Abstract
The complexity of asthma is underscored by the number of cell types and mediators implicated in the pathogenesis of this heterogeneous syndrome. Type 2 CD4+ T-cells (Th2) and more recently, type 2 innate lymphoid cells dominate current descriptions of asthma pathogenesis. However, another important source of these type 2 cytokines, especially interleukin (IL)-5 and IL-13, are CD8+ T-cells, which are increasingly proposed to play an important role in asthma pathogenesis, because they are abundant and are comparatively insensitive to corticosteroids. Many common triggers of asthma exacerbations are mediated via corticosteroid-resistant pathways involving neutrophils and CD8+ T-cells. Extensive murine data reveal the plasticity of CD8+ T-cells and their capacity to enhance airway inflammation and airway dysfunction. In humans, Tc2 cells are predominant in fatal asthma, while in stable state, severe eosinophilic asthma is associated with greater numbers of Tc2 than Th2 cells in blood, bronchoalveolar lavage fluid and bronchial biopsies. Tc2 cells strongly express CRTH2, the receptor for prostaglandin D2, the cysteinyl leukotriene receptor 1 and the leukotriene B4 receptor. When activated, these elicit Tc2 cell chemotaxis and production of chemokines and type 2 and other cytokines, resulting directly or indirectly in eosinophil recruitment and survival. These factors position CD8+ Tc2 cells as important and underappreciated effector cells contributing to asthma pathogenesis. Here, we review recent advances and new insights in understanding the pro-asthmatic functions of CD8+ T-cells in eosinophilic asthma, especially corticosteroid-resistant asthma, and the molecular mechanisms underlying their pathologic effector function.
Short abstract
Alongside Th2 and ILC2 cells, CD8+ T-cells are a cellular source of type 2 cytokines. We review recent findings and insights into the pathologic effector functions of type 2 CD8+ T-cells in eosinophilic asthma, especially steroid-resistant disease. http://bit.ly/2KbVGL2
Introduction
The complex heterogeneity of asthma is reflected in the number of cell types, mediators and pathways described in the pathogenesis of this syndrome [1]. The clinical variability between patients and even in the same patient at different stages of their disease suggest different mechanistic pathways [2, 3]. T-lymphocytes play a major role in the pathophysiology of asthma, but that alone does not address involvement of the many different subsets of T-cells. Moreover, the pathogenesis of asthma has been linked to the production of type 2 cytokines, which can be expressed by several cell types in the lung. Type 2 CD4+ T-cells (Th2) and their capacity to secrete pro-allergic cytokines, interleukin (IL)-4, IL-5 and IL-13 dominate descriptions of asthma pathogenesis [4], particularly eosinophilic and corticosteroid-responsive asthma. Type 2 innate lymphoid cells (ILC2), which are lineage-negative and lack a T-cell receptor (TCR), have received attention based on their early presence and capacity for similar type 2 cytokine production [5]. Th9 cells act via IL-9 to enhance pro-allergic cytokine expression, airway mast cell recruitment, eosinophilia, airway hyperresponsiveness (AHR) and mucus cell metaplasia in murine models [6]. Th17 cells and their release of IL-17 are proposed to trigger a neutrophilic response in the airways leading to corticosteroid-refractory asthma [7], although, to date, blockade of IL-9 [8] and IL-17 [9] have not proved effective in clinical trials. Invariant natural killer T-cells were implicated in promoting AHR in mice [10], although these cells proved to be rare in human airways [11], in contrast to the abundant mucosal associated invariant T-cell subset [12]. Countering these pro-allergic lymphocyte responses are regulatory T-cells, natural and inducible, attenuating asthma responses through secretion of IL-10 and transforming growth factor-β [13–15]. In contrast to CD4+ T-cells, the role of CD8+ T-cells was suggested to balance the responses of CD4+ T-cells through the secretion of interferon (IFN)-γ [16]. However, until recently few studies have directly examined the presence or role of CD8+ T-cells in asthma pathogenesis. Nonetheless, in experimental models and where they have been examined in human asthma, CD8+ T-cells were proposed to play an important role in asthma pathogenesis, in large part because they are insensitive to corticosteroids compared with CD4+ T-cells and because they have the capacity to undergo transcriptional reprogramming from IFN-γ-secreting cells (Tc1) to type 2 cytokine secreting cells (Tc2), especially producing IL-13 and IL-5 [17]. These two factors position CD8+ Tc2 cells as potentially important effector cells in asthma pathogenesis, especially in severe, corticosteroid-resistant asthma.
Corticosteroid-resistant asthma
Corticosteroids have multiple mechanisms of action, so it is likely that their effects in asthma occur via several mechanisms, acting on corticosteroid-sensitive cells which undergo apoptosis or in attenuating susceptible pathways and functional programmes. Although corticosteroids remain “first-line” therapy in asthma, increasingly there is a recognition that some patients experience severe asthma with persistent symptoms despite high-dose inhaled or oral corticosteroids [18]. It is likely that other cell types and pathways, which are corticosteroid-resistant, underlie the immunopathology in these individuals, labelled as corticosteroid-resistant asthmatics. Furthermore, corticosteroids have incomplete efficacy in preventing or treating exacerbations [19, 20], supporting this notion that the diverse triggers for these events (table 1) involve distinct cell types which are more intrinsically corticosteroid-resistant, including neutrophils, Th17 cells [21] and potentially CD8+ T-cells [17]. It is for this group of severe asthmatics that many of the newer biologic agents have been targeted.
TABLE 1.
Common triggers for asthma exacerbations are mediated by different pathways, frequently involving steroid-unresponsive neutrophils and CD8 cells
| Allergen exposure | Viral infection | Ozone/diesel exhaust | Cigarette smoke | Bacterial infection | |
| Predominant pathway | Th2 cells, IgE | Th1 cells, leukotrienes | Th1 cells, leukotrienes | Th1 cells, leukotrienes | Th17 cells, IL-1β, IL-6, TNF |
| Predominant effector cells | Eosinophils, Mast-cells, CD4 T-cells | Neutrophils, CD8 T-cells | Neutrophils, CD8 T-cells | Neutrophils, CD8 T-cells | Neutrophils |
| Steroid responsiveness | High | Low | Low | Low | Low |
Th1/2 cells: type 1/2 CD4+ T-cells; IL: interleukin; TNF: tumour necrosis factor.
CD8+ Tc2 cells in experimental allergic airways disease
In addition to CD4+ Th2 cells and type 2 ILCs, the role of type 2 cytokine-secreting CD8+ Tc2 cells in allergic airways disease has been demonstrated extensively in models of experimental asthma. A number of studies in mice reported that CD8+ T-cells play a protective role in allergic disease [22–26]. Regulatory or suppressive effects on lung allergic responses were associated with secretion of type 1 cytokines such as IL-12 and IFN-γ [16, 25, 26]. In contrast, the plasticity of CD8+ T-cells and their pro-asthmatic activities have now been confirmed in many studies. Depletion of CD8+ T-cells attenuated AHR and airway inflammation in mice exposed to allergen exclusively via the airways, in the absence of systemic sensitisation [27]. The responses were restored following reconstitution of CD8+ T-cells, but not IL-13-deficient CD8+ T-cells. CD8+ Tc2 cells have been shown to be prime sources of type 2 cytokines [28–32]. Mice deficient in CD8 develop significantly lower AHR, eosinophilic inflammation and IL-13 levels in bronchoalveolar lavage (BAL) fluid compared with wild-type mice, and these responses are restored by adoptive transfer of antigen-primed CD8+ T-cells [24, 28, 33]. The capacity of CD8+ T-cells to produce type 2 cytokines in mice was dependent on interactions between CD4+ and CD8+ T-cells with allergen-sensitised CD4+ T-cells providing the critical differentiation factor, IL-4 [28].
