Abstract
Since 2018 and currently in 2019, the United States and Canada experienced a rapidly spreading measles virus outbreak. The developing outbreak may be due to a lack of vaccination, an inadequate dosage of measles (MMR) vaccine, clusters of intentionally under-vaccinated children, imported measles from global travel, and from those who are immunocompromised or have other life-threatening diseases. The infection originated mainly from travelers who acquired measles abroad and has thus led to a major outbreak and health concern not only in the United States and Canada but also in other parts of the world. According to World Health Organization, from January 2019 through September 2019, 1234 cases of measles have been reported in the United States and 91 reported cases in Canada, while in 2018, 372 and 28 cases were reported in the United States and Canada, respectively. A potential driving factor to the increased cases maybe because fewer children have been vaccinated over the last number of years in both countries. This article is a narrative review of cases discussing the measles outbreak among partially vaccinated and unvaccinated children and adults in the United States and Canada in 2018 and 2019.
Keywords: measles, child, adult, vaccination, disease outbreaks, United States, Canada
What do we already know about this topic?
Since 2018 and currently in 2019, the United States and Canada are experiencing a rapidly spreading measles virus outbreak. The developing outbreak may be due to a lack of vaccination, an inadequate dosage of measles (MMR) vaccine, clusters of intentionally under-vaccinated children, imported measles from global travel, and from those who are immunocompromised or have other life-threatening diseases. The infection originated from travelers who acquired measles abroad and brought it back to the United States and Canada. This has lead to a major outbreak and health concern globally.
How does your research contribute to the field?
This review confirms that the cases of measles infection are higher among the unvaccinated population, which consists mainly of children defined as 18 years of age and below, or below 18 years of age depending on the source age classification. The majority of measles outbreaks currently in the United States and Canada are due to unvaccinated individuals who have been in contact with the viral particle.
What are your research’s implications toward theory, practice, or policy?
To contain the disease and prevent future outbreaks, we would recommend that all children, travelers, and susceptible individuals be vaccinated with the MMR vaccine. The recent spike in vaccine deterrence, coupled with the increase in international travel, has created the perfect circumstance for the disease to enter into areas where it was once considered eliminated, such as the United States and Canada. Anti-vaccination groups should be met with a public health awareness campaign to sensitize people and counter the unfounded arguments against vaccination.
Introduction
Measles is an airborne communicable disease that spreads rapidly through aerosolized respiratory droplets.1 It is caused by the measles virus; a spherical, nonsegmented, enveloped, negative-sense single-stranded RNA virus who is a member of the genus Morbillivirus within the family Paramyxovirus.1,2 Humans are the only hosts of the measles virus.3 The main virulence of the measles virus is the transmembrane hemagglutinin and fusion glycoproteins found in the envelope of the virus.4 Paramyxovirus also causes parainfluenza (croup), respiratory syncytial virus (RSV) and mumps, but with measles being the most contagious out of all of them.2
The measles virus is a highly infectious disease with a 90% secondary attack rate among immunocompromised individuals and unvaccinated populations. This virus can survive at least 2 hours in droplet form, with airborne particles causing a continual presence of the virus in the air and on environmental surfaces.5 Measles, also known as Rubeola or the 10-day measles, causes a viral exanthem or skin rash.6 Initial symptoms include cough, coryza, and conjunctivitis leading to a high fever and blue-white Koplik spots on the buccal mucosa, which within 2 to 3 days later is followed by a maculopapular rash that starts on the head and neck and then spreads downward.1 Symptoms can appear 7 to 18 days after the initial exposure to the virus but can appear as late as 19 to 21 days from exposure. Complications such as otitis media and pneumonia occur in about 6% to 7% of reported cases.5 Other possible sequelae of measles may include croup, subacute sclerosing panencephalitis, or blindness.6 Measles encephalitis occurs in about 1 of every 1000 reported cases. Lack of vaccination against the measles virus is the leading cause of preventable deaths in children worldwide.5 Measles can be prevented with the MMR (measles, mumps, and rubella) vaccine.3 A single dose of the MMR vaccine is not adequate to protect against the measles outbreak with morbidity and mortality; therefore, a second dose is crucial for effective measles control.7 The first dose should be administered to children aged 12 to 15 months, which is effective in preventing 93% of measles, and the second dose should be administered after age 4 to 6 years or at least 28 days after the first dose, which would then make it 97% effective.3 Post high school students who have not been vaccinated should also receive 2 doses of the MMR vaccine, with the second one at least 28 days after the first dose. Adults born after 1957, who did not get the vaccine as a child, should get at least 1 dose of the MMR vaccine.3
Although the measles virus is serologically monotypic, genetic analysis of the wild-type nucleotide sequences has determined that there are 8 clades (A-H), which have been divided into 25 genotypes.8 The number of clades has remained the same since 1998, yet the number of genotypes within each has increased.9 Clades A, E, and F all have a single genotype, while clades B, C, D, G, and H have multiple genotypes.10 The current vaccine strains have shown that they were derived from a single genotype, genotype A.3
