Abstract
Background
Few studies have focused on behavioral changes that occur prior to entering treatment for an alcohol use disorder (AUD). In two studies (Stasiewicz et al., 2013, Epstein et al., 2005), pretreatment reductions in alcohol use were associated with better treatment outcomes. Identifying patterns of pretreatment change has the potential to inform clinical decision making.
Methods
This study sought to identify pretreatment change trajectories in individuals seeking outpatient treatment for AUD (N = 205) using finite mixture modeling based on changes in number of days abstinent per week (NDA).
Results
The analysis identified three pretreatment trajectory classes. Class 1 (High Abstinence—Minimal Increase; HA-MI) (n = 64; 31.2%) reported a high level of pretreatment NDA with minimal change during an eight-week pretreatment interval. Class 2 (Low Abstinence—Steady Increase; LA-SI) (n = 73; 35.6%) reported a low level of pretreatment NDA followed by a steady increase beginning two weeks prior to the phone screen. Class 3 (Non-abstinent—Accelerated Increase (NA-AI) (n = 68; 33.2%) reported no or very low levels of pretreatment NDA but demonstrated an increase following the phone screen. With regard to within-treatment change, Class 1 demonstrated the least and Class 3 demonstrated the most change in NDA. From baseline to 6-month follow-up, Class 3 added 2.31 abstinent days per week, Class 2 added .69 days, and Class 1 added .63 days. The increase in NDA for Class 3 was significantly different from the other two classes; however, Class 3 reported fewer overall days abstinent at 6-month follow-up.
Conclusions
Study results have clinical and research implications including recommended changes to treatment protocols and research designs. Understanding the impact of pretreatment trajectories of alcohol use on within-treatment and post-treatment outcomes may provide important information about adapting treatment to increase efficiency and effectiveness.
Keywords: Pretreatment change, Alcohol use disorder, Alcohol, Treatment, Behavior change
INTRODUCTION
Improvements in addictive behavior frequently take place without professional treatment (Sobell et al., 1991). In the case of alcohol problems, unaided change is more common than professionally-aided change (Sobell et al., 1996). Even among those entering treatment, there is much in their accounts to suggest that a large component of the change process is self-directed (Orford et al., 2006b). Together, these findings challenge the assumption that the majority of change only occurs after treatment entry and suggests that behavior change must be examined through a broader lens (Willenbring, 2007).
Psychosocial treatments that are the focus of randomized clinical trials are embedded within a much larger system of change-promoting processes. This “larger system” includes processes that occur before, during, and after a course of formal treatment. In both psychotherapy and substance abuse research, there is a wealth of data on behavioral change that occurs during and following treatment. In contrast, few studies have focused on change that occurs prior to entering treatment. In the general psychotherapy literature, studies of pretreatment change have shown that symptom change consistently occurs after the initial phone call when an appointment is scheduled, before the first treatment session (Kindsvatter et al., 2010, Lawson, 1994, Ness and Murphy, 2001, West et al., 2011, Weiner-Davis, 1987). In the substance abuse literature, a similar pattern has been observed in studies that report reductions in or cessation of use that occurs between the initial phone call and the first clinical-research assessment (Epstein et al., 2005, Kaminer et al., 2008, Morgenstern et al., 2007, Ondersma et al., 2012, Penberthy et al., 2007, Sobell, 2011, Stasiewicz et al., 2013).
Several of these studies found changes in alcohol use after the initial phone call (when screening information is obtained), but before the baseline assessment (Epstein et al., 2005, Sobell, 2011, Stasiewicz et al., 2013). In two studies, greater pretreatment reductions in the quantity and frequency of alcohol use predicted better 3-month (Stasiewicz et al., 2013) and 12-month drinking outcomes (Epstein et al., 2005). Thus, it appears that significant change in drinking may occur after the decision to seek treatment but before the first treatment session, and that these changes often are maintained during and following a course of treatment. Assessment reactivity (Clifford and Davis, 2012) has been offered as a possible explanation for pretreatment change in drinking. However, reactivity cannot explain all such changes, as several studies show significant change occurring before the baseline assessment, when assessment reactivity is most likely to occur. Moreover, two studies showed change occurring between 2 and 4 weeks before the participant-initiated phone call, thus further calling into question assessment reactivity as the sole explanation for pretreatment change (Sobell, 2011, Stasiewicz et al., 2013).
Sobell (2011) has suggested that simply being exposed to an advertisement for treatment may trigger a decision that leads to successful behavior change. In a similar vein, Orford and colleagues (Orford et al., 2006b, Orford et al., 2006a), using data from qualitative interviews with participants in a large clinical trial conducted in the United Kingdom (i.e., UK Alcohol Treatment Trial), identified several cognitive or contextual events that occurred prior to or concurrent with the decision to seek treatment that seemed to promote pretreatment change. These included thinking differently about the problem (e.g., weighing pros and cons), receiving encouragement for change from family and friends, experiencing a catalyst or event that triggered change (e.g., negative alcohol-related incident), making the initial phone call, and finally, participating in the baseline assessment. All of these processes can promote pretreatment changes in alcohol use and several are suggestive of a more natural or self-guided change process.
Although the accumulation of knowledge about self-change processes has been largely empirical, several theoretical models of behavior self-change have been posited (Sobell, 2007). Despite their differences, these models of change or decisional processes (e.g., (Janis, 1977, Prochaska and DiClemente, 1984, Deci and Ryan, 1985, Baumeister, 1996) converge on the identification of a cognitively-based, cost-benefit evaluation process. That is, over time, individuals weigh the pros and cons of their alcohol use and when they perceive that negatives outweigh the positives, they are more likely to decide to stop or reduce their drinking.
Although no one model or theory has emerged as dominant in identifying the causes of pretreatment change in drinking, models of behavior change provide a useful starting point. For example, constructs relevant to the initiation and maintenance of behavior change should be assessed (e.g., commitment and self-efficacy). Given how little is currently known about pretreatment change, and its potential influence on mechanisms of change and treatment outcomes (Stasiewicz et al., 2013, Hallgren et al., In press, Noyes et al., 2018), casting a wider net at this early stage of research may help to promote a better understanding of how people initiate such changes.
The present study is an investigation of pretreatment change in a treatment-seeking sample of men and women with AUD. The study has three objectives: (1) identify pretreatment change trajectories; (2) examine differences between pretreatment trajectory classes on demographic variables, alcohol problem severity, and measures of health behavior change constructs; and (3) examine the relationship between pretreatment trajectory classes and treatment outcome. The information obtained in pursuit of these objectives has the potential to inform clinical decision-making and improve alcohol treatment outcomes by adapting treatment based on an individual’s pretreatment change status.
MATERIALS AND METHODS
Participants
Participants (N = 220) were recruited via radio and television advertisements for an outpatient alcohol treatment study (see Appendix). Study participants were (a) men and women between the ages of 18 to 65 years who (b) met DSM-5 criteria for AUD, (c) consumed alcohol in the past 3 months, (d) lived within commuting distance of the treatment site, and (e) provided written informed consent. Exclusion criteria included (a) diagnosis of a severe mental illness (i.e., schizophrenia, bipolar disorder), (b) current drug use diagnosis other than tobacco or marijuana, (c) attended substance abuse treatment during the past 6 months, and (d) legally mandated to attend treatment.
The Institutional Review Board at the University at Buffalo approved the study. Of the 359 men and women screened, 65 (18.1%) were ineligible and 66 (18.4%) were no longer interested or lost to contact prior to study enrollment. Of the remaining 228 (63.5%) individuals who completed the in-person baseline assessment, eight were ineligible. The remaining 220 individuals enrolled in the study. Fifteen participants who completed the baseline assessment either declined to continue with the study or were lost to contact and thus their drinking data for the Baseline to Treatment Session 1 interval could not be collected. The analyses are based on the remaining 205 participants.
