ABSTRACT
Missed opportunities for vaccination (MOV) is a poor reflection of the quality of care for children attending health facilities. It also contributes to a reduction in overall immunization coverage. Although there is a growing interest in the use of quality improvement (QI) in complex health systems to improve health outcomes, the degree to which this approach has been used to address MOV is poorly understood. We conducted a scoping review using Arksey and O’Malley’s framework to investigate the extent to which QI has been used in health facilities to reduce MOV. The review followed five stages as follows: (1) identifying the research question; (2) identifying the relevant studies; (3) selecting the studies; (4) charting data; and (5) collating, summarizing, and reporting results. The search strategy included electronic databases and gray literature. A total of 12 literatures on QI projects focused on addressing MOV were identified. Eleven were published manuscripts, and one was a conference presentation. All the QI projects published were conducted in the United States and majority were between 2014 and 2018. In these projects, 45 change ideas targeting providers, clients, and health system were used. This study generated important evidence on the use of QI in health facilities to reduce MOV. In addition, the result suggests that there is a growing interest in the use of this approach to address MOV in recent years. However, no literature was found in low- and middle-income countries especially sub-Saharan Africa.
KEYWORDS: Missed opportunities for vaccination, immunization, vaccination, quality improvement, scoping review, quality of care, implementation science
Introduction
Immunization is one of the most effective and cost-effective public health interventions for preventing morbidity and mortality from common childhood infectious diseases.1−3 In addition to averting deaths, immunization also improves long-term productivity and has positive ecological externalities.4 As a result childhood immunization is considered a priority child health service in health facilities.5 Despite this, many children who are eligible for vaccination often make contact with health services and are still missed by the immunization sub-system thus resulting in missed opportunities for vaccination (MOV).6 This MOV can occur during health care visits for curative or preventive services.6,7 Its prevalence in low- and middle-income (LMIC) countries is estimated to be 32.2%.6 A recent review on MOV among African children from 14 countries found a pooled prevalence of 27.26%.8 In the same study, the complexity of MOV was highlighted.8 Using complex adaptive systems lens, it was shown that interrelated and interdependent factors which originate from multiple stakeholders including caregivers, health workers as well as health systems managers are responsible for MOV.8 According to the World Health Organization, MOV contributes to a further reduction in childhood immunization coverage level at district and national level.9 Its impact on this important public health indicator has reinvigorate WHO’s interest in address it across health systems.9
Quality improvement (QI), which originated from industrial manufacturing, has emerged as one of the main approaches for improving health outcomes within complex health systems.10-13 This is because QI methodologies enable the use of multicomponent interventions concurrently to institute change at multiple levels and allows experiential learning.12,14,15 Within the context of immunization programs, QI would differ from general implementation activities designed to improve uptake of immunization. This is because QI process would involve specific activities like baseline data collection, testing iterative cycles of intervention packages to improve immunization uptake, brainstorming on progress, and periodic reflections on the change packages supported by continuous data collection on the outcome of interest which can then be used to inform modifications. Several QI models exist; however, the most commonly used are Model for Improvement (MFI), lean, and six sigma.16-20 MFI is a hybrid of two frameworks: total quality management (TQM) and rapid cycle improvement (RCI).21 It uses plan-do-study-act (PDSA) cycles to test change ideas.21 Lean and six sigma are somewhat similar; however, lean is concerned with reducing wastage, while six sigma focuses on reducing process variation.22 Lean six sigma is an integration of the two models which focuses on defect prevention and is usually used when wastage and process variation coexists.23
At core, QI entails process change with resultant variation in outcomes.10,11 It has been used in health facilities in high-income countries to improve neonatal and child health outcomes.24-26 Similarly, there is also evidence of its use to strengthen health systems in LMIC.27 Studies conducted in Rwanda, Ghana, and Nigeria have demonstrated the impact of QI on maternal health outcomes.28-30 However, there is scarcity of information on how QI has been applied within the immunization system to reduce MOV.
Therefore, in this study, we explored the extent to which QI has been used to address MOV using a scoping review methodology.31 We adopted Arksey and O’Malley’s framework for conducting scoping review.31 The review followed five stages as follows:1 identifying the research question2; identifying the relevant studies3; selecting the studies4; charting data; and5 collating, summarizing, and reporting results.31 For this study, we defined a scoping review as a research synthesis technique for mapping literature on a particular field of study or topic to identify key concepts and gaps so as to inform further research, as well as policy and practice.32
We chose to use a scoping review method as we intend to explore the degree to which QI has been applied in health-care setting to reduce MOV, rather than sum up available evidence on the effect of QI on MOV.33 This review methodology is as transparent as a systematic review as it employs rigorous approaches to identify literature that are relevant to a research question.33 It is suitable for broad questions that would likely combine diverse literature.33 Using a scoping review will enable us to identify different types of change ideas for reducing MOV that have been used to broadly target stakeholders such as caregivers, health workers and health systems.33 Our study filled existing knowledge gap by presenting a broad descriptive overview of the application of QI in health-care setting to reduce MOV. This study is relevant for researchers as it highlighted the nature and characteristics of available literature on the topic. It is also relevant for health practitioners and policy makers that are planning to use QI approach within their setting to address this problem. This scoping review was conducted before embarking on a QI project in primary health-care facilities in a resource constrained setting.
The objectives of this study were as follows:
To map and describe existing literature on QI projects to reduce MOV within the context of routine childhood immunization.
To identify the QI models, change ideas, and study designs used in QI projects to reduce MOV within the context of routine childhood immunization.
Results
A total of 12 publications met the eligibility criteria for this review. The total number of publications that were assessed for eligibility is 19, and 7 were excluded as shown in Figure 1. In two of the excluded studies, the focus was on general pediatric care.34,35 Others focused on immunization coverage.36-40 The electronic databases search yielded nine publications. Manual search of the reference list of eligible publication yielded an additional two publications. While the gray literature search yielded one conference presentation. No publication was obtained from the organizations that were contacted.
