Abstract
Importance
Children with severe hearing loss are known to have more behavioral problems and may perform worse at school than children without. Few large-scale studies of slight to mild hearing loss are available.
Objective
To examine the relevance of slight to mild hearing loss by studying its association with behavioral problems and school performance.
Design, Setting, and Participants
This cross-sectional study was performed within an ongoing prospective birth cohort study in Rotterdam, the Netherlands. Participants were part of a population-based sample of children. Between ages 9 and 11 years, 5355 children underwent audiometric and behavioral evaluations. Children were excluded if they had missing data for either audiometry or both outcomes. Data were collected from April 2012 through October 2015. Data were analyzed from March to June 2018.
Exposures
Audiometric evaluation included pure-tone audiometry tests and speech-in-noise testing.
Main Outcomes and Measures
Child behavior was rated by the primary caregiver using the Child Behavior Checklist at ages 9 to 11 years (n = 4471). School performance was measured with a standardized test at age 12 years (n = 2399).
Results
The final sample included 4779 participants who were a mean (SD) age of 9.8 (0.3) years. The sample had nearly equal distribution between boys (n = 2200; 49.2%) and girls (n = 2271; 50.8%). Associations of hearing thresholds with behavioral problems differed between boys and girls. Among boys, higher pure-tone hearing thresholds at low frequencies were associated with higher total problem, social problem, and attention problem scores (total problems for the better-hearing ear: β = 0.01; 95% CI, 0-0.02). Higher speech reception thresholds were associated with higher attention problem scores among girls (β = 0.04; 95% CI, 0-0.08). Higher speech reception thresholds were associated with poorer school performance scores for both boys and girls (β = −0.06; 95% CI, −0.10 to −0.02).
Conclusions and Relevance
Higher hearing thresholds during pure-tone audiometric and speech-in-noise testing were associated with higher behavioral problem scores and poorer school performance. This supports the relevance of slight to mild hearing loss with these outcomes in school-aged children.
This cross-sectional study explores the association of slight to mild hearing loss with behavioral problems and school performance in children.
Key Points
Question
What is the association of slight to mild hearing loss with behavioral problems and school performance outcomes in children aged 9 to 11 years?
Findings
In this cross-sectional study, among 4779 children, increased hearing thresholds in the range of slight to mild hearing loss were associated with higher behavioral problem scores and lower test scores at the end of primary school.
Meaning
Children with slight to mild hearing loss may already show more behavioral problems and poorer school performance; these findings indicate the relevance of slight to mild hearing loss in daily life.
Introduction
Hearing loss among children is prevalent, with recent population-based studies reporting increased pure-tone hearing thresholds among 15.2% to 22.6% of school-aged children.1,2,3 These figures comprise mainly slight hearing loss at the 16-dB to 25-dB hearing level (HL), which often is not acknowledged as clinically relevant. In practice, relevant hearing loss is usually defined as hearing loss of mild or worse degree, starting from a hearing threshold of 26-dB to 40-dB HL.4 Given this discrepancy between scientific studies and clinical practice, the clinical relevance of slight to mild hearing loss remains unknown.5 However, children with increased hearing thresholds, although limited, may experience negative consequences.
The literature shows that children with mild to severe hearing loss have worse language development and school performance than those without.6,7,8 For instance, compared with children with normal hearing, children with mild or severe hearing impairment displayed lower scores on short-term and sequential memory, attention, language, and verbal and nonverbal IQ tests. Also, children with mild to severe hearing loss showed more emotional and behavioral problems than children with normal hearing.9 Similar associations with behavioral problems and school performance are suggested among children with slight to mild hearing loss.10,11 However, large population-based studies are scarce.
The objective of the present study is to examine the association of hearing thresholds and slight to mild hearing loss with behavior and school performance among children from a large population-based cohort. These results will help to clarify the clinical relevance of slight to mild hearing loss in children.
Methods
Study Design and Sample
The current study was embedded in the Generation R Study,12 a prospective population-based birth cohort study in Rotterdam, the Netherlands, that observes its participants from early fetal life until young adulthood. Participants were born between January 2002 and December 2006, underwent regular physical examinations, and completed repeated questionnaires. At the age of approximately 9 years, children and their primary caregivers were invited for another examination phase. A total of 7393 children visited the research center and/or completed questionnaires.13 Children were eligible for the present study if they completed pure-tone audiometric testing (n = 5368). Exclusion criteria were moderate or worse bilateral hearing loss (hearing threshold, >40-dB HL) or missing data for both behavioral and school performance outcomes (n = 589). Oral and written informed consent was obtained for all measurements. The study design and all research aims were approved by the medical ethics committee of Erasmus University Medical Center, Rotterdam, the Netherlands.
