Abstract
Objectives:
To compare the clinical value of three frailty indicators in a screening pathway for identifying older men and women who are at risk of falls.
Design:
A prospective cohort study.
Setting and Participants:
Four thousand Chinese adults (2000 men) aged 65 years or above were recruited from the community in Hong Kong.
Methods:
The Cardiovascular Health Study Criteria (CHS), the FRAIL scale, and the Study for Osteoporosis and Fracture Criteria (SOF) were included for evaluation. Fall history was used as a comparative predictor. Recurrent falls during the second year after baseline was the primary outcome. The area under the receiver operating characteristic curve (AUC) was used to evaluate the ability of the frailty indicators and fall history to predict recurrent falls. Independent predictors identified in logistic regression were put in the Classification and Regression Tree (CART) analysis to evaluate their performance in screening high-risk fallers.
Results:
Fall history predicts recurrent falls in both men and women (AUC: men=0.681; women=0.645) better than all frailty indicators (AUC≤0.641). After adjusting for fall history, only FRAIL (AUC=0.676) and SOF (AUC=0.673) remained as significant predictors for women while no frailty indicator remained significant in men.
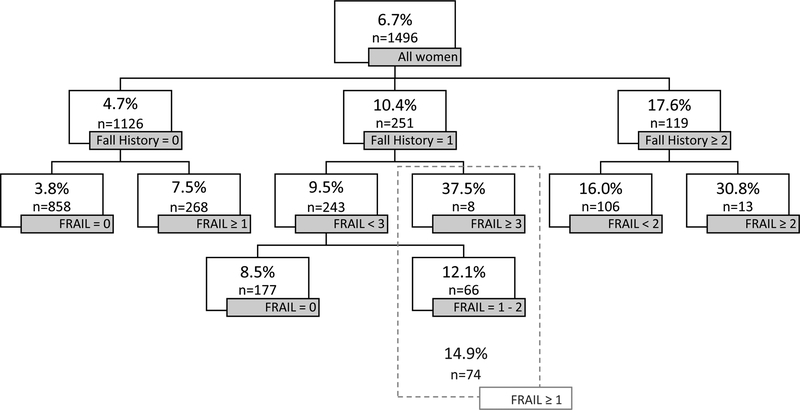
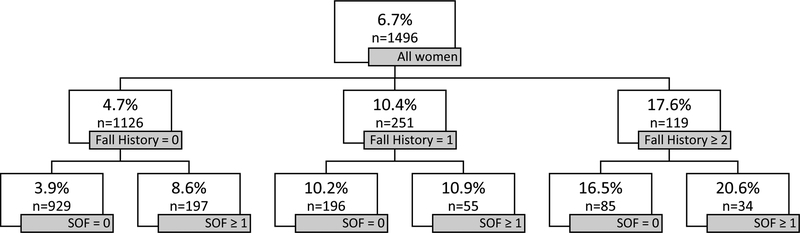
FRAIL could classify older women into two groups with distinct chances of being a recurrent faller in people with no fall history (3.8% vs 7.5%), a single fall history (9.5% vs 37.5%), and history of recurrent falls (16.0% vs 30.8%). SOF has limited ability in identifying recurrent fallers in the group of elderly with a single fall history (no fall history: 3.9% vs 8.6%; single fall history: 10.2% vs 10.9%; history of recurrent falls: 16.5% vs 20.6%).
Conclusion and Implication:
SOF and FRAIL could provide some additional prediction value to fall history in older women but not men. FRAIL could be clinically useful in identifying older women at risk of recurrent falls, especially in those with a single fall history.
Keywords: Frailty, falls, screening, elderly
Brief summary:
The FRAIL scale could be clinically useful in identifying older women at risk of recurrent falls, especially in those with a single fall history.
