Disease control strategies that focus on acute primary syphilis and core transmission groups could enhance the control of syphilis among men who have sex with men.
Supplemental digital content is available in the text.
Abstract
The syphilis epidemic among men who have sex with men (MSM) has been increasing steadily. Many syphilis control programs focus on assuring treatment of all persons diagnosed with early syphilis without prioritizing acute primary syphilis or specific subgroups. Acute primary syphilis is highly infectious and contributes to a high proportion of new cases. Surveillance data show that among MSM with incident syphilis (primary or secondary) only about 35% are identified in the primary stage, indicating that most primary cases are missed and untreated. Patients with primary syphilis and large numbers of sex partners may play a major role in maintaining syphilis transmission. Considering those issues, sexually transmitted disease (STD) programs should consider increasing their focus on primary syphilis by assigning primary cases the highest priority, expanding client and clinician health education, and increasing the detection of primary syphilis through increased serologic screening frequency among high-risk MSM. Furthermore, syphilis control programs should implement steps to identify asymptomatic high-probable occult primary cases based on low titer (≤1:8) and recent seroconversion. Finally, to address core transmission groups, programs should implement periodic risk assessment to identify persons with a high number of sex partners and offer these individuals risk-reduction counseling, case management, and selective syphilis preexposure or postexposure doxycycline chemoprophylaxis. Although reprioritizing prevention efforts might be challenging, the Centers for Disease Control and Prevention, community advocacy groups, university STD research centers, and national STD prevention training centers can assist by providing support for consensus discussions and direction in developing operational guidance, some of which may be best delivered through STD and human immunodeficiency virus program partnerships.
In the late 1990s syphilis began increasing among men who have sex with men (MSM). In 2017, among men reported with primary or secondary syphilis (P&S) and with known gender of sex partners, 80% were MSM and nearly half (46%) were co-infected with the human immunodeficiency virus (HIV).1 Primary and secondary syphilis has been increasing nationally each year since 2001 and the number of cases reported in 2017 (30,644 cases, 9.5 per 100,000 population) was the highest since 1993.1
Over the past few decades, numerous biomedical and behavioral interventions to control syphilis among MSM have been proposed and some implemented, but little success has been realized.2,3 Recently, calls have been made about the need for new intervention ideas.3–5 Among MSM, modifying sexual behavior and delivering sexually transmitted infection (STI) related health care are difficult to achieve due to stigma, homophobia, and lack of culturally competent medical services. Many of those concerns should be addressed in any comprehensive prevention plan.5,6 However, this commentary is focused primarily on the biomedical intervention components of syphilis control.
The strategy for controlling syphilis is based on the early detection and treatment of infectious cases and the early prophylactic treatment of exposed sex partners.7 However, to be effective that strategy requires a large and well trained public health workforce.7 We propose an approach that may improve the efficacy and efficiency of syphilis control efforts among MSM by focusing on acute infectious primary syphilis and the core groups where transmission is common. Furthermore, those principles will apply to women and heterosexual men.
Our aim is to provide a rationale and supporting data that will encourage sexually transmitted disease (STD) programs to review program operations to evaluate and prioritize those activities which should have the most impact on syphilis transmission. The rationale for this new approach is based on the concepts of the sexually transmitted infection reproductive number7–9 and the core group theory of STI transmission epidemiology.10 Most STD control practitioners are aware of those concepts, but to date monitoring the factors that predict the reproductive number and the characteristics of core group members has not been systematically performed, nor incorporated into syphilis prevention program design and evaluation.
REPRODUCTIVE NUMBER AND CORE GROUP THEORY OF TRANSMISSION
The reproductive number (R0) for syphilis is the average number of new infections produced through sexual exposure by an infectious person. In a given population, R0 indicates whether an infection is increasing (R0 > 1), decreasing (R0 < 1), or remaining stable (R0 = 1). R0 is a function of three essential measures of infection transmission—(B) transmission efficiency, which is the average probability that an infectious person will infect a susceptible sex partner given exposure, (c) number of new susceptible sex partners exposed during the period selected, and (D) the duration of infectiousness expressed as the proportional number of infectious days per period selected. Decreasing the values of B, c, or D lowers the reproductive number R0. Lowering the R0 below 1 will extinguish an epidemic.
Administering antibiotics to infectious patients rapidly limits the duration (D) of the infectious period.7 Preventively treating sex partners incubating infection before becoming infectious also prevents transmission. The STD control programs promote the use of condoms to reduce transmission efficiency (B) and sex partner reduction (c), but few programs routinely monitor these 3 measures (duration of infectious period, condom use and partner numbers) and use them to direct interventions.
