Abstract
Background:
Prior studies in heroin use disorder reported low rates (10%) of suicidal intention with non-fatal opioid overdose but did not assess dimensional ratings of suicidal ideation. This study aims to quantify the frequency and intensity of ratings of desire to die and perceived overdose risk proximal to the most recent opioid overdose event among individuals admitted for opioid use disorder detoxification/stabilization.
Methods:
Cross-sectional study (June 2017-July 2018) assessing patterns of opioid use and variables related to overdose history was conducted in a not-for-profit psychiatric hospital. Adults (>18 years) with opioid use disorder were eligible and 120 of 122 participants completed all measures. Forty-one percent were women and 85% self-identified as white. Participants’ perceptions of the likelihood of overdose and their suicidal motivations (defined as desire to die) prior to most recent opioid overdose was self-rated on a scale of 0 (no desire to die/no risk of death) to 10 (I definitely wanted to die/I definitely thought I would die).
Results:
Most (92%) surviving opioid overdose used heroin/fentanyl; over half reported some desire to die prior to their most recent overdose, with 36% reporting strong (>7/10) desire to die and 21% reporting 10/10 “I definitely wanted to die.” Perceptions of overdose risk were also variable, with 30% reporting no (0/10) likelihood of overdose and 13% reporting a high (10/10) likelihood.
Conclusions:
Suicidal motivation prior to opioid overdose is common and falls along a continuum of severity. Longitudinal studies are needed to determine if suicide prevention interventions may reduce opioid overdose in those at risk.
Keywords: Opioid Use Disorder, Opioid Overdose, Suicide, Suicidal Motivation, Overdose Prevention
1. Introduction
Death related to opioid poisoning is epidemic and still increasing in the United States across all age groups, as is premature death by suicide (Bohnert and Ilgen, 2019; Cunningham et al., 2018; Oquendo and Volkow, 2018; VanHouten et al., 2019). These epidemics share common risk factors including severe or chronic trauma exposures, depression/anxiety and other mental health disorders, substance use disorders, and moderate-to-severe chronic pain (Dasgupta et al., 2018; Maloney et al., 2007; Rizvi et al., 2017; Trout et al., 2017) as well as population risk factors (e.g., regional barriers to health care) (Jones et al., 2018) and social determinants such as intergenerational, cumulative financial adversity (Case and Deaton, 2017).
Suicide attempt and unintentional opioid overdose also commonly co-occur within individuals. Among people with opioid use disorder (OUD), 20-30% of people report a history of both unintentional overdose and suicide attempt (Darke et al., 2015; Maloney et al., 2009). Large population studies confirm that individuals with OUD who survive an opioid overdose remain at significantly elevated risk for repeat, fatal opioid overdose (Olfson et al., 2018b) and for death by suicide (Bogdanowicz et al., 2016; Olfson et al., 2018a), compared to the general population. Multiple clinical correlates are associated with opioid overdose and/or suicidal behavior in those having OUD, including use of heroin (Baldwin et al., 2018; Dai et al., 2019; Darke et al., 2015; Hakansson et al., 2008; Park et al., 2018), history of opioid injection (Bohnert et al., 2011; Hakansson et al., 2008), multiple substance treatment admissions (Peterson et al., 2019), polysubstance use (Bohnert et al., 2011; Bradvik et al., 2009; Darke et al., 2004; Jonsson et al., 2007), benzodiazepine use (Bohnert et al., 2017; Darke, 1996; Hakansson et al., 2008; Jones and McAninch, 2015), co-occurring psychiatric disorder (Bohnert et al., 2017; Darke et al., 2004; Darke et al., 2015; Maloney et al., 2007), history of sexual/physical trauma (Bohnert et al., 2011; Darke et al., 2004; Stein et al., 2017), pain (Fudalej et al., 2015), violence directed toward other (Bohnert et al., 2011; Hakansson et al., 2008) and history of suicide attempt or persistent suicidal ideation (Darke et al., 2004; Darke et al., 2007; Hakansson et al., 2008; Maloney et al., 2007; Pan et al., 2014). Temporal trends with respect to prescription opioid overdose are worrisome: a large, multi-site Canadian study of opioid-related injuries from 2011-2017 show high rates of opioid-related suicide attempts (45% of the total sample), with the greatest rate increase among adolescents and older adults (Do et al., 2018). In the US, a significant increase in prescription opioid-related suicidality has been reported for older adults (West et al., 2015), a significant portion of adolescent prescription opioid misuse is suicidal (Zosel et al., 2013), and opioid-related suicide rates (predominantly prescription opioid-related) doubled between 1999 and 2009 (Braden et al., 2017). Emergency department visits for nonfatal substance overdose have noted greater self-harm intent among those taking opioids or sedatives, compared with other substances of abuse (Albert et al., 2015; Bohnert et al., 2018). A recent US hospital-based study of opioid overdose survivors reported 21% of the sample endorsed intentional self-harm verified by interview, almost exclusively using prescription opioids (Conner et al., 2018).
A significant challenge to understanding the overlap between unintentional and intentional opioid overdose is that most definitions conceptualize these as distinct events. Historically, studies in heroin use disorder samples reported that 10% or fewer make a suicide attempt by intentional opioid overdose, and thus concluded that most opioid overdose deaths in heroin use disorder are not misclassified suicides (Conner et al., 2007; Darke and Ross, 2001; Maloney et al., 2009; Tollefsen et al., 2016).
