Abstract
Exposure therapy has strong empirical support as a treatment for anxiety and related disorders, yet not all participants see clinically meaningful reduction in symptoms, and some experience return of fear. In this review, we examine the theoretical models of exposure therapy, from early precursors to the contemporary inhibitory learning model. The inhibitory learning model is applied to examine one potential method of improving outcomes in exposure therapy: increasing variability in the progression of the exposure hierarchy. We explore mechanisms that support the use of variability in exposure, including the violation of expectancies to enhance learning. In addition, the role of intolerance of uncertainty in anxiety is examined; variable exposure therapy could target this transdiagnostic mechanism in anxiety and related disorders. Suggestions for future research are then offered.
Keywords: Exposure therapy, Inhibitory learning, Intolerance of uncertainty
Exposure is a key component of effective treatment for anxiety and related disorders. A large body of evidence supports the efficacy of exposure in the treatment of obsessive-compulsive disorder (OCD; Abramowitz, 1996, 1997; Abramowitz, Franklin, & Foa, 2002; Foa & McLean, 2016; Gava et al., 2009; Rosa-Alcázar, Sánchez-Meca, Gómez-Conesa, & Marín-Martínez, 2008), posttraumatic stress disorder (PTSD; Foa & McLean, 2016; McLean & Foa, 2011; Powers, Halpern, Ferenschak, Gillihan, & Foa, 2010), specific phobias (Choy, Fyer, & Lipsitz, 2007; Grös & Antony, 2006), social anxiety disorder (Gould, Buckminster, Pollack, Otto, & Yap, 1997; Rodebaugh, Holaway, & Heimberg, 2004; Taylor, 1996), and panic disorder (Barlow, Craske, Cerny, & Klosko, 1989; Craske, Brown, & Barlow, 1991; Gould, Ott, & Pollack, 1995). Exposure therapy is based on principles of fear extinction, in which classically conditioned stimuli gradually lose their phobic quality through repeated exposure without the feared negative consequences (Myers & Davis, 2007). However, the theory behind exposure and the specific techniques used in therapy have evolved since the initial conceptualization of exposure therapy in the mid-twentieth century. Historical perspectives on exposure therapy are reviewed before turning to contemporary theoretical models and applications. Adult clients are the primary focus of this review; for a detailed review of historical approaches to exposure with an emphasis on children, see Davis and Ollendick (2005).
Theories of Exposure Therapy: A Historical Perspective
Systematic Desensitization and Flooding
The earliest approach to exposure therapy was systematic desensitization (Wolpe, 1958; 1961). Wolpe outlined three key components to systematic desensitization: relaxation training, the construction of a hierarchy of feared stimuli or situations, and progression through this hierarchy through alternating exposure and relaxation. The theoretical basis of systematic desensitization, Wolpe’s reciprocal inhibition theory, is the counter-conditioning of feared stimuli. Typically, exposure to these stimuli is paired with relaxation in order to evoke a response incompatible with fear or anxiety; however, other methods such humor, pleasurable food, or sexual behavior could be paired with the stimulus as well (Davis & Ollendick, 2005; Wolpe, 1958). Wolpe suggests that the counter-conditioning of feared stimuli with relaxation or another pleasurable experience eliminates avoidance and inhibits anxious responses. Early research on systematic desensitization, in the form of case studies and some experimental designs, demonstrated greater efficacy of systematic desensitization compared to fear extinction paradigms that did not use relaxation (Rachman, 1967).
An alternative approach to systematic desensitization used a technique termed “flooding,” in which stimuli that evoke intense fear responses are presented to the client immediately, without progression up a hierarchy and without pairing an incompatible response (Marks, 1972; Morganstern, 1973). The literature on the effectiveness of flooding techniques is more mixed than that of systematic desensitization, partly due to the confounding of flooding with implosive therapy, which involves imaginal exposure to extreme and unrealistic stimuli (Morganstern, 1973; Smith, Dickson, & Sheppard, 1973). Some studies have demonstrated the relative effectiveness of flooding over systematic desensitization (Boulougouris, Marks, & Marset, 1971; Marks, Boulougouris, & Marset, 1971; Marshall, Gauthier, Christie, Currie, & Gordon, 1977; see Smith, Dickson, & Sheppard, 1973 for a review), while others have reported mixed results and raised ethical concerns over the use of flooding in anxious clients (Morganstern, 1973). Concerns have also been raised about clients’ acceptability of flooding. A cross-over study comparing flooding and desensitization noted that clients were surprisingly accepting of flooding, and some clients even preferred flooding to desensitization because they felt it was more effective (Marks et al., 1971). Notably, these clients were highly motivated to pursue treatment, as the trial required a large number of sessions; clients who are less highly motivated might not find flooding to be as acceptable. Additionally, flooding is thought to be less acceptable for children (King & Gullone, 1990).
In 1975, Marks published an extensive literature review on systematic desensitization and determined that the active ingredient in this treatment was the exposure to feared stimuli, not relaxation (Marks, 1975; Tryon, 2005). After the publication of this review, behavioral modification research and theory focused on “exposure therapy” instead of systematic desensitization or flooding, although some recent studies suggest that flooding may still have utility (Moulds & Nixon, 2006).
Modeling
Albert Bandura’s theory of social learning has also been applied to the extinction of fear. Bandura and colleagues suggested that individuals with phobias could learn approach behavior and experience reduced fear through modeling, or observing others approach a feared object or situation without negative consequences (Bandura, Blanchard, & Ritter, 1969; Bandura, Grusec, & Menlove, 1967; Ritter, 1968). For example, a person with a snake phobia would watch someone else interact confidently with a snake without displaying fear. When the model did not experience a negative outcome, the client would learn that behavioral approach of snakes was not as dangerous as feared and can change their behavior accordingly. After observing appropriately modeled approach behavior and practicing it, the client gains coping skills and self-efficacy, which is likely to increase future approach behavior and decrease fear (Bandura, 1977). Modeling has been shown to be more effective than systematic desensitization for the treatment of multiple phobias (Bandura et al., 1969; Shaw & Thoresen, 1974) and is especially effective when the model shares characteristics like age and gender with the client (Kazdin, 1974; Meichenbaum, 1971). Although modeling leads to beneficial outcomes, approaches in which the client attempts the approach behavior themselves after modeling leads to greater reductions of fear and higher self-efficacy compared to vicarious experience alone (Bandura, Adams, & Beyer, 1977). A combination of modeling and exposure is commonly used in the treatment of phobias and other anxiety disorders, especially for children (Davis & Ollendick, 2005).
Emotional Processing Theory
A revised theory of exposure therapy, emotional processing, took hold in the 1980s (Foa & Kozak, 1986; Rachman, 1980). Emotional processing theory drew upon Lang’s bioinformational model of fear (Lang, 1977, 1979), which notes the importance of changes in physiology (e.g., heart rate) in response to emotional stimuli as an indicator of improvement during systematic desensitization (Lang, Melamed, & Hart, 1970). These physiological changes occur in response to fear imagery and were hypothesized as the key to the emotional processing of fear (Lang, 1977). Noting that systematic desensitization, flooding, and modeling approaches could all successfully reduce fear, Rachman suggested that “the transformation or neutralization of emotion-provoking stimuli,” which is “facilitated by repeated presentations, by stimuli presented for certain minimal durations, by piecemeal presentations, by minimizing distractions, (and) by inducing a low level of arousal” could be the common principle that explains their effectiveness (Rachman, 1980, p. 57). Thus, Rachman introduced a recipe for successful exposure therapy for fear.
Using Lang’s bioinformational model, Foa and Kozak (1986) discuss the fear memory as the basic propositional representation that is represented in the brain and is targeted during exposure. This representation includes basic information about the feared situation or stimulus, information about potential responses to the situation or stimulus (verbal, physiological, or behavioral), and interpretations about the meaning of both the stimulus and the responses. Together, this structure can be modified in memory through exposure; the modification of memory is the mechanism through which emotional processing reduces fear (Foa & Kozak, 1986). To measure the degree of emotional processing that has taken place, three indicators can be used. First, initial reports of fear, often measured by physiological signs such as an increase in heart rate and/or electrodermal activity, indicate that the fear memory has been “activated.” Second, clients undergoing successful emotional processing habituate within a given session of exposure, and therefore experience lower levels of arousal at the end of exposure than at the beginning. Finally, between-session habituation should also occur, such that feared stimuli are less fear-provoking at the beginning of the second session of exposure than at the initial fear exposure, and initial fear activation continues to decrease as the sessions continue. Habituation, measured by physiological changes as well as self-reported levels of fear, is the key indicator of fear reduction. Reduced physiological responding to fear stimuli and decreased self-reported levels of experienced fear (subjective units of distress, or SUDS) suggests that corrective learning has occurred and exposure has been successful. Additional considerations for successful exposure therapy include matching the exposure content as closely to the initial fear memory as possible, a sufficiently long enough exposure session to allow for habituation, and conducting exposure free from distraction (Foa & Kozak, 1986; Foa & McNally, 1996).
Based on these principles, traditional exposure therapy involves gradual progression through a hierarchy of feared stimuli, repeating each step until habituation has occurred. The idea that exposure therapy should be conducted in a gradual or graded manner is pervasive throughout the field. Most manuals of exposure therapy discuss the creation of a fear hierarchy with the client and progression through the hierarchy from the easiest to most difficult item. Graded exposure is based on the theory of habituation: first, the client must habituate to a lower level of anxiety before progressing to a new exposure item; then, they must habituate to a slightly higher level of anxiety for the next item, and so on. Research suggests that clients habituate more quickly to less arousing stimuli (i.e., items lower on a client’s hierarchy), which may motivate the client to continue on to more arousing items (Watts, 1971). However, the limited research that examines how clients progress through the hierarchy suggests that order does not particularly matter (Gelder et al., 1973; Hodgson, Rachman, & Marks, 1972). Manuals typically suggest graded exposure for practical reasons, such as to increase client buy-in and compliance (Abramowitz, Deacon, & Whiteside, 2011; Foa & Wilson, 2001; Powers, Smits, Leyro, & Otto, 2007). Others have noted the potential for anxiety and avoidance to be reinforced if a client fails an exposure task, which may cause a disruption in the therapeutic alliance (March, 1995). Although gradual progression through a hierarchy is in line with the emotional processing model, empirical research supporting this approach as the mechanism of treatment outcome during exposure therapy is limited.
