Abstract
Background
Electronic health records (EHRs) have become ubiquitous in orthopaedics. Although they offer certain benefits, they have been cited as a factor that can contribute to provider burnout. Little is known about the degree to which EHR adoption is associated with provider and practice characteristics or outpatient and surgical volume.
Questions/purposes
(1) What was the rate of EHR adoption in orthopaedics and how are physician and practice characteristics associated with adoption? (2) How is EHR adoption related to outpatient productivity? (3) How is EHR adoption associated with surgical volume?
Methods
We conducted this retrospective analysis by linking three publicly available Medicare databases, which we chose for their reliability in reporting because they are provided by a government-funded entity. We included providers in the 2016 Physician Compare dataset who reported a primary specialty of orthopaedic surgery. The EHR adoption status for these providers between 2011 and 2016 was determined using the Meaningful Use Eligible Professional public use files, which we chose to standardize both adoption and usage of EHRs. Provider characteristics, from the Physician Compare dataset, were compared between non-adopters, early adopters (who adopted EHR in 2011 and 2012), and late adopters (2016) using a multivariate logistic analysis, due to the binary nature of the dependent variable (adoption). To measure productivity and billing, we used the 2012 and 2016 Medicare Utilization and Payment datasets. To measure productivity before and after EHR adoption, we compared the number of services for select Current Procedural Terminology codes between 2012 and 2016 for providers who first adopted EHR in 2013, and performed the same comparison for non-adopters for the same years. Paired t-tests were used where volume in 2012 and 2016 were being compared, and multivariate analysis was performed.
Results
By 2016, 10,904 of 21,484 orthopaedic providers (51%) had adopted EHRs, with an increase from 8% to 46% during the incentive phase (2011 to 2014) and an increase from 44% to 51% during the penalty phase (2015 to 2016). After analyzing factors associated with adoption, it was most notable that for every additional year since graduation, the odds of adopting EHR later increased by 4.14 (95% confidence interval 4.00 to 4.33; p < 0.001). After adoption, providers who adopted EHRs increased the mean number of Medicare outpatient visits per year from 439 to 470 (mean difference, increase of 31 procedures [95% CI 24 to 39]; p < 0.001), and providers who did not use EHRs decreased from 378 to 368 visits per year (median difference, decrease of 10 procedures [95% CI 8.0 to 12.0]; p < 0.001). EHR was not associated with billing for Level 4-5 visits, after adjusting for practice size and pre-adoption volumes (p = 0.32; R2 = 0.51). EHR adoption was not associated with surgical volume for 10 of 11 common orthopaedic procedures. However, two additional TKA procedures annually could be attributed to EHR adoption, when compared with non-adopters (p = 0.03; R2 = 0.65). After adoption, orthopaedic surgeons increased their annual TKA volume from 42 to 48 (mean difference, increase of 6 [95% CI 4.0 to 7.0]; p < 0.001), while non-adopting orthopaedic surgeons increased their annual surgical volume for TKA from 28 to 30 (median difference, increase of 2 [95% CI 2.0 to 4.0]; p < 0.001).
Conclusions
In orthopaedics, the Health Information Technology for Economic and Clinical Health (HITECH) Act resulted in approximately half of self-reported orthopaedic surgeons adopting EHR from 2011 to 2016. Considering the high cost of most EHRs and the substantial investment in adoption incentives, this adoption rate may not be sufficient to fully realize the objectives of the HITECH Act. Diffusion of technology is a vast field of study within social theory. Prominent sociologist Everett M. Rogers details its complexity in Diffusion of Innovations. Diffusion of technology is impacted by factors such as the possibility to sample the innovation without commitment, opinion leadership, and observability of results in a peer network, to name a few. Incorporating these principles, where appropriate, into a more focused action plan may facilitate technological diffusion for future innovations. Lastly, EHR adoption was not associated with higher-level billing or surgical volume. This might suggest that EHRs have not had a meaningful clinical benefit, but this needs to be further investigated by relating these trends to patient outcomes or other quality measures.
Level of Evidence
Level III, therapeutic study.
Introduction
Orthopaedic surgeons use a variety of technologies in their daily practices to care for patients (such as medical devices and intraoperative navigation), manage associated business processes (for example, enterprise or billing software), enhance provider productivity (including the use of smartphones), or promote patient engagement (such as patient portals). These technologies typically spread throughout orthopaedics via a bottom-up approach: individual orthopaedic surgeons try the technology and then adopt if it is useful. Other surgeons see the benefits and then adopt the technology based on the experience of early adopters. The advantage of this approach is that the experience of the early adopters can be used to refine and enhance the technology, accelerating further adoption across orthopaedics.