At the population level, the core group theory of STI epidemiology postulates that the overall prevalence of STIs in a community is dependent upon the existence of a core transmission group in which a sexual network of infectious patients and susceptible sex partners maintains a persistent reservoir of infection. Without that core group, the R 0 is <1 and the infection cannot be sustained. Core groups often have high STI prevalence, high numbers of new sex partners, and dense sexual networks. Impacting transmission within the core group should lead to a substantial overall STI decrease in the larger community.7–11
PRIMARY SYPHILIS
Importance of Primary Syphilis
Although it is possible to transmit syphilis from any stage of untreated infection, the majority of syphilis transmission most likely occurs through sexual contact with a highly infectious acute primary stage chancre.7,11 Secondary syphilis case patients also have infectious lesions (mucous patches and condyloma lata) which are present in approximately 30% of secondary cases,11,12 and in some secondary cases healing potential infectious primary chancres are still present.13 In one modeling study, transmission probability was set at 0.30 from the primary stage and 0.075 from the secondary stage.11 Another report using empirical data from the national syphilis control program estimated that untreated primary syphilis cases would generate on average 0.17 new infections per week, while secondary case would only generate 0.05 new infections per week.7 Although syphilis transmission probabilities by stage in real-world community settings are difficult to ascertain, considerable secondary stage syphilis transmission seems unlikely because of the lower inherent transmission probability and because patients usually have generalized symptoms (malaise, fever, generalized lymphadenopathy) and appear ill (visible rash) which may inhibit sexual activity during this phase of clinical illness. Transmission during the true latent phase seems very unlikely without the presence of an infectious syphilitic lesion.14
Based on modeling and other studies, promptly treating all persons with primary syphilis and their exposed sex partners will prevent primary syphilis among exposed sex partners and will considerably shorten the overall duration of syphilis infectiousness (D) by directly decreasing the duration of primary infection and indirectly by decreasing the number of secondary cases, and thus reducing the reproductive number (R0).11,15,16 Furthermore, one modeling study indicated that intervening with the very small number of very high-risk core group members (those with ~ 15–25 sex partners per month, >200–300 per year) substantially decreases communitywide syphilis incidence.11
Occult Primary Syphilis—A Syphilis Control Priority
Syphilitic chancres are usually painless and may go unnoticed even when located externally (e.g. genital or perianal area). Among MSM (and women), chancres may also be located in the oropharynx or anal canal/rectum17 and are unrecognized or “occult.” Although most experienced STD clinicians are aware of that, no programmatic strategy has been put forth to identify unrecognized chancres. Because it is impractical in most clinical settings to use screening procedures like anoscopy, laryngoscopy, or other endoscopic examinations to visualize a possible occult lesion, we propose a presumptive diagnosis of occult primary syphilis be made indirectly using serologic titer and other supporting clinical and sexual exposure information.
Low reactive titers (≤1:8): Text book descriptions of persons with clinical primary syphilis indicate that at the time of diagnosis, nontreponemal titers are usually reactive at a low level17 which suggests that low titer reports may include many persons with asymptomatic occult or unreported clinical primary syphilis. A recent study of reported clinical primary cases among men (13,873 with a reactive titer) found at diagnosis that 36% had a low nontreponemal titer (<= 1:8).18 Two other recent studies showed a similar titer distribution.19,20 The task at hand for the STD program is to determine whether a low titer report is a primary infection in the early phase of the 3-week primary stage, a later stage of syphilis infection, previously treated syphilis case (serofast), a repeat titer conducted for treatment monitoring, or a biologic false-positive21 (Fig. 1).
Figure 1.
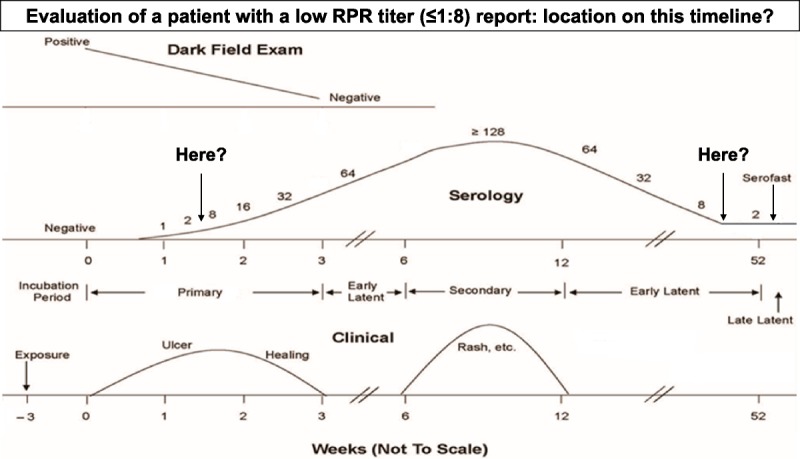
Syphilis symptoms, stages, and serologic titers timeline.
