This cohort study estimates the incidence of postoperative glaucoma and glaucoma suspect among patients who underwent cataract surgery before age 13 years and evaluates potential risk factors.
Key Points
Question
What is the incidence risk of glaucoma or glaucoma suspect during the first year after lensectomy in children younger than 13 years, and what are the associated risk factors?
Findings
In this cohort study of 702 pediatric patients (970 eyes), glaucoma or glaucoma suspect developed in 66 of 970 eyes (adjusted overall incidence risk, 6.3%) within 1 year after unilateral or bilateral lensectomy. Age of 3 months or younger at lensectomy and aphakia were associated with subsequent glaucoma or glaucoma suspect.
Meaning
This study’s findings suggest that, although all children should be monitored for glaucoma following lensectomy, increased attention should be given to infants 3 months or younger at lensectomy and children with aphakia after lensectomy.
Abstract
Importance
Glaucoma can occur following cataract removal in children, and determining the risk for and factors associated with glaucoma and glaucoma suspect in a large cohort of children after lensectomy can guide clinical practice.
Objective
To estimate the incidence of glaucoma and glaucoma suspect and describe its management in the first year following lensectomy in children before 13 years of age.
Design, Setting, and Participants
A multicenter clinical research registry containing data for 1361 eyes of 994 children who underwent unilateral or bilateral lensectomy between June 2012 and July 2015 at 1 of 61 sites in the United States (n = 57), Canada (n = 3), and the United Kingdom (n = 1). Patients were eligible for inclusion in the study if they were enrolled in the registry within 45 days after lensectomy and had at least 1 office visit between 6 and 18 months after lensectomy. Patient data were reviewed, and glaucoma and glaucoma suspect were diagnosed by investigators using standardized criteria. Statistical analysis was performed between June 2017 and August 2019.
Exposures
Clinical care 6 to 18 months after lensectomy.
Main Outcomes and Measures
Incidence risk using standardized definitions of glaucoma and glaucoma suspect after lensectomy.
Results
Among 702 patients included in this cohort study, 353 (50.3%) were male and 427 (60.8%) were white; mean age at lensectomy was 3.4 years (range, 0.04-12.9 years). After lensectomy, glaucoma or glaucoma suspect was diagnosed in 66 of 970 eyes (adjusted overall incidence risk, 6.3%; 95% CI, 4.8%-8.3%). Glaucoma was diagnosed in 52 of the 66 eyes, and glaucoma suspect was diagnosed in the other 14 eyes. Mean age at lensectomy in these 66 eyes was 1.9 years (range, 0.07-11.2 years), and 40 of the 66 (60.6%) were eyes of female patients. Glaucoma surgery was performed in 23 of the 66 eyes (34.8%) at a median of 3.3 months (range, 0.9-14.8 months) after lensectomy. The incidence risk of glaucoma or glaucoma suspect was 15.7% (99% CI, 10.1%-24.5%) for 256 eyes of infants 3 months or younger at lensectomy vs 3.4% (99% CI, 1.9%-6.2%) for 714 eyes of infants older than 3 months (relative risk, 4.57; 99% CI, 2.19-9.57; P < .001) and 11.2% (99% CI, 7.6%-16.7%) for 438 aphakic eyes vs 2.6% (99% CI, 1.2%-5.6%) for 532 pseudophakic eyes (relative risk, 4.29; 99% CI, 1.84-10.01; P < .001). No association was observed between risk of developing glaucoma or glaucoma suspect and any of the following variables: sex, race/ethnicity, laterality of lensectomy, performance of anterior vitrectomy, prelensectomy presence of anterior segment abnormality, or intraoperative complications.
Conclusions and Relevance
This study found that glaucoma or glaucoma suspect developed in a small number of eyes in the first year after lensectomy and may be associated with aphakia and younger age at lensectomy. Frequent monitoring for signs of glaucoma following lensectomy is warranted, especially in infants 3 months or younger at lensectomy and in children with aphakia after lensectomy.
