From 2000 to 2016, the incidence of bronchiolitis hospitalization and mortality in US children decreased, whereas mechanical ventilation use and hospital cost substantially increased.
Abstract
OBJECTIVES:
To investigate the temporal trend in the national incidence of bronchiolitis hospitalizations, their characteristics, inpatient resource use, and hospital cost from 2000 through 2016.
METHODS:
We performed a serial, cross-sectional analysis of nationally representative samples (the 2000, 2003, 2006, 2009, 2012, and 2016 Kids’ Inpatient Databases) of children (age <2 years) hospitalized for bronchiolitis. We identified all children hospitalized with bronchiolitis by using International Classification of Diseases, Ninth Revision, Clinical Modification 466.1 and International Classification of Diseases, 10th Revision, Clinical Modification J21. Complex chronic conditions were defined by the pediatric complex chronic conditions classification by using inpatient data. The primary outcomes were the incidence of bronchiolitis hospitalizations, mechanical ventilation use, and hospital direct cost. We examined the trends accounting for sampling weights.
RESULTS:
From 2000 to 2016, the incidence of bronchiolitis hospitalization decreased from 17.9 to 13.5 per 1000 person-years in US children (25% decrease; Ptrend < .001). In contrast, the proportion of bronchiolitis hospitalizations among overall hospitalizations increased from 16% to 18% (Ptrend < .001). There was an increase in the proportion of children with a complex chronic condition (6%–13%; 117% increase), hospitalization to children’s hospital (15%–29%; 93% increase), and mechanical ventilation use (2%–5%; 184% increase; all Ptrend < .001). Likewise, the hospital cost increased from $449 million to $734 million (63% increase) nationally (with an increase in geometric mean of cost per hospitalization [from $3267 to $4086; 25% increase; Ptrend < .001] adjusted for inflation) from 2003 to 2016.
CONCLUSIONS:
From 2000 through 2016, the incidence of bronchiolitis hospitalizations among US children declined. In contrast, mechanical ventilation use and nationwide hospital direct cost substantially increased.
What’s Known on This Subject:
During the previous decade, the incidence of bronchiolitis hospitalization significantly decreased in the United States.
What This Study Adds:
During the current decade, bronchiolitis hospitalization incidence and mortality among US children continued to decline. By contrast, there were significant increases in the proportion of patients with pediatric complex chronic conditions, hospitalization to children’s hospitals, mechanical ventilation use, and cost.
Bronchiolitis is the most common lower respiratory tract infection among young children in the United States.1 Almost all children are exposed to respiratory syncytial virus (RSV) and other causative pathogens (eg, rhinovirus) during the first 2 years of life.2 Of these, ∼40% of children develop clinical bronchiolitis and up to 3% are hospitalized.3 In 2009 alone, there were ∼130 000 bronchiolitis hospitalizations (18% of infant hospitalizations), with a direct cost of $550 million, in the United States.4
In the 2000s, the overall incidence of bronchiolitis hospitalization among US children decreased, whereas the use of mechanical ventilation and charge per hospitalization increased.4 Additionally, studies continued to report wide between-hospital variation in the inpatient bronchiolitis management.5–7 In this context, over the past 2 decades, there have been nationwide efforts to improve and standardize bronchiolitis diagnosis and management (such as the 2006 and 2014 American Academy of Pediatrics clinical practice guidelines for bronchiolitis).1,8 Despite the clinical and public health importance, the temporal trends in bronchiolitis hospitalizations among US children during the current decade remains uncertain.
To address this knowledge gap, we used a nationally representative sample of US children hospitalized with bronchiolitis to investigate the temporal trends in hospitalization incidence, their characteristics, mechanical ventilation use, and related cost from 2000 to 2016.
Methods
Study Design and Setting
We performed a serial, cross-sectional analysis of a nationally representative sample of children hospitalized for bronchiolitis in 2000, 2003, 2006, 2009, 2012, and 2016 using the Healthcare Cost and Utilization Project’s (HCUP) Kids’ Inpatient Database (KID), compiled by the Agency for Healthcare Research and Quality. The KID is designed to make national estimates for hospital use and outcomes; it is the only all-payer inpatient care database for US children. The KID is a stratified sample of all pediatric hospitalizations from states that participate in the HCUP. The states provide discharge-level data on all hospitalizations from all nonfederal, short-term general and specialty hospitals in the state. The KID contains an 80% stratified sample of pediatric hospitalizations. In 2016, the KID contained the information for ∼7 million weighted hospital discharges from 4200 hospitals across 46 states plus the District of Columbia. The details of the KID have been described elsewhere.9 The KID has been used to investigate the temporal trends in various conditions and validated against the National Hospital Discharge Survey.10–13 The Institutional Review Board of Massachusetts General Hospital approved this analysis.
