Abstract
Background
Benralizumab is an interleukin-5 receptor alpha–directed cytolytic monoclonal antibody. Treatment with benralizumab significantly reduces exacerbations and improves lung function after 1 year for patients with severe, uncontrolled eosinophilic asthma.
Objective
We explored whether benralizumab efficacy was sustained after an additional year of treatment while maintaining an acceptable safety profile.
Methods
Data from the pivotal 48-week SIROCCO and 56-week CALIMA studies were integrated with data from the predefined 56-week adult phase of the BORA extension study to provide a 2-year integrated efficacy and safety analysis of benralizumab. BORA enrolled patients who had completed SIROCCO or CALIMA. Patients receiving benralizumab 30 mg subcutaneously, either every 4 weeks (Q4W) or every 8 weeks (Q8W; first three doses Q4W), were assessed. Efficacy was evaluated based on baseline blood eosinophil counts from the pivotal studies (≥300 and <300 cells/μL).
Results
Mean treatment exposures were 24.3 (Q4W, n=518) and 24.6 (Q8W, n=512) months. Exacerbation frequency reductions observed in SIROCCO/CALIMA were maintained; 50% of the patients had no exacerbations during the 2-year study period (crude exacerbation rate, Q8W: 0.56 exacerbations/year for patients with blood eosinophil counts ≥300 cells/μL). Lung function improvements with benralizumab were maintained for 2 years, as represented by increases in mean prebronchodilator forced expiratory volume in 1 second from baseline of 0.343 L and 0.364 L with 1 and 2 years of benralizumab Q8W treatment, respectively, for patients with blood eosinophil counts ≥300 cells/μL. Health-related quality of life improvements with benralizumab observed in the pivotal studies were also sustained. Adverse events and serious adverse event rates were similar between the BORA extension and SIROCCO/CALIMA periods, with no new or unexpected occurrence of adverse events.
Conclusion
This benralizumab 2-year integrated analysis further supports long-term use of benralizumab for patients with severe, uncontrolled eosinophilic asthma.
Keywords: asthma, benralizumab, clinical features, eosinophilic inflammation, interleukin-5 receptor, safety
Plain Language Summary
Why Was The Study Done?
In two Phase III studies (SIROCCO and CALIMA), benralizumab treatment was evaluated for 1 year for patients with severe, uncontrolled asthma with elevated eosinophil counts, a cellular source of inflammation. Benralizumab reduced the occurrence of asthma attacks and improved lung function and asthma symptoms with an acceptable safety and tolerability profile. We evaluated whether the efficacy and safety profile of benralizumab was maintained after an additional year of treatment.
What Did The Researchers Do And Find?
We integrated the first year of benralizumab treatment data from SIROCCO and CALIMA with data from the Phase III BORA safety extension study (study of patients from SIROCCO and CALIMA who continued treatment for an additional year). We determined that reductions in the occurrence of asthma attacks and improvements in lung function and asthma symptoms were maintained during the second year of benralizumab treatment with an acceptable and stable safety profile.
What Do These Results Mean?
Benralizumab provides long-term benefit for patients with severe, uncontrolled asthma with elevated eosinophil counts while maintaining an acceptable and stable safety profile.
Introduction
Worldwide, asthma affects greater than 339 million people, with approximately 10% having severe or uncontrolled asthma.1,2 Patients with severe, uncontrolled asthma experience high disease burden, including recurrent exacerbations and hospitalizations,3 despite treatment with traditional therapies including oral corticosteroids (OCS). Targeting eosinophilic inflammation, which is present for approximately 50% of patients with asthma4 and is associated with greater disease severity, represents a new approach to treat severe, uncontrolled asthma.5,6
Benralizumab is an interleukin-5 receptor alpha–directed cytolytic monoclonal antibody that induces direct, rapid, and nearly complete depletion of eosinophils via enhanced antibody-dependent cell-mediated cytotoxicity.7,8 The efficacy and safety of benralizumab have been evaluated in three pivotal Phase III studies: SIROCCO, CALIMA, and ZONDA.9–11 In the 48-week SIROCCO and 56-week CALIMA studies, patients aged 12–75 years with severe, uncontrolled asthma received benralizumab 30 mg, either every 4 weeks (Q4W) or every 8 weeks (Q8W; first three doses Q4W), or placebo and maintenance therapy with inhaled corticosteroids (ICS) plus long-acting β2-agonists (LABA).9,10 The primary and key secondary endpoints in these studies included annual exacerbation rate ratio versus placebo and change from baseline in prebronchodilator forced expiratory volume in 1 second (FEV1) at end of treatment. In these studies, benralizumab Q8W significantly reduced asthma exacerbations by 28–51% relative to placebo for patients with baseline blood eosinophil counts ≥300 cells/μL.9,10 In the 28-week ZONDA study, benralizumab reduced OCS dosage from baseline by 75% compared with a 25% reduction with placebo for adult patients with baseline blood eosinophil counts ≥150 cells/μL.11
Patients who completed SIROCCO, CALIMA, or ZONDA and chose to continue long-term treatment were invited to enroll in the BORA Phase III extension study to provide additional efficacy and safety data.12 Adults enrolled in BORA continued treatment for up to 56 weeks, and adolescents could continue treatment for up to 108 weeks. The predefined primary analysis for BORA included data for both adults and adolescents who completed 56 weeks of treatment. These data have been evaluated and results have been published for patients originally in SIROCCO/CALIMA.12 In the published report, evaluated data encompassed the 56-week period since BORA enrollment.12 Analysis of the first year of BORA (second year of benralizumab treatment) indicated that the safety profile of benralizumab was consistent with published results from the pivotal studies.12
Unlike the previous report, here we present an analysis that encompasses the first 2 years of treatment with benralizumab instead of focusing only the second year of treatment. We integrated data from the adult completion phase of BORA with results from SIROCCO and CALIMA. Because of differences in study designs and overall objectives between SIROCCO/CALIMA and ZONDA, the integrated analysis of ZONDA and BORA was performed separately and will be reported in another publication. We explored whether the efficacy benefit and safety observed in SIROCCO and CALIMA were maintained with an additional year of treatment.
Materials And Methods
Study Design And Participants
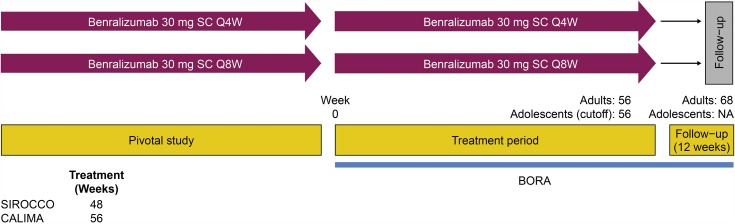
Specific details of the individual study designs have been published.9,10,12 The integrated analysis design is summarized in Figure 1. Data were evaluated for patients who were originally in SIROCCO or CALIMA and moved into BORA (allowing evaluation of 2 years of data). Data from BORA could be integrated with SIROCCO and CALIMA because of the trials’ similar treatment duration (48 and 56 weeks, respectively), identical endpoints, consistent efficacy and safety assessment schedule, and inclusion/exclusion criteria.9,10 Patients who received placebo in the pivotal studies were randomized to one of the two active treatment groups when they entered BORA. Therefore, because they did not remain on the same treatment throughout the follow-up period, they are not included in the integrated analysis.