However, suicidal motivations occur along a continuum of intensity varying across time (Bergmans et al., 2017). Several studies have collected qualitative data on suicidal motivations prior to opioid overdose (Bennett et al., 2017; Conner et al., 2018; Darke and Ross, 2001; Do et al., 2018; Heale et al., 2003; Neale, 2000; Yarborough et al., 2016). Of these studies, only three were specific to OUD populations (Darke and Ross, 2001; Heale et al., 2003; Neale, 2000) and assessed suicide intention dichotomously, while also capturing narratives that reflect ambivalence about death and negative events preceding opioid overdose. The narratives in Neale et al. (2000) specifically convey reports of fatigue with life, inability to cope, or apathy about death without an immediate intent to die by suicide (Neale, 2000). A quantitative understanding of the prevalence of suicidal motivation prior to opioid overdose is a significant gap in the literature on this topic. Improved understanding of the association between suicidal motivations and opioid overdose events may be important to prevention, as current universal prevention strategies (e.g., reducing means by reducing opioid prescribing, naloxone rescue of opioid overdose, and providing access to behavioral health care, including medications to treat opioid use disorder) may not be sufficiently specific or timely in the case of a suicidally-motivated drug poisoning.
The aim of this study was to characterize suicidal motivation and overdose risk perceptions among individuals with a history of surviving an opioid overdose, who entered treatment for opioid use disorder. We assessed the degree to which, prior to their most recent opioid overdose, people with opioid use disorder (1) perceived that they would be likely to overdose, and (2) experienced a desire to die.
2. Methods
2.1. Participants
Adults age 18 years and older seeking treatment for opioid use disorder (N=356) were recruited from an inpatient detoxification/stabilization unit at an academically-affiliated psychiatric hospital. This program provides short-term stabilization and detoxification for people with substance use disorders. Inclusion criteria also required participants to be able to provide written informed consent and be currently enrolled in substance use disorder treatment. Participants were ineligible for the study if they presented with psychiatric or medical conditions or cognitive impairment that were so severe it would inhibit their ability to understand study questionnaires and perform study procedures; no participants were excluded for this reason.
Among the total 356 participants with substance use disorders recruited between June 2017 – July 2018 in a larger study of clinical characteristics of adults with substance use disorders, we studied a subset who reported seeking treatment for opioid use disorder (n=122). Two participants were excluded from the analysis because they failed to complete the study measures. The final study sample comprised 120 participants (41% female). The mean age was 34 years (SD=10.4) and the sample was 89% white and 7% Hispanic/Latinx. Of the 120 participants, 64% reported attending at least some college (2 years of college, associate degree or trade school), 37% were employed full-time and 59% were never married.
Most participants had a co-occurring psychiatric disorder (60%) and were current smokers (80%). Additionally, 32% had a prior history of suicide attempt (81% by overdose, 22% by hanging, 8% by wrist cutting, and 8% unknown or other), 15% had a prior history of self-harm (94% self-cutting, 12% head banging or self-hitting), and 26% had been engaged in mental health care at the time of admission. History of violent behavior was mostly associated with interpersonal/domestic violence, and 15% endorsed violent behavior. Several people declined to report race (n=5), education (n=1), marital status (n=1) or smoking status (n=2); medical record data on suicide, self-harm and violent behavior could not be accessed for 4 participants.
2.2. Procedure
Research staff recruited participants by describing the study purpose to groups of people receiving treatment on an inpatient detoxification unit. Interested participants were given a description of the study and provided written informed consent; this study was approved by the local institutional review board. The participants completed a 20-minute battery of self-report measures on a tablet computer. These measures captured several constructs of interest, including substance use and related variables. Measures included in the current study are listed below.
2.3. Measures
Participants self-reported demographic information including age, gender, race, education, employment, and marital status. Substance use history, including prior substance use disorder treatment, was measured by self-administered questionnaires. Information on psychiatric history was extracted from each participant’s medical records for the current episode of care following completion of the survey. Specifically, we extracted current psychiatric and substance use disorder diagnoses and lifetime history of suicidal and self-injurious behaviors. Participants also completed the self-report measures described below. Clinical variables of interest were selected based on the literature and availability of data sources: primary opioid used (heroin and/or fentanyl vs. prescription opioids only (Baldwin et al., 2018; Dai et al., 2019; Darke et al., 2015; Hakansson et al., 2008; Park et al., 2018), history of opioid injection (Bohnert et al., 2011; Hakansson et al., 2008), age at first opioid misuse (King and Chassin, 2007), number of prior detoxification treatments (Peterson et al., 2019), benzodiazepine misuse in the past 12 months (Bohnert et al., 2017; Darke, 1996; Hakansson et al., 2008; Jones and McAninch, 2015), co-occurring psychiatric disorders (Bohnert et al., 2017; Darke et al., 2004; Darke et al., 2015; Maloney et al., 2007), history of suicide attempt (Darke et al., 2004; Darke et al., 2007; Hakansson et al., 2008; Maloney et al., 2007; Pan et al., 2014), and chronic pain (Fudalej et al., 2015). In addition to variables that have been associated with overdose in prior studies, we added two additional variables that have been associated with suicide risk, current smoking status (Poorolajal and Darvishi, 2016) and anxiety sensitivity (Stanley et al., 2018).
