This cross-sectional study based on national data from 1998 through 2017 assesses the incidence and mechanisms of head and neck injuries associated with cell phone use, especially during activities such as walking and driving.
Key Points
Question
Is increasing cell phone use associated with the number of head and neck injuries in the United States?
Findings
In this cross-sectional study based on a sample of 2501 reported cases from a national database (76 043 estimated weighted cases), the number of head and neck injuries related to cell phone use was found to have increased steadily over a recent 20-year period.
Meaning
This study’s findings suggest that growing dependence on cell phones in modern life may require that steps be taken to educate and promote safe practices for using these devices.
Abstract
Importance
As cell phones gain more influence in daily life, they also become potentially more hazardous. Injuries resulting from cell phone use have long been reported largely in the context of driving-related incidents, but other mechanisms of injury have been underreported.
Objective
To assess the incidence, types, and mechanisms of head and neck injuries associated with cell phone use.
Design, Setting, and Participants
Retrospective cross-sectional study using data from a national database of individuals with head and neck injuries related to cell phone use who presented to emergency departments in the United States between January 1998 and December 2017.
Main Outcomes and Measures
Incidence, types, and mechanisms of injury related to cell phone use in the US population.
Results
A reported total of 2501 patients (1129 [55.0%] female, 795 [38.8%] white, and 772 [37.6%] aged 13-29 years) presented with injuries of the head and neck related to cell phone use; the estimated weighted national total was 76 043 patients (42 846 females [56.3%], 34 894 [45.9%] white, and 29 956 [39.4%] aged 13-29 years). The most commonly reported subsites of injuries in the head and neck region included the head (33.1% of estimated total); face, including eyelid, eye area, and nose (32.7%); and neck (12.5%). The most common injury diagnoses included laceration (26.3% of estimated total), contusion/abrasion (24.5%), and internal organ injury (18.4%). Age group distributions showed that most injuries associated with cell phone user distraction occurred among individuals aged 13 to 29 years (60.3%; Cramer V = 0.29). In addition, those younger than 13 years were significantly more likely to sustain direct mechanical injury from a cell phone (82.1%) than to have a cell phone use–associated injury (17.9%) (Cramer V = 0.305), whereas a cell phone use–associated injury was more likely than a direct mechanical injury to occur among those aged 50 to 64 years (68.2% vs 31.8%; Cramer V = 0.11) and those older than 65 years (90.3% vs 9.7%; Cramer V = 0.29).
Conclusions and Relevance
Cell phone–related injuries to the head and neck have increased steeply over the recent 20-year period, with many cases resulting from distraction. Although the disposition of most cases is simple, some injuries bear a risk of long-term complications. Many of these injuries occurred among those aged 13 to 29 years and were associated with common activities, such as texting while walking. These findings suggest a need for patient education about injury prevention and the dangers of activity while using these devices.
Introduction
Since their invention, cell phones have played a major role in the daily lives of American adults. Approximately 96% of Americans own a cell phone, provoking interest in their role in causing injury. Given that head and neck traumas make up approximately 5% of emergency department (ED) visits in the United States, cell phone use in relation to such injuries could be of public health concern, in particular because of the psychological and financial burdens such injuries may entail.1,2,3 In addition, knowledge of the mechanism of injury is vital for patient risk stratification and trauma management,3 and understanding the mechanisms of common cell phone–related injuries can aid health care professionals in assessing patient needs. Health care professionals and public safety officials also must be aware of the epidemiologic nature of such injuries in order to provide adequate counseling and give input for legislation to protect the population.
The Consumer Product Safety Commission maintains the National Electronic Injury Surveillance System (NEISS) database, which collects data about ED visits from approximately 100 hospitals in the United States. The NEISS data are stratified on the basis of ED size and geographic location. The database provides information regarding injuries related to various categories of consumer products. Previously, the NEISS database has been used successfully to examine a number of patient characteristics, activities, and products associated with head and neck trauma.4,5,6
Methods
Database Overview
The NEISS database is available to the general public through the Consumer Product Safety Commission website.7 Individuals at participating institutions enter information extracted from daily ED records into the database using a specific set of guidelines that are outlined in the NEISS Coding Manual.8 All variables, including age, sex, race/ethnicity, body part injured, diagnosis and disposition, location where the event occurred, related product information, and narrative description of the event, are entered by the institution according to instructions outlined in the coding manual. These data are then compiled by the Consumer Product Safety Commission and made available on the NEISS website.7 This study was exempt from institutional review board approval because all patient data were deidentified as per the Rutgers New Jersey Medical School policy.