The emotional processing model of exposure therapy has contributed a great deal to the treatment of anxiety and related disorders. However, not all clients respond to exposure therapy treatment (Foa, Liebowitz, et al., 2005; Jacoby & Abramowitz, 2016), and some experience a return of fear after treatment (Eisen et al., 2013; Simpson, Franklin, Cheng, Foa, & Liebowitz, 2005; Vervliet, Craske, & Hermans, 2013). Additionally, a thorough review of the evidence suggests that emotional processing theory’s indices of learning (initial fear activation, within-session habituation, and between-session habituation) are not necessary for learning to occur (Craske et al., 2008). Initial fear activation predicts positive outcome in some studies (Beckham, Vrana, May, Gustafson, & Smith, 1990; Foa, Riggs, Massie, & Yarczower, 1995; Kozak, Foa, & Steketee, 1988; Lang, Melamed, & Hart, 1970; Pitman et al., 1996), but not in others (Foa et al., 1983; Kamphuis & Telch, 2000; Rauch, Foa, Furr, & Filip, 2004; Telch et al., 2004). Similarly, evidence is mixed for a relationship between within-session habituation and outcome, with some studies finding a positive correlation (Beckham et al., 1990; Foa et al., 1983; Pitman et al., 1996), while others found no relationship (Kozak et al., 1988; Riley et al., 1995). A few studies have also demonstrated the effectiveness of exposure even when exposure was terminated at high levels of anxiety (Emmelkamp & Mersch, 1982; Rachman, Craske, Tallman, & Solyom, 1986). In other studies, participants who achieved 100% fear reduction during exposure had more return of fear than participants who stopped exposure after a 50% reduction in fear (Rachman, Robinson, & Lopatka, 1987), and participants who “overlearned” by repeating exposure trials after reaching 100% fear reduction did not fare better than participants who stopped when they reached 100% fear reduction (Rachman & Lopatka, 1988). Between-session habituation is positively correlated with outcomes in some studies (Foa et al., 1983; Kozak et al., 1988; Lang et al., 1970; Rauch et al., 2004), but other studies have noted that between-session habituation is not necessary for improvement to occur (Tsao & Craske, 2000), and that heart rate is not always a reliable index of between-session habituation (Kozak et al., 1988; Lang & Craske, 2000; Rowe & Craske, 1998). Across these studies, inconsistencies in how habituation was measured (subjectively vs. physiologically, using heart rate or electrodermal activity), methodological differences in the number and length of exposure sessions, and differences in sample characteristics (diagnosis, comorbidity) may all contribute to the disparate findings reported. Careful examination of potential covariates is needed in future studies of the mechanisms of exposure.
Another body of evidence that contradicts the claim that between-session habituation is a necessary component of successful of exposure therapy is the research on the efficacy of one-session exposure therapy for specific phobias. While PTSD and OCD usually require a full course of exposure therapy treatment (eight to twelve sessions or more), many phobias can be effectively treated in a single session (Ollendick et al., 2009; Öst, 1989). If between-session habituation were necessary for effective exposure treatment, one-session treatments would not be effective. One-session treatment of flying phobia, blood-injection-injury phobia, spider phobia, claustrophobia, and other specific phobias has shown comparable outcomes to five-session treatment, with clinically significant improvements maintained for follow-up periods as long as four years (Öst, Alm, Brandberg, & Breitholtz, 2001; Öst, Brandberg, & Alm, 1997; Öst, Hellström, & Kåver, 1992). One-session treatment is also effective for youth as well as adults (Davis & Ollendick, 2005; Ollendick et al., 2009; Öst, Svensson, Hellström, & Lindwall, 2001). Öst states that the goal of one-session exposure treatment is to “expose the patient to the phobic situation in a controlled way, and enable him/her to stay in the situation until realizing that the feared consequence does not occur” (Öst, 1989, p. 3). Here, the emphasis is not necessarily on fear reduction, but on learning that feared consequences do not occur and reducing avoidance behaviors.
Other studies demonstrate that fear expression is not a reliable indicator of effective fear learning. Memory research indicates that performance during instruction is not a reliable sign that learning has occurred (Bjork & Bjork, 2006). In addition, emotion regulation research suggests that toleration of fear may be more important than reduction in fear, and deficits in emotion regulation and emotional avoidance of fear and anxiety may lead to the development of anxiety disorders (Forsyth, Eifert, & Barrios, 2006; Hofmann, Sawyer, Fang, & Asnaani, 2012; Wirtz, Hofmann, Riper, & Berking, 2014). An experimental examination of intensive interoceptive exposure for panic disorder demonstrated that intensive interoceptive exposure was more effective than standard interoceptive exposure, which was fully mediated by improvement in fear toleration and violation of the expectation of negative outcomes (Deacon et al., 2013). When using interoceptive exposure to treat panic disorder, the focus is on changing maladaptive beliefs regarding the inherent dangerousness of panic-related body sensations by exposing patients to those sensations. By targeting anxiety sensitivity in this regard, the client learns that although panic symptoms are uncomfortable, the feared negative consequences of having a panic attack (going crazy; having a heart attack; death) do not occur. Increasing tolerance of negative emotional experiences is key to reducing functional impairment, as distressed clients learn how to cope with their emotional and physiological responses to stress and return to activities they had previously avoided. This kind of change is exemplified by statements such as “I felt anxious, but I did it anyway.” Notably, increased emotional distress tolerance is a key goal of several behavioral therapies, including cognitive-behavioral therapy (CBT) and acceptance and commitment therapy (ACT; Hayes, Strosahl, & Wilson, 1999; Leyro, Zvolensky, & Bernstein, 2010).
Inhibitory Learning Model
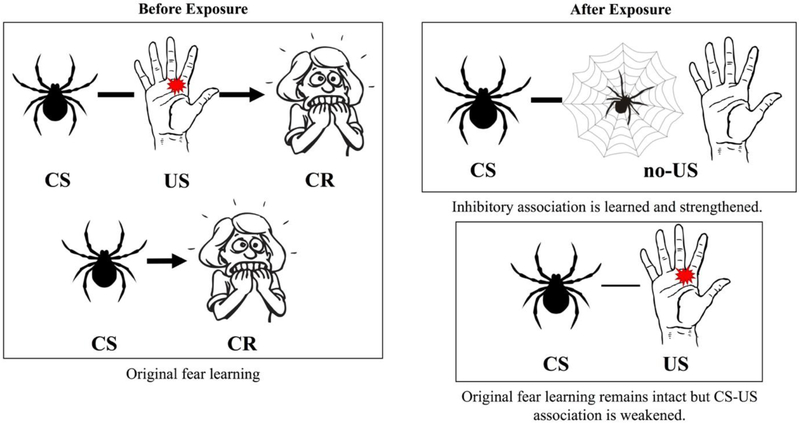
The inhibitory learning model has been proposed as an alternative explanation for the mechanisms of exposure (Craske et al., 2008). Rather than emphasizing habituation, this model asserts that learning new associations between feared objects or situations and a lack of objective danger is central to fear extinction. These new associations are strengthened through repeated exposure. From a Pavlovian conditioning perspective, the original fear learning remains intact, but new inhibitory associations between the conditioned stimulus (CS) and the unconditioned stimulus (US) are formed and strengthened (Bouton, 1993). The new learning is represented by the CS-no US pairing. For example, a person with spider phobia associates spiders (CS) with the possibility of receiving a spider bite (US), to which they react with fear. The accompanying sympathetic arousal, such as heart pounding, skin sweating, and feeling faint, becomes a conditioned response to the spider. Through exposure therapy, a new association between the spider and an absence of being bitten is learned as the client experiences spiders in a safe environment and is not harmed; this is sometimes referred to as safety learning (Vervliet et al., 2013). The goal of exposure therapy, therefore, is to strengthen this inhibitory association so that it becomes stronger than the original excitatory fear association (Figure 1). According to the inhibitory learning model, fear is not necessarily reduced in exposure; rather, an increased tolerance of fear is learned (Craske et al., 2008).
Figure 1.
The inhibitory learning model. The weight of the bar pairing the conditioned stimulus (CS) and unconditioned stimulus (US) depicts the strength of the association. A client with a spider phobia may initially associate spiders with receiving a painful bite, based on either past experience or imagined consequences. After fear learning, the spider alone will evoke fear, even without negative consequences. During repeated exposure, the client learns that seeing a spider is unlikely to result in a spider bite – most spiders are harmless and spend their time in webs, not attacking people. This is the CS-no US association. The original CS-US pairing is still intact, because the client knows that some spiders might bite, and there is a remote possibility she could come in contact with one. However, this association has been weakened, because the client has interacted with spiders in a variety of contexts and knows that the chances of a negative outcome are slim and not as severe as she imagined.
Modifying Exposure to Improve Inhibitory Learning: The Role of Variability
Increasing variability is one potential modification to the delivery of exposure therapy that could maximize inhibitory learning (Craske, Treanor, Conway, Zbozinek, & Vervliet, 2014). Variability in exposure can take many forms, including variability in the stimulus, in its presented context, or in the order in which stimuli are presented during or across sessions. It is suggested that variability enhances the storage capacity for new information and creates additional cues for memory retrieval (Bjork & Bjork, 1992, 2006; Estes, 1955). Context and stimulus variability appear to be key in the generalization of learning, which allows clients to apply what they have learned to new contexts and new stimuli that were not encountered during exposure therapy (Craske et al., 2014; Kircanski et al., 2012). The importance of variable stimuli was demonstrated by a study of spider phobia using multiple spiders in exposure, which led to better maintenance of treatment gains compared to exposure using a single spider (Rowe & Craske, 1998). Bandura and Menlove (1968) tested modeling for children with dog phobia and found that those who observed models interacting with multiple dogs of various sizes and breeds performed more approach behaviors at follow-up compared to children who observed modeled behavior with a single dog.
The order in which feared stimuli are presented can also be varied in exposure. Instead of conducting graded exposure by progressing through a hierarchy in a predictable manner, therapists could select items from the hierarchy without regard to the level of anxiety the client has assigned to the item (Craske et al., 2014). This variability is likely to produce variable levels of fear during the course of exposure, which may enhance learning. Emotional states are strong retrieval cues, and variation in fear may increase the salience of the association between a previously feared object or situation and a lack of extreme negative consequences (Bjork & Bjork, 1992, 2006; Craske et al., 2014). Although clients may learn to tolerate increasing amounts of fear as they progress through a standard exposure hierarchy, hierarchical progression is not a necessary condition of increased fear tolerance. Clients may learn to better tolerate varying levels of fear if they do not proceed linearly through a hierarchy. The unpredictability of varying the items on an exposure hierarchy creates a treatment context that not only facilitates fear tolerance but also has more external validity. Increased fear tolerance may also lead to improved self-efficacy, which predicts positive treatment outcome and is hypothesized to be a key component of therapeutic change (Bandura, 1977; Craske et al., 2008; Williams, 1990; Williams, Dooseman, & Kleinfield, 1984; Williams, Kinney, & Falbo, 1989; Williams, Turner, & Peer, 1985).
Two studies to date have examined the effects of variability in an exposure hierarchy on clinical outcomes. In a study of college students with a fear of heights, those who completed exposure in a random, variable manner by approaching the outside railing of various floors of a building in a random order experienced similar reductions in their fear of heights compared to those in the graded exposure condition, who went through exposure at gradually increasing heights. However, those in the variable exposure group reported greater reductions on a broad measure of anxiety, the Beck Anxiety Inventory, than those in the graded exposure group (Lang & Craske, 2000). These initial findings indicate that variable exposure is at least as effective as standard exposure, with variable exposure potentially leading to increased generalization in fear learning. Although reductions in the specific fear of heights were equivalent, variable exposure may have allowed participants to generalize what they learned during exposure to other anxious experiences, leading to reduced anxiety in other situations. Generalization can and does occur in the context of standard exposure (Ollendick, Öst, Reuterskiöld & Costa, 2010), but variable exposure may confer additional benefit, although more research is needed to compare these exposure techniques directly.