Figure 1.
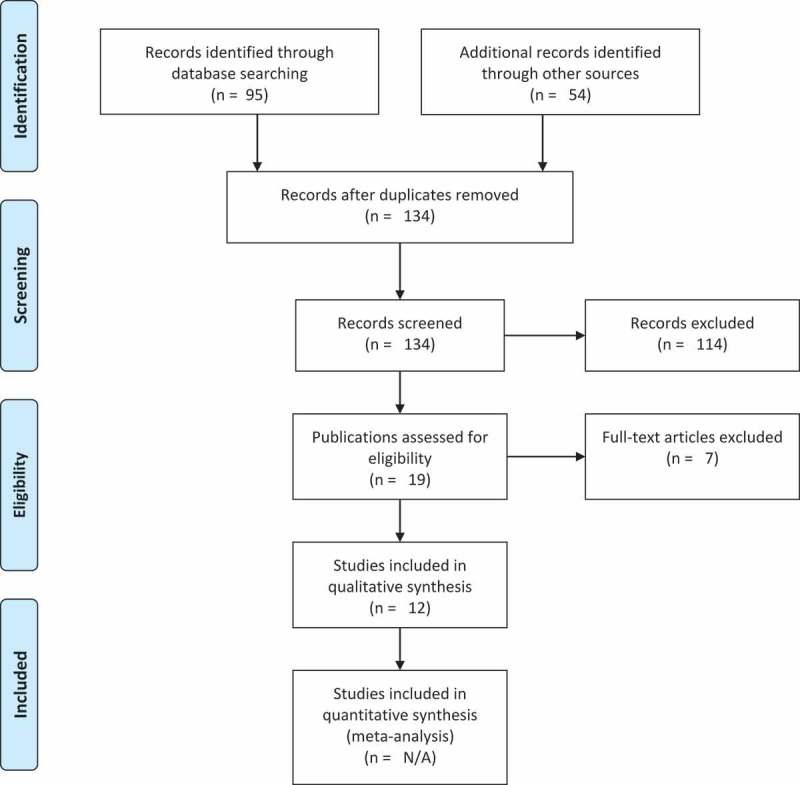
Adapted PRISMA flow chart.
Description of the characteristics of included publications
The country affiliation of all the first authors included in this review was the United States of America (USA). Their type of institutional affiliation varies with 50% affiliated with a university. Majority of included literature were published in the last 5 y (2014–2018). Other bibliometric characteristics of the publications are shown on Table 1.
Table 1.
General features of publications on use of quality improvement to address missed opportunities for childhood vaccination.
| Characteristics | Frequency | Percentage |
|---|---|---|
| Year of publication | ||
| 1999–2003 | 2 | 16.67 |
| 2004–2008 | 1 | 8.33 |
| 2009–2013 | 0 | |
| 2014–2018 | 9 | 75.00 |
| Country affiliation | ||
| United States of America | 12 | 100 |
| Others | 0 | |
| Publication type | ||
| Published literature | 11 | 91.67 |
| Conference proceedings | 1 | 8.33 |
| Type of institutional affiliation of first author | ||
| University | 5 | 41.67 |
| Hospital | 4 | 33.33 |
| Government agency | 3 | 25.00 |
QI interventions
Most of the QI projects that were conducted covered routine childhood immunization, while four focused solely on human papillomavirus (HPV) vaccine. In one of the projects, the age group of the target population for HPV vaccine extended till 26 y. This extension to 26 y of age is a function of United States recommendations for catch-up immunization for women who did not receive HPV vaccine as adolescents. In one of the projects, a QI intervention was instituted in a primary care clinic in Denver to reduce MOV among children up to 25 months of age.41 This clinic is in an inner-city teaching hospital that serves low-income families.41 Three difference change ideas chart prompts, provider education, and provider reminders were implemented.41 The change ideas targeted nurses and clinicians.41 Details of each literature with the vaccines and target population are presented on Table 2. Although all the QI projects were implemented within a health facility the level of health care vary across studies.41-51 The context within which these QI projects were implemented also varies from one another.41-51 One of the QI practices was implemented within a health center in an urban public university.42 In another study, the QI practice was implemented in a clinic that serves mainly low-income families.41
Table 2.
Target population and vaccine(s) targeted in quality improvement practices to address missed opportunities for vaccination.
| Authors | Study title | Target population | Vaccine(s) |
|---|---|---|---|
| Published literature | |||
| Daley, M. F., et al. | Quality improvement in immunization delivery following an unsuccessful immunization recall41 | Children aged 3–35 months | All routine immunization |
| Daly, K. L., et al. | A University Health Initiative to Increase Human Papillomavirus Vaccination Rates42 | Young adults aged 18–26 y | Human papillomavirus (HPV) vaccine |
| Fiks, A. G., et al. | Improving HPV Vaccination Rates Using Maintenance-of-Certification Requirements43 | Adolescents aged 11–17 y | Human papillomavirus (HPV) vaccine |
| Jones, K. B., et al. | Improving Immunizations in Children: A Clinical Break-even Analysis44 | Children aged 3 y and below | All routine immunization |
| Krantz, L., et al. | Increasing HPV Vaccination Coverage Through Provider-Based Interventions45 | Adolescents aged 13–17 y | Human papillomavirus (HPV) vaccine |
| Moore, K. L., et al. | Tennessee‘s 3-Star Report: Using Available Data Systems to Reduce Missed Opportunities to Vaccinate Preteens46 | Adolescents aged 11–13 y | Tetanus-diphtheria-pertussis vaccine (Tdap), Quadrivalent meningococcal vaccine (Men-ACWY), and Human papillomavirus (HPV) vaccine |
| Rand, C. M., et al. | A Learning Collaborative Model to Improve Human Papillomavirus Vaccination Rates in Primary Care47 | Adolescents aged 11–17 y | Human papillomavirus (HPV) vaccine |
| Jones, K. B., et al. | Improving pediatric immunization rates: description of a resident-led clinical continuous quality improvement project48 | Children aged 3 y and below | All routine immunization |
| Sinn, J. S., et al. | Improving immunization rates in private pediatric practices through physician leadership49 | Children aged 9–30 months | All routine immunization |
| Melinkovich, P., et al. | Improving pediatric immunization rates in a safety-net delivery system50 | Children aged 3 y and below | All routine immunization |
| Carlin, E., et al. | Using Continuous Quality Improvement Tools to Improve Pediatric Immunization Rates51 | Children aged 2 y and below | All routine immunization |
| Conference presentation | |||
| Gurov, Heidi | Assessment-Feedback-Incentive-Exchange (AFIX) Overview(73) | Children below 35 months of age, and adolescents aged 13–17 y | All routine immunization |
In all the QI projects conducted, QI teams implemented multiple change ideas (interventions) targeting various levels of stakeholders.41-51 The change ideas were about evenly divided between provider- and patient-focused strategies with few cross-cutting strategies. In Table 3, all the compiled change ideas are classified according to their level of influence.