Case Selection and Analysis
The NEISS database was queried by using the “telephones or telephone accessories” category within the NEISS Estimates Query Builder to identify cases involving injuries related to the use of a cell phone. Cases involving injuries to the head and neck that occurred between January 1998 and December 2017 were included. Variables collected included patient demographics, diagnosis, site of injury, associated product, and a brief narrative description of the event. The narratives were then analyzed to obtain information regarding the specific device used and the mechanism of injury.
Narratives in the database are required to include “details about the product(s) and sequence of events.”8 These narratives were individually reviewed by 2 independent reviewers (N.G., A.B.L.). Cases in which the narrative explicitly or implicitly described the use of a cell phone (eg, “walking to school while using a phone”) were classified as cell phone-related injury cases; any other cases were classified as telephone-related injury cases. Only cases that were related specifically to a cell phone were included in the analysis. Cases in which the mechanism of injury was not specifically associated with a cell phone (eg, a syncopal episode while answering the telephone) were excluded from the study sample. Cases in which a device caused direct physical damage to the injured person (eg, a cell phone battery exploding or a cell phone hitting the face) were classified as direct mechanical (DM) injuries, whereas injuries associated with other factors (primarily distraction) were classified as cell phone use–associated (CPA) injuries. In cases in which there was no clear agreement on classification, a third reviewer (R.P.) adjudicated.
Categorization of events into the DM or CPA injury group was exclusive in that each event was assigned to only 1 category. However, the categorization of activities associated with each event was not limited to 1 category. For example, an event in which the narrative described an individual as texting while driving was included in the texting and driving categories concurrently. In addition, if the narrative about a specific event described an individual as being distracted by cell phone use, that event was broadly categorized as a case of distraction. The category of events due to distraction included those in which the narrative described 1 or more of the aforementioned activities (eg, texting while driving or walking) along with narratives where the distraction was evident but the specific activity could not be determined or was far less common (eg, playing a video game on a cell phone).
Statistical Analysis
The weight variable provided by the NEISS database was used to extrapolate an estimated number of nationwide cases from each reported case included in the analysis. Incidence was calculated by using national population estimates obtained from the US Census Bureau,9 and 95% CIs were calculated by using a 2-tailed mid-P exact test.10 Two-tailed χ2 testing was implemented for analysis of categorical variables. Effect size in χ2 analysis was calculated using the Cramer V.11 Level of association was interpreted as small (Cramer V = 0.10-0.30), medium (Cramer V = >0.30 to 0.50), or large (Cramer V > 0.50). Statistical analysis was performed using SPSS Statistics, version 23 (IBM).
Results
Between January 1998 and December 2017, a reported total of 2501 patients (1129 [55.0%] female, 795 [38.8%] white, and 772 [37.6%] aged 13-29 years) presented to EDs in the United States with injuries of the head and neck related to cell phone use; the estimated weighted national total was 76 043 patients (42 846 [56.3%] female, 34 894 [45.9%] white, and 29 956 [39.4%] aged 13-29 years). Patient demographic and clinical information is presented in Table 1. The largest proportion of incidents occurred at home (843 of 2051 reported events [41.1%]; 30 984 [40.7%] of the estimated weighted total), and the disposition of the majority of cases was treated and released or released without treatment (1923 of 2051 reported events [93.8%]; 71 559 [94.1%] of the estimated weighted total) (Table 1). The most common sites of injury were the head (33.1% of the estimated weighted total); the face, including the eyelid, eye area, and nose (32.7%); and the neck (12.5%). The most common injury diagnoses included laceration (26.3% of the estimated weighted total), contusion/abrasion (24.5%), and internal organ injury (18.4%) (Table 1).
