Abstract
Pituitary adenylate cyclase activating polypeptide (PACAP) is an evolutionarly conserved neuropeptide which is produced by various neuronal and non-neuronal cells, including cartilage and bone cells. PACAP has trophic functions in tissue development, and it also plays a role in cellular and tissue aging. PACAP takes part in the regulation of chondrogenesis, which prevents insufficient cartilage formation caused by oxidative and mechanical stress. PACAP knockout (KO) mice have been shown to display early aging signs affecting several organs. In the present work, we investigated articular cartilage of knee joints in young and aged wild-type (WT) and PACAP KO mice. A significant increase in the thickness of articular cartilage was detected in aged PACAP gene–deficient mice. Amongst PACAP receptors, dominantly PAC1 receptor was expressed in WT knee joints and a remarkable decrease was found in aged PACAP KO mice. Expression of PKA-regulated transcription factors, Sox5, Sox9 and CREB, decreased both in young and aged gene deficient mice, while Sox6, collagen type II and aggrecan expressions were elevated in young but were reduced in aged PACAP KO animals. Increased expression of hyaluronan (HA) synthases and HA-binding proteins was detected parallel with an elevated presence of HA in aged PACAP KO mice. Expression of bone related collagens (I and X) was augmented in young and aged animals. These results suggest that loss of PACAP signaling results in dysregulation of cartilage matrix composition and may transform articular cartilage in a way that it becomes more prone to degenerate.
Keywords: Aggrecan, Collagen expression, Sox9, Sox5, Sox6, Hyaluronic acid
Introduction
Articular cartilage is a unique type of connective tissue in the skeletal system with very poor regenerative capacity. Major factors behind this phenomenon are its avascular, aneural nature and the postmitotic character of adult chondrocytes. This tissue covers the articular surface of synovial joints providing frictionless gliding surface and shock absorption during locomotion (Redondo et al. 2018). High water content of the extracellular matrix (ECM) and the specific collagen fibre orientation pattern is partly responsible for the resilience, weight bearing capacity and flexibility of the tissue (Redondo et al. 2018). In the superficial layer of articular cartilage, a proliferation zone can be identified, which has an important function in maintaining the elasticity of articular surface (Antons et al. 2018). Mature articular cartilage is composed of a specific ECM with dominantly collagen type II fibres, which run in a specific arcade-like orientation, and collagen type IX and XI associate to the core of the fibres in a healthy collagen network. The ground substance of cartilage ECM is rich in proteoglycans (PG) such as aggrecan (Laasanen et al. 2003). The glycosaminoglycan hyaluronic acid (HA) is another essential component of the ECM in articular cartilage as it forms a specific network with the PGs and binds high amounts of water. In the deep layers of articular cartilage (hypertrophic zone and calcification zone), ECM becomes calcified providing a tissue with intermediate biomechanical properties interconnecting articular cartilage and subchondral bone. In this region, chondrocytes are terminally differentiated hypertrophic cells which subsequently undergo apoptosis and the whole tissue serves as a template for trabecular bone formation (Zevenbergen et al. 2018). If any of the components mentioned above are downregulated or the balance in their expression is disturbed, cartilage homeostasis can become severely impaired (Li et al. 2018). In pathological conditions, such as inflammation, oxidative stress or increased mechanical force, the composition of cartilage-specific ECM can be disintegrated and cartilage degeneration may occur (Poulet and Staines 2016).
Secretion of cartilage-specific molecules is regulated by various signaling pathways in developing articular cartilage. Activation of PKA plays a crucial role in this process (Zakany et al. 2002) and can phosphorylate Sox9 or CREB transcription factors (Zakany et al. 2005). More active, phosphorylated forms of these transcription factors are transported to the nuclei and induce the expression of aggrecan and collagen type II. Inhibition of PKA leads to decreased cartilage formation (Zakany et al. 2001; Zakany et al. 2002) primarily via the lower activation of Sox9. Besides Sox9, other members of the SoxE family can also be activated in cartilage formation such as Sox5 and Sox6 (Liu and Lefebvre 2015). Alterations in the expression of the latter two transcription factors leads to a modified, pathologically deformed skeleton and impaired cartilage formation (Lefebvre et al. 2001). Although protein kinase A (PKA) is a key regulator in cartilage formation or regeneration, several other pathways have also been shown to participate. The importance of hedgehog (HH) (Juhasz et al. 2015b), ERK (Zakany et al. 2005) or protein kinase C (PKC) signaling (Matta et al. 2011) is unquestionable. Certain members of the Ser/Thr phosphatases such as protein phosphatase 2A (PP2A) (Zakany et al. 2001) and PP2B (Zakany et al. 2005) are also proven to play a regulatory role in proper cartilage formation. Although the regulatory factors in chondroprogenitor cell differentiations are being characterized, there are still numerous signaling connections not clarified. Amongst these, pituitary adenylate cyclase activating polypeptide (PACAP) is a recently identified player.
PACAP was identified and isolated from the central nervous system (CNS) by Miyata et al. (1989). It has two biologically active forms, PACAP 1-38 and PACAP 1-27, which are evolutionarily well conserved (Vaudry et al. 2009). The neuropeptides have three major G protein coupled receptors, namely PAC1, VPAC1 and VPAC2. PAC1 receptor has the highest affinity to the neuropeptide, and the activation of the receptor triggers adenylate cyclase activity leading to increased concentration of intracellular cAMP and ultimately activates PKA signaling (Gourlet et al. 1997). A positive role of PACAP has been shown in in vitro cartilage formation (Juhasz et al. 2014a), and its protective role has been proven against oxidative stress (Juhasz et al. 2015a; Juhasz et al. 2014a) and mechanical force induced damage (Juhasz et al. 2015b; Szentleleky et al. 2019). Furthermore, PACAP receptor expression has been shown in osteoarthritic cartilage (Giunta et al. 2015), and a pivotal function of PACAP has also been demonstrated in bone formation (Jozsa et al. 2018; Juhasz et al. 2014b). Differentiation of other peripheral cells and organs can be related to proper PACAP signaling such as development of sperms (Reglodi et al. 2018c), teeth (Fulop et al. 2018; Sandor et al. 2014) and brain (Vaudry et al. 2009). On the other hand, lack of PACAP influences aging processes in different tissues (Reglodi et al. 2018b) and is related to accumulation of amyloid deposits (Reglodi et al. 2018b). Lack of the neuropeptide also modulates the vasomotor response of arteries (Ivic et al. 2017) and retina functions (Kovacs-Valasek et al. 2017) during aging.
Although there are some studies on PACAP in aging, no experimental data is available on the regulation of cartilage aging. Cells of the hyaline cartilage have extremely long lifespan but little is known about their signaling alterations in aging. As accelerated aging has been demonstrated in PACAP gene–deficient mice, we investigated the in vivo signaling alterations in young and aged wild-type (WT) and PACAP knock out (KO) mice.
Materials and methods
Animals
Generation and maintenance of the PACAP-deficient mice on the CD1 background have been described in detail (Hashimoto et al. 2001). They were backcrossed for at least ten generations with the CD1 strain. Genotype was tested with PCR reactions. For the experiments, we sacrificed 3-month-old (“young”) and 1-year-old (“aged”) wild-type (WT, n = 20–20) and homozygous PACAP-deficient (PACAP KO, n = 20–20) mice. Animals were fed and watered ad libitum, under light/dark cycles of 12/12 h. Hind limbs were removed after sacrificing the mice with an overdose of pentobarbital sodium (100 mg/kg bw). All procedures were performed in accordance with the ethical guidelines approved by the University of Pécs (permission number: BA02/2000-15024/2011).
Staining procedure
Knee joints were dissected, and after additional tissues were removed, samples were washed in PBS three times and fixed in a 4:1 mixture of absolute ethanol and 40% formaldehyde. Joints were decalcified in 4% EDTA for 4 weeks until bones became soft. Then samples were dehydrated in ascending alcohol row and embedded in paraffin. Five-micrometre-thick serial sections were made. After rehydration haematoxylin-eosin (HE) (Sigma-Aldrich, MO, USA) and dimethylmethylene blue (DMMB) (Sigma-Aldrich, MO, USA), stainings were performed. All staining protocols were carried out according to the instructions of manufacturer. Photomicrographs were taken using DP74 camera (Olympus Corporation, Tokyo, Japan) on Olympus Bx53 microscope (Olympus Corporation, Tokyo, Japan).
Cartilage thickness measurement
Measurement of mean thickness of cartilage on a convex segment
For the measurement of articular cartilage thickness, a customized mathematical formula was used. A circular arc that best fits to the surface of the cartilage was constructed in Adobe Illustrator19.0.0 (Adobe Inc., San Jose, CA, USA) with the help of the SubScribe plug-in (Astute Graphics Limited, UK). Two arbitrary perpendicular lines (radiuses, r) were then drawn from this arc, defining the α angle and the segment of the cartilage used for the measurement. Both α and r were measured in pixels in Adobe Illustrator. Length of the scale bar was measured as well for calculating the conversion ratio from pixels to micrometres (Fig. 1a). Area of the bound segment of the cartilage was measured using the ImageJ 1.40 g freeware freehand selection tool. Thickness () was defined as the difference of the radius of the outer and inner circles of an annulus that had an outer arc conforming to the surface of the cartilage and the area of which equals that of the portion of cartilage bound by the radiuses. Thus, A was the area of the annulus sector of angle α and was calculated as follows:
Fig. 1.