Table 3.
Classification of quality improvement interventions (change ideas) used in quality improvement projects to address missed opportunities for vaccination.
| Interventions for providers | Interventions for clients | Cross-cutting interventions |
|---|---|---|
| Place registry-generated copy of child’s immunization data on front of chart at every visit41 | Providing a strong recommendation for vaccination at every visit42 | Improve record keeping by keeping immunization history current49 |
| Make notation on clinician encounter form whenever child is due to visit41 | Using patient reminder systems42 | Record keeping51 |
| Educate providers regarding methods for reducing missed opportunities41 | Implementing campus-based marketing strategies42 | Developing an immunization registry to track patients50 |
| Place reminder posters prominently in clinic41 | Use of consistent language to recommend HPV vaccine43 | |
| Prevent missed opportunities to vaccinate by increasing provider acknowledgement of vaccine history42 | Provider emphasizing the vaccine as a tool for cancer prevention43 | |
| Distributing immunization records for all scheduled pediatric patients to provider medical-assistants teamlets44 | Provider emphasizing the vaccines at acute visits43 | |
| Educational seminar on HPV for physicians, residents, nurses, and medical assistants45 | Mailing letters to caregivers of children under 3 years of age providing information on reasons for immunization and encourage them to make appointment to obtain missing immunizations44 | |
| Weekly individualized audit to providers who missed an opportunity to vaccinate a patient against HPV45 | Administering all recommended vaccines at the same visit46 | |
| Allowing staffs to schedule their HPV visits45 | Making strong recommendations for vaccines46 | |
| Support staffs indicating to providers when client is HPV vaccine eligible45 | Discussing the need for immunizations with caregivers at that day’s visit48 | |
| “Best practice alert” for HPV in EMR45 | Use all clinical encounter to screening at every visit49 | |
| Electronic reminders using Huddle45 | Administer immunization at some sick visits49 | |
| Auditing and feedback46 | Administer immunization at any opportunity49 | |
| Providers were trained on offering a strong recommendation for HPV vaccination47 | Using only true contraindication to immunization49 | |
| Practices implemented provider prompts and/or standing orders and/or reminder/recall if desired47 | Simultaneous administration of multiple vaccines49 | |
| Provide monthly feedback on missed opportunities for vaccination to assess their progress47 | Administering DTP at 12 or 15 months instead of 18 months49 | |
| Teach residents about the principles of FOCUS-PDSA through didactic lecture48 | Recommendations pertained to missed opportunities51 | |
| Printing daily report with the immunization record for that day’s pediatric patients48 | Encourage parents to bring immunization record to all clinic visits49 | |
| Algorithms for catch-up of patients not on schedule or with incomplete immunizations51 | Educating parents even when refusal occur73 | |
| Conducting regular assessment of immunization levels with provision of clinic-specific feedback50 | ||
| Holding team-based quality improvement meetings50 | ||
| Use of standing orders on immunization in clinics73 | ||
| Training of health care providers73 |
HPV: human papilloma virus; EMR: Electronic Medical Record; FOCUS-PDSA: Find Organize Clarify Understand Select–Plan Do Study Act.
QI models, methods, and study designs
In three of the reviewed publications, continuous quality improvement (CQI) model was used.44,48,49 Only one publication reported the use of collaborative QI model.47 The use of PDSA as the method for QI was reported in four studies.43,44,47,48 In all the publications QI practice was implemented by QI teams.41-51 In the QI projects identified, quasi experimental designs like pre-post design, before and after studies, and time series designs were used to evaluate the effect of the interventions.41,44-49
Discussion
Summary of results
We embarked on this scoping review to explore the extent to which QI has been used to address MOV within the context of routine childhood immunization. Our objective was to map and describe existing literature, and identify the QI models, change ideas, and study designs used in QI projects. Our search for published and gray literature yielded 12 publications (11 published literature, and 1 conference presentation). Based on the charted information from these publications, we found that all the QI projects were implemented in the United States and majority of them were conducted between 2014 and 2018. In the QI projects implemented, multicomponent change ideas were used. We identified 45 change ideas across all the projects and classified them into three namely interventions for providers, interventions for clients, and cross-cutting interventions. It was beyond the ambit of this scoping review to conduct an evaluation of the methodological quality of individual studies included.
Strengths and limitations of the study
A key strength of this review is that we employed a rigorous and transparent search strategy to identify existing literature on the use of QI to address MOV. In addition, we did not restrict our search to any language, date of publication or document type. Some limitations of this review should also be considered. Despite the comprehensiveness of our search strategy, we cannot conclude that we found all the publications due to the broad nature of QI as a field of practice. It is still possible that we missed some papers. We were also unable to obtain publications and reports from organizations engaged in QI projects for immunization, as such, it is possible that other non-public literature exist that have not been included in this review.