Transcriptional reprogramming of CD8+ T-cells from a Tc1 to a Tc2 phenotype
CD8+ T-cells, similar to other T-cell subsets, exhibit plasticity and can undergo transcriptional reprogramming, redirecting their functional activities. Antigen-specific CD8+ T-cells committed to IFN-γ production, when exposed to IL-4 in vitro or in an atopic environment, transit through distinct differentiation stages characterised by changes in transcription and translation, resulting in IL-13-producing CD8+ T-cells [34] (figure 1). In CD8+ T-cells, IL-4 resulted in the epigenetic poising of the Il13 locus through the gain of permissive and loss of repressive histone modifications, which were co-regulated with recruitment of RNA polymerase II. In addition, IL-4 was required for Gata3 expression in CD8+ T-cells and IL-4-dependent recruitment of GATA3 protein to the Il-13 promoter. Thus, in an allergic inflammatory lung microenvironment containing IL-4, eosinophilic asthma resulted from CD8+ T-cells epigenetically poised for Tc2 conversion via differential histone modifications at lineage-specific promoter regions [34].
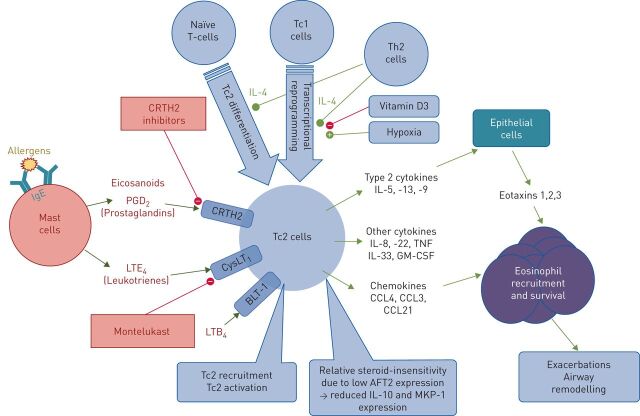
FIGURE 1.
Under the influence of interleukin-(IL)-4, type 2 CD8+ (Tc2) cells differentiate from naïve CD8+ T-cells or arise by transcriptional reprograming of Tc1 cells. Tc2 cells highly express chemoattractant receptor-homologous molecule expressed on Th2 cells (CRTH2), a receptor for prostaglandin D2 (PGD2). In addition, Tc2 cells express the cysteinyl leukotriene receptor 1 (CysLT1) and leukotriene B4 receptor (BLT-1). Inflammatory stimuli, such as cross-linking of immunoglobulin (Ig)E on mast cells, leads to production of eicosanoids. Through CRTH2, PGD2 elicits Tc2 cell chemotaxis, activation and production of chemokines, type 2 cytokines and other cytokines, resulting directly or indirectly in eosinophil recruitment and survival. In turn, airway eosinophilia is associated with airway remodelling and exacerbations. ATF2: activating transcription factor-2; CCL: C-C motif chemokine ligand; GM-CSF: granulocyte–macrophage colony-stimulating factor; LT: leukotriene; MKP: mitogen-activated protein kinase phosphatase; Th2 cells: type 2 CD4+ T-cells; TNF: tumour necrosis factor.
Corticosteroid-insensitivity of CD8+ T-cells
How might these Tc2 cells contribute to corticosteroid-resistant disease? Corticosteroids effectively suppress inflammatory responses through repression of many immune genes by means of interaction with the glucocorticoid receptor. However, susceptibility to corticosteroids differs among T-cell subpopulations and states of maturity [35]. Administration of corticosteroids to asthmatic patients results in significant decreases in numbers of CD4+ but not CD8+ T-cells in peripheral blood [36]. Activated human [37] and mouse [38] CD8+ T-cells are more resistant to corticosteroids than CD4+ T-cells. Therefore, other than CD4+ T-cells, CD8+ T-effector cells are proposed to play an important role in the pathophysiology of inflammatory diseases, especially after initiation of corticosteroid treatment.
Glucocorticoid insensitivity of lymphocytes has also been described in a number of human diseases [39–43] with data demonstrating that human CD8+ T-cells, similar to mouse CD8+ T-cells, are relatively corticosteroid-insensitive compared to CD4+ T-cells [37, 44]. One mechanism which may explain this differential sensitivity to corticosteroids is lower expression of the DNA binding protein and histone acetyltransferase activating transcription factor-2 (ATF2) in CD8+ than CD4+ T-cells [44]. While the inhibitory (transrepression) immunosuppressive effects of corticosteroids on cytokine secretion and cell proliferation are similar in both subsets, as ATF2 is required for corticosteroid-induced transactivation, CD8+ T-cells have reduced corticosteroid-induced transactivation including reduced IL-10 induction [44].
CYP11A1 activation is required for CD8+ Tc2 differentiation
Activation of the steroidogenic enzyme, CYP11A1 is an essential component in the development of Tc2-mediated experimental asthma. This mitochondrial P450 cytochrome is the first and rate-limiting enzyme in steroidogenesis converting cholesterol to pregnanolone. In the presence of IL-4, CYP11A1 enzymatic activation was a critical regulator of Tc2 conversion, resulting in increased IL-13 and decreased IFN-γ production [34, 45]. Of interest, vitamin D3 is a key modulator of the functional conversion of CD8+ T-cells from an IFN-γ- to an IL-13-producing cell [45]. This appears to be, at least in part, through the regulation of CYP11A1 enzymatic activation, an effect driven by vitamin D3-mediated changes in the recruitment of vitamin D receptor (VDR) transcription factors to the promoter region of CYP11A1. This was parallelled by changes in the enzymatic activation of CYP11A1 and the prevention of lung allergic responses. Of note, in humans, an epistatic effect between genetic variants in CYP11A1 and VDR was shown with protective effects on the development of asthma in children [45].
Hypoxia enhances CD8+Tc2 differentiation
Another feature distinguishing CD8+ T-cells from CD4+ T-cells is the response to tissue hypoxia, which occurs in many pathological conditions including asthma and promotes expression of genes through post-translational modifications and stabilisation of the α-subunits of hypoxia-inducible factors (HIF-1α and HIF-2α) [46]. Although hypoxia can inhibit T-lymphocyte function, robust T-cell responses occur at many hypoxic inflammatory sites [47, 48] and hypoxic exposure significantly amplified CD8+ Tc2 differentiation, with increased release of IL-13 in vitro and augmentation of lung allergic responses in vivo [49]. The IL-4-dependent increases in Tc2 differentiation under hypoxia were dependent on HIF-1α. This combination of corticosteroid insensitivity and activation of the hypoxia response pathway and HIF-1α upregulation resulting in increased IL-13 production in Tc2 cells may thus contribute to maintenance of corticosteroid-resistant asthma.
CD8+ T-cells in human asthma
The discovery in the early 1990s of the pathogenic role of type-2 cytokines constituted a key conceptual advance. The seminal work by Robinson et al. [50] used in situ hybridisation to show elevated type 2 cytokine mRNA for IL-2, -3, -4 and -5 in BAL fluid cytospins from atopic asthmatics compared to healthy controls. Follow-up studies demonstrated activation measured by CD25 upregulation of CD4+ cells, but not CD8+ cells, during allergen challenge [51], and was associated with symptoms and impaired lung function [52]. Many subsequent studies supported the paradigm of pathogenic type 2 secreting CD4+ Th2 cells in asthma pathogenesis, dominating asthma thinking and research [1, 53]. Importantly, many of these studies did not directly examine the presence or function of CD8+ T-lymphocytes. Moreover, in many of the molecular studies identifying type 2 signatures in cells from the airways of asthmatics, the specific cell source of these cytokines was not determined [20], even though numbers of CD8+ T-cells outnumbered CD4+ T-cells [54–57]. It is only more recently that other type 2 cytokine secreting cells in the lung have been identified [57–62] and that CD8+ T-cells have also been recognised as major producers of type 2 cytokines. Indeed, human blood CD8+ T-cells produce more IL-4 than CD4+ T-cells [63]. This was subsequently confirmed by in situ hybridisation and immunohistochemistry on bronchial biopsies, showing that IL-4 and IL-5 were produced by both CD4+ and CD8+ T-cells, as well as mast cells and eosinophils within the airways [64]. Moreover, CD8+ cells secreting IL-4, -5 and -13 and specific for the dominant house dust mite aeroallergen Derp 1 are found in human atopic disease and associated with disease severity, with responses believed to be mediated through antigen cross-presentation [32].