Figure 1.
Benralizumab 2-Year Integrated Analysis Study Design.
Abbreviations: NA, not available; Q4W, every 4 weeks; Q8W, every 8 weeks (first three doses Q4W); SC, subcutaneously.
In the integrated analysis, patients receiving benralizumab 30 mg subcutaneously, either Q4W or Q8W, with high-dosage (or medium-dosage for CALIMA) inhaled corticosteroids plus long-acting β2-agonists in the pivotal studies who continued into BORA were assessed. Full inclusion and exclusion criteria for the pivotal studies and BORA used in the benralizumab 2-year integrated analysis have been reported.9,10,12
Ethics
Compliance details for each study in the benralizumab 2-year integrated analysis have been reported.9,10,12 Before any patients were enrolled, an independent ethics committee or institutional review board at each study center approved the clinical study protocol (details provided in the Supplementary materials), and the national regulatory authority either approved the clinical study protocol or received a notification according to local regulations. All patients provided written informed consent at enrolment. This study was conducted in accordance with the principles of the Declaration of Helsinki and was consistent with the International Council for Harmonisation/Good Clinical Practice.
Outcomes
Long-term efficacy endpoints for patients who completed the SIROCCO/CALIMA pivotal studies and transitioned into the BORA extension study included asthma exacerbations (annual asthma exacerbation rate [AER] and AER associated with hospitalizations and emergency department [ED] visits), change from baseline in lung function (FEV1), asthma control (Asthma Control Questionnaire 6 [ACQ-6]), general health-related quality of life (Asthma Quality of Life Questionnaire [standardized] for 12 years and older [AQLQ{S}+12]), and blood eosinophil counts. The long-term safety and tolerability endpoints were adverse events, serious adverse events, hypersensitivity, and immunogenicity. Treatment exposure and rate of adverse events per 100-patient-years (100-PYs) at risk were determined.
Statistical Analysis
The all patients set (APS) included patients who received at least one dose of benralizumab in SIROCCO/CALIMA regardless of entry into BORA. The full analysis set (FAS) included patients who received benralizumab, completed SIROCCO/CALIMA, and received at least one dose of benralizumab in BORA. The FAS excluded patients who, during BORA, transitioned into MELTEMI (NCT02808819), a subsequent separate open-label, 130-week safety extension study. These patients (<20% of the total treated population) did not have the opportunity to complete the full treatment period. As such, inclusion in the FAS could have confounded adverse event rates and annualized exacerbation data (patients who transitioned into MELTEMI were also excluded from the primary analysis of BORA).12
The benralizumab 2-year integrated analysis included patients who received benralizumab and high-dosage ICS/LABA. Analyses were performed for patients with baseline blood eosinophil counts ≥300 cells/μL and <300 cells/μL in the pivotal studies. Efficacy endpoints for the integrated analysis involving SIROCCO and CALIMA were conducted on the FAS. Integrated safety analyses with BORA are reported for the patients originally in the SIROCCO and CALIMA studies only and were conducted on the FAS and APS. For the APS, results are presented for independently adjudicated new malignancies, discontinuations during the on-treatment period, and deaths.
No placebo comparison is available for the long-term integrated data. Therefore, data were summarized with descriptive statistics (mean, standard deviation [SD], median, range), qualitative summaries, and 95% confidence intervals. All analyses were conducted with SAS® System (SAS Institute Inc., Cary, NC, United States) version 9.4 or later.
Results
Patients
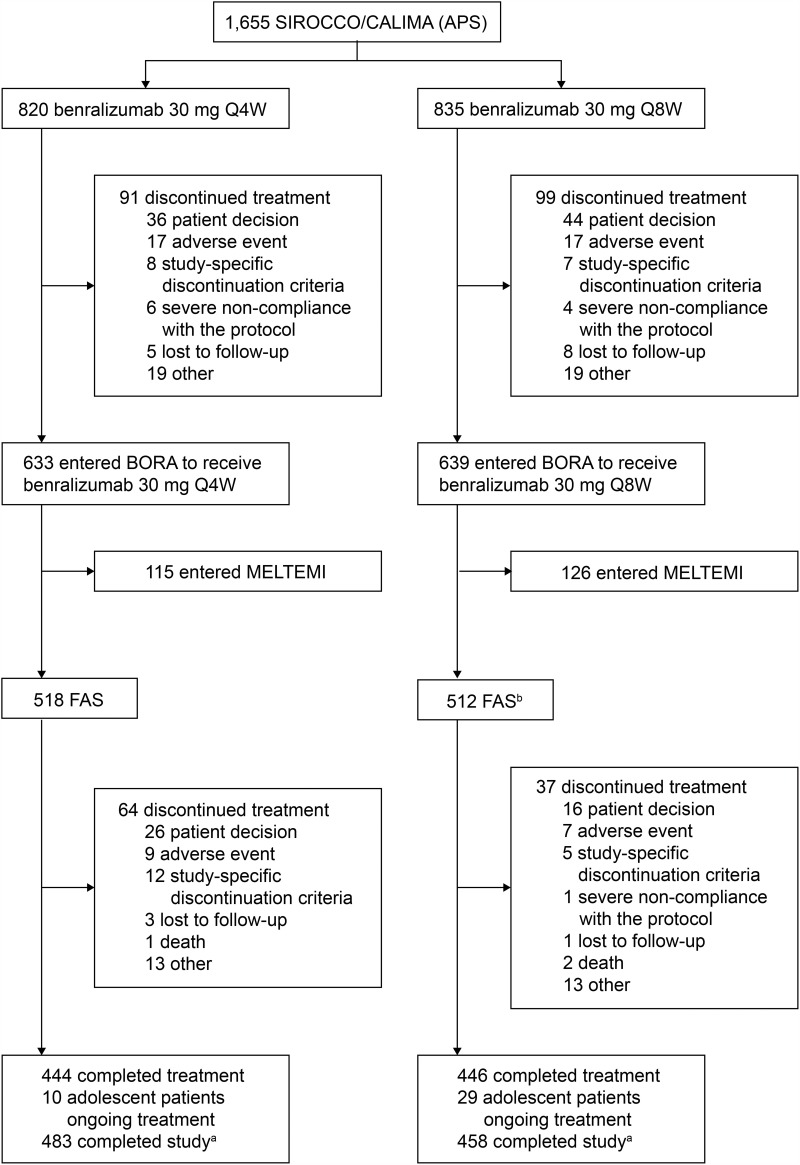
The SIROCCO/CALIMA FAS consisted of 1030 patients (Figure 2). Of patients originally in SIROCCO or CALIMA, 18% (n=291) discontinued treatment. The primary reason for discontinuation from SIROCCO/CALIMA was individual patient decision (42%, n=122 [pivotal and BORA studies]) (Figure 2). Demographics and baseline clinical characteristics were, in general, balanced between treatment groups (Table 1). During the benralizumab 2-year integrated analysis, patients in SIROCCO/CALIMA receiving benralizumab Q4W and Q8W had mean (SD) on-treatment durations of 24.3 (2.7, n=518) and 24.6 (2.4, n=512) months, respectively (Table S1).
