Abstract
Chronic diseases have become serious threats to public health in China; the risk is particularly high for internal migrants. Chronic disease education is a key to the prevention and control of chronic diseases for such population. The national population-based Migrants Population Dynamic Monitoring Survey (MPSMA) was used to examine the current status and delivery methods of chronic disease education among internal migrants, from both provincial level and individual’s level. The study population included 402 587 internal migrants. Multilevel logistic regression was used to investigate factors that were related to chronic diseases education. In total, only 33.9% of the participants received chronic disease education. In the final model, parameter estimates on key variables from both individual and provincial level were significant (P < .001). Participants from provinces with higher level of health care resources and lower density of internal migrants were more likely to receive chronic disease education. The percentage and methods of receiving education varied across different age groups. This study suggests that future chronic disease education in China need to be more focused on areas with high density of internal migrants and younger internal migrants with low level of education and income. Attention should be paid to use tailored education methods to different populations.
Keywords: chronic disease, health education, internal migrants, health services accessibility, secondary data analysis
What do we already know about this topic?
Chronic disease education is crucial to chronic disease education among internal migrants who suffered high chronic disease risk and health inequalities comparing with local residents.
How does your research contribute to the field?
This research used Big Data and multilevel logistic regression models to examine current status, predicating factors, and delivery methods of chronic disease education among internal migrants.
What are your research’s implications toward theory, practice, or policy?
Our study indicates that future chronic disease education in China need to heighten attention to focus on areas with high density of internal migrants and younger internal migrants with low educational level and low income; also attention should be paid to use different education methods to target audience from different age groups.
Introduction
Chronic diseases have become serious threats to public health in China, accounting for 86.6% of total death and more than 70% of disease burden.1 What is even worse is that China is undergoing a period of rapid urbanization, environmental changes, and aging problem, which are predicted to increase the burden of chronic diseases.2 The Chinese government has implemented a plan of chronic diseases prevention and control (2017-2025) to confront this challenge and developed strategies particularly focused on the at-risk populations, including migrant populations.1
The rapid increase of internal migrant population in China, which reached to 282 million by the year 2016, has generated a great difficulty in prevention and control of chronic diseases, and required special attention.3 Internal migrants in China refer to those who migrate across county boundaries and reside in other areas of China without local household registration.4 The local household registration is permanent residence permission in the receiving area, aiming at control of population mobility. More importantly, local household registration is also decisive eligibility for local public health care and other social benefits.5 Therefore, without local household registration, combined with insufficient provisions of public health care, internal migrants generally have poor access to health care and other social benefits in the receiving areas.6 Generally speaking, there exist health care access inequalities between local residents and internal migrants.7 In addition, comparing with local residents, internal migrants are at socioeconomically disadvantaged status, as they are likely to be engaged in low-paying jobs in labor-intensive industries, which may cause socioeconomic disparities in health.8,9 Furthermore, many of them have unhealthy lifestyle, including relatively high prevalence of tobacco, excessive alcohol consumption, insufficient intake of vegetable and fruit, and physical inactivity, which would lead to high risk of chronic diseases.10
Health education is a key element to health promotion. Chronic disease education plays a significant role in chronic disease control and prevention for internal migrants. Although internal migrants, comparing with local residents, are generally less accessible to adequate health care service and comfortable housing, adoption of healthy lifestyle could help to reduce chronic disease risk created by socioeconomic disadvantages among internal migrants.11-13 With better knowledge of chronic disease, internal migrants can better assess outcomes of their daily behaviors, which is beneficial for them to shape a healthy lifestyle.14-17 On the contrary, patients with chronic diseases make everyday decisions to manage their illness according to their knowledge about the disease, and patient self-management has been proved to be effective to chronic disease care and control, which requires patients to apply their knowledge to care process.18,19
Despite the importance of chronic disease knowledge among internal migrants, very little is known about the current status and delivery methods of chronic disease education among internal migrants. This knowledge could inform policymakers to design policy and health care professionals to deliver the education in the most effective way. To address this knowledge gap, we used data from the national population-based Migrants Population Dynamic Monitoring Survey (MPSMA) to test whether resources at provincial level are associated with individual’s chronic diseases knowledge education and to examine the rate of education received on chronic diseases knowledge and education methods in different age groups. The research questions are listed as follows:
What individual and provincial characters were associated with internal migrants receiving chronic diseases education?
Were there any significant differences in chronic disease education receiving rate among internal migrants across different age groups?
Were there significant differences in effective education methods among internal migrants in different age groups?
