Abstract
The past several decades have witnessed growing geographic disparities in life expectancy within the United States, yet the mortality experience of U.S. cities has received little attention. We examine changes in men’s life expectancy at birth for the 25 largest U.S. cities from 1990 to 2015, using mortality data with city of residence identifiers. We reveal remarkable increases in life expectancy for several U.S. cities. Men’s life expectancy increased by 13.7 years in San Francisco and Washington, DC, and by 11.8 years in New York between 1990 and 2015, during which overall U.S. life expectancy increased by just 4.8 years. A significant fraction of gains in the top-performing cities relative to the U.S. average is explained by reductions in HIV/AIDS and homicide during the 1990s and 2000s. Although black men tended to see larger life expectancy gains than white men in most cities, changes in socioeconomic and racial population composition also contributed to these trends.
Keywords: Cities, Life expectancy, United States, HIV/AIDS, Homicide
Introduction
Life expectancy at birth in the United States has risen relatively slowly in the past three decades compared with other high-income countries (Crimmins et al. 2011). Since 1990, American men have gained 4.8 years, and women have gained just 2.6 years (Xu et al. 2016). In contrast, other high-income countries in Europe, East Asia, and Oceania have gained an average of 6.7 years among men and 4.9 years among women (United Nations Population Division 2017). As a result, life expectancy in the United States is now 2.3 years shorter than the average of all high-income countries and shows no signs of catching up (Case and Deaton 2015; United Nations Population Division 2017). U.S. life expectancy at birth has continued to diverge from that of its peers, declining between 2014 and 2017, the first such decline in close to a century (Murphy et al. 2018).
This period has also witnessed growth in both socioeconomic and geographic disparities in life expectancy within the United States. Beginning in the 1980s, there has been a growing divergence in life expectancy across U.S. counties, leading to a gap of more than 20 years between the best- and worst-off counties (Chetty et al. 2016; Dwyer-Lindgren et al. 2017; Ezzati et al. 2008). Similarly, the gap in age-standardized mortality between the U.S. South and the rest of the country widened between 1965 and 2004 (Fenelon 2013), owing to particularly sluggish mortality improvement in the South compared with the West and Northeast. Accompanying these geographic disparities were expanding gaps in life expectancy by educational attainment for both men and women (Ho and Fenelon 2015).
Amid growing geographic and social divergence, there may be some more favorable trends: life expectancy in New York City increased by 3.0 years between 2001 and 2010, more than the 1.7 years gained nationally (Li et al. 2016; Preston and Elo 2014). Importantly, these improvements were accompanied by substantial reductions in racial disparities. The New York City Department of Health and Mental Hygiene attributed this success to the city’s public health investments (Summers et al. 2009). However, the causes of this remarkable growth are likely to be varied and complex (Muennig et al. 2016). Furthermore, it is unknown whether the gains in New York City reflect its specific experience or a broader pattern shared by other major cities.
This study examines the profound and uneven sociodemographic changes occurring in major U.S. cities and their relationship to changes in men’s life expectancy. Our focus is on the experience of major U.S. cities relative to the United States as a whole, during a period of relative stagnation in U.S. life expectancy compared with other high-income countries. We limit our analysis to the 25 largest cities—an understudied population in the growing literature on regional and geographic trends in U.S. mortality. The experience of major cities is also situated within the broader context of increasing rural disadvantage in mortality (Singh and Siahpush 2014) as well as a shifting regional pattern of U.S. mortality (Elo et al. 2018; Fenelon 2013).
Using a mix of mortality data that contain city of residence identifiers and sociodemographic data from the U.S. Census Bureau, we calculate changes in men’s life expectancy in the 25 largest U.S. cities from 1990 to 2015. We then explore the relationship between changes in life expectancy across cities and the uneven resurgence of U.S. cities since 1990. The factors we consider include economic revitalization (as measured by educational attainment and income), reductions in violent crime, declines in HIV/AIDS, racial composition (and race-specific life expectancy), and changing shares of foreign-born. Our findings suggest that changing economic, social, and racial compositions as well as medical innovation (particularly the introduction of effective treatments for HIV/AIDS) have extended life expectancy in America’s largest cities. Our results raise important questions about geographic trends in mortality in the United States and provide the foundation for a fruitful research agenda on contextual contributions to population health in the twenty-first century.
Background
Recent studies have highlighted the growing gap between U.S. divisions, states, counties, rural and urban areas, and metropolitan and nonmetropolitan areas (Chetty et al. 2016; Dwyer-Lindgren et al. 2017; Elo et al. 2018; Fenelon 2013; Montez et al. 2016). However, the mortality experience in the urban core of major U.S. cities has received little attention in this literature (Li et al. 2016; Muennig et al. 2016; Preston and Elo 2014). The studies that have examined large U.S. cities have largely focused on New York City, which experienced substantial improvements in quality of life in recent decades. These studies documented that New York City has seen enormous improvements in life expectancy over the past two to three decades but that these improvements cannot be explained by local public health programs alone (Muennig et al. 2016). Instead, Preston and Elo (2014) demonstrated that mortality improvements in New York City were observed across many causes of death and a variety of subpopulations. Li et al. (2016) indicated that improvements in heart disease and cancer during the 2000s were more salient than in previous years.
Major cities are critical geographic units because the population is concentrated in cities, large cities possess enormous social and economic influence, and cities have undergone substantial change over the past 25 years (Savitch and Kantor 2002). In 1990, 1 in 8 Americans—more than 31 million people—lived in the 25 largest U.S. cities. We discuss four key factors that have impacted cities since 1990 and are particularly salient for life expectancy: economic revitalization, homicide, HIV, and health behaviors.
The Economic Resurgence of American Cities
Quality of life in U.S. cities declined in the decades following the middle of the twentieth century (Beauregard 2003). The population in many large cities peaked in 1950, and subsequent decades saw significant growth in non–central city metropolitan populations (suburbanization) (Hobbs and Stoops 2002). For instance, although the population of Washington, DC (proper) declined by 24 % between 1950 and 1990, the Washington, DC, metropolitan area grew by 183 % (Hobbs and Stoops 2002). Although the central city accounted for 55 % of the metropolitan area population in 1950, it was reduced to less than 15 % of the regional population by 1990 (Hobbs and Stoops 2002). Middle-class white populations left cities for suburbs, aided by racialized housing policies that excluded African Americans from purchasing homes in certain neighborhoods (Freund 2010; Galster and Keeney 1988). At the same time, much of the collective force of public policy investment followed the suburbanization of America’s large metropolitan areas, leaving physical infrastructure and the economic base of many cities neglected by the late twentieth century (Downs 1997; Glaeser and Gottlieb 2006). These trends, combined with economic restructuring, took a toll on the fortunes of many large cities in the 1960s, 1970s, and 1980s (Sassen 1990). Cities with strong industrial pasts were among the hardest hit (Glaeser and Gottlieb 2006).
Many U.S. cities have experienced a remarkable recovery from the urban nadir of the 1980s. Since the late 1980s, median household income and educational attainment have substantially improved in many cities (Curtis 1997; Owens 2016). For example, median household income increased by nearly 60 % in San Francisco between 1990 and 2015, compared with just 10 % growth nationwide. These improvements have been accompanied by renewed population growth in most cities that is being driven by both internal and international migration (Wei and Knox 2014).
Not all cities have benefited equally. In fact, Owens’ (2016) study of city trajectories between 1990 and 2010 found that 52 of the 100 largest U.S. cities saw a decline in an index of economic well-being that combined indicators of total population size, educational attainment, household income, employment, and housing vacancies. Her analysis suggests that cities that replaced their industrial base with professional, technical, and managerial jobs fared better than cities that shifted toward service sector employment. Divergent between-city trends in revitalization and differential subgroup experiences within resurgent American cities may be tied to differential trends in life expectancy between and within cities.
Homicide
Violent crime rates have declined by 50 % nationwide since 1991, and nearly every U.S. city has experienced at least some decrease over the period (Friedman et al. 2017). However, the magnitude of these trends varies across cities (Friedman et al. 2017). Violent crime rates declined by more than 70 % in Boston, Los Angeles, New York City, Chicago, and Washington, DC. In contrast, Baltimore, Detroit, and Memphis saw relatively modest declines or even slight increases.
Homicides tend to occur among younger men aged 15–34 and thus have a significant impact on life expectancy (Centers for Disease Control and Prevention (CDC) 2016). The homicide rate declined from just less than 10 per 100,000 people in the early 1990s to 5.3 in 2016 (CDC 2016). The reasons underlying declines in homicide remain unclear (Levitt 2004). Several candidate explanations—including the rise and cessation of the crack epidemic, changes in policing, and changes in the demographic character of cities—have been considered (Curtis 1997; Fagan et al. 1997; Golub and Johnson 1997; Messner et al. 2007; Rosenfeld et al. 2007). However, no single explanation sufficiently describes the geographic and temporal patterns of homicide reduction.
HIV/AIDS
The HIV/AIDS epidemic came to the United States in 1980–1981 and quickly spread through some of the largest cities. Peaking in 1995 at more than 40,000 annual deaths, the epidemic was notable for causing deaths of mostly younger adults aged 25–44 (CDC 2003). The impacts of the HIV/AIDS epidemic were highly concentrated by geography and were especially strong in particular subpopulations, such as injection drug users, men who have sex with men, and African Americans (Karon et al. 2001). Deaths for HIV/AIDS rose sharply in San Francisco during the 1980s, peaking in the early 1990s (CDC 2003). It was responsible for fully 15 % of all deaths in San Francisco in 1992 and for one in four deaths among men. Among other cities hit by the epidemic were New York City, Baltimore, Seattle, Boston and Washington, DC (CDC 2003). Following the introduction of combination anti-retroviral therapy (ART) and the proliferation of needle exchanges, deaths from HIV/AIDS declined rapidly (Vittinghoff et al. 1999), falling by more than 70 % nationwide in just five years and by 90 % by 2015. For cities suffering disproportionately from the epidemic, the swift reduction in HIV/AIDS mortality may have provided significant benefits to life expectancy.
