Abstract
Introduction:
Improving diet is a prime target for the prevention and management of chronic disease. The communal coping model suggests that families can mitigate shared risk of chronic disease through encouragement of healthful eating, eliciting preventive behaviors.
Method:
Using network data from 69 Australian families across three ancestry groups (Anglo, Italian, and Asian) with varied family health histories, the present study applied social network analysis to identify patterns of intergenerational encouragement of healthful eating behavior within families, and assess whether patterns varied by family ancestry or disease density.
Results:
Findings indicated variation in patterns of health encouragement by ancestry such that Asian-Australian families were most distinct from the other ancestry groups. While there was no main effect of familial disease history, it moderated the effect of Italian ancestry on intergenerational encouragement patterns.
Discussion:
These results provide important context for future family-based interventions that leverage normative patterns of intergenerational exchange of encouragement or aim to modify such patterns in an effort to improve family health.
Keywords: Intergenerational relationships, family communication, family networks
Complex, chronic diseases, including cardiovascular disease, cancer, and diabetes, are the leading cause of death and disability worldwide (World Health Organization, 2014) and account for more than 90% of all mortality in Australia (Australian Institute of Health and Welfare, 2014). Some migrant groups, including Asian and European migrants, experience elevated rates of these diseases relative to the Australian-born population and those who remain in their country of origin, while others benefit from the protective effects of maintaining country-of-origin lifestyles (Anikeeva et al., 2012; Hodge, English, O’Dea, & Giles, 2004; Wahlqvist, 2002). Poor diet/nutrition is a shared, modifiable risk factor for lifestyle-related diseases, including heart disease, diabetes, breast and colorectal cancer (Key et al., 2004; Mente, de Koning, Shannon, & Anand, 2009). Through encouragement of healthful eating, family members can elicit preventive health behaviors and mitigate risk of chronic disease (Ashida, Wilkinson, & Koehly, 2012; de Heer et al., 2016; Ersig, Williams, Hadley, & Koehly, 2009).
Here, we aim to understand patterns of health encouragement that occur within multigenerational families. Health encouragement refers to an interpersonal mechanism through which health-promoting behaviors are influenced by direct communication, social facilitation, or social modeling (Skapinsky et al., 2018). Previous studies have demonstrated an effect of behavioral encouragement within families (e.g., between spousal and parent-child dyads) on increases in physical activity (de Heer et al., 2016; Skapinsky et al., 2018). Using innovative social network methods, we examined how Australian families from three different backgrounds (Anglo-Australians, Italian-Australians, and Asian-Australians) exchange healthful eating encouragement. Specifically, we identified patterns of individuals’ perceptions of healthful eating encouragement exchanges (i.e., provision and receipt), and considered whether family ancestry and disease history are associated with these patterns. Findings were interpreted under the Communal Coping Model, which offers insight into how family members promote and maintain members’ health and well-being (Afifi, Hutchinson, & Krouse, 2006; Lyons, Mickelson, Sullivan, & Coyne, 1998). Interpersonal processes that underlie the communal coping framework include communication about a shared health threat, joint appraisal of the threat and belief that a joint effort is useful for addressing it, and shared engagement in strategies for reducing the threat. We conceptualize encouragement of healthful eating behavior as cooperative action taken by family members to address the shared threat of disease.
Intergenerational Exchange Patterns
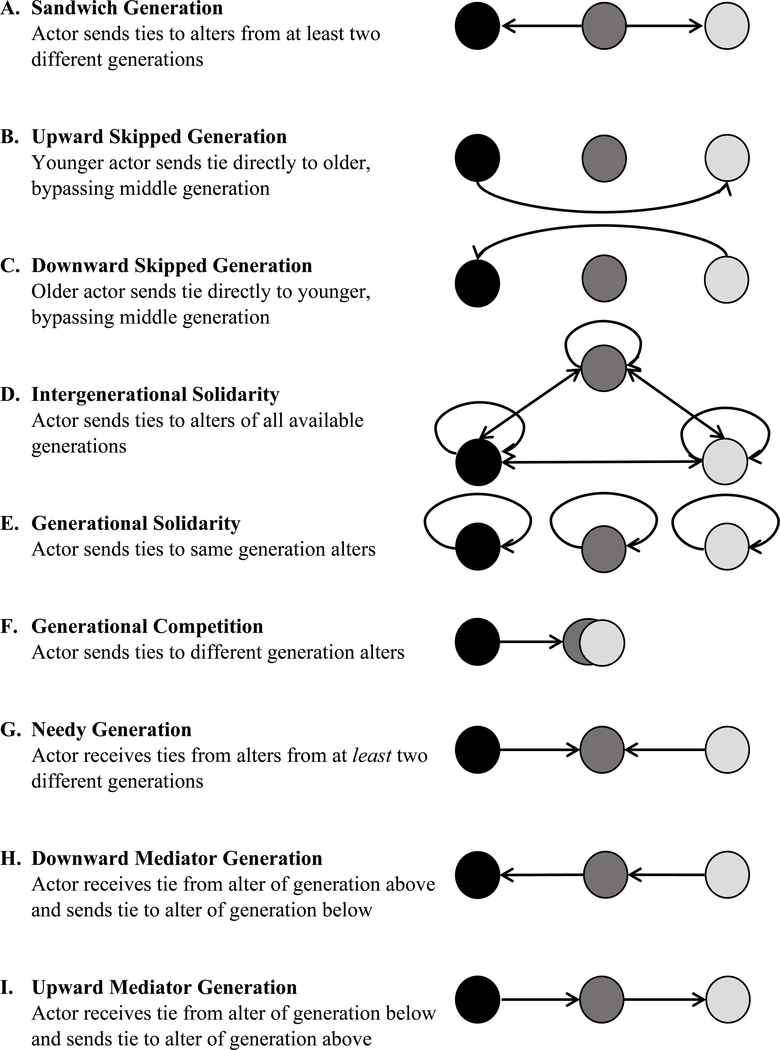
Families are complex systems comprised of structured interpersonal relationships (“networks”), in which information, resources, and support (“ties”) are exchanged among individual family members (“actors”; Wasserman & Faust, 1994). Using generational membership to categorize actors into structural classes within a family network, we can uncover common patterns of intergenerational exchange. Marcum and Koehly (2015) describe how intra- and intergenerational exchange converges on nine distinct patterns (Figure 1). These exchange patterns are not mutually exclusive but can occur jointly within a family system. We focus on four patterns that are commonly described in the literature to characterize healthful eating encouragement within families: 1) sandwich generation; 2) downward skipped-generation, 3) upward skipped-generation; and 4) intergenerational solidarity.