Table 1. Clinical and Demographic Characteristics of Persons With Cell Phone–Related Injuries Occurring From 1998 Through 2017a.
| Characteristic | Reported Injuries, No. | Estimated National Total Injuries, No. (Weighted %) |
|---|---|---|
| Age, y | ||
| <13 | 463 | 12 360 (16.3) |
| 13-29 | 772 | 29 956 (39.4) |
| 30-49 | 392 | 16 095 (21.2) |
| 50-64 | 182 | 7884 (10.4) |
| ≥65 | 242 | 9747 (12.8) |
| Sex | ||
| Male | 922 | 33 197 (43.7) |
| Female | 1129 | 42 846 (56.3) |
| Race/ethnicity | ||
| Unknown | 702 | 24 507 (32.2) |
| White | 795 | 34 894 (45.9) |
| Black | 359 | 10 549 (13.9) |
| Other | 148 | 4749 (6.2) |
| Asian | 27 | 984 (1.3) |
| American Indian or Alaska Native | 3 | 213 (0.3) |
| Native Hawaiian or Pacific Islander | 2 | 146 (0.2) |
| Location | ||
| Not recorded | 666 | 24 919 (32.8) |
| Home | 843 | 30 984 (40.7) |
| Farm or ranch | 1 | 5 (0) |
| Street or highway | 342 | 13 357 (17.6) |
| Other public property | 150 | 5306 (7.0) |
| Industrial site | 1 | 16 (0) |
| School | 31 | 970 (1.3) |
| Recreational or sports venue | 17 | 486 (0.6) |
| Disposition | ||
| Treated and released or released without treatment | 1923 | 71 559 (94.1) |
| Treated and transferred to another hospital | 14 | 663 (0.9) |
| Treated and admitted | 90 | 2883 (3.8) |
| Admitted for observation | 5 | 104 (0.1) |
| Left against medical advice | 19 | 833 (1.1) |
| Body part injured | ||
| Head | 713 | 25 182 (33.1) |
| Face, including eyelid, eye area, and nose | 669 | 24 886 (32.7) |
| Neck | 226 | 9518 (12.5) |
| Eyeball | 217 | 8336 (11.0) |
| Mouth, including lips, tongue, and teeth | 145 | 4811 (6.3) |
| Ear | 81 | 3310 (4.4) |
| Diagnosis | ||
| Laceration | 575 | 19 989 (26.3) |
| Contusion or abrasion | 451 | 18 604 (24.5) |
| Internal organ injury | 394 | 13 965 (18.4) |
| Other or not stated | 319 | 10 782 (14.0) |
| Strain or sprain | 130 | 5824 (7.7) |
| Concussion | 67 | 2570 (3.4) |
| Foreign body | 59 | 2207 (2.9) |
| Fracture | 56 | 2102 (2.8) |
The total number of reported events was 2051, and the total estimated weighted number of events nationwide was 76 043. Category sums may not equal these totals because of missing data.