Figure 2.
Trial profile for benralizumab 2-year integrated analysis. aIncluding patients who discontinued treatment but attended all study visits. bOne patient did not receive treatment and one patient did not fulfill eligibility criteria.
Abbreviations: APS, all patients set; FAS, full analysis set; Q4W, every 4 weeks; Q8W, every 8 weeks (first three doses Q4W).
Table 1.
Demographics And Baseline Clinical Characteristics Of Benralizumab 2-Year Integrated Analysis Patients (FAS)a
| SIROCCO/CALIMA Blood Eosinophil Counts ≥300 Cells/μL | ||
|---|---|---|
| Benralizumab 30 mg Q4W (n=323) | Benralizumab 30 mg Q8W (n=318) | |
| Age (years), mean (SD) | 49.4 (13.1) | 48.0 (14.5) |
| Age group (years), n (%) | ||
| ≥12–<18 | 11 (3) | 17 (5) |
| ≥18–75 | 312 (97) | 301 (95) |
| Sex, n (%) | ||
| Male | 118 (37) | 129 (41) |
| Female | 205 (64) | 189 (59) |
| Race, n (%) | ||
| White | 245 (76) | 237 (75) |
| Black or African-American | 5 (2) | 7 (2) |
| Asian | 56 (17) | 53 (17) |
| Otherb | 17 (5) | 21 (7) |
| Ethnic group, n (%) | ||
| Hispanic or Latino | 71 (22) | 64 (20) |
| Not Hispanic or Latino | 252 (78) | 254 (80) |
| BMI (kg/m2), mean (SD) | 28.9 (7.4) | 27.8 (6.0) |
| Eosinophil count (cells/µL), median (range) | 470 (0–2800) | 460 (10–3110) |
| Prebronchodilator FEV1 (L), mean (SD) | 1.7 (0.55) | 1.7 (0.62) |
| Prebronchodilator FEV1 (% predicted normal), mean (SD) | 57.8% (13.8) | 57.4% (14.5) |
| Reversibility (%), median (range) | 24.9% (24.5) | 24.1% (22.2) |
| Prebronchodilator FEV1/FVC, mean (SD) | 61.6 (11.4) | 60.4 (12.5) |
| ACQ-6 score, mean (SD) | 2.7 (0.9) | 2.7 (0.9) |
| Time since asthma diagnosis (years), median (range) | 14.7 (1.3–66.2) | 15.4 (1.1–58.3) |
| Number of exacerbations in the past 12 months | 2.9 (1.8) | 2.7 (1.4) |
| 2 exacerbations, n (%) | 199 (62) | 200 (63) |
| ≥3 exacerbations, n (%) | 124 (38) | 118 (37) |
| Patients with ≥1 exacerbation in the past 12 months resulting in hospitalizations or ED visits, n (%) | 93 (29) | 98 (31) |
| AQLQ(S)+12 score, mean (SD) | 4.0 (1.0) | 3.9 (1.0) |
Notes: aBaseline data from preceding pivotal studies. bNative Hawaiian or “other” Pacific Islander, American Indian or Alaska Native and other.
Abbreviations: ACQ-6, Asthma Control Questionnaire 6; AQLQ(S)+12, Asthma Quality of Life Questionnaire (standardized) for 12 years and older; BMI, body mass index; ED, emergency department; FAS, full analysis set; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; Q4W, every 4 weeks; Q8W, every 8 weeks (first three doses Q4W); SD, standard deviation.
Efficacy Outcomes
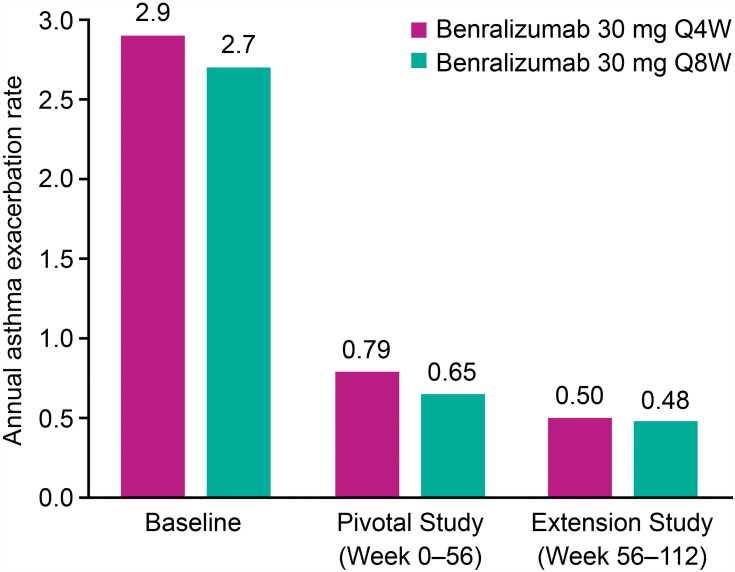
Efficacy outcomes discussed in the text for exacerbations, FEV1, ACQ-6, and AQLQ(S)+12 are reported for patients who had blood eosinophil counts ≥300 cells/μL at baseline in the original SIROCCO/CALIMA studies, unless otherwise indicated. Approximately 50% of the patients had no exacerbations during the 2-year study period, regardless of benralizumab dosage (Q4W or Q8W) or pivotal study baseline blood eosinophil counts (≥300 or <300 cells/μL) (Table 2). For approximately 12% of the patients, exacerbations led to hospitalizations or ED visits. Crude exacerbation rates (exacerbations/year) for the 318 patients receiving benralizumab Q8W over the 2-year period (0.56) were consistent with rates reported for these patients over the pivotal study and extension periods for Q8W (0.65 and 0.48, respectively) (Figure 3).
Table 2.
