Key Points
Question
Is the articulated alar rim graft (AARG) associated with improved function of the nasal airway and aesthetic outcomes?
Findings
This case series of 90 patients examined the creation, placement, and function of the AARG. A retrospective review showed statistically significant improvement in Nasal Obstruction Symptom Evaluation Survey scores in patients who had AARGs placed; aesthetic analysis by raters on a Likert scale showed cosmetic improvement in patients with a deep alar margin furrow; and morphometric analysis of preoperative and postoperative nasal base shapes showed a trend toward a more equilateral ideal shape.
Meaning
The AARG may improve the functional airway in select patients and the aesthetics of the nose in patients with a significant alar margin furrow or a pinched-appearing nasal tip.
This case series analyzes the functional and aesthetic outcomes of articulated alar rim graft placement on nasal airway function, nasal base shape change, and appearance.
Abstract
Importance
The design, use, and indications for the articulated alar rim graft (AARG) and the functional and aesthetic improvements that can be achieved have not been fully characterized.
Objective
To analyze the functional and aesthetic outcomes of AARG placement on nasal airway function, nasal base shape change, and appearance.
Design, Setting, and Participants
A case series study of patients who underwent septorhinoplasty with placement of AARG at University of California, Irvine Medical Center, from 2015 to 2018 was carried out. Surgical data recorded included stage of rhinoplasty (primary vs revision), use of spreader grafts, rim grafts (and dimensions), caudal septal extension graft (CSEG), lateral crural tensioning (LCT), and turbinate reductions.
Main Outcomes and Measures
Preoperative and postoperative Nasal Obstruction Symptom Evaluation Survey (NOSE) surveys were analyzed and correlated with AARG geometry, use of CSEG, and the LCT maneuver. Preoperative and postoperative alar base views were evaluated by fitting base shape to a parametric numerical model to categorize each to 1 of 6 shape categories. Blinded reviewers rated alar furrow severity and the alar ridge presence using a Likert scale for both preoperative and postoperative images to subjectively gauge aesthetic outcomes.
Results
Overall, 90 patients with both preoperative and postoperative NOSE scores who underwent septorhinoplasty and placement of an AARG were included. Of the 90 patients, 60 were women (mean age, 38.2 years). Patient NOSE scores (70.4 preoperatively to 25.1 postoperatively) significantly improved from preoperation to postoperation (P < .001), regardless of AARG size, CSEG, or LCT. Alar base shape parametric analysis showed preoperative to postoperative improvements were significant for anterior-to-posterior ratio mass distribution (95% CI, −0.16 to 0.02; P = .05) and vertical projection-to-horizontal base width ratio (95% CI, 0.01-0.32; P = .02) in flat noses and cloverleafing for narrow noses (95% CI, −0.05 to −0.01; P = .001); enhancement approached significance for reduction in lateral scalloping in cloverleaf noses (P = .06). Aesthetic analysis showed that there was a statistically significant improvement for the alar furrow (95% CI, −0.68 to −0.29 for rater 1; −0.54 to −0.27 for rater 2; and −0.59 to −0.27 for rater 3; P < .001) for all raters and for the alar ridge (95% CI, 0.16-0.48; P < .001) for 1 rater.
Conclusions and Relevance
To our knowledge, this is the first study to demonstrate that AARG use is associated with statistically significant improvement in NOSE scores. Placement of AARGs may improve posterior mass ratios in flat noses and lateral cloverleafing in narrow noses as suggested by quantitative shape change parameter analysis. The placement of AARGs was associated with aesthetic and functional enhancement in the cloverleaf deformity, which is associated with a prominent alar furrow, and often external nasal valve collapse. Patient selection is key when placing AARGs.
Level of Evidence
NA.