Methods
Data
We used data collected by 2014 and 2015 waves of the MPSMA in China. The 2014 and 2015 MPSMA was approved by the National Health and Family Planning Commission Ethics Review Board, and all participants provided informed consent. This second data analysis was approved by the School of Nursing, Fudan University (IRB#TYSA2016-3-1). The MPSMA was annually conducted in migrants’ destination areas by the Migrant Population Service Center of China, aiming at evaluating condition of public health use and improving effect of related policy. The MPSMA took annual national data of migrants from each province as the sampling frame, and used a stratified 3-stage probability proportionate to size (PPS) sampling. The survey covered 433 cities from all 31 provinces in mainland China. To participate in the survey, the respondents had to be aged more than 18 years, migrated across county boundaries, and resided in the area at the time of the survey for more than 1 month. All participants received a written informed consent form and an oral explanation of the purpose and content of the research. The survey was conducted through a face-to-face interview. The national representative sample contains 402 587 respondents with relatively small sampling errors within acceptable range.18,20
Measures
Dependent variable
To determine the condition of receiving chronic disease education among internal migrants, we measured whether the internal migrants had received chronic disease education in the residing areas, and what kind of methods they used to receive such education. We used self-reported responses to a question that whether they had received any chronic disease education during their stay in the residing areas. (1 = yes, 0 = otherwise). If they had, they were asked to report the methods of chronic disease education received by choosing from the following response categories: lecture, book/magazine, media, face-to-face consultation, online health care consultation, community advocacy, bulletin board, and SMS/WeChat. WeChat is the most widely used Chinese multipurpose app with messaging and social media.
Independent Variables
Provincial-level variables
We used 3 macro variables to measure population structure and health care resources in each province: density of health care professionals (number of health care professionals per 1000 population), density of internal migrants (total number per 10 000 population), and age structure of the local population (portion of population aged 60 and above in the whole population). The data of health care professionals’ density and population aged structure were collected from Statistical Yearbook of China 2015 released by National Bureau of Statistics of PRC, and the data of density of migrants were collected by China’s sampling survey on 1% of the population in 2015.
Individual-level variables
Sociodemographic variables
The sociodemographic variables included age (18-95; age was top coded as 95), gender (1 = female, 0 = male), and marital status (1 = married or living with partner, 0 = otherwise). We measured socioeconomic status (SES) by educational levels (0 = middle school and below, 1 = high school or equivalent, 2 = college, 3 = graduate or professional), monthly income (0 = less than 1500, 1 = 1500-5000, 3 = more than 5000, calculated in Chinese currency CNY, which equals to $0.160 in 2015), health record, which is an electronic file to record personal health information for both health service providers and individuals (1 = had health record, 0 = otherwise), and basic medical insurance (1 = had basic medical insurance, 0 = otherwise).
Migration characteristics
We measured condition of migration through 4 migrant-related covariates: reasons of migration (1 = working or studying, 0 = otherwise), migration duration (continuous variable calculated by year), type of household registration (1 = rural, 0 = urban), and preference of long-term (over 5 years) living in the receiving area (1 = had preference of long-term living, 0 = otherwise).
Data Analysis
We used weighted analysis to describe the characteristics of participants and provincial variation of education receiving rates on chronic diseases. In addition, we conducted hierarchical logistic regression modeling (HLM) to explore the relationship between age and provincial characteristics with chronic disease education controlling for other covariates. HLM accommodates variance among migrants in the same province, as well as captures mathematical differences among provinces and migrants. We performed following 3 steps of multilevel logistic regression models to estimate the effects of provincial characters and age on chronic disease education. For all 3 models, level 1 is individual level, whereas level 2 is provincial level. Model 1 is a null model which separates total variance according to individual level and provincial level. Intraclass correlation coefficient (ICC) was used to determine the accuracy of the estimation. According to the clustering of data, we decided to calculate the Design Effect (DEFF), which is based on the ICC and the average cluster size. If DEFF ≥ 2, we found it necessary to build the multilevel logistic regression model. Model 2 is random coefficient model which includes all covariates on individual level with random effect. Model 3 is the outcomes model, in which intercepts and slopes are both used by coefficient. Considering the sample size, we considered a 2-tailed P value less than .001 for statistical significance in all analyses. We used SPSS, version 23.0 (Armonk, NY: IBM Corp.) and HLM 7.0 to conduct data analysis.
Results
Population Characteristics
Table 1 provides the characteristics information of the sampled population. The sampled population included 402 587 internal migrants. Fifty-seven percentage of participants were male, with an average age of 35.4 (SD = 9.7). The age range for the vast majority of the participants was from 18 to 35 (53.5%) and 36 to 60 (43.7%). More than 65% of the participants obtained an education level of 9th grade or less. More than half (56.2%) of the participants showed preference for long-term residence. Only 26.1% of the participants had health record. The average migration duration was 5.61 (SD = 4.89) years.