Asthma Exacerbations For SIROCCO/CALIMA Pivotal Study Patients In The Benralizumab 2-Year Integrated Analysis (FAS, On-Treatment period)
| Blood Eosinophil Counts ≥300 Cells/μLa | Blood Eosinophil Counts <300 Cells/μLa | |||
|---|---|---|---|---|
| Benralizumab 30 mg Q4W (n=323) | Benralizumab 30 mg Q8W (n=318) | Benralizumab 30 mg Q4W (n=165) | Benralizumab 30 mg Q8W (n=166) | |
| All exacerbations | ||||
| Patients with ≥1 exacerbation, n (%) | 152 (47) | 157 (49) | 85 (52) | 90 (54) |
| Crude annual rate (95% CI) | 0.65 (0.59, 0.71) | 0.56 (0.51, 0.62) | 0.80 (0.71, 0.90) | 0.68 (0.60, 0.77) |
| Exacerbations per patient, mean (SD) | 1.3 (2.3) | 1.2 (1.8) | 1.6 (3.1) | 1.4 (2.0) |
| Exacerbations leading to hospitalizations or ED visits | ||||
| Patients with ≥1 exacerbation, n (%) | 39 (12) | 37 (12) | 26 (16) | 19 (11) |
| Crude annual rate (95% CI) | 0.10 (0.08, 0.13) | 0.08 (0.06, 0.11) | 0.11 (0.08, 0.15) | 0.08 (0.05, 0.12) |
| Exacerbations per patient, mean (SD) | 0.2 (0.7) | 0.2 (0.5) | 0.2 (0.6) | 0.2 (0.5) |
| Exacerbations leading to hospitalizations | ||||
| Patients with ≥1 exacerbation, n (%) | 18 (6) | 19 (6) | 20 (12) | 12 (7) |
| Crude annual rate (95% CI) | 0.05 (0.03, 0.07) | 0.04 (0.02, 0.06) | 0.08 (0.05, 0.11) | 0.05 (0.03, 0.08) |
| Exacerbations per patient, mean (SD) | 0.1 (0.5) | 0.1 (0.3) | 0.2 (0.4) | 0.1 (0.5) |
Notes: Published annual rate for the pooled SIROCCO and CALIMA placebo patients with blood eosinophil counts ≥300 cells/µL at end of the pivotal studies was 1.14. Data from FitzGerald et al.19 aEosinophil counts at baseline of preceding pivotal studies.
Abbreviations: CI, confidence interval; ED, emergency department; FAS, full analysis set; Q4W, every 4 weeks; Q8W, every 8 weeks (first three doses Q4W); SD, standard deviation.
Figure 3.
Annual asthma exacerbation rate for patients in SIROCCO/CALIMA pivotal study (Full analysis set, on-treatment period, blood eosinophil counts ≥300 cells/µLa). n values are 323/318 for patients receiving benralizumab 30 mg Q4W and Q8W, respectively. Baseline value represents exacerbation rate over the year before pivotal study entry. aBlood eosinophil counts at baseline of preceding pivotal studies.
Abbreviations: Q4W, every 4 weeks; Q8W, every 8 weeks (first three doses Q4W).
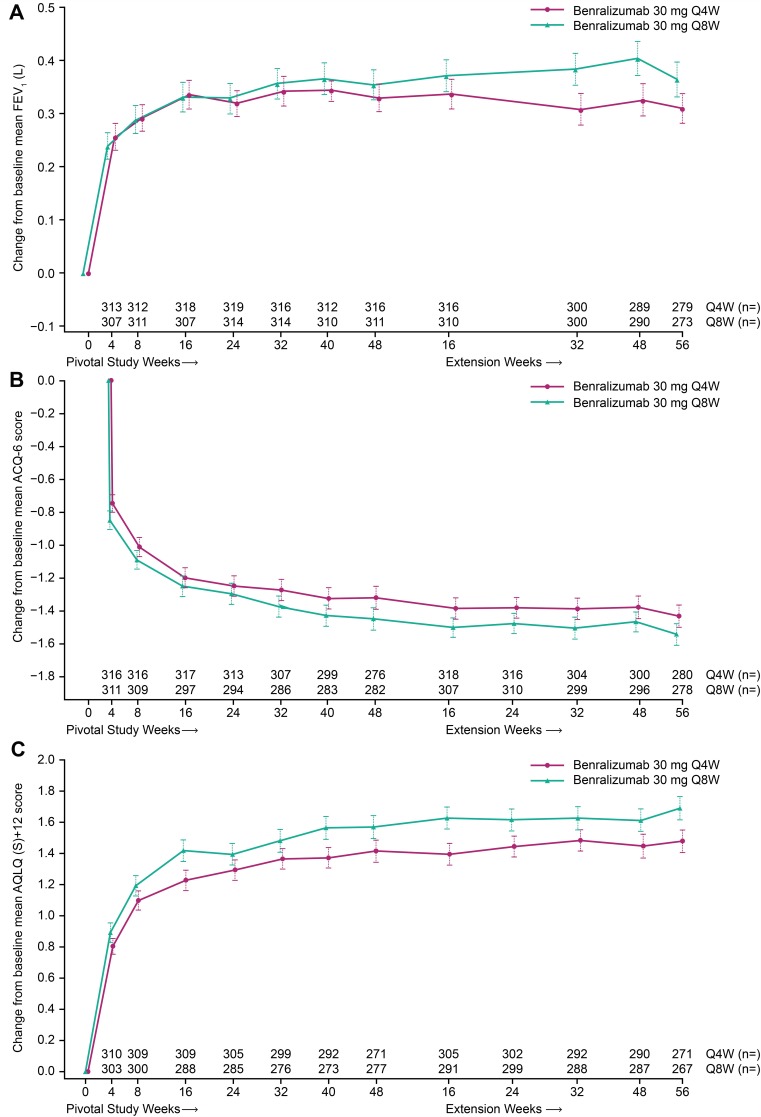
Improvements in FEV1, ACQ-6, and AQLQ(S)+12 that were observed at the end of treatment (EOT) with benralizumab in the pivotal studies were maintained during the extended treatment period (Table 3, Figure 4). Similar improvements were obtained throughout treatment with the benralizumab Q4W and Q8W dosages. Greater changes from baseline were observed throughout the 2-year integrated analysis for patients with blood eosinophil counts ≥300 versus <300 cells/μL in the pivotal studies (Table 3).
Table 3.