In a study of college students with contamination fear, participants in both the standard and variable exposure groups had decreases in contamination fear, obsessions and compulsions, and subjective fear ratings during exposure from pre- to post-treatment (Kircanski et al., 2012). Interestingly, greater variability in subjective fear was found to predict lower subjective fear at follow-up. While random, variable exposure did not lead to better outcomes than traditional graded exposure, participants who experienced more variability in their fear during the exposure session, regardless of condition, achieved lower fear ratings at follow-up. Because disgust habituates more slowly than fear (McKay, 2006; Smits, Telch, & Randall, 2002), it is possible that the effects of variable exposure on contamination fear, in which disgust is a key component, may be weaker than its effects on other phobias. Consistent with this view, a study of individuals with public-speaking fear found that those who experienced higher emotional variability during exposure had greater reduction of fear at follow-up one week later (Culver, Stoyanova, & Craske, 2012). Variability of the subjective fear experienced during exposure may be an important mechanism of change that can be facilitated by varying the items on an exposure hierarchy.
Variability in the exposure hierarchy may also enhance expectancy violation, which is proposed to maximize exposure therapy outcomes (Craske et al., 2014). Expectancy violation is based on the premise that incongruence between an expected outcome and the actual outcome is critical for learning (Rescorla & Wagner, 1972; Schultz & Dickinson, 2000). The experience of surprise, partly due to the recognition of a prediction error, enhances learning and memory recall (Alexander & Brown, 2012; Chumbley et al., 2014; Egner, 2011; Holland & Gallagher, 2006), and thus may be critical in inhibitory learning. It is theorized that surprise facilitates attention to the association being learned, which may enhance the salience and recall of that specific association (Rescorla & Wagner, 1972; Mackintosh, 1975; Schultz & Dickinson, 2000). Thus, recall of new associations between a feared object and the lack of a feared consequence resulting from interaction with that object would be strengthened if expectancies can be violated during exposure therapy. For example, a client with social anxiety who expects that others will judge him harshly in social situations avoids making eye contact with individuals in a meeting when he is asked to give a presentation. His therapist may suggest that he conduct a behavioral experiment in which he pays attention to the reactions of others during his next presentation, to see if they are actually scowling while he speaks. He is surprised to see that his coworkers are actually rather engaged during his presentation, and some even smile and nod in agreement. Because their reactions are so different from what he expected, this becomes a salient memory for the client, and he is able to more easily recall this disconfirming experience when giving subsequent presentations.
When exposure occurs under conditions that are constrained and predictable, learning tends to be contextualized. Although new learning is easily retrieved in the context of therapy, it does not always generalize to other contexts. In contrast, varying exposure (even just varying the exposure environment in an unpredictable fashion) may significantly facilitate learning. Variability in the exposure context has important implications for the return of fear (Bouton, 1993). Even when clients have successfully completed an adequate trial of exposure therapy, they may find that their anxiety returns once they leave the original treatment context, typically the therapist’s office. These effects have also been demonstrated in the laboratory in analogue samples (Culver, Stoyanova, & Craske, 2011; Mineka, Mystkowski, Hladek, & Rodriguez, 1999; Rodriguez, Craske, Mineka, & Hladek, 1999; Vervliet et al., 2013). However, when exposure is conducted in multiple contexts, clients tend to experience less return of fear than when exposure is conducted in a single context. In laboratory studies, the use of multiple contexts during exposure has led to less renewal of fear in those with spider phobia (Bandarian-Balooch, Neumann, & Boschen, 2015; Shiban, Pauli, & Mühlberger, 2013) and snake phobia (Olatunji, Tomarken, Wentworth, & Fritzsche, 2017) compared to those with whom exposure was conducted in a single context. Compared to single-context exposure, multiple-context exposure led to lower self-reported anxiety, attenuated physiological response, and greater approach in behavioral approach tasks at follow-up. The use of multiple contexts has also been found to reduce distress toward disgust stimuli, which may have implications for disorders in which disgust plays a crucial role, such as contamination-based OCD (Viar-Paxton & Olatunji, 2012).
Tolerating Uncertainty: A Potential Mechanism for Variable Exposure
Some individuals are intolerant of uncertainty, meaning they have trouble enduring “the aversive response triggered by the perceived absence of salient, key, or sufficient information, and sustained by the associated perception of uncertainty” (Carleton, 2016, p. 31). Intolerance of uncertainty may affect fear learning and fear extinction. Two recent studies have demonstrated that individuals with high intolerance of uncertainty do not discriminate between threat and safety cues during fear acquisition and have slower fear extinction than those with low intolerance of uncertainty (Morriss, Macdonald, & van Reekum, 2016; Morriss, Christakou, & van Reekum, 2016). The generalization of threat to safety cues among those high in intolerance of uncertainty compared to those low in intolerance of uncertainty is also characterized by greater activity in the amygdala (Morriss, Christakou, & van Reekum, 2015), which is a key brain structure involved in fear conditioning and extinction (Davis, 1992; Etkin & Wager, 2007; Myers & Davis, 2007; Phillips & Ledoux, 1992). These findings suggest that those high in intolerance of uncertainty may not fully benefit from traditional exposure-based interventions that are based on extinction learning principles.
Although intolerance of uncertainty was originally conceptualized as a key component underlying worry, and therefore is especially relevant in generalized anxiety disorder (GAD; Freeston, Rheaume, Letarte, Dugas, & Ladouceur, 1994; Ladouceur et al., 2000), intolerance of uncertainty has also been linked to OCD (Holaway, Heimberg, & Coles, 2006; Jacoby, Fabricant, Leonard, Riemann, & Abramowitz, 2013; Tolin, Abramowitz, Brigidi, & Foa, 2003), PTSD (Boelen, Reijntjes, & Smid, 2016; Oglesby, Boffa, Short, Raines, & Schmidt, 2016), panic disorder (Carleton et al., 2014; Carleton, Fetzner, Hackl, & McEvoy, 2013), and most other anxiety disorders (see Carleton, 2016 for a review). Intolerance of uncertainty is now considered a transdiagnostic factor across anxiety and depression (Carleton et al., 2012; McEvoy & Mahoney, 2011) and is a major potential target for treatment (Boswell, Thompson-Hollands, Farchione, & Barlow, 2013; Einstein, 2014; McEvoy & Erceg-Hurn, 2016). Variable exposure may increase tolerance of uncertainty by promoting inhibitory learning and increasing approach behavior in uncertain, real-world situations, which could potentially result in better treatment outcomes. Those high in intolerance of uncertainty may be especially prone to generalizing learned threat when uncertain, which then compromises fear extinction learning. This suggests that those high in intolerance of uncertainty may benefit from an exposure approach in which the situations or stimuli to be faced are uncertain.
Mindfulness-based treatments such as ACT emphasize the need to be flexible in the face of the unexpected and the importance of tolerating discomfort in arousing situations (Einstein, 2014). In CBT, cognitive restructuring and behavioral experiments can help address high threat estimation of uncertain events (Einstein, 2014), and therapists can address their clients’ cognitive bias that unpredictability is dangerous and intolerable. Exposure allows clients to learn that feared situations are not harmful, and that they can tolerate increased anxiety. Similarly, clients could be expected to learn through exposure that uncertainty itself is not harmful and can be tolerated. For example, a therapist with a client with a fear of dogs might conduct exposure with multiple kinds of dogs of varying sizes in a variety of locations. The client may express greater fear of German shepherds compared to dachshunds, but she may also fear not knowing what kind of dogs she will encounter on her walk to work. If she and her therapist work together in exposure situations that are not limited by a progression from small dogs to large dogs, the client may learn that she can tolerate both her fear of dogs as well as her fear of the inherent uncertainty of which dogs she may come into contact with on a daily basis.
We propose that intolerance of uncertainty is acquired, at least in part, through one’s learning history. A general fear of the unknown is common in young children, especially behaviorally inhibited young children (Kagan & Snidman, 2004), and may serve an adaptive purpose of avoiding danger when vulnerable or in the absence of a protective caretaker (Bowlby, 1973; Carleton, 2016). Individuals can also acquire high intolerance of uncertainty through observational learning of others’ (particularly caregivers’) fear and avoidance of uncertain events, or by being punished for venturing out into uncertain situations. For example, an anxious parent with high intolerance of uncertainty may be overprotective of their child and prohibit the child from playing outside unsupervised or going to a new friend’s house without having met their parents. A child who is constantly overprotected has limited experience with uncertainty and therefore cannot learn that uncertainty is not inherently dangerous, just as avoidance prevents fear extinction (or new inhibitory fear learning) and maintains long-term anxiety. In exposure therapy, the client learns new associations between uncertainty and a lack of inherent danger, and they learn to tolerate their anxiety even in uncertain situations. These associations are strengthened through practice, and variable exposure may allow for additional, more generalized learning.
Case Examples of Implementing Variable Exposure
What might the application of a variable exposure approach look like in practice? In these hypothetical case examples, we explore aspects of variability in the exposure hierarchy for adult clients with a variety of target concerns. Note that we refer to a client’s SUDS or distress level throughout the examples as a marker of the level of difficulty in the hierarchy item, rather than the client’s response to it. SUDS are not typically part of the inhibitory learning model, as there is no emphasis on habituation (Craske et al., 2014). However, clinicians might find this addition useful, especially if they are new to the inhibitory learning model and are accustomed to using SUDS in their practice. SUDS are not used to determine when to end an exposure session; instead, clinicians should focus on violating a client’s expectancy or reaching a goal set collaboratively with the client. For example, a client might set a goal of being in the room with a spider in an open cage for five minutes, regardless of how distressed they may feel. In these examples, separate SUDS data are gathered from the client to measure the distress experienced in regard to both their fear itself and the uncertainty in the situation. Separating these concepts may help some clients realize that the distress they feel is partly due to uncertainty, providing motivation to increase tolerance of uncertainty as well as fear. The use of SUDS may also benefit clients who prefer structure and concrete measures in their therapy, especially as they can see quantifiable changes in their distress levels during treatment. Clients should be reminded, however, that successful treatment is marked by the ability to do exposures even when distressing, not necessarily in the reduction of distress. Clinicians should emphasize tolerance of fear and uncertainty and being able to act in spite of being afraid as treatment goals. Finally, exposure is unlikely to be the sole component of a client’s therapy, and variability is not the only aspect of exposure that can be adapted to improve inhibitory learning. Craske and colleagues (2014) give several additional case examples of exposure therapy that maximizes inhibitory learning using additional factors beyond variability.