The Opioid Overdose Questionnaire was developed for use in this study to assess thoughts, motivations, and behaviors associated with opioid overdose in participants seeking treatment for OUD. The measure included items assessing history of overdose (definition adapted from Wilder et al., 2016; defined as: “when a toxic amount of a drug or drugs overwhelms the body such that a person is no longer able to respond to others or breathe adequately, resulting in Narcan naloxone rescue and or emergency medical care. An overdose can occur with prescription or recreational drugs, or a combination of both, and can be deliberate or unintentional”) and number of prior overdoses and thoughts prior to the most recent overdose. Specifically, participants were asked two questions about beliefs concerning death prior to their most recent overdose: “Just before your most recent overdose, how likely did you think that you would overdose?” and “Just before your most recent overdose, how strongly did you want to die?”. Responses were scored from 0-10, with higher scores indicating greater likelihood of overdosing and greater desire to die.
The Opioid History Questionnaire was developed to track lifetime opioid use histories in participants seeking treatment for opioid use disorder, and captured characteristics such as primary opioid used (i.e., prescription opioids, heroin, and fentanyl) and age at first use. The measure was adapted from the Prescription Opiate Analgesic Use History Questionnaire (Weiss et al., 2011).
The Anxiety Sensitivity Index-3 (ASI-3) is an 18-item self-report measure assessing the fear of anxiety symptoms, such as racing thoughts and increased heart rate. Participants rate how much they agree with the statement from 0 (very little) to 4 (very much). The measure is scored on a total scale from 0 to 72 with higher scores indicating greater anxiety sensitivity (Taylor et al., 2007).
Chronic pain was assessed by two questions from the Brief Pain Inventory (Cleeland and Ryan, 1994). The first question asked about the presence of pain, not including every day pains such as headaches, sprains, and toothaches; for this study, we also directed participants to exclude pain associated with withdrawal. The second question assessed duration of pain. Chronic pain is defined as pain lasting longer than 3 months. This definition is consistent with the International Association for the Study of Pain (Merskey and Bogduk, 1994).
2.4. Data Analysis
First, we evaluated skewness and normality in our clinical variables of interest. We then compared those with and without a history of opioid overdose to examine differences in sociodemographic and clinical characteristics, conducting X2 tests for categorical variables and independent sample t-tests for continuous variables (a Mann-Whitney U test was conducted for one variable that demonstrated significant deviation from normality: number of prior detoxification treatments). We adjusted the significance level to account for multiple comparisons (Bonferroni-corrected p-value≤.003). Finally, we used descriptive statistics to characterize the frequency of desire to die and likelihood of overdose prior to an overdose, as well as patterns of opioid use and stressors that may have precipitated an overdose. Analyses were conducted in SPSS Version 20.
3. Results
Of the 120 participants seeking treatment for opioid use disorder, 45% (n=54) had overdosed at least once. Among those who had ever overdosed, the mean number of overdoses was 5.3 (SD=7.1, median = 3, 5 respondents reported > 13 overdoses, range=1 to 36). Of those who had overdosed, 37% reported that their most recent overdose occurred within the past month and 76% within the past year. Additionally, 28% of participants (n=14) reported that an event or stressor led to their most recent overdose. Ninety-one percent of participants (n=48) reported using opioids regularly or daily in the month before their overdose, and 9% (n=5) relapsed after a period of opioid abstinence.
3.1. Group Differences by Overdose History
Groups were compared on sociodemographic and clinical variables (Table 1). Based on the adjusted alpha controlling for multiple tests, participants who had overdosed were more likely to use heroin and/or fentanyl than prescription opioids only, to have a history of opioid injection, and to have had more lifetime detoxification treatments. The overdose group were also more likely to have a co-occurring psychiatric disorder and a history of a prior suicide attempt. Past overdose was not associated with the following sociodemographic variables: age, gender, race, education, marital status, or employment. Several clinical variables were not associated with past overdose: age at first opioid misuse, past-year benzodiazepine misuse, current smoking, chronic pain, and anxiety sensitivity score.
Table 1.
Sociodemographic and clinical variables by opioid overdose history.
