Abstract
The US Department of Health and Human Services has launched a large-scale plan that aims to “End the HIV Epidemic” (EtHE) in America, including ambitious goals and targets over the next 5 to 10 years.
To be successful, the EtHE Plan will require timely dissemination of relevant metrics to inform the broad array of stakeholders who are in a position to act in support of the plan’s goals. Metrics should include both population health outcome metrics and implementation metrics that track the deployment and uptake of specific intervention delivery strategies. In addition to the usual HIV care continuum metrics that include all people living with HIV in the denominator, metrics dedicated to those not yet reached (i.e., as the denominator) are essential to help target EtHE implementation efforts. Special attention is required around metrics and targets that inform and drive action on HIV-related health disparities.
Well-chosen metrics and a well-designed dissemination system can serve as important tools to assess the progress of the EtHE Plan, and to identify and disseminate lessons learned quickly within and across jurisdictions aiming to end HIV as a local public health threat.
The US Department of Health and Human Services recently announced a large-scale plan aiming to “End the HIV Epidemic” (EtHE) in America, including ambitious goals and targets over the next 5 to 10 years.1,2 Motivating the EtHE Plan are the major implementation gaps reflected in official national statistics, which include an estimated 37 000 new HIV infections that occur every year,3 more than 60% of the 1.1 million people living with HIV (PLWH) in the United States not receiving continuous medical care, and nearly half of all PLWH (49%) not on treatment or not virally suppressed.4 These suboptimal outcomes drive avoidable HIV-related morbidity, mortality, and onward HIV transmission in the United States, as well as major disparities in HIV incidence and mortality rates.
To be successful, at a minimum, these major implementation gaps must be bridged by the EtHE Plan. The need to rapidly learn and disseminate lessons while simultaneously implementing the plan suggests that efforts to achieve the EtHE Plan’s goals and targets should be framed as an implementation science challenge. If implementation science is about improving the uptake, engagement, and ultimately the impact of evidence-based interventions, then the EtHE Plan must fully leverage the best of what the field of implementation science has to offer for population health.5 This includes tremendous opportunity to generate useful evidence during the implementation process to rapidly inform course corrections over the plan’s 10-year time horizon. Indeed, the plan’s implementers at the federal, state, and local levels must not only be discerning consumers of scientific evidence as they select and deploy the plan’s programmatic components; they are also in a position to generate the critical evidence needed to inform the deployment of programmatic implementation strategies in ways that optimize the plan’s impact.
A prerequisite to the success of the EtHE Plan and other large-scale implementation efforts (e.g., the President’s Emergency Plan for AIDS Relief [PEPFAR]) is the timely dissemination of relevant metrics, with adequate epidemiological, programmatic, and demographic resolution. In addition to providing the ability to assess the degree of progress toward the EtHE Plan’s goals, well-chosen and rapidly disseminated metrics can help quickly identify geographic areas or populations that are either not being adequately reached by implementation efforts or not experiencing their desired impact. Broadly disseminating key metrics can also inform the implementation activities of a wide array of “whole-of-society” stakeholders2 across multiple sectors (e.g., health care, education, public, nonprofit, community-based, advocacy, research) at the county, state, and federal levels who are in a position to act in support of the plan’s goals and targets.
EVOLVING METRICS TO SUPPORT ENDING HIV EPIDEMICS
Metrics for large-scale programmatic and policy initiatives, such as the EtHE Plan, should include the following:
-
1.
Population health outcome metrics that relate directly to the central goals and targets of the EtHE Plan (e.g., incidence rate, proportion virally suppressed).
-
2.
Implementation metrics that reflect the timing and location of deployment of the specific implementation strategies intended to result in achieving the EtHE Plan’s goals (e.g., launching a preexposure prophylaxis [PrEP] center of excellence or a provider education campaign). These metrics need not reflect all the HIV-related implementation strategies or activities going on in a given jurisdiction, but it is critical to track actions that are taking place directly as a result of the EtHE Plan, which may take the form of new strategies, strengthening of existing strategies, or shifting the balance of funding allocated for prevention versus treatment.
-
3.
Implementation metrics that broadly reflect the uptake of and engagement in these strategies (e.g., number of people initiating and receiving PrEP at the center of excellence; number of providers trained on PrEP via the education campaign) by the specific target population that the plan intends to reach (e.g., young gay and bisexual men who have sex with men).
-
4.
Disparities metrics that monitor disparities in both population health outcomes and implementation outcomes. Using implementation metrics can capture and characterize differences in implementation approaches as well as their uptake and engagement within and across jurisdictions. This in turn can yield important insights to help “course correct” and to optimize future impact of the plan.