Higher reactive titers (≥ 1:16): As the primary stage of infection progresses, nontreponemal titers can rise to higher levels by the end of the primary stage. The same study of reported clinical primary syphilis among men found at diagnosis 29% had titer of 1:16 to 1:32, and 35% had a titer of ≥ 1:64.18 Some of those cases with higher titer reports may be the result of prior syphilis which can modify the clinical course of subsequent syphilis such that titers are higher and rise more quickly, and disease stages progress more rapidly.22,23 The same pattern has been observed in persons with HIV co-infection which is often a marker of prior syphilis. Repeat syphilis among MSM is relatively common (annual rate of repeat infection ~2–10%).24–26
Communitywide Missed Primary Syphilis—A Bigger Issue
National STD surveillance data show that a low proportion of incident clinical P&S cases are reported in the primary stage. Over the most recent 6-year period (2012–2017), on average, only 32% of P&S cases in the United States were identified in the primary stage. This suggests that a minimum of ~15,000 untreated infectious primary cases are being missed annually. This pattern was also observed among MSM in several state and local health jurisdictions (Table 1). Furthermore, although a considerable number of primary stage syphilis infections are missed among persons with early latent syphilis, estimating the number of missed primary cases among those is difficult because early latent cases are frequently misclassified.27
TABLE 1.
Estimated Annual Primary Syphilis Case Missed Among Reported Primary and Secondary Cases, Total and Among MSM, by Jurisdiction, Syphilis Control Among MSM, 2019
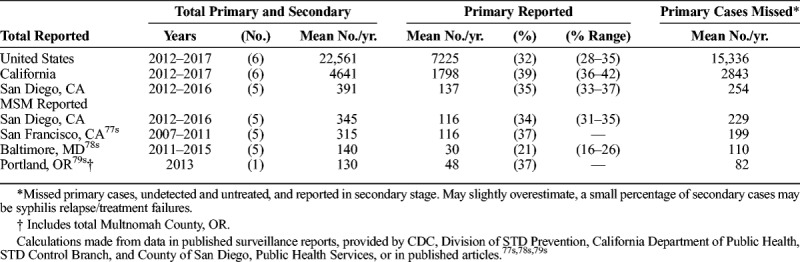
The failure to identify and treat a large proportion of primary syphilis cases is partially explained by occult syphilis in MSM. In San Diego County during 2012 to 2016, among reported male P&S cases, MSM were substantially less likely identified in the primary stage (34%), as were women (27%), compared with heterosexual men (51%) (personal communication, Lawrence Wang, MPH, County of San Diego, December 2018). Analysis of San Diego County reported male P&S cases (2003–2005) showed among MSM who practiced receptive anal sex, only 27% were reported in the primary stage compared with 52% of MSM who did not report receptive anal sex,28 and among men with secondary syphilis, only 13% of MSM reported a history of a primary lesion, compared with 37% of heterosexual men.29 Taken together, those finding strongly suggest that missed and untreated occult primary syphilis occurs frequently among asymptomatic MSM, likely has a duration of infectiousness (D) of 3 or more weeks, and plays an important role in syphilis transmission among MSM.
Factors Contributing to Missed Primary Syphilis
Lack of community-level knowledge about STDs and syphilis in particular may contribute to poor recognition of primary syphilis signs and symptoms and a failure to seek care. Very little information assessing syphilis knowledge among persons at risk has been published. In 2006, one evaluation among US MSM showed that general syphilis knowledge was low.30 More recently, two evaluations of social marketing campaigns showed overall only approximately 40% of respondents who were MSM, knew that syphilis symptoms included a sore or rash.31s,32s Other studies showed among patients seeking care for primary syphilis symptoms, time from symptom onset to care was delayed on average 1 to 2 weeks.33s–35s
Inadequate serologic screening also contributes to missed early syphilis cases among MSM. The Centers for Disease Control and Prevention (CDC) guidelines and others recommend syphilis screening annually for MSM and more frequently for those at high risk.36s–38s Among HIV-infected patients in care, annual screening coverage was ~ 60%.39s,40s A recent modeling study suggested that increasing screening frequency of high-risk MSM to every 3 months was needed to produce a substantial decrease in community syphilis incidence.41s
SYPHILIS INTERVENTIONS
Shifting Operational Priorities to Primary Syphilis
A reordering of priorities to provide timely intervention for persons with primary syphilis at high risk of transmission and their recent sex partners should be a principle concern of syphilis control programs. Some actions can be initiated without much additional effort or resources, those requiring moderate operational changes or more resources can be considered in a phased-in approach, and others may require collaborative efforts locally and substantial support from STD leaders and organizations (Table, Phased-in Management Priorities, Supplemental Digital Content, http://links.lww.com/OLQ/A394).