Introduction
The reported frequency of glaucoma or glaucoma suspect after cataract removal in infants and children varies, likely owing to different study designs, participant characteristics, and length of follow-up.1,2,3,4,5,6,7,8 In infants younger than 1 year at the time of lensectomy, glaucoma or glaucoma suspect has been reported within 1 year in 12%, increasing to 32% by 5 years. The Pediatric Eye Disease Investigator Group (PEDIG) developed a 5-year data registry to collect data on children undergoing lensectomy before 13 years of age.9 Herein, we (1) estimated the incidence of glaucoma or glaucoma suspect reported in the first year after lensectomy and (2) evaluated possible risk factors.
Methods
This cohort study followed a design reported previously.9 After obtaining approval from the local institutional review board, written informed consent from parent(s) or guardian(s), and assent from the child according to local institutional review board guidelines, study investigators enrolled 994 children (1361 eyes) younger than 13 years who underwent unilateral or bilateral lensectomy during the preceding 45 days at 1 of 61 sites in the United States (n = 57), Canada (n = 3), and the United Kingdom (n = 1) in a clinical research registry. (The full list of participating sites is provided in the eAppendix in the Supplement.) Medical and ophthalmic data were collected from medical record review at enrollment and annually thereafter. Participants were enrolled between June 2012 and July 2015, and annual visits occurred from January 2013 through August 2016. Data were analyzed between June 2017 and August 2019. If a contralateral eye underwent surgery within 1 year after lensectomy in the study eye, data for the contralateral eye were included in the analysis. Eyes with a preoperative diagnosis of either glaucoma or glaucoma suspect (90 eyes of 76 participants) or traumatic cataract (80 eyes of 78 participants) were excluded from analysis (Box). For the remaining 1191 eyes of 854 participants, data were included only if an office visit was documented between 6 and 18 months after lensectomy.
Box. Definitions of Glaucoma and Glaucoma Suspect.
-
The baseline presence of glaucoma or glaucoma suspect, which resulted in exclusion of the affected eye from the study, was defined by a report of the presence prior to lensectomy of at least 1 of the following conditions:
A diagnosis of glaucoma or glaucoma suspect by the investigator
Patient receiving systemic or ocular medications for glaucoma
Intraocular pressure (IOP) higher than 21 mm Hg
-
Glaucoma or glaucoma suspect after lensectomy was defined by any of the following criteria reported at the most recent office visit occurring between 6 months and 18 months following lensectomy:
Surgery for glaucoma in the eye
Use of systemic or ocular medications for glaucoma
Investigator diagnosis of glaucoma or glaucoma suspect in the eye
-
For diagnosing glaucoma or glaucoma suspect, investigators were provided the following criteria:
-
Glaucoma is defined as IOP higher than 21 mm Hg plus 1 of the following:
Abnormal corneal enlargement (≥11 mm)
Increased optic nerve cupping (postoperative increase of ≥0.2 in the horizontal cup-disc ratio compared with the preoperative ratio)
Use of an IOP-lowering medication
Glaucoma surgery
Glaucoma suspect is defined as IOP higher than 21 mm Hg without evidence of optic nerve damage, use of an IOP-lowering medication, or glaucoma surgery.
-
Statistical Analysis
The primary outcome was the proportion of eyes in which glaucoma or glaucoma suspect developed after lensectomy (Box). Poisson regression was used to estimate the overall number and percentage of eyes (with 95% CI) that developed glaucoma or glaucoma suspect and the relative risk (with 99% CI) for glaucoma or glaucoma suspect of each of the following baseline factors: race/ethnicity, sex, age at lensectomy, laterality of lensectomy (unilateral or bilateral), other ocular abnormalities (presence or absence), anterior vitrectomy (yes or no), intraocular lens (IOL) implantation, and the occurrence of intraoperative complications (yes or no). Backward stepwise selection was used to identify baseline factors associated with glaucoma or glaucoma suspect. At each step, the model factor with the largest P value was eliminated if the 2-sided P was >.01, and the eliminated factor with the smallest P value was added if the 2-sided P was <.01. Generalized estimating equations were used to account for the correlation between eyes of participants who received bilateral lensectomy. Analyses were performed using SAS software, version 9.4 (SAS Institute Inc).