Introduction
Creation of a favorable nasal tip complex requires an understanding of how surgical maneuvers impact surface topology. Many classic tip refinement techniques such as cross-hatching decrease support at the junction between the tip and alar lobule, potentially creating irregularities along the alar margin. Dome sutures alone may pinch the tip, creating unfavorable lines crossing the alar margin.1 Classic rim grafts can help alter alar margin curvature, stabilize alae that collapse with inspiration, correct alar retraction or flare, and conceal cephalic malposition of the lower lateral cartilage (LLC).2,3 However, long-term notching deformities in the anterior-medial ala can occur.4 Classic rim grafts are limited by the degree of mechanical stability they can impart to the alar lobule and are not designed to address aesthetic concerns or stability in the soft triangle.
The articulated alar rim graft (AARG) was first described by Davis.5,6,7 The senior author (B.J-F.W.) has adopted Davis’s technique since 2012 and have reported on its use with a few minor modifications (Video).8,9 The grafts are triangular in shape, beveled cephalically, medially, and tapered laterally. The medial aspect overlaps and is sutured to the corresponding dome and lateral crus. AARGs are oriented approximately 90-degrees to midline, define the position of the alar margin, and are inserted into precise subcutaneous alar pockets (Figure 1). The AARG partially traverses the region of the soft tissue triangle, and may function as a facet graft.10 Use of the AARG is optimally combined with caudal septal extension graft placement (CSEG), which provides a secure fixation point. The AARG may be combined with a lateral crural tensioning maneuver (LCT), if this is needed to improve the functional airway or correct crural convexity.7,8,11
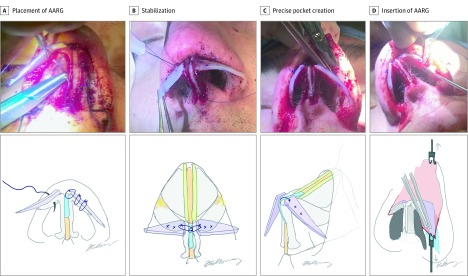
Figure 1. Articulated Alar Rim Graft (AARG) Placement and Design.
A, The AARG is placed using 2 sutures between the domes and the AARG. A third (most medial) suture is placed between the AARG, the dome, and the caudal septal extension graft . B, Stabilization of AARG with needle and forcep as sutures are placed. C, Creation of precise pocket, extension of marginal incision, oblique view of AARG. D, Insertion of AARG into pocket.
Video. Articulated Alar Rim Grafts in Septorhinoplasty.
This procedure video illustrates the authors’ surgical technique for placing articulated alar rim grafts in septorhinoplasty.
Although surgical technique using AARGs have been described in the literature,7,8,9,11 to our knowledge there have not been any detailed studies examining functional and aesthetic outcomes with quantitative methods and statistical analysis. Here a series of 90 patients who underwent AARG placement is presented. The objectives were to (1) review and analyze functional outcomes, factoring in the outcomes of LCT and CSEG placement; (2) assess cosmetic changes using Likert scale analysis; (3) perform quantitative parametric analysis of the alar base shape change; and (4) identify indications and contraindications for AARG use.
Methods
Study Design
We conducted an institutional review board approved retrospective review of patients at UC Irvine Medical Center from 2015 to 2018 who underwent septorhinoplasty and placement of AARGs, by the senior author (B.J-F.W.). All patients who had AARGs placed were included. Data recorded included demographics, preoperative physical examination including classification of septal deformity, internal/external valve collapse, and the modified Cottle maneuver. Surgical data recorded included stage of rhinoplasty (primary vs revision), use of spreader grafts, rim grafts (and dimensions), CSEGs, LCT, and turbinate reductions.
Preoperative and postoperative digital photographs were recorded in 9 standard views, and written consent was obtained. Only patients with a complete high-quality preoperative and postoperative images were included.
Nasal Obstruction and Septoplasty Effectiveness (NOSE) Survey
Only patients who completed both preoperative and postoperative NOSE surveys were included. If a patient had multiple NOSE surveys corresponding to serial postoperative visits, the most recent survey was used. Paired sample t tests were performed to identify relationships between NOSE score and AARG dimensions, CSEG use, and LCT.