Study Sample
We identified all children (age <2 years) hospitalized for bronchiolitis8 using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code of 466.1 in the 2000–2012 data or International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes of J21 in the 2016 data in the primary or secondary diagnosis fields on the basis of the approach used in previous studies.4,14–16 To minimize the potential misclassification with respiratory distress syndrome or transient tachypnea of the newborn, we excluded the hospitalizations for routine births identified using the Clinical Classifications Software (CCS) code 218 in any fields.17,18
Measurements
The KID contains the information on patient demographics (eg, age, sex, race and/or ethnicity), primary insurance (payer), hospitalization day (weekday or weekend), hospitalization diagnoses and procedures, hospital length of stay, disposition, and inpatient charge, as well as cost for hospitalization. Primary payer was grouped into public sources, private payers, and other types. Diagnoses and procedures were available by using the ICD-9-CM or ICD-10-CM, and CCS. CCS is a methodology developed by the Agency for Healthcare Research and Quality to group ICD-9-CM or ICD-10-CM codes into clinically sensible and mutually exclusive categories. Pediatric complex chronic conditions, consisting of 10 categories (cardiovascular, respiratory, neuromuscular, renal, gastrointestinal, hematologic or immunologic, metabolic, other congenital or genetic, malignancy, and neonatal), were defined by the pediatric complex chronic conditions classification system version 219 on the basis of the inpatient diagnosis and procedure codes. Additionally, the KID also contains hospital characteristics, such as the US region (northeast, south, midwest, and west),20 urban-rural status, teaching status,20 and designation as a children’s hospital.20
Outcome Measures
The primary outcomes were the incidence of bronchiolitis hospitalization, use of invasive or noninvasive mechanical ventilation, and hospital direct cost. The secondary outcomes were length of stay and hospital mortality. The use of invasive and noninvasive mechanical ventilation was identified by ICD-9-CM and ICD-10-CM procedure codes (Supplemental Table 3), according to previous studies.4,21 We computed the direct costs using the cost-to-charge ratios for the 2003–2016 hospitalizations (the cost-to-charge ratio was not available in 2000). The cost information was obtained from the hospital accounting reports collected by the Centers for Medicare and Medicaid Services.22 Data were reweighted to analyze the cost according to the HCUP recommendations.23
Statistical Analysis
We investigated the temporal trends in the weighted estimates of outcomes in 2000, 2003, 2006, 2009, 2012, and 2016. To compute the incidence of bronchiolitis hospitalization, the annual number of estimated bronchiolitis hospitalizations was divided by the population estimate (eg, the number of general population aged <2 years) from the US Census Bureau.24 To address a possibility that changes in diagnostic preference25 and the transition from ICD-9-CM to ICD-10-CM explain the temporal trends in hospitalization incidence across the study years (ie, diagnostic substitution), we also examined the temporal trends for the hospitalization incidence for pneumonia (CCS code 122), other upper respiratory infections (CCS code 126), asthma (CCS code 128), other lower respiratory diseases (CCS code 133), and other upper respiratory diseases (CCS code 134) using the primary and secondary diagnosis fields. We used the Cochran-Armitage test, a statistical method that tests for a trend in binomial proportions (eg, bronchiolitis hospitalization: yes or no) across levels of an ordinal variable (eg, calendar years), to examine temporal trends for binary outcomes. Because the study objective was to examine the temporal trends (rather than the causal relationship between calendar years and outcomes), we did not adjust for covariates. We also performed the nonparametric test, an extension of the Wilcoxon rank test,26 to examine temporal trends for continuous outcomes. To facilitate direct comparisons of direct cost across the years, we converted all costs to 2016 US dollars using the Consumer Price Index.27
We also conducted a series of sensitivity analyses to examine the temporal trends in different subpopulations. First, we repeated the primary analysis limited to infants (age <1 year). Second, we also repeated the analysis in the subgroups of children with bronchiolitis as the primary diagnosis. Third, we limited the analysis to children without complex chronic conditions. Fourth, we repeated the analysis in infants hospitalized with the primary diagnosis of bronchiolitis and without any complex chronic conditions. Finally, we limited the analysis to children with a complex chronic condition. We conducted the analyses using Stata 15.0 (Stata Corp, College Station, TX) and R version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria), with accounting for the complex sampling design to obtain proper variance estimations.
Results
Bronchiolitis Hospitalization Incidence
There were 490 650 hospitalizations for bronchiolitis in the United States, corresponding to a weighted estimate of 775 858 hospitalizations in the 6 data sets (2000, 2003, 2006, 2009, 2012, and 2016). Overall, this accounted for 17% of all hospitalizations for children (age <2 years) and 18% for infants (age <1 year) after excluding all routine births.
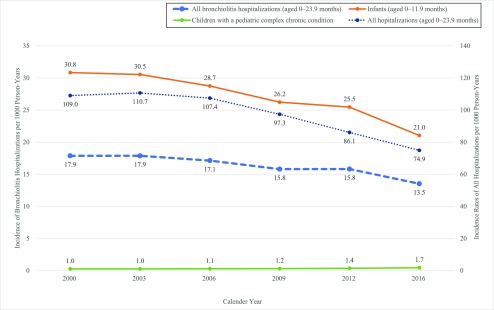
From 2000 through 2016, there was a decrease in the incidence of bronchiolitis hospitalization from 17.9 (95% confidence [CI] 16.5–19.3) to 13.5 (95% CI 12.2–14.9) per 1000 person-years (25% decrease; Ptrend < .001; Fig 1; Supplemental Fig 4). This downward trend was observed across all subpopulations (Ptrend < .001) except for children with a complex chronic condition (70% increase; Ptrend < .001). In parallel, the incidence of total hospitalizations declined (31% decrease; Ptrend < .001) during the same period. Consequently, the annual proportion of bronchiolitis hospitalizations among the total hospitalizations for children increased (16% [95% CI 16%–17%] to 18% [95% CI 17%–19%]; 10% increase; Ptrend < .001; Table 1).
FIGURE 1.
Incidence of bronchiolitis hospitalizations and all hospitalizations per 1000 children in the United States, 2000–2016. Overall, there was a significant decrease in the incidence of bronchiolitis hospitalization (25% decrease; Ptrend < .001) and all hospitalizations (31% decrease; Ptrend < .001) from 2000 through 2016. Likewise, there was a significant decrease in the incidence in infants (32% decrease; Ptrend < .001). By contrast, there was a significant increase in children with complex chronic conditions (70% increase; Ptrend < .001).
TABLE 1.