Figure 1.
Models of intergenerational exchange triadic structures, adapted from Marcum and Koehly (2015)
Middle-aged adults with simultaneous obligations to their own children and aging parents may feel a responsibility to be a hub of health encouragement for members of both generations. This pattern of encouragement exemplifies the “sandwich generation” pattern (Miller, 1981), in which an actor from one generation sends ties (i.e., encouragement) to members from two other generations (Figure 1A). In some multigenerational households, grandparents have a central role in caring for grandchildren (Hayslip & Kaminski, 2005), including influencing children’s eating behavior (Bell, Perry, & Prichard, 2018). Children may also actively encourage health behaviors of older family members, especially as they gain independence and exposure to different norms and behaviors (de la Haye, de Heer, Wilkinson, & Koehly, 2014). Consequently, the parent generation may be absent from health encouragement exchanges and instead exchanges occur directly between the oldest and youngest generations, characterized by “skipped” generation patterns (Rhodes et al., 2016; Figures 1B and 1C). Finally, given how social roles and generational positions shape health encouragement, all family members may share responsibility in unique ways resulting in “intergenerational solidarity (Figure 1D). Older generations often possess greater knowledge of family disease history and pass this onto younger generations to inform health behavior (Ashida, Kaphingst, Goodman, & Schafer, 2013). Younger generations might simultaneously encourage older family members to adopt healthful behaviors, especially for chronic disease management (de la Haye et al., 2014; Laroche et al., 2009). Thus, intergenerational solidarity occurs when family members of one generation are equally likely to encourage healthful eating behaviors in those of all generations, including their own, subsuming all other exchange patterns.
We focus primarily on four exchange patterns because they represent prominent patterns of relationships established over the life course of the family (Putney & Bengtson, 2003). It should be noted that families do not conform to one single triadic structure, but rather, experience the co-occurrence of multiple patterns of intergenerational health encouragement. Thus, we consider the four focal patterns in the context of all nine patterns of intergenerational exchange described by Marcum and Koehly (2015). Further, we hypothesize that these patterns may vary based on family ancestry and disease history.
Considering Familial Ancestry and Disease History
Beyond individual family differences, variation in health encouragement patterns may be attributed to family-level factors, such as ancestry and disease history. In Western cultures, resources and support traditionally flow downward through generations (Bengtson, 2001). Intergenerational relations in Asian societies are rooted in filial piety, which emphasizes the role of younger generations as the primary support of their elders (Liu, Ng, Weatherall, & Loong, 2000). Although expectations of elderly Asian parents have shifted as a result of acculturation, strong support for filial piety remains among migrant Asian families (Liu et al., 2000). Younger generations of migrant families have also been found to be brokers of health information, especially when there is a language barrier (Marcum & Koehly, 2015). Taken together, we expect to see health encouragement flow upward more frequently in Italian- and Asian-Australian families, both migrant populations, relative to Anglo-Australians, as exemplified by sandwich generation and upward-skipped patterns. Moreover, the collectivist culture that characterizes Asian societies may manifest at the family level such that we observe intergenerational solidarity patterns of health encouragement among Asian-Australian families more frequently than in Anglo-Australian families.
Families often vary in their specific health concerns because diseases tend to cluster within families (Koehly et al., 2009). Awareness of shared risk shapes health communication, support, and behavior (Ashida et al., 2013). Previous studies have examined the influence of genetic risk information or family health history (FHH) on health behavior change (de Heer et al., 2016; McBride et al., 2010), but less is known about how baseline knowledge of family disease history in the absence of intervention influences health encouragement patterns. For example, after multiple cancer diagnoses, a family might identify as a “cancer family” (Palmquist et al., 2010), and subsequently encourage healthful behaviors among its members. In the present study, we developed family-level disease densities based on reported diagnoses of heart disease, diabetes, breast and colorectal cancer within the family to capture family disease history.