Aesthetic Evaluation
A 3-point Likert scale scored frontal and alar base views of each preoperative and postoperative image set. Three blinded reviewers (H.C., C.H., H.B.) were presented a slide with paired frontal and base views of either preoperative or postoperative patients in a randomized order. Only patients with adequate preoperative and postoperative frontal and base views were included. Two aesthetic features were evaluated: the alar furrow and the alar ridge. The alar margin furrow is a sulcus between the nasal tip and anatomically represents the point where the lateral crus begins its course cephalically and in general where the dilator naris inserts into the skin soft tissue envelope.9 On base view, it usually appears as an indention between the 2 alae and tip and can contribute to the “scalloped” appearance. A deep furrow medially positioned is aesthetically unfavorable. The alar ridge is a softly beveled elevation running parallel to the alar margin and terminates near the tip defining point, creating a crisp highlight along the alar rim; the ridge is a favorable attribute (Figure 2).9
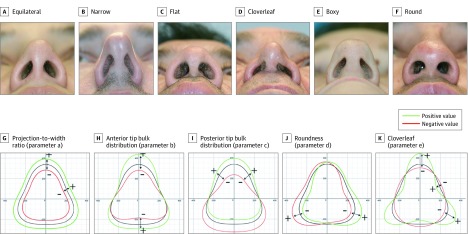
Figure 2. Qualitative Aesthetic Analysis and Results.
A, Visual depictions of alar margin furrow with preoperative (left, Likert scale score of 1, severe) and postoperative (right, Likert scale score of 3, absent) photographs of a patient who had an articulated alar rim graft placed. B, Top patient demonstrates a Likert scale score of 3 (well defined), while the bottom patient demonstrates (from left to right) a Likert scale score of 1 (none), 2 (average), and 3 (crisp).
The alar furrow Likert scale consisted of (1) deep furrow; (2) intermediate furrow; and (3) no furrow. The alar ridge Likert scale consisted of (1) no alar ridge, rounded ala; (2) intermediate alar ridge; and (3) crisp alar ridge with excellent contour highlight. Intraclass correlation coefficients were run to determine how strongly raters resembled one another, and then paired t tests were used to calculate differences between preoperative and postoperative aesthetic ratings.
Geometric Analysis
The analysis of aesthetic outcomes was performed first outlining each preoperative and postoperative nasal base shape, and then curve fitting it to a 5-parameter regression model that accurately recapitulates base view geometry.12 The custom software performs a curve-fit and calculates 5 key parameters (a, b, c, d, and e) that recapitulate base shape (Figures 2 and 3). Each of the 5 parameters control a specific aspect of base shape:
Figure 3. Quantitative Morphometric Analysis.
A-F, Nasal base shapes categorized by perimeter geometry (Barnes et al12). G-K, Five characteristic parameters used to replicate the nasal base shape.12 The plus signs (+) indicate an increase in this parameter value in green with respect to control (black), whereas the minus signs (−) indicate a decrease in the parameter value (red).
a: Scaling factor that normalizes the images
b: Ratio of vertical projection to horizontal base width
c: Anterior (larger c) to posterior (smaller c) distribution of tip bulk or mass
d: Symmetry (right is positive value, left is negative, midline is 0)
e: Cloverleaf shape; larger e indicates greater scalloping
For the present analysis, parameters a and d reflect only overall size and left/right skew. They were omitted from analysis. By consensus opinion of 3 investigators (C.H., C.B., and H.C.), each preoperative and postoperative alar base image was categorized as: equilateral, narrow, flat, cloverleaf, boxy, and round. In the cloverleaf-shaped nose, the tip and 2 ala form a trilobular structure reminiscent of cloverleaf. Scalloping from the base view refers to clefting between each “leaf” creating a more lobulated rather than smooth equilateral triangle-shaped nose. Paired t tests between the clinically defined 6 categories (eg, boxy, narrow) for preoperative and postoperative images and the numerical 4 selected numerical parameters (b, c, and e). Based on previous work,12 scatterplot diagrams of parameter b vs e provides a convenient means to visually categorize base shape because base shape archetypes tend to cluster around specific values for b and e. Only patients with adequate preoperative and postoperative alar base views were included.