Table 1.
Demographic Characteristics and Outcomes Among Migrants, Pooled Migrants Population Dynamic Monitoring Survey Data 2014–2015 (N = 402 587).
| Variables | Percentage/Mean (SD) |
|---|---|
| Female (%) | 48.6 |
| Age, mean (SE) | 35.4 (9.7) |
| Marital status (%) | |
| Married | 81.4 |
| Single | 19.6 |
| Educational attainment (%) | |
| <Middle school | 65.8 |
| High school or equivalent | 21.0 |
| College | 12.8 |
| >College degree | 0.4 |
| Monthly income, mean (SD) | 7075.6 (10 160.2) |
| Having health record (%) | 26.1 |
| Having urban resident medical basic insurance (%) | 5.7 |
| Long-term residence inclination (%) | |
| Yes | 56.2 |
| No or unsure | 43.8 |
| Length of migration, mean (SD) | 5.61 (4.89) |
| Reason of migration (%) | |
| Working or studying | 89.8 |
| Others | 10.5 |
| Type of household (%) | |
| Rural | 84.0 |
| Urban | 16.0 |
| Received chronic disease education (%) | 33.9 |
Portion and Methods of Chronic Disease Education Among Internal Migrants
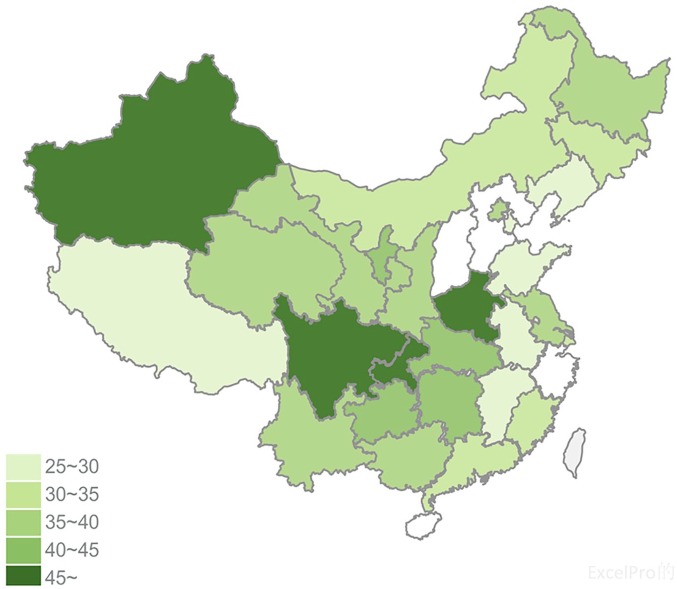
In full sample, only 33.9% of the participants received chronic disease education (Table 1). Figure 1 shows the education rates on chronic diseases among internal migrants by province. Among 31 provinces of Chinese mainland, there were 7 provinces that showed an above 40% rate of chronic disease education, while 4 provinces reported a less than 25% education rate among respondents. Chongqing showed the highest education rate of 52.7% while Hebei Province showed the lowest rate of 21.2%. Generally, provinces in western and middle regions had higher education rate than that in the east region.
Figure 1.
Rate of internal migrants receiving chronic disease education among 31 provinces in China.