Dietary habits developed early in life have long-term implications. Thus, prevention efforts may be directed downward towards younger generations (de Heer et al., 2016; de la Haye et al., 2014). Additionally, health maintenance and disease management in older generations may serve as the impetus for directing health encouragement efforts upwards. Thus, the influences of family disease history on healthful eating encouragement are bidirectional. Families aim to prevent disease in younger generations while simultaneously supporting disease management in older generations (Koehly, 2016), resulting in sandwich generation, skipped-generation, and/or intergenerational solidarity patterns. Finally, the risk and diagnosis of chronic diseases are not uniformly distributed throughout the population. Beyond the independent influences of ancestry and disease history, we examine whether ancestry moderates the effect of familial disease history on patterns of intergenerational health encouragement.
Using family-level data, this study: 1) identified the extent to which different patterns of intergenerational encouragement of healthful eating occur within multigenerational families, and 2) assessed whether these patterns varied by family ancestry and disease history. This study extends the results of prior work on intergenerational health communication from a communal coping perspective (e.g., Marcum & Koehly, 2015) by uniquely including informants from three generations. By identifying patterns of intergenerational encouragement that naturally occur within families, we provide a basis from which to evaluate whether these patterns of encouragement of healthy eating behaviors are effective in motivating behavior change that mitigates chronic disease risk through intervention. Furthermore, applying social network analysis to family-level data enables a richer understanding of how families communicate and support healthful behaviors across generations, informing future interventions and policies.
Method
Participants
The Families SHARE Australia project is an intervention study which sought to evaluate the impact of family health history (FHH)-based risk for common, chronic diseases on family-level encouragement of, and intentions to engage in, preventive health behaviors (see Wilson et al., 2016). Women, particularly mothers, are often more active in health communication and disease prevention in the family (Koehly et al., 2009; Williams, 2007). Thus, mothers from three ethnic groups, Anglo-Australian, Italian-Australian, and Asian-Australians (Vietnamese- and Chinese-Australian) were recruited through advertisement in ethnically targeted areas of the city (see Hughes, Hutchinson, Prichard, Chapman, & Wilson, 2015). Initial eligibility requirements for participation included having at least one Australian-born child aged 10–18 living at home (i.e., index child participant) and at least four additional family members spanning three generations, including the index child’s generation, living in Australia and willing to participate. The final family-level sample (n = 69) included 42 Anglo-Australian, 19 Italian-Australian, and 8 Asian-Australian families (Table 1).
Table 1.
Family-level descriptive characteristics by ancestry
| Anglo (n = 42) | Italian (n = 19) M (SD) |
Asian (n = 8) | |
|---|---|---|---|
| Family egos | 4.81 (0.94) | 4.84 (0.90) | 4.00 (0.76) |
| Family network size | 7.40 (2.32) | 6.42 (1.89) | 6.63 (1.41) |
| Family network % female | 62 (22) | 66 (14) | 69 (15) |
| Family income | 4.49 (1.69) | 4.60 (1.87) | 3.77 (1.76) |
| Index child age | 11.71 (2.96) | 10.61 (4.75) | 12.75 (3.15) |
| Family disease density | 0.05 (0.04) | 0.10 (0.06) | 0.05 (0.03) |
| n (%) families | |||
| Heart disease diagnosis | 36 (86%) | 14 (74%) | 3 (38%) |
| Diabetes diagnosis | 25 (60%) | 17 (89%) | 4 (50%) |
| Breast cancer diagnosis | 21 (50%) | 9 (47%) | 3 (38%) |
| Colorectal cancer diagnosis | 15 (36%) | 9 (47%) | 1 (13%) |
| 3-generation family | 39 (93%) | 17 (89%) | 8 (100%) |
| 4-generation family | 3 (7%) | 2 (11%) | 0 (0%) |
Notes. Family network size includes respondent egos and non-respondent alters. Family income ranges from 1 to 9 (1 = $0–20,000; 2 = $20,001–35,000; 3 = $35,001–50,000; 4 = $50,001–75,000; 5 = $75,001–100,000; 6 = $100,001–125,000; 7 = $125,001–150,000; 8 = $150,001–200,000; 9 = $200,001 or more). Diagnosis measures represent number of families in the sample with at least one diagnosis of each of the four diseases.
Procedures
A detailed description of the Families SHARE Australia project protocol has been previously published (Wilson et al., 2016). Each participant was asked to complete a baseline and 6-month follow-up assessment, including surveys of lifestyle behaviors, attitudes, risk perceptions, and social network assessment. The present study used baseline assessment data.
Measures
Outcome: Healthful eating encouragement.