Syphilis Case Management
Time is of the essence in the management of persons with primary syphilis (clinical or occult) and secondary syphilis with infectious lesions (concomitant syphilitic chancres, condyloma lata, or oral mucous patches). Patients clinically diagnosed will most likely receive treatment at the time of diagnosis, whereas occult primary syphilis is diagnosed by screening serologic testing. Both the provider and STD program very likely will receive the reactive screening test report at the same time, and those patients need to be treated without delay. Sex partner services need to be promptly provided for all locatable sex partners with priority for partners exposed in the past 30 days with top priority for those exposed during the case's symptomatic infectious period (D period). If more than 1 locatable sex partner is reported, multiple field investigators should be assigned to prevent delays in preventive treatment. Weekly meetings of investigator and other program staff should be conducted to review cases and share information about places where cases meet sex partners.
Monitoring primary syphilis intervention activities will require rigorous time-based measures. Systematically collecting reproductive number metrics to analyze and monitor, and separately analyzing primary syphilis case interviews, field services partner records, and other case management activities are also needed. More complex operational activities under the direction of the STD program can be considered and phased-in over time (Table, Phased-in Management Priorities, Supplemental Digital Content, http://links.lww.com/OLQ/A394).
Identifying More Primary Syphilis Cases
Health education for MSM and clinicians: Educational activities should be initiated or expanded for MSM and clinicians to include information about the classic visible signs and symptoms of syphilis, the importance of treatment of a highly infectious syphilitic chancre even though it may be causing little or no discomfort, the treatment advantages of detecting early syphilis, the risk of acute neurosyphilis, and new information about the subtle signs and symptoms of an occult primary lesion located in the anal/rectal area or oropharynx. For clinicians, additional educational materials should also include information on the importance of a routine oropharyngeal and anogenital physical examination of persons at risk of acquiring syphilis, the criteria for diagnosing both high- and intermediate-probable occult primary infection and high-probable core group members (Table 2), and the need for prompt treatment of primary, secondary, and early latent syphilis and preventive treatment of recent sex partners, including a liberal use of presumptive treatment for cases and partners.
TABLE 2.
Occult Primary Syphilis and Core Group Definitions

Serologic screening: Increasing serologic screening frequency to every 3 months for high-risk MSM is recommended. For HIV-infected MSM, syphilis testing can be obtained concurrent with clinical visits, ordered with prescription renewals, measures of CD4 T-cell counts, or plasma HIV viral loads.38s For MSM taking HIV preexposure prophylaxis, syphilis testing should occur at quarterly clinical care visits concomitant with HIV testing. Screening is more likely to occur in HIV care clinics with automated laboratory testing protocols42s–44s and among other clinics with established syphilis screening protocols.45s,46s Additional methods to increase screening among MSM outside of medical care have been described.5,47s,48s
High-risk MSM, especially those who are HIV-infected and not able to decrease risky sexual behaviors,49s,50s may be motivated to participate in frequent screening by making them aware that primary syphilis is highly infectious, treating early/occult primary syphilis requires only a single penicillin injection (versus three injections if the duration of infection cannot be determined), and a new infection may present with serious complications—acute ocular or auditory symptoms or neurosyphilis requiring an intensive diagnostic evaluation, treatment process, and possible long term disability.51s–54s Previous estimates of the risk for acute symptomatic neurosyphilis among MSM with early syphilis are approximately 1.2% to 1.8%,51s,55s,56s but more recent data indicate that the risk of developing vision or hearing changes along with other symptoms or signs of neurosyphilis is 3.5%.57s
Occult primary syphilis determination: Following the identification of latent syphilis, there needs to be a process to determine if the patient has primary syphilis and might have an occult primary lesion. Occult primary syphilis is likely if the patient has a new reactive nontreponemal titer ≤ 1:8, confirmed by a treponemal test, is an MSM, and reports receptive anal/oral sex in the past 3 months. The most important factor in making that determination is whether the reported low titer is a recent seroconversion from a recent nonreactive to reactive titer.
We developed a schematic that provides operational definitions of probable occult primary syphilis. A high-probable case is defined as recent seroconversion from a nonreactive titer within the past 12 months to a reactive titer of ≤1:8. An intermediate-probable case differs from high-probable in that there is no recent nonreactive titer, or the latest was >12 months ago (late seroconversion). Low-probable cases occur among patients with a history of syphilis and no nonreactive nontreponemal titer postsyphilis treatment (Fig. 2, Table 2).
Figure 2.
