Abstract.
Schoolchildren are commonly linked to influenza transmission. Handwashing with soap has been shown to decrease infections; however, improving handwashing practices using soap and water is difficult in low-resource settings. In these settings, alternative hygiene options, such as hand sanitizer, could improve handwashing promotion to reduce influenza virus infections. We conducted a cluster randomized control trial in 24 primary schools in Dhaka to assess the effectiveness of hand sanitizer and a respiratory hygiene education intervention in reducing influenza-like illness (ILI) and laboratory-confirmed influenza during June–September 2015. Twelve schools were randomly selected to receive hand sanitizer and respiratory hygiene education, and 12 schools received no intervention. Field staff actively followed children daily to monitor for new ILI episodes (cough with fever) through school visits and by phone if a child was absent. When an illness episode was identified, medical technologists collected nasal swabs to test for influenza viruses. During the 10-week follow-up period, the incidence of ILI per 1,000 student-weeks was 22 in the intervention group versus 27 in the control group (P-value = 0.4). The incidence of laboratory-confirmed influenza was 53% lower in the intervention schools (3/1,000 person-weeks) than in the control schools (6/1,000 person-weeks) (P-value = 0.01). Hand sanitizer and respiratory hygiene education can help to reduce the risk of influenza virus transmission in schools.
INTRODUCTION
Influenza-associated respiratory infections cause severe illness and death worldwide. Globally, seasonal influenza–associated excess mortality rates are estimated to be 4.0–8.8 per 100,000 individuals per year (290,000–646,000 respiratory deaths per year), whereas 9,000–106,000 influenza-associated respiratory deaths occur among children aged < 5 years annually.1 The mortality and morbidity burden of acute respiratory infections associated with influenza was estimated to be higher in less developed regions, such as Bangladesh.2,3 In Dhaka, the capital city of Bangladesh, the incidence of childhood pneumonia associated with influenza was four per 100 child-years.4 During 2011–2012, the estimated mortality burden of influenza-associated respiratory infections was 13 deaths per 100,000 among children aged < 5 years and 88 deaths per 100,000 among persons aged > 60 years in Bangladesh.5
Schoolchildren commonly contribute to community-wide influenza virus transmission.6 Epidemiological studies suggest that in a typical epidemic, influenza affects schoolchildren first, then this population may transmit the virus among family members and then to the general community.7–9 High infection rates among children may be due to lower immunity and a large number of contacts from overcrowding at schools in many low-income countries, such as Bangladesh.10,11 Considering the potential effect of influenza virus infection on children and subsequently their families, prevention strategies in schools might reduce the individual and societal burden of influenza.
Although annual vaccination is considered a primary prevention strategy for influenza virus infection,12 seasonal influenza vaccination has not been widely promoted in Bangladesh or other lower income countries because of cost, limited resources, and competing priorities in the health care system.13 In the absence of vaccine and antiviral treatment, handwashing with soap has been recommended as the primary and cost-effective prevention measure for influenza-associated respiratory infection.14 Several intervention trials in low- and middle-income countries have concluded that intensive handwashing promotion in school settings can reduce diarrheal and respiratory disease incidence.15–19 A randomized controlled trial in Pakistan reported a statistically significant effect of handwashing in protecting children from respiratory infections.20 A study conducted in Egypt also reported that handwashing, in combination with health messages, reduced the incidence of influenza-like illness (ILI) and influenza virus infections among schoolchildren.21 In addition, respiratory hygiene education regarding proper ways to cover cough and sneeze is another feasible method to reduce influenza virus transmission in schools.22–24 A pilot study conducted in four primary schools in Dhaka city on coughing and sneezing into upper sleeve was found feasible and acceptable.25
Although there is evidence that these behavior change interventions can reduce infection, handwashing with soap and practicing respiratory hygiene in Bangladesh are uncommon. An observational study of respiratory hygiene practices among schoolchildren in urban and rural Bangladesh showed that students did not wash hands with soap and water after respiratory events (coughing and sneezing) and observed that 85% of children coughed or sneezed into the open air.22 Although several recent studies have demonstrated significant improvement in handwashing behavior among students in schools, in Bangladesh,26,27 handwashing with water may be difficult in school settings because water and soap supplies are limited because of cost and availability.22,28 In a national hygiene survey conducted in 2014, only 21% of the schools in Bangladesh had a handwashing location where water and soap were available.29 Hand sanitizer could be a useful public health intervention for reducing influenza virus transmission. A study conducted at three elementary schools in California reported that in the absence of standard handwashing facilities at schools, waterless alcohol-based hand sanitizer was as an effective alternative to water and soap for handwashing.30 Hand sanitizer is a good option for the settings where water and soap are not readily available or limited, and, as it is easy to use, it may help to facilitate handwashing behavior of students in school settings. However, in low-income settings, limited research has been conducted on the behavioral and health impact of hand sanitizer use.31 If hand sanitizer is found to effectively reduce transmission of respiratory pathogens in Bangladesh, the government could consider supplying hand sanitizer at a minimum during a pandemic situation as a primary preventive measure or more consistently throughout the school year to reduce the illness during seasonal epidemics.
In this study, we evaluated the effectiveness of a behavior change intervention with hand sanitizer and respiratory hygiene messages in school settings to reduce the incidence of influenza virus infections among schoolchildren in Dhaka, Bangladesh.
MATERIALS AND METHODS
Research design.
We conducted a cluster-randomized controlled trial to assess the effectiveness of waterless alcohol-based hand sanitizer in combination with respiratory hygiene education in reducing ILI and laboratory-confirmed influenza among primary schoolchildren in Bangladesh over a single influenza season. The primary outcomes measured were ILI and laboratory-confirmed influenza virus infection. The study was conducted in 2015 during a 10-week period during the influenza season, June–September. A 6-week school vacation period from the 3rd week of June to the 3rd week of July was excluded from our analysis.
Settings.