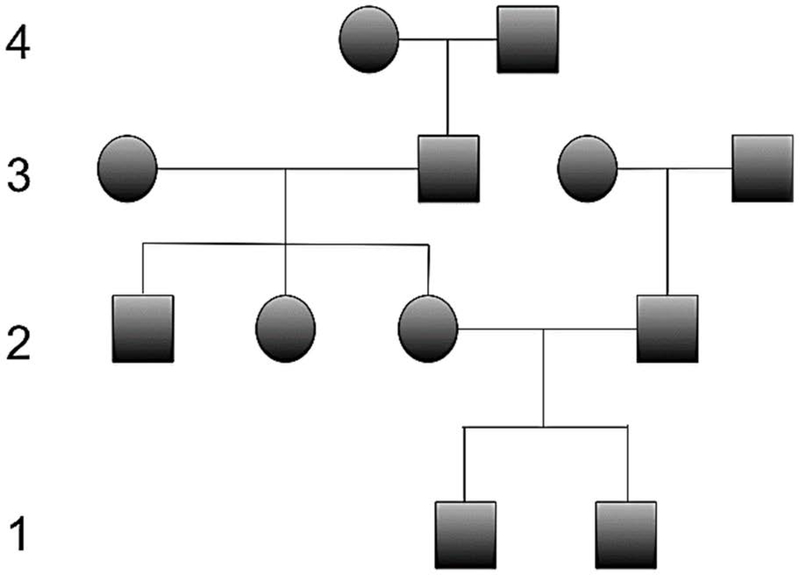
Our dependent variable is the pattern of intergenerational exchange in families formed by encouragement of healthful eating behavior between family members across generations. The ties used to construct the network were measured using four items: in-ties, or connections directed from alters to a participant, were measured with two items: “[Who], over the past 3 months, has encouraged you to eat [fruits and vegetables/fibre]?”; out-ties, or connections directed from a participant to alters, were measured with two items: “[Who] have you encouraged to eat [fruits and vegetables/fibre]?” Directed ties as reported by the respondents were constructed based on the union of the two items (Supplemental Materials). Next, generational position was determined based on relationship to the index child participant, or “generation 1” (Figure 2). Family networks were constructed to include both respondent egos and non-respondent alters. Networks included nuclear/step-family, extended family, and family through marriage and excluded enumerated friends and coworkers. The final outcomes were calculated by counting the number of triadic features in a network that are consistent with each of the nine intergenerational exchange pathways (Figure 1) and dividing by the number of each of those features that were possible (Lienert, Koehly, Reed-Tsochas, & Marcum, 2019; Marcum & Koehly, 2015).
Figure 2.
Pedigree depicting generational positions of family network wherein generation 1 represents the child generation (e.g. index child, siblings, and first cousins), generation 2 represents the parent generation (e.g. mother, father, aunts, uncles, and non-blood relatives), generation 3 represents the grandparent generation, and generation 4 represents the great-grandparent generation.
Ancestry.
Cultural ancestry was determined by adult participants’ nativity status and ethnic self-identification (“Do you identify your family as [Australian/Vietnamese, Australian/Chinese, Australian/Italian or Australian/Other]?”) and represented different waves of migration to Australia (Supplemental Materials).
Disease density.
Family history of disease was operationalized using disease density, the fraction of affected individuals per family. Diagnoses of heart disease, diabetes, breast and colorectal cancer of the index child’s first- and second-degree relatives, as reported by the mother, were summed to create a count of total diagnoses, then divided by four (total diseases) times the family size to calculate disease density. Possible values range from 0 to 1, where 0 represents no disease diagnoses in the family and 1 represents diagnosis of all four diseases among all family members. Higher values indicated greater familial disease density.
Covariates.
Participants reported their gender, age, and income, as well as gender of and relationship to non-respondent alters from which family network-level demographic variables were constructed, including percentage of females and mean income (Table 1).
Analysis Strategy
We used seemingly unrelated regression (SUR) models to estimate the propensity of each of nine intergenerational exchange pathways to occur, accounting for covariation between the nine intergenerational exchange patterns (Zellner, 1962). To handle the complexity of the co-occurrence of encouragement patterns, we allow the variation from the triadic structure in one equation to enter into the others simultaneously (Supplemental Materials). The first set of models estimated the main effects of disease risk and ancestry (Model 1), and the second set included their interaction (Model 2). All models controlled for family income and percentage of females in the family network as these covariates may contribute to intergenerational encouragement of health behavior. The interaction model, with eight parameters and 68 degrees of freedom, has a power of 0.4 to detect a statistically significant effect at the .05 alpha level, making this a low- powered test and results should be interpreted as such (Supplemental Materials).
