Abstract
Background:
Women are at risk for mood disturbance during treatment for breast cancer.
Objective:
To identify classes of women experiencing similar trajectories of depressed mood and anxiety while receiving chemotherapy for breast cancer and to determine associated antecedents and outcomes. The specific aims were to (1) determine the distinct trajectory classes associated with severity of depressed mood and anxiety reported by women undergoing cycles 2 and 3 of chemotherapy for breast cancer, (2) determine if class membership is associated with various antecedent variables, (3) determine if class membership is associated with days of missed work and hours spent lying down.
Methods:
In a secondary analysis, classes were identified using Latent Growth Mixture Modeling (LGMM). Antecedents and outcomes related to class membership were explored.
Results:
Participants (n=166, mean age 53 years, S.D.±10.8) were mostly Caucasian (91.46%); half with early stage disease. Two trajectories of depressed mood and anxiety were identified. Receipt of Doxorubicin was associated with the higher severity class for depressed mood (p < .01) and anxiety (p = .04). No college education (p =.03) or spending more hours lying down (p =.03) was associated with the higher severity class for anxiety.
Conclusions:
Distinct trajectories of mood disturbance are distinguished by baseline severity. Further study is needed to determine if biologic or genomic factors are associated with class membership.
Implications for Practice: Identification of women at risk for mood disturbance may allow clinicians to intensify symptom management. Mood disturbance early in the treatment trajectory warrants management to improve outcomes.
Introduction
There is a high prevalence of depression (24–54%) and anxiety (6–74%) in women receiving chemotherapy for breast cancer.1–5 Symptoms of depression and anxiety are more common in oncology patients than in the general population and are often referred to jointly as psychological distress.6 Mood disturbance may be related to worries about disease progression, changes in functional ability, and concerns about the future and may include feeling sadness or feeling down, changeable emotions, lack of interest, feelings of hopelessness, or excessive worry.2,7 Chemotherapy may reduce ability to function both physically and cognitively, leading to increased psychological distress.2 Additionally, mood disturbance is associated with shorter recurrence-free periods and overall survival.7 Worth noting is evidence that mood disturbance in oncology patients may result in treatment non-adherence, increased hospitalization, impaired quality of life, poor prognosis, and increased mortality.6,8,9
Treatment-related symptoms during chemotherapy for breast cancer are associated with long-term outcomes relative to adherence, functional status, employment and mortality. As such, identification of those at risk for mood disturbance during chemotherapy treatment for breast cancer is important.6,8,9 Identifying distinct patterns of mood disturbance and correlates of those patterns may allow for targeted symptom management and reduction in poor outcome. Eight reported studies have included subgroup analyses of classes of women with breast cancer experiencing similar trajectories of mood disturbance and potential correlates of class membership.10–17 These reports have described 3–5 classes with distinct trajectories of mood disturbance across various time-points in the breast cancer trajectory. Potential correlates of class membership include quality of life, younger age, treatment modality, employment, education, and social support.10–17 Importantly, while longitudinal in design, each of these studies evaluated symptoms of psychological distress and correlates at specific time-points, ranging from 3–7 times over 6–55 months, but did not examine patterns throughout chemotherapy treatment.
Evaluating the temporal aspect, antecedents, and consequences of the symptom trajectory is challenging, but important, as changes occur in symptom severity over time.18 The purpose of this study was to identify distinct patterns of depressed mood and anxiety in women receiving chemotherapy for breast cancer and to determine if antecedents and outcomes are associated with class membership. The specific aims were to (1) determine the distinct trajectory classes associated with severity of depressed mood and anxiety reported by women undergoing cycles 2 and 3 of chemotherapy for breast cancer, (2) determine if class membership is associated with various antecedents variables, (3) determine if class membership is associated with days of missed work and hours spent lying down.
This study was framed by the Dynamic Symptoms Model which describes the complex nature and longitudinal trajectory of the symptom experience, incorporating patterns of symptom change over time, as well as antecedents and consequences to those patterns.18,19 Consistent with the model, the current study includes potential antecedents to the symptom trajectory (demographic and clinical variables), growth parameters of the symptom trajectory, and potential consequences of the symptom trajectory (days of missed work and hours spent lying down). Framed within this model, the analysis described here describes the longitudinal trajectory of the symptoms of depressed mood and anxiety during chemotherapy and the relationships between the symptom trajectory and potential antecedents and consequences.
Methods
Participants and Setting
Data from 3 longitudinal studies that utilized the automated telephone system for data collection were used in this secondary analysis.20,21
Study 1
Study 1 was a randomized clinical trial testing the automated system for monitoring and managing symptoms during chemotherapy.20 Participants in Study 1 were recruited from Cancer Centers of the Carolinas in Greenville, South Carolina, and Intermountain Hematology/Oncology Associates, Wasatch Hematology/Oncology Associates, and Huntsman Cancer Institute, all in Salt Lake City, Utah. All participants, regardless of group assignment, were instructed to participate in a daily phone call with the automated system, where they were asked to report on the severity of and distress associated with 10 symptoms, including depressed mood and anxiety. For the experimental group, 2 thresholds were set to alert the participant’s healthcare provider and team, either an alert when a symptom was rated as greater than or equal to 5 or 7 (depending on the symptom) and trend alerts based on a pattern of moderate to severe levels reported over three out of the past 7 days. The control group used the same automated system to report on the presence of symptoms and rated those symptoms in the same manner as the experimental group. No provider alerts were generated for the control group, although participants in both groups were advised to notify their provider for any concerns about their symptoms. There was no effect for the main hypothesis that the experimental group would have less symptom severity, symptom distress, and symptom interference with normal activities when compared to the control group. Therefore, data from all participants in Study 1 with a breast cancer diagnosis, regardless of study group, were utilized in this secondary analysis.