Patient and Hospital Characteristics of Bronchiolitis Hospitalizations in the US Children, 2000–2016
| 2000 | 2003 | 2006 | 2009 | 2012 | 2016 | Ptrenda | |
|---|---|---|---|---|---|---|---|
| Age 0–23.9 mo | |||||||
| Weighted No. bronchiolitis | 136 757 | 141 436 | 137 236 | 127 634 | 125 142 | 107 653 | — |
| Weighted No. total hospitalizations | 834 618 | 876 894 | 862 018 | 787 833 | 681 520 | 596 664 | — |
| Total hospitalizations,b % | 16 (16–17) | 16 (16–17) | 16 (16–17) | 16 (16–17) | 18 (18–19) | 18 (17–19) | <.001 |
| Age 0–11.9 mo | |||||||
| Weighted No. bronchiolitis | 118 910 | 121 411 | 116 200 | 104 985 | 100 275 | 83 533 | — |
| Weighted No. total hospitalizations | 639 150 | 669 810 | 655 736 | 591 022 | 515 288 | 460 827 | — |
| Total hospitalizations,c % | 19 (18–19) | 18 (18–19) | 18 (17–18) | 18 (17–18) | 19 (19–20) | 18 (17–19) | .003 |
| RSV bronchiolitis,d % | 9 (8–10) | 9 (8–9) | 9 (9–10) | 9 (9–10) | 11 (10–11) | 10 (10–11) | <.001 |
| Patient demographics | |||||||
| Age | <.001 | ||||||
| 0–11.9 mo | 87 (86–88) | 86 (85–86) | 85 (84–86) | 82 (81–83) | 80 (79–81) | 78 (76–79) | |
| 12–23.9 mo | 13 (12–14) | 14 (14–15) | 15 (15–16) | 18 (17–19) | 20 (19–21) | 22 (21–24) | |
| Male sex | 59 (59–60) | 59 (59–59) | 58 (58–59) | 59 (58–59) | 58 (58–58) | 58 (58–59) | <.001 |
| Race and/or ethnicity | |||||||
| Non-Hispanic white | 42 (39–46) | 34 (32–37) | 35 (32–37) | 39 (36–41) | 43 (41–45) | 42 (39–45) | <.001 |
| Non-Hispanic African American | 13 (12–15) | 12 (11–13) | 11 (10–12) | 14 (12–16) | 16 (14–17) | 16 (14–18) | <.001 |
| Hispanic | 21 (19–24) | 20 (18–23) | 22 (19–25) | 25 (22–27) | 24 (22–27) | 22 (20–25) | <.001 |
| Other or unknown | 23 (21–26) | 34 (31–37) | 32 (29–36) | 23 (20–26) | 17 (15–20) | 20 (16–23) | <.001 |
| Primary payer | |||||||
| Public | 53 (51–54) | 57 (56–59) | 60 (58–61) | 63 (62–65) | 65 (63–66) | 63 (61–65) | <.001 |
| Private | 41 (39–43) | 37 (35–38) | 34 (32–36) | 31 (30–33) | 30 (29–31) | 32 (30–34) | <.001 |
| Other | 6 (6–7) | 6 (5–6) | 6 (6–7) | 6 (5–7) | 5 (5–6) | 5 (4–5) | <.001 |
| Hospitalization day | <.001 | ||||||
| Weekdaye | 78 (77–78) | 77 (77–76) | 77 (77–78) | 77 (76–77) | 76 (75–76) | 75 (74–75) | |
| Weekend | 22 (22–23) | 23 (22–23) | 23 (22–23) | 23 (23–24) | 24 (24–25) | 25 (25–26) | |
| Any pediatric complex chronic conditionsf | 6 (5–6) | 6 (5–6) | 6 (6–7) | 8 (7–8) | 9 (8–9) | 13 (12–13) | <.001 |
| Cardiovascular conditions | 2 (2–2) | 2 (2–2) | 2 (2–2) | 2 (2–3) | 3 (3–3) | 4 (4–4) | <.001 |
| Respiratory conditions | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–2) | 2 (2–2) | <.001 |
| Neurologic and neuromuscular conditions | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) | <.001 |
| Prematurityg | 0.3(0.2–0.5) | 0.3 (0.3–0.4) | 0.4 (0.3–0.9) | 1 (0.8–1) | 1 (1–1) | 2 (2–2) | <.001 |
| Hospital characteristics | |||||||
| Region | |||||||
| Northeast | 18 (15–22) | 16 (14–18) | 17 (15–20) | 18 (15–22) | 18 (14–22) | 19 (15–24) | <.001 |
| Midwest | 18 (14–21) | 22 (19–25) | 23 (19–25) | 20 (17–24) | 22 (18–26) | 22 (18–28) | <.001 |
| South | 40 (36–44) | 42 (38–46) | 40 (36–43) | 40 (36–44) | 39 (35–43) | 35 (30–41) | <.001 |
| West | 24 (20–28) | 20 (17–24) | 20 (17–24) | 22 (18–26) | 22 (18–26) | 23 (19–28) | .97 |
| Location and teaching status | |||||||
| Rural | 20 (18–23) | 20 (18–22) | 16 (15–18) | 16 (15–18) | 12 (11–14) | 7 (6–8) | <.001 |
| Urban nonteaching | 31 (28–34) | 33 (30–36) | 31 (28–34) | 33 (29–36) | 25 (22–28) | 13 (11–15) | <.001 |
| Urban teaching | 48 (44–52) | 47 (44–50) | 52 (49–56) | 51 (47–55) | 63 (29–66) | 80 (77–82) | <.001 |
| Hospital designation | <.001 | ||||||
| Non–children’s hospital | 85 (80–89) | 85 (82–87) | 83 (79–87) | 81 (76–84) | 78 (73–82) | 71 (65–77) | |
| Children’s hospital | 15 (11–20) | 15 (13–18) | 17 (14–21) | 19 (16–22) | 22 (18–27) | 29 (23–35) |
Data are expressed as % (95% confidence interval) unless otherwise indicated. —, not applicable.