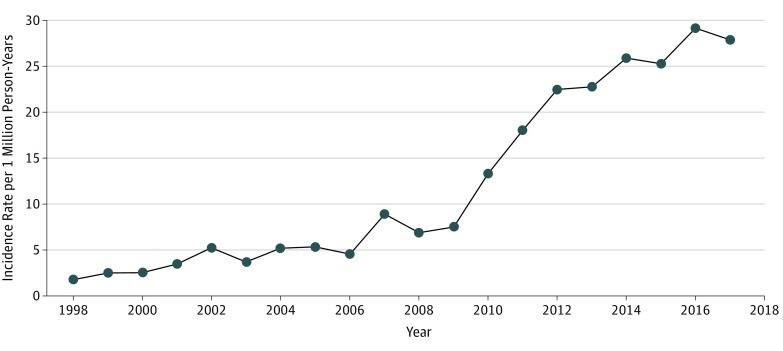
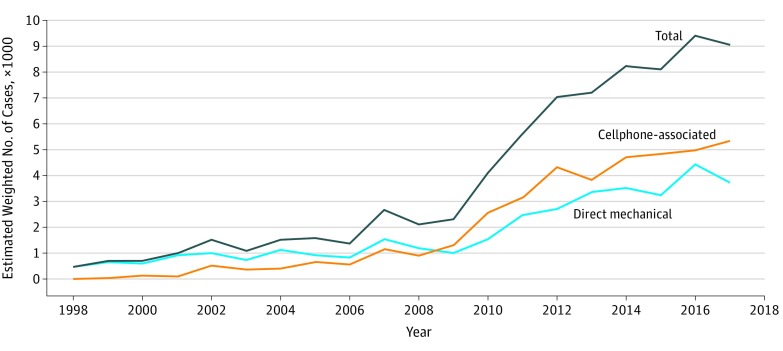
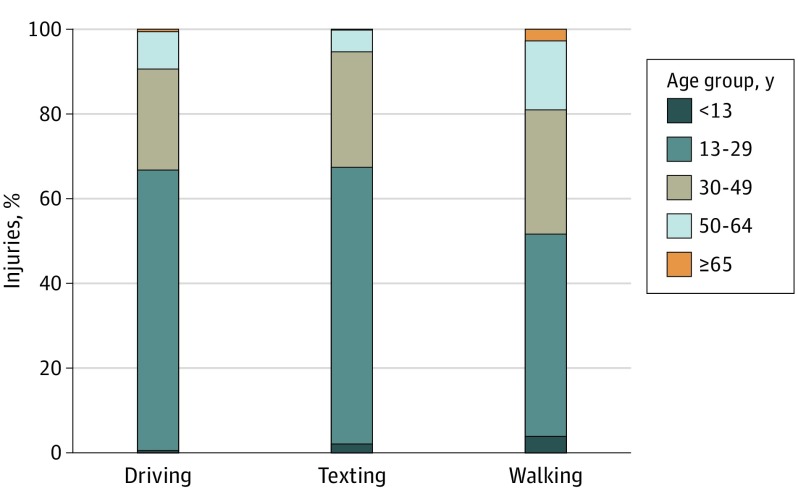
During this 20-year period, the incidence of cell phone–related injuries in the United States increased steadily, with a sharp increase occurring in 2007 at 8.99 new cases per 1 million person-years (95% CI, 8.66-9.34 reported cases; 2709 estimated weighted cases), followed by a much steeper increase to a peak of 29.19 new cases per 1 million person-years (95% CI, 28.61-29.79; 9431 estimated weighted cases) in 2016 (Figure 1, Figure 2, and eTable 1 in the Supplement). Direct mechanical injuries and CPA injuries followed similar trends over time (Figure 2). A total of 14 150 estimated weighted cases were due to distraction, as determined from the narratives provided. Of those 14 150 cases, 7240 occurred while the individual was driving and using a cell phone, 1022 while texting, and 5080 while walking and using a smartphone. In 90 of those 5080 cases, playing Pokémon Go (The Pokémon Company) was implicated as a reason for injury. Age group distributions showed that most injuries caused by distraction occurred among individuals aged 13 to 29 years (60.3%; Cramer V = 0.29) (Figure 3 and eTable 2 in the Supplement). In addition, those younger than 13 years were substantially more likely to sustain a DM injury than a CPA injury (82.1% vs 17.9%; Cramer V = 0.31), whereas a CPA injury was more likely to occur than a DM injury among those aged 50 to 64 years (68.2% vs 31.8%; Cramer V = 0.11) and those 65 years or older (90.3% vs 9.7%; Cramer V = 0.29) (Table 2).
Figure 1. Incidence of Cell Phone–Related Injuries From January 1998 Through December 2017.
Figure 2. Number of Reported Cell Phone–Related Injury Events, 1998 Through 2017.
Figure 3. Activities During Cell Phone Use–Associated (CPA) Injury by Age Group.
Percentages represent the proportion of all CPA injuries that occurred during the particular activity for each age group. For example, 23.8% of all CPA injuries while driving occurred in those aged 30 to 49 years. Cramer V for driving was 0.22; for texting, 0.18; and for walking, 0.13.