Study 2
The purpose of Study 2 was to test the efficacy of the automated telephone system combined with self-care strategies and Nurse Practitioner delivered, guideline-based symptom care in decreasing symptom severity and distress and interference with functional performance.21 Participants in Study 2 were recruited from Huntsman Cancer Institute and Vanderbilt University Medical Center in Nashville, Tennessee. Participants were randomized to an experimental intervention group or a control group. All participants completed a daily call with the automated telephone system, the same system used in Study 1, expanded to include 4 new components. First, participants were asked to report on the presence of 11 symptoms, including depressed mood and anxiety. For all symptoms, when present, participants were asked to rate the severity of and distress associated with the symptoms on a Likert scale (0–10). Additionally, the Study 2 experimental participants were given self-care symptom management suggestions by the automated system, automated provider alerts for uncontrolled symptoms, and unrelieved symptoms at moderate or greater levels generated an alert to the study Nurse Practitioner who initiated follow-up care. Participants in the usual care group were not given self-care strategies nor had unrelieved symptoms alerted to their provider or managed by the study Nurse Practitioner, but were reminded to call their healthcare provider for symptom concerns. Differences in reported symptoms between the groups were found, with a potential main effect of the intervention on symptom severity, distress, or interference with functional performance. For that purpose, only data collected from participants randomized to the control group were utilized in this secondary analysis.
Study 3
Study 3 was an observational study using the same automated system for symptom data collection and involved no intervention or usual care group assignment. All participants completed a daily call with the automated telephone system, the same system used in Study 1. Participants were asked to report on the severity of and distress associated with 11 symptoms, including depressed mood and anxiety. Participants in Study 3 were recruited from Huntsman Cancer Institute.
Sample
Eligibility requirements for inclusion in this secondary analysis included (1) being a woman diagnosed with breast cancer, (2) beginning initial treatment with chemotherapy, and (3) with completed study measures through cycle 2 and cycle 3. All data from eligible participants in Study 1 and Study 3 and those in the usual care group in Study 2 were included in this secondary analysis.
The sampling frame consisted of 259 women pooled from the 3 parent studies. Of these, 80 women who were randomized to the intervention group for Study 2 were excluded. In addition, 13 women who did not complete study measures through cycles 2 and 3 were excluded. A total sample of 166 women completed study measures through cycles 2 (n=165) and 3 (n=155) on at least 3 days were included in this secondary analysis. To account for varying cycle lengths, only data from the first 14 days of each cycle were included.
Measures
All parent studies utilized similar instrumentation. Demographic and disease-related data were collected at baseline and included age, sex, race/ethnicity, employment status, education, extent of disease and details of the chemotherapy protocol. Daily symptom data were collected using the automated telephone system. Single-item indicators were used to assess each symptom, which have established and acceptable reliability and validity.22–24 Conditional branching was used, where participants were asked during a daily automated phone call beginning with the first day of the chemotherapy cycle, “During the past 24 hours did you experience depressed mood (or anxiety)?” A no response was scored as zero and a yes response elicited further questioning using a 1 to 10 Likert scale for the severity of that particular symptom. Daily hours spent lying down and whether or not employed participants were able to attend work were collected daily using the same automated system.
Study Procedures
This study was reviewed by Institutional Review Board (IRB) at the University of Utah. All participants signed a written, informed consent upon enrollment in the parent studies which were approved by IRBs at each participating institution.
Statistical Analysis
The Software Statistical Package for the Social Sciences (SPSS), version 23.0 was used for data management and analysis. P values less than .05 were considered statistically significant and because this was a hypothesis-generating study, there was no adjustment for multiplicity.
Descriptive statistics were generated on the sample characteristics. The prevalence of individual symptoms during the first 14 days of each cycle was determined and described. The percent of days depressed mood and anxiety were reported with severity of zero, severity of 1–10, and severity of 4–10 (moderate to severe levels) was determined.25 Cycles were studied individually to capture potential differences in the symptom trajectories of consecutive cycles.
Aim 1. To determine the distinct trajectory classes associated with severity of depressed mood and anxiety reported by women undergoing cycles 2 and 3 of chemotherapy for breast cancer.
Latent Growth Mixture Modeling (LGMM) was used to identify classes that display homogenous trajectories of depressed mood and anxiety in each cycle, separately. An initial 1-class model was tested, and subsequent classes were added in ascending order to determine the best model fit. Step-wise models were evaluated on multiple fit criteria, including the Bayesian Information Criterion (BIC) and entropy. Smaller BIC values and entropy values closer to 1.0 suggested a better model fit.26,27 The best-fitting model was examined for the percent of the sample in each class (greater than 5%) and inspected graphically to determine if the predicted trajectories were theoretically relevant.
Using the models for depressed mood and anxiety, the model-predicted class membership was obtained for each individual on each symptom during each cycle using posterior probabilities. While there is uncertainty in predicted class membership, the entropy and posterior probabilities as previously reported for our models suggest a strong model fit and predicted class membership was treated as an observed variable for the purposes of this analysis.28 Class membership assignment was used to test for differences across the classes on antecedents and outcomes. Fisher’s exact chi-square was used to account for small cell sizes. In cases where classes did not display homogeneity of variance, the Welch statistic was used. LGMM can accommodate data in which the number and timing of observations vary among patients.
Aim 2. To determine if class membership is associated with various antecedents variables, including demographic and clinical characteristics.
After establishing the classes for the severity of each symptom, age, stage of disease, education, employment, marital status, and chemotherapy regimen were compared to class membership for depressed mood and anxiety using chi-square and independent-samples t tests. Given the large diversity of chemotherapy regimens and the sample size, it was not statistically possible to interpret comparison between the individual regimens. Instead, tests were conducted on 2 agents of interest, whether or not women received Doxorubicin or a Taxane as part of their regimen.
Aim 3. To determine if class membership is associated with days of missed work and hours spent lying down.