Measles virus genotyping has a crucial part to play in following and tracking of transmission routes during outbreak investigations. Genotyping results can help find connections between different cases.3 It is a way to differentiate the cases if a patient has a wild-type measles infection or a reaction to a recent vaccination.11 Also, the measles virus genotyping may be able to aid in determining which foreign country could be the cause of an imported US case.12 Transmission chain tracking by genotyping can be done in combination with other epidemiologic factors including, but not limited to, travel histories, exposure histories, and other characteristics to help narrow down the location of cause.8
The Centers for Disease Control and Prevention (CDC) in 1978 had a goal to eradicate measles globally by using vaccinations.3 In the year 2000, in the United States, measles was declared eliminated due to the absence of continuous disease for greater than 12 months. This quickly changed with an increase in the number of travelers who got measles abroad and brought it back to both Canada and the United States, or in communities that are unvaccinated.3 World Health Organization (WHO) regions over the globe are experiencing a pandemic with the recent measles outbreaks.13 Africa has had 134 494 reported cases of measles between 2018 to early 2019, with 2013 deaths caused by this virus within this time frame. South America has also experienced an increase in measles reporting from 2018 to early 2019 with 16 173 confirmed cases and 88 deaths. Measles outbreak in France began in 2017 with 2913 confirmed cases and no deaths recorded, but have now declined due to mandatory vaccination for all children born after January 1, 2018. Serbia, like France, started seeing an increase in measles cases in 2017 with 5076 and has acknowledged this to be the largest outbreak in 25 years. Ukraine has had one of the highest incidences of a measles outbreak, with 80 618 reported cases since 2017. Between January 1, 2019, and February 18, 2019, 8400 cases of measles have been reported in the Philippines and 130 deaths within that same time frame.13 In 2018, there were 372 reported cases in the United States and 1234 measles cases from January 2019 through September 2019.3 In 2019, there have been 91 reported cases of measles through the end of September in Canada.5 The purpose of this article is to review the outbreak of measles in unvaccinated and partially vaccinated children and adults in the United States and Canada in 2018 and 2019.
Method
An electronic literature review search was performed on PubMed, Google Scholar, and MedLine Plus. The search was limited to peer-reviewed articles published from January 1, 1979, until October 09, 2019, for the compiled U.S. and Canada data. The articles were selected if it included keywords such as measles, child and public health, infectious disease, child vaccination, vaccine hesitancy and refusal, elimination, and the prevalence of the outbreak in the United States and Canada within 2018 and 2019. Articles were then reviewed and included based on the applicability to the topic.
Review of Measles Cases in Unvaccinated or Partially Immunized Children: An Ongoing Outbreak in the United States and Canada
For this study, a total of 40 articles were retrieved and utilized for the references, among which 8 articles were used for case analysis of reported cases in the United States and Canada. This study included unvaccinated children below 18 years of age, partially immunized people who were not able to receive the two recommended doses of MMR at age 12 to 18 months and between 4 to 6 years of age, also an uncategorized age group which might include adults.14 The data presented in this study reflect the total reported cases at that specific time when this review was conducted, but the total number of cases might differ as the data get updated. Another important point to keep in mind is that these data were collected from several sources and the reported criterion among these sources varies. Each county/neighborhood uses different data parameters to report the number of measles cases detected.
The refusal to vaccinate is considered one of the top 10 global health threats to contracting measles. The reason for vaccination hesitancy is multifactorial, but the 2 main ones are having a lack of confidence in the health care provider and difficulty to access vaccines despite the worldwide availability of vaccines.15 The percentage of unvaccinated children has quadrupled since 2001, with most of them having had no vaccination and millions more only receiving some crucial shots.16 Based on one of the studies done on primary school children, to analyze the main reasons for vaccine refusal, about 47% of parents refused to vaccinate their children.17 Parents’ preference to have the vaccination done by their general physician accounted for most of the refusals, followed by autism and bowel disorders thought to be associated with vaccines, vaccination side effects, or only the parents wish to have a single vaccine done.17
Another study done by Phadke and colleagues also showed that 41.8% of cases of measles reported were from unvaccinated children due to nonmedical exemptions.18 However, vaccine refusal was not the only reason behind the outbreaks of these vaccine-preventable diseases. There were different trends noticed with vaccine refusal by diseases, such as a higher prevalence of measles cases than pertussis, as specifically seen in this study.18
Measles Surveillance Data
It is crucial to identify the suspected cases of measles through surveillance data to control the disease. Unfortunately, the number of reported cases per state does not reflect the actual number of cases occurring in the community, as many people do not seek health care and never get diagnosed.