Specific Phobia: Kate
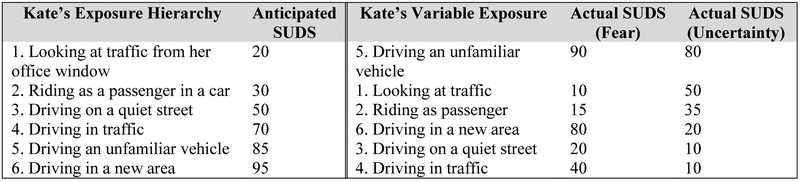
Kate is a client with a specific phobia of driving. Kate’s therapist wants to maximize the violation of expectancies during Kate’s exposure by inducing extra variability (after first confirming that Kate has sufficient skills to operate a vehicle safely). Kate is asked to discuss her fear of driving and describe multiple contexts and gradations of exposure to driving that would make her anxious. She assigns a distress rating to each of these situations and arranges them in a typical exposure hierarchy, as shown in Figure 2. The therapist then discusses the importance of learning in variable contexts and the fact that in the real world, we do not know what situations we might face on a daily basis. To demonstrate, the therapist randomly selects one of Kate’s feared tasks by rolling a die. In this first exposure, the therapist rolls a 5, and Kate is asked if she is willing to complete the task of driving an unfamiliar vehicle with the therapist. Kate is then asked what the expected outcome of driving an unfamiliar vehicle would be, and she might state that she is 95% sure she would be in a car accident if she were to drive under those conditions. Kate might then borrow a car from a friend or family member and conduct a driving exposure with the therapist in the unfamiliar vehicle. After a sufficient period of driving, during which Kate may still express high levels of fear, Kate and her therapist return to the office to discuss the outcome of the exposure. The therapist emphasizes the fact that Kate was 95% sure she would crash the car and is instead unharmed and that she was able to handle her fear despite being put into a difficult and unexpected situation. Kate and her therapist continue working through the rest of her hierarchy in random order in subsequent sessions, as summarized in Figure 2. While Kate is not particularly intolerant of uncertainty, her therapist may still consider keeping track of Kate’s SUDS in response to uncertainty to point out any potential changes in her distress as her expectancy of negative outcomes changes. Kate is likely to experience reduced distress after completing multiple sessions of exposure, but her clinician should emphasize Kate’s behavioral accomplishments rather than her reduced fear.
Figure 2.
Kate’s exposure hierarchy, variable exposure, and SUDS.
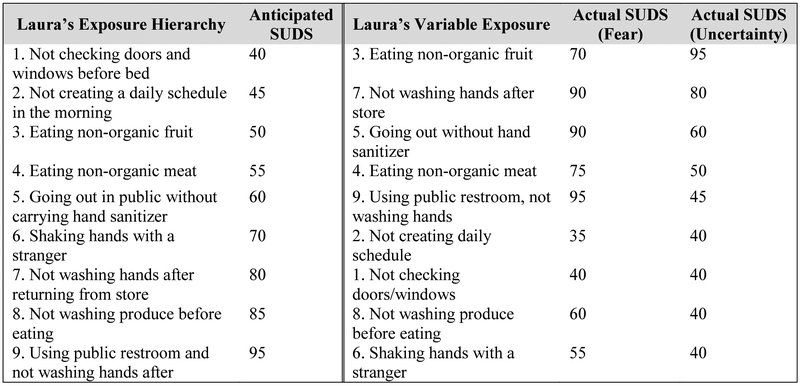
Contamination-Based OCD: Laura
Laura is a 37-year old mother of two with OCD. She has a fear of contamination, which is pervasive in many aspects of her life. She fears being contaminated from “impure, unnatural” foods and products and avoids consuming and cooking foods that are not organic. She avoids public places where she may encounter disgusting situations or sick people, such as public restrooms and waiting rooms, and she washes her hands excessively. Laura also describes herself as a perfectionist who is concerned about not raising her children “right” and feels responsible for their absolute safety at all times. She constantly checks locks, seat belts, and appliances to make sure they are safe. Laura has a high intolerance of uncertainty and plans nearly every aspect of her and her children’s days and “freaks out” if their schedules change. She presents to therapy at the urging of her husband.
Laura’s therapist decides to try random, variable exposure with Laura, with the hope that Laura might learn that while both uncertainty and potential contamination may be unpleasant, they are not inherently dangerous. She administers the short form of the Intolerance of Uncertainty Scale (Carleton, Norton, & Asmundson, 2007) at the beginning of each session to measure Laura’s progress after completing that week’s homework. Laura’s therapist also wants to increase Laura’s sense of self-efficacy by demonstrating through exposure that Laura can handle the uncertainty of being exposed to germs, even without extensive preparation. Although Laura would prefer to have a lengthy discussion about how to prepare for each exposure exercise, her therapist suggests that they give it a shot together and emphasizes that Laura will learn the most by doing, rather than talking about her fear. Laura creates a hierarchy of feared situations (see Figure 3), with many of the items involving not engaging in a compulsive behavior that could “undo” the risk of contamination after exposure (i.e., exposure and response prevention).
Figure 3.
Laura’s exposure hierarchy, variable exposure, and SUDS.
At each session, Laura’s therapist randomly selects one behavioral task that they will work on together, with repeated practice of that task in variable situations as homework. In addition to measuring Laura’s SUDS in response to confronting her contamination fear, Laura’s therapist also asks her about her SUDS in reference to confronting uncertainty as they proceed through variable exposure, as shown in Figure 3. Laura’s therapist also discusses the importance of not engaging in washing compulsions or checking rituals after these exposure exercises. Although Laura is initially very distressed by not knowing if she will become ill and seeks reassurance from her therapist, Laura’s therapist does not provide reassurance of the relative safety of each activity, rather stating that they can deal with the anxiety and discomfort of not knowing if their actions will lead to health problems, such as cancer, in the long run. Laura’s initial fear SUDS ratings are high, but her uncertainty SUDS are decreasing each week, as is her score on the Intolerance of Uncertainty Scale, meaning she is getting better at dealing with the uncertainty of each exposure. When Laura expresses some concern that she is not seeing enough improvement, Laura’s therapist uses some motivational interviewing techniques to remind Laura that she is here not only to improve her own quality of life, but to be a better wife to her husband and mother to her children. In addition, Laura’s therapist praises her for being willing to stick with treatment even though the exposures make her highly anxious, emphasizing Laura’s increased fear tolerance and not getting stuck on Laura’s limited reduction in fear. Although Laura’s SUDS tend to stay high during in-session exposures, she notices that she feels less anxious when completing homework assignments. Laura reports feeling increasingly able to handle uncertainty despite the persistence of moderate anxiety, and she tells the therapist that she has seen a decrease in her obsessive thoughts and an increased ability to resist compulsive behaviors. Laura and her therapist might decide to end therapy after seeing a clinically significant reduction in her obsessive and compulsive symptoms, with an agreement to follow-up by phone every month or so to manage any return of fear that may occur.
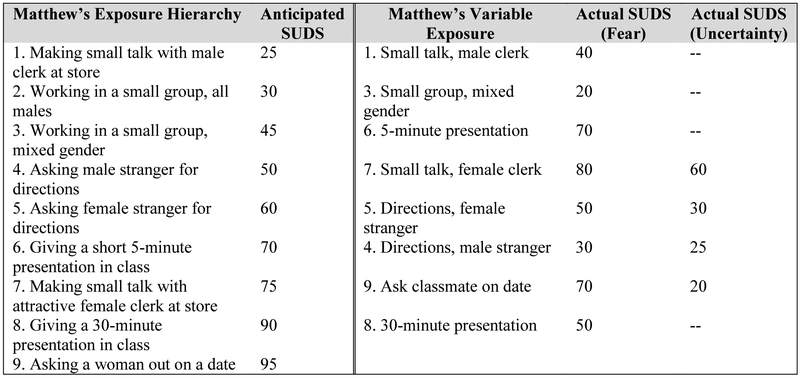
Social Anxiety: Matthew
Matthew is a 19-year-old male client with social anxiety disorder. In particular, he is concerned about public speaking when giving class presentations and interacting socially with women in the context of dating relationships. Initially, Matthew is skeptical about the idea of exposure therapy, but he is motivated to improve his social anxiety to succeed in college and his relationships. After psychoeducation on exposure therapy, fear extinction, and the inhibitory learning model, Matthew agrees to try exposure with his therapist. Matthew’s therapist also suggests that they try exposure in a variety of situations and in a variable order to maximize the learning that will take place. Matthew agrees that it will be helpful to do a lot of kinds of exposure exercises, but is concerned that he will not be able to handle starting with the most difficult items. Matthew and his therapist agree that they can start with an easy item or two and then increase the variability in the difficulty level of their exposure. Matthew creates a hierarchy, displayed in Figure 4, which includes a mix of potential exposures involving public speaking and interacting with female peers. In initial sessions, Matthew and his therapist discuss cognitive biases that underlie his social anxiety, while Matthew practices the first item on his exposure hierarchy, interacting with a male clerk at his local grocery store, for homework. In the following sessions, Matthew mentions that he has a short class presentation and some opportunities for group work in class next week. Although Matthew would prefer to work with other male students as his second exposure, during class he is assigned to a mixed gender group. He keeps a log of his SUDS during the week’s activities. Although these exposures were anticipated and did not involve a high degree of uncertainty, they involved variability in the levels of expected fear, which Matthew’s therapist thought would benefit his inhibitory learning. The following week, Matthew and his therapist decide to practice in vivo exposures together, and Matthew’s therapist writes down activities from his hierarchy and draws them out of a hat as truly random and variable exposures. Matthew has a final class assignment to complete a 30-minute presentation on a historical topic, and he and his therapist set the goal of working through the rest of the hierarchy in random order before this presentation. After the final class presentation exposure is complete, Matthew and his therapist review what he learned about himself and about others from the exposure exercises. They wrap-up therapy with Matthew agreeing to continue practicing exposure exercises as they arise in real world situations.
Figure 4.
Matthew’s exposure hierarchy, variable exposure, and SUDS.
Additional Clinical Considerations When Implementing Variable Exposure
Like Matthew, some clients may be resistant to the idea of variable exposure, even after thorough psychoeducation on the benefits of variability in exposure and the inhibitory learning model. This resistance may lead to a rupture in the therapeutic alliance or even treatment drop-out if not properly addressed. Instead of starting exposure with the premise of random progression through the exposure hierarchy, variability might be introduced after a few graded exposures of lower difficulty once the client has gained confidence in his or her ability to stay in the distressing situation (Craske et al., 2014). Clinicians should consider their client’s distress tolerance in deciding how to proceed with exposure. Clients with high distress tolerance could probably adjust to random exposure hierarchy progression without much difficulty, while clients with low distress tolerance may need a more graded approach. With these clients, the therapist might instead choose to focus on variability in other aspects of the exposure, including variable contextual factors such as location (e.g., in the office vs. at a nearby shopping mall vs. near the client’s home) and type of stimulus (e.g., many different breeds of dogs). Clinicians are encouraged to find a balance between stretching the client outside of their comfort zone and maintaining a strong working relationship. Emphasizing that effective exposure treatment involves desirable difficulties (Bjork, 1994; Craske et al., 2008; Jacoby & Abramowitz, 2016) may help clients understand that exposure is not an easy task, but tolerating discomfort and arousal and working together to attempt challenges are some of the principal goals of therapy. Variability may benefit the client, but as with traditional exposure, the process of implementing the intervention should always be a collaborative effort between client and therapist.