Health Behaviors: Smoking, Obesity, and Alcohol/Drugs
Public health investments and health-related behaviors have shifted markedly but unevenly since the 1980s and may have contributed to changes in life expectancy. The percentage of U.S. adults who smoke fell from approximately 40 % in 1964 to 25.5 % in 1990 and to 16.8 % in 2014 (Jamal et al. 2015; U.S. Department of Health and Human Services 2014). These changes did not occur evenly across geographic regions, and up to 80 % of the divergence in state-level mortality between 1965 and 2004 can be attributed to differential changes in smoking-related mortality (Fenelon 2013).
At the same time, the mortality impacts of obesity have risen sharply since the 1980s, and obesity is one of the most important reasons for the relatively slow improvement of U.S. life expectancy during this period (Preston et al. 2018). Although the prevalence of obesity has increased in all regions of the United States, variation by region and urban/rural status remains large (Lundeen et al. 2018).
Finally, alcohol- and drug-related mortality are strongly patterned by geography and may contribute to differential life expectancy trends across cities (Monnat 2018).
Socioeconomic and Racial Composition
Contemporaneous to shifting economic fortunes, many cities also experienced large changes in the sociodemographic structure of their populations. The influx of largely white, younger, and higher-income residents to urban centers may have displaced existing low-income and minority populations (Hwang 2015; Timberlake and Johns-Wolfe 2017; Wei and Knox 2014). If populations migrating into cities tend to have higher life expectancy than those migrating out, compositional shifts may give the appearance of rising life expectancy. However, Brummet and Reed (2018), using longitudinally linked census records, observed only a small degree of out- migration among original residents in response to gentrification (a 3 percentage point increase in out-migration in the most gentrifying areas), with out-migration concentrated among low- educated renters and high-educated homeowners. Furthermore, they did not find evidence of declines in the economic well-being of original neighborhood residents, regardless of whether they moved or stayed in response to gentrification. Finally, an increase in the foreign-born fraction of U.S. city populations may have led to increases in life expectancy through compositional change.
Data and Methods
Our mortality data come from public-use and restricted-use Multiple Cause of Death (MCD) microdata files provided through a data use agreement with the National Center for Health Statistics (NCHS). The restricted-use files provide information on state, county, and city of residence of each decedent in each year from 2005 through 2015.1 For the years 1988–2004, we use data from the public-use MCD files that contain city-level identifiers for cities with more than 100,000 residents. We tabulate the number of deaths in each city by sex and age group (0, 1–4, 5–9, …, 80–84, 85+) combined into multiyear periods. The need for aggregating periods comes from the relatively small number of deaths in particular age-sex-city-year cells, particularly for children and adolescents. We use the following periods: 1988–1992, 1993–1997, 1998–2002, 2003–2006, 2007–2010, and 2011–2015. For simplicity, we concentrate on the early period (1988–1992) and the late period (2011–2015) in the description of results. Population denominators come from NCHS bridged-race county population files for coextensive city-counties (same geographic boundaries for city and county), including Washington, DC, and from city population estimates from the U.S. Census Bureau and American Community Survey (ACS) for noncoextensive cities (cities located within a larger surrounding county), obtained through IPUMS at the University of Minnesota (Manson et al. 2017). For noncoextensive cities, we linearly interpolate age-specific population denominators in intercensal years. We also obtain economic and demographic population characteristics of cities in 1990 from U.S. Census Summary File 3 and for 2011–2015 using the five-year ACS estimates.
We focus on the 25 largest U.S. cities by population based on the 1990 census (Table 1). We calculate age-specific death rates for each city by sex and period (Preston et al. 2000). We focus on men’s life expectancy because mortality risk is highly conditioned by gender. However, results are qualitatively similar for women (see section A in the online appendix), although the magnitude of life expectancy change is smaller.
Table 1.
25 largest U.S. cities by population, 1990 census
| Rank | City | State | Total Population | Male Population |
|---|---|---|---|---|
| 1 | New York City | NY | 7,322,564 | 3,884,877 |
| 2 | Los Angeles | CA | 3,485,398 | 1,735,343 |
| 3 | Chicago | IL | 2,783,726 | 1,449,021 |
| 4 | Houston | TX | 1,630,553 | 821,505 |
| 5 | Philadelphia | PA | 1,585,577 | 847,814 |
| 6 | San Diego | CA | 1,110,549 | 544,085 |
| 7 | Detroit | MI | 1,027,974 | 551,160 |
| 8 | Dallas | TX | 1,006,877 | 511,736 |
| 9 | Phoenix | AZ | 983,403 | 495,814 |
| 10 | San Antonio | TX | 935,933 | 485,238 |
| 11 | San Jose | CA | 782,248 | 384,539 |
| 12 | Baltimore | MD | 736,014 | 392,501 |
| 13 | Indianapolis | IN | 731,327 | 383,909 |
| 14 | San Francisco | CA | 723,959 | 361,462 |
| 15 | Jacksonville | FL | 635,230 | 324,864 |
| 16 | Columbus | OH | 632,910 | 327,336 |
| 17 | Milwaukee | WI | 628,088 | 331,251 |
| 18 | Memphis | TN | 610,337 | 325,327 |
| 19 | Washington | DC | 606,900 | 323,930 |
| 20 | Boston | MA | 574,283 | 298,311 |
| 21 | Seattle | WA | 516,259 | 264,217 |
| 22 | El Paso | TX | 515,342 | 268,179 |
| 23 | Cleveland | OH | 505,616 | 268,405 |
| 24 | New Orleans | LA | 496,938 | 266,055 |
| 25 | Nashville-Davidson | TN | 488,374 | 256,665 |
| Total | 31,056,379 | 16,103,544 |
Source: U.S. Census Bureau, 1990 decennial census.
To maintain consistency of the death rate calculation, we use deaths by city of residence rather than city of occurrence partially because the denominator of the death rate calculation includes resident population by age and sex, which means that all deaths ostensibly come from the at-risk resident population. This approach is also consistent with the methods used by NCHS to calculate state-specific life tables (CDC 2016).2 We calculate abridged life tables by sex for each city and the United States as a whole in each period using standard methods to produce life expectancy at birth (Preston et al. 2000).
We also calculate age-specific and age-standardized death rates for selected causes of death based on ICD 9 (1988–1998) and ICD 10 (1999–2015) codes. To examine the contribution of age distribution and causes of death to the change in life expectancy across U.S. cities, we use Arriaga’s (1984) decomposition method. We code causes of death according to meaningful categories of interest, including HIV/AIDS, homicide, lung cancer, other cancers, heart disease, chronic obstructive pulmonary disease (COPD), chronic liver disease, diabetes, and drug overdoses.3
Results
Life Expectancy by City, 1988–2015
Men’s life expectancy at birth by city in each five-year period is shown in Table 2. Cities are sorted by the number of years of life expectancy gained between the early period (1988–1992) and the late period (2011–2015). The largest gains occurred in San Francisco, Washington, DC, and New York City. San Francisco and Washington, DC, each gained 13.7 years between the early and late periods, whereas life expectancy rose by only 4.8 years for men nationwide. In the early period, men in Washington, DC, lagged the national life expectancy by more than 10 years (71.9 vs. 61.7 years) and had the lowest life expectancy of any major city. By the late period, the gap had closed to just 1 year. Likewise, life expectancy in San Francisco trailed the U.S. average by more than 5 years in the early period. By the late period, San Franciscans outlived the nation as a whole by 3.5 years. Life expectancy among New York City men improved from 4 years below the national average to 2.6 years above it. Other cities that exhibited gains in life expectancy substantially above the national average include Los Angeles, Chicago, and Boston. Each gained between 9 and 10 years of life expectancy between the early and late period.4
Table 2.
Men’s life expectancy at birth and years gained in 25 largest U.S. cities: 1988–2015
| 1988–1992 | 1993–1997 | 1998–2002 | 2003–2006 | 2007–2010 | 2011–2015 | Years Gained 1988–2015 | |
|---|---|---|---|---|---|---|---|
| City | |||||||
| San Francisco | 66.4 | 69.7 | 75.0 | 77.3 | 79.0 | 80.1 | 13.7 |
| Washington, DC | 61.7 | 63.6 | 68.2 | 70.3 | 72.8 | 75.4 | 13.7 |
| New York City | 67.5 | 70.6 | 74.6 | 76.5 | 78.0 | 79.3 | 11.8 |
| Los Angeles | 69.5 | 72.3 | 74.8 | 75.8 | 77.7 | 79.1 | 9.5 |
| Chicago | 65.9 | 67.7 | 70.5 | 72.7 | 73.9 | 75.1 | 9.2 |
| Boston | 68.7 | 71.1 | 73.6 | 75.1 | 76.5 | 77.8 | 9.2 |
| New Orleans | 63.9 | 64.6 | 67.4 | 67.8 | 70.2 | 72.6 | 8.7 |
| San Jose | 73.7 | 75.2 | 77.3 | 79.3 | 80.0 | 81.1 | 7.5 |
| Dallas | 68.3 | 70.1 | 72.7 | 73.7 | 74.8 | 75.5 | 7.2 |
| Seattle | 71.5 | 71.7 | 74.6 | 76.6 | 77.5 | 78.6 | 7.1 |
| Philadelphia | 65.4 | 66.3 | 68.8 | 69.7 | 71.2 | 72.4 | 7.0 |
| Houston | 66.9 | 69.2 | 71.5 | 72.6 | 73.4 | 73.8 | 6.9 |
| San Diego | 73.0 | 74.4 | 76.3 | 77.8 | 79.1 | 79.8 | 6.8 |
| Phoenix | 71.2 | 71.4 | 73.0 | 74.5 | 76.4 | 77.7 | 6.6 |
| Detroit | 63.0 | 64.1 | 65.8 | 66.7 | 67.5 | 69.6 | 6.6 |
| Baltimore | 62.9 | 62.0 | 64.3 | 66.2 | 68.3 | 69.4 | 6.4 |
| Memphis | 66.2 | 66.5 | 67.9 | 69.1 | 70.5 | 71.2 | 5.0 |
| Jacksonville | 69.2 | 70.7 | 71.6 | 72.1 | 73.0 | 74.1 | 4.8 |
| Columbus | 69.7 | 70.4 | 71.6 | 72.1 | 73.2 | 74.5 | 4.8 |
| Nashville | 69.3 | 69.7 | 71.3 | 72.2 | 73.2 | 74.1 | 4.7 |
| Cleveland | 65.2 | 66.2 | 68.3 | 68.7 | 69.0 | 69.6 | 4.3 |
| San Antonio | 70.6 | 70.8 | 72.5 | 73.3 | 74.0 | 74.3 | 3.7 |
| El Paso | 72.7 | 73.2 | 74.7 | 75.3 | 76.4 | 76.3 | 3.7 |
| Milwaukee | 69.4 | 69.8 | 70.4 | 71.1 | 72.3 | 72.9 | 3.5 |
| Indianapolis | 69.4 | 69.8 | 70.6 | 71.6 | 72.5 | 72.5 | 3.1 |
| United States | 71.9 | 72.9 | 74.2 | 75.2 | 76.1 | 76.7 | 4.8 |
Sources: Authors’ calculations from restricted-use vital statistics data and U.S. census population enumerations and estimates.