Behavioral and School Performance Outcomes
Child behavior between ages 9 and 11 years was assessed using a parental questionnaire, the Child Behavior Checklist (CBCL), a measure designed for children aged 6 to 18 years.13,14 The CBCL is a widely used, reliable, and valid measure for emotional and behavioral problems and is also validated in Dutch.15,16 The CBCL was completed by the primary caregiver, usually the mother. Items concerned the previous 6 months and were rated on a 3-point Likert scale (not true, somewhat true, or very true). Besides the total problem score, the current study used the attention problem, social problem, internalizing problem, and externalizing problem subscales.
School performance was measured using a standardized school achievement test of the Central Institute for Test Development (Cito). The Cito test is used by approximately 77% of primary schools in the Netherlands as a standardized measure of academic performance.17,18,19 The test assesses different areas, including language, mathematics, and world orientation (optional), and gives an indication of the child’s intelligence, motivation, concentration, and drive to learn. It is administered in the final year of primary school, just before children move on to secondary school, usually around age 12 years. After the number of correct answers is determined, final scores range from 501 to 550 and inform parents and teachers about the most suitable type of secondary education (eTable 2 in theSupplement). The Cito test scores for the study participants were obtained from Cito if they were available and if participant consent was given.
Hearing Determinants
Audiometric testing was conducted in all children during the physical assessment between ages 9 and 11 years. All audiometric tests were conducted by trained research assistants in a soundproofed booth according to standard 8253-1 from the International Organization for Standardization.
Pure-tone audiometric testing was performed at 7 frequencies (0.5, 1, 2, 3, 4, 6, and 8 kHz) using the shortened ascending method based on standard 8253-1. Air-conduction pure-tone hearing thresholds were defined by the intensity level at which the tone was heard in 2 of 3 ascents, as described by le Clercq et al.1 On the basis of the overall pure-tone average, the better-hearing ear was determined. For both ears, the low-frequency pure-tone average (LPTA; mean of 0.5, 1, and 2 kHz) and high-frequency pure-tone average (HPTA; mean of 3, 4, and 6 kHz) were calculated. Missing data for pure-tone audiometric testing were due to technical problems or lack of time.
Subsequently, speech-in-noise testing was performed if time allowed. The speech reception threshold (SRT) in decibel signal-to-noise ratio (SNR) was determined using the Dutch digits-in-noise test, which is validated for use in children 5 years and older.20 The test offered digit triplets and speech-shaped noise (stationary at a constant LPTA level of 70-dB sound pressure) in the better-hearing ear in a specified ratio, starting the first triplet at a −10-dB SNR. After 24 triplets, the SRT (in SNR) was automatically calculated by the computer for the last 20 SNRs.
Covariates
Covariates were selected based on the literature or previous findings. Sex and gestational age of the children were obtained from the medical records from community midwives and obstetricians. Gestational age at birth was categorized as preterm birth (<37 weeks’ gestation) or term birth. Global area of origin was based on the self-reported country of birth of the parents and categorized according to Kooijman et al13 as Western (European, Western American [including the United States and Canada], Western Asian [including Japan and Indonesia], or Oceania) or non-Western. Household income was classified as low, middle, or high based on total study population tertiles. Maternal education was based on the highest attained educational level and classified as low (no or primary education only), middle (secondary/vocational education), or high (higher level of professional education or university education). Maternal and paternal psychopathologic symptoms included anxiety, depressive symptoms, hostility, and psychoticism and were assessed using the Brief Symptom Inventory.21
Statistical Analyses
The CBCL problem scores and Cito test scores were used as continuous outcome variables, assessing the total scores as well as their respective subscale scores. Because of skewness, a square root transformation was applied to the CBCL problem scores. Standardized z scores were used for both CBCL problem scores (after square root transformation) and Cito test scores.
Multiple linear regression analyses were used to study the association of hearing acuity with CBCL problem and Cito test scores. All analyses were adjusted for sex and age of the child. Other covariates were included when they changed the effect estimates by 10% or more. On the basis of this criterion, gestational age at birth, ethnicity of the child, maternal educational level, household income, and parental psychopathologic symptoms were included in the analyses. Year of Cito testing and CBCL attention problem scores were additionally included in the analyses of school performance. Because possible sex differences were considered, we tested interaction terms of hearing thresholds analyzing sex in association with behavior and school performance. If an interaction was present (defined as P < .10), the analyses were stratified by sex. All analyses were checked for nonlinearity, which was not present, using restricted cubic splines with 3 knots. Statistical significance was set at α < .05 using a 2-tailed test.