Results
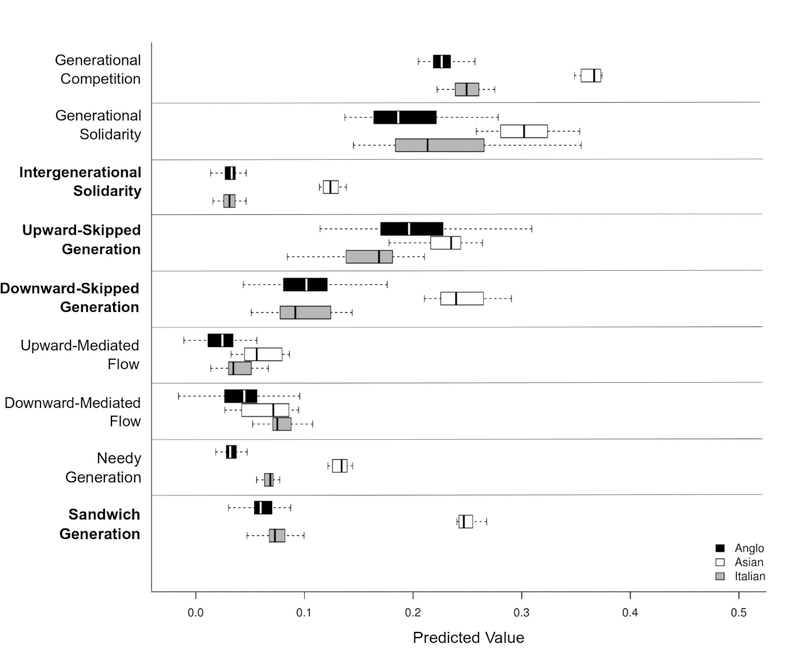
Box-and-whisker plots depict the predictive distribution of the nine intergenerational exchange patterns for encouragement of healthful eating behavior by ancestry (Figure 3). Although there is evidence for each of the nine exchange patterns, some appear to be more commonly observed in these networks than others based on the predicted median value. Generational competition and generational solidarity, for example, occur more frequently than upward- and downward-mediated flow. The relatively small boxplots, in sandwich and needy generation for example, indicated that families within each ancestry group were relatively consistent in their propensity for exhibiting these patterns of health encouragement. Additionally, for several patterns (e.g., sandwich generation, intergenerational solidarity), non-overlapping boxes indicated that Asian-Australian families are distinct from the others. We focus on results for sandwich generation, upward-skipped, downward-skipped, and intergenerational solidarity patterns. See supplemental materials for results of the remaining patterns.
Figure 3.
Box-and-Whisker plots depicting distribution of predicted values of intergenerational encouragement exchange structures by ancestry from Model 1 in the order of relative propensity to occur. Median values are indicated by the black or white bands and whiskers extend to 1.5 times the interquartile range of the distribution. Boxes represent the full range of each ancestry group’s predicted rates of use of each of the nine intergenerational exchange structure in health encouragement, net of alternative exchange structures and after adjusting for other covariates. The four focal exchange structures are indicated in bold.
Using SUR, significant differences due to ancestry were observed in the occurrence of sandwich generation and intergenerational solidarity, but not upward- or downward-skipped patterns (Table 2). Compared to Anglo-Australians, Asian-Australian families exhibited a greater propensity for the sandwich generation pattern (Model 1). Asian families were also more likely to demonstrate the intergenerational solidarity pattern of health encouragement when compared to Anglo-Australians. Italian ancestry was not significantly associated with patterns of health encouragement.
Table 2.
Results from seemingly unrelated regression (SUR) demonstrating propensity for observing intergenerational contact patterns of encouragement of healthful eating
| Sandwich Generation | Downward-Skipped | Upward-Skipped | Intergenerational Solidarity |
|||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Intercept | 0.07 (0.07) |
0.03 (0.07) |
−0.03 (0.14) |
−0.07 (0.15) |
0.25 (0.22) |
0.16 (0.23) |
0.06 (0.04) |
0.04 (0.05) |
| Ancestry | ||||||||
| Asian | 0.19*** (0.04) |
0.11 (0.07) |
0.14 (0.08) |
0.22 (0.16) |
0.04 (0.13) |
−0.009 (0.24) |
0.10*** (0.03) |
0.04 (0.05) |
| Italian | 0.01 (0.03) |
0.11* (0.05) |
−0.03 (0.07) |
0.05 (0.11) |
−0.03 (0.10) |
0.18 (0.17) |
−0.005 (0.02) |
0.04 (0.03) |
| Disease density | −0.08 (0.28) |
0.56 (0.41) |
0.64 (0.59) |
1.37 (0.93) |
0.13 (0.90) |
1.60 (1.41) |
0.03 (0.18) |
0.29 (0.28) |
| Family income | −0.005 (0.008) |
−0.005 (0.007) |
0.007 (0.02) |
0.006 (0.02) |
0.01 (0.02) |
−0.009 (0.02) |
−0.005 (0.005) |
−0.005 (0.005) |
| % family female | 0.03 (0.07) |
0.05 (0.21) |
0.11 (0.15) |
0.13 (0.15) |
−0.15 (0.22) |
−0.12 (0.22) |
−0.005 (0.05) |
−0.0003 (0.04) |
| Disease density by Ancestry | ||||||||
| Asian | 1.52 (1.16) |
−1.42 (2.62) |
0.83 (3.97) |
1.16 (0.78) |
||||
| Italian |
−1.35* (0.54) |
−1.18 (1.22) |
−2.82 (1.85) |
−0.60 (0.36) |
||||
| Adjusted R2 | 0.233 | 0.322 | −0.0009 | −0.016 | −0.057 | −0.045 | 0.135 | 0.196 |
Notes. Reference group for ancestry = Anglo-Australian. McElroy R2 for the system of models (i.e., all encouragement patterns) equaled 0.104 for Model 1 and 0.167 for Model 2.
p < .05;
p < .01;
p < .001
Familial disease history was not directly associated with patterns of health encouragement, but it did moderate the association between Italian ancestry and health encouragement patterns. Italian-Australians’ propensity for the sandwich generation pattern was moderated by familial disease density such that this positive association was attenuated as disease density increased (Model 2). In other words, Italian-Australian families with relatively high disease density were less likely than families with lower disease density to adopt sandwich generation patterns of healthful eating encouragement. Families’ propensity for demonstrating upward-skipped, downward-skipped, and intergenerational solidary patterns for healthful eating encouragement were not significantly moderated by familial disease density.
