Abstract
Chronic wasting disease (CWD) is a highly contagious prion disease affecting captive and free-ranging cervid populations. CWD has been detected in United States, Canada, South Korea and, most recently, in Europe (Norway, Finland and Sweden). Animals with CWD release infectious prions in the environment through saliva, urine and feces sustaining disease spreading between cervids but also potentially to other non-cervids ruminants (e.g. sheep, goats and cattle). In the light of these considerations and due to CWD unknown zoonotic potential, it is of utmost importance to follow specific surveillance programs useful to minimize disease spreading and transmission. The European community has already in place specific surveillance measures, but the traditional diagnostic tests performed on nervous or lymphoid tissues lack sensitivity. We have optimized a Real-Time Quaking-Induced Conversion (RT-QuIC) assay for detecting CWD prions with high sensitivity and specificity to try to overcome this problem. In this work, we show that bank vole prion protein (PrP) is an excellent substrate for RT-QuIC reactions, enabling the detection of trace-amounts of CWD prions, regardless of prion strain and cervid species. Beside supporting the traditional diagnostic tests, this technology could be exploited for detecting prions in peripheral tissues from live animals, possibly even at preclinical stages of the disease.
Subject terms: Biological techniques, Neuroscience
Introduction
Chronic Wasting Disease (CWD) is a prion disease, a neurodegenerative disorder that affects cervid populations. It was first identified in 1967 in a captive mule deer from Colorado. CWD was then diagnosed across a wide area of North America1 where it is spreading extensively. It has also been reported in South Korea, as a consequence of infected animals imported from Canada2 and has most recently been reported in Europe3 (Norway, Finland and Sweden4,5). To date, CWD has been identified in mule deer (Odocoileus hemionus)6, black-tailed deer (Odocoileus hemionus), white-tailed deer (Odocoileus virginianus)7, elk (Cervus canadensis)6,8 moose (Alces alces)9, reindeer (Rangifer tarandus tarandus) and red deer (Cervus elaphus)2,10–12.
As in other prion diseases, the causative agent is considered to be an abnormally folded isoform of the prion protein (PrPC), named prion or PrPSc13, which accumulates mostly in the central nervous system (CNS). PrPC plays important roles in several physiological processes and is evolutionarily conserved amongst different mammalian species3,6,14–19. Misfolded PrPSc propagates through conformational templating where PrPC is converted into PrPSc thus acquiring infectious features and sustaining disease13,20.
Horizontal transmission of CWD is highly efficient, through both animal-to-animal contact and exposure to environments contaminated with prion infected material (e.g. excreta, placenta or carcasses)21–24. Polymorphisms in the PrP gene (Prnp) are known to affect (i) animal susceptibility to CWD, (ii) transmission efficiency between species, (iii) clinical and (iv) neuropathological features of the disease25–28. For instance, deer PrPC is characterized by having a glycine (G) or serine (S) at codon 96 of Prnp29,30; Moose PrPC contains either lysine (K) or glutamine (Q) at position 10931; Elk PrPC has either methionine (M) or leucine (L) at position 13226; Reindeer PrPC has aspartic acid (D) or asparagine (N) at residue 17631; Mule deer PrPC contains either serine (S) or phenylalanine (F) at position 22532 while Whitetail deer is characterized by having alanine (A) or glycine (G) at position 116 and glutamine (Q) or lysine (K) at position 22628. These amino acids determine important variability in disease phenotypes or susceptibility to CWD infection. For example, the expression of L at position 132 of elk PrP appears to confer, at least partially, resistance to CWD when compared to the more prevalent 132 M allele33. Similarly, the expression of S at position 96 of deer PrP is linked to reduced incidence of CWD34.
Thus, other than dictating CWD susceptibility, PrP polymorphisms seem to play an important role in prion strains selection35–37. Strains are extremely relevant in prion diseases since they determine variability in clinical phenotype of the disease, and influence the characteristics of PrPSc that acquires distinct biochemical properties (e.g., electrophoretic mobility in Western blot (WB) and analysis of glycoforms ratio after treatment with proteinase K) and differentially accumulates in specific brain areas38–43. Differences in strain behavior and features are known to rely on different abnormal conformations that could be acquired by PrPSc. Strains conformational mutations can be further promoted during CWD transmission between species where PrPSc is subjected to important processes of selection and adaptation in the new host36,44–46.
Definite CWD diagnosis relies on post-mortem detection of PrPSc in the brainstem and the head lymph nodes47–49 using rapid tests (enzyme-linked immunosorbent assays (ELISA), WB and/or immunohistochemistry (IHC))50–52. PrPSc can be detected in peripheral lymphoid tissues (especially those associated with the alimentary canal) of most CWD affected animals, like in sheep affected with classical scrapie, before it can be detected in the brain48,53,54. For instance, IHC analyses of the palatine tonsils and recto-anal mucosa-associated lymphoid tissues (RAMALT) are used for an ante-mortem diagnosis of CWD in deer49,55–57. Nevertheless, in some CWD affected elks, while PrPSc is detected in the brain, the presence of PrPSc in the lymphoid tissues can be minimal or undetectable, which represents an important limitation for the ante-mortem diagnosis58,59. Similarly, Norwegian moose and red deer show PrPSc in the brain but PrPSc was not detected in lymphoid tissues3,9,60. Reindeer in Norway, conversely, have detectable lymphoid PrPSc accumulation even in animals where no PrPSc is detected in the CNS3.
However, at early stages of the disease, also the amount of PrPSc in peripheral lymph nodes is lower than the detection threshold of traditional diagnostic techniques61. In this case, the most reliable way to detect low titer of infectious prions is therefore by animal bioassay. Even though these experiments remain the gold standard for measuring low amounts of infectivity, they are time consuming, expensive and can therefore not be used as screening tests62–65.
Thanks to the recent development of in vitro cell-free amplification techniques, including the Protein Misfolding Cyclic Amplification (PMCA) and the Real Time Quaking Induced Conversion (RT-QuIC) assays, it is possible to detect trace-amounts of CWD prions in different peripheral tissues and biological fluids66. In particular, PMCA showed the presence of PrPSc in muscles67, feces68,69, saliva70, cerebrospinal fluid (CSF)71 and even the blood of animals at different stages of CWD infection72,73. Unfortunately, there is no universal PMCA substrate for amplifying CWD from different species. This technique, therefore would seem not to be the method of choice when analyzing samples that are collected in the field (feces or saliva) from species with unknown origin. In RT-QuIC, through alternate cycles of incubation and shaking, prions force the substrate of reaction (recombinant PrP) to adopt β-sheet structures74. These abnormally folded PrP proteins aggregate and form amyloid fibrils whose growth is monitored with Thioflavin-T (ThT) fluorescent dye. The assay has been used extensively for detecting CWD prions in nasal swabs75, lymphoid tissues76, CSF71, blood77, saliva78,79, urine80 and feces81,82 of animals at clinical and, sometimes, preclinical stages of disease. The presence of CWD prions in the saliva, urine and feces of affected animals suggests that substantial environmental contamination can occur during the entire course of the disease, especially considering that sialorrhea and polyuria are common in diseased animals83–87. Moreover, prions can persist in the environment for many years and thus represent a serious risk of future contamination upon restocking of CWD-exposed areas1,88–93.
For this reason, RT-QuIC due to its high sensitivity and high-throughput potential can have useful applications for ante-mortem identification of CWD infected animals. However, the technique detects different prion strains or strains belonging to different species with variable efficiency. To date, most of the RT-QuIC experiments described in the literature have been performed using primarily Syrian hamster or deer PrP as substrate of reaction (see Table 1). In the present study, RT-QuIC analyses were performed on serial dilutions of brain homogenates collected from both healthy and CWD-affected Norwegian moose, reindeer and red deer, using different substrates. We evaluated the ability of truncated PrP from Syrian hamster, bank vole, deer, reindeer and elk to detect brain derived PrPSc regardless of animal species or prion strain. This is also the first time where RT-QuIC has been used to analyze samples from CWD affected Norwegian reindeer.
Table 1.
Summary of RT-QuIC substrates (PrP) used to analyze different tissues of CWD affected cervid species.
