Abstract
Background:
While growing literature is stressing the link between Autistic Traits (AT) and trauma-/stress-related disorders, in both conditions significant differences have been separately reported.
Objective:
This study aims to evaluate the relationship between AT and trauma-/stress-related symptoms with respect to sex.
Methods:
178 university students were assessed with the Structured Clinical Interview for DSM-5, the Trauma and Loss Spectrum (TALS) and the Adult Autism Subthreshold Spectrum (AdAS). In order to evaluate sex differences in trauma-/stress-related symptoms among subjects with higher or lower AT, the sample was split in two groups with an equal number of subjects on the basis of the median score reported on AdAS Spectrum (“AdAS high scorers” and “AdAS low scorers”).
Results:
Females reported significantly higher TALS total score, Loss events and Grief reaction domain scores than males in the whole sample, while AdAS high scorers reported significantly higher TALS total and domain scores than AdAS low scorers. A significant interaction between high/low AdAS score and sex emerged for TALS domains, with females scoring significantly higher than males only among AdAS low scorers, specifically on Loss events, Grief reaction, Re-experiencing and Personal characteristics/Risk factors domains. Finally, among AdAS high scorers a significantly higher rate of subjects fulfilled symptomatological criteria for PTSD than among AdAS low scorers, without sex differences.
Conclusion:
Our results confirm a significant relationship between AT and trauma-/stress-related symptoms, which seems to prevail on sex differences among high-risk subjects.
Keywords: Autism spectrum, PTSD, Subthreshold traits, AdAS, Sex, Student population, Vulnerability factors
1. INTRODUCTION
Autism Spectrum Disorder (ASD) is a neurodevelopmental condition characterized by persistent deficits in social communication and interactions, in association with narrow interests and repetitive behaviors [1]. A strong genetic component has been recognized in ASD, and generally, the disorder comes to clinical attention during childhood [2, 3]. However, recently an increasing number of studies is focusing on mild forms of ASD, or even on sub-threshold Autistic Traits (AT), which do not properly fulfill the Diagnostic and Statistical Manual of Mental Disorder (DSM) criteria: while milder forms of ASD may come to clinical attention only in adulthood, when patients develop other disorders in comorbidity, AT may remain entirely undiagnosed during lifetime [4-6]. AT can be usually found among first-degree relatives of ASD probands, where they are known with the label of “broad autism phenotype” [7-9], but they may also be found in some high-risk groups from the general population, such as university students, and in particular those enrolled in high-ranking universities [10-18]. The importance of AT lies in the fact that they seem to play a pivotal role as a vulnerability factor towards the development of several kinds of psychiatric disorders [19-24]. In the last few years, a growing body of evidence has reported significant rates of comorbidity between milder forms of ASD (or AT) and other psychiatric disorders, such as personality disorders as well as anxiety, mood and stress-related disorders [18, 25-29]. In this framework, it is noteworthy that to date, scant literature has paid specific attention to investigate the relationship between ASD, AT, and the spectrum of post-traumatic symptomatology. While Mehtar and Mukaddes [30] stressed a high Prevalence of Post-traumatic Stress Disorder (PTSD) in children with ASD (around 67%), Storch et al. [31] found that suicidal thoughts and behaviors were frequent in young adults with ASD, and related to the presence of depression and PTSD, suggesting that these patients may be considered as a low-resilience group with a higher vulnerability for developing trauma and stress-related disorders. However, other studies showed lower rates of comorbidity between PTSD and ASD [32]. Some authors suggested that the inconsistencies reported about the association between full-blown ASD and PTSD may be explained considering that ASD patients are frequently unable to properly report traumatic events, due to their difficulties in mentalization of traumatic contents and processing stressful situations [32-34]. Kato and colleagues [35] also detected a higher prevalence (70%) of adjustment disorders in ASD patients who attempted suicide, assuming that not only mood disorders but also adjustment disorders may be associated with higher suicidal risk in these subjects. Other authors, comparing ASD patients who have been exposed to a natural disaster with an unexposed group with ASD, reported a significant worsening of adaptive functioning in exposed subjects [36]. Some literature stressed the presence of a consistent association also between PTSD or adjustment disorders and AT [35, 37]. Recently, Dell’Osso et al. [38] reported a significant correlation between the autism dimension of ruminative thinking and post-traumatic symptomatology such as re-experiencing and arousal in a sample of fathers of children with epilepsy. As suggested by previous studies, among subjects with ASD or AT the difficulties in externalizing emotions, eventually seeking for help, as well as the deficits in adjusting to stressful events of daily life, may result in an inability to successfully cope not only with major traumatic events, but even to milder events, developing post-traumatic symptoms. This hypothesis is in line with the PTSD Complex (cPTSD) model [39-42]. cPTSD is defined as a syndrome that can be detected even in response to mild and repeated stressful experiences, especially in high-risk subjects [39-43], and it is characterized by a higher tendency to chronicity, typically featuring dissociative symptoms, maladaptive behaviors, emotional dysregulation, negative self-perception [33, 44, 45]. What is noteworthy of this model is how it describes the possibility of developing, especially for high-risk subjects, a chronic form of PTSD, with a greater prevalence of maladaptive symptoms and emotional dysregulation. Thus a specific subset of PTSD may be developed in response to events of a lower traumatic impact than those described in DSM-5 criterion A, but repeated and prolonged in time. In this framework, it is also noteworthy that, while ASD is a diagnosis with a higher prevalence among males [46, 47], results from literature generally show higher PTSD rates in women compared to men [48-51]. It should be noted that an increasing number of studies is stressing the necessity to pay more attention to female presentations of autism spectrum, which may be significantly different to those typically reported among males, remaining consequently undiagnosed, especially when hidden by other disorders in comorbidity, including stress-related disorders [6, 47, 52, 53]. In the light of reported data, the present study aims to investigate sex differences in the relationship between post-traumatic stress symptoms and autism spectrum in a sample of university students from high-ranking universities. We chose this specific population because, as reported above, it is considered a high-risk group for AT. Moreover, university students generally show also a higher prevalence of social anxiety, a condition frequently associated with substance abuse and AT: social anxiety is hypothesized to mask autism spectrum symptoms among females [43, 54-61]. University students usually face higher levels of stress [62]. In particular, we aim to evaluate in this population the possible effect of AT on the expression of trauma/stress-related symptoms, with a specific focus on sex differences. In this regard, we aim to evaluate also whether the role of sex in the expression of trauma- and stress-related symptoms may be different in subjects with lower or higher AT. We hypothesized to find a significant relationship between the presence of AT and post-traumatic spectrum, as well as significant interactions between the presence of AT and sex concerning the expression of post-traumatic symptoms.