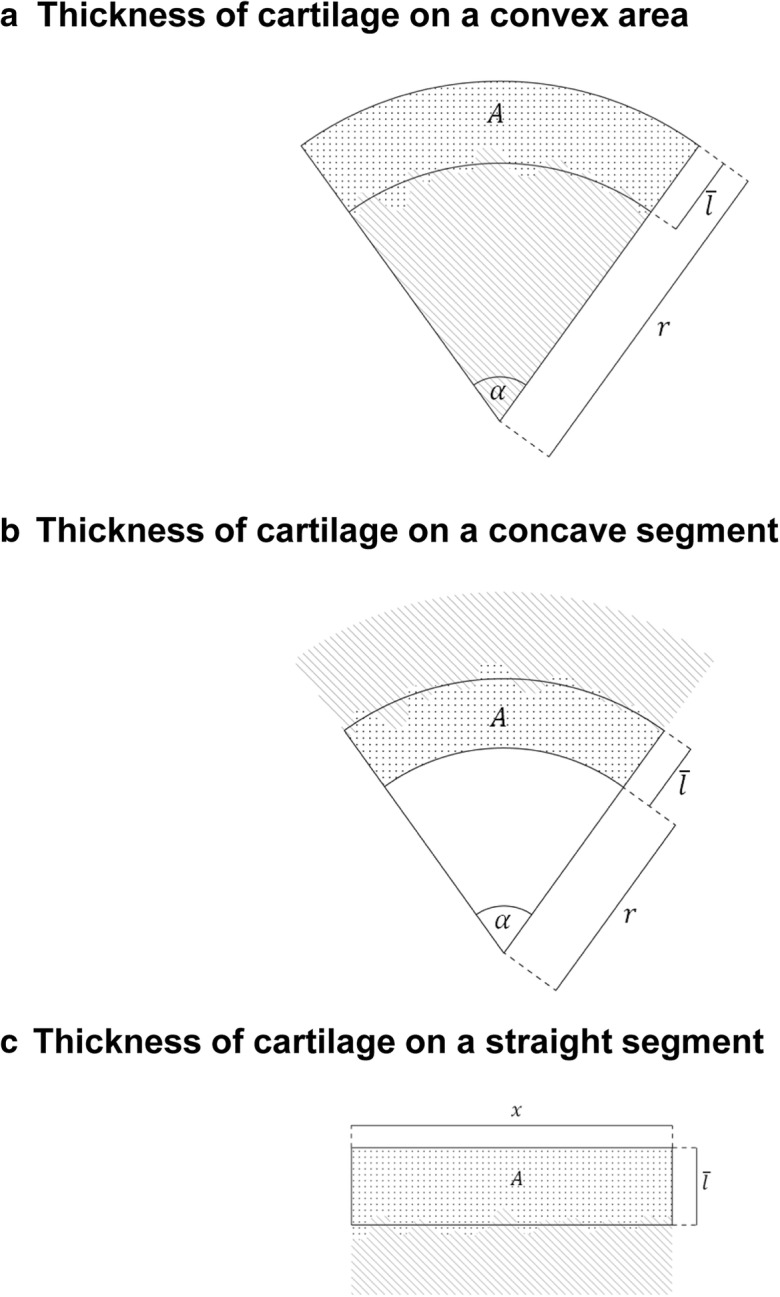
Measurement of mean thickness of cartilage. Convex segment (a): the mean thickness () of the cartilage (dotted area) is the difference of the outer and inner radius of the annulus segment that has an area equal to the area (A) of the cartilage segment of the same α angle. Mean thickness can be calculated with the formula for the area of an annulus segment. The striped area represents subchondral bone. r—outer radius of the constructed annulus segment. Concave segment (b): measuring the thickness of cartilage on a concave segment. Dotted and striped areas represent cartilage and subchondral bone, respectively. A—area of the cartilage segment of α, —mean thickness, r—inner radius of the constructed annulus segment. Straight segment (c): measuring the thickness of cartilage on a straight segment. Dotted and stripped areas represent cartilage and subchondral bone, respectively. A—area of the cartilage segment, —mean thickness, x—width of the constructed rectangle and the selected segment of cartilage
After rearranging and solving the quadratic equation for , the thickness of the cartilage is converted to micrometres.
Measurement of mean thickness of cartilage on a concave segment
Essentially, the same process was carried out, with some changes made to the equation (Fig. 1b).
Measuring mean thickness of cartilage on a straight segment
Thickness () was the height of the rectangle that had an area equal to that of and the same width (x) as the selected segment of cartilage (Fig. 1c).
Immunohistochemistry
Knee joints were dissected, and additional tissues were removed. Joints were washed in PBS three times and fixed in a 4:1 mixture of absolute ethanol and 40% formaldehyde for 24 h. Joints were decalcified in 4% EDTA for 4 weeks until bones became soft. Then, samples were dehydrated in graded ethanol series and embedded in paraffin. Five micrometres of serial sections were made. Sections were rehydrated in descending alcohol row and washed in PBST (phosphate-buffered saline supplemented with 1% Tween-20) three times. Nonspecific binding sites were blocked in PBST supplemented with 1% bovine serum albumin (BSA, Amresco LLC, Solon, OH, USA) at 37 °C for 30 min in a humidified-chamber.
For collagen typeX detection, a monoclonal anti-collagen type X (Sigma-Aldrich, MO, USA) at a dilution of 1:500 was used at 4 °C overnight. Primary antibody was visualized with anti-mouse Alexa555 secondary antibody (Life Technologies Corporation, Carlsbad, CA, USA) at a dilution of 1:1000. Slides were mounted in Vectashield Hard Set mounting medium (Vector Laboratories, Peterborough, England).
Hyaluronic acid (HA) was detected by using a biotinylated HA-binding complex in 5 μg/mL concentration (bHABC, kindly provided by R. Tammi and M. Tammi, Department of Anatomy, University of Kuopio, Kuopio, Finland) at 4 °C overnight. The reaction was visualized with Streptavidin-Alexa555 (2 μg/mL, Invitrogen Corporation, Carlsbad, CA, USA) for fluorescence microscopy. Tissues were mounted in Vectashield Hard Set mounting medium (Vector Laboratories, Ltd. Peterborough, UK).
Photomicrographs of collagen type X immunohistochemistry were taken using an Olympus DP72 camera on a Nikon Eclipse E800 microscope (Nikon Corporation, Tokyo, Japan). Images were acquired using cellSense Entry 1.5 software (Olympus, Shinjuku, Tokyo, Japan) with constant camera settings to allow comparison of fluorescent signal intensities. Images of Alexa555 were overlaid using Adobe Photoshop version 10.0 software.
RT-PCR analysis
Articular cartilage from knee joints was isolated under microscope, and samples were kept in RNAlater (Sigma-Aldrich MO, USA). Tissues were cryo-ground in liquid nitrogen and dissolved in Trizol (Applied Biosystems, Foster City, CA, USA) and kept at − 70 °C for 24 h, and after the addition of 20% RNase-free chloroform, samples were centrifuged at 4 °C at 10,000×g for 15 min. Samples were incubated in 500 μL of RNase-free isopropanol at − 20 °C for 1 h; then, total RNA was harvested in RNase free water and stored at − 20 °C. The assay mixture for reverse transcriptase reaction contained 2 μg RNA, 0.112 μM oligo(dT), 0.5 mM dNTP and 200 units of High Capacity RT (Applied Bio-Systems, Foster City, CA, USA) in 1× RT buffer. For the sequences of primer pairs and further details of polymerase chain reactions, see Table 1. Amplifications were performed in a thermal cycler (Labnet MultiGene™ 96-well Gradient Thermal Cycler; Labnet International, Edison, NJ, USA) in a final volume of 11 μL (containing 1 μL forward and reverse primers [0.4 μM], 0.5 μL dNTP [200 μM], and 5 units of Promega GoTaq® DNA polymerase in 1× reaction buffer) as follows: 95 °C, 2 min, followed by 35 cycles (denaturation, 94 °C, 1 min; annealing at optimized temperatures as given in Table 1 for 1 min; extension, 72 °C, 90 s) and then 72 °C, 10 min. PCR products were analysed by electrophoresis in 1.2% agarose gel containing ethidium bromide. Actin was used as internal control. Optical density of signals was measured by using ImageJ 1.40 g freeware, and results were normalized to the optical density of control tissue.
Table 1.
Nucleotide sequences, amplification sites, GenBank accession numbers, amplimer sizes and PCR reaction conditions for each primer pair are shown
| Gene | Primer | Nucleotide sequence (5′ → 3′) | GenBank ID | Annealing temperature (°C) | Amplimer size (bp) |
|---|---|---|---|---|---|
| preproPACAP | Sense | GAA GAC GAG GCT TAC GAC CA (314–333) | NM_001315503.1 | 58 | 288 |
| Antisense | GTC CGA GTG GCG TTT GGT (584–601) | ||||
| PAC1 | Sense | TATTACTACCTGTCGGTGAAG(912–932) | NM_007407.4 | 52 | 213 |
| Antisense | ATGACTGCTGTCCTGCTC (1107–1124) | ||||
| VPAC1 | Sense | TTT GAG GAT TTC GGG TGC (974–991) | NM_011703.4 | 53 | 266 |
| Antisense | TGG GCC TTA AAG TTG TCG (1222–1239) | ||||
| VPAC2 | Sense | CTC CTG GTA GCC ATC CTT (805–822) | NM_009511.2 | 53 | 149 |
| Antisense | ATG CTG TGG TCG TTT GTG (936–953) | ||||
| PKA (Prkaca) | Sense | GCAAAGGCTACAACAAGGC (847–865) | NM_008854 | 53 | 280 |
| Antisense | ATGGCAATCCAGTCAATCG (1109–1126) | ||||
| CREB (Creb1) | Sense | AGATTGCCACATTAGCCC (95–112) | NM_031017.1 | 52 | 441 |
| Antisense | GCTGTATTGCTCCTCCCT (518–535) | ||||
| Sox9 | Sense | GTA CCC GCA TCT GCA CAA CG (378–397) | NM_011448 | 62 | 521 |
| Antisense | GTG GCA AGT ATT GGT CAA ACT CAT T (874–898) | ||||
| Sox6 | Sense | GGA GTC GGG AGC GTG AAA (483–500) | NM_001277326.1 | 54 | 381 |
| Antisense | GGC GAG CAA GGT CCA TTT (846–863) | ||||
| Sox5 | Sense | GCT CCA TAC AAC TCA TCT AC (504–523) | NM_011444.3 | 53 | 181 |
| Antisense | TGT CTT CTG GCT CAT TCT (667–684) | ||||
| Aggrecan | Sense | CGG GAA GGT TGC TAT GGT G (782–800) | NM_007424.2 | 59 | 359 |
| Antisense | CCT GTC TGG TTG GCG TGT A (1122–1140) | ||||
| Col2a1 | Sense | AAA GAC GGT GAG ACG GGA GC (1900–1919) | NM_001113515 | 63 | 289 |
| Antisense | GAC CAT CAG TAC CAG GAG TGC C (2167–2188) | ||||
| Chst11 | Sense | TGC TAT GTG CCC AAG GTA (822–839) | NM_021439.2 | 55 | 466 |
| Antisense | CGA GGT CGT AGT GGA TGTG (1269–1287) | ||||
| HAS2 | Sense | ACAGGCATCTCACGAACC (1479–1496) | NM_008216.3 | 51 | 415 |
| Antisense | ATC TTG GCG GGA AGT AAA (1876–2893) | ||||
| HAS3 | Sense | TCGGCGATTCGGTGGACT (835–852) | NM_001331048.1 | 59 | 280 |
| Antisense | TGCTGGAGGAGGCTGTTGC (1096–1114) | ||||
| HAPLN1 | Sense | GGC TCA GGA ATC CAC AAA (217–234) | BC066853 | 55 | 284 |
| Antisense | GGA AAG TAA GGG AAC ACC A (482–500) | ||||
| RHAMM | Sense | GAG GGA CTC AGG ACA AAC (374–391) | NM_013552.2 | 49 | 485 |
| Antisense | TTC TTC TAA CTG GGC AAT (8412–858) | ||||
| CD44 | Sense | GGATTCATCCCAACGCTAT (600–618) | NM_009851.2 | 53 | 216 |
| Antisense | ACT CGC CCT TCT TGC TGT (798–815) | ||||
| Col1a1 | Sense | GGG CGA GTG CTG TGC TTT (237–254) | BC050014 | 62 | 388 |
| Antisense | GGG ACC CAT TGG ACC TGA A (606–624) | ||||
| Col10a1 | Sense | TTC TGG GAT GCC GCT TGT C (1602–1620) | NM_009925 | 61 | 263 |
| Antisense | TCG TAG GCG TGC CGT TCT T (1846–1864) | ||||
| Actin (Actb) | Sense | GCCAACCGTGAAAAGATGA (419–437) | NM_007393.5 | 54 | 462 |
| Antisense | CAAGAAGGAAGGCTGGAAAA (861–880) |
Western blot analysis
Articular cartilage of knee joints was removed under microscope and was kept in 100 μL of homogenization RIPA. Tissues were cryo-ground in liquid nitrogen. After centrifugation, tissue pellets were suspended in 100 μL of homogenization RIPA and samples were stored at − 70 °C. Suspensions were sonicated by pulsing burst for 30 s at 40 A (Cole-Parmer, IL, USA). For setting equal protein concentration, BCA protein assay was used (Pierce™, MA, USA) and Laemmli electrophoresis sample buffer (4% SDS, 10% 2-mercaptoethanol, 20% glycerol, 0.004% bromophenol blue, 0.125 M TrisHCl pH 6.8) was added to cell lysates and boiled for 10 min. About 10 μg of protein was separated by 7.5% SDS-PAGE gel for detection of PAC1, VPAC1, VPAC2, PKA, CREB, P-CREB, Sox9, P-Sox9, Sox5, Sox6, collagen type I, collagen type X, Chst11, HAS2, HAS3, RHAMM, HAPLN1, and CD44 and by 5% SDS-PAGE gel for detection collagen type II and aggrecan. Proteins were transferred electrophoretically to nitrocellulose membranes with TransTurbo blot (Bio-Rad Laboratories, CA, USA) in 10 min. After blocking with 5% non-fat dry milk in phosphate-buffered saline (PBST) with 0.1% Tween 20, membranes were washed and exposed to the primary antibodies overnight at 4 °C in the dilution as given in Table 2. After washing for 30 min in PBST, membranes were incubated with anti-rabbit IgG (Bio-Rad Laboratories, CA, USA) in 1:1500 and anti-mouse IgG (Bio-Rad Laboratories, CA, USA) in 1:1500 dilution. Signals were detected by enhanced chemiluminescence (Advansta Inc., San Jose, CA, USA) according to the instructions of the manufacturer and documented by gel documentary system (Fluorchem E, ProteinSimple, CA, USA). Optical density of Western blot signals was measured by using ImageJ 1.40g freeware, and results were normalized to that of control samples.