P value for trend test.
Proportion of bronchiolitis hospitalizations among the total hospitalizations for children aged <2 y after excluding routine birth.
Proportion of bronchiolitis hospitalizations among the total hospitalizations for children aged <12 mo after excluding routine birth.
Identified by ICD-9-CM code of 466.11 and ICD-10-CM code of J21.0.
Hospitalization on Monday, Tuesday, Wednesday, Thursday, or Friday.
Ten pediatric complex chronic conditions were defined by the pediatric complex chronic conditions classification system version 2. Of these 10 categories, 3 major conditions are presented.
Defined by <37 wk of gestation or low birth weight (<2500 g), identified by ICD-9-CM code of 765.0, 765.0X, 765.1, 765.1X, or 765.21-28 and ICD-10-CM code of P07.0, P07.0X, P07.1, P07.1X, P07.2, P07.2X, P07.3, or P07.3X.
To determine if diagnostic substitutions contributed to the trends, we also examined the trends in pneumonia, other upper respiratory infections, asthma, other lower respiratory diseases, and other upper respiratory diseases. From 2000 to 2016, the observed decline in bronchiolitis hospitalization incidence was mirrored by the concurrent decrease in hospitalization incidence for these diagnoses (all Ptrend < .001; Supplemental Fig 5).
Patient and Hospital Characteristics
The patient and hospital characteristics of bronchiolitis hospitalization in the US children in the six 1-year periods are summarized in Table 1. Children hospitalized for bronchiolitis in more recent years were more likely to have a complex chronic condition (from 6% in 2000 to 13% in 2016; 117% increase; Ptrend < .001). Additionally, there was a significant increase in the proportion of children hospitalized to an urban teaching hospital (48%–80%; 67% increase; Ptrend < .001) and children’s hospital (15%–29%; 93% increase; Ptrend < .001).
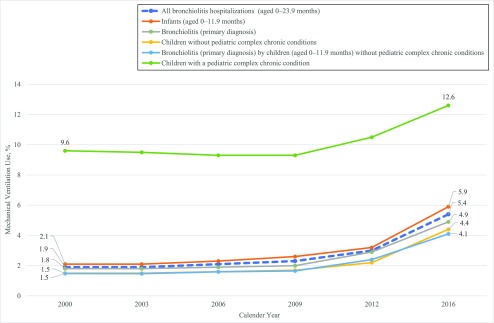
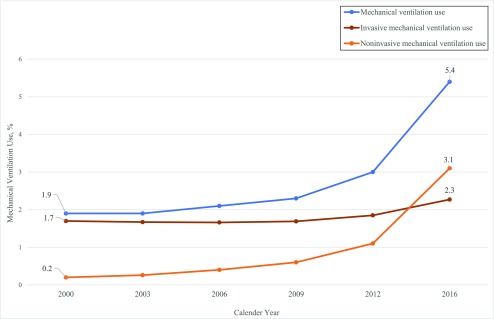
Mechanical Ventilation Use, Hospital Length of Stay, and Mortality
From 2000 to 2016, the proportion of children who underwent mechanical ventilation increased from 2% in 2000 to 5% in 2016 (184% increase; Ptrend < .001; Fig 2). Although the upward trend was observed across the subpopulations (all Ptrend < .001), children with a complex chronic condition had the highest mechanical ventilation use (12.7%) in 2016. Although the use of invasive mechanical ventilation modestly increased (35% increase), that of noninvasive mechanical ventilation substantially increased (1450% increase; both Ptrend < .001; Fig 3).
FIGURE 2.
In-hospital mechanical ventilation use for US children with bronchiolitis according to different subpopulations, 2000–2016. Overall, the proportion of mechanical ventilation use in bronchiolitis hospitalizations increased from 2000 to 2016 (184% increase; Ptrend < .001). Similarly, there was a significant increase in mechanical ventilation use across all different subpopulations (all Ptrend < .001).
FIGURE 3.
In-hospital invasive and noninvasive mechanical ventilation use for US children with bronchiolitis, 2000–2016. From 2000 to 2016, whereas the use of invasive mechanical ventilation modestly increased (34% increase; Ptrend < .001), that of noninvasive mechanical ventilation substantially increased (1450% increase; Ptrend < .001).
During the same period, there was no clinically meaningful change in the hospital length of stay during the study period (Supplemental Table 4) except for the decrease among the patients with mechanical ventilation use (median: 10 days in 2000 to 7 days in 2016; Ptrend < .001).
Over the study period, the hospital mortality for bronchiolitis modestly declined (0.06% [95% CI 0.04%–0.09%] to 0.05% [95% CI 0.03%–0.06%]; Ptrend = 0.02; Supplemental Table 5). Although there was an apparent increase in the mortality between 2012 and 2016, the number of in-hospital deaths was relatively small in both years (31 and 50, respectively). Although the downward temporal trend was observed across all subpopulations, it was more evident in the patients with mechanical ventilation use (2.3% [95% CI 1.4%–3.6%) to 0.5% [95% CI 0.3%–0.8%]; 78% decrease; Ptrend < .001).