By contrast, the integration of electronic health record (EHR) technology into practice has been different. EHRs were introduced through a two-step, top-down approach described in the Health Information Technology for Economic and Clinical Health (HITECH) Act [40, 19]. The first step was to incentivize providers to adopt EHR, with more than USD 27 billion allocated to implementing the HITECH Act [19]. Providers were paid up to USD 44,000 if they could demonstrate that they were using EHR “meaningfully” [8], generally defined as using the technology to enhance care [28, 35, 40]. After 4 years of incentives, providers began to be penalized for not using EHRs at a meaningful level [12]. The rationale for this top-down approach was rapid spread of EHRs. The benefits of EHRs—improved quality, efficiency, and the health of populations—were, according to David Blumenthal, President of the Commonwealth Fund, “essential to improving the health and healthcare of Americans” [5], thus necessitating as rapid deployment as possible.
After implementation of the HITECH Act, the rates of EHR adoption increased across all health-service fields. Before incentive payments were initiated, approximately 20% of all office-based providers providing direct care to patients (excluding radiologists, pathologists, and anesthesiologists) used at least a basic EHR [17]. By 2013, approximately 80% of office-based providers reported using any EHR [17]. EHR adoption rates in hospitals also increased from less than 10% in 2009 to more than 80% by 2015 [21]. Studies on the impact of EHR adoption on provider productivity have produced mixed results. In studies of primary care physicians, it was found that EHRs can improve efficiency for certain providers, defined as the number of weekly patient visits [4]. However, EHR adoption has demonstrated negative effects on provider productivity and satisfaction [22, 24]. In one academic orthopaedic practice, surgeons reported having decreased efficiency resulting from performing additional, unnecessary tasks that were previously handled by other members of the health care team, as well as spending more time per patient encounter [22]. They also reported having diminished teaching time [22]. At the practice level, more providers were needed to manage the same number of patients, increasing costs for the institution [22]. A cumbersome interface and hours of additional work time to incorporate this technology have led to increased physician stress and burnout [18]. Furthermore, providers were encouraged to use the clinical decision support tools to attest to Meaningful Use objectives [11]. The association between these functions and surgical decision-making has not been explored. Orthopaedic surgeons reported that EHR implementation had the greatest negative impact compared with other specialties [18], raising the issue of whether EHR has had a clinical benefit worth the costs and disruption of HITECH. No study to date that we know of has simultaneously examined clinical adoption of EHR by orthopaedic surgeons and productivity post-adoption on a national scale.
Therefore, we asked (1) What was the rate of EHR adoption in orthopaedics and how are physician and practice characteristics associated with adoption? (2) Is EHR adoption associated with outpatient billing? (3) Is EHR adoption associated with surgical volume?
Materials and Methods
Study Design and Setting
This was a retrospective study of multiple publicly available secondary databases. We used data from 2011 to 2016.
Databases
To investigate the spread of EHR in orthopaedics, we relied on a public-use dataset that listed providers attesting to using EHR meaningfully and thus were eligible to receive Medicare incentives. These data are available at the Centers for Medicare & Medicaid (CMS) in the Meaningful Use Eligible Professional Public Use Files from 2011 to 2016 [9]. We chose the Meaningful Use database to identify those orthopaedic surgeons who adopted an EHR. There are two benefits to this dataset. The first benefit is reliability; since CMS monitors providers for fraud, false attestation is unlikely. It is also unlikely that providers would not attest after completing the required measures. The second benefit of the Meaningful Use dataset is that it allowed us to separate the providers who adopted EHR for patient care from those who only used EHRs primarily for billing. To examine physician characteristics, we relied on the 2016 Physician Compare dataset from the CMS to collect data on the year of medical school graduation, self-reported specialty, and number of group practice members [14]. Although this is not an exhaustive set of associated factors, these variables were readily available and we felt they adequately addressed certain pre-existing questions related to EHR usage (such as whether older providers lag behind with technology). To assess productivity, we included the 2012 and 2016 Medicare Provider Utilization and Payment Data Set [10]. Only physicians who billed 11 Medicare patients for at least one Current Procedural Terminology (CPT) code in a calendar year were included in this dataset. To our knowledge, the Meaningful Use dataset has not been extensively used in prior database studies. Linkage of the Medicare Utilization and Payment data and Physician Compare data by National Provider Identifier (NPI) has been used in prior studies [12].