CD8+ T-cells in fatal asthma
In human asthma, indirect evidence for the pathogenic involvement of CD8+ T-cells is provided by studies of post mortem samples. Fatal asthma is characterised by infiltrates of T-cells, macrophages and activated eosinophils, which, in contrast to stable asthma, is associated with a CD8+ T-cell predominance, with CD8+ cells outnumbering CD4+ cells 2:1 in the interstitium of distal airways, and 6:1 in the lamina propria of proximal airways [65]; in another study, CD8+ cells were present, but numbers were not increased [66]. In addition, asthma death was associated with activated peribronchial cytotoxic CD8+ T-cells with higher expression of CD25 and a 10-fold higher expression of the cytotoxicity marker perforin [67]. These cells expressed both type-1 (IFN-γ) and type 2 (IL-4) cytokines, but asthma death was associated with an increase of more than double in the ratio of type 2 to type 1 cells, implicating Tc2 cells specifically in the inflammatory process. Similarly, a post mortem study from Brazil found higher numbers of granzyme A- and granzyme B-expressing cells in the lamina propria and adventitia in fatal asthma, out of which ∼50% of granzyme-positive cells were CD8+ [68].
CD8+ T-cells in stable asthma
While observations from fatal asthma may not be fully generalisable, a number of clinical studies have observed associations between airway CD8+ T-cell frequencies and stable asthma. CD8+ T-cell frequencies were increased in BAL fluid in asthma; this increase was greater for CD8+ cells than for CD4+ or CD3+ cells [69, 70], and was correlated with AHR [70]. Increased BAL fluid CD8+ cells have been described specifically associated with eosinophilic lung diseases including asthma [71].
In bronchial biopsies, CD8+ T-cells were enriched in the lamina propria in asthma [57, 72], being present despite regular inhaled corticosteroid treatment, and were also associated with AHR measured by methacholine challenge, while AHR did not correlate with CD4+ T-cells.
More recently, the Unbiased Biomarkers in Prediction of Respiratory Disease Outcomes (U-BIOPRED) study performed a large transcriptomic and immunohistochemical analysis on epithelial brushings and biopsies from 107 patients with moderate–severe asthma and identified two distinct subtypes associated with high type 2 cytokine expression [73]. The group characterised by the highest submucosal eosinophilia, high exhaled nitric oxide fraction, frequent exacerbations and high oral corticosteroid use were marked by significantly increased CD3+ and CD8+ T-cells, but with no differences in CD4+ T-cells, again showing a strong association between CD8+ cells and eosinophilic airways disease. In contrast, in type-2-low, IL-6-high asthma, sputum transcriptomics found lower expression of CD8+ T-cell signatures [74].
Activation of CD8+ T-cells
Significant activation of circulating CD8+ T-cells in peripheral blood has been seen in severe asthma and correlated with downregulation of specific microRNAs (miR-146a/b and miR-28–5p) and differential expression of multiple intronic long noncoding RNAs which might regulate CD8+ T cell activities [75]. Asthma is associated with increased expression in circulating CD8+ T-cells, specifically of mitogen kinase kinase 3, a proinflammatory member of the p38 mitogen activated protein kinase pathway implicated in neutrophil recruitment [76].
Multiple genome wide association studies have identified ORMDL3 as an important asthma-susceptibility locus associated with childhood asthma [54, 77–79]. A recent epigenetic analysis of human peripheral blood leukocyte subsets found decreased DNA methylation levels in the 5′ untranslated region of ORMDL3 specifically in CD8+ T-cells, which might explain the increased ORMDL3 mRNA expression observed in CD8+ T-cells compared with other leukocytes [79]. As increased ORMDL3 expression promotes T-cell activation and pro-inflammatory cytokine production, this also associates CD8+ T-cells in the link between this risk-allele and asthma pathogenesis.
Within the airways, CD8+ T-cells may be activated by allergens cross-presented by class I major histocompatibility complex on airway dendritic cells [25], and indeed BAL fluid CD8+ frequencies are increased after segmental allergen challenge [80]. Additionally, activated human CD8+ T-cells express the receptors for the key airway epithelial cell alarmins IL-33 [81] and thymic stromal lymphopoietin (TSLP) and its ligation by TSLP enhances their proliferation [82, 83]. TSLP also acts indirectly via pulmonary inflammatory dendritic cells to enhance antiviral CD8+ T cell responses [84] and to induce IL-5/-13-producing CD4+ [85] and CD8+ T-cells [86]. Likewise, IL-33 potently enhances antiviral CD8+ T-cell responses [87]. An association of CD8+ cells with cigarette use [56] suggests that smoke may also activate CD8+ cells, while Tc2 cells in both mice and humans express perforin and granzyme [88] and induction of granzyme A mRNA and protein have been demonstrated in response to diesel fume particulates in human bronchoscopy samples [89].
CD8+ Tc2 conversion during viral infection
Viruses play a key role in acute asthma [90], being responsible for ∼80% of asthma exacerbations [91]. Thus, it might be expected that viral infections contribute to an association between CD8+ cells and asthma (table 1). Although the mechanisms supporting these associations are incompletely understood, viral infection of epithelial cells can trigger the release of important alarmins such as IL-25 and IL-33 increasing type 2-related airway inflammation and mucin production [92, 93]. In experimental models of asthma, virus-specific CD8+ T-cells can switch to IL-5 production and induce airway eosinophilia [94]. In vitro studies showed that IL-4 could switch virus-specific CD8+ T-cells to IL-5 production. Thus, a viral infection which leads to recruitment of virus-specific CD8+ T-cells to the airways, in an atopic asthma environment, the presence of IL-4 could trigger CD8+ Tc2 conversion and release of type 2 cytokines. Severe respiratory syncytial virus (RSV) infection in early life is suspected to play a role in the later development of wheezing and asthma [95]. In contrast to initial RSV infection at a later stage, early infection in mice with RSV followed by reinfection at a later stage resulted in increased AHR, airway eosinophilic inflammation, mucus hyperproduction and IL-13-producing CD8+ T-cells [96, 97]. Inhibition of IL-13 abolished AHR and mucus hyperproduction. As discussed later, a unique population of IL-6Rα-high effector memory CD8+ T-cells was found in peripheral blood of asthmatics with an increased frequency compared to healthy control subjects [98]. These effector memory CD8+ T-cells exclusively produced IL-5 and IL-13 in response to asthma-associated RSV and bacterial superantigens [98]. These data, in contrast to those from an in vitro study [99], suggest that Tc2 cell populations arising from polarisation early in life might persist long term in vivo.
Longitudinal studies of CD8+ cells are associated with lung function decline
Few longitudinal studies have investigated T-cell subsets. However, one study performed bronchoscopies before and 2 years into a 7.5-year prospective follow-up of a cohort of adults with atopic asthma [100]. Over time, decline in post-bronchodilator forced expiratory volume in 1 s (FEV1) correlated not with typical markers of eosinophilic inflammation (bronchial biopsy eosinophils) or remodelling (subepithelial reticular membrane thickness), but with bronchial biopsy CD8+ cells measured either at baseline or at the 2-year time point. A strength of this study is that the findings were confirmed by subsequent follow-up of the same patients at 14 years [101]. Decline in FEV1 was highest in those with high CD8+ numbers at baseline or those with high CD8+ numbers or high granzyme B expression at the 14-year time point; these associations were specific to CD8+ cells, being weaker or not observed with CD4+ cells.