United States of America—Measles Outbreaks in 2018 and 2019
The numbers of cases seen in Table 1 are laboratory-confirmed cases from WHO. Measles outbreaks are depicted by month and year. The data ranged from January 2018 to September 2019. A total of 28 confirmed cases in the year 2018 and 91 cases in the year 2019 in Canada were reported to WHO thus far. A total of 372 confirmed cases in 2018 and 1234 cases in 2019 in the United States were reported to WHO.9 This case count is preliminary and will continue to change with the ongoing outbreak. It should also be kept in mind that the cases are reported at irregular intervals, providing multiple months of data in 1 month. Moreover, future months are reported as 0 and are updated, as data becomes available.
Table 1.
Measles Reported Cases in the United States of America and Canada in 2018 and 2019.
| Country | Year | Month |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep | Oct | Nov | Dec | ||
| USA | 2018 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 372 |
| USA | 2019 | 52 | 154 | 181 | 317 | 277 | 114 | 69 | 70 | 0 | — | — | — |
| Canada | 2018 | 1 | 2 | 1 | 4 | 5 | 4 | 2 | 2 | 3 | 1 | 2 | 1 |
| Canada | 2019 | 7 | 15 | 18 | 10 | 19 | 9 | 8 | 5 | 0 | — | — | — |
Source. Data source from WHO updated on October 8, 2019.9
Note. World Health Organization (WHO) reported measles cases that were laboratory confirmed.
New York—Rockland County measles outbreak in children (age ≤ 18) who are unvaccinated, partially vaccinated, and/or of unknown MMR vaccination status
According to the CDC from January 1 to October 3, 2019, there has been a total of 1250 individual cases of measles that have been confirmed in 31 states as the reporting period for 2019 began on December 30, 2018.19 As of September 25, 2019, there are 312 confirmed and reported cases of measles in Rockland County.20 The outbreak was declared over on September 25, 2019.
Vaccination rates for confirmed measles cases in Rockland County
79.5% have had 0 MMRs
5.8% have had 1 MMRs
3.2% have had 2 MMRs
11.5% of unknown status
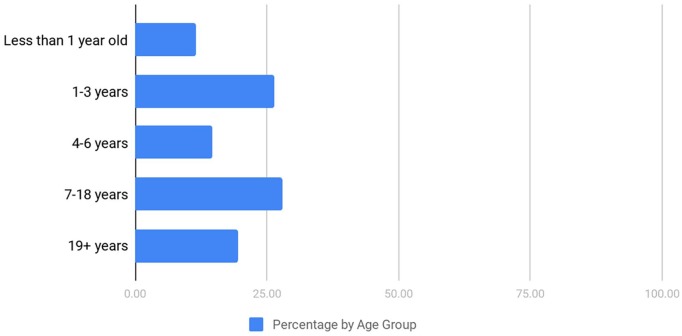
As depicted in Figure 1, 312 of the total number of measles cases were reported at Rockland County. Most of the cases were of unvaccinated persons, which accounts for 79.5% of the cases that were reported. According to the Rockland County report of September 25, 2019, the measles cases were as a result of unvaccinated persons being exposed to international travelers who have measles.19
Figure 1.
Age groups of confirmed measles cases in Rockland County.
Note. Data source from Rockland County: 2018-2019 measles outbreak in Rockland County.19
New York—Brooklyn measles outbreak in children (age < 18) and adult age population who are unvaccinated, partially vaccinated, and/or of unknown MMR vaccination status
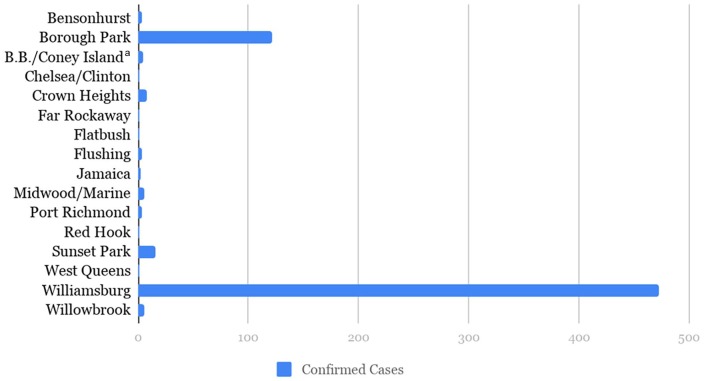
In Brooklyn, there have been 649 confirmed cases of measles as of September 3, 2019, and within a window, from September 2018 and August 2019.20 The first case of measles was diagnosed in a child who contracted the disease while on a visit to Israel.21 There have been additional people who acquired measles without any recent travel history.
The data in Figure 2 represents the cases that were reported in different neighborhoods of New York City. Out of a total of 649 cases, 525 were children below 18 years of age, and 124 were 18 years and over. Of the 525 that were children, 472 were unvaccinated, 40 had 1 prior MMR vaccine, 11 had 2 prior MMR vaccines and 2 were unknown. The measles outbreak in the Orthodox Jewish community accounts for 285 cases since it began in October 2018.22
Figure 2.