Many of the usual metrics employed for monitoring implementation and the impact of HIV service implementation at scale—including the HIV care continuum, 90-90-90 metrics, and PrEP coverage—are useful and necessary for EtHE, but they are likely not sufficient.6–8 These status quo metrics have some shortcomings that pose at least two key challenges to their ability to adequately support the implementation goal of rapidly ending HIV epidemics as a local public health threat.
The first challenge is that the denominators of these status quo metrics usually include all people living with HIV (PLWH), the majority of whom are already reached (i.e., diagnosed persons who are stable on treatment with durable viral suppression). However, a main focus of the EtHE Plan will necessarily and primarily be on PLWH who have not yet been reached or fully supported by public health and medical services (i.e., undiagnosed persons who are out of care or not durably suppressed on treatment). For example, new metrics that focus on care continuum outcomes only for newly diagnosed persons in the prior year, or viral suppression outcomes only among those who were not durably suppressed in a given year, could greatly help focus implementation activities where they are needed most. Because these kinds of metrics also employ a cohort or panel approach with smaller denominators more focally relevant to EtHE implementation, they have the added benefit of being more sensitive to the potential impact of targeted implementation.
The second challenge is that the status quo metrics lack critical elements reflecting the timeliness (or lack thereof) with which key care continuum milestones are achieved. This makes it very challenging to help focus implementation efforts on achieving progress toward the fundamental goals of early diagnosis, early care linkage, and early antiretroviral therapy initiation relative to HIV seroconversion.6 Indeed, a fundamental premise underlying the public health response to HIV epidemics around the globe, and one that is clearly reflected in the goals of the national EtHE Plan, is that diagnosing and treating all persons with HIV as soon as possible after seroconversion is the most effective way to reduce the risk of both HIV-related morbidity and mortality and onward HIV transmission. Evidence suggests that the United States has substantial room for improvement in this area. For example, although recent national data on the median CD4 count at diagnosis reported to the Centers for Disease Control and Prevention (CDC) are unfortunately not routinely disseminated by the CDC and most state and local health departments, the median CD4 count at diagnosis in New York City was 385 cells per microliter in 2017 (up slightly from 334 cells/µL in 2007).9 Notably, this is well below the median CD4 count in the treatment arm of the INSIGHT START trial (650 cells/µL) and the HIV Prevention Trials Network trial HPTN 052 (442 cells/µL), which reduced mortality and onward transmission, respectively.6
To address both of these challenges, we recently proposed the addition of new metrics and targets using information on pretreatment CD4 counts to help evolve the global public health response to HIV epidemics.6 Specifically, to help increase the focus of implementation efforts on achieving earlier diagnosis, earlier linkage to care, and earlier antiretroviral therapy initiation for as-yet unreached PLWH, we recommend targets as follows: 90% of persons with newly diagnosed HIV, 90% of persons newly linked to care, and 90% of persons newly initiating antiretroviral therapy should have pretreatment CD4 counts greater than 500 cells per microliter.6 The EtHE Plan and implementing jurisdictions should consider adopting these or similar metrics and targets.
ADDRESSING HEALTH DISPARITIES VIA THE ETHE PLAN
To address existing implementation and health outcome disparities (and to prevent further exacerbating them), special attention should be paid to developing metrics and targets that monitor and inform action on HIV-related disparities by race/ethnicity, sociodemographic factors, sexual and gender minority status, substance use, and geography in both implementation outcomes and health outcomes. The updated National HIV/AIDS Strategy incorporated metrics and targets for disparities in HIV diagnoses, viral suppression, and stigma; it has reported that, for new HIV diagnoses (as a proxy for HIV incidence), disparities targets were not met for gay and bisexual men, young Black gay and bisexual men, and persons living in the US South during the period 2010 to 2015.10 Given the major disparities in HIV incidence, and the potential for these disparities to be further exacerbated through differential access to HIV testing, PrEP, HIV treatment, and treatment adherence support, special attention must be paid to the use of metrics and targets to inform action and course corrections aimed at mitigating disparities. Indeed, existing HIV-related health disparities remain ever poised to be perpetuated or even worsened through inequitable implementation that may be otherwise “blind” to disparities. A poignant example is illustrated by the uptake of PrEP, where in 2017 Blacks made up 41% of persons with newly diagnosed HIV11 but only 11% of those on PrEP.12 Without explicit attention to these disparities, PrEP implementation under the EtHE Plan will not only perpetuate but will likely further exacerbate existing racial/ethnic disparities in HIV incidence.