| Species | Prion | Tissue analyzed | Substrate | Year | References |
|---|---|---|---|---|---|
| Deer | CWD | Brain | Deer PrP (24–234) | 2010 | 130 |
| Deer | CWD | Brain, urine and feces | Deer PrP (24–234) | 2013 | 80 |
| Deer | CWD | Saliva | Syrian hamster PrP (90–231) | 2013 | 79 |
| Deer | CWD | Blood | Syrian hamster PrP (90–231) | 2013 | 77 |
| Deer | CWD | CSF | Syrian hamster PrP (90–231) | 2013 | 71 |
| Deer | CWD | Retropharyngeal lymph node | Syrian hamster PrP (90–231) | 2014 | 131 |
| Deer | CWD | Brain, saliva | Syrian hamster PrP (90–231) | 2015 | 132 |
|
Deer Elk |
CWD | Brain | Bank vole (23–230) | 2015 | 100 |
| Deer | CWD | Saliva, urine | Syrian hamster PrP (90–231) | 2015 | 78 |
| Deer | CWD | Brain | Deer PrP (23–231) | 2015 | 124 |
| Deer | CWD | RAMALT, nasal brush | Syrian hamster PrP (90–231) | 2016 | 75 |
| Elk | CWD | RAMALT, nasal brush | Syrian hamster PrP (90–231) | 2016 | 76 |
| Deer | CWD | Feces | Syrian hamster PrP (90–231) | 2016 | 69 |
| Deer | CWD | Brain, lymphoid tissues | Syrian hamster PrP (90–231) | 2017 | 133 |
| Deer | CWD | Ovary tissue, uterine tissue, placentome, amniotic and allantoic fluids | Syrian hamster PrP (90–231) | 2017 | 134 |
| Deer | CWD | Brain | Deer PrP (24–234) | 2017 | 135 |
| Deer | CWD | Gastrointestinal tissues (e.g. omasum, abomasum, colon, cecum) and lymphoid tissues (e.g. spleen, tonsils) | Syrian hamster PrP (90–231) | 2017 | 136 |
| Elk | CWD | Feces | Syrian hamster PrP (90–231) | 2017 | 82 |
| Elk | CWD | RAMALT | Syrian hamster PrP (90–231) | 2017 | 137 |
| Deer | CWD | Saliva | Syrian hamster PrP (90–231) | 2017 | 138 |
|
Deer Elk |
CWD | RAMALT | White-tailed deer PrP (25–232) | 2017 | 139 |
| Mule deer PrP (25–232) | |||||
| Fallow deer PrP (25–232) | |||||
| Elk PrP (25–232) | |||||
| Reindeer PrP (25–232) | |||||
| Elk | CWD | Blood, rectal biopsy | Syrian hamster PrP (90–231) | 2018 | 140 |
|
Deer Elk |
CWD | Retropharyngeal lymph node, brain | Syrian hamster PrP (90–231) | 2018 | 60 |
| Deer | CWD | Saliva | Syrian hamster PrP (90–231) | 2018 | 70 |
| Elk | CWD | Brain | Elk PrP (23–231) | 2018 | 141 |
| Elk | CWD | Brain | Syrian hamster PrP (90–231) | 2019 | 4 |
| Deer | CWD | Brain | Syrian hamster PrP (90–231) | 2019 | 142 |
| Deer | CWD | Brain, eyelids | Syrian hamster PrP (90–231) | 2019 | 143 |
Our results indicate that the use of bank vole PrP provided efficient prion detection in all CWD affected animals, even in the instances where traditional diagnostic methods (WB, IHC or ELISA) failed to demonstrate the presence of PrPSc. This optimized RT-QuIC assay could therefore be used as a screening test for CWD detection. It could also be a useful research tool for analyzing other tissues with low levels of PrPSc like peripheral tissues from live animals or excreta (such as urine, saliva and blood) that can be collected through non-invasive procedures. Moreover, although there are no documented cases of natural interspecies transmission of CWD to non-cervid animals, many livestock (especially sheep and goats) which share their habitat with diseased cervids will be exposed to prions and could potentially be infected. Although there is a so-called “species barrier”, which is related to differences in PrP sequences between donor and acceptor animals that can limit the efficiency of prion transmission between species (spillover phenomenon that occur for instance from cervids to small ruminants), the potential risk of breaking such barrier cannot be excluded. For instance, CWD transmission to other species (especially human) cannot be completely ruled out at present64,94,95. For this reason, identifying preclinical CWD affected animals is of fundamental importance for minimizing horizontal disease transmission.
Results
TeSeETM WB analysis detects prions in brain or lymph nodes of CWD affected animals
The CWD affected animals used in this study were identified through the Norwegian surveillance program for CWD that has been started in 2016. These animals were firstly diagnosed by TeSeETM ELISA test and then confirmed by WB analysis (diagnostic statuses are summarized in Table 2). To verify the presence of different distribution patterns of CWD prions in both brain and lymph nodes WB analyses were finally performed. Proteinase K resistant PrP (PrPres) was found in the samples from all the CWD affected moose (Mo1, Mo2 and Mo3) and red deer (Rd1), while PrPres was detected only in 3 out of 7 brain samples of CWD affected reindeer (Fig. 1a). In contrast, PrPres was not found in the lymph nodes of CWD affected moose and red deer but always detected in lymph nodes of the CWD affected reindeer (Re1-Re7) (Fig. 1b). PrPres was not detected in any of the samples (brain or lymph node) collected from healthy animals.
Table 2.
Demographic information and TeSeETM WB results of the Norwegian animals included in this study.
| Species | Sample ID | Status | Geographic origin | Sex | Age(y) | PrPres detection | |
|---|---|---|---|---|---|---|---|
| Brain | LN | ||||||
| Alces alces | Mo1 | CWD | Lierne | Female | 13 | + | − |
| Mo2 | CWD | Selbu | Female | 13 | + | − | |
| Mo3 | CWD | Selbu | Female | 14 | + | − | |
| Mo4 | Healthy | Råde | Unknown | >1 | − | − | |
| Mo5 | Healthy | Voss | Male | >1 | − | − | |
| Cervus elaphus | Rd1 | CWD | Gjemnes | Female | 16 | + | − |
| Rd2 | Healthy | Eid | Female | >1 | − | − | |
| Rd3 | Healthy | Årdal | Male | >1 | − | − | |
| Rangifer tarandus tarandus | Re1 | CWD | Nordfjella | Male | >1 | + | + |
| Re2 | CWD | Nordfjella | Female | >1 | + | + | |
| Re3 | CWD | Nordfjella | Male | >1 | + | + | |
| Re4 | CWD | Nordfjella | Female | >1 | − | + | |
| Re5 | CWD | Nordfjella | Male | 1.5 | − | + | |
| Re6 | CWD | Nordfjella | Female | >1 | − | + | |
| Re7 | CWD | Nordfjella | Male | 8 | − | + | |
| Re8 | Healthy | Lom | Male | >1 | − | − | |
| Re9 | Healthy | Lom | Female | >1 | − | − | |
Figure 1.
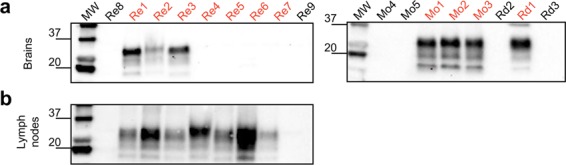
TeSeETM WB results of brain and lymph nodes collected from the healthy (black) and CWD affected (red) animals included in the study. (a) PrPres was detected in all brain homogenates of CWD affected moose (Mo1, Mo2, Mo3), red deer (Rd1) and 3 brain homogenates (out of 7) of CWD affected reindeer. Notably, no PrPres was detected in the brains of CWD affected reindeer 4, 5, 6, and 7; (b) PrPres was however detected in the lymph nodes of all the CWD affected reindeer. PrPres was not found in brain and lymph nodes of healthy animals. Numbers on the left of the Western blots indicate molecular weights (kDa).
RT-QuIC analysis with bank vole PrP enables efficient prion detection in brain samples from cervids where PrPSc was biochemically detected
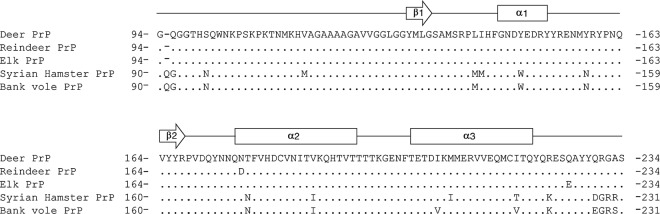
With the aim of evaluating the efficiency of different substrates in detecting CWD prions in different cervid species, RT-QuIC experiments were performed using recombinant PrP proteins with amino acidic sequences belonging to the following animal species: Syrian hamster, bank vole (109 M), deer (96 G), reindeer (176D) and elk (132 M) (Fig. 2). According to the most recent publications (see Table 1), we decided to use truncated proteins since the C-terminal protein domain allows prion detection with high sensitivity and specificity96,97. Evaluation of the overall RT-QuIC performance was based on brain samples collected from CWD affected animals where PrPSc was detected by means of TeSeETM ELISA and WB. Brain homogenates of Rd1, Mo1, Mo2, Mo3, Re1, Re2 and Re3 were diluted from 10−5 to 10−7 and subjected to RT-QuIC analysis. Brain samples of healthy animals (Rd2, Rd3, Mo4, Mo5, Re8 and Re9) were used as controls.
Figure 2.
Amino acid sequences of recombinant PrP proteins used for RT-QuIC experiments. The amino acid sequence of deer PrP was used as reference for aligning the sequences of reindeer, elk, Syrian hamster and bank vole PrP. Arrows and rectangles indicate beta-sheets (β1 and β2) and alpha helix (α1, α2 and α3) secondary structures, respectively.
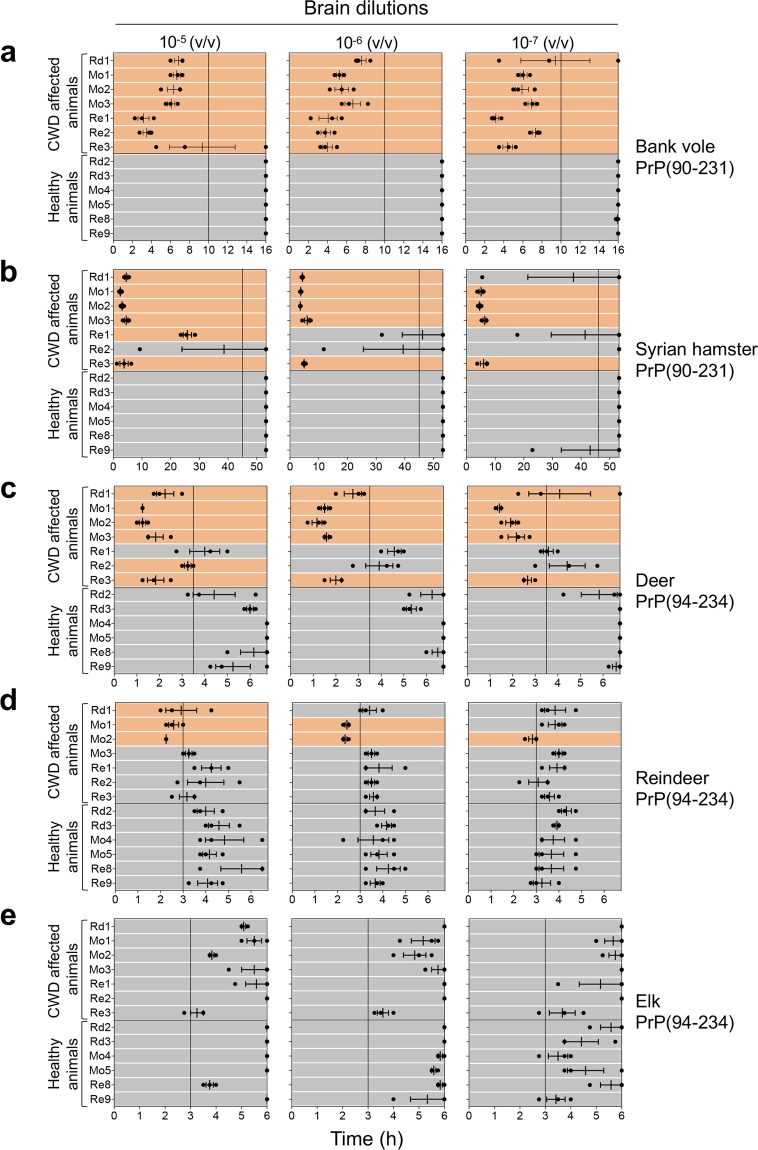
Regardless of the animal species or brain dilution, bank vole PrP enabled PrPSc detection with a higher sensitivity and specificity compared to the other tested substrates (Fig. 3a). Particularly, all CWD affected animals’ samples induced RT-QuIC seeding activity within 10 hours while those of healthy controls did not. The reaction was stopped at 16 hours because at this point negative controls started to induce unspecific seeding activity.