Daily measures of hours spent lying down were averaged for each individual for each cycle 2 and 3. Days of missed work were summed for all employed participants for each cycle 2 and 3. To answer this aim, differences across the classes were explored using independent-samples t tests. Only employed participants were included in the analysis for days missed work.
Results
Sample demographic and clinical characteristics for the 166 women included in this secondary analysis have been previously reported.29 Participants ranged in age from 24 to 80 years (mean age = 52.91, SD = 10.8). Most women were White (91.46%), married (75%), and not currently working (62.8%). The majority of the sample had some education beyond high school (75.3%) and 40.36% were diagnosed with Stage II breast cancer. Participants received over 12 regimens of chemotherapy, with 50.0% receiving a regimen including Doxorubicin and 28.9% receiving a regimen including a Taxane.
The prevalence of depressed mood and anxiety and the percent of days reported with severity of zero, severity of 1–10, and severity of 4–10 (moderate to severe levels) are presented in Table 1. Sixty percent of women reported depressed mood during cycle 2 and 53.2% of women reported depressed mood during cycle 3 at a severity greater than zero at least one time. During cycle 2, 46.7% of women reported anxiety and 39.7% of women reported anxiety during cycle 3 at a severity greater than zero at least one time. During cycle 2, 42.2% of women reported moderate to severe levels (severity 4–10) of depressed mood and 35.3% of women reported moderate to severe levels (severity 4–10) of depressed mood during cycle 3 at least one time. During cycle 2, 28.5% of women and during cycle 3, 25.6% of women reported moderate to severe levels (severity 4–10) of anxiety at least one time.
Table 1.
Symptom Prevalence and Mean Number of Days at Moderate to Severe Levels
| Symptom | Cycle | No. (%) of Women Reported Symptom Severity Greater than 0 at Least Once |
Mean no. Days (SD), Range of Symptom Reported with Severity Greater than 0 |
No. (%) of Women Reported Symptom Severity Greater than 3 at Least Once |
Mean no. Days (SD), Range of Symptom Reported with Severity Greater than 3 |
No. Days (%) Symptom Reported Level 0 |
No. Days (%) Symptom Reported Level 1–10 |
No. Days (%) Symptom Reported Level 4–10 |
|---|---|---|---|---|---|---|---|---|
| Depressed Mood a | 2 | 99 (60.0%) | 3.60 (3.21), 1–13 | 70 (42.4%) | 3.23 (2.84), 1–12 | 1455 (80.3%) | 356 (19.7%) | 226 (12.5%) |
| 3 | 83 (53.2%) | 3.47 (3.11), 1–14 | 55 (35.3%) | 2.87 (2.86), 1–13 | 1416 (83.1%) | 288 (16.9%) | 158 (9.3%) | |
| Anxiety a | 2 | 77 (46.7%) | 3.34 (3.17), 1–13 | 47 (28.5%) | 2.91 (2.83), 1–11 | 1544 (85.3%) | 267 (14.7%) | 147 (8.2%) |
| 3 | 62 (39.7%) | 3.56 (3.62), 1–13 | 40 (25.6%) | 2.65 (2.56), 1–9 | 1483 (87.0%) | 221 (13.0%) | 106 (6.2%) |
n=165, cycle 2; n=156, cycle 3; 1811(78.4%) days reported cycle 2, 1704(78.0%) days reported cycle 3; 499(21.6%) days missing cycle 2, 480(22.0%) days missing cycle 3
Aim 1. To determine the distinct trajectory classes associated with severity of depressed mood and anxiety reported by women undergoing cycles 2 and 3 of chemotherapy for breast cancer.
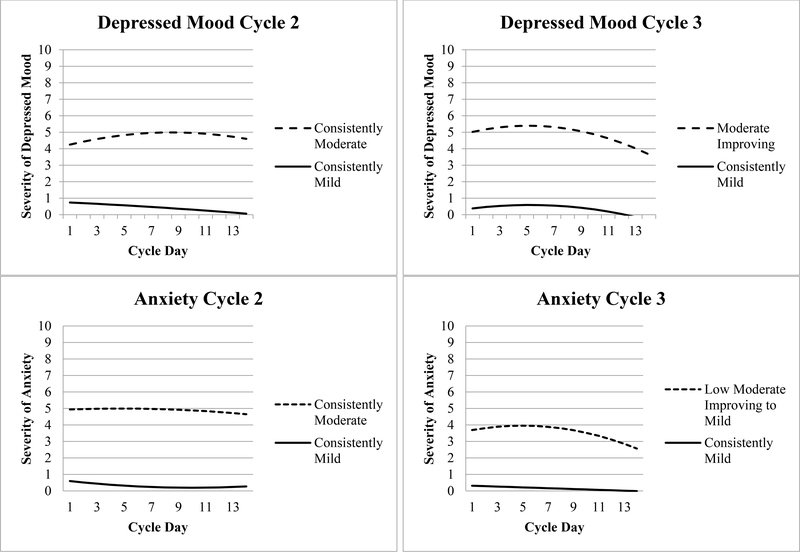
Multiclass latent growth mixture models were evaluated for both symptoms and fit indices are presented in Table 2. Growth factors for the classes are presented in Table 3 and trajectory graphs are presented in the Figure. The severity of depressed mood and anxiety reported in the trajectory models were described using common category nomenclature for symptom severity, none (0), mild (1–3), moderate (4–7), and severe (7–10) derived from commonly used National Comprehensive Cancer Network (NCCN) guidelines.25 Two distinct trajectories classes were identified for depressed mood and anxiety during each cycle but the nature of the trajectories varied from cycle 2 to 3. The majority of participants were in the consistently mild depressed mood class (91% in cycle 2; 94% in cycle 3) with a low depressed mood on day 1 (0.78 ± 0.16; 0.27 ± 0.09) which maintained over the first 14 days of both cycles. Nine percent of women during cycle 2 were in the consistently moderate depressed mood class and reported moderate severity on day 1 (4.04 ± 0.76), which maintained over the first 14 days of both cycles. During cycle 3, 6% of women were in the moderate improving depressed mood class and reported moderate severity on day 1 (4.82 ± 0.63), which improved slightly over the cycle.