Results
There were 90 patients with both preoperative and postoperative NOSE scores with AARG placement, 62 females, and the mean age was 38.2 years. Thirty-six patients underwent secondary rhinoplasty. All 90 patients had some degree of nasal airway obstruction, 44 had sustained nasal trauma prior to surgery. Alar base shape categorization consisted of 22 equilateral noses, 15 narrow noses, 15 boxy noses, 11 round noses, 5 flat noses, and 4 cloverleaf noses. Sixty-one patients underwent LCT, 75 had CSEG placement, and the mean (SD) AARG length was 19.6 (2.4) × 4.8 (1.6) mm. Eighty-five of the 90 participants had spreader grafts placed at the time of surgery, and 71 had an inferior turbinate submucosal resection and outfracture. The NOSE score follow-up dates ranged from 12 to 1135 days with a mean of 259 days (8.5 months). The mean (SD) preoperative NOSE score was 70.4 (24.9) and mean (SD) postoperative score was 25.1 (25.4), which significantly improved from preoperative to postoperative (P < .001) result, regardless of AARG size, CSEG, or LCT. Comparison of group differences for CSEG vs no CSEG, LCT vs no LCT, and large (length >19.6 mm) vs small AARG (length <19.6 mm) using independent sample t tests in preoperative and postoperative NOSE scores did not show any significant differences between groups (eTable 1 in the Supplement).
Aesthetic analysis included 85 patients (eTable 2 in the Supplement). For the alar margin furrow, analysis showed that there was a statistically significant improvement (P < .001) for all 3 raters. Intraclass correlation coefficients between the 3 raters were significant for the preoperative and postoperative alar furrow. For the alar ridge, the intraclass correlation was significant preoperatively and postoperatively between all 3 raters, but there was statistical improvement postoperatively seen by only 1 rater.
For quantitative alar base analysis, there were 72 patients included. Alar base shape parametric analysis demonstrated that preoperative to postoperative changes in shape were significant for parameters c (95% CI, −0.16 to 0.02; P = .05) and b (95% CI, 0.01-0.32; P = .02) in flat noses, and parameter e in narrow noses (95% CI, −0.05 to 0.02; P = .001). Preoperative to postoperative changes were not significant for parameter e in cloverleaf noses (95% CI, −0.11 to 0.02; P = .06), parameter e in flat noses (95% CI, −0.11 to 0.02; P = .07), and parameter b (95% CI, −0.03 to 0.20; P = .07) and c (95% CI, −0.10 to 0.02; P = .08) in round noses. Figure 4 summarizes these findings.
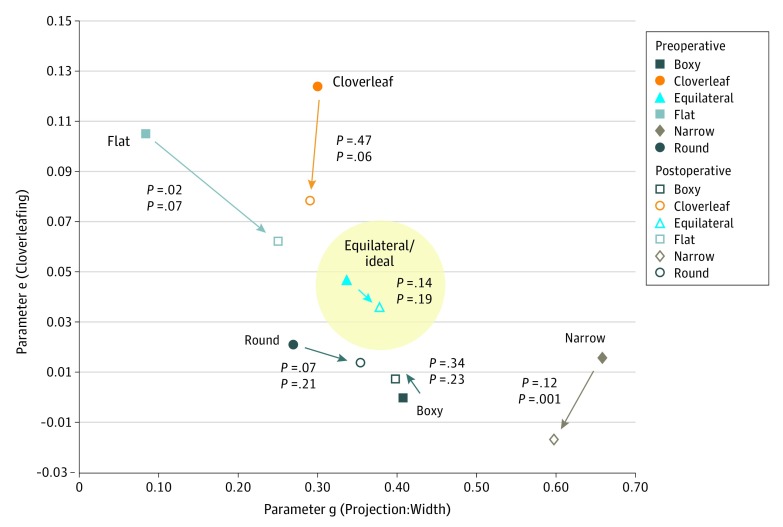
Figure 4. Nasal Shape Preoperative and Postoperative Changes.