2. MATERIALS AND METHODS
We enrolled 178 students from three Italian universities of excellence (the “Scuola Superiore di Catania” of Catania, the “Collegio Universitario di Merito” of Pavia and the “Scuola Superiore Sant'Anna” of Pisa), which are characterized by advanced training programs and highly selective admission exams. All the subjects have been evaluated by the Structured Clinical Interview for DSM-5 (SCID-5) [63] to assess the presence of psychiatric disorders according to DSM-5 criteria. Subsequently, they have been assessed with the Trauma and Loss Spectrum, Self-report version (TALS-SR) and with the Adult Autism Subthreshold Spectrum (AdAS Spectrum). The study was conducted by the Declaration of Helsinki. The Ethics Committee of the Azienda Ospedaliero-Universitaria of Pisa approved all recruitment and assessment procedures. All participants provided written informed consent after having received a clear description of the study and having the opportunity to ask questions. According to the aims of the study, in order to evaluate the presence of sex differences in trauma- and stress-related symptoms among subjects with higher or lower AT, we split the sample into two groups with the same number of subjects on the basis of the median score reported on AdAS Spectrum total score (high scorers above 48.5 and low scorers below 48.5) naming the new dichotomous variable that identifies the two groups “totAdAS”.
2.1. Measures
The Adult Autism Subthreshold Spectrum (AdAS Spectrum): The AdAS Spectrum is an instrument developed by Dell'Osso et al. [47] to evaluate the presence of the broad spectrum of full-threshold and sub-threshold ASD sympto- matology in adults with average intelligence and without language impairment. Specific attention has been paid to include items to detect also atypical and sex-specific autism spectrum phenotypes. The questionnaire consists of seven domains, yielding a total of 160 dichotomous items. The AdAS Spectrum demonstrated a Kuder-Richardson's coefficient of 0.964, and it also showed a high correlation with other instruments commonly employed for assessing autism spectrum: the Autism Spectrum Quotient (Pearson's r correlation=0.77) and the Ritvo Autism and Asperger Diagnostic Scale 14-item version (Pearson's r correlation 0.83).
The Trauma and Loss Spectrum (TALS-SR): The TALS-SR is an instrument developed to evaluate a broad dimension of stress-, loss-, and trauma-related symptoms [64, 65]. It is composed of 116 dichotomous items divided into nine domains. The instrument has been tailored to assess not only full-blown manifestations but also sub-threshold symptoms, atypical, and associated features of both peritraumatic and post-traumatic reactions. Moreover, the TALS-SR evaluates also the impact of loss events and milder stressful events across a lifetime. The questionnaire demonstrated Kuder-Richardson coefficients above 0.50 and positive correlations between the domains (Pearson's r correlation coefficients ranging from 0.46 to 0.76) [64, 65].
2.2. Statistical Analyses
We used t-tests for independent samples to compare AdAS Spectrum total and domain scores observed in males and females within the two groups. We used a two-way ANOVA to study the effect of totAdAS and sex and their possible interaction on TALS-SR total score, while we utilized a two-way MANOVA to study the effect of totAdAS and sex on TALS-SR domain scores, which are strongly correlated each other.
Finally, we used a Classification Tree Analysis with the Chi-squared Automated Interaction Detection (CHAID) growing method to study how totAdAS and sex can interact each other in predicting the endorsement of all PTSD symptomatological criteria (criteria B-E). This analysis is indeed a powerful tool to study how to split the effect and to locate the most robust interaction with the dependent variable. Classification tree analysis is represented graphically as an inverted tree. Beginning with a root node, which includes all cases, the tree grows iteratively by identifying the critical discriminating variables in the predictor set. At each step, CHAID chooses the independent variable that has the strongest relationship with the dependent variable. Categories of each predictor merge if they are not significantly different concerning the dependent variable.
All statistical analyses were performed with SPSS, version 24 [66].
3. RESULTS
Socio-demographic characteristics of the sample, as well as psychiatric comorbidities, according to SCID-5, are reported elsewhere [18]. The sample was composed of 178 subjects: 89 AdAS Spectrum high scorers (40 females, 49 males), 89 AdAS Spectrum low scorers (45 females, 44 males). Considering the AdAS Spectrum domains, the highest percentage mean scores were found for the domains Restricted interests and rumination (39.25±19.63) and Non-verbal communication (36.20±17.02), followed by Childhood/adolescence (33.84±19.19), Inflexibi- lity and adherence to routine (31.21±15.33), Verbal communi- cation (27.72±16.24), Empathy (22.05±18.44) and Hyper-Hypo reactivity to sensory input (21.55±16.48). No significant sex differences emerged for AdAS Spectrum total and domain scores among high scorers as well as among low scorers, except for the domain Hyper-Hypo reactivity to sensory input for which, among low scorers, females reported significantly higher scores than males (2.47±2.23 vs. 1.50±1.28; t=2.51; p=0.014). The two-way ANOVA highlighted significant main effects of totAdAS [F(1,175)=62.11, p<0.001] and Sex [F(1, 175)=5.64, p=0.019] on TALS-SR total score, while it did not detect any significant interaction of totAdAS * Sex [F(1,175)=2.87, p=0.092]. In particular, AdAS Spectrum high scorers and females reported significant higher TALS-SR total score than AdAS Spectrum low scorers (35.46±15.64 vs. 18.89±12.79) and males (29.21±16.59 vs. 25.20±16.25) respectively. The MANOVA analysis showed a significant main effect of totAdAS (p<0.001) and of Sex (p=0.005) on TALS-SR domain scores. Furthermore, a significant interaction of totAdAS * Sex emerged (p=0.028) (Table 1). Specifically, AdAS Spectrum high scorers showed significantly higher TALS-SR scores than AdAS Spectrum low scorers (Fig. 1), and females showed significantly higher TALS-SR scores than males on TALS-SR Loss events and Grief reaction (Fig. 2). Regarding the totAdAS * Sex interaction, while no significant sex differences emerged among AdAS Spectrum high scorers, in the group of AdAS Spectrum low scorers females reported significantly higher scores than males in the following TALS-SR domains: Loss events (30.44±13.64 vs. 20.23±13.89, p=0.001), Grief reaction (29.71±19.35 vs. 17.40±14.74, p=0.001), Re-experiencing (23.21±23.90 vs. 9.30±15.13, p=0.002) and Personal characteristics/Risk factor (20.32±18.65 vs. 12.29±11.49, p=0.017) (Fig. 3a and Fig. 3b). The decision tree model provided the dichotomous variable “PTSD_5” (indicating the presence or absence of full-blown PTSD symptomatology) as dependent variable and totAdAS and Sex as independent variables. According to our results, 30 subjects (17.1%) fulfilled DSM-5 symptomatological criteria for PTSD, with a significantly higher proportion among AdAS Spectrum high scorers than among low scorers (27.6% vs. 6.8%, p<0.001), while no significant differences emerged concerning sex (Fig. 4).