Table 2.
Table of antibodies used in the experiments
| Antibody | Host animal | Dilution | Distributor |
|---|---|---|---|
| Anti-PAC1 | Rabbit, polyclonal | 1:600 | Sigma-Aldrich, St. Louis, MO, USA |
| Anti-VPAC1 | Rabbit, polyclonal | 1:800 | Alomone Labs., Jerusalem, Israel |
| Anti-VPAC2 | Rabbit, polyclonal | 1:600 | Abcam, Cambridge, UK |
| Anti-Coll. I. | Mouse, monoclonal | 1:1000 | Sigma-Aldrich, St. Louis, MO, USA |
| Anti-CREB | Rabbit, polyclonal | 1:800 | Millipore, Billerica, MA, USA |
| Anti-P-CREB | Rabbit, polyclonal | 1:800 | Millipore, Billerica, MA, USA |
| Anti-Coll. II. | Mouse, monoclonal | 1:500 | Novus Biologicals, Littleton, CO, USA |
| Anti-HAS2 | Rabbit, polyclonal | 1:300 | Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA |
| Anti-HAS3 | Rabbit, polyclonal | 1:300 | Sigma-Aldrich, St. Louis, MO, USA |
| Anti-Coll. X. | Rabbit, polyclonal | 1:500 | Sigma-Aldrich, St. Louis, MO, USA |
| Anti-Sox9 | Rabbit, polyclonal | 1:600 | Abcam, Cambridge, UK |
| Anti-P-Sox9 | Rabbit, polyclonal | 1:800 | Sigma-Aldrich, St. Louis, MO, USA |
| Anti-PKA | Rabbit, polyclonal | 1:800 | Cell Signaling, Danvers, MA, USA |
| Anti-RHAMM | Mouse, monoclonal | 1:500 | Novocastra Laboratories Ltd., Newcastle, UK |
| Anti-Aggrecan | Rabbit, polyclonal | 1:600 | Millipore, Billerica, MA, USA |
| Anti-HAPLN1 | Mouse, monoclonal | 1:500 | R&D Systems, Minneapolis, MN, USA |
| Anti-Chst11 | Rabbit, polyclonal | 1:600 | Sigma-Aldrich, St. Louis, MO, USA |
| Anti-CD44 | Mouse, polyclonal | 1:800 | R&D Systems, Minneapolis, MN, USA |
| Anti-Sox5 | Rabbit, polyclonal | 1:500 | Abcam, Cambridge, UK |
| Anti-Sox6 | Rabbit, polyclonal | 1:500 | Abcam, Cambridge, UK |
| Anti-actin | Mouse, monoclonal | 1:10000 | Sigma-Aldrich, St. Louis, MO, USA |
Statistical analysis
All data are representative of at least five independent experiments. Where applicable, data are expressed as mean ± SEM. Statistical analysis was performed by Student’s t test. Threshold for statistically significant differences as compared to respective control (wild-type animals) was set at *p < 0.05.
Results
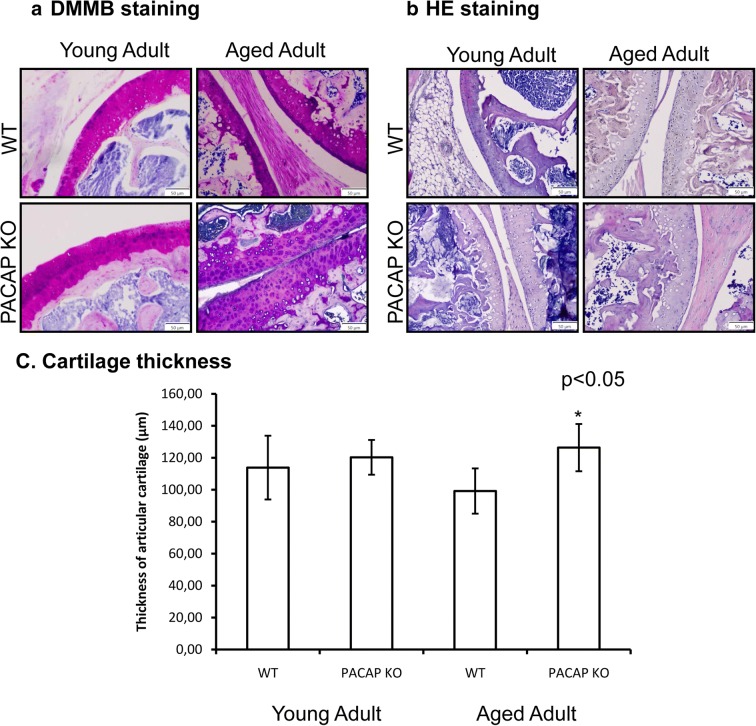
Thickness of articular cartilage increased in aged PACAP gene–deficient mice
DMMB staining was performed to demonstrate the presence of metachromatic ECM components (PGs, sulphated GAGs). There was similar metachromasia in young WT and PACAP gene–deficient mice, while metachromasia was paler in aged KO cartilage (Fig. 2a). No significant macroscopic alterations were detected in the morphology of young WT or PACAP KO articular cartilage with HE staining. Furthermore, morphologically, no differences were visible in the articular cartilage of knee joints in aged WT or PACAP gene–deficient mice (Fig. 2b). Thickness of articular cartilage was measured with a mathematical geometric method in 10 different joints both in tibial and femoral articular cartilages. In young PACAP animals, cartilage was tendentiously thicker but no significant alterations were measured compared with WT mice (Fig. 2c). On the contrary, significantly thicker cartilage was detected in aged PACAP KO mice compared with aged WT animals (Fig. 2c).
Fig. 2.
Morphological analysis of knee joints of young and aged WT and PACAP KO mice. Dimethylmethylene blue (DMMB) (a) and hematoxylin-eosin (HE) staining (b) were used to visualize the histological differences. Original magnification was × 20. Scale bar: 50 μm. Geometric analysis (c) of mouse articular cartilage. Representative data of 10 independent experiments. Asterisks indicate significant (*p < 0.05) difference in thickness of cartilage compared to the respective control
PACAP receptors diminished in aged cartilage of PACAP KO mice
As PACAP can act on three different receptors, we monitored mRNA and protein expressions of PAC1, VPAC1 and VPAC2 receptors in articular cartilage. In young animals, only WT cartilage showed PACAP expression as it was expected (Fig. 3a). On the other hand, no preproPACAP expression was detected in aged WT or PACAP KO animals (Fig. 3a). Expression of the main PACAP-binding receptor, PAC1, was detected in WT and PACAP gene–deficient young animals with equal expression (Fig. 3a, b). In aged cartilage, no PAC1 receptor mRNA or protein expression was detected (Fig. 3a, b). Moreover, VPAC1 expression was similar to PAC1 with an absence in aged PACAP gene–deficient mice (Fig. 3a, b), while VPAC2 was not detectable in hyaline cartilage.
Fig. 3.