Scatterplot of preoperative and postoperative nasal base shapes of parameters b (vertical projection to horizontal base width) and e (degree of cloverleafing) showing a trend in all shapes except for narrow toward the ideal, equilateral shape.
Discussion
Functional Nasal Airway Outcomes
The NOSE scores improved in patients who had AARG placement, though obviously many other airway improvement maneuvers simultaneously contributed to air flow improvement, such as septoplasty, turbinate reduction, LCT, and importantly, spreader grafting. The reduction in NOSE scores from 69.5 to 27.8 was consistent with other rhinoplasty study outcomes.13,14,15 Identifying the effects of isolated AARG placement would be difficult to perform in any clinical study because nasal airway obstruction is usually owing to multisite obstruction and multiple maneuvers are performed.
Likewise, CSEG use and the LCT maneuver, although not specifically aimed at airway improvement, provide midline structural support11 and increase tension across the alar lobule, respectively. In this series, 75 (83%) patients who underwent AARG also had a CSEG, which improves stability.1 It provides a second suture fixation point for the AARG in addition to its ipsilateral dome, enhancing the cantilever effect, creating a “post” to resist vertically oriented force vectors on the nasal tip. Determining the association of the LCT maneuver with reduced dynamic collapse of the external valve remains difficult. The isolated effect of the LCT maneuver will likely be best determined using computational modeling, as would be the case with other rhinoplasty manuevers.16
The effect of AARGs would be greatest on patients where obstruction and dynamic collapse at the external valve occurs owing to lack of alar lobule stability or stiffness. External valve compromise was clinically evident in 64 patients. Validating this assertion is difficult because solitary external valve collapse is uncommon and other airway maneuvers are performed simultaneously. Reconfiguration of internal framework structure alone should improve the airway, and the amount of cartilage used is generally less than that used in lateral crural strut grafts.17,18 The indications for strut graft use and AARG are decidedly different. Since adoption of the AARG approach in 2012, the senior author (B.J-F.W.) has seldom performed lateral crural strut grafting even in cases of crural recurvature, cephalic malposition, or severe secondary rhinoplasty alar deformity. Overall our results in functional NOSE scale outcomes are consistent with those of other studies, many of which were not randomized, not prospective, and used spreader grafts, strut grafts, and other airway improving maneuvers in combination with the maneuver being assessed by this study.13,14,15,19
Aesthetic Evaluation and Analysis
The AARG can provide several cosmetic improvements in rhinoplasty that are associated with optimized social perceptions.20 Placement of AARGs correct the deep sulcus between tip and alar subunits (alar margin furrow).9 Often, noses with a deep alar margin furrow also have the lobular cloverleaf deformity. This is often caused by cephalically oriented LLCs owing to poor alar soft tissue support. Often there is external nasal valve collapse, especially in revisions where cephalic trim and transdomal sutures were used.6 This deformity contrasts with Toriumi’s1 description of an ideal smooth transition in this region. The near 90-degree angle of the AARG to the sagittal midline corrects this deformity by creating structural support along the alar rim. The cantilevered nature of the AARG augments the LLCs to provide support, further effacing this furrow. This is consistent with the results from our aesthetic analysis because all 3 raters found a significant improvement in the alar margin furrow with AARGs. This triad, the cloverleaf nose, alar margin furrow, and external nasal valve collapse, is an excellent indication for placement of an AARG.