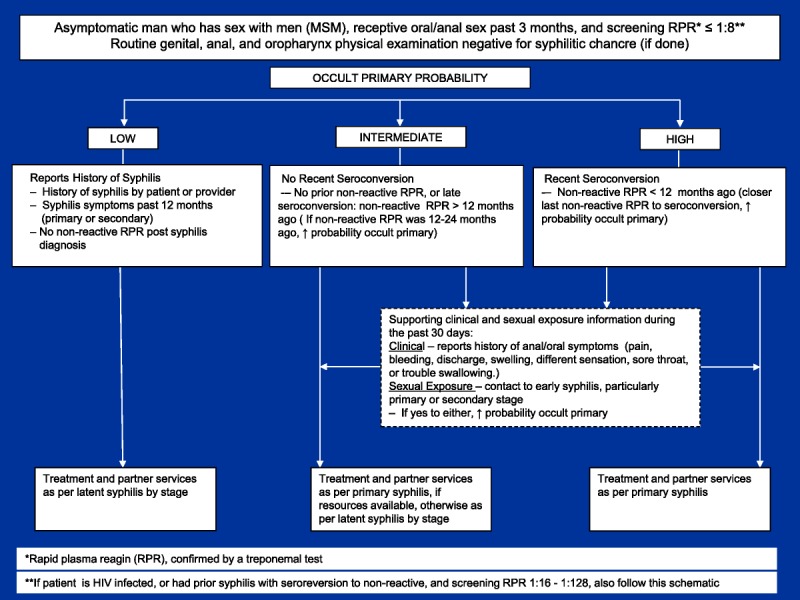
Occult primary syphilis schematic probability determination.
Those case classifications can also be supported with additional information: the shorter the time between the previous nonreactive titer to the reactive seroconversion screening titer, the presence of any subtle anal/oral symptoms, or a history of recent sexual exposure to syphilis, increase the probability estimate of occult primary syphilis (Fig. 2). In addition, an oropharyngeal or anogenital examination may find a visible lesion and thus, clinical primary syphilis. However, the lack of a physical examination should not delay occult primary syphilis investigative and intervention activities. High-probable occult primary syphilis should be managed by the syphilis control program similar to clinical primary syphilis. Intermediate-probable occult primary syphilis can be similarly managed, if resources are available, especially if supporting information increases the probability estimate of occult primary syphilis. Similar to MSM, women with a reactive syphilis screening test may also have occult primary syphilis and should also be evaluated using the schematic. Primary syphilis is often missed in women.
In addition, because prior syphilis may result in rapidly rising higher titers,22,23 MSM with HIV co-infection, or MSM with prior syphilis following adequate treatment (seroreversion to a nonreactive non-treponemal test), with a reactive screening titer of 1:16 to 1:128, should also be evaluated using the same schematic as patients having a screening titer of ≤ 1:8.
Patients showing a 4-fold rise in nontreponemal titer from a low reactive prior nontreponemal titer are difficult to categorize. Such a finding may indicate a new infection, syphilis relapse, or titer fluctuations from changes in immunity. Clinical and prevention services can be managed on a case-by-case basis.
CORE GROUP INTERVENTIONS
Core Group Members
There are many reports describing the characteristics of those in core transmission groups.9,41s,58s–64s Those studies generally concluded that core group transmission interventions may decrease syphilis transmission, and should be implemented and evaluated. However, currently, there is no consensus on an operational definition of a core group member,10 and to our knowledge, no prevalence data or specific core intervention program evaluations have been reported. In the following section we describe ways to identify, classify, and manage probable core group members. Those classifications and interventions will need to be monitored and evaluated.
Identifying Probable Core Group Members
Periodic risk assessment: The key determinants for persons most likely to be syphilis core group members are recent history of syphilis and the number of sex partners in past 30 days. Such information can be obtained through frequent routine periodic assessment of sexual behavior and STI history. Self-administered risk assessment is acceptable to both clinicians and patients seen in STD and HIV clinics.64s–66s Many larger sexual health clinics use kiosks or provide computer tablets for self-administered behavioral data collection. To access most persons at risk for syphilis, we recommend that a brief self-administered risk assessment tool be developed and used by each patient at each visit to an STD, HIV, or men's health clinic, to an HIV testing site, and to each partner receiving partner services. The most important data are the number of sex partners in the past 30 days, the date of the last test for syphilis, syphilis treatment history, and locations for meeting recent sex partners (eg, specific venues, clubs, websites, and social media sites). In addition, including health education information in the risk assessment tool about syphilis signs/symptoms and complications, and the importance of regular frequent testing and prompt treatment, may over time, with repeated use at each visit, increase patients' syphilis knowledge and decrease the time from onset of symptoms to seeking care.