Introduction
Frailty is a syndrome to describe the decrease in reserve and resistance to stressors due to the accumulation of deficits in multiple physiologic systems.1,2 This causes an increase in the vulnerability to adverse outcomes.3 Frailty was found to be associated with multiple adverse health outcomes, which includes mortality, hospitalization, disability and falls.4,5
Among these adverse health outcomes, fall is a manifestation of frailty before progressing to disability and mortality.6 About one-third of the elderly over 60 years old fall once or more in one year.7,8 It causes serious complications including fear of falling, restriction in activities and fractures.9,10 Risk factors of falls, which include a reduction in muscle strength and mobility functions, closely resemble the characteristics of frailty.11–14 Therefore, it has been a rising interest in using frailty assessments to predict falls. Two recently published systematic reviews concluded that frailty indicators based on the assessment of clinical phenotypes are significant predictors of future falls.15,16 It suggests that frailty assessment could be used to identify older adults with high fall risk for interventions.
However, before concluding that these frailty indicators based on phenotypes have a role in clinical practice to identify people at high risk of falls, their comparative and additional value on top of existing, simple fall predictors have to be evaluated. History of falls has consistently been found to be one of the strongest predictors of future falls and is utterly easy to assess.11,17,18 Indeed, according to the practice guideline for prevention of falls in older persons as formulated by the American and British Geriatrics Society, history of falls is the most important screening criteria used for identifying community-dwelling older people at high risk of fall.19 Fall history well serves as the benchmark predictor for comparison.
Unfortunately, existing studies have rarely included the history of falls as a covariate while establishing the predictive ability of frailty indicators on falls.16,20–23 Only a few studies have considered falls as a confounding variable in their analyses and the results on whether frailty remained as a predictor of falls were mixed.17,24,25 Contradicting results were also reported when predicting models were conducted separately in people with or without a history of falls at baseline.26,27 Hence, whether assessments of frailty have clinical value on the prediction of future falls remains uncertain. A possible reason for the disparity in results could be the difference in frailty indicators included for evaluation. A comprehensive evaluation that included the major frailty indicators based on clinical phenotypes has to be performed. Further, it is important to evaluate the possible role of frailty indicators in a clinically useable pathway. To the best of our knowledge, no attempt of incorporating frailty indicator in a clinical pathway for identifying potential fallers is currently available.
To answer the above questions, this study has four aims. First, to provide a comparison of the fall prediction ability of frailty indicators based on clinical phenotypes. Second, to compare these assessments against fall history, a simple and well-validated predictor, in the prediction of recurrent falls. Third, to assess the combined effect of fall history and frailty assessment on fall prediction. Finally, to evaluate the role of frailty indicators in a practical model for identifying future recurrent fallers.
METHODS
Participants
Four thousand community-dwelling older men and women aged 65 and above attended an initial assessment at the School of Public Health of the Chinese University of Hong Kong from August 2001 to December 2003 for the Mr. OS and Ms. OS Hong Kong cohort study. The participants were mainly recruited through posting advertisement in housing estates and local community centers. The sample was age-stratified so there is an approximately equal number of participants in the age range of 65 to 69, 70 to 74, and 75 or older. Individuals with the following characteristics were excluded from the study: (1) unable to walk independently, (2) had bilateral hip replacement, (3) had a reduced chance of survival in the 4 years following recruitment due to known medical condition (e.g., cancer, heart diseases, end-stage renal diseases, chronic lung diseases), (4) inability to provide informed consent. The methodology has been previously described.28 All surviving participants were invited to a second examination between August 2003 and December 2005 (n=3427; men=1745), from which the information collected was used as a baseline in the present analysis and provided data required to formulate all candidate frailty indicators. Data from the third examination between August 2005 and November 2008 (n=3153; men=1566) provided prospective fall information. The study was approved by the clinical research ethics committee of the Chinese University of Hong Kong and informed consents were obtained from the participants.
Assessment
Each participant completed a series of assessments in one day in each visit with a team of trained research assistants. The detailed information about the assessments was previously published.5 The data collected in the second visit, including grip strength, the time taken to walk 6 meters, and the ability to complete the five-time repeated chair stand test, was used in calculating the scores of all the frailty indicators. Weight loss in two years was calculated by the difference in weight between the first and second visit. Questionnaires were used to obtain information about physical activity level, self-reported health, and medical history.
