Abstract
Background/Objectives:
Valued life activities are activities an individual deems particularly important or meaningful. Surgery in older adults can affect their ability to perform valued activities, but data are lacking. We characterized these activities and assessed performance of them following surgery.
Design:
Retrospective observational study.
Setting:
Preoperative program for older adults undergoing elective surgery at an academic hospital.
Participants:
Older adults (N=194) in the program from 2/2015 to 2/2018.
Measurements:
Preoperative written questionnaire asked, “What are the activities that are most important to you to be able to do when you return home from surgery?” Participants could list up to three activities. Content analysis was used to develop domains of valued life activities and categorize responses. Postoperative questionnaires and medical records were used to determine ability to perform activities six months after surgery.
Results:
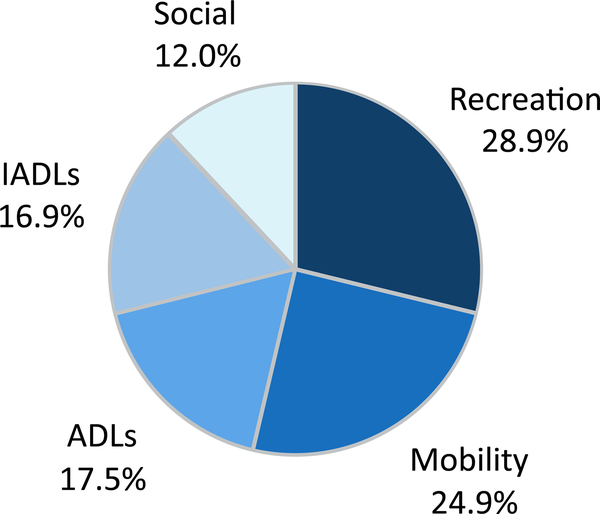
Of 194 participants (mean age 74.9 ± 9.1 years), 57.7% were female, 33.5% had more than two comorbid conditions. We elicited 510 valued activities, with a mean of 2.6 (± 0.7) activities per participant. Content analysis revealed five categories: 1) recreational activities (28.9%); 2) mobility (24.9%); 3) activities of daily living (ADLs, 17.5%); 4) instrumental activities of daily living (IADLs, 16.9%); and 5) social activities (12.0%). Ultimately, 154 participants had surgery, of which 27.3% were unable to perform one of their valued activities at six months. Performance varied between activity categories; 91.9% of mobility activities, 90.8% of ADLs, 80.3% of IADLs, 77.3% of social activities, and 65.5% of recreational activities were able to be performed after surgery.
Conclusion:
Older adults expressed a wide range of valued life activities. Over a quarter were unable to engage in at least one valued life activity after surgery, with recreation being the most commonly affected. Assessment of valued life activities should be incorporated into the perioperative management of older adults.
Keywords: Geriatric surgery, Older adults, Valued life activity, Function
INTRODUCTION
Older adults constitute a substantial proportion of the surgical population, with over a third of all inpatient procedures performed on those aged 65 years and older.1 Given current aging trends, this proportion is expected to increase over time.2 Despite advances in surgical care, older adults remain at increased risk for serious postoperative complications, which in turn can potentially limit their ability to engage in valued life activities.3 A valued life activity is any activity deemed to be particularly pleasurable or meaningful to an individual and can encompass self-care tasks, social interactions, and leisure interests.4 The principle of valued life activities is based on the concept that how an individual evaluates a particular health state is dependent on idiosyncratic functional goals.5 Thus, two older adults can hold divergent views on the same health impairment based on how it interferes with the activities they consider important.