Changes In Lung Function, ACQ-6, And AQLQ(S)+12 With Benralizumab During The 2-Year Integrated Analysis Period For SIROCCO/CALIMA Pivotal Study Patients (FAS, On-Treatment period)
| Blood Eosinophil Counts ≥300 Cells/μLa | Blood Eosinophil Counts <300 Cells/μLa | |||
|---|---|---|---|---|
| Benralizumab 30 mg Q4W (n=323) | Benralizumab 30 mg Q8W (n=318) | Benralizumab 30 mg Q4W (n=165) | Benralizumab 30 mg Q8W (n=166) | |
| Prebronchodilator FEV1 (L) | ||||
| Baseline, mean (SD), n | 1.703 (0.555), 323 | 1.741 (0.621), 318 | 1.668 (0.556), 163 | 1.758 (0.612), 166 |
| Change at pivotal study EOT,b mean (SD), n | 0.328 (0.449), 313 | 0.343 (0.507), 305 | 0.158 (0.433), 158 | 0.174 (0.421), 165 |
| Change at extension Week 56, mean (SD), n | 0.310 (0.481), 279 | 0.364 (0.544), 273 | 0.128 (0.449), 139 | 0.134 (0.446), 143 |
| ACQ-6 | ||||
| Baseline, mean (SD), n | 2.73 (0.91), 323 | 2.74 (0.90), 318 | 2.75 (0.94), 165 | 2.76 (0.92), 166 |
| Change at pivotal study EOT,b mean (SD), n | −1.36 (1.16), 322 | −1.44 (1.13), 315 | −1.04 (1.18), 165 | −1.09 (0.99), 166 |
| Change at extension Week 56, mean (SD), n | −1.43 (1.13), 280 | −1.54 (1.09), 278 | −1.15 (1.08), 143 | −1.16 (1.03), 144 |
| AQLQ(S)+12 | ||||
| Baseline, mean (SD), n | 3.96 (0.98), 314 | 3.90 (0.99), 307 | 4.01 (0.93), 161 | 3.96 (1.01), 163 |
| Change at pivotal study EOT,b mean (SD), n | 1.41 (1.16), 314 | 1.58 (1.23), 306 | 1.01 (1.16), 161 | 1.11 (1.09), 163 |
| Change at extension Week 56, mean (SD), n | 1.48 (1.20), 271 | 1.69 (1.24), 267 | 1.12 (1.07), 139 | 1.28 (1.07), 141 |
Notes: Published least squares mean changes from baseline for the pooled SIROCCO and CALIMA placebo patients with blood eosinophil counts ≥300 cells/µL at end of the pivotal studies were 0.224 L (prebronchodilator FEV1), −1.16 (ACQ-6), and 1.27 (AQLQ[S]+12). Data from FitzGerald et al.19 aEosinophil counts at baseline of preceding pivotal studies. bWeek 48 for SIROCCO and Week 56 for CALIMA.
Abbreviations: ACQ-6, Asthma Control Questionnaire 6; AQLQ(S)+12, Asthma Quality of Life Questionnaire (standardized) for 12 years and older; EOT, end of treatment; FAS, full analysis set; FEV1, forced expiratory volume in 1 second; Q4W, every 4 weeks; Q8W, every 8 weeks (first three doses Q4W); SD, standard deviation.
Figure 4.
Change from SIROCCO/CALIMA pivotal study baseline in (A) Lung Function (FEV1), (B) ACQ-6, and (C) AQLQ(S)+12 with benralizumab during the 2-year integrated analysis (Full analysis set, on-treatment period, blood eosinophil counts ≥300 cells/µLa). Error bars represent standard error. aBlood eosinophil counts at baseline of preceding pivotal studies.
Abbreviations: ACQ-6, Asthma Control Questionnaire 6; AQLQ(S)+12, Asthma Quality of Life Questionnaire (standardized) for 12 years and older; FEV1, forced expiratory volume in 1 second; Q4W, every 4 weeks; Q8W, every 8 weeks (first three doses Q4W).
Safety Outcomes
Adverse and serious adverse event rates for patients, regardless of blood eosinophil counts, who received benralizumab in SIROCCO/CALIMA and continued into BORA were similar for the Q4W and Q8W cohorts for the integrated period (43.05 vs. 41.48 and 9.05 vs. 7.52 per 100-PYs, respectively) (Table 4), with no new or unexpected occurrence of adverse events. For patients who received benralizumab in SIROCCO/CALIMA, adverse and serious adverse event rates were similar for both treatment cohorts during either the pivotal study or extension periods of the 2-year integrated analysis (Table S2). For these patients, adverse event rates were numerically greater during the pivotal study period than during the extension period.
Table 4.
Adverse Events, Injection-Site Reactions, And Hypersensitivity For SIROCCO/CALIMA Pivotal Study Patients During The 2-Year Integrated Analysis Period (FAS, On-Treatment Period, All Patients Regardless Of Blood Eosinophil Count)
| Benralizumab 30 mg Q4W (n=518) (Exp=1049.97)a | Benralizumab 30 mg Q8W (n=512) (Exp=1051.11)a | |||
|---|---|---|---|---|
| n (%) | Event Rate (per 100-Patient-Years) | n (%) | Event Rate (Per 100-Patient-Years) | |
| Any AE | 452 (87) | 43.05 | 436 (85) | 41.48 |
| Any AE leading to treatment discontinuation | 10 (2) | 0.95 | 8 (2) | 0.76 |
| AEs in ≥5% of patientsb | ||||
| Viral upper respiratory tract infection | 138 (27) | 13.14 | 137 (27) | 13.03 |
| Upper respiratory tract infection | 63 (12) | 6.00 | 67 (13) | 6.37 |
| Bronchitis | 60 (12) | 5.71 | 66 (13) | 6.28 |
| Sinusitis | 33 (6) | 3.14 | 35 (7) | 3.33 |
| Influenza | 31 (6) | 2.95 | 28 (6) | 2.66 |
| Pharyngitis | 31 (6) | 2.95 | 28 (6) | 2.66 |
| Acute sinusitis | 24 (5) | 2.29 | 34 (7) | 3.23 |
| Rhinitis | 26 (5) | 2.48 | 31 (6) | 2.95 |
| Any SAE | 95 (18) | 9.05 | 79 (15) | 7.52 |
| SAEs in ≥1% of patients | ||||
| Worsening asthma | 36 (7) | 3.43 | 30 (6) | 2.85 |
| Nasal polyps | 3 (1) | 0.29 | 0 (0) | 0 |
| Pneumonia bacterial | 3 (1) | 0.29 | 2 (<1) | 0.19 |
| Pneumonia | 3 (1) | 0.29 | 1 (<1) | 0.10 |
| Influenza | 3 (1) | 0.29 | 0 (0) | 0 |
| Osteoarthritis | 1 (<1) | 0.10 | 3 (1) | 0.29 |
| SAEs associated with infections | 16 (3) | 1.52 | 17 (3) | 1.62 |
| Deathsc | 1 (<1) | 0.10 | 2 (<1) | 0.19 |
| Injection-site reactions | 27 (5) | 2.57 | 20 (4) | 1.90 |
| Hypersensitivity AEs | 30 (6) | 2.86 | 19 (4) | 1.81 |
Notes: aTotal on-treatment period (years) across all patients in the specific group. bAs defined in Medical Dictionary for Regulatory Activities version 20.0. cPatients who entered BORA. Ten deaths were reported for patients who received benralizumab in SIROCCO/CALIMA, regardless of whether they entered BORA.
Abbreviations: AE, adverse event; exp, exposure; FAS, full analysis set; Q4W, every 4 weeks; Q8W, every 8 weeks (first three doses Q4W); SAE, serious adverse event.