Discussion
Families are a valuable resource in intervention efforts aimed at preventing chronic disease and promoting healthful behaviors. The purpose of this study was to characterize naturally occurring patterns of intergenerational encouragement of healthful eating and assess whether these patterns varied by ancestry and family disease risk through the application of social network analysis.
Healthful eating encouragement flowed upward, downward, and laterally across generations within families, with generational competition, generational solidarity, and upward- skipped generation patterns being most prominent, suggesting that these familial exchange patterns warrant more research attention than has been given in the past. We observed variation in several patterns by ancestry group. Most notably, Asian-Australian families were distinct from Anglo- or Italian-Australians in their demonstration of intergenerational solidarity, whereby all generations assume the responsibility for health encouragement. Equitable engagement by all generations in the shared process of health encouragement demonstrates communal coping (Afifi et al., 2006). Thus, Asian-Australian families may serve as a model for health encouragement patterns from a communal coping perspective. These families were also more likely to demonstrate the sandwich generation pattern, consistent with traditional practices of filial piety. Asian-Australian families could be distinct from Italian- and Anglo-Australian due to different periods of migration and, consequently, differences in acculturation. Thus, it is unclear whether these differences are a result of ancestry or acculturation.
Interestingly, we did not observe a main effect of ancestry on the presence of the skipped generation patterns in the present study (independent from intergenerational solidarity), despite previous evidence in the literature of direct exchanges between grandparents and grandchildren (Bell et al., 2018; Marcum & Koehly, 2015; Rhodes et al., 2016). However, these studies did not compare exchange patterns across ancestry groups. As well, our focus was on health encouragement rather than health information exchange, indicating that exchange patterns within families may differ by resource type.
Under the communal coping model, family disease history is conceptualized as a shared stressor among family members that would elicit collective action (e.g., encouragement of healthful behaviors; Lyons et al., 1998). When members’ health is threatened by shared risk of chronic disease, the communal coping model posits that families will mobilize healthful behaviors aimed at preventing or managing disease. The lack of an association between familial disease density and healthful eating encouragement in the current study suggests that family disease history may not be a salient factor when thinking about health behavior, or that family members are unaware of their shared risks. Future work considering the reciprocal roles of disease risk appraisals and health encouragement would elucidate the cognitive processes that underlie communal coping within families. Alternatively, this result may be attributed to a lack of sufficient variation in family disease history across the sample.
Family health history (FHH) based interventions have been shown to change how families think about their family disease history and, consequently, in activating encouragement of prevention-related behaviors (de Heer et al., 2016). Interestingly, greater familial disease density did reduce the propensity for Italian-Australian families to exhibit the sandwich generation pattern. Although encouragement patterns of Italian-Australian families tended to mirror those of Anglo-Australians, in the context of higher disease density and potential intensification of health concerns, these families may have reverted to the encouragement patterns of their culture-of-origin. Acculturation effects, measured by time since migration for example, should be examined to disentangle whether this reduction was in favor of other encouragement patterns.
The link between family disease history and health encouragement patterns is likely bidirectional. For example, Asian-Australia families’ lower disease density might be attributed to their use of intergenerational exchange patterns of health encouragement. The healthful eating encouragement patterns observed in the present study might represent long-term patterns or cultural norms that have been established over multiple generations, serving as preventive in nature and, consequently, reducing risk of chronic disease over time. Longitudinal studies assessing health encouragement over time would help to clarify directionality.
This study contributes to a larger understanding of the intergenerational interactions that can impact healthy eating within families from different ancestry groups. However, some limitations should be addressed in future research. First, the sample might include families already focused on health or who spend significant time together and therefore, may not be representative of Australian families at large. The number of families in the sample, particularly of Asian ancestry, is low, hindering generalizability and limiting statistical power. Additionally, missing perspectives from family networks could change the observed patterns of intergenerational exchange. However, this study is noteworthy in its successful recruitment of multiple family informants from three generations to delineate such patterns, yielding a relatively large sample for comparative network analysis. Finally, our measure of family disease density was based on mother-reported disease diagnoses within a family relative to the index child and does not capture individual family members’ knowledge of family disease history. Disease density also does not measure each individual’s unique disease risk, but rather, is an objective, family-level measure. Future studies assessing the longitudinal, intervention data of Families SHARE can determine the extent to which individuals’ personalized disease risk shape health encouragement and behavior.