QI and MOV
Our study confirms the emerging interest in QI as majority of identified literature were published between 2014 and 2018. As practitioners increasingly understand and begin to view MOV from the complexity lens, a further rise in the use of QI to address it might occur. However, the overall volume of QI projects to address MOV, which is a health-care quality issue with substantial population health implications, was low. Furthermore, all the identified publications were for projects conducted in the United States. Although global organizations such as the WHO recognize the role of QI in health systems, its use in immunization systems in LMIC to reduce MOV seems low.52 Many factors including paucity of skills to conduct and report QI interventions or failure to publish QI projects might be contributing to this.
Authors of the publications included in this review reported the use of multiple change ideas which is consistent with the science of improvement.10 While some of these change ideas are targeted at providers, others focus on clients and the system, thus enabling a multipronged approach. However, the process of selection of these change ideas were rarely described enough to enable replication in other settings. In a resident-led clinical QI project to improve immunization rate, third year residents engage immunization stakeholders to implement a set of activities.48 These activities include printing daily immunization reports, distributing them to health-care providers and discussion about immunization with parents and guardians.48 However, it is unclear how the residents arrived at these choice of change ideas.48
Most of the QI projects reviewed reported only the QI outcome measure and this practice is inconsistent with current guidance on QI in health care.53 It is essential to include and report on process and balancing measures as well.53 Process measures will enable QI practitioners to track whether the system is performing as planned.53 While balancing measure will allow tracking of the influence of the QI project on other parts of the system.53 Balancing measures are particularly important as it will provide information on whether the change ideas causing improvement in one unit, is decreasing a desirable outcome in others. In addition to these measures, more recent improvement models have also included implementation outcomes.54
Due to the “real world” context within which QI are implemented, quasi experimental designs are sometimes more feasible.55 As expected, most of the publications reported the use of these study designs. However, it is important to consider additional design features to these quasi-experimental designs or conduct pragmatic or hybrid trials to improve confidence in the effect measure attributed to QI interventions.56-59
Implications for research
In view of our findings, we recommend more research. Our research recommendations, which follow the EPICOT+ format, are presented in Box 1.60
Box 1.
Use of EPICOT+ to highlight research recommendations based on gaps identified in a scoping review on the use of quality improvement to address missed opportunities for vaccination.
| Element | Recommendation(s) |
| Core elements | |
| Evidence (State of evidence) | Existing quality improvement projects for addressing missed opportunities for vaccination among children were conducted in the United States. |
| Population (Population of interest) | Quality improvement projects addressing missed opportunities for vaccination targeting;
|
| Interventions |
|
| Comparisons outcomes | Control (non-intervention) health facilities |
|
|
| Time stamp | July 2018 |
| Optional element | |
| Study type | Quasi experimental design (Interrupted time series design with non-equivalent control groups), pragmatic trials and implementation-effectiveness hybrid trials. |
We recommend the use of standardized guidance such as Standards for QUality Improvement Reporting Excellence – SQUIRE 2.0 to report future studies.61 This would greatly enhance the sharing of best practices. Also, researcher and practitioners can place related gray literature on repositories that are accessible to wide range of audience.
Methodology
A review team was established comprising of the principal investigator and three supervisors with expertise in research synthesis, epidemiology, and vaccinology.62 The team deliberated upon and agreed on the broad research question to be addressed as well as the review protocol.
Stage 1: identify the research question
The scoping review question was, “What is the nature and extent of use of QI approaches in health facilities to reduce missed opportunities for vaccination within the context of routine childhood immunization?” Due to the broad nature of this review question, with its main focus on mapping existing literature, a systematic review would not be appropriate.63 Since emerging consensus on knowledge synthesis methodologies have made clearer the applicability of a broad range of other methods, we used this to inform our choice of scoping review methodology to answer this question.64,65
Since routine childhood immunization for children extend to those in the adolescent age group, they were included as part of the population of interest.66 The detailed population intervention comparator and outcome (PICO) elements for the review question are shown in Box 2.
Box 2.
PICO elements for scoping review question.
| Population | Children and adolescents |
| Intervention | Quality improvement |
| Comparator | Usual practice |
| Outcome | Proportion, frequency or percentage of missed opportunities for vaccination |
| Study setting | Health facilities |
For this study, we adopted the Cochrane Effectiveness Practice and Organization of Care (EPOC) group’s definition of QI as “an iterative process to review and improve care that includes the involvement of health-care teams, analysis of a process or system, a structured process improvement method or problem-solving approach, and use of data analysis to assess change”.67 Since our interest is in routine childhood immunization, the following antigens were considered: Bacillus Calmette-Guerin (BCG), hepatitis B, Polio, Diphtheria-Tetanus-Pertussis containing vaccine, Haemophillus influenzae type b, pneumococcal (conjugate), rotavirus, measles, rubella, and HPV.66 Other antigens such as yellow fever, Japanese encephalitis, tick-borne encephalitis, typhoid, cholera, meningococcal, hepatitis A, rabies, dengue, mumps, seasonal influenza, and varicella that are indicated for children under certain conditions like place of residence, type of population, and immunization program were also considered.66
Stage 2: identifying relevant studies
To identify literature (published and unpublished) appropriate for answering the research question, we employed a search strategy involving:
Three3 electronic databases and manual search of reference lists of relevant studies
Google search
Contacting networks and organizations involved in QI
Electronic databases
Three3 electronic databases: PubMed, Scopus, and Web of Science were searched on 4th July 2018 on the Internet. These databases were selected to ensure a comprehensive inclusion of all published literature. To ensure that all possible publications were found, date, language, or document type restrictions were not specified during database search. Using the research question, we developed the following search terms: “quality improvement”, “implementation strategy”, “implementation process”, “Plan do study act”, “define measure analyze improve control”, “define measure analyze improve control”, “define measure analyze design verify”, “define measure analyze design verify”, ”lean six sigma”, “immunization”, “missed opportunities”, “infant”, “childhood”, “teenager”, and “adolescent” among others. These search terms are keywords that combine QI with missed opportunities for vaccination in children and adolescent. The search terms were tailored to each database. Detailed search strategy developed with input from an information specialist is attached as Appendix. All citations exported from databases were imported to Endnote X7.7.1. While on the reference manager, duplicate of citations were removed. The reference list of the selected manuscripts was also manually searched to identify any relevant paper that reported the use of QI approach to address missed opportunities for vaccination.
