Abstract
Introduction
Periconception obesity is associated with a higher risk for adverse perinatal outcomes such as gestational diabetes mellitus, preeclampsia, large for gestational age, operative delivery and preterm birth. Lifestyle interventions during pregnancy have resulted in insufficient effects on reducing these perinatal complications. A few reasons for this disappointing effect can be suggested: (1) the time period during pregnancy for improvement of developmental circumstances is too short; (2) the periconception period in which complications originate is not included; and (3) lifestyle interventions may not have been sufficiently multidisciplinary and customised. A preconception lifestyle intervention might be more effective to reduce perinatal complications. Therefore, the aim of the Towards Prepared mums study is to evaluate the effect of a lifestyle intervention starting prior to conception on lifestyle behaviour change.
Methods and analysis
This protocol outlines a non-blinded, randomised controlled trial. One hundred and twelve women (18–40 years of age) with overweight or obesity (body mass index≥25.0 kg/m2) who plan to conceive within 1 year will be randomised to either the intervention or care as usual group. The intervention group will receive a multidisciplinary, customised lifestyle intervention stimulating physical activity, a healthy diet and smoking cessation, if applicable. The lifestyle intervention and monitoring will take place until 12 months postpartum. The primary outcome is difference in weight in kg from baseline to 6 weeks postpartum. Secondary outcomes are gestational weight gain, postpartum weight retention, smoking cessation, dietary and physical activity habits. Furthermore, exploratory outcomes include body composition, cardiometabolic alterations, time to pregnancy, need for assisted reproductive technologies, perinatal complications of mother and child, and lung function of the child. Vaginal and oral swabs, samples of faeces, breast milk, placenta and cord blood will be stored for evaluation of microbial flora, epigenetic markers and breast milk composition. Furthermore, a cost-effectiveness analysis will take place.
Ethics and dissemination
Ethical approval was obtained from the Medical Ethical Committee of Maastricht University Medical Centre+ (NL52452.068.15/METC152026). Knowledge derived from this study will be made available by publications in international peer-reviewed scientific journals and will be presented at (inter)national scientific conferences. A dissemination plan for regional and national implementation of the intervention is developed.
Trial registration number
ClinicalTrials.gov NCT02703753.
Keywords: preventive medicine, perinatology, maternal medicine, fetal medicine
Strengths and limitations of this study.
This randomised controlled trial is innovative by evaluating effects of a lifestyle intervention that starts prior to conception and continues until 1 year postpartum.
The strength of the intervention is its multidisciplinary and personalised approach, taken into account the wishes, needs and opportunities of the women at risk.
This study will collect a broad range of data, including longitudinal data regarding mechanisms hypothesised to be involved in the intergenerational transmission of diseases, which is scarcely studied yet and allows the generation of new hypotheses.
Women who are willing to participate in the study are potentially more motivated to change their lifestyle, also when allocated to the care as usual group.
The sample size calculated to answer the primary research question may be relatively small in order to achieve sufficient power for the effect evaluation of some outcome measurements, which therefore should be seen as exploratory.
Introduction
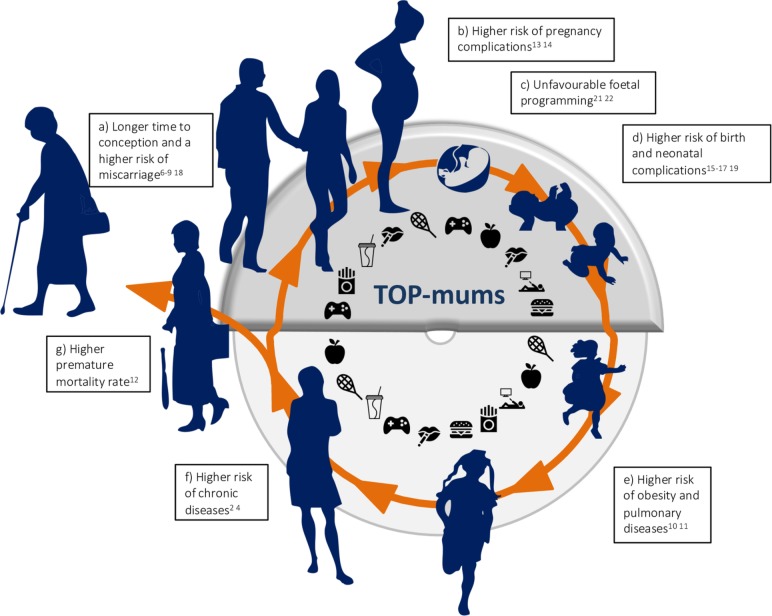
Worldwide, the prevalence of chronic diseases such as cardiovascular diseases, dyslipidaemia and diabetes mellitus is increasing. The rising burden from these chronic diseases imposes new challenges for healthcare.1 Key risk factors in the development of chronic diseases are lifestyle habits such as smoking, lack of physical activity, unhealthy diet and being overweight. As illustrated in figure 1, there is increasing evidence suggesting that the detrimental effects of being exposed to a certain lifestyle originate from the periconceptional period.2–5 By tackling its earliest origins, improving preconception lifestyle is hypothesised to benefit global public health by addressing the increasing problem of chronic diseases.
Figure 1.
This vicious circle illustrates the intergenerational transmission of disease. The Towards Prepared mums (TOP-mums) study focuses on lifestyle improvement and the effects of this lifestyle improvement in the period between preconception and 1 year postpartum as illustrated in the upper part of the circle. The effects of an unhealthy lifestyle in this period can impact health of the entire life span: (a) longer time to conception and a higher risk for miscarriage; (b) higher risk for pregnancy complications such as gestational diabetes mellitus, gestational hypertension and preeclampsia; (c) unfavourable fetal programming by epigenetic processes modulating gene transcription, and by transmission of an unfavourable composition of microbial flora from mother to child; (d) higher risk for birth and neonatal complications such as operative delivery, small and large for gestational age, preterm birth and admission to the neonatal intensive care unit; (e) higher risk for developing obesity and pulmonary diseases such as wheezing and asthmatic disease; (f) higher risk for chronic diseases such as diabetes mellitus type 2, cardiovascular diseases and dyslipidaemia; (g) higher premature mortality rate.
Overweight and obesity before and during pregnancy negatively impact fertility,6–8 pregnancy and birth outcomes,4 9 and increase the risk for the development of chronic disease for both mother and child.10–12 During pregnancy, women who are overweight or obese are at increased risk to develop complications such as gestational hypertension (GH), preeclampsia and gestational diabetes mellitus (GDM), and are more often in need of an emergency caesarean delivery.13 14 In addition, maternal obesity is associated with a higher risk for adverse perinatal outcomes such as congenital abnormalities, large for gestational age (LGA), and birth trauma as consequence of shoulder dystocia.15 16 Besides, neonates of women with obesity are more likely to be admitted to the neonatal intensive care unit.17 In addition to overweight, it is clearly established that maternal smoking negatively affects the health of mother and newborn. Maternal smoking decreases fertility18 and intrauterine exposure to smoking is associated with a higher risk for small for gestational age (SGA) and preterm birth.19
The risk of adverse events among offspring can extend through adulthood, demonstrating a vicious circle of intergenerational transmission of diseases.3 5 20 Several studies suggest that intrauterine exposure to an unhealthy lifestyle can increase the risk of cardiovascular, metabolic and endocrine disease in adult life by unfavourable fetal programming.2 5 Studies in animals indicate that epigenetic processes might be an important link between maternal lifestyle habits, and the risk for developing obesity and chronic diseases in adult offspring. Epigenetic processes modulate gene transcription, establishing a detrimental epigenome during embryogenesis and early development of the fetus.21 Furthermore, recent research suggests a role for the microbiota in the intergenerational transmission of obesity.22 Bacterial diversity is influenced by obesity and gestational weight gain.23 It is hypothesised that the transfer of an obesogenic microbial flora from mother to child during birth contributes to the intergenerational transmission of diseases.24
In an attempt to prevent perinatal complications, previous studies investigated the effect of lifestyle behaviour modification during pregnancy. Although these interventions were successful in limiting gestational weight gain, they were unsuccessful in reducing GDM, preeclampsia and LGA in women with obesity.25 It could be suggested that starting during pregnancy, the time span to achieve sufficient impact on pregnancy outcomes might be too short. In addition, most study protocols did not include a multidisciplinary and customised approach and did not take into account the effects of lifestyle during the periconception period in which perinatal complications often originate. Data from large population-based studies have shown that reducing body mass index (BMI) from overweight or obesity before the first pregnancy to normal weight before the subsequent pregnancy decreased the risk of GDM and LGA.26 27 Therefore, a lifestyle intervention that starts during the preconception phase might be promising in reducing pregnancy and birth complications and thereby provide a more promising start for the future generation.