Randomly-selected difficult exposure items may potentially induce very high anxiety in clients. A client’s experience of high anxiety is not in itself problematic, as therapists can emphasize the importance of tolerating anxiety, and clients should not necessarily expect their anxiety to decrease during exposure after receiving psychoeducation on the inhibitory learning model. However, clients in these situations may refuse to attempt difficult exposures initially, or they may want to end a distressing exposure immediately. The role of the therapist is to be a gentle but firm coach in these situations, helping the client meet challenges head on and providing encouragement but not reassurance. In fact, helping clients avoid difficult exposures can be harmful and increase the likelihood of relapse (Gillihan, Williams, Malcoun, Yadin, & Foa, 2012). Although the therapist should certainly not force the client to complete an exposure exercise (Abramowitz, Deacon, & Whiteside, 2011), some level of resistance is common and can usually be worked through by reminding clients of the treatment rationale and their own motivations for treatment. Additionally, since within-session habituation is not a necessary component of successful exposure therapy, terminating an exposure even when the client is highly distressed may still lead to successful learning, provided that additional exposure trials are completed afterwards (Craske et al., 2008; Emmelkamp & Mersch, 1982; Rachman et al., 1986). Therapists can frame these exercises as desirable difficulties, noting that they are challenging but intentional and useful. Therapists can also help clients evaluate their experiences after exposure by discussing what was learned and emphasizing that worst outcomes (i.e., “going crazy,” death) did not occur. Clients should be praised for being willing to work hard during exposure, emphasizing effort over changes in distress. Along with motivational interviewing, these practices may help clients choose to continue with treatment even when difficult.
While violating client expectancies during therapy is typically beneficial for learning, therapists need to be careful in planning exposure exercises to avoid unnecessary failures. For clients with social anxiety, attempting to give a presentation at work or school without any prior practice may lead to negative evaluation from their peers, although the result is unlikely to be as disastrous as might be predicted by these individuals. Working on basic social skills may be necessary before exposure, but repeating skill-building exercises over and over is unlikely to benefit a socially anxious client without some exposure to feared situations. As another example, if Kate did not have sufficient driving skills, she and her therapist would need to work on building up her skills before embarking on any exposures that involve actual driving. However, difficult exposures are not necessarily dangerous. Driving an unfamiliar vehicle is a task that many individuals must do at some point in their lives and very rarely results in a car accident. For a client with a dog phobia, a therapist should not conduct exposure with a dog that has a history of aggressive behavior and biting, but the therapist should not limit themselves only to the smallest and best-behaved dogs available. The therapist has to be able to tolerate some uncertainty in the outcome of the exposure, as long as unnecessary risks are avoided.
Finally, all of our case examples involve adults who are motivated to complete exposure therapy, which may be less useful for conducting exposure therapy with children who are there at the behest of their parents. Parents will need psychoeducation about the inhibitory learning model so that they are willing to undertake these exposures at home with their child. In particular, therapists will need to make it clear to parents that providing reassurance (“I promise we’ll start with an easy item first when we do this at home”; “Nothing bad will happen when you do your homework”) is counterproductive and prevents direct exposure to the actual fear. This parental behavior is common and interferes with a child’s learning to tolerate uncertainty. Parents should also be instructed how to model approach behaviors in variable situations, helping children understand that exposure requires effort (Bandura & Adams, 1977; Bandura & Menlove, 1968). Tracking a child’s progress in a visual way (e.g., star charts, stickers) is recommended. Some children might benefit from variable exposure being introduced in the form of a game; for example, therapists and parents could frame the activities as “exposure bingo.” Anxious children might be more unwilling to accept the possibility of completing a challenging exposure right away, and emphasizing variability in the exposure stimuli or context might be more practical than introducing a variable hierarchy progression. Inhibitory learning mechanisms have been suggested to play a role in fear extinction for children with anxiety disorders as well as adults (McGuire, Orr, Essoe et al., 2016; McGuire, Orr, Wu et al., 2016), but more research examining the inhibitory learning model in exposure with children is needed.
Conclusions
Although traditional approaches to exposure therapy have called for gradual progression though the fear hierarchy, the inhibitory learning approach suggests that there may be value in a more variable approach to progressing through the fear hierarchy for some clients, along with the introduction of variability in other aspects of exposure including stimuli and context. Additional research is needed to determine (a) if random, variable exposure is more effective than traditional graded exposure, at least for some individuals, (b) if increased tolerance of uncertainty is a mediating factor in the treatment of anxiety, and (c) if tolerance of uncertainty can be increased through random, variable exposure. Potential moderators, including age, should also be examined to determine which clients might benefit from variability in the exposure hierarchy. Outcomes of variable exposure may also differ depending on whether the disorder targeted centrally involves fear (e.g., public speaking fear) or disgust (e.g., contamination fear). If intolerance of uncertainty is a more stable construct and does not change over the course of treatment, it may be a moderator of treatment outcomes instead of a mediator; individuals with high intolerance of uncertainty might experience additional benefit from learning associations between uncertainty and a lack of negative consequences in variable exposure compared to individuals with lower intolerance of uncertainty. Alternatively, individuals with very high intolerance of uncertainty may be unable to handle variable exposure and may prefer a graded approach to exposure or otherwise be unwilling to agree to treatment. It is important to note that intolerance of uncertainty is just one process that may be useful in explaining the potentially beneficial effects of a variable approach to progressing through the fear hierarchy. More research is clearly needed to examine the incremental efficacy of variable approach to progressing through the fear hierarchy as well as the various mechanisms of action posited by the inhibitory learning approach to exposure therapy.
References
- Abramowitz JS (1996). Variants of exposure and response prevention in the treatment of obsessive-compulsive disorder: A meta-analysis. Behavior Therapy, 27(4), 583–600. doi: 10.1016/S0005-7894(96)80045-1 [DOI] [Google Scholar]
- Abramowitz JS (1997). Effectiveness of psychological and pharmacological treatments for obsessive-compulsive disorder: A quantitative review. Journal of Consulting and Clinical Psychology, 65(1), 44–52. doi: 10.1037/0022-006X.65.1.44 [DOI] [PubMed] [Google Scholar]
- Abramowitz JS, Deacon BJ, & Whiteside SPH (2011). Exposure therapy for anxiety: Principles and practice. New York, NY: Guilford Press. [Google Scholar]
- Abramowitz JS, Franklin ME, & Foa EB (2002). Empirical status of cognitive-behavioral therapy for obsessive-compulsive disorder: A meta-analytic review. Romanian Journal of Cognitive and Behavioral Psychotherapies, 2(2), 89–104. [Google Scholar]
- Alexander WH, & Brown JW (2012). Medial prefrontal cortex as an action-outcome predictor. Nature Neuroscience, 14(10), 1338–1344. doi: 10.1038/nn.2921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandarian-Balooch S, Neumann DL, & Boschen MJ (2015). Exposure treatment in multiple contexts attenuates return of fear via renewal in high spider fearful individuals. Journal of Behavior Therapy and Experimental Psychiatry, 47, 138–144. doi: 10.1016/j.jbtep.2014.12.006 [DOI] [PubMed] [Google Scholar]
- Bandura A (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191–215. doi: 10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- Bandura A, & Adams NE (1977). Analysis of self-efficacy theory of behavioral change. Cognitive Therapy and Research, 1(4), 287–310. doi: 10.1007/BF01663995 [DOI] [Google Scholar]
- Bandura A, Adams NE, & Beyer J (1977). Cognitive processes mediating behavioral change. Journal of Personality and Social Psychology, 35(3), 125–139. doi: 10.13185/JM2013.01102 [DOI] [PubMed] [Google Scholar]
- Bandura A, Blanchard EB, & Ritter B (1969). Relative efficacy of desensitization and modeling approaches for inducing behavioral, affective, and attitudinal changes. Journal of Personality and Social Psychology, 13(3), 173–199. doi: 10.1037/h0028276 [DOI] [PubMed] [Google Scholar]
- Bandura A, Grusec JE, & Menlove FL (1967). Vicarious extinction of avoidance behavior. Journal of Personality and Social Psychology, 5(1), 16–23. doi: 10.1037/h0024182 [DOI] [PubMed] [Google Scholar]
- Bandura A, & Menlove FL (1968). Factors determining vicarious extinction of avoidance behavior through symbolic modeling. Journal of Personality and Social Psychology, 8(2), 99–108. doi: 10.1037/h0025260 [DOI] [PubMed] [Google Scholar]
- Barlow DH, Craske MG, Cerny JA, & Klosko JS (1989). Behavioral treatment of panic disorder. Behavior Therapy, 20(2), 261–282. doi: 10.1016/S0005-7894(89)80073-5 [DOI] [Google Scholar]