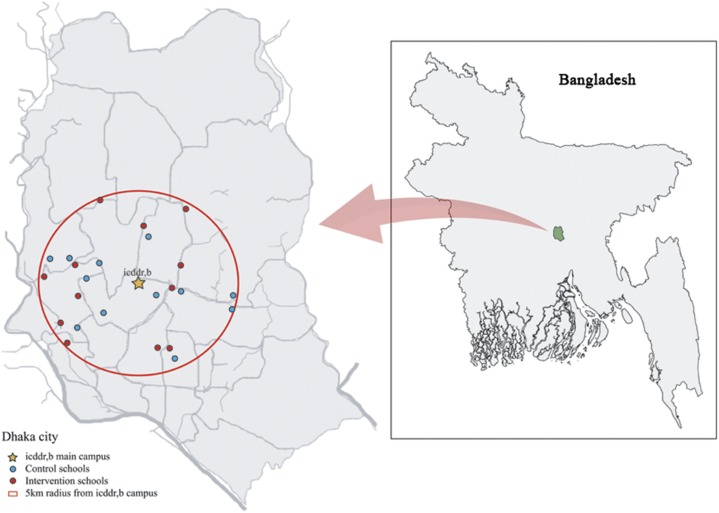
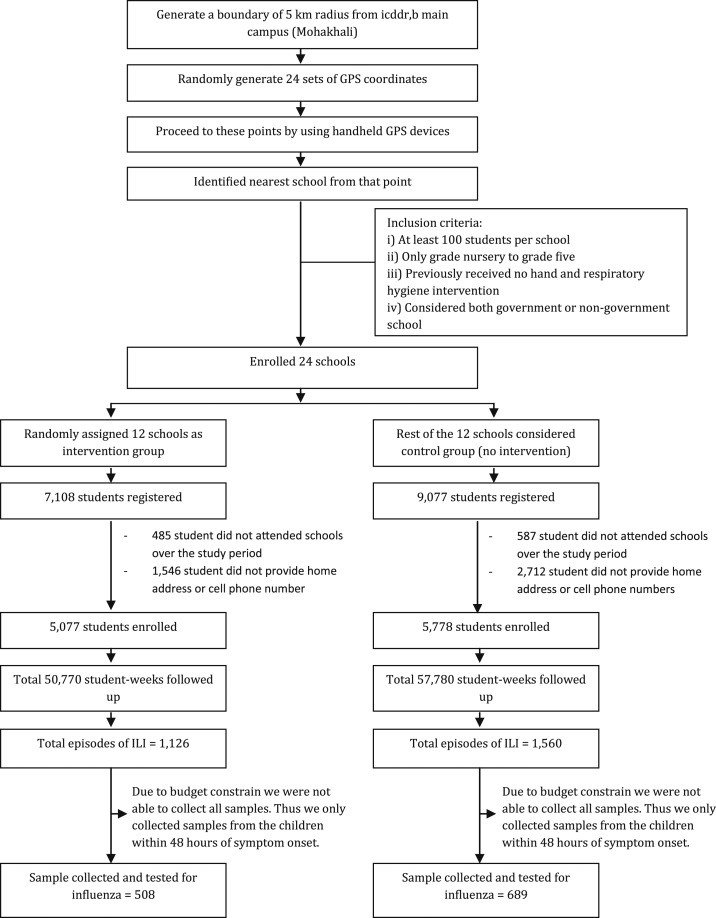
We conducted this study in 24 randomly selected primary schools in Dhaka. Primary schools in Bangladesh provide education to children aged 5–10 years (nursery–grade 5). We randomly generated 24 global positioning system (GPS) coordinates within a 5-km radius of the International Center for Diarrheal Disease Research, Bangladesh (icddr,b) campus, located in the middle of Dhaka (Figure 1). Field staff visited each GPS point and identified the nearest primary school. We included both government and private schools that had at least 100 enrolled students. We excluded schools that offered education above grade 5 because of differences in student populations, as well as schools that had previously received a hand or respiratory hygiene intervention. If the school was eligible for inclusion, field staff sought written consent from the headmaster/mistress of the school to participate in the study. If the school did not consent or if the school did not meet the inclusion criteria, field staff identified the next nearest primary school (Figure 2). We did not provide any incentives to any schools to participate in the study.
Figure 1.
Location of schools selected for either the intervention or control arms within a 5-km radius of International Center for Diarrheal Disease Research, Bangladesh (icddr,b) campus in Dhaka, Bangladesh. This figure appears in color at www.ajtmh.org.
Figure 2.
Study flow diagram.
Sample size calculation.
Influenza-like illness incidence was the outcome used for our power calculations. We assumed the ILI incidence among schoolchildren in Dhaka to be 20 per 100 person-years , based on an estimated incidence of ILI in children aged 6–10 years in Managua, Nicaragua, of 24 per 100 person-years.32 We anticipated that the intervention group would have an incidence of 10 ILI episodes per 100 person-years . We considered an equal number of intervention schools and control schools to reduce 10% ILI incidence with 80% statistical power and 5% significance level . We used the following equation to calculate the appropriate sample size33:
where y = person year, c = cluster, and k = between-cluster variation.
Based on these assumptions, we determined that 12,220 person-weeks of follow-up per study arm would be needed. We enrolled 12 schools per arm with > 100 students each and followed students within the schools for 10 weeks. Accounting for a design effect of 1.5, a required minimum of 1,081 person-weeks of follow-up per school was needed. The minimum number of person-weeks for the schools in each arm would be 12,972 person-weeks, providing adequate power to detect possible differences.
Interventions.
We randomly allocated all enrolled schools into one of two groups using a computer-based random number generator and randomly assigned each group to one of two arms: an intervention arm (12 schools) and a control arm (12 schools). Control schools did not receive any of the hand sanitizer or hand and respiratory hygiene education intervention during the study period. However, at the end of the study period, we provided educational materials to each of the enrolled students that included a plastic ruler containing messages on handwashing with soap and respiratory hygiene etiquette. Intervention schools received a two-component intervention: 1) hand sanitizer placed in each classroom and outside toilets at each school and 2) hand and respiratory hygiene education. We used hand sanitizer that was manufactured by a local pharmaceutical company and was available commercially in Bangladesh (price: US$ 5.75/L). This hand sanitizer contained about 63% ethyl alcohol. We delivered the hand sanitizer in colorless, transparent 1.5-L local plastic bottles and affixed them to the wall in all classrooms and outside of all toilets in the intervention schools. Field staff refilled the bottles at the schools as needed throughout the intervention period. All children were encouraged to use the hand sanitizer at five key times during the day: 1) when entering into the classroom; 2) after sneezing, coughing, or blowing their nose; 3) after using the toilet/washroom; 4) before eating any food; and 5) when leaving the school at the end of the day.
We implemented a previously developed respiratory hygiene behavior change intervention for elementary schools in Bangladesh that reduced the proportion of students who coughed and sneezed in the open air (from 92% to 47%) and increased the proportion of students who coughed and sneezed into their upper sleeve (from 0% to 39%) after 4 weeks of the intervention.25 In the intervention schools, we provided hand and respiratory hygiene education, including what to do if their hands were dirty, why students should wash their hands, benefits of washing hands and of using hand sanitizer, and the procedure for washing hands using hand sanitizer. We also taught students to cover their mouth and nose with the upper part of their sleeve while coughing and/or sneezing.