Table 2.
Model Fit for Latent Growth Mixture Models
| Modela | Log Likelihood | BICb | Entropy | Posterior Probability | Class Proportions |
|---|---|---|---|---|---|
| Depressed Mood | |||||
| Cycle 2 | |||||
| 1 class | −3,861.42 | 7,755.71 | N/A | N/A | N/A |
| 2 class | −3,470.9 | 6,982.42 | .990 | .997, .995 | 91%, 9% |
| 3 class | −3,359.91 | 6,768.17 | .987 | .998, .992,.961 | 84%, 9%, 7% |
| Cycle 3 | |||||
| 1 class | −3,362.53 | 6,756.98 | N/A | N/A | N/A |
| 2 class | −2,827.07 | 5,792.57 | 1.000 | 1.000, 1.000 | 94%, 6% |
| 3 class | −2,782.16 | 5,611.26 | .998 | 1.000, .989, 1.000 | 94%, 5%, 2% |
| Anxiety | |||||
| Cycle 2 | |||||
| 1 class | −3,509.86 | 7,052.60 | N/A | N/A | N/A |
| 2 class | −3,029.89 | 6,100.39 | 1.000 | 1.000, 1.000 | 95%, 5% |
| 3 class | −2,918.53 | 5,887.40 | .995 | .992, 1.000 | 85%, 12%, 3% |
| Cycle 3 | |||||
| 1 class | −3,076.95 | 6,185.83 | N/A | N/A | N/A |
| 2 class | −2,621.09 | 5,281.63 | .997 | .999, 1.000 | 92%, 8% |
| 3 class | −2,552.07 | 5,151.09 | .995 | .999, .991, 1.000 | 90%, 6%, 4% |
Classes were added step-wise to the model, models were evaluated on the BIC, entropy, and examined for the number of subjects in each class and graphed visually
Bayesian Information Criterion
Table 3.
Growth Factor Means and Predicted Frequencies for Each Class
| Class | Intercept | Slope | Quadratic Term | Class Count |
|---|---|---|---|---|
| Depressed Mood | ||||
| Cycle 2 | ||||
| Consistently Mild | 0.78a | −0.04 | 0.00 | 148.50 |
| Consistently Moderate | 4.04a | 0.22 | −0.01 | 14.85 |
| Cycle 3 | ||||
| Consistently Mild | 0.27 | 0.13 | −0.01 | 155.10 |
| Moderate Improving | 4.82a | 0.23 | −0.02* | 9.90 |
| Anxiety | ||||
| Cycle 2 | ||||
| Consistently Mild | 0.69a | −0.10* | 0.01* | 156.75 |
| Consistently Moderate | 4.90a | 0.03 | 0.00 | 8.25 |
| Cycle 3 | ||||
| Consistently Mild | 0.34a | −0.03 | 0.00 | 156.75 |
| Low Moderate Improving to Mild | 3.53a | 0.17 | −0.02 | 8.25 |
p <. 05
Figure.
Individual symptom trajectory model
The majority of participants were in the consistently mild anxiety classes (95% in cycle 2; 92% in cycle 3) and reported low anxiety on cycle day 1 (0.69 ± 0.13; 0.34 ± 0.07) that remained stable over the first 14 days of both cycles. During cycle 2, 5% of women were in the consistently moderate anxiety class and reported moderate anxiety on cycle day 1 (4.92 ± 1.70) that remained stable. During cycle 3, 8% of women were in the low moderate improving to mild anxiety class and reported moderate anxiety on cycle day 1 (3.53 ± 0.61) that improved to mild levels. Women in the moderate anxiety class did report higher anxiety in cycle 2 when compared to cycle 3.
Aim 2. To determine if class membership is associated with various antecedents variables, including demographic and clinical characteristics.
Results of the tests for differences in demographic and clinical characteristics across classes are presented in Table 4 for depressed mood and Table 5 for anxiety. Only the comparison of education to class membership for anxiety during cycle 3 and the comparison of whether or not women received Doxorubicin to class membership for depressed mood and anxiety during cycle 3 were related. During cycle 3, high school graduates were more likely to be in the moderate anxiety class and those with an undergraduate degree were more likely to be in minimal anxiety class. In addition, those in the moderate severity class for both symptoms during cycle 3 were more likely to have received Doxorubicin. All respondents in the moderate severity class for depressed mood and 83.3% of respondents in the moderate class for anxiety during cycle 3 received Doxorubicin.
Table 4.