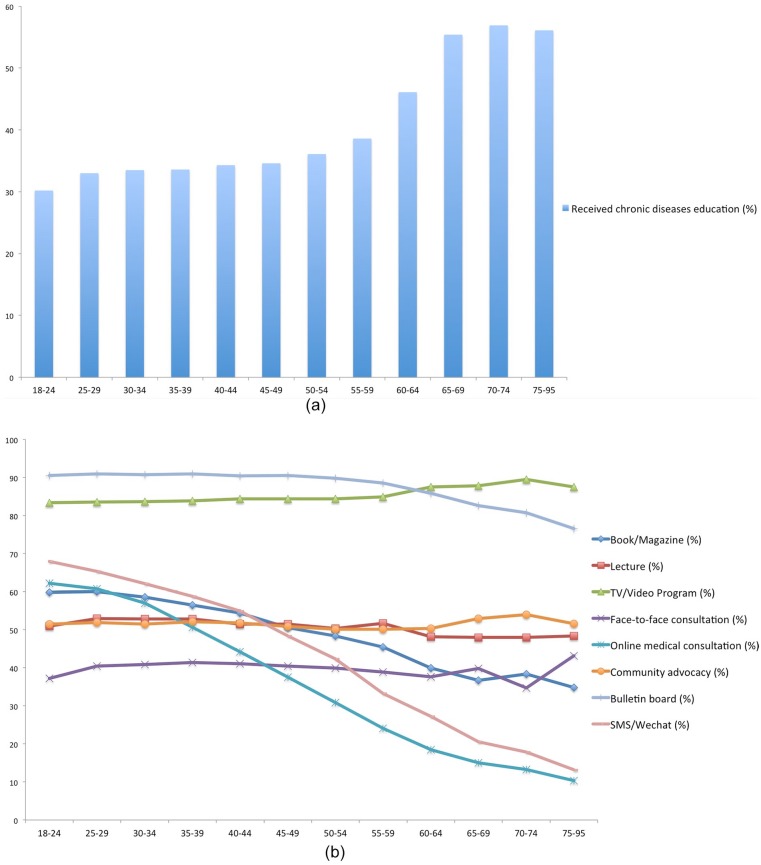
Figure 2(a) shows information of education rates among different age groups. In terms of age groups, the finding shows a tendency that older age groups have higher rate of receiving chronic disease education. The participants aged 70 to 74 years reported the highest portion of chronic disease education (56.9%) while age group of 18 to 24 reported lowest rate of 30.2%, and there existed a sharp increase among groups of aged 55 to 59, 60 to 64, and 65 to 69. Figure 2(b) presents frequencies of using various approaches of receiving the information across different age groups. In full sample, bulletin board (90.6%), TV/video programs (84.0%), and SMS/WeChat (58.0%) were the most common methods of receiving chronic diseases education. The frequency of using online medical consultation and SMS/WeChat showed a trend of decline with increasing age; the rates were the highest in the age group 18 to 24 (62.2% and 68%, respectively) and the lowest in group 75 to 95 (10.3% and 13.2%, respectively). In general, the use frequency of new media including online consultation and SMS/Wechat was relatively low in groups aged 60 and above.
Figure 2.
(a) Education rate of chronic disease by age among migrants, pooled Migrants Population Dynamic Monitoring Survey Data 2014-2015. (b) Frequencies of using various approaches of receiving chronic diseases by age among migrants, pooled Migrants Population Dynamic Monitoring Survey Data 2014-2015.
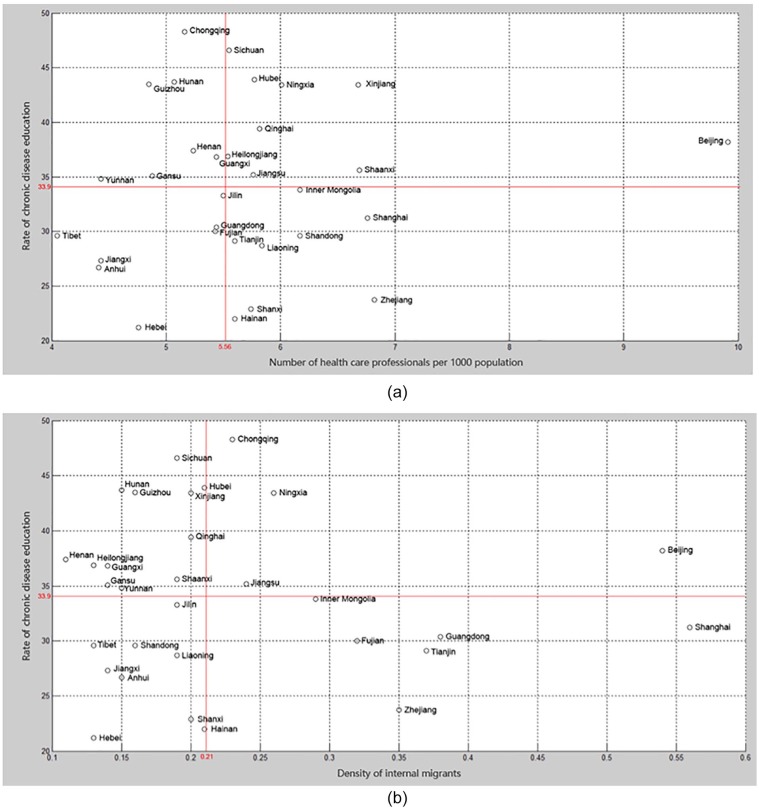
Figure 3 presents the associations of the education rate and health care resources as well as internal migrants’ density among 31 provinces. Average number of health care professionals in 1000 population was 5.56, and average density of internal migrants was 0.21. Due to high-level health care resources and internal migrants density, Beijing had a relatively high rate of receiving chronic disease education, while Shanghai and Zhejiang presented low education rate. As main migration destinations, Guangdong, Tianjin, and Fujian with high level of migration density reported relatively low education rate. Anhui, Hebei, Jiangxi, and Tibet with limited health care resources also showed low education rate.