The most common adverse events reported for SIROCCO/CALIMA patients who received benralizumab and entered BORA were viral upper respiratory tract infection, upper respiratory tract infection, and bronchitis (Table 4, FAS). Worsening asthma was the most common serious adverse event, with an event rate of 3.43 (Q4W) and 2.85 (Q8W) per 100-PYs. There were 10 patients (1%) who had a serious adverse event considered related to benralizumab (Q4W: anaphylactic reaction, hepatitis/multiple organ dysfunction syndrome [same patient], interstitial lung disease, and syncope; Q8W: prostate cancer, chronic kidney disease, worsening asthma, arthralgia, non-cardiac chest pain, and bacterial pneumonia).
Independently adjudicated new malignancies occurred for 7 (1%, event rate 0.46 per 100-PYs) and 5 (1%, event rate 0.32 per 100-PYs) SIROCCO/CALIMA patients who received benralizumab Q4W or Q8W, respectively, regardless of entry into BORA (APS). For the Q8W cohort, malignancy rates were low and similar between the pivotal study and extension periods (n=1 [<1%], event rate 0.13 per 100-PYs vs. n=3 [<1%], event rate 0.48 per 100-PYs, respectively). A similar rate of serious infections occurred for patients who received benralizumab Q4W or Q8W and entered BORA (Table 4, FAS). The most common serious infections for those receiving benralizumab Q8W were bacterial pneumonia, appendicitis, and cellulitis (n=2 [<1%]). Similar rates of serious infections were observed for the Q8W cohort at the end of the pivotal study and extension periods (n=8 [2%], event rate 1.53 per 100-PYs vs. n=9 [2%], event rate 1.70 per 100-PYs). No cases of helminth infections were reported.
Similar percentages of SIROCCO/CALIMA patients discontinued treatment because of adverse events between the two benralizumab cohorts who entered BORA (Table 4, FAS). For patients receiving benralizumab in SIROCCO/CALIMA, regardless of entry into BORA (APS), 27 (3%, event rate 1.95 per 100-PYs) and 26 (3%, event rate 1.85 per 100-PYs) receiving benralizumab Q4W and Q8W, respectively, discontinued treatment during the on-treatment period. The most common reason for discontinuation for the Q8W cohort was urticaria (n=3 [<1%]). There were 10 deaths reported for patients who received benralizumab in SIROCCO/CALIMA, regardless of entry into BORA (APS; n=3 for those who entered BORA; Table 4, FAS), with an equal number reported for both benralizumab Q4W and Q8W cohorts (n=5 [1%], event rate 0.36 per 100-PYs). For patients who initially received benralizumab in SIROCCO/CALIMA, none of the deaths were considered associated with benralizumab; one was related to asthma.9,10,12 Further details on these deaths have been published.9,10,12
Similar percentages of patients who received benralizumab Q4W or Q8W experienced injection-site reactions (Table 4). Hypersensitivity was also comparable between treatment groups. Anti-drug antibodies (ADAs) were expressed by 15% and 17% of the patients who received benralizumab Q4W and Q8W, respectively, with 9% (Q4W) and 13% (Q8W) having neutralizing antibodies (Table S3). Similar expressions of ADAs were observed for patients at EOT for the pivotal and extension study periods. There was no indication that ADA status adversely affected efficacy (Table S3). Low blood eosinophil counts were maintained in the extension period with benralizumab treatment and were slightly greater for patients who were ADA positive than those who were ADA negative (Table S4).
Discussion
Benralizumab is an efficacious treatment for patients with severe, uncontrolled eosinophilic asthma based on results of the SIROCCO, CALIMA, ZONDA, and BORA Phase III studies.9–12 Although there is a strong relationship between eosinophil counts and asthma severity,4–6 it is unclear if there are compensatory mechanisms that could increase asthma severity upon long-term depletion of eosinophils with benralizumab, which acts not only by reducing eosinophil recruitment but also by inducing eosinophil death.7,8 Furthermore, eosinophils are associated with host protection against parasitic, bacterial, and viral infections and have a potential role in the anti-tumor immune response.13,14 Consequently, it is important to understand the long-term efficacy and safety of benralizumab use for patients with severe, uncontrolled eosinophilic asthma.
We present the 2-year integrated analysis for patients treated with benralizumab who entered the BORA safety extension study from the SIROCCO/CALIMA pivotal Phase III studies, in which primary and key secondary endpoints were associated with exacerbation control and lung function.9,10,12 We evaluated maintenance of efficacy and safety for patients who received benralizumab in the pivotal studies and 1 year of treatment in the first year of the BORA study. Our findings complement those in a previous report of the first year of BORA, which specifically addressed efficacy and safety in the year after patients entered BORA and did not include data from the pivotal study period.12 Thus, this current report presents new information on the maintenance of efficacy and safety in the second year of treatment, with safety presented as both cumulative events throughout the 2 years of treatment and relative changes from the first to the second year of treatment.
The benralizumab 2-year integrated analysis results indicate that the efficacy improvements observed in the first year of treatment were maintained during the second year. Over the 2-year period, the crude AER for the benralizumab Q8W cohort with blood eosinophil counts ≥300 cells/µL was 0.56, comparable to that reported individually for SIROCCO (0.65) and CALIMA (0.66).9,10 During the extension period, crude AER was numerically smaller (0.48) than that obtained during the pivotal study period (0.65). Improvements in lung function for the Q8W cohort with blood eosinophil counts ≥300 cells/µL (mean change from baseline in prebronchodilator FEV1) observed at the pivotal study EOT (0.343 L) were maintained in the extension period (0.364 L) and were consistent with those reported in the SIROCCO (0.398 L) and CALIMA (0.330 L) studies.9,10 Similar maintenance of efficacy was found for improvements in ACQ-6 and AQLQ(S)+12 scores. Also, indirectly associated with maintained efficacy, 77% of the patients who received benralizumab in SIROCCO/CALIMA entered BORA and 86% completed treatment in BORA. This was despite the relative burden associated with clinical trial participation and with the acknowledgment that there may be many reasons patients discontinue participation in a clinical trial.
For patients with blood eosinophil counts <300 cells/μL who received benralizumab Q8W, the crude AER over the integrated analysis period was 0.68, indicating a potential long-term benefit for these patients. Possibly, a percentage of these patients may have eosinophilic inflammation of the airways that was not clearly identified through blood eosinophil counts.15–17 It has been reported that patients who do not have elevated blood eosinophil counts, having nasal polyposis, a history of OCS use, exacerbation history, or forced vital capacity <65% of the predicted achieve greater responses to benralizumab than those without these baseline factors.18,19 For patients with blood eosinophil counts <300 cells/μL, AER reductions with benralizumab were 6–33% greater for patients with versus without any of these baseline factors.18 Some of these factors are associated with eosinophilic inflammation and should be considered when choosing benralizumab treatment for patients with blood eosinophil counts <300 cells/μL.