Studies conducted in older adults and in those with chronic illnesses have shown that the inability to engage in a valued life activity is associated with negative perceptions of health status, lower quality of life metrics, and psychological distress.5–8 When these activities were first characterized in older adults, social and recreational activities together represented half of reported valued life activities, while those that involved personal autonomy comprised one-fifth, highlighting the relative importance of social and recreational activities. Currently, studies on postoperative outcomes in older adults have focused on basic functional assessments, such as performance of Activities of Daily Living (ADLs) and Instrumental Activities of Daily Living (IADLs).9,10 While some studies have utilized more complex measures of physical functioning3, such as household chores, only a handful have investigated participation in leisure activities11 and none have used valued life activities. As surgery can potentially affect one’s ability to perform certain valued life activities beyond self-care tasks, such as social and recreational pursuits, and these activities have been identified as important by older adults, the inclusion of such activity assessments is both imperative and informative.3 However, as of yet the identity of these activities and the ability of older adults to participate in them following surgery has not been described.
The primary objective of this study was to elicit and categorize the valued life activities of older adults preparing for an elective major surgical procedure. Our secondary aim was to determine the proportion of valued life activities that participants were able to perform within six months after surgery.
METHODS
Setting and participants
Participants were recruited between February 2015 and February 2018 upon referral to a multidisciplinary preoperative program designed for older adults at the University of California, San Francisco Medical Center, a tertiary academic medical institution. Participants were referred to this program by their surgeon after their surgical consultation took place. Details of this program have been described previously.12 Referral criteria were the following: scheduled for an elective operation or listed for organ transplant and aged 80 and older, or aged 60 and older with a concomitant geriatric syndrome (e.g., weakness, cognitive impairment, malnutrition). This study was approved by the Institutional Review Board at the University of California, San Francisco.
Measures
Participants’ valued life activities were elicited with a written questionnaire given upon referral to the preoperative program. The questionnaire included the following open-ended question: “What are the activities that are most important to you to be able to do when you return home from surgery?” Participants could provide up to three responses, by listing one, two or three activities in no particular order. This question was created by the multidisciplinary preoperative program and the team (geriatrician, physical and occupational therapists) would use the answers to obtain an understanding of what activities were important for the patient and engage in a conversation regarding expected recovery for the activity. Self-reported demographic and clinical information were obtained with the same questionnaire.
For those participants who underwent surgery, we determined the ability to perform their valued life activities within six months after the initial surgical procedure. This was done through (1) detailed postoperative questionnaires, which included the 12-item Short Form Health Survey (SF-12), the Katz ADL Index and the Lawton IADL Scale, sent at one, two, three, and six months after the date of the procedure and (2) review of the participant’s medical record.13–15 Participation in ADL and IADL valued activities was determined using the Katz ADLs Index and the Lawton IADLs Scale. Ability to engage in social activities was assessed with an SF-12 question that asks, “During the past 4 weeks, how much of the time has your physical or emotional problems interfered with your social activities (like visiting with friends, relatives, etc.)?” on a 5-point Likert scale. Participants who gave responses of “4 – A little of the time” or “5 – None of the time” were considered able to engage in social activities. Ability to participate in recreational activities that were physical in nature was determined with the SF-12 question, “Does your health now limit you in these activities? If so, how much? Activities, such as moving a table, pushing a vacuum cleaner, bowling, or playing golf”. This question uses a 3-point scale and participants providing responses of “3 – No, not limited at all” were considered able to perform physical recreational activities. To determine performance of mobility activities and sedentary recreational activities (for example “watching TV”) that are not covered by SF-12 questions, as well as to address any missing data in the questionnaires, participant medical records were reviewed. The study team examined all available notes, discharge summaries, and electronic communication within six months of the surgical procedure to determine ability to engage in the valued activity. For participants with multiple procedures, medical record review included the six months from the date of the initial procedure. Details regarding the methodology used to determine ability to perform valued activities are summarized in Supplementary Table S1.
