical studies of targeted treatments for HER2-positive breast cancer brain metastases.
| Authors & Year | Regimen | Target | N | cRR (%) | PFS (mo) | OS (mo) |
|---|---|---|---|---|---|---|
| Lin et al., 2009 | Lapatinib +/- capecitabine | HER2/EGFR | 242 | 6-20 | 2.4-3.7 | 6.4 |
| Bachelot et al., 2013 (LANDSCAPE) | Lapatinib + capecitabine | HER2/EGFR | 45 | 66 | 5.5 | 17 |
| Freedman et al., 2019 | Neratinib + capecitabine | HER2/EGFR | 49 | 33-49 | 3.1-5.5 | 13.3-15.1 |
| Krop et al., 2015 (EMILIA) | T-DM1 | HER2 | 45 | -- | 5.9 | 26.8 |
| Bartsch et al., 2015 | T-DM1 | HER2 | 10 | 50 | 5 | -- |
Abbreviations: cRR: CNS response rate; mo: months; N: # patients; OS: overall survival; PFS: progression free survival; T-DM1: trastuzumab emtansine.
Trastuzumab is a monoclonal humanized antibody directed against the extracellular domain of HER2 and is highly effective for the treatment of HER2-positive breast cancer [69–71]. Although trastuzumab cannot cross the intact BBB due to its large molecular size, studies have suggested trastuzumab penetration in BM secondary to BBB breakdown [72]. Retrospective studies have shown response of BM to intravenous trastuzumab [73], and prospective trials assessing the efficacy of trastuzumab in the treatment of HER2-positive breast cancer BM are underway (NCT02571530 and NCT01325207). Currently, however, evidence for the use of trastuzumab in the treatment of breast cancer BM is still accumulating.
Lapatinib is a small receptor tyrosine kinase inhibitor that interferes with both HER2 and EGFR signaling and is believed to cross the BBB, albeit to a limited extent in the commonly used dosing regimen [74]. An open-label, multicenter phase II trial included 242 patients with HER2-positive breast cancer and BM who had been treated with trastuzumab and a combination of WBRT and SRS, followed by lapatinib [75]. CNS partial response was seen in 6% of patients, stable disease in 37%, and progressive disease in 46%. There were no complete responses. OS in the study was 6.4 months and PFS was 2.4 months. An extension of the trial included 50 patients who received additional treatment with lapatinib plus capecitabine, resulting in CNS partial response rate of 20% (no complete responses) and PFS of 3.7 months. The LANDSCAPE trial was an open-label, multicenter phase II trial that evaluated the response of radiation-naïve HER2-positive breast cancer BM to first-line lapatinib-capecitabine [76]. Out of the total 45 patients, partial CNS responses were seen in 29 (66%), median OS was 17 months, and PFS was 5.5 months. Clinical trials investigating the efficacy of lapatinib in combination with WBRT or SRS for treatment of HER2-positive breast cancer BM are ongoing (NCT01622868). Two additional dual HER2 and EGFR inhibitors, afatinib and neratinib, are undergoing clinical trials for treatment of BM from HER2-positive breast cancer with promising results [77, 78]. In summary, dual HER2 and EGFR inhibitors exhibit modest CNS activity and may be used in the management of HER2-positive breast cancer BM.
Trastuzumab emtansine (T-DM1) is an antibody-drug conjugate of trastuzumab and the cytotoxic microtubule-inhibitor DM1 (also known as emtansine). This was approved for the treatment of metastatic HER2-positive breast cancer based on the phase III EMILIA trial which compared T-DM1 with lapatinib plus capecitabine and found improved PFS, OS, and objective response rate for T-DM1 [79]. A subsequent retrospective analysis of the EMILIA trial looked at the response rates of patients with BM at baseline and found significantly longer OS in those treated with T-DM1 (26.8 months) compared to lapatinib-capecitabine (12.9 months) [80]. A study examining T-DM1 as primary systemic therapy for BM from HER2-positive breast cancer found clinical benefit for CNS disease in 5 of 10 patients [81]. T-DM1 demonstrated CNS activity for HER2-positive breast cancer BM, but additional clinical studies are needed due to the small sample size and retrospective nature of existing evidence.
IMMUNE CHECKPOINT INHIBITORS
Cancer immunotherapy refers to the modulation of the host’s immune system to treat malignancies and includes the use of checkpoint inhibitors (anti-CTLA-4 and anti-PD-1/PD-L1 antibodies) to amplify the patient’s own antitumor immune response [7]. Checkpoint inhibitors have previously shown strong efficacy in extracranial advanced melanoma and NSCLC. However, the intracranial immune response is highly regulated and most checkpoint inhibitor clinical trials have excluded patients with BM [82]. More recent studies have yielded promising results regarding the use of checkpoint inhibitors for treatment of melanoma and NSCLC BM, and additional trials are underway (Table 4) [51, 83].
Table 4. Selected clinical studies of immune checkpoint inhibitors for brain metastases.
| Authors & Year | Regimen | Mechanism | Primary cancer | N | cRR (%) | PFS (mo) | OS (mo) |
|---|---|---|---|---|---|---|---|
| Margolin et al., 2012 | IPI | CTLA-4 | Melanoma | 72 | 10-25 | -- | 3.7-7.0 |
| Di Giacomo et al., 2012 (NIBIT-M1) | IPI + FTM | CTLA-4 | Melanoma | 20 | 50 | 3.0 | 12.7 |
| Kluger et al., 2019 | Pembrolizumab | PD-1/PD-L1 | Melanoma | 23 | 26 | 2 | 17 |
| Goldberg et al., 2016 | Pembrolizumab | PD-1/PD-L1 | NSCLC | 18 | 33 | -- | 7.7 |
| Tawbi et al., 2018 | Nivolumab + IPI | PD-1/PD-L1 + CTLA-4 | Melanoma | 94 | 55 | -- | -- |
| Long et al., 2018 | Nivolumab +/- IPI | PD-1/PD-L1 +/- CTLA-4 | Melanoma | 76 | 6-46 | 2.3-NR | 5.1-NR |
Abbreviations: cRR: CNS response rate; FTM: fotemustine; IPI: ipilimumab; mo: months; N: # patients; NR: not reached; OS: overall survival; PFS: progression free survival.
Anti-CTLA-4 antibody
Ipilimumab is a monoclonal antibody directed against CTLA-4, which is involved in downregulating cytotoxic T-cell production, and is approved for treatment of metastatic melanoma [84]. Systemic response rates in melanoma patients range from 11-21%, with better response reported in patients with BRAF wild-type melanoma with PD-L1 expression [85, 86]. Intracranial activity of ipilimumab was first described in a post hoc analysis of a phase III trial which included 82 patients with asymptomatic BM and found reduced mortality with the agent [87]. This was followed by an open-label phase II study of ipilimumab that included 72 patients (51 asymptomatic, 21 symptomatic) with melanoma BM [88]. Intracranial response was seen in 13 of 51 (25%) asymptomatic patients and two of 21 (10%) symptomatic patients. Median OS was 7.0 months in asymptomatic and 3.7 months in symptomatic patients. Another open-label phase II trial administered combination ipilimumab-fotemustine to patients with metastatic melanoma with and without CNS involvement (NIBIT-M1) [89]. The study included data on 20 patients with asymptomatic BM who had intracranial response rate of 10 out of 20 (50%), median OS of 12.7 months, and PFS of 3.0 months. Following the optimistic results of the phase II trial, a phase III trial comparing fotemustine versus fotemustine-ipilimumab versus ipilimumab-nivolumab in melanoma patients with BM is currently underway (NIBIT-M2, NCT02460068). In summary, the anti-CTLA-4 antibody ipilimumab has demonstrated efficacy against melanoma BM and additional data are accruing.