Description of Experiment, Treatment, or Surgery
The sample of orthopaedic providers was created by including those who identified their primary specialty as “Orthopedic Surgery” in the Physician Compare dataset. All providers with non-physician credentials were excluded. A final sample of 21,484 orthopaedic surgeons was identified. To answer our first question regarding the adoption rate, we designated all providers who attested to having either Stage 1 or Stage 2 meaningful use as “adopters,” and this was repeated for each year from 2011 to 2016; Stage 1 and Stage 2 meaningful use are determined by the extent of completion of several core and menu objectives, such as patient education and electronic prescription usage [11]. The percent linkage between the Meaningful Use datasets and the Physician Compare dataset indicated the percentage of adopters for that year. Any provider in the dataset who did not adopt, and therefore was not in the meaningful use dataset, was designated as a “nonadopter.” Datasets were linked by national provider identifier. The number of providers attesting to meaningful use was reported as a percentage of the total number of providers in the sample (n = 21,484) from 2011 to 2016. A logistic regression was performed to investigate the association between provider and practice characteristics between adoption at time periods where adoption had notably increased. Specifically, we analyzed “early adoption” pertaining to 2011 to 2012, and “late adoption” pertaining to 2016.
For the second question evaluating outpatient productivity before and after EHR adoption, we extracted data from the Physician Compare, Eligible Provider Meaningful Use, and Medicare Utilization and Payment datasets. Providers who had a primary specialty of orthopaedic surgery and first adopted EHR in 2013, according to the Meaningful Use dataset, were designated as adopters. Outpatient volume in 2012 was considered the “before” measurement, and 2013 was chosen as the initiation point of EHR adoption as to provide adequate time for the provider to acclimate to the new technology before the “after” measurement in 2016. Providers who did not have linkable data in the Meaningful Use dataset were designated as non-adopters. The number of services billed for Levels 1 through 5 for both Established and New patients was assessed for both adopters and non-adopters in 2012 and 2016. These visits were grouped into “High Level” (all Level 4 and Level 5) and “Low Level” (all Levels 1, 2, and 3) for 2012 and 2016. The association between EHR adoption and the number of higher level visits billed in 2016 was assessed with a multiple regression, including adjustment for group practice size and pre-adoption volume for Low and High visits.
For the third question, we identified providers who had a primary specialty of orthopaedic surgery and first adopted EHR in 2013. Providers from this sample who had Medicare billing data for at least one of the following orthopaedic conditions, determined with CPT codes for both 2012 and 2016, were included: TKA, THA, arthroscopic subacromial decompression, open carpal tunnel release, intertrochanteric fracture fixation, lumbar spine decompression, meniscectomy (medial or lateral), meniscectomy (medial and lateral), rotator cuff repair, arthroplasty for hip fracture, and trigger finger. The number of services performed in 2016 was assessed as a function of EHR adoption and 2012 case volume with multiple regression for each CPT code.
Statistical Analysis, Study Size
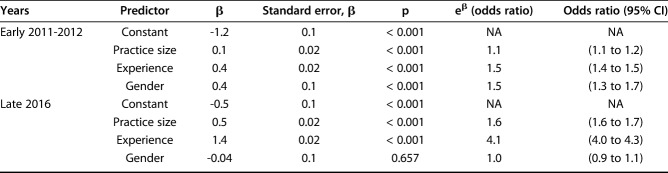
We performed a logistic regression analysis to investigate the factors associated with the increases in adoption in 2011 and in 2016 (Table 1). For both timepoints, we examined the variables of group practice size and years since medical school graduation using the Physician Compare dataset. We chose a logistic regression to model the data since the dependent variable, EHR adoption, is binary. Data were considered parametric if skewness was less than 2 and kurtosis was less than 12. For parametric and nonparametric data, we reported means and medians, and we used paired t-tests and Wilcoxon Rank Sum tests, respectively. Multiple regressions were performed to model outpatient and surgical volume as a function of EHR adoption. Effect size is reported as a logistic regression odds ratio or linear coefficients. All data management and analyses were conducted using RStudio Version 1.1.447 (RStudio, Boston, MA, USA).
Table 1.
Logistic regression analysis of physician and practice characteristics influencing early and late EMR adoption
Results
Rate of and Factors Associated with EHR Adoption
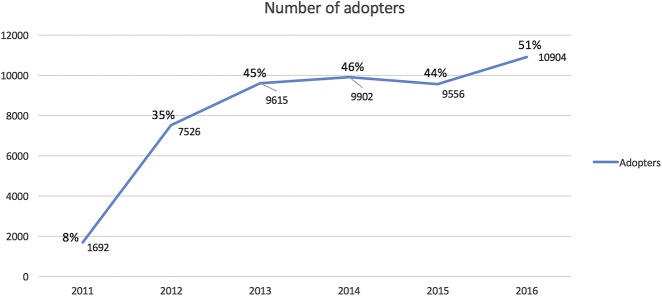
The initiation of the HITECH incentives in 2011 resulted in a large increase in EHR adoption (Fig. 1). A total of 7526 of 21,484 orthopaedic providers (35%) adopted EHR in the first 2 years of the incentives. Subsequently, growth slowed with an additional 10% gain in 2013; growth was flat from 2013 to 2015. The number of adopters was slightly reduced in 2015, which was the first year of penalties. By 2016, 10,904 of 21,484 self-reported orthopaedic surgeons (51%) had adopted the EHR. For adoption in the early phase of HITECH (2011-2012), every additional year since medical school graduation increased odds of adoption by 1.47 (95% CI 1.42 to 1.52; p < 0.001) and every additional group practice member increased odds of adoption by 1.11 (95% CI 1.08 to 1.15; p < 0.001). In the later phases of HITECH (2016), for every additional year since medical school graduation, the odds of late adoption increased by 4.14 (95% CI 4.00 to 4.33; p < 0.001), and for every additional group practice member, the odds of late adoption increased by 1.64 (95% CI 1.58 to 1.70; p < 0.001).