For missing data on covariates, we used multiple imputation according to the predictive mean matching method in SPSS, version 24.0 (IBM). Ten independent data sets were generated, and pooled estimates were calculated. Measures of association are presented using standardized β coefficients with 95% CIs. Statistical analyses were carried out using R statistical software, version 3.3.2 (The R Foundation).
Results
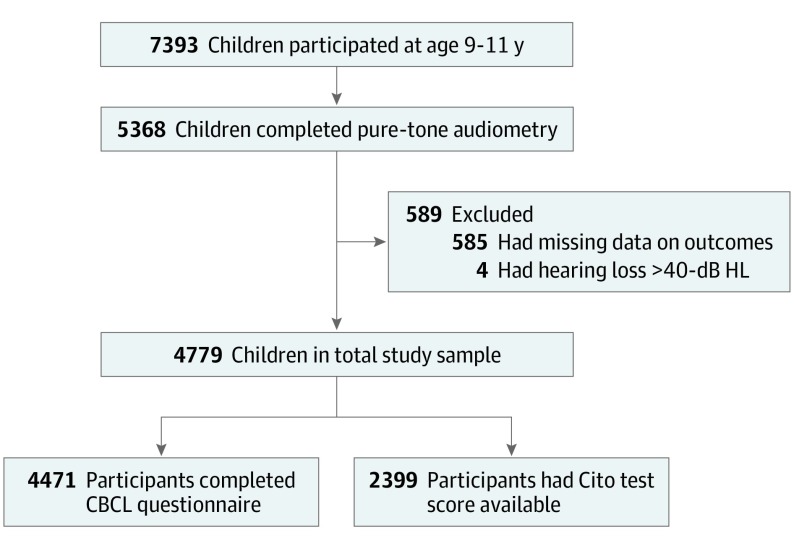
The final study sample included 4779 children: 4471 children (93.6%) in the analyses of behavioral problems and 2399 children (50.2%) in the analyses of school performance (Figure 1). The children included in the analyses were slightly younger, were more often from Western areas of origin, had better hearing, and had a higher maternal educational level and household income than children who were excluded from the study (eTable 1 in the Supplement). Table 1 shows the descriptive characteristics of the study sample. The included children had a mean (SD) age of 9.8 (0.3) years with a nearly even distribution of boys and girls (Table 1). Besides a slightly better SRT among the school performance study sample, there were no differences between the study samples.
Figure 1. Flowchart of the Included Study Sample.
CBCL indicates Child Behavior Checklist; Cito, Central Institute for Test Development; HL, hearing level.
Table 1. Descriptive Characteristics of the Behavior Study Sample in the Study Population.
| Characteristic | Behavior Study Sample, No. (%) |
|---|---|
| No. of participants | 4471 |
| Sociodemographic Characteristics | |
| Age, median (IQR), y | 9.7 (9.6-9.9) |
| Sex | |
| Male | 2200 (49.2) |
| Female | 2271 (50.8) |
| Ethnicity | |
| Western | 3280 (73.4) |
| Non-Western | 1142 (25.5) |
| Missing | 49 (1.1) |
| Gestational age at birth, mean (SD), wka | 39.8 (1.9) |
| Birth weight, mean (SD), g | 3417.0 (577.6) |
| Maternal educational level | |
| None or primary education only | 84 (1.9) |
| Secondary education | 1455 (32.5) |
| Higher education | 2535 (56.7) |
| Missing | 397 (8.9) |
| Household income, tertile | |
| Lowest | 953 (21.3) |
| Middle | 1465 (32.8) |
| Highest | 1460 (32.7) |
| Missing | 593 (13.3) |
| Hearing Acuity | |
| Better-hearing ear, mean (SD), dB HL | |
| LPTA | 6.5 (4.7) |
| HPTA | 6.6 (4.9) |
| Worse-hearing ear, mean (SD), dB HL | |
| LPTA | 9.2 (5.9) |
| HPTA | 9.8 (6.3) |
| SRT, mean (SD), dB SNR | 5.7 (1.5) |
Abbreviations: HL, hearing level; HPTA, high-frequency pure-tone average; IQR, interquartile range; LPTA, low-frequency pure-tone average; SNR, signal-to-noise ratio; SRT, speech reception threshold.
There were 270 children (6.1%) with preterm birth (gestational age <37 wk).