Analysis
Participant demographic and clinical characteristics were tabulated and their frequencies calculated. We then analyzed the valued life activities using content analysis to identify substantive categories of valued activities.16 Creation of the categories was informed by prior research on valued life activities, healthcare goals, and quality-of-life domains.5,17–19 Once the categories were delineated, two reviewers (AK and MD) independently categorized each of the valued activities into one of the constructed categories. Categorization differences were used to determine inter-rater reliability and were resolved through discussion to achieve consensus, with involvement of a third reviewer (VT) as necessary. Frequency of each activity category was tabulated and reported as counts and percentages. For activities which required medical chart review to adjudicate, two reviewers (AK and MD) independently assessed ability to perform the valued activity and met regularly to achieve consensus. Cohen’s kappa was used to measure inter-rater agreement for both activity characterization and medical record abstraction. A chi-squared test was used to assess differences between categories in ability to perform the valued activity. To investigate the effects of possible measurement error for the activities that could not be verified either by the medical record or postoperative questionnaires, we conducted two sensitivity analyses: (1) assuming all unverifiable activities could be performed and (2) assuming they could not be performed. Finally, we calculated the proportion of older adults who were unable to participate in one of their stated valued activities within six months of surgery.
RESULTS
Patient Characteristics
Of the 383 older adults referred to the preoperative geriatric program, 166 declined to participate in the study. An additional 23 individuals did not provide a response to the question regarding valued activities on the initial written questionnaire. Thus, 194 participants remained in the study sample. The mean age of participants was 74.9 years (standard deviation ± 9.1), 57.7% were female, 65.5% were white, and 13.9% were Hispanic (Table 1). Half of the participants had a college degree and almost all (95.8%) were community-dwelling. The majority (60.8%) were scheduled for an oncologic surgical procedure and 14.8% a non-oncologic colorectal procedure. The remainder were scheduled for an orthopedic (6.2%), vascular (6.2%), other general surgery (7.7%) procedure, or were listed for solid organ transplant (4.6%). Most participants (54.6%) had one or two comorbid conditions, while one-third had more than two comorbid conditions. At baseline, almost two thirds (63.9%) were fully independent in all ADLs, while 40.7% were fully independent in all IADLs. Ultimately, 79.4% (N = 154) underwent surgery.
Table 1.
Baseline Characteristics of Participants
| Characteristic | Valuea N = 194 |
|---|---|
| Age, mean (SD), y | 74.9 (9.1) |
| Female | 112 (57.7) |
| Race/ethnicity | |
| White | 127 (65.5) |
| Asian or Pacific Islander | 28 (14.4) |
| Hispanic | 27 (13.9) |
| Other | 12 (6.2) |
| Education | |
| < High School | 17 (8.8) |
| High School | 75 (38.9) |
| College | 101 (52.3) |
| Living in facility | 8 (4.2) |
| Comorbid conditions | |
| 0 | 23 (11.9) |
| 1–2 | 106 (54.6) |
| >2 | 65 (33.5) |
| Fully independent ADLs | 124 (63.9) |
| Fully independent IADLs | 79 (40.7) |
| Planned Surgical Procedure | |
| Oncologic | 118 (60.8) |
| Non-oncologic colorectal | 28 (14.4) |
| Orthopedic | 12 (6.2) |
| Vascular | 12 (6.2) |
| Solid organ transplant | 9 (4.6) |
| Other | 15 (7.7) |
SD = standard deviation
ADL = Activities of daily living
IADL = Instrumental activities of daily living
Data are given as mean (SD) or number (percentage).
Characterization of Valued Life Activities
The 194 participants provided 510 unique valued life activities, with a mean of 2.6 (± 0.7) activities per participant. Five major categories of life activities were identified: recreation, mobility, ADLs, IADLs, and social (Figure 1). Inter-rater reliability for characterization of the valued life activities was excellent (κ = 0.93).
Figure 1.
Characterization of Valued Life Activities (N= 510 activities). ADLs = Activities of Daily Living. IADLs = Instrumental Activities of Daily Living. Mobility includes ambulation and driving. Example of social activity: “attending church”, and recreational activity: “watch TV”, and “golf”.
Recreation
The most commonly reported (28.9%) valued life activity was one that involved an interest, sport, or hobby performed for personal enjoyment (Table 2). These recreational activities ranged from sedentary pursuits, including “knitting”, “reading”, and “watch TV”, to more physically active hobbies such as “golf”, “fishing”, and “garage sales”. A small proportion were high intensity physical activities, for example “cycling” and “hiking”.
Table 2.