Grey literature
Advanced Google search using the following URL: https://www.google.com/advanced_search was implemented to identify gray literatures that are relevant to the review question.68 The keywords that were used for electronic database search were also applied. The search filters were left at their default setting so as to include results in any language, from any geographical region, and without data limits among others. Since Google search has the tendency to produce high search volume, we limited our search to the first 5047 results.69
Networks and organizations
Experts at the American Academy of Pediatrics were contacted by email with a request for any published or unpublished report on the use of QI approaches to address missed opportunities for vaccination among children. The use of QI practices is part of the academy’s mission of ensuring high standards of health for children.70
Stage 3: study selection
A set of eligibility criteria with inclusion and exclusion criteria were developed while preparing the protocol to help in removing studies that did not answer the review question. It was agreed that these eligibility criteria can be modified post hoc as the authors become more familiar with the studies.
Inclusion criteria were as follows:
All literature reporting a QI approach aimed at reducing missed opportunities for vaccination for children and adolescents.
Vaccines that are used for routine immunization
QI approaches implemented in a health facility setting
Exclusion criteria were as follows:
QI aimed at improving immunization rate in high-risk children with deficient immune system
QI approaches implemented within a community setting
After identifying relevant literature, two authors independently screened the titles and abstracts of all publications obtained from the electronic databases. If the studies broadly described the use of QI in a health facility setting to reduce missed opportunities for vaccination, its full text was retrieved. There was no masking of reviewers involved in the screening to author name or journal. It was agreed apriori that the full text of publications without abstracts will automatically be considered. The prespecified inclusion and exclusion criteria were applied to the full text of the publications to identify the “best fit”. The assistance of librarians at the medicine and health sciences library of Stellenbosch University, South Africa, was sought to help retrieve articles that were published in journals that the university did not subscribe to. It was also agreed that if full text could not be retrieved, then abstract can used. During the study selection, the two reviewers resolved any disagreements through discussion. Figure 1 is a four-phased flow diagram from identification through inclusion.71 The Google search results were also screened by the two authors.
Stage 4: charting the data
Two authors independently charted key information from the included publications. An Excel spreadsheet was used for this purpose. The charting approach used was similar to that of a narrative review as we obtained information about the QI projects.72 The recorded information is presented in Table 4.
Table 4.
Key information charted and their description.
| Information | Description |
|---|---|
| General characteristics | |
| ID | Identifier of the publication |
| Year of publication | Year of publication of the document |
| Country | Location of institution of the first author |
| Type of publication | Type of document |
| Language | Language of publication |
| Setting and target population | |
| Level of health-care | Category of health facility where the quality improvement project was implemented |
| Context | Setting in which the quality improvement project was conducted |
| Target population | Individuals whom the quality improvement was meant to have an impact on |
| Age group of target population | Age category of the individuals targeted in the quality improvement project |
| Quality improvement process | |
| Quality Improvement (QI) strategy | The strategies that were used during the quality improvement project |
| Quality Improvement (QI) team | People responsible for implementing the quality improvement project |
| Quality Improvement (QI) model | Theoretical framework or model of the quality improvement project |
| Quality Improvement (QI) method | Process of iterative implementation of the quality improvement activities |
| Vaccines | Antigens that were targeted |
Stage 5: collating, summarizing, and reporting the results
Charted information was collated using Microsoft Excel 2016. Same software was used for coding the data. Analysis was done using Microsoft Excel as well. Number of published literatures over the study periods were calculated. Descriptive statistics (frequency and percentage) of country affiliation, language of publication, publication type, and institutional affiliation of authors was also calculated. Vaccines targeted in each QI interventions were presented.
Conclusion
This scoping review identified and described the extent of current publications on use of QI approach to address MOV. There is a growing interest in the use of QI to improve health outcomes, and this was also observed for MOV. Given that only few publications were found, all of which were conducted in the United States, buttresses the need for this systematic appraisal of currently available literature. No published or gray literature was found in LMIC especially sub-Saharan Africa.