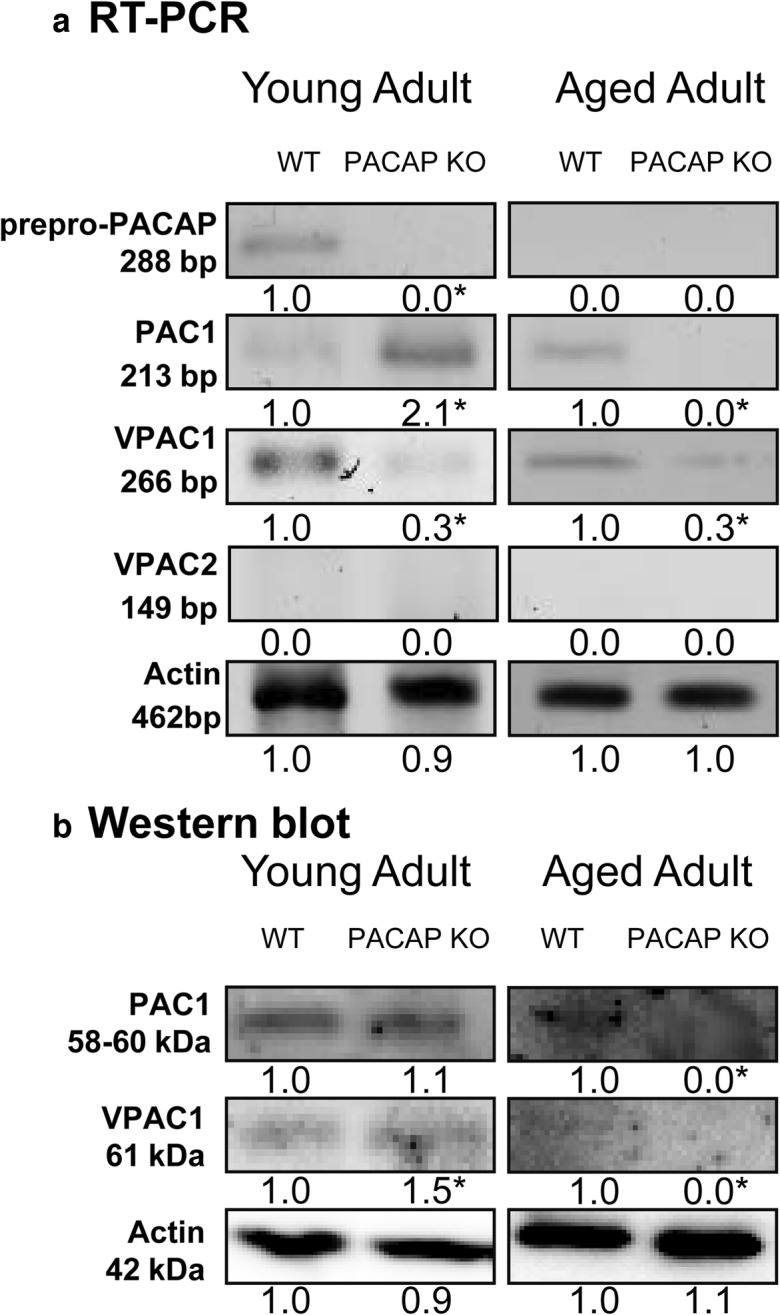
Investigation of PACAP and its receptors in articular cartilage. mRNA (a) and protein (b) expression of preproPACAP, PAC1, VPAC1 and VPAC2 receptors of cartilage. For RT-PCR and Western blot reactions, actin was used as control. Optical signal density was measured and results were normalized to the WT controls. For a and b, numbers below signals represent integrated signal densities determined by ImageJ software. Asterisks indicate significant (*p < 0.05) alteration of expression compared to the respective control. Representative data of 5 independent experiments
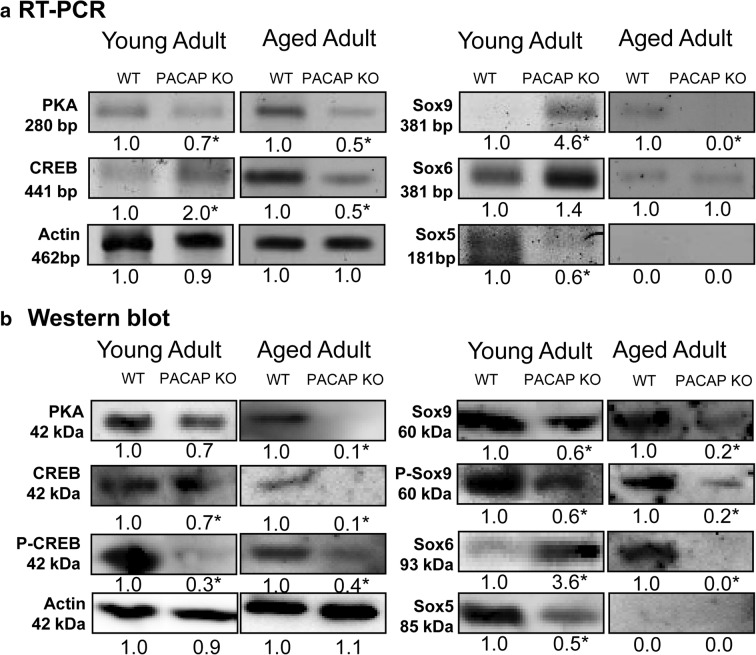
Expression of canonical PACAP downstream signaling molecules altered in PACAP gene–deficient animals
Next, classical downstream targets of PACAP binding were investigated. Both the mRNA and protein expressions of PKA were reduced in young PACAP KO cartilages (Fig. 4a, b). Moreover, in aged PACAP, gene–deficient cartilage protein expression of PKA was hardly detectable with this method (Fig. 4a, b). CREB mRNA and protein expressions did not significantly change in young PACAP KO articular cartilage but its phosphorylated, more active form decreased in aged cartilage. The mRNA and protein expressions of CREB and the protein expression of P-CREB were reduced (Fig. 4a, b). Next, expression of SoxE family members followed. In young cartilage, the mRNA expression of Sox9 was significantly elevated, while a significant decrease was detected in Sox9 and P-Sox9 protein expressions (Fig. 4a, b). Analysis of Sox6 expression showed an unexpected result. In young PACAP KO animals elevated mRNA and protein expressions of Sox6 were detected (Fig. 4a, b), while Sox6 protein became undetectable in aged PACAP gene–deficient mice (Fig. 4a, b). Finally, Sox5 mRNA and protein expressions significantly decreased in young PACAP KO cartilage and no expression was detected in old WT and PACAP KO mice (Fig. 4a, b).
Fig. 4.
Investigation of canonical PACAP signalization in cartilage. mRNA (a) and protein (b) expression of PKA, CREB, Sox9, Sox6, and Sox5. For RT-PCR and Western blot reactions, actin was used as control. Optical signal density was measured and results were normalized to the WT controls. For a and b, numbers below signals represent integrated signal densities determined by ImageJ software. Asterisks indicate significant (*p < 0.05) alteration of expression compared to the respective control. Representative data of 5 independent experiments
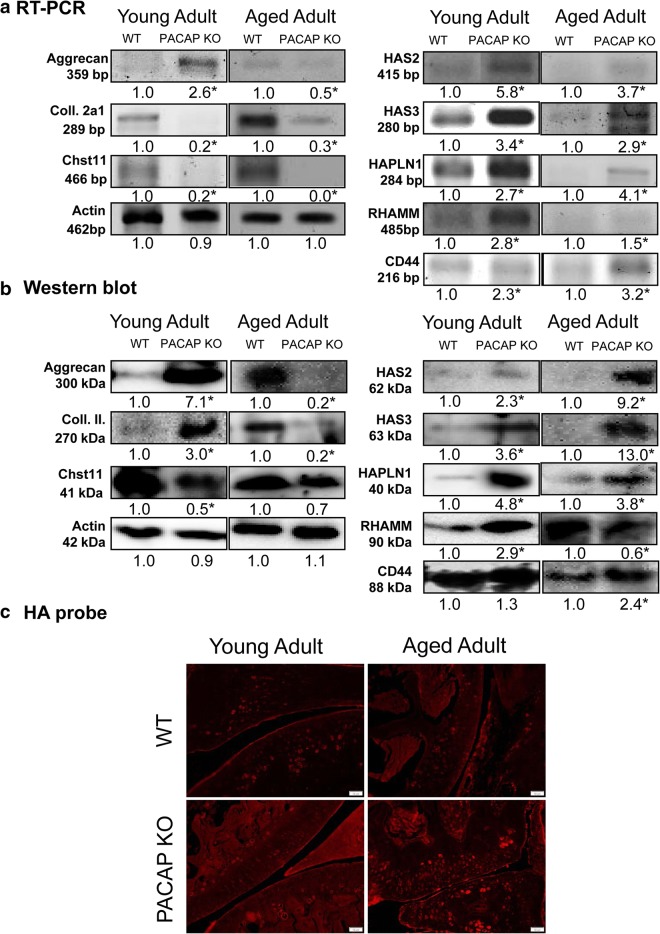
Alterations of ECM production in PACAP KO mice
In further steps, effects of PACAP and aging were monitored in production of cartilage specific ECM. Aggrecan, the main proteoglycan of hyaline cartilage showed an elevated mRNA and protein expression in young PACAP gene–deficient mice (Fig. 5a, b). On the contrary, both the mRNA and protein expressions were reduced in aged PACAP KO mice (Fig. 5a, b). Interestingly, the mRNA expression of collagen type II was diminished, but increased protein expression was detected in young PACAP KO cartilage (Fig. 5a, b). In aged PACAP gene–deficient mice, both the mRNA and protein expressions of collagen type II were decreased (Fig. 5a, b). Chst11 catalyses the transfer of sulphate to chondroitin. Both the mRNA and protein expressions of this transferase decreased in young and aged PACAP gene–deficient articular cartilage (Fig. 5a, b). HAPLN1 (link protein) can stabilize the aggregates of aggrecan monomers with HA and helps with the formation of the cartilage specific ECM network. Similarly to aggrecan core, protein expression HAPLN1 showed an increased expression in young PACAP KO animals but it reduced during aging (Fig. 5a, b). Production of HA in cartilage is regulated by two hyaluronan synthases, HAS2 and HAS3. Interestingly, the mRNA and the protein expressions of these enzymes elevated in both young and aged PACAP KO mice (Fig. 5a, b). Binding of HA can occur intracellularly by RHAMM or on the cell surface by CD44. mRNA and protein expressions of RHAMM and CD44 were elevated in young PACAP gene–deficient mice (Fig. 5a, b). On the contrary, RHAMM expression decreased in aged PACAP KO mice. CD44 protein expression similarly to HAS enzymes elevated in aged PACAP gene–deficient animals (Fig. 5a, b).
Fig. 5.
ECM production in articular cartilage. a mRNA and b protein expressions of Aggrecane, collagen type II, HAPLN1, HAS2, HAS3, RHAMM and CD44 in articular cartilage. Actin was used as a control. Numbers below signals represent integrated signal densities determined by ImageJ software. Asterisks indicate significant (*p < 0.05) alteration of expression compared to the respective control. c HA-binding probe in hyaline cartilage. Original magnification was × 20. Scale bar: 50 μm. Representative data of 5 independent experiments
HA content of articular cartilage was also investigated, and high amount of GAG was visible around the chondrons of WT articular cartilage (Fig. 5c). The amount of HA was increased both in young and aged PACAP gene–deficient mice (Fig. 5c).