Subsets of peripheral blood CD8+ cells
These human studies describe disease associations with CD8+ cells, but what is known of type 2 cytokine-secreting CD8+ T-cells, specifically? Definitions of Tc2 cells vary between studies and are based either on intracellular expression of a type 2 cytokine (IL-4 [102], IL-5 [64], IL-13 [4, 88]) in CD8+ T-cells or on co-expression of CD8 with a surrogate surface marker such as the prostaglandin D2 receptor 2, CRTH2 [88]).
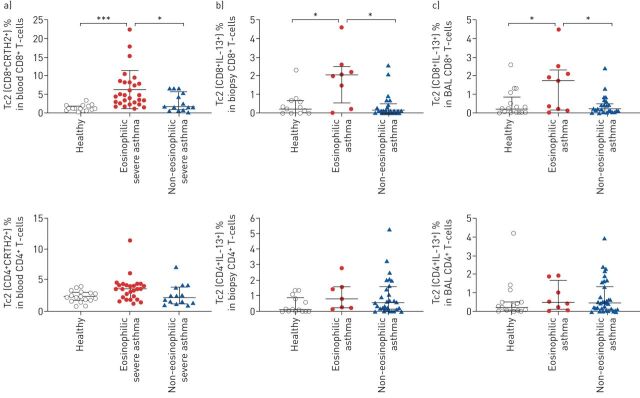
Resting blood CD8+ cells produce more IL-4 in asthma than in health [103], and several studies reported increases in Tc2 cells in peripheral blood in asthma, while this association was typically stronger than with Th2 cells. In one report, circulating CD8+IL-4+ cells were increased in allergic asthma [103], and in another CD8+IL-5+ cells were significantly increased in eosinophilic asthma [104]; this was not true for CD4+IL-5+ cells [104]. Similarly, peripheral blood CD8+IL-13+ Tc2 cells were increased in asthma, and correlated most with severe disease and with the eosinophilic phenotype [88] (figure 2). In the same cohort, significant increases in CD4+IL-13+ Th2 cells were observed only in mild disease [4, 88], but not with eosinophilic disease. Tc2 frequencies were associated with nasal polyposis and with current cigarette use. Moreover, a positive correlation was shown between frequencies of peripheral blood CD8+IL13+ Tc2 cells and type 2 lung inflammation, measured by expression of IL-4 by sputum T-cells, but again there was no such association with blood CD4+IL13+ Th2 cells [88]. Similarly, we and others have found using CRTH2 as a surface marker for type 2 cells, that CD4+CRTH2+ Th2 cells were not associated with eosinophilic disease [88, 105], while peripheral blood CD8+CRTH2+ cells were strongly associated with the severe eosinophilic phenotype [88].
FIGURE 2.
Tc2 cells are enriched in eosinophilic asthma. a) Frequencies of CD3+CD8+CRTH2+ Tc2 and CD3+CD4+CRTH2+ Th2 cells in CD4+ or CD8+ T-cells in total peripheral blood leucocytes compared between healthy controls and severe asthma patient groups (eosinophilic and non-eosinophilic) in a cohort from Oxford, UK by flow cytometry. b,c) Tc2 cells are increased in lung in eosinophilic asthma in a cohort from Southampton, UK. Frequencies of CD3+CD8+IL-13+ and CD3+CD4+IL-13+ T-cells in b) bronchial biopsy and c) bronchoalveolar lavage (BAL) compared between healthy controls and asthma groups (eosinophilic and non-eosinophilic) by intracellular cytokine staining. *: p<0.05, ***: p<0.001. Reproduced and modified from [88] with permission.
Data regarding peripheral blood IFN-γ-secreting Tc1 cells are less clear-cut. Three studies reported increased frequencies of IFN-γ-secreting CD8+ cells in peripheral blood in asthma versus health [106–108]. Conversely, another report found reduced blood Tc1 cells in allergic asthma [109] and we observed no significant differences between asthma and health [110].
CD8+IL6-Rα+ cells
IL-6Rα expression has been described as a surface marker for effector memory CD8+ T (TEM)-cells. IL-6 is a pro-inflammatory cytokine and biomarker of systemic inflammation and metabolic dysfunction, and has been associated with more severe, obesity-related asthma [111], and with frequent exacerbations in poorly controlled, non-type-2 asthma [112]. CD8+IL-6Rα+ TEM-cells express the type-2-associated nuclear transcription factor GATA3, produce high levels of IL-5 and IL-13 and are increased in the peripheral blood of asthmatics [98].
Tc2 cells in human airway tissue
As with peripheral blood, BAL fluid CD8+ T-cell lines produced more IL-5 in asthma than in health [113]. Likewise, unstimulated sputum CD8+ T-cells produced more IL-4 and IL-5 in asthma than in health, and this increase was related more closely to the severity of AHR for CD8+ than CD4+ T-cells, both in terms of the magnitude and the statistical strength of the association [102]. Similarly, both CD8+ and CD4+ IL-4 producing T-cells were increased in BAL fluid in asthma and eosinophilic bronchitis, but the strength of this association was stronger for Tc2 than Th2 cells [107].
BLT1 is the high-affinity receptor for leukotriene B4 expressed on a variety of cell types [114]. In allergen-sensitised and -challenged mice, it was the CD8+BLT1+ and not the CD8+BLT1− T-cell subset that was associated with IL-13-mediated asthma and dependent on LTB4 release from mast cells [115–118]. Using BLT1 as a surface marker of type 2 cells, we found CD8+BLT1+ and CD8+BLT1+IL-13+ cells to be more increased in BAL fluid in asthma than in health, with the highest expression of IL-13 found in CD8+ rather than CD4+ cells [107]. Furthermore, this CD8+BLT1+IL-13+ subset in BAL correlated with the presence of asthma and with markers of atopy (serum IgE), airway remodelling (reticular basement membrane thickness) and the degree of airflow obstruction (FEV1 and forced expiratory flow at 25–75% of forced vital capacity) [119].
This finding of a stronger disease association for Tc2 than Th2 cells emerges consistently from multiple studies, including data from cohorts studied in Southampton and Oxford (UK). While some increases in CD4+IL-13+ Th2 cells were demonstrated in bronchial biopsies in asthma overall, Th2 cells were only significantly enriched in mild, steroid-naïve, atopic asthma, but were not associated with airway eosinophilia [88]. Th2-cells were not enriched in steroid-treated moderate asthma, or subjects with severe asthma on high dose inhaled or oral steroids [4]. In contrast, in the same cohort we observed increases in CD8+IL-13+ Tc2 cells in eosinophilic asthma, in bronchial biopsies and in BAL fluid. Moreover, these high bronchial biopsy CD8+IL-13+ Tc2 frequencies were associated with high bronchodilator reversibility.
How might Tc2 cells contribute to inflammation in eosinophilic asthma? The onset of severe eosinophilic asthma commonly follows a viral respiratory tract infection, which could promote CD8+ T-cell activation, and in the presence of IL-4, this would favour transcriptional reprogramming and conversion to Tc2 cells. These cells might then be further activated either in an antigen-specific manner by aeroallergens or viruses, or in a TCR-independent manner by inflammatory mediators. Since Tc2 cells express CRTH2 and CysLT1 (receptors for prostaglandin D2 (PGD2) and leukotriene E4 (LTE4), respectively), we investigated their ligands in the airways in asthma. PGD2 was increased in the airways of all severe asthma patients, but elevated LTE4 was specific to the severe eosinophilic phenotype [88]. In vitro, PGD2 and LTE4 were chemattractants for Tc2 cells. This attraction was synergistic and could be inhibited by a CRTH2 antagonist, and to a lesser extent by the CysLT1 antagonist montelukast. PGD2 and LTE4 synergistically enhanced Tc2 production of IL-5 and IL-13, and this effect was more potent in Tc2 than Th2 cells. A specific source of these inflammatory mediators could be mast cells. IgE cross-linking of mast cells triggered release of PGD2 and LTE4 [88], which could induce both migration and production of IL-5 and IL-13 by Tc2 cells. In turn, supernatants from stimulated Tc2 cells contained IL-5 and granulocyte–macrophage colony-stimulating factor and could directly activate eosinophils and upregulate eotaxin release from bronchial epithelial cells [88].