Procedures
All phone interviews, assessments, and treatment occurred at a publicly-funded outpatient substance abuse clinic. Participants calling in response to radio and television advertisements were screened for eligibility, which included questions regarding recent alcohol use, and treatment-related measures (e.g., commitment to change). At the conclusion of the telephone screen, those who were eligible to continue were scheduled for an in-person baseline assessment session approximately one week later (M = 9.2, SD = 4.3, Range = 3-29 days), which involved multiple self-report questionnaires and a semi-structured interview to determine diagnoses for alcohol and substance use disorders. The first treatment session was scheduled to occur approximately one week following the baseline assessment (M = 9.2, SD = 4.7, Range = 2-29 days). Approximately 90% (n =184) of participants had intervals ranging from 3 to 14 days for both weeks (i.e., phone screen to baseline and baseline to the first treatment session). Prior to meeting with the therapist for the first treatment session, a brief Timeline Follow-back (Sobell and Sobell, 1992) of daily alcohol use since the baseline assessment was completed. Treatment was adapted from an abstinence-oriented 12-session Cognitive-Behavioral Coping Skills Therapy (CBT)(Kadden et al., 1992) developed for use in Project MATCH (Allen et al., 1997). End of treatment (EOT) and 3- and 6-month post-treatment assessments were conducted. Assessments included questions about alcohol use, alcohol-related consequences, alcohol abstinence self-efficacy, and other indicators of post-treatment functioning (e.g., positive and negative affect).
Pretreatment Phase
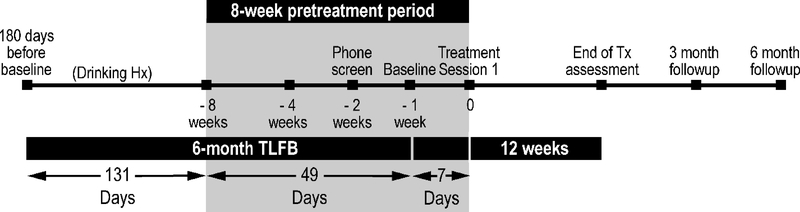
Research demonstrating pretreatment change in alcohol consumption shows that approximately 4-weeks prior to initiating treatment, a substantial proportion of individuals reduce or stop their alcohol consumption (Epstein et al., 2005, Stasiewicz et al., 2013). To increase confidence in the identification of pretreatment change, and rule out such change as part of an extended pattern of variability in pretreatment drinking, we extended the pretreatment phase from 4 to 8 weeks prior to the first treatment session. Figure 1 depicts the study timeline, which includes the pretreatment phase. In addition to the drinking history period (HX), the pretreatment phase includes a 6-week period prior to the phone screen (PS), a one-week period between the PS and the in-person baseline assessment (PS-BL), and a one-week period between the baseline assessment and the first treatment session (BL-TX1).
Figure 1.
Study timeline showing the 8-week pretreatment period.
Measures
Unless otherwise indicated, all measures were administered at the baseline assessment. Alcohol use disorder diagnoses were determined by administration of a brief standardized diagnostic interview and symptom checklist based on the Mini International Neuropsychiatric Interview (Sheehan et al., 1998). All measures have been used extensively in prior alcohol research and have good psychometric properties. Internal consistency for measures in the current sample ranged from good to excellent (αs = 0.78 – 0.96) with the exception of the SOCRATES Ambivalence and TSRQ Amotivation subscales which were acceptable (αs = 0.67 and 0.58, respectively).
Alcohol Use Disorders Identification Test-C (AUDIT-C) (Bush et al., 1998)
The AUDIT-C is a 3-item screening tool developed to identify persons who are hazardous drinkers or who have active alcohol use disorders. Each item has five response options. Responses are weighted such that between 0 and 4 points are possible per item. The AUDIT-C was administered during the phone screen as a check to ensure that individuals referred on to the baseline assessment were likely to meet DSM-5 criteria for an alcohol use disorder. This measure has good sensitivity and specificity for identifying men and women with an AUD.
Timeline Follow-Back (TLFB) (Sobell and Sobell, 1992)
The TLFB is a calendar-based retrospective recall interview of daily alcohol use. Participants completed the TFLB at several time points: baseline (i.e., past 180 days), first treatment session (i.e., days since baseline session), during treatment, end-of-treatment, and 3- and 6-months post-treatment. Research with the TLFB has demonstrated that drinking behavior can be reliably assessed over longer intervals (Carey, 1997, Maisto et al., 1982, Sobell et al., 1979).
Mini International Neuropsychiatric Interview. (Sheehan et al., 1998)
This diagnostic measure was adapted for this study and based on the DSM-5 diagnostic criteria. The current study began recruitment during the transition from the DSM-IV to the DSM-5 and the new version of the MINI was not published for two years. The substance use disorder modules were modified (i.e., the addition of the craving item) to reflect the revised DSM-5 diagnostic criteria.
Alcohol Dependence Scale (ADS) (Skinner and Allen, 1982)
The ADS is a 25-item measure of the severity of alcohol dependence. It assesses alcohol withdrawal symptoms, impaired control over drinking, awareness of a compulsion to drink, increased tolerance to alcohol, and salience of alcohol-seeking behavior. The individual items have varying response options, ranging from 2 to 4 choices with higher scores indicating greater dependence.
Short Inventory of Problems-Alcohol (SIP-A) (Miller et al., 1995)
The SIP-A is a 15-item measure of the adverse consequences of alcohol use. Participants indicate how often each of the listed consequences has occurred in the past 3 months (“never,” “once or a few times,” “once or twice a week,” “daily or almost daily”; scored 0-3).
Alcohol and Drug Consequences Questionnaire (ADCQ)(Cunningham et al., 1997)
The ADCQ is a 33-item scale assessing the costs and benefits of changing an alcohol problem. Participants were asked how important each of the items would be if they stopped or cut down their alcohol use. Items are rated on a 0 (not applicable) to 5 (extremely important) Likert scale and form two subscales: (1) costs of change and (2) benefits of change.
Stages of Change and Treatment Readiness Scale (SOCRATES)(Miller and Tonigan, 1996)
The SOCRATES is a 19-item measure designed to assess awareness of problem drinking and motivation to change drinking behavior. Items are rated on a 1 (strongly disagree) to 5 (strongly agree) Likert scale and form three subscales: (1) ambivalence, (2) recognition, and (3) taking steps to make a change.
Alcohol Abstinence Self-efficacy Scale (AASE)(DiClemente et al., 1994)
The AASE is a 20-item measure developed to assess the construct of self-efficacy as applied to alcohol abstinence. Participants rate their confidence to abstain in each situation on a 5-point Likert scale that ranges from 1 (not at all likely) to 5 (extremely likely). A brief 6-item version was administered at the PS (McKiernan et al., 2011), and the full 20-item measure was administered at the baseline assessment.
Commitment to Quitting Drinking Scale (CQDS)
This scale is an adaptation of the Commitment to Quitting Smoking Scale (CQSS) (Kahler et al., 2007), which is an 8-item measure conceptualized as the state of being personally obligated to persist in quitting smoking despite potential difficulties, craving and discomfort. The CQSS was modified to assess participants’ commitment to quit drinking. The measure was administered at the PS.
Positive and Negative Affect Scale (PANAS) (Watson et al., 1988)
The PANAS is a 20-item scale administered to assess levels of non-specific positive and negative mood. The PANAS was administered at the PS and the baseline assessment.
Treatment Self-regulation Questionnaire (TSRQ) (Deci and Ryan, 1985)
The TSRQ is a 15-item measure that assesses a person’s reasons for engaging in or changing a health behavior. In the current study, we assessed “reasons for participating in treatment for managing my alcohol use.” Responses are provided using a seven-point Likert scale ranging from 1 (not at all true) to 7 (very true). There are four subscales: (1) autonomous motivation, (2) introjection, (3) external regulation, and (4) amotivation.