We integrated our respiratory hygiene messages into the school’s hygiene curriculum. Following the recommendations from the headmaster/headmistress and members of school management committees, we identified potential teachers in each intervention school who were responsible for dissemination of the intervention messages throughout the intervention period. We trained the selected teachers on intervention messages and behavior change communications over 2 days. These selected teachers communicated these messages with other teachers in their schools. All teachers in intervention schools also received on-site training on the use of hand sanitizer, as well as on how to prevent respiratory secretions from spreading by covering their mouth and nose by the upper part of their sleeve. In addition, a video clip that has been previously developed by icddr,b scientists based on respiratory hygiene practice was delivered during behavior change communication sessions to the students. Behavior change materials (available in the Supplemental Appendix) demonstrating sneezing and coughing into the sleeve and how to use hand sanitizer were distributed and placed around the intervention schools. Classroom teachers conveyed intervention messages three times per week during their regular hygiene education classes. In these health education classes, they emphasized the use of hand sanitizer at key times and encouraged children to practice proper respiratory hygiene behaviors. Classroom teachers also used hand sanitizer in the classroom to encourage students.
Data collection.
Baseline survey.
We conducted a baseline survey in all participating schools before randomization. During the baseline survey, trained field-workers collected information about the number of classes and the class size, physical structure of the classes, and handwashing facilities available at schools. After obtaining consent from the school headmaster/headmistress, field-workers collected current student information from the school register. Each school’s headmaster/headmistress assisted field staff to prepare and send an informational letter to inform and describe the study to parents of students and to request contact names, phone numbers, and physical addresses for each child. Using computer-generated random numbers, we randomly selected 15% of children from each classroom and school to conduct a household survey to determine economic status and living conditions. For example, if a school had five classrooms with 20 children each, three children from each classroom were selected for the household survey for a total of 15 children at the school. After obtaining written informed consent, trained field-workers collected household data about parent’s occupation, assets, household size, ventilation, bedroom size, and fuel used for cooking through an in-person interview.
Structured observation.
Field staff conducted structured observations at 12 participating schools (six intervention schools and six control schools) for approximately 5 hours per school to observe handwashing and respiratory hygiene behaviors of the children at the baseline and at the end of the intervention. Two field staff members visited each randomly selected school in the morning, stayed for 2–3 hours (total 5 hours by two field staff), and sat in two different locations in a classroom or outside the classroom where they could observe the entrance to the toilets and handwashing facilities, including the hand sanitizer dispenser. They used a structured observation data collection form to record observations of the children’s handwashing and respiratory hygiene behaviors during school hours.
ILI surveillance and sample collection.
Field staff visited each school every other day during the intervention period and screened students for new ILI episodes with assistance from teachers and by visiting each classroom. Primarily, schoolteachers asked students during the first session of the day about any symptoms developed among students in their class and notified the field staff assigned to that school. The field staff visited classrooms with ill children and verified the information provided by the teachers, and again asked all students about any respiratory symptoms. If a child reported ILI symptoms, the field staff talked to their parent/guardian over phone to confirm symptoms and also measured temperature using a thermometer to determine if the child reported having fever. An ILI episode was defined as measured fever ≥ 38°C or subjective fever and cough. If a child was absent, the field staff followed up by phone to identify the reason for absenteeism and to determine if the child met the ILI case definition. If a child in a participating school had an ILI episode, a trained medical technologist visited the child’s household to obtain consent from the child’s parent/guardian and collect a nasal swab from the child within 48 hours of symptom onset. If it was outside the 48-hour window, the sample was not collected.
In addition, on the same days as ILI surveillance, field staff measured the level of hand sanitizer in the morning and in the afternoon to calculate the amount of hand sanitizer used per day per school and enrolled children.
Laboratory testing.
Nasal swabs were transported in virus transport media to icddr,b virology laboratory on the same day of sample collection and stored in −70°C freezers. Total nucleic acid was extracted from the nasal swabs, and laboratory personnel performed real-time reverse transcriptase–polymerase chain reaction using fluorescent Taqman probes to detect influenza A and B and their subtypes using primers and probes designed by the CDC, Atlanta, as described previously.34,35
Statistical analyses.
We counted handwashing practice as the number of instances when a student washed their hands with water, and water and soap, or used hand sanitizer at recommended key times. We observed the total number of handwashing opportunities, and handwashing instances were counted during the observation period. We calculated the percentage of handwashing practices by dividing the number of handwashing instances by the total number of handwashing opportunities. One child could have several instances of proper handwashing practice recorded during the intervention period. We calculated the difference in difference (DID) for handwashing events during the recommended key times, for coughing and sneezing into open air, and for coughing and sneezing into upper arm using the number of instances counted during the observation period between control and intervention schools through regression analysis, and accounted for the school-level clustering effect. We also calculated the amount of sanitizer used per enrolled children per day at each school.
We calculated the incidence of ILI and laboratory-confirmed influenza virus infections per 1,000 student-weeks during the study period for both the control and intervention groups. To calculate incidence in each group (control and intervention), we calculated person time contribution by each students in the selected schools. Student-week was calculated by the period of intervention (from the beginning of the intervention till the end of the intervention) for each student. Maximum contribution time was 10 weeks. As the intervention was only for 10 weeks and in the middle of the academic year, there was no dropout. We estimated the incidence rate ratio (IRR) of ILI and laboratory-confirmed influenza virus infections to compare the intervention and control groups using univariate Poisson regression and included the school-level cluster effect to estimate the adjusted CI (95% CI) and P-value. Univariate models were used to identify factors associated with ILI and laboratory-confirmed influenza virus infections that were statistically significant (P-value ≤ 0.05). Multivariable Poisson regression analysis was used to adjust for risk factors that were statistically significant in univariate analysis to estimate an adjusted IRR (AIRR) of ILI and considered school-level cluster as a clustering effect. Analyses were performed using the statistical program STATA® version 13.0 (Stata Corp., College Station, TX). The analytical plan of this randomized controlled trial was not preregistered.
RESULTS
We enrolled 10,855 students in the study (intervention schools: 5,077children and control schools: 5,778 children), for 108,550 student-weeks of observation (Figure 2). The average number of children per school was 423 (SD: 244) in the intervention schools and 482 (SD: 331) in the control schools. Regarding handwashing facilities at the baseline, 10 schools in the intervention group and 12 schools in the control group had water and only one school in each group had soap available for handwashing. The remaining two intervention schools did not have water at the handwashing stations (Table 1). Household information was collected from 1,560 households (872 households from intervention group and 688 households from control group). The household size, monthly household expenses, and ventilation in the bedroom were similar between families of enrolled children in the intervention and control schools (Table 2). There were some reported differences in assets available at home between families of children in intervention and control schools, including the type of fuel used for cooking, ownership of land, and the bedroom size at the household level (Table 2).