Conclusion
In summary, in addition to the many descriptions of involvement of CD4+ Th2 cells in human asthma, increasingly, studies have shown increased frequencies and activation of Tc2 cells both in peripheral blood and in airway tissues. In a number of these studies, the strength of Tc2 cell associations with eosinophilic phenotypes and with markers of airways inflammation and bronchial hyperreactivity were consistently stronger than those observed with Th2 cells, and were consistent with experimental findings in allergen-sensitised mice. Recent mechanistic human studies have begun to elucidate how these cells could participate in driving the type 2 pro-inflammatory responses in severe eosinophilic asthma. Phenotypic differences between T-cell subsets suggest that Tc2 cells may be less steroid-responsive, and are implicated in a variety of triggers known to elicit asthma exacerbations. Given the advances in technology and approaches to limited cell number analyses in lung tissue and BAL fluid, it is important to combine determinations of both CD4+ and CD8+ T-cell numbers and function in the various phenotypes of asthma, not only in steady state, but over the longitudinal course of asthma in the same patient and in cohorts.
Many questions remain unresolved, including what are the original environmental or genetic triggers for Tc2 development? What are the critical epigenetic modifications which maintain these cells as a persistent population expressing common transcriptional programmes? And ultimately, of greatest interest, how might these underappreciated contributors to severe asthma be targeted therapeutically?
Footnotes
Submitted article, peer reviewed.
Author contributions: T.S.C. Hinks, R.D. Hoyle and E.W. Gelfand jointly conceived the article, conducted the literature review and drafted the manuscript. All authors approved the final manuscript.
Conflict of interest: T.S.C. Hinks reports grants from The Wellcome Trust and The Guardians of the Beit Fellowship, during the conduct of the study; and reports personal fees from AstraZeneca, TEVA, and Peer Voice, outside the submitted work.
Conflict of interest: R.D. Hoyle has nothing to disclose.
Conflict of interest: E.W. Gelfand has nothing to disclose.
Support statement: This work was supported by grants from the Wellcome Trust (104553/z/14/z, 211050/Z/18/z) and the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC) (to T.S.C. Hinks), the Medical Research Council (UK) (to R.D. Hoyle) and grants HL-36577 and AI-77609 from the National Institutes of Health (to E.W. Gelfand). The views expressed are those of the authors and not those of the NHS, NIHR or NIH. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Lambrecht BN, Hammad H. The immunology of asthma. Nat Immunol 2015; 16: 45–56. [DOI] [PubMed] [Google Scholar]
- 2.Chung KF, Adcock IM. How variability in clinical phenotypes should guide research into disease mechanisms in asthma. Ann Am Thorac Soc 2013; 10: Suppl. S109–S117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gelfand EW, Alam R. The other side of asthma: steroid-refractory disease in the absence of TH2-mediated inflammation. J Allergy Clin Immunol 2015; 135: 1196–1198. [DOI] [PubMed] [Google Scholar]
- 4.Hinks TS, Zhou X, Staples KJ, et al. . Innate and adaptive T-cells in asthmatic patients: relationship to severity and disease mechanisms. J Allergy Clin Immunol 2015; 136: 323–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walker JA, Barlow JL, McKenzie AN. Innate lymphoid cells – how did we miss them? Nat Rev Immunol 2013; 13: 75–87. [DOI] [PubMed] [Google Scholar]
- 6.Koch S, Sopel N, Finotto S. Th9 and other IL-9-producing cells in allergic asthma. Semin Immunopathol 2017; 39: 55–68. [DOI] [PubMed] [Google Scholar]
- 7.Zhao J, Lloyd CM, Noble A. Th17 responses in chronic allergic airway inflammation abrogate regulatory T-cell-mediated tolerance and contribute to airway remodeling. Mucosal Immunol 2013; 6: 335–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oh CK, Leigh R, McLaurin KK, et al. . A randomized, controlled trial to evaluate the effect of an anti-interleukin-9 monoclonal antibody in adults with uncontrolled asthma. Respir Res 2013; 14: 93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Busse WW, Holgate S, Kerwin E, et al. . Randomized, double-blind, placebo-controlled study of brodalumab, a human anti-IL-17 receptor monoclonal antibody, in moderate to severe asthma. Am J Respir Crit Care Med 2013; 188: 1294–1302. [DOI] [PubMed] [Google Scholar]
- 10.Umetsu DT, Dekruyff RH. Immune dysregulation in asthma. Curr Opin Immunol 2006; 18: 727–732. [DOI] [PubMed] [Google Scholar]
- 11.Vijayanand P, Seumois G, Pickard C, et al. . Invariant natural killer T cells in asthma and chronic obstructive pulmonary disease. N Engl J Med 2007; 356: 1410–1422. [DOI] [PubMed] [Google Scholar]
- 12.Hinks TS. Mucosal-associated invariant T cells in autoimmunity, immune-mediated diseases and airways disease. Immunology 2016; 148: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sakaguchi S, Sakaguchi N, Asano M, et al. . Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol 1995; 155: 1151–1164. [PubMed] [Google Scholar]
- 14.Joetham A, Takeda K, Taube C, et al. . Naturally occurring lung CD4+CD25+ T cell regulation of airway allergic responses depends on IL-10 induction of TGF-β. J Immunol 2007; 178: 1433–1442. [DOI] [PubMed] [Google Scholar]
- 15.Joetham A, Schedel M, O'Connor BP, et al. . Inducible and naturally occurring regulatory T cells enhance lung allergic responses through divergent transcriptional pathways. J Allergy Clin Immunol 2017; 139: 1331–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takeda K, Dow SW, Miyahara N, et al. . Vaccine-induced CD8+ T cell-dependent suppression of airway hyperresponsiveness and inflammation. J Immunol 2009; 183: 181–190. [DOI] [PubMed] [Google Scholar]
- 17.Gelfand EW, Joetham A, Wang M, et al. . Spectrum of T-lymphocyte activities regulating allergic lung inflammation. Immunol Rev 2017; 278: 63–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chung KF, Wenzel SE, Brozek JL, et al. . International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J 2014; 43: 343–373. [DOI] [PubMed] [Google Scholar]
- 19.Bel EH, Sousa A, Fleming L, et al. . Diagnosis and definition of severe refractory asthma: an international consensus statement from the Innovative Medicine Initiative (IMI). Thorax 2011; 66: 910–917. [DOI] [PubMed] [Google Scholar]
- 20.Peters MC, Kerr S, Dunican EM, et al. . Refractory airway type 2 inflammation in a large subgroup of asthmatic patients treated with inhaled corticosteroids. J Allergy Clin Immunol 2019; 143: 104–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singhania A, Wallington JC, Smith CG, et al. . Multitissue transcriptomics delineates the diversity of airway T cell functions in asthma. Am J Respir Cell Mol Biol 2018; 58: 261–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kallinich T, Beier KC, Wahn U, et al. . T-cell co-stimulatory molecules: their role in allergic immune reactions. Eur Respir J 2007; 29: 1246–1255. [DOI] [PubMed] [Google Scholar]
- 23.O'Sullivan SM. Asthma death, CD8+ T cells, and viruses. Proc Am Thorac Soc 2005; 2: 162–165. [DOI] [PubMed] [Google Scholar]