Figure 3.
(a) Rate of chronic disease education among internal migrants and number of health care professionals per 1000 population in 31 provinces. (b) Rate of chronic disease education among internal migrants and density of internal migrants in 31 provinces.
Multilevel Logistic Regression
Table 2 presents results of multilevel logistic regression models. Model 3 shows that the following factors were associated with a higher likelihood of receiving chronic disease education: male participants with older age, higher education level, higher monthly income, with basic medical insurance, health record, urban household registration, shorter migration duration, and with long-term residence preference (more than 5 years), and from province with higher portion of older people, more health care resources, and lower density of internal migrants.
Table 2.
Fixed-Effect and Random-Effect Estimates for Models of Receiving CHRONIC DISEASES Education, Pooled Migrants Population Dynamic Monitoring Survey Data 2014–2015.
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | CI | P | OR | CI | P | OR | CI | P | |
| Fixed effects | |||||||||
| Intercept, γ00 | 0.514 | 0.510, 0.517 | .000 | 0.237 | 0.223, 0.252 | .000 | 0.169 | 0.158, 0.181 | .000 |
| Individual level | |||||||||
| Age, β1j | 1.011 | 1.010, 1.012 | .000 | 1.010 | 1.009, 1.011 | .000 | |||
| Female, β2j | 0.987 | 0.973, 1.001 | .062 | 0.982 | 0.968, 0.995 | .000 | |||
| Married, β3j | 1.124 | 0.874, 0.908 | .000 | 1.116 | 0.879, 0.914 | .000 | |||
| Educational level, β4j | 1.219 | 1.203, 1.234 | .000 | 1.214 | 1.199, 1.230 | .000 | |||
| Monthly income, β5j | 1.067 | 1.059, 1.074 | .000 | 1.078 | 1.071, 1.086 | .000 | |||
| Having health record, β6j | 2.215 | 2.183, 2.248 | .000 | 2.206 | 2.174, 2.239 | .000 | |||
| Having basic medical insurance, β7j | 1.222 | 0.797, 0.841 | .000 | 1.214 | 0.802, 0.846 | .000 | |||
| Rural household, β8j | 0.917 | 0.899, 0.935 | .000 | 0.937 | 0.918, 0.956 | .000 | |||
| Having long-term preference more than 5 years, β9j | 1.266 | 1.248, 1.285 | .000 | 1.250 | 1.232, 1.268 | .000 | |||
| Migration duration, β10j | 0.939 | 0.933, 0.945 | .000 | 0.934 | 0.927, 0.940 | .000 | |||
| Migrate for working or studying, β11j | 1.020 | 0.961, 1.001 | .058 | 1.036 | 0.941, 0.981 | .000 | |||
| Province level | |||||||||
| Age structure of migrants (number of elderly more than 60 years old per 100 population) γ01 | 1.086 | 1.077, 1.094 | .000 | ||||||
| Density of health care professionals (total number per 1000 population), γ02 | 1.061 | 1.052, 1.070 | .000 | ||||||
| Density of migrants (total number per 100 000), γ03 | 0.626 | 0.581, 0.676 | .000 | ||||||
| Random effects | |||||||||
| Intercept variance, | 0.000 | 0.044 | 0.061 | ||||||
| Level 1 variance, | 3.290 | 3.290 | 3.290 | ||||||
| −2LL | 572 429.6 | 571 999.9 | 571 849.0 | ||||||
Note. OR = odds ratio; CI = confidence interval; LL = log-likelihood ratio test.
Discussion
To the best of our knowledge, this is the first study using a nationally based data to examine the current status of chronic disease education among internal migrants in China. Our study indicates that provincial characters played an important role in internal migrants receiving chronic disease education. There exist significant differences in rates and methods of receiving chronic disease education across age groups.
Our study findings suggest that provincial health care resources were positively associated with the rate of chronic disease education among internal migrants. A previous study showed that the health of internal migrants did not benefit from local public health care service provisions, mainly due to barriers created by the household registration system.21 This finding implied that it is difficult to promote internal migrants’ health by increasing allocation of health care resources. Comparing with health care service, health education is more equally accessible for internal migrants and local residents due to media publicity, regardless of restriction created by household registration.22 Therefore, increasing input in health care resources could help indirectly improve health condition among internal migrants by improving their chronic disease knowledge and keeping healthy habits, which is important to health promotion and beneficial to break down pattern of health inequalities between internal migrants and local residents.