Table 1. MANOVA: TALS-SR domains as dependent variables, sex and totAdAS as independent variables.
| Effect | Pillai's Trace | F (9,163) | p |
|---|---|---|---|
| Intercept | 0.882 | 135.824 | <0.001 |
| totAdAS | 0.335 | 9.135 | <0.001 |
| Sex | 0.132 | 2.748 | 0.005 |
| totAdAS*Sex | 0.106 | 2.152 | 0.028 |
Fig. (1).
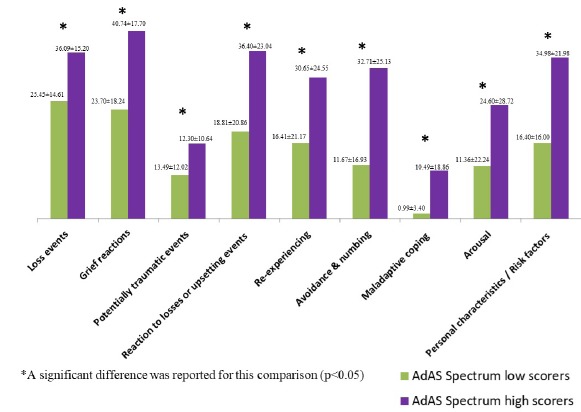
AdAS Spectrum score effect on TALS-SR domain scores: comparison of TALS-SR domain scores between AdAS Spectrum high and low scorers (percentage scores).
Fig. (2).
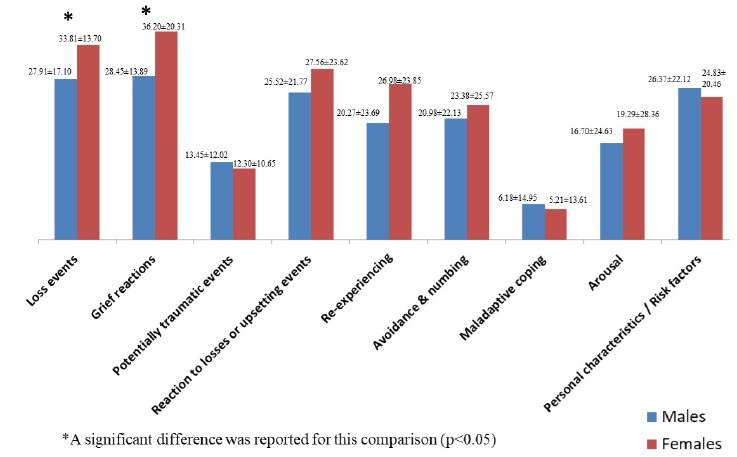
Sex effect on TALS-SR domain scores: comparison of TALS-SR domain scores between males and females within the whole sample (percentage scores).
Fig. (3a).
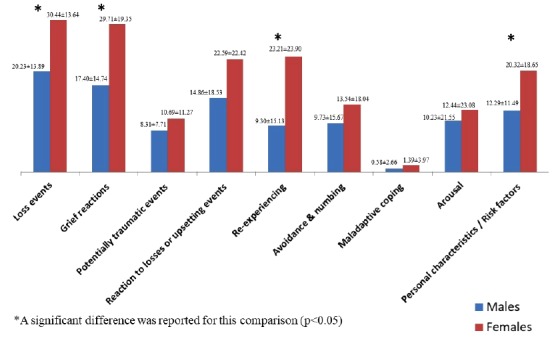
Sex and AdAS Spectrum score effect on TALS-SR domain scores: comparison of TALS-SR domain scores between males and females among AdAS Spectrum low scorers (percentage scores).
Fig. (3b).
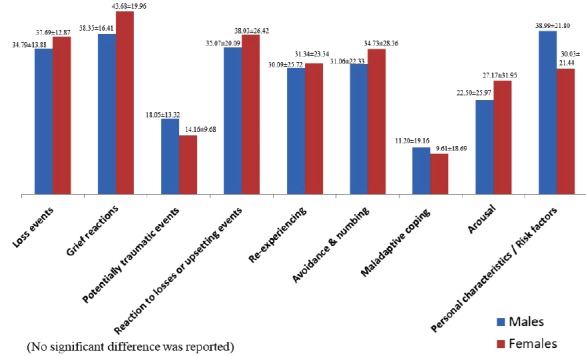
Sex and AdAS Spectrum score effect on TALS-SR domain scores: comparison of TALS-SR domain scores between males and females among AdAS Spectrum high scorers (percentage scores).
Fig. (4).
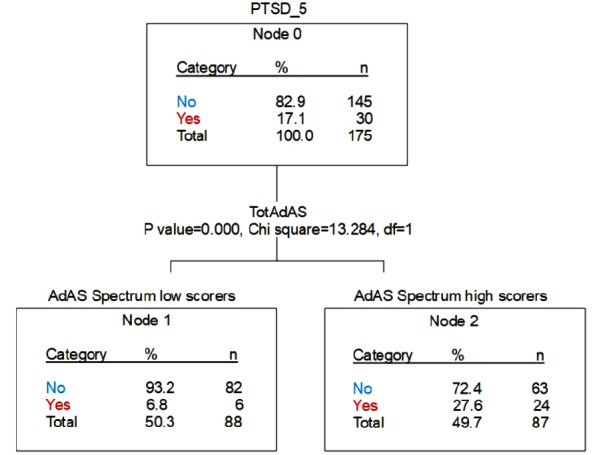
Decision tree model: “PTSD_5” (presence of full-blown PTSD symptomatology according to DSM-5) as the dependent variable, AdAS Spectrum high/low score and Sex as independent variables.