Fig. 1.
This figure demonstrates the EMR adoption rate from 2011 to 2016 in a sample of self-reported orthopaedic surgeons (n = 21,484)
Association Between EHR Adoption and Outpatient Volume
Adopters increased annual billing for outpatient visits after EHR adoption for New Patient Level 3 from 93 to 101 (mean difference, increase of 8 [95% CI 6.0 to 11.0]; p < 0.001), Established Patient Level 3 by 22 visits from 195 to 217 (median difference, increase of 22 [95% CI 16.0 to 27.0]; p < 0.001), and Established Patient Level 4 from 78 to 107 (median difference, increase of 29 [95% CI 24.0 to 34.0]; p < 0.001). For all visit levels combined, providers who adopted EHRs increased the mean number of Medicare outpatient visits per year from 439 to 470 (mean difference, increase of 31 procedures [95% CI 24 to 39]; p < 0.001). In the same time frame, non-adopters increased annual billing for New Patient Level 3 by two visits from 92 to 94 (mean difference, increase of 2 [95% CI 1.0 to 4.0]; p = 0.01), Established Patient Level 3 from 180 to 187 (median difference, increase of 7 [95% CI 4.0 to 10.0]; p < 0.001), and Established Patient Level 4 from 78 to 91 (median difference, increase of 13 [95% CI 11.0 to 16.0]; p < 0.001). However, overall, non-adopting provider billing for outpatient visits decreased from 378 to 368 (median difference, decrease of 10 [95% CI 8.0 to 12.0]; p < 0.001). After adjusting for group practice size and pre-adoption clinic volume, EHR adoption was not found to be associated with billing for Level 4-5 visits (R2 = 0.51; p = 0.32).
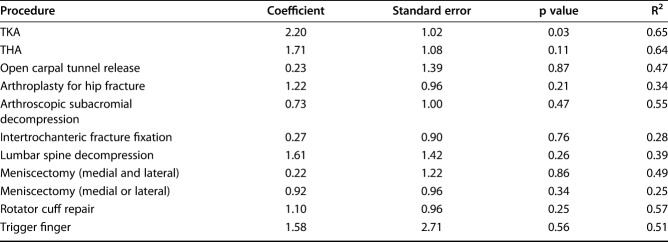
Association Between EHR Adoption and Surgical Volume
After EHR adoption, orthopaedic surgeons increased their volume of TKA from 42 to 48 (mean difference, increase of 6 [95% CI 4.0 to 7.0]; p < 0.001), increased their THA volume from 32 to 39 (mean difference, increase of 7 [95% CI 6.0 to 9.0]; p < 0.001), increased the volume of rotator cuff repair from 20 to 23 (mean difference, increase of 3 [95% CI, 2.0 to 5.0]; p < 0.001), lumbar spine decompression from 29 to 33 (mean difference, increase of 4 [95% CI 2.0 to 6.0]; p < 0.001), and trigger finger from 31 to 35 (mean difference, increase of 4 [95% CI 1.0 to 8.0]; p = 0.03). In the same time frame, non-adopters increased annual surgical volume for TKA from 28 to 30 (median difference, increase of 2 [95% CI 2.0 to 4.0]; p < 0.001), THA from 23 to 27 (median difference, increase of 4 [95% CI 4.0 to 5.0]; p < 0.001), rotator cuff repair from 19 to 20 (median difference, increase of 1 [95% CI, 1.0 to 3.0]; p = 0.001), lumbar spine decompression from 29 to 32 (mean difference, increase of 3 [95% CI 1.0 to 4.0), and trigger finger from 33 to 38 (mean difference, increase of 5 [95% CI 2.0 to 7.0]; p < 0.001). After adjusting for group practice size and pre-adoption surgical volume, we found no association between EHR adoption and surgical volume for 10 of 11 common orthopaedic procedures (Table 2). However, after adjusting for group practice size, two additional TKA procedures annually can be attributed to EHR adoption when compared with non-adopters (R2 = 0.65; p = 0.03).
Table 2.