- 24.Miyahara N, Swanson BJ, Takeda K, et al. . Effector CD8+ T cells mediate inflammation and airway hyper-responsiveness. Nat Med 2004; 10: 865–869. [DOI] [PubMed] [Google Scholar]
- 25.Wells JW, Cowled CJ, Giorgini A, et al. . Regulation of allergic airway inflammation by class I-restricted allergen presentation and CD8 T-cell infiltration. J Allergy Clin Immunol 2007; 119: 226–234. [DOI] [PubMed] [Google Scholar]
- 26.Sarantopoulos S, Lu L, Cantor H. Qa-1 restriction of CD8+ suppressor T cells. J Clin Invest 2004; 114: 1218–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hamelmann E, Oshiba A, Paluh J, et al. . Requirement for CD8+ T cells in the development of airway hyperresponsiveness in a marine model of airway sensitization. J Exp Med 1996; 183: 1719–1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koya T, Miyahara N, Takeda K, et al. . CD8+ T cell-mediated airway hyperresponsiveness and inflammation is dependent on CD4+IL-4+ T cells. J Immunol 2007; 179: 2787–2796. [DOI] [PubMed] [Google Scholar]
- 29.Erard F, Wild MT, Garcia-Sanz JA, et al. . Switch of CD8 T cells to noncytolytic CD8-CD4- cells that make TH2 cytokines and help B cells. Science 1993; 260: 1802–1805. [DOI] [PubMed] [Google Scholar]
- 30.Sad S, Marcotte R, Mosmann TR. Cytokine-induced differentiation of precursor mouse CD8+ T-cells into cytotoxic CD8+ T cells secreting Th1 or Th2 cytokines. Immunity 1995; 2: 271–279. [DOI] [PubMed] [Google Scholar]
- 31.Cerwenka A, Carter LL, Reome JB, et al. . In vivo persistence of CD8 polarized T cell subsets producing type 1 or type 2 cytokines. J Immunol 1998; 161: 97–105. [PubMed] [Google Scholar]
- 32.Seneviratne SL, Jones L, King AS, et al. . Allergen-specific CD8+ T cells and atopic disease. J Clin Invest 2002; 110: 1283–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miyahara N, Takeda K, Kodama T, et al. . Contribution of antigen-primed CD8+ T cells to the development of airway hyperresponsiveness and inflammation is associated with IL-13. J Immunol 2004; 172: 2549–2558. [DOI] [PubMed] [Google Scholar]
- 34.Jia Y, Takeda K, Han J, et al. . Stepwise epigenetic and phenotypic alterations poise CD8+ T cells to mediate airway hyperresponsiveness and inflammation. J Immunol 2013; 190: 4056–4065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fernández-Ruiz E, Rebollo A, Nieto MA, et al. . IL-2 protects T cell hybrids from the cytolytic effect of glucocorticoids. Synergistic effect of IL-2 and dexamethasone in the induction of high-affinity IL-2 receptors. J Immunol 1989; 143: 4146–4151. [PubMed] [Google Scholar]
- 36.Corrigan CJ, Haczku A, Gemou-Engesaeth V, et al. . CD4 T-lymphocyte activation in asthma is accompanied by increased serum concentrations of interleukin-5. Effect of glucocorticoid therapy. Am Rev Respir Dis 1993; 147: 540–547. [DOI] [PubMed] [Google Scholar]
- 37.Chung EH, Jia Y, Ohnishi H, et al. . Leukotriene B4 receptor 1 is differentially expressed on peripheral T cells of steroid-sensitive and -resistant asthmatics. Ann Allergy Asthma Immunol 2014; 112: 211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ohnishi H, Miyahara N, Dakhama A, et al. . Corticosteroids enhance CD8+ T cell-mediated airway hyperresponsiveness and allergic inflammation by upregulating leukotriene B4 receptor 1. J Allergy Clin Immunol 2008; 121: 864–871. [DOI] [PubMed] [Google Scholar]
- 39.Thewissen M, Somers V, Hellings N, et al. . CD4+CD28null T cells in autoimmune disease: pathogenic features and decreased susceptibility to immunoregulation. J Immunol 2007; 179: 6514–6523. [DOI] [PubMed] [Google Scholar]
- 40.Fasth AE, Snir O, Johansson AA, et al. . Skewed distribution of proinflammatory CD4+CD28null T cells in rheumatoid arthritis. Arthritis Res Ther 2007; 9: R87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yokoyama Y, Fukunaga K, Ikeuchi H, et al. . The CD4+CD28null and the regulatory CD4+CD25high T-cell phenotypes in patients with ulcerative colitis during active and quiescent disease, and following colectomy. Cytokine 2011; 56: 466–470. [DOI] [PubMed] [Google Scholar]
- 42.Vallejo AN. CD28 extinction in human T cells: altered functions and the program of T-cell senescence. Immunol Rev 2005; 205: 158–169. [DOI] [PubMed] [Google Scholar]
- 43.Yao H, Rahman I. Role of histone deacetylase 2 in epigenetics and cellular senescence: implications in lung inflammaging and COPD. Am J Physiol Lung Cell Mol Physiol 2012; 303: L557–L566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li LB, Leung DY, Strand MJ, et al. . ATF2 impairs glucocorticoid receptor-mediated transactivation in human CD8+ T cells. Blood 2007; 110: 1570–1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schedel M, Jia Y, Michel S, et al. . 1,25D3 prevents CD8+Tc2 skewing and asthma development through VDR binding changes to the Cyp11a1 promoter. Nat Commun 2016; 7: 10213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Palazon A, Goldrath AW, Nizet V, et al. . HIF transcription factors, inflammation, and immunity. Immunity 2014; 41: 518–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dang EV, Barbi J, Yang HY, et al. . Control of TH17/Treg balance by hypoxia-inducible factor 1. Cell 2011; 146: 772–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kumar V, Gabrilovich DI. Hypoxia-inducible factors in regulation of immune responses in tumour microenvironment. Immunology 2014; 143: 512–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ning F, Takeda K, Schedel M, et al. . Hypoxia enhances CD8+ TC2 cell-dependent airway hyperresponsiveness and inflammation through hypoxia-inducible factor 1α. J Allergy Clin Immunol 2019; 143: 2026–2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Robinson DS, Hamid Q, Ying S, et al. . Predominant TH2-like bronchoalveolar T-lymphocyte population in atopic asthma. N Engl J Med 1992; 326: 298–304. [DOI] [PubMed] [Google Scholar]
- 51.Robinson D, Hamid Q, Bentley A, et al. . Activation of CD4+ T-cells, increased TH2-type cytokine mRNA expression, and eosinophil recruitment in bronchoalveolar lavage after allergen inhalation challenge in patients with atopic asthma. J Allergy Clin Immunol 1993; 92: 313–324. [DOI] [PubMed] [Google Scholar]
- 52.Robinson DS, Bentley AM, Hartnell A, et al. . Activated memory T helper cells in bronchoalveolar lavage fluid from patients with atopic asthma: relation to asthma symptoms, lung function, and bronchial responsiveness. Thorax 1993; 48: 26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Larché M, Robinson DS, Kay AB. The role of T lymphocytes in the pathogenesis of asthma. J Allergy Clin Immunol 2003; 111: 450–463. [DOI] [PubMed] [Google Scholar]
- 54.Ferreira MA, McRae AF, Medland SE, et al. . Association between ORMDL3, IL1RL1 and a deletion on chromosome 17q21 with asthma risk in Australia. Eur J Hum Genet 2011; 19: 458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Leckie MJ, Jenkins GR, Khan J, et al. . Sputum T lymphocytes in asthma, COPD and healthy subjects have the phenotype of activated intraepithelial T-cells (CD69+ CD103+). Thorax 2003; 58: 23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ravensberg AJ, Slats AM, van Wetering S, et al. . CD8+ T cells characterize early smoking-related airway pathology in patients with asthma. Respir Med 2013; 107: 959–966. [DOI] [PubMed] [Google Scholar]