Statistical Analyses
The Data Structure
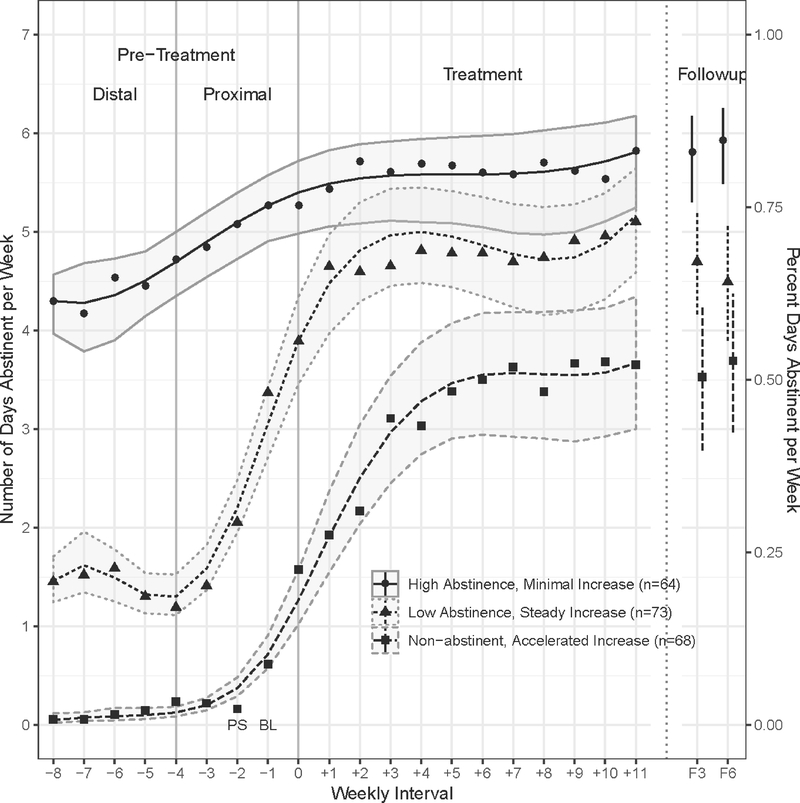
The data for each participant was a time series of 20 weekly intervals in which each interval, except the first, consisted of the number of days abstinent (NDA) for that week (see Fig 2). The first interval, in contrast, was the mean of a participant’s NDA for the previous 19 weeks (i.e., drinking history). The response variable NDA was thus an integer value ranging from 0 to 7. The 20-weekly interval series was segmented into three phases with the start of treatment being Week 0.1 The first phase was the Distal Pretreatment phase from Weeks −8 to −4. The second was the Proximal Pretreatment phase from Weeks −4 to 0. The third phase was the Treatment phase from Weeks 0 to 11. A fourth Follow-up phase was appended at Months 3 and 6, but was analyzed separately. The amount of missing data was small and monotone, with only 17 out of 205 subjects (8.3%) having any missing data and the amount ranging from 1 to 11 missing responses among these 17 subjects. The 6-month follow-up rate was 91.7%.
Figure 2.
Fitted and observed mean days abstinent per week for each pretreatment trajectory class.
Statistical Model
The overall statistical model was a finite mixture model (McLachlan and Peel, 2000) for which each basic model was a longitudinal binomial model with serial correlation. We postulated that the responses could exhibit different trajectories in the Distal-Pretreatment, Proximal-Pretreatment, and Treatment phases. To accommodate these possibly different trajectories the basic model was a logistic link for a cubic spline with predetermined knots at Week −4 and Week 0 (Hastie et al., 2001). The serial correlation was assumed to be first-order autoregressive [AR(1)]. To determine the number of classes, a second, truncated basic model was used in which only Weeks −8 to 0 were used with a single knot at −4 and for which responses were assumed independent.
Statistical Estimation
The estimation of the finite mixture of cubic spline models proceeded in three steps. The first step determined the adequacy of the longitudinal, cubic spline, binomial-logistic, AR(1) regression model. The cubic spline regression with knots at −4 and 0 weeks was fitted to the response variable for the entire 20 weeks of observations for all subjects without class structure by generalized estimating equations (GEE) (Diggle et al., 1994, Hardin and Hilbe, 2013) as implemented in the R (Team, 2018) package geepack (Halekoh et al., 2006). Predicted values were obtained from the estimated model along with pointwise 95% probability intervals via simulation. Model adequacy was determined by comparisons with mean responses at each data point, probability intervals, data visualization, and assessing the serial correlation structure.
In the second step, the number of components in the mixture model (McLachlan and Peel, 2000) was determined by the truncated basic model using the first 8 weeks of Pretreatment. There was no missing data in this subset. Using the R package flexmix (Leisch, 2004), the mixture was fitted for 1 to 10 possible classes. The choice of number of classes was based on information statistics (AIC, BIC) and their scree plots and interpretive heuristics, together with theoretical knowledge. The adequacy of the class separation was assessed by clustering diagnostics.
Once the number of classes was determined, the full basic model was again used for the full 20 observations within each class. Separate GEE analyses were used to estimate the parameters for each within-class model. Each model-based estimate was the expected value of the model that belonged to the class with the highest estimated probability (Fraley and Raftery, 2002) and pointwise 95% probability intervals by simulation. For the Follow-up phase, the means and 95% confidence intervals were estimated for the follow-up responses at 3 and 6 months.
Two additional, post-hoc analyses were conducted. The first analysis compared the trajectories of the responses during the Pretreatment phase between Weeks −4 and 0 among the three classes. Models consisting of logistic-binomial, AR(1), quadratic polynomials with class-by-polynomial interactions were fitted to these data. The second analysis compared the change in NDAs from the beginning to the end of treatment, as well as to the 3- and 6-months points among the three classes. Additional details regarding the statistical models and procedures may be found in the Supplement.
RESULTS
Pretreatment Trajectory Classes
The model diagnostics conducted in the first step showed that the longitudinal, cubic spline, logistic-binomial, and full basic model adequately fit the data. Linear and quadratic spline models did not adequately fit the observed means and the quartic model did not improve the fit over the cubic model. The observed means corresponded closely to the predicted values, falling within the 95% pointwise confidence intervals. The observed serial correlation was AR(1) with the estimated correlation r = .90,se = .011, so that the serial correlation decreased exponentially from .90 at lag 1 to .17 at lag 19. The patterns of observed autocorrelations matched the estimated autocorrelation.
The determination of the number of mixture components yielded 8 possible classes based on the minimum AIC and BIC information statistics. Scree plots showed a substantial decrease in the AIC and BIC from one to three classes followed by attenuated decreases for more than three. The 3-class mixture showed only slight overlap among the classes. Thus, the 3-class mixture was selected in an effort to balance model fit with interpretability.
For the final estimation, three cubic splines with knots at −4 and 0 weeks and serial correlation were fitted to the entire 20 weeks of observations, one for each of the 3 classes. Figure 2 presents for each class the observed mean days abstinent and fits, along with the corresponding 95% pointwise probability intervals.
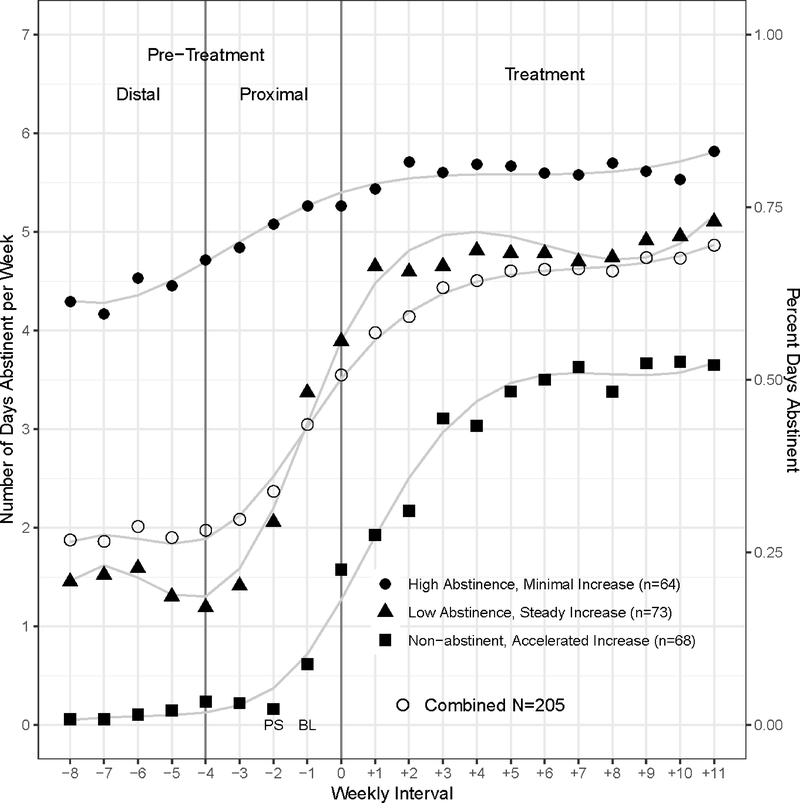
The first class, named High Abstinence—Minimal Increase (HA-MI), represents individuals (n = 64; 31.2%) who reported a high level of pretreatment NDA with a slight linear increase (p < .043) during the eight-week pretreatment interval. The second class, named Low Abstinence—Steady Increase (LA-SI), represents individuals (n = 73; 35.6%) who reported a low level of pretreatment NDA followed by a substantial linear increase (p < .0001) beginning two weeks prior to the PS and continuing up to the first treatment session. The third class, named Non-abstinent Accelerated Increase (NA-AI), represents individuals (n = 68; 33.2%) who reported no or very low levels of pretreatment NDA, but demonstrated an accelerated increase (p < .0054) following the PS and continuing up to the first treatment session. Figure 3 shows how the three derived trajectories compare to the trajectory for the combined sample.