Table 2. Events by Injury Type and Age Group.
| Age, y | Events, Estimated Weighted National Total, No. (%) | Effect Size, Cramer V | |
|---|---|---|---|
| Direct Mechanical Injury (Reported n = 1012; Weighted n = 36 091) | Cell Phone Use–Associated Injury (Reported n = 1039; Weighted n = 39 952) | ||
| <13 | 10 146 (82.1) | 2214 (17.9) | 0.31 |
| 13-29 | 15 195 (50.7) | 14 761 (49.3) | 0.05 |
| 30-49 | 7302 (45.4) | 8793 (54.6) | 0.02 |
| 50-64 | 2506 (31.8) | 5378 (68.2) | 0.11 |
| ≥65 | 942 (9.7) | 8806 (90.3) | 0.29 |
Discussion
Our analysis appears to indicate that the incidence of cell phone–related injuries to the head and neck was relatively infrequent until it began to increase in 2007, with a brief peak followed by a much faster progression than previously seen. This period also coincides with the release of the first major successful smartphone in the US market, the iPhone️ (Apple Inc). Although mobile telephones were gaining popularity prior to that time point, their functions were limited, and they were therefore less likely to be major distractions when compared with modern-day smartphones. Providing constant access to a variety of applications and internet browsers, these devices have become a necessary but potentially dangerous tool used by most people in the United States.
Cell phone use has been widely studied as a possible cause of an increasing number of motor vehicle crashes in the United States.12,13,14,15,16 In their analysis of ambulatory cell phone–related injuries, Smith et al17 identified injuries related to cell phone use while walking as a phenomenon increasing in frequency. In their study, which focused on injury to the whole body (not only the head and neck), the most common injury type was fracture or dislocation.
The most common diagnosis in our analysis was laceration, followed by contusion and abrasion. Traumatic lacerations are extremely common, with an estimated 6 million patients treated in EDs and an estimated cost of $3 billion each year.18 Facial lacerations and their subsequent repairs make up a large proportion of this health care spending, with many studies focusing on cost-saving techniques and proper patient management in an attempt to reduce costs.19,20 Although these injuries may not appear to be of major concern, facial lacerations can be a source of significant patient disease burden. Facial lacerations and subsequent scarring can lead to anxiety and lowered self-esteem, sometimes resulting in antisocial behavioral changes in extreme cases.21,22,23 Lacerations also carry a 2% to 5% risk of infection, which significantly increases the possibility of cosmetic dissatisfaction and need for scar revision.24,25
Another diagnosis that was prevalent in the present study was internal organ injury. With respect to the head, the NEISS Coding Manual8 requires the most severe diagnosis to be coded. For example, although concussion is a separate diagnosis, any diagnosis deemed more severe (eg, subdural hematoma or cerebral contusion) is coded as an “internal organ injury.” Analyzing the data, we found that this diagnosis most commonly referred to traumatic brain injury. Given that most patients were discharged and not admitted for treatment, we assume that these were cases of mild traumatic brain injury. Patients with mild traumatic brain injury are able to be discharged without additional intervention; however, these patients are still at risk for postconcussion syndrome.26 The symptoms of postconcussion syndrome can vary in severity from mild (headache, nausea, or fatigue) to severe (memory problems, emotional lability, or depression); therefore, these patients must be followed up closely after discharge.27
Comparing DM and CPA injuries among age groups produced an interesting result with regard to patients younger than 13 years (Table 2). In this age group, the rate of DM injuries was much higher than that in the other age groups. Many of the narratives for these DM injuries described either parents accidentally injuring the child with a cell phone that was in their hand or a child using the cell phone and accidentally injuring themselves. These data are concordant with those provided by the National Center for Injury Prevention and Control, which show that injuries categorized as “unintentionally struck by or against” are among the most common for this age group.28 Thermal injury from cellp hone batteries has been well documented in the literature, but, to our knowledge, the role of cell phones themselves as a possible cause of physical damage has not been explored.29 Modern smartphones may be substantial in size and weight and, under particular circumstances, can cause physical damage, especially to a child.