Calculation of the frailty indicators
Cardiovascular Health Study Criteria (CHS)
CHS is a commonly used clinical frailty assessment tools.3 It measures five criteria including exhaustion, unintentional weight loss of 5%, grip strength in the lowest quintile, walking speed in the lowest quintile, and energy expenditure in the lowest quintile. Matching each criterion would score 1 point. The total score ranges from 0–5 with a higher score indicating an increase in frailty.
FRAIL scale (FRAIL)
FRAIL was proposed as a bedside screening tool for measuring frailty.29,30 The domains assessed by FRAIL are largely similar to CHS. It also examines exhaustion, weight loss, strength and walking ability but it assesses the number of illnesses instead of low energy expenditure as in CHS. The advantage of the FRAIL scale is that a quintile from a population range is not required as no cutoff is needed for scoring. The presence of a symptom would score one point on the FRAIL scale, which has a total score of five.
Study for Osteoporosis and Fracture Criteria (SOF)
SOF is the simplest frailty indicator included in this study.22 It was designed to be practical for use in clinical practice. A similar rating system to the FRAIL scale is adopted so that no population range is required. It consists of only three items, which capture exhaustion, weight loss and the inability to perform five chair stands. The presence of one of the above symptoms would score one point on the SOF scale, which has a total score of three.
Equivalent variables that were used to calculate scores of the three frailty indicators in the present study were listed in Table 1.
Table 1.
Criteria of the three frailty indicators based on clinical phenotypes
| Definition | Variable used | CHS | FRAIL | SOF |
|---|---|---|---|---|
| Exhaustion / Fatigue | Reporting no energy | √ | √ | √ |
| Unintentional weight loss / Weight loss >5% | Unintentional weight loss / Weight loss >5% in past 2 years | √ | √ | √ |
| Grip strength in the lowest quintile | Grip strength in the lowest quintile | √ | ||
| Inability to climb one flight of stairs | Cannot climb up 10 steps | √ | ||
| Inability to do 5 chair stand | Unable to complete the 5 times repeated chair stand test | √ | ||
| Walking speed in the lowest quintile | Walking speed in the lowest quintile | √ | ||
| Ambulation (inability to walk one block) | Having some problem in walking | √ | ||
| Low energy expenditure (PASE in the lowest quintile) | PASE in the lowest quartile | √ | ||
| > 5 illnesses | > 5 diseases | √ | ||
| Total score | 5 | 5 | 3 |
Fall record
Participants were interviewed for their history of falls in the previous year at baseline, which was used as a comparative predictor.
Prospective fall, the primary outcome, was recorded in the third visit. The number of fall in the previous year was collected in an interview. Recurrent fallers were those who had two or more falls during the 1-year period. A fall was defined as any unintentional rest on the ground resulting from a loss of balance.
Statistical analysis
Statistical analysis was conducted using the statistical package SAS, version 9.4 (SAS Institute, Inc., Cary, NC) except that Classification and Regression Tree (CART) was done by the R software (version 3.5.1). Men and women were analyzed separately as gender was found to be a significant contributor to the heterogeneity in the prediction of falls by frailty indicators in a recent meta-analysis.15 Logistic regression was conducted to evaluate the ability of various frailty indicators and fall history on the prediction of recurrent falls. Receiver operating characteristic (ROC) curve was constructed to evaluate the ability of different frailty indicators and past fall history to discriminate between non-recurrent fallers and recurrent fallers in the follow-up. The area under the ROC curve (AUC) was used to measure the concordance of the predictive values with the actual outcomes. The differences in AUCs across the predictive models were compared using chi-square test of homogeneity. Frailty indicators that were found to be significant predictors of recurrent falls would be put into the CART analysis to identify a practical screening process for efficient fall risk screening. All statistical tests were two-sided. A P-value of less than 0.05 was considered statistically significant.
RESULTS
Characteristics of the 3427 participants assessed at baseline were presented in Table 2. The percentage of participants who had one or more falls during the follow-up period was 15.5% for men and 22.4% for women while those had two or more falls was 4.2% for men and 6.5% for women.
Table 2.