The number of confirmed cases in Brooklyn by neighborhood.
Note. Data source from NYC Health.20 Updated on October 9, 2019.
aBrighton Beach/Coney Island.
Washington—Clark County, Pierce County, Snohomish County, and King County measles outbreak in children (age ≤ 18) and adult age population who are unvaccinated, partially vaccinated, and/or of unknown MMR vaccination status
There have been a total of 86 outbreaks in Washington State as of August 19, 2019. Of these cases, 71 were reported in Clark County, 12 cases in King County, 2 cases in Pierce and 1 case in Snohomish. It was noted that 71 of the cases were children 18 years of age and below and most of them never received the MMR vaccination as indicated in Table 2.23 The outbreak was declared over on August 28, 2018.
Table 2.
The number of confirmed cases in Washington State and Vaccination status.
| Age range (in years) | Number of cases |
|---|---|
| Below 1 year | 2 |
| 1-10 years | 52 |
| 11-18 years | 17 |
| 19-29 years | 3 |
| 30-39 years | 5 |
| 40-49 years | 4 |
| 50-59 years | 3 |
| Vaccination status (confirmed cases) | Total |
| 0 doses | 66 |
| 1 dose | 5 |
| 2 or more doses | 4 |
| Unknown | 11 |
Note. Data source from Washington State Department of Health. Updated on October 9, 2019.23
New Jersey—Ocean County and Monmouth County measles outbreak in unreported age group(s) and of unknown MMR vaccination status
There were 19 cases reported in Ocean County and Monmouth County, New Jersey, combined as of October 3, 2019. These cases were linked to certain locations that people were exposed to during that period.24
California State—measles outbreak in children (age < 18) and adult age population who are unvaccinated, partially vaccinated, and/or of unknown MMR vaccination status
In 2019, 4 out of 5 outbreaks in California were linked to international travel. As of October 9, 2019, there were 70 confirmed cases in California.25 The current cases from different counties are shown in Table 3.25
Table 3.
Total Reported Measles Cases in California State in 2019.
| County | Total cases | Pediatric cases (< 18 years) | Adult cases (18 years or older) |
|---|---|---|---|
| Alamedaa | 1 | 0 | 1 |
| Los Angelesb | 20 | 3c | 17 |
| Orange | 5 | 2 | 3 |
| Placer | 3 | 2 | 1 |
| Sacramento | 3 | 2 | 1 |
| San Bernardino | 2 | 1 | 1 |
| San Diego | 2 | 1 | 1 |
| San Francisco | 1 | 0 | 1 |
| San Mateo | 6 | 1 | 5 |
| Santa Barbara | 2 | 0 | 2 |
| Santa Clara | 5 | 1 | 4 |
| Santa Cruz | 1 | 0 | 1 |
| Others | 19 | 3 | 16 |
| Total | 70 | 16 | 54 |
Note. Data source from California Public Health Department, 2019 on measles outbreak by county.25
Alameda County includes 2 health departments that report cases separately: Alameda County and Berkeley City.
Los Angeles County includes 3 health departments that report cases separately: Los Angeles County, Pasadena City, and Long Beach City.
The rash onset for one of these patients occurred in late December 2018.
Canada Weekly Reported Measles Cases in Children and Adult Age Group(s) in 2018-2019
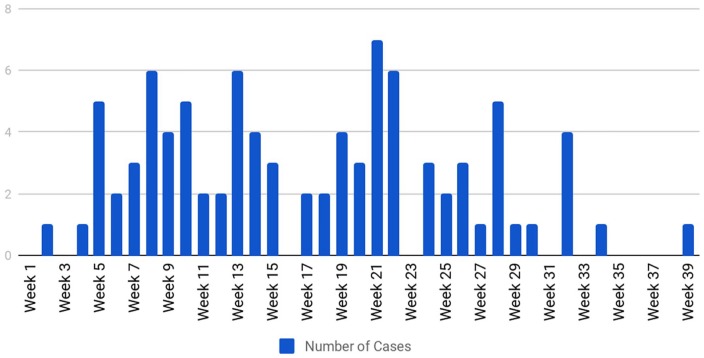
Measles outbreaks in Canada arose mainly due to people traveling abroad and being exposed to measles.26 Unvaccinated children are more prone to acquire measles infection. The most commonly reported age group is 10 to 14 years.27 There have been few outbreaks of measles in Canada over the past years, which raises the concern for high measles coverage. Immigration is a huge risk factor, which directly correlates with the number of cases observed in Canada,26 thus making it more challenging to eliminate measles from Canada.27
It should be kept in mind that the measles data reported by the Government of Canada are based on weekly terms rather than monthly, as in the United States, and they also use different data parameters to report their cases. The data in Figure 3 represent the number of reported measles cases by the onset of rash in Canada between December 30, 2018 (week 1) and September 28, 2019 (week 39).28 As shown in Figure 3, the number of measles cases has been increasing compared with previous data years from the CDC. The first reported case in 2019 happened on week 2 from January 6, 2019, to January 12, 2019. The reported case during week 2 happened in the province of British Columbia, which reported to have been imported from the Philippines. Subsequently, on week 4, 1 case of measles was reported in the province of British Columbia, involving a traveler returning from Vietnam.