In addition, participants from provinces with higher density of internal migrants were less likely to receive chronic disease education, which should be attributed to condition in Shanghai, Guangdong, Tianjin, Zhejiang, and Fujian. These provinces with extremely high density of internal migration reported low education rate that is far below average. As main migration destinations located in eastern China, these provinces generally hold high threshold for household registration to restrict a large number of internal migrants to transfer into local residents, in case of predictably increasing burdens to public services.23 In addition, local dialect in these provinces hold dominant position in daily language use, especially in Guangdong, Fujian, Shanghai, and Zhejiang, where local dialects are quite different from mandarin (official language in China) and hard for internal migrants to understand and speak. These circumstances lead to difficulty of cultural recognition and social integration for internal migrants.24 As a result, comparing with middle and western China, internal migrants in these eastern areas suffered a lower level of social integration and less interaction with local residents.25 Internal migrants with better social integration condition were more open-minded to the information provided by local communities. A previous study showed that internal migrants with better social integration were more likely to use public health services, which made them more accessible to receive chronic disease education.6 Moreover, it should be noted that these provinces are also developed areas in China. Comparing with underdeveloped areas, developed areas generally hold bigger spatial variation on house rent. In developed areas, the gap of house rent between urban center and rural or urban-rural fringe areas is larger than that in underdeveloped areas, which is also a reflection of larger income gap in developed areas.26 As a result, internal migrants, who are generally engaged in low-paying jobs, are more likely to gather in outskirt, rural or urban-rural fringe areas to save living cost.27 We used MPSMA data to make additional analysis on living environment of internal migrants and found that in provinces with dense internal migration, portion of internal migrants living in rural or urban-rural fringe areas is significantly higher than that in other provinces. For example, in Hunan, a less-developed province with low density of internal migrants, there were 14.3% of internal migrants living in rural or urban-rural fringe areas; while in Zhejiang, the developed province with high density of internal migrants, the portion reached up to 57%. Different from developed countries, there exist huge disparities between urban and rural areas in China.28 Rural or urban-rural fringe areas in China are generally unable to provide high-quality living environment, adequate facilities, or community health care service.29 Considering the vital role of community advocacy in health education, participants from provinces with higher density of internal migrants were less likely to receive chronic disease education.29 This presented a problem that provinces with larger number of internal migrants have already faced a greater challenge of health care, which could be even exacerbated by increasing burden resulted from lower rate of chronic disease education. In addition, provinces with high migrants’ density are main migration destination areas in China, where internal migrants seek for improvement of life quality. However, internal migrants in those areas showed low rate of chronic disease education, which hindered procedure of chronic disease prevention and control. So, main migration destinations should particularly make effort in improving chronic disease education for internal migrants, especially in rural or urban-rural fringe areas.
Our study also shows that there is an age difference in approaches of receiving chronic disease education. Older internal migrants from province with higher density of older population were more likely to receive chronic disease education, and older age groups had a higher rate of receiving chronic disease education than younger age groups. This trend is consistent with age distribution of chronic diseases incidence.30,31 Another finding worth noting is that the rate of receiving chronic disease education among younger groups were much lower than that in older groups. For example, education rate of groups aged 18 to 39 years was approximately only half of that in groups aged 65 and above. This presented serious problems. First, chronic diseases are becoming more prevalent among young and middle-aged adults, which poses a challenge that requires more education on chronic disease.32 Second, primary risk factors for chronic diseases such as tobacco use, excessive alcohol consumption, lack of exercise, and poor nutrition are likely to occur at young age, especially in less-developed countries. It is more effective to address risk factors early through chronic disease education than trying to change behaviors in later life.32,33
Considering the importance of chronic disease education and low education rate among internal migrants, it is important to use effective methods to deliver the education. Previous research indicated that community activity is helpful to improve health services accessibility among internal migrants.29 Findings from this study also suggest that community-based education was very effective, as bulletin board was the most frequently used methods, and community advocacy also maintained a stable and relatively high level of use among all age groups. Our finding is also supported by previous study that younger and older groups have different preferences to education method.34 Online media (e.g., SMS/WeChat) are more preferable to younger adults, as it provides benefit to convenience and privacy, while older adults suffered more obstacles to access new technology such as vision problem or learning difficulty.35 With high-speed technology development in recent years, the use of new media is increasing, whereas the use of traditional media declines among internal migrants, especially in younger age groups, to which chronic disease education should particularly target to.36 However, despite increasing use of new media, our finding suggests that traditional media (e.g., TV/Video program) remained vital to chronic disease education among internal migrants, especially for older internal migrants. Therefore, to improve chronic disease education among internal migrants, more resources should be directed to community-based health services, and it is necessary to provide multiple options to internal migrants from different age groups.