APPENDIX
PUBMED
(infant[mh] OR infant[tiab] OR infants[tiab] OR infancy[tiab] OR toddler*[tiab] OR preterm*[tiab] OR prematur*[tiab] OR postmatur*[tiab] OR baby[tiab] OR babies[tiab] OR neonat*[tiab] OR newborn[tiab] OR preschool*[tiab] OR pre-school*[tiab] OR child[mh] OR child*[tiab] OR kindergar*[tiab] OR pupil*[tiab] OR schoolchild*[tiab] OR teen*[tiab] OR youth[tiab] OR youths[tiab] OR youngster*[tiab] OR young person*[tiab] OR young people[tiab] OR minors[mh] OR minors[tiab] OR puberty[mh] OR puberty[tiab] OR pubescen*[tiab] OR prepubescen*[tiab] OR paediatric*[tiab] OR pediatric*[tiab] OR peadiatric*[tiab] OR schools[mh:noexp] OR school*[tiab] OR kid[tiab] OR kids[tiab] OR boy*[tiab] OR girl*[tiab] OR creche*[tiab] OR highschool*[tiab] OR “secondary school”[tiab] OR juvenil*[tiab] OR adolescent[mh] OR adolescen*[tiab])
AND
quality improvement[mh] OR (quality[tiab] AND (system*[tiab] OR process*[tiab] OR improvement*[tiab] OR enhancement*[tiab] OR strateg*[tiab] OR intervention*[tiab] OR management[tiab])) OR implementation strateg*[tiab] OR implementation process*[tiab]
OR
Plan do study act[tiab] OR plan do check act[tiab] OR define measure analyze improve control[tiab] OR define measure analyse improve control[tiab] OR define measure analyse design verify[tiab] OR define measure analyze design verify[tiab] OR lean six sigma[tiab]
AND
Immunization[mh] OR immuni*[tiab] OR vaccin*[tiab] OR revaccin*[tiab] OR innoculat*[tiab] OR inoculat*[tiab]
AND
Missed[tiab] AND opportunit*[tiab]
WEB OF Science (1970–2018)
ts = (infant OR toddler* OR preterm* OR prematur* OR baby OR babies OR neonat* OR newborn OR preschool* OR pre-school* OR child OR child*OR kindergar* OR pupil* OR schoolchild* OR teen* OR youth OR youths OR youngster* OR young person* OR young people OR minors OR minors OR puberty OR pubescen* OR prepubescen* OR paediatric*] OR pediatric* OR peadiatric* OR kid OR boy* OR girl* OR creche* OR highschool* OR “secondary school” OR juvenil* OR adolescent OR adolescen*)
AND
ts = (“quality improvement” OR “quality system*” OR “quality network*” OR “quality process* OR “quality improvement*” OR “quality enhancement*” OR “quality strateg*” OR “quality intervention*” OR “quality management” OR “implementation strategy*” OR “implementation process*”)
OR
ts = (“Plan do study act” OR “plan do check act” OR “define measure analyze improve control” OR “define measure analyse improve control” OR “define measure analyse design verify” OR “define measure analyze design verify” OR lean OR “six sigma”)
AND
ts = (Immunization OR immuni* OR vaccin* OR revaccin* OR innoculat* OR inoculat*)
AND
ts = (“missed opportunities for vaccination” OR “missed opportunities for immunization” OR Missed near/3 opportunit*)
SCOPUS
TITLE-ABS-KEY (“quality improvement” OR “quality system*” OR “quality network*” OR “quality process*” OR “quality improvement*” OR “quality enhancement*” OR “quality strateg*” OR “quality intervention*” OR “quality management” OR “implementation strategy*” OR “implementation process*” OR “Plan do study act” OR “plan do check act” OR “define measure analyze improve control” OR “define measure analyse improve control” OR “define measure analyse design verify” OR “define measure analyze design verify” OR lean OR “six sigma”)
TITLE-ABS-KEY (infant OR toddler* OR preterm* OR prematur* OR baby OR babies OR neonat* OR newborn OR preschool* OR pre-school* OR child OR child*OR kindergar* OR pupil* OR schoolchild* OR teen* OR youth OR youths OR youngster* OR young person* OR young people OR minors OR minors OR puberty OR pubescen* OR prepubescen* OR paediatric*] OR pediatric* OR peadiatric* OR kid OR boy* OR girl* OR creche* OR highschool* OR “secondary school” OR juvenil* OR adolescent OR adolescen*)
TITLE-ABS-KEY (Immunization OR immuni* OR vaccin* OR revaccin* OR innoculat* OR inoculat*)
Funding Statement
The research reported in this publication was supported by the South African Medical Research Council with funds received from the National Research Foundation of South Africa through its competitive program for rated researchers. This work is based on research supported wholly/in part by the National Research Foundation of South Africa (Grant Number: 106035). OAU receives support from National Institute of Health’s Official Development Assistance (ODA) funding. The views expressed in this publication are solely those of the authors.
Acknowledgments
The authors would like to thank Joy Oliver of Cochrane South Africa, South African Research Council, Tygerberg, for reviewing the search strategy used in this review. They would also like to thank the following librarians: Tracey Louw and Pamela Nyokwana, at the Medicine and Health Science Library of Stellenbosch University, South Africa.
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the authors.
Contributors
AAA conceptualized the study, drafted the review protocol, conducted the literature search, screened publications and charted data, conducted the data analysis and interpretation, and wrote the first draft of the manuscript. CSW, OAU, MAG reviewed and approved the protocol, contributed to data analysis and interpretation, manuscript development and approved the final manuscript. EOW screened publication and charted of data and contributed to manuscript development.