Characterization of Valued Life Activities for All 194 Participants Preparing for Elective Surgery
| Category | Frequency N = 510b |
Illustrative Responsesa |
|---|---|---|
| Recreation | 28.9% | “reading”, “cycling”, “bowling”, “garage sales”, “knitting” |
| Mobility | 24.9% | “up and walking”, “walk the stairs”, “driving the car” |
| Activities of Daily Living | 17.5% | “personal hygiene”, “bathing” “able to get up by myself”, “basic self-care”, |
| Instrumental Activities of Daily Living | 16.9% | “household chores”, “clean my house” “grocery shopping”, “prepare light meals” |
| Social | 12.0% | “enjoying time with friends and family”, “go to church”, “playing bridge” |
Responses to written question, “What are the activities that are most important to you to be able to do when you return home from surgery?”
Participants could provide up to three activities.
Mobility
One-quarter of valued activities dealt with mobility, which we defined as those activities that allow one to travel to a desired location, be that indoors or outdoors.18 This characterization encompassed activities such as ambulation as well as the operation of a motor vehicle. The majority (77.1%) of mobility activities were directly related to ambulation, with responses ranging from nonspecific “walking”, to more detailed goals such as “normal movement around home”, “walking without pain”, and “walk around on my own”. The remainder of mobility activities (22.9%) were related to operating a vehicle, with responses such as “driving” and “able to drive my car”.
ADLs
Of the 510 activities, 17.5% were identified as ADLs, which includes all the following basic self-care behaviors: bathing, dressing and grooming, toileting, transferring, and feeding. Several participants identified these activities in general terms, for example “safely do personal basics during recovery” and “self-care”. However, most ADL activities were described specifically. Examples include “use shower and dress myself”, “getting up from toilet” and “eating by myself; nobody has to feed me”. Of all the ADL activities, 32.6% were general statements of self-care, followed by toileting (20.2%), bathing (18.0%), feeding (10.1%), transferring (10.1%), and dressing/grooming (9.0%).
IADLs
Activities identified as IADLs comprised 16.9% of valued life activities. This category was defined as complex skills that allow an individual to live independently and includes shopping, preparing meals, managing finances and medication, housework and basic home maintenance. Again, some participants named this activity broadly, responding with “doing normal activities around the house” and “house responsibilities”, but most identified a specific IADL such as “able to prepare food for me to eat”, “cleaning home”, and “grocery shopping”. General statements of living independently in one’s home and preparing meals were the most common responses in this category, with each comprising 31.4% of IADL activities. This was followed by housework and home maintenance (29.1%), shopping (7.0%), and lastly managing finances (1.2%).
Social
Social activities, which were distinguished as those that focused on a participant’s interaction with others, represented a distinct subset (12.0%) of valued life activities. Responses involving family were common, for example “playing with granddaughter”, “family gatherings”, and “visit family”. Other examples in this category dealt with participation in a certain community, such as “comeback to my support group”, “playing bridge”, and “attending church”. Responses also included broad social activities like “socialize” and “phoning many folks”.
Ability to Perform Valued Life Activities After Surgery
Ability to perform valued life activities was assessed for the 154 participants who had surgery. These participants provided 410 valued activities, of which 22 activities were unable to be verified due to incomplete postoperative questionnaires and medical records, resulting in 388 valued activities where performance could be evaluated.
There was a statistically significant difference (p<0.001) in ability to perform valued activities between the five categories (Table 3). The vast majority of ADL and mobility valued activities (90.8% and 91.9% respectively) were able to be performed within 6 months of the surgical procedure. Of the 61 IADL activities identified, 80.3% were could be performed by 6 months. Performance was lower for recreation and social valued activities; only 77.3% of social and 65.5% of recreation activities were able to be performed. Ultimately, of the 154 individuals who had surgery, 27.3% (N=42) were unable to engage in at least one of their identified valued life activities within six months of surgery.
Table 3.