Anti-PD-1/PD-L1 antibodies
Nivolumab and pembrolizumab are anti-PD-1/PD-L1 antibodies which have been approved for advanced melanoma and NSCLC [7]. They have been found to be superior to ipilimumab for advanced melanoma with systemic response rates ranging from 33-57%, but these studies excluded patients with BM [85, 90]. A recently completed single-center, phase II study of pembrolizumab enrolled melanoma and NSCLC patients with newly diagnosed asymptomatic or progressing BM who did not require immediate treatment with steroids. Among the 18 NSCLC patients, intracranial response rate was six (33%, four complete and two partial), and median OS was 7.7 months [91]. In the 23 melanoma patients, intracranial response rate was six (26%, four complete and two partial), OS was 17 months, and PFS was 2 months [92]. Another multicenter phase II trial of ipilimumab-nivolumab included data on 94 patients with advanced melanoma and asymptomatic BM [93]. This study found intracranial response rate of 55% (24 complete, 28 partial responses). Finally, a multicenter, open-label, randomized phase II trial reported on 60 patients with melanoma and asymptomatic BM with no previous local therapy who received ipilimumab-nivolumab (cohort A) or nivolumab alone (cohort B) [94]. The study also included 16 patients with BM who had neurological symptoms, leptomeningeal disease, or local therapy failure and underwent therapy with nivolumab alone (cohort C). Intracranial response rates were 16 of 35 (46%) in cohort A, five of 25 (20%) in cohort B, and one of 16 (6%) in cohort C. Median OS was not yet reached in cohort A, was 18.5 months in B, and was 5.1 months in C. Median intracranial PFS was not reached in cohort A, was 2.5 months in B, and was 2.3 months in C. Overall, the anti-PD-1/PD-L1 antibodies, nivolumab and pembrolizumab, appear to be effective in treating intracranial manifestations of metastatic melanoma; pembrolizumab may also be efficacious in managing NSCLC BM.
Predicting response to immune checkpoint inhibitors
The identification of biomarkers to predict response to immune checkpoint inhibitors has been explored in recent years. Histopathological studies have demonstrated critical links between tumor-infiltrating immune cell density and distribution, PD-1 expression in immune cells, and PD-L1 expression in tumor cells with overall disease prognosis in patients with lung cancer and melanoma BM [82, 95–97]. For instance, high tumor PD-L1 expression has been widely explored as a potential predictive biomarker for selecting patients who will derive benefit from anti-PD-1/PD-L1 therapy in primary NSCLC and melanoma, but studies have not specifically focused on BM [98, 99]. Furthermore, interferon-γ is an important regulator of immunity that is produced by natural killer and activated T-cells and induces PD-L1 expression as an adaptive response to endogenous antitumor immunity in numerous primary extracranial cancer cells, as well as in multiple components of the glioma microenvironment [100, 101]. Expression of interferon-γ and interferon-γ-inducible genes correlate with response to anti-PD-1/PD-L1 agents in primary melanoma and NSCLC: patients with both interferon-γ and PD-L1-positivity (as defined by greater than 25% of tumor cells) demonstrated the highest response rates [100, 102, 103]. Additionally, high somatic mutational burden as characterized by whole-exome sequencing or various next generation sequencing panels has been correlated with sustained clinical benefit from immune checkpoint inhibitors in a growing number of extracranial cancers including melanoma, NSCLC, urothelial cancer, and head and neck squamous cell carcinoma [104–107]. Both FoundationOne CDx and MSK-IMPACT sequencing panels have been approved by the FDA for measurement of tumor mutational burden [108]. Finally, studies have suggested that activation of the Ras-MAPK pathway may be a useful biomarker for predicting response to immune checkpoint inhibitors [109–111]. In general, although these biomarkers show promise in primary NSCLC and melanoma, additional studies validating their ability to predict response to immunotherapy specifically in intracranial disease are still needed.
IMPLICATIONS FOR PRACTICE AND FUTURE DIRECTIONS
For targeted agents and immune checkpoint inhibitors, baseline MRI should be performed within a month prior to initiating treatment, followed by an image approximately every two to three months for the first year and an increasing interval thereafter. This interval has not been studied rigorously, but allows early detection of treatment failure and switching to more traditional therapies if indicated.
To assess patients receiving immunotherapy, the immunotherapy Response Assessment for Neuro-Oncology (iRANO) criteria were developed [112]. Importantly, if the contrast-enhanced MRI suggests progression within the first 6 months of treatment, there should be a confirmation image before stopping therapy. The goal of this recommendation is to allow for the possibility that significant enhancement may reflect an inflammatory response to the tumor, and an efficacious response. Waiting for this confirmatory MRI, optimally up to three months later, is dependent on the patient being clinically stable. This is a complicated point, as advancing symptoms may be secondary to a worsening brain lesion, regardless of the etiology being anti-tumor inflammation or tumor progression. Another point is that after treatment with immunotherapy, new enhancing lesions may appear as a result of anti-tumor responses against previously unknown but present lesions that were not detected on MRI. In this case, new changes on an MRI reflect response and not treatment failure. Lastly, if there has been a decrease in steroids within two weeks of MRI, the MRI-detected lesion cannot necessarily be called progressive, but rather non-evaluable. Patients with significant changes by iRANO criteria after 6 months of initiating immunotherapy are considered as no longer deriving benefit.
MRI sequences such as perfusion and cerebral blood volume are used in some centers to try to distinguish between inflammation and tumor progression, but there is little validation data published. PET/MRI is another potentially useful tool. A hypometabolic lesion on PET/MRI increases the confidence that the change is less likely tumor progression; however, there are not yet norms to define how much avidity inflammatory responses may have.
Finally, additional phase 0 trials are needed to test whether targeted systemic therapies are penetrating BM. These trials would involve upfront treatment with targeted agents followed by surgical resection and ideally both determination of drug concentration and evidence of “on-target” activity within resected tissue. Such trials could have the additional benefit of validating surrogate response biomarkers, which would optimally be less invasive than needle biopsy or surgical resection.
CONCLUSIONS
Local treatment with surgery, SRS, and WBRT remain the mainstays of therapy for BM, but emerging evidence regarding the efficacy of targeted systemic treatments and immunotherapy continues to accumulate. For NSCLC, numerous clinical trials have demonstrated CNS activity for inhibitors of EGFR and ALK. Systemic therapy using BRAF-inhibitors with and without trametinib has resulted in encouraging outcomes for patients with melanoma BM. Several targeted options are available for breast cancer BM that overexpress HER2. Immune checkpoint inhibitors including anti-CTLA-4 and anti-PD-1/PD-L1 antibodies are yielding impressive responses in melanoma and NSCLC BM. Management of eligible patients will require increased multidisciplinary discussion incorporating novel systemic treatment approaches prior or in addition to local therapy. In these cases, close follow-up with CNS imaging is necessary to evaluate response to targeted agents, with surgery or radiation as alternatives at disease progression.