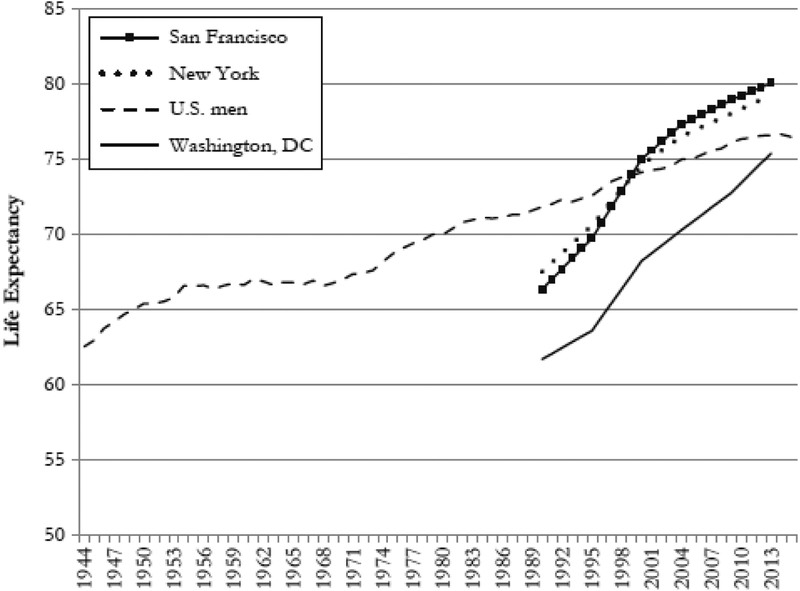
The improvement in men’s life expectancy in San Francisco, Washington, DC, and New York City is particularly remarkable given the 23-year time span. Gains in each city amounted to more than half a year per year during the period. As shown in Fig. 1, it took 71 years for U.S. men’s life expectancy to increase by 13.7 years, the number of years gained since 1990 in San Francisco and Washington, DC (Xu et al. 2016).
Fig. 1.
Men’s life expectancy at birth 1944–2015: United States, San Francisco, New York City, and Washington, DC. Life expectancy at birth for men in Washington, DC, San Francisco, New York City, and the United States as a whole. Data for Washington, DC, San Francisco, and New York City are pooled in five-year periods for 1988–2015. Sources: U.S. life expectancy from Human Mortality Database. Washington, DC, and San Francisco life expectancies are based on authors’ calculations from National Vital Statistics System data.
Overall, 17 of the 25 cities posted life expectancy gains for men that exceeded the national average; the weighted average life expectancy of the 25 cities rose by 8.6 years, from 4 years below the U.S. average to nearly matching the U.S. average. Despite this progress, gains across cities were uneven. In contrast to the significant gains in Washington, DC, other majority African American cities experienced considerably smaller gains. For example, Baltimore, Detroit, Cleveland, and Memphis each gained 7 or fewer years, and life expectancy growth for Cleveland was relatively sluggish (gain of 4.3 years). Other cities in the Midwest also experienced relatively slow gains in life expectancy, including 4.8 years in Columbus, 3.5 years in Milwaukee, and 3.1 years in Indianapolis. Washington, DC, began the period with lower life expectancy than each of these cities (including a 4.5-year deficit with Memphis) but ended the period with a significant advantage over all of them.
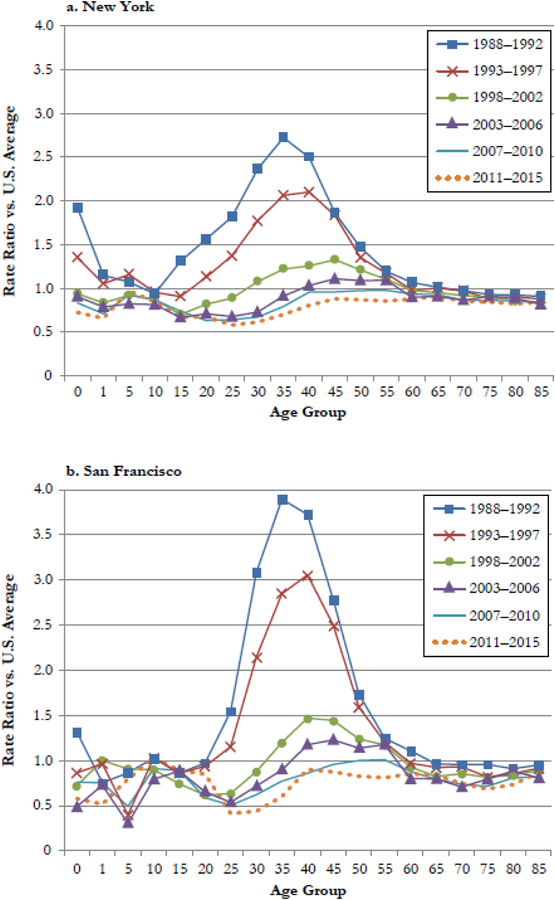
Age-Specific Contributions
Although most deaths occur after age 50 (CDC 2016), the cities experiencing the greatest improvements in life expectancy during this period often did so via improvements in mortality in early adulthood. Men in San Francisco, Washington, DC, and New York City showed 80 % to 90 % reductions in death rates in the 25–44 age range (Fig. 2). This is in contrast to cities showing much less improvement in life expectancy, such as Indianapolis and Milwaukee, which experienced declines of only about 10 % in the 25–44 range. The top performers also showed considerable improvement in infant mortality, posting reductions of 70 % to 80 %. Infant mortality in New York City dropped from 90 % above the national average in the early period to 28 % below the national average in the later period. Age-specific mortality declines by city are shown in Tables A5 and A6, and city-specific declines in infant mortality are shown in Table A7 (online appendix).
Fig. 2.
Men’s age-specific mortality risk relative to the national average by city and period
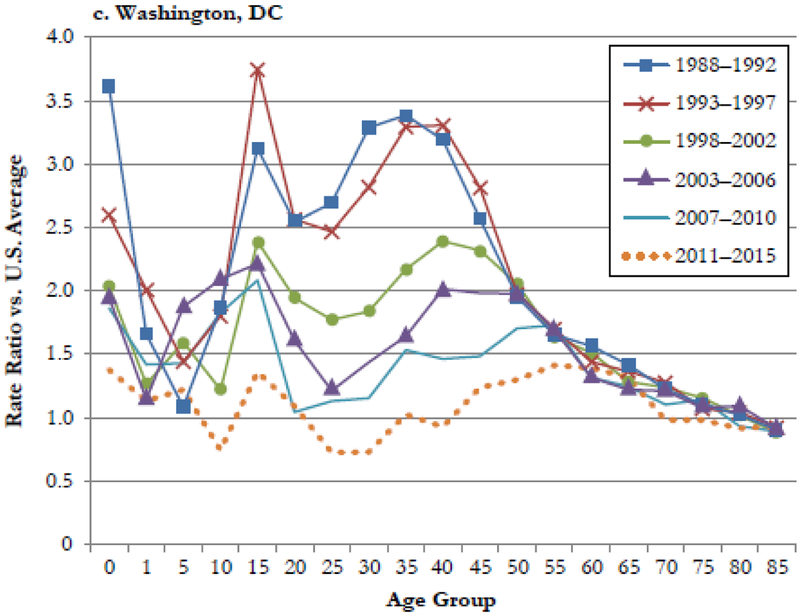
HIV/AIDS and Homicide
In the following sections, we examine the relationship between men’s life expectancy gains across U.S. cities, mortality from major causes of death, and socioeconomic indicators. Panel a of Fig. 3 shows trends in the age-standardized death rates for HIV/AIDS in select cities in each five-year period. In the early period, San Francisco had a considerably higher death rate than any other city, at 250 per 100,000—more than 13 times the national average. New York City, Washington, DC, Baltimore, and Boston also experienced high AIDS death rates in the 1990s. Other cities, such as San Jose, had AIDS death rates similar to the national average. The decline of AIDS deaths in the 1990s had a significant impact on life expectancy in the cities with the highest death rates.
Fig. 3.
Age-adjusted death rate from HIV/AIDS and homicide among men in selected cities, 1988–2015
The cause-of-death decompositions in Table 3 present the contribution of specific causes of death to changes in men’s life expectancy in U.S. cities relative to the national average. As a result of reductions in AIDS mortality among men in San Francisco, their life expectancy grew 4.7 years more than the U.S. average, accounting for 53 % of the 8.8 years gained in San Francisco relative to the United States as a whole. Drops in AIDS–related deaths were responsible for 2 years of the relative gain in Washington, DC (23 % of the relative gain), 1.9 years in New York City (28 % of the relative gain), and 1.3 years in Los Angeles (27 % of the relative gain). Although declines in mortality due to HIV/AIDS contributed to life expectancy gains for all cities relative to the national average, these gains were relatively small in many cities (e.g., 0.35 years in Memphis) that posted life expectancy gains at or below the national average.5 Cause-of-death contributions among women are shown in Table A2 (online appendix).
Table 3.