Table 1.
School and student characteristics at baseline of intervention and control schools in Dhaka city, 2015
| Intervention | Control | |
|---|---|---|
| Student characteristics | Mean (SD), N = 5,077 | Mean (SD), N = 5,778 |
| Average students per school | 423 (244) | 482 (331) |
| Nursery | 48 (22) | 43 (25) |
| Grade 1 | 72 (39) | 97 (73) |
| Grade 2 | 84 (52) | 114 (100) |
| Grade 3 | 86 (57) | 89 (63) |
| Grade 4 | 74 (51) | 68 (38) |
| Grade 5 | 60 (44) | 70 (79) |
| Average of student per school according to gender | ||
| Boys | 200 (117) | 223 (161) |
| Girls | 223 (129) | 256 (171) |
| School characteristics | n (%), N = 12 | n (%), N = 12 |
|---|---|---|
| Handwashing location | ||
| Indoors (< 10 steps from classroom) | 7 (58) | 7 (58) |
| Indoors (> 10 steps from classroom) | 4 (33) | 4 (33) |
| Outdoors (> 10 steps from classroom) | 1 (8) | 1 (8) |
| Handwashing facilities available at the handwashing location | ||
| Water | 10 (83) | 12 (100) |
| Soap | 1 (8) | 1 (8) |
| Hand/respiratory hygiene taught in the school curriculum | ||
| Yes | 8 (67) | 9 (75) |
| No | 4 (33) | 3 (25) |
Table 2.
Student household characteristics at baseline (N = 1,560)
| Description | Intervention (N = 688) | Control (N = 872) |
|---|---|---|
| n (%) | n (%) | |
| Source of household income | ||
| Formal employment/service | 405 (59) | 479 (55) |
| Self-employment | 27 (4) | 43 (5) |
| Casual/contract job | 57 (8) | 95 (11) |
| Day labor | 102 (15) | 93 (11) |
| Rikshaw/van puller | 46 (7) | 99 (11) |
| Driver, motor vehicle | 51 (7) | 63 (7) |
| Household size (member), mean (SD) | 5.0 (1.6) | 4.9 (1.5) |
| Monthly household expenditure (USD) | ||
| ≤ 10,000 BDT (< 120) | 98 (14) | 144 (17) |
| 10,001–20,000 BDT (120–240) | 514 (75) | 630 (72) |
| 20,001–30,000 BDT (240–360) | 59 (9) | 82 (9) |
| > 30,000 BDT (> 360) | 17 (2) | 16 (2) |
| Availability of assets | ||
| Electricity | 688 (100) | 872 (100) |
| Wardrobe/almirah | 412 (60) | 385 (44) |
| Table | 297 (43) | 342 (39) |
| Chair/bench | 338 (49) | 360 (41) |
| Wristwatch/wall clock | 399 (58) | 485 (56) |
| Bed | 583 (85) | 712 (82) |
| Chouki | 163 (24) | 193 (22) |
| Radio | 14 (2) | 24 (3) |
| Electric fan | 679 (99) | 860 (99) |
| Television | 588 (85) | 740 (85) |
| Bicycle | 63 (9) | 47 (5) |
| Motorcycle | 11 (1) | 8 (1) |
| Refrigerator | 234 (34) | 229 (26) |
| Sewing machine | 136 (20) | 99 (11) |
| Mobile phone | 676 (98) | 843 (97) |
| Type of fuel used for cooking | ||
| Wood/charcoal/kerosene | 88 (13) | 59 (7) |
| Gas/electricity | 600 (87) | 813 (93) |
| Household-owned land | 462 (67) | 487 (56) |
| Windows and doors in bedrooms | ||
| ≥ 3 walls with a window or door | 145 (21) | 161 (18) |
| 2 walls with a window or door | 9 (1) | 10 (1) |
| 1 wall with a window and door | 398 (58) | 499 (57) |
| Only one door and no windows | 136 (20) | 202 (23) |
BDT = Bangladesh taka.
Handwashing and respiratory hygiene behavior.
At the baseline, observed handwashing events during the recommended key times were similar between the schools (intervention: 15% and control: 16% [P-value = 0.7]). In 97% of observed handwashing events, only water was used (Table 3). At the end of the intervention, observed handwashing with soap or sanitizer at key times was more common in the intervention schools than in the control schools. Among the total opportunities for handwashing at key times observed by field staff during the structured observations at the end of the intervention (intervention schools: total 921 opportunities and control schools: total 802 opportunities), 604 (66%) schoolchildren in the intervention group washed their hands and 171 (21%) schoolchildren in the control group washed their hands (DID = 45%; 95% CI = 21%, 69%). During this structured observation period, hand sanitizer was used in 91% of the observed handwashing events in the intervention schools at the end of the intervention period (Table 3). The average consumption of hand sanitizer per child per day was 4.3 mL (95% CI = 1.5 mL, 7.1 mL), with an estimated cost in Bangladesh Taka 2 (US$0.03) per day per child. At the baseline, the proportion of coughing and sneezing into open air was 77% (74/96) in intervention schools and 56% (85/151) in control schools. At the end of the intervention, coughing and sneezing into open air among the students at intervention schools decreased to 37% (47/127) during observation (DID = −63%; 95% CI = −98%, −27%). The proportion of instances when proper cough or sneeze etiquette was observed was 33% (n = 42) in the intervention group compared with 2% in the control group at the end of the intervention period (DID = 33%; 95% CI = 33%, 33.1%).
Table 3.
Observed handwashing practice among students at recommended key times at the baseline and at the end of the intervention
| Recommended key times | Control group | Intervention group | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Handwashing opportunities | Washed hands | Handwashing agents used | Handwashing opportunities | Washed hands | Handwashing agents used | |||||||||||||||
| Sanitizer | Soap + water | Only water | Sanitizer | Soap + water | Only water | |||||||||||||||
| Baseline | Endline | Baseline | Endline | Baseline | Endline | Baseline | Endline | Baseline | Endline | Baseline | Endline | Baseline | Endline | Baseline | Endline | Baseline | Endline | Baseline | Endline | |
| n | n | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n | n | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| At arrival at school | 49 | 50 | 4 (10) | 12 (24) | – | – | – | – | 4 (100) | 12 (100) | 109 | 87 | 9 (8) | 72 (83) | – | 70 (97) | – | – | 9 (100) | 2 (3) |
| After coughing and sneezing | 151 | 118 | 1 (1) | 1 (1) | – | 1 (100) | – | – | 1 (100) | – | 96 | 127 | 2 (2) | 40 (32) | – | 39 (97) | – | 1 (3) | 2 (100) | – |
| After toilet/washroom use | 139 | 262 | 53 (38) | 136 (52) | – | – | 3 (6) | 3 (2) | 50 (94) | 133 (98) | 311 | 217 | 91 (29) | 168 (77) | – | 135 (80) | 5 (5) | 13 (8) | 86 (95) | 20 (12) |
| Before having any food | 181 | 305 | 34 (19) | 18 (6) | – | – | – | 2 (11) | 34 (100) | 16 (89) | 498 | 318 | 62 (12) | 195 (61) | – | 181 (92) | – | 7 (4) | 62 (100) | 7 (4) |
| Leaving school at the end of the day | 63 | 67 | 0 (0) | 4 (4) | – | – | – | 3 (75) | – | 1 (25) | 77 | 172 | 0 (0) | 129 (75) | – | 126 (98) | – | 2 (1) | – | 1 (1) |
| Total | 583 | 802 | 92 (16) | 171 (21) | – | 1 (1) | 3 (3) | 8 (5) | 89 (97) | 162 (95) | 1,091 | 921 | 164 (15) | 604 (66) | – | 551 (91) | 5 (3) | 23 (5) | 159 (97) | 30 (5) |
Incidence of ILI and laboratory-confirmed influenza.