4. DISCUSSION
Our study aimed to investigate the role of sex in the relationship between AT and trauma/stress-related symptoms in a university study population. Results showed how prevalence and features of trauma- and stress-related symptomatology are related and influenced by both AT and sex, as detected by the AdAS Spectrum. Despite there was a wide agreement about the conceptualization of ASD as a disorder mainly distributed among males [46, 47], in our sample no significant sex differences were found with regard to AdAS Spectrum total and domains scores, with the exception of Hyper-Hypo reactivity to sensory input domain score, which was higher among females in the AdAS Spectrum low scorer group. These data seem to be in line with the recent literature, which is stressing the hypothesis that sex differences in the prevalence of AT could be overestimated because of a lack of detection of the female phenotype when assessed by the commonly employed instruments [47, 52, 67]. On the other hand, our sample (students enrolled in high-ranking universities) might be considered a high-risk group for AT [10-17, 59], and this may have affected our results about sex differences. In our sample, AdAS Spectrum high scorers reported higher TALS-SR total mean scores than AdAS Spectrum low scorers. In particular, in each TALS-SR domain, we can see a statistically significant effect of the AdAS Spectrum score, which suggests that people with more AT present also a consistent number of symptoms related to the trauma and stress dimensions. These results seem to confirm, at least in a high-risk population, previous findings about a higher prevalence of adjustment disorders and PTSD among subjects with autism spectrum [37, 43, 68, 69], along with the hypothesis that ASD may act as a vulnerability factor for developing symptoms after a traumatic event [18, 33, 70, 71]. Females reported higher TALS-SR total scores than males in the whole sample, with a significant and independent effect of sex on TALS-SR total score. Moreover, women showed significantly higher scores than men in TALS-SR Loss events and Grief reaction domains. This is in line with the higher vulnerability of females to develop stress-related symptoms reported in previous studies [72-80]. Globally these results may suggest that the presence of AT, which results in reduced coping strategies and difficulties in processing stressful experiences, lead to a higher vulnerability towards a broad range of trauma- or stress-related symptoms, both in male and in the female sex. On the other hand, females, although showing higher trauma- or stress-related symptoms than males, seem to show more frequently in particular loss events and grief reactions, as previously reported in other studies [77-82]. In this framework, it is noteworthy also that, while among AdAS Spectrum loss scorers females reported higher levels than males in TALS-SR Loss events, Grief reaction, Re-experiencing and Personal characteristics/Risk factors domains, no sex differences were found among AdAS Spectrum high scorers. It is interesting to note how these data seem to suggest that the presence of AT might eliminate the protective factor linked to sex towards post-traumatic symptom development, leading to an equally higher distribution in both sexes among subjects with AT. We also found an interesting feature about the TALS-SR Personal characteristics/Risk factors, Maladaptive coping and Potentially traumatic events domains: while among the AdAS Spectrum low scorer group, symptoms measured by these domains were significantly higher among females, in the AdAS Spectrum high scorer group we can see a tendency to a switch in the prevalence of the same symptoms, which seem to be more frequent among males, although the difference observed was not significant. This is in line with the previous data that reported how AT could play a mediating role on sex differences in the expression of PTSD psychopathology [38]. Our results showed that males who present high levels of AT might result to be more vulnerable, even compared to females, towards traumas and stressors. A possible explanation may be found in the higher proneness of males to develop maladaptive and risky behaviors, such as to be provocative or impulsive or to acquire a peculiar pattern of sensation seeking, among high-risk groups [78-80, 83]. Considering that subjects with AT may have difficulties in emotional expression and impairment in peer relations, it is also possible that the stressor would be enhanced by the lack of the ability to request and obtain social support [18, 25, 38]. In this framework, according to data from different studies and samples, it seems that females with AT may be able to develop more effective strategies for coping with their social communication deficit, including also imitating others' behaviors, thus reaching more social support [47, 52, 53, 55, 84]. This sample was not exposed to a specific traumatic event and, as reported elsewhere [18], nobody showed a full-blown diagnosis of PTSD according to DSM-5 criteria. Nevertheless, we found a percentage mean score of 12.90±11.36 on the TALS-SR domain Potentially traumatic events, which assesses the experience during lifetime not only of major traumatic events but also of milder stressful events (such as repeated failure in school or at work, being bullied, etc). Even in this case, the AdAS Spectrum high scorer group showed significantly higher mean scores than AdAS Spectrum low scorers. Moreover, we found a prevalence of 17.1% of subjects that endorsed all the symptomatological criteria for PTSD (criteria B-E), with a significantly higher rate among AdAS Spectrum high scorers and without sex differences. The presence of higher trauma- and stress-related spectrum symptoms among subjects with AT is in line with previous literature, which reports that AT may be considered a consistent vulnerability factor for adjustment disorders and PTSD [5, 22, 30, 32, 35, 37, 43, 85]. From this point of view, our results seem to suggest that some subjects may suffer from a PTSD-like symptomatology even if they do not have a history of major traumatic events, as conceptualized yet by the Complex PTSD (cPTSD) model [41]. In line with this hypothesis, our data may further confirm the higher susceptibility of subjects with AT to develop stress-related symptoms also after mild stressful events. Moreover, it can also be hypothesized that some subjects, and in particular those with AT, may fail in reporting, during the clinical interview, the presence of a major traumatic event in their clinical history, due to their difficulties in properly externalizing and in coping with the traumatic experiences. Consequently, in subjects with AT it is possible that a cPTSD symptomatology, or even a full-blown PTSD, would remain partially or entirely unrecognized, leading these patients to receive a diagnosis of a different mental illness [4-6, 33, 43]. This study should be considered in light of some important limitations. First, the design was cross-sectional, and this prevented us from clarifying the temporal relationship between AT and trauma- and stress-related symptoms, as well as to make inferences about the stability over time of the associations found. Second, we employed self-report instruments, which may eventually facilitate over- or understatements in reporting symptoms. Moreover, this is an exploratory study, conducted in a small size sample of high-risk subjects, and further studies are warranted to clarify the relationship between AT, sex, and vulnerability to traumatic experiences. Nevertheless, given the above limitations, our study seems to confirm the presence of a strong relationship between AT and trauma- and stress-related symptoms, that seems to prevail on the effect on sex among high-risk subjects. From a clinical point of view, a better understanding of the role of AT as a predisposing factor towards the development of post-traumatic stress symptoms, as well as a higher awareness of possible sex-related differences in clinical presentations, may lead to improve both prevention and therapeutic strategies for these conditions, that frequently also show high treatment resistance.
ACKNOWLEDGEMENTS
Declared none.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee of the Azienda Ospedaliero-Universitaria of Pisa, Italy.