Cause-of-death contributions to city gains in men’s life expectancy relative to U.S. average, 1988–2015
| Total Gain vs. United States | HIV/AIDS | Homicide | Lung Cancer | Heart Disease | Liver Disease | COPD | Diabetes | Drug Overdoses | Other Cancer | Residual | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| San Francisco | 8.88 | 4.72 | 0.10 | 0.09 | 0.90 | 0.33 | 0.28 | 0.17 | 0.37 | 0.32 | 1.58 |
| Washington, DC | 8.87 | 2.00 | 1.78 | 0.27 | −0.15 | 0.51 | 0.17 | 0.05 | 0.03 | 0.53 | 3.67 |
| New York City | 6.90 | 1.90 | 0.92 | 0.06 | 0.43 | 0.24 | 0.19 | 0.02 | 0.23 | 0.25 | 2.65 |
| Los Angeles | 4.66 | 1.29 | 0.75 | 0.12 | 0.36 | 0.12 | 0.16 | −0.07 | 0.38 | 0.19 | 1.37 |
| Chicago | 4.32 | 0.79 | 0.28 | 0.13 | 0.51 | 0.30 | 0.15 | 0.03 | 0.19 | 0.18 | 1.77 |
| Boston | 4.33 | 1.14 | 0.30 | 0.17 | 1.01 | 0.15 | 0.20 | 0.07 | 0.00 | 0.30 | 0.96 |
| New Orleans | 3.83 | 1.39 | 0.18 | 0.18 | 0.25 | 0.16 | 0.22 | 0.28 | −0.40 | 0.25 | 1.33 |
| San Jose | 2.61 | 0.47 | −0.14 | 0.05 | 0.57 | 0.11 | 0.34 | −0.16 | 0.28 | 0.22 | 0.86 |
| Dallas | 2.33 | 1.21 | 0.91 | 0.23 | −0.08 | 0.05 | 0.11 | 0.05 | 0.09 | 0.07 | −0.31 |
| Seattle | 2.26 | 1.25 | 0.12 | 0.16 | 0.16 | 0.00 | 0.23 | 0.03 | 0.18 | −0.05 | 0.18 |
| Philadelphia | 2.15 | 0.87 | 0.15 | 0.16 | −0.07 | 0.24 | 0.03 | 0.03 | −0.13 | 0.07 | 0.80 |
| Houston | 2.07 | 1.28 | 0.52 | 0.22 | 0.14 | 0.01 | 0.08 | 0.00 | 0.18 | −0.09 | −0.27 |
| San Diego | 1.95 | 1.12 | 0.17 | 0.03 | −0.27 | 0.07 | 0.19 | −0.03 | 0.22 | −0.05 | 0.50 |
| Phoenix | 1.72 | 0.40 | 0.03 | 0.13 | 0.24 | −0.05 | 0.07 | −0.13 | 0.02 | 0.26 | 0.74 |
| Detroit | 1.71 | 0.56 | 0.52 | 0.14 | −0.83 | 0.56 | −0.02 | 0.04 | −0.08 | 0.06 | 0.77 |
| Baltimore | 1.59 | 0.94 | −0.41 | 0.24 | −0.41 | 0.22 | 0.04 | 0.00 | −0.24 | 0.08 | 1.13 |
| Memphis | 0.19 | 0.35 | 0.01 | 0.16 | 0.03 | 0.03 | 0.03 | −0.15 | −0.04 | −0.08 | −0.13 |
| Jacksonville | −0.04 | 0.41 | 0.29 | 0.16 | −0.04 | −0.01 | −0.02 | −0.04 | −0.08 | −0.06 | −0.63 |
| Columbus | −0.08 | 0.42 | −0.39 | 0.17 | 0.22 | −0.06 | −0.09 | −0.06 | −0.24 | 0.15 | −0.21 |
| Nashville | −0.12 | 0.35 | −0.01 | 0.06 | 0.38 | 0.02 | 0.02 | −0.06 | −0.09 | −0.25 | −0.55 |
| Cleveland | −0.53 | 0.43 | −0.07 | 0.02 | 0.13 | −0.01 | −0.14 | −0.06 | −0.43 | −0.10 | −0.30 |
| San Antonio | −1.13 | 0.51 | 0.45 | −0.02 | −0.57 | −0.09 | −0.01 | −0.04 | 0.04 | −0.26 | −1.13 |
| El Paso | −1.19 | 0.20 | 0.06 | −0.05 | −0.42 | −0.29 | 0.05 | −0.11 | 0.37 | −0.30 | −0.71 |
| Milwaukee | −1.38 | 0.43 | −0.07 | −0.10 | −0.53 | 0.03 | 0.01 | 0.02 | −0.24 | −0.16 | −0.75 |
| Indianapolis | −1.77 | 0.33 | −0.39 | 0.07 | −0.42 | −0.07 | −0.19 | 0.04 | −0.31 | −0.11 | −0.69 |
Notes: Numbers shown reflect the number of years of life expectancy gained in each city relative to the U.S. national average from mortality decline from each cause of death. Positive values indicate greater mortality improvement in the focal city than in the United States as a whole. Negative numbers indicate either less mortality improvement or greater mortality increase in the city relative to the United States as a whole. Cause contributions are calculated using Arriaga’s method (1984). Cause-of-death codes used are shown in Table B3, online appendix.
Trends in homicide death rates for selected cities are shown in panel b of Fig. 3. In Washington, DC, homicide mortality has declined by nearly 75 % since the early period, from a high of 95 per 100,000 to just 25 per 100,000. New York City and Los Angeles registered similarly large declines but from lower baselines than Washington, DC. Relative to the national average, the decline in homicide was responsible for a relative increase in life expectancy of 1.8 years in Washington, DC, 0.9 years in New York City and Dallas, and 0.75 years in Los Angeles. However, not all cities with high homicide rates in the early period experienced a decline over time. For instance, the homicide rate in Detroit declined during the 1990s but has remained stable since 2000. Baltimore has shown no sustained change in homicide since the early period. In contrast, Milwaukee and Cleveland experienced relative increases in homicide mortality during this period, which dragged down life expectancy in comparison with the national average.
Homicide declines reflect one component of the more generalized trend in reduced crime rates in large central cities (Sharkey et al. 2017). Additional life expectancy gains are likely attributable to progress against violent crime more broadly given that exposure to violence exacerbates poor outcomes in high-poverty urban neighborhoods (Friedson and Sharkey 2015). Figure B5 in the online appendix shows a strong positive relationship between the magnitude of declines in violent crime and the number of years of life expectancy gained between 1990 and 2015. Overall, the combination of declines in AIDS and homicide deaths explained 54 % (4.8 years) of the relative life expectancy gains among men in San Francisco, 43 % (3.8 years) in Washington, DC, and 41 % (2.8 years) in New York City.
Health Behaviors
Cause-of-death contributions can also be used to infer the role of health-related behaviors, such as cigarette smoking, obesity, and alcohol and drug use (Stokes and Preston 2017). Heart disease, lung cancer, and diabetes make relatively small contributions to gains in life expectancy for the top-performing cities, and the pattern of the contribution of these causes of death across cities does not match overall gains. The contribution of diabetes to gains in life expectancy in each city relative to the United States as a whole tends to be very small (ranging from −0.16 years to 0.28 years) and not consistently positive. Similarly, the contribution of lung cancer is relatively small (ranging from −0.10 years to 0.27 years).6 Both smoking and obesity may contribute to heart disease mortality, which likewise does not seem to drive city gains in life expectancy relative to the U.S. average. In contrast to these causes of death, both liver disease and drug overdoses made contributions to city life expectancy gain in a pattern that matched national gains in life expectancy.
Socioeconomic and Racial Composition
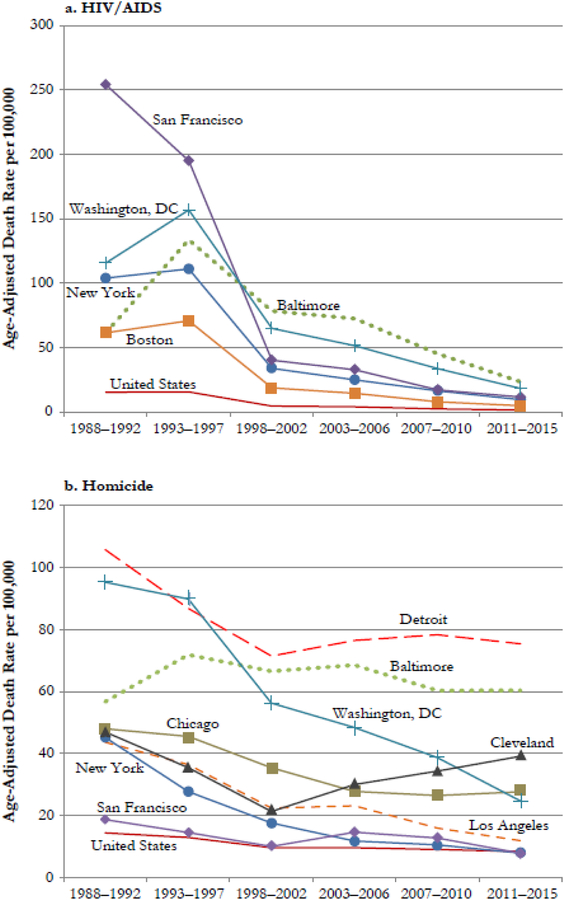
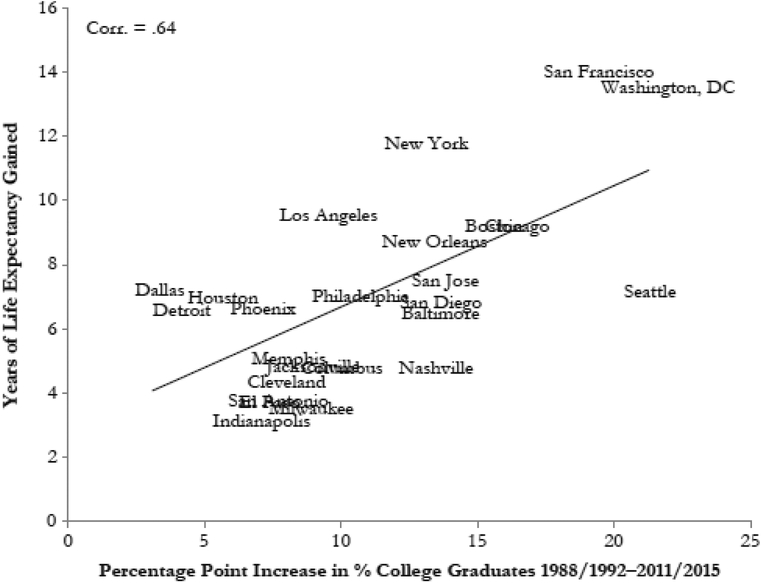
Figure 4 shows the relationship between the change in the percentage of adults aged 25 or older with a college degree and the number of years gained in men’s life expectancy between the early and late period. There is a strong relationship (correlation = .64) between increases in the college-educated population and the number of years of life expectancy gained. A similar relationship exists between the change in the median income relative to the national average and years gained (see Fig. B2, online appendix). These graphs suggest that cities that experienced relatively large shifts in socioeconomic composition also experienced relatively large gains in life expectancy, although we are unable to calculate education-specific life expectancy by city.7
Fig. 4.