Figure 3.
A comparison of the three trajectory classes with the trajectory for the combined sample.
Demographics
Table 1 presents the demographic characteristics of all study participants separately by pretreatment change trajectory class. There were no significant differences between trajectory classes for any of the demographic variables assessed.
Table 1.
Descriptive Statistics for Participants by Pretreatment Change Trajectory Class (N=205)
| Classes | ||||
|---|---|---|---|---|
| Class 1 HA-MI n=64 (31.22%) | Class 2 LA-SI n=73 (35.61%) | Class 3 NA-AI n=68 (33.17%) | P-value | |
| Age, mean (SD) | 52.20 (9.32) | 51.11 (9.58) | 52.50 (9.54) | 0.66a |
| Gender, n (%) | ||||
| Male | 41 (64.06) | 45 (61.64) | 39 (57.35) | 0.73b |
| Female | 23 (35.94) | 28 (38.36) | 29 (42.65) | |
| Race, n (%) | ||||
| White/Caucasian | 57 (89.06) | 64 (87.67) | 60 (88.24) | 0.78b |
| Black/African-American | 4 (6.25) | 6 (8.22) | 6 (8.82) | |
| American Indian/Alaskan Native | 0 | 2 (2.74) | 0 | |
| Native Hawaiian/Pacific Islander | 1 (1.56) | 0 | 0 | |
| Other | 2 (3.13) | 1 (1.37) | 2 (2.94) | |
| Hispanic/Latino, n (%) | ||||
| No | 62 (98.41) | 70 (95.89) | 63 (92.65) | 0.30b |
| Yes | 1 (1.59) | 3 (4.11) | 5 (7.35) | |
| Education, n (%) | ||||
| ≤High school | 16 (26.23) | 14 (20.90) | 13 (19.40) | 0.59b |
| Some college | 9 (14.75) | 16 (23.88) | 17 (25.37) | |
| College graduate | 36 (59.02) | 37 (55.22) | 37 (55.22) | |
| Income, n (%) | ||||
| <$10,000 | 3 (4.69) | 3 (4.23) | 2 (2.94) | 0.96b |
| >$10,000–40,000 | 17 (26.56) | 17 (23.94) | 17 (25.00) | |
| >$40,000–70,000 | 22 (34.38) | 21 (29.58) | 23 (33.82) | |
| >$70,000 | 22 (34.38) | 30 (42.25) | 26 (38.24) | |
Note: SD = Standard deviation; HA-MI = High Abstinence-Minimal Increase; LA-SI = Low Abstinence-Steady Increase; NA-AI = Non-Abstinence-Accelerated Increase.
P-value from Analysis of Variance (ANOVA) test
P-value from the Fisher’s Exact test
Drinking Characteristics
Table 2 presents the drinking characteristics of the sample, including quantity and frequency of alcohol consumption for the 131-day drinking history period (HX)2 and the extent of alcohol dependence, alcohol problems or AUD severity at baseline. Class 1 (HA-MI) reports the highest percent days abstinent (PDA) and differs significantly from each of the other 2 classes. Class 3 (NA-AI) reports the lowest PDA and differs significantly from each of the other 2 classes. An identical pattern exists for percent days heavy drinking (PDH), but Class 1 (HA-MI) reports the lowest percentage of PDH and Class 3 (NA-AI) reports the highest percentage of PDH. There were no differences between classes on measures of AUD severity or alcohol dependence severity assessed at the in-person baseline assessment. However, the classes differed on AUDIT-C scores assessed during the PS with Class 3 reporting a significantly higher score compared to Classes 1 and 2.
Table 2.
Drinking Historya and Alcohol Problem Severity Assessed at Baseline (N=205)
| Classes | ||||||
|---|---|---|---|---|---|---|
| Class 1 HA-MI n=64 (31.22%) | Class 2 LA-SI n=73 (35.61%) | Class 3 NA-AI n=68 (33.17%) | F-value | P-value | d.f. | |
| Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Drinks per drinking day | 7.15 (4.81) | 6.35 (3.73) | 7.62 (4.72) | 1.51 | 0.22b | 192 |
| % days abstinent/week | 60.63 (18.1)a | 20.59 (14.48)b | 1.91 (3.33)c | 142.26 | <0.0001b | 204 |
| % days of heavy/bingec drinking | 26.25 (22.51)a | 53.93 (32.37)b | 70.91 (36.01)c | 34.71 | <0.0001b | 204 |
| AUDIT-C | 8.30 (2.21)a | 8.85 (2.08) | 9.63 (1.73)b | 7.36 | 0.0008b | 204 |
| SIP-A | 35.36 (8.34) | 36.64 (8.38) | 34.93 (8.94) | 0.77 | 0.46b | 204 |
| Alcohol Dependence Scale | 38.88 (7.12) | 39.67 (6.30) | 39.06 (6.76) | 0.27 | 0.76b | 203 |
| DSM-5 Category | n, % | n, % | n, % | |||
| Mild (2–3) | 4 (6.25) | 1 (1.37) | 2 (2.94) | 0.65d | 4 | |
| Moderate (4–5) | 7 (10.94) | 10 (13.70) | 9 (13.24) | |||
| Severe (6–11) | 53 (82.81) | 62 (84.93) | 57 (83.82) | |||
Note: SD = Standard deviation; HA-MI = High Abstinence-Minimal Increase; LA-SI = Low Abstinence-Steady Increase; NA-AI = Non-Abstinence-Accelerated Increase.
131-day drinking history period
P-value from Analysis of Variance (ANOVA) test
4 or more drinks for women and 5 or more drinks for men, in one day
Table probability from the Fisher’s Exact test
Subscripts denote significant differences.
Individual Difference Characteristics
Table 3 presents data from baseline self-report measures of constructs hypothesized to be related to pretreatment change status. A common pattern emerges with Class 3 (NA-AI) and 2 (LA-SI), differing significantly from Class 1 (HA-MI), but not from each other. This pattern holds for the AASE, CQSS, and the Recognition and Taking Steps subscales of the SOCRATES. In addition, Class 3 (NA-AI) reports significantly higher scores on the Costs of Change subscale of the ADCQ compared to Classes 1 and 2. Finally, compared to Class 3, Class 1 (HA-MI) reports significantly higher scores on the External Regulation Scale of the TSRQ and the Ambivalence scale of the SOCRATES. For these same two variables, Class 2 reports significantly higher scores than Class 3 and significantly lower scores than Class 1.
Table 3.