Figure 3.
RT-QuIC results of CWD affected animals with detectable PrPSc in the brain. RT-QuIC analysis of serial brain homogenate dilutions (from 10−5 to 10−7) from CWD affected animals and controls with (a) bank vole, (b) Syrian hamster, (c) deer, (d) reindeer and (e) elk recombinant truncated PrP. Each sample was analyzed in triplicate and black dots indicate the time taken for each replicate to reach the fluorescence threshold (lag phase). The vertical line indicates the time threshold set up for each PrP substrate. Rd: red deer, Mo: moose; Re: reindeer. Mean value and standard error of the mean (S.E.M) are shown.
Compared to the bank vole PrP, Syrian hamster PrP substrate did not detect all CWD affected animals’ samples and the sensitivity decreased at higher dilutions. In particular, one (Re2), two (Re1 and Re2) or three (Re1, Re2 and Rd1) CWD affected animals’ samples were not detected at 10−5, 10−6 or 10−7 dilutions, respectively (Fig. 3b). Notably, this substrate hardly detected Norwegian reindeer CWD prions compared to the moose and red deer ones. The reaction was stopped at 53 hours and none of the negative controls induced unspecific reaction. We analyzed whether the prion protein sequence homology between CWD prions and substrate could increase the power of discrimination between prion affected and healthy animals. We then analyzed the samples using PrP substrates with amino acid sequences of deer, reindeer and elk. Surprisingly, while deer PrP (Fig. 3c) was still able to detect CWD affected animals’ samples with sensitivity and specificity quite comparable to that of Syrian hamster PrP, reindeer (Fig. 3d) and elk PrP (Fig. 3e) were characterized by a very rapid aggregation in both the positive and the negative samples. Even with a time threshold of 3 hours, we could not clearly discriminate between CWD affected animals and healthy controls. Thus, PrP substrates with cervid sequences appear to be less efficient in detecting CWD prions than those with bank vole and Syrian hamster sequences.
Two brain samples from CWD affected white-tailed deer (WTd) from North America were included in the RT-QuIC analysis to verify whether the overall performance of the assay could have been influenced by the origin of the CWD prions (Norway vs North America). The two isolates were provided to the Norwegian Veterinary Institute in Oslo in 2006 as part of a ring trial (courtesy of Aru Balachandran, Canadian Food Inspection Agency, Alberta, Canada). In this case, their seeding activities were similar to that of Norwegian CWD affected deer, in terms of lag phase and fluorescence intensity (Fig. 4 and see Supplementary Fig. S1).
Figure 4.
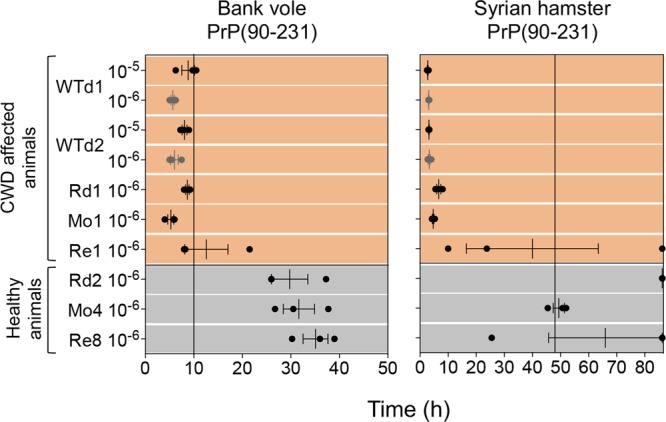
RT-QuIC results of CWD affected Norwegian and North American cervid species. Brain homogenates were diluted at 10−5 and/or 10−6 and analyzed by RT-QuIC using bank vole and Syrian hamster recombinant truncated PrP. Each sample was analyzed in triplicate and black dots indicate the time taken for each replicate to reach the fluorescence threshold (lag phase). The vertical line indicates the time threshold set up for each PrP substrate. WTd: white tailed deer (North America); Rd: red deer; Mo: moose; Re: reindeer. Mean value and standard error of the mean (S.E.M) are shown.
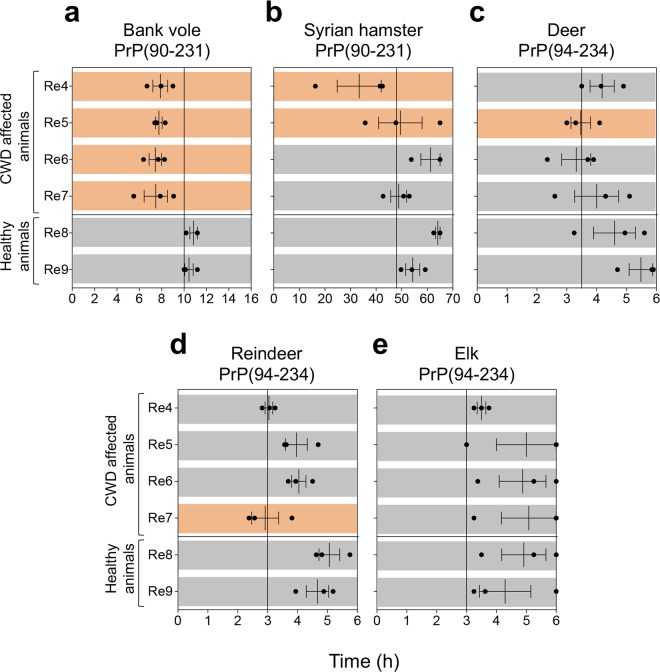
RT-QuIC analysis with bank vole PrP enables efficient prion detection in reindeer brain samples where PrPSc was not biochemically detected
Finally, we have analyzed samples collected from CWD affected reindeer (Re4, Re5, Re6, Re7) where PrPSc had only been detected in the lymph nodes and not the brain with TeSeETM ELISA and WB. We decided not to perform serial dilutions given the lack of WB signal in the brain samples and chose a dilution of 10−5. As previously observed, the bank vole PrP was the most efficient at detecting prions in all the CWD affected reindeer (Fig. 5a). The Syrian hamster PrP did not detect 2 out of 4 CWD samples (Re6 and Re7) (Fig. 5b); whilst deer (Fig. 5c) and reindeer PrP (Fig. 5d) did not detect 3 out of the 4 CWD samples (Re4, Re6, Re7 and Re4, Re5, Re6, respectively). Elk PrP did not detect any of them (Fig. 5e).
Figure 5.
RT-QuIC results of CWD affected reindeer where PrPSc was not biochemically detected in the brain. Brain homogenates were diluted at 10−5 and analyzed by RT-QuIC using (a) bank vole, (b) Syrian hamster, (c) deer, (d) reindeer and (e) elk recombinant truncated PrP. Each sample was analyzed in triplicate and black dots indicate the time to reach the fluorescence threshold (lag-phase) of each replicate. The vertical line indicates the time threshold set up for each PrP substrate. Rd: red deer; Mo: moose; Re: reindeer. Mean value and standard error of the mean (S.E.M) are shown.
Discussion
First discovered in deer in Colorado many decades ago, CWD rapidly spread to many other American states98 and Canada10. In April 2016, the disease was diagnosed in a Norwegian reindeer from the Nordfjella area3. This was the first case of CWD in Europe, and the first reindeer reported with naturally occurring CWD. This disease is contagious within cervid populations and can efficiently transmit directly between animals or through the environment. Healthy animals can be infected after close contact with saliva, urine and feces of affected ones (direct horizontal transmission) or after being exposed to environments contaminated with excreta or carcasses of diseased animals (indirect horizontal transmission). Prions persist in the environment for long time and contribute significantly to disease spreading.
In Europe surveillance programs are aimed at detecting the presence of CWD in wild and farmed cervids. The validated and approved diagnostic tests require animals to be sacrificed for sampling the CNS (e.g. brainstem) and/or lymphoid tissue for ELISA, WB and IHC based analyses61. Although these tests reach high levels of diagnostic accuracy for CWD, PrPSc accumulation in brain and lymphoid tissues can be lower than the detection threshold of the tests, especially in the early stages of disease. In addition, different CWD prion strains can affect test performance, as in the case of Nor98/atypical scrapie99.