- Beckham JC, Vrana SR, May JG, Gustafson DJ, & Smith GR (1990). Emotional processing and fear measurement synchrony as indicators of treatment outcome in fear of flying. Journal of Behavior Therapy and Experimental Psychiatry, 21(3), 153–162. doi: 10.1016/0005-7916(90)90002-3 [DOI] [PubMed] [Google Scholar]
- Bjork RA (1994). Memory and metamemory considerations in the training of human beings In J., & A. P. (Eds.), Metacognition: Knowing about knowing (pp. 185–205). Cambridge, MA: The MIT Press. [Google Scholar]
- Bjork RA, & Bjork EL (1992). A new theory of disuse and an old theory of stimulus fluctuation In Healy A, Kosslyn S, & Shiffrin R (Eds.), From learning processes to cognitive processes: Essays in honor of William K. Estes. Hillsdale, NJ: Erlbaum. [Google Scholar]
- Bjork RA, & Bjork EL (2006). Optimizing treatment and instruction: Implications of a new theory of disuse In Nilsson LG, & Ohta N (Eds.), Memory and society: Psychological perspectives. New York, NY: Psychology Press. [Google Scholar]
- Boelen PA, Reijntjes A, & Smid GE (2016). Concurrent and prospective associations of intolerance of uncertainty with symptoms of prolonged grief, posttraumatic stress, and depression after bereavement. Journal of Anxiety Disorders, 41, 1–8. doi: 10.1016/j.janxdis.2016.03.004 [DOI] [PubMed] [Google Scholar]
- Boswell JF, Thompson-Hollands J, Farchione TJ, & Barlow DH (2013). Intolerance of uncertainty: A common factor in the treatment of emotional disorders. Journal of Clinical Psychology, 69(6), 630–645. doi: 10.1002/jclp.21965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulougouris JC, Marks IM, & Marset P (1971). Superiority of flooding (implosion) to desensitisation for reducing pathological fear. Behaviour Research and Therapy, 9(1), 7–16. doi: 10.1016/0005-7967(71)90030-1 [DOI] [PubMed] [Google Scholar]
- Bouton ME (1993). Context, time, and memory retrieval in the interference paradigms of Pavlovian learning. Psychological Bulletin, 114(1), 80–99. [DOI] [PubMed] [Google Scholar]
- Bowlby J (1973). Separation: Anxiety and Anger. New York, NY: Basic Books. [Google Scholar]
- Carleton RN (2016). Into the unknown: A review and synthesis of contemporary models involving uncertainty. Journal of Anxiety Disorders, 39, 30–43. doi: 10.1016/j.janxdis.2016.02.007 [DOI] [PubMed] [Google Scholar]
- Carleton RN, Duranceau S, Freeston MH, Boelen PA, McCabe RE, & Antony MM (2014). “But it might be a heart attack”: Intolerance of uncertainty and panic disorder symptoms. Journal of Anxiety Disorders, 28(5), 463–470. doi: 10.1016/j.janxdis.2014.04.006 [DOI] [PubMed] [Google Scholar]
- Carleton RN, Fetzner MG, Hackl JL, & McEvoy PM (2013). Intolerance of uncertainty as a contributor to fear and avoidance symptoms of panic attacks. Cognitive Behaviour Therapy, 42(4), 328–341. doi: 10.1080/16506073.2013.792100 [DOI] [PubMed] [Google Scholar]
- Carleton RN, Mulvogue MK, Thibodeau MA, McCabe RE, Antony MM, & Asmundson GJG (2012). Increasingly certain about uncertainty: Intolerance of uncertainty across anxiety and depression. Journal of Anxiety Disorders, 26(3), 468–479. doi: 10.1016/j.janxdis.2012.01.011 [DOI] [PubMed] [Google Scholar]
- Carleton RN, Norton PJ, & Asmundson GJG (2007). Fearing the unknown: A short version of the Intolerance of Uncertainty Scale. Journal of Anxiety Disorders, 21(1), 105–117. doi: 10.1016/j.janxdis.2006.03.014 [DOI] [PubMed] [Google Scholar]
- Choy Y, Fyer AJ, & Lipsitz JD (2007). Treatment of specific phobia in adults. Clinical Psychology Review, 27, 266–286. doi: 10.1016/j.cpr.2006.10.002 [DOI] [PubMed] [Google Scholar]
- Chumbley JR, Burke CJ, Stephan KE, Friston KJ, Tobler PN, & Fehr E (2014). Surprise beyond prediction error. Human Brain Mapping, 35(9), 4805–4814. doi: 10.1002/hbm.22513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craske MG, Brown TA, & Barlow DH (1991). Behavioral treatment of panic disorder: A two-year follow-up. Behavior Therapy, 22(3), 289–304. doi: 10.1016/S0005-7894(05)80367-3 [DOI] [Google Scholar]
- Craske MG, Kircanski K, Zelikowsky M, Mystkowski JL, Chowdhury N, & Baker AS (2008). Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy, 46(1), 5–27. doi: 10.1016/j.brat.2007.10.003 [DOI] [PubMed] [Google Scholar]
- Craske MG, Treanor M, Conway CC, Zbozinek TD, & Vervliet B (2014). Maximizing exposure therapy: An inhibitory learning approach. Behaviour Research and Therapy, 58, 10–23. doi: 10.1016/j.brat.2014.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Culver NC, Stoyanova M, & Craske MG (2011). Clinical relevance of retrieval cues for attenuating context renewal of fear. Journal of Anxiety Disorders, 25(2), 284–292. doi: 10.1016/j.janxdis.2010.10.002 [DOI] [PubMed] [Google Scholar]
- Culver NC, Stoyanova M, & Craske MG (2012). Emotional variability and sustained arousal during exposure. Journal of Behavior Therapy and Experimental Psychiatry, 43(2), 787–793. doi: 10.1016/j.jbtep.2011.10.009 [DOI] [PubMed] [Google Scholar]
- Davis M (1992). The role of the amygdala in fear and anxiety. Annual Review of Neuroscience, 15, 353–375. doi: 10.1146/annurev.neuro.15.1.353 [DOI] [PubMed] [Google Scholar]
- Davis TE, & Ollendick TH (2005). Empirically supported treatments for specific phobia in children: Do efficacious treatments address the components of a phobic response? Clinical Psychology: Science and Practice, 12(2), 144–160. doi: 10.1093/clipsy/bpi018 [DOI] [Google Scholar]
- Deacon BJ, Kemp JJ, Dixon LJ, Sy JT, Farrell NR, & Zhang AR (2013). Maximizing the efficacy of interoceptive exposure by optimizing inhibitory learning: A randomized controlled trial. Behaviour Research and Therapy, 51(9), 588–596. doi: 10.1016/j.brat.2013.06.006 [DOI] [PubMed] [Google Scholar]
- Egner T (2011). Surprise! A unifying model of dorsal anterior cingulate function? Nature Neuroscience, 14(10), 1219–1220. doi: 10.1038/nn.2932 [DOI] [PubMed] [Google Scholar]
- Einstein DA (2014). Extension of the transdiagnostic model to focus on intolerance of uncertainty: A review of the literature and implications for treatment. Clinical Psychology: Science and Practice, 21(3), 280–300. doi: 10.1111/cpsp.12077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmelkamp PMG, & Mersch PP (1982). Cognition and exposure in vivo in the treatment of agoraphobia: Short-term and delayed effects. Cognitive Therapy and Research, 6(1), 77–90. doi: 10.1007/BF01185728 [DOI] [Google Scholar]
- Eisen JL, Sibrava NJ, Boisseau CL, Mancebo MC, Stout RL, Pinto A, & Rasmussen SA (2013). Five-year course of obsessive-compulsive disorder: Predictors of remission and relapse. Journal of Clinical Psychiatry, 74(3), 233–239. doi: 10.4088/JCP.12m07657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estes WK (1955). Statistical theory of distributional phenomena in learning. Psychological Review, 62(5), 369–377. doi: 10.1037/h0046888 [DOI] [PubMed] [Google Scholar]
- Etkin A, & Wager TD (2007). Functional neuroimaging of anxiety: A meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. The American Journal of Psychiatry, 164(10), 1476–1488. doi: 10.1176/appi.ajp.2007.07030504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99(1), 20–35. doi: 10.1037/0033-2909.99.1.20 [DOI] [PubMed] [Google Scholar]
- Foa EB, Liebowitz MR, Kozak MJ, Davies S, Campeas R, Franklin ME, … Tu X (2005). Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. American Journal of Psychiatry, 162(1), 151–161. doi: 10.1176/appi.ajp.162.1.151 [DOI] [PubMed] [Google Scholar]
- Foa EB, & McLean CP (2016). The efficacy of exposure therapy for anxiety-related disorders and its underlying mechanisms: The case of OCD and PTSD. Annual Review of Clinical Psychology, 12(1), 1–28. doi: 10.1146/annurev-clinpsy-021815-093533 [DOI] [PubMed] [Google Scholar]
- Foa EB, & McNally RJ (1996). Mechanisms of change in exposure therapy. Current Controversies in the Anxiety Disorders, 329–343. [Google Scholar]
- Foa EB, Riggs DS, Massie ED, & Yarczower M (1995). The impact of fear activation and anger on the efficacy of exposure treatment for posttraumatic stress disorder. Behavior Therapy, 26, 487–499. doi: 10.1016/S0005-7894(05)80096-6 [DOI] [Google Scholar]
- Foa EB, & Wilson R (2001). Stop obsessing! New York: Bantam Books. [Google Scholar]
- Forsyth JP, Eifert GH, & Barrios V (2006). Fear conditioning in an emotion regulation context: A fresh perspective on the origins of anxiety disorders In Craske MG, Hermans D, & Vansteenwegen D (Eds.), Fear and learning: From basic processes to clinical implications (pp. 133–153). Washington, DC: American Psychological Association. [Google Scholar]
- Freeston MH, Rheaume J, Letarte H, Dugas MJ, & Ladouceur R (1994). Why do people worry? Personality and Individual Differences, 17(6), 791–802. doi: 10.1016/0191-8869(94)90048-5 [DOI] [Google Scholar]
- Gava I, Barbui C, Aguglia E, Carlino D, Churchill R, De Vanna M, & McGuire H (2009). Psychological treatments versus treatment as usual for obsessive compulsive disorder (OCD). Cochrane Database of Systematic Reviews, 1–47. doi: 10.1002/14651858.CD005333.pub2 [DOI] [PubMed] [Google Scholar]
- Gelder MG, Bancroft JHJ, Gath DH, Johnston DW, Mathews AM, & Shaw PM (1973). Specific and non-specific factors in behaviour therapy. British Journal of Psychiatry, 123(575), 445–462. doi: 10.1192/bjp.123.4.445 [DOI] [PubMed] [Google Scholar]
- Gillihan SJ, Williams MT, Malcoun E, Yadin E, & Foa EB (2012). Common pitfalls in exposure and response prevention (EX/RP) for OCD. Journal of Obsessive-Compulsive and Related Disorders, 1(4), 251–257. doi: 10.1016/j.jocrd.2012.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gould RA, Buckminster S, Pollack MH, Otto MW, & Yap L (1997). Cognitive-behavioral and pharmacological treatment for social phobia: A meta-analysis. Clinical Psychology: Science and Practice, 4(4), 291–306. doi: 10.1111/j.1468-2850.1997.tb00123.x [DOI] [Google Scholar]
- Gould RA, Ott MW, & Pollack MH (1995). A meta-analysis of treatment outcome for panic disorder. Clinical Psychology Review, 15(8), 819–844. doi: 10.1016/0272-7358(95)00048-8 [DOI] [Google Scholar]