The safety profile for patients at Year 2 was consistent with that at Year 1 of the analysis for all patients, regardless of blood eosinophil counts. Adverse event rates for the Q8W cohort were numerically smaller for the extended period compared with the pivotal study period, and serious adverse event rates were similar across study periods for the APS of patients who received benralizumab in SIROCCO/CALIMA, regardless of entry into BORA. Serious infection rates were similar for the Q8W cohort in the extended period and in the pivotal study period for patients who continued into BORA. In particular, no cases of helminth infections were reported, assuring that reducing eosinophil counts does not impair response to parasitic infections. A low frequency of malignancies was also reported, with event rates of 0.13 per 100-PYs and 0.48 per 100-PYs in the pivotal study and extension periods, respectively, for the Q8W cohort.
Despite extended treatment with benralizumab, there were no apparent increases in ADA concentrations compared with pivotal study EOT, indicating that ADA development is an early event. Furthermore, there was no obvious effect of ADA concentration on efficacy or safety, although there was a slight effect on blood eosinophil counts.
The long-term efficacy and safety of benralizumab findings presented in this study compare favorably to results from two extension studies performed for mepolizumab, a human anti-interleukin monoclonal antibody, for a similar patient population with severe, uncontrolled eosinophilic asthma.20,21 In the COSMOS 52-week open-label extension of the MENSA and SIRIUS trials, patients received mepolizumab 100 mg subcutaneously Q4W with a median treatment exposure of 17.6 months (range, 1–22 months).20 For patients who received mepolizumab in both the initial and extension studies, the percentages of patients with AEs and SAEs during COSMOS were 87% (n=360/414) and 15% (n=64/414), respectively, similar to that observed with benralizumab.20 A similar percentage of these patients experienced exacerbations (46%, n=191/414) as compared with this benralizumab study (49% for benralizumab Q8W, n=157/318), but annual exacerbation rate was greater with mepolizumab (0.90, 95% CI 0.78, 1.04) versus benralizumab Q8W in this study (0.56, 95% CI 0.51, 0.62).20 In the COLUMBA study (open-label extension; patients invited to participate 12‒28 months after completing the DREAM study), patients received mepolizumab 100 mg subcutaneously Q4W for a mean duration of 3.5 years (range, 4 weeks to 4.5 years).21 AEs and SAEs were reported for 94% (n=326/347) and 23% (n=79/347) of patients.21 During COLUMBA, annual exacerbation rates were 0.71 (Week 0–52), 0.82 (Week >52–104), and 0.71 (Week >104–156).
A limitation of this study is the lack of placebo control during the second year of analysis. Although exacerbations were less frequent in the extension period than in the pivotal study period, in the absence of a placebo arm, it is not possible to determine whether the smaller rates relate to an increasing benefit with longer benralizumab treatment. Although payers and patients prefer a shorter treatment period, these 2-year data confirmed the sustained benefit and safety profiles of benralizumab. However, they did not address whether relapse may occur after benralizumab withdrawal. An additional limitation was the potential for selection bias, as patients entered BORA only if they completed their respective treatments in the pivotal studies, and patients who discontinued early may have had different outcomes. Nevertheless, the efficacy values presented are consistent with what was reported as significant (or nominally significant) relative to placebo in the respective pivotal studies.9,10 Likewise, the safety profile, which was similar between patients who received placebo or benralizumab in the pivotal studies,9,10 was consistent with what was reported for Year 2 in this study. Another limitation was the restricted number of patients followed for the full 1-year extension because of the rollover of patients into MELTEMI, a separate open-label, 130-week safety extension study. This also created the potential for selection bias, as patients who entered MELTEMI may have had different outcomes than those who did not enter MELTEMI.
Conclusion
In summary, the 2-year integrated analysis of efficacy and safety results from the SIROCCO, CALIMA, and BORA Phase III studies further supports the use of benralizumab for the treatment of patients with severe, uncontrolled asthma. This analysis will be important in guiding clinician decisions on the long-term use of benralizumab.
Acknowledgments
Writing and editing support, including preparation of the draft manuscript under the direction and guidance of the authors, incorporating author feedback, and manuscript submission, was provided by Alan Saltzman, PhD (JK Associates, Inc., Conshohocken, PA, United States), and Michael A. Nissen, ELS (AstraZeneca, Gaithersburg, MD, United States). This support was funded by AstraZeneca. Some of these data were presented in a poster at the American Thoracic Society (ATS) International Conference, May 17–22, 2019, Dallas, TX, USA, as a poster presentation. The poster abstract was published in American Journal of Respiratory and Critical Care Medicine: 2019;199:A2676. https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2019.199.1_MeetingAbstracts.A2676.
Funding Statement
AstraZeneca and Kyowa Hakko Kirin funded the SIROCCO, CALIMA, ZONDA, and BORA studies. Writing and editing support, including preparation of the draft manuscript under the direction and guidance of the authors, incorporating author feedback and manuscript submission, was funded by AstraZeneca.
Abbreviations
100-PYs, 100-patient-years; ACQ-6, Asthma Control Questionnaire 6; ADA, anti-drug antibody; AER, asthma exacerbation rate; APS, all patients set; AQLQ(S)+12, Asthma Quality of Life Questionnaire [standardized] for 12 years and older; ED, emergency department; EOT, end of treatment; FAS, full analysis set; FEV1, forced expiratory volume in 1 second; ICS, inhaled corticosteroids; LABA, long-acting β2-agonists; OCS, oral corticosteroids; Q4W, every 4 weeks; Q8W, every 8 weeks; SD, standard deviation.
Data-Sharing Statement
Data underlying the findings described in this manuscript may be requested in accordance with AstraZeneca’s data-sharing policy described at https://astrazenecagroup-dt.pharmacm.com/DT/Home.