In this work we evaluated the efficiency of the highly sensitive RT-QuIC assay in detecting low amounts of CWD prion in different Norwegian cervid species. Our aim was to set up optimal conditions for PrPSc detection, regardless of prion strains and animal species. For this reason, brain homogenates of CWD affected moose, red deer and reindeer were serially diluted and subjected to RT-QuIC analysis performed using Syrian hamster, bank vole, deer, reindeer and elk PrP as reaction’s substrates.
Our results indicated that the bank vole PrP enabled CWD prion detection in every brain dilution of all cervid species, especially in reindeer where PrPSc detection was more challenging compared to the other species and we could clearly discriminate CWD affected animals from healthy controls. A slightly less efficient detection of CWD prions was observed using Syrian hamster PrP. By using bank vole PrP we could detect prions in brain samples of reindeer that had tested negative with traditional diagnostic tests. Moreover, we efficiently detected PrPSc in samples from North American cervids, which have CWD prion strains that might be different from those found in Norway9. Thus, the use of bank vole PrP overcomes strain-related effects which are known to influence the efficiency of the RT-QuIC. The capability of bank vole PrP to detect a wide range of prion strains has already been reported100 and here we demonstrate for the first time that this substrate enables high efficient detection of multiple CWD strains in different Norwegian CWD affected cervids.
Efficient transmission of TSE infection requires a close similarity between the primary amino acid sequence of the PrP in the donor and in the recipient animal. This allows PrPSc to interact specifically with and convert the host’s PrPC into the disease-associate isoform and could explain why CWD is so easily transmissible between different cervid species26,101,102. Our results showed that the efficiency of the RT-QuIC test was reduced by the use of deer PrP, especially in reindeer, and the sensitivity dropped drastically when using reindeer and elk PrP. Nevertheless, similar observations have been made in the field of human prion diseases: the use of human PrP substrate for RT-QuIC analyses results in lower sensitivity and specificity compared to Syrian hamster or bank vole PrP for detecting PrPSc in peripheral tissues (e.g. cerebrospinal fluid and olfactory mucosa) of prion diseased patients103–107.
PrP sequences of other species, including human and non-cervid ruminants, are dissimilar to that of cervids and this limits the efficiency of interspecies CWD transmission. Nevertheless, the potential risk of interspecies transmission of CWD represents a serious public health concern since humans, cattle and sheep could be exposed to CWD prions through the consumption of prion-infected feed or from contact with a prion-contaminated environment. It is estimated that more than 60% of Americans have eaten deer or elk meat or their derived products108 while a large number of cattle, sheep and goats have grazed in CWD contaminated environments. Thankfully, controlled natural exposure studies and targeted surveillance programs currently indicate no cases of natural interspecies transmission of CWD10,109–113.
Experimentally, CWD can efficiently be transmitted by intracerebral inoculation in mice, mink, squirrel monkeys, ferrets, sheep and some cattle10,109,114–118. But attempts to transmit to transgenic mice overexpressing human prion protein119 or to Cynomologus macaques120, which are evolutionarily closer to humans, were unsuccessful. This suggests little or no zoonotic potential. The efficiency of CWD transmission to humans has been also evaluated in vitro with highly sensitive PMCA and RT-QuIC techniques. Some studies showed that the human PrP can be converted to the pathologic form by CWD prions. It was suggested that the efficiency of this conversion is highly influenced by (i) human PrP polymorphism (recipient), (ii) cervid PrP polymorphism (donor) and (iii) isolates origin (strain)121–125. Overall, experiments performed using in vitro amplification techniques suggest that the species barrier between cervids and human is not absolute. However, although these techniques mimic in vitro the process of prion conversion, they lack many of the biological interactions occurring in vivo and the results, regarding the study of the complex phenomenon of the species barrier, should be carefully interpreted. In addition, the species barrier does not only depend on the PrP sequence homology between host and recipient, but also the prion strain. It is therefore conceivable that different CWD strains may have different abilities at crossing the species barrier. Many other factors may play a pivotal role in driving this phenomenon. CWD prions can undergo to processes of selection and adaptation once the interspecies transmission has occurred, with the generation of new prion conformers more prone to propagate in the new host and likely easier to transmit within the species126,127. For instance, prions from cattle affected by bovine spongiform encephalopathy (BSE) crossed the species barrier (although with low efficiency) and infected humans, generating a new disease named variant Creutzfeldt-Jakob disease (vCJD)128. There is therefore considerable concern that CWD prions could cross the species barrier, adapt to humans and result in new forms of prion disease. The ongoing surveillance has not reported any documented cases of CWD transmission to humans at present. However, the lack of interspecies transmission cannot definitively be ruled out112,129.
Our optimized RT-QuIC performed with bank vole PrP could be used as first step screening assay followed by traditional confirmatory TeSeE ELISA, WB or IHC assays to increase the accuracy of CWD detection in affected animals. After a process of validation where many more samples of CWD affected animals and negative controls will be analyzed with this technique, it could be employed as new tool for the diagnosis of CWD either at clinical or preclinical stage of the disease. In addition, considering its elevated analytical sensitivity and rapidity, RT-QuIC might also be exploited for a quick and efficient PrPSc detection in tissues and biological fluids, such as urine, saliva or feces. These samples are easier to collect than CNS and lymphoid tissues and do not require immobilization or euthanasia of animals. This test could also be used to confirm the absence of infection in animals prior to restocking. Finally, other than monitoring the spreading of CWD prions between cervid species, RT-QuIC with bank vole PrP can be further extended to evaluate the presence of prions in tissues collected from other animals (e.g. sheep, goats, cattle) eventually exposed to contaminated environment.
In conclusion, we provide evidence that RT-QuIC performed with bank vole PrP as reaction substrate is capable of detecting CWD prions, regardless of the cervid species, strains and geographical origin, with good analytical sensitivity and specificity. This rapid and useful technique is, in combination with traditional diagnostic tests, ideal for screening samples containing low concentrations of CWD prions.
Materials and Methods
Compliance with Ethical Standards
All animal samples included in this study were provided by the Norwegian surveillance program for CWD in compliance with ethical standards.
Animals
The following animals from Norway were included in the study: (i) 5 Moose (Alces alces) (3 affected by CWD and 2 healthy animals), (ii) 3 red deer (Cervus elaphus) (1 affected by CWD and 2 healthy animals) and (iii) 9 reindeer (Rangifer tarandus tarandus) (7 affected by CWD and 2 healthy animals). The information concerning the animal’s geographical origin, sex, age and diagnostic status is summarized in Table 2.
TeSeETM ELISA and WB tests for CWD diagnosis
All the CWD affected animals were first detected by the Norwegian surveillance program for CWD, using commercially available tests for the detection of PrPSc. Brain tissues and a piece of lymph node were homogenized at 20% (weight/volume) in individual grinding tubes. Rapid test TeSeETM SAP ELISA (Bio-Rad) was carried out according to the manufacturer’s instruction. Positive ELISA samples were then analyzed with TeSeETM Western blot (Bio-Rad) for confirmation.
TeSeETM Western blot analysis of brain and lymph nodes samples
The homogenates submitted to Western blot were collected from the grinding tubes primarily analyzed by rapid test TeSeE™ ELISA. The WB test was performed, with slight modifications, according to the manufacturer’s instructions. Briefly, PrPC was digested by incubating the homogenates with Proteinase K (20 µl per ml) for 10 min at 37 °C. Electrophoresis was performed using mini-PROTEAN® TGX™ Precast Gels (Bio-Rad) and Power Pac Universal (first 10 min at 60 V followed by approximately 35 min at 120 V). Gels were then electroblotted using semi-dry transfer apparatus (Trans-Blot® Turbo™ Transfer System, Bio-Rad) onto polyvinylidene fluoride (PVDF) membrane (Bio-Rad). The immunoblotting process began by blocking the membrane, to prevent unspecific bindings, with the kit’s block solution for 30 min, then a second 30 min incubation was carried out using monoclonal antibodies SHa31 (AbI from the kit) and an additional monoclonal antibody (P4) at a dilution of 1:1000. Lastly, a 20 min incubation with goat anti-mouse immunoglobulin G (IgG) antibody conjugated with horseradish peroxidase (AbII from the kit) was carried out. The test’s chemiluminescent substrate ECL (Western blotting detecting reagents, Amersham ECLTM) was then added and the chemiluminescent signals were visualized using ChemiDoc System (Bio-Rad). The samples were declared positive if characteristic banding patterns of PK-resistant core of PrPSc were present.
RT-QuIC recombinant substrates production
Truncated Syrian hamster (90–231), reindeer (94–234; 176D), deer (94–234; 96 G), elk (94–234; 132 M) and bank vole PrP (90–231; 109 M) constructs were purchased from GenScript. The constructs were expressed in Escherichia coli BL21 (DE3) cells (Stratagene). Freshly transformed overnight culture was inoculated into Luria Bertani (LB) medium and 100 μg/mL ampicillin. At 0.8 OD600 expression was induced with isopropyl b-D galactopyranoside (IPTG) to a final concentration of 0.75 mM. Cells were grown in a BioStat-B plus fermentor (Sartorius). The cells were lysed by a homogenizer (PandaPLUS 2000) and the inclusion bodies were suspended in buffer containing 25 mM Tris-HCl, 5 mM EDTA, 0.8% TritonX100, pH 8, and then in bi-distilled water several times. Inclusion bodies containing recombinant proteins were dissolved in 5 volumes of 8 M guanidine hydrochloride (GndHCl), loaded onto pre-equilibrated HiLoad 26/60 Superdex 200-pg column, and eluted in 25 mM Tris–HCl (pH 8), 5 mM ethylenediaminetetraacetic acid (EDTA), and 6 M GndHCl at a flow/rate of 2 mL/min. Proteins refolding was performed by dialysis against refolding buffer (20 mM sodium acetate and 0.005% NaN3 (pH 5.5)) using a Spectrapor membrane. Purified proteins were analyzed by SDS-polyacrylamide gel electrophoresis under reducing conditions and Western blot. Aliquots of the recombinant proteins were stored at −80 °C in 10 mM phosphate buffer (pH 5.8).