Measures of Constructs Potentially Related to Change Status (N=205)
| Classes | ||||||
|---|---|---|---|---|---|---|
| Class 1 HA-MI n=64 (31.22%) | Class 2 LA-SI n=73 (35.61%) | Class 3 NA-AI n=68 (33.17%) | F-value | P-valuea | d.f. | |
| AASE, Self-efficacy | 3.54 (0.87)a | 3.00 (0.71)b | 2.84 (0.67)b | 15.42 | <0.0001 | 203 |
| PANAS, Positive Affect | 3.30 (0.81) | 3.12 (0.89) | 2.99 (0.74) | 2.41 | 0.09 | 204 |
| PANAS, Negative Affect | 2.61 (1.12) | 2.55 (1.06) | 2.56 (0.94) | 0.08 | 0.93 | 204 |
| Task persistence | 1.77 (0.50) | 1.62 (0.59) | 1.64 (0.57) | 1.37 | 0.26 | 203 |
| CQSS-A, Commitment | 35.23 (5.45)a | 32.64 (6.00)b | 31.68 (5.64)b | 6.80 | 0.001 | 204 |
| Socrates | ||||||
| Recognition | 4.21 (0.57)a | 3.94 (0.67)b | 3.93 (0.54)b | 4.52 | 0.01 | 203 |
| Ambivalence | 4.13 (0.86)a | 3.89 (0.69) | 3.72 (0.73)b | 4.71 | 0.01 | 203 |
| Taking steps | 4.40 (0.61)a | 4.07 (0.64)b | 3.83 (0.67)b | 13.12 | <0.0001 | 203 |
| TSRQ | ||||||
| Autonomous | 6.55 (0.63) | 6.33 (0.86) | 6.31 (0.72) | 2.10 | 0.13 | 203 |
| Introjected regulation | 6.33 (0.95) | 6.14 (1.01) | 5.96 (1.21) | 1.93 | 0.15 | 204 |
| External regulation | 4.96 (1.60)a | 4.41 (1.71) | 4.13 (1.55)b | 4.43 | 0.01 | 204 |
| Amotivation | 2.03 (1.16) | 2.02 (1.16) | 2.12 (1.16) | 0.13 | 0.88 | 204 |
| ADCQ | ||||||
| Costs of change | 2.80 (1.03)a | 3.01 (0.86)a | 3.41 (0.88)b | 7.47 | 0.0007 | 204 |
| Benefits of change | 4.11 (0.75) | 4.18 (0.68) | 4.12 (0.59) | 0.19 | 0.83 | 204 |
Note: SD = Standard deviation; HA-MI = High Abstinence-Minimal Increase; LA-SI = Low Abstinence-Steady Increase; NA-AI = Non-Abstinence-Accelerated Increase.
from Analysis of Variance (ANOVA) test
Subscripts denote significant differences.
Relationship of Pretreatment Trajectories to Within- and Post-treatment Changes in Drinking
Table 4 contains values for within- and between-class change in NDA from baseline to the post-treatment assessment and the 3- and 6-month treatment follow-up assessments. For within-class change, NDA for Class 1 (HA-MI) increased significantly from baseline to each of the three post-treatment assessment time points. NDA for Class 2 (LA-SI) increased significantly from baseline to post-treatment and from baseline to the 3-month follow-up only. Finally, NDA for Class 3 (NA-AI) increased significantly from baseline to each of the three post-treatment assessment time points.
Table 4.
Within and Between Class Change in Days Abstinent at End of Treatment and 3- and 6-month Follow-up Assessments
| End of treatment | 3-mos follow-up | 6-mos follow-up | ||||
|---|---|---|---|---|---|---|
| Est. (SE) | Wald | Est. (SE) | Wald | Est. (SE) | Wald | |
| Within class change in days abstinent by time point | ||||||
| Baseline | ||||||
| Class 1 (HA-MI) | .55 (.27) | 4.27* | .57 (.29) | 3.94* | .63 (.27) | 5.49* |
| Class 2 (LA-SI) | 1.22 (.32) | 14.24*** | .91 (.33) | 7.77** | .69 (.37) | 3.58 |
| Class 3 (NA-AI) | 2.22 (.41) | 28.80*** | 2.24 (.39) | 32.19*** | 2.31 (.40) | 33.34*** |
| Between class change in days abstinent slope by time point | ||||||
| Baseline | ||||||
| Class 1 v. Class 2 | .67 (.42) | 2.56 | .34 (.43) | .61 | .06 (.45) | .02 |
| Class 1 v. Class 3 | 1.67 (.49) | 11.51*** | 1.67 (.49) | 11.71*** | 1.68 (.48) | 12.15*** |
| Class 2 v. Class 3 | 1.00 (.53) | 3.61 | 1.33 (.51) | 6.73** | 1.62 (.54) | 8.90*** |
p < .05
p < .01
p < .001.
Note: Class 1= High Abstinence-Minimal Increase; Class2 = Low Abstinence-Steady Increase; Class 3= Non-abstinence-Accelerated Increase
For between-class change, the change in NDA in Class 2 (LA-SI) was not statistically different from the change in Class 1 at any of the three post-treatment assessment time points. The change in NDA in Class 3 (NA-AI) was significantly greater than the change in Class 1 at each of the three post-treatment assessment time points and significantly greater than the change in Class 2 at the 3- and 6-month follow-up assessments.
We also examined changes in drinks per drinking day (DDD) across the three classes and found no between-class differences in the pattern of change F(4.74, 220.30) = .47, p = .789. However, all three classes did reduce their drinks per drinking day. There was an overall quadratic trend across the three classes, such that DDD decreased from baseline (M = 6.53, SD = 2.86) to end of treatment (M = 4.51, SD = 2.81) and 3-month follow-up (M = 4.48, SD = 2.96), and then increased at 6-month follow-up (M = 5.04, SD = 3.30).
DISCUSSION
This study provides evidence that a substantial subset of individuals who initiate treatment for an AUD begin to change (i.e., reduce) their drinking prior to attending the first treatment session. Using finite mixture modeling we identified three pretreatment trajectory classes: 1) High Abstinence—Minimal Increase (HA-MI), 2) Low Abstinence—Steady Increase (LA-SI), and 3) Non-Abstinent—Accelerated Increase (NA-AI). Thus, all three trajectory classes demonstrated pretreatment change in NDA per week, but the classes differed on the amount of change, when the change began (i.e., before or after phone screen), and the rate of change. With regard to treatment effects, this trajectory classification was predictive of within-treatment changes in drinking as well as post-treatment drinking outcomes. To summarize, NA-AI participants demonstrated the greatest change from baseline to all post-treatment assessment time points; LA-SI participants demonstrated a significant effect at post-treatment and 3 months but not at 6 months; and HA-MI participants demonstrated a small yet significant change in drinking from baseline to all post-treatment assessment time points. Thus, NA-AI participants, the group that was drinking daily or nearly every day during the 8-week pretreatment phase reduced their drinking the most during treatment and demonstrated the greatest change in drinking at the follow-up assessments relative to their baseline. This group’s pattern of pretreatment change also resembles assessment-related behavior change (Clifford and Davis, 2012) as demonstrated by an accelerated rate of change that began after the phone screen and which continued up to the first treatment session.
To our knowledge, the present study is the first specifically designed to capture changes in drinking prior to the first treatment session in a sample of men and women with AUD. These findings add to the growing literature (Epstein et al., 2005, Stasiewicz et al., 2013, Kaminer et al., 2008, Morgenstern et al., 2007, Ondersma et al., 2012, Penberthy et al., 2007, Sobell, 2011) demonstrating that for some individuals, a substantial reduction in drinking takes place prior to the initiation of formal treatment, with changes occurring as early as two weeks prior to placing a call to a treatment program.
The present study also extends previous work by examining differences between the three pretreatment trajectory classes on individual difference variables including demographics, alcohol use and alcohol problem severity, and several variables that have been well established as broadly related to health behavior change (e.g., self-efficacy, commitment to change). The three classes were found not to differ on any of the demographic variables assessed. Notably, Class 2 (LA-SI), which demonstrated the most pretreatment change, did not differ from the other two classes on self-reported levels of social, educational, or economic resources, which have been shown in other research to support individual health behavior change (Kelly and Barker, 2016).
With regard to pretreatment alcohol consumption, there were no between-class differences in drinks per drinking day. However, Class 3 (NA-AI) reported significantly more heavy drinking days compared to Class 1 and Class 2. Although Class 3 reported fewer days abstinent and more heavy drinking days, there were no between-class differences on several measures of alcohol problem severity. Average scores for alcohol-related problems were in the ninth decile of the SIP-A (Miller et al., 1995) and in the severe level of dependence on the ADS (Skinner and Allen, 1982). Also, more than 80% of participants in each group met DSM-5 criteria for AUD-severe (i.e., 6-11 symptoms). Thus, alcohol problem severity does not appear to be a factor in distinguishing pretreatment trajectory classes. However, the absence of an association between alcohol problem severity and class may be due to range restriction (i.e., the majority of participants scored high on all measures of severity) or may reflect the fact that associations between consumption and psychosocial functioning are often found to be low (Witkiewitz, 2019).