Even if PrEP uptake by race/ethnicity was commensurate with the risks posed by the HIV epidemic, there would still be limitations with the status quo PrEP coverage metrics. This is because most population-based data on PrEP uptake are based on insurance claims or pharmacy prescriptions, a major limitation of which is that they do not provide epidemiological or behavioral information on persons using PrEP. This in turn limits the ability to assess both PrEP coverage and the major barriers and facilitators of PrEP uptake among those at highest risk for HIV acquisition. There is a need for systematic, mixed-methods approaches to both quantify and gain more in-depth insights surrounding the reasons for missed HIV prevention opportunities among those with recent HIV seroconversion, and the use of such insights to reshape ongoing implementation. New, national observational cohorts recruited online, supported by the National Institutes of Health’s Limited Interaction Targeted Epidemiology (LITE) to advance HIV prevention mechanisms,13 aimed at assessing PrEP uptake may be more useful for this. The LITE cohorts, which represent all 50 US states, Puerto Rico, and Guam, include gay and bisexual men as well as transmen and transwomen who have sex with men—groups at very high risk of HIV acquisition. These cohort studies also collect detailed epidemiological, sociodemographic, and sexual behavior information, as well as potential barriers to engaging in HIV prevention.14,15
OPPORTUNITIES AND CHALLENGES
Implementation of the EtHE Plan presents both opportunities and challenges related to disseminating metrics.
Opportunities
The best-designed metrics will be of little value unless they are in the form of actionable information that rapidly reaches the wide array of stakeholders who are in a position to act toward the achievement of the EtHE Plan’s goals. Moreover, the metrics must be disseminated in a timely enough manner that course corrections in implementation can be made and lessons learned can be derived quickly. Unlike the National HIV/AIDS Strategy, the national EtHE Plan will deploy strategies in specific geographic areas and will need to disseminate metrics beyond topline, national-level indicators with a three-year data lag.10 An initiative as large as the national EtHE Plan, with its wide range of information needs related to metrics, will likely require the use of a public-facing system to disseminate all plan-related metrics in relation to targets, similar to New York State’s Ending the Epidemic (EtE) Dashboard system (www.etedashboardny.org),16 the Fast Track Cities portal (http://www.fast-trackcities.org), PEPFAR Dashboards (https://data.pepfar.gov/dashboards), and the Foundation for AIDS Research’s Monitoring, Evaluation, and Reporting Database (https://mer.amfar.org).
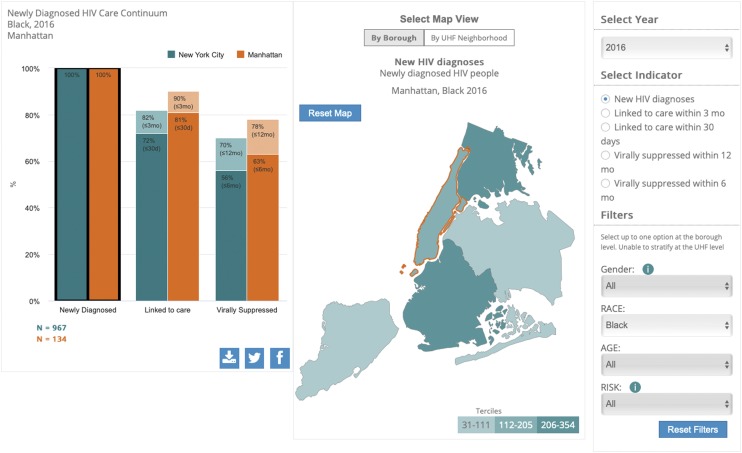
Different stakeholders and actors need different levels of information. Some may be interested in national or statewide metrics reflecting all PLWH in the country or state; others may want only metrics specific to one city, county, or population. New York’s EtE Dashboard system, which was specifically called for in New York State’s EtE Blueprint,17,18 utilizes interactive data visualizations for key metrics of the initiative that make it possible for users to view metrics that are specific to geographic area(s) and population(s) of interest. For example, it is possible to visualize the most recent HIV care continuum for the entire state of New York. It is also possible to visualize the most recent HIV care continuum for Black New Yorkers with newly diagnosed HIV that shows the proportion that were virally suppressed within 6 months and 12 months of their diagnosis (Figure 1) in Manhattan (lighter bars) compared with all of New York City (darker bars). There is also social media integration that allows users to further disseminate the tailored information they generate via Twitter or Facebook, or to download a graphic file to include in a presentation or grant proposal. Such features that allow users to retrieve and independently disseminate or leverage tailored information are important tools to help engage and mobilize multiple key actors around a common implementation agenda.