Ability to Perform Valued Life Activities Six Months after Elective Surgerya
| Category | Able to be Performed |
Unable to be Performed |
Total N = 388b |
|---|---|---|---|
| Mobility | 91 (91.9%) | 8 (8.1%) | 99 |
| Activities of Daily Living | 59 (90.8%) | 6 (9.2%) | 65 |
| Instrumental Activities of Daily Living | 49 (80.3%) | 12 (19.7%) | 61 |
| Social | 34 (77.3%) | 10 (22.7%) | 44 |
| Recreation | 77 (65.5%) | 41 (34.5%) | 119 |
p<0.001 for differences in performance between categories.
Total number of valued life activities provided by the 154 participants who underwent surgery.
Of the activities intended to be assessed by the postoperative questionnaires, 48.0% needed to be confirmed with medical record review due to incomplete or missing questionnaires, and 22 activities were unable to be assessed by either method. Subsequent sensitivity analyses revealed performance differences between activity categories remained even when assuming that the 22 unverifiable activities could be performed (Supplementary Table S2). Inter-rater reliability for assessment of performance for valued activities abstracted from the medical record was moderate (κ = 0.53).
DISCUSSION
Older adults preparing for elective surgery endorsed a wide range of valued life activities important for them to engage in after their procedure. Although many of the valued life activities were grounded in the traditional measures of function (ADLs, IADLs, and mobility), a large proportion were centered on recreation and a distinct subset were social activities. Over a quarter of participants were unable to engage in at least one of their valued life activities by six months. While ADL and mobility activities were largely able to be performed within the first six months after surgery, three-quarters of social activities and only a little over two-thirds of recreational activities were able to be performed by this time.
When valued life activities were first analyzed in older adults, social and recreational activities together comprised the majority of activities, with social outnumbering recreational four to one,5 while those activities that allowed individuals to care for oneself and live independently represented only a fifth of valued activities. In contrast, our analysis of the valued activities of older adults preparing for surgery revealed that many activities, represented by the categories of ADLs, IADLs, and mobility, were those that would allow an older adult to live independently in their home or community. Social activities were a much smaller proportion of valued activities in our cohort. Contextual factors may explain this finding; older adults undergoing surgery may consider different activities important compared to adults who are not facing an acute health challenge. Our identification of valued activities that represent ADLs, IADLs, and mobility aligns with prior work demonstrating the importance of function and independence for older adults with serious illness.14 Moreover, we found that some participants were unable to perform valued ADL and IADL activities. This supports the growing body of evidence for a prolonged decline in postoperative function in some older adults undergoing surgical treatment.21,22 In one prospective cohort, 9% of patients exhibited persistent ADL disability and 19% IADL disability six months following major abdominal surgery.9 Collectively, this information can be used to inform expectations regarding postoperative recovery for these activities.
Our results also shed light on the unique recreational and social valued activities not often addressed or elicited in the preoperative setting. The findings of this study suggest that older adults undergoing surgery may have more difficulty engaging in these types of activities compared to the traditional measures of function such as ADLs and IADLs. This can be partially explained by the known ceiling effects found in ADL and IADL scales.23 Additionally, previous studies have shown that ADLs and IADLs represent a continuum of increasingly complex tasks, with social and leisure activities being at the far end of this continuum.23,24 Therefore, the fact that recreational activities, which can be far more complex than basic ADLs, are less likely able to be performed following surgery could be expected. This finding may have important implications for surgical patients, as prior work has shown that a decline in the ability to perform recreational activities or engage in social interactions in particular is associated with negative psychological outcomes.6 Moreover, if there is a lasting inability to perform valued activities, assisting individuals in finding satisfactory replacement activities may allow them to maintain a more positive sense of health and well-being.8