However, trajectory class differences were found for several variables associated with health behavior change. Relative to Class 3 (NA-AI), individuals in Class 1 (HA-MI) and Class 2 (LA-SI) reported fewer costs associated with changing alcohol use. Class 1 also reported greater confidence in their ability to abstain, greater commitment to quitting, and greater motivation to change relative to Classes 2 and 3. Given that constructs were assessed at baseline, it is possible that these differences reflect individuals’ self-observation of recent behavior. For example, Class 1 reported a consistently greater number of days abstinent per week during the pretreatment phase and would be expected to report greater abstinence self-efficacy. It seems plausible, however, that stronger commitment and abstinence self-efficacy and fewer perceived costs of change preceded and were at least partially responsible for the higher NDA reported by Class 1.
Without resolving issues of causality, the results of this study suggest that the number of days abstinent (NDA) per week just prior to initiating treatment is inversely related to the amount of change in drinking during treatment and with post-treatment alcohol use. Specifically, Class 1 and Class 2, which reported greater NDA prior to treatment entry, made less within-treatment change, whereas Class 3 (NA-AI), which reported the fewest NDA per week prior treatment, demonstrated the greatest change in NDA per week at each of the three post-treatment assessments.
Although Class 3 (NA-AI) showed the most within treatment change, this class reported fewer abstinent days per week relative to Classes 1 and 2 at all three post-treatment assessments. Thus, Class 3 may derive benefit from increased treatment duration or additional aftercare following treatment. They also may benefit from additional time spent addressing obstacles or barriers to change. Such efforts may help to maintain treatment gains, initiate additional change and prevent relapse, and are consistent with current NIAAA research priorities on recovery processes (NIH, 2019). Class 1 (HA-MI), which demonstrated the least amount of change in days abstinent during treatment, may benefit from a treatment approach that emphasizes alternative end-points such as reducing the number of heavy drinking days and improving non-consumption outcomes such as craving, psychosocial functioning, and quality of life (Witkiewitz, 2013). Finally, Class 2 (LA-SI), which showed the greatest increase in NDA during the pretreatment phase, might benefit from a treatment approach that supports and reinforces changes already made and offers guidance for avoiding relapse. A useful clinical approach with such clients may be to ask them how they were able to make pretreatment changes (Rosengren et al., 2000) (Berg and Miller, 1992). Moreover, knowledge that pretreatment change has occurred may be of value to clinicians in being able to identify and capitalize on client strengths, enhance self-efficacy, and continue progress and maintain gains.
Several additional clinical and research implications follow from the results of this study. One such implication is that a person’s pretreatment drinking behavior should be assessed and used to make decisions in clinical trials investigating adaptive treatment approaches. Such approaches, which utilize aspects of patients’ current functioning as a basis for assignment to treatment condition (Petry et al., 2012), have been increasingly considered in clinical research. However, trials have not yet investigated pretreatment change as a patient characteristic for determining initial treatment decisions. The phenomenon of pretreatment change is relatively widespread, occurring across a number of mental health disorders (e.g., anxiety, depression), in addition to alcohol use disorders. Making use of the predictive value of this phenomenon has great appeal in settings where a premium is placed on the efficiency with which clinicians are able to make decisions regarding appropriate treatment assignment or duration. Importantly, results from such studies have the potential simultaneously to conserve resources and improve treatment outcomes. To date, we know of no published data that examines whether different intensities or types of treatments are appropriate and beneficial for those who change their drinking behavior during the pretreatment interval as compared with individuals who make no or few pretreatment changes in drinking.
Treatment may play a different role for individuals who demonstrate significant pretreatment change. In these instances, treatment may consolidate, rather than initiate, positive changes in drinking (Tucker, 1995). In support of this idea, one study (Stasiewicz et al., 2013) found that their pretreatment change group showed no further significant within-treatment change in drinking, in contrast to the non-change group, which demonstrated increases in PDA and decreases in DDD. Studies that assign pretreatment changers to active versus delayed treatment could shed light on the consolidation versus initiation role of treatment.
In addition to the aforementioned clinical implications, results from the current study have implications for research design and analysis. The phenomenon of pretreatment change poses a challenge to standard methods of evaluating treatment effects as linear over time (Ondersma et al., 2012). Given that the analysis of clinical trial data commonly uses the last pretreatment time point as a baseline, any “anticipation effects” that occur after baseline assessment but before the first treatment session cannot be attributed to treatment itself (Ondersma et al., 2012). In addition, including individuals who demonstrate substantial pretreatment change (i.e., LA-SI) diminishes within-treatment effects as they demonstrate less change during treatment as a result of the improvements in drinking that participants have made on their own prior to the start of treatment (Stasiewicz et al., 2013).
In response to these issues, one approach is to conduct analyses separately for those who demonstrate significant pretreatment change in drinking versus those who do not, either as two separate groups or by including change versus no-change status as a covariate. However, because participants themselves determine whether they belong to a change or no-change condition, causal inference regarding the impact of treatment would be confounded with self-selection. Another approach would be to move the end of the baseline period to much earlier, perhaps two weeks before the PS, to eliminate pretreatment change altogether in measuring treatment effects. While this maneuver may be analytically successful, the design now includes “anticipation effects” prior to treatment as part of the treatment itself. This approach would allow for causal inference regarding treatment in a clinical trial but would include “anticipation of treatment” (which cannot logically vary as a function of the not-yet determined treatment assignment condition) as part of the mechanism of treatment change. A variant of this approach would be to include multiple baselines in an attempt to isolate the anticipation effect. Nonetheless, this approach runs afoul of the critique offered by Ondersma et al (2012).
The best, but most difficult approach, is to conduct random assignment to treatment after the participant’s pretreatment change status has been determined (i.e., immediately prior to the start of treatment). The treatment effect would then be contained within the change or non-change classifications, and the causal inferences would remain valid within classification. This approach, in effect, generates two randomized studies, one for change and one for non-change, but has the advantage of allowing separate treatments for each. In fact, this is the approach that we have taken in an ongoing non-inferiority trial (NIAAA, R01 AA023179). Finally, future research should further refine the classification of pretreatment change status with the dual purpose of increasing our understanding of the factors that promote pretreatment change for these individuals and providing treatments that will assist them in capitalizing on the positive changes they have already made. Though recommendations about the specific content of tailored treatment are bolstered by between-class comparisons of change (see Table 4), there is a methodological issue to consider. Bounded outcome variables, such as the one used in this study, pose a methodological challenge for research. The challenge emerges in the ceiling and floor effects, both of which are manifest in this study. The NA-AI class, by virtue of having the fewest days abstinent at treatment initiation, had the most room to change. The HA-MI and LA-SI classes, by virtue of having more days abstinent, had less room to change, and it is more difficult for them to improved. Nevertheless, future research should focus on developing additional strategies or interventions to initiate and promote greater change in drinking in the NA-AI class.
The current study has several limitations. First, this study used a single sample of AUD treatment-seekers and thus, it’s not certain that the classification model would produce similar results in other samples. Second, most participants met DSM-5 criteria for severe AUD, which limits the generalizability of the results to individuals with mild and moderate AUD. Also, given the high rate of severe AUD and high alcohol dependence of our sample, we were not able to examine the impact of AUD severity on pretreatment change status. Third, as mentioned above, the use of a bounded outcome variable (number of days abstinent per week) imposes ceiling and floor effects. To address the constraints of ceiling and floor effects, future research might consider measuring a spectrum of outcome variables, such as psychosocial functioning and quality of life (Kiluk et al., 2019). Finally, the classification approach used was empirically driven. No underlying psychological mechanisms for catalysts of change or for the trajectories of change, such as commitment and motivation to change drinking, were incorporated in the analysis. We welcome new developments that would refine and improve classification methods for evaluating pretreatment change.