Multiple regressions for effect of EMR adoption on surgical case volume
Discussion
Electronic health records have become a ubiquitous tool for patient care. While orthopaedic surgeons use a variety of technologies, EHR is unusual in that its diffusion was actively driven by government incentives. Studying technology diffusion can provide valuable insight into the usability, limitations, or reception of a product. No studies to our knowledge detail the spread of EHR while accounting for specific feature usage in the delivery of orthopaedic care. Furthermore, associations between EHR use and orthopaedic productivity have been suggested in studies of single institutions but have not been analyzed on a larger scale [37, 39]. This issue is important because of the financial burden for the institution and the time burden for the clinician that accompany EHR implementation. The EHR has also been cited as a major driving factor in provider burnout, which has additional implications for productivity and efficiency [30, 31, 34]. In this investigation, we found no evidence of upcoding practices or differences in surgical decision making between adopters and nonadopters. Finally, for the financial investment in incentive payments, only about half of orthopaedic surgeons had adopted EHR to the Meaningful Use standard by 2016.
Limitations
This study relies on secondary database data and thus has the usual limitations of a secondary data analysis. First, providers who adopted EHR but did not attest to Meaningful Use have been counted as non-adopters in this analysis. We did not see this as an impediment to the analysis, since standardization of usage was a crucial component to the study. The reader should be mindful that this analysis accounts for both EHR adoption and the use of specific features. Second, our study relied on identification of orthopaedic surgeons in the Physician Compare dataset. We identified 21,484 providers from this dataset, although an estimate of total orthopaedic providers around this time was 35,742 [38]. Some providers may not have been included due to variations in their self-reported specialty (primary versus secondary specialty) or failure to be considered a Medicare Eligible Provider, thus not being present on the Physician Compare dataset. We did not see this as a disqualifying issue for our analysis, because most providers were included, and the providers who are present on the Physician Compare dataset as an eligible provider would be more likely to be present on other Medicare databases, increasing the likelihood of finding linkable data. Third, this study cannot account for procedures or outpatient visits covered by private insurers, since Medicare databases were used. However, we feel that our study still captures billing behavior adequately despite not including the factor of private insurance, as evidenced by the fit of our linear regressions.
Rate of and Factors Associated with EHR Adoption
The HITECH Act allocated funds to incentivize providers to adopt EHR and use it according to meaningful use guidelines. The “carrot and stick” strategy used here increased the percentage of adoption from 8% to 51% of the orthopaedic provider sample, with the incentive “carrot” phase demonstrating a greater rise in adoption rates than the “stick” phase. Even the carrot phase lost momentum as prospective payment decreased, as evidenced by the flattened curve from 2013 to 2015. Although the meaningful use penalties began in 2015, Medicare was liberal with hardship waivers during that year, which may explain the slight dip observed in 2015 [25]. The most striking aspect of this progression is that for the billions of dollars invested by the government for incentive payments, only half of self-reported orthopaedic surgeons adopted EHR that qualified as “meaningful use” [19]. The associations between practice size and provider experience, as evidenced by odds ratios, were greater for late adoption. Older providers and larger institutions notably had more meaningful use attestations in the second year of penalty payments. The sharp increase in adopter group practice size in 2016 may be the result of consolidation, suggesting that HITECH troubled small-practice management and resulted in small-practice aggregation [36]. Larger practices may have been able to diffuse the impact of Medicare penalties for late adoption [7]. The peak of older providers adopting technology later supports conventional belief that older physicians may lag behind in adapting to technological advancement [15] and may support the arguments that EHRs are in general difficult to use and can interfere with care [6, 23]. Older providers may be affected more because they experience greater disruption in the work flow they have spent more time developing, or because they may lack the appropriate computer skills to adopt efficiently [2]. Considering the large proportion of older orthopaedic surgeons, including those who transition to part-time practice later in their careers [13], adoption may improve if functional or intuitive EHR design is prioritized.
Association Between EHR Adoption and Provider Outpatient Billing
This relationship was important to investigate since reports of upcoding have been released [16]. The exact role of EHR in this practice is unclear; some claim that the thorough documentation with EHR would promote accurate billing, while others point to the ease of functions such as copy-paste that may lead to inaccurate recordkeeping [26, 29]. We were therefore interested in evaluating the association between higher-level billing and EHR adoption. Our findings do not support EHR as an associated factor for upcoding practices. Additionally, adopters demonstrated an increase in billing of total outpatient procedures post-adoption. This is in contrast to a study by Hollenbeck et al. [22], which found no difference in orthopaedic patient volume after EHR implementation in a single institution, although more providers were needed to see the same number of patients. Although our study found an overall increase in productivity, it should be noted that adopters are treated as a uniform group in this study. One study by Bae et al. [4] found that productivity differed between older and younger providers after EHR adoption due to differences in workflow. Workflow is perhaps the most important determinant of how EHR will affect productivity and, when customized by each provider for his or her individual preference, can help overcome initial setbacks during acclimation [27]. Therefore, it may be helpful to allocate specific resources for education to encourage clinicians to explore different options for usage and effectively incorporate it into practice. It is important to note that there are reports of decreased efficiency with the EHR [18, 22], but because this study could not measure the time spent by clinicians during patient encounters or with the EHR, we cannot comment on efficiency. Rather, our study does not support long-term effects of EHR on provider productivity defined by patient volume.