HUMAN AND ANIMAL RIGHTS
No Animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1964, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all individual participants included in the study.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICTS OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 2.Billeci L., Calderoni S., Conti E., Gesi C., Carmassi C., Dell’Osso L., Cioni G., Muratori F., Guzzetta A. The broad autism (Endo)phenotype: Neurostructural and neurofunctional correlates in parents of individuals with autism spectrum disorders. Front. Neurosci. 2016;10:346. doi: 10.3389/fnins.2016.00346. https://doi.org/doi [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carpita B., Muti D., Dell’Osso L. Oxidative stress, Maternal diabetes, and Autism spectrum disorders. Oxid. Med. Cell. Longev. 2018;2018:3717215. doi: 10.1155/2018/3717215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dell’Osso L., Luche R.D., Gesi C., Moroni I., Carmassi C., Maj M. From Asperger’s Autistischen Psychopathen to DSM-5 Autism spectrum disorder and beyond: A subthreshold autism spectrum model. Clin. Pract. Epidemiol. Ment. Health. 2016;12:120–131. doi: 10.2174/1745017901612010120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dell’Osso L., Dalle Luche R., Maj M. Adult autism spectrum as a transnosographic dimension. CNS Spectr. 2016;21(2):131–133. doi: 10.1017/S1092852915000450. [DOI] [PubMed] [Google Scholar]
- 6.Carmassi C., Bertelloni C.A., Salarpi G., Diadema E., Avella M.T., Dell’Oste V., Dell’Osso L. Is there a major role for undetected autism spectrum disorder with childhood trauma in a patient with a diagnosis of bipolar disorder, self-injuring and multiple comorbidities? Case Rep. Psychiatry. 2019;2019:4703795. doi: 10.1155/2019/4703795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dawson G., Estes A., Munson J., Schellenberg G., Bernier R., Abbott R. Quantitative assessment of autism symptom-related traits in probands and parents: Broader Phenotype Autism Symptom Scale. J. Autism Dev. Disord. 2007;37(3):523–536. doi: 10.1007/s10803-006-0182-2. [DOI] [PubMed] [Google Scholar]
- 8.Losh M., Childress D., Lam K., Piven J. Defining key features of the broad autism phenotype: a comparison across parents of multiple- and single-incidence autism families. Am. J. Med. Genet. B. Neuropsychiatr. Genet. 2008;147B(4):424–433. doi: 10.1002/ajmg.b.30612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Losh M., Adolphs R., Poe M.D., Couture S., Penn D., Baranek G.T., Piven J. Neuropsychological profile of autism and the broad autism phenotype. Arch. Gen. Psychiatry. 2009;66(5):518–526. doi: 10.1001/archgenpsychiatry.2009.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baron-Cohen S., Wheelwright S., Skinner R., Martin J., Clubley E. The autism-spectrum quotient (AQ): evidence from Asperger syndrome/high-functioning autism, males and females, scientists and mathematicians. J. Autism Dev. Disord. 2001;31(1):5–17. doi: 10.1023/A:1005653411471. [DOI] [PubMed] [Google Scholar]
- 11.Wakabayashi A., Baron-Cohen S., Wheelwright S., Tojo Y. The Autism-Spectrum Quotient (AQ) in Japan: A cross-cultural comparison. J. Autism Dev. Disord. 2006;36(2):263–270. doi: 10.1007/s10803-005-0061-2. [DOI] [PubMed] [Google Scholar]
- 12.Pisula E., Kawa R., Szostakiewicz Ł., Łucka I., Kawa M., Rynkiewicz A. Autistic traits in male and female students and individuals with high functioning autism spectrum disorders measured by the Polish version of the Autism-Spectrum Quotient. PLoS One. 2013;8(9):e75236. doi: 10.1371/journal.pone.0075236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choteau L., Raynal P., Goutaudier N., Chabrol H. Psychopathological traits in college students from top-ranking french schools: Do autistic features impair success in science when associated with schizotypal traits? Psychiatry Res. 2016;237:218–223. doi: 10.1016/j.psychres.2016.01.038. [DOI] [PubMed] [Google Scholar]
- 14.Sierro G., Rossier J., Mohr C. Validation of the French Autism Spectrum Quotient scale and its relationships with schizotypy and Eysenckian personality traits. Compr. Psychiatry. 2016;68:147–155. doi: 10.1016/j.comppsych.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 15.Trevisan D., Birmingham E. Examining the relationship between autistic traits and college adjustment. Autism. 2016;20(6):719–729. doi: 10.1177/1362361315604530. [DOI] [PubMed] [Google Scholar]
- 16.Shi L.J., Liu W.H., Shi H.S., Yan C., Wang Y., Wang Y., Cheung E.F.C., Chan R.C.K. Co-occurrence of autistic and schizotypal traits and its association with emotional and psychosocial function in Chinese college students. Psychiatry Res. 2017;248:64–70. doi: 10.1016/j.psychres.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 17.Stevenson J.L., Hart K.R. Psychometric Properties of the Autism-Spectrum Quotient for Assessing Low and High Levels of Autistic Traits in College Students. J. Autism Dev. Disord. 2017;47(6):1838–1853. doi: 10.1007/s10803-017-3109-1. [DOI] [PubMed] [Google Scholar]
- 18.Dell'Osso L, Carpita B, Cremone IM, et al. The mediating effect of trauma and stressor related symptoms and ruminations on the relationship between autistic traits and mood spectrum. Psychiatry Research. 2018;S0165-1781(18):30826–6. doi: 10.1016/j.psychres.2018.10.040. [DOI] [PubMed] [Google Scholar]
- 19.Towbin K.E., Pradella A., Gorrindo T., Pine D.S., Leibenluft E. Autism spectrum traits in children with mood and anxiety disorders. J. Child Adolesc. Psychopharmacol. 2005;15(3):452–464. doi: 10.1089/cap.2005.15.452. [DOI] [PubMed] [Google Scholar]
- 20.Kunihira Y., Senju A., Dairoku H., Wakabayashi A., Hasegawa T. ‘Autistic’ traits in non-autistic Japanese populations: relationships with personality traits and cognitive ability. J. Autism Dev. Disord. 2006;36(4):553–566. doi: 10.1007/s10803-006-0094-1. [DOI] [PubMed] [Google Scholar]