Ultimately, our findings indicate that the valued life activities of older adults undergoing surgery include more than the basic functional activities that are represented by ADLs and IADLs. However, much of the surgical literature regarding older adults is limited to assessing just these measures.3 The wide breadth of value life activities reported by older adults, coupled with the fact that certain categories of activities were unable to be performed following surgery more so than others, signals the need to incorporate assessment of valued life activities into the perioperative care of this population. By limiting the focus to how surgery affects ADLs, IADLs, and mobility, this assumes that these are the most meaningful activities for older adults. However, our results reveal that this assumption may be flawed. As such, clinicians may consider inquiring about the valued life activities identified by their patients. Furthermore, measuring performance of valued life activities in future studies of postoperative outcomes aligns with the goals of patient-centered outcomes research.25
This study does have several limitations. The study population was selected from a preoperative program designed for frail older adults, and was predominately white, well-educated, and community-dwelling, which could limit generalizability to a more diverse population. Since each participant could provide up to three valued activities in any order, this study could not detect if certain activities were more important than others for individual participants. Moreover, contextual factors, such as how information regarding the risks of surgery and expected postoperative recovery was communicated to participants, could have altered what valued activities were provided. Given the open-ended nature of the question, particularly regarding the time period as “after you return home from surgery”, participants could have been naming activities they wanted to perform during the immediate postoperative period, or more distal to the surgery. There also exists a potential for misclassification as well as overlap among the categories of valued activities. Additionally, since the post-operative questionnaires did not contain a specific question about performance in the participant’s chosen activities, this had to be assessed indirectly using the SF-12 and medical chart review, which could also induce possible measurement error. Missing or incomplete postoperative questionnaires required reliance on the medical record to assess performance; inter-rater reliability for medical record abstraction was moderate. Finally, as the majority of participants were being treated for an oncological disease, it is difficult to determine if it was the surgical procedure, the natural course of their disease, or other non-surgical treatments, such as chemotherapy, that was responsible for the impaired performance in valued activities that was found.
In conclusion, older adults identified a wide variety of functional abilities, hobbies, and social pursuits important for them to participate in following surgery, with recreational activities constituting a large proportion. Not all valued life activities could be performed within six months of surgery, particularly for those identified as social and recreational activities. Given over a quarter of participants were unable to engage in one of their valued activities, assessment of valued life activities should be incorporated into the perioperative management of older adults.
Supplementary Material
ACKNOWLEDGMENTS
Financial Disclosure: AK was supported by the National Institute on Aging (NIA) at the National Institute of Health (NIH) Research Training in Geriatric Medicine (T32 AG000212). MB was supported by the NIA Medical Student Training in Aging Research Program and the University of California, San Francisco (UCSF) Claude D. Pepper Older Americans Independence Center. RS was supported in part by the NIA at the NIH (K24 AG054415). EF was supported in part by the NIA at the NIH (R21 AG054208). VLT was supported in part by the NIA Early Medical/Surgical Specialists’ Transition to Aging Research (R03 AG056342), and the UCSF Clinical and Translational Science Institute Career Development Program (KL2 TR001870).
Sponsor’s Role: Sponsors had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of the paper.
Footnotes
SUPPLEMENTAL INFORMATION
Conflict of Interest: Dr. Finlayson reports being founding shareholder of Ooney Inc., a digital health company. Remaining authors have no conflicts to report.
Earlier versions of these findings were presented at the American Geriatrics Society Annual Meeting in Portland, OR on May 2nd, 2019.
REFERENCES
- 1.National Center for Health Statistics. Number of all-listed procedures for discharges from short-stay hospitals, by procedure category and age: United States, 2010. Available at: https://www.cdc.gov/nchs/data/nhds/4procedures/2010pro4_numberprocedureage.pdf. Accessed December 18, 2018.