Years of life expectancy gained and change in college graduates by city, 1988–2015. Sources: Life expectancy based on authors calculations from National Vital Statistics System data. Increase in college graduates from 1990 decennial census and 2011–2015 ACS.
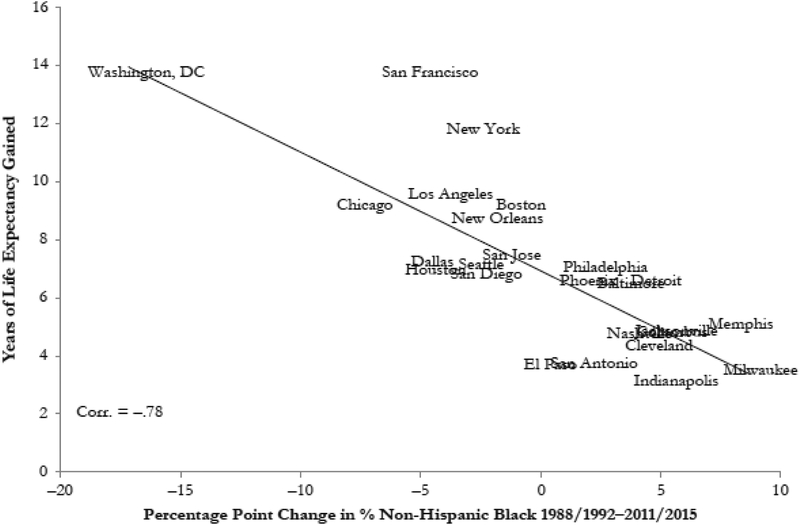
Socioeconomic shifts during this period were also frequently accompanied by changing racial and ethnic composition. Data from the census and ACS indicate steady declines in the population of African Americans in many cities concomitant with increases in the Hispanic and Asian populations. For the most part, declines in the black population of major U.S. cities did not occur alongside corresponding increases in the non-Hispanic white population. In fact, only Washington, DC, experienced an increase in the percentage of the population that was non-Hispanic white between 1990 and 2015 (from 27 % to 36 %). The population composition of Washington, DC, shifted from 65 % black in the early period to just 48 % in the later period. The cities of Chicago and San Francisco also experienced significant declines in the percentage black (totals by city shown in Table B1, online appendix). Figure 5 shows the relationship between the change in the percentage black and the number of years gained, which is strongly negative (correlation = −.78). These results suggest that gains in life expectancy occurred alongside the declining African American shares in many cities. In contrast, cities that saw substantial gains in percentage black (e.g., Milwaukee, Memphis, and Indianapolis) were often those with the most sluggish gains in life expectancy.
Fig. 5.
Years of life expectancy gained and change in percentage black by city, 1988–2015. Sources: Life expectancy is based on authors calculations from National Vital Statistics System data. Change in percentage black from 1990 decennial census and 2011–2015 ACS.
The 1990s and 2000s saw a rapid increase in the foreign-born population in the United States. The foreign-born have a documented longevity advantage over the native-born in the United States (Blue and Fenelon 2011). Analyses in section A of the online appendix demonstrate that although cities with larger foreign-born populations have longer life expectancies (Fig. B3), we find no relationship between changes in the percentage of the population that is foreign-born and gains in life expectancy (Fig. B4).
Life Expectancy by Race
The strong correlation between changes in the racial composition and changes in life expectancy (see Fig. 5) may have occurred as a result of migration patterns that displaced populations with lower life expectancy and saw increases in populations with higher life expectancy. However, the figure does not provide evidence of whether gains in life expectancy were shared across racial groups during the period.
In Table 4, we present life expectancy for black and white men in each city in the early and late periods (results for women shown in Table A4, online appendix).8 Calculating race-specific life expectancy by city is complicated by differences in the collection of racial data on the death certificate and the U.S. Census. A 1997 Office of Management and Budget directive mandated the collection of multiple race categories in federal data products, which effectively broke the existing single-race time series. Bridged-race population estimates, which translate multiple race categories to one of the four race categories used prior to 1997, are available for eight coextensive city-counties (Washington, DC, San Francisco, Baltimore, Jacksonville, Philadelphia, New York City, New Orleans, and Nashville). For the remaining 17 cities (noncoextensive), we use an adjustment method that applies the bridged population pattern from the surrounding county (see section C of the online appendix for details).
Table 4.
Men’s life expectancy trends by race for selected cities 1988–1992 and 2011–2015
| Black | White | |||||
|---|---|---|---|---|---|---|
| 1988–1992 | 2011–2015 | Years Gained | 1988–1992 | 2011–2015 | Years Gained | |
| Coextensive City-County | ||||||
| Washington, DC | 57.67 | 69.77 | 12.10 | 72.01 | 83.54 | 11.53 |
| New York City | 63.09 | 77.77 | 14.68 | 68.77 | 78.80 | 10.03 |
| San Francisco | 59.43a | 69.91a | 10.49 | 64.34 | 79.43 | 15.09 |
| Philadelphia | 60.93 | 69.96 | 9.02 | 69.00 | 73.53 | 4.54 |
| Baltimore | 59.83 | 67.21 | 7.38 | 67.88 | 72.71 | 4.83 |
| Jacksonville | 62.70 | 72.12 | 9.42 | 71.23 | 75.01 | 3.77 |
| New Orleans | 61.02 | 68.88 | 7.86 | 68.82 | 77.77 | 8.95 |
| Nashville | 64.62 | 71.50 | 6.88 | 71.90 | 75.94 | 4.03 |
| Noncoextensive | ||||||
| Boston | 65.95 | 77.35 | 11.40 | 69.37 | 77.48 | 8.12 |
| Los Angeles | 59.69 | 70.93 | 11.23 | 70.47 | 79.44 | 8.97 |
| Phoenix | 64.58a | 74.70 | 10.12 | 71.45 | 77.83 | 6.38 |
| Chicago | 59.82 | 68.58 | 8.76 | 69.38 | 78.15 | 8.77 |
| San Diego | 67.80 | 76.12a | 8.32 | 73.15 | 79.83 | 6.68 |
| San Jose | 68.46a | 76.77a | 8.32 | 72.74 | 79.06 | 6.33 |
| El Paso | 69.55a | 77.29a | 7.74 | 72.71 | 76.36 | 3.65 |
| Dallas | 63.05 | 69.97 | 6.92 | 70.01 | 77.32 | 7.31 |
| Columbus | 65.41 | 72.19 | 6.78 | 70.96 | 75.21 | 4.26 |
| Detroit | 62.04 | 68.60 | 6.57 | 65.50 | 70.87a | 5.37 |
| Houston | 62.35 | 68.59 | 6.24 | 68.20 | 75.42 | 7.22 |
| Memphis | 62.83 | 68.70 | 5.87 | 69.89 | 75.43 | 5.54 |
| San Antonio | 66.06a | 71.89 | 5.83 | 70.82 | 74.33 | 3.51 |
| Cleveland | 62.41 | 68.08 | 5.67 | 67.38 | 70.82 | 3.43 |
| Seattle | 66.46a | 71.96a | 5.50 | 71.80 | 79.35 | 7.55 |
| Milwaukee | 65.10 | 69.49 | 4.38 | 71.12 | 75.10 | 3.99 |
| Indianapolis | 65.35 | 69.44 | 4.09 | 70.67 | 73.70 | 3.03 |
| United States | 64.50 | 72.30 | 7.80 | 72.70 | 76.70 | 4.00 |
Notes: Race-specific life expectancy is calculated using deaths from Multiple Cause of Death (MCD) files and population data from NCHS bridged-race files and U.S. Census population estimates. Bridged-race population estimates predict race identification on death certificates in order to allow calculation of death rates by race. Estimates are produced only for counties, so only coextensive city-counties use complete bridged-race population data. Population data for other cities are based on an adjusted method that applies the bridging pattern from the surrounding county (see online appendix, section C, for more details).
Figures are based on less than 50,000 annual residents and should be interpreted with caution.
As with overall life expectancy gains, San Francisco, Washington, DC, and New York City experienced the largest gains among both blacks and whites (Table 4). Black men gained 14.6 years in New York City, 12.1 years in Washington, DC, and 10.5 years in San Francisco. Likewise, white men gained 10.0 years in New York City, 11.5 years in Washington, DC,9 and 15.1 years in San Francisco. Additionally, we find gains in black men’s life expectancy of more than 11 years in Boston and Los Angeles. In contrast, many other cities experienced only modest gains in black life expectancy. For example, black men in Baltimore, Detroit, and Milwaukee gained fewer years than black men nationwide during this period, and had life expectancy at least 2.5 years less than the national average for black men.
Although whites still outlive blacks nationally and in nearly every city considered in the late period, Table 4 also demonstrates substantial convergence in life expectancy between blacks and whites. Nationally, there was a 3.8-year reduction in the black-white gap from 1990 to 2015. Boston nearly completely eliminated the 3.4-year gap that existed in the early period. New York City reduced its gap by 4.7 years. However, some cities witnessed increasing black-white disparities. For example, Seattle’s gap increased by 2 years, and San Francisco experienced a 4.6-year widening in the gap, to nearly 10 years.