Participants’ characteristics
| Mean (SD)/ Freq (%) | P-value* | ||
|---|---|---|---|
| Men (n=1745) |
Women (n=1682) |
||
| Age | 73.9 (4.9) | 74.1 (5.2) | 0.379 |
| History of falls at baseline | < 0.001 | ||
| none | 1440 (82.5%) | 1272 (75.6%) | |
| 1 | 224 (12.8%) | 282(16.8%) | |
| 2 or more | 81 (4.6%) | 128 (7.6%) | |
| Cardiovascular Health Study Criteria (CHS) | < 0.001 | ||
| 0 | 789 (45.2%) | 633 (37.6%) | |
| 1 | 582 (33.4%) | 581 (34.5%) | |
| 2 | 268 (15.4%) | 303(18.0%) | |
| 3 | 90 (5.2%) | 123 (7.3%) | |
| 4 | 15 (0.86%) | 38 (2.3%) | |
| 5 | 1 (0.06%) | 4 (0.24%) | |
| FRAIL scale (FRAIL) | < 0.001 | ||
| 0 | 1392 (79.8%) | 1227 (73.0%) | |
| 1 | 299(17.1%) | 344 (20.5%) | |
| 2 | 38 (2.2%) | 80 (4.8%) | |
| 3 | 14 (0.8%) | 29(1.7%) | |
| 4 | 2(0.11%) | 2 (0.12%) | |
| 5 | 0 (0%) | 0 (0%) | |
| Study for Osteoporosis and Fracture Criteria (SOF) | < 0.001 | ||
| 0 | 1499 (85.9%) | 1339 (79.6%) | |
| 1 | 236(13.5%) | 315(18.7%) | |
| 2 | 9 (0.52%) | 27(1.6%) | |
| 3 | 1 (0.06%) | 1 (0.06%) | |
| Number of fall during follow-up | < 0.001 | ||
| none | 1324 (84.6%) | 1229 (77.6%) | |
| 1 | 177(11.3%) | 252(15.9%) | |
| 2 or more | 65 (4.2%) | 103 (6.5%) | |
P-value of t-test or chi-square test
After adjusting for age, fall history predicted recurrent falls in both men and women (AUC: men=0.681; women=0.645). Only the FRAIL criteria predicted recurrent falls in men (OR=1.59; 95%CI=1.08–2.32; AUC=0.641). CHS and SOF criteria were marginally insignificant. In women, both FRAIL and SOF significantly predicted recurrent falls (FRAIL: OR=1.25, 95%CI=1.25–2.09, AUC=0.607; SOF: OR=1.77, 95%CI=1.20–2.63, AUC=0.586) (Table 3). The AUC of fall history was the highest in both sexes. After additionally adjusting for fall history, FRAIL became insignificant in men; while FRAIL and SOF remained significant for women in logistic regression (Table 3). The increases in AUC upon adding FRAIL and SOF in the prediction model, on top of fall history and age, were marginally significant in women (p≤0.078).
Table 3.
Prediction ability of frailty indicators on recurrent falls
| Men | Women | |||||
|---|---|---|---|---|---|---|
| OR (95%CI) |
AUC | p-value§ | OR (95%CI) |
AUC | p-value§ | |
| CHS† | 1.29 (0.98, 1.70) | 0.634 | 1.15 (0.94, 1.41) | 0.565 | ||
| FRAIL† | 1.59 (1.08,2.32)* |
0.641 | 1.62 (1.25,2.09)* | 0.607 | ||
| SOF† | 1.80 (0.99, 3.26) | 0.634 | 1.77 (1.20,2.63)* | 0.586 | ||
| Fall History† | ||||||
| None | Reference | 0.681 | Reference | 0.645 | ||
| 1 | 2.21 (1.15,4.25)* | 2.32 (1.42,3.79) | ||||
| 2 or more | 7.27 (3.63, 14.55)* | 4.35 (2.52, 7.50) | ||||
| CHS‡ | 1.20 (0.91, 1.58) |
0.693 | 0.297 | 1.10 (0.89, 1.35) | 0.656 | 0.440 |
| FRAIL‡ | 1.35 (0.91, 2.00) | 0.683 | 0.816 | 1.48 (1.14, 1.93)* | 0.676 | 0.064 |
| SOF‡ | 1.57 (0.86, 2.88) | 0.678 | 0.806 | 1.57 (1.06,2.35)* | 0.673 | 0.078 |
P-value < 0.05
Adjusted for age
Adjusted for age and history of falls
P-value indicating the difference in AUC between the model including the frailty indicator on top of fall history and age, and the model including only fall history and age.