Aim
The primary aim of this study is to evaluate the impact of a preconception lifestyle intervention on weight change in women with overweight or obesity and with a child wish. Secondary study aims are to evaluate the effect of the lifestyle intervention on gestational weight gain, postpartum weight retention and lifestyle habits such as physical activity, dietary intake and smoking behaviour. In addition, we will explore the effects of the intervention on cardiometabolic alterations, body composition, time to pregnancy, need for assisted reproductive technologies (ART) and perinatal complications such as GDM, GH, preeclampsia, SGA, LGA and preterm birth, cardiometabolic alterations and lung function of the child. Furthermore, effects on the microbial flora, epigenetics and breast milk composition will be evaluated. Finally, a cost-effectiveness analysis of the lifestyle intervention will be conducted.
Methods and analysis
This protocol was developed in accordance with the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) 2013 Statement (see online supplement 1: SPIRIT checklist).28
bmjopen-2019-030236supp001.pdf (63.2KB, pdf)
Study design
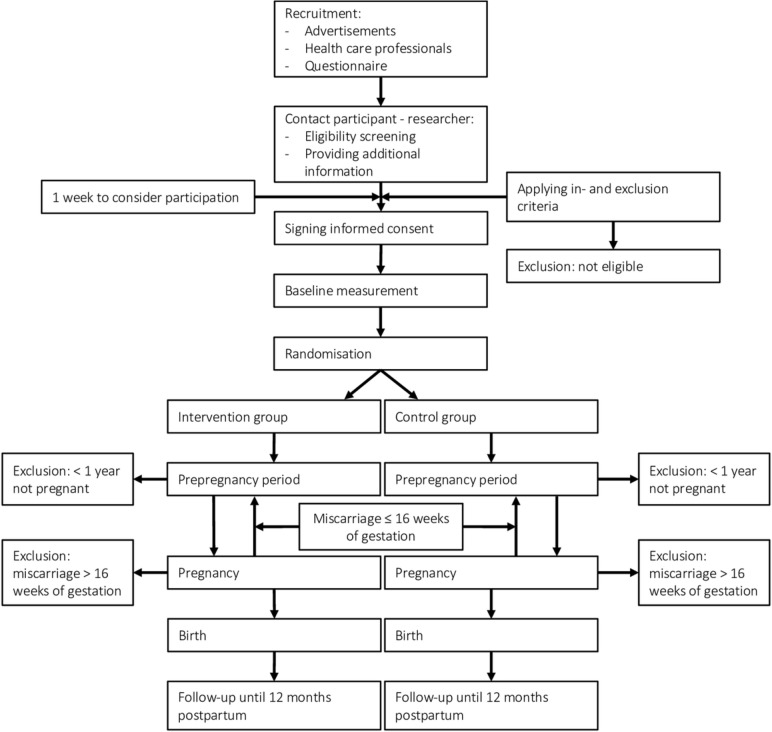
This study is a randomised controlled trial (RCT) in which the participants and investigators will not be blinded due to pragmatic reasons. Participants will be randomised 1:1 in either the intervention or ‘care as usual’ group using block randomisation, with random block sizes of 2, 4 or 6. Randomisation will be stratified for overweight (BMI 25.0–29.9 kg/m2), obesity (BMI ≥30.0 kg/m2) and smoking status. The study will start before conception and will continue during pregnancy until 1 year after delivery. The lifestyle intervention and follow-up will end for women who are not pregnant within 1 year after randomisation and in case of a fetal demise between 16 and 24 weeks of gestational age (considered dropout). In case of a miscarriage before 16 weeks of gestational age, women will continue their participation in the study in order to follow-up a potential second pregnancy. Also for these women, the lifestyle intervention and follow-up will end when they are not pregnant within 1 year of initial randomisation.
After childbirth, both parents will be informed about participation of their child in the study both verbally as well as by the information letter. Participation of the child will only be feasible when both parents sign informed consent (see online supplement 2: inform consent form child). When women/parents decide to quit participation, they will be asked to continue completing the cost and quality of life questionnaires. This will enable us to perform an adequate as possible cost-effectiveness analysis. A flow chart of these procedures is presented in figure 2.
Figure 2.
Flow chart of study procedures.
bmjopen-2019-030236supp002.pdf (55.2KB, pdf)
Setting and study population
The study will be conducted in the South of Limburg, the Netherlands, and is initiated and coordinated by Maastricht UMC+. Women will be eligible to participate in this study when meeting the following criteria: planning to conceive within 1 year, 18–40 years of age and having a BMI ≥25.0 kg/m². Smoking is neither an inclusion nor an exclusion criterion. Only women who are able to read and speak Dutch or English will be included. Being treated in a fertility clinic is not an exclusion criterion. Women will be excluded when pregnant at the moment of randomisation. In addition, women will be excluded in case of haemodynamic significant heart disease, restrictive lung disease, congenital metabolic disease, diabetes type II dependent on medication, when intellectually disabled according to the Diagnostic and Statistical Manual of Mental Disorders (DSM5) criteria,29 or when they underwent bariatric surgery in the past.
Recruitment
Multiple recruitment strategies will be used to reach an adequate number of potential participants (see sample size). Recruitment will take place in the region of Maastricht, South of Limburg, the Netherlands. In 2018, in this region, 1400 children were born.30 Gynaecologists, midwives, general practitioners and the Dutch youth healthcare system (a preventive healthcare system available for all children aged 0–19 years in the Netherlands) will be involved in recruiting women. At Maastricht UMC+, women may visit a gynaecologist for ART or may visit the preconception outpatient clinic because being at risk for developing pregnancy complications. In addition, women may visit their midwife with regard to the ‘child-wish consultation’ or their general practitioner for removing or discussing their birth control. Women in the period between two pregnancies will also visit the Dutch youth healthcare system with their previous child(ren). In addition, subjects will be recruited via advertisements in local newspapers, magazines and websites for (expecting) young mothers, and via targeted social media campaigns for women of childbearing age living in the Maastricht area. Third, for another (cross-sectional) study (manuscript in preparation), women of reproductive age in the region received a questionnaire in which they would indicate whether they would be interested in participation in the current study. When inclusion criteria for the current study are met, these women will be contacted for participation.
Sample size
A sample size calculation was conducted for the primary outcome measure, defined as the mean difference in body weight in kg from baseline to 6 weeks postpartum. In a previous study that evaluated the effect of a lifestyle intervention in subfertile women, a mean reduction of 3.4 kg resulted in a higher natural conception rate.31 Furthermore, 5%–10% weight reduction was associated with a reduction of type 2 diabetes incidence in adults at risk due to a BMI ≥24.0 kg/m².32 During pregnancy, lifestyle interventions resulted in 1.5 kg reduction in gestational weight gain.33 In some studies, this weight reduction was associated with a lower prevalence of preeclampsia.33 Taken into account these previous results, we determined a mean difference of 5±7 kg between the study groups as clinically relevant. For the sample size calculation, an alpha of 0.05 (two sided) and a power of 80% are used. Taken into account a drop-out rate of 44% (based on drop-out rates of other lifestyle interventions (22%),31 34–37 fetal demise after 16 weeks of gestation (1%),38 39 and time to pregnancy >12 months (21%),7 40 41 a total of 112 subjects will be included in the current study.