Results
A total of 970 eyes of 702 patients were included in the analysis; 221 eyes of 152 patients without a documented office visit 6 to 18 months after lensectomy were excluded. Baseline characteristics of the sample are given in eTable 1 in the Supplement. Among the 702 patients who were included, 353 (50.3%) were male and 427 (60.8%) were white; mean age at lensectomy was 3.4 years (range, 0.04-12.9 years). Patients with an office visit were younger at lensectomy than those without an office visit (mean [SD] age, 3.4 [3.5] years vs 5.4 [4.1] years). Glaucoma or glaucoma suspect was diagnosed in 66 of 970 eyes (incidence risk after adjusting for correlation between eyes of participants who underwent bilateral lensectomy, 6.3%; 95% CI, 4.8%-8.3%) (Table). The presence of glaucoma in 52 of these 66 eyes was established on the basis of glaucoma surgery (n = 23), investigator diagnosis of glaucoma (n = 17), or use of glaucoma medications without investigator diagnosis of glaucoma (n = 12); glaucoma suspect was deemed present in the other 14 eyes. Mean age at lensectomy in the 66 eyes with a diagnosis of glaucoma or glaucoma suspect was 1.9 years (range, 0.07-11.2 years), and 40 of the 66 eyes (60.6%) were those of female patients.
Table. Risk of Glaucoma or Glaucoma Suspect According to Characteristics at Time of Lensectomy.
| Characteristic | No. of Eyes | Eyes With Glaucoma or Glaucoma Suspect, No. | Eyes With Glaucoma or Glaucoma Suspect, % (95% or 99% CI)a | Relative Risk (99% CI) | P Value |
|---|---|---|---|---|---|
| Overall measures | 970 | 66 | 6.3 (4.8-8.3) | NA | NA |
| Sex | |||||
| Female | 484 | 40 | 7.5 (4.7-12.0) | 1.47 (0.70-3.07) | .17 |
| Male | 486 | 26 | 5.1 (2.9-9.1) | 1 [Reference] | |
| Race/ethnicity | |||||
| African American | 117 | 15 | 11.0 (5.0-24.1) | 1.83 (0.74-4.58) | .43 |
| Other | 100 | 7 | 5.8 (1.8-18.4) | 0.96 (0.27-3.36) | |
| Hispanic | 160 | 7 | 4.6 (1.6-13.0) | 0.76 (0.24-2.40) | |
| White | 593 | 37 | 6.0 (3.7-9.7) | 1 [Reference] | |
| Anterior segment abnormality in addition to cataractb | |||||
| Yes | 102 | 14 | 12.9 (4.5-37.3) | 2.37 (0.68-8.32) | .08 |
| No | 857 | 51 | 5.4 (3.5-8.5) | 1 [Reference] | |
| Anterior vitrectomy at lensectomyc | |||||
| Yes | 739 | 58 | 7.0 (4.8-10.3) | 1.82 (0.83-3.98) | .04 |
| No | 219 | 7 | 3.9 (1.8-8.4) | 1 [Reference] | |
| Age at lensectomy | |||||
| ≤3 mo | 256 | 41 | 15.7 (10.1-24.5) | 4.57 (2.19-9.57) | <.001 |
| >3 mo to <13 y | 714 | 25 | 3.4 (1.9-6.2) | 1 [Reference] | |
| Primary intraocular lens implantd | |||||
| No | 438 | 53 | 11.2 (7.6-16.7) | 4.29 (1.84-10.01) | <.001 |
| Yes | 532 | 13 | 2.6 (1.2-5.6) | 1 [Reference] | |
| Laterality of cataracte | |||||
| Bilateral | 577 | 46 | 7.8 (4.9-12.5) | 1.54 (0.74-3.19) | .13 |
| Unilateral | 393 | 20 | 5.1 (2.9-8.9) | 1 [Reference] | |
| Intraoperative complications | |||||
| Yesf | 105 | 17 | 11.0 (4.6-26.2) | 1.94 (0.73-5.18) | .08 |
| No | 865 | 49 | 5.6 (3.8-8.5) | 1 [Reference] |
Abbreviation: NA, not applicable.