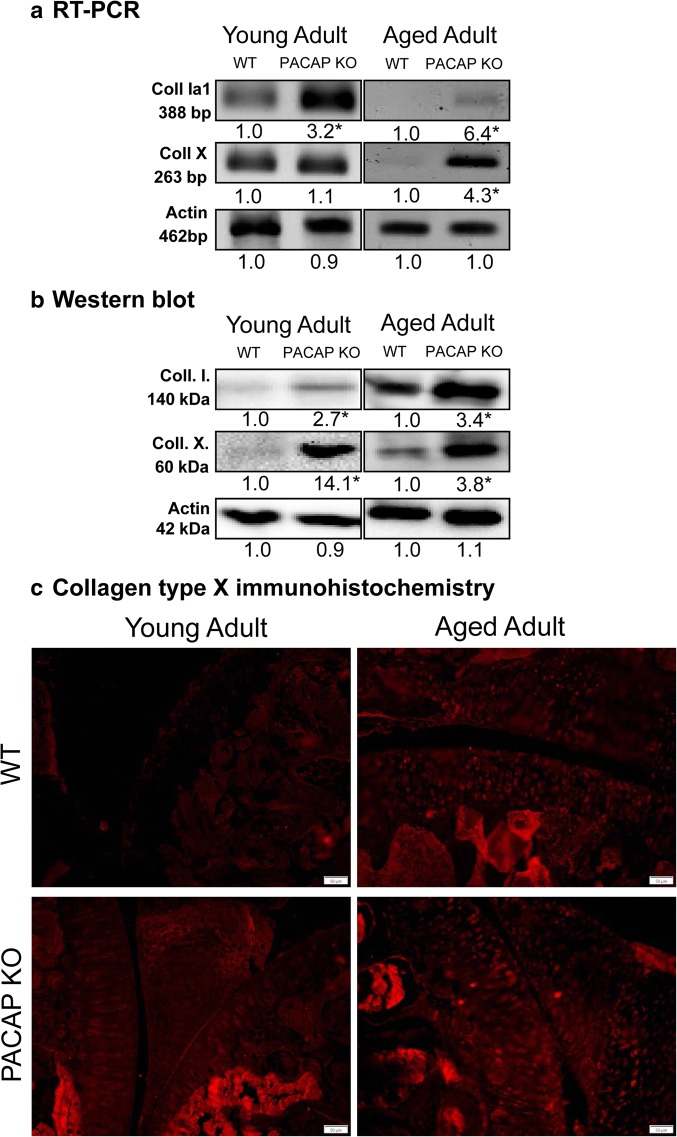
Bone-specific collagens accumulated in PACAP KO cartilage in aging
Furthermore, we investigated the expression of collagen type I and X which specifically appears in bony calcified structures. mRNA and protein expressions of collagen type I increased in young PACAP KO cartilage, and even stronger elevation was detected in aged PACAP KO joints (Fig. 6a, b). Collagen type X mRNA expression did not significantly alter, but dramatic protein expression elevation was detected in young PACAP KO mice (Fig. 6a, b). In aged PACAP KO joints, highly elevated mRNA and protein expression of collagen type X were detected (Fig. 6a, b). Location of collagen type X was followed by immunohistochemistry. In young WT mice, almost undetectable amount of collagen type X was shown in articular cartilage, while subchondral bone showed normal immunopositivity (Fig. 6c). In PACAP KO young animals, intensified immunopositivity was identified in subchondral bone and increased positivity was visible in articular cartilage (Fig. 6c). Both in WT and PACAP KO–aged mice, strong signal was detected in the subchondral region; moreover, strong collagen type X positivity appeared around the chondrons of articular cartilage (Fig. 6c).
Fig. 6.
Collagen expression in cartilage. mRNA (a) and protein (b) expressions of collagen type I and X in cartilage. For RT-PCR and Western blot reactions, actin was used as controls. Numbers below signals represent integrated signal densities determined by ImageJ software. Asterisks indicate significant (*p < 0.05) alteration of expression compared to the respective control. c Collagen type X immunohistochemistry in hyaline cartilage. Original magnification was × 20. Scale bar: 50 μm. Representative data of 5 independent experiments
Discussion
In the present work, we demonstrated that genetical ablation of PACAP causes morphological and biochemical alterations in articular cartilage possibly turning this tissue more prone to degenerative diseases such as osteoarthritis (OA). Mature articular cartilage is an avascular and aneural tissue with a very low metabolic activity. Chondrocytes live in a milieu where they are exposed to acidic pH and low oxygen tension, and nutrients are transported to the cells by diffusion from the synovial fluid. Developing chondrocytes establish the specific zonal architecture of articular cartilage during foetal development (Zhang et al. 2012). Terminally differentiated hypertrophic chondrocytes secrete a cartilage matrix rich in collagen type X and the calcified cartilage of hypertrophic zone in articular cartilage provides a biomechanical transition between hyaline cartilage and the subchondral bone (Mora et al. 2018). Biologically proper internal structure of articular cartilage is needed for the optimal weight bearing capability and joint function. Several signaling pathways contribute to the formation of collagen type II-rich ECM (Fodor et al. 2013; Juhasz et al. 2014c; Matta et al. 2008; Matta et al. 2011; Varga et al. 2011; Zakany et al. 2005; Zakany et al. 2002). In aging, the normal homeostasis of articular cartilage becomes shifted toward matrix degradation. Age related alterations of chondrocytes phenotype and signaling or remodeling disorders have been reviewed by Davies et al. (2017). Injury or overload of articular cartilage, particularly in elderly people, can induce OA (Bolduc et al. 2018) and when it developes, a progressive degradation of ECM may lead to a complete destruction of cartilage (Jimenez et al. 2018; Mora et al. 2018). Aging or OA-related matrix degradation of articular cartilage is hardly treatable; only few methods are used in the clinical practice such as advanced glycation end products (AGE) treatment (Satake et al. 2018) or corticosteroid injections (Mora et al. 2018). With these interventions, decrease of joint inflammation and conservation of the status of articular cartilage can be the main goal. Shifting aging-related cartilage alterations toward later life periods or modifying senescent chondrocytes can be another possibility (Hou et al. 2018; Jeon et al. 2018). Currently, stem cell therapy seems an emerging method for prevention both of the age-related cartilage degradation and OA formation (Krajewska-Wlodarczyk et al. 2018).
PACAP was found to exert protecting effects in different tissues. It can be beneficial in treatments of retinopathy (Szabadfi et al. 2016), Parkinson’s disease (Brown et al. 2014) and ischemia (Reglodi et al. 2018d). It is also known that PACAP induces the activation of anti-apoptotic processes and leads to decreases of pro-apoptotic factors (Reglodi et al. 2018a). Deficient PACAP-signaling was found in various neurodegenerative diseases such as Alzheimer’s disease (Wu et al. 2006) and Parkinson’s disease (Feher et al. 2018). Furthermore, reduced metabolism is detected in aging process (LaRoche et al. 2018; Nacarelli et al. 2018; Tian et al. 2017) which can be compensated by PACAP (Mansouri et al. 2016). Aging can lead to several skeletal and oral diseases such as dental root caries or alveolar bone loss (An et al. 2018); on the other hand, PACAP regulates the development of teeth (Fulop et al. 2018). Regarding cartilage and bone development and disease models, our group previously described that PACAP has a positive effect on chondrogenesis with the elevation of Sox9 activation (Juhasz et al. 2014a) and prevents the harmful effects of oxidative stress and mechanical overload in in vitro chondrogenesis (Juhasz et al. 2014a; Juhasz et al. 2015b). The presence of PACAP receptors in hyaline cartilage was demonstrated in chicken high density chondrifying cell cultures (Juhasz et al. 2014a) and in human OA (Giunta et al. 2015). Furthermore, the addition of PACAP influenced the expression of ECM molecules, such as HA (Juhasz et al. 2014a) or collagens (Juhasz et al. 2015b). The lack of PACAP resulted in a signaling disorder femur development (Jozsa et al. 2018). Although the importance of PACAP-signaling and its positive role in OA is likely (Grassel and Muschter 2018), the role of PACAP in pathogenesis of cartilage disorders is not extensively studied and no information is available about its function in cartilage aging.
It is known that increased thickness of calcified cartilage can be detected in hip joints in early stages of OA (Hartlev et al. 2018). In knee joints of aged PACAP KO mice, significant thickening of articular cartilage and subchondral bone, along with decreased metachromasia, was our most obvious histological observation. This increase was parallel with disturbed ratio of the various components in the ECM. In aged PACAP KO animals, more collagen type I, elevated HA content was detected along with decrease of aggrecan and type II collagen. Loss of aggrecan was also proved by reduced metachromasia with DMMB. Altogether, these alterations can lead to softening of the articular cartilage which could induce thickening of subchondral bone. These microscopic morphological changes seem very similar to initial stages of OA (Lahm et al. 2017). It also suggests that the neuropeptide is involved in the inhibition of articular cartilage aging by maintaining chondrocyte plasticity (Varela-Eirin et al. 2018).
Along with aging, loss of PAC1 receptor was detected in articular cartilage of PACAP KO mice, which can be a factor triggering an ECM formation disorder (Fig. 7). This finding further supports the importance of PAC1 receptor activation in cartilage differentiation and proper ECM synthesis (Juhasz et al. 2014a). Similarly, PAC1 receptor reduction was also shown in retinal aging of PACAP KO mice (Kovacs-Valasek et al. 2017), although elevation was detected in young gene deficient mice. This further strengthens the hypothesis that presence of PACAP receptors exerts tissue-specific effects during aging (Reglodi et al. 2018b). VPAC1 receptor expression was identified in articular cartilage, its expression was almost undetectably low, suggesting that PAC1 is the dominant receptor in this tissue (Juhasz et al. 2014a).
Fig. 7.