When distraction-related injuries were stratified by age group, we again found significant differences between groups. Those aged 13 to 29 years were significantly more likely to be injured during activities such as driving, walking, and texting (Figure 3 and eTable 2 in the Supplement). This finding is in concordance with those of prior studies, which showed more frequent CPA injuries among adolescents than in other age groups in the settings of both driving and walking.30,31,32 The majority of public health projects targeting cell phone use among teenagers and young adults focus on cell phone use while driving as a major risk for injury.33 Recent attention has also been given to augmented reality–based video games that make use of walking mechanics. One example is Pokémon Go, a game released in 2016 and subsequently identified in the medical literature as a potential safety risk.34,35,36 In the present analysis, we estimated 90 weighted cases in which this game was the activity leading up to injury.
Our study’s findings suggest a need for public education about the risks of cell phone use and distracted behavior during other activities as well as driving. In addition, recent literature has stratified distraction-related injuries according to the type of distraction, commonly categorizing distractions as visual, manual, or cognitive.37,38 Attempts should be made to use these categories in future analyses and in public education about injuries due to distraction. With an increasing number of devices and applications competing for users’ attention, it is more important than ever to ensure the safe use of smartphones. Specifically, high-risk age groups should be targeted for education to prevent unnecessary injury.
Limitations
To our knowledge, this is the first study to investigate the role of cell phones and cell phone–related distractions in injuries to the head and neck. With a major part of the US population owning cell phones, most of which are smartphones, understanding the risks of these devices is important for injury prevention and trauma management. However, this study is not without limitations. The NEISS database includes reported ED visits for injuries related to various devices but does not include information related to visits to urgent care centers or other health care settings. The database also lacks information regarding patient comorbidities, treatment, and outcome, which would provide a valuable addition to understanding the management of these patients’ injuries. As is the case with many database analyses, the database used in this analysis relies on information gathered from a variety of institutions and personnel capable of making errors in documentation or of mischaracterizing events. Despite these limitations, we believe the findings in this study provide valuable insight into the nature of this common cause of head and neck injuries.
Conclusions
Cell phones are ubiquitous in the US population, and their incorporation into our daily lives is ever growing. As we become more reliant on these devices, it is important to understand the risks associated with their use. Cell phone–related injuries to the head and neck have increased over a recent 20-year period, with many cases resulting from distraction. Although most of these injuries are not severe, some bear a risk of long-term complications. A large number of these injuries occur among those aged 13 to 29 years and are related to common activities such as texting and walking. These findings suggest an opportunity for injury prevention through patient education about the dangers of using a cell phone while performing other activities.
eTable 1. Incidence of Cell Phone Related Injuries per Year
eTable 2. Activities During Injury by Age Group
References
- 1.Corso P, Finkelstein E, Miller T, Fiebelkorn I, Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Inj Prev. 2015;21(6):434-440. doi: 10.1136/ip.2005.010983rep [DOI] [PubMed] [Google Scholar]
- 2.Bisson JI, Shepherd JP, Dhutia M. Psychological sequelae of facial trauma. J Trauma. 1997;43(3):496-500. doi: 10.1097/00005373-199709000-00018 [DOI] [PubMed] [Google Scholar]
- 3.Sethi RKV, Kozin ED, Fagenholz PJ, Lee DJ, Shrime MG, Gray ST. Epidemiological survey of head and neck injuries and trauma in the United States. Otolaryngol Head Neck Surg. 2014;151(5):776-784. doi: 10.1177/0194599814546112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Youssef P, Povolotskiy R, Mukherjee TJ, Kandinov A, Paskhover B. Pediatric facial injuries: hitting close to home. J Craniomaxillofac Surg. 2018;46(9):1539-1543. doi: 10.1016/j.jcms.2018.05.054 [DOI] [PubMed] [Google Scholar]
- 5.Povolotskiy R, Youssef P, Kaye R, Paskhover B. Facial fractures in young adults: a national retrospective study. Ann Otol Rhinol Laryngol. 2019;128(6):516-523. doi: 10.1177/0003489419830114 [DOI] [PubMed] [Google Scholar]
- 6.Hanba C, Svider PF, Chen FS, et al. Race and sex differences in adult facial fracture risk. JAMA Facial Plast Surg. 2016;18(6):441-448. doi: 10.1001/jamafacial.2016.0714 [DOI] [PubMed] [Google Scholar]
- 7.US Consumer Product Safety Commission NEISS highlights, data and query builder. https://www.cpsc.gov/cgibin/NEISSQuery/home.aspx. Accessed October 26, 2019.