Tests of Mean Differences and Associations among Categories for Antecedents and Outcomes of Depressed Mood Class Membership
| Characteristic | Consistently Mild |
Consistently Low Moderate |
Omnibus Test | |
|---|---|---|---|---|
| Cycle 2 | ||||
| Age (in years) | 52.29 (11.01) | 50.66 (8.95) |
t(159) = 1.23, p = .27 |
|
| Education | χ2 = 0.88, p = .98 |
|||
| Less than high school | 6 (4.4%) | 0 (0.0%) | ||
| High school | 25 (18.4%) | 5 (20.8%) | ||
| Undergraduate/Technical School | 88 (64.7%) | 16 (66.7%) | ||
| Postgraduate | 17 (12.5%) | 3 (12.5%) | ||
| Marital Status | χ2 = 1.27, p = .50 |
|||
| Married | 105 (76.1%) | 16 (66.7%) | ||
| Not Married | 33 (23.9%) | 8 (33.3%) | ||
| Employment | χ2 = 1.88, p = .46 |
|||
| Employed | 54 (39.1%) | 6 (25.0%) | ||
| Not Employed | 84 (60.9%) | 18 (75.0%) | ||
| Stage | χ2 = 2.43, p = .64 |
|||
| I | 15 (11.0%) | 5 (20.8%) | ||
| II | 58 (42.6%) | 9 (37.5%) | ||
| III | 31 (22.8%) | 6 (25.0%) | ||
| IV | 32 (23.5%) | 4 (16.7%) | ||
| Doxorubicin | χ2 = 1.13, p = .34 |
|||
| Yes | 63(47.7%) | 7(35.0%) | ||
| No | 69(52.3%) | 13(65.0%) | ||
| Taxane | χ2 = .43, p = .61 |
|||
| Yes | 43(32.6%) | 8(40.0%) | ||
| No | 89(67.4%) | 12(60.0%) | ||
| Hours Spent Lying Down | 10.57 (2.63) | 10.33 (3.82) |
t(27) = 0.30, p = .77 |
|
| Days Missed Work (n=20) | 2.28 (1.81) | 4.0 (0.00) |
t(18) = 1.73, p = .21 |
|
| Cycle 3 | ||||
| Age (years) | 52.73 (10.97) | 53.56 (10.73) |
t(150) = 0.05, p = .82 |
|
| Education | χ2 = 2.01, p = .68 |
|||
| Less than high school | 5 (3.5%) | 0 (0.0%) | ||
| High School | 24 (16.9%) | 3 (33.3%) | ||
| Undergraduate/Technical School | 94 (66.2%) | 5 (55.6%) | ||
| Postgraduate | 19 (13.4%) | 1 (11.1%) | ||
| Marital Status | χ2 = 2.55, p = .32 |
|||
| Married | 109 (75.7%) | 5 (55.6%) | ||
| Not Married | 35 (24.3%) | 4 (44.4%) | ||
| Employment | χ2 = 0.78, p = 1.00 |
|||
| Employed | 57 (39.6%) | 3 (33.3%) | ||
| Not Employed | 87 (60.4%) | 6 (66.7%) | ||
| Stage | χ2 = 1.58, p = 0.84 |
|||
| I | 19 (13.3%) | 0 (0.0%) | ||
| II | 60 (42.0%) | 5 (55.6%) | ||
| III | 33 (23.2%) | 2 (22.2%) | ||
| IV | 31 (21.8%) | 2 (22.2%) | ||
| Doxorubicin | χ2 = 7.21, p < .01a |
|||
| Yes | 74(51.4%) | 8(100.0%) | ||
| No | 70(48.6%) | 0(0.0%) | ||
| Taxane | χ2 = 1.68, p = .27 |
|||
| Yes | 50 (34.7%) | 1(12.5%) | ||
| No | 94 (65.3%) | 7(87.5%) | ||
| Hours Spent Lying Down | 10.59 (2.72) | 10.24 (4.15) |
t(150) = 0.36, p = .72 |
|
| Days Missed Work (n=27) | 1.56(1.71) | 1.00(0.00) |
t(25) = 0.21, p = .65 |
|
p<.05
Table 5.
Tests of Mean Differences and Associations among Categories for Antecedents and Outcomes of Anxiety Class Membership
| Characteristic | Consistently Mild |
Consistently Moderate |
Omnibus Test | |
|---|---|---|---|---|
| Cycle 2 | ||||
| Age (in years) | 52.53 (10.72) | 59.13 (9.76) |
t(159) = 3.25, p = .07 |
|
| Education | χ2 = 6.45, p = .13 |
|||
| Less than high school | 5 (3.3%) | 1 (11.1%) | ||
| High school | 26 (17.2%) | 4 (44.4%) | ||
| Undergraduate/Technical School | 99 (65.6%) | 4 (44.4%) | ||
| Postgraduate | 21 (13.9%) | 0 (0.0%) | ||
| Marital Status | χ2 = 0.73, p = 1.00 |
|||
| Married | 114 (74.5%) | 7 (77.8%) | ||
| Not Married | 39 (25.5%) | 2 (22.2%) | ||
| Employment | χ2 = 6.76, p = .05 |
|||
| Employed | 60 (39.2%) | 0 (0.0%) | ||
| Not Employed | 93 (60.8%) | 9 (100.0%) | ||
| Stage | χ2 = 4.21, p = .36 |
|||
| I | 20 (13.2%) | 0 (0.0%) | ||
| II | 65 (43.0%) | 2 (14.3%) | ||
| III | 33 (21.9%) | 3 (21.4%) | ||
| IV | 33 (21.9%) | 9 (64.3%) | ||
| Doxorubicin | Χ2 = 1.51, p = .29 |
|||
| Yes | 76 (52.8%) | 6 (75.0%) | ||
| No | 68 (47.2%) | 2 (25.0%) | ||
| Taxane | χ2 = 0.28, p = .72 |
|||
| Yes | 49 (34.0%) | 2 (25.0%) | ||
| No | 95 (66.0%) | 6 (75.0%) | ||
| Hours Spent Lying Down |
10.41 (2.77) | 12.53 (3.03) |
t(162) = −2.21, p = .03a |
|
| Days Missed Work (n=20) |
2.45 (1.79) | 0 (0.00) | ||
| Characteristic |
Consistently Mild |
Low Moderate to Mild |
Omnibus Test | |
| Cycle 3 | ||||
| Age (years) | 52.69 (10.90) | 53.87 (8.73) |
t(150) = .13, p = .72 |
|
| Education | χ2 = 9.70, p = .03a |
|||
| Less than high school | 4 (2.9%) | 1 (7.7%) | ||
| High school | 22 (15.8%) | 5 (38.5%) | ||
| Undergraduate/Technical School | 95 (68.3%) | 5 (38.5%) | ||
| Postgraduate | 18 (12.9%) | 2 (15.4%) | ||
| Marital Status | χ2 = 3.52, p = .24 |
|||
| Married | 107 (76.4%) | 7 (53.8%) | ||
| Not Married | 33 (23.6%) | 6 (46.2%) | ||
| Employment | χ2 = 3.90, p = .15 |
|||
| Employed | 56 (39.7%) | 4 (33.3%) | ||
| Not Employed | 85 (60.3%) | 8 (66.7%) | ||
| Stage | χ2 = 2.85, p = .58 |
|||
| I | 19 (13.7%) | 0 (0.0%) | ||
| II | 60 (43.2%) | 5 (38.5%) | ||
| III | 31 (22.3%) | 4 (30.8%) | ||
| IV | 29 (20.9%) | 4 (30.8%) | ||
| Doxorubicin | χ2 = 4.53, p = .04a |
|||
| Yes | 72 (51.4%) | 10 (83.3%) | ||
| No | 68 (48.6%) | 2 (16.7%) | ||
| Taxane | χ2 = 1.67, p = .23 |
|||
| Yes | 49(35.0%) | 2(16.7%) | ||
| No | 91(65.0%) | 10(83.3%) | ||
| Hours Spent Lying Down |
10.44 (2.75) | 11.87(3.20) |
t(150) = −1.77, p = .08 |
|
| Days Missed Work (n=27) |
1.46(1.67) | 2.00(1.73) |
t(25) = 0.28 p = .60 |
|
p<.05
Aim 3. To determine if class membership is associated with days of missed work and hours spent lying down.