| Overdose (n=54) |
No Overdose (n=66) |
χ2/t | p-value | |
|---|---|---|---|---|
| Sociodemographic variables | ||||
| Age (mean, SD) | 33.7 (9.1) | 35.1 (11.4) | 0.72 | .473 |
| Female, % | 40.7 | 40.9 | 0.00 | .985 |
| White race, % | 92.2 | 85.9 | 1.10 | .295 |
| ≥ Some college, % | 68.5 | 61.5 | 0.63 | .428 |
| Never married, % | 66.7 | 52.3 | 2.511 | .113 |
| Employed full-time, % | 27.8 | 43.9 | 3.341 | .068 |
| Clinical variables | ||||
| Primary opioid used (fentanyl and/or heroin), %a | 92.3 | 64.1 | 12.82 | .001 |
| History of opioid injection, % | 83.3 | 33.3 | 30.11 | .001 |
| Age first opioid misuse (mean, SD) | 20.6 (8.7) | 23.0 (8.4) | 1.54 | .126 |
| Prior detoxifications (median)b | 5 | 2 | 1037.50 | .001 |
| Past year benzodiazepine misuse, % | 63.0 | 48.5 | 2.52 | .113 |
| Current smoker, % | 83.3 | 76.6 | 0.83 | .363 |
| Psychiatric comorbidity, % | 72.2 | 50.0 | 6.11 | .013 |
| History of suicide attempt, % | 50.0 | 17.2 | 14.22 | .001 |
| Chronic pain, % | 28.3 | 38.1 | 1.15 | .284 |
| Anxiety sensitivity (mean, SD) | 29.7(17.7) | 27.5 (17.8) | −0.65 | .518 |
Reference category is prescription opioids only
For number of prior detoxifications, Mann-Whitney U test is reported.
3.2. Beliefs About Overdose: Likelihood of Overdose and Desire to Die
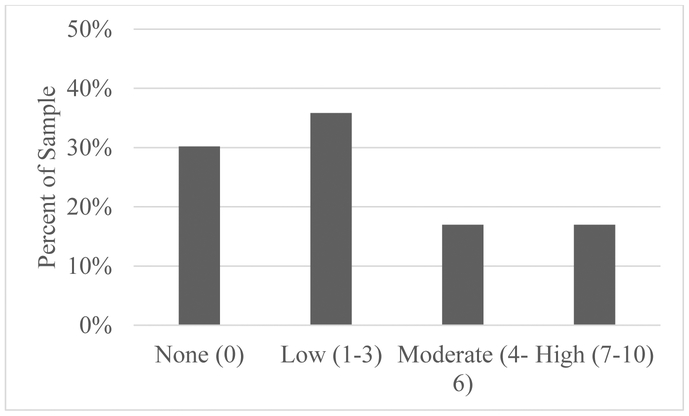
Self-reported beliefs about overdose likelihood and desire to die were examined. When rating beliefs about overdose likelihood prior to their most recent overdose (Figure 1), participants reported on average low-moderate perceptions for the likelihood that they would overdose (mean=3.1, SD=3.4, possible range=0-10). Most (68.8%) reported at least some possibility of overdose. Significant variability was reported in these ratings, with 30.2% of participants (n=16) reporting that they believed it was not at all likely they would overdose (0 out of 10) and 13.2% (n=7) answering that it was “extremely likely” (10 out of 10).
Figure 1.
Perceived likelihood of overdose prior to last overdose.
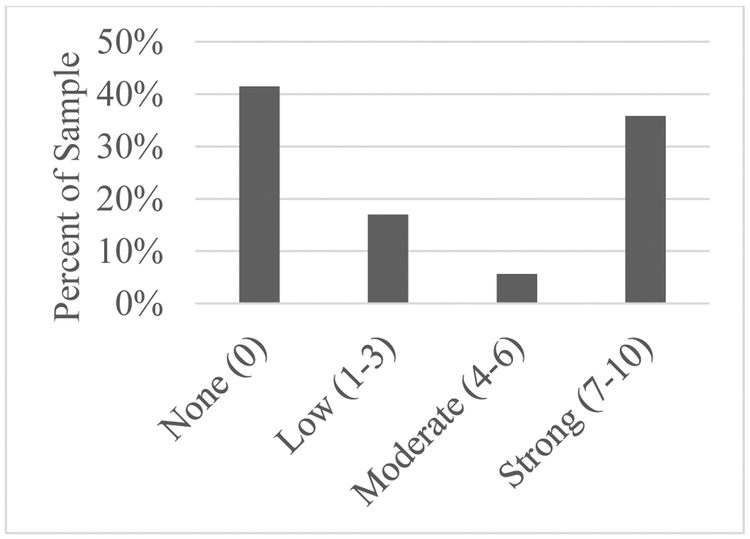
Participants reported how strongly they wanted to die before their most recent overdose (Figure 2). On average, participants reported a low-moderate rating (mean=3.8, SD=4.1, possible range=0-10) for their desire to die. This included 41.5% (n=22) of individuals’ reporting “I did not want to die” (score=0 out of 10) before their most recent overdose, whereas the remaining 58.5% (n=31) expressed at least some desire to die (score >0). More than one-third of the sample (35.8%, n=19) reported a strong desire to die before their most recent overdose (≥7 out of 10), and 20.8% (n=11) reported “I definitely wanted to die” (score=10 out of 10). Ratings of desire to die and perceived likelihood of overdose were moderately correlated (r=.51, p<.001). Even among the 11 participants who reported that they “definitely wanted to die,” 4 perceived their likelihood of overdose to be <2, 2 reported a moderate likelihood, and 5 reported 10 out of 10, with 2 in between. Ratings of perception of overdose risk and desire to die were not associated with time since last overdose (range: <1 month ago to >4 years ago; Pearson’s r=−.26 and −.16, p-values>.06, for likelihood of overdose and desire to die, respectively).
Figure 2.
Desire to die prior to last overdose.