Child Hearing Acuity and Behavioral Problems
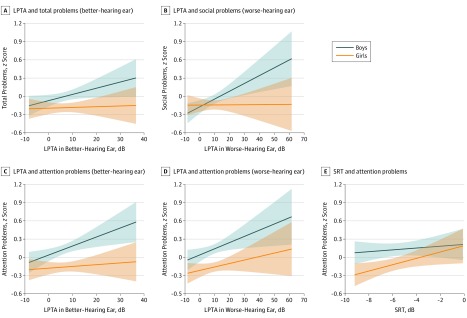
The analyses of hearing acuity with total behavioral problem scores showed a significant interaction between LPTA and sex (F = 5.59; P = .02), after which the analyses were stratified. Figure 2 displays the significant results stratified by sex. All individual analyses are presented in eTable 3 in the Supplement.
Figure 2. Association of Standardized Child Hearing Acuity With Standardized Behavioral Problem Scores in Boys (n = 2200) and Girls (n = 2271).
A, Low-frequency pure-tone average (LPTA) of the better-hearing ear with Child Behavior Checklist total problem z scores. B, Low-frequency pure-tone average of the worse-hearing ear with Child Behavior Checklist social problem z scores. C, Low-frequency pure-tone average of the better-hearing ear with Child Behavior Checklist attention problem z scores. D, Low-frequency pure-tone average of the worse-hearing ear with Child Behavior Checklist attention problem z scores. E, Speech reception threshold (SRT) with Child Behavior Checklist attention problem z scores (data available for 1228 boys and 1260 girls). All analyses were adjusted for age, gestational age at birth, global area of origin, maternal educational level, household income, and maternal and paternal psychopathologic symptoms.
Among boys, higher LPTA in the better-hearing ear was associated with a higher CBCL total problem score after adjustment for all relevant covariates (per 1-dB LPTA: β = 0.010; 95% CI, 0.001-0.018) (Figure 2A). More specifically, for every 1-dB higher LPTA, the problem score was 0.01 SD higher, corresponding with a 0.15-point higher score. This was mainly due to an association of the LPTA of the better-hearing ear with attention problems (per 1-dB LPTA: β = 0.012; 95% CI, 0.003-0.020 (Figure 2B). The LPTA of the worse-hearing ear was also associated with attention problems among boys (per 1-dB LPTA: β = 0.009; 95% CI, 0.002-0.016) (Figure 2C), as well as with social problems (per 1-dB LPTA: β = 0.010; 95% CI, 0.002-0.017) (Figure 2D). The HPTA of neither the better-hearing ear nor the worse-hearing ear (nor SRT) were associated with CBCL scores among boys. Hearing acuity was not associated with internalizing or externalizing CBCL scores among boys.
Among girls, higher SRTs were associated with more attention problems (per 1-dB SRT: β = 0.039; 95% CI, 0.002-0.076) (Figure 2E). This corresponds to a 0.13-point higher attention problem score for every 1-dB higher SRT. No other associations of SRTs or pure-tone hearing thresholds with CBCL problem scores were observed among girls.
Child Hearing Acuity and School Performance
The analyses with school performance outcomes showed that higher HPTA in the worse-hearing ear and higher SRTs were associated with lower total Cito test scores (HPTA: β = −0.006; 95% CI, −0.012 to −0.001; SRT: β = −0.061; 95% CI, −0.097 to −0.024) (Table 2). For each 1-dB higher HPTA, total Cito scores were 0.1 points lower, and for each 1-dB higher SRT, total Cito scores were 0.6 points lower. The LPTA and HPTA in either ear were not associated with total scores or with scores on the subscales for language and mathematics. The SRTs were associated with both language (β = −0.054; 95% CI, −0.088 to −0.019) and mathematics (β = −0.054; 95% CI, −0.090 to −0.018) subscale scores. All pure-tone hearing thresholds were associated with Cito test scores on the optional world orientation scale (LPTA of the better-hearing ear: β = −0.011; 95% CI, −0.021 to −0.001; LPTA of the worse-hearing ear: β = −0.013; 95% CI, −0.022 to −0.005; corresponding with a 0.1-point lower score per 1-dB higher LPTA), whereas SRTs were not. No sex interactions were found.
Table 2. Association of Standardized Child Hearing Acuity With Central Institute for Test Development (Cito) Test z Scores and Cito Test Subscale z Scores (n = 2399).