Percentages are adjusted for correlation between the eyes of patients who underwent bilateral lensectomy. The 95% CI is presented for overall outcome measures, and the 99% CI is presented for outcome measures pertaining to the specified demographic or procedural characteristic.
Ocular abnormality of the cornea, iris, or anterior chamber noted at the time of lensectomy. Excludes 11 eyes with anterior segment abnormality unknown.
Excludes 12 eyes with anterior vitrectomy unknown.
No indicates aphakia, yes, pseudophakia.
Not all eyes with cataracts were eligible for inclusion in the study.
The following surgical complications were reported at the time of lensectomy: cloudy cornea (11 eyes), dislocated implant (1 eye), hyphema (5 eyes), iris damage (6 eyes), iris prolapse (4 eyes), iris sphincterotomy (1 eye), lens fragment in vitreous (3 eyes), acute ocular hypertension (19 eyes), retained cortex (5 eyes), return to operating room (1 eye), unplanned iridectomy (4 eyes), and other (30 eyes).
Treatment included surgery in 23 of 66 eyes (34.8%), medication alone for 26 eyes (39.4%), and observation alone for 17 eyes (25.8%). The median (range) time interval from lensectomy to glaucoma surgery was 3.3 months (0.9-14.8 months); median age at lensectomy for this group was 1.4 months (range, 0.9-58.7 months). Twenty of the 23 surgical procedures for treatment of glaucoma (87.0%) were performed in eyes of children who had undergone lensectomy before age 3 months; these procedures included angle surgery, trabeculectomy, glaucoma drainage device placement, and peripheral iridectomy (eTable 2 in the Supplement).
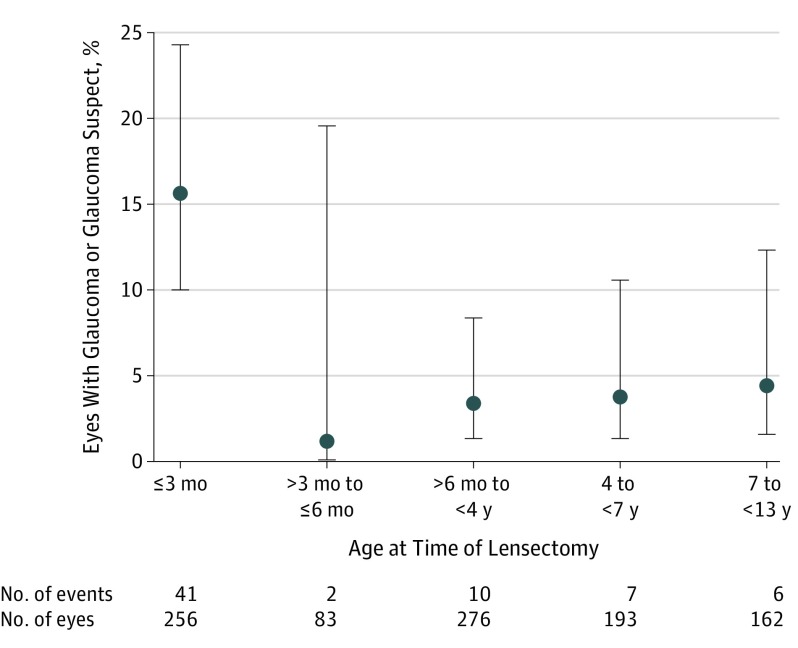
Backward stepwise selection resulted in 2 equivalent univariate models that showed associations for age (≤3 vs >3 months) and IOL implantation (aphakia vs pseudophakia) with glaucoma or glaucoma suspect. The incidence risk of glaucoma or glaucoma suspect was 15.7% (99% CI, 10.1%-24.5%) for 256 eyes of infants 3 months or younger at lensectomy vs 3.4% (99% CI, 1.9%-6.2%) for 714 eyes of infants older than 3 months (relative risk, 4.57; 99% CI, 2.19-9.57; P < .001) (Figure); the risk was 11.2% (99% CI, 7.6%-16.7%) in 438 aphakic eyes vs 2.6% (99% CI, 1.2%-5.6%) in 532 pseudophakic eyes (relative risk, 4.29; 99% CI, 1.84-10.01) (Table). No association was observed between risk of developing glaucoma or glaucoma suspect and other baseline characteristics (Table). Sensitivity analyses (1) including only data for eyes with glaucoma and not for those with glaucoma suspect (eTable 3 in the Supplement) and (2) limited to eyes of patients with a postoperative visit between 9 and 15 months (data not shown) yielded similar results.