Footnotes
Author contributions
R.H.H. and A.H.K. were involved in conception and design of the article. R.H.H. drafted the article. All authors critically revised and reviewed the submitted version of the manuscript. A.H.K. performed study supervision.
CONFLICTS OF INTEREST
A.H.K. received research grants from Monteris Medical and Stryker, which have no direct relation with this study. G.P.D. is a co-founder of Immunovalent, which is unrelated to this study. MGC receives royalties from UpToDate and research support from Neoimmunetech, which do not have direct relation to this study.
FUNDING
This work was in part funded by the Christopher Davidson and Knight Family Fund as well as the Duesenberg Research Fund (both to A.H.K.). This work was partly supported by National Institute of Neurological Disorders and Stroke of the National Institutes of Health (NIH) under award number R01NS107833 (M.G.C.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- 1. Chamberlain MC, Baik CS, Gadi VK, Bhatia S, Chow LQ. Systemic therapy of brain metastases: non-small cell lung cancer, breast cancer, and melanoma. Neuro Oncol. 2017; 19:i1–i24. 10.1093/neuonc/now197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS, Young B. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 1990; 322:494–500. 10.1056/NEJM199002223220802. [DOI] [PubMed] [Google Scholar]
- 3. Elder JB, Nahed BV, Linskey ME, Olson JJ. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guidelines on the Role of Emerging and Investigational Therapties for the Treatment of Adults With Metastatic Brain Tumors. Neurosurgery. 2019; 84:E201–E3. 10.1093/neuros/nyy547. [DOI] [PubMed] [Google Scholar]
- 4. Nahed BV, Alvarez-Breckenridge C, Brastianos PK, Shih H, Sloan A, Ammirati M, Kuo JS, Ryken TC, Kalkanis SN, Olson JJ. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guidelines on the Role of Surgery in the Management of Adults With Metastatic Brain Tumors. Neurosurgery. 2019; 84:E152–E5. 10.1093/neuros/nyy542. [DOI] [PubMed] [Google Scholar]
- 5. Eichler AF, Chung E, Kodack DP, Loeffler JS, Fukumura D, Jain RK. The biology of brain metastases-translation to new therapies. Nat Rev Clin Oncol. 2011; 8:344–56. 10.1038/nrclinonc.2011.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shonka N, Venur VA, Ahluwalia MS. Targeted Treatment of Brain Metastases. Curr Neurol Neurosci Rep. 2017; 17:37. 10.1007/s11910-017-0741-2. [DOI] [PubMed] [Google Scholar]
- 7. Berghoff AS, Venur VA, Preusser M, Ahluwalia MS. Immune Checkpoint Inhibitors in Brain Metastases: From Biology to Treatment. Am Soc Clin Oncol Educ Book. 2016; 35:e116–22. 10.14694/EDBK_100005. [DOI] [PubMed] [Google Scholar]
- 8. Liao BC, Lin CC, Yang JC. Second and third-generation epidermal growth factor receptor tyrosine kinase inhibitors in advanced nonsmall cell lung cancer. Curr Opin Oncol. 2015; 27:94–101. 10.1097/CCO.0000000000000164. [DOI] [PubMed] [Google Scholar]
- 9. Di Lorenzo R, Ahluwalia MS. Targeted therapy of brain metastases: latest evidence and clinical implications. Ther Adv Med Oncol. 2017; 9:781–96. 10.1177/1758834017736252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sorensen JB, Hansen HH, Hansen M, Dombernowsky P. Brain metastases in adenocarcinoma of the lung: frequency, risk groups, and prognosis. J Clin Oncol. 1988; 6:1474–80. 10.1200/JCO.1988.6.9.1474. [DOI] [PubMed] [Google Scholar]
- 11. Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol. 2004; 22:2865–72. 10.1200/JCO.2004.12.149. [DOI] [PubMed] [Google Scholar]
- 12. Sordella R, Bell DW, Haber DA, Settleman J. Gefitinib-sensitizing EGFR mutations in lung cancer activate anti-apoptotic pathways. Science. 2004; 305:1163–7. 10.1126/science.1101637. [DOI] [PubMed] [Google Scholar]
- 13. Park SJ, Kim HT, Lee DH, Kim KP, Kim SW, Suh C, Lee JS. Efficacy of epidermal growth factor receptor tyrosine kinase inhibitors for brain metastasis in non-small cell lung cancer patients harboring either exon 19 or 21 mutation. Lung Cancer. 2012; 77:556–60. 10.1016/j.lungcan.2012.05.092. [DOI] [PubMed] [Google Scholar]
- 14. Sperduto PW, Wang M, Robins HI, Schell MC, Werner-Wasik M, Komaki R, Souhami L, Buyyounouski MK, Khuntia D, Demas W, Shah SA, Nedzi LA, Perry G et al. A phase 3 trial of whole brain radiation therapy and stereotactic radiosurgery alone versus WBRT and SRS with temozolomide or erlotinib for non-small cell lung cancer and 1 to 3 brain metastases: Radiation Therapy Oncology Group 0320. Int J Radiat Oncol Biol Phys. 2013; 85:1312–8. 10.1016/j.ijrobp.2012.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kim JE, Lee DH, Choi Y, Yoon DH, Kim SW, Suh C, Lee JS. Epidermal growth factor receptor tyrosine kinase inhibitors as a first-line therapy for never-smokers with adenocarcinoma of the lung having asymptomatic synchronous brain metastasis. Lung Cancer. 2009; 65:351–4. 10.1016/j.lungcan.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 16. Iuchi T, Shingyoji M, Sakaida T, Hatano K, Nagano O, Itakura M, Kageyama H, Yokoi S, Hasegawa Y, Kawasaki K, Iizasa T. Phase II trial of gefitinib alone without radiation therapy for Japanese patients with brain metastases from EGFR-mutant lung adenocarcinoma. Lung Cancer. 2013; 82:282–7. 10.1016/j.lungcan.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 17. Lee SM, Lewanski CR, Counsell N, Ottensmeier C, Bates A, Patel N, Wadsworth C, Ngai Y, Hackshaw A, Faivre-Finn C. Randomized trial of erlotinib plus whole-brain radiotherapy for NSCLC patients with multiple brain metastases. J Natl Cancer Inst. 2014; 106:dju151. 10.1093/jnci/dju151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Raben D, Helfrich BA, Chan D, Johnson G, Bunn PA, Jr. ZD1839, a selective epidermal growth factor receptor tyrosine kinase inhibitor, alone and in combination with radiation and chemotherapy as a new therapeutic strategy in non-small cell lung cancer. Semin Oncol. 2002; 29:37–46. 10.1093/jnci/dju151. [DOI] [PubMed] [Google Scholar]