Preparation of the samples for RT-QuIC analyses
Brain tissues were homogenized at 10% (weight/volume) in Bio Rad buffer (from TeSeETM grinding tubes), serially diluted (from 10−5 to 10−7) and subjected to RT-QuIC analysis. Two brain tissues of CWD affected white tailed deer (WTd) collected from North America (used for a ring trial for CWD diagnosis in 2006) were homogenized, diluted at 10−5 and 10−6 and included in the analysis.
RT-QuIC experimental procedures
Protein substrate solutions were allowed to thaw at room temperature and filtered through a 100 kDa Nanosep centrifugal device (Pall Corporation). Samples were analyzed in triplicate in a black 96-well optical flat bottom plate (ThermoScientific). The final reaction volume was 100 µL and the reagents (Sigma) were concentrated as follow: 150 mM NaCl, 0.002% SDS, 10 mM PBS, 1 mM EDTA, 10 µM ThT and 0.13 mg/ml of recPrP. To avoid contamination, reaction mixes were prepared and loaded (98 µL) onto the microplate in a prion-free laboratory. After the addition of 2 µL of diluted brain homogenates (from 10−5 to 10−7), the plate was sealed with a sealing film (ThermoScientific) and inserted into a FLUOstar OPTIMA microplate reader (BMG Labtech). The plate was incubated at 55 °C with cycles of 1 min shaking (at 600 rpm, double orbital) and 1 min incubation. Fluorescence readings (480 nm) were taken every 15 min (30 flashes per well at 450 nm). A sample was considered positive if the two highest fluorescence values (AU) of the replicates were greater than 10.000 AU and at least two, out of three replicates, crossed the time threshold that was set for each recombinant substrate. We set the following time thresholds for each PrP: (i) Syrian hamster 48 hours, (ii) bank vole 10 hours, (iii) deer 3.5 hours, (iv) reindeer 3 hours and (v) elk 3 hours. In particular, we have evaluated the time at which the unspecific aggregation of each PrP template occurred in the presence of negative samples (analyzed at least three different times). We have then set this value as time-threshold. Therefore, all samples able to promote PrP aggregation before this time-threshold were considered able to exert a seeding activity while the others were considered unable to promote a seeding activity for each PrP substrate. Data are plotted in graphs showing the time taken for each replicate (black dots) to reach the fluorescence threshold (lag phase).
Statistical analyses and graphic representation
Statistical analysis (mean and standard error of the mean (S.E.M.)) and graphic representations of our data were performed using the Prism software (v5.0 GraphPad).
Supplementary information
Acknowledgements
The authors wish to thank Luigi Celauro (SISSA) for technical support in RT-QuIC substrates preparation and Rebecca Davidson (Norwegian Veterinary Institute) for critical review of the manuscript. This study was supported in part by the Italian Ministry of Health (GR-2013–02355724 and RC) and Associazione Italiana Encefalopatie da Prioni (A.I.En.P.) to FM and by the Norwegian Directorate of Agriculture (Reindeer Husbandry Development Fund) project 17/20695-11 to SLB.
Author contributions
E.B., T.T.V., S.L.B. and F.M. designed the experiments and E.B., T.T.V., L.T. and F.A.C. performed the practical work. G.S. produced the recombinant proteins. E.B., T.T.V., S.L.B. and F.M. wrote the manuscript and E.B., T.T.V., G.L., G.G., S.L.B. and F.M. critically revised it. All the authors read and approved the final manuscript.
Data availability
All data generated or analyzed during this study are included in this published article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Edoardo Bistaffa and Tram Thu Vuong.
Supplementary information
is available for this paper at 10.1038/s41598-019-55078-x.
References
- 1.Haley NJ, Hoover EA. Chronic wasting disease of cervids: current knowledge and future perspectives. Annu Rev Anim Biosci. 2015;3:305–325. doi: 10.1146/annurev-animal-022114-111001. [DOI] [PubMed] [Google Scholar]
- 2.Sohn HJ, et al. A case of chronic wasting disease in an elk imported to Korea from Canada. J Vet Med Sci. 2002;64:855–858. doi: 10.1292/jvms.64.855. [DOI] [PubMed] [Google Scholar]
- 3.Benestad SL, Mitchell G, Simmons M, Ytrehus B, Vikoren T. First case of chronic wasting disease in Europe in a Norwegian free-ranging reindeer. Vet Res. 2016;47:88. doi: 10.1186/s13567-016-0375-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Race B, Williams K, Chesebro B. Transmission studies of chronic wasting disease to transgenic mice overexpressing human prion protein using the RT-QuIC assay. Vet Res. 2019;50:6. doi: 10.1186/s13567-019-0626-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Osterholm, M. T. et al. Chronic Wasting Disease in Cervids: Implications for Prion Transmission to Humans and Other Animal Species. MBio10, 10.1128/mBio.01091-19 (2019). [DOI] [PMC free article] [PubMed]
- 6.Williams ES, Young S. Neuropathology of chronic wasting disease of mule deer (Odocoileus hemionus) and elk (Cervus elaphus nelsoni) Vet Pathol. 1993;30:36–45. doi: 10.1177/030098589303000105. [DOI] [PubMed] [Google Scholar]
- 7.Samuel MD, Storm DJ. Chronic wasting disease in white-tailed deer: infection, mortality, and implications for heterogeneous transmission. Ecology. 2016;97:3195–3205. doi: 10.1002/ecy.1538. [DOI] [PubMed] [Google Scholar]
- 8.Ball K. Chronic wasting disease in a Rocky Mountain elk. Can Vet J. 2002;43:880–882. [PMC free article] [PubMed] [Google Scholar]
- 9.Pirisinu L, et al. Novel Type of Chronic Wasting Disease Detected in Moose (Alces alces), Norway. Emerg Infect Dis. 2018;24:2210–2218. doi: 10.3201/eid2412.180702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saunders SE, Bartelt-Hunt SL, Bartz JC. Occurrence, transmission, and zoonotic potential of chronic wasting disease. Emerg Infect Dis. 2012;18:369–376. doi: 10.3201/eid1803.110685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moore SJ, et al. Horizontal Transmission of Chronic Wasting Disease in Reindeer. Emerg Infect Dis. 2016;22:2142–2145. doi: 10.3201/eid2212.160635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilch S, et al. Chronic wasting disease. Top Curr Chem. 2011;305:51–77. doi: 10.1007/128_2011_159. [DOI] [PubMed] [Google Scholar]
- 13.Prusiner SB. Novel proteinaceous infectious particles cause scrapie. Science. 1982;216:136–144. doi: 10.1126/science.6801762. [DOI] [PubMed] [Google Scholar]
- 14.Spraker TR, et al. Spongiform encephalopathy in free-ranging mule deer (Odocoileus hemionus), white-tailed deer (Odocoileus virginianus) and Rocky Mountain elk (Cervus elaphus nelsoni) in northcentral Colorado. J Wildl Dis. 1997;33:1–6. doi: 10.7589/0090-3558-33.1.1. [DOI] [PubMed] [Google Scholar]
- 15.Spraker TR, et al. Distribution of protease-resistant prion protein and spongiform encephalopathy in free-ranging mule deer (Odocoileus hemionus) with chronic wasting disease. Vet Pathol. 2002;39:546–556. doi: 10.1354/vp.39-5-546. [DOI] [PubMed] [Google Scholar]
- 16.Williams ES. Scrapie and chronic wasting disease. Clin Lab Med. 2003;23:139–159. doi: 10.1016/S0272-2712(02)00040-9. [DOI] [PubMed] [Google Scholar]
- 17.Williams ES, Young S. Spongiform encephalopathies in Cervidae. Rev Sci Tech. 1992;11:551–567. doi: 10.20506/rst.11.2.611. [DOI] [PubMed] [Google Scholar]
- 18.Williams ES, Young S. Spongiform encephalopathy of Rocky Mountain elk. J Wildl Dis. 1982;18:465–471. doi: 10.7589/0090-3558-18.4.465. [DOI] [PubMed] [Google Scholar]
- 19.Legname G. Elucidating the function of the prion protein. PLoS Pathog. 2017;13:e1006458. doi: 10.1371/journal.ppat.1006458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen FE, Prusiner SB. Pathologic conformations of prion proteins. Annu Rev Biochem. 1998;67:793–819. doi: 10.1146/annurev.biochem.67.1.793. [DOI] [PubMed] [Google Scholar]
- 21.Prusiner SB. Molecular biology of prion diseases. Science. 1991;252:1515–1522. doi: 10.1126/science.1675487. [DOI] [PubMed] [Google Scholar]
- 22.Mabbott Neil. How do PrPSc Prions Spread between Host Species, and within Hosts? Pathogens. 2017;6(4):60. doi: 10.3390/pathogens6040060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller MW, Williams ES, Hobbs NT, Wolfe LL. Environmental sources of prion transmission in mule deer. Emerg Infect Dis. 2004;10:1003–1006. doi: 10.3201/eid1006.040010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Selariu A, et al. In utero transmission and tissue distribution of chronic wasting disease-associated prions in free-ranging Rocky Mountain elk. J Gen Virol. 2015;96:3444–3455. doi: 10.1099/jgv.0.000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Otero A, et al. Prion protein polymorphisms associated with reduced CWD susceptibility limit peripheral PrP(CWD) deposition in orally infected white-tailed deer. BMC Vet Res. 2019;15:50. doi: 10.1186/s12917-019-1794-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Rourke KI, et al. PrP genotypes of captive and free-ranging Rocky Mountain elk (Cervus elaphus nelsoni) with chronic wasting disease. J Gen Virol. 1999;80(Pt 10):2765–2769. doi: 10.1099/0022-1317-80-10-2765. [DOI] [PubMed] [Google Scholar]