Hospital Cost
From 2003 to 2016, the geometric mean of direct cost per hospitalization increased from $3267 (95% CI $3188–$3345) to $4086 (95% CI $3912–$4260; 25% increase; Ptrend < .001; Table 2). Furthermore, despite the decreased hospitalization incidence, the total cost for bronchiolitis hospitalization increased from $449 million (95% CI $421–$478 million) to $734 million (95% CI $660–$809 million) nationally, adjusted for inflation (63% increase). This increase was driven largely by the increasing cost in patients with complex chronic conditions ($36 million [95% CI $33–$40 million] to $217 million [95% CI $187–$248 million]; 502% increase) and those who underwent invasive mechanical ventilation ($77 million [95% CI $59–$95 million]–$144 million [95% CI $120–$168 million]; 87% increase) in addition to the parallel increase in the cost in patients without complex chronic conditions (25% increase) and those without mechanical ventilation use (23% increase). Additionally, the total direct cost for patients hospitalized for a children’s hospital also substantially increased ($100 million [95% CI $79–$121 million] to $329 million [95% CI $264–$394 million]; 229% increase).
TABLE 2.
Total Cost and Cost per Hospitalization for Bronchiolitis Hospitalization, According to Different Subpopulations, 2003–2016
| Cost | ||||||
|---|---|---|---|---|---|---|
| 2003 | 2006 | 2009 | 2012 | 2016 | Ptrenda | |
| All bronchiolitis hospitalizations, children aged 0–23.9 mo | ||||||
| Total direct cost (95% CI)b | 449 (421–478) | 735 (677–793) | 641 (588–694) | 701 (637–765) | 734 (660–809) | .42 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 3267 (3188–3345) | 3624 (3509–3740) | 3479 (3369–3589) | 3523 (3378–3669) | 4086 (3912–4260) | <.001 |
| Sensitivity analyses | ||||||
| Infants aged 0–11.9 mo | ||||||
| Total direct cost (95% CI)b | 381 (356–405) | 639 (587–691) | 547 (499–594) | 583 (528–639) | 599 (540–659) | .42 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 3294 (3213–3376) | 3696 (3574–3817) | 3552 (3434–3670) | 3594 (3440–3749) | 4212 (4032–4392) | <.001 |
| Bronchiolitis, primary diagnosis | ||||||
| Total direct cost (95% CI)b | 413 (386–439) | 636 (585–687) | 522 (476–568) | 598 (543–652) | 596 (534–658) | .58 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 3235 (3156–3313) | 3563 (3449–3676) | 34,06 (3293–3518) | 3470 (3324–3618) | 3967 (3792–4141) | <.001 |
| Children without pediatric complex chronic conditions | ||||||
| Total direct cost (95% CI)b | 413 (388–439) | 613 (570–657) | 515 (477–554) | 542 (497–587) | 517 (469–565) | .58 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 3192 (3116–3278) | 3465 (3360–3569) | 3300 (3201–3398) | 3305 (3176–3435) | 3749 (3598–3899) | <.001 |
| Bronchiolitis, primary diagnosis, by children aged 0–11.9 mo without pediatric complex chronic conditions | ||||||
| Total direct cost (95% CI)b | 326 (305–347) | 467 (433–502) | 361 (331–391) | 388 (355–422) | 339 (308–371) | .90 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 3195 (3116–3274) | 3471 (3362–3579) | 3296 (3189–3402) | 3320 (3183–3458) | 3724 (3572–3876) | <.001 |
| Children with a pediatric complex chronic condition | ||||||
| Total direct cost (95% CI)b | 36 (33–40) | 121 (104–139) | 126 (108–144) | 159 (149–180) | 217 (187–248) | .046 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 5069 (4855–5284) | 7055 (6634–7476) | 6788 (6425–7151) | 6871 (6473–7270) | 7465 (7050–7880) | <.001 |
| Stratification by use of mechanical ventilation | ||||||
| With mechanical ventilation use | ||||||
| Total direct cost (95% CI)b | 94 (75–113) | 114 (95–132) | 117 (100–134) | 141 (122–161) | 195 (163–226) | .046 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 10 093 (9053–11 134) | 25 212 (22 589–27 834) | 25 618 (23 415–27 820) | 21 445 (18 493–24 397) | 18 525 (15 841–21 208) | <.001 |
| Invasive mechanical ventilation use | ||||||
| Total direct cost (95% CI)b | 77 (59–95) | 103 (85–120) | 105 (90–121) | 118 (101–135) | 144 (120–168) | .046 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 10 376 (9301–11 450) | 29 243 (26 311–32 174) | 33 204 (30 390–36 019) | 29 671 (23 068–36 275) | 36 207 (33 191–39 223) | <.001 |
| Noninvasive mechanical ventilation use | ||||||
| Total direct cost (95% CI)b | 17 (14–20) | 11 (8–14) | 12 (9–14) | 23 (18–29) | 51 (36–66) | .15 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 9090 (6587–11 594) | 14 209 (12 737–15 681) | 12 125 (11 082–13 168) | 12 595 (11 541–13 648) | 11 446 (10 101–12 792) | <.001 |
| Without mechanical ventilation use | ||||||
| Total direct cost (95% CI)b | 440 (412–468) | 621 (577–666) | 524 (485–564) | 560 (512–607) | 539 (492–587) | .58 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 3242 (3163–3320) | 3478 (3373–3583) | 3321 (3221–3420) | 3337 (3204–3470) | 3747 (3597–3897) | <.001 |
| Stratification by hospital designation | ||||||
| Non–children’s hospital | ||||||
| Total direct cost (95% CI)b | 349 (329–370) | 519 (482–556) | 434 (404–465) | 434 (399–469) | 405 (367–444) | .97 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 3054 (2983–3125) | 3304 (3208–3399) | 3113 (3034–3193) | 3060 (2952–3168) | 3412 (3279–3544) | <.001 |
| Children’s hospital | ||||||
| Total direct cost (95% CI)b | 100 (79–121) | 216 (170–262) | 207 (162–251) | 267 (213–322) | 329 (264–394) | .07 |
| Cost per hospitalization, geometric mean (95% CI)c,d | 4696 (4421–4970) | 5619 (5111–6127) | 5883 (5406–6360) | 5805 (5146–6464) | 6506 (5924–7088) | <.001 |
P value for trend test. Cost was adjusted for inflation.