- 19. Williams KJ, Telfer BA, Stratford IJ, Wedge SR. ZD1839 (‘Iressa’), a specific oral epidermal growth factor receptor-tyrosine kinase inhibitor, potentiates radiotherapy in a human colorectal cancer xenograft model. Br J Cancer. 2002; 86:1157–61. 10.1038/sj.bjc.6600182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Welsh JW, Komaki R, Amini A, Munsell MF, Unger W, Allen PK, Chang JY, Wefel JS, McGovern SL, Garland LL, Chen SS, Holt J, Liao Z et al. Phase II trial of erlotinib plus concurrent whole-brain radiation therapy for patients with brain metastases from non-small-cell lung cancer. J Clin Oncol. 2013; 31:895–902. 10.1200/JCO.2011.40.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hoffknecht P, Tufman A, Wehler T, Pelzer T, Wiewrodt R, Schutz M, Serke M, Stohlmacher-Williams J, Marten A, Maria Huber R, Dickgreber NJ Afatinib Compassionate Use C. Efficacy of the irreversible ErbB family blocker afatinib in epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor (TKI)-pretreated non-small-cell lung cancer patients with brain metastases or leptomeningeal disease. J Thorac Oncol. 2015; 10:156–63. 10.1097/JTO.0000000000000380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Greig SL. Osimertinib: First Global Approval. Drugs. 2016; 76:263–73. 10.1007/s40265-015-0533-4. [DOI] [PubMed] [Google Scholar]
- 23. Zeng Q, Wang J, Cheng Z, Chen K, Johnstrom P, Varnas K, Li DY, Yang ZF, Zhang X. Discovery and Evaluation of Clinical Candidate AZD3759, a Potent, Oral Active, Central Nervous System-Penetrant, Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor. J Med Chem. 2015; 58:8200–15. 10.1021/acs.jmedchem.5b01073. [DOI] [PubMed] [Google Scholar]
- 24. Shaw AT, Yeap BY, Mino-Kenudson M, Digumarthy SR, Costa DB, Heist RS, Solomon B, Stubbs H, Admane S, McDermott U, Settleman J, Kobayashi S, Mark EJ et al. Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. J Clin Oncol. 2009; 27:4247–53. 10.1200/JCO.2009.22.6993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wong DW, Leung EL, So KK, Tam IY, Sihoe AD, Cheng LC, Ho KK, Au JS, Chung LP, Pik Wong M University of Hong Kong Lung Cancer Study G. The EML4-ALK fusion gene is involved in various histologic types of lung cancers from nonsmokers with wild-type EGFR and KRAS. Cancer. 2009; 115:1723–33. 10.1002/cncr.24181. [DOI] [PubMed] [Google Scholar]
- 26. Rangachari D, Yamaguchi N, VanderLaan PA, Folch E, Mahadevan A, Floyd SR, Uhlmann EJ, Wong ET, Dahlberg SE, Huberman MS, Costa DB. Brain metastases in patients with EGFR-mutated or ALK-rearranged non-small-cell lung cancers. Lung Cancer. 2015; 88:108–11. 10.1016/j.lungcan.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ricciuti B, De Giglio A, Mecca C, Arcuri C, Marini S, Metro G, Baglivo S, Sidoni A, Bellezza G, Crino L, Chiari R. Precision medicine against ALK-positive non-small cell lung cancer: beyond crizotinib. Med Oncol. 2018; 35:72. 10.1007/s12032-018-1133-4. [DOI] [PubMed] [Google Scholar]
- 28. Costa DB, Shaw AT, Ou SH, Solomon BJ, Riely GJ, Ahn MJ, Zhou C, Shreeve SM, Selaru P, Polli A, Schnell P, Wilner KD, Wiltshire R et al. Clinical Experience With Crizotinib in Patients With Advanced ALK-Rearranged Non-Small-Cell Lung Cancer and Brain Metastases. J Clin Oncol. 2015; 33:1881–8. 10.1200/JCO.2014.59.0539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chun SG, Choe KS, Iyengar P, Yordy JS, Timmerman RD. Isolated central nervous system progression on Crizotinib: an Achilles heel of non-small cell lung cancer with EML4-ALK translocation? Cancer Biol Ther. 2012; 13:1376–83. 10.4161/cbt.22255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Maillet D, Martel-Lafay I, Arpin D, Perol M. Ineffectiveness of crizotinib on brain metastases in two cases of lung adenocarcinoma with EML4-ALK rearrangement. J Thorac Oncol. 2013; 8:e30–1. 10.1097/JTO.0b013e318288dc2d. [DOI] [PubMed] [Google Scholar]
- 31. Takeda M, Okamoto I, Nakagawa K. Clinical impact of continued crizotinib administration after isolated central nervous system progression in patients with lung cancer positive for ALK rearrangement. J Thorac Oncol. 2013; 8:654–7. 10.1097/JTO.0b013e31828c28e7. [DOI] [PubMed] [Google Scholar]
- 32. Kim DW, Mehra R, Tan DSW, Felip E, Chow LQM, Camidge DR, Vansteenkiste J, Sharma S, De Pas T, Riely GJ, Solomon BJ, Wolf J, Thomas M et al. Activity and safety of ceritinib in patients with ALK-rearranged non-small-cell lung cancer (ASCEND-1): updated results from the multicentre, open-label, phase 1 trial. Lancet Oncol. 2016; 17:452–63. 10.1016/S1470-2045(15)00614-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Crino L, Ahn MJ, De Marinis F, Groen HJ, Wakelee H, Hida T, Mok T, Spigel D, Felip E, Nishio M, Scagliotti G, Branle F, Emeremni C et al. Multicenter Phase II Study of Whole-Body and Intracranial Activity With Ceritinib in Patients With ALK-Rearranged Non-Small-Cell Lung Cancer Previously Treated With Chemotherapy and Crizotinib: Results From ASCEND-2. J Clin Oncol. 2016; 34:2866–73. 10.1200/JCO.2015.65.5936. [DOI] [PubMed] [Google Scholar]
- 34. Shaw AT, Kim TM, Crino L, Gridelli C, Kiura K, Liu G, Novello S, Bearz A, Gautschi O, Mok T, Nishio M, Scagliotti G, Spigel DR et al. Ceritinib versus chemotherapy in patients with ALK-rearranged non-small-cell lung cancer previously given chemotherapy and crizotinib (ASCEND-5): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2017; 18:874–86. 10.1016/S1470-2045(17)30339-X. [DOI] [PubMed] [Google Scholar]
- 35. Soria JC, Tan DSW, Chiari R, Wu YL, Paz-Ares L, Wolf J, Geater SL, Orlov S, Cortinovis D, Yu CJ, Hochmair M, Cortot AB, Tsai CM et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study. Lancet. 2017; 389:917–29. 10.1016/S0140-6736(17)30123-X. [DOI] [PubMed] [Google Scholar]
- 36. Gadgeel SM, Gandhi L, Riely GJ, Chiappori AA, West HL, Azada MC, Morcos PN, Lee RM, Garcia L, Yu L, Boisserie F, Di Laurenzio L, Golding S et al. Safety and activity of alectinib against systemic disease and brain metastases in patients with crizotinib-resistant ALK-rearranged non-small-cell lung cancer (AF-002JG): results from the dose-finding portion of a phase 1/2 study. Lancet Oncol. 2014; 15:1119–28. 10.1016/S1470-2045(14)70362-6. [DOI] [PubMed] [Google Scholar]