| Measure | Cito Test z Score, β (95% CI)a |
|---|---|
| Cito Test Total Score | |
| Better-hearing ear | |
| LPTA | 0.002 (−0.010 to −0.006) |
| HPTA | −0.005 (−0.012 to 0.002) |
| Worse-hearing ear | |
| LPTA | −0.004 (−0.011 to 0.002) |
| HPTA | −0.006 (−0.012 to −0.001) |
| SRTb | −0.061 (−0.097 to −0.024) |
| Cito Language Subscale Score | |
| Better-hearing ear | |
| LPTA | −0.001 (−0.008 to 0.006) |
| HPTA | −0.003 (−0.010 to 0.004) |
| Worse-hearing ear | |
| LPTA | −0.004 (−0.011 to 0.002) |
| HPTA | −0.005 (−0.011 to 0) |
| SRTb | −0.054 (−0.088 to −0.019) |
| Cito Mathematics Subscale Score | |
| Better-hearing ear | |
| LPTA | −0.003 (−0.010 to 0.004) |
| HPTA | −0.007 (−0.014 to 0) |
| Worse-hearing ear | |
| LPTA | −0.003 (−0.009 to 0.004) |
| HPTA | −0.006 (−0.011 to 0) |
| SRTb | −0.054 (−0.090 to −0.018) |
| Cito World Orientation Subscale Scorec | |
| Better-hearing ear | |
| LPTA | −0.011 (−0.021 to −0.001) |
| HPTA | −0.010 (−0.019 to −0.001) |
| Worse-hearing ear | |
| LPTA | −0.013 (−0.022 to −0.005) |
| HPTA | −0.013 (−0.020 to −0.005) |
| SRTd | −0.035 (−0.084 to 0.014) |
Abbreviations: HPTA, high-frequency pure-tone average; LPTA, low-frequency pure-tone average; SRT, speech reception threshold.
Adjusted for age, sex, gestational age at birth, global area of origin, maternal educational level, household income, Child Behavior Checklist attention problem score, maternal and paternal psychopathologic symptoms, and year of Cito testing.
Data available for 1191 participants.
Optional subscale from the Cito test with a smaller sample (n = 1418).
Data available for 677 participants.
Discussion
Our study showed that higher hearing thresholds with pure-tone audiometric and speech-in-noise testing were associated with more behavioral problems and poorer school performance. These findings support the clinical relevance of slight to mild hearing loss in daily life.
Slightly impaired development of auditory perception may underlie problems in behavior and school performance among children with slight to mild hearing loss. Auditory processing and auditory separation develop during childhood22 and are estimated to be adultlike by approximately 12 years of age.23 Younger children are still developing their auditory memory and are likely more dependent on complete auditory input. In addition, hearing in daily life is dependent on binaural functioning. Hearing thresholds in the better-hearing ear depict the potential perception of sound, and those in the worse-hearing ear represent binaural function and possible asymmetric or unilateral hearing loss.24,25 In general, vowels tend to be low pitched, whereas consonants include high frequencies.26 To understand speech, sufficient hearing thresholds at both low and high frequencies are required. In the present study, we hypothesized that reduced auditory input, expressed as increased hearing thresholds in the range of slight to mild hearing loss, would affect child functioning in daily life.
We showed an association of higher HPTA in the worse-hearing ear and higher SRTs with lower Cito test scores. Every 1-dB increase in HPTA and SRT corresponded to an approximately 0.1-point and 0.6-point decrease in Cito test score, respectively. Taking our findings into account, a child with hearing at the 0-dB HL (ie, normal hearing) had a mean (SD) Cito test score of 538 (9.3) points, whereas a child with slight hearing loss (hearing threshold of 15-dB to 25-dB HL) had a mean (SD) Cito test score between 536 (9.8) and 537 (12.5) points. Although the absolute difference attributed to hearing thresholds might be small, it might affect the advised secondary educational level of the child (eTable 2 in the Supplement). High-frequency, asymmetric, and unilateral hearing loss were found to be associated with impaired speech recognition.25,27 Children with a higher HPTA in the worse-hearing ear are likely to miss distinctions of speech, especially with background noise, as often is the case in the classroom. We observed that SRTs were more strongly associated with Cito test scores than were pure-tone hearing thresholds. The SRTs involve a more complex combination of pathways, including central processing, and therefore might have a stronger association with the child’s cognitive functioning than pure-tone hearing thresholds. In addition, SRTs are dependent on the child’s age.28 The Cito test is taken in the final grade of primary school, generally around 12 years of age.19 With this in mind, our findings are in line with those of Bess et al.10 They observed lower scores on reading and language tests for children aged 9 years with slight to mild hearing loss but not for children aged 11 and 15 years. Language and mathematics are considered important skills in the Dutch school system, and children frequently receive extra training in these subjects. Therefore, worse language and mathematics development might be obviated by extra tutoring in the older children, or even by repeating a grade. In contrast, pure-tone hearing thresholds were associated with world orientation scores. World orientation, including geography and history, is not included in the final Cito test scores and has fewer consequences for secondary school level. For this reason, it might be considered a less important school performance outcome than language and mathematics. These areas of school performance may have more sensitivity in identifying children who struggle to keep up. In addition, whereas language (especially grammar and spelling) and mathematics are based on written exercises, world orientation is probably based more on oral narratives and thus is more dependent on auditory status.