- 2.Etzioni DA, Liu JH, Maggard MA, Ko CY. The Aging Population and Its Impact on the Surgery Workforce. Ann Surg 2003;238(2):170–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hshieh TT, Saczynski J, Gou RY, et al. Trajectory of Functional Recovery After Postoperative Delirium in Elective Surgery. Ann Surg 2017;265(4):647–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katz P Function, disability, and psychological well-being. Adv Psychosom Med 2004;25:41–62. [DOI] [PubMed] [Google Scholar]
- 5.Ditto PH, Druley JA, Moore KA, Danks JH, Smucker WD. Fates worse than death: The role of valued life activities in health-state evaluations. Health Psychol 1996;15(5):332–343. [DOI] [PubMed] [Google Scholar]
- 6.Katz PP, Yelin EH. Activity loss and the onset of depressive symptoms: do some activities matter more than others? Arthritis Rheum 2001;44(5):1194–1202. [DOI] [PubMed] [Google Scholar]
- 7.Katz PP, Yelin EH, Eisner MD, Earnest G, Blanc PD. Performance of valued life activities reflected asthma-specific quality of life more than general physical function. J Clin Epidemiol 2004;57(3):259–267. [DOI] [PubMed] [Google Scholar]
- 8.Katz P, Morris A, Gregorich S, et al. Valued Life Activity Disability Played a Significant Role in Self-Rated Health among Adults with Chronic Health Conditions. J Clin Epidemiol 2009;62(2):158–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lawrence V, Hazuda H, Cornell J, et al. Functional independence after major abdominal surgery in the elderly. J Am Coll Surg 2004;199(5):762–772. [DOI] [PubMed] [Google Scholar]
- 10.Brinson Z, Tang VL, Finlayson E. Postoperative Functional Outcomes in Older Adults. Curr Surg Rep 2016;4(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaturvedi RK, Blaise M, Verdon J, et al. Cardiac Surgery in Octogenarians: Long-Term Survival, Functional Status, Living Arrangements, and Leisure Activities. Ann Thorac Surg 2010;89(3):805–810. [DOI] [PubMed] [Google Scholar]
- 12.Kata A, Sudore R, Finlayson E, Broering JM, Ngo S, Tang VL. Increasing Advance Care Planning Using a Surgical Optimization Program for Older Adults. J Am Geriatr Soc 2018;66(10):2017–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of Illness in the Aged. The Index of ADL: A Standardized Measure of Biological and Psychosocial Function. JAMA 1963;185:914–919. [DOI] [PubMed] [Google Scholar]
- 14.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist 1969;9(3):179–186. [PubMed] [Google Scholar]
- 15.Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34(3):220–233. [DOI] [PubMed] [Google Scholar]
- 16.Bernard HR, Wutich A, Ryan GW. Analyzing Qualitative Data: Systematic Approaches, 2nd Ed. Thousand Oaks, CA: Sage Publication; 2017. [Google Scholar]
- 17.Karel MJ, Mulligan EA, Walder A, Martin LA, Moye J, Naik AD. Valued life abilities among veteran cancer survivors. Health Expect 2016;19(3):679–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pietersma S, de Vries M, van den Akker-van Marle ME Domains of quality of life: results of a three-stage Delphi consensus procedure among patients, family of patients, clinicians, scientists and the general public. Qual Life Res 2014;23(5):1543–1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Naik AD, Martin LA, Moye J, Karel MJ . Health Values and Treatment Goals of Older, Multimorbid Adults Facing Life-Threatening Illness. J Am Geriatr Soc 2016;64(3):625–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fried TR, Tinetti ME, Iannone L, O’Leary JR, Towle V, Van Ness PH. Health outcome prioritization as a tool for decision making among older persons with multiple chronic conditions. Arch Intern Med 2011;171(20):1854–1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kwon S, Symons R, Yukawa M, Dasher N, Legner V, Flum DR. Evaluating the association of preoperative functional status and postoperative functional decline in older patients undergoing major surgery. Am Surg 2012;78(12):1336–1344. [PMC free article] [PubMed] [Google Scholar]
- 22.Rønning B, Wyller TB, Jordhøy MS, et al. Frailty indicators and functional status in older patients after colorectal cancer surgery. J Geriatr Oncol 2014;5(1):26–32 [DOI] [PubMed] [Google Scholar]
- 23.Fieo R, Manly JJ, Schupf N, Stern Y. Functional Status in the Young–Old: Establishing a Working Prototype of an Extended-Instrumental Activities of Daily Living Scale. J Gerontol. 2014;69(6):766–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gross AL, Jones RN, Inouye SK. Development of a composite measure of physical functioning for older persons. Res Aging 2015;37(7):671–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frank L, Basch E, Selby JV. The PCORI Perspective on Patient-Centered Outcomes Research. JAMA 2014;312(15):1513–1514. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.