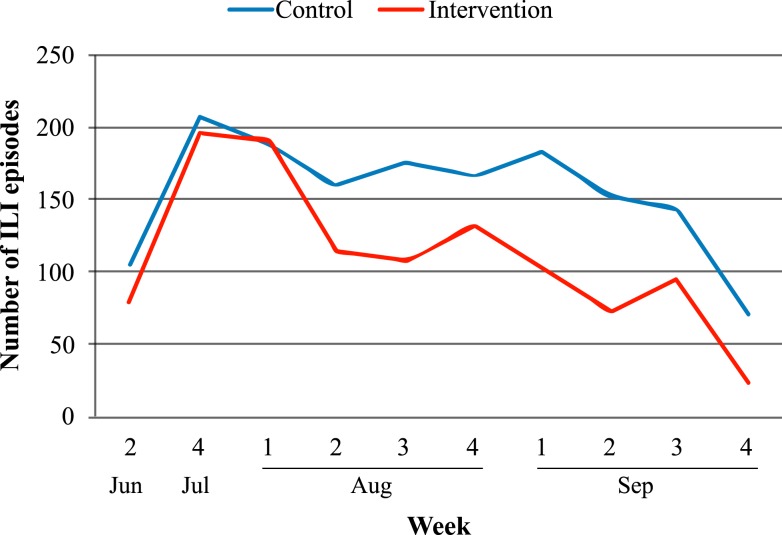
We identified 2,686 ILI episodes during the 10-week observation period across all schools. Of these episodes, 1,560 were identified in control schools (58%) and 1,126 were identified in intervention schools (42%). In the first 3 weeks of the intervention period, the number of weekly ILI episodes per school was similar between intervention and control, but as the intervention progressed, the number of ILI episodes identified among students at intervention schools was lower than that at control schools (Figure 3). Across the observation period, 924 students in the intervention schools (18%) had at least one ILI episode: 769 students (15%) had one episode and 155 students (3%) had more than one episode. By comparison, 1,214 students in control schools (21%) had at least one ILI episode: 955 students (17%) had one episode and 259 students (4%) had more than one episode. The incidence of ILI was 22 per 1,000 student-weeks among children in the intervention schools and 27 per 1,000 student-weeks among children in the control schools (Table 4). The incidence of ILI per 1,000 students-weeks was 18% lower in the intervention group than in the control group, but the difference was not statistically significant, even after adjusting for gender (AIRR:0.8, 95% CI = 0.5, 1.3, P-value = 0.4) (Table 5).
Figure 3.
Number of influenza-like illness (ILI) episodes by week and study group in Dhaka, Bangladesh, June–September 2015 (N = 10,855). Note: Schools were on vacation from the 3rd week of June through the 3rd week of July 2015. This figure appears in color at www.ajtmh.org.
Table 4.
Incidence rate of ILI and laboratory-confirmed influenza among children of participated schools during the 10-week observation period from June to September 2015
| Description | ILI | Laboratory-confirmed influenza | ||
|---|---|---|---|---|
| Control | Intervention | Control | Intervention | |
| n/T (IR per 1,000 student-week; 95% CI) | n/T (IR per 1,000 student-week; 95% CI) | n/T (IR per 1,000 student-week; 95% CI) | n/T (IR per 1,000 student-week; 95% CI) | |
| Total children | 1,560/57,780 (27; 17–42) | 1,126/50,770 (22; 17–29) | 43/6,890 (6; 4–10) | 15/5,080 (3; 2–4) |
| According to gender* | ||||
| Boys | 607/26,770 (23; 14–36) | 446/24,010 (19; 14–24) | 18/2,610 (7; 4–13) | 8/1,910 (4; 2–8) |
| Girls | 953/30,730 (31; 20–48) | 680/26,740 (25; 19–33) | 25/4,280 (6; 4–10) | 7/3,170 (2; 1–4) |
| According to grade of students | ||||
| Nursery | 144/5,120 (28; 15–53) | 77/5,770 (13; 8–24) | 5/540 (9; 2–30) | 1/300 (3; 1–16) |
| Grade 1 | 310/11,690 (27; 16–43) | 169/8,690 (19; 14–28) | 4/1,040 (4; 1–12) | 1/650 (2; 1–11) |
| Grade 2 | 335/13,640 (25; 15–42) | 250/10,040 (25; 18–35) | 6/1,330 (5; 2–9) | 2/1,110 (2; 1–6) |
| Grade 3 | 316/10,690 (30; 20–43) | 228/10,260 (22; 15–32) | 6/1,500 (4; 2–7) | 4/1,040 (4; 2–8) |
| Grade 4 | 267/8,190 (33; 24–44) | 222/8,830 (25; 20–31) | 10/1,430 (7; 3–14) | 4/1,070 (4; 1–10) |
| Grade 5 | 188/8,450 (22; 10–50) | 180/7,180 (25; 19–33) | 12/1,050 (11; 8–17) | 3/910 (3; 1–10) |
| According to wealth status (household)† | ||||
| Poorest | 51/2,140 (24; 14–41) | 20/1,320 (15; 8–29) | 0/240 (0) | 0/110 (0) |
| Below middle | 35/1,510 (23; 14–38) | 24/1,230 (20; 11–34) | 0/150 (0) | 0/120 (0) |
| Middle | 55/1,820 (30; 14–67) | 34/1,250 (27; 19–39) | 2/300 (7; 2–23) | 0/130 (0) |
| Upper middle | 50/1,870 (27; 13–55) | 22/1,300 (17; 9–34) | 1/290 (3; 1–24) | 1/120 (8; 1–58) |
| Rich | 41/1,380 (30; 19–47) | 35/1,780 (20; 13–30) | 3/190 (16; 6–44) | 1/210 (5; 1–27) |
| According to cooking fuel at household† | ||||
| Wood/kerosene/charcoal | 15/590 (25; 15–44) | 16/880 (18; 9–38) | 0/70 (0) | 0/50 (0) |
| Gas/electricity | 217/8,130 (27; 15–46) | 119/6,000 (20; 15–26) | 6/1,100 (5; 3–11) | 2/640 (3; 1–11) |
IR = incidence rate; ILI = influenza-like illness; T = total student-week; n = total episodes of ILI/influenza positive.