Data are presented as US dollars (million). Cost was adjusted for inflation.
Data are presented as US dollars. Cost was adjusted for inflation.
P value for trend test in unweighted samples because of the discontinuity in hospital identification codes between 2009 and 2012. Cost was adjusted for inflation.
Discussion
Using nationally representative US data of hospitalized children during 2000 to 2016, we found significant decreases in the incidence of bronchiolitis hospitalizations, whereas its proportion among the overall hospitalizations increased. We also found that the in-hospital mortality for bronchiolitis declined during the 17-year period. In contrast, there was a substantial increase in the proportion of children with a complex chronic condition, hospitalizations to children’s hospitals, use of mechanical ventilation (particularly in the use of noninvasive mechanical ventilation), and direct inpatient cost. Although these observations suggest a net improvement in clinical outcome of bronchiolitis, the inpatient resource use remains substantial (eg, ∼108 000 hospitalizations with a direct cost of $734 million) in 2016 alone.
Continued Decline in Bronchiolitis Hospitalization Incidence and Mortality
After the United States experienced a 2.4-fold increase in the incidence of bronchiolitis hospitalization through the 1980–1990s,28 authors of a previous study reported a decrease in the incidence between 2000 and 2009.4 The current study extends these earlier reports by demonstrating a sustained reduction in the incidence of bronchiolitis hospitalizations over the current decade, particularly in infants and children without complex chronic conditions. Interestingly, the proportion of bronchiolitis hospitalizations among the overall hospitalizations by children relatively increased from 16% to 18%. This finding is likely attributable to the observations (ie, bronchiolitis hospitalizations decreased at a slower rate than the overall hospitalizations), which suggest not only an overall improvement in pediatric care and health care use but also opportunities for improvement in bronchiolitis care. In parallel, the in-hospital mortality also declined. The reasons for the observed reductions are likely multifactorial. For example, these findings may reflect reductions in disease incidences as well as improvement in prevention measures (eg, decrease in environmental tobacco smoke exposure).29,30 Alternatively, nonbiological factors, such as the continued efforts to optimize bronchiolitis care, including the dissemination of the 2006 and 2014 American Academy of Pediatrics guidelines for bronchiolitis diagnosis and management,1,8 may have contributed to the incremental improvement in clinical metrics and outcomes.31
In contrast, one might surmise that the observed temporal patterns are explained by potential changes in diagnostic coding practice during the study period, particularly at the ICD-9-CM and ICD-10-CM transition period. However, we observed no compensatory increases in hospitalization incidence for other respiratory conditions with clinical manifestations similar to those of bronchiolitis (eg, pneumonia, other upper respiratory infections, asthma, other lower respiratory diseases, and other upper respiratory diseases). Instead, there were concurrent declines in their hospitalization incidences in addition to the decrease in the overall hospitalization incidence in the US children. Therefore, diagnostic substitution is unlikely to fully explain the observed reduction in the incidence of bronchiolitis hospitalizations.
Increased Resource Use and Cost
The apparent reduction in the hospitalization incidence and mortality sharply contrasts with the upward trends in the proportion of children who were hospitalized in an urban teaching hospital and children’s hospital as well as the use of mechanical ventilation. The etiologies for the observed increase remain to be elucidated. For example, the increase in the proportion of children with a complex chronic condition both in the general pediatric population32,33 and in children with bronchiolitis in more recent years might have contributed to the increased health care resource use. Indeed, this population is known to have a higher likelihood of hospitalization to a children’s hospital and increased health care use.33,34 Consistently, the current study also revealed the highest mechanical ventilation use in children with a complex chronic condition during their bronchiolitis hospitalization. However, the absolute proportion of this population remained small (13% of total bronchiolitis hospitalization in 2016). Alternatively, it is also possible that these patterns reflect an improvement in the coordination of care through regional care systems for critically ill (similar to neonatal intensive care systems35) and more liberal use of mechanical ventilation (particularly noninvasive mechanical ventilation), thereby contributing to the decreases in mortality. Furthermore, these mechanisms are not mutually exclusive.
Parallel to the increased hospital resource use, we also observed a 63% increase in the nationwide direct cost from 2003 to 2016, despite the overall decline in the bronchiolitis hospitalization incidence with a relatively stable hospital length of stay. Whereas the cost per hospitalization significantly increased in all subpopulations during the 17-year period, the increased nationwide cost for bronchiolitis hospitalizations was largely attributable to the increased cost in children with complex chronic conditions as well as critically ill children who underwent mechanical ventilation. The population with complex chronic conditions is known to have more intensive resource use (including noninvasive and invasive respiratory support) during hepatizations, thereby leading to a higher hospital cost.4,33 Additionally, we also observed the increase in cost in children without complex chronic conditions or mechanical ventilation use, suggesting that the observed increase in the nationwide cost for bronchiolitis is also attributable to the well-documented role of physician and hospital service fees in the increasing cost.36 Furthermore, the literature has continued to report inconsistencies between clinicians as to the best bronchiolitis management, which is demonstrated by the wide variability in diagnosis and care in this population.5–7 This mechanism might also have attributed, at least partially, to the observed increases in health care use and hospital cost.
The observed reduction in hospitalization incidence and mortality supports a cautious optimism that the bronchiolitis morbidities can be further reduced. Yet, the health care use and cost in children hospitalized for bronchiolitis in the United States remains substantial in 2016. The identification of these temporal trends should not only motivate future studies into the determinants of the rising use and cost but also encourage renewed efforts to develop better systems of care that achieve high-quality, cost-effective care in this large population of sick children.