- 27.O’Rourke KI, et al. Polymorphisms in the prion precursor functional gene but not the pseudogene are associated with susceptibility to chronic wasting disease in white-tailed deer. J Gen Virol. 2004;85:1339–1346. doi: 10.1099/vir.0.79785-0. [DOI] [PubMed] [Google Scholar]
- 28.Johnson C, et al. Prion protein polymorphisms in white-tailed deer influence susceptibility to chronic wasting disease. J Gen Virol. 2006;87:2109–2114. doi: 10.1099/vir.0.81615-0. [DOI] [PubMed] [Google Scholar]
- 29.Wilson GA, et al. Polymorphisms at the PRNP gene influence susceptibility to chronic wasting disease in two species of deer (Odocoileus Spp.) in western Canada. J Toxicol Environ Health A. 2009;72:1025–1029. doi: 10.1080/15287390903084264. [DOI] [PubMed] [Google Scholar]
- 30.Johnson CJ, et al. Prion protein polymorphisms affect chronic wasting disease progression. PLoS One. 2011;6:e17450. doi: 10.1371/journal.pone.0017450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wik L, et al. Polymorphisms and variants in the prion protein sequence of European moose (Alces alces), reindeer (Rangifer tarandus), roe deer (Capreolus capreolus) and fallow deer (Dama dama) in Scandinavia. Prion. 2012;6:256–260. doi: 10.4161/pri.19641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jewell JE, Conner MM, Wolfe LL, Miller MW, Williams ES. Low frequency of PrP genotype 225SF among free-ranging mule deer (Odocoileus hemionus) with chronic wasting disease. J Gen Virol. 2005;86:2127–2134. doi: 10.1099/vir.0.81077-0. [DOI] [PubMed] [Google Scholar]
- 33.O’Rourke KI, et al. Elk with a long incubation prion disease phenotype have a unique PrPd profile. Neuroreport. 2007;18:1935–1938. doi: 10.1097/WNR.0b013e3282f1ca2f. [DOI] [PubMed] [Google Scholar]
- 34.Robinson SJ, Samuel MD, O’Rourke KI, Johnson CJ. The role of genetics in chronic wasting disease of North American cervids. Prion. 2012;6:153–162. doi: 10.4161/pri.19640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Angers RC, et al. Prion strain mutation determined by prion protein conformational compatibility and primary structure. Science. 2010;328:1154–1158. doi: 10.1126/science.1187107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Perrott MR, Sigurdson CJ, Mason GL, Hoover EA. Evidence for distinct chronic wasting disease (CWD) strains in experimental CWD in ferrets. J Gen Virol. 2012;93:212–221. doi: 10.1099/vir.0.035006-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bian J, et al. Primary structural differences at residue 226 of deer and elk PrP dictate selection of distinct CWD prion strains in gene-targeted mice. Proc Natl Acad Sci USA. 2019;116:12478–12487. doi: 10.1073/pnas.1903947116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bessen RA, Marsh RF. Identification of two biologically distinct strains of transmissible mink encephalopathy in hamsters. J Gen Virol. 1992;73(Pt 2):329–334. doi: 10.1099/0022-1317-73-2-329. [DOI] [PubMed] [Google Scholar]
- 39.Bessen RA, Marsh RF. Distinct PrP properties suggest the molecular basis of strain variation in transmissible mink encephalopathy. J Virol. 1994;68:7859–7868. doi: 10.1128/jvi.68.12.7859-7868.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bruce ME, Fraser H. Scrapie strain variation and its implications. Curr Top Microbiol Immunol. 1991;172:125–138. doi: 10.1007/978-3-642-76540-7_8. [DOI] [PubMed] [Google Scholar]
- 41.Bruce ME. Scrapie strain variation and mutation. Br Med Bull. 1993;49:822–838. doi: 10.1093/oxfordjournals.bmb.a072649. [DOI] [PubMed] [Google Scholar]
- 42.Bruce ME, McConnell I, Fraser H, Dickinson AG. The disease characteristics of different strains of scrapie in Sinc congenic mouse lines: implications for the nature of the agent and host control of pathogenesis. J Gen Virol. 1991;72(Pt 3):595–603. doi: 10.1099/0022-1317-72-3-595. [DOI] [PubMed] [Google Scholar]
- 43.Fraser H, Dickinson AG. Scrapie in mice. Agent-strain differences in the distribution and intensity of grey matter vacuolation. J Comp Pathol. 1973;83:29–40. doi: 10.1016/0021-9975(73)90024-8. [DOI] [PubMed] [Google Scholar]
- 44.Herbst A, Velasquez CD, Triscott E, Aiken JM, McKenzie D. Chronic Wasting Disease Prion Strain Emergence and Host Range Expansion. Emerg Infect Dis. 2017;23:1598–1600. doi: 10.3201/eid2309.161474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Duque Velasquez C, et al. Deer Prion Proteins Modulate the Emergence and Adaptation of Chronic Wasting Disease Strains. J Virol. 2015;89:12362–12373. doi: 10.1128/JVI.02010-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Meyerett C, et al. In vitro strain adaptation of CWD prions by serial protein misfolding cyclic amplification. Virology. 2008;382:267–276. doi: 10.1016/j.virol.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 47.Peters J, Miller JM, Jenny AL, Peterson TL, Carmichael KP. Immunohistochemical diagnosis of chronic wasting disease in preclinically affected elk from a captive herd. J Vet Diagn Invest. 2000;12:579–582. doi: 10.1177/104063870001200618. [DOI] [PubMed] [Google Scholar]
- 48.Sigurdson CJ, et al. Oral transmission and early lymphoid tropism of chronic wasting disease PrPres in mule deer fawns (Odocoileus hemionus) J Gen Virol. 1999;80(Pt 10):2757–2764. doi: 10.1099/0022-1317-80-10-2757. [DOI] [PubMed] [Google Scholar]
- 49.Keane DP, et al. Comparison of retropharyngeal lymph node and obex region of the brainstem in detection of chronic wasting disease in white-tailed deer (Odocoileus virginianus) J Vet Diagn Invest. 2008;20:58–60. doi: 10.1177/104063870802000110. [DOI] [PubMed] [Google Scholar]
- 50.Guiroy DC, Williams ES, Yanagihara R, Gajdusek DC. Topographic distribution of scrapie amyloid-immunoreactive plaques in chronic wasting disease in captive mule deer (Odocoileus hemionus hemionus) Acta Neuropathol. 1991;81:475–478. doi: 10.1007/BF00310125. [DOI] [PubMed] [Google Scholar]
- 51.Guiroy DC, Williams ES, Song KJ, Yanagihara R, Gajdusek DC. Fibrils in brain of Rocky Mountain elk with chronic wasting disease contain scrapie amyloid. Acta Neuropathol. 1993;86:77–80. doi: 10.1007/BF00454902. [DOI] [PubMed] [Google Scholar]
- 52.Hibler CP, et al. Field validation and assessment of an enzyme-linked immunosorbent assay for detecting chronic wasting disease in mule deer (Odocoileus hemionus), white-tailed deer (Odocoileus virginianus), and Rocky Mountain elk (Cervus elaphus nelsoni) J Vet Diagn Invest. 2003;15:311–319. doi: 10.1177/104063870301500402. [DOI] [PubMed] [Google Scholar]
- 53.Fox KA, Jewell JE, Williams ES, Miller MW. Patterns of PrPCWD accumulation during the course of chronic wasting disease infection in orally inoculated mule deer (Odocoileus hemionus) J Gen Virol. 2006;87:3451–3461. doi: 10.1099/vir.0.81999-0. [DOI] [PubMed] [Google Scholar]
- 54.van Keulen LJ, et al. Immunohistochemical detection of prion protein in lymphoid tissues of sheep with natural scrapie. J Clin Microbiol. 1996;34:1228–1231. doi: 10.1128/jcm.34.5.1228-1231.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wild MA, Spraker TR, Sigurdson CJ, O’Rourke KI, Miller MW. Preclinical diagnosis of chronic wasting disease in captive mule deer (Odocoileus hemionus) and white-tailed deer (Odocoileus virginianus) using tonsillar biopsy. J Gen Virol. 2002;83:2629–2634. doi: 10.1099/0022-1317-83-10-2629. [DOI] [PubMed] [Google Scholar]
- 56.Keane D, et al. Validation of use of rectoanal mucosa-associated lymphoid tissue for immunohistochemical diagnosis of chronic wasting disease in white-tailed deer (Odocoileus virginianus) J Clin Microbiol. 2009;47:1412–1417. doi: 10.1128/JCM.02209-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wolfe LL, et al. PrPCWD in rectal lymphoid tissue of deer (Odocoileus spp.) J Gen Virol. 2007;88:2078–2082. doi: 10.1099/vir.0.82342-0. [DOI] [PubMed] [Google Scholar]
- 58.Spraker TR, Balachandran A, Zhuang D, O’Rourke KI. Variable patterns of distribution of PrP(CWD) in the obex and cranial lymphoid tissues of Rocky Mountain elk (Cervus elaphus nelsoni) with subclinical chronic wasting disease. Vet Rec. 2004;155:295–302. doi: 10.1136/vr.155.10.295. [DOI] [PubMed] [Google Scholar]
- 59.Monello RJ, et al. Efficacy of antemortem rectal biopsies to diagnose and estimate prevalence of chronic wasting disease in free-ranging cow elk (Cervus elaphus nelsoni) J Wildl Dis. 2013;49:270–278. doi: 10.7589/2011-12-362. [DOI] [PubMed] [Google Scholar]
- 60.Davenport KA, et al. Comparative analysis of prions in nervous and lymphoid tissues of chronic wasting disease-infected cervids. J Gen Virol. 2018;99:753–758. doi: 10.1099/jgv.0.001053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.EFSA Panel on Biological Hazards (BIOHAZ)Antonia. R. et al. Scientific opinion on chronic wasting disease (II). EFSA Journal, 10.2903/j.efsa.2018.5132 (2017).