4. Discussion
The results of this study suggest that a significant number of treatment-seeking patients with OUD experience suicidal motivation prior to nonfatal opioid overdose. In our sample, almost 60% of participants reported some suicidal motivation, and 36% reported a high level. Importantly, the full range of our continuous scale was represented, indicating that suicidal motivation likely falls along a continuum in this population. Affirming our hypothesis, a substantial portion of the sample (42%) definitively reported no desire to die (0/10), while the remaining 58% varied in their level of desire to die, with 21% reporting a definite desire to die.
Past studies have documented low rates of self-reported suicidal intention (i.e., acting for the purpose of killing oneself) with opioid overdose, e.g., 10% of intentional heroin overdoses (Darke and Ross, 2001). However, our data suggest that some degree of desire to die may be common prior to overdose. Although a higher desire to die was associated with a greater perceived likelihood of overdose, this was only a moderate correlation. Even among those with a strong desire to die, perceived likelihood of overdose varied. We did not assess intention to die; consideration of each of these dimensions is an important future direction for research.
Replicating past studies of OUD, on average, participants perceived the probability of an overdose to be low; this thought process has been termed overly “optimistic” (McGregor et al., 1998). The combination of low perceived overdose risk but some presence of desire to die may be particularly dangerous in facilitating potentially lethal opioid use behaviors (e.g., using alone, using more than usual, impulsively using from an unknown or unsafe supplier, and polydrug use) even in the absence of clear intention to die by suicide (c.f., (Bennett et al., 2017; Pouget et al., 2017)). Screening OUD patients on these two factors may inform the need for more in-depth screening and/or provision of preventive interventions to reduce overdose risk, particularly in an era in which the probability of lethal overdose is increased with the high availability of high-potency illicit fentanyl and its analogues.
Consistent with the literature, several variables consistent with more severe OUD were also associated with overdose history, including primary use of heroin and/or fentanyl, history of opioid injection, more previous detoxification treatment admissions, and history of suicide attempt. Clinicians treating patients with OUD should be particularly mindful of the overdose risk among patients with these characteristics.
Our study only included participants who had a history of nonfatal overdoses. Clinical correlates and beliefs about desire to die and overdose likelihood prior to a fatal overdose may differ. Rockett and colleagues have argued for changes to post-mortem data tracking and analysis to improve understanding of death due to drug overdose (Rockett et al., 2018a, 2018b). Prospective studies that consider these risk factors over time will be needed to improve understanding of the risks for fatal and nonfatal overdose.
We acknowledge several study limitations. First, our sample was relatively small, precluding analyses of correlates of suicidal cognitions (e.g., number of prior overdoses). Secondly, the only method for obtaining data on suicidal thoughts is through retrospective self-reporting, which is subject to recall bias. Thirdly, the population sample was predominantly white and the setting is a private psychiatric facility; both factors limit generalizability of the results. Nonetheless, our sample rates of opioid overdose and suicide attempt histories were consistent with larger studies of OUD conducted in multiple settings (Bogdanowicz et al., 2016; Darke et al., 2015; Dunn et al., 2016). Sample rates also aligned with results from a recent study by Morizio and colleagues (Morizio et al., 2017), who compared survivors of heroin overdose vs. prescription opioid overdose. They also found greater frequency of overdose and injection drug use among people using heroin, although they did not examine suicidal motivations prior to overdose. Replication studies are urgently needed, as some current projections indicate continued escalation through 2030 for suicide and drug poisoning mortality (Best et al., 2018). Novel, comprehensive prevention measures, including improved upstream approaches to self-injury mortality (Rockett et al., 2018a), need strong consideration. Future studies that consider temporality of the variables of interest, including psychiatric diagnoses, overdose and suicide would help to clarify the patterns among these variables. Finally, this study did not measure the potentially important variables regarding recovery network supports and the impact of “recovery social capital” on rates of opioid overdose, suicide attempts, and participant perceptions related to overdose risk and desire to die. Nor were we able to analyze structured assessment of adverse childhood events which have been associated with opioid overdose (Stein et al., 2017). Future studies including these variables are needed.
There are several important future directions in this line of research. First, expanded assessments that consider the complexity of suicidal thoughts and behaviors to include suicidal motivation (i.e., desire to die) and intention will improve understanding of how these dimensions may contribute to overdose. Second, prospective studies examining how suicidal motivation and intention are associated with future substance use behaviors and both fatal and non-fatal overdose will be essential to improving prediction of these events and to identifying potential preventive interventions. Finally, although our data are preliminary in nature, the frequency of desire to die in this population prior to an overdose highlights the importance of testing suicide prevention interventions in addition to standard of care (naloxone education and distribution, recommendations for medication-based treatment for opioid use disorder) in people with a history of opioid overdose.
These data support the hypothesis that suicidal motivation falls along a continuum, and augments the literature suggesting that the classification of a drug overdose as either “unintentional” or “intentional” may not always reflect accurately upon either the behavioral episode itself or the treatment interventions most appropriate for preventing drug-related mortality. Our findings suggest that suicidal motivations are present among a significant portion of patients surviving opioid overdose, and the need for prospective studies to investigate associations between suicidal thoughts, opioid use, and overdose events is important for improving prevention of opioid-related mortality.
Highlights.
Death rates due to opioid-related overdose continue to rise.