- 37. Shaw AT, Gandhi L, Gadgeel S, Riely GJ, Cetnar J, West H, Camidge DR, Socinski MA, Chiappori A, Mekhail T, Chao BH, Borghaei H, Gold KA et al. Alectinib in ALK-positive, crizotinib-resistant, non-small-cell lung cancer: a single-group, multicentre, phase 2 trial. Lancet Oncol. 2016; 17:234–42. 10.1016/S1470-2045(15)00488-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ou SH, Ahn JS, De Petris L, Govindan R, Yang JC, Hughes B, Lena H, Moro-Sibilot D, Bearz A, Ramirez SV, Mekhail T, Spira A, Bordogna W et al. Alectinib in Crizotinib-Refractory ALK-Rearranged Non-Small-Cell Lung Cancer: A Phase II Global Study. J Clin Oncol. 2016; 34:661–8. 10.1200/JCO.2015.63.9443. [DOI] [PubMed] [Google Scholar]
- 39. Gadgeel SM, Shaw AT, Govindan R, Gandhi L, Socinski MA, Camidge DR, De Petris L, Kim DW, Chiappori A, Moro-Sibilot DL, Duruisseaux M, Crino L, De Pas T et al. Pooled Analysis of CNS Response to Alectinib in Two Studies of Pretreated Patients With ALK-Positive Non-Small-Cell Lung Cancer. J Clin Oncol. 2016; 34:4079–85. 10.1200/jco.2016.68.4639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Novello S, Mazieres J, Oh IJ, de Castro J, Migliorino MR, Helland A, Dziadziuszko R, Griesinger F, Kotb A, Zeaiter A, Cardona A, Balas B, Johannsdottir HK et al. Alectinib versus chemotherapy in crizotinib-pretreated anaplastic lymphoma kinase (ALK)-positive non-small-cell lung cancer: results from the phase III ALUR study. Ann Oncol. 2018; 29:1409–16. 10.1093/annonc/mdy121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Peters S, Camidge DR, Shaw AT, Gadgeel S, Ahn JS, Kim DW, Ou SI, Perol M, Dziadziuszko R, Rosell R, Zeaiter A, Mitry E, Golding S et al. Alectinib versus Crizotinib in Untreated ALK-Positive Non-Small-Cell Lung Cancer. N Engl J Med. 2017; 377:829–38. 10.1056/NEJMoa1704795. [DOI] [PubMed] [Google Scholar]
- 42. Gainor JF, Shaw AT. J-ALEX: alectinib versus crizotinib in ALK-positive lung cancer. Lancet. 2017; 390:3–4. 10.1016/s0140-6736(17)31074-7. [DOI] [PubMed] [Google Scholar]
- 43. Gadgeel S, Peters S, Mok T, Shaw AT, Kim DW, Ou SI, Perol M, Wrona A, Novello S, Rosell R, Zeaiter A, Liu T, Nuesch E et al. Alectinib versus crizotinib in treatment-naive anaplastic lymphoma kinase-positive (ALK+) non-small-cell lung cancer: CNS efficacy results from the ALEX study. Ann Oncol. 2018; 29:2214–22. 10.1093/annonc/mdy405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Camidge DR, Kim DW, Tiseo M, Langer CJ, Ahn MJ, Shaw AT, Huber RM, Hochmair MJ, Lee DH, Bazhenova LA, Gold KA, Ou SI, West HL et al. Exploratory Analysis of Brigatinib Activity in Patients With Anaplastic Lymphoma Kinase-Positive Non-Small-Cell Lung Cancer and Brain Metastases in Two Clinical Trials. J Clin Oncol. 2018; 36:2693–701. 10.1200/jco.2017.77.5841. [DOI] [PubMed] [Google Scholar]
- 45. Camidge DR, Kim HR, Ahn MJ, Yang JC, Han JY, Lee JS, Hochmair MJ, Li JY, Chang GC, Lee KH, Gridelli C, Delmonte A, Garcia Campelo R et al. Brigatinib versus Crizotinib in ALK-Positive Non-Small-Cell Lung Cancer. N Engl J Med. 2018; 379:2027–39. 10.1056/NEJMoa1810171. [DOI] [PubMed] [Google Scholar]
- 46. Shaw AT, Felip E, Bauer TM, Besse B, Navarro A, Postel-Vinay S, Gainor JF, Johnson M, Dietrich J, James LP, Clancy JS, Chen J, Martini JF et al. Lorlatinib in non-small-cell lung cancer with ALK or ROS1 rearrangement: an international, multicentre, open-label, single-arm first-in-man phase 1 trial. Lancet Oncol. 2017; 18:1590–9. 10.1016/s1470-2045(17)30680-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Solomon BJ, Besse B, Bauer TM, Felip E, Soo RA, Camidge DR, Chiari R, Bearz A, Lin CC, Gadgeel SM, Riely GJ, Tan EH, Seto T et al. Lorlatinib in patients with ALK-positive non-small-cell lung cancer: results from a global phase 2 study. Lancet Oncol. 2018; 19:1654–67. 10.1016/s1470-2045(18)30649-1. [DOI] [PubMed] [Google Scholar]
- 48. Davies MA. Targeted therapy for brain metastases. Adv Pharmacol. 2012; 65:109–42. 10.1016/B978-0-12-397927-8.00005-1. [DOI] [PubMed] [Google Scholar]
- 49. Bedikian AY, Wei C, Detry M, Kim KB, Papadopoulos NE, Hwu WJ, Homsi J, Davies M, McIntyre S, Hwu P. Predictive factors for the development of brain metastasis in advanced unresectable metastatic melanoma. Am J Clin Oncol. 2011; 34:603–10. 10.1097/COC.0b013e3181f9456a. [DOI] [PubMed] [Google Scholar]
- 50. Fife KM, Colman MH, Stevens GN, Firth IC, Moon D, Shannon KF, Harman R, Petersen-Schaefer K, Zacest AC, Besser M, Milton GW, McCarthy WH, Thompson JF. Determinants of outcome in melanoma patients with cerebral metastases. J Clin Oncol. 2004; 22:1293–300. 10.1200/JCO.2004.08.140. [DOI] [PubMed] [Google Scholar]
- 51. Young GJ, Bi WL, Wu WW, Johanns TM, Dunn GP, Dunn IF. Management of intracranial melanomas in the era of precision medicine. Oncotarget. 2017; 8:89326–47. 10.18632/oncotarget.19223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ramanujam S, Schadendorf D, Long GV. Systemic therapies for melanoma brain metastases: which drug for whom and when? Chin Clin Oncol. 2015; 4:25. 10.3978/j.issn.2304-3865.2015.06.06. [DOI] [PubMed] [Google Scholar]
- 53. Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, Davis N, Dicks E, Ewing R et al. Mutations of the BRAF gene in human cancer. Nature. 2002; 417:949–54. 10.1038/nature00766. [DOI] [PubMed] [Google Scholar]
- 54. Jakob JA, Bassett RL, Jr. , Ng CS, Curry JL, Joseph RW, Alvarado GC, Rohlfs ML, Richard J, Gershenwald JE, Kim KB, Lazar AJ, Hwu P, Davies MA. NRAS mutation status is an independent prognostic factor in metastatic melanoma. Cancer. 2012; 118:4014–23. 10.1002/cncr.26724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Dummer R, Goldinger SM, Turtschi CP, Eggmann NB, Michielin O, Mitchell L, Veronese L, Hilfiker PR, Felderer L, Rinderknecht JD. Vemurafenib in patients with BRAF(V600) mutation-positive melanoma with symptomatic brain metastases: final results of an open-label pilot study. Eur J Cancer. 2014; 50:611–21. 10.1016/j.ejca.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 56. McArthur GA, Maio M, Arance A, Nathan P, Blank C, Avril MF, Garbe C, Hauschild A, Schadendorf D, Hamid O, Fluck M, Thebeau M, Schachter J et al. Vemurafenib in metastatic melanoma patients with brain metastases: an open-label, single-arm, phase 2, multicentre study. Ann Oncol. 2017; 28:634–41. 10.1093/annonc/mdw641. [DOI] [PubMed] [Google Scholar]