- 8.Consumer Product Safety Commission. NEISS Coding Manual. https://www.cpsc.gov/s3fs-public/2019_NEISS_Coding_Manual.pdf. Published January 2019. Accessed May 2019.
- 9.US Census Bureau Home page. http://www.census.gov. Accessed October 26, 2019.
- 10.Berry G, Armitage P. Mid-p confidence intervals: a brief review. J R Stat Soc D Statistician. 1995;44(4):417-423. https://www.jstor.org/stable/2348891. Accessed October 27, 2019. [Google Scholar]
- 11.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 12.Foss RD, Goodwin AH. Distracted driver behaviors and distracting conditions among adolescent drivers: findings from a naturalistic driving study. J Adolesc Health. 2014;54(5)(suppl):S50-S60. doi: 10.1016/j.jadohealth.2014.01.005 [DOI] [PubMed] [Google Scholar]
- 13.Overton TL, Rives TE, Hecht C, Shafi S, Gandhi RR. Distracted driving: prevalence, problems, and prevention. Int J Inj Contr Saf Promot. 2015;22(3):187-192. doi: 10.1080/17457300.2013.879482 [DOI] [PubMed] [Google Scholar]
- 14.Truong LT, Nguyen HTT, De Gruyter C. Mobile phone use while riding a motorcycle and crashes among university students. Traffic Inj Prev. 2019;20(2):204-210. doi: 10.1080/15389588.2018.1546048 [DOI] [PubMed] [Google Scholar]
- 15.Wilson FA, Stimpson JP. Trends in fatalities from distracted driving in the United States, 1999 to 2008. Am J Public Health. 2010;100(11):2213-2219. doi: 10.2105/AJPH.2009.187179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zatezalo N, Erdogan M, Green RS. Road traffic injuries and fatalities among drivers distracted by mobile devices. J Emerg Trauma Shock. 2018;11(3):175-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith DC, Schreiber KM, Saltos A, Lichenstein SB, Lichenstein R. Ambulatory cell phone injuries in the United States: an emerging national concern. J Safety Res. 2013;47:19-23. doi: 10.1016/j.jsr.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 18.Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Adv Data. 2007;(386):1-32. [PubMed] [Google Scholar]
- 19.Kuwabara K, Imanaka Y, Ishizaki T. Quality and productive efficiency in simple laceration treatment. J Eval Clin Pract. 2006;12(2):164-173. doi: 10.1111/j.1365-2753.2006.00597.x [DOI] [PubMed] [Google Scholar]
- 20.Drolet BC, Tandon VJ, Ha AY, et al. Unnecessary emergency transfers for evaluation by a plastic surgeon: a burden to patients and the health care system. Plast Reconstr Surg. 2016;137(6):1927-1933. doi: 10.1097/PRS.0000000000002147 [DOI] [PubMed] [Google Scholar]
- 21.Singer AJ, Mach C, Thode HC Jr, Hemachandra S, Shofer FS, Hollander JE. Patient priorities with traumatic lacerations. Am J Emerg Med. 2000;18(6):683-686. doi: 10.1053/ajem.2000.16312 [DOI] [PubMed] [Google Scholar]
- 22.Brown BC, McKenna SP, Siddhi K, McGrouther DA, Bayat A. The hidden cost of skin scars: quality of life after skin scarring. J Plast Reconstr Aesthet Surg. 2008;61(9):1049-1058. doi: 10.1016/j.bjps.2008.03.020 [DOI] [PubMed] [Google Scholar]
- 23.Tebble NJ, Adams R, Thomas DW, Price P. Anxiety and self-consciousness in patients with facial lacerations one week and six months later. Br J Oral Maxillofac Surg. 2006;44(6):520-525. doi: 10.1016/j.bjoms.2005.10.010 [DOI] [PubMed] [Google Scholar]