Despite these limitations, our innovative approach utilizing a multi-informant, multigenerational design allows for a more comprehensive understanding of how families encourage healthful diets. Future research should consider which health encouragement patterns are most effective for promoting healthful eating, and other behaviors (e.g., physical activity) and attitudes. Equipped with such information and the results of the current study, interventions could be designed based on specific features of family encouragement networks found to be most effective in promoting healthful eating. These could include engaging family encouragers as interventionists, leveraging existing ties, or activating new ties within the family network. Importantly, our findings demonstrate that a one-size-fits-all approach is insufficient, and that families have a unique culture that encompasses their ancestry and shared social history, both of which may influence how resources are exchanged (Koehly et al., 2003). Generalizing this study to other societies with culturally diverse populations and migration histories would provide greater insight into health communication and behavior within families, setting the stage for the development of interventions to reduce and manage chronic disease through family support systems.
Supplementary Material
Acknowledgements:
This trial is funded by a project linkage grant between the Australian Research Council and Cancer Council SA (Project ID: LP100200549). This research was supported, in part, by funding from the Intramural Research Program of the National Human Genome Research Institute (ZIAHG20335)
References
- Afifi TD, Hutchinson S, & Krouse S. (2006). Toward a theoretical model of communal coping in postdivorce families and other naturally occurring groups. Communication Theory, 16(3), 378–409. 10.1111/j.1468-2885.2006.00275.x [DOI] [Google Scholar]
- Anikeeva O, Bi P, Hiller JE, Ryan P, Roder D, & Han GS (2012). Trends in cancer mortality rates among migrants in Australia: 1981–2007. Cancer Epidemiology, 36(2), 11–16. https://doi.org/10.1016Zj.canep.2011.10.011 [DOI] [PubMed] [Google Scholar]
- Ashida S, Kaphingst KA, Goodman M, & Schafer EJ (2013). Family health history communication networks of older adults: Importance of social relationships and disease perceptions. Health Education & Behavior, 40(5), 612–619. 10.1177/1090198112473110 [DOI] [PubMed] [Google Scholar]
- Ashida S, Wilkinson AV, & Koehly LM (2012). Social influence and motivation to change health behaviors among Mexican-origin adults: Implications for diet and physical activity. American Journal of Health Promotion, 26(3), 176–179. 10.4278/ajhp.100107-QUAN-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare. (2014). Chronic disease — Australia’s biggest health challenge. Australia’s Health 2014, 14(AUS 178), 1–11. [Google Scholar]
- Bell DC, Belli-McQueen B, & Haider A. (2007). Partner naming and forgetting: recall of network members. Social Networks, 29(2), 279–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell LK, Perry RA, & Prichard I. (2018). Exploring grandparents’ roles in young children’s lifestyle behaviors and the prevention of childhood obesity: An Australian perspective. Journal of Nutrition Education and Behavior, 50(5), 516–521. 10.1016/jjneb.2017.12.007 [DOI] [PubMed] [Google Scholar]
- Bengtson VL (2001). Beyond the nuclear family: The increasing importance of multigenerational bonds. Journal of Marriage and Family, 63(February), 1–16. [Google Scholar]
- Brashears ME, Hoagland E, & Quintane E. (2016). Sex and network recall accuracy. Social Networks, 44, 74–84. [Google Scholar]
- Brewer DD (2000). Forgetting in the recall-based elicitation of personal and social networks. Social Networks, 22(1), 29–43. [Google Scholar]
- de Heer HD, de la Haye K, Skapinsky K, Goergen AF, Wilkinson AV, & Koehly LM (2016). Lets move together: A randomized trial of the impact of family health history on encouragement and co-engagement in physical activity of Mexican-origin parents and their children. Health Education & Behavior. 10.1177/1090198116644703 [DOI] [Google Scholar]
- De La Haye K, De Heer HD, Wilkinson AV, & Koehly LM (2014). Predictors of parent-child relationships that support physical activity in Mexican-American families. Journal of Behavioral Medicine, 37(2), 234–244. 10.1007/s10865-012-9471-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ersig AL, Williams JK, Hadley DW, & Koehly LM (2009). Communication, encouragement, and cancer screening in families with and without mutations for hereditary nonpolyposis colorectal cancer: a pilot study. Genetics in Medicine : Official Journal of the American College of Medical Genetics, 11(10), 728–734. 10.1097/GIM.0b013e3181b3f42d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayslip B, & Kaminski PL (2005). Grandparents raising their grandchildren : A review of the literature and suggestions for practice. The Gerontologist, 45(2), 262–269. [DOI] [PubMed] [Google Scholar]
- Hodge AM, English DR, O’Dea K, & Giles GG (2004). Increased diabetes incidence in Greek and Italian migrants to Australia: How much can be explained by known risk factors? Diabetes Care, 27(10), 2330–2334. 10.2337/diacare.27.10.2330 [DOI] [PubMed] [Google Scholar]
- Hughes D, Hutchinson A, Prichard I, Chapman J, & Wilson C. (2015). Challenges associated with recruiting multigenerational, multicultural families into a randomised controlled trial: Balancing feasibility with validity. Contemporary Clinical Trials, 43, 185–193. 10.1016/_j.cct.2015.06.004 [DOI] [PubMed] [Google Scholar]