CART analyses were hence conducted in women, using FRAIL and SOF as potential candidates. Considering that history of falls is stronger than all frailty indicators in the prediction of recurrent falls, CART analyses were conducted separately for subjects with no fall history, those with a single fall history, and those who had equal or more than two falls. For FRAIL, the cutoff scores identified were one, three, and two for the three subgroups respectively. These cutoffs effectively separated older women into two groups with distinct chances of becoming recurrent fallers (no fall history: 3.8% vs 7.5%; a single fall history: 9.5% vs 37.5%; history of recurrent falls: 16.0% vs 30.8%). A secondary cutoff for people with a single fall history was identified at the score of one (Figure 1). If a score of one was used as an initial cutoff, the chance of being a recurrent faller would be 8.5% and 14.9% for the low- and high-risk group respectively. For SOF, a consistent cutoff at the score of one was identified in all three groups (Figure 2). It had limited ability to predict recurrent falls in people with a single fall history (no fall history: 3.9% vs 8.6%; a single fall history: 10.2% vs 10.9%; history of recurrent falls: 16.5% vs 20.6%).
Figure 1. CART decision tree for using the FRAIL criteria to predict recurrent falls in older women stratified by fall history.
The percentage in the box indicates the percentage of recurrent fallers.
Figure 2. CART decision tree for using the SOF criteria to predict recurrent falls in older women stratified by fall history.
The percentage in the box indicates the percentage of recurrent fallers.
DISCUSSION
This is the first study that explores the potential clinical role of frailty indicators on screening for elderly at risk of falls. The predictive ability of all frailty indicators and history of falls were better in men than women after adjusting for age. A cohort that separated men and women for the analysis of CHS and SOF in predicting falls also yielded similar results (AUC: men=0.63; women=0.61).22,23 Reasons causing the gender disparity remain largely unclear.15
Among the three frailty indicators, FRAIL had the best ability to predict recurrent falls in women, followed by SOF. CHS had the worst predictive ability. A previous study conducted in the United States reported that the predictive ability of CHS and SOF were essentially the same in older women (AUC=0.61).22 However, SOF (AUC=0.59) had better predictive ability than CHS (AUC=0.57) in the present study conducted in Hong Kong. This could be attributed to the difference in frailty distribution across the frailty indicators between the two samples. The frailty distributions in SOF (47% of the participants has a score = 0) and CHS (37% of the participants has a score = 0) were largely similar in the study conducted in the United States.22 However, 73% of the women in our study scored zero in SOF while only 37% scored zero under the CHS criteria. The vast difference in frailty distribution across the frailty indicators could be due to the fact that our samples were less frail compared with those in the United States.22 This has a great impact on CHS as it adopts a relative scoring system. All participants in the lowest quintile received one score in three of the five items. SOF and FRAIL adopted an absolute scoring system where scores were given only upon the presence of the frailty characteristics. Together with previous studies, our finding showed that the absolute scoring system used in SOF and FRAIL may provide a more consistent result independent of the population data. In men, FRAIL is the only criteria that could significantly predict recurrent falls and has the strongest predictive ability. The result yielded in CHS and SOF were very similar to the finding in the study conducted in the United States (AUC=0.63).23
None of the frailty indicators could outperform fall history in the prediction of recurrent falls. The frailty indicators included in the analysis primarily assess physical functioning of the older people. However, falls have multifactorial risk factors, including visual deficit, cognitive impairment, depression, medication, environmental risk and etc.14,31 These factors might have contributed in previous fall episodes and at the same time predisposed the elderly to falling in the future. This may explain the fact that fall history is a better predictor to future falls than all candidate frailty indicators. The clinical value of frailty indicators on identifying potential recurrent fallers resorts to its ability to provide additional value to fall history.