For both symptoms, the t-tests for both hours spent lying down and days of missed work were nonsignificant (see Tables 4 and 5), with the exception of hours spent lying down and anxiety class membership during cycle 2. Women in the moderate anxiety class reported higher daily hours spent lying down when compared to women in the minimal anxiety class during cycle 2 (p = .03*).
Discussion
The prevalence of depressed mood and anxiety was similar to previously reported findings.1–5 In our sample, it was common to report depressed mood and anxiety at a severity greater than zero at least once, but many women reported a consistently mild severity. The LGMM recovered 2 classes of depressed mood during cycle 2, including a consistently mild depressed mood class and a consistently moderate depressed mood class. Two classes of depressed mood were recovered during cycle 3, including a consistently mild depressed mood class and a moderate improving depressed mood class. While the consistently mild depressed mood class experienced a severity of less than 1 over both cycles, the moderate improving depressed mood class during cycle 2 and the moderate improving depressed mood class during cycle 3 experienced a severity of 4 or higher. During cycle 3 only, the moderate improving depressed mood reported a decrease in the severity of depressed mood as the cycle progressed, but the severity remained at moderate levels. Of importance, women in the moderate severity classes reported a baseline severity of depressed mood at a moderate level. The symptoms of mood disturbance have been reported to increase at initiation of chemotherapy, but generally remain stable during treatment.30 This suggests that women who report higher levels of depressed mood at the beginning of the cycle maintain this symptom at moderate to severe levels through the end of the cycle.
The LGMM recovered 2 classes of anxiety during both cycles, with a consistently mild anxiety class during both cycles and a consistently moderate anxiety class during cycle 2 and a low moderate improving to mild anxiety class during cycle 3. Similar to depressed mood, the moderate classes reported a severity of anxiety of greater than 3 across both cycles, with severity levels slightly higher during cycle 2 when compared to cycle 3. Only the low moderate improving to mild anxiety class reported improvement in the severity of anxiety during the first 14 days of chemotherapy.
A few recent reports of classes of trajectories of depression and psychological distress in women with breast cancer have found 4 or 5 class models as the best fit.11–15, 17 Differences in the number of trajectories identified may be due to methodological discrepancies, where, for example, Deshields et al11 used a cut-point placement based on CES-D scores at 3 time points following treatment and Dunn et al12 modeled trajectories based on CES-D scores prior to and monthly for 6 months after surgery for breast cancer. The use of the CES-D cut-points as opposed to the continuous severity single-item measure and the time points measured (every 3 months or monthly) would certainly elicit differing patterns of trajectories when compared to daily measures. Daily single-item measures may be useful for capturing the trajectory of change during a cycle of chemotherapy, while also reducing participant burden associated with multi-item symptom measures. Finally, varying analysis methods used to identify classes may have also contributed to inconsistencies in findings.
Identifying factors that contribute to symptom trajectories allows clinicians to target those at risk for increased symptom experiences during chemotherapy. Various demographic and clinical characteristics were examined as possibly distinguishers of depressed mood and anxiety class membership. None of the demographic or clinical characteristics were found to be associated with depressed mood or anxiety class membership, with the exception of education. During cycle 3, high school graduates were more likely to be in the moderate anxiety class and women with an undergraduate degree were more likely to be in the mild anxiety class. This finding, in combination with findings reported by Lam et al15 of an association between education and psychological distress trajectory, suggest that higher education may be protective against anxiety during chemotherapy treatment. While several studies have correlated younger age with increased mood disturbance, a relationship between age and trajectory class membership was not found in this sample.6,11,12,15 Importantly, during cycle 3, women in the moderate class for both depressed mood and anxiety were more likely to have received Doxorubicin as part of their chemotherapy regimen than not. While Doxorubicin did have a significant effect on mood disturbance class membership in our sample, it is unknown if that effect is dose-dependent or related to other agents received in combination with Doxorubicin, and further study is needed.
During cycle 2 only, women in the consistently moderate anxiety class reported statistically significant greater average daily hours spent lying down (mean hours = 12.53, SD = 3.03) when compared to women in the consistently mild anxiety class (mean hours = 10.41, SD = 2.77). No reports were found where differences in activity level or resting hours were compared with severity of anxiety during treatment for breast cancer and it is unknown why this difference among the classes was not found during cycle 3 in our sample.