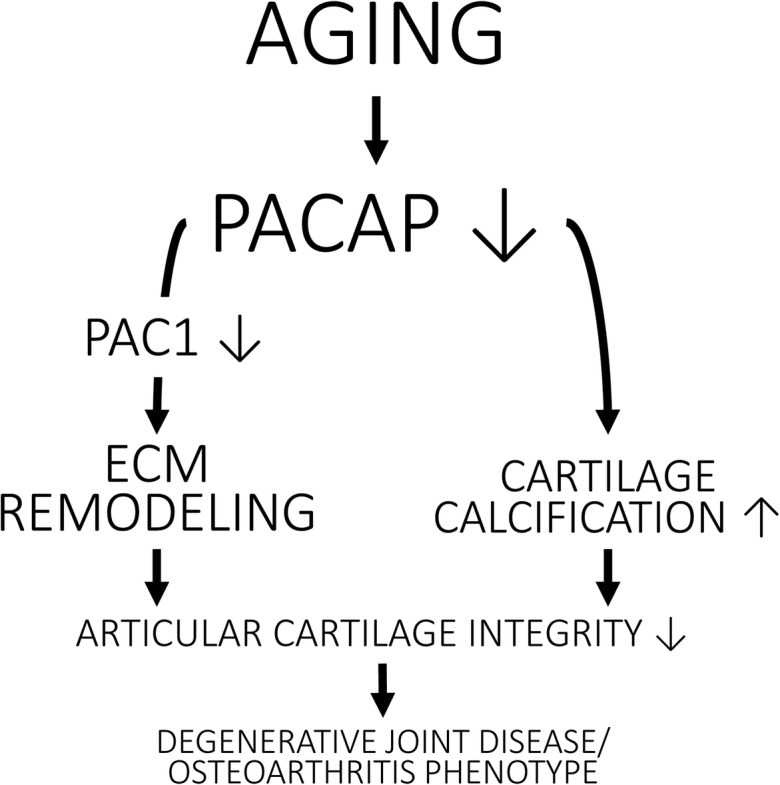
PACAP function in aging. Concentration of PACAP and expression of PAC1 receptor reduce in aging process of articular cartilage. Reduction of the neuropeptide induces decreased cartilage remodeling but enhances the calcification processes of articular cartilage. Therefore, PACAP is important in maintaining cartilage integrity and prevents formation of pathological illnesses such as osteoarthritis
Although the expression of PKA is not PACAP-dependent, we detected reduced PKA expression in aged PACAP gene–deficient mice. As PKA phosphorylates CREB and Sox9 transcription factors, this observation can explain the decreased activation and expression of these transcription factors. Reduced phosphorylation of CREB and Sox9 was more pronounced in aged articular cartilage (Zhang et al. 2016). We have described earlier that activation of Sox9 also depends on PAC1 receptor activation (Juhasz et al. 2014a), and the lack of the neuropeptide further decreased the Sox9-dependent aggrecan and collagen expression (Zhang et al. 2016). These results suggest that the presence of PACAP is necessary for maintenance of continuous activation of Sox9 to produce and maintain the cartilage specific matrix expression. Sox5 and Sox6 are also positive regulators of chondrogenesis (Nishimura et al. 2018), and the lack of PACAP reduces the expression of Sox5 but elevates Sox6 expression. It seems that the reduced Sox9 expression is compensated in the lack of the neuropeptide by the elevated Sox6 expression in articular cartilage of young adults. A very similar phenomenon was identified in testis of PACAP KO mice, where the decreased Sox9 expression was compensated by an elevated Sox10 production (Reglodi et al. 2018c). Sox6 elevation resulted in the increase of aggrecan and collagen type II expression in young PACAP gene–deficient mice, accounting for the normal cartilage morphology. Similar compensatory mechanisms were identified in teeth of PACAP KO mice by the activation of Notch signaling (Fulop et al. 2018) or in femurs where augmented BMP signaling normalized the bone formation (Jozsa et al. 2018). Sox5 and Sox6 play important roles in the formation of proper articular cartilage morphology during development (Dy et al. 2010), but Sox5 function is diminished in aging process. Although Sox6 is detectable in aged WT mice, it is not present in PACAP KO animals. The decreased expression of Sox6 resulted in the loss of compensatory mechanism and further reduced aggrecan and collagen type II expression leading to the structural disorder of ECM in articular cartilage of PACAP gene–deficient mice. Moreover, lowered transferase (Chst11) expression can be the explanation of the decreased presence of sulphated glycosaminoglycans which was shown by a paler metachromasia in aged PACAP KO mice. Sox9, Sox5 and Sox6 are the major transcription factors of chondrogenesis, and their activation results various gene activations (Akiyama and Lefebvre 2011). Here we gave evidence that PACAP-signaling plays an essential role in Sox9 and Sox5 function, but Sox6, at least, partly was PACAP independently activated and compensated the lowered function of Sox9 and Sox5 in young PACAP KO mice. Our results suggest that the activation of Sox transcription factors is age dependent and in case of Sox9 this was demonstrated previously (Zhang et al. 2016). We observed that the absence of PACAP further reduced Sox9 and Sox5 function, and it further strengthens the hypothesis that PACAP can keep balancing in crosstalks of various signaling pathways even during aging of tissues (Fig. 7) (Jozsa et al. 2018; Niewiadomski et al. 2013; Szentleleky et al. 2019).
Interestingly, the thickness of articular cartilage increases in aging PACAP KO mice; therefore, we analysed the HA homeostasis of hyaline cartilage. Expression of HAS-ses and HA-binding proteins and receptors such as HAPLN1 and CD44 increases in young and aged PACAP KO mice. Furthermore, the presence of HA is elevated in the articular cartilage during aging. Coincidently, in aged synovial cavity, decreased expression of HA was detected (Temple-Wong et al. 2016). Increased serum HA level was shown in aged population which can be a diagnostic sign of OA (Inoue et al. 2011). Moreover, aggrecanase can induce the HA release from aged articular cartilage which can enhance the destruction of the cartilage matrix during degenerative joint diseases such as OA (Chockalingam et al. 2004). Increased MMP activity was detected in the ECM of cardiac muscle tissue during aging (Meschiari et al. 2017), but we showed a PACAP-dependent reduction of MMPs in mechanical overload of chondrogenic cell cultures (Szentleleky et al. 2019). RHAMM is an intracellular HA-binding receptor which can be activated by ERK (Katona et al. 2016). Its expression is reduced in aged PACAP KO animals, suggesting that intracellular HA function is decreased as it was demonstrated in skin aging (Tzellos et al. 2009). Therefore, the appearance of HA around the chondrons can reflect on imbalanced HA distribution and may be a sign of ECM degradation in PACAP KO knee joints. Previously, we demonstrated that PACAP addition resulted in a reduced expression of hyaluronidases and aggrecenases in stress reactions (Szentleleky et al. 2019). We suppose that chondrocytes cannot precisely control aggrecanase activation in PACAP KO mice. In aged cartilage, the elevated aggrecanase activity is proven to trigger HA release into the synovial cavity. Our results indicate that PACAP is a key molecule in maintaining cartilage matrix and keeping the balance between matrix production and degradation (Fig. 7) (Juhasz et al. 2015b; Szentleleky et al. 2019). Furthermore, the absence of PACAP probably triggers an early aging process which shows the characteristic signs of OA (Fig. 7).
In addition, we also detected increased expression and presence of collagen type I and X in aged articular cartilages. The expression of these collagens is stronger in PACAP gene–deficient mice. In intervertebral disc degradation an increased collagen type X was shown (Hristova et al. 2011) or age related elevation of collagen type X was demonstrated in bone and ligament healing (Wang et al. 2006). Furthermore, aging induced the expression elevation of collagen type I and X in mandibular condylar cartilage (Inoue et al. 2002). We also published that addition of PACAP can induce the normalization of collagen type X expression in mechanical overload (Juhasz et al. 2015b). Additionally, PACAP deficiency increased collagen type I expression in femurs (Jozsa et al. 2018). According to our previous results, PACAP can act on cartilage ECM structure via activation hedgehog signaling (Juhasz et al. 2015b). The absence of PACAP disturbs signaling crosstalks of hedgehog activation, subsequently augments the expression of bone-specific collagen expressions and enhances cartilage matrix calcification. These findings further confirm that the lack of PACAP triggers an accelerated cartilage aging and the appearance of non-specific collagens in cartilage may cause OA-like cartilage matrix formation (Fig. 7).
In conclusion, we provided evidence that PACAP has an important function in proper cartilage matrix production in young animals as it seems to keep the balance between matrix production and matrix degradation (Fig. 7). The lack of the neuropeptide disturbs normal ECM composition of articular cartilage leading to early signs of aging in this tissue, which ultimately can cause a degenerative joint disease (Fig. 7).
Acknowledgements
The authors are grateful for Mrs. Krisztina Bíró for excellent technical assistance.
Abbreviations
- cAMP
cyclic adenosine monophosphate
- CD44
cluster of differentiation 44
- CNS
central nervous system
- CREB
cAMP response element-binding protein
- Chst11
carbohydrate sulphotransferase 11
- dNTP
deoxynucleotide triphosphate
- ECM
extracellular matrix
- EDTA
ethylene diamine tetra-acetic acid
- EGTA
ethylene glycol-bis(β-aminoethyl ether)-N,N,N′,N′-tetraacetic acid
- ERK
extracellular signal–regulated kinase
- FBS
foetal bovine serum
- FGF
fibroblast growth factor
- GAG
glycosaminoglycan
- HA
hyaluronic acid
- HAPLN
hyaluronan and proteoglycan link protein
- HAS
hyaluronan synthase
- HH
hedgehog
- MAPK
mitogen-activated protein kinase
- OA
osteoarthritis
- PAC1
pituitary adenylate cyclase–activating polypeptide type I receptor
- PACAP
pituitary adenylate cyclase–activating polypeptide
- PBS
phosphate-buffered saline
- PBST
phosphate-buffered saline supplemented with 1% Tween-20
- PG
proteoglycan
- PLC
phospholipase C
- PKA
protein kinase A
- PKC
protein kinase C
- PP2A and B
protein phosphatase 2A and B
- RT-PCR
reverse transcription followed by polymerase chain reaction
- RHAMM
receptor for hyaluronan mediated motility
- Sox
SRY-related HMG-BOX gene
- TGFβ
transforming growth factor-β
- VIP
vasoactive intestinal peptide
- VPAC
vasoactive intestinal peptide receptor
- WNT
wingless related integration site
Author contributions
Study conception and design: T J, D R, V Sz, B B, S T, V Sz, J V and T J performed the molecular biologycal analysis. V Sz and H P were responsible for the DMMB and HE staining. B F and A Jwere responsible for the animal care and removing the limbs. Geometric analysis were performed by B B. Acquisition of data: V Sz, B F, A T. Analysis and interpretation of data: V Sz, B B, T J, H P, A J, A T, R Z, D R. Participated in drafting the manuscript: V Sz, S T, R Z, T J, D R
Funding information
Open access funding provided by University of Debrecen (DE). NKFIK115874, K119759, NKFIHFK129190, PTE AOK Research Grant, MTA-TKI 14016, GINOP-2.3.2-15-2016-00050 “PEPSYS”, New National Excellence Program of the Ministry of Human Capacities (UNKP-16-4-IV.), 2017-1.2.1-NKP-2017-00002 Nemzeti Agykutatási Program EFOP-3.6.1.-16-2016-00004 Comprehensive Development for Implementing Smart Specialization Strategies at the University of Pecs, EFOP-3.6.2-16-2017-00008 “The role of neuro-inflammation in neurodegeneration: from molecules to clinics”, Centre for Neuroscience of the University of Pecs, EFOP-3.6.3-VEKOP-16-2017-00009, University of Debrecen (OTKA Bridging Fund), EFOP-3.6.1.-16-2016-00004 Comprehensive Development for Implementing Smart Specialization Strategies at the University of Pécs (Budapest, Hungary), NAP 2017-1.2.1-NKP-2017-00002 and OTKA-NN 114458. The project is co-financed by the European Union and the European Social Fund. Bolyai Janos Research Scholarship (J.T., A.T.). Szodoray Lajos and Magyary Zoltán Funds by Hungarian Academy of Science and the European Union and the State of Hungary, co-financed by the European Social Funding. Fund in the framework of TÁMOP 4.2.4 (J.T.). A/2-11-1-2012-0001 “National Excellence Program”. Higher Education Institutional Excellence Program of the Ministry of Human Capacities FIKPII.
Compliance with ethical standards
All procedures were performed in accordance with the ethical guidelines approved by the University of Pécs (permission number: BA02/2000-15024/2011).
Competing interests
The authors declare that there are no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Vince Szegeczki and Balázs Bauer; Dóra Reglődi and Tamás Juhász contributed equally to this work.