Opioid overdose and suicide attempts are common in those with opioid use disorder.
Desire to die before opioid overdose ranges continuously from “none” to “definite.”
Suicide prevention interventions may reduce opioid overdose and suicide attempts.
Acknowledgments
Role of Funding Source
Funding for effort on this project was provided by the following sources: NIDA grants K23 DA035297 (Dr. McHugh), R21 DA046521 (Dr. McHugh), UG1 DA15831 (Dr. Weiss), and K24 DA022288 (Dr. Weiss), and the Charles Engelhard Foundation (Dr. Weiss). NIDA had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Conflict of Interest
Roger Weiss consulted to GW Pharmaceuticals and Janssen Pharmaceuticals.
All other authors declare they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Albert M, McCaig LF, Uddin S, 2015. Emergency department visits for drug poisoning: United States, 2008-2011. NCHS Data. Brief 1–8. [PubMed] [Google Scholar]
- Baldwin N, Gray R, Goel A, Wood E, Buxton JA, Rieb LM, 2018. Fentanyl and heroin contained in seized illicit drugs and overdose-related deaths in British Columbia, Canada: An observational analysis. Drug Alcohol. Depend. 185, 322–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett AS, Elliott L, Golub A, Wolfson-Stofko B, Guarino H, 2017. Opioid-involved overdose among male Afghanistan/Iraq-Era U.S. military veterans: A multidimensional perspective. Subst. Use. Misuse 52, 1701–1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmans Y, Gordon E, Eynan R, 2017. Surviving moment to moment: The experience of living in a state of ambivalence for those with recurrent suicide attempts. Psychol. Psychother 90, 633–648. [DOI] [PubMed] [Google Scholar]
- Best AF, Haozous EA, Berrington de Gonzalez A, Chernyavskiy P, Freedman ND, Hartge P, Thomas D, Rosenberg PS, Shiels MS, 2018. Premature mortality projections in the USA through 2030: a modelling study. Lancet. Public. Health 3, e374–e384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogdanowicz KM, Stewart R, Chang CK, Downs J, Khondoker M, Shetty H, Strang J, Hayes RD, 2016. Identifying mortality risks in patients with opioid use disorder using brief screening assessment: Secondary mental health clinical records analysis. Drug. Alcohol. Depend 164, 82–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert AS, Roeder KM, Ilgen MA, 2011. Suicide attempts and overdoses among adults entering addictions treatment: comparing correlates in a U.S. National Study. Drug. Alcohol. Depend 119, 106–112. [DOI] [PubMed] [Google Scholar]
- Bohnert ASB, Ilgen MA, 2019. Understanding Links among Opioid Use, Overdose, and Suicide. N. Engl. J. Med 380, 71–79. [DOI] [PubMed] [Google Scholar]
- Bohnert ASB, Walton MA, Cunningham RM, Ilgen MA, Barry K, Chermack ST, Blow FC, 2018. Overdose and adverse drug event experiences among adult patients in the emergency department. Addict. Behav 86, 66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert KM, Ilgen MA, Louzon S, McCarthy JF, Katz IR, 2017. Substance use disorders and the risk of suicide mortality among men and women in the US Veterans Health Administration. Addiction. 112, 1193–1201. [DOI] [PubMed] [Google Scholar]
- Braden JB, Edlund MJ, Sullivan MD, 2017. Suicide Deaths With Opioid Poisoning in the United States: 1999-2014. Am. J. Public. Health 107, 421–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradvik L, Berglund M, Frank A, Lindgren A, Lowenhielm P, 2009. Number of addictive substances used related to increased risk of unnatural death: a combined medico-legal and case-record study. BMC. Psychiatry 9, 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, Deaton A, 2017. Mortality and morbidity in the 21(st) century. Brookings. Pap. Econ. Act 2017, 397–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleeland CS, Ryan KM, 1994. Pain assessment: Global use of the Brief Pain Inventory. Ann. Acad. Med. Singapore 23, 129–138. [PubMed] [Google Scholar]
- Conner KR, Britton PC, Sworts LM, Joiner TE Jr., 2007. Suicide attempts among individuals with opiate dependence: the critical role of belonging. Addict Behav 32, 1395–1404. [DOI] [PubMed] [Google Scholar]
- Conner KR, Wiegand TJ, Kaukeinen K, Rachel G, Schult R, Heavey SC, 2018. Prescription-, illicit-, and self-harm opioid overdose cases treated in hospital. J. Stud. Alcohol. Drugs. 79, 893–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Walton MA, Carter PM, 2018. The major causes of death in children and adolescents in the United States. N. Engl. J. Med 379, 2468–2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai Z, Abate MA, Smith GS, Kraner JC, Mock AR, 2019. Fentanyl and fentanyl-analog involvement in drug-related deaths. Drug Alcohol Depend 196, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke, 1996. Fatal heroin 'overdose': a review. Addiction. 91, 1765–1772. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, 2001. The relationship between suicide and heroin overdose among methadone maintenance patients in Sydney, Australia. Addiction. 96, 1443–1453. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Lynskey M, Teesson M, 2004. Attempted suicide among entrants to three treatment modalities for heroin dependence in the Australian Treatment Outcome Study (ATOS): prevalence and risk factors. Drug. Alcohol. Depend 73, 1–10. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Marel C, Mills KL, Slade T, Burns L, Teesson M, 2015. Patterns and correlates of attempted suicide amongst heroin users: 11-year follow-up of the Australian treatment outcome study cohort. Psychiatry. Res 227, 166–170. [DOI] [PubMed] [Google Scholar]