Association Between EHR Adoption and Surgical Volume
With this question, we intended to evaluate any potential consequences of the EHR technology on surgical decision-making using surgical volume as a proxy. We evaluated surgical volume as an endpoint of the impact of outpatient EHR because of the intended function of the EHR technology. It was ideally meant to be a thorough documentation system and clinical support tool. Therefore, its impact as a patient care tool is a crucial question. Implementation of outpatient EHR could have affected surgical volume for a few reasons. First, the clinical decision support available in the EHR could alter the surgeon’s perception of perceived risks and benefits of certain operative or nonoperative treatments for each patient. Second, altered workflow after EHR implementation has been reported to affect the physician-patient relationship. Physician decision making may be influenced by reduced time with the patient, or by fatigue, burnout, or stress with the burden of the new workflow. Furthermore, impaired patient interactions could affect interest in undergoing surgery with a specific provider. The role of EHR in medical decision making is still being investigated, and although there are several factors that drive the decision to perform surgery, this analysis was merely a screening test for potential differences in surgical management between adopters and non-adopters. In our findings, out of 11 common orthopaedic procedures, only TKA showed an association between adoption and more annual procedures per provider (Table 2). This could be the result of increased pressure to operate to offset implementation and maintenance costs. It may also be related to the increase in overall Medicare outpatient visits, which may lead to increased referral for surgery. The possibility of a Type I statistical error (a false rejection of the null hypothesis, that is, falsely concluding that there was a difference for TKA when in fact there may not have been one) should also be considered, since this was the only procedure where a difference was identified; because of the lack of differences with other procedures, we suggest that EHR has not yet shown clinical benefit. We believe this should be studied in the context of patient outcomes. In surgical fields, EMR theoretically might improve quality of care by reducing medication errors, improving communication among a team of providers, and facilitating access to pertinent patient information [3]. However, a few studies have failed to demonstrate an improvement in primary care patient outcomes, such as blood pressure or A1c with the EHR [1, 20, 33], but this has not been extensively studied in surgical subspecialties.
Conclusions
EHR technology continues to diffuse throughout orthopaedic practices. The HITECH Act attempted to accelerate the process through a two-step approach—the “carrot and stick” incentive-payment model, which recruited about half of orthopaedic surgeons within several years. While our study cannot comment on the efficacy of the HITECH Act, we implore policymakers to consider alternative options for future developments other than the blanket approach used here, since the EHR will certainly not be the last technological advancement. Prominent sociologist Everett M. Rogers details the complexity of adoption in Diffusion of Innovations [32]. Diffusion of technology is influenced by numerous factors such as having the option to sample technology without commitment, opinion leadership, and observability of results in a peer network, to name a few [32]. From the few ideas listed, we can observe that EHR lacked trialability and had minimal observability of results in a social network, as all providers were encouraged to adopt simultaneously. Incorporating these principles and others described in diffusion theory, where appropriate and applicable, into a more focused action plan may facilitate technological diffusion for future innovations. For example, applying a niche approach may work in healthcare, where the demands and priorities of different healthcare providers can vary considerably. Since interoperability was one of the major objectives of the HITECH Act, a 51% adoption rate may not have been effective enough to realize that goal. Additionally, our study did not detect upcoding practices or changes in surgical decision making related to EHR adoption on a large scale. However, these trends may still be of interest to analyze at the institution-level to optimize clinical efficiency and decision support, as relevant to the needs of that institution. The lack of differences between adopters and non-adopters may imply lack of clinical benefit of the EHR, but this must be studied in the context of patient outcomes. Future studies should perhaps focus on quantifying the value of adoption and relating this to patient outcomes, which could be answered by cost-benefit analyses or financial models for different types of practices.
Acknowledgments
We thank Daniel Korschun PhD, associate professor of marketing at the Lebow College of Business, Drexel University, for his input on statistical methodology.