Potential Limitations
This study has several potential limitations. First, because of the use of administrative data, there are potential errors in recording diagnoses resulting in under- or overestimation of the incidence of bronchiolitis hospitalizations. Similarly, the transition from the ICD-9-CM to ICD-10-CM may have caused a discontinuity in the trends over the study period. However, our sensitivity analysis revealed similar downward trends in the hospitalization incidence for potentially misclassified diagnoses and conditions. Therefore, it is unlikely that misclassifications and diagnostic substitutions have fully explained the observed temporal trends. Second, the data availability of the KID precluded us from evaluating potential annual variations in RSV and other respiratory viruses. Yet, the observed trends revealed consistent trends (eg, the consistent decrease in the incidence of bronchiolitis hospitalizations) rather than year-by-year fluctuations. Additionally, the prevalence of RSV bronchiolitis was likely to be underestimated in the current study. This research question is better examined by active surveillance or high-quality prospective studies of children with severe bronchiolitis. Third, the KID contains hospital discharge-level records (ie, not patient-level records). Thus, we were unable to assess repeat health care use outcomes (eg, rehospitalizations). Although a small proportion of children might have been readmitted in the same calendar year, the number of mortality outcomes does not change. Fourth, the KID does not contain some helpful clinical and environmental information (eg, palivizumab use and household smoking exposure). Our study had an objective to investigate the nationwide trends in health care use and outcomes and should facilitate further investigations into the possible mechanisms that explain our findings. Similarly, the KID samples consisted of hospitalizations, and they were thus unable to evaluate temporal changes in insurance composition of the nation. Lastly, although the study data consisted of a nationally representative sample, we must generalize our inferences cautiously beyond children hospitalized with bronchiolitis (eg, those with bronchiolitis in ambulatory settings). Nonetheless, our data remain directly relevant to >100 000 children hospitalized (and their families) yearly in the United States. These children are precisely the population for which effective preventive and therapeutic strategies are most urgently needed.3
Conclusions
On the basis of the analysis of nationally representative US data of children hospitalized for bronchiolitis during 2000 to 2016, we found downward trends in the overall incidence of bronchiolitis hospitalization and hospital mortality. By contrast, we also observed substantial increases in the proportion of children with a complex chronic condition, hospitalizations to a children’s hospital, use of mechanical ventilation, and direct inpatient cost. For clinicians and researchers, our observations underscore the importance of continued efforts to develop effective prevention, treatment, and prognostication strategies for bronchiolitis, particularly in infants at high risk for severe bronchiolitis, which will, in turn, not only lead to additional improvement in the patient outcomes but also curb the rising hospital costs.
Glossary
- CCS
Clinical Classifications Software
- CI
confidence interval
- HCUP
Healthcare Cost and Utilization Project
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- ICD-10-CM
International Classification of Diseases, 10th Revision, Clinical Modification
- KID
Kids’ Inpatient Database
- RSV
respiratory syncytial virus
Footnotes
Drs Fujiogi, Goto, Yasunaga, Fujishiro, Mansbach, Camargo Jr, and Hasegawa participated in the concept and design, analysis and interpretation of data, and drafting or revising of the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: The current study is supported by grants from the National Institutes of Health (Bethesda, MD): R01 AI-127507, R01 AI-134940, R01 AI-137091, and UG3/UH3 OD-023253. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis Diagnosis and management of bronchiolitis. Pediatrics. 2006;118(4):1774–1793 [DOI] [PubMed] [Google Scholar]
- 2.Glezen WP, Taber LH, Frank AL, Kasel JA. Risk of primary infection and reinfection with respiratory syncytial virus. Am J Dis Child. 1986;140(6):543–546 [DOI] [PubMed] [Google Scholar]
- 3.Hasegawa K, Mansbach JM, Camargo CA Jr. Infectious pathogens and bronchiolitis outcomes. Expert Rev Anti Infect Ther. 2014;12(7):817–828 [DOI] [PubMed] [Google Scholar]
- 4.Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA Jr. Trends in bronchiolitis hospitalizations in the United States, 2000-2009. Pediatrics. 2013;132(1):28–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christakis DA, Cowan CA, Garrison MM, et al. . Variation in inpatient diagnostic testing and management of bronchiolitis. Pediatrics. 2005;115(4):878–884 [DOI] [PubMed] [Google Scholar]
- 6.Macias CG, Mansbach JM, Fisher ES, et al. . Variability in inpatient management of children hospitalized with bronchiolitis. Acad Pediatr. 2015;15(1):69–76 [DOI] [PubMed] [Google Scholar]
- 7.Florin TA, Byczkowski T, Ruddy RM, et al. . Variation in the management of infants hospitalized for bronchiolitis persists after the 2006 American Academy of Pediatrics bronchiolitis guidelines. J Pediatr. 2014;165(4):786–792.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ralston SL, Lieberthal AS, Meissner HC, et al. ; American Academy of Pediatrics. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis [published correction appears in Pediatrics. 2015;136(4):782]. Pediatrics. 2014;134(5). Available at: www.pediatrics.org/cgi/content/full/134/5/e1474 [DOI] [PubMed] [Google Scholar]
- 9.Healthcare Cost and Utilization Project. Overview of the Kids’ Inpatient Database. Rockville, MD: Agency for Healthcare Research and Quality; 2018. Available at: www.hcup-us.ahrq.gov/kidoverview.jsp. Accessed May 10, 2019 [Google Scholar]