- Darke S, Ross J, Williamson A, Mills KL, Havard A, Teesson M, 2007. Patterns and correlates of attempted suicide by heroin users over a 3-year period: Findings from the Australian treatment outcome study. Drug. Alcohol. Depend 87, 146–152. [DOI] [PubMed] [Google Scholar]
- Dasgupta N, Beletsky L, Ciccarone D, 2018. Opioid crisis: No easy fix to its social and economic determinants. Am. J. Public. Health 108, 182–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Do MT, Chang VC, Tibebu S, Thompson W, Ugnat AM, 2018. Sentinel surveillance of suspected opioid-related poisonings and injuries: trends and context derived from the electronic Canadian Hospitals Injury Reporting and Prevention Program, March 2011 to June 2017. Health. Promot. Chronic. Dis. Prev. Can 38, 317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn KE, Barrett FS, Yepez-Laubach C, Meyer AC, Hruska BJ, Petrush K, Berman S, Sigmon SC, Fingerhood M, Bigelow GE, 2016. Opioid overdose experience, risk behaviors, and knowledge in drug users from a rural versus an urban setting. J. Subst. Abuse. Treat 71, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fudalej S, Ilgen M, Kolodziejczyk I, Podgorska A, Serafin P, Barry K, Wojnar M, Blow FC, Bohnert A, 2015. Somatic Comorbidity and Other Factors Related to Suicide Attempt Among Polish Methadone Maintenance Patients. J. Addict. Med 9, 433–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakansson A, Schlyter F, Berglund M, 2008. Factors associated with history of non-fatal overdose among opioid users in the Swedish criminal justice system. Drug. Alcohol. Depend 94, 48–55. [DOI] [PubMed] [Google Scholar]
- Heale P, Dietze P, Fry C, 2003. Intentional overdose among heroin overdose survivors. J. Urban. Health 80, 230–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, McAninch JK, 2015. Emergency department visits and overdose deaths from combined use of opioids and benzodiazepines. Am. J. Prev. Med 49, 493–501. [DOI] [PubMed] [Google Scholar]
- Jones CW, Christman Z, Smith CM, Safferman MR, Salzman M, Baston K, Haroz R, 2018. Comparison between buprenorphine provider availability and opioid deaths among US counties. J. Subst. Abuse. Treat 93, 19–25. [DOI] [PubMed] [Google Scholar]
- Jonsson AK, Holmgren P, Druid H, Ahlner J, 2007. Cause of death and drug use pattern in deceased drug addicts in Sweden, 2002-2003. Forensic. Sci. Int 169, 101–107. [DOI] [PubMed] [Google Scholar]
- King KM, Chassin L, 2007. A prospective study of the effects of age of initiation of alcohol and drug use on young adult substance dependence. J. Stud. Alcohol Drugs 68, 256–265. [DOI] [PubMed] [Google Scholar]
- Maloney E, Degenhardt L, Darke S, Mattick RP, Nelson E, 2007. Suicidal behaviour and associated risk factors among opioid-dependent individuals: a case-control study. Addiction. 102, 1933–1941. [DOI] [PubMed] [Google Scholar]
- Maloney E, Degenhardt L, Darke S, Nelson EC, 2009. Are non-fatal opioid overdoses misclassified suicide attempts? Comparing the associated correlates. Addict. Behav 34, 723–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGregor C, Darke S, Ali R, Christie P, 1998. Experience of non-fatal overdose among heroin users in Adelaide, Australia: circumstances and risk perceptions. Addiction. 93, 701–711. [DOI] [PubMed] [Google Scholar]
- Merskey H, Bogduk N (Eds.), 1994. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms International Association for the Study of Pain, Task Force on Taxonomy, second ed. IASP Press, Seattle. [Google Scholar]
- Morizio KM, Baum RA, Dugan A, Martin JE, Bailey AM, 2017. Characterization and management of patients with heroin versus nonheroin opioid overdoses: Experience at an Academic Medical Center. Pharmacotherapy. 37, 781–790. [DOI] [PubMed] [Google Scholar]
- Neale J, 2000. Suicidal intent in non-fatal illicit drug overdose. Addiction 95, 85–93. [DOI] [PubMed] [Google Scholar]
- Olfson M, Crystal S, Wall M, Wang S, Liu SM, Blanco C, 2018a. Causes of death after nonfatal opioid overdose. JAMA. Psychiatry 75, 820–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M, Wall M, Wang S, Crystal S, Blanco C, 2018b. Risks of fatal opioid overdose during the first year following nonfatal overdose. Drug. Alcohol. Depend 190, 112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Volkow ND, 2018. Suicide: A Silent Contributor to Opioid-Overdose Deaths. N. Engl. J. Med 378, 1567–1569. [DOI] [PubMed] [Google Scholar]