- 21.Pine D.S., Guyer A.E., Goldwin M., Towbin K.A., Leibenluft E. Autism spectrum disorder scale scores in pediatric mood and anxiety disorders. J. Am. Acad. Child Adolesc. Psychiatry. 2008;47(6):652–661. doi: 10.1097/CHI.0b013e31816bffa5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kanne S.M., Christ S.E., Reiersen A.M. Psychiatric symptoms and psychosocial difficulties in young adults with autistic traits. J. Autism Dev. Disord. 2009;39(6):827–833. doi: 10.1007/s10803-008-0688-x. [DOI] [PubMed] [Google Scholar]
- 23.Matsuo J., Kamio Y., Takahashi H., Ota M., Teraishi T., Hori H., Nagashima A., Takei R., Higuchi T., Motohashi N., Kunugi H. Autistic-like traits in adult patients with mood disorders and schizophrenia. PLoS One. 2015;10(4):e0122711. doi: 10.1371/journal.pone.0122711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu J., Gong J., Nie G., He Y., Xiao B., Shen Y., Luo X. The mediating effects of childhood neglect on the association between schizotypal and autistic personality traits and depression in a non-clinical sample. BMC Psychiatry. 2017;17(1):352. doi: 10.1186/s12888-017-1510-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dell’Osso L., Muti D., Carpita B., et al. The Adult Autism Subthreshold Spectrum (AdAS) model: A neurodevelopmental approach to mental disorders. Journal of Psychopathology. 2018;24:118–124. [Google Scholar]
- 26.Dell’Osso L., Cremone I.M., Carpita B., Fagiolini A., Massimetti G., Bossini L., Vita A., Barlati S., Carmassi C., Gesi C. Correlates of autistic traits among patients with borderline personality disorder. Compr. Psychiatry. 2018;83:7–11. doi: 10.1016/j.comppsych.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 27.Dell’Osso L., Carpita B., Gesi C., Cremone I.M., Corsi M., Massimetti E., Muti D., Calderani E., Castellini G., Luciano M., Ricca V., Carmassi C., Maj M. Subthreshold autism spectrum disorder in patients with eating disorders. Compr. Psychiatry. 2018;81:66–72. doi: 10.1016/j.comppsych.2017.11.007. https://doi.org/doi [DOI] [PubMed] [Google Scholar]
- 28.Dell’Osso L., Abelli M., Carpita B., Pini S., Castellini G., Carmassi C., Ricca V. Historical evolution of the concept of anorexia nervosa and relationships with orthorexia nervosa, autism, and obsessive-compulsive spectrum. Neuropsychiatr. Dis. Treat. 2016;12:1651–1660. doi: 10.2147/NDT.S108912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dell’Osso L., Cremone I.M., Carpita B., Dell’Oste V., Muti D., Massimetti G., Barlati S., Vita A., Fagiolini A., Carmassi C., Gesi C. Rumination, posttraumatic stress disorder, and mood symptoms in borderline personality disorder. Neuropsychiatr. Dis. Treat. 2019;15:1231–1238. doi: 10.2147/NDT.S198616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mehtar M., Mukaddes N.M. Posttraumatic Stress Disorder in individuals with diagnosis of Autistic Spectrum Disorders. Res. Autism Spectr. Disord. 2011;5:539–546. doi: 10.1016/j.rasd.2010.06.020. [DOI] [Google Scholar]
- 31.Storch E.A., Sulkowski M.L., Nadeau J., Lewin A.B., Arnold E.B., Mutch P.J., Jones A.M., Murphy T.K. The phenomenology and clinical correlates of suicidal thoughts and behaviors in youth with autism spectrum disorders. J. Autism Dev. Disord. 2013;43(10):2450–2459. doi: 10.1007/s10803-013-1795-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stavropoulos KK, Bolourian Y, Blacher J. Differential Diagnosis of Autism Spectrum Disorder and Post Traumatic Stress Disorder: Two Clinical Cases. Journal of Clinical Medicine. 2018;7:piiE71. doi: 10.3390/jcm7040071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.King R. Complex Post-Traumatic Stress Disorder: implications for individuals with Autism Spectrum Disorders- Part 1. J. Dev. Disabil. 2010;16:91–100. [Google Scholar]
- 34.Dell’Osso L., Abelli M., Pini S., Carpita B., Carlini M., Mengali F., Tognetti R., Rivetti F., Massimetti G. The influence of gender on social anxiety spectrum symptoms in a sample of university students. Riv. Psichiatr. 2015;50(6):295–301. doi: 10.1708/2098.22688. [DOI] [PubMed] [Google Scholar]
- 35.Kato K., Mikami K., Akama F., Yamada K., Maehara M., Kimoto K., Kimoto K., Sato R., Takahashi Y., Fukushima R., Ichimura A., Matsumoto H. Clinical features of suicide attempts in adults with autism spectrum disorders. Gen. Hosp. Psychiatry. 2013;35(1):50–53. doi: 10.1016/j.genhosppsych.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 36.Valenti M., Ciprietti T., Egidio C.D., Gabrielli M., Masedu F., Tomassini A.R., Sorge G. Adaptive response of children and adolescents with autism to the 2009 earthquake in L’Aquila, Italy. J. Autism Dev. Disord. 2012;42(6):954–960. doi: 10.1007/s10803-011-1323-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Roberts A.L., Koenen K.C., Lyall K., Robinson E.B., Weisskopf M.G. Association of autistic traits in adulthood with childhood abuse, interpersonal victimization, and posttraumatic stress. Child Abuse Negl. 2015;45:135–142. doi: 10.1016/j.chiabu.2015.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dell’Osso L., Corsi M., Gesi C., Bertelloni C.A., Massimetti G., Peroni D., Bonuccelli A., Orsini A., Carmassi C. Adult Autism Subthreshold Spectrum (AdAS Spectrum) in parents of pediatric patients with epilepsy: Correlations with post-traumatic stress symptoms. Compr. Psychiatry. 2018;83:25–30. doi: 10.1016/j.comppsych.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 39.Terr L.C. Childhood traumas: an outline and overview. Am. J. Psychiatry. 1991;148(1):10–20. doi: 10.1176/ajp.148.1.10. [DOI] [PubMed] [Google Scholar]
- 40.Herman J.L. Complex PTSD: a syndrome in survivors of prolonged and repeated trauma. J. Trauma. Stress. 1992;5:377–391. doi: 10.1002/jts.2490050305. [DOI] [Google Scholar]
- 41.Van der Kolk B. Developmental trauma disorder. Toward a rational diagnosis for children with complex trauma histories. Psychiatr. Ann. 2005;35:401–408. doi: 10.3928/00485713-20050501-06. [DOI] [Google Scholar]
- 42.Hofvander B., Delorme R., Chaste P., Nydén A., Wentz E., Ståhlberg O., Herbrecht E., Stopin A., Anckarsäter H., Gillberg C., Råstam M., Leboyer M. Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders. BMC Psychiatry. 2009;9:35. doi: 10.1186/1471-244X-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dell’Osso L., Dalle Luche R., Carmassi C. A new perspective in post-traumatic stress disorder: which role for unrecognized autism spectrum? Int. J. Emerg. Ment. Health. 2015;17:436–438. doi: 10.4172/1522-4821.1000e188. [DOI] [Google Scholar]