Probable core group members: For the small number of persons with very high numbers of sex partners, we propose a case definition of a high-probable core group member based only on having = > 10 sex partners in the past 30 days. For intermediate-probable core group members, defined as those with 5 to 9 sex partners in the past 30 days, we suggest a subcategory based on HIV infection status and syphilis history (Table 2).
Services for high-probable core group members: High-probable core group members should be actively followed through frequent face-to-face or text-based peer counseling to provide “health coaching services” to improve adherence to recommended screening and risk reduction interventions, to facilitate making referrals to other needed services (mental health or substance use services, if indicated), and to help support use of syphilis preexposure or postexposure chemoprophylaxis.50 The number of high-probable core group members should be very small in any given jurisdiction, but prevention services should be available and might best be initiated and evaluated in partnership with HIV prevention or HIV care programs for patients with high-risk behaviors.
Services for intermediate-probable core group members: For those in the subcategory, program staff should periodically remind those individuals about the importance of frequent syphilis and other STI screening, the location and availability of service providers, the signs and symptoms of syphilis and its complications, and conduct risk assessments.
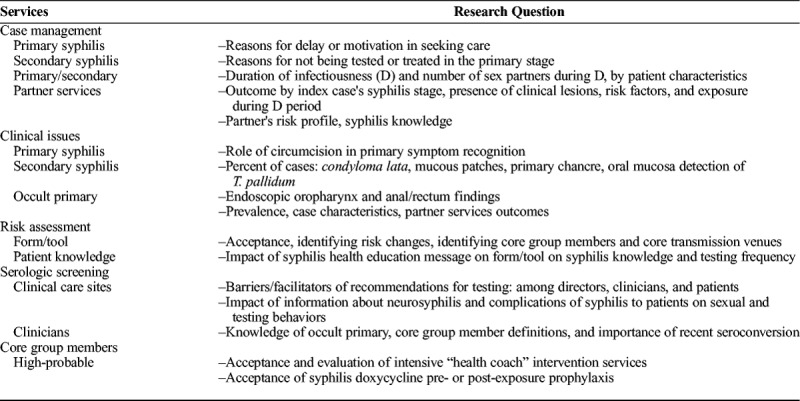
Future Research
Because many of our recommendations and suggestions have not been tested or evaluated, there will be a need for a variety of pilot studies and detailed examination of program operations (Table 3). Case management for high-probable core group members will require a collaborative process to define the specifics and scope of the services and a step-by-step evaluation to address acceptability and impact on syphilis transmission. In addition, clinical research to determine the true frequency of occult primary lesions could be accomplished by endoscopic examination of the oropharynx and the anal canal/rectum among MSM with high-probable occult primary syphilis. Lastly, implementation science research on how to best deliver preexposure or postexposure chemoprophylaxis with doxycycline to maximize impact and minimize adverse effects is urgently needed.
TABLE 3.
Future Research Issues, Syphilis Control Among MSM, 2019
DISCUSSION
The underlying principle supporting the proposed programmatic shift to focus on clinical and occult primary syphilis and the risk of transmission is the acceptance that preventing transmission is a high priority objective of syphilis control. If so, all operational intervention and service delivery activities should be evaluated relative to that objective. Many activities are effective at preventing syphilis transmission whereas some may have minimal or no impact, but are important to carry out to improve personal health, reduce the individual complications of syphilis, and for other reasons. Developing a methodology to classify the transmission impact of different interventions at a very detailed level within the broader groups (ie, surveillance, case interviews, partner services, counseling, and health education) and subsequent monitoring standards are needed to prioritize intervention activities.
A challenge for STD program directors wanting to focus more efforts on primary syphilis will be to implement procedures to evaluate low-titer reactive serologies among MSM to identify those with high-probable asymptomatic occult primary syphilis. In doing so, we encourage adopting the term “occult primary” and assigning a subcategory surveillance code under early latent syphilis to monitor incidence and measures of intervention services. Among high-probable occult primary syphilis, the lowest titer seroconversions are most important because they usually occur in the first 7 to 10 days of the primary stage when timely interventions can have the most impact on the duration of syphilis infectiousness (D). To help accomplish that, we recommend redirecting resources to evaluate all reported reactive serologic tests and developing databases capturing prior nonreactive test results. Patients tested in STD clinics and in HIV care clinics should have past test results routinely available to disease investigators.
Another challenge will be to obtain more information about why so many persons with syphilis are not being diagnosed in the primary stage, and to develop strategies to increase detection of those cases. In the current epidemic among MSM, implementing intensive screening programs is an important tool for identifying more MSM with early latent infection, many of whom may have occult primary infections in need of prompt treatment. For all persons at risk of acquiring syphilis, effective patient and clinician health education about the signs and symptoms of clinical primary syphilis and the subtle signs and symptoms of occult primary syphilis are needed to facilitate prompt diagnosis and treatment.