Summary and Conclusions
These limitations aside, to our knowledge this is the first study specifically designed to examine pretreatment changes in drinking in a sample of men and women seeking treatment for AUD. Using a finite mixture model approach to classification, we identified 3 pretreatment change trajectory groups accelerating at different rates with regard to weekly NDA. One group demonstrated minimal or no change during the 8-week pretreatment period. A second group began the process of pretreatment change approximately 2 weeks prior to the PS and demonstrated greater change in NDA per week than the other two classes and the third group demonstrated an accelerated pattern of change that began after the PS. With regard to the impact of pretreatment change on later outcomes (Epstein et al., 2005, Stasiewicz et al., 2013, Rosengren et al., 2000), Class 3 (NA-AI) demonstrated the most within-treatment change, Class 2 (LA-SI) demonstrated the most pretreatment change, but less within-treatment change compared to Class 3 (NA-AI), and Class 1 (HA-MI) also demonstrated significant within-treatment change although less change relative to the other two classes. At the 6-month follow-up, Classes 1 and 3, but not Class 2, continued to demonstrate a significant and positive outcome for NDA. Thus, while two previous studies found that pretreatment change in alcohol use predicted better 3-month (Stasiewicz et al., 2013) and 12-month (Epstein et al., 2005) treatment outcomes, the results of this study show the greatest treatment effect for Class 3, the non-abstinent group. However, with regard to the absolute value of days abstinent per week, having more days abstinent in the week prior to the first treatment session is predictive of more abstinent days at the end of treatment and at 3- and 6-months following treatment. Study findings emphasize the importance of not treating all individuals entering alcohol treatment as though they have the same treatment needs, as this may be a highly inefficient use of resources. Instead, treatment should be adapted to account for the impact of pretreatment trajectories of alcohol use on within-treatment and post-treatment outcomes, thus making treatment more efficient and potentially more effective for those who change more or less prior to treatment.
Supplementary Material
Acknowledgments
This research was supported by RO1 AA022080 and T32 AA007583 from the National Institute on Alcohol Abuse and Alcoholism at the National Institutes of Health. The funding source had no role in the study design, collection, analyses, and interpretation of the data, writing of the manuscript or the decision to submit the manuscript for publication.
Appendix
Study Advertisement
Concerned about your drinking? Has a loved one or friend ever expressed concerns about your drinking? If this is you, then pay close attention to this opportunity. The University at ________ is offering confidential research-based treatment for men and women who are experiencing problems with alcohol.
This confidential program is run by professional and understanding counselors…
Take the first step and call 555-55-55 today. That’s 555-55-55 to find out more about this confidential research-based treatment program, available at no cost to you through the University at ______________. The number again is 555-55-55.
Footnotes
There are 12 treatment sessions that are represented in Figure 2 as 11 weekly intervals. Timepoint “0” represents the weekly interval between the baseline assessment and the first treatment session.
A 180-day timeline follow-back was conducted at the baseline assessment. The 8-week pretreatment phase includes the 7-week period (49 days) prior to the baseline plus the 1-week period between baseline and the first treatment session. To obtain the number of days in the Drinking history interval (HX) we subtracted 49 days from 180, which resulted in 131 days.
References
- ALLEN J, ANTON RF, BABOR TF, CARBONARI J, CARROLL KM, CONNORS GJ, COONEY NL, DEL BOCA FK, DICLEMENTE CC, DONOVAN D, KADDEN RM, LITT M, LONGABAUGH R, MATTSON M, MILLER WR, RANDALL CL, ROUNSAVILLE BJ, RYCHTARIK RG, STOUT RL, TONIGAN JS, WIRTZ PW & ZWEBEN A 1997. Project MATCH secondary a priori hypotheses. Addiction, 92, 1671–1698. [PubMed] [Google Scholar]
- BAUMEISTER RF 1996. The crystallization of discontent in the process of major life change In: WEINBERGER TFHJL (ed.) Can Personality Change. Washington, DC: American Psychological Association. [Google Scholar]
- BERG IK & MILLER SD 1992. Working with the Problem Drinker, New York, Norton. [Google Scholar]
- BUSH K, KIVLAHAN DR, MCDONELL MB, FIHN SD, BRADLEY KA & PROJECT ACQI 1998. The AUDIT alcohol consumption questions (AUDIT-C) - An effective brief screening test for problem drinking. Archives of Internal Medicine, 158, 1789–1795. [DOI] [PubMed] [Google Scholar]
- CAREY KB 1997. Reliability and validity of the time-line follow-back interview among psychiatric outpatients: A preliminary report. Psychology of Addictive Behaviors, 11, 26–33. [Google Scholar]
- CLIFFORD PR & DAVIS CM 2012. Alcohol treatment research assessment exposure: a critical review of the literature. Psychol Addict Behav, 26, 773–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CUNNINGHAM JA, SOBELL LC, GAVIN DR, SOBELL MB & BRESLIN FC 1997. Assessing motivation for change: Preliminary development and evaluation of a scale measuring the costs and benefits of changing alcohol or drug use. Psychology of Addictive Behaviors, 11, 107–114. [Google Scholar]
- DECI EL & RYAN RM 1985. Intrinsic Motivation and Self-Determination in Human Behavior, New York, Plenum. [Google Scholar]
- DICLEMENTE CC, CARBONARI JP, MONTGOMERY RP & HUGHES SO 1994. The Alcohol Abstinence Self-Efficacy scale. J Stud Alcohol, 55, 141–8. [DOI] [PubMed] [Google Scholar]
- DIGGLE PJ, LIANG KY & ZEGER SL 1994. Analysis of Longitudinal Data, Oxford, UK, Clarendon Press. [Google Scholar]
- EPSTEIN EE, DRAPKIN ML, YUSKO DA, COOK SM, MCCRADY BS & JENSEN NK 2005. Is alcohol assessment therapeutic? Pretreatment change in drinking among alcohol dependent women. Journal of Studies on Alcohol, 66, 369–378. [DOI] [PubMed] [Google Scholar]
- FRALEY C & RAFTERY AE 2002. Model-based clustering, discriminant analysis, and density estimation. Journal of the American Statistical Association, 97, 611–631. [Google Scholar]
- HALEKOH U, HOJSGAARD S & YAN J 2006. The R Package geepack for Generalized Estimating Equations. Journal of Statistical Software, 15, 1–11. [Google Scholar]
- HALLGREN KA, EPSTEIN EE & MCCRADY BS In press. Changes in hypothesized mechanisms of change before and after initiating abstinence in cognitive-behavioral therapy for women with alcohol use disorder. Behavior Therapy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HARDIN JW & HILBE JM 2013. Generalized estimating equations, Boca Raton, FL, CRC Press. [Google Scholar]
- HASTIE TJ, TIBSHIRANI RJ & FRIEDMAN J 2001. The Elements of Statistical Learning: Data Mining, Inference, and Prediction, New York, NY, Springer. [Google Scholar]
- JANIS ILM, L. 1977. Decision-making: A Psychological Analysis of Conflict, Choice, and Commitment, New York, NY, Free Press. [Google Scholar]
- KADDEN R, CARROLL K, DONOVAN D, MONTI P, ABRAMS D, LITT M, & & HESTER R 1992. Cognitive-behavioral coping skills therapy manual, Maryland, NIAAA. [Google Scholar]
- KAHLER CW, LACHANCE HR, STRONG DR, RAMSEY SE, MONTI PM & BROWN RA 2007. The commitment to quitting smoking scale: initial validation in a smoking cessation trial for heavy social drinkers. Addict Behav, 32, 2420–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KAMINER Y, BURLESON JA & BURKE RH 2008. Can Assessment Reactivity Predict Treatment Outcome Among Adolescents with Alcohol and Other Substance Use Disorders? Substance Abuse, 29, 63–69. [DOI] [PubMed] [Google Scholar]
- KELLY MP & BARKER M 2016. Why is changing healt-related behavior so difficult? Public Health, 136, 109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KILUK BD, FITZMAURICE GM, STRAIN EC & WEISS RD 2019. What defines a clinically meaningful outcome in the treatment of substance use disorders: reductions in direct consequences of drug use or improvement in overall functioning? Addiction, 114, 9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KINDSVATTER A, OSBORN CJ, BUBENZER D & DUBA JD 2010. Client Perceptions of Pretreatment Change. Journal of Counseling and Development, 88, 449–456. [Google Scholar]
- LAWSON D 1994. Identifying pretreatment change. Journal of Counseling and Development, 7, 244–248. [Google Scholar]
- LEISCH F 2004. FlexMix: A general framework for finite mixture models and latent class regression in R. Journal of Statistical Software, 11, 1–18. [Google Scholar]
- MAISTO SA, SOBELL MB & SOBELL LC 1982. Reliability of self-reports of low ethanol consumption by problem drinkers over 18 months of follow-up. Drug and Alcohol Dependence, 9, 273–278. [DOI] [PubMed] [Google Scholar]
- MCKIERNAN P, CLOUD R, PATTERSON DA, WOLF S, GOLDER S & BESEL K 2011. Development of a brief abstinence self-efficacy measure. Journal of Social Work Practice and the Addictions, 11, 245–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MCLACHLAN G & PEEL D 2000. Finite Mixture Models, New York, NY, Wiley. [Google Scholar]
- MILLER WR & TONIGAN JS 1996. Assessing drinkers’ motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). Psychology of Addictive Behaviors, 10, 81–89. [Google Scholar]
- MILLER WR, TONIGAN S & LONGABAUGH R 1995. The Drinker Inventory of Consequences (DrinC): An instrument for assessing adverse consequences of alcohol abuse NIAAA Project MATCH monograph series. Washington, D.C.: Government Printing Office. [Google Scholar]
- MORGENSTERN J, IRWIN TW, WAINBERG ML, PARSONS JT, MUENCH F, BUX DA, KAHLER CW, MARCUS S, & & SCHULZ-HEIK J 2007. A randomized controlled trial of goal choic interventions for alcohol use disorders among men who have sex with men. Journal of Consulting and Clinical Psychology, 75, 72–84. [DOI] [PubMed] [Google Scholar]
- NESS ME & MURPHY JJ 2001. Pretreatment change reports by clients in a university counseling center: Relationship to inquiry technique, client, and situational variables. Journal of College Counseling, 4, 20–31. [Google Scholar]
- NIH. 2019. Understanding Processes of Recovery in the Treatment of Alcohol Use Disorder [Online]. Available: https://grants.nih.gov/grants/guide/pa-files/PA-18-619.html [Accessed 2019].