Footnotes
One of the authors certifies that she (AFC), or a member of her immediate family, has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Slack Inc (Thorofare, NJ, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from ACI (Bala Cynwyd, PA, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Stryker (Mahwah, NJ, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from bOne (Knolls, NJ, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Joint Purification Systems (San Diego, CA, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from American Medical Foundation (Philadelphia, PA, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Hyalex (Boston, MA, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from DJO (Dallas, TX, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Sonoran Biosciences (Scottsdale, AZ, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Graftworx (Menlo Park, CA, USA); has received or may receive payments or benefits, during the study period, in an amount of USD 10,000 to USD 100,000 from OREF (Rosemont, IL, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Pfizer (New York, NY, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000) from Avanos (Alpharetta, GA, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Irrisept (Lawrenceville, GA, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Convatec (Deeside, United Kingdom); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from 3M (Maplewood, MN, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Recro (Malvern, PA, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Zimmer (Warsaw, IN, USA); has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000) from Heraeus (Hanau, Germany), all outside the submitted work.
Each remaining author certifies that neither he nor she, nor any member of his or her immediate family, has any commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Drexel University College of Medicine, Philadelphia, PA, USA.
References
- 1.Afonso AM, Alfonso S, Morgan TO. Short-term impact of meaningful use stage 1 implementation: a comparison of health outcomes in 2 primary care clinics. J Ambul Care Manage. 2017;40:316-326. [DOI] [PubMed] [Google Scholar]
- 2.Ajami S., Bagheri-Tadi T. Barriers for Adopting Electronic Health Records (EHRs) by Physicians. Acta Inform Med. 2013;21:129-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alexander I. Electronic medical records for the orthopaedic practice. Clin Orthop Relat Res. 2007;457:114-119. [DOI] [PubMed] [Google Scholar]
- 4.Bae J., Encinosa W.E. National estimates of the impact of electronic health records on the workload of primary care physicians. BMC Health Services Research. 2016;16:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blumenthal D. Stimulating the adoption of health information technology. N Engl J Med. 2009;360:1477-1479. [DOI] [PubMed] [Google Scholar]
- 6.Bowman S. Impact of electronic health record systems on information integrity: quality and safety implications. Perspect Health Inf Manag. 2013;10:1c. [PMC free article] [PubMed] [Google Scholar]
- 7.Burt CW, Sisk JE. Which physicians and practices are using electronic medical records? Health Aff (Millwood). 2005;24:1334-1343. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Medicare and Medicaid Services. An introduction to the Medicare EHR incentive program for eligible professionals. https://www.cms.gov/regulations-and-guidance/legislation/ehrincentiveprograms/downloads/beginners_guide.pdf. Accessed March 27, 2019.
- 9.Centers for Medicare and Medicaid Services. Meaningful use data: public use files. Available at: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/PUF.html. Accessed March 27, 2019.
- 10.Centers for Medicare and Medicaid Services. Medicare provider utilization and payment data: physician and other supplier. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Physician-and-Other-Supplier.html. Accessed March 27, 2019.
- 11.Centers for Medicare and Medicaid Services. Stage 1 vs. Stage 2 comparison table for eligible professionals. Available at: https://www.cms.gov/regulations-and-guidance/legislation/EHRIncentivePrograms/Downloads/Stage1vsStage2CompTAblesforEP.pdf. Accessed March 27, 2019.
- 12.Chapman T, Zmistowski B, Purtill JJ, Chen AF. Profiles of practicing female orthopaedists caring for Medicare patients in the United States. J Bone Joint Surg Am. 2018;100:e69. [DOI] [PubMed] [Google Scholar]
- 13.Cherf J, Buckley A. AAOS Now. Census examines orthopaedic workforce trends. Available at: https://www.aaos.org/AAOSNow/2017/Aug/Managing/managing02/?ssopc=1. Accessed May 2, 2019.
- 14.Data.Medicare.gov. Physician compare national downloadable file. Available at: https://data.medicare.gov/data/physician-compare. Accessed March 27, 2019.