In this commentary, we have described primary syphilis as “acute” and “highly infectious” as a way to inform program directors and clinicians caring for MSM about the importance of identifying clinical and occult primary syphilis and promptly intervening to prevent transmission. A similar approach was promoted among HIV prevention programs and HIV care providers when it became apparent that acute HIV infection, whether symptomatic or not, was highly infectious, playing a major role in transmission, and often missed by routine antibody testing. Both the individual and community benefit from the detection and immediate treatment of acute HIV infection.67s–69s That realization led to more testing for acute HIV infection, the development of new diagnostics assays and testing algorithms to identify acute HIV infection and the education of clinicians seeing high-risk patients. We encourage STD programs and community advocates to follow that example and redirect efforts and resources to detect and control acute highly infectious primary syphilis.
In response to the increasing epidemic of syphilis, the CDC held a Syphilis Summit meeting in January 2016.70 In April 2017, it issued a Call to Action plan to control syphilis71 and subsequently, several review and commentary articles were published addressing many of the issues that may be encountered in modifying current syphilis control program operations.3,5,72s–76s Given limited resources, the Syphilis Summit and the Call to Action plan recommended concerted efforts to prevent the complications of syphilis: congenital syphilis and neurosyphilis, without a major focus on reducing syphilis transmission. However, lowering communitywide syphilis incidence would in turn impact both of those serious preventable outcomes.3 Considerable discussion among all stakeholders will be needed to seek consensus on STD program priorities because major changes in program objectives and operations will present multiple challenges and most likely require more resources and reprioritization of existing services.
Supplementary Material
Appendix
For further supplemental references, see http://links.lww.com/OLQ/A395.
Footnotes
Acknowledgments: The authors acknowledge the support and substantive review comments from Thomas A. Farley, MD, MPH, Commissioner, Philadelphia Department of Public Health; San Diego County syphilis reported case data collection and analysis from Marjorie Richardson, MPH and Lawrence Wang, MPH, County of San Diego, Health and Human Services; and manuscript preparation support from Kathleen A. Gunn, MPH.
Conflict of Interest and source of funds: None declared.
Disclaimer: The findings and conclusions in this report are those of the authors and do not represent official positions of UCSD or UCLA.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (http://www.stdjournal.com).
REFERENCES
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2017. Atlanta: U.S. Department of Health and Human Services, 2018. Accessed Jan 5, 2019 https://www.cdc.gov/std/stats17/2017-STD-Surveillance-Report_CDC-clearance-9.10.18.pdf. [Google Scholar]
- 2.Fenton KA, Wasserheit JN. The courage to learn from our failures: syphilis control in men who have sex with men. Sex Transm Dis 2007; 34:162–165. [DOI] [PubMed] [Google Scholar]
- 3.Peterman TA, Cha S. Context-appropriate interventions to prevent syphilis: a narrative review. Sex Transm Dis 2018; 45(Suppl1):S65–S71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schillinger JA, Slutsker JS, Pathela P, et al. The epidemiology of syphilis in New York City: historic trends and the current outbreak among men who have sex with men, 2016. Sex Transm Dis 2018; 45(Suppl1):S48–S54. [DOI] [PubMed] [Google Scholar]
- 5.Golden MR, Dombrowski JC. Syphilis control in the postelimination era: implications of a new syphilis control initiative for sexually transmitted disease/human immunodeficiency virus programs. Sex Transm Dis 2018; 45(Suppl1):S86–S92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Douglas JM, Peterman TA, Fenton KA. Syphilis among men who have sex with men: challenges to syphilis elimination in the United States. Sex Transm Dis 2005; 32(Suppl):S80–S83. [DOI] [PubMed] [Google Scholar]
- 7.Cates W, Jr., Rothenberg RB, Blount JH. Syphilis control. the historic context and epidemiologic basis for interrupting sexual transmission of Treponema pallidum. Sex Transm Dis 1996; 23:68–75. [DOI] [PubMed] [Google Scholar]
- 8.Brunham RC, Plummer FA. A general model of sexually transmitted disease epidemiology and its implications for control. Med Clin North Am 1990; 74:1339–1352. [DOI] [PubMed] [Google Scholar]