Procedure
Subjects will be recruited via advertisements in newspapers, social media and via healthcare professionals (eg, general practitioners, midwives, gynaecologists). On registration, women will be contacted by phone to test for eligibility based on inclusion and exclusion criteria, and the patient information letter will be provided. One week of consideration to participate in the study will follow, before a baseline visit will be scheduled and informed consent will be obtained (online supplement 3: informed consent form). During the baseline visit, height and weight will be measured to confirm the inclusion criteria of BMI ≥25.0 kg/m². Based on BMI and smoking status, subjects will be allocated to either the intervention or care as usual group by the online randomisation programme ALEA (ALEA Clinical B.V., Abcoude, the Netherlands). Study visits will take place at Maastricht UMC+and will take place during consultation with the personal lifestyle coach in order to minimise time investment. Within the scope of this study, health checks will be performed in addition to regular clinical practice, which might incidentally reveal aberrant findings. These findings will be discussed with the subject’s primary caregiver (eg, general practitioner, midwife and/or gynaecologist) who will be responsible for adequate follow-up and/or treatment.
bmjopen-2019-030236supp003.pdf (57.6KB, pdf)
Care as usual
Both study groups will receive care as usual. In addition, women in the intervention group will receive the lifestyle intervention as described below. In the Netherlands, usual care for women before pregnancy includes access to the general practitioner and child wish consultations by a midwife. In addition, ART are part of care as usual for subfertile women according to the Dutch infertility guidelines.42 Access to ART will remain available during study participation. Pregnant women have access to their general practitioner and their midwife and/or gynaecologist. After pregnancy, maternity care in the first week postpartum at home will support breast feeding. In addition, frequent consultations will take place at the youth healthcare division and for both mother and child access to the general practitioner is ensured. During these three periods, healthcare professionals will give lifestyle advices (according to national guidelines) when women specifically request for help regarding this topic or when healthcare professionals have other reasons for providing advice (eg, when women have a cardiometabolic risk factor). In addition, healthcare professionals are not restricted to refer women to additional lifestyle guidance (eg, by a dietician or lifestyle coach) when needed. Use of additional lifestyle guidance in the care as usual group will be registered and taken into account in the effect evaluation.
Lifestyle intervention
The Towards Prepared mums (TOP-mums) lifestyle intervention is a multidisciplinary intervention in which physical activity, a healthy diet, and if applicable, smoking cessation will be stimulated. The design of the study is based on a qualitative study executed by our research group to determine the needs and wishes of the women in the target population (results not published yet). This has resulted in a personalised programme, in which each participating woman will be assigned to her own personal lifestyle coach, who has a medical background and is trained in motivational interviewing.43 44 On a regular basis, subjects will meet their coach (online supplement 4: schedule consultations), who will develop a lifestyle programme in concordance with each woman. To this end, lifestyle habits will be assessed by a nutritional diary, questionnaires and activity tracker at baseline. Based on this assessment, goals for improvements will be formulated. Dependent on the personal situation, participants may choose which goal to work on first, for which a combination of supporting programme is available (see below). The programme will be offered in the periods before, during and after pregnancy, with specific lifestyle advice for each phase. This lifestyle intervention is easily accessible, innovative by the adaptive and proactive approach and the structured offer of lifestyle guidance.
bmjopen-2019-030236supp004.pdf (33.4KB, pdf)
Smarter pregnancy
Each woman will be provided with a free subscription to the mHealth coaching programme ‘Smarter Pregnancy’ (Erasmus MC, University Medical Centre, Rotterdam, the Netherlands) that has been shown to improve nutrition and other lifestyle behaviours in this target population before.45–48 The programme offers personal coaching for 26 weeks, which is based on current personal circumstances, pregnancy, nutrition and lifestyle status. The tailored coaching includes a maximum of three digital posts per week, providing advice, seasonal recipes for healthy meals and additional questions addressing lifestyle behaviour, taking into account pregnancy status.
Psychological guidance
For women who suffer from eating disorders in combination with overweight or obesity, psychological support can help with sustainable improvement of lifestyle. In order to determine the appropriate supporting programme that meet the wishes and needs of the women, a standardised quick-scan on eating habits (see online supplement 5: screening eating disorders) will be used. A psychologist will assess the results and when an eating disorder is suspected, women will meet a psychologist of Co-eur who applies the DSM-5 criteria for comfirmation.29 Co-eur is a mental healthcare institution specialised in the treatment of obesity in combination with eating disorders, in which a team of psychologists, dieticians and physiotherapists is involved in the treatment programme.49 The cornerstone of this programme is targeting both the eating disorder and possible underlying psychological comorbidities (eg, depression). Moreover, a sustainable change of lifestyle, and improvements of social and labour participation will be targeted. Cognitive–behavioural therapy, cue exposure and system therapy are techniques that will be used. In general, this involves coaching sessions two to three times a week, for 4 months.
bmjopen-2019-030236supp005.pdf (33.5KB, pdf)
Dietary guidance
A trained dietician will provide individual dietary advice every 1 or 2 months, according to the recommendations of the Netherlands Nutrition Centre.50 The main focus is targeting a healthy diet by improving dairy, fruit and vegetable intake, and decreasing the intake of low-nutritional, energy-dense foods. During pregnancy, a target for the maximum gestational weight gain will be set, according to the Institute of Medicine guidelines.51 In the postpartum period, dietary advice for both mother and child will be provided. Breast feeding will be encouraged by a trained lactation consultant. The frequency of dietician appointments is not fixed and can be adapted to the wishes and needs of the women, but a general guideline is provided in online supplement 4.
Physical activity
To support weekly physical activity at moderate intensity, a physical activity programme conducted by professionals trained in physical education will be offered by the sports department of the municipality of Maastricht. In the preconception period, the physical activity programme will focus on improving aerobic capacity, muscle strengthening and increasing energy expenditure. The variable activities will take place at different times and locations to facilitate participation. During pregnancy, sessions will be conducted by a physiotherapist who is trained in offering a sports programme for pregnant women (ZwangerFit). Physical fitness, muscle strengthening, coordination and stabilisation, especially for the pelvic muscles are hallmark of this training. It is previously shown that pregnancy-specific exercises reduce the risk of lower back pain, and sick leave because of lumbopelvic pain during pregnancy.52 Starting at 6 weeks postpartum, up to 9 months postpartum, a paediatric physiotherapist will provide individual training sessions with a focus on emotional bonding, fun in playing for mother and baby and stimulating motor development of the child. These sessions will take place in the home environment. In addition, the paediatric physiotherapist will discuss participation in other activities such as baby swimming classes or baby mindfulness.
Smoking cessation
To target smoking cessation, the personal lifestyle coach will apply motivational interviewing techniques to support women to quit smoking. If necessary, women can be referred to a specialised smoking cessation coach for more extensive guidance.
Outcomes
To determine the effects of the lifestyle intervention on the health of the women and child, anthropometric, cardiometabolic, lifestyle habits, perinatal and postpartum outcomes will be measured and registered. In addition, blood, faecal, urine and breast milk samples will be collected according to the scheme as presented in table 1.
Table 1.