We observed that LPTA was associated with CBCL problem scores among boys. More specifically, LPTA in the better-hearing ear was associated with the total problem score, LPTA in the worse-hearing ear was associated with social problems, and LPTA in both the better-hearing and worse-hearing ears was associated with attention problems. Among girls, SRTs were associated with attention problem scores. No other associations were observed among girls. Attention and social problems among children with hearing loss have been described previously, including in slight to mild hearing loss.9,10 Amplification or cochlear implantation may even reduce problems among children with hearing loss.6,29,30 The association with attention and social problems in these children could be explained by increased difficulties listening to speech under adverse conditions, requiring more energy compared with normal-hearing peers.31 Although high-frequency hearing is involved in the understanding of speech, nearly all vowels and many consonants are at low frequencies, supporting the importance of LPTA to perceive speech. This could explain the association of LPTA with attention and social problems among boys. However, considering the perception of speech, an association of SRT with attention problems was expected not only among girls but also among boys.
To our knowledge, this is the first study reporting different associations of slight to mild hearing loss with behavioral problems and school performance between boys and girls. In childhood and early adolescence, boys are more likely to show avoidant or unproductive coping behaviors, whereas girls display more problem-focused coping strategies and social-support seeking.32,33 Among adolescents who are deaf or hard of hearing, girls tend to seek more social support than boys.34 Moreover, deaf boys tend to have more difficulty achieving good relationships with normal-hearing peers than deaf girls.35 Our results suggest that social problems among boys with hearing loss also apply to slight to mild hearing loss.
We observed no association of hearing thresholds with scores on internalizing problem or externalizing problem subscales. A 2015 systematic review9 showed that associations of hearing loss with internalizing and externalizing problems are inconsistent in the literature and most often not stratified by sex. Considering both these and our current findings, the effects of slight to mild hearing loss are likely to be more general rather than affecting specific domains of functioning, such as emotional problems or disruptive behavior.
Strengths and Limitations
The present study has several strengths, including a large population-based sample that reflects the relatively common prevalence of slight hearing loss. Second, several potential confounders have been considered in the analyses. The results for behavioral problems were independent of parental psychopathologic symptoms and socioeconomic background, and the results for school performance were independent of any attention problems. Nevertheless, residual confounding cannot be excluded.
Other limitations must be considered as well. In a cross-sectional study, it is difficult to infer the direction of the associations. We assume that hearing loss is a precursor to behavioral problems and poor school performance, but these problems might lead to hearing loss owing to a poor lifestyle or more risky behavior. Also, children with behavioral problems may tend to perform worse on audiometric testing, which requires the participant’s concentration. Furthermore, we used behavioral problem scores as rated by the primary caregiver, which could be biased. The Cito test scores are a more objective measure, although they reflect a single measurement that could be influenced by situational factors, such as stress, fatigue, or illness. Because the study sample was based on the general population and children with more severe hearing loss were excluded, we do not believe that additional disabilities associated with hearing loss or the use of hearing loss interventions, such as hearing aids, influenced the results. No information was available on whether children or their parents or caregivers were aware of the child’s hearing status.
Generation R Study12,13 participants were most often of Dutch origin and relatively highly educated, and the study takes place in the Dutch school system. This makes generalization of the results to other countries more difficult. Future studies should include longitudinal analyses to replicate the observed associations across different ages and to give more insight in the direction of the association. These studies should preferably include children’s self-reported emotional and behavioral problems as well as an objective measure of educational performance. For now, children with known increased hearing thresholds should be given a front seat in the classroom or auditory devices to optimize their auditory input. In children who seem to struggle, show aberrant behavior, or have poorer school performance, hearing testing should be considered.
Conclusions
Our findings demonstrate that children with slight to mild hearing loss appear to perform worse at school than children with normal hearing. Additionally, boys with slight to mild hearing loss appear to have slightly more attention and social problems compared with girls with slight to mild hearing loss. Although the observed associations may be small, these findings emphasize that children with increased hearing thresholds (without overt hearing loss) may experience poorer functioning in daily life and may benefit from extra support. On the other hand, possible hearing loss should be considered for children who experience attention, social, or school performance difficulties. The relevance of slight to mild hearing loss should be acknowledged not only in scientific research but also in clinical practice.
eTable 1. Differences between included (n = 4779) and excluded (n = 589) participants.
eTable 2. Cito test scores and corresponding advice for secondary educational level.
eTable 3. The association of child hearing acuity with standardized behavioral problem scores in boys (n = 2200) and girls (n = 2271).