FIGURE 1—
Screen Shot From New York’s Ending the Epidemic (EtE) Dashboard System Showing an Interactive Visualization for Persons With Newly Diagnosed HIV in Manhattan (Orange) Versus the Rest of New York City (Turquoise)
Source. Reproduced with permission from www.etedashboardny.org.
Challenges
Data and metrics must be timely to be most useful to stakeholders. At the national level, surveillance data for new diagnoses occurring in 2017 reported to the CDC by health departments were disseminated by the CDC in November 2018.11 A national lag time of less than 12 months is impressive, and it seems likely that, with the necessary additional support and investment in state and local surveillance infrastructure by the EtHE Plan, state and local health departments could achieve an even shorter lag time. Thus, to minimize data lag, it may be important to provide a set of standard metric definitions and common data architecture for health departments to generate EtHE metrics, and then decentralize the ability to upload and disseminate them within a unified, common dashboard system. In New York City, the lag time for disseminating a complicated set of surveillance-based metrics on the EtHE Dashboard was reduced from more than 18 months in 2016 to less than 12 months by 2018,19 in part because of the blueprint recommendations and the state’s subsequent investment in surveillance infrastructure, which is critical to the EtE initiative’s success. Finally, a lack of data for some key outcomes and metrics will exist in many counties, especially for outcomes that can only be estimated, like the number of new HIV infections (true incidence), the proportion of PLWH with undiagnosed HIV, or the proportion of PLWH on HIV treatment. However, even though treatment status and the timing of treatment initiation are not captured in population-based HIV surveillance, methods have recently been developed that allow it to be reasonably inferred from longitudinal viral load data.20,21
CONCLUSIONS
Despite these challenges, the very committed communities of individuals and organizations working to respond to local HIV epidemics in the United States have an unprecedented and unparalleled amount of increasingly timely epidemiological and programmatic data to leverage in support of their implementation efforts. It will be important to evolve the status quo HIV metrics and targets to help better focus and support implementers in their efforts to achieve earlier diagnosis and earlier treatment initiation following seroconversion, and to accelerate increasing coverage of PrEP among those at highest risk for HIV acquisition. In addition to assessing the progress of the EtHE Plan toward achieving its goals, well-chosen health outcome and implementation metrics, combined with a well-designed dissemination system, are essential tools for accelerating impact within and across those jurisdictions aiming to end HIV as a local public health threat.
ACKNOWLEDGMENTS
This work was supported by funding from the US National Institutes of Health (NIH), including the Einstein, Rockefeller, CUNY Center for AIDS Research (ERC CFAR, P30 AI124414), and the HIV Center for Clinical and Behavioral Studies (P30 MH043520), the New York State Department of Health AIDS Institute, and the CUNY Institute for Implementation Science in Population Health.
Thanks to the New York State AIDS Institute (John Fuller, Johanne Morne, Dan O’Connell, Bruce Agins) for their review and input on the design and content of New York’s Ending the Epidemic (EtE) Dashboard; Benjamin Katz, McKaylee Robertson, Sarah Kulkarni, Diane Addison, Olga Tymejczyk, Abigail Baim-Lance, and Denis Nash for curating data; Ashish Joshi and YConnect for Web development, including dashboard visualizations; the New York State Department of Health and Mental Hygiene (Rachael Lazar, Sarah Braunstein, Demetre Daskalakis); and the many other key stakeholders who helped shape the vision and needs for New York’s EtE dashboard, including the EtE Task Force members and the EtE Task Force Data Committee.
Note. The views expressed in this article are those of the author and not necessarily those of the US NIH or the New York State AIDS Institute.
CONFLICTS OF INTEREST
The author reports no conflicts of interest.
Footnotes
REFERENCES
- 1.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA. 2019;321(9):844–845. doi: 10.1001/jama.2019.1343. [DOI] [PubMed] [Google Scholar]
- 2.HIV.gov. What is “Ending the HIV Epidemic: A Plan for America”? 2019. Available at: https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview. Accessed August 1, 2019.
- 3.Song R, Hall HI, Green TA, Szwarcwald CL, Pantazis N. Using CD4 data to estimate HIV incidence, prevalence, and percent of undiagnosed infections in the United States. J Acquir Immune Defic Syndr. 2017;74(1):3–9. doi: 10.1097/QAI.0000000000001151. [DOI] [PubMed] [Google Scholar]
- 4.HIV.gov. Data and trends: US statistics. 2019. Available at: https://www.hiv.gov/hiv-basics/overview/data-and-trends/statistics. Accessed August 1, 2019.