- 57. Falchook GS, Long GV, Kurzrock R, Kim KB, Arkenau TH, Brown MP, Hamid O, Infante JR, Millward M, Pavlick AC, O'Day SJ, Blackman SC, Curtis CM et al. Dabrafenib in patients with melanoma, untreated brain metastases, and other solid tumours: a phase 1 dose-escalation trial. Lancet. 2012; 379:1893–901. 10.1016/S0140-6736(12)60398-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Long GV, Trefzer U, Davies MA, Kefford RF, Ascierto PA, Chapman PB, Puzanov I, Hauschild A, Robert C, Algazi A, Mortier L, Tawbi H, Wilhelm T et al. Dabrafenib in patients with Val600Glu or Val600Lys BRAF-mutant melanoma metastatic to the brain (BREAK-MB): a multicentre, open-label, phase 2 trial. Lancet Oncol. 2012; 13:1087–95. 10.1016/S1470-2045(12)70431-X. [DOI] [PubMed] [Google Scholar]
- 59. Solit DB, Rosen N. Resistance to BRAF inhibition in melanomas. N Engl J Med. 2011; 364:772–4. 10.1056/NEJMcibr1013704. [DOI] [PubMed] [Google Scholar]
- 60. Su F, Viros A, Milagre C, Trunzer K, Bollag G, Spleiss O, Reis-Filho JS, Kong X, Koya RC, Flaherty KT, Chapman PB, Kim MJ, Hayward R et al. RAS mutations in cutaneous squamous-cell carcinomas in patients treated with BRAF inhibitors. N Engl J Med. 2012; 366:207–15. 10.1056/NEJMoa1105358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Oberholzer PA, Kee D, Dziunycz P, Sucker A, Kamsukom N, Jones R, Roden C, Chalk CJ, Ardlie K, Palescandolo E, Piris A, MacConaill LE, Robert C et al. RAS mutations are associated with the development of cutaneous squamous cell tumors in patients treated with RAF inhibitors. J Clin Oncol. 2012; 30:316–21. 10.1200/JCO.2011.36.7680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Shi H, Hugo W, Kong X, Hong A, Koya RC, Moriceau G, Chodon T, Guo R, Johnson DB, Dahlman KB, Kelley MC, Kefford RF, Chmielowski B et al. Acquired resistance and clonal evolution in melanoma during BRAF inhibitor therapy. Cancer Discov. 2014; 4:80–93. 10.1158/2159-8290.CD-13-0642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Robert C, Karaszewska B, Schachter J, Rutkowski P, Mackiewicz A, Stroiakovski D, Lichinitser M, Dummer R, Grange F, Mortier L, Chiarion-Sileni V, Drucis K, Krajsova I et al. Improved overall survival in melanoma with combined dabrafenib and trametinib. N Engl J Med. 2015; 372:30–9. 10.1056/NEJMoa1412690. [DOI] [PubMed] [Google Scholar]
- 64. Davies MA, Saiag P, Robert C, Grob JJ, Flaherty KT, Arance A, Chiarion-Sileni V, Thomas L, Lesimple T, Mortier L, Moschos SJ, Hogg D, Marquez-Rodas I et al. Dabrafenib plus trametinib in patients with BRAF(V600)-mutant melanoma brain metastases (COMBI-MB): a multicentre, multicohort, open-label, phase 2 trial. Lancet Oncol. 2017; 18:863–73. 10.1016/S1470-2045(17)30429-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Chang EL, Lo S. Diagnosis and management of central nervous system metastases from breast cancer. Oncologist. 2003; 8:398–410. 10.1634/theoncologist.8-5-398. [DOI] [PubMed] [Google Scholar]
- 66. Lassman AB, DeAngelis LM. Brain metastases. Neurol Clin. 2003; 21:1–23. vii. 10.1016/S0733-8619(02)00035-X. [DOI] [PubMed] [Google Scholar]
- 67. Harbeck N, Luftner D, Marschner N, Untch M, Augustin D, Briest S, Ettl J, Haidinger R, Muller L, Muller V, Ruckhaberle E, Wuerstlein R, Thomssen C. ABC4 Consensus: Assessment by a German Group of Experts. Breast Care (Basel). 2018; 13:48–58. 10.1159/000486722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Venur VA, Leone JP. Targeted Therapies for Brain Metastases from Breast Cancer. Int J Mol Sci. 2016; 17:1543. 10.3390/ijms17091543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Gianni L, Eiermann W, Semiglazov V, Lluch A, Tjulandin S, Zambetti M, Moliterni A, Vazquez F, Byakhov MJ, Lichinitser M, Climent MA, Ciruelos E, Ojeda B et al. Neoadjuvant and adjuvant trastuzumab in patients with HER2-positive locally advanced breast cancer (NOAH): follow-up of a randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet Oncol. 2014; 15:640–7. 10.1016/S1470-2045(14)70080-4. [DOI] [PubMed] [Google Scholar]
- 70. Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE, Jr. Davidson NE, Tan-Chiu E, Martino S, Paik S, Kaufman PA, Swain SM, Pisansky TM, Fehrenbacher L et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005; 353:1673–84. 10.1056/NEJMoa052122. [DOI] [PubMed] [Google Scholar]
- 71. Piccart-Gebhart MJ, Procter M, Leyland-Jones B, Goldhirsch A, Untch M, Smith I, Gianni L, Baselga J, Bell R, Jackisch C, Cameron D, Dowsett M, Barrios CH et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med. 2005; 353:1659–72. 10.1056/NEJMoa052306. [DOI] [PubMed] [Google Scholar]
- 72. Kurihara H, Hamada A, Yoshida M, Shimma S, Hashimoto J, Yonemori K, Tani H, Miyakita Y, Kanayama Y, Wada Y, Kodaira M, Yunokawa M, Yamamoto H et al. (64)Cu-DOTA-trastuzumab PET imaging and HER2 specificity of brain metastases in HER2-positive breast cancer patients. EJNMMI Res. 2015; 5:8. 10.1186/s13550-015-0082-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Bartsch R, Rottenfusser A, Wenzel C, Dieckmann K, Pluschnig U, Altorjai G, Rudas M, Mader RM, Poetter R, Zielinski CC, Steger GG. Trastuzumab prolongs overall survival in patients with brain metastases from Her2 positive breast cancer. J Neurooncol. 2007; 85:311–7. 10.1007/s11060-007-9420-5. [DOI] [PubMed] [Google Scholar]
- 74. Medina PJ, Goodin S. Lapatinib: a dual inhibitor of human epidermal growth factor receptor tyrosine kinases. Clin Ther. 2008; 30:1426–47. 10.1016/j.clinthera.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 75. Lin NU, Dieras V, Paul D, Lossignol D, Christodoulou C, Stemmler HJ, Roche H, Liu MC, Greil R, Ciruelos E, Loibl S, Gori S, Wardley A et al. Multicenter phase II study of lapatinib in patients with brain metastases from HER2-positive breast cancer. Clin Cancer Res. 2009; 15:1452–9. 10.1158/1078-0432.CCR-08-1080. [DOI] [PubMed] [Google Scholar]