Overview of the measurements at different time points during the study
| Baseline | Preconception | Pregnancy | Birth | Postpartum | ||||||||||||||||
| 1 month | 2months | 3months | 6months | 9months | 12months | 6weeks | 12weeks | 20weeks | 26weeks | 32weeks | 36weeks | 40weeks | 6weeks | 3months | 6months | 9months | 12months | |||
| Anthropometric measurements | ||||||||||||||||||||
| Weight, BMI, waist and hip circumference mother | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||
| Body composition mother | x | x | x | |||||||||||||||||
| Weight, height and BMI child | x | x | x | x | x | |||||||||||||||
| Cardiometabolic outcomes | ||||||||||||||||||||
| Blood pressure mother | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||
| Pulse wave velocity mother | x | x | x | x | x | x | x | x | x | |||||||||||
| Retinal image mother | x | x | x | x | x | x | x | x | x | |||||||||||
| Glucose, insulin levels, lipid profile, liver enzymes mother | x | x | x | x | x | x | x | x | ||||||||||||
| OGTT mother | x | x | x | |||||||||||||||||
| Glucose, insulin levels, lipid profile child (cord blood) | x | |||||||||||||||||||
| Glucose, insulin, lipid profile child | x | |||||||||||||||||||
| Lifestyle habits | ||||||||||||||||||||
| Accelerometer mother | x | x | x | x | x | x | x | |||||||||||||
| Baecke questionnaire mother | x | x | x | x | x | x | x | |||||||||||||
| Nutrition diary mother | x | x | x | x | x | x | x | |||||||||||||
| Three Factor Eating Questionnaire mother | x | x | x | x | x | x | x | |||||||||||||
| Vitamin D mother | x | x | ||||||||||||||||||
| Smoking behaviour questionnaire mother | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||
| CO measurement mother | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||
| Urine cotinin mother | x | x | x | x | x | x | x | |||||||||||||
| Feeding pattern child | x | x | x | x | x | |||||||||||||||
| Perinatal outcomes | ||||||||||||||||||||
| Time to pregnancy | x | |||||||||||||||||||
| Need for assisted reproductive technologies | x | |||||||||||||||||||
| Miscarriage | x | |||||||||||||||||||
| Pregnancy complications (GDM, GH, preeclampsia, IUGR) | x | x | x | |||||||||||||||||
| Method of delivery | x | |||||||||||||||||||
| Induction of labour | x | |||||||||||||||||||
| Postpartum measurements | ||||||||||||||||||||
| Birth weight | x | |||||||||||||||||||
| Gestational age | x | |||||||||||||||||||
| Apgar score | x | |||||||||||||||||||
| Stillbirth | x | |||||||||||||||||||
| Sample collection | ||||||||||||||||||||
| Microbiome sampling mother | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||
| Epigenetic sampling | x | |||||||||||||||||||
| Breast milk sampling | x | |||||||||||||||||||
| Microbiome sampling child | x | x | ||||||||||||||||||
| Cost-effectiveness analysis | ||||||||||||||||||||
| Cost questionnaire | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||
| EQ-5D-5L | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||
When women become pregnant at a certain time point before completing all preconception measurements, the remaining preconception measurements will be cancelled. Women will continue with measurements in the pregnancy period accordingly. The same procedure will take place when women give birth before 40 weeks of gestational age.
BMI, body mass index; CO, carbon monoxide; EQ-5D-5L, quality of life measurement; GDM, gestational diabetes mellitus; GH, gestational hypertension; IUGR, intrauterine growth restriction; OGTT, oral glucose tolerance test.
The first step in determining what the effect is of the lifestyle intervention proposed in this study is to examine the effect of the intervention on lifestyle behaviour change. It is assumed that lifestyle behaviour change results in weight change which is an objective outcome measurement. Based on the hypothesis that weight change will result in cardiometabolic changes, the next step is to study whether weight change has influence on secondary and exploratory outcomes.
Anthropometric measurements
Body weight will be assessed in underwear with no shoes in kg to the nearest 0.1 kg using a medical calibrated weight scale (Model 799, seca gmbh & co. kg., Chino, USA), at each study visit. Height will be determined by a stadiometer (Model 220, seca gmbh & co. kg.) calibrated in 0.1 cm intervals. BMI will be calculated as the weight in kg divided by height in metres squared. Gestational weight gain is defined as weight in kg from 6 weeks of pregnancy to the last prenatal study visit and will be compared with the Institute of Medicine guidelines.51 Postpartum weight retention is defined as the difference in weight in kg between 6 weeks of gestational age and 6 months postpartum.
Waist and hip circumferences will be measured with a non-elastic tape at the end of a natural breath at midpoint between the top of the iliac crest and the lower margin of the last palpable rib and at the widest point of the hip, respectively, standing on both feet equally with arms hanging down. The waist/hip ratio will be calculated. Furthermore, the body composition (ie, fat and fat-free mass) will be measured at three time points during the study using deuterium dilution as described before.53 During pregnancy, calculations for fat mass and fat-free mass will be adjusted for gestational specific fat-free mass in which deuterium is distributed as well.54 55
Lifestyle habits
To objectively measure physical activity level, participants will wear an accelerometer (ActiGraph, model wGT3X-BT, Pensacola, Florida, USA) for 7 days. Furthermore, the validated Baecke questionnaire will be used to measure work, sport and leisure activities.56 To register dietary habits, women will be asked to complete a 7-day nutritional diary. In addition, the validated Three Factor Eating Questionnaire will be used to assess three aspects of eating behaviour: cognitive restraint, disinhibition and hunger.57 As a component of the nutritional assessment, serum 25-hydroxyvitamin D will be measured using the Immulite-1000 (Siemens Healthcare Diagnostics, Erlangen, Germany). Vitamin D insufficiency is defined as <50 nmol/L.58 Smoking habits will be assessed by a questionnaire focussing on smoking behaviour, quitting history, the intention to quit, nicotine dependence and self-efficacy. Biochemical verification of tobacco will be assessed through the piCObabyTM carbon monoxide (CO) monitor (Bedfont Scientific, Harrietsham, Maidstone, Kent) by measuring CO in exhaled breath. Long-term use of tobacco will be measured by the assessment of cotinin in urine.
Cardiometabolic outcomes
Fasting blood samples will be taken at different time points before, during and after pregnancy to determine blood glucose and insulin levels, lipid profile and liver enzymes (table 1). Fasting plasma glucose will be determined using the Cobas 8000 modular analyser (F. Hoffmann-La Roche, Basel, Switzerland) and serum insulin concentrations using the Immulite-1000. Accordingly, the homeostatic model assessment of insulin resistance will be calculated (fasting glucose (mmol/L)*(fasting insulin (µU/L)/22.5)).59 All participants will undergo an oral glucose tolerance test (OGTT) at baseline, 26 weeks of gestational age and 12 months postpartum. Blood glucose and insulin concentrations will be measured 1 and 2 hours after ingestion of 75 g glucose. Fasting serum total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglycerides, free-fatty acids, serum alanine transaminase, aspartate transaminase, gamma-glutamyl transferase and alkaline phosphatase concentrations will be determined using the Cobas 8000 modular analyser.
Cardiovascular alterations will be measured by systolic and diastolic blood pressure (SBP and DBP), using a validated automatic device (A&D Medical UA-789XL, Saitama, Japan) on the left arm after 5–10 min rest in a sitting position for four times, with 1 min rest in between. Mean SBP and DBP of the three last measurements will be calculated. Although cardiovascular morbidity such as a high blood pressure might not be present in women participating in the study (yet), a precursor might already be present and might play a role in the transmission of health risk to the next generation. Since arterial stiffness and retinal microvasculature are both established as prognostic parameters for cardiometabolic morbidity,60 61 these measurements are included in this study. Arterial stiffness will be assessed by the carotid-femoral and carotid-radial pulse wave velocity and Augmentation Index using the SphygmoCor device, model EM3 (ArtCor, Sydney, Australia). Further, retinal vascular images will be made of the right eye using a retina camera (Topcon TRC-NW-300, Topcon Corporation, Tokyo, Japan). The images will be analysed to measure the diameter of the four largest retinal arterioles and venules and to calculate the arteriovenous ratio.
Perinatal outcomes
Time to pregnancy is defined as the period between having the explicit wish to become pregnant to the moment of conception. The need for ART and the reason for this (eg, chronic anovulation, not able to conceive for >12 months despite an ovulatory cycle) will be registered. Miscarriage, GDM, GH, preeclampsia, intrauterine growth restriction (IUGR), operative delivery, induction of labour, preterm birth, stillbirth and congenital malformations will be registered after verifying medical records. Miscarriage is defined as the loss of the fetus before 16 weeks of gestation. Stillbirth is defined as intrauterine fetal death after 16 weeks of gestation. GDM, GH, preeclampsia and IUGR will be determined according to the guidelines of the Dutch Society of Obstetrics and Gynaecology. GDM is defined as a diagnosis of hyperglycaemia during pregnancy, in a woman without pre-existing diabetes mellitus. The Dutch national guideline is in line with the WHO guideline on Diagnosis and Classification of Diabetes Mellitus, which defined hyperglycaemia as the presence of either a fasting plasma glucose ≥7.0 mmol/L or 2 hours plasma glucose ≥7.8 mmol/L following a 75 g OGTT.62 63 GH is defined as SBP of at least 140 mm Hg and/or DBP of at least 90 mm Hg after 20 weeks of gestational age.64 Preeclampsia is defined as GH accompanied by proteinuria (at least 300 mg protein in a 24 hours urine collection).64 IUGR is defined as estimated fetal weight <p10, abdominal circumference <p10 or a decrease in growth of at least 20 percentiles within a minimal time frame of 2 weeks.65 Preterm birth is defined as birth before 37 weeks of gestation and will be subdivided in spontaneous (delivery started by primary contractions or spontaneous rupture of membranes) and indicated (including the performance of a caesarean delivery before onset of labour or induction of labour) preterm birth. Perinatal outcomes will be derived from hospital birth registries.