Figure 3.
The number of measles cases reported in Canada in the year 2019 by week of rash onset.
Note. Data source from the Government of Canada Measles Cases by Week of Rash Onset Reports in 2019. The reported weeks are as follows: week 1 (December 30, 2018, to January 5, 2019), week 2 (January 6, 2019, to January 12, 2018), and so on.28
Between January 27, 2019, and February 2, 2019 (week 5), there were a total of 5 reported cases when the onset of rash occurred. Two of the reported cases happened in the province of Quebec, where one of them was acquired while traveling through Poland, and the other through Ukraine.28 The remaining 3 cases happened in the province of British Columbia, where 1 of them was acquired while traveling through the Philippines and the other 2 through Vietnam. According to an article published in the Montreal Gazette, inadequate vaccination has been identified as a common factor in individuals affected by the recent measles outbreak in Canada.29 Interestingly, it is important to note that recent statistical data, from 2016 to 2017, indicates that as many as 82% of primary school children were vaccinated against measles, whereas 88% of high school students in Quebec were vaccinated against measles.30
In week 6, from February 3, 2019, to February 9, 2019, there were a total of 2 reported cases.28 One of the suspected cases happened in the province of British Columbia without any previous travel history. In weeks 7 to 9, there were a total of 13 cases reported. Most of these cases happened in the province of British Columbia, which were linked to school-related cluster outbreaks.28 Based on a news article during that period, there have been 8 confirmed cases of measles at Ecole Secondaire Jules-Verne and Ecole Rose-des-Vents who had a 70% rate of measles vaccination.31
In weeks 10 and 11, there were a total of 7 reported cases and 5 of these cases happened in the province of British Columbia, 1 in Alberta, and 1 in Quebec.28 In week 12, 2 cases were reported. One of the patients had a reported travel history to Oregon and the other patient had a recent travel history to Bangladesh.
In weeks 13 to 16, there were a total of 13 reported cases of measles. Four of the reported cases happened in the province of Ontario that was imported from Pakistan, Bangladesh, and East Asia. Seven of the other cases happened in the province of British Columbia and was contacted while traveling through Vietnam. The remaining 2 cases were reported in Alberta and Quebec.
In weeks 17 to 19, there were 8 reported cases of measles. Two of the cases in week 17 were from the province of British Columbia and New Brunswick. The case in British Columbia was acquired while traveling to several countries in Asia, whereas that of New Brunswick was acquired while traveling to several countries in Europe. For the 2 cases reported in week 18, the first case reported from the province of Québec was exposed to an unknown source but reported recent travel to France. The second case was reported from the province of Ontario and was acquired while traveling to the Philippines. For the 4 cases reported in week 19, the first case reported from the province of New Brunswick is linked to an earlier case that had recent travel to several countries in Europe and for the second and third cases reported from the province of Ontario, one was acquired while traveling to the Philippines, and the other was acquired while traveling to the United States. The fourth case was reported in the province of Quebec.28
In week 20, from May 12, 2019, to May 18, 2019, there were a total of 3 reported cases.28 One of the cases happened in the province of Alberta with a recent travel history to Vietnam. The second case was reported in the province of Ontario with a recent trip to France/Germany. The last case was reported in the province of Quebec.
In weeks 21 to 25, there were 18 reported cases of measles. Seven of the cases in week 21 were from the province of New Brunswick that was acquired from a previously reported case in New Brunswick. For the 6 cases that were reported in week 22, 3 were from the province of New Brunswick and the other 3 were from Alberta, Quebec, and Ontario, respectively. Two of which were linked to recent travel to Vietnam. There were no cases reported in week 23, but 3 cases were reported in week 24 and 2 in week 25. Two of which were linked to recent travel to the United States and India.
In weeks 26 to 30, there were 11 reported cases of measles. The majority of these cases were reported by the province of Quebec that was acquired as part of an ongoing outbreak in the greater Montreal area that began on June 2019.28 One of the cases reported by the province of British Columbia was acquired while traveling through the Philippines.
Finally, from weeks 31 to 39, there were 6 reported cases of measles. Four cases were reported in week 32 by the province of Quebec. The first case was exposed either in Quebec or while traveling to New York State. The second and third cases had no history of travel outside of Quebec, but are from the same community as the first case. The fourth case was exposed while traveling to Cambodia.28 The remaining 2 cases were reported in week 34 and week 39 in the province of Quebec.