The alar ridge is a subtle elevation of soft tissue that parallels the alar margin. Presence of an alar ridge is aesthetically pleasing, but is often difficult to appreciate, depending on the lighting and pose. There was no significance among raters for improvement/creation of the alar ridge. We did not include oblique views in the aesthetic analysis, and inclusion might have contributed to better intrarater agreement.
Geometric Analysis
For nearly 100 years, nasal base shape analysis has relied on the use of descriptive categorization, Likert scale analysis, or expert panel evaluations. Although useful, they lack rigor, prompting development of quantitative methods to describe nasal base geometry.12 This bias-free approach uses a model that accurately recapitulates nasal base contour via a 5-parameter curve fit. Preoperative and postoperative tracking of parameter changes provides information on shape change that is more elegant and accurate than simple linear and angular measurement. Visual tracking of shape change for individual noses as a categorized group can now be displayed using a scatterplot (Figure 3). Application of this approach suggests that AARG use (along with LCT) creates a more equilateral-shaped nasal base. The 2-parameter (b, vertical projection to horizontal base width and e, degree of cloverleafing) diagram demonstrates there is a general progression for all but narrow nasal shapes toward the equilateral triangle shape zone indicated in Figure 3 by the circular region of interest. This shift toward the equilateral triangle zone by the preoperative/postoperative pairs suggest that this base shape is ideal and consistent with both general practice and classic cannon.
In flat noses, there was significant improvement in projection-to-width ratios (parameter b) and anterior-to-posterior distribution (parameter c). Flat noses usually require placement of a CSEG to increase tip projection, and often the LCT maneuver to recruit more lateral crura and create narrower tip defining points. The AARG can be designed to add more projection, enhancing an equilateral shape. Cloverleaf is a base shape wherein AARG use is effective for significant reduction in scalloping. Analysis tended toward a reduction in scalloping in both flat and cloverleaf noses. Data was limited by the small numbers in the cloverleaf (n = 4) and flat nose (n = 5) categories, though there is a continuum of contours across phenotypes.
In round noses, both the projection-to-width ratios (parameter b) and the anterior-to-posterior mass distribution ratios (parameter c) trended toward improvement after AARG placement, as by design they create a more equilateral shape particularly when combined with dome suture techniques. Traditionally a very round or bulbous tip can be converted to a well-defined equilateral shape by combining the CSEG and LCT maneuver with AARGs. This eliminates structural loss that may result from a cephalic trim, or mechanical instability from cross hatching or morcellation, and consumes less cartilage than strut graft placement.7,8,11
The quantitative approach provides insight on nasal geometry, and recent analytic methods have described overall nasal shape.21 These techniques could transform reporting of outcomes for aesthetic rhinoplasty. Nasal base phenotype varies along a continuum, and noses may share features of more than 1 archetypal shape. The mean values for shape parameters, which when plotted on a scatter diagram (Figure 4), illustrates the distribution of phenotypes.
Indications and Contraindications for AARGS
Indications for AARGS are similar to classic rim grafts in the setting of external nasal valve collapse. Unique indications for AARGs include correction of deficient soft triangle support and the aggressive effacement of the alar margin furrow.9 The AARG is optimal when placed in combination with a CSEG, which stabilizes the entire tip complex. It are also essentially imperative when performing LCT maneuvers to correct alar lobule weakness produced by recruitment.6,7,8
In select patients, AARGs can contribute to improved air flow by increasing alar lobule stiffness in addition to providing contour refinement. Placement of AARGs can improve the appearance of the soft triangle, and enhance the alar ridge.9 Also, the AARG can improve the appearance of the nasal base, by creating a more ideal equilateral shape of the nasal base.12 Figure 5 shows preoperative and postoperative photos of a patient who had an AARG placed.
Figure 5. Primary Rhinoplasty in a Patient With a Boxy Tip.
Clinical images of a patient who underwent primary rhinoplasty with a boxy tip, including internal and external nasal valve collapse. Osteotomies, septal cartilage graft for spreader grafts, caudal septal extension grafts, and articulated alar rim grafts were used for reconstruction. Note that there is more equilateral alar base shape in panel D relative to panel C.