There are a couple of possible explanations for why none of the other demographic or clinical variables were associated with class membership in this sample. First, the number of women who were classified in the moderate to severe trajectory for depressed mood (9% of respondents in cycle 2 and 6% in cycle 3) and anxiety (5% of respondents in cycle 2 and 8% of respondents in cycle 3) was low. Additionally, more than half of the women in the sample did not experience even a single day of either symptom. Henselmans et al14 also found a large group of women who experienced no mood disturbance during chemotherapy, suggesting that not all women, or even a large percentage of women, experience these symptoms. In our sample, in particular, the low class counts for the moderate trajectory classes for depressed mood and anxiety may have decreased the power and ability to detect differences among the classes on these potentially related variables. Second, class trajectories may be predicted by variables other than demographic and clinical determinants, such as genetic factors. A lack of association between demographic characteristics and symptoms may be related to a possible relationship between biologic mechanisms and genetic and epigenetic determinants with symptoms.31,32 Further study is needed to determine whether these variables may distinguish class membership for symptoms of mood disturbance.
Limitations
Limitations of this study include a lack of data for several relevant variables of interest, including history of psychological illness and comorbidities. One of the strongest correlates of symptoms of mood disturbance during cancer treatment is a history of psychological illness, poor coping, or distress prior to initiation of treatment.6 Because of the nature of our study, data for these variables were unavailable.
Our sample as limited in racial and ethnic diversity. In addition, our sample was relatively homogenous in marital status (74.1% married). It is unknown whether married women receive more support than nonmarried and potentially influenced presence of mood disturbance. Of the reviewed literature, only Helgeson et al13 reported on social support as a predictive correlate of trajectories of psychological adjustment. Further study is needed with diverse samples to determine whether race/ethnicity or social support can explain differences in the trajectories of mood disturbance.
The use of a single-item measure for symptom severity has limitations, including the risk for increased measurement error when compared to measures using multiple items. Single-items measures have reported reliability and validity and are useful for minimizing participant burden when capturing frequent symptom assessments and monitoring symptoms over time.22−24 Although numerous sources cite good reliability and validity with use of single-item measure, some would argue that more than one item is needed in symptom studies. For practical purposes, single-item measures are useful in symptom studies, allow for frequent measurement without substantial participant burden, and data were available for this secondary analysis using single-item measures.22−24
Particular care should be used in interpreting our results with regards to extracted predicted class memberships. Given the use of daily symptom severity reporting to define our symptom trajectory classes, there may be more variability within the classes around the parameter estimates than what is described in the models. In addition, predicted class memberships are based on probabilities, and while treated as observed variables in these analyses, care should be used to not over-extend the interpretation.
Implications for Practice
Recognizing the existence of a percentage of women who experience mood disturbance at moderate or greater severity during chemotherapy is important because not all women will require the same level of symptom management. The findings of the current study suggest that for a percentage of women, further evaluation of mood disturbance may be needed to determine whether the reported depressed mood or anxiety are clinically meaningful. Monitoring and management of symptoms of mood disturbance should be tailored to the individual needs of the patient, considering the potential of a small percentage of women who may require intensified evaluation and management. Importantly, this study describes the trajectories of the symptoms of depressed mood and anxiety using a single-item severity score, which may not represent clinically meaningful levels of depressed mood and anxiety. Nurses in clinical practice must incorporate assessment and management of mood disturbance early during the course of chemotherapy. Clinicians should be aware that those who present with a moderate depressed mood or anxiety early during a chemotherapy cycle may experience persistent depressed mood or anxiety.
Conclusions
We present 2 distinct trajectory classes of depressed mood and anxiety during cycles 2 and 3 of chemotherapy, with potential antecedents and outcomes associated with trajectory class membership. Future research should focus on the identification of potential correlates for class membership, including genetic and molecular determinants. Additionally, as this was an exploratory study, results of this study should be replicated in larger samples to determine whether these same classes are consistent and if, with larger class counts, correlates and long-term outcomes may be attributed to class membership. Interventions should be developed to assist women with symptoms of mood disturbance throughout chemotherapy, targeting those women who report symptoms of mood disturbance early in a cycle of chemotherapy.
Acknowledgments
Funding: Supported in part by a T32 Institutional Training Grant in Cancer, Aging, and End of Life Care (T32NR013456), National Institutes of Health, NIH/DHHS (R01 CA89474 Mooney, PI), and NIH/DHHS (R01 CA120558 Mooney, PI).
Footnotes
The authors have no conflicts of interest to disclose.
Contributor Information
Meagan Whisenant, Department of Symptom Research, Division of Internal Medicine, The University of Texas MD Anderson Cancer Center, Houston, Texas.
Bob Wong, College of Nursing and Huntsman Cancer Institute, University of Utah, Salt Lake City, Utah.
Sandra A. Mitchell, Outcomes Research Brant, National Cancer Institute, Rockville, Maryland.
Susan L. Beck, College of Nursing and Huntsman Cancer Institute University of Utah, Salt Lake City, Utah.
Kathi Mooney, College of Nursing and Huntsman Cancer Institute University of Utah, Salt Lake City, Utah.