Figure. Glaucoma or Glaucoma Suspect According to Age at Time of Lensectomy.
Data markers represent the risk of developing glaucoma or glaucoma suspect for each age category, and corresponding error bars represent the 99% CI for each risk. Poisson regression, using generalized estimating equations to adjust for the correlation between eyes of participants who underwent bilateral lensectomy, was used to estimate the incidence risk and corresponding 99% CI for each age category.
Discussion
Glaucoma or glaucoma suspect was reported for a minority of eyes in the first year after lensectomy in children younger than 13 years, with a higher incidence risk among those younger than 3 months at surgery than among those 3 months or older (15.7% vs 3.4%) and a higher risk in aphakic eyes compared with pseudophakic eyes (11.2% vs 2.6%).
The adjusted overall incidence risk of 6.3% for glaucoma plus glaucoma suspect in this large prospective registry is lower than that found in the prospective study by the British Isles Congenital Cataract Interest Group (BICCG)2 and the prospective Infant Aphakia Treatment Study (IATS) at 1 year after lensectomy; however, children older than 2 years were included in our registry, which likely reduced the observed rate. When we limited our analysis to the 339 eyes of 234 participants who were 6 months or younger at lensectomy, we obtained a risk of 11.4%, similar to the 1-year glaucoma risk of 13% reported in the BICCG study for infants 6 months or younger at lensectomy and to the 1-year risk of 12% reported in the prospective IATS study of unilateral cataract surgery performed in children older than 1 month but younger than 7 months. As in our study, the BICCG study found young age at lensectomy to be a risk factor for glaucoma after surgery for bilateral cataracts, and IATS also reported that younger age at lensectomy was a significant risk factor. Unlike our study, neither of the 2 aforementioned studies identified an association between IOL implantation and the risk of glaucoma (the BICCG study) or glaucoma plus glaucoma suspect (the IATS).
Limitations
Our study has several limitations. Our ability to identify risk factors for glaucoma or glaucoma suspect was limited by the low rate of glaucoma and glaucoma suspect. In addition, anterior vitrectomy and aphakia were more frequent in younger children, making it difficult to separate the contributions of these surgical variables from the contribution of age to the observed association with glaucoma and glaucoma suspect. Moreover, 152 (17.8%) of 854 patients who were enrolled in the clinical registry and were initially deemed eligible for participation in the study but who did not have a documented office visit between 6 and 18 months after lensectomy were excluded from our analysis.
Findings from this clinical registry are similar to those of prior studies, highlighting the risk of glaucoma and glaucoma suspect following lensectomy in children and adolescents. The timing of lensectomy in infancy must balance the desire to maximize vision (favoring earlier removal) against the desire to minimize the glaucoma risk (favoring later removal). Unmeasured ocular features in our study, rather than lensectomy itself, may predispose those requiring lensectomy at a younger age to diagnoses of glaucoma and glaucoma suspect. Although very young age at lensectomy and the presence of aphakia after lensectomy were associated with the occurrence of glaucoma or glaucoma suspect in the first year following lensectomy, these events also occurred in older children and pseudophakic eyes.