* Information missing for 30 children (28 children in the control schools and two children in the intervention schools).
† Only 15% of children were surveyed at the household level.
Table 5.
Incidence rate ratio (IRR) of ILI and laboratory-confirmed influenza among students in intervention and control schools
| Outcome | IR per 1,000 student-weeks | IRR (95% CI) | P-value | AIRR* (95% CI) | P-value | |
|---|---|---|---|---|---|---|
| Intervention | Control | |||||
| ILI | 22 | 27 | 0.8 (0.5, 1.3) | 0.4 | 0.8 (0.5, 1.3) | 0.4 |
| Laboratory-confirmed influenza | 3 | 6 | 0.5 (0.3, 0.8) | 0.01 | N/A | – |
AIRR = adjusted incidence rate ratio; ILI = influenza-like illness; IR = incidence rate; N/A = not applicable. Note: We did not find any factors that were statistically significant for laboratory-confirmed influenza in univariate analyses.
* Adjusted for gender.
Among students meeting the ILI case definition, 1,197 (total: 45%, intervention group: 45%, and control group: 44%) were tested for influenza viruses. Because of resource constraint, we were not able to test all samples. Among the children who were tested for influenza viruses, the incidence of influenza virus infection was lower in the intervention schools (3.0 per 1,000 student-weeks) than in the control schools (6.2 per 1,000 student-weeks) (Table 4). We did not identify any students with multiple influenza virus infections during the study period. The incidence per 1,000 student-weeks of laboratory-confirmed influenza among children in the intervention schools was 53% lower than the incidence among children in the control schools, and the difference was statistically significant (IRR: 0.5, 95% CI = 0.3, 0.8; P-value = 0.01) (Table5).
DISCUSSION
This study suggests that the respiratory hygiene intervention that included cough etiquette and proper use of hand sanitizer with hygiene education regarding when and how to use hand sanitizer was associated with a reduction in laboratory-confirmed influenza among schoolchildren in urban Bangladesh. However, the study did not find an effect of these interventions on the ILI incidence.
Our study findings are consistent with previous studies where intensive use of hand sanitizer with hygiene education was successful in reducing respiratory illnesses caused by influenza and diarrheal disease among schoolchildren in other settings.30,36–40 Our study found a 53% reduction in the incidence of influenza virus infections among children who received hand sanitizer along with respiratory hygiene education. This finding was similar to the 52% reduction in influenza A virus infections found in a study conducted among elementary schoolchildren in Pittsburgh that used hand sanitizer and cough hygiene40 and to a study conducted in Egypt that found a 47% reduction in laboratory-confirmed influenza virus infections among schoolchildren using soap and water.21 A meta-analysis suggests that handwashing alone confers no benefit for preventing influenza, but a combination of hand hygiene with face masks was found to have statistically significant efficacy against laboratory-confirmed influenza although it might not have focused exclusively on schools.41 Therefore, it is possible that we found a significant difference in the incidence of laboratory-confirmed influenza between groups because the intervention was a combination of hand sanitizer use and respiratory hygiene.
Increased handwashing practices among primary school students over the study time period and high uptake of hand sanitizer use in the intervention schools in our study indicate that hand sanitizer intervention with hygiene messages was acceptable to and feasible for schoolchildren. However, we were not able to assess whether the hand and respiratory hygiene program would be sustainable or could continue without donor support. Although providing all schools in Bangladesh with an adequate supply of hand sanitizer would be difficult, such an intervention could reduce the economic loss associated with influenza illnesses. Bhuiyan et al.42 reported that influenza-associated illness caused an estimated 169 million dollars of economic loss in 2010 in Bangladesh. Furthermore, because we integrated our hygiene messages into the regular school hygiene curriculum and trained teachers to teach behavior change communication sessions, we believe the intervention implementation approach could be sustainable, as teachers within schools directly communicate respiratory hygiene messages regularly to the students. However, continuations of the interventions require periodic training of teachers to remind them of the intervention messages and to train new teachers.
Previous studies have shown that schoolchildren have a tendency to adopt new health behaviors into their daily life following educational campaigns at school.15 Hand hygiene programs including health education and use of hand sanitizer in the classroom have been found to be cost-effective. Specifically, there was cost savings associated with a reduction in absenteeism in a previously reported randomized control trial.43 In an effort to make our intervention more sustainable, we used locally sourced hand sanitizer, which may reduce the cost to maintain this intervention. Although the cost of the intervention per day per child is minimal, maintaining this type of intervention remains a challenge for schools in Bangladesh, especially government schools, where there is no separate budgetary allocation for operation and maintenance of the school sanitation and hand hygiene from the Ministry of Education. Only a small amount of funding is allocated for schools from the local government, and schools do not receive these funds on a regular basis. Future prevention efforts could explore the feasibility of including hand sanitizer with hygiene messages in the overall influenza prevention strategy in Bangladesh.