References
- 1.le Clercq CMP, van Ingen G, Ruytjens L, et al. Prevalence of hearing loss among children 9 to 11 years old: the Generation R Study. JAMA Otolaryngol Head Neck Surg. 2017;143(9):928-934. doi: 10.1001/jamaoto.2017.1068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Su BM, Chan DK. Prevalence of hearing loss in US children and adolescents: findings from NHANES 1988-2010. JAMA Otolaryngol Head Neck Surg. 2017;143(9):920-927. doi: 10.1001/jamaoto.2017.0953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang J, le Clercq CMP, Sung V, et al. Cross-sectional epidemiology of hearing loss in Australian children aged 11-12 years old and 25-year secular trends. Arch Dis Child. 2018;103(6):579-585. doi: 10.1136/archdischild-2017-313505 [DOI] [PubMed] [Google Scholar]
- 4.Clark JG. Uses and abuses of hearing loss classification. ASHA. 1981;23(7):493-500. [PubMed] [Google Scholar]
- 5.Schlauch RS, Carney E. The challenge of detecting minimal hearing loss in audiometric surveys. Am J Audiol. 2012;21(1):106-119. doi: 10.1044/1059-0889(2012/11-0012) [DOI] [PubMed] [Google Scholar]
- 6.Khan S, Edwards L, Langdon D. The cognition and behaviour of children with cochlear implants, children with hearing aids and their hearing peers: a comparison. Audiol Neurootol. 2005;10(2):117-126. doi: 10.1159/000083367 [DOI] [PubMed] [Google Scholar]
- 7.Tomblin JB, Harrison M, Ambrose SE, Walker EA, Oleson JJ, Moeller MP. Language outcomes in young children with mild to severe hearing loss. Ear Hear. 2015;36(suppl 1):76S-91S. doi: 10.1097/AUD.0000000000000219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lieu JE. Unilateral hearing loss in children: speech-language and school performance. B-ENT. 2013;(suppl 21):107-115. [PMC free article] [PubMed] [Google Scholar]
- 9.Stevenson J, Kreppner J, Pimperton H, Worsfold S, Kennedy C. Emotional and behavioural difficulties in children and adolescents with hearing impairment: a systematic review and meta-analysis. Eur Child Adolesc Psychiatry. 2015;24(5):477-496. doi: 10.1007/s00787-015-0697-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bess FH, Dodd-Murphy J, Parker RA. Children with minimal sensorineural hearing loss: prevalence, educational performance, and functional status. Ear Hear. 1998;19(5):339-354. doi: 10.1097/00003446-199810000-00001 [DOI] [PubMed] [Google Scholar]
- 11.Khairi Md Daud M, Noor RM, Rahman NA, Sidek DS, Mohamad A. The effect of mild hearing loss on academic performance in primary school children. Int J Pediatr Otorhinolaryngol. 2010;74(1):67-70. doi: 10.1016/j.ijporl.2009.10.013 [DOI] [PubMed] [Google Scholar]
- 12.Hofman A, Jaddoe VW, Mackenbach JP, et al. Growth, development and health from early fetal life until young adulthood: the Generation R Study. Paediatr Perinat Epidemiol. 2004;18(1):61-72. doi: 10.1111/j.1365-3016.2003.00521.x [DOI] [PubMed] [Google Scholar]
- 13.Kooijman MN, Kruithof CJ, van Duijn CM, et al. The Generation R Study: design and cohort update 2017. Eur J Epidemiol. 2016;31(12):1243-1264. doi: 10.1007/s10654-016-0224-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Achenbach TM, Ruffle TM. The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatr Rev. 2000;21(8):265-271. doi: 10.1542/pir.21-8-265 [DOI] [PubMed] [Google Scholar]
- 15.Ivanova MY, Achenbach TM, Rescorla LA, et al. Preschool psychopathology reported by parents in 23 societies: testing the seven-syndrome model of the child behavior checklist for ages 1.5-5. J Am Acad Child Adolesc Psychiatry. 2010;49(12):1215-1224. doi: 10.1097/00004583-201012000-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verhulst FC, Van der Ende J. ASEBA Manual: Questionnaires for Ages 6 to 18 Years [in Dutch] . Rotterdam, the Netherlands: ASEBA Nederland; 2013. [Google Scholar]
- 17.College voor Toetsen en Examens Throwback Central Final Test 2015 [in Dutch]. https://www.centraleeindtoetspo.nl/binaries/centraleeindtoets/documenten/publicaties/2016/09/09/terugblik-centrale-eindtoets-2015/Terugblik_2015_met_rectificatie_aug_2016.pdf. Accessed October 22, 2019.
- 18.van der Lubbe M. The End of Primary School Test. https://docplayer.net/21810435-The-end-of-primary-school-test-marleen-van-der-lubbe-cito-the-netherlands.html. Accessed April 17, 2018.