Several other issues are worth the discussion. First, our finding indicates that with a better use of health services such as health records, internal migrants were more likely to receive chronic disease education, as health records could provide health knowledge and management. However, comparing with local residents with household registration, internal migrants maintained a much lower use of health record.6 Therefore, to improve the use of health record among internal migrants is important. Second, sociodemographic variables were significantly related to receiving chronic disease education. Participants who were married with higher education level, higher monthly income, and urban household registry were more likely to receive knowledge of chronic diseases. This indicates that chronic disease education should particularly focus on those rural internal migrants with low education level and low income.
Limitations
Our study has some limitations listed as following. First, the analysis was based on the self-reported data which may have reporting bias. Second, we used a cross-sectional analysis, which may fail to tease out cause-and-effect relationships. Third, the lack of data on chronic diseases and risk factors made this study unable to further identify diseases or risk factors associated with chronic diseases education. Future work in this direction will be particularly important to help develop public health interventions. Nonetheless, this study presents a valuable data for a future longitudinal analysis among migrants’ population.
Conclusion
Our study generated new knowledge about the chronic disease education among internal migrants in China. From 2014 to 2015, MPDMS data showed significant differences of receiving chronic disease education among different age groups and also showed provincial disparities with different level of public health care resources and internal migrants density. To enhance chronic disease education among internal migrants, local governments should increase investment on health care services. Attention should be paid to use different education methods to target audience from different age groups. Our study indicates that future chronic disease education in China need to heighten the attention to focus on areas with high density of internal migrants and younger internal migrants with low educational level and low income.
Footnotes
Author Contributions: M.G., Z.Z., and B.W. came up with the original idea for this article and also analyzed the data. M.G. wrote most of the manuscript. Z.Z., B.W., and T.D. helped draft and review the manuscript. Z.Z., B.W., and H.M. helped to revise the manuscript. M.G. and Z.Z. contributed equally to this work. All authors read and approved the final manuscript.
Author’s Note: Tingyue Dong is now affiliated with Beijing Administration Institute.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Mengdi Guo  https://orcid.org/0000-0002-4396-5748
https://orcid.org/0000-0002-4396-5748
References
- 1. General Office of the State Council of China. Medium and Long-Term Development Program of Chronic Diseases Prevention and Treatment in China (2017-2025). http://www.gov.cn/zhengce/content/2017-02/14/content_5167886.htm. Accessed February 14, 2017.
- 2. Beaglehole R, Epping-Jordan J, Patel V, et al. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet. 2008;372(9642):940-949. [DOI] [PubMed] [Google Scholar]
- 3. Wang L, Kong L, Wu F, Bai Y, Burton R. Preventing chronic diseases in China. Lancet. 2005;366:1821-1824. [DOI] [PubMed] [Google Scholar]
- 4. Gong P, Liang S, Carlton EJ, et al. Urbanisation and health in China. Lancet. 2012;379(9818):843-852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chan KW. The household registration system and migrant labor in China: notes on a debate. Popul Dev Rev. 2010;36(2):357-364. [DOI] [PubMed] [Google Scholar]
- 6. Zhang J, Lin S, Liang D, Qian Y, Zhang D, Hou Z. Public health services utilization and its determinants among internal migrants in china: evidence from a nationally representative survey. Int J Environ Res Public Health. 2017;14(9):1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rodriguez-Alvarez E, Lanborena N, Borrell LN. Health services access inequalities between native and immigrant in a Southern European region. Int J Health Serv. 2019;49(1):108-126. [DOI] [PubMed] [Google Scholar]
- 8. National Health and Family Planning Commission. China Migrants Population Development Report. Beijing, China: China Population Press; 2015. [Google Scholar]
- 9. Lipscomb HJ, Loomis D, McDonald MA, et al. A conceptual model of work and health disparities in the United States. Int J Health Serv. 2006;36(1):25-50. [DOI] [PubMed] [Google Scholar]