Ethics approval
Not applicable
References
- 1.Akmatov MK, Kretzschmar M, Kramer A, Mikolajczyk RT.. Timeliness of vaccination and its effects on fraction of vaccinated population. Vaccine. 2008;26(31):3805–11. doi: 10.1016/j.vaccine.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 2.Stack ML, Ozawa S, Bishai DM, Mirelman A, Tam Y, Niessen L, Walker DG, Levine OS. Estimated economic benefits during the ‘decade of vaccines’ include treatment savings, gains in labor productivity. Health Aff. 2011;30(6):1021–28. doi: 10.1377/hlthaff.2011.0382. [DOI] [PubMed] [Google Scholar]
- 3.Akmatov MK, Mikolajczyk RT. Timeliness of childhood vaccinations in 31 low and middle-income countries. J Epidemiol Community Health. 2012;66(7):e14. doi: 10.1136/jech.2010.109538. [DOI] [PubMed] [Google Scholar]
- 4.Deogaonkar R, Hutubessy R, van der Putten I, Evers S, Jit M. Systematic review of studies evaluating the broader economic impact of vaccination in low and middle income countries. BMC Public Health. 2012;12(1):878. doi: 10.1186/1471-2458-12-878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization Standards for improving the quality of care for children and young adolescents in health facilities. Geneva (Switzerland): World Health Organization; 2018. [Google Scholar]
- 6.Sridhar S, Maleq N, Guillermet E, Colombini A, Gessner BD. A systematic literature review of missed opportunities for immunization in low- and middle-income countries. Vaccine. 2014;32(51):6870–79. doi: 10.1016/j.vaccine.2014.10.063. [DOI] [PubMed] [Google Scholar]
- 7.Hutchins SS, Jansen HA, Robertson SE, Evans P, Kim-Farley RJ. Studies of missed opportunities for immunization in developing and industrialized countries. Bull WHO. 1993;71:549–60. [PMC free article] [PubMed] [Google Scholar]
- 8.Adamu AA, Sarki AM, Uthman OA, Wiyeh AB, Gadanya MA, Wiysonge CS. Prevalence and dynamics of missed opportunities for vaccination among children in Africa: applying systems thinking in a systematic review and meta-analysis of observational studies. Expert Rev Vaccines. 2019. doi: 10.1080/14760584.2019.1588728. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization Planning guide to reduce missed opportunities for vaccination. Geneva (Switzerland): World Health Organization; 2017. [Google Scholar]
- 10.Shojania KG, Grimshaw JM. Evidence-based quality improvement: the state of the science. Health Aff. 2005;24(1):138–50. doi: 10.1377/hlthaff.24.1.138. [DOI] [PubMed] [Google Scholar]
- 11.Batalden PB, Davidoff F. What is “quality improvement” and how can it transform healthcare?. London: BMJ Publishing Group Ltd; 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leviton L. Reconciling complexity and classification in quality improvement research. BMJ Qual Saf. 2011;20(Suppl 1):i28–i9. doi: 10.1136/bmjqs.2010.046375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.James BC, Savitz LA. How Intermountain trimmed health care costs through robust quality improvement efforts. Health Aff. 2011;30(6):1185–91. doi: 10.1377/hlthaff.2011.0358. [DOI] [PubMed] [Google Scholar]
- 14.Kraft S, Carayon P, Weiss J, Pandhi N. A simple framework for complex system improvement. Am J Med Qual. 2015;30(3):223–31. doi: 10.1177/1062860614530184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dixon-Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the health foundation‘s programme evaluations and relevant literature. BMJ Qual Saf. 2012;21:876–884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Batalden PB, Stoltz PK. A framework for the continual improvement of health care: building and applying professional and improvement knowledge to test changes in daily work. Jt Comm J Qual Improv. 1993;19:424–47. [DOI] [PubMed] [Google Scholar]
- 17.Burgess N, Radnor Z. Evaluating Lean in healthcare. Int J Health Care Qual Assur. 2013;26(3):220–35. doi: 10.1108/09526861311311418. [DOI] [PubMed] [Google Scholar]
- 18.Radnor ZJ, Holweg M, Waring J. Lean in healthcare: the unfilled promise? Soc Sci Med. 2012;74(3):364–71. doi: 10.1016/j.socscimed.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 19.Powell A, Rushmer R, Davies H. A systematic narrative review of quality improvement models in health care. Glasgow: NHS Quality Improvement Scotland; 2009. [Google Scholar]
- 20.Corn JB. Six sigma in health care. Radiol Technol. 2009;81:92–95. [PubMed] [Google Scholar]
- 21.Series B, Kilo CM. A framework for collaborative improvement: lessons from the institute for healthcare improvement’s breakthrough series. Qual Manag Health Care. 1998;6:1–13. [DOI] [PubMed] [Google Scholar]
- 22.Dahlgaard JJ, Mi Dahlgaard-Park S. Lean production, six sigma quality, TQM and company culture. The TQM Mag. 2006;18(3):263–81. doi: 10.1108/09544780610659998. [DOI] [Google Scholar]
- 23.Pepper MP, Spedding TA. The evolution of lean Six Sigma. Int J Qual Reliab Manage. 2010;27(2):138–55. doi: 10.1108/02656711011014276. [DOI] [Google Scholar]
- 24.Horbar JD, Rogowski J, Plsek PE, Delmore P, Edwards WH, Hocker J, Kantak AD, Lewallen P, Lewis W, Lewit E, et al. Collaborative quality improvement for neonatal intensive care. Pediatrics. 2001;107:14–22. [DOI] [PubMed] [Google Scholar]
- 25.Birenbaum HJ, Dentry A, Cirelli J, Helou S, Pane MA, Starr K, Melick CF, Updegraff L, Arnold C, Tamayo A, et al. Reduction in the incidence of chronic lung disease in very low birth weight infants: results of a quality improvement process in a tertiary level neonatal intensive care unit. Pediatrics. 2009;123(1):44–50. doi: 10.1542/peds.2007-2872. [DOI] [PubMed] [Google Scholar]
- 26.Chin MH, Alexander-Young M, Burnet DL. Health care quality-improvement approaches to reducing child health disparities. Pediatrics. 2009;124(Supplement 3):S224–S36. doi: 10.1542/peds.2009-1100K. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leatherman S, Ferris TG, Berwick D, Omaswa F, Crisp N. The role of quality improvement in strengthening health systems in developing countries. Int J Qual Health Care. 2010;22(4):237–43. doi: 10.1093/intqhc/mzq028. [DOI] [PubMed] [Google Scholar]