Discussion
In the past 25 years, there has been a significant resurgence in the economic, social, and physical well-being of urban America. America’s major cities—characterized by large economies, strong cultural institutions, and infrastructure—have shown remarkable improvements in life expectancy during this period. Three cities stand out in their improvement in life expectancy from 1990 to the present: men in New York City, Washington, DC, and San Francisco gained more than 11 years of life expectancy in less than 25 years. Men’s life expectancy in these cities increased by more than one-half year per year during this period, with the most rapid gains occurring during the late 1990s. Between the five-year periods of 1993–1997 and 1998–2002, life expectancy increased by 5.3 years in San Francisco, 4.6 years in Washington, DC, and 4 years in New York City. It has taken 71 years for U.S. men’s life expectancy to increase by the same number of years gained in Washington, DC, and San Francisco since 1990. Slightly behind these top performers are other successful cases: specifically, Los Angeles, Chicago, and Boston each gained 9–10 years of life expectancy during this period. These gains are particularly significant when placed in the context of U.S. men’s life expectancy as a whole, which increased by fewer than 5 years from 1988–1992 to 2011–2015.
Overall, 17 of the 25 largest cities experienced greater gains in life expectancy than the national average. The favorable trend seen in major U.S. cities relative to the national average reflects the broader trend of diverging life expectancy between rural and urban areas in the United States (Singh and Siahpush 2014). Indeed, many rural counties have seen almost no improvement in life expectancy since the mid-1980s (Ezzati et al. 2008; Institute for Health Metrics and Evaluation 2016), a period of tremendous improvements in America’s largest cities. The widening urban/rural gap in health and mortality is also manifested in the growing regional divergence in mortality outcomes (Fenelon 2013); specifically, the southern states have fallen increasingly far behind the Northeast and West Coast (Population Reference Bureau 2018). The surging life expectancy of many large cities, particularly those on the East and West Coasts, are not isolated trends but are instead reflections of broader processes of geographic inequality that have unfolded over the past three to four decades.
The encouraging trends in many cities have occurred alongside more concerning developments in others, including Baltimore, Detroit, Milwaukee, Indianapolis, and Cleveland. A particularly concerning case is Baltimore, which exhibits the lowest life expectancy of any major U.S. city, remaining under 70 years for men. In contrast with its near neighbor Washington, DC, Baltimore has experienced significantly less favorable trajectories of economic opportunity and growth in recent years and is one of the few large cities to see below-average performance in measures of economic prosperity (Shearer et al. 2017). These trends are likely to have manifested in trajectories of health, well-being, and life expectancy.
Explanations for Remarkable Life Expectancy Gains in Large Cities
Reductions in mortality due to HIV/AIDS made a significant contribution to life expectancy gains in most cities, although this effect was particularly large in San Francisco, Washington, DC, and New York City. The public policy response to the HIV/AIDS epidemic was arguably delayed relative to the severity of its impacts. San Francisco’s gay community, particularly gay men of color, were the hardest hit population by the epidemic, with more than 40 % being diagnosed with AIDS by 1994 (Katz 1997). Activists claimed that the Reagan Administration’s reluctance to tackle rising AIDS mortality reflected homophobia and racism given the demographics of communities most burdened by the epidemic (Francis 2012). As a result, citizen activism was key in developing policies to curb HIV infection, including the street-based needle exchange program Prevention Point, which began in 1988 (Watters and Clark 1994). A key feature of this movement was its local character, which resulted in heterogeneous responses across cities. In the 1990s, technological developments played a bigger role.
The development of highly active ART had a nearly immediate impact on the death rate from HIV, and ultimately led to a greater than 90 % drop in deaths among men in many of the hardest-hit cities (CDC 2016; Kaplan et al. 2000). Declines in mortality owing to this new technology resulted in significant life expectancy gains, including 4.7 additional years of life expectancy gained in San Francisco relative to the United States as a whole.
Declines in violent crime that occurred between the early 1990s and the present also had a major impact. However, the nationwide reduction in violent crime masks large divergences among U.S. cities: although some cities have seen enormous decreases in violence, others have remained near their 1990s levels. Crime reduction has been identified as a key contributor to improvements in life expectancy in New York (Messner et al. 2007), and the benefits are especially concentrated in high-violence, low-income neighborhoods (Sharkey et al. 2017). Our results demonstrate that these trends were also observed in other cities. Cities with very successful reductions in crime rates—specifically, Los Angeles, Chicago, Boston, and Dallas, and Washington, DC—are also those that tended to experience large gains in life expectancy, both for black and for white populations. Cities that have experienced smaller declines or increases in violent crime—such as Milwaukee, Cleveland, Indianapolis, and Memphis—have seen the smallest life expectancy gains (see Fig. B5 in the online appendix for this relationship). We are unable to attribute this relationship to the causal effect of declining crime rates. However, cities with large reductions in homicide deaths experienced larger overall gains in life expectancy compared with cities with small to no reductions. One notable exception to this pattern is San Francisco, which experienced large increases in life expectancy but little relative change in homicide death rates.
The experience of many large cities with violent crime and HIV/AIDS during the 1990s is important to view within the broader context of geographic trends in mortality in the United States. The municipal responses to the violent crime wave and the AIDS crisis in New York City were particularly effective (Preston and Elo 2014), but our results indicate that other cities may have implemented similar approaches with similar results. The declines in homicide and HIV mortality in many cities were notable both for their magnitude as well as for their speed. These successes are relevant within the current context of growing urban-rural inequalities. Economic and health indicators in nonmetropolitan areas of the United States have diverged from those of large cities during same period, reflecting at least in part the drug overdose epidemic (Monnat 2018). However, coordinated efforts to reduce the mortality burden of HIV/AIDS and homicide, and their successes, may offer a promising roadmap for addressing the drug overdose crisis that has negatively impact life expectancy in the South and Appalachia (Rigg et al. 2018). Perhaps relatedly, top-performing cities also tended to experience more favorable trends in liver disease and drug overdose mortality than the U.S. average.
Although cigarette smoking and obesity together account for a large fraction of adult deaths in the United States, and have contributed to regional trends in U.S. mortality (Fenelon 2013; Montez et al. 2016; Tencza et al. 2014), we do not find strong evidence that they are driving the gains in life expectancy for U.S. cities. Smoking reduction policies, such as indoor bans and cigarette taxes, began as city ordinances in many states, subsequently impacting state-level policy (Montez et al. 2017; Shipan and Volden 2006). However, these city-specific differences do not appear to be related to differential changes in life expectancy (see Table A12, online appendix). Obesity also appears to play very little role in the trends observed, despite the fact that obesity prevalence nearly doubled nationwide over the study period (Fryar et al. 2018). Our data cannot directly assess the role of obesity, but we find that obesity-related causes of death—including heart disease and diabetes—make relatively small contributions to city gains in life expectancy relative to the United States as a whole. Additionally, although deaths related to smoking and obesity largely occur at later ages (Fenelon 2013; Preston et al. 2018), life expectancy gains in the top-performing cities were largely driven by improvements in early adulthood and younger ages.
Socioeconomic and Racial Composition
At the city level, changes in population composition can have significant implications for changes in life expectancy. We find that changes in the educational and racial distribution of cities were associated with changes in life expectancy. Cities that saw the largest increases in college graduates (e.g., San Francisco and Washington, DC) and/or the largest decreases in the black population (e.g., Chicago and Washington, DC) also tended to be the places with the largest gains in life expectancy. Conversely, cities with relatively modest increases in college graduates and increases in the black population (e.g., Indianapolis and Milwaukee) experienced smaller life expectancy gains than the national average. These associations raise the possibility that the remarkable gains in life expectancy that we observe were not shared by all population subgroups. This finding is consistent with county-level evidence suggesting that economic and social characteristics are sufficient to explain differences in mortality between rural and urban counties (Spencer et al. 2018). However, we cannot be certain that these associations reflect a causal relationship between compositional change and life expectancy change.
We examine life expectancy trends separately by race to determine whether urban life expectancy gains are occurring unequally for blacks and whites. In the top-performing cities—San Francisco, New York City, and Washington, DC—life expectancy grew by similarly large amounts for blacks and whites. Black men’s life expectancy also increased by more than a decade in Boston, Los Angeles, and Phoenix. Furthermore, in most cities, black men gained more years of life expectancy than white men during the observation period despite the fact that white populations exhibited greater increases in levels of education and income than black populations in most cities (Table B2, online appendix). New York City and Boston saw the black-white gap significantly reduced or eliminated. Finally, the cities with the smallest overall gains in life expectancy (Milwaukee, Cleveland, and Indianapolis) also tended to have the smallest overall gains among both blacks and whites. These results do not rule out the possibility that city life expectancy increases have at least in part reflected changing population compositions, but they do indicate that gains are not simply concentrated among whites.
Our results add to a larger literature concerned with documenting and explaining heterogeneous economic development across U.S. cities since the 1980s (e.g., Florida 2003; Porter 2000; Sweeney and Feser 1998). Our results suggest that U.S. cities have had not only uneven economic growth but also uneven trends in life expectancy. Two proximate mechanisms could explain our results. The first is a compositional shift in which successful cities experienced an influx of populations with relatively low mortality risk and a decline in populations with relatively high mortality risk. The second mechanism is real improvements in life expectancy shared by all populations. Our race-specific results are suggestive that all populations within successful cities experienced gains and that migration cannot explain all the heterogeneity across cities, but our results are clearly not definitive.
One potential explanation for the pattern of city improvements involves the long-run strength and character of local institutions. Albeit certainly debated, institutions are potentially a necessary antecedent (and not the result of) long-run development (Acemoglu et al. 2001). The six top-performing cities—San Francisco, New York City, Los Angeles, Chicago, Boston, and Washington, DC—stand out as international centers of cultural and economic activity and have long histories of strong amenities and commensurate institutional infrastructure. Although many of these cities experienced periods of decline during the 1970s and 1980s, their existing stock and character of cultural, social, and economic institutions may have provided the infrastructure necessary to successfully adjust to economic realignment, violent crime waves, and other public health and social crises (Florida 2014). Strong and diverse economic, cultural, and social institutions may have been instrumental in helping cities address the HIV/AIDS epidemic and early 1990s crime wave. In terms of economic development as well as life expectancy, the role of both formal and informal institutions may be to provide the flexible resources necessary to address structural shifts in the economy and to respond to threats to public health (Padgett and Powell 2012; Storper 2013).