Postpartum measurements
Birth weight, Apgar score 1 and 5 min after birth, SGA and LGA will be derived from birth registries. SGA and LGA are defined as birth weight below the 10th percentile, and above the 90th percentile of normal values for gestational age and gender, respectively.66 Growth charts from the first year of life will be derived from regular youth healthcare visits that are part of the Dutch healthcare system. Cord blood samples at birth and plasma at 1 year of age will be collected to determine glucose, insulin and lipid profile. Infant lung function will be assessed by measurements of Functional Residual Capacity, Lung Clearance Index, Tidal Volume and airway resistance using the tremoFlo C-100 Airwave Oscillometry System (THORASYS, Montreal, QC, Canada) at 6 weeks and 12 months postpartum, according to international standards.67 Furthermore, feeding practices will be registered in terms of formula or (exclusive) breast feeding.
Sample collection
During the past years, it has been indicated that obesity is related to microbial dysbiosis.68–71 Notably, studies indicated that during pregnancy, the developing fetal gut is primed by the gut microbiota and intestinal permeability of the mother, particularly towards the later stages of gestation.72 73 In addition, a major determinant of the microbiota composition of newborns is the mode of delivery. Vaginally delivered infants harbour bacterial communities resembling those of the maternal vagina, whereas the gut microbiota of caesarean section delivered infants are enriched in maternal skin microbiota.74 75 There are also indications that breast milk harbours a specific microbial community; however, literature is scarce. Therefore, we aim to determine the microbiota composition of mothers and children (faecal, oral, vaginal, breast milk) and determine the role of weight loss herein. In addition, breast milk composition/metabolome will be investigated,76 77 and placenta tissue will be collected for RNA-sequencing analysis, histology and epigenetics.
Faeces will be collected at home using the TagHemi collection system (TagHemi, Zeijen, The Netherlands), and divided over two sterile tubes at home (Sarstedt, Nürmbrecht, Germany). Subjects will be instructed to freeze their samples immediately after defecation and use a cool transport container for transport to the university. Within 1 week, participants will take the samples to the university for storage at −80°C until further analysis. Stool samples will be collected at baseline, which will be repeated every 3 months for the scope of the study, including each trimester of pregnancy. Child faecal samples will be collected at age 6 weeks and 12 months. Vaginal (of the mother) and oral (of mother and child) swabs will be stored in transport buffer at −80°C until further analysis. Breast milk will be collected and stored as reported by Lipkie et al.78 Placental tissue will be collected and stored as described before.79 Microbiota profiles will be generated. Quantitative DNA methylation analysis will be performed to explore epigenetic changes. Regions of interest will be determined at the moment analyses will be performed, to adhere to the most current literature among epigenetic changes.
Cost-effectiveness analysis
Questionnaires will be used to obtain insight in care utilisation. To determine costs (ie, regarding healthcare, patient and family costs, and costs outside the healthcare sector), a questionnaire is developed taking into account the stage women are in (preconception, pregnant, postpartum). To generate quality adjusted life years, quality of life is measured by the validated five-level version of EuroQol-5D questionnaire.80 81
Incentives
Parking and travel costs will be reimbursed. In order to acknowledge women for their efforts, during each study period (preconception, pregnancy, postpartum) an incentive is included such as a free 3D ultrasound during pregnancy.
Public and patient involvement
To increase adherence, women in the target population were involved in the overall design of the current study. A large group of women of childbearing age was interviewed to identify facilitators and barriers to participate in a lifestyle intervention that were incorporated in the current protocol. In addition, the intervention for each participating woman will be adapted to her personal needs, possibilities and social situation. Main results will be disseminated to trial participants and they are involved in the development of an appropriate method of dissemination. Therefore, participating women have a central position in the intervention and are involved in every phase of the study.
Data management
Data will be collected using electronic case record forms (MACRO, Elsevier B.V., Amsterdam, the Netherlands) that were adapted to the requirements of the current study. By using MACRO, the data collected are according to the Findable, Accessible, Interoperable and Reusable criteria.82 Data will be securely stored for 15 years.
Statistical analysis plan
Data will be analysed using SPSS V.24.0 for Windows (SPSS Incorporated). Descriptive statistics will be performed for baseline characteristics of the study population. Parametric data will be presented as means with SD, and non-parametric distributed variables as median with IQRs. Since the design is a repeated-measures RCT, linear mixed-model techniques based on the intention-to-treat principle will be used to analyse the difference between intervention and care as usual group with respect to primary and secondary outcome measurements. This technique corrects for within-subject correlation and deals with missing values at random. Survival analysis will be used to determine the HR for smoking cessation and time to pregnancy. Exploratory, paired sample t-tests will be used to test for change in exploratory outcomes. Analyses will be adjusted for the stratification factors overweight/obesity and smoking status. A p value<0.05 will be considered statistically significant.
Ethics and dissemination
This study will be monitored independently by the Clinical Trial Centre Maastricht. All adverse events will be registered and reported to the medical ethics committee of Maastricht UMC+.
The knowledge derived from this study will be made available for the scientific community by publications in international peer reviewed scientific journals and will be presented at (inter)national scientific conferences. Study results will be relevant for both researchers as well as for primary care providers (ie, midwives, general practitioners and youth healthcare workers) and secondary care providers (ie, gynaecologists, hospital-based midwives and paediatricians). Furthermore, study results will be presented and discussed with policy-makers and the public domain.
The TOP-mums lifestyle intervention makes use of existing, regional initiatives (that are financially covered) for a sustainable solution for lifestyle improvement. Therefore, in case proven to be a successful intervention, the approach of TOP-mums can easily be extended to a broader area. A dissemination plan for regional and national implementation is developed.
Discussion
The main goal of our RCT is to study the effects of a multidisciplinary lifestyle intervention for women who plan to conceive, who are at higher risk for perinatal morbidity because of overweight or obesity. The TOP-mums study is one of the first studies that investigates the effect of a multidisciplinary and personalised lifestyle intervention starting in the preconception phase, on different behavioural, cardiovascular and perinatal outcomes of both mother and child before, during and after pregnancy. There is growing evidence that lifestyle-related aberrations of maternal metabolic health and placenta function occur during the first trimester of pregnancy, prior to when most interventions are started.33 83 To foster healthy living from conception on, the lifestyle intervention in this study is initiated prior to conception.
Previous research regarding preconception lifestyle interventions is limited and the effectiveness of multidisciplinary and customised interventions is unclear.84–86 The majority of existing studies targeted subfertile women undergoing ART and discontinued the intervention once women became pregnant. When considering interpregnancy weight change, it has been shown that weight loss between pregnancies can reduce the incidence rates of perinatal complications.26 This paves the way to execute an extensive effect evaluation of the lifestyle intervention in the current study. The study will significantly contribute to the elaboration of the knowledge on the effects of preconception lifestyle guidance on improving health for the current and next generations. One of the strengths of our study is that the lifestyle intervention is developed based on the experiences and wishes of the target group itself and is customised to the personal objectives of each participant. Another asset of this study is the amount of data collected, allowing us to better understand the consequences and intermediating factors of lifestyle on the health of mother and child.
The current protocol has some limitations. First, most subjects might enter the study based on intrinsic motivation to implement lifestyle changes. This might result in the search for additional lifestyle guidance, also when allocated to the care as usual group, thereby potentially diluting the intervention effect. Second, although pregnancy can be seen as a ‘teachable moment’, poor adherence and high drop-out rates are frequently reported for this type of lifestyle interventions.87 However, based on experience of our research group, we expect that the design of the current lifestyle intervention, including a customised approach and the organisation of activities in proximity of subject’s home and at different time points, will limit drop-out rates.88 It is possible that additional measurements for data collection might be experienced as extensive by the participants. However, the long-standing experience of our research group with other lifestyle interventions89–91 is that participants mostly appreciate monitoring of their health, which in addition often increases motivation.