- 44.Cloitre M., Garvert D.W., Brewin C.R., Bryant R.A., Maercker A. Evidence for proposed ICD-11 PTSD and complex PTSD: a latent profile analysis. Eur. J. Psychotraumatol. 2013;4:20706. doi: 10.3402/ejpt.v4i0.20706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maercker A., Brewin C.R., Bryant R.A., Cloitre M., van Ommeren M., Jones L.M., Humayan A., Kagee A., Llosa A.E., Rousseau C., Somasundaram D.J., Souza R., Suzuki Y., Weissbecker I., Wessely S.C., First M.B., Reed G.M. Diagnosis and classification of disorders specifically associated with stress: proposals for ICD-11. World Psychiatry. 2013;12(3):198–206. doi: 10.1002/wps.20057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baron-Cohen S. The extreme male brain theory of autism. Trends Cogn. Sci. (Regul. Ed.) 2002;6(6):248–254. doi: 10.1016/S1364-6613(02)01904-6. [DOI] [PubMed] [Google Scholar]
- 47.Dell’Osso L., Gesi C., Massimetti E., Cremone I.M., Barbuti M., Maccariello G., Moroni I., Barlati S., Castellini G., Luciano M., Bossini L., Rocchetti M., Signorelli M., Aguglia E., Fagiolini A., Politi P., Ricca V., Vita A., Carmassi C., Maj M. Adult Autism Subthreshold Spectrum (AdAS Spectrum): Validation of a questionnaire investigating subthreshold autism spectrum. Compr. Psychiatry. 2017;73:61–83. doi: 10.1016/j.comppsych.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 48.Carmassi C., Akiskal H.S., Yong S.S., Stratta P., Calderani E., Massimetti E., Akiskal K.K., Rossi A., Dell’Osso L. Post-traumatic stress disorder in DSM-5: estimates of prevalence and criteria comparison versus DSM-IV-TR in a non-clinical sample of earthquake survivors. J. Affect. Disord. 2013;151(3):843–848. doi: 10.1016/j.jad.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 49.Carmassi C., Dell’Osso L., Manni C., Candini V., Dagani J., Iozzino L., Koenen K.C., de Girolamo G. Frequency of trauma exposure and Post-Traumatic Stress Disorder in Italy: analysis from the World Mental Health Survey Initiative. J. Psychiatr. Res. 2014;59:77–84. doi: 10.1016/j.jpsychires.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cénat J.M., Derivois D. Assessment of prevalence and determinants of posttraumatic stress disorder and depression symptoms in adults survivors of earthquake in Haiti after 30 months. J. Affect. Disord. 2014;159:111–117. doi: 10.1016/j.jad.2014.02.025. [DOI] [PubMed] [Google Scholar]
- 51.Carmassi C., Corsi M., Bertelloni C.A., Carpita B., Gesi C., Pedrinelli V., Massimetti G., Peroni D.G., Bonuccelli A., Orsini A., Dell’Osso L. Mothers and fathers of children with epilepsy: gender differences in post-traumatic stress symptoms and correlations with mood spectrum symptoms. Neuropsychiatr. Dis. Treat. 2018;14:1371–1379. doi: 10.2147/NDT.S158249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Baron-Cohen S, Cassidy S, Auyeung B, et al. Attenuation of Typical Sex Differences in 800 Adults with Autism vs. 3,900 Controls PloS One. 2014;2014.9:e102251. doi: 10.1371/journal.pone.0102251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lai M.C., Baron-Cohen S., Buxbaum J.D. Understanding autism in the light of sex/gender. Mol. Autism. 2015;6:24. doi: 10.1186/s13229-015-0021-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sbrana A., Bizzarri J.V., Rucci P., Gonnelli C., Doria M.R., Spagnolli S., Ravani L., Raimondi F., Dell’Osso L., Cassano G.B. The spectrum of substance use in mood and anxiety disorders. Compr. Psychiatry. 2005;46(1):6–13. doi: 10.1016/j.comppsych.2004.07.017. [DOI] [PubMed] [Google Scholar]
- 55.Attwood T., Grandin T., Faherty C., et al. Asperger’s and girls. Arlington, TX: Future Horizons; 2006. [Google Scholar]
- 56.Jobe L.E., White S.W. Loneliness, social relationships, and a broader autism phenotype in college students. Pers. Individ. Dif. 2007;42:1479–1489. doi: 10.1016/j.paid.2006.10.021. [DOI] [Google Scholar]
- 57.Clark J. Asperger’s in pink: pearls of wisdom from inside the bubble of raising a child with Asperger’s. Arlington, TX: Future Horizons; 2010. [Google Scholar]
- 58.White S.W., Ollendick T.H., Bray B.C. College students on the autism spectrum: prevalence and associated problems. Autism. 2011;15(6):683–701. doi: 10.1177/1362361310393363. [DOI] [PubMed] [Google Scholar]
- 59.Dell’Osso L., Abelli M., Pini S., Carlini M., Carpita B., Macchi E., Gorrasi F., Mengali F., Tognetti R., Massimetti G. Dimensional assessment of DSM-5 social anxiety symptoms among university students and its relationship with functional impairment. Neuropsychiatr. Dis. Treat. 2014;10:1325–1332. doi: 10.2147/NDT.S59348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Marazziti D., Abelli M., Baroni S., et al. Recent findings on the pathophysiology of social anxiety disorder. Clinical Neuropsychiatry. 2014;11:91–100. [Google Scholar]
- 61.Marazziti D., Abelli M., Baroni S., Carpita B., Ramacciotti C.E., Dell’Osso L. Neurobiological correlates of social anxiety disorder: an update. CNS Spectr. 2015;20(2):100–111. doi: 10.1017/S109285291400008X. [DOI] [PubMed] [Google Scholar]
- 62.Garlow S.J., Rosenberg J., Moore J.D., Haas A.P., Koestner B., Hendin H., Nemeroff C.B. Depression, desperation, and suicidal ideation in college students: results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depress. Anxiety. 2008;25(6):482–488. doi: 10.1002/da.20321. [DOI] [PubMed] [Google Scholar]
- 63.First M.B., Williams J.B., Karg R.S., et al. SCID-5-CV: Structured Clinical Interview for DSM-5 Disorders, Clinician Version. Arlington, VA: American Psychiatric Association; 2015. [Google Scholar]