We do not find that changes in foreign-born populations were associated with life expectancy gains. Although foreign-born populations tend to live longer than the native-born (Blue and Fenelon 2011), changes in the relative size of foreign-born populations were not significantly related to city life expectancy gains. That we did not find this relationship does not negate the possibility that the changing composition of the foreign-born population may have contributed to gains in cities with large immigrant populations. As foreign-born populations have shifted from older European-born individuals to younger individuals from Latin America and Asia (Kandel 2011; Singh and Hiatt 2006), life expectancy may have increased for the foreign-born as a result of changing composition. However, Preston and Elo (2014) found smaller life expectancy gains among the foreign-born than among the U.S.-born in New York City from 1990 to 2010.
Limitations
Our analysis has limitations that reflect our reliance on vital statistics and our focus on subnational geographies. Our observation period begins in 1988, which may miss trends from the 1980s. Table A8 (online appendix) extends the life expectancy calculations back to 1980 and shows similar results, although many of the top-performing cities lost ground during the 1980s. Our focus on trends among men in large U.S. cities is intended to highlight more discernible trends, but the overall pattern of city life expectancy gains is similar among women. We present companion analyses for women in section A of the online appendix. Our results suggest that socioeconomic and racial composition changes likely contributed to changes in city life expectancy, but we are unable to directly quantify the contribution of changing educational or income distributions of city populations. However, Table B2 in the online appendix indicates that socioeconomic compositional shifts were not always straightforward increases in high-SES populations coupled with declines in low-SES population
Because our data come from vital statistics and are based on city of residence at the time of death, we cannot determine individuals’ length of residence in their city at the time of death. As a result, changes in residence leading up to death—such as entry into long-term care institutions—could potentially bias estimates of mortality at older ages, particularly if nursing homes tend to cluster outside of cities. However, this bias is unlikely to impact our estimates of years gained relative to the United States as a whole for most cities given that these gains tend to be driven by relative improvements at younger ages.
Conclusion
One of the most remarkable social trends of the past three decades in the United States is the substantial changes seen in large central cities. The return of population growth after decades of decline has occurred alongside neighborhood revitalization, reduced racial residential segregation, and changing economic opportunities, but widening within-city income inequalities (Chetty et al. 2016; Shearer et al. 2017). Along with these trends has come extraordinary improvement in the life expectancy of city populations, and concomitantly a widening mortality gap between urban and rural America (Preston and Elo 2014; Singh and Siahpush 2014). The favorable life expectancy trends in many major cities runs in contrast to the corresponding trend in the United States as a whole, where life expectancy has increasingly fallen behind that of other high-income countries (Avendano and Kawachi 2014). American cities have something valuable to offer policymakers interested in identifying solutions to the underperformance of U.S. life expectancy. Cities should occupy a key part of the future research agenda on improving population health, and work should focus on isolating the factors responsible for the remarkable gains in top-performing cities.
Supplementary Material
Acknowledgments
We acknowledge infrastructure support from the Maryland Population Research Center P2C Award (P2C-HD041041). We are grateful to Isaac Sasson for helpful comments.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Data for state, county, and city of residence were public use for units with more than 100,000 residents in the MCD file from 1959–2004 and were removed in 2005 at the request of state vital statistics agencies. We requested geographic identifiers for the years 2005–2015 from NAPHSIS and received data from NCHS through a data use agreement.
Residential change among older adults prior to death could bias estimates of mortality risk for central cities, particularly if long-term care institutions are differentially located inside or outside central cities, and if these location patterns have changed over time. However, this is unlikely to substantively impact our results, largely because old-age mortality makes little contribution to gains in life expectancy over this period in cities relative to the United States as a whole.
Table B3 in the online appendix lists the ICD codes used for each cause of death.
The starting year of 1990 was chosen to reflect the beginning of sociodemographic changes in many large cities. In Tables A8 (men) and A9 (women) of the online appendix, we present life expectancy estimates for 1979–1981 (centered on 1980) as well.
It is likely that deaths from HIV/AIDS were underenumerated during the early period given the relative recency of the epidemic (Preston and Elo 2014). Evidence for this is that “Other Infectious Diseases” also make significant contributions to the gains in life expectancy for many of the cities with high mortality from AIDS. As a result, the total contributions of HIV/AIDS in Table 3 likely understate the total contribution. It is unclear whether the undercounting of HIV/AIDS deaths varies across cities.
A more formal assessment of the role of cigarette smoking in Table A12 (online appendix) supports the finding that smoking’s contribution to city-specific gains was likely small.
U.S. death certificates added indicators of educational attainment until 1989, but data were reported from only 21 states. By 2015, still only 49 states were reporting educational attainment information on death certificates. Furthermore, population denominators by age, sex, and education are estimated using the ACS and are subject to large sampling error. As a result, we are unable to directly calculate life expectancy by educational group within cities.
For consistency over time, we calculate life expectancy for whites and blacks, including Hispanics. Changes over time in the identification of Hispanic origin may make it difficult to obtain comparable estimates of life expectancy for non-Hispanic whites and non-Hispanic blacks for cities in 1988–1992 and 2011–2015.
The life expectancy of white men and women in Washington, DC, in the late period is particularly notable. Whites in Washington, DC, outlive U.S. white men by 6.8 years and U.S. white women by 5.8 years. In fact, in Washington, DC, life expectancy among white men is 2.5 years above the leading country globally (Iceland, at 80.9 years) for white men, and that among white women is 0.7 years above the leading country (Japan, at 86.7 years).
References
- Acemoglu D, Johnson S, & Robinson JA (2001). The colonial origins of comparative development: An empirical investigation. American Economic Review, 91, 1369–1401. [Google Scholar]
- Arriaga EE (1984). Measuring and explaining the change in life expectancies. Demography, 21, 83–96. [PubMed] [Google Scholar]
- Avendano M, & Kawachi I (2014). Why do Americans have shorter life expectancy and worse health than do people in other high-income countries? Annual Review of Public Health, 35, 307–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauregard RA (2003). Voices of decline: The postwar fate of U.S. cities. New York, NY: Routledge. [Google Scholar]
- Blue L, & Fenelon A (2011). Explaining low mortality among US immigrants relative to native-born Americans: The role of smoking. International Journal of Epidemiology, 40, 786–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brummet Q, & Reed D (2018). Gentrification and the location and well-being of original neighborhood residents. Unpublished manuscript. Retrieved from https://www.aeaweb.org/conference/2019/preliminary/paper/y7ZD9E9K
- Case A, & Deaton A (2015). Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences, 112, 15078–15083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2003). Compressed Mortality, 1979–1998 [CDC WONDER Database]. Hyattsville, MD: National Center for Health Statistics; Accessed from https://wonder.cdc.gov/cmf-icd9.html [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2016). Underlying Cause of Death, 1999–2015 [CDC WONDER Database]. Hyattsville, MD: National Center for Health Statistics; Accessed from http://wonder.cdc.gov/ucd-icd10.html [Google Scholar]
- Chetty R, Stepner M, Abraham S. Lin S, Scuderi B, Turner N, … Cutler D (2016). The association between income and life expectancy in the United States, 2001–2014. JAMA, 315, 1750–1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Preston SH, & Cohen B (2011). Explaining divergent levels of longevity in high-income countries. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Curtis R (1997). The improbable transformation of inner-city neighborhoods: Crime, violence, drugs, and youth in the 1990s. Journal of Criminal Law and Criminology, 88, 1233–1276. [Google Scholar]
- Downs A (1997). The challenge of our declining big cities. Housing Policy Debate, 8, 359–408. [Google Scholar]
- Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, Morozoff C, Mackenbach JP, van Lenthe FJ, … Murray CJL (2017). Inequalities in life expectancy among US counties, 1980 to 2014: Temporal trends and key drivers. JAMA Internal Medicine, 177, 1003–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo IT, Hendi A, Ho J, & Preston S (2018, April). Trends in US mortality by region and metropolitan-nonmetropolitan continuum between 1990 and 2015. Paper presented at the annual meeting of the Population Association of America, Denver, CO. [Google Scholar]
- Ezzati M, Friedman AB, Kulkarni SC, & Murray CJL (2008). The reversal of fortunes: Trends in county mortality and cross-county mortality disparities in the United States. PLoS Medicine, 5, e66 10.1371/journal.pmed.0050066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagan J, Zimring FE, & Kim J (1997). Declining homicide in New York City: A tale of two trends. Journal of Criminal Law and Criminology, 88, 1277–1324. [Google Scholar]
- Fenelon A (2013). Geographic divergence in mortality in the United States. Population and Development Review, 39, 611–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florida R (2003). Cities and the creative class. City & Community, 2, 3–19. [Google Scholar]
- Florida R (2014). The creative class and economic development. Economic Development Quarterly, 28, 196–205. [Google Scholar]
- Francis DP (2012). Deadly AIDS policy failure by the highest levels of the US government: A personal look back 30 years later for lessons to respond better to future epidemics. Journal of Public Health Policy, 33, 290–300. [DOI] [PubMed] [Google Scholar]