- 10.Leventhal JM, Gaither JR. Incidence of serious injuries due to physical abuse in the United States: 1997 to 2009. Pediatrics. 2012;130(5). Available at: www.pediatrics.org/cgi/content/full/130/5/e847 [DOI] [PubMed] [Google Scholar]
- 11.Gipson DS, Messer KL, Tran CL, et al. . Inpatient health care utilization in the United States among children, adolescents, and young adults with nephrotic syndrome. Am J Kidney Dis. 2013;61(6):910–917 [DOI] [PubMed] [Google Scholar]
- 12.Heaton PC, Tundia NL, Schmidt N, Wigle PR, Kelton CM. National burden of pediatric hospitalizations for inflammatory bowel disease: results from the 2006 Kids’ Inpatient Database. J Pediatr Gastroenterol Nutr. 2012;54(4):477–485 [DOI] [PubMed] [Google Scholar]
- 13.Maxwell BG, Nies MK, Ajuba-Iwuji CC, Coulson JD, Romer LH. Trends in hospitalization for pediatric pulmonary hypertension. Pediatrics. 2015;136(2):241–250 [DOI] [PubMed] [Google Scholar]
- 14.Hasegawa K, Tsugawa Y, Brown DF, Mansbach JM, Camargo CA Jr. Temporal trends in emergency department visits for bronchiolitis in the United States, 2006 to 2010. Pediatr Infect Dis J. 2014;33(1):11–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hasegawa K, Tsugawa Y, Tsai CL, Brown DF, Camargo CA Jr. Frequent utilization of the emergency department for acute exacerbation of chronic obstructive pulmonary disease. Respir Res. 2014;15:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goto T, Faridi MK, Camargo CA, Hasegawa K. The association of aspirin use with severity of acute exacerbation of chronic obstructive pulmonary disease: a retrospective cohort study. NPJ Prim Care Respir Med. 2018;28(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Healthcare Cost and Utilization Project. Clinical Classifications Software (CCS) for ICD-9-CM. Rockville, MD: Agency for Healthcare Research and Quality; 2017. Available at: www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed May 20, 2019 [Google Scholar]
- 18.Healthcare Cost and Utilization Project. Clinical Classifications Software (CCS) for ICD-10-CM-PCS (Beta Version). Rockville, MD: Agency for Healthcare Research and Quality; 2018. Available at: https://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp. Accessed July 2, 2019 [Google Scholar]
- 19.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14(1):199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Healthcare Cost and Utilization Project. KID Description of Data Elements: KID_STRATUM - Stratum Used To Post-Stratify Hospital. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Available at: www.hcup-us.ahrq.gov/db/vars/kid_stratum/kidnote.jsp. Accessed February 20, 2019 [Google Scholar]
- 21.Goto T, Hirayama A, Faridi MK, Camargo CA Jr, Hasegawa K. Obesity and severity of acute exacerbation of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2018;15(2):184–191 [DOI] [PubMed] [Google Scholar]
- 22.Healthcare Cost and Utilization Project. HCUP KID Description of Data Elements: TOTCHG - Total Chargers, Cleaned. Rockville, MD: Agency for Healthcare Research and Quality; 2008. Available at: www.hcup-us.ahrq.gov/db/vars/totchg/kidnote.jsp. Accessed May 20, 2019 [Google Scholar]
- 23.Healthcare Cost and Utilization Project Cost-to-charge ratio files. Rockville, MD. Agency for Healthcare Research and Quality. 2018. Available at: www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed February 20, 2019
- 24.US Census Bureau Census regions and divisions of the United States. Available at: https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf. Accessed October 21, 2019
- 25.Mansbach JM, Espinola JA, Macias CG, Ruhlen ME, Sullivan AF, Camargo CA Jr. Variability in the diagnostic labeling of nonbacterial lower respiratory tract infections: a multicenter study of children who presented to the emergency department. Pediatrics. 2009;123(4). Available at: www.pediatrics.org/cgi/content/full/123/4/e573 [DOI] [PubMed] [Google Scholar]
- 26.Cuzick J. A Wilcoxon-type test for trend. Stat Med. 1985;4(1):87–90 [DOI] [PubMed] [Google Scholar]
- 27.US Bureau of Labor Statistics. Consumer Price Index: CPI home. Available at: https://www.bls.gov/cpi/. Accessed June 26, 2019
- 28.Shay DK, Holman RC, Newman RD, et al. . Bronchiolitis-associated hospitalizations among US children, 1980-1996. JAMA. 1999;282(15):1440–1446 [DOI] [PubMed] [Google Scholar]
- 29.Zhang X, Johnson N, Carrillo G, Xu X. Decreasing trend in passive tobacco smoke exposure and association with asthma in U.S. children. Environ Res. 2018;166:35–41 [DOI] [PubMed] [Google Scholar]
- 30.Agaku IT, Vardavas CI. Disparities and trends in indoor exposure to secondhand smoke among U.S. adolescents: 2000-2009. PLoS One. 2013;8(12):e83058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mittal V, Darnell C, Walsh B, et al. . Inpatient bronchiolitis guideline implementation and resource utilization. Pediatrics. 2014;133(3). Available at: www.pediatrics.org/cgi/content/full/133/3/e730 [DOI] [PubMed] [Google Scholar]
- 32.Perrin JM, Bloom SR, Gortmaker SL. The increase of childhood chronic conditions in the United States. JAMA. 2007;297(24):2755–2759 [DOI] [PubMed] [Google Scholar]
- 33.Simon TD, Berry J, Feudtner C, et al. . Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics. 2010;126(4):647–655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peltz A, Hall M, Rubin DM, et al. . Hospital utilization among children with the highest annual inpatient cost. Pediatrics. 2016;137(2):e20151829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jensen EA, Lorch SA. Effects of a birth hospital’s neonatal intensive care unit level and annual volume of very low-birth-weight infant deliveries on morbidity and mortality. JAMA Pediatr. 2015;169(8):e151906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shin E. Hospital responses to price shocks under the prospective payment system. Health Econ. 2019;28(2):245–260 [DOI] [PubMed] [Google Scholar]