Overall, there has been a total of 112 measles cases reported across Canada. The majority of these cases were reported in the provinces of British Columbia, New Brunswick, Ontario, and Quebec.28 According to the Government of Canada, 22 cases were omitted due to the missing date of rash onset.
Discussion
One of the main tools used in preventative medicine to mitigate the burden of diseases and protect the population from diseases is immunization through the administration of vaccines. The global use of vaccines has immensely decreased and in some cases completely eradicated the incidence and spread of childhood diseases.18 One example of eradication is the case of smallpox. Despite its overwhelming impact on the human population,32 widespread vaccination efforts eradicated the disease by 1977, thus eliminating smallpox as a threat to the human population.32-34 Another example is polio, which has been almost eradicated worldwide thanks to WHO’s polio eradication initiative.35 Despite the evidence-based rationale behind the benefits of vaccines, as a tool to provide immunity against diseases, there has been opposition to the use of vaccines.36 Some of these alternate views are based on personal, religious, or cultural sentiments that believe that vaccines can cause more harm than good in people who receive them. Individuals who depend solely on herd immunity fail to recognize that reduced immunization within a population leads to weak herd immunity, which consequently leads to an increase in vaccine-preventable disease processes and outcomes. Studies have shown that a 96% to 99% vaccination rate is required to preserve herd immunity.36 The recent global pandemic outbreak of measles infection has been linked to individuals who either did not receive the measles vaccine or failed to complete the recommended dosage of the vaccine to confer adequate immunity against measles infection.37 It is important to note that although vaccination is important to curtail the spread of measles, studies have shown that vaccinated individuals could be at risk due to vaccine failure. One particular study shows that when vaccine failure occurs, in previously vaccinated individuals within a community, an outbreak or introduction of measles virus in such community will lead to an increased spread and propagation of the virus and measles infection among susceptible individuals.38
The recent outbreak of measles infection has created an urgency that prompted public health officials, government officials, researchers, clinicians, media and the general population to opt for urgent solutions. It is of concern that the longer the pandemic lasts, the more likely the disease’s resurgence will become a global epidemic, due to its ease of transmission through aerosolized respiratory droplets and the exponential rate of international travel.13 According to the CDC, this alarming figure has been linked to individuals who visited countries like Ukraine, with a recorded incidence of measles infection of over 80 000 since 2017. It is important to note that although the recent outbreak (2019) is the largest in the United States, there have been other outbreaks of lesser magnitude. For instance, there were 11 outbreaks in 2013 with one of them having 58 cases, and in 2014 there were 23 measles outbreaks with one large outbreak having more than 350 cases. In 2018, 82 individuals imported measles into the United States from other countries resulting in a total of 17 outbreaks and 372 confirmed cases in the United States.39 Among the 17 outbreaks, 3 were seen in the states of New York and New Jersey; these were associated with unvaccinated travelers returning from Israel, which is experiencing an ongoing outbreak.40 This is the largest number of imported cases since 2000 when measles was at its lowest rate in the United States.13
Measles is still very common in some regions of the world such as in Africa, Asia, Europe, and the Pacific, and as studies have shown, travelers infected by the virus import the virus into other regions where the virus has been reintroduced, such as the United States. When the airborne virus reaches under-vaccinated communities in these regions, it spreads rapidly via aerosolized respiratory droplets creating a cascade of events that leads to the widespread of measles infection.37
The resurgence of widespread measles infection is not limited to the United States, as other countries are now seeing resurgence. In Canada, the number of outbreaks directly correlates with the influx of economic migrants from regions where measles is endemic.26 This factor is a sole operant that challenges the complete elimination of measles infection in Canada. Between December 2018 and through the end of September 2019, 112 cases have been reported in Canada and these cases were reported in travelers from the Philippines, Vietnam, Poland, Ukraine, Japan, and the United States.28 The virus can remain viable in the air for approximately 2 hours and unvaccinated individuals have an approximately 90% chance of contracting the disease with the potential of affecting 9 to 18 other people.37 Other countries, like Venezuela and several countries in Europe where endemic measles transmission had been previously abated, have seen a resurgence in reported cases, which will likely lead to the reestablishment of endemic measles crisis. Measles has plagued human populations for decades with infection characterized by malaise, fever, conjunctivitis, cough, rash, and coryza. With effective treatment, most people will recover from measles infection, yet approximately 100 000 people die from measles per year globally.37 Despite the widespread use of vaccines, measles is the leading cause of vaccine-preventable illness and deaths among global cases.13
Conclusion
This review indicates that the risk of occurrence for measles infection correlates with an elevated risk in unvaccinated populations, and in this subset, the risk seems particularly higher in children 18 years of age and below, or below 18 years of age. Of course, further studies must be conducted to gain a proper visual of the vaccination’s true impact. Measles infection among unvaccinated individuals is associated with the majority of measles outbreaks in the United States and Canada. We can derive from statistics and evidence that vaccination successfully subdues the prevalence of the disease. To contain the disease and prevent future outbreaks, we would recommend that all children, travelers, and susceptible individuals be vaccinated with the MMR vaccine based on their national medical recommendations and guidelines. In the United States, most schools and daycares require children to be immunized. University students, health care workers, travelers, and other susceptible groups should also be vaccinated to achieve success. The recent spike in vaccine deterrence, coupled with the increase in international travel, has created the perfect circumstance for the disease to enter into areas where it was once considered eliminated, such as the United States and Canada. The general public’s distrust of vaccines needs to be met with medically backed information that allows them to make better-informed decisions, based on global statistics and trends. Vaccines have become a controversial issue and owing to this controversy, mandatory vaccinations would usually be met with opposition. Anti-vaccination groups should be met with a public health awareness campaign to sensitize people and counter the unfounded arguments against vaccination. In countries such as France, where vaccines have become mandatory, the implementation has successfully lowered the incidence rate of measles. Although France has one of the highest rates of incidences among the European countries, this decrease in outbreaks should be further studied and a cause identified across various age groups. Vaccinating school-aged children in France had a perceived impact on the incidence rate among the general population; expanding vaccinations to also include susceptible adults could potentially have an even greater impact. Through identifying positive impacts such as immunization, and implementing them, a large shift can be replicated in other nations.