- 62.Bae SE, Jung S, Kim HY, Son HS. Correlation analysis for the incubation period of prion disease. Prion. 2012;6:276–281. doi: 10.4161/pri.19638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gibbs CJ, Jr., et al. Creutzfeldt-Jakob disease (spongiform encephalopathy): transmission to the chimpanzee. Science. 1968;161:388–389. doi: 10.1126/science.161.3839.388. [DOI] [PubMed] [Google Scholar]
- 64.Prusiner SB, et al. Transgenetic studies implicate interactions between homologous PrP isoforms in scrapie prion replication. Cell. 1990;63:673–686. doi: 10.1016/0092-8674(90)90134-Z. [DOI] [PubMed] [Google Scholar]
- 65.Giles Kurt, Woerman Amanda L., Berry David B., Prusiner Stanley B. Bioassays and Inactivation of Prions. Cold Spring Harbor Perspectives in Biology. 2017;9(8):a023499. doi: 10.1101/cshperspect.a023499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Boerner S, Wagenfuhr K, Daus ML, Thomzig A, Beekes M. Towards further reduction and replacement of animal bioassays in prion research by cell and protein misfolding cyclic amplification assays. Lab Anim. 2013;47:106–115. doi: 10.1177/0023677213476856. [DOI] [PubMed] [Google Scholar]
- 67.Daus ML, et al. Presence and seeding activity of pathological prion protein (PrP(TSE)) in skeletal muscles of white-tailed deer infected with chronic wasting disease. PLoS One. 2011;6:e18345. doi: 10.1371/journal.pone.0018345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pulford B, et al. Detection of PrPCWD in feces from naturally exposed Rocky Mountain elk (Cervus elaphus nelsoni) using protein misfolding cyclic amplification. J Wildl Dis. 2012;48:425–434. doi: 10.7589/0090-3558-48.2.425. [DOI] [PubMed] [Google Scholar]
- 69.Denkers ND, Henderson DM, Mathiason CK, Hoover EA. Enhanced prion detection in biological samples by magnetic particle extraction and real-time quaking-induced conversion. J Gen Virol. 2016;97:2023–2029. doi: 10.1099/jgv.0.000515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Davenport, K. A., Hoover, C. E., Denkers, N. D., Mathiason, C. K. & Hoover, E. A. Modified Protein Misfolding Cyclic Amplification Overcomes Real-Time Quaking-Induced Conversion Assay Inhibitors in Deer Saliva To Detect Chronic Wasting Disease Prions. J Clin Microbiol56, 10.1128/JCM.00947-18 (2018). [DOI] [PMC free article] [PubMed]
- 71.Haley NJ, et al. Prion-seeding activity in cerebrospinal fluid of deer with chronic wasting disease. PLoS One. 2013;8:e81488. doi: 10.1371/journal.pone.0081488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kramm C, et al. Detection of Prions in Blood of Cervids at the Asymptomatic Stage of Chronic Wasting Disease. Sci Rep. 2017;7:17241. doi: 10.1038/s41598-017-17090-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Haley NJ, Mathiason CK, Zabel MD, Telling GC, Hoover EA. Detection of sub-clinical CWD infection in conventional test-negative deer long after oral exposure to urine and feces from CWD+ deer. PLoS One. 2009;4:e7990. doi: 10.1371/journal.pone.0007990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Atarashi R, et al. Simplified ultrasensitive prion detection by recombinant PrP conversion with shaking. Nat Methods. 2008;5:211–212. doi: 10.1038/nmeth0308-211. [DOI] [PubMed] [Google Scholar]
- 75.Haley NJ, et al. Antemortem Detection of Chronic Wasting Disease Prions in Nasal Brush Collections and Rectal Biopsy Specimens from White-Tailed Deer by Real-Time Quaking-Induced Conversion. J Clin Microbiol. 2016;54:1108–1116. doi: 10.1128/JCM.02699-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Haley NJ, et al. Seeded Amplification of Chronic Wasting Disease Prions in Nasal Brushings and Recto-anal Mucosa-Associated Lymphoid Tissues from Elk by Real-Time Quaking-Induced Conversion. J Clin Microbiol. 2016;54:1117–1126. doi: 10.1128/JCM.02700-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Elder AM, et al. In vitro detection of prionemia in TSE-infected cervids and hamsters. PLoS One. 2013;8:e80203. doi: 10.1371/journal.pone.0080203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Henderson DM, et al. Longitudinal Detection of Prion Shedding in Saliva and Urine by Chronic Wasting Disease-Infected Deer by Real-Time Quaking-Induced Conversion. J Virol. 2015;89:9338–9347. doi: 10.1128/JVI.01118-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Henderson DM, et al. Rapid antemortem detection of CWD prions in deer saliva. PLoS One. 2013;8:e74377. doi: 10.1371/journal.pone.0074377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.John TR, Schatzl HM, Gilch S. Early detection of chronic wasting disease prions in urine of pre-symptomatic deer by real-time quaking-induced conversion assay. Prion. 2013;7:253–258. doi: 10.4161/pri.24430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cheng YC, et al. Early and Non-Invasive Detection of Chronic Wasting Disease Prions in Elk Feces by Real-Time Quaking Induced Conversion. PLoS One. 2016;11:e0166187. doi: 10.1371/journal.pone.0166187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Henderson DM, et al. Detection of chronic wasting disease prion seeding activity in deer and elk feces by real-time quaking-induced conversion. J Gen Virol. 2017;98:1953–1962. doi: 10.1099/jgv.0.000844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Moreno Julie A., Telling Glenn C. Molecular Mechanisms of Chronic Wasting Disease Prion Propagation. Cold Spring Harbor Perspectives in Medicine. 2017;8(6):a024448. doi: 10.1101/cshperspect.a024448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Denkers ND, Seelig DM, Telling GC, Hoover EA. Aerosol and nasal transmission of chronic wasting disease in cervidized mice. J Gen Virol. 2010;91:1651–1658. doi: 10.1099/vir.0.017335-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Haley NJ, Seelig DM, Zabel MD, Telling GC, Hoover EA. Detection of CWD prions in urine and saliva of deer by transgenic mouse bioassay. PLoS One. 2009;4:e4848. doi: 10.1371/journal.pone.0004848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Haley NJ, et al. Detection of chronic wasting disease prions in salivary, urinary, and intestinal tissues of deer: potential mechanisms of prion shedding and transmission. J Virol. 2011;85:6309–6318. doi: 10.1128/JVI.00425-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mathiason CK, et al. Infectious prions in the saliva and blood of deer with chronic wasting disease. Science. 2006;314:133–136. doi: 10.1126/science.1132661. [DOI] [PubMed] [Google Scholar]
- 88.Pritzkow S, et al. Grass plants bind, retain, uptake, and transport infectious prions. Cell Rep. 2015;11:1168–1175. doi: 10.1016/j.celrep.2015.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hannaoui S, Schatzl HM, Gilch S. Chronic wasting disease: Emerging prions and their potential risk. PLoS Pathog. 2017;13:e1006619. doi: 10.1371/journal.ppat.1006619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gough KC, Maddison BC. Prion transmission: prion excretion and occurrence in the environment. Prion. 2010;4:275–282. doi: 10.4161/pri.4.4.13678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Almberg ES, Cross PC, Johnson CJ, Heisey DM, Richards BJ. Modeling routes of chronic wasting disease transmission: environmental prion persistence promotes deer population decline and extinction. PLoS One. 2011;6:e19896. doi: 10.1371/journal.pone.0019896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Denkers ND, Telling GC, Hoover EA. Minor oral lesions facilitate transmission of chronic wasting disease. J Virol. 2011;85:1396–1399. doi: 10.1128/JVI.01655-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Johnson CJ, et al. Prions adhere to soil minerals and remain infectious. PLoS Pathog. 2006;2:e32. doi: 10.1371/journal.ppat.0020032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hill AF, et al. Species-barrier-independent prion replication in apparently resistant species. Proc Natl Acad Sci USA. 2000;97:10248–10253. doi: 10.1073/pnas.97.18.10248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bistaffa E, Rossi M, De Luca CMG, Moda F. Biosafety of Prions. Prog Mol Biol Transl Sci. 2017;150:455–485. doi: 10.1016/bs.pmbts.2017.06.017. [DOI] [PubMed] [Google Scholar]
- 96.Rossi Marcello, Baiardi Simone, Parchi Piero. Understanding Prion Strains: Evidence from Studies of the Disease Forms Affecting Humans. Viruses. 2019;11(4):309. doi: 10.3390/v11040309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Orrú Christina, Hughson Andrew, Groveman Bradley, Campbell Katrina, Anson Kelsie, Manca Matteo, Kraus Allison, Caughey Byron. Factors That Improve RT-QuIC Detection of Prion Seeding Activity. Viruses. 2016;8(5):140. doi: 10.3390/v8050140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.CDC. https://www.cdc.gov/prions/cwd/occurrence.html.