Author Contributions
JMF, ERB, AB, WWB, GTF, and UJM conceived and designed the study. LB, PB, and UJM acquired the data. All authors made substantial contributions to the analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
JMF is an advisory board member for AstraZeneca, Boehringer Ingelheim, Novartis, Sanofi-Regeneron, reports research grants from AstraZeneca, Sanofi Regeneron, and Teva and has received honoraria for lectures from AstraZeneca, Sanofi Regeneron, Boehringer Ingelheim, GlaxoSmithKline, and Novartis during the conduct of this study. ERB has performed clinical trials through his former employer, the Wake Forest School of Medicine, the University of Arizona, and Genentech, and has served as a paid consultant for AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, MedImmune, Novartis, Regeneron, Sanofi-Aventis, Sanofi Genzyme, and TEVA. AB has received personal fees from Actelion, AstraZeneca, Boehringer Ingelheim, Chiesi Pharmaceuticals, GlaxoSmithKline, Novartis, Regeneron, Roche, and Teva; received grants from Boehringer Ingelheim and GlaxoSmithKline; received non-financial support from Actelion, AstraZeneca, Biogen, Boehringer Ingelheim, Galapagos, Novartis, Chiesi Pharmaceuticals, Roche, and Vertex; and has been an advisory board member for Actelion, AstraZeneca, Boehringer Ingelheim, Chiesi Pharmaceuticals, Gilead, GlaxoSmithKline, Novartis, Regeneron, and Teva outside of the submitted work. WWB reports personal fees from AstraZeneca, Boston Scientific, Genentech, GlaxoSmithKline, Novartis, Sanofi, GlaxoSmithKline, Gossamer Bio, Elsevier, Arrowhead, resTORbio, Medscape and Teva, outside of the submitted work. GTF reports grants, personal fees and non-financial support from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Novartis, Pearl Therapeutics and Sunovion; grants and personal fees from Verona, Theravance, Mylan and Sanofi; grants from Altavant; and personal fees from Innoviva, CSL Behring and Circassia. LB, PB, and UJM are employees of AstraZeneca Pharmaceuticals. The authors report no other conflicts of ineterestin this work.
References
- 1.Global Asthma Network. The global asthma report. 2018. Available from: http://www.globalasthmareport.org/Global Asthma Report 2018.pdf. Accessed October 25, 2019. [Google Scholar]
- 2.Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–373. doi: 10.1183/09031936.00202013 [DOI] [PubMed] [Google Scholar]
- 3.O’Byrne PM, Pedersen S, Schatz M, et al. The poorly explored impact of uncontrolled asthma. Chest. 2013;143(2):511–523. doi: 10.1378/chest.12-0412 [DOI] [PubMed] [Google Scholar]
- 4.Zhang JY, Wenzel SE. Tissue and BAL based biomarkers in asthma. Immunol Allergy Clin North Am. 2007;27(4):623–632. doi: 10.1016/j.iac.2007.09.003 [DOI] [PubMed] [Google Scholar]
- 5.Price D, Wilson AM, Chisholm A, et al. Predicting frequent asthma exacerbations using blood eosinophil count and other patient data routinely available in clinical practice. J Asthma Allergy. 2016;9:1–12. doi: 10.2147/JAA.S97973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Talini D, Novelli F, Bacci E, et al. Sputum eosinophilia is a determinant of FEV1 decline in occupational asthma: results of an observational study. BMJ Open. 2015;5(1):e005748. doi: 10.1136/bmjopen-2014-005748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kolbeck R, Kozhich A, Koike M, et al. MEDI-563, a humanized anti-IL-5 receptor alpha mAb with enhanced antibody-dependent cell-mediated cytotoxicity function. J Allergy Clin Immunol. 2010;125(6):1344–1353. doi: 10.1016/j.jaci.2010.04.004 [DOI] [PubMed] [Google Scholar]
- 8.Pham TH, Damera G, Newbold P, Ranade K. Reductions in eosinophil biomarkers by benralizumab in patients with asthma. Respir Med. 2016;111:21–29. doi: 10.1016/j.rmed.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 9.Bleecker ER, FitzGerald JM, Chanez P, et al. Efficacy and safety of benralizumab for patients with severe asthma uncontrolled with high-dosage inhaled corticosteroids and long-acting β2-agonists (SIROCCO): a randomised, multicentre, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2115–2127. doi: 10.1016/S0140-6736(16)31324-1 [DOI] [PubMed] [Google Scholar]
- 10.FitzGerald JM, Bleecker ER, Nair P, et al. Benralizumab, an anti-interleukin-5 receptor α monoclonal antibody, as add-on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2016;388(10056):2128–2141. doi: 10.1016/S0140-6736(16)31322-8 [DOI] [PubMed] [Google Scholar]
- 11.Nair P, Wenzel S, Rabe KF, et al. Oral glucocorticoid-sparing effect of benralizumab in severe asthma. N Engl J Med. 2017;376(25):2448–2458. doi: 10.1056/NEJMoa1703501 [DOI] [PubMed] [Google Scholar]
- 12.Busse WW, Bleecker ER, FitzGerald JM, et al. Long-term safety and efficacy of benralizumab in patients with severe, uncontrolled asthma: 1-year results from the BORA phase 3 extension trial. Lancet Respir Med. 2019;7(1):46–59. doi: 10.1016/S2213-2600(18)30406-5 [DOI] [PubMed] [Google Scholar]
- 13.Wen T, Rothenberg ME. The regulatory function of eosinophils. Microbiol Spectr. 2016;4(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramirez GA, Yacoub MR, Ripa M, et al. Eosinophils from physiology to disease: a comprehensive review. Biomed Res Int. 2018;2018:9095275. doi: 10.1155/2018/9095275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hastie AT, Moore WC, Li H, et al. Biomarker surrogates do not accurately predict sputum eosinophil and neutrophil percentages in asthmatic subjects. J Allergy Clin Immunol. 2013;132(1):72–80. doi: 10.1016/j.jaci.2013.03.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fowler SJ, Tavernier G, Niven R. High blood eosinophil counts predict sputum eosinophilia in patients with severe asthma. J Allergy Clin Immunol. 2015;135(3):822–824. doi: 10.1016/j.jaci.2014.09.034 [DOI] [PubMed] [Google Scholar]
- 17.Wagener AH, de Nijs SB, Lutter R, et al. External validation of blood eosinophils, FE(NO) and serum periostin as surrogates for sputum eosinophils in asthma. Thorax. 2015;70(2):115–120. doi: 10.1136/thoraxjnl-2014-205634 [DOI] [PubMed] [Google Scholar]
- 18.Bleecker ER, Wechsler ME, FitzGerald JM, et al. Baseline patient factors impact on the clinical efficacy of benralizumab for severe asthma. Eur Respir J. 2018;52(4):1800936. doi: 10.1183/13993003.00936-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.FitzGerald JM, Bleecker ER, Menzies-Gow A, et al. Predictors of enhanced response with benralizumab for patients with severe asthma: pooled analysis of the SIROCCO and CALIMA studies. Lancet Respir Med. 2018;6(1):51–64. doi: 10.1016/S2213-2600(17)30344-2 [DOI] [PubMed] [Google Scholar]
- 20.Lugogo N, Domingo C, Chanez P, et al. Long-term efficacy and safety of mepolizumab in patients with severe eosinophilic asthma: a multi-center, open-label, phase IIIb study. Clin Ther. 2016;38(9):2058–2070. doi: 10.1016/j.clinthera.2016.07.010 [DOI] [PubMed] [Google Scholar]
- 21.Khatri S, Moore W, Gibson PG, et al. Assessment of the long-term safety of mepolizumab and durability of clinical response in patients with severe eosinophilic asthma. J Allergy Clin Immunol. 2019;143(5):1742–1751. doi: 10.1016/j.jaci.2018.09.033 [DOI] [PubMed] [Google Scholar]