In women, FRAIL and SOF, but not CHS, could provide additional predictive ability on top of fall history. In men, all frailty indicators failed to provide additional value on top of fall history. The difference in the finding across gender could be because fall history alone can better predict future recurrent falls in men than women (AUC: 0.681 vs 0.645). There is thus less room for the frailty indicators to provide additional predictive ability. Unfortunately, no previous study that has analyzed men and women separately with the adjustment for fall history is available for comparison. All existing studies that provided adjustment for fall history recruited either only women or both genders. The study involved only women reported a significant result,24 whereas the study included both genders reported an insignificant finding in a multivariate model using the backward elimination approach.17 Despite multiple factors (i.e., sample size, population) might have contributed to the difference in results, this might be a piece of indirect supportive evidence to our finding that frailty indicators may provide added value to predict recurrent falls only in women.
In order to examine how the frailty indicators can assist in identifying future recurrent fallers in clinical practice, CART analysis was incorporated to identify cutoff scores. Fall history was used as a first line screening due to its better predictive ability and ease of assessment. We found that the FRAIL criteria could effectively separate older women with distinct fall risks in all three categories (i.e., no fall history, a single fall history, history of recurrent falls). SOF, however, was ineffective in people with a single fall history.
People with a history of recurrent falls in the previous year have a greatly increased fall risk and should undergo a comprehensive fall risk assessment regardless of the score of the frailty indicators.19 However, in this group of older women, we would be able to identify those at a very high risk of falls using the FRAIL criteria (30.8% risk of recurrent falls). This is more clinically useful than the screening achieved by the SOF (20.6% risk of recurrent falls) given the overall risk of being a recurrent faller in the future is 17.6% in older women with a history of recurrent falls.
Both the SOF and FRAIL were effective in identifying older women with higher fall risk in those without any history of fall in the previous year. SOF was slightly better in isolating the higher risk population in this group. However, the absolute risk in the high-risk group identified by the two frailty indicators in people with no history of fall remained relatively low at 7.5% for FRAIL and 8.6% for SOF. The number of frailty assessment that has to be conducted is also large as the majority of the population has no fall history at baseline.8,32
Frailty assessment would hence be the most valuable in people with a single history of fall. With the cutoff score of one, the FRAIL criteria could identify 74 out of 251 participants who had a 14.9% chance of being a recurrent faller versus 8.5% in the remaining 177 participants, which indicates a 75% increase in risk. The high-risk group has a chance of becoming a recurrent faller close to those who had a history of recurrent falls (17.6%). Those with a FRAIL score of three or more even have the rate hiked up to 37.5% (i.e., three in eight participants). Given that FRAIL is a simple assessment that can be easily used during a medical encounter or even as a self-administered questionnaire,30 it has sound clinical potential for screening fall risk in older women who experienced a single fall in the past year. SOF failed to provide a meaningful separation in this group.
Despite the large sample size we have in this cohort, the number of recurrent fallers during follow-up is small due to the low fall rate. Fall incidence was recorded with a recall period of 1 year, which may underestimate the number of falls experienced by the subjects by approximately 13%.33 Still, our fall rate matches well with other studies conducted in the Chinese population.8 This indicates that our data is reasonably representative. The distributions of frailty indicators are right-skewed, the weighting of the larger value of frailty indicators was smaller than that of the smaller value. So the odds ratio of frailty indicators estimated for recurrent fall may be underestimated. We have included only individuals who can walk and come to our center for assessment. Our participants represent a healthier sample of the community population in Hong Kong. Surrogates were used in some of the items that composed the frailty indicators.
CONCLUSIONS AND IMPLICATIONS
FRAIL has the highest predictive ability to future recurrent falls in older men and women compare with other frailty indicators. However, none of the frailty indicators is better in predicting recurrent falls than fall history. SOF and FRAIL could provide some additional prediction value to fall history in older women but not men. Particularly in people with a single history of fall, FRAIL has potential clinical value in identifying older women at risk of recurrent falls.
Acknowledgement:
The authors would like to thank the Jockey Club Centre for Osteoporosis Care and Control for their assistance in data collection and all the participants for contributing to the study.