- 9.Hook EW., III Biomedical issues in syphilis control. Sex Transm Dis 1996; 23:5–8. [DOI] [PubMed] [Google Scholar]
- 10.Thomas JC, Tucker MJ. The development and use of the concept of a sexually transmitted disease core. J Infect Dis 1996; 174(Suppl2):S134–S143. [DOI] [PubMed] [Google Scholar]
- 11.Oxman GL, Smolkowski K, Noell J. Mathematical modeling of epidemic syphilis transmission. implications for syphilis control programs. Sex Transm Dis 1996; 23:30–39. [DOI] [PubMed] [Google Scholar]
- 12.Tramont EC. Treponema pallidum (syphilis). In: Mandell GL, Douglas RG, Bennet SE, eds. Principles and Practice of Infectious Diseases. New York: Churchill Livingstone, 1990:1794–1808. [Google Scholar]
- 13.Rompalo AM, Joesoef MR, O'Donnell JA, et al. Clinical manifestations of early syphilis by HIV status and gender: results of the syphilis and HIV study. Sex Transm Dis 2001; 28:158–165. [DOI] [PubMed] [Google Scholar]
- 14.Lossick JG, Kraus SJ. Syphilis. In: Evans AS, Brachman PS, eds. Bacterial Infections in Humans: Epidemiology and Control. 2nd ed New York: Plenum Medical Book Company, 1991:675–695. [Google Scholar]
- 15.Garnett GP, Aral SO, Hoyle DV, et al. The natural history of syphilis. implications for the transmission dynamics and control of infection. Sex Transm Dis 1997; 24:185–200. [DOI] [PubMed] [Google Scholar]
- 16.Kahn RH, Peterman TA, Arno J, et al. Identifying likely syphilis transmitters: implications for control and evaluation. Sex Transm Dis 2006; 33:630–635. [DOI] [PubMed] [Google Scholar]
- 17.Sparling PF, Swartz MN, Musher DM, et al. Clinical manifestations of syphilis. In: Holmes KK, Sparling PF, Stamm WE, et al., eds. Sexually Transmitted Diseases. 4th ed New York, NY: McGraw Hill, 2008:663–688. [Google Scholar]
- 18.Cha S, Matthias JM, Rahman M, et al. Reactor grids for prioritizing syphilis investigations: are primary syphilis cases being missed? Sex Transm Dis 2018; 45:648–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Samoff E, Koumans EH, Gibson JJ, et al. Pre-treatment syphilis titers: distribution and evaluation of their use to distinguish early from late latent syphilis and to prioritize contact investigations. Sex Transm Dis 2009; 36:789–793. [DOI] [PubMed] [Google Scholar]
- 20.Wong T, Singh AE, De P. Primary syphilis: serological treatment response to doxycycline/tetracycline versus benzathine penicillin. Am J Med 2008; 121:903–908. [DOI] [PubMed] [Google Scholar]
- 21.Gunn RA, Lee M, Oh C, et al. Syphilis serologic prevalence monitoring among STD clinic clients: correlation with reported syphilis incidence, San Diego, CA, 1985–2004. Sex Transm Dis 2007; 34:749–753. [DOI] [PubMed] [Google Scholar]
- 22.Kenyon C, Tsoumanis A, Osbak K, et al. Repeat syphilis has a different immune response compared with initial syphilis: an analysis of biomarker kinetics in two cohorts. Sex Transm Infect 2018; 94:180–186. [DOI] [PubMed] [Google Scholar]
- 23.Magnuson HJ, Thomas EW, Olansky S, et al. Inoculation syphilis in human volunteers. Medicine 1956; 35:33–82. [DOI] [PubMed] [Google Scholar]
- 24.Cohen SE, Chew Ng RA, Katz KA, et al. Repeat syphilis among men who have sex with men in California, 2002–2006: implications for syphilis elimination efforts. Am J Public Health 2012; 102:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brewer TH, Peterman TA, Newman DR, et al. Reinfections during the Florida syphilis epidemic 2000–2008. Sex Transm Dis 2011; 38:12–17. [DOI] [PubMed] [Google Scholar]
- 26.Phipps W, Kent CK, Kohn R, et al. Risk factors for repeat syphilis in men who have sex with men, San Francisco. Sex Transm Dis 2009; 36:331–335. [DOI] [PubMed] [Google Scholar]
- 27.Peterman TA, Kahn RH, Ciesielski CA, et al. Misclassification of the stages of syphilis: implications for surveillance. Sex Transm Dis 2005; 32:144–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gunn RA. Expedited intervention services for possible occult primary syphilis among MSM with asymptomatic incident syphilis. Sex Transm Dis 2009; 36:594–595. [DOI] [PubMed] [Google Scholar]
- 29.Gunn RA, Lee MA, Peterman TA. Syphilis among men who have sex with men: are occult primary stage lesions limiting the effectiveness of traditional case and partner services? National STD Prevention Conference. Jacksonville, FL: May 8–11 2006. Abstract 371. [Google Scholar]
- 30.Sánchez JP, Kaltwassar S, McClellan M, et al. Educational video tool to increase syphilis knowledge among black and Hispanic male patients. J Health Care Poor Underserved 2010; 21:371–385. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