References
- Akiyama H, Lefebvre V. Unraveling the transcriptional regulatory machinery in chondrogenesis. J Bone Miner Metab. 2011;29:390–395. doi: 10.1007/s00774-011-0273-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- An JY, Darveau R, Kaeberlein M. Oral health in geroscience: animal models and the aging oral cavity. GeroScience. 2018;40:1–10. doi: 10.1007/s11357-017-0004-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antons J, Marascio MGM, Nohava J, Martin R, Applegate LA, Bourban PE, Pioletti DP. Zone-dependent mechanical properties of human articular cartilage obtained by indentation measurements. J Mater Sci Mater Med. 2018;29:57. doi: 10.1007/s10856-018-6066-0. [DOI] [PubMed] [Google Scholar]
- Bolduc Jesalyn A., Collins John A., Loeser Richard F. Reactive oxygen species, aging and articular cartilage homeostasis. Free Radical Biology and Medicine. 2019;132:73–82. doi: 10.1016/j.freeradbiomed.2018.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown D, Tamas A, Reglodi D, Tizabi Y. PACAP protects against inflammatory-mediated toxicity in dopaminergic SH-SY5Y cells: implication for Parkinson’s disease. Neurotox Res. 2014;26:230–239. doi: 10.1007/s12640-014-9468-x. [DOI] [PubMed] [Google Scholar]
- Chockalingam PS, Zeng W, Morris EA, Flannery CR. Release of hyaluronan and hyaladherins (aggrecan G1 domain and link proteins) from articular cartilage exposed to ADAMTS-4 (aggrecanase 1) or ADAMTS-5 (aggrecanase 2) Arthritis Rheum. 2004;50:2839–2848. doi: 10.1002/art.20496. [DOI] [PubMed] [Google Scholar]
- Davies JMS, Cillard J, Friguet B, Cadenas E, Cadet J, Cayce R, Fishmann A, Liao D, Bulteau AL, Derbré F, Rébillard A, Burstein S, Hirsch E, Kloner RA, Jakowec M, Petzinger G, Sauce D, Sennlaub F, Limon I, Ursini F, Maiorino M, Economides C, Pike CJ, Cohen P, Salvayre AN, Halliday MR, Lundquist AJ, Jakowec NA, Mechta-Grigoriou F, Mericskay M, Mariani J, Li Z, Huang D, Grant E, Forman HJ, Finch CE, Sun PY, Pomatto LCD, Agbulut O, Warburton D, Neri C, Rouis M, Cillard P, Capeau J, Rosenbaum J, Davies KJA. The oxygen paradox, the French paradox, and age-related diseases. Geroscience. 2017;39(5–6):499–550. doi: 10.1007/s11357-017-0002-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dy P, et al. Synovial joint morphogenesis requires the chondrogenic action of Sox5 and Sox6 in growth plate and articular cartilage. Dev Biol. 2010;341:346–359. doi: 10.1016/j.ydbio.2010.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feher M, Gaszner B, Tamas A, Gil-Martinez AL, Fernandez-Villalba E, Herrero MT, Reglodi D. Alteration of the PAC1 receptor expression in the basal ganglia of MPTP-induced parkinsonian macaque monkeys. Neurotox Res. 2018;33:702–715. doi: 10.1007/s12640-017-9841-7. [DOI] [PubMed] [Google Scholar]
- Fodor J, et al. Store-operated calcium entry and calcium influx via voltage-operated calcium channels regulate intracellular calcium oscillations in chondrogenic cells. Cell Calcium. 2013;54:1–16. doi: 10.1016/j.ceca.2013.03.003. [DOI] [PubMed] [Google Scholar]
- Fulop B. D., Sandor B., Szentleleky E., Karanyicz E., Reglodi D., Gaszner B., Zakany R., Hashimoto H., Juhasz T., Tamas A. Altered Notch Signaling in Developing Molar Teeth of Pituitary Adenylate Cyclase-Activating Polypeptide (PACAP)-Deficient Mice. Journal of Molecular Neuroscience. 2018;68(3):377–388. doi: 10.1007/s12031-018-1146-7. [DOI] [PubMed] [Google Scholar]
- Giunta S, Castorina A, Marzagalli R, Szychlinska MA, Pichler K, Mobasheri A, Musumeci G. Ameliorative effects of PACAP against cartilage degeneration. Morphological, immunohistochemical and biochemical evidence from in vivo and in vitro models of rat osteoarthritis. Int J Mol Sci. 2015;16:5922–5944. doi: 10.3390/ijms16035922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gourlet P, Vandermeers A, Vertongen P, Rathe J, de Neef P, Cnudde J, Waelbroeck M, Robberecht P. Development of high affinity selective VIP1 receptor agonists. Peptides. 1997;18:1539–1545. doi: 10.1016/S0196-9781(97)00228-3. [DOI] [PubMed] [Google Scholar]
- Grassel S, Muschter D (2018) Do neuroendocrine peptides and their receptors qualify as novel therapeutic targets in osteoarthritis? Int J Mol Sci 19. 10.3390/ijms19020367 [DOI] [PMC free article] [PubMed]
- Hartlev Louise Brøndt, Klose-Jensen Rasmus, Thomsen Jesper Skovhus, Nyengaard Jens Randel, Boel Lene Warner Thorup, Laursen Mogens Berg, Laurberg Trine Bay, Nielsen Andreas Wiggers, Steengaard-Pedersen Kristian, Hauge Ellen-Margrethe. Thickness of the bone-cartilage unit in relation to osteoarthritis severity in the human hip joint. RMD Open. 2018;4(2):e000747. doi: 10.1136/rmdopen-2018-000747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashimoto H., Shintani N., Tanaka K., Mori W., Hirose M., Matsuda T., Sakaue M., Miyazaki J.-i., Niwa H., Tashiro F., Yamamoto K., Koga K., Tomimoto S., Kunugi A., Suetake S., Baba A. Altered psychomotor behaviors in mice lacking pituitary adenylate cyclase-activating polypeptide (PACAP) Proceedings of the National Academy of Sciences. 2001;98(23):13355–13360. doi: 10.1073/pnas.231094498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou A, et al. Cellular senescence in osteoarthritis and anti-aging strategies. Mech Ageing Dev. 2018;175:83–87. doi: 10.1016/j.mad.2018.08.002. [DOI] [PubMed] [Google Scholar]
- Hristova GI, Jarzem P, Ouellet JA, Roughley PJ, Epure LM, Antoniou J, Mwale F. Calcification in human intervertebral disc degeneration and scoliosis. J Orthop Res. 2011;29:1888–1895. doi: 10.1002/jor.21456. [DOI] [PubMed] [Google Scholar]
- Inoue H, Hiraki Y, Nawa T, Ishizeki K. Phenotypic switching of in vitro mandibular condylar cartilage during matrix mineralization. Anat Sci Int. 2002;77:237–246. doi: 10.1046/j.0022-7722.2002.00031.x. [DOI] [PubMed] [Google Scholar]
- Inoue R, et al. Knee osteoarthritis, knee joint pain and aging in relation to increasing serum hyaluronan level in the Japanese population. Osteoarthr Cartil. 2011;19:51–57. doi: 10.1016/j.joca.2010.10.021. [DOI] [PubMed] [Google Scholar]
- Ivic I, et al. Aging-induced modulation of pituitary adenylate cyclase-activating peptide- and vasoactive intestinal peptide-induced vasomotor responses in the arteries of mice. J Vasc Res. 2017;54:359–366. doi: 10.1159/000481781. [DOI] [PubMed] [Google Scholar]
- Jeon OH, David N, Campisi J, Elisseeff JH. Senescent cells and osteoarthritis: a painful connection. J Clin Invest. 2018;128:1229–1237. doi: 10.1172/JCI95147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez G, Cobo-Molinos J, Antich C, Lopez-Ruiz E. Osteoarthritis: trauma vs disease. Adv Exp Med Biol. 2018;1059:63–83. doi: 10.1007/978-3-319-76735-2_3. [DOI] [PubMed] [Google Scholar]
- Józsa Gergő, Szegeczki Vince, Pálfi Andrea, Kiss Tamás, Helyes Zsuzsanna, Fülöp Balázs, Cserháti Csaba, Daróczi Lajos, Tamás Andrea, Zákány Róza, Reglődi Dóra, Juhász Tamás. Signalling Alterations in Bones of Pituitary Adenylate Cyclase Activating Polypeptide (PACAP) Gene Deficient Mice. International Journal of Molecular Sciences. 2018;19(9):2538. doi: 10.3390/ijms19092538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juhasz T, et al. Pituitary adenylate cyclase activating polypeptide (PACAP) signalling exerts chondrogenesis promoting and protecting effects: implication of calcineurin as a downstream target. PLoS One. 2014;9:e91541. doi: 10.1371/journal.pone.0091541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juhasz T, et al. Pituitary adenylate cyclase-activating polypeptide (PACAP) signalling enhances osteogenesis in UMR-106 cell line. J Mol Neurosci. 2014;54:555–573. doi: 10.1007/s12031-014-0389-1. [DOI] [PubMed] [Google Scholar]
- Juhasz T, et al. Mechanical loading stimulates chondrogenesis via the PKA/CREB-Sox9 and PP2A pathways in chicken micromass cultures. Cell Signal. 2014;26:468–482. doi: 10.1016/j.cellsig.2013.12.001. [DOI] [PubMed] [Google Scholar]
- Juhasz T, Helgadottir SL, Tamas A, Reglodi D, Zakany R. PACAP and VIP signaling in chondrogenesis and osteogenesis. Peptides. 2015;66:51–57. doi: 10.1016/j.peptides.2015.02.001. [DOI] [PubMed] [Google Scholar]
- Juhasz T, et al. Pituitary adenylate cyclase activating polypeptide (PACAP) pathway is induced by mechanical load and reduces the activity of hedgehog signaling in chondrogenic micromass cell cultures. Int J Mol Sci. 2015;16:17344–17367. doi: 10.3390/ijms160817344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katona E, et al. PP2B and ERK1/2 regulate hyaluronan synthesis of HT168 and WM35 human melanoma cell lines. Int J Oncol. 2016;48:983–997. doi: 10.3892/ijo.2015.3313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs-Valasek A, et al. Accelerated retinal aging in PACAP knock-out mice. Neuroscience. 2017;348:1–10. doi: 10.1016/j.neuroscience.2017.02.003. [DOI] [PubMed] [Google Scholar]
- Krajewska-Włodarczyk Magdalena, Owczarczyk-Saczonek Agnieszka, Placek Waldemar, Osowski Adam, Wojtkiewicz Joanna. Articular Cartilage Aging-Potential Regenerative Capacities of Cell Manipulation and Stem Cell Therapy. International Journal of Molecular Sciences. 2018;19(2):623. doi: 10.3390/ijms19020623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laasanen MS, Töyräs J, Korhonen RK, Rieppo J, Saarakkala S, Nieminen MT, Hirvonen J, Jurvelin JS. Biomechanical properties of knee articular cartilage. Biorheology. 2003;40:133–140. [PubMed] [Google Scholar]
- Lahm A, Dabravolski D, Spank H, Merk H, Esser J, Kasch R. Regional differences of tibial and femoral cartilage in the chondrocyte gene expression, immunhistochemistry and composite in different stages of osteoarthritis. Tissue Cell. 2017;49:249–256. doi: 10.1016/j.tice.2017.02.004. [DOI] [PubMed] [Google Scholar]