- Freund DMP (2010). Colored property: State policy and white racial politics in suburban America. Chicago, IL: University of Chicago Press. [Google Scholar]
- Friedman M, Grawert AC, & Cullen J (2017). Crime trends 1990–2016. New York, NY: Brennan Center for Justice, New York University School of Law. [Google Scholar]
- Friedson M, & Sharkey P (2015). Violence and neighborhood disadvantage after the crime decline. Annals of the American Academy of Political and Social Science, 660, 341–358. [Google Scholar]
- Fryar CD, Carroll MD, & Ogden CL (2018). Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–62 through 2015–2016 [Health e-Stats]. Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Galster GC, & Keeney WM (1988). Race, residence, discrimination, and economic opportunity: Modeling the nexus of urban racial phenomena. Urban Affairs Review, 24, 87–117. [Google Scholar]
- Glaeser EL, & Gottlieb JD (2006). Urban resurgence and the consumer city. Urban Studies, 43, 1275–1299. [Google Scholar]
- Golub AL, & Johnson BD (1997). Crack’s decline: Some surprises across U.S. cities (Research in Brief Series). Washington, DC: National Institute of Justice, Office of Justice Programs, U.S. Department of Justice. [Google Scholar]
- Ho JY, & Fenelon A (2015). The contribution of smoking to educational gradients in U.S. life expectancy. Journal of Health and Social Behavior, 56, 307–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobbs F, & Stoops N (2002). Demographic trends in the 20th century (U.S. Census Bureau, Census 2000 Special Reports, Series No. CENSR-4). Washington, DC: U.S. Government Printing Office. [Google Scholar]
- Hwang J (2015). Gentrification in changing cities: Immigration, new diversity, and racial inequality in neighborhood renewal. Annals of the American Academy of Political and Social Science, 660, 319–340. [Google Scholar]
- Institute for Health Metrics and Evaluation. (2016). US health map. Seattle, WA: Institute for Health Metrics and Evaluation; Available from http://vizhub.healthdata.org/subnational/usa [Google Scholar]
- Jamal A, Homa DM, O’Connor E, Babb SD, Caraballo RS, Singh T, … King BA (2015). Current cigarette smoking among adults—United States, 2005–2014. Morbidity and Mortality Weekly Report, 64, 1233–1240. [DOI] [PubMed] [Google Scholar]
- Kandel WA (2011). The U.S. foreign-born population: Trends and selected characteristics (Congressional Research Service Report for Congress No. R41592). Washington, DC: Congressional Research Service. [Google Scholar]
- Kaplan JE, Hanson D, Dworkin MS, Frederick T, Bertolli J, Lindegren MS, … Jones JL (2000). Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretroviral therapy. Clinical Infectious Diseases, 30(Suppl. 1), S5–S14. [DOI] [PubMed] [Google Scholar]
- Karon JM, Fleming PL, Steketee RW, & De Cock KM (2001). HIV in the United States at the turn of the century: an epidemic in transition. American Journal of Public Health, 91, 1060–1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz MH (1997). AIDS epidemic in San Francisco among men who report sex with men: Successes and challenges of HIV prevention. Journal of Acquired Immune Deficiency Syndrome, 14(Suppl. 2), S38–S46. [DOI] [PubMed] [Google Scholar]
- Levitt SD (2004). Understanding why crime fell in the 1990s: Four factors that explain the decline and six that do not. Journal of Economic Perspectives, 18(1), 163–190. [Google Scholar]
- Li W, Maduro GA, & Begier EM (2016). Increased life expectancy in New York City, 2001–2010: An exploration by cause of death and demographic characteristics Journal of Public Health Management & Practice, 22, 255–264. [DOI] [PubMed] [Google Scholar]
- Lundeen EA, Park S, Pan L, O’Toole T, Matthews K, & Blanck HM (2018). Obesity prevalence among adults living in metropolitan and nonmetropolitan counties—United States, 2016. Morbidity and Mortality Weekly Report, 67, 653–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manson S, Schroeder J, Van Riper D, & Ruggles S (2017). IPUMS National Historical Geographic Information System: Version 12.0 [Database]. Minneapolis: University of Minnesota; 10.18128/D050.V12.0 [DOI] [Google Scholar]
- Messner SF, Galea S, Tardiff KJ, Tracy M, Bucciarelli A, Piper T, … Vlahov D (2007). Policing, drugs, and the homicide decline in New York City in the 1990s. Criminology, 45, 385–414. [Google Scholar]
- Monnat SM (2018). Factors associated with county-level differences in U.S. drug-related mortality rates. American Journal of Preventive Medicine, 54, 611–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez JK, Hayward MD, & Wolf DA (2017). Do U.S. states’ socioeconomic and policy contexts shape adult disability? Social Science & Medicine, 178, 115–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez JK, Zajacova A, & Hayward MD (2016). Explaining inequalities in women’s mortality between U.S. States. SSM—Population Health, 2, 561–571. 10.1016/j.ssmph.2016.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muennig P, Masters R, Vail D, & Hakes J (2016). The effects of New York City’s coordinated public health programmes on mortality through 2011. International Journal of Epidemiology, 46, 1239–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy SL, Xu J, Kochanek KD, & Arias E (2018). Mortality in the United States, 2017 (NCHS Data Brief No. 328). Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
- Owens A (2016, November). Urban revitalization in U.S. cities and neighborhoods, 1990 to 2010. Paper prepared for the 21st Century Cities Initiative Symposium, Johns Hopkins University, Baltimore, MD Retrieved from http://21cc.jhu.edu/wp-content/uploads/2017/07/owens_21cc_neighborhood_transformation_final.pdf [Google Scholar]
- Padgett JF, & Powell WW (2012). The emergence of organizations and markets. Princeton, NJ: Princeton University Press. [Google Scholar]
- Population Reference Bureau. (2018). Declines in adult death rates lag in the U.S. south. Washington, DC: Population Reference Bureau; Retrieved from https://assets.prb.org/prb17/mortality/index.html [Google Scholar]
- Porter ME (2000). Location, competition, and economic development: Local clusters in a global economy. Economic Development Quarterly, 14, 15–34. [Google Scholar]
- Preston SH, & Elo IT (2014). Anatomy of a municipal triumph: New York City’s upsurge in life expectancy. Population and Development Review, 40, 1–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston SH, Heuveline P, & Guillot M (2000). Demography: Measuring and modeling population processes. New York, NY: Wiley-Blackwell. [Google Scholar]
- Preston SH, Vierboom YC, & Stokes A (2018). The role of obesity in exceptionally slow US mortality improvement. Proceedings of the National Academy of Sciences, 115, 957–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rigg KK, Monnat SM, & Chavez MN (2018). Opioid-related mortality in rural America: Geographic heterogeneity and intervention strategies. International Journal of Drug Policy, 57, 119–129. [DOI] [PubMed] [Google Scholar]
- Rosenfeld R, Fornango R, & Rengifo AF (2007). The impact of order- maintenance policing on New York City homicide and robbery rates: 1988–2001. Criminology, 45, 355–384. [Google Scholar]
- Sassen S (1990). Economic restructuring and the American city. Annual Review of Sociology, 16, 465–490. [Google Scholar]
- Savitch HV, & Kantor P (2002). Cities in the international marketplace: The political economy of urban development in North America and western Europe. Princeton, NJ: Princeton University Press. [Google Scholar]
- Sharkey P, Torrats-Espinosa G, & Takyar D (2017). Community and the crime decline: The causal effect of local nonprofits on violent crime. American Sociological Review, 82, 1214–1240. [Google Scholar]
- Shearer R, Friedhoff A, Shah I, & Berube A (2017). Metro monitor: An index of inclusive economic growth in the 100 largest U.S. metropolitan areas (Metropolitan Policy Program Report). Washington, DC: Brookings Institution. [Google Scholar]
- Shipan CR, & Volden C (2006). Bottom- up federalism: The diffusion of antismoking policies from U.S. cities to states. American Journal of Political Science, 50, 825–843. [Google Scholar]
- Singh GK, & Hiatt RA (2006). Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreign-born populations in the United States, 1979–2003. International Journal of Epidemiology, 35, 903–919. [DOI] [PubMed] [Google Scholar]
- Singh GK, & Siahpush M (2014). Widening rural-urban disparities in life expectancy, U.S., 1969–2009. American Journal of Preventive Medicine, 46, e19–e29. [DOI] [PubMed] [Google Scholar]
- Spencer JC, Wheeler SB, Rotter JS, & Holmes GM (2018). Decomposing mortality disparities in urban and rural U.S. counties. Health Services Research, 53, 4310–4331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes A, & Preston SH (2017). The contribution of rising adiposity to the increasing prevalence of diabetes in the United States. Preventive Medicine, 101, 91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storper M (2013). Keys to the city: How economics, institutions, social interaction, and politics shape development. Princeton, NJ: Princeton University Press. [Google Scholar]
- Summers C, Cohen L, Havusha A, Sliger F, & Farley T (2009). Take care New York 2012: A policy for a healthier New York City. New York: New York City Department of Health and Mental Hygiene. [Google Scholar]
- Sweeney SH, & Feser EJ (1998). Plant size and clustering of manufacturing activity. Geographical Analysis, 30, 45–64. [Google Scholar]
- Tencza C, Stokes A, & Preston S (2014). Factors responsible for mortality variation in the United States: A latent variable analysis. Demographic Research, 31, 27–70. 10.4054/DemRes.2014.31.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timberlake JM, & Johns-Wolfe E (2017). Neighborhood ethnoracial composition and gentrification in Chicago and New York, 1980 to 2010. Urban Affairs Review, 53, 236–272. [Google Scholar]
- U.S. Department of Health and Human Services. (2014). The health consequences of smoking—50 years of progress: A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. [Google Scholar]
- United Nations Population Division. (2017). World population prospects: 2017 revision. New York, NY: United Nations Department of Economic and Social Affairs, Population Division. [Google Scholar]
- Vittinghoff E, Scheer S, O’Malley P, Colfax G, Holmberg SD, & Buchbinder SP (1999). Combination antiretroviral therapy and recent declines in AIDS incidence and mortality. Journal of Infectious Diseases, 179, 717–720. [DOI] [PubMed] [Google Scholar]
- Watters JK, & Clark GL (1994). Syringe and needle exchange as HIV/AIDS prevention for injection drug users. JAMA, 271, 115–120. [PubMed] [Google Scholar]
- Wei F, & Knox PL (2014). Neighborhood change in metropolitan America, 1990 to 2010. Urban Affairs Review, 50, 459–489. [Google Scholar]
- Xu J, Murphy SL, Kochanek KD, & Arias E (2016). Mortality in the United States, 2015 (NCHS Data Brief No. 267). Hyattsville, MD: National Center for Health Statistics. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.