- 24.Quinn JV, Polevoi SK, Kohn MA. Traumatic lacerations: what are the risks for infection and has the “golden period” of laceration care disappeared? Emerg Med J. 2014;31(2):96-100. doi: 10.1136/emermed-2012-202143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Perelman VS, Francis GJ, Rutledge T, Foote J, Martino F, Dranitsaris G. Sterile versus nonsterile gloves for repair of uncomplicated lacerations in the emergency department: a randomized controlled trial. Ann Emerg Med. 2004;43(3):362-370. doi: 10.1016/j.annemergmed.2003.09.008 [DOI] [PubMed] [Google Scholar]
- 26.Jagoda AS, Bazarian JJ, Bruns JJ Jr, et al. ; American College of Emergency Physicians; Centers for Disease Control and Prevention . Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Ann Emerg Med. 2008;52(6):714-748. doi: 10.1016/j.annemergmed.2008.08.021 [DOI] [PubMed] [Google Scholar]
- 27.Jagoda A, Riggio S. Mild traumatic brain injury and the postconcussive syndrome. Emerg Med Clin North Am. 2000;18(2):355-363. doi: 10.1016/S0733-8627(05)70130-9 [DOI] [PubMed] [Google Scholar]
- 28.National Center for Injury Prevention and Control; Centers for Disease Control and Prevention WISQARS nonfatal injury data. https://www.cdc.gov/injury/wisqars/nonfatal.html. Accessed August 10, 2019.
- 29.Mankowski PJ, Kanevsky J, Bakirtzian P, Cugno S. Cellular phone collateral damage: a review of burns associated with lithium battery powered mobile devices. Burns. 2016;42(4):e61-e64. doi: 10.1016/j.burns.2015.10.012 [DOI] [PubMed] [Google Scholar]
- 30.Mirman JH, Durbin DR, Lee Y-C, Seifert SJ. Adolescent and adult drivers’ mobile phone use while driving with different interlocutors. Accid Anal Prev. 2017;104:18-23. doi: 10.1016/j.aap.2017.04.014 [DOI] [PubMed] [Google Scholar]
- 31.Nasar JL, Troyer D. Pedestrian injuries due to mobile phone use in public places. Accid Anal Prev. 2013;57:91-95. doi: 10.1016/j.aap.2013.03.021 [DOI] [PubMed] [Google Scholar]
- 32.National Highway Traffic Safety Administration. Distracted driving in fatal crashes, 2017. https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/812700. Published April 2019. Accessed October 15, 2019.
- 33.National Highway Traffic Safety Administration. Teen driving; resources. https://www.nhtsa.gov/road-safety/teen-driving#resources. Published 2017. Accessed October 15, 2019.
- 34.Barbieri S, Vettore G, Pietrantonio V, et al. Pedestrian inattention blindness while playing Pokémon Go as an emerging health-risk behavior: a case report. J Med Internet Res. 2017;19(4):e86. doi: 10.2196/jmir.6596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ayers JW, Leas EC, Dredze M, Allem JP, Grabowski JG, Hill L. Pokémon GO—a new distraction for drivers and pedestrians. JAMA Intern Med. 2016;176(12):1865-1866. doi: 10.1001/jamainternmed.2016.6274 [DOI] [PubMed] [Google Scholar]
- 36.Richards KG, Wong KY, Khan M. Augmented reality game-related injury. BMJ Case Rep. 2018;11(1):e224012. doi: 10.1136/bcr-2017-224012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harbluk JL, Noy YI, Trbovich PL, Eizenman M. An on-road assessment of cognitive distraction: impacts on drivers’ visual behavior and braking performance. Accid Anal Prev. 2007;39(2):372-379. doi: 10.1016/j.aap.2006.08.013 [DOI] [PubMed] [Google Scholar]
- 38.Strayer DL, Watson JM, Drews FA. Cognitive distraction while multitasking in the automobile In: Ross B, ed. The Psychology of Learning and Motivation. Vol. 54. Burlington, VT: Academic Press/Elsevier; 2011:29-58. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Incidence of Cell Phone Related Injuries per Year
eTable 2. Activities During Injury by Age Group