Footnotes
Author Contributions: A.S.: Conceptualization, and design, approval of the final version, responsibility for accuracy, and integrity of all aspects of research. C.O.: Supervision and revising the article for intellectual content; editing. A.M.: Writing—review and editing; project administration. O.A.: Writing—review and editing. A.F.A.: Writing—review and editing. S.P.: Writing—review and editing. J.G.: Writing—review and editing. S.Y.: Writing—review and editing. J.M.: Writing—review and editing. H.C.: Writing—review and editing.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Adekunle Sanyaolu  https://orcid.org/0000-0002-6265-665X
https://orcid.org/0000-0002-6265-665X
References
- 1. Naim HY. Measles virus. Hum Vaccin Immunother. 2014;11(1):21-26. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4514292/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Scott. Science Direct. 2017. https://www.sciencedirect.com/topics/neuroscience/measles-virus.
- 3. CDC. 2018. https://www.cdc.gov/measles/hcp/index.html.
- 4. Public Health Agency of Canada. 2011. https://www.canada.ca/en/public-health/services/laboratory-biosafety-biosecurity/pathogen-safety-data-sheets-risk-assessment/measles-virus.html.
- 5. Government of Canada. 2019. https://www.canada.ca/en/public-health/services/diseases/measles.html.
- 6. Stanford Children’s Health. 2019. https://www.stanfordchildrens.org/en/topic/default?id=rubeola-measles-90-P02543.
- 7. Strebel P, Cochi S, Grabowsky M, et al. The unfinished measles immunization agenda. J Infect Dis. 2003;187(1):S1-S7. doi: 10.1086/368226. [DOI] [PubMed] [Google Scholar]
- 8. CDC. 2019. Retrieved from http://www.cdc.gov/measles/lab-tools/genetic-analysis.html
- 9. World Health Organization. Measles and Rubella surveillance data. 2019. https://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/active/measles_monthlydata/en/.
- 10. Riddell MA, Rota JS, Rota PA. Review of the temporal and geographical distribution of measles virus genotypes in the pre-vaccine and post vaccine eras. Virol J. 2005;2:87 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1318492/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bellini WJ, Rota JS, Rota PA. Virology of measles virus. J Infect Dis. 1994;170(Suppl 1):S15-S23. https://www.ncbi.nlm.nih.gov/pubmed/7930749. [DOI] [PubMed] [Google Scholar]
- 12. Rota PA, Brown K, Mankertz A, et al. Global distribution of measles genotypes and measles molecular epidemiology. J Infect Dis. 2011;204(Suppl_1):S514-S523. https://academic.oup.com/jid/article/204/suppl_1/S514/2194335. [DOI] [PubMed] [Google Scholar]
- 13. CDC. 2019. https://www.cdc.gov/globalhealth/measles/globalmeaslesoutbreaks.htm.
- 14. Tanne JH. Measles: two US outbreaks are blamed on low vaccination rates. Br Med J. 2019;364:l312. doi: 10.1136/bmj.l312. [DOI] [PubMed] [Google Scholar]
- 15. The World Health Organization. Ten threats to global health in 2019. 2019. https://www.who.int/emergencies/ten-threats-to-global-health-in-2019.
- 16. The New York Times. How to inoculate against anti-vaxxers. 2019. https://www.nytimes.com/2019/01/19/opinion/vaccines-public-health.html.