There are several important limitations in this study. First, the study team, schoolchildren, their parents, and teachers were not blinded to the intervention. It is, therefore, possible that underreporting of illness in the intervention schools may have contributed to information bias. However, regular school visits, monitoring by the principal investigator or field supervisors, the use of a standardized case definition to identify illness, and equal proportion of ILI cases that were assessed for influenza may have reduced possible information and reporting bias. Although it is not possible to confirm that respiratory illnesses were not missed, the proportion of respiratory specimens testing positive for influenza viruses was consistent with routine surveillance during this period in Bangladesh. A second limitation was the use of an observer in the classroom that may have influenced student behavior.44 Observed handwashing may have increased more in intervention schools than in control schools, as the children in the intervention schools knew they were supposed to be washing their hands, whereas the children in the control schools might not have. The children may also have been more likely to use the hand sanitizer while being observed. The observed proportion of handwashing with soap or sanitizer in this study should therefore be interpreted as the upper limit of handwashing. Moreover, the impact on the objective outcome suggests that the intervention did have some impact of handwashing behavior. A third limitation is that we do not know how much of the benefit may have been due to the altered coughing or sneezing behavior and how much was due to improved hand hygiene. Because we evaluated a combined intervention, we cannot evaluate their separate effects. Because the behavior change intervention related to proper respiratory hygiene would not require ongoing financial support for purchasing sanitizer, further studies might explore evaluating respiratory hygiene messaging alone. Another limitation is the short duration of observation (a total of 10 weeks of observation), which may have led to an underestimation of the intervention effect because of the weeks required for students to adopt a new habit or an overestimation because if continued, the practices might wane. To monitor for true behavior change, period observations would need to be conducted among the children and the schools that were part of this study. In addition, for some of our interventions, continued availability of hand sanitizer would be required for sustained handwashing behavior change. Moreover, the disruption to ILI surveillance during the school break is another limitation, as this period typically coincides with peak influenza circulation activity. This may have resulted in underestimation of the occurrence of influenza virus infections and limited our ability to fully evaluate the effectiveness of our interventions as there was a 6-week lapse in intervention messaging. However, we evaluated school-level intervention, and given the short incubation period of influenza viruses, we likely did not miss many infections that occurred just before the school break. Last, schools in Dhaka may not be representative of all schools across Bangladesh or schools in other countries, as schools in Dhaka are comparatively more crowded than those in rural areas. However, the participating schools are representative of most schools in Dhaka regarding infrastructures, the number of student per schools, and handwashing facilities available at schools.29
Despite the study limitations, our findings suggest that hand sanitizer can be used as an alternative hygiene method to soap and water for handwashing and hygiene in school settings to reduce the incidence of influenza virus infection, especially in low-resource settings, as soap and water are not typically available in schools. In Bangladesh, where there is no annual vaccination policy for seasonal influenza, the use of hand sanitizer in combination with hand and respiratory hygiene education could play an important role in the prevention of influenza virus infections among at-risk schoolchildren. Hand sanitizer may help to reduce the burden of influenza in low-income countries, particularly in a setting where water is scarce. Schoolchildren are likely important for community transmission of influenza, so considering the possible secondary benefits of preventing influenza among schoolchildren, this set of interventions could be cost-effective. Further studies are needed to understand the sustainability and cost of these interventions.
Supplemental appendix
Acknowledgment:
We acknowledge the Department of Primary Education, Ministry of Primary and Mass Education, Government of Bangladesh, for their support to implement this project. We are grateful to the school management committee, schoolteachers, schoolchildren and their parents, and the field team for their support and valuable contribution to facilitate the project-related activities. International Center for Diarrheal Disease Research, Bangladesh is thankful to the Government of Bangladesh, Canada, Sweden, and the United Kingdom for providing core/unrestricted support. icddr,b also acknowledges with gratitude the commitment of CDC to its research efforts.
Note: Supplemental appendix appear at www.ajtmh.org.
REFERENCES
- 1.Iuliano AD, et al. 2018. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet 391: 1285–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brooks WA, et al. 2010. Influenza is a major contributor to childhood pneumonia in a tropical developing country. Pediatr Infect Dis J 29: 216–221. [DOI] [PubMed] [Google Scholar]
- 3.Nair H, et al. 2011. Global burden of respiratory infections due to seasonal influenza in young children: a systematic review and meta-analysis. Lancet 378: 1917–1930. [DOI] [PubMed] [Google Scholar]
- 4.Homaira N, et al. 2012. Incidence of respiratory virus-associated pneumonia in urban poor young children of Dhaka, Bangladesh, 2009–2011. PLoS One 7: e32056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmed M, et al. 2018. Estimates of seasonal influenza‐associated mortality in Bangladesh, 2010–2012. Influenza Other Respir Viruses 12: 65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heikkinen T, 2006. Influenza in children. Acta Paediatr 95: 778–784. [DOI] [PubMed] [Google Scholar]
- 7.Glezen WP, 2006. Herd protection against influenza. J Clin Virol 37: 237–243. [DOI] [PubMed] [Google Scholar]
- 8.Glezen WP, 1996. Emerging infections: pandemic influenza. Epidemiol Rev 18: 64–76. [DOI] [PubMed] [Google Scholar]
- 9.Fujii H, Takahashi H, Ohyama T, Hattori K, Suzuki S, 2002. Evaluation of the school health surveillance system for influenza, Tokyo, 1999–2000. Jpn J Infect Dis 55: 97–99. [PubMed] [Google Scholar]
- 10.Haque F, et al. 2017. Influenza B virus outbreak at a religious residential school for boys in northern Bangladesh, 2011. Influenza Other Respir Viruses 11: 165–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neuzil KM, Hohlbein C, Zhu Y, 2002. Illness among schoolchildren during influenza season: effect on school absenteeism, parental absenteeism from work, and secondary illness in families. Arch Pediatr Adolesc Med 156: 986–991. [DOI] [PubMed] [Google Scholar]
- 12.Bridges CB, Kuehnert MJ, Hall CB, 2003. Transmission of influenza: implications for control in health care settings. Clin Infect Dis 37: 1094–1101. [DOI] [PubMed] [Google Scholar]
- 13.Luby SP, Brooks WA, Zaman K, Hossain S, Ahmed T, 2008. Infectious diseases and vaccine sciences: strategic directions. J Health Popul Nutr 26: 295–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saunders-Hastings P, Crispo JAG, Sikora L, Krewski D, 2017. Effectiveness of personal protective measures in reducing pandemic influenza transmission: a systematic review and meta-analysis. Epidemics 20: 1–20. [DOI] [PubMed] [Google Scholar]