- 57.Hirosako S, Goto E, Tsumori K, et al. . CD8 and CD103 are highly expressed in asthmatic bronchial intraepithelial lymphocytes. Int Arch Allergy Immunol 2010; 153: 157–165. [DOI] [PubMed] [Google Scholar]
- 58.Fallon PG, Ballantyne SJ, Mangan NE, et al. . Identification of an interleukin (IL)-25-dependent cell population that provides IL-4, IL-5, and IL-13 at the onset of helminth expulsion. J Exp Med 2006; 203: 1105–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kang Z, Swaidani S, Yin W, et al. . Epithelial cell-specific Act1 adaptor mediates interleukin-25-dependent helminth expulsion through expansion of Lin −c-Kit+ innate cell population. Immunity 2012; 36: 821–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fort MM, Cheung J, Yen D, et al. . IL-25 induces IL-4, IL-5, and IL-13 and Th2-associated pathologies in vivo. Immunity 2001; 15: 985–995. [DOI] [PubMed] [Google Scholar]
- 61.Hammad H, Plantinga M, Deswarte K, et al. . Inflammatory dendritic cells – not basophils – are necessary and sufficient for induction of Th2 immunity to inhaled house dust mite allergen. J Exp Med 2010; 207: 2097–2111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lloyd CM, Hessel EM. Functions of T cells in asthma: more than just TH2 cells. Nat Rev Immunol 2010; 10: 838–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Stanciu LA, Shute J, Holgate ST, et al. . Production of IL-8 and IL-4 by positively and negatively selected CD4+ and CD8+ human T cells following a four-step cell separation method including magnetic cell sorting (MACS). J Immunol Methods 1996; 189: 107–115. [DOI] [PubMed] [Google Scholar]
- 64.Ying S, Humbert M, Barkans J, et al. . Expression of IL-4 and IL-5 mRNA and protein product by CD4+ and CD8+ T cells, eosinophils, and mast cells in bronchial biopsies obtained from atopic and nonatopic (intrinsic) asthmatics. J Immunol 1997; 158: 3539–3544. [PubMed] [Google Scholar]
- 65.Faul JL, Tormey VJ, Leonard C, et al. . Lung immunopathology in cases of sudden asthma death. Eur Respir J 1997; 10: 301–307. [DOI] [PubMed] [Google Scholar]
- 66.de Magalhães Simões S, dos Santos MA, da Silva Oliveira M, et al. . Inflammatory cell mapping of the respiratory tract in fatal asthma. Clin Exp Allergy 2005; 35: 602–611. [DOI] [PubMed] [Google Scholar]
- 67.O'Sullivan S, Cormican L, Faul JL, et al. . Activated, cytotoxic CD8+ T lymphocytes contribute to the pathology of asthma death. Am J Respir Crit Care Med 2001; 164: 560–564. [DOI] [PubMed] [Google Scholar]
- 68.Annoni R, Silva LF, Nussbaumer-Ochsner Y, et al. . Increased expression of granzymes A and B in fatal asthma. Eur Respir J 2015; 45: 1485–1488. [DOI] [PubMed] [Google Scholar]
- 69.Walker C, Kaegi MK, Braun P, et al. . Activated T-cells and eosinophilia in bronchoalveolar lavages from subjects with asthma correlated with disease severity. J Allergy Clin Immunol 1991; 88: 935–942. [DOI] [PubMed] [Google Scholar]
- 70.Kelly CA, Stenton SC, Ward C, et al. . Lymphocyte subsets in bronchoalveolar lavage fluid obtained from stable asthmatics, and their correlations with bronchial responsiveness. Clin Exp Allergy 1989; 19: 169–175. [DOI] [PubMed] [Google Scholar]
- 71.Walker C, Bauer W, Braun RK, et al. . Activated T cells and cytokines in bronchoalveolar lavages from patients with various lung diseases associated with eosinophilia. Am J Respir Crit Care Med 1994; 150: 1038–1048. [DOI] [PubMed] [Google Scholar]
- 72.Sont JK, Han J, van Krieken JM, et al. . Relationship between the inflammatory infiltrate in bronchial biopsy specimens and clinical severity of asthma in patients treated with inhaled steroids. Thorax 1996; 51: 496–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kuo CS, Pavlidis S, Loza M, et al. . A transcriptome-driven analysis of epithelial brushings and bronchial biopsies to define asthma phenotypes in U-BIOPRED. Am J Respir Crit Care Med 2017; 195: 443–455. [DOI] [PubMed] [Google Scholar]
- 74.Peters MC, Ringel L, Dyjack N, et al. . A transcriptomic method to determine airway immune dysfunction in T2-high and T2-low asthma. Am J Respir Crit Care Med 2019; 199: 465–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tsitsiou E, Williams AE, Moschos SA, et al. . Transcriptome analysis shows activation of circulating CD8+ T cells in patients with severe asthma. J Allergy Clin Immunol 2012; 129: 95–103. [DOI] [PubMed] [Google Scholar]
- 76.Holand T, Riffo-Vasquez Y, Spina D, et al. . A role for mitogen kinase kinase 3 in pulmonary inflammation validated from a proteomic approach. Pulm Pharmacol Ther 2014; 27: 156–163. [DOI] [PubMed] [Google Scholar]
- 77.Moffatt MF, Gut IG, Demenais F, et al. . A large-scale, consortium-based genomewide association study of asthma. N Engl J Med 2010; 363: 1211–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Galanter J, Choudhry S, Eng C, et al. . ORMDL3 gene is associated with asthma in three ethnically diverse populations. Am J Respir Crit Care Med 2008; 177: 1194–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Acevedo N, Reinius LE, Greco D, et al. . Risk of childhood asthma is associated with CpG-site polymorphisms, regional DNA methylation and mRNA levels at the GSDMB/ORMDL3 locus. Hum Mol Genet 2015; 24: 875–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Bratke K, Böttcher B, Leeder K, et al. . Increase in granzyme B+ lymphocytes and soluble granzyme B in bronchoalveolar lavage of allergen challenged patients with atopic asthma. Clin Exp Immunol 2004; 136: 542–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yang Q, Li G, Zhu Y, et al. . IL-33 synergizes with TCR and IL-12 signaling to promote the effector function of CD8+ T cells. Eur J Immunol 2011; 41: 3351–3360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Akamatsu T, Watanabe N, Kido M, et al. . Human TSLP directly enhances expansion of CD8+ T cells. Clin Exp Immunol 2008; 154: 98–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rochman Y, Leonard WJ. The role of thymic stromal lymphopoietin in CD8+ T cell homeostasis. J Immunol 2008; 181: 7699–7705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yadava K, Sichelstiel A, Luescher IF, et al. . TSLP promotes influenza-specific CD8+ T-cell responses by augmenting local inflammatory dendritic cell function. Mucosal Immunol 2013; 6: 83–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Watanabe N, Hanabuchi S, Marloie-Provost MA, et al. . Human TSLP promotes CD40 ligand-induced IL-12 production by myeloid dendritic cells but maintains their Th2 priming potential. Blood 2005; 105: 4749–4751. [DOI] [PubMed] [Google Scholar]
- 86.Gilliet M, Soumelis V, Watanabe N, et al. . Human dendritic cells activated by TSLP and CD40L induce proallergic cytotoxic T cells. J Exp Med 2003; 197: 1059–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Bonilla WV, Fröhlich A, Senn K, et al. . The alarmin interleukin-33 drives protective antiviral CD8+ T cell responses. Science 2012; 335: 984–989. [DOI] [PubMed] [Google Scholar]