- 64.Dell’osso L., Shear M.K., Carmassi C., Rucci P., Maser J.D., Frank E., Endicott J., Lorettu L., Altamura C.A., Carpiniello B., Perris F., Conversano C., Ciapparelli A., Carlini M., Sarno N., Cassano G.B. Validity and reliability of the Structured Clinical Interview for the Trauma and Loss Spectrum (SCI-TALS). Clin. Pract. Epidemiol. Ment. Health. 2008;4:2. doi: 10.1186/1745-0179-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dell’Osso L., Carmassi C., Rucci P., Conversano C., Shear M.K., Calugi S., Maser J.D., Endicott J., Fagiolini A., Cassano G.B. A multidimensional spectrum approach to post-traumatic stress disorder: comparison between the Structured Clinical Interview for Trauma and Loss Spectrum (SCI-TALS) and the Self-Report instrument (TALS-SR). Compr. Psychiatry. 2009;50(5):485–490. doi: 10.1016/j.comppsych.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 66.Corp I.B.M. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp. Released; 2016. [Google Scholar]
- 67.Lai M.C., Baron-Cohen S., Buxbaum J.D. Understanding autism in the light of sex/gender. Mol. Autism. 2015;6:24. doi: 10.1186/s13229-015-0021-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Takara K., Kondo T. Comorbid atypical autistic traits as a potential risk factor for suicide attempts among adult depressed patients: a case-control study. Ann. Gen. Psychiatry. 2014;13(1):33. doi: 10.1186/s12991-014-0033-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Takara K., Kondo T. Autism spectrum disorder among first-visit depressed adult patients: diagnostic clues from backgrounds and past history. Gen. Hosp. Psychiatry. 2014;36(6):737–742. doi: 10.1016/j.genhosppsych.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 70.Kerns C.M., Newschaffer C.J., Berkowitz S.J. Traumatic childhood events and autism spectrum disorder. J. Autism Dev. Disord. 2015;45(11):3475–3486. doi: 10.1007/s10803-015-2392-y. [DOI] [PubMed] [Google Scholar]
- 71.Haruvi-Lamdan N., Horesh D., Golan O. PTSD and autism spectrum disorder: Co-morbidity, gaps in research, and potential shared mechanisms. Psychol. Trauma. 2018;10(3):290–299. doi: 10.1037/tra0000298. [DOI] [PubMed] [Google Scholar]
- 72.Helzer J.E., Robins L.N., McEvoy L. Post-traumatic stress disorder in the general population. Findings of the epidemiologic catchment area survey. N. Engl. J. Med. 1987;317(26):1630–1634. doi: 10.1056/NEJM198712243172604. [DOI] [PubMed] [Google Scholar]
- 73.Kessler R.C., Sonnega A., Bromet E., Hughes M., Nelson C.B. Posttraumatic stress disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 74.Favaro A., Rodella F.C., Colombo G., Santonastaso P. Post-traumatic stress disorder and major depression among Italian Nazi concentration camp survivors: a controlled study 50 years later. Psychol. Med. 1999;29(1):87–95. doi: 10.1017/S0033291798007855. [DOI] [PubMed] [Google Scholar]
- 75.Kessler R.C., Chiu W.T., Demler O., Merikangas K.R., Walters E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.O’Toole B.I., Catts S.V. Trauma, PTSD, and physical health: an epidemiological study of Australian Vietnam veterans. J. Psychosom. Res. 2008;64(1):33–40. doi: 10.1016/j.jpsychores.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 77.Dell’Osso L., Carmassi C., Musetti L., Socci C., Shear M.K., Conversano C., Maremmani I., Perugi G. Lifetime mood symptoms and adult separation anxiety in patients with complicated grief and/or post-traumatic stress disorder: a preliminary report. Psychiatry Res. 2012;198(3):436–440. doi: 10.1016/j.psychres.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 78.Dell’osso L., Carmassi C., Stratta P., Massimetti G., Akiskal K.K., Akiskal H.S., Maremmani I., Rossi A. Gender differences in the relationship between maladaptive behaviors and post-traumatic stress disorder. A study on 900 L’Aquila 2009 earthquake survivors. Front. Psychiatry. 2013;3:111. doi: 10.3389/fpsyt.2012.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Carmassi C., Stratta P., Massimetti G., Bertelloni C.A., Conversano C., Cremone I.M., Miccoli M., Baggiani A., Rossi A., Dell’Osso L. New DSM-5 maladaptive symptoms in PTSD: gender differences and correlations with mood spectrum symptoms in a sample of high school students following survival of an earthquake. Ann. Gen. Psychiatry. 2014;13:28. doi: 10.1186/s12991-014-0028-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Carmassi C., Akiskal H.S., Bessonov D., Massimetti G., Calderani E., Stratta P., Rossi A., Dell’Osso L. Gender differences in DSM-5 versus DSM-IV-TR PTSD prevalence and criteria comparison among 512 survivors to the L’Aquila earthquake. J. Affect. Disord. 2014;160:55–61. doi: 10.1016/j.jad.2014.02.028. [DOI] [PubMed] [Google Scholar]
- 81.Dell’osso L., Carmassi C., Rucci P., Ciapparelli A., Conversano C., Marazziti D. Complicated grief and suicidality: the impact of subthreshold mood symptoms. CNS Spectr. 2011;16(1):1–6. doi: 10.1017/S1092852912000090. [DOI] [PubMed] [Google Scholar]
- 82.Dell’osso L., Carmassi C., Corsi M., Pergentini I., Socci C., Maremmani A.G., Perugi G. Adult separation anxiety in patients with complicated grief versus healthy control subjects: relationships with lifetime depressive and hypomanic symptoms. Ann. Gen. Psychiatry. 2011;10(1):29. doi: 10.1186/1744-859X-10-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dell’osso L., Carmassi C., Rucci P., Ciapparelli A., Paggini R., Ramacciotti C.E., Conversano C., Balestrieri M., Marazziti D. Lifetime subthreshold mania is related to suicidality in posttraumatic stress disorder. CNS Spectr. 2009;14(5):262–266. doi: 10.1017/S1092852900025426. [DOI] [PubMed] [Google Scholar]
- 84.Lai M.C., Lombardo M.V., Auyeung B., Chakrabarti B., Baron-Cohen S. Sex/gender differences and autism: setting the scene for future research. J. Am. Acad. Child Adolesc. Psychiatry. 2015;54(1):11–24. doi: 10.1016/j.jaac.2014.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dell’Osso L., Conversano C., Corsi M., Bertelloni C.A., Cremone I.M., Carpita B., Carbone M.G., Gesi C., Carmassi C. Polysubstance and behavioral addictions in a patient with bipolar disorder: Role of lifetime subthreshold autism spectrum. Case Rep. Psychiatry. 2018;2018:1547975. doi: 10.1155/2018/1547975. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