We reviewed all patients whose gap in preoperative vs postoperative NOSE scores were 20 or less; this consisted of 7 patients. Reasons cited were persistent nasal airway obstruction owing to turbinate hypertrophy, residual septal spur, residual internal nasal valve collapse, and sinusitis. None of these lower NOSE score gaps were attributed to AARG failure.
Limitations
The most significant limitation was the retrospective nature of this study and relatively short follow-up interval. We only had 90 participants in this series, and it is a growing body of patients; these more recent patients had more detailed data sets that had been collected for the purposes of this research as it has evolved. Over 100 patients were excluded owing to insufficient data sets. Complications included 7 patients who had a postoperative infection, 3 patients who required revision owing to persistent nasal airway obstruction (residual septal spur, internal nasal valve collapse, enlarged inferior turbinate), and 1 with a postoperative seroma/hematoma that was drained and resolved without consequence.
Conclusions
The placement of AARGs is associated with statistically significant improvement in NOSE scores. The AARG improves the ratio of vertical projection to horizontal base width in flat noses, anterior to posterior mass ratios in flat noses, and lateral scalloping in narrow noses overall, suggest an iteration in shape change toward the equilateral phenotype, which is aesthetically ideal. Unlike lateral crural strut grafts, AARG cartilage consumption is small. The AARG creates aesthetic and functional enhancement correction of base view scalloping, which is associated with a prominent alar furrow, and often external nasal valve collapse.
eTable 1. Characteristics of Patients and Functional Results
eTable 2. Results of Qualitative Aesthetic Analysis
References
- 1.Toriumi DM. New concepts in nasal tip contouring. Arch Facial Plast Surg. 2006;8(3):156-185. doi: 10.1001/archfaci.8.3.156 [DOI] [PubMed] [Google Scholar]
- 2.Boahene KDO, Hilger PA. Alar rim grafting in rhinoplasty: indications, technique, and outcomes. Arch Facial Plast Surg. 2009;11(5):285-289. doi: 10.1001/archfacial.2009.68 [DOI] [PubMed] [Google Scholar]
- 3.Rohrich RJ, Raniere J Jr, Ha RY. The alar contour graft: correction and prevention of alar rim deformities in rhinoplasty. Plast Reconstr Surg. 2002;109(7):2495-2505. http://www.ncbi.nlm.nih.gov/pubmed/12045582. Accessed May 10, 2018. doi: 10.1097/00006534-200206000-00050 [DOI] [PubMed] [Google Scholar]
- 4.Gruber RP, Fox P, Peled A, Belek KA. Grafting the alar rim: application as anatomical graft. Plast Reconstr Surg. 2014;134(6):880e-887e. doi: 10.1097/PRS.0000000000000764 [DOI] [PubMed] [Google Scholar]
- 5.Davis RE. Nasal tip complications. Facial Plast Surg. 2012;28(3):294-302. doi: 10.1055/s-0032-1312700 [DOI] [PubMed] [Google Scholar]
- 6.Davis RE. Revision of the overresected nasal tip complex. Facial Plast Surg. 2012;28(4):427-439. doi: 10.1055/s-0032-1319844 [DOI] [PubMed] [Google Scholar]
- 7.Davis RE. Lateral crural tensioning for refinement of the wide and underprojected nasal tip: rethinking the lateral crural steal. Facial Plast Surg Clin North Am. 2015;23(1):23-53. doi: 10.1016/j.fsc.2014.09.003 [DOI] [PubMed] [Google Scholar]
- 8.Foulad A, Volgger V, Wong B. Lateral crural tensioning for refinement of the nasal tip and increasing alar stability: a case series. Facial Plast Surg. 2017;33(3):316-323. doi: 10.1055/s-0037-1602143 [DOI] [PubMed] [Google Scholar]