- Grös DF, & Antony MM (2006). The assessment and treatment of specific phobias: A review. Current Psychiatry Reports, 8(4), 298–303. doi: 10.1007/s11920-006-0066-3 [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, & Wilson KG (1999). Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford Press. [Google Scholar]
- Hodgson R, Rachman S, & Marks IM (1972). The treatment of chronic obsessive-compulsive neurosis: Follow-up and further findings. Behaviour Research and Therapy, 10(2), 181–189. doi: 10.1016/S0005-7967(72)80012-3 [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Fang A, & Asnaani A (2012). Emotion dysregulation model of mood and anxiety disorders. Depression and Anxiety, 29(5), 409–416. doi: 10.1002/da.21888 [DOI] [PubMed] [Google Scholar]
- Holaway RM, Heimberg RG, & Coles ME (2006). A comparison of intolerance of uncertainty in analogue obsessive-compulsive disorder and generalized anxiety disorder. Journal of Anxiety Disorders, 20(2), 158–174. doi: 10.1016/j.janxdis.2005.01.002 [DOI] [PubMed] [Google Scholar]
- Holland PC, & Gallagher M (2006). Different roles for amygdala central nucleus and substantia innominata in the surprise-induced enhancement of learning. The Journal of Neuroscience, 26(14), 3791–3797. doi: 10.1523/JNEUROSCI.0390-06.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacoby RJ, & Abramowitz JS (2016). Inhibitory learning approaches to exposure therapy: A critical review and translation to obsessive-compulsive disorder. Clinical Psychology Review, 49, 28–40. doi: 10.1016/j.cpr.2016.07.001 [DOI] [PubMed] [Google Scholar]
- Jacoby RJ, Fabricant LE, Leonard RC, Riemann BC, & Abramowitz JS (2013). Just to be certain: Confirming the factor structure of the Intolerance of Uncertainty Scale in patients with obsessive-compulsive disorder. Journal of Anxiety Disorders, 27(5), 535–542. doi: 10.1016/j.janxdis.2013.07.008 [DOI] [PubMed] [Google Scholar]
- Kagan J, & Snidman N (2004). The long shadow of temperament. Boston, MA: Harvard College. [Google Scholar]
- Kamphuis JH, & Telch MJ (2000). Effects of distraction and guided threat reappraisal on fear reduction during exposure-based treatments for specific fears. Behaviour Research and Therapy, 38(12), 1163–1181. doi: 10.1016/S0005-7967(99)00147-3 [DOI] [PubMed] [Google Scholar]
- Kazdin AE (1974). Covert modeling, model similarity, and reduction of avoidance behavior. Behavior Therapy, 5(3), 325–340. doi: 10.1016/S0005-7894(74)80002-X [DOI] [Google Scholar]
- King NJ, & Gullone E (1990). Acceptability of fear reduction procedures with children. Journal of Behavior Therapy and Experimental Psychiatry, 21(1), 1–8. doi: 10.1016/0005-7916(90)90042-J [DOI] [PubMed] [Google Scholar]
- Kircanski K, Mortazavi A, Castriotta N, Baker AS, Mystkowski JL, Yi R, & Craske MG (2012). Challenges to the traditional exposure paradigm: Variability in exposure therapy for contamination fears. Journal of Behavior Therapy and Experimental Psychiatry, 43(2), 745–751. doi: 10.1016/j.jbtep.2011.10.010 [DOI] [PubMed] [Google Scholar]
- Kozak MJ, Foa EB, & Steketee G (1988). Process and outcome of exposure treatment with obsessive-compulsives: Psychophysiological indicators of emotional processing. Behavior Therapy, 19(2), 157–169. doi: 10.1016/S0005-7894(88)80039-X [DOI] [Google Scholar]
- Ladouceur R, Dugas MJ, Freeston MH, Léger E, Gagnon F, & Thibodeau N (2000). Efficacy of a cognitive-behavioral treatment for generalized anxiety disorder: Evaluation in a controlled clinical trial. Journal of Consulting and Clinical Psychology, 68(6), 957–964. doi: 10.1037//0022006X.68.6.957 [DOI] [PubMed] [Google Scholar]
- Lang AJ, & Craske MG (2000). Manipulations of exposure-based therapy to reduce return of fear: A replication. Behaviour Research and Therapy, 38(1), 1–12. doi: 10.1016/S00057967(99)00031-5 [DOI] [PubMed] [Google Scholar]
- Lang PJ (1977). Imagery in therapy: An information processing analysis of fear. Behavior Therapy, 8, 862–886. doi: 10.1016/S0005-7894(77)80157-3 [DOI] [PubMed] [Google Scholar]
- Lang PJ (1979). A bio-informational theory of emotional imagery. Psychophysiology, 16(6), 495–512. doi: 10.1111/j.1469-8986.1979.tb01511.x [DOI] [PubMed] [Google Scholar]
- Lang PJ, Melamed BG, & Hart J (1970). A psychophysiological analysis of fear modification using an automated desensitization procedure. Journal of Abnormal Psychology, 76(2), 220–234. doi: 10.1037/h0029875 [DOI] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, & Bernstein A (2010). Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin, 136(4), 576–600. doi: 10.1037/a0019712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackintosh NJ (1975). A theory of attention: Variations in the associability of stimuli with reinforcement. Psychological Review, 82(4), 276–298. doi: 10.1037/h0076778 [DOI] [Google Scholar]
- March JS (1995). Cognitive-behavioral psychotherapy for children and adolescents with OCD: A review and recommendations for treatment. Journal of the American Academy of Child and Adolescent Psychiatry, 34(1), 7–18. doi: 10.1097/00004583-199501000-00008 [DOI] [PubMed] [Google Scholar]
- Marks IM (1972). Perspective on flooding. Seminars in Psychiatry, 4, 129–138. [PubMed] [Google Scholar]
- Marks IM (1975). Behavioral treatments of phobic and obsessive-compulsive disorders: A critical appraisal. Progress in Behavior Modification, 1, 65–158. [Google Scholar]
- Marks IM, Boulougouris JC, & Marset P (1971). Flooding versus desensitization in the treatment of phobic patients: A crossover study. British Journal of Psychiatry, 119, 353–375. [DOI] [PubMed] [Google Scholar]
- Marshall WL, Gauthier J, Christie MM, Currie DW, & Gordon A (1977). Flooding therapy: Effectiveness, stimulus characteristics, and the value of brief in vivo exposure. Behaviour Research and Therapy, 15, 79–87. [DOI] [PubMed] [Google Scholar]
- McEvoy PM, & Erceg-Hurn DM (2016). The search for universal transdiagnostic and trans-therapy change processes: Evidence for intolerance of uncertainty. Journal of Anxiety Disorders, 41, 96–107. doi: 10.1016/j.janxdis.2016.02.002 [DOI] [PubMed] [Google Scholar]
- McEvoy PM, & Mahoney AEJ (2011). Achieving certainty about the structure of intolerance of uncertainty in a treatment-seeking sample with anxiety and depression. Journal of Anxiety Disorders, 25(1), 112–122. doi: 10.1016/j.janxdis.2010.08.010 [DOI] [PubMed] [Google Scholar]
- McGuire JF, Orr SP, Essoe JKY, McCracken JT, Storch EA, & Piacentini J (2016). Extinction learning in childhood anxiety disorders, obsessive compulsive disorder and post-traumatic stress disorder: implications for treatment. Expert Review of Neurotherapeutics, 16(10), 1155–1174. doi: 10.1080/14737175.2016.1199276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire JF, Orr SP, Wu MS, Lewin AB, Small BJ, Phares V, … Storch EA (2016). Fear conditioning and extinction in youth with obsessive-compulsive disorder. Depression and Anxiety, 33(3), 229–237. doi: 10.1002/da.22468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay D (2006). Treating disgust reactions in contamination-based obsessive-compulsive disorder. Journal of Behavior Therapy and Experimental Psychiatry, 37(1), 53–59. doi: 10.1016/j.jbtep.2005.09.005 [DOI] [PubMed] [Google Scholar]
- McLean CP, & Foa EB (2011). Prolonged exposure therapy for post-traumatic stress disorder: A review of evidence and dissemination. Expert Review of Neurotherapeutics, 11(8), 1151–1163. doi: 10.1586/ern.11.94 [DOI] [PubMed] [Google Scholar]
- Meichenbaum DH (1971). Examination of model characteristics in reducing avoidance behavior. Journal of Personality and Social Psychology, 17(3), 298–307. doi: 10.1037/h0030593 [DOI] [Google Scholar]
- Mineka S, Mystkowski JL, Hladek D, & Rodriguez BI (1999). The effects of changing contexts on return of fear following exposure therapy for spider fear. Journal of Consulting and Clinical Psychology, 67(4), 599–604. doi: 10.1037/0022-006X.67.4.599 [DOI] [PubMed] [Google Scholar]
- Morganstern KP (1973). Implosive therapy and flooding procedures: A critical review. Psychological Bulletin, 79(5), 318–334. [DOI] [PubMed] [Google Scholar]
- Morriss J, Christakou A, & van Reekum CM (2015). Intolerance of uncertainty predicts fear extinction in amygdala-ventromedial prefrontal cortical circuitry. Biology of Mood & Anxiety Disorders, 5(1), 1–13. doi: 10.1186/s13587-015-0019-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morriss J, Christakou A, & van Reekum CM (2016). Nothing is safe: Intolerance of uncertainty is associated with compromised fear extinction learning. Biological Psychology, 121, 187–193. doi: 10.1016/j.biopsycho.2016.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morriss J, Macdonald B, & van Reekum CM (2016). What is going on around here? Intolerance of uncertainty predicts threat generalization. PLoS ONE, 11(5): e0154494. doi: 10.1371/journal.pone.0154494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulds ML, & Nixon RDV (2006). In vivo flooding for anxiety disorders: Proposing its utility in the treatment posttraumatic stress disorder. Journal of Anxiety Disorders, 20(4), 498–509. doi: 10.1016/j.janxdis.2005.05.005 [DOI] [PubMed] [Google Scholar]
- Myers KM, & Davis M (2007). Mechanisms of fear extinction. Molecular Psychiatry, 12(2), 120–150. doi: 10.1038/sj.mp.4001939 [DOI] [PubMed] [Google Scholar]
- Oglesby ME, Boffa JW, Short NA, Raines AM, & Schmidt NB (2016). Intolerance of uncertainty as a predictor of post-traumatic stress symptoms following a traumatic event. Journal of Anxiety Disorders, 41, 1–6. doi: 10.1016/j.janxdis.2016.01.005 [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Tomarken A, Wentworth B, & Fritzsche L (2017). Effects of exposure in single and multiple contexts on fear renewal: The moderating role of threat-specific and nonspecific emotionality. Journal of Behavior Therapy and Experimental Psychiatry, 54, 270–277. doi: 10.1016/j.jbtep.2016.09.004 [DOI] [PubMed] [Google Scholar]