References
- 1.Bower JE, Ganz PA, Irwin MR, et al. Inflammation and behavioral symptoms after breast cancer treatment: do fatigue, depression, and sleep disturbance share a common underlying mechanism? J Clin Oncol. 2011;29(26):3517–3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaston-Johansson F, Fall-Dickson JM, Bakos AB, et al. (1999). Fatigue, pain, and depression in pre-autotransplant breast cancer patients. Cancer Pract. 1999;7(5):240–247. [DOI] [PubMed] [Google Scholar]
- 3.Kim HJ, Barsevick AM, Tulman L, et al. Treatment-related symptom clusters in breast cancer: a secondary analysis. J Pain Symptom Manage. 2008;36(5):468–479. [DOI] [PubMed] [Google Scholar]
- 4.Liu L, Fiorentino L, Natarajan L, et al. Pre-treatment symptom cluster in breast cancer patients is associated with worse sleep, fatigue and depression during chemotherapy. Psychooncology. 2009;18(2):187–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.So WK, Marsh G, Ling WM, et al. The symptom cluster of fatigue, pain, anxiety, and depression and the effect on the quality of life of women receiving treatment for breast cancer: a multicenter study. Oncol Nurs Forum. 2009;36(4):E205–214. [DOI] [PubMed] [Google Scholar]
- 6.Gold M, Dunn LB, Phoenix B, et al. Co-occurrence of anxiety and depressive symptoms following breast cancer surgery and its impact on quality of life. Eur J Oncol Nurs. 2016;20:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Groenvold M, Petersen MA, Idler E, et al. Psychological distress and fatigue predicted recurrence and survival in primary breast cancer patients. Breast Cancer Res Treat. 2007;105(2):209–219. [DOI] [PubMed] [Google Scholar]
- 8.Jones SM, LaCroix AZ, Li W, et al. Depression and quality of life before and after breast cancer diagnosis in older women from the Women’s Health Initiative. J Cancer Surviv. 2015;9(4):620–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12(2):160–174. [DOI] [PubMed] [Google Scholar]
- 10.Bidstrup PE, Christensen J, Mertz BG, et al. Trajectories of distress, anxiety, and depression among women with breast cancer: Looking beyond the mean. Acta Oncol. 2015;54(5):789–796. [DOI] [PubMed] [Google Scholar]
- 11.Deshields T, Tibbs T, Fan MY, et al. Differences in patterns of depression after treatment for breast cancer. Psychooncology. 2006;15(5):398–406. [DOI] [PubMed] [Google Scholar]
- 12.Dunn LB, Cooper BA, Neuhaus J, et al. Identification of distinct depressive symptom trajectories in women following surgery for breast cancer. Health Psychol. 2001;30(6):683–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Helgeson VS, Snyder P, Seltman H. Psychological and physical adjustment to breast cancer over 4 years: identifying distinct trajectories of change. Health Psychol. 2004;23(1):3–15. [DOI] [PubMed] [Google Scholar]
- 14.Henselmans I, Helgeson VS, Seltman H, et al. Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychol. 2010;29(2):160–168. [DOI] [PubMed] [Google Scholar]
- 15.Lam WW, Bonanno GA, Mancini AD, et al. Trajectories of psychological distress among Chinese women diagnosed with breast cancer. Psychooncology. 2010;19(10):1044–1051. [DOI] [PubMed] [Google Scholar]
- 16.Lam WW, Shing YT, Bonanno GA, et al. Distress trajectories at the first year diagnosis of breast cancer in relation to 6 years survivorship. Psychooncology. 2012;21(1):90–99. [DOI] [PubMed] [Google Scholar]
- 17.Wang AW, Chang CS, Chen ST, et al. Identification of posttraumatic growth trajectories in the first year after breast cancer surgery. Psychooncology. 2014;23(12):1399–1405. [DOI] [PubMed] [Google Scholar]
- 18.Brant JM, Beck S, Miaskowski C Building dynamic models and theories to advance the science of symptom management research. J Adv Nurs. 2010;66(1):228–240. [DOI] [PubMed] [Google Scholar]
- 19.Brant JM, Dudley WM, Beck S, et al. Evolution of the Dynamic Symptoms Model. Oncol Nurs Forum. 2016;43(5):651–654. [DOI] [PubMed] [Google Scholar]
- 20.Mooney KH, Beck SL, Friedman RH, et al. Automated monitoring of symptoms during ambulatory chemotherapy and oncology providers’ use of the information: a randomized controlled clinical trial. Support Care Cancer. 2014;22(9):2343–2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mooney KH, Beck SL, Wong B, et al. Automated home monitoring and management of patient-reported symptoms during chemotherapy: results of the symptom care at home RCT. Cancer Med. 2017;6(3):537–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cleeland CS, Mendoza TR. Symptom measurement by patient report In: Cleeland CS, Fisch MJ, Dunn AJ eds. Cancer Symptom Science. New York, NY: Cambridge University Press; 2011:268–284. [Google Scholar]
- 23.Sloan JA, Loprinzi CL, Kuross SA, et al. Randomized comparison of four tools measuring overall quality of life in patients with advanced cancer. J Clin Oncol. 1998;16(11):3662–73. [DOI] [PubMed] [Google Scholar]
- 24.Mooney K, Berry P, Wong B, et al. Helping cancer-family caregivers with end-of-life home symptom management: Initial evaluation of an automated symptom monitoring and coaching system. Journal of Clinical Oncology. 2014;32(31):85. [Google Scholar]
- 25.Swarm R, Abernethy AP, Anghelescu DL, et al. Adult cancer pain. J Natl Compr Can Netw. 2010;8(8):904–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Colder CR, Campbell RT, Ruel E, et al. A finite mixture model of growth trajectories of adolescent alcohol use: predictors and consequences. J Consult Clin Psychol. 2002;70(4):976–985. [DOI] [PubMed] [Google Scholar]
- 27.Muthen B, Muthen LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24(6):882–891. [PubMed] [Google Scholar]
- 28.Jung T, Wickrama KA. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2(1):302–317. [Google Scholar]
- 29.Whisenant M, Wong B, Mitchell S, et al. Distinct trajectories of fatigue and sleep disturbance in women receiving chemotherapy for breast cancer. Oncol Nurs Forum. 2017;44(6):739–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nieboer P, Buijs C, Rodenhuis S, et al. Fatigue and relating factors in high-risk breast cancer patients treated with adjuvant standard or high-dose chemotherapy: a longitudinal study. J Clin Oncol. 2005;23(33):8296–8304. [DOI] [PubMed] [Google Scholar]
- 31.Cleeland CS, Bennett GJ, Dantzer R, et al. Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97(11):2919–2925. [DOI] [PubMed] [Google Scholar]
- 32.Miaskowski C, Cooper BA, Melisko M, et al. Disease and treatment characteristics do not predict symptom occurrence profiles in oncology outpatients receiving chemotherapy. Cancer. 2014;120(15):2371–2378. [DOI] [PMC free article] [PubMed] [Google Scholar]