- LaRoche DP, Melanson EL, Baumgartner MP, Bozzuto BM, Libby VM, Marshall BN. Physiological determinants of walking effort in older adults: should they be targets for physical activity intervention? GeroScience. 2018;40:305–315. doi: 10.1007/s11357-018-0032-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lefebvre V, Behringer RR, de Crombrugghe B. L-Sox5, Sox6 and Sox9 control essential steps of the chondrocyte differentiation pathway. Osteoarthr Cartil. 2001;9(Suppl A):S69–S75. doi: 10.1053/joca.2001.0447. [DOI] [PubMed] [Google Scholar]
- Li L, Duan X, Fan Z, Chen L, Xing F, Xu Z, Chen Q, Xiang Z. Mesenchymal stem cells in combination with hyaluronic acid for articular cartilage defects. Sci Rep. 2018;8:9900. doi: 10.1038/s41598-018-27737-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Chia-Feng, Lefebvre Véronique. The transcription factors SOX9 and SOX5/SOX6 cooperate genome-wide through super-enhancers to drive chondrogenesis. Nucleic Acids Research. 2015;43(17):8183–8203. doi: 10.1093/nar/gkv688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansouri S, Lietzau G, Lundberg M, Nathanson D, Nystrom T, Patrone C. Pituitary adenlylate cyclase activating peptide protects adult neural stem cells from a hypoglycaemic milieu. PLoS One. 2016;11:e0156867. doi: 10.1371/journal.pone.0156867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matta C, Fodor J, Szijgyarto Z, Juhasz T, Gergely P, Csernoch L, Zakany R. Cytosolic free Ca2+ concentration exhibits a characteristic temporal pattern during in vitro cartilage differentiation: a possible regulatory role of calcineurin in Ca-signalling of chondrogenic cells. Cell Calcium. 2008;44:310–323. doi: 10.1016/j.ceca.2007.12.010. [DOI] [PubMed] [Google Scholar]
- Matta C, et al. PKCdelta is a positive regulator of chondrogenesis in chicken high density micromass cell cultures. Biochimie. 2011;93:149–159. doi: 10.1016/j.biochi.2010.09.005. [DOI] [PubMed] [Google Scholar]
- Meschiari CA, Ero OK, Pan H, Finkel T, Lindsey ML. The impact of aging on cardiac extracellular matrix. GeroScience. 2017;39:7–18. doi: 10.1007/s11357-017-9959-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyata A, Arimura A, Dahl RR, Minamino N, Uehara A, Jiang L, Culler MD, Coy DH. Isolation of a novel 38 residue-hypothalamic polypeptide which stimulates adenylate cyclase in pituitary cells. Biochem Biophys Res Commun. 1989;164:567–574. doi: 10.1016/0006-291X(89)91757-9. [DOI] [PubMed] [Google Scholar]
- Mora JC, Przkora R, Cruz-Almeida Y. Knee osteoarthritis: pathophysiology and current treatment modalities. J Pain Res. 2018;11:2189–2196. doi: 10.2147/JPR.S154002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nacarelli Timothy, Azar Ashley, Altinok Oya, Orynbayeva Zulfiya, Sell Christian. Rapamycin increases oxidative metabolism and enhances metabolic flexibility in human cardiac fibroblasts. GeroScience. 2018;40(3):243–256. doi: 10.1007/s11357-018-0030-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niewiadomski P, Zhujiang A, Youssef M, Waschek JA. Interaction of PACAP with Sonic hedgehog reveals complex regulation of the hedgehog pathway by PKA. Cell Signal. 2013;25:2222–2230. doi: 10.1016/j.cellsig.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishimura Riko, Hata Kenji, Nakamura Eriko, Murakami Tomohiko, Takahata Yoshifumi. Transcriptional network systems in cartilage development and disease. Histochemistry and Cell Biology. 2018;149(4):353–363. doi: 10.1007/s00418-017-1628-7. [DOI] [PubMed] [Google Scholar]
- Poulet Blandine, Staines Katherine A. New developments in osteoarthritis and cartilage biology. Current Opinion in Pharmacology. 2016;28:8–13. doi: 10.1016/j.coph.2016.02.009. [DOI] [PubMed] [Google Scholar]
- Redondo Michael L., Naveen Neal B., Liu Joseph N., Tauro Tracy M., Southworth Taylor M., Cole Brian J. Preservation of Knee Articular Cartilage. Sports Medicine and Arthroscopy Review. 2018;26(4):e23–e30. doi: 10.1097/JSA.0000000000000226. [DOI] [PubMed] [Google Scholar]
- Reglodi Dora, Atlasz Tamas, Jungling Adel, Szabo Edina, Kovari Petra, Manavalan Sridharan, Tamas Andrea. Alternative Routes of Administration of the Neuroprotective Pituitary Adenylate Cyclase Activating Polypeptide. Current Pharmaceutical Design. 2019;24(33):3892–3904. doi: 10.2174/1381612824666181112110934. [DOI] [PubMed] [Google Scholar]
- Reglodi D., Atlasz T., Szabo E., Jungling A., Tamas A., Juhasz T., Fulop B. D., Bardosi A. PACAP deficiency as a model of aging. GeroScience. 2018;40(5-6):437–452. doi: 10.1007/s11357-018-0045-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reglodi D, et al. Disturbed spermatogenic signaling in pituitary adenylate cyclase activating polypeptide-deficient mice. Reproduction. 2018;155:129–139. doi: 10.1530/REP-17-0470. [DOI] [PubMed] [Google Scholar]
- Reglodi D, Vaczy A, Rubio-Beltran E, MaassenVanDenBrink A (2018d) Protective effects of PACAP in ischemia J Headache Pain 19:19 doi:10.1186/s10194-018-0845-3 [DOI] [PMC free article] [PubMed]
- Sandor B, et al. Structural and morphometric comparison of the molar teeth in pre-eruptive developmental stage of PACAP-deficient and wild-type mice. J Mol Neurosci. 2014;54:331–341. doi: 10.1007/s12031-014-0392-6. [DOI] [PubMed] [Google Scholar]
- Satake Y, Takahashi K, Saito M, Takai S. Objective colorimetric evaluation of aging-related articular cartilage degeneration. J Nippon Med School. 2018;85:157–165. doi: 10.1272/jnms.JNMS.2018_85-23. [DOI] [PubMed] [Google Scholar]
- Szabadfi K, et al. Pituitary adenylate cyclase activating polypeptide, a potential therapeutic agent for diabetic retinopathy in rats: focus on the vertical information processing pathway. Neurotox Res. 2016;29:432–446. doi: 10.1007/s12640-015-9593-1. [DOI] [PubMed] [Google Scholar]
- Szentléleky Eszter, Szegeczki Vince, Karanyicz Edina, Hajdú Tibor, Tamás Andrea, Tóth Gábor, Zákány Róza, Reglődi Dóra, Juhász Tamás. Pituitary Adenylate Cyclase Activating Polypeptide (PACAP) Reduces Oxidative and Mechanical Stress-Evoked Matrix Degradation in Chondrifying Cell Cultures. International Journal of Molecular Sciences. 2019;20(1):168. doi: 10.3390/ijms20010168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temple-Wong MM, Ren S, Quach P, Hansen BC, Chen AC, Hasegawa A, D’Lima DD, Koziol J, Masuda K, Lotz MK, Sah RL. Hyaluronan concentration and size distribution in human knee synovial fluid: variations with age and cartilage degeneration. Arthritis Res Ther. 2016;18:18. doi: 10.1186/s13075-016-0922-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian Q, et al. RHEB1 insufficiency in aged male mice is associated with stress-induced seizures. GeroScience. 2017;39:557–570. doi: 10.1007/s11357-017-9997-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzellos TG, et al. Extrinsic ageing in the human skin is associated with alterations in the expression of hyaluronic acid and its metabolizing enzymes. Exp Dermatol. 2009;18:1028–1035. doi: 10.1111/j.1600-0625.2009.00889.x. [DOI] [PubMed] [Google Scholar]
- Varela-Eirin M, Loureiro J, Fonseca E, Corrochano S, Caeiro JR, Collado M, Mayan MD. Cartilage regeneration and ageing: targeting cellular plasticity in osteoarthritis. Ageing Res Rev. 2018;42:56–71. doi: 10.1016/j.arr.2017.12.006. [DOI] [PubMed] [Google Scholar]
- Varga Z, et al. Switch of voltage-gated K+ channel expression in the plasma membrane of chondrogenic cells affects cytosolic Ca2+−oscillations and cartilage formation. PLoS One. 2011;6:e27957. doi: 10.1371/journal.pone.0027957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaudry D, et al. Pituitary adenylate cyclase-activating polypeptide and its receptors: 20 years after the discovery. Pharmacol Rev. 2009;61:283–357. doi: 10.1124/pr.109.001370. [DOI] [PubMed] [Google Scholar]
- Wang IE, Mitroo S, Chen FH, Lu HH, Doty SB. Age-dependent changes in matrix composition and organization at the ligament-to-bone insertion. J Orthop Res. 2006;24:1745–1755. doi: 10.1002/jor.20149. [DOI] [PubMed] [Google Scholar]
- Wu ZL, Ciallella JR, Flood DG, O’Kane TM, Bozyczko-Coyne D, Savage MJ. Comparative analysis of cortical gene expression in mouse models of Alzheimer’s disease. Neurobiol Aging. 2006;27:377–386. doi: 10.1016/j.neurobiolaging.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Zakany R, et al. Okadaic acid-induced inhibition of protein phosphatase 2A enhances chondrogenesis in chicken limb bud micromass cell cultures. Anat Embryol. 2001;203:23–34. doi: 10.1007/s004290000128. [DOI] [PubMed] [Google Scholar]
- Zakany R, et al. Protein phosphatase 2A is involved in the regulation of protein kinase A signaling pathway during in vitro chondrogenesis. Exp Cell Res. 2002;275:1–8. doi: 10.1006/excr.2002.5487. [DOI] [PubMed] [Google Scholar]
- Zakany R, et al. Hydrogen peroxide inhibits formation of cartilage in chicken micromass cultures and decreases the activity of calcineurin: implication of ERK1/2 and Sox9 pathways. Exp Cell Res. 2005;305:190–199. doi: 10.1016/j.yexcr.2004.12.016. [DOI] [PubMed] [Google Scholar]
- Zevenbergen L., Gsell W., Cai L., Chan D.D., Famaey N., Vander Sloten J., Himmelreich U., Neu C.P., Jonkers I. Cartilage-on-cartilage contact: effect of compressive loading on tissue deformations and structural integrity of bovine articular cartilage. Osteoarthritis and Cartilage. 2018;26(12):1699–1709. doi: 10.1016/j.joca.2018.08.009. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Wang F, Tan H, Chen G, Guo L, Yang L. Analysis of the mineral composition of the human calcified cartilage zone. Int J Med Sci. 2012;9:353–360. doi: 10.7150/ijms.4276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M, Lu Q, Miller AH, Barnthouse NC, Wang J. Dynamic epigenetic mechanisms regulate age-dependent SOX9 expression in mouse articular cartilage. Int J Biochem Cell Biol. 2016;72:125–134. doi: 10.1016/j.biocel.2016.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]