To conclude, the current TOP-mums protocol describes a personalised lifestyle intervention starting in preparation of conception, continuing until 1 year after birth. By improving lifestyle already in the preconception phase, the earliest origins of chronic disease might be tackled, thereby disrupting the vicious circle of transferring harmful lifestyle influences from generation to generation. The outcomes of the current multidisciplinary, customised lifestyle intervention might provide valuable information for public health initiatives to foster a healthy start for our next generation.
Supplementary Material
Acknowledgments
The authors would like to acknowledge Anita Badart (dietician, Voedingspraktijk Rond & Gezond, Geulle, the Netherlands), Esther Jansen and Erik Aller (psychologist and manager respectively, Co-eur, Hoensbroek, the Netherlands), Hein Poell (coordinator, Maastricht Sport, Maastricht, the Netherlands), Marieke Albert-Calon (physiotherapist, Fysiotherapie Medisch Centrum Sint Pieter, Maastricht, the Netherlands), Sylvia Heddema (smoking cessation coach and manager, SineFuma, Breda, the Netherlands) for their input and expertise regarding the content of the lifestyle intervention. In addition, they would like to acknowledge the research teams that provided their input and expertise regarding the outcome measurements: Guy Plasqui (body composition, Maastricht University, Maastricht), Jogchum Plat (cardiovascular outcomes, Maastricht University, Maastricht), Paul Savelkoul and John Penders (microbiota, Maastricht University, Maastricht), Aafke van Montfoort (epigenetics, Maastricht University, Maastricht), Silvia Evers (cost-effectiveness analysis, Maastricht University, Maastricht). Lastly, they would like to thank all women who participated in our prior qualitative study for their valuable input regarding the desired content and set-up of the lifestyle intervention.
Footnotes
Contributors: Study concept and design: YEGT, KDGvdK, MEAS, ED, LJIZ, RPMS-T, BWK and ACEV. Acquisition of data: YEGT and LMPK. Draft of manuscript and statistical analysis: YEGT, KDGvdK, LMPK and ACEV. Revision content of manuscript: YEGT, DR, KDGvdK, MEAS, ED, RPMS-T, LJIZ, BWK and ACEV. All authors read and approved the manuscript for final publication. ACEV has the primary responsibility for the final content.
Funding: This study is partly funded by Maastricht UMC+ (PI-00231). Other parts of the study are covered by The Netherlands Organisation for Health Research and Development (project number 524005516), and the Christine Bader Foundation Irene Child Hospital (project number 546).
Competing interests: RPMS-T is initiator and developer of Smarter Pregnancy and does not have a commercial interest. The Department of Obstetrics and Gynaecology of the Erasmus MC, University Medical Centre in Rotterdam is owner of this mHealth coaching tool.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Murray CJL, Vos T, Lozano R, et al. . Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2197–223. 10.1016/S0140-6736(12)61689-4 [DOI] [PubMed] [Google Scholar]
- 2. Godfrey KM, Barker DJP. Fetal programming and adult health. Public Health Nutr 2001;4:611–24. 10.1079/PHN2001145 [DOI] [PubMed] [Google Scholar]
- 3. Godfrey KM, Reynolds RM, Prescott SL, et al. . Influence of maternal obesity on the long-term health of offspring. Lancet Diabetes Endocrinol 2017;5:53–64. 10.1016/S2213-8587(16)30107-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Steegers-Theunissen RPM, Twigt J, Pestinger V, et al. . The periconceptional period, reproduction and long-term health of offspring: the importance of one-carbon metabolism. Hum Reprod Update 2013;19:640–55. 10.1093/humupd/dmt041 [DOI] [PubMed] [Google Scholar]
- 5. Gluckman PD, Hanson MA, Cooper C, et al. . Effect of in utero and early-life conditions on adult health and disease. N Engl J Med 2008;359:61–73. 10.1056/NEJMra0708473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brewer CJ, Balen AH. The adverse effects of obesity on conception and implantation. Reproduction 2010;140:347–64. 10.1530/REP-09-0568 [DOI] [PubMed] [Google Scholar]
- 7. Hassan MAM, Killick SR. Negative lifestyle is associated with a significant reduction in fecundity. Fertil Steril 2004;81:384–92. 10.1016/j.fertnstert.2003.06.027 [DOI] [PubMed] [Google Scholar]
- 8. Homan GF, Davies M, Norman R. The impact of lifestyle factors on reproductive performance in the general population and those undergoing infertility treatment: a review. Hum Reprod Update 2007;13:209–23. 10.1093/humupd/dml056 [DOI] [PubMed] [Google Scholar]
- 9. Lashen H, Fear K, Sturdee DW. Obesity is associated with increased risk of first trimester and recurrent miscarriage: matched case-control study. Hum Reprod 2004;19:1644–6. 10.1093/humrep/deh277 [DOI] [PubMed] [Google Scholar]
- 10. Scholtens S, Wijga AH, Brunekreef B, et al. . Maternal overweight before pregnancy and asthma in offspring followed for 8 years. Int J Obes 2010;34:606–13. 10.1038/ijo.2009.194 [DOI] [PubMed] [Google Scholar]
- 11. Gilliland FD, LI YU-FEN, Peters JM. Effects of maternal smoking during pregnancy and environmental tobacco smoke on asthma and wheezing in children. Am J Respir Crit Care Med 2001;163:429–36. 10.1164/ajrccm.163.2.2006009 [DOI] [PubMed] [Google Scholar]
- 12. Di Angelantonio E, Bhupathiraju S, Wormser D, et al. . Body-Mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 2016;388:776–86. 10.1016/S0140-6736(16)30175-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Scott-Pillai R, Spence D, Cardwell CR, et al. . The impact of body mass index on maternal and neonatal outcomes: a retrospective study in a UK obstetric population, 2004-2011. BJOG 2013;120:932–9. 10.1111/1471-0528.12193 [DOI] [PubMed] [Google Scholar]
- 14. Voerman E, Santos S, Inskip H, et al. . Association of gestational weight gain with adverse maternal and infant outcomes. JAMA 2019;321:1702–15. 10.1001/jama.2019.3820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu P, Xu L, Wang Y, et al. . Association between perinatal outcomes and maternal pre-pregnancy body mass index. Obes Rev 2016;17:1091–102. 10.1111/obr.12455 [DOI] [PubMed] [Google Scholar]
- 16. Stothard KJ, Tennant PWG, Bell R, et al. . Maternal overweight and obesity and the risk of congenital anomalies: a systematic review and meta-analysis. JAMA 2009;301:636–50. 10.1001/jama.2009.113 [DOI] [PubMed] [Google Scholar]
- 17. Ramachenderan J, Bradford J, McLean M. Maternal obesity and pregnancy complications: a review. Aust N Z J Obstet Gynaecol 2008;48:228–35. 10.1111/j.1479-828X.2008.00860.x [DOI] [PubMed] [Google Scholar]
- 18. Hyland A, Piazza K, Hovey KM, et al. . Associations between lifetime tobacco exposure with infertility and age at natural menopause: the women's health Initiative observational study. Tob Control 2016;25:706–14. 10.1136/tobaccocontrol-2015-052510 [DOI] [PubMed] [Google Scholar]
- 19. Ko T-J, Tsai L-Y, Chu L-C, et al. . Parental smoking during pregnancy and its association with low birth weight, small for gestational age, and preterm birth offspring: a birth cohort study. Pediatr Neonatol 2014;55:20–7. 10.1016/j.pedneo.2013.05.005 [DOI] [PubMed] [Google Scholar]
- 20. Eriksson JG, Sandboge S, Salonen MK, et al. . Long-Term consequences of maternal overweight in pregnancy on offspring later health: findings from the Helsinki birth cohort study. Ann Med 2014;46:434–8. 10.3109/07853890.2014.919728 [DOI] [PubMed] [Google Scholar]
- 21. Burdge GC, Slater-Jefferies J, Torrens C, et al. . Dietary protein restriction of pregnant rats in the F 0 generation induces altered methylation of hepatic gene promoters in the adult male offspring in the F1 and F2 generations. Br J Nutr 2007;97:435–9. 10.1017/S0007114507352392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gohir W, Ratcliffe EM, Sloboda DM. Of the bugs that shape us: maternal obesity, the gut microbiome, and long-term disease risk. Pediatr Res 2015;77:196–204. 10.1038/pr.2014.169 [DOI] [PubMed] [Google Scholar]
- 23. Nieuwdorp M, Gilijamse PW, Pai N, et al. . Role of the microbiome in energy regulation and metabolism. Gastroenterology 2014;146:1525–33. 10.1053/j.gastro.2014.02.008 [DOI] [PubMed] [Google Scholar]
- 24. Bäckhed F, Roswall J, Peng Y, et al. . Dynamics and stabilization of the human gut microbiome during the first year of life. Cell Host Microbe 2015;17:690–703. 10.1016/j.chom.2015.04.004 [DOI] [PubMed] [Google Scholar]
- 25. i-WIP Collaborative Group Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: meta-analysis of individual participant data from randomised trials. BMJ 2017;358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Getahun D, Ananth CV, Peltier MR, et al. . Changes in prepregnancy body mass index between the first and second pregnancies and risk of large-for-gestational-age birth. Am J Obstet Gynecol 2007;196:530.e1–8. 10.1016/j.ajog.2006.12.036 [DOI] [PubMed] [Google Scholar]
- 27. Whiteman VE, Aliyu MH, August EM, et al. . Changes in prepregnancy body mass index between pregnancies and risk of gestational and type 2 diabetes. Arch Gynecol Obstet 2011;284:235–40. 10.1007/s00404-011-1917-7 [DOI] [PubMed] [Google Scholar]
- 28. Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. . Spirit 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. American Psychiatric Association Diagnostic and statistical manual of mental disorders. 5th ed Washington, DC, 2013. [Google Scholar]
- 30. Statistics Netherlands StatLine: birth, key numbers fertility, maternal age, region. Available: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/37201/table?ts=1561462862456 [Accessed 25 Jun 2019].