- Pan CH, Jhong JR, Tsai SY, Lin SK, Chen CC, Kuo CJ, 2014. Excessive suicide mortality and risk factors for suicide among patients with heroin dependence. Drug. Alcohol. Depend 145, 224–230. [DOI] [PubMed] [Google Scholar]
- Park JN, Weir BW, Allen ST, Chaulk P, Sherman SG, 2018. Fentanyl-contaminated drugs and non-fatal overdose among people who inject drugs in Baltimore, MD. Harm Reduct. J 15, 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C, Liu Y, Xu L, Nataraj N, Zhang K, Mikosz CA, 2019. U.S. National 90-Day Readmissions After Opioid Overdose Discharge. Am. J. Prev. Med 56, 875–881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poorolajal J, Darvishi N, 2016. Smoking and Suicide: A Meta-Analysis. PLoS One. 11(7):e0156348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouget ER, Bennett AS, Elliott L, Wolfson-Stofko B, Almenana R, Britton PC, Rosenblum A, 2017. Development of an opioid-related Overdose Risk Behavior Scale (ORBS). Subst. Abus 38, 239–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SJ, Iskric A, Calati R, Courtet P, 2017. Psychological and physical pain as predictors of suicide risk: evidence from clinical and neuroimaging findings. Curr. Opin. Psychiatry 30, 159–167. [DOI] [PubMed] [Google Scholar]
- Rockett IRH, Caine ED, Connery HS, Greenfield SF, 2018a. Mortality in the United States from self-injury surpasses diabetes: a prevention imperative. Inj. Prev 25, 331–333. [DOI] [PubMed] [Google Scholar]
- Rockett IRH, Caine ED, Stack S, Connery HS, Nolte KB, Lilly CL, Miller TR, Nelson LS, Putnam SL, Nestadt PS, Jia H, 2018b. Method overtness, forensic autopsy, and the evidentiary suicide note: A multilevel National Violent Death Reporting System analysis. PLoS One.13(5), e0197805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley IH, Boffa JW, Rogers ML, Hom MA, Albanese BJ, Chu C, Capron DW, Schmidt NB, Joiner TE, 2018. Anxiety sensitivity and suicidal ideation/suicide risk: A meta-analysis. J Consult. Clin. Psychol 86(11):946–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Conti MT, Kenney S, Anderson BJ, Flori JN, Risi MM, Bailey GL, 2017. Adverse childhood experience effects on opioid use initiation, injection drug use, and overdose among persons with opioid use disorder. Drug and Alcohol Dependence, 179, 325–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Abramowitz JS, Holaway RM, Sandin B, Stewart SH, Coles M, Eng W, Daly ES, Arrindell WA, Bouvard M, Cardenas SJ, 2007. Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychol. Assess 19, 176–188. [DOI] [PubMed] [Google Scholar]
- Tollefsen IM, Thiblin I, Helweg-Larsen K, Hem E, Kastrup M, Nyberg U, Rogde S, Zahl PH, Ostevold G, Ekeberg O, 2016. Accidents and undetermined deaths: re-evaluation of nationwide samples from the Scandinavian countries. BMC. Public. Health 16, 449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trout ZM, Hernandez EM, Kleiman EM, Liu RT, 2017. Prospective prediction of first lifetime suicide attempts in a multi-site study of substance users. J. Psychiatr. Res 84, 35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanHouten JP, Rudd RA, Ballesteros MF, Mack KA, 2019. Drug Overdose Deaths Among Women Aged 30-64 Years - United States, 1999-2017. MMWR. Morb. Mortal. Wkly. Rep 68, 1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RD, Potter JS, Fiellin DA, Byrne M, Connery HS, Dickinson W, Gardin J, Griffin ML, Gourevitch MN, Haller DL, Hasson AL, Huang Z, Jacobs P, Kosinski AS, Lindblad R, McCance-Katz EF, Provost SE, Selzer J, Somoza EC, Sonne SC, Ling W, 2011. Adjunctive counseling during brief and extended buprenorphine-naloxone treatment for prescription opioid dependence: a 2-phase randomized controlled trial. Arch. Gen. Psychiatry 68, 1238–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West NA, Severtson SG, Green JL, Dart RC, 2015. Trends in abuse and misuse of prescription opioids among older adults. Drug. Alcohol. Depend 149, 117–121. [DOI] [PubMed] [Google Scholar]
- Wilder CM, Miller SC, Tiffany E, Winhusen T, Winstanley EL, Stein MD, 2016. Risk factors for opioid overdose and awareness of overdose risk among veterans prescribed chronic opioids for addiction or pain. Journal of addictive diseases, 35(1), 42–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yarborough BJ, Stumbo SP, Janoff SL, Yarborough MT, McCarty D, Chilcoat HD, Coplan PM, Green CA, 2016. Understanding opioid overdose characteristics involving prescription and illicit opioids: A mixed methods analysis. Drug. Alcohol. Depend 167, 49–56. [DOI] [PubMed] [Google Scholar]
- Zosel A, Bartelson BB, Bailey E, Lowenstein S, Dart R, 2013. Characterization of adolescent prescription drug abuse and misuse using the Researched Abuse Diversion and Addiction-related Surveillance (RADARS((R))) System. J. Am. Acad. Child. Adolesc. Psychiatry 52, 196–204.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]