- 15.Bowen A, Ma H, Ou J, Billhimer W, Long T, Mintz E, Hoekstra RM, Luby S, 2007. A cluster-randomized controlled trial evaluating the effect of a handwashing-promotion program in Chinese primary schools. Am J Trop Med Hyg 76: 1166–1173. [PubMed] [Google Scholar]
- 16.Freeman MC, Greene LE, Dreibelbis R, Saboori S, Muga R, Brumback B, Rheingans R, 2012. Assessing the impact of a school-based water treatment, hygiene and sanitation programme on pupil absence in Nyanza Province, Kenya: a cluster-randomized trial. Trop Med Int Health 17: 380–391. [DOI] [PubMed] [Google Scholar]
- 17.Lopez-Quintero C, Freeman P, Neumark Y, 2009. Hand washing among school children in Bogota, Colombia. Am J Public Health 99: 94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nicholson JA, Naeeni M, Hoptroff M, Matheson JR, Roberts AJ, Taylor D, Sidibe M, Weir AJ, Damle SG, Wright RL, 2014. An investigation of the effects of a hand washing intervention on health outcomes and school absence using a randomised trial in Indian urban communities. Trop Med Int Health 19: 284–292. [DOI] [PubMed] [Google Scholar]
- 19.Rabie T, Curtis V, 2006. Handwashing and risk of respiratory infections: a quantitative systematic review. Trop Med Int Health 11: 258–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luby SP, Agboatwalla M, Feikin DR, Painter J, Billhimer W, Altaf A, Hoekstra RM, 2005. Effect of handwashing on child health: a randomised controlled trial. Lancet 366: 225–233. [DOI] [PubMed] [Google Scholar]
- 21.Talaat M, Afifi S, Dueger E, El-Ashry N, Marfin A, Kandeel A, Mohareb E, El-Sayed N, 2011. Effects of hand hygiene campaigns on incidence of laboratory-confirmed influenza and absenteeism in schoolchildren, Cairo, Egypt. Emerg Infect Dis 17: 619–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nasreen S, Azziz‐Baumgartner E, Gurley ES, Winch PJ, Unicomb L, Sharker MA, Southern D, Luby SP, 2010. Prevalent high‐risk respiratory hygiene practices in urban and rural Bangladesh. Trop Med Int Health 15: 762–771. [DOI] [PubMed] [Google Scholar]
- 23.Nizame FA, Nasreen S, Unicomb L, Southern D, Gurley ES, Arman S, Kadir MA, Azziz-Baumgartner E, Luby SP, Winch PJ, 2011. Understanding community perceptions, social norms and current practice related to respiratory infection in Bangladesh during 2009: a qualitative formative study. BMC Public Health 11: 901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tellier R, 2006. Review of aerosol transmission of influenza A virus. Emerg Infect Dis 12: 1657–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sultana F, Nizame FA, Southern DL, Unicomb L, Winch PJ, Luby SP, 2017. Pilot of an elementary school cough etiquette intervention: acceptability, feasibility, and potential for sustainability. Am J Trop Med Hyg 97: 1876–1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dreibelbis R, Kroeger A, Hossain K, Venkatesh M, Ram PK, 2016. Behavior change without behavior change communication: nudging handwashing among primary school students in Bangladesh. Int J Environ Res Public Health 13: E129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grover E, Hossain MK, Uddin S, Venkatesh M, Ram PK, Dreibelbis R, 2018. Comparing the behavioural impact of a nudge‐based handwashing intervention to high‐intensity hygiene education: a cluster‐randomised trial in rural Bangladesh. Trop Med Int Health 23: 10–25. [DOI] [PubMed] [Google Scholar]
- 28.WHO , 2008. World Health Statistics 2008. Geneva, Switzerland: World Health Organization Press; Available at: https://www.who.int/whosis/whostat/2008/en/. Accessed October 23, 2019. [Google Scholar]
- 29.WaterAid Unit BPS, International Centre for Diarrhoeal Disease Research B , 2014. Bangladesh National Hygiene Baseline Survey: Preliminary Report. Available at: https://washmatters.wateraid.org/publications/bangladesh-national-hygiene-baseline-survey-preliminary-report-2014. Accessed October 23, 2019. [Google Scholar]
- 30.White CG, Shinder FS, Shinder AL, Dyer DL, 2001. Reduction of illness absenteeism in elementary schools using an alcohol-free instant hand sanitizer. J Sch Nurs 17: 248–265. [PubMed] [Google Scholar]
- 31.Pickering AJ, Boehm AB, Mwanjali M, Davis J, 2010. Efficacy of waterless hand hygiene compared with handwashing with soap: a field study in Dar es Salaam, Tanzania. Am J Trop Med Hyg 82: 270–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gordon A, Ortega O, Kuan G, Reingold A, Saborio S, Balmaseda A, Harris E, 2009. Prevalence and seasonality of influenza-like illness in children, Nicaragua, 2005–2007. Emerg Infect Dis 15: 408–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hayes RJ, Bennett S, 1999. Simple sample size calculation for cluster-randomized trials. Int J Epidemiol 28: 319–326. [DOI] [PubMed] [Google Scholar]
- 34.Erdman DD, Weinberg GA, Edwards KM, Walker FJ, Anderson BC, Winter J, González M, Anderson LJ, 2003. GeneScan reverse transcription-PCR assay for detection of six common respiratory viruses in young children hospitalized with acute respiratory illness. J Clin Microbiol 41: 4298–4303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.WHO , 2011. Manual for the Laboratory Diagnosis and Virological Surveillance of Influenza. Geneva, Switzerland: WHO Press. Available at: https://www.who.int/influenza/gisrs_laboratory/manual_diagnosis_surveillance_influenza/en/. Accessed October 23, 2019. [Google Scholar]
- 36.Correa JC, Pinto D, Salas LA, Camacho JC, Rondón M, Quintero J, 2012. A cluster-randomized controlled trial of handrubs for prevention of infectious diseases among children in Colombia. Rev Panam Salud Publica 31: 476–484. [DOI] [PubMed] [Google Scholar]
- 37.Morton JL, Schultz AA, 2004. Healthy hands: use of alcohol gel as an adjunct to handwashing in elementary school children. J Sch Nurs 20: 161–167. [DOI] [PubMed] [Google Scholar]
- 38.Pandejpong D, Danchaivijitr S, Vanprapa N, Pandejpong T, Cook EF, 2012. Appropriate time-interval application of alcohol hand gel on reducing influenza-like illness among preschool children: a randomized, controlled trial. Am J Infect Control 40: 507–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pickering AJ, Davis J, Blum AG, Scalmanini J, Oyier B, Okoth G, Breiman RF, Ram PK, 2013. Access to waterless hand sanitizer improves student hand hygiene behavior in primary schools in Nairobi, Kenya. Am J Trop Med Hyg 89: 411–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stebbins S, et al. 2011. Reduction in the incidence of influenza A but not influenza B associated with use of hand sanitizer and cough hygiene in schools: a randomized controlled trial. Pediatr Infect Dis J 30: 921–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wong VW, Cowling BJ, Aiello AE, 2014. Hand hygiene and risk of influenza virus infections in the community: a systematic review and meta-analysis. Epidemiol Infect 142: 922–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bhuiyan MU, et al. 2014. Economic burden of influenza‐associated hospitalizations and outpatient visits in Bangladesh during 2010. Influenza Other Respir Viruses 8: 406–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guinan M, McGuckin M, Ali Y, 2002. The effect of a comprehensive handwashing program on absenteeism in elementary schools. Am J Infect Control 30: 217–220. [DOI] [PubMed] [Google Scholar]
- 44.Ram PK, et al. 2010. Is structured observation a valid technique to measure handwashing behavior? Use of acceleration sensors embedded in soap to assess reactivity to structured observation. Am J Trop Med Hyg 83: 1070–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.