- Key T, Schatzkin A, Willett WC, Allen NE, Spencer EA, & Travis RC (2004). Diet, nutrition and the prevention of cancer. Public Health Nutrition, 7(1A), 187–200. 10.1079/phn2003588 [DOI] [PubMed] [Google Scholar]
- Koehly LM (2016). It’s interpersonal: Family relationships, genetic risk, and caregiving. The Gerontologist, 00(00), gnw103. https://doiorg/ 10.1093/geront/gnw103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koehly LM, Morris BA, Skapinsky K, Goergen A, & Ludden A. (2015). Evaluation of the Families SHARE workbook: an educational tool outlining disease risk and healthy guidelines to reduce risk of heart disease, diabetes, breast cancer and colorectal cancer. BMC Public Health, 75(1), 1120 10.1186/s12889-015-2483-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koehly LM, Peters JA, Kenen R, Hoskins LM, Ersig AL, Kuhn NR, ... Greene MH (2009). Characteristics of health information gatherers, disseminators, and blockers within families at risk of hereditary cancer: Implications for family health communication interventions. American Journal of Public Health, 99(12), 2203–2209. 10.2105/AJPH.2008.154096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koehly LM, Peterson SK, Watts BG, Kempf KKG, Vernon SW, & Gritz ER (2003). A social network analysis of communication about hereditary nonpolyposis colorectal cancer genetic testing and family functioning Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology, 12(4), 304–313. [PubMed] [Google Scholar]
- Laroche HH, Davis MM, Forman J, Palmisano G, Reisinger HS, Tannas C, ... Heisler M. (2009). Children’s Roles in Parents’ Diabetes Self-Management. American Journal of Preventive Medicine, 37(6 SUPPL. 1), S251–S261. 10.1016/_j.amepre.2009.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lienert J, Koehly L, Reed-Tsochas F, & Marcum CS (2019). An efficient counting method for the colored triad census. Social Networks, 58(April), 136–142. 10.1016/_j.socnet.2019.04.003 [DOI] [Google Scholar]
- Liu JH, Ng SH, Weatherall A, & Loong C. (2000). 13-Filial Piety, Acculturation, and Intergenerational Communication Among New Zealand Chinese. Basic and Applied Social Psychology, 22(3), 213–223. 10.1207/S15324834BASP2203_8 [DOI] [Google Scholar]
- Lyons RF, Mickelson KD, Sullivan MJL, & Coyne JC (1998). Coping as a communal process. Journal of Personal and Relationships, 15(June 2016), 579–605. 10.1177/0265407598155001 [DOI] [Google Scholar]
- Marcum CS, & Koehly LM (2015). Inter-generational contact from a network perspective. Advances in Life Course Research, 24, 10–20. 10.1016/_j.alcr.2015.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Bowen D, Brody LC, Condit CM, Croyle RT, Gwinn M, ... Valente TW (2010). Future health applications of genomics. Priorities for communication, behavioral, and social sciences research. American Journal of Preventive Medicine, 38(5), 556–565. 10.1016/_j.amepre.2010.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mente A, de Koning L, Shannon HS, & Anand SS (2009). A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med, 169(7), 659–669. 10.1001/archinternmed.2009.38 [DOI] [PubMed] [Google Scholar]
- Miller DA (1981). The “sandwich” generation: Adult children of the aging. Social Work, 26(5), 419–423. [Google Scholar]
- Palmquist AEL, Koehly LM, Peterson SK, Shegog M, Vernon SW, & Gritz ER (2010). “The cancer bond”: Exploring the formation of cancer risk perception in families with Lynch Syndrome. Journal of Genetic Counseling, 19(5), 473–486. 10.1007/s10897-010-9299-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putney NM, & Bengtson VL (2003). Intergenerational relations in changing times In Mortimer JT & Shanahan MJ (Eds.), Handbook of the Life Course. New York: Klewer Academic/Plenum Publishers. [Google Scholar]
- Rhodes K, Chan F, Prichard I, Coveney J, Ward P, & Wilson C. (2016). Intergenerational transmission of dietary behaviours: A qualitative study of Anglo-Australian, Chinese- Australian and Italian-Australian three-generation families. Appetite, 103(November), 309–317. 10.1016/_j.appet.2016.04.036 [DOI] [PubMed] [Google Scholar]
- Skapinsky KF, Persky S, Lewis M, Goergen A, Ashida S, De Heer HD, ... Koehly LM (2018). Heart disease risk information, encouragement, and physical activity among Mexican-origin couples: Self- or spouse-driven change? Translational Behavioral Medicine, 5(1), 95–104. 10.1093/tbm/ibx012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlqvist ML (2002). Asian migration to Australia: food and health consequences. Asia Pacific Journal of Clinical Nutrition, 11 Suppl 3(April), 18–19. 10.1046/j1440-6047.11.supp3.13.x [DOI] [PubMed] [Google Scholar]
- Williams KP (2007). Kin Keeper. Journal of Human Behavior in The Social Environment, 15(2/3), 291–305. 10.1300/J137v15n02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson CJ, de la Haye K, Coveney J, Hughes DL, Hutchinson A, Miller C, ... Koehly LM (2016). Protocol for a randomized controlled trial testing the impact of feedback on familial risk of chronic diseases on family-level intentions to participate in preventive lifestyle behaviors. BMC Public Health, 16, 1–11. 10.1186/s12889-016-3623-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2014). Global status report on noncommunicable diseases 2014. World Health Organization; https://doi.org/ISBN9789241564854 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.