- 76. Bachelot T, Romieu G, Campone M, Dieras V, Cropet C, Dalenc F, Jimenez M, Le Rhun E, Pierga JY, Goncalves A, Leheurteur M, Domont J, Gutierrez M et al. Lapatinib plus capecitabine in patients with previously untreated brain metastases from HER2-positive metastatic breast cancer (LANDSCAPE): a single-group phase 2 study. Lancet Oncol. 2013; 14:64–71. 10.1016/S1470-2045(12)70432-1. [DOI] [PubMed] [Google Scholar]
- 77. Cortés J, Dieras V, Ro J, Barriere J, Bachelot T, Hurvitz S, Le Rhun E, Espié M, Kim SB, Schneeweiss A, Sohn JH, Nabholtz J-M, Kellokumpu-Lehtinen PL et al. Afatinib alone or afatinib plus vinorelbine versus investigator's choice of treatment for HER2-positive breast cancer with progressive brain metastases after trastuzumab, lapatinib, or both (LUX-Breast 3): a randomised, open-label, multicentre, phase 2 trial. Lancet Oncology. 2015; 16:1700–10. 10.1016/s1470-2045(15)00373-3. [DOI] [PubMed] [Google Scholar]
- 78. Freedman RA, Gelman RS, Anders CK, Melisko ME, Parsons HA, Cropp AM, Silvestri K, Cotter CM, Componeschi KP, Marte JM, Connolly RM, Moy B, Van Poznak CH et al. TBCRC 022: A Phase II Trial of Neratinib and Capecitabine for Patients With Human Epidermal Growth Factor Receptor 2-Positive Breast Cancer and Brain Metastases. J Clin Oncol. 2019; 37:1081–89. 10.1200/JCO.18.01511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Verma S, Miles D, Gianni L, Krop IE, Welslau M, Baselga J, Pegram M, Oh DY, Dieras V, Guardino E, Fang L, Lu MW, Olsen S et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012; 367:1783–91. 10.1056/NEJMoa1209124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Krop IE, Lin NU, Blackwell K, Guardino E, Huober J, Lu M, Miles D, Samant M, Welslau M, Dieras V. Trastuzumab emtansine (T-DM1) versus lapatinib plus capecitabine in patients with HER2-positive metastatic breast cancer and central nervous system metastases: a retrospective, exploratory analysis in EMILIA. Ann Oncol. 2015; 26:113–9. 10.1093/annonc/mdu486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Bartsch R, Berghoff AS, Vogl U, Rudas M, Bergen E, Dubsky P, Dieckmann K, Pinker K, Bago-Horvath Z, Galid A, Oehler L, Zielinski CC, Gnant M et al. Activity of T-DM1 in Her2-positive breast cancer brain metastases. Clin Exp Metastasis. 2015; 32:729–37. 10.1007/s10585-015-9740-3. [DOI] [PubMed] [Google Scholar]
- 82. Berghoff AS, Preusser M. The inflammatory microenvironment in brain metastases: potential treatment target? Chin Clin Oncol. 2015; 4:21. 10.3978/j.issn.2304-3865.2015.06.03. [DOI] [PubMed] [Google Scholar]
- 83. O'Kane GM, Leighl NB. Systemic Therapy of Lung Cancer CNS Metastases Using Molecularly Targeted Agents and Immune Checkpoint Inhibitors. CNS Drugs. 2018; 32:527–42. 10.1007/s40263-018-0526-4. [DOI] [PubMed] [Google Scholar]
- 84. Weber J. Review: anti-CTLA-4 antibody ipilimumab: case studies of clinical response and immune-related adverse events. Oncologist. 2007; 12:864–72. 10.1634/theoncologist.12-7-864. [DOI] [PubMed] [Google Scholar]
- 85. Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Cowey CL, Lao CD, Schadendorf D, Dummer R, Smylie M, Rutkowski P, Ferrucci PF, Hill A, Wagstaff J et al. Combined Nivolumab and Ipilimumab or Monotherapy in Untreated Melanoma. N Engl J Med. 2015; 373:23–34. 10.1056/NEJMoa1504030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Postow MA, Chesney J, Pavlick AC, Robert C, Grossmann K, McDermott D, Linette GP, Meyer N, Giguere JK, Agarwala SS, Shaheen M, Ernstoff MS, Minor D et al. Nivolumab and ipilimumab versus ipilimumab in untreated melanoma. N Engl J Med. 2015; 372:2006–17. 10.1056/NEJMoa1414428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Hodi FS, O'Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, Akerley W, van den Eertwegh AJ, Lutzky J et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010; 363:711–23. 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Margolin K, Ernstoff MS, Hamid O, Lawrence D, McDermott D, Puzanov I, Wolchok JD, Clark JI, Sznol M, Logan TF, Richards J, Michener T, Balogh A et al. Ipilimumab in patients with melanoma and brain metastases: an open-label, phase 2 trial. Lancet Oncol. 2012; 13: 459–65. 10.1016/S1470-2045(12)70090-6. [DOI] [PubMed] [Google Scholar]
- 89. Di Giacomo AM, Ascierto PA, Pilla L, Santinami M, Ferrucci PF, Giannarelli D, Marasco A, Rivoltini L, Simeone E, Nicoletti SVL, Fonsatti E, Annesi D, Queirolo P et al. Ipilimumab and fotemustine in patients with advanced melanoma (NIBIT-M1): an open-label, single-arm phase 2 trial. Lancet Oncol. 2012; 13:879–86. 10.1016/S1470-2045(12)70324-8. [DOI] [PubMed] [Google Scholar]
- 90. Schachter J, Ribas A, Long GV, Arance A, Grob JJ, Mortier L, Daud A, Carlino MS, McNeil C, Lotem M, Larkin J, Lorigan P, Neyns B et al. Pembrolizumab versus ipilimumab for advanced melanoma: final overall survival results of a multicentre, randomised, open-label phase 3 study (KEYNOTE-006). Lancet. 2017; 390: 1853–62. 10.1016/S0140-6736(17)31601-X. [DOI] [PubMed] [Google Scholar]
- 91. Goldberg SB, Gettinger SN, Mahajan A, Chiang AC, Herbst RS, Sznol M, Tsiouris AJ, Cohen J, Vortmeyer A, Jilaveanu L, Yu J, Hegde U, Speaker S et al. Pembrolizumab for patients with melanoma or non-small-cell lung cancer and untreated brain metastases: early analysis of a non-randomised, open-label, phase 2 trial. Lancet Oncol. 2016; 17:976–83. 10.1016/S1470-2045(16)30053-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Kluger HM, Chiang V, Mahajan A, Zito CR, Sznol M, Tran T, Weiss SA, Cohen JV, Yu J, Hegde U, Perrotti E, Anderson G, Ralabate A et al. Long-Term Survival of Patients With Melanoma With Active Brain Metastases Treated With Pembrolizumab on a Phase II Trial. Journal of Clinical Oncology. 2019; 37:52. 10.1200/Jco.18.00204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Tawbi HA, Forsyth PA, Algazi A, Hamid O, Hodi FS, Moschos SJ, Khushalani NI, Lewis K, Lao CD, Postow MA, Atkins MB, Ernstoff MS, Reardon DA et al. Combined Nivolumab and Ipilimumab in Melanoma Metastatic to the Brain. N Engl J Med. 2018; 379:722–30. 10.1056/NEJMoa1805453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Long GV, Atkinson V, Lo S, Sandhu S, Guminski AD, Brown MP, Wilmott JS, Edwards J, Gonzalez M, Scolyer RA, Menzies AM, McArthur GA. Combination nivolumab and ipilimumab or nivolumab alone in melanoma brain metastases: a multicentre randomised phase 2 study. Lancet Oncol. 2018; 19:672–81. 10.1016/S1470-2045(18)30139-6. [DOI] [PubMed] [Google Scholar]