- 17. Hadjikoumi I, Niekerk KV, Scott C. MMR catch up campaign: reasons for refusal to consent. Arch Dis Child. 2006; 91(7):621 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2082853/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Phadke VK, Bednarczyk RA, Salmon DA, Omer SB. Association between vaccine refusal and vaccine-preventable diseases in the United States: a review of measles and pertussis. JAMA. 2016; 315(11):1149-1158. https://www.ncbi.nlm.nih.gov/pubmed/26978210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rockland County. 2018-2019 Measles outbreaks in Rockland County. 2019. http://rocklandgov.com/departments/health/measles-information/.
- 20. NYC Health. Recent infections in Brooklyn. 2019. https://www1.nyc.gov/site/doh/health/health-topics/measles.page.
- 21. NYC Health. Health department warns Orthodox Jewish community of increase in measles cases. 2019. https://www1.nyc.gov/site/doh/about/press/pr2018/pr084-18.page.
- 22. NYC Health. Health department issues commissioner’s orders to all Yeshivas in Williamsburg to exclude unvaccinated students or face violations and possible closure. 2019. https://www1.nyc.gov/site/doh/about/press/pr2019/commissioner-orders-all-yeshivas-to-exclude-unvaccinated-students.page.
- 23. Washington State Department Health. Measles outbreak 2019. 2019. https://www.doh.wa.gov/YouandYourFamily/IllnessandDisease/Measles/MeaslesOutbreak.
- 24. State of New Jersey Department Health. 2019 measles outbreak, Ocean County. 2019. https://www.state.nj.us/health/cd/topics/measles.shtml.
- 25. California Department of Public Health. Measles outbreak. 2019. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/Immunization/measles.aspx.
- 26. Crowcroft NS. The challenges of sustaining measles elimination in Canada. Can Commun Dis Rep. 2014;40(12):261-264. doi: 10.14745/ccdr.v40i12a07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sherrard L, Hiebert J, Cunliffe J, Mendoza L, Cutler J. Measles surveillance in Canada: 2015. Can Commun Dis Rep. 2016;42(7):139-145. doi: 10.14745/ccdr.v42i07a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Government of Canada. Measles and Rubella weekly monitoring reports 2019. 2019. https://www.canada.ca/en/public-health/services/diseases/measles/surveillance-measles/measles-rubella-weekly-monitoring-reports-2019.html.
- 29. Montreal Gazette. Montreal measles alert underscores need to vaccinate, authorities say 2019. 2019. https://montrealgazette.com/news/local-news/montreal-measles-alert-underscores-need-to-vaccinate-authorities-say.
- 30. Sate et Services Sociaux Québec. Immunization coverage data in Quebec 2019. 2019. http://www.msss.gouv.qc.ca/professionnels/vaccination/piq-impacts-des-programmes-de-vaccination/donnees-de-couverture-vaccinale-au-quebec/.
- 31. CBC. B.C. measles outbreak: 33 students, staff ordered to stay home from schools 2019. 2019. https://www.cbc.ca/news/canada/british-columbia/bc-measles-outbreak-33-students-staff-stay-home- 15025834. [Google Scholar]
- 32. Bradford A. Smallpox: the world’s first eradicated disease. 2019. https://www.livescience.com/65304-smallpox.html.
- 33. World Health Organization. The global eradication of smallpox: final report of the Global Commission for the Certification of Smallpox Eradication, Geneva, December 1979. 1980. https://apps.who.int/iris/handle/10665/39253.
- 34. Behbehani AM. The smallpox story. Pediatr Infect Dis J. 1984;3(3):289. [Google Scholar]
- 35. Plotkin S. History of vaccination. Proc Natl Acad Sci. 2014;111(34):12283-12287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hussain A, Ali S, Ahmed M, Hussain S. The anti-vaccination movement: a regression in modern medicine. Cureus. 2018;10(7):e2919. doi: 10.7759/cureus.2919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Paules CI, Marston HD, Fauci AS. Measles in 2019—Going backward. N Engl J Med. 2019;380(23):2185-2187. doi: 10.1056/NEJMp1905099. [DOI] [PubMed] [Google Scholar]
- 38. Sugerman DE, Barskey AE, Delea MG, et al. Measles outbreak in a highly vaccinated population, San Diego, 2008: role of the intentionally under vaccinated. Pediatrics. 2010;125(4):747-755. [DOI] [PubMed] [Google Scholar]
- 39. Centers for Disease Control Prevention. Measles cases and outbreaks. 2019. https://www.cdc.gov/measles/cases-outbreaks.html.
- 40. McDonald R, Schnabel-Ruppert P, Souto M, et al. Notes from the field: measles outbreaks from imported cases in Orthodox Jewish communities—New York and New Jersey, 2018–2019. Morb Mortal Wkly Rep. 2019;68(19):444-445. 10.15585/mmwr.mm6819a4externalicon. [DOI] [PMC free article] [PubMed] [Google Scholar]