- Ollendick TH, Öst L-G, Reuterskiöld L, & Costa N (2010). Comorbidity in youth with specific phobias: Impact of comorbidity on treatment outcome and the impact of treatment on comorbid disorders. Behaviour Research and Therapy, 48(9), 827–831. doi: 10.1016/j.brat.2010.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ollendick TH, Öst L-G, Reuterskiöld L, Costa N, Cederlund R, Sirbu C, … Jarrett MA (2009). One-session treatment of specific phobias in youth: A randomized clinical trial in the United States and Sweden. Journal of Consulting and Clinical Psychology, 77(3), 504–516. doi: 10.1037/a0015158 [DOI] [PubMed] [Google Scholar]
- Öst L-G (1989). One-session treatment for specific phobias. Behaviour Research and Therapy, 27(1), 1–7. doi: 10.1016/0005-7967(89)90113-7 [DOI] [PubMed] [Google Scholar]
- Öst L-G, Alm T, Brandberg M, & Breitholtz E (2001). One vs five sessions of exposure and five sessions of cognitive therapy in the treatment of claustrophobia. Behaviour Research and Therapy, 39(2), 167–183. doi: 10.1016/S0005-7967(99)00176-X [DOI] [PubMed] [Google Scholar]
- Öst L-G, Brandberg M, & Alm T (1997). One versus five sessions of exposure in the treatment of flying phobia. Behaviour Research and Therapy, 35(11), 987–996. doi: 10.1016/S0005-7967(97)00077-6 [DOI] [PubMed] [Google Scholar]
- Öst L-G, Hellström K, & Kåver A (1992). One versus five sessions of exposure in the treatment of injection phobia. Behavior Therapy, 23(2), 263–281. doi: 10.1016/S0005-7894(05)80385-5 [DOI] [Google Scholar]
- Öst L-G, Svensson L, Hellström K, & Lindwall R (2001). One-session treatment of specific phobias in youths: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 69(5), 814–824. doi: 10.1037/0022-006X.69.5.814 [DOI] [PubMed] [Google Scholar]
- Phillips RG, & Ledoux JE (1992). Differential contribution of amygdala and hippocampus to cued and contextual fear conditioning. Behavioral Neuroscience, 106(2), 274–285. doi: 10.1037/0735-7044.106.2.274 [DOI] [PubMed] [Google Scholar]
- Pitman RK, Orr SP, Altman B, Longpre RE, Poiré RE, Macklin ML, Michaels MJ, & Steketee GS (1996). Emotional processing and outcome of imaginal flooding therapy in vietnam veterans with chronic posttraumatic stress disorder. Comprehensive Psychiatry, 37(6), 409–418. doi: 10.1016/S0010-440X(96)90024-3 [DOI] [PubMed] [Google Scholar]
- Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, & Foa EB (2010). A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review, 30(6), 635–641. doi: 10.1016/j.cpr.2010.04.007 [DOI] [PubMed] [Google Scholar]
- Powers MB, Smits JAJ, Leyro TM, & Otto MW (2007). Translational research perspectives on maximizing the effectiveness of exposure therapy In Richard DCS & Lauterbach DL (Eds.), Handbook of exposure therapies (pp. 109–126). Burlington, MA: Academic Press. [Google Scholar]
- Rachman S (1967). Systematic desensitization. Psychological Bulletin, 67(2), 93–103. doi: 10.1037/h0024212 [DOI] [PubMed] [Google Scholar]
- Rachman S (1980). Emotional processing. Behaviour Research and Therapy, 18(1), 51–60. doi: 10.1016/0005-7967(80)90069-8 [DOI] [PubMed] [Google Scholar]
- Rachman S, Craske M, Tallman K, & Solyom C (1986). Does escape behavior strengthen agoraphobic avoidance? A replication. Behavior Therapy, 17(4), 366–384. doi: 10.1016/S0005-7894(86)80069-7 [DOI] [Google Scholar]
- Rachman S, & Lopatka C (1988). Return of fear: Underlearning and overlearning. Behaviour Research and Therapy, 26(2), 99–104. doi: 10.1016/0005-7967(88)90108-8 [DOI] [PubMed] [Google Scholar]
- Rachman S, Robinson S, & Lopatka C (1987). Is incomplete fear-reduction followed by a return of fear? Behaviour Research and Therapy, 25(1), 67–69. doi: 10.1016/0005-7967(87)90116-1 [DOI] [PubMed] [Google Scholar]
- Rauch SAM, Foa EB, Furr JM, & Filip JC (2004). Imagery vividness and perceived anxious arousal in prolonged exposure treatment for PTSD. Journal of Traumatic Stress, 17(6), 461–465. doi: 10.1007/s10960-004-5794-8 [DOI] [PubMed] [Google Scholar]
- Rescorla RA, & Wagner AR (1972). A theory of Pavlovian conditioning: Variations in the effectiveness of reinforcement and non-reinforcement In Prokasy AH (Ed.), Classical conditioning II: Current research and theory (pp. 64–99). New York: Appleton-Century-Croft. [Google Scholar]
- Riley WT, McCormick MGF, Simon EM, Stack K, Pushkin Y, Overstreet MM, Carmona JJ, & Magakian C (1995). Effects of alprazolam dose on the induction and habituation processes during behavioral panic induction treatment. Journal of Anxiety Disorders, 9(3), 217–227. doi: 10.1016/0887-6185(95)00003-7 [DOI] [Google Scholar]
- Ritter B (1968). The group desensitization of children’s snake phobias using vicarious and contact desensitization procedures. Behaviour Research and Therapy, 6(1), 1–6. doi: 10.1016/0005-7967(68)90033-8 [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Holaway RM, & Heimberg RG (2004). The treatment of social anxiety disorder. Clinical Psychology Review, 24(7), 883–908. doi: 10.1016/j.cpr.2004.07.007 [DOI] [PubMed] [Google Scholar]
- Rodriguez BI, Craske MG, Mineka S, & Hladek D (1999). Context-specificity of relapse: Effects of therapist and environmental context on return of fear. Behaviour Research and Therapy, 37(9), 845–862. doi: 10.1016/S0005-7967(98)00106-5 [DOI] [PubMed] [Google Scholar]
- Rosa-Alcázar AI, Sánchez-Meca J, Gómez-Conesa A, & Marín-Martínez F (2008). Psychological treatment of obsessive-compulsive disorder: A meta-analysis. Clinical Psychology Review, 28(8), 1310–1325. doi: 10.1016/j.cpr.2008.07.001 [DOI] [PubMed] [Google Scholar]
- Rowe MK, & Craske MG (1998). Effects of varied-stimulus exposure training on fear reduction and return of fear. Behaviour Research and Therapy, 36(7-8), 719–734. doi: 10.1016/S00057967(97)10017-1 [DOI] [PubMed] [Google Scholar]
- Schultz W, & Dickinson A (2000). Neuronal coding of prediction errors. Annual Review of Neuroscience, 23, 473–500. doi: 10.1146/annurev.neuro.23.1.473 [DOI] [PubMed] [Google Scholar]
- Shaw DW, & Thoresen CE (1974). Effects of modeling and desensitation in reducing dentist phobia. Journal of Counseling Psychology, 21(5), 415–420. doi: 10.1037/h0037102 [DOI] [Google Scholar]
- Shiban Y, Pauli P, & Mühlberger A (2013). Effect of multiple context exposure on renewal in spider phobia. Behaviour Research and Therapy, 51(2), 68–74. doi: 10.1016/j.brat.2012.10.007 [DOI] [PubMed] [Google Scholar]
- Simpson HB, Franklin ME, Cheng J, Foa EB, & Liebowitz MR (2005). Standard criteria for relapse are needed in obsessive-compulsive disorder. Depression and Anxiety, 21(1), 1–8. doi: 10.1002/da.20052 [DOI] [PubMed] [Google Scholar]
- Smith RD, Dickson AL, & Sheppard L (1973). Review of flooding procedures (implosion) in animals and man. Perceptual and Motor Skills, 37, 351–374. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Telch MJ, & Randall PK (2002). An examination of the decline in fear and disgust during exposure-based treatment. Behaviour Research and Therapy, 40, 1243–1253. doi: 10.1016/S0005-7967(01)00094-8 [DOI] [PubMed] [Google Scholar]
- Taylor S (1996). Meta-analysis of cognitive-behavioral treatments for social phobia. Journal of Behavior Therapy and Experimental Psychiatry, 27(1), 1–9. doi: 10.1016/0005-7916(95)00058-5 [DOI] [PubMed] [Google Scholar]
- Telch MJ, Valentiner DP, Ilai D, Young PR, Powers MB, & Smits JAJ (2004). Fear activation and distraction during the emotional processing of claustrophobic fear. Journal of Behavior Therapy and Experimental Psychiatry, 35(3), 219–232. doi: 10.1016/j.jbtep.2004.03.004 [DOI] [PubMed] [Google Scholar]
- Tolin DF, Abramowitz JS, Brigidi BD, & Foa EB (2003). Intolerance of uncertainty in obsessive-compulsive disorder. Journal of Anxiety Disorders, 17(2), 233–242. doi: 10.1016/S0887-6185(02)00182-2 [DOI] [PubMed] [Google Scholar]
- Tryon WW (2005). Possible mechanisms for why desensitization and exposure therapy work. Clinical Psychology Review, 25(1), 67–95. doi: 10.1016/j.cpr.2004.08.005 [DOI] [PubMed] [Google Scholar]
- Tsao JCI, & Craske MG (2000). Timing of treatment and return of fear: Effects of massed, uniform, and expanding exposure schedule. Behavior Therapy, 31, 479–497. doi: 10.1016/S0005-7894(00)80026-X [DOI] [Google Scholar]
- Vervliet B, Craske MG, & Hermans D (2013). Fear extinction and relapse: State of the art. Annual Review of Clinical Psychology, 9, 215–48. doi: 10.1146/annurev-clinpsy-050212-185542 [DOI] [PubMed] [Google Scholar]
- Viar-Paxton M, & Olatunji BO (2012). Context effects on habituation to disgust-relevant stimuli. Behavior Modification, 36(5), 705–722. doi: 10.1177/0145445512446189 [DOI] [PubMed] [Google Scholar]
- Watts F (1971). Desensitization as an habituation phenomenon: I. Stimulus intensity as determinant of the effects of stimulus lengths. Behaviour Research and Therapy, 9(3), 209–217. doi: 10.1016/0005-7967(71)90006-4 [DOI] [PubMed] [Google Scholar]
- Williams SL (1990). Guided mastery treatment of agoraphobia: Beyond stimulus exposure In Hersen M, Eisler RM, & Miller PM (Eds.), Progress in behavior modification (Vol. 26, pp. 89–121). Thousand Oaks, CA: Sage. [PubMed] [Google Scholar]
- Williams SL, Dooseman G, & Kleinfield E (1984). Comparative effectiveness of guided mastery and exposure treatments for intractable phobias. Journal of Consulting and Clinical Psychology, 52(4), 505–518. doi: 10.1037/0022-006X.52.4.505 [DOI] [PubMed] [Google Scholar]
- Williams SL, Kinney PJ, & Falbo J (1989). Generalization of therapeutic changes in agoraphobia: The role of perceived self-efficacy. Journal of Consulting and Clinical Psychology, 57(3), 436–442. doi: 10.1037/0022-006X.57.3.436 [DOI] [PubMed] [Google Scholar]
- Williams SL, Turner SM, & Peer DF (1985). Guided mastery and performance desensitization treatments for severe acrophobia. Journal of Consulting and Clinical Psychology, 53(2), 237–247. doi: 10.1037/0022-006X.53.2.237 [DOI] [PubMed] [Google Scholar]
- Wirtz CM, Hofmann SG, Riper H, & Berking M (2014). Emotion regulation predicts anxiety over a five-year interval: A cross-lagged panel analysis. Depression and Anxiety, 31(1), 87–95. doi: 10.1002/da.22198 [DOI] [PubMed] [Google Scholar]
- Wolpe J (1958). Psychotherapy by reciprocal inhibition. Stanford, CA: Stanford University Press. [Google Scholar]
- Wolpe J (1961). The systematic desensitzation treatment of neuroses. The Journal of Nervous and Mental Disease, 132(3), 189–203. [DOI] [PubMed] [Google Scholar]