- 28.Oyesola R, Shehu D, Maru I. Improving emergency obstetric care at a state referral hospital, Kebbi State, Nigeria. Int J Gynecol Obstet. 1997;59:S2. doi: 10.1016/S0020-7292(97)00150-1. [DOI] [PubMed] [Google Scholar]
- 29.Djan J, Kyei‐Faried S, Twum S, Danquah J, Ofori M, Browne E. Upgrading obstetric care at the health center level, Juaben, Ghana. Int J Gynecol Obstet. 1997;59:S2. doi: 10.1016/S0020-7292(97)00151-3. [DOI] [PubMed] [Google Scholar]
- 30.Kayongo M, Butera J, Mboninyibuka D, Nyiransabimana B, Ntezimana A, Mukangamuje V. Improving availability of EmOC services in Rwanda—CARE‘s experiences and lessons learned at Kabgayi Referral Hospital. Int J Gynecol Obstet. 2006;92(3):291–98. doi: 10.1016/j.ijgo.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 31.Arksey H, O‘Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 32.Daudt HM, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13(1):48. doi: 10.1186/1471-2288-13-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pham MT, Rajic A, Greig JD, Sargeant JM, Papadopoulos A, McEwen SA. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–85. doi: 10.1002/jrsm.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Patterson BL, Gregg WM, Biggers C, Barkin S. Improving delivery of EPSDT well-child care at acute visits in an academic pediatric practice. Pediatrics. 2012;130(4):e988–95. doi: 10.1542/peds.2012-0355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shaw JS, Wasserman RC, Barry S, Delaney T, Duncan P, Davis W, Berry P. Statewide quality improvement outreach improves preventive services for young children. Pediatrics. 2006;118(4):e1039–47. doi: 10.1542/peds.2005-2699. [DOI] [PubMed] [Google Scholar]
- 36.Chung RJ, Walter EB, Kemper AR, Dayton A. Keen on teen vaccines: improvement of adolescent vaccine coverage in rural North Carolina. J Adolesc Health. 2015;56(5 Suppl):S14–6. doi: 10.1016/j.jadohealth.2014.10.272. [DOI] [PubMed] [Google Scholar]
- 37.Malone K, Clark S, Palmer JA, Lopez S, Pradhan M, Furth S, Kim J, Fisher B, Laskin B. A quality improvement initiative to increase pneumococcal vaccination coverage among children after kidney transplant. Pediatr Transplant. 2016;20(6):783–89. doi: 10.1111/petr.12742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pahud B, Clark S, Herigon JC, Sherman A, Lynch DA, Hoffman A, Jackson MA. A pilot program to improve vaccination status for hospitalized children. Hosp Pediatr. 2015;5(1):35–41. doi: 10.1542/hpeds.2014-0027. [DOI] [PubMed] [Google Scholar]
- 39.Perkins RB, Zisblatt L, Legler A, Trucks E, Hanchate A, Gorin SS. Effectiveness of a provider-focused intervention to improve HPV vaccination rates in boys and girls. Vaccine. 2015;33(9):1223–29. doi: 10.1016/j.vaccine.2014.11.021. [DOI] [PubMed] [Google Scholar]
- 40.Harris JG, Maletta KI, Ren B, Olson JC. Improving pneumococcal vaccination in pediatric rheumatology patients. Pediatrics. 2015;136(3):e681–6. doi: 10.1542/peds.2014-2512. [DOI] [PubMed] [Google Scholar]
- 41.Daley MF, Steiner JF, Kempe A, Beaty BL, Pearson KA, Jones JS, Lowery NE, Berman S. Quality improvement in immunization delivery following an unsuccessful immunization recall. Ambulatory Pediatr: Off J Ambulatory Pediatr Assoc. 2004;4(3):217–23. doi: 10.1367/A03-176R.1. [DOI] [PubMed] [Google Scholar]
- 42.Daly KL, Halon PA, Aronowitz T, Ross G. A university health initiative to increase human papillomavirus vaccination rates. J Nurse Pract. 2016;12(6):e281–e6. doi: 10.1016/j.nurpra.2016.02.013. [DOI] [Google Scholar]
- 43.Fiks AG, Luan X, Mayne SL. Improving HPV vaccination rates using maintenance-of-certification requirements. Pediatrics. 2016;137(3):e20150675. doi: 10.1542/peds.2015-0675. [DOI] [PubMed] [Google Scholar]
- 44.Jones KB, Spain C, Wright H, Gren LH. Improving immunizations in children: a clinical break-even analysis. Clin Med Res. 2015;13(2):51–57. doi: 10.3121/cmr.2014.1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Krantz L, Ollberding NJ, Beck AF, Carol Burkhardt M. Increasing HPV vaccination coverage through provider-based interventions. Clin Pediatr. 2018;57(3):319–26. doi: 10.1177/0009922817722014. [DOI] [PubMed] [Google Scholar]
- 46.Moore KL, Fankhauser MK, Hull PC. Tennessee‘s 3-star report: using available data systems to reduce missed opportunities to vaccinate preteens. Biomed Inform Insights. 2016;8(Suppl 2):15–21. doi: 10.4137/BII.S40207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rand CM, Tyrrell H, Wallace-Brodeur R, Goldstein NPN, Darden PM, Humiston SG, Albertin CS, Stratbucker W, Schaffer SJ, Davis W, et al. A learning collaborative model to improve human papillomavirus vaccination rates in primary care. Acad Pediatr. 2018;18(2S):S46–S52. doi: 10.1016/j.acap.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 48.Jones KB, Gren LH, Backman R. Improving pediatric immunization rates: description of a resident-led clinical continuous quality improvement project. Fam Med. 2014;46:631–35. [PubMed] [Google Scholar]
- 49.Sinn JS, Morrow AL, Finch AB. Improving immunization rates in private pediatric practices through physician leadership. Arch Pediatr Adolesc Med. 1999;153(6):597–603. doi: 10.1001/archpedi.153.6.597. [DOI] [PubMed] [Google Scholar]
- 50.Melinkovich P, Hammer A, Staudenmaier A, Berg M. Improving pediatric immunization rates in a safety-net delivery system. Jt Comm J Qual Patient Saf. 2007;33:205–10. [DOI] [PubMed] [Google Scholar]
- 51.Carlin E, Carlson R, Nordin J. Using continuous quality improvement tools to improve pediatric immunization rates. Jt Comm J Qual Improv. 1