- 10. Chen ZH, Zhang M, Li YC, Huang ZJ, Wang LM. Co-prevalence of chronic disease risk factors and influencing factors in floating population in China. J Epidemic Dis China. 2017;38(9):1226-1230. [DOI] [PubMed] [Google Scholar]
- 11. Derose KP, Escarce JJ, Lurie N. Immigrants and health care: sources of vulnerability. Health Aff. 2007;26(5):1258-1268. [DOI] [PubMed] [Google Scholar]
- 12. Zhu Y. The floating population’s household strategies and the role of migration in China’s regional development and integration. Int J Popul Geogr. 2003;9(6):485-502. [Google Scholar]
- 13. Feng W, Zuo XJ, Ruan DC. Rural migrants in Shanghai: living under the shadow of socialism. Int Migr Rev. 2002;36(2):520-545. [Google Scholar]
- 14. Marmot M, Friel S, Bell R, Houweling TA, Taylor S. Commission on social determinants of health: closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661-1669. [DOI] [PubMed] [Google Scholar]
- 15. Khaw KT, Wareham N, Bingham S, Welch A, Luben R, Day N. Combined impact of health behaviors and mortality in men and women: the EPIC-Norfolk prospective population study. PLoS Med. 2008;5(1):e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Martinez-Gomez D, Guallar-Castillon P, Leon-Munoz LM, Lopez-Garcia E, Rodriguez-Artalejo F. Combined impact of traditional and non-traditional health behaviors on mortality: a national prospective cohort study in Spanish older adults. BMC Med. 2013; 11(1):47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Braveman P, Gruskin S. Defining equity in health. J Epidemiol Commun Health. 2003;57(4):254-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Holman H, Lorig K. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004;119(3):239-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002; 288(19):2469-2475. [DOI] [PubMed] [Google Scholar]
- 20. Rong B, Li L, Yuan C. The empirical study of migrant identity under the perspective of social change-based the migrant dynamic monitoring survey data in China. Popul Dev. 2013;6:19-25. [Google Scholar]
- 21. Wang Q. Health of the elderly migration population in China: benefit from individual and local socioeconomic status? Int J Environ Res Public Health. 2017;14(4):370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kwak N. Revisiting the knowledge gap hypothesis: education, motivation, and media use. Commun Res. 1999;26(4):385-413. [Google Scholar]
- 23. Sun Z. Explaining Regional Disparities of China’s Economic Growth: Geography, Policy and Infrastructure. Berkeley, CA: University of California; 2013. [Google Scholar]
- 24. Chen Z, Lu M, Xu L. Returns to dialect: identity exposure through language in the Chinese labor market. China Econ Rev. 2014;30:27-43. [Google Scholar]
- 25. Sun Y, Jia Z. The social integration among the floating population of China in 2012. China J Drug Depend. 2016;25:440-448. (in Chinese) [Google Scholar]
- 26. Lu M. Big Nation Needs Bigger City. Shanghai, China: Press of Shanghai People; 2016. [Google Scholar]
- 27. Chen Y, Yin Z, Xie Q. Suggestions to ameliorate the inequity in urban/rural allocation of healthcare resources in China. Int J Equity Health. 2014;13(1):34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Blanchard O, Giavazzi F. Rebalancing growth in China: a three handed approach. China World Econ. 2006;14(4):1-20. [Google Scholar]
- 29. Guo J, Wen HY, Zhou QY. Status and determinants on basic public health services of floating population. Chin J Health Policy. 2014;7:51-56. [Google Scholar]
- 30. Liang Y, Shi MC, Yu KY, et al. Age distribution of common chronic diseases and correlative analysis. J Chronic Dis Prev Contr China. 2003;11:170-171. (In Chinese) [Google Scholar]
- 31. Piazza JR, Charles ST, Almeida DM. Living with chronic health conditions: age differences in affective well-being. J Gerontol B Psychol Sci Soc Sci. 2007;62(6):313-121. [DOI] [PubMed] [Google Scholar]
- 32. Population Reference Bureau. Chronic Diseases Do Affect Youth. https://www.prb.org/youth-and-chronic-diseases/. Accessed September 8, 2011.
- 33. World Health Organization. Global Status Report on Non-communicable Diseases 2010. http://whqlibdoc.who.int/publications/2011/9789240686458_eng.pdf. Accessed September 2, 2011.
- 34. Kern DE, Bass EB, Thomas PA. Curriculum Development for Medical Education: A Six Step Approach. Baltimore, MA: Johns Hopkins University Press; 1998. [Google Scholar]
- 35. Centeno J. Methods of teaching and learning of the elderly: care in rehabilitation. Can J Nurs Informat. 2011;6(1):1-7. [Google Scholar]
- 36. Stephen AT, Galak J. The complementary roles of traditional and social media publicity in driving marketing performance. Fontainebleau. 2009;97:1-38. [Google Scholar]