- 95. Teglasi V, Reiniger L, Fabian K, Pipek O, Csala I, Bago AG, Varallyai P, Vizkeleti L, Rojko L, Timar J, Dome B, Szallasi Z, Swanton C et al. Evaluating the significance of density, localization, and PD-1/PD-L1 immunopositivity of mononuclear cells in the clinical course of lung adenocarcinoma patients with brain metastasis. Neuro Oncol. 2017; 19:1058–67. 10.1093/neuonc/now309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Harter PN, Bernatz S, Scholz A, Zeiner PS, Zinke J, Kiyose M, Blasel S, Beschorner R, Senft C, Bender B, Ronellenfitsch MW, Wikman H, Glatzel M et al. Distribution and prognostic relevance of tumor-infiltrating lymphocytes (TILs) and PD-1/PD-L1 immune checkpoints in human brain metastases. Oncotarget. 2015; 6:40836–49. 10.18632/oncotarget.5696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Berghoff AS, Ricken G, Widhalm G, Rajky O, Dieckmann K, Birner P, Bartsch R, Holler C, Preusser M. Tumour-infiltrating lymphocytes and expression of programmed death ligand 1 (PD-L1) in melanoma brain metastases. Histopathology. 2015; 66:289–99. 10.1111/his.12537. [DOI] [PubMed] [Google Scholar]
- 98. Brody R, Zhang Y, Ballas M, Siddiqui MK, Gupta P, Barker C, Midha A, Walker J. PD-L1 expression in advanced NSCLC: Insights into risk stratification and treatment selection from a systematic literature review. Lung Cancer. 2017; 112:200–15. 10.1016/j.lungcan.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 99. Meng X, Huang Z, Teng F, Xing L, Yu J. Predictive biomarkers in PD-1/PD-L1 checkpoint blockade immunotherapy. Cancer Treat Rev. 2015; 41:868–76. 10.1016/j.ctrv.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 100. Shukuya T, Carbone DP. Predictive Markers for the Efficacy of Anti-PD-1/PD-L1 Antibodies in Lung Cancer. J Thorac Oncol. 2016; 11:976–88. 10.1016/j.jtho.2016.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Qian J, Wang C, Wang B, Yang J, Wang Y, Luo F, Xu J, Zhao C, Liu R, Chu Y. The IFN-gamma/PD-L1 axis between T cells and tumor microenvironment: hints for glioma anti-PD-1/PD-L1 therapy. J Neuroinflammation. 2018; 15:290. 10.1186/s12974-018-1330-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Herbst RS, Soria JC, Kowanetz M, Fine GD, Hamid O, Gordon MS, Sosman JA, McDermott DF, Powderly JD, Gettinger SN, Kohrt HE, Horn L, Lawrence DP et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014; 515:563–7. 10.1038/nature14011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Gibney GT, Weiner LM, Atkins MB. Predictive biomarkers for checkpoint inhibitor-based immunotherapy. Lancet Oncol. 2016; 17:e542–e51. 10.1016/S1470-2045(16)30406-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Snyder A, Makarov V, Merghoub T, Yuan J, Zaretsky JM, Desrichard A, Walsh LA, Postow MA, Wong P, Ho TS, Hollmann TJ, Bruggeman C, Kannan K et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med. 2014; 371:2189–99. 10.1056/NEJMoa1406498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, Lee W, Yuan J, Wong P, Ho TS, Miller ML, Rekhtman N, Moreira AL et al. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015; 348:124–8. 10.1126/science.aaa1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Boussiotis VA. Somatic mutations and immunotherapy outcome with CTLA-4 blockade in melanoma. N Engl J Med. 2014; 371:2230–2. 10.1056/NEJMe1413061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Chan TA, Yarchoan M, Jaffee E, Swanton C, Quezada SA, Stenzinger A, Peters S. Development of tumor mutation burden as an immunotherapy biomarker: utility for the oncology clinic. Ann Oncol. 2019; 30:44–56. 10.1093/annonc/mdy495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Allegretti M, Fabi A, Buglioni S, Martayan A, Conti L, Pescarmona E, Ciliberto G, Giacomini P. Tearing down the walls: FDA approves next generation sequencing (NGS) assays for actionable cancer genomic aberrations. J Exp Clin Cancer Res. 2018; 37:47. 10.1186/s13046-018-0702-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Loi S, Dushyanthen S, Beavis PA, Salgado R, Denkert C, Savas P, Combs S, Rimm DL, Giltnane JM, Estrada MV, Sanchez V, Sanders ME, Cook RS et al. RAS/MAPK Activation Is Associated with Reduced Tumor-Infiltrating Lymphocytes in Triple-Negative Breast Cancer: Therapeutic Cooperation Between MEK and PD-1/PD-L1 Immune Checkpoint Inhibitors. Clin Cancer Res. 2016; 22:1499–509. 10.1158/1078-0432.CCR-15-1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Hu-Lieskovan S, Mok S, Homet Moreno B, Tsoi J, Robert L, Goedert L, Pinheiro EM, Koya RC, Graeber TG, Comin-Anduix B, Ribas A. Improved antitumor activity of immunotherapy with BRAF and MEK inhibitors in BRAF(V600E) melanoma. Sci Transl Med. 2015; 7:279ra41. 10.1126/scitranslmed.aaa4691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Kakavand H, Wilmott JS, Menzies AM, Vilain R, Haydu LE, Yearley JH, Thompson JF, Kefford RF, Hersey P, Long GV, Scolyer RA. PD-L1 Expression and Tumor-Infiltrating Lymphocytes Define Different Subsets of MAPK Inhibitor-Treated Melanoma Patients. Clin Cancer Res. 2015; 21:3140–8. 10.1158/1078-0432.CCR-14-2023. [DOI] [PubMed] [Google Scholar]
- 112. Okada H, Weller M, Huang R, Finocchiaro G, Gilbert MR, Wick W, Ellingson BM, Hashimoto N, Pollack IF, Brandes AA, Franceschi E, Herold-Mende C, Nayak L et al. Immunotherapy response assessment in neuro-oncology: a report of the RANO working group. Lancet Oncol. 2015; 16:e534–e42. 10.1016/S1470-2045(15)00088-1. [DOI] [PMC free article] [PubMed] [Google Scholar]