- 5.Baim-Lance A, Zimba R, Nash D. Implementation science for population health toolkit. 2019. Available at: cunyisph.org/isph-toolkit. Accessed August 31, 2019.
- 6.Nash D, Robertson M. How to evolve the response to the global HIV epidemic with new metrics and targets based on pre-treatment CD4 counts. Curr HIV/AIDS Rep. 2019;16(4):304–313. doi: 10.1007/s11904-019-00452-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perlman DC, Jordan AE, Nash D. Conceptualizing care continua: lessons from HIV, hepatitis C virus, tuberculosis and implications for the development of improved care and prevention continua. Front Public Health. 2017;4:296. doi: 10.3389/fpubh.2016.00296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Horn T, Sherwood J, Remien RH et al. Towards an integrated primary and secondary HIV prevention continuum for the United States: a cyclical process model. J Int AIDS Soc. 2016;19(1):21263. doi: 10.7448/IAS.19.1.21263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. ETEDashboard. People newly diagnosed with HIV, New York City (2006–2017). 2019. Available at: http://etedashboardny.org/data/new-diagnoses-and-linkage/new-diagnoses-trends-nyc. Accessed August 1, 2019.
- 10.HIV.gov. National HIV/AIDS strategy for the United States: updated to 2020. 2017 progress report. Available at: https://files.hiv.gov/s3fs-public/NHAS_Progress_Report_2017.pdf. Accessed August 1, 2019.
- 11.Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2017. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2017-vol-29.pdf. Accessed November 6, 2019.
- 12.Huang YA, Zhu W, Smith DK, Harris N, Hoover KW. HIV preexposure prophylaxis, by race and ethnicity—United States, 2014–2016. MMWR Morb Mortal Wkly Rep. 2018;67(41):1147–1150. doi: 10.15585/mmwr.mm6741a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Institutes of Health. Limited Interaction Targeted Epidemiology (LITE) to advance HIV prevention (UG3/UH3) 2016. Available at: https://grants.nih.gov/grants/guide/rfa-files/rfa-ai-16-031.html. Accessed November 6, 2019.
- 14.Nash D, Stief M, McCrate K et al. A Web-based pre-exposure prophylaxis–era sample of vulnerable HIV-negative gay and bisexual men, transmen and transwomen who have sex with men: a protocol for an observational cohort study. JMIR Res Protoc. 2019;8(9):e13715. doi: 10.2196/13715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.PRIDE Health Research Consortium. Large-scale study of HIV-negative MSM across the nation. 2019. Available at: https://www.prideresearch.org/lite-grant.html. Accessed August 1, 2019.
- 16.Joshi A, Amadi C, Katz B, Kulkarni S, Nash D. A human-centered platform for HIV infection reduction in New York: development and usage analysis of the Ending the Epidemic (ETE) Dashboard. JMIR Public Health Surveill. 2017;3(4):e95. doi: 10.2196/publichealth.8312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.New York State Dept of Health. Ending the AIDS epidemic in New York State. 2015. Available at: https://www.health.ny.gov/diseases/aids/ending_the_epidemic. Accessed August 1, 2019.
- 18.New York State ETE Taskforce. 2015 blueprint for achieving the goal set forth by Governor Cuomo to end the epidemic in New York State by the end of 2020. Available at: https://www.health.ny.gov/diseases/aids/ending_the_epidemic/docs/blueprint.pdf. Accessed August 1, 2019.
- 19.ETEDashboard. Newly released 2017 HIV surveillance data for New York City—with a record low data lag of <12 months. 2018. Available at: http://etedashboardny.org/newly-released-2017-hiv-surveillance-data-for-new-york-city-with-a-record-low-data-lag-of. Accessed August 1, 2019.
- 20.Braunstein SL, Robertson MM, Myers J, Nash D. Using HIV viral load from surveillance to estimate the timing of antiretroviral therapy initiation. J Acquir Immune Defic Syndr. 2016;73(2):222–227. doi: 10.1097/QAI.0000000000001052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Braunstein S, Robertson M, Myers J, Abraham B, Nash D. Increase in CD4+ T-cell count at the time of HIV diagnosis and antiretroviral treatment initiation among persons with HIV in New York City. J Infect Dis. 2016;214(11):1682–1686. doi: 10.1093/infdis/jiw438. [DOI] [PMC free article] [PubMed] [Google Scholar]