- NOYES ET, LEVINE JA, SCHLAUCH RC, CRANE C, CONNORS GJ, MAISTO SA & & DEARING RL 2018. Impact of pretreatment change on mechanism of behavior change research: An applied example using alcohol abstinence self-effiacy. Journal of Studies on Alcohol and Drugs, 79, 223–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ONDERSMA SJ, WINHUSEN T & LEWIS DF 2012. Pre-treatment change in a randomized trial with pregnant substance-abusing women in community-based outpatient treatment. Contemporary Clinical Trials, 33, 1074–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ORFORD J, HODGSON R, COPELLA A, JOHN B, SMITH M, BLACK R, FRYER K, HANDFORTH L, ALWYN T, KERR C, THISTLETHWAITE G & SLEGG G 2006a. The clients’ perspective on change during treatment for an alcohol problem: qualitative analysis of follow-up interviews in the UK Alcohol Treatment Trial. Addiction, 101, 60–68. [DOI] [PubMed] [Google Scholar]
- ORFORD J, KERR C, COPELLA A, HODGSON R, ALWYN T, BLACK R, SMITH M, THISTLETHWAITE G, WESTWOOD A & SLEGG G 2006b. Why people enter treatment for alcohol problems: Findings from UK alcohol treatment trial pre-treatment interviews. Journal of Substance Use, 11, 161–176. [Google Scholar]
- PENBERTHY JK, AIT-DAOUD N, BRETON M, KOVATCHEV B, DICLEMENTE CC & JOHNSON BA 2007. Evaluating readiness and treatment seeking effects in a pharmacotherapy trial for alcohol dependence. Alcoholism: Clinical and Experimental Research, 31, 1538–1544. [DOI] [PubMed] [Google Scholar]
- PETRY NM, BARRY D, ALESSI SM, ROUNSAVILLE BJ & CARROLL KM 2012. A randomized trial adapting contingency management targets based on initial abstinence status of cocaine-dependent patients. Journal of Consulting and Clinical Psychology, 80, 276–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PROCHASKA JO & DICLEMENTE CC 1984. The Transtheoretical Approach: Crossing Traditional Boundaries of Therapy, Homewood, Illinois, Dow Jones-Irwin. [Google Scholar]
- ROSENGREN DB, DOWNEY L & DONOVAN DM 2000. “I already stopped”: Abstinence prior to treatment. Addiction, 95, 65–76. [DOI] [PubMed] [Google Scholar]
- SHEEHAN DV, LECRUBIER Y, SHEEHAN KH, AMORIM P, JANVAS J, WEILLER E, HERGUETA T, BAKER R & & DUNBAR G 1998. The Mini International Neuropsychiatric Interview (MINI): The development and validationof a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry, 59, 38–66. [PubMed] [Google Scholar]
- SKINNER HA & ALLEN BA 1982. Alcohol dependence syndrome: Measurement and validation. Journal of Abnormal Psychology, 91, 199–209. [DOI] [PubMed] [Google Scholar]
- SOBELL LC 2007. The Phenomenon of Self-Change” Overview and Key Issues In: KLINGEMANN H & SOBELL LC (eds.) Promoting Self-Change from Addictive Behaviors: Practical Implications for Policy, Prevention, and Treatment. Springer. [Google Scholar]
- SOBELL LC 2011. Self-change: Findings and implications for the treatment of addictive behaviors. 8th Annual INEBRIA Conference Boston, MA. [Google Scholar]
- SOBELL LC, CUNNINGHAM JA & SOBELL MB 1996. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. American Journal of Public Health, 86, 966–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SOBELL LC, MAISTO SA, SOBELL MB & COOPER AM 1979. Reliability of alcohol abusers’ self-reports of drinking behavior. Behaviour Research and Therapy, 17, 157–160. [DOI] [PubMed] [Google Scholar]
- SOBELL LC & SOBELL MB 1992. Timeline Follow-back: A technique for assessing self-reported ethanol consumption In: ALLEN J & LITTEN RZ (eds.) Measuring alcohol consumption: Psychosocial and biological methods. Totowa, NJ: Humana Press. [Google Scholar]
- SOBELL LC, SOBELL MB & TONEATTO T 1991. Recovery from Alcohol Problems without Treatment In: HEATHER N, MILLER WR & GREELEY J (eds.) Self Control and the Addictive Behaviours. New South Wales, Australia: Maxwell Macmillan. [Google Scholar]
- STASIEWICZ PR, SCHLAUCH RC, BRADIZZA CM, BOLE CW & COFFEY SF 2013. Pretreatment changes in drinking: relationship to treatment outcomes. Psychol Addict Behav, 27, 1159–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TEAM, R. C. 2018. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- TUCKER JA 1995. Predictors of help-seeking and the termporal relationship of help to recovery among treated and untreated recovered problem drinkers. Addiction, 90, 805–8069. [DOI] [PubMed] [Google Scholar]
- WATSON D, CLARK L & TELLEGEN A 1988. Development and validation of brief measures of positive and negative affect: The PANAS. Journal of Personality and Social Psychology, 54, 1063–1070. [DOI] [PubMed] [Google Scholar]
- WEINER-DAVIS M, DE SHAZER S, & GINGERICH WJ 1987. Building on pretreatment change to construct the therapeutic solution. Journal of Marital and Family Therapy, 13, 359–363. [Google Scholar]
- WEST DS, HARVEY-BERINO J, KRUKOWSKI RA & SKELLY JM 2011. Pretreatment weight change is associated with obesity treatment outcomes. Obesity, 19, 1791–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WILLENBRING ML 2007. A broader view of change in drinking behavior. Alcoholism: Clinical and Experimental Research, 31, 84S–86S. [DOI] [PubMed] [Google Scholar]
- WITKIEWITZ K 2013. “Success” following alcohol treatment. Alcoholism: Clinical and Experimental Research, 37, E9–E13. [DOI] [PubMed] [Google Scholar]
- WITKIEWITZ K 2019. Double standards and gold standards in the evaluation of how a person feels and functions in substance use disosrder pharmacotherapy trials. Addiction, 114, 16–17. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.