Funding sources: This work was supported by the National Institutes of Health (grant R01 AR049439-01A1) and the Research Grants Council Earmarked (grant CUHK4101/02 M)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of Deficits as a Proxy Measure of Aging. Sci World J 2001;1:323–336. doi: 10.1100/tsw.2001.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walston J, Hadley EC, Ferrucci L, et al. Research Agenda for Frailty in Older Adults: Toward a Better Understanding of Physiology and Etiology: Summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc. 2006;54(6):991–1001. doi: 10.1111/j.1532-5415.2006.00745.x [DOI] [PubMed] [Google Scholar]
- 3.Fried LP, Tangen CM, Walston J, et al. Frailty in Older Adults: Evidence for a Phenotype. J Gerontol Ser A Biol Sci Med Sci. 2001;56(3):M146–M157. doi: 10.1093/gerona/56.3.M146 [DOI] [PubMed] [Google Scholar]
- 4.De Vries OJ, Peeters GMEE, Lips P, Deeg DJH Does frailty predict increased risk of falls and fractures? A prospective population-based study. Osteoporos Int. 2013;24(9):2397–2403. doi: 10.1007/s00198-013-2303-z [DOI] [PubMed] [Google Scholar]
- 5.Woo J, Leung J, Morley JE. Comparison of frailty indicators based on clinical phenotype and the multiple deficit approach in predicting mortality and physical limitation. J Am Geriatr Soc. 2012;60(8):1478–1486. doi: 10.1111/j.1532-5415.2012.04074.x [DOI] [PubMed] [Google Scholar]
- 6.Morley JE, Perry HM III, Miller DK. Editorial: Something about frailty. J Gerontol A Biol Sci Med Sci. 2002;57(11):698–704. doi: 10.1093/gerona/57.11.M698 [DOI] [PubMed] [Google Scholar]
- 7.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane database Syst Rev. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kwan MMS, Close JCT, Wong AKW, Lord SR. Falls incidence, risk factors, and consequences in Chinese older people: A systematic review. J Am Geriatr Soc. 2011;59(3):536–543. doi: 10.1111/j.1532-5415.2010.03286.x [DOI] [PubMed] [Google Scholar]
- 9.Boyd R, Stevens JA. Falls and fear of falling: Burden, beliefs and behaviours. Age Ageing. 2009;38(4):423–428. doi: 10.1093/ageing/afp053 [DOI] [PubMed] [Google Scholar]
- 10.Fletcher PC, Hirdes JP. Restriction in activity associated with fear of falling among community-based seniors using home care services. Age Ageing. 2004;33(3):273–279. doi: 10.1093/ageing/afh077 [DOI] [PubMed] [Google Scholar]
- 11.Woo J, Leung J, Wong S, Kwok T, Lee J, Lynn H. Development of a simple scoring tool in the primary care setting for prediction of recurrent falls in men and women aged 65 years and over living in the community. J Clin Nurs. 2009;18(7):1038–1048. doi: 10.1111/j.1365-2702.2008.02591.x [DOI] [PubMed] [Google Scholar]
- 12.Morley JE, Vellas B, Abellan van Kan G, et al. Frailty Consensus: A Call to Action. J Am Med Dir Assoc. 2013;14(6):392–397. doi: 10.1016/j.jamda.2013.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chu LW, Chi I, Chiu AYY. Incidence and predictors of falls in the Chinese elderly. Ann Acad Med Singapore. 2005;34(1):60–72. doi:15726221 [PubMed] [Google Scholar]
- 14.Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: A review of the literature. Maturitas. 2013;75(1):51–61. doi: 10.1016/j.maturitas.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 15.Kojima G Frailty as a Predictor of Future Falls Among Community-Dwelling Older People: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. 2015;16(12):1027–1033. doi: 10.1016/j.jamda.2015.06.018 [DOI] [PubMed] [Google Scholar]
- 16.Cheng MH, Chang SF. Frailty as a Risk Factor for Falls Among Community Dwelling People: Evidence From a Meta-Analysis. J Nurs Scholarsh. 2017:529–536. doi: 10.1111/jnu.12322 [DOI] [PubMed] [Google Scholar]