- 19.College voor Toetsen en Examens Throwback 2016: results of the End of Primary Education Test [in Dutch]. https://www.centraleeindtoetspo.nl/binaries/centraleeindtoets/documenten/publicaties/2017/04/04/terugblik-2016/CvTE_PO_terugblik_2016-def.pdf. Accessed October 22, 2019.
- 20.Smits C, Theo Goverts S, Festen JM. The digits-in-noise test: assessing auditory speech recognition abilities in noise. J Acoust Soc Am. 2013;133(3):1693-1706. doi: 10.1121/1.4789933 [DOI] [PubMed] [Google Scholar]
- 21.De Beurs E. Brief Symptom Inventory [in Dutch] . Leiden, the Netherlands: Pits Publishers; 2004. [Google Scholar]
- 22.Yathiraj A, Vanaja CS. Age related changes in auditory processes in children aged 6 to 10 years. Int J Pediatr Otorhinolaryngol. 2015;79(8):1224-1234. doi: 10.1016/j.ijporl.2015.05.018 [DOI] [PubMed] [Google Scholar]
- 23.Keith RW. Development and standardization of SCAN-C Test for Auditory Processing Disorders in Children. J Am Acad Audiol. 2000;11(8):438-445. [PubMed] [Google Scholar]
- 24.Kuppler K, Lewis M, Evans AK. A review of unilateral hearing loss and academic performance: is it time to reassess traditional dogmata? Int J Pediatr Otorhinolaryngol. 2013;77(5):617-622. doi: 10.1016/j.ijporl.2013.01.014 [DOI] [PubMed] [Google Scholar]
- 25.Vila PM, Lieu JE. Asymmetric and unilateral hearing loss in children. Cell Tissue Res. 2015;361(1):271-278. doi: 10.1007/s00441-015-2208-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ladefoged P. Vowels and Consonants: An Introduction to the Sounds of Languages. Oxford, United Kingdom: Blackwell; 2001. [Google Scholar]
- 27.Van Tasell DJ, Yanz JL. Speech recognition threshold in noise: effects of hearing loss, frequency response, and speech materials. J Speech Hear Res. 1987;30(3):377-386. doi: 10.1044/jshr.3003.377 [DOI] [PubMed] [Google Scholar]
- 28.Koopmans WJA, Goverts ST, Smits C. Speech recognition abilities in normal-hearing children 4 to 12 years of age in stationary and interrupted noise. Ear Hear. 2018;39(6):1091-1103. doi: 10.1097/AUD.0000000000000569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Horn DL, Davis RA, Pisoni DB, Miyamoto RT. Development of visual attention skills in prelingually deaf children who use cochlear implants. Ear Hear. 2005;26(4):389-408. doi: 10.1097/00003446-200508000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quittner AL, Barker DH, Snell C, et al. Improvements in visual attention in deaf infants and toddlers after cochlear implantation. Audiol Med. 2007;5(4):242-249. doi: 10.1080/16513860701745401 [DOI] [Google Scholar]
- 31.Downs DW. Effects of hearing and use on speech discrimination and listening effort. J Speech Hear Disord. 1982;47(2):189-193. doi: 10.1044/jshd.4702.189 [DOI] [PubMed] [Google Scholar]
- 32.Eschenbeck H, Kohlmann C-W, Lohaus A. Gender differences in coping strategies in children and adolescents. J Individ Differ. 2007;28(1):18-26. doi: 10.1027/1614-0001.28.1.18 [DOI] [Google Scholar]
- 33.Morales Rodríguez FM, Torres MVT, Páez JM. Gender and age differences in how children cope with daily stress. Electron J Res Educ Psychol. 2012;10(1):95-110. [Google Scholar]
- 34.Eschenbeck H, Gillé V, Heim-Dreger U, Schock A, Schott A. Daily stress, hearing-specific stress and coping: self-reports from deaf or hard of hearing children and children with auditory processing disorder. J Deaf Stud Deaf Educ. 2017;22(1):49-58. doi: 10.1093/deafed/enw053 [DOI] [PubMed] [Google Scholar]
- 35.Martin D, Bat-Chava Y. Negotiating deaf-hearing friendships: coping strategies of deaf boys and girls in mainstream schools. Child Care Health Dev. 2003;29(6):511-521. doi: 10.1046/j.1365-2214.2003.00371.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Differences between included (n = 4779) and excluded (n = 589) participants.
eTable 2. Cito test scores and corresponding advice for secondary educational level.
eTable 3. The association of child hearing acuity with standardized behavioral problem scores in boys (n = 2200) and girls (n = 2271).