- 15.Decker SL, Jamoom EW, Sisk JE. Physicians in nonprimary care and small practices and those age 55 and older lag in adopting electronic health record systems. Health Aff (Millwood). 2012;31:1108-1114. [DOI] [PubMed] [Google Scholar]
- 16.Department of Health and Human Services, Office of Inspector General. Coding trends of Medicare evaluation and management services. Available at: https://oig.hhs.gov/oei/reports/oei-04-10-00180.pdf. Accessed March 27, 2019
- 17.Furukawa MF, King J, Patel V, Hsiao C, Adler-Milstein J, Jha AK. Despite substantial progress in EHR adoption, health information exchange and patient engagement remain low in office settings. Health Aff (Millwood) . 2014;33:1672-1679. [DOI] [PubMed] [Google Scholar]
- 18.Gardner RL, Cooper E, Haskell J, Harris DA, Poplau S, Kroth PJ, Linzer M. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc. 2019;26:106-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gold M, McLaughlin C. Assessing HITECH implementation and lessons: 5 years later. Milbank Q. 2016;94:654-687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greiver M. Rebuttal: do electronic medical records improve quality of care? No. Can Fam Physician. 2015;61:e436, e438. [PMC free article] [PubMed] [Google Scholar]
- 21.Henry J, Pylypchuk Y, Searcy T, Patel V. Adoption of electronic health record systems among U.S. non-federal acute care hospitals: 2008-2015. Health IT Dashboard: HealthIt.Gov; 2016. Available at: https://dashboard.healthit.gov/evaluations/data-briefs/non-federal-acute-care-hospital-ehr-adoption-2008-2015.php. Accessed: March 27, 2019 [Google Scholar]
- 22.Hollenbeck SM, Bomar JD, Wenger DR, Yaszay B. Electronic medical record adoption: the effect on efficiency, completeness, and accuracy in an academic orthopaedic practice. J Pediatr Orthop . 2017;37:424-428. [DOI] [PubMed] [Google Scholar]
- 23.Howe JL, Adams KT, Hettinger AZ, Ratwani RM. Electronic health record usability issues and potential contribution to patient harm. JAMA. 2018;319:1276-1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Howley MJ, Chou EY, Hansen N, Dalrymple PW. The long-term financial impact of electronic health record implementation. J Am Med Inform Assoc . 2015;22:443-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hurt A. Understanding meaningful use penalties in 2015. Physicians practice: Modern Medicine Network; 2014. Available at: https://www.physicianspractice.com/ehr/understanding-meaningful-use-penalties-2015. Accessed March 27, 2019.
- 26.Loria K.Medical Economics. Why is there a problem with upcoding and overbilling? Available at: https://www.medicaleconomics.com/health-law-and-policy/why-there-problem-upcoding-and-overbilling. Accessed March 27, 2019.
- 27.McBride M.Medical Economics. How to create EHR workflows that increase productivity. Available at: https://www.medicaleconomics.com/article/how-create-ehr-workflows-increase-productivity. Accessed May 5, 2019. [PubMed]
- 28.Menachemi N, Collum T. Benefits and drawbacks of electronic health record systems; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murphy K.EHR Intelligence. Fraudulent EHR use leads to multi-million dollar settlement. Available at: https://ehrintelligence.com/news/fraudulent-ehr-use-leads-to-multi-million-dollar-settlement. Accessed March 27, 2019.
- 30.Catalyst NEJM. Physicians are facing a crisis. Available at: https://catalyst.nejm.org/videos/physicians-facing-crisis-emr-burnout/. Accessed March 27, 2019.
- 31.Patel RS, Bachu R, Adikey A, Malik M, Shah M. Factors related to physician burnout and its consequences: A Review. Behav Sci. 2018;8:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rogers EM. (1962) Diffusion of Innovations. New York, NY: The Free Press [Google Scholar]
- 33.Selvaraj S, Fonarow GC, Sheng S, Matsouaka RA, DeVore AD, Heidenreich PA, Hernandez AF, Yancy CW, Bhatt DL. Association of electronic health record use with quality of care and outcomes in heart failure: an analysis of get with the guidelines-heart failure. J Am Heart Assoc. 2018;7: pii: e008158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shanafelt TD, Dyrbye LN, Sinsky C, Hasan O, Satele D, Sloan J, West CP. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91:836-48 [DOI] [PubMed] [Google Scholar]
- 35.Shekelle PG, Morton SC, Keeler EB. Costs and benefits of health information technology. Evid Rep Technol Assess (Full Rep) . 2006:1-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sines CC, Griffin GR. Potential effects of the electronic health record on the small physician practice: a Delphi study. Perspect Health Inf Manag . 2017;14 1f. [PMC free article] [PubMed] [Google Scholar]
- 37.Scott DJ, Labro E, Penrose CT, Bolognesi MP, Wellman SS, Mather RC. The Impact of Electronic Medical Record Implementation on Labor Cost and Productivity at an Outpatient Orthopaedic Clinic. J Bone Joint Surg Am. 2018; 100: p1549-1556. [DOI] [PubMed] [Google Scholar]
- 38.SK&A. Market profile of U.S. orthopedic surgeons. Available at: http://www.coa.org/docs/SKA.pdf. Accessed March 27, 2019.
- 39.Webb ML, Bohl DD, Fischer JM, Samuel AM, Lukasiewicz AM, Basques BA, Grauer JN. Electronic Health Record Implementation is Associated with a Negligible Change in Outpatient Volume and Billing. Am J Orthop (Belle Mead NJ). 2017;46: E172-176. [PubMed] [Google Scholar]
- 40.111-5 PL. Health Information Technology. TITLE XIII; 2009. https://www.hhs.gov/sites/default/files/ocr/privacy/hipaa/understanding/coveredentities/hitechact.pdf. Accessed March 27, 2019. [Google Scholar]