- 17.Wu TY, Chie WC, Sen Yang R, Kuo KL, Wong WK, Liaw CK. Risk factors for single and recurrent falls: A prospective study of falls in community dwelling seniors without cognitive impairment. Prev Med (Baltim). 2013;57(5):511–517. doi: 10.1016/j.ypmed.2013.07.012 [DOI] [PubMed] [Google Scholar]
- 18.Scott V, Votova K, Scanlan A, Close J. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term and acute care settings. Age Ageing. 2007;36(2):130–139. doi: 10.1093/ageing/afl165 [DOI] [PubMed] [Google Scholar]
- 19.Panel on Prevention of Falls in Older Persons AGS and BGS. Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–157. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 20.Sheehan J, O’Connell DL, Cunningham C, Crosby L, Kenny Anne R. The relationship between increased body mass index and frailty on falls in community dwelling older adults. BMC Geriatr. 2013;13:132. doi: 10.1186/1471-2318-13-132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Forti P, Rietti E, Pisacane N, Olivelli V, Maltoni B, Ravaglia G. A comparison of frailty indexes for prediction of adverse health outcomes in an elderly cohort. Arch Gerontol Geriatr. 2012;54(1):16–20. doi: 10.1016/j.archger.2011.01.007 [DOI] [PubMed] [Google Scholar]
- 22.Ensrud KE. Comparison of 2 Frailty Indexes for Prediction of Falls, Disability, Fractures, and Death in Older Women. Arch Intern Med. 2008;168(4):382. doi: 10.1001/archinternmed.2007.113 [DOI] [PubMed] [Google Scholar]
- 23.Ensrud KE, Ewing SK, Cawthon PM, et al. A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc. 2009;57(3):492–498. doi: 10.1111/j.1532-5415.2009.02137.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tom SE, Adachi JD, Anderson FA, et al. Frailty and fracture, disability, and falls: A multiple country study from the global longitudinal study of osteoporosis in women. J Am Geriatr Soc. 2013;61(3):327–334. doi: 10.1111/jgs.12146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li G, Ioannidis G, Pickard L, et al. Frailty index of deficit accumulation and falls: data from the Global Longitudinal Study of Osteoporosis in Women (GLOW) Hamilton cohort. BMC Musculoskelet Disord. 2014;15(1):185. doi: 10.1186/1471-2474-15-185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ensrud KE, Ewing SK, Taylor BC, et al. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2007;62(7):744–751. [DOI] [PubMed] [Google Scholar]
- 27.Fang X, Shi J, Song X, et al. And mortality in older Chinese adults: Results from the Beijing longitudinal study of aging. J Nutr Health Aging. 2012;16(10):903–907. doi: 10.1007/s12603-012-0368-6 [DOI] [PubMed] [Google Scholar]
- 28.Kwok AWL, Gong JS, Wang YXJ, et al. Prevalence and risk factors of radiographic vertebral fractures in elderly Chinese men and women: Results of Mr. OS (Hong Kong) and Ms. OS (Hong Kong) studies. Osteoporos Int. 2013;24(3):877–885. doi: 10.1007/s00198-012-2040-8 [DOI] [PubMed] [Google Scholar]
- 29.van Kan GA, Rolland YM, Morley JE, Vellas B. Frailty: Toward a Clinical Definition. J Am Med Dir Assoc. 2008;9(2):71–72. doi: 10.1016/j.jamda.2007.11.005 [DOI] [PubMed] [Google Scholar]
- 30.Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16(7):601–608. doi:10.1007-S12603-012-0084-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.American Geriatrics Society British Geriatrics Society, American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Guideline for the Prevention of Falls in Older Persons. J Am Geriatr Soc. 2001;49(5):664–672. doi: 10.1046/j.1532-5415.2001.49115.x [DOI] [PubMed] [Google Scholar]
- 32.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane database Syst Rev. 2009;(2):CD007146. doi: 10.1002/14651858.CD007146.pub2 [DOI] [PubMed] [Google Scholar]
- 33.Cummings SR, Nevitt MC, Kidd S. Forgetting Falls. The Limited Accuracy of Recall of Falls In the Elderly. J Am Geriatr Soc. 1988;36(7):613–616. doi: 10.1111/j.1532-5415.1988.tb06155.x [DOI] [PubMed] [Google Scholar]