Conclusions
The associations observed in this study between postoperative aphakia and younger age at lensectomy and the development of glaucoma or glaucoma suspect within the first year after lensectomy suggest that frequent monitoring of children is warranted after lensectomy, especially of infants 3 months or younger at the time of lensectomy and children with aphakia. We expect to identify additional cases of glaucoma and glaucoma suspect in our cohort after 5 years of follow-up, perhaps with a different risk factor profile. Such long-term data may help the pediatric cataract surgeon better understand the risk factors and pathogenesis of glaucoma following lensectomy and may lead to improved treatment strategies.
eAppendix. Participating Clinical Sites
eTable 1. Baseline Characteristics of Eligible Children/Eyes Grouped by Those With and Those Without an Office Visit Between 6 and 18 Months Post-lensectomy
eTable 2. Glaucoma Surgery Performed in First Year Following Lensectomy
eTable 3. Risk of Glaucoma Only (Excluding Glaucoma Suspect) According to Characteristics at Time of Lensectomy
References
- 1.Beck AD, Freedman SF, Lynn MJ, Bothun E, Neely DE, Lambert SR; Infant Aphakia Treatment Study Group . Glaucoma-related adverse events in the Infant Aphakia Treatment Study: 1-year results. Arch Ophthalmol. 2012;130(3):300-305. doi: 10.1001/archophthalmol.2011.347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Solebo AL, Russell-Eggitt I, Cumberland PM, Rahi JS; British Isles Congenital Cataract Interest Group . Risks and outcomes associated with primary intraocular lens implantation in children under 2 years of age: the IoLunder2 cohort study. Br J Ophthalmol. 2015;99(11):1471-1476. doi: 10.1136/bjophthalmol-2014-306394 [DOI] [PubMed] [Google Scholar]
- 3.Freedman SF, Lynn MJ, Beck AD, Bothun ED, Örge FH, Lambert SR; Infant Aphakia Treatment Study Group . Glaucoma-related adverse events in the first 5 years after unilateral cataract removal in the Infant Aphakia Treatment Study. JAMA Ophthalmol. 2015;133(8):907-914. doi: 10.1001/jamaophthalmol.2015.1329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mataftsi A, Haidich AB, Kokkali S, et al. Postoperative glaucoma following infantile cataract surgery: an individual patient data meta-analysis. JAMA Ophthalmol. 2014;132(9):1059-1067. doi: 10.1001/jamaophthalmol.2014.1042 [DOI] [PubMed] [Google Scholar]
- 5.Lambert SR, Purohit A, Superak HM, Lynn MJ, Beck AD. Long-term risk of glaucoma after congenital cataract surgery. Am J Ophthalmol. 2013;156(2):355-361.e2. doi: 10.1016/j.ajo.2013.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirwan C, Lanigan B, O’Keefe M. Glaucoma in aphakic and pseudophakic eyes following surgery for congenital cataract in the first year of life. Acta Ophthalmol. 2010;88(1):53-59. doi: 10.1111/j.1755-3768.2009.01633.x [DOI] [PubMed] [Google Scholar]
- 7.Beck AD, Chang TC, Freedman SF, eds. Definition, classification and differential diagnosis In: Weinreb RN, Grajewski A, Papadopoulos M, Grigg J, Freedman SF, eds. Childhood Glaucoma. Amsterdam, the Netherlands: Kugler Publications; 2013. WGA Consensus Series, No. 9. [Google Scholar]
- 8.Urban B, Bakunowicz-Łazarczyk A. Aphakic glaucoma after congenital cataract surgery with and without intraocular lens implantation. Klin Oczna. 2010;112(4-6):105-107. [PubMed] [Google Scholar]
- 9.Repka MX, Dean TW, Lazar EL, et al. ; Pediatric Eye Disease Investigator Group . Cataract surgery in children from birth to less than 13 years of age: baseline characteristics of the cohort. Ophthalmology. 2016;123(12):2462-2473. doi: 10.1016/j.ophtha.2016.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Participating Clinical Sites
eTable 1. Baseline Characteristics of Eligible Children/Eyes Grouped by Those With and Those Without an Office Visit Between 6 and 18 Months Post-lensectomy
eTable 2. Glaucoma Surgery Performed in First Year Following Lensectomy
eTable 3. Risk of Glaucoma Only (Excluding Glaucoma Suspect) According to Characteristics at Time of Lensectomy