- 99.Fediaevsky A, et al. A descriptive study of the prevalence of atypical and classical scrapie in sheep in 20 European countries. BMC Vet Res. 2008;4:19. doi: 10.1186/1746-6148-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Orru CD, et al. Bank Vole Prion Protein As an Apparently Universal Substrate for RT-QuIC-Based Detection and Discrimination of Prion Strains. PLoS Pathog. 2015;11:e1004983. doi: 10.1371/journal.ppat.1004983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kaluz S, Kaluzova M, Flint AP. Sequencing analysis of prion genes from red deer and camel. Gene. 1997;199:283–286. doi: 10.1016/s0378-1119(97)00382-x. [DOI] [PubMed] [Google Scholar]
- 102.Cervenakova L, Rohwer R, Williams S, Brown P, Gajdusek DC. High sequence homology of the PrP gene in mule deer and Rocky Mountain elk. Lancet. 1997;350:219–220. doi: 10.1016/s0140-6736(05)62387-2. [DOI] [PubMed] [Google Scholar]
- 103.Orru CD, et al. A test for Creutzfeldt-Jakob disease using nasal brushings. N Engl J Med. 2014;371:519–529. doi: 10.1056/NEJMoa1315200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Franceschini A, et al. High diagnostic value of second generation CSF RT-QuIC across the wide spectrum of CJD prions. Sci Rep. 2017;7:10655. doi: 10.1038/s41598-017-10922-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Redaelli V, et al. Detection of prion seeding activity in the olfactory mucosa of patients with Fatal Familial Insomnia. Sci Rep. 2017;7:46269. doi: 10.1038/srep46269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.McGuire LI, et al. Real time quaking-induced conversion analysis of cerebrospinal fluid in sporadic Creutzfeldt-Jakob disease. Ann Neurol. 2012;72:278–285. doi: 10.1002/ana.23589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.McGuire LI, et al. Cerebrospinal fluid real-time quaking-induced conversion is a robust and reliable test for sporadic creutzfeldt-jakob disease: An international study. Ann Neurol. 2016;80:160–165. doi: 10.1002/ana.24679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Abrams JY, Maddox RA, Harvey AR, Schonberger LB, Belay ED. Travel history, hunting, and venison consumption related to prion disease exposure, 2006-2007 FoodNet Population Survey. J Am Diet Assoc. 2011;111:858–863. doi: 10.1016/j.jada.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 109.Kurt TD, Sigurdson CJ. Cross-species transmission of CWD prions. Prion. 2016;10:83–91. doi: 10.1080/19336896.2015.1118603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Belay ED, et al. Chronic wasting disease and potential transmission to humans. Emerg Infect Dis. 2004;10:977–984. doi: 10.3201/eid1006.031082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Williams ES, O’Toole D, Miller MW, Kreeger TJ, Jewell JE. Cattle (Bos Taurus) Resist Chronic Wasting Disease Following Oral Inoculation Challenge or Ten Years’ Natural Exposure in Contaminated Environments. J Wildl Dis. 2018;54:460–470. doi: 10.7589/2017-12-299. [DOI] [PubMed] [Google Scholar]
- 112.Beringue V, Vilotte JL, Laude H. Prion agent diversity and species barrier. Vet Res. 2008;39:47. doi: 10.1051/vetres:2008024. [DOI] [PubMed] [Google Scholar]
- 113.Sigurdson CJ. A prion disease of cervids: chronic wasting disease. Vet Res. 2008;39:41. doi: 10.1051/vetres:2008018. [DOI] [PubMed] [Google Scholar]
- 114.Hamir AN, et al. Experimental transmission of chronic wasting disease agent from mule deer to cattle by the intracerebral route. J Vet Diagn Invest. 2005;17:276–281. doi: 10.1177/104063870501700313. [DOI] [PubMed] [Google Scholar]
- 115.Harrington RD, et al. A species barrier limits transmission of chronic wasting disease to mink (Mustela vison) J Gen Virol. 2008;89:1086–1096. doi: 10.1099/vir.0.83422-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Marsh RF, Kincaid AE, Bessen RA, Bartz JC. Interspecies transmission of chronic wasting disease prions to squirrel monkeys (Saimiri sciureus) J Virol. 2005;79:13794–13796. doi: 10.1128/JVI.79.21.13794-13796.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Race B, et al. Chronic wasting disease agents in nonhuman primates. Emerg Infect Dis. 2014;20:833–837. doi: 10.3201/eid2005.130778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hamir AN, et al. Transmission of chronic wasting disease of mule deer to Suffolk sheep following intracerebral inoculation. J Vet Diagn Invest. 2006;18:558–565. doi: 10.1177/104063870601800606. [DOI] [PubMed] [Google Scholar]
- 119.Sandberg MK, et al. Chronic wasting disease prions are not transmissible to transgenic mice overexpressing human prion protein. J Gen Virol. 2010;91:2651–2657. doi: 10.1099/vir.0.024380-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Race B, et al. Susceptibilities of nonhuman primates to chronic wasting disease. Emerg Infect Dis. 2009;15:1366–1376. doi: 10.3201/eid1509.090253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kurt TD, et al. Human prion protein sequence elements impede cross-species chronic wasting disease transmission. J Clin Invest. 2015;125:1485–1496. doi: 10.1172/JCI79408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Barria MA, Libori A, Mitchell G, Head MW. Susceptibility of Human Prion Protein to Conversion by Chronic Wasting Disease Prions. Emerg Infect Dis. 2018;24:1482–1489. doi: 10.3201/eid2408.161888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Barria MA, Telling GC, Gambetti P, Mastrianni JA, Soto C. Generation of a new form of human PrP(Sc) in vitro by interspecies transmission from cervid prions. J Biol Chem. 2011;286:7490–7495. doi: 10.1074/jbc.M110.198465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Davenport KA, et al. Insights into Chronic Wasting Disease and Bovine Spongiform Encephalopathy Species Barriers by Use of Real-Time Conversion. J Virol. 2015;89:9524–9531. doi: 10.1128/JVI.01439-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Luers L, et al. Seeded fibrillation as molecular basis of the species barrier in human prion diseases. PLoS One. 2013;8:e72623. doi: 10.1371/journal.pone.0072623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Bartz JC, Bessen RA, McKenzie D, Marsh RF, Aiken JM. Adaptation and selection of prion protein strain conformations following interspecies transmission of transmissible mink encephalopathy. J Virol. 2000;74:5542–5547. doi: 10.1128/jvi.74.12.5542-5547.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Padilla D, et al. Sheep and goat BSE propagate more efficiently than cattle BSE in human PrP transgenic mice. PLoS Pathog. 2011;7:e1001319. doi: 10.1371/journal.ppat.1001319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hill AF, et al. The same prion strain causes vCJD and BSE. Nature. 1997;389(448-450):526. doi: 10.1038/38925. [DOI] [PubMed] [Google Scholar]
- 129.Waddell L, et al. Current evidence on the transmissibility of chronic wasting disease prions to humans-A systematic review. Transbound Emerg Dis. 2018;65:37–49. doi: 10.1111/tbed.12612. [DOI] [PubMed] [Google Scholar]
- 130.Wilham JM, et al. Rapid end-point quantitation of prion seeding activity with sensitivity comparable to bioassays. PLoS Pathog. 2010;6:e1001217. doi: 10.1371/journal.ppat.1001217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Haley NJ, et al. Detection of chronic wasting disease in the lymph nodes of free-ranging cervids by real-time quaking-induced conversion. J Clin Microbiol. 2014;52:3237–3243. doi: 10.1128/JCM.01258-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Henderson DM, et al. Quantitative assessment of prion infectivity in tissues and body fluids by real-time quaking-induced conversion. J Gen Virol. 2015;96:210–219. doi: 10.1099/vir.0.069906-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hoover, C. E. et al. Pathways of Prion Spread during Early Chronic Wasting Disease in Deer. J Virol91, 10.1128/JVI.00077-17 (2017). [DOI] [PMC free article] [PubMed]
- 134.Nalls, A. V. et al. Infectious Prions in the Pregnancy Microenvironment of Chronic Wasting Disease-Infected Reeves’ Muntjac Deer. J Virol91, 10.1128/JVI.00501-17 (2017). [DOI] [PMC free article] [PubMed]
- 135.Hannaoui S, et al. Destabilizing polymorphism in cervid prion protein hydrophobic core determines prion conformation and conversion efficiency. PLoS Pathog. 2017;13:e1006553. doi: 10.1371/journal.ppat.1006553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Davenport KA, et al. PrPC expression and prion seeding activity in the alimentary tract and lymphoid tissue of deer. PLoS One. 2017;12:e0183927. doi: 10.1371/journal.pone.0183927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Manne S, et al. Ante-mortem detection of chronic wasting disease in recto-anal mucosa-associated lymphoid tissues from elk (Cervus elaphus nelsoni) using real-time quaking-induced conversion (RT-QuIC) assay: A blinded collaborative study. Prion. 2017;11:415–430. doi: 10.1080/19336896.2017.1368936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Davenport, K. A. et al. Assessment of Chronic Wasting Disease Prion Shedding in Deer Saliva with Occupancy Modeling. J Clin Microbiol56, 10.1128/JCM.01243-17 (2018). [DOI] [PMC free article] [PubMed]
- 139.Haley NJ, et al. Estimating chronic wasting disease susceptibility in cervids using real-time quaking-induced conversion. J Gen Virol. 2017;98:2882–2892. doi: 10.1099/jgv.0.000952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Haley NJ, et al. Chronic wasting disease management in ranched elk using rectal biopsy testing. Prion. 2018;12:93–108. doi: 10.1080/19336896.2018.1436925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Moore SJ, et al. Pathologic and biochemical characterization of PrP(Sc) from elk with PRNP polymorphisms at codon 132 after experimental infection with the chronic wasting disease agent. BMC Vet Res. 2018;14:80. doi: 10.1186/s12917-018-1400-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.McNulty E, et al. Comparison of conventional, amplification and bio-assay detection methods for a chronic wasting disease inoculum pool. PLoS One. 2019;14:e0216621. doi: 10.1371/journal.pone.0216621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Cooper SK, et al. Detection of CWD in cervids by RT-QuIC assay of third eyelids. PLoS One. 2019;14:e0221654. doi: 10.1371/journal.pone.0221654. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article.