- 9.Goodrich JL, Wong BJF. Optimizing the soft tissue triangle, alar margin furrow, and alar ridge aesthetics: analysis and use of the articulate alar rim graft. Facial Plast Surg. 2016;32(6):646-655. doi: 10.1055/s-0036-1596049 [DOI] [PubMed] [Google Scholar]
- 10.Kridel RWH, Chiu RJ. The management of alar columellar disproportion in revision rhinoplasty. Facial Plast Surg Clin North Am. 2006;14(4):313-329, vi. doi: 10.1016/j.fsc.2006.06.015 [DOI] [PubMed] [Google Scholar]
- 11.Ballin AC, Kim H, Chance E, Davis RE. The articulated alar rim graft: reengineering the conventional alar rim graft for improved contour and support. Facial Plast Surg. 2016;32(4):384-397. doi: 10.1055/s-0036-1585573 [DOI] [PubMed] [Google Scholar]
- 12.Barnes CH, Chen H, Chen JJ, Su E, Moy WJ, Wong BJF. Quantitative analysis and classification of the nasal base using a parametric model. JAMA Facial Plast Surg. 2018;20(2):160-165. doi: 10.1001/jamafacial.2017.1785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rudy S, Moubayed SP, Most SP. Midvault Reconstruction in Primary Rhinoplasty. Facial Plast Surg. 2017;33(2):133-138. doi: 10.1055/s-0036-1598016 [DOI] [PubMed] [Google Scholar]
- 14.Yeo N-K, Jang YJ. Rhinoplasty to correct nasal deformities in postseptoplasty patients. Am J Rhinol Allergy. 2009;23(5):540-545. doi: 10.2500/ajra.2009.23.3344 [DOI] [PubMed] [Google Scholar]
- 15.Standlee AG, Hohman MH. Evaluating the effect of spreader grafting on nasal obstruction using the NOSE Scale. Ann Otol Rhinol Laryngol. 2017;126(3):219-223. doi: 10.1177/0003489416685320 [DOI] [PubMed] [Google Scholar]
- 16.Brandon BM, Austin GK, Fleischman G, et al. Comparison of airflow between spreader grafts and butterfly grafts using computational flow dynamics in a cadaveric model. JAMA Facial Plast Surg. 2018;20(3):215-221. doi: 10.1001/jamafacial.2017.1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gunter JP, Friedman RM. Lateral crural strut graft: technique and clinical applications in rhinoplasty. Plast Reconstr Surg. 1997;99(4):943-952. http://www.ncbi.nlm.nih.gov/pubmed/9091939. Accessed May 30, 2018. doi: 10.1097/00006534-199704000-00001 [DOI] [PubMed] [Google Scholar]
- 18.Losquadro WD, Bared A, Toriumi DM. Correction of the retracted alar base. Facial Plast Surg. 2012;28(2):218-224. doi: 10.1055/s-0032-1309302 [DOI] [PubMed] [Google Scholar]
- 19.Kandathil CK, Spataro EA, Laimi K, Moubayed SP, Most SP, Saltychev M. Repair of the lateral nasal wall in nasal airway obstruction: a systematic review and meta-analysis. JAMA Facial Plast Surg. 2018;20(4):307-313. doi: 10.1001/jamafacial.2018.0036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nellis JC, Ishii M, Bater KL, et al. Association of rhinoplasty with perceived attractiveness, success, and overall health. JAMA Facial Plast Surg. 2018;20(2):97-102. doi: 10.1001/jamafacial.2017.1453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galantucci LM, Lavecchia F, Pastore P, Percoco G. Application of off-the-shelf stereo-cameras for the 3D assessment of morphometric variations caused by rhinoplasty. J Med Eng Technol. 2017;41(3):186-199. doi: 10.1080/03091902.2017.1281356 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Characteristics of Patients and Functional Results
eTable 2. Results of Qualitative Aesthetic Analysis