- 88.Hilvering B, Hinks TSC, Stöger L, et al. . Synergistic activation of pro-inflammatory type-2 CD8+ T lymphocytes by lipid mediators in severe eosinophilic asthma. Mucosal Immunol 2018; 11: 1408–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pfeffer PE, Ho TR, Mann EH, et al. . Urban particulate matter stimulation of human dendritic cells enhances priming of naive CD8 T lymphocytes. Immunology 2018; 153: 502–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Johnston SL, Pattemore PK, Sanderson G, et al. . The relationship between upper respiratory infections and hospital admissions for asthma: a time-trend analysis. Am J Respir Crit Care Med 1996; 154: 654–660. [DOI] [PubMed] [Google Scholar]
- 91.Johnston SL, Pattemore PK, Sanderson G, et al. . Community study of role of viral infections in exacerbations of asthma in 9–11 year old children. BMJ 1995; 310: 1225–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jackson DJ, Makrinioti H, Rana BM, et al. . IL-33-dependent type 2 inflammation during rhinovirus-induced asthma exacerbations in vivo. Am J Respir Crit Care Med 2014; 190: 1373–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Beale J, Jayaraman A, Jackson DJ, et al. . Rhinovirus-induced IL-25 in asthma exacerbation drives type 2 immunity and allergic pulmonary inflammation. Sci Transl Med 2014; 6: 256ra134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Coyle AJ, Erard F, Bertrand C, et al. . Virus-specific CD8+ cells can switch to interleukin 5 production and induce airway eosinophilia. J Exp Med 1995; 181: 1229–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sigurs N, Gustafsson PM, Bjarnason R, et al. . Severe respiratory syncytial virus bronchiolitis in infancy and asthma and allergy at age 13. Am J Respir Crit Care Med 2005; 171: 137–141. [DOI] [PubMed] [Google Scholar]
- 96.Dakhama A, Park JW, Taube C, et al. . The enhancement or prevention of airway hyperresponsiveness during reinfection with respiratory syncytial virus is critically dependent on the age at first infection and IL-13 production. J Immunol 2005; 175: 1876–1883. [DOI] [PubMed] [Google Scholar]
- 97.Han J, Dakhama A, Jia Y, et al. . Responsiveness to respiratory syncytial virus in neonates is mediated through thymic stromal lymphopoietin and OX40 ligand. J Allergy Clin Immunol 2012; 130: 1175–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lee N, You S, Shin MS, et al. . IL-6 receptor α defines effector memory CD8+ T cells producing Th2 cytokines and expanding in asthma. Am J Respir Crit Care Med 2014; 190: 1383–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Fox A, Harland KL, Kedzierska K, et al. . Exposure of human CD8+ T cells to type-2 cytokines impairs division and differentiation and induces limited polarization. Front Immunol 2018; 9: 1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.van Rensen EL, Sont JK, Evertse CE, et al. . Bronchial CD8 cell infiltrate and lung function decline in asthma. Am J Respir Crit Care Med 2005; 172: 837–841. [DOI] [PubMed] [Google Scholar]
- 101.den Otter I, Willems LN, van Schadewijk A, et al. . Lung function decline in asthma patients with elevated bronchial CD8, CD4 and CD3 cells. Eur Respir J 2016; 48: 393–402. [DOI] [PubMed] [Google Scholar]
- 102.Cho SH, Stanciu LA, Holgate ST, et al. . Increased interleukin-4, interleukin-5, and interferon-γ in airway CD4+ and CD8+ T cells in atopic asthma. Am J Respir Crit Care Med 2005; 171: 224–230. [DOI] [PubMed] [Google Scholar]
- 103.Stanciu LA, Shute J, Promwong C, et al. . Increased levels of IL-4 in CD8+ T cells in atopic asthma. J Allergy Clin Immunol 1997; 100: 373–378. [DOI] [PubMed] [Google Scholar]
- 104.Stoeckle C, Simon HU. CD8+ T cells producing IL-3 and IL-5 in non-IgE-mediated eosinophilic diseases. Allergy 2013; 68: 1622–1625. [DOI] [PubMed] [Google Scholar]
- 105.Palikhe NS, Laratta C, Nahirney D, et al. . Elevated levels of circulating CD4+ CRTh2+ T cells characterize severe asthma. Clin Exp Allergy 2016; 46: 825–836. [DOI] [PubMed] [Google Scholar]
- 106.Magnan AO, Mély LG, Camilla CA, et al. . Assessment of the Th1/Th2 paradigm in whole blood in atopy and asthma. Increased IFN-γ-producing CD8+ T cells in asthma. Am J Respir Crit Care Med 2000; 161: 1790–1796. [DOI] [PubMed] [Google Scholar]
- 107.Brightling CE, Symon FA, Birring SS, et al. . TH2 cytokine expression in bronchoalveolar lavage fluid T lymphocytes and bronchial submucosa is a feature of asthma and eosinophilic bronchitis. J Allergy Clin Immunol 2002; 110: 899–905. [DOI] [PubMed] [Google Scholar]
- 108.Cho SH, Stanciu LA, Begishivili T, et al. . Peripheral blood CD4+ and CD8+ T cell type 1 and type 2 cytokine production in atopic asthmatic and normal subjects. Clin Exp Allergy 2002; 32: 427–433. [DOI] [PubMed] [Google Scholar]
- 109.Grob M, Schmid-Grendelmeier P, Joller-Jemelka HI, et al. . Altered intracellular expression of the chemokines MIP-1α, MIP-1β and IL-8 by peripheral blood CD4+ and CD8+ T cells in mild allergic asthma. Allergy 2003; 58: 239–245. [DOI] [PubMed] [Google Scholar]
- 110.Hinks TSC. The Role of T Cell Subsets in the Airways in Asthma. Southampton, University of Southampton, 2013. [Google Scholar]
- 111.Peters MC, McGrath KW, Hawkins GA, et al. . Plasma interleukin-6 concentrations, metabolic dysfunction, and asthma severity: a cross-sectional analysis of two cohorts. Lancet Respir Med 2016; 4: 574–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jevnikar Z, Östling J, Ax E, et al. . Epithelial IL-6 trans-signaling defines a new asthma phenotype with increased airway inflammation. J Allergy Clin Immunol 2019; 143: 577–590. [DOI] [PubMed] [Google Scholar]
- 113.Till S, Li B, Durham S, et al. . Secretion of the eosinophil-active cytokines interleukin-5, granulocyte/macrophage colony-stimulating factor and interleukin-3 by bronchoalveolar lavage CD4+ and CD8+ T cell lines in atopic asthmatics, and atopic and non-atopic controls. Eur J Immunol 1995; 25: 2727–2731. [DOI] [PubMed] [Google Scholar]
- 114.Gelfand EW. Importance of the leukotriene B4-BLT1 and LTB4-BLT2 pathways in asthma. Semin Immunol 2017; 33: 44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Miyahara N, Takeda K, Miyahara S, et al. . Leukotriene B4 receptor-1 is essential for allergen-mediated recruitment of CD8+ T cells and airway hyperresponsiveness. J Immunol 2005; 174: 4979–4984. [DOI] [PubMed] [Google Scholar]
- 116.Miyahara N, Takeda K, Miyahara S, et al. . Requirement for leukotriene B4 receptor 1 in allergen-induced airway hyperresponsiveness. Am J Respir Crit Care Med 2005; 172: 161–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Taube C, Miyahara N, Ott V, et al. . The leukotriene B4 receptor (BLT1) is required for effector CD8+ T cell-mediated, mast cell-dependent airway hyperresponsiveness. J Immunol 2006; 176: 3157–3164. [DOI] [PubMed] [Google Scholar]
- 118.Miyahara N, Ohnishi H, Miyahara S, et al. . Leukotriene B4 release from mast cells in IgE-mediated airway hyperresponsiveness and inflammation. Am J Respir Cell Mol Biol 2009; 40: 672–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Dakhama A, Collins ML, Ohnishi H, et al. . IL-13-producing BLT1-positive CD8 cells are increased in asthma and are associated with airway obstruction. Allergy 2013; 68: 666–673. [DOI] [PMC free article] [PubMed] [Google Scholar]