- 31. Mutsaerts MAQ, van Oers AM, Groen H, et al. . Randomized trial of a lifestyle program in obese infertile women. N Engl J Med 2016;374:1942–53. 10.1056/NEJMoa1505297 [DOI] [PubMed] [Google Scholar]
- 32. Knowler WC, Fowler SE. 10-Year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. Lancet 2009;374:1677–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Thangaratinam S, Rogozinska E, Jolly K, et al. . Effects of interventions in pregnancy on maternal weight and obstetric outcomes: meta-analysis of randomised evidence. BMJ 2012;344:e2088 10.1136/bmj.e2088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Vinter CA, Jensen DM, Ovesen P, et al. . The lip (lifestyle in pregnancy) study: a randomized controlled trial of lifestyle intervention in 360 obese pregnant women. Diabetes Care 2011;34:2502–7. 10.2337/dc11-1150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Althuizen E, van der Wijden CL, van Mechelen W, et al. . The effect of a counselling intervention on weight changes during and after pregnancy: a randomised trial. BJOG 2013;120:92–9. 10.1111/1471-0528.12014 [DOI] [PubMed] [Google Scholar]
- 36. Hoeger KM, Kochman L, Wixom N, et al. . A randomized, 48-week, placebo-controlled trial of intensive lifestyle modification and/or metformin therapy in overweight women with polycystic ovary syndrome: a pilot study. Fertil Steril 2004;82:421–9. 10.1016/j.fertnstert.2004.02.104 [DOI] [PubMed] [Google Scholar]
- 37. Foster GD, Wyatt HR, Hill JO, et al. . A randomized trial of a low-carbohydrate diet for obesity. N Engl J Med 2003;348:2082–90. 10.1056/NEJMoa022207 [DOI] [PubMed] [Google Scholar]
- 38. Simpson JL. Incidence and timing of pregnancy losses: relevance to evaluating safety of early prenatal diagnosis. Am J Med Genet 1990;35:165–73. 10.1002/ajmg.1320350205 [DOI] [PubMed] [Google Scholar]
- 39. Zhou H, Liu Y, Liu L, et al. . Maternal pre-pregnancy risk factors for miscarriage from a prevention perspective: a cohort study in China. Eur J Obstet Gynecol Reprod Biol 2016;206:57–63. 10.1016/j.ejogrb.2016.07.514 [DOI] [PubMed] [Google Scholar]
- 40. Ramlau-Hansen CH, Thulstrup AM, Nohr EA, et al. . Subfecundity in overweight and obese couples. Hum Reprod 2007;22:1634–7. 10.1093/humrep/dem035 [DOI] [PubMed] [Google Scholar]
- 41. Hull MG, North K, Taylor H, et al. . Delayed conception and active and passive smoking. The Avon longitudinal study of pregnancy and childhood study Team. Fertil Steril 2000;74:725–33. [DOI] [PubMed] [Google Scholar]
- 42. Nederlandse Vereniging voor Obstetrie en Gynaecologie Landelijke netwerkrichtlijn Subfertiliteit, 2010. Available: https://www.nvog.nl/wp-content/uploads/2018/02/Subfertiliteit-landelijke-netwerkrichtlijn-1.0-20-05-2011.pdf
- 43. Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult Clin Psychol 2003;71:843–61. 10.1037/0022-006X.71.5.843 [DOI] [PubMed] [Google Scholar]
- 44. Miller WR, Rollnick S. Motivational interviewing, second edition: preparing people for change. Guilford Publications, 2002. [Google Scholar]
- 45. Van Dijk MR, Huijgen NA, Willemsen SP, et al. . Impact of an mHealth platform for pregnancy on nutrition and lifestyle of the reproductive population: a survey. JMIR mHealth uHealth 2016;4:e53 10.2196/mhealth.5197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Van Dijk MR, Koster MPH, Rosman AN, et al. . Opportunities of mHealth in preconception care: preferences and experiences of patients and health care providers and other involved professionals. JMIR Mhealth Uhealth 2017;5:e123 10.2196/mhealth.7834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. van Dijk MR, Koster MPH, Willemsen SP, et al. . Healthy preconception nutrition and lifestyle using personalized mobile health coaching is associated with enhanced pregnancy chance. Reprod Biomed Online 2017;35:453–60. 10.1016/j.rbmo.2017.06.014 [DOI] [PubMed] [Google Scholar]
- 48. van Dijk MR, Oostingh EC, Koster MPH, et al. . The use of the mHealth program smarter pregnancy in preconception care: rationale, study design and data collection of a randomized controlled trial. BMC Pregnancy Childbirth 2017;17:46 10.1186/s12884-017-1228-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Available: www.co-eur.com
- 50. The Netherlands Nutrition Centre De Schijf van Vijf. Available: https://www.voedingscentrum.nl/nl/gezond-eten-met-de-schijf-van-vijf.aspx [Accessed 18 Jul 2018].
- 51. Institute of Medicine Weight gain during pregnancy: reexamining the guidelines. Washington (DC): National Academies Press (US), 2009. [PubMed] [Google Scholar]
- 52. Shiri R, Coggon D, Falah-Hassani K. Exercise for the prevention of low back and pelvic girdle pain in pregnancy: a meta-analysis of randomized controlled trials. European Journal of Pain 2018;22:19–27. 10.1002/ejp.1096 [DOI] [PubMed] [Google Scholar]
- 53. Westerterp KR, Wouters L, van Marken Lichtenbelt WD. The Maastricht protocol for the measurement of body composition and energy expenditure with labeled water. Obes Res 1995;3:49–57. 10.1002/j.1550-8528.1995.tb00007.x [DOI] [PubMed] [Google Scholar]
- 54. Catalano PM, Wong WW, Drago NM, et al. . Estimating body composition in late gestation: a new hydration constant for body density and total body water. Am J Physiol Endocrinol Metab 1995;268:E153–8. 10.1152/ajpendo.1995.268.1.E153 [DOI] [PubMed] [Google Scholar]
- 55. van Raaij JM, Peek ME, Vermaat-Miedema SH, et al. . New equations for estimating body fat mass in pregnancy from body density or total body water. Am J Clin Nutr 1988;48:24–9. 10.1093/ajcn/48.1.24 [DOI] [PubMed] [Google Scholar]
- 56. Baecke JA, Burema J, Frijters JER. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr 1982;36:936–42. 10.1093/ajcn/36.5.936 [DOI] [PubMed] [Google Scholar]
- 57. Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res 1985;29:71–83. 10.1016/0022-3999(85)90010-8 [DOI] [PubMed] [Google Scholar]
- 58. Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet 1998;351:805–6. 10.1016/S0140-6736(05)78933-9 [DOI] [PubMed] [Google Scholar]
- 59. Matthews DR, Hosker JP, Rudenski AS, et al. . Homeostasis model assessment: insulin resistance and ?-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985;28:412–9. 10.1007/BF00280883 [DOI] [PubMed] [Google Scholar]
- 60. Ben-Shlomo Y, Spears M, Boustred C, et al. . Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol 2014;63:636–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ding J, Wai KL, McGeechan K, et al. . Retinal vascular caliber and the development of hypertension: a meta-analysis of individual participant data. J Hypertens 2014;32:207–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Nederlandse Vereniging voor Obstetrie en Gynaecologie Richtlijn diabetes mellitus en zwangerschap, 2018. Available: https://www.nvog.nl/wp-content/uploads/2018/10/NVOG-richtlijn-Diabetes-mellitus-en-zwangerschap-v3.0-2018.pdf
- 63. World Health Organization Definition, diagnosis and classification of diabetes mellitus and its complications : report of a WHO consultation. Part 1, Diagnosis and classification of diabetes mellitus, 1999. Available: https://apps.who.int/iris/handle/10665/66040
- 64. Nederlandse Vereniging voor Obstetrie en Gynaecologie Richtlijn Hypertensieve aandoeningen in de zwangerschap, 2011. Available: https://richtlijnendatabase.nl/richtlijn/hypertensieve_aandoeningen_in_de_zwangerschap/hypertensieve_aandoeningen_-_startpagina.html
- 65. Nederlandse Vereniging voor Obstetrie en Gynaecologie Richtlijn Foetale groeirestrictie, 2018. Available: https://www.nvog.nl/wp-content/uploads/2018/08/NVOG-richtlijn-FGR-2017-definitief-incl.-aanpassingen-Doppler-ACM-aug.-2018.pdf
- 66. Visser GHA, Eilers PHC, Elferink-Stinkens PM, et al. . New Dutch reference curves for birthweight by gestational age. Early Hum Dev 2009;85:737–44. 10.1016/j.earlhumdev.2009.09.008 [DOI] [PubMed] [Google Scholar]
- 67. Stocks J, Sly PD, Tepper RS, et al. . Infant respiratory function testing. New York: Wiley-Liss, 1996. [Google Scholar]
- 68. Galley JD, Bailey M, Kamp Dush C, et al. . Maternal obesity is associated with alterations in the gut microbiome in toddlers. PLoS One 2014;9:e113026 10.1371/journal.pone.0113026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Ley RE. Obesity and the human microbiome. Curr Opin Gastroenterol 2010;26:5–11. 10.1097/MOG.0b013e328333d751 [DOI] [PubMed] [Google Scholar]
- 70. Lundgren SN, Madan JC, Emond JA, et al. . Maternal diet during pregnancy is related with the infant stool microbiome in a delivery mode-dependent manner. Microbiome 2018;6 10.1186/s40168-018-0490-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Seganfredo FB, Blume CA, Moehlecke M, et al. . Weight-Loss interventions and gut microbiota changes in overweight and obese patients: a systematic review. Obes Rev 2017;18:832–51. 10.1111/obr.12541 [DOI] [PubMed] [Google Scholar]
- 72. Kerr CA, Grice DM, Tran CD, et al. . Early life events influence whole-of-life metabolic health via gut microflora and gut permeability. Crit Rev Microbiol 2015;41:326–40. 10.3109/1040841X.2013.837863 [DOI] [PubMed] [Google Scholar]
- 73. Koren O, Goodrich JK, Cullender TC, et al. . Host remodeling of the gut microbiome and metabolic changes during pregnancy. Cell 2012;150:470–80. 10.1016/j.cell.2012.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Dominguez-Bello MG, Costello EK, Contreras M, et al. . Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A 2010;107:11971–5. 10.1073/pnas.1002601107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Dominguez-Bello MG, De Jesus-Laboy KM, Shen N, et al. . Partial restoration of the microbiota of cesarean-born infants via vaginal microbial transfer. Nat Med 2016;22:250–3. 10.1038/nm.4039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Kon IY, Shilina NM, Gmoshinskaya MV, et al. . The study of breast milk IGF-1, leptin, ghrelin and adiponectin levels as possible reasons of high weight gain in breast-fed infants. Ann Nutr Metab 2014;65:317–23. 10.1159/000367998 [DOI] [PubMed] [Google Scholar]
- 77. Sadr Dadres G, Whitaker KM, Haapala JL, et al. . Relationship of maternal weight status before, during, and after pregnancy with breast milk hormone concentrations. Obesity 2019;27:621–8. 10.1002/oby.22409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Lipkie TE, Morrow AL, Jouni ZE, et al. . Longitudinal survey of carotenoids in human milk from urban cohorts in China, Mexico, and the USA. PLoS One 2015;10:e0127729 10.1371/journal.pone.0127729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Nelissen ECM, Dumoulin JCM, Busato F, et al. . Altered gene expression in human placentas after IVF/ICSI. Hum Reprod 2014;29:2821–31. 10.1093/humrep/deu241 [DOI] [PubMed] [Google Scholar]
- 80. Herdman M, Gudex C, Lloyd A, et al. . Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 2011;20:1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Janssen MF, Pickard AS, Golicki D, et al. . Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res 2013;22:1717–27. 10.1007/s11136-012-0322-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Wilkinson MD, Dumontier M, Aalbersberg IJJ, et al. . The fair guiding principles for scientific data management and stewardship. Sci Data 2016;3 10.1038/sdata.2016.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Catalano P, deMouzon SH. Maternal obesity and metabolic risk to the offspring: why lifestyle interventions may have not achieved the desired outcomes. Int J Obes 2015;39:642–9. 10.1038/ijo.2015.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Temel S, van Voorst SF, Jack BW, et al. . Evidence-Based preconceptional lifestyle interventions. Epidemiol Rev 2014;36:19–30. 10.1093/epirev/mxt003 [DOI] [PubMed] [Google Scholar]
- 85. Hillemeier MM, Downs DS, Feinberg ME, et al. . Improving women's preconceptional health: findings from a randomized trial of the strong healthy women intervention in the central Pennsylvania women's health study. Womens Health Issues 2008;18:S87–96. 10.1016/j.whi.2008.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Lan L, Harrison CL, Misso M, et al. . Systematic review and meta-analysis of the impact of preconception lifestyle interventions on fertility, obstetric, fetal, anthropometric and metabolic outcomes in men and women. Hum Reprod 2017;32:1925–40. 10.1093/humrep/dex241 [DOI] [PubMed] [Google Scholar]
- 87. Mutsaerts MAQ, Kuchenbecker WKH, Mol BW, et al. . Dropout is a problem in lifestyle intervention programs for overweight and obese infertile women: a systematic review. Hum Reprod 2013;28:979–86. 10.1093/humrep/det026 [DOI] [PubMed] [Google Scholar]
- 88. Burgess E, Hassmén P, Pumpa KL. Determinants of adherence to lifestyle intervention in adults with obesity: a systematic review. Clin Obes 2017;7:123–35. 10.1111/cob.12183 [DOI] [PubMed] [Google Scholar]
- 89. Willeboordse M, van de Kant KDG, Tan FES, et al. . Correction: a multifactorial weight reduction programme for children with overweight and asthma: a randomized controlled trial. PLoS One 2016;12:e0181130 10.1371/journal.pone.0181130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Hutchinson SG, van Breukelen G, van Schayck CP, et al. . Motivational interviewing and urine cotinine feedback to stop passive smoke exposure in children predisposed to asthma: a randomised controlled trial. Sci Rep 2017;7:15473 10.1038/s41598-017-15158-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Rijks JM, Plat J, Mensink RP, et al. . Children with morbid obesity benefit equally as children with overweight and obesity from an ongoing care program. J Clin Endocrinol Metab 2015;100:3572–80. 10.1210/jc.2015-1444 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-030236supp001.pdf (63.2KB, pdf)
bmjopen-2019-030236supp002.pdf (55.2KB, pdf)
bmjopen-2019-030236supp003.pdf (57.6KB, pdf)
bmjopen-2019-030236supp004.pdf (33.4KB, pdf)
bmjopen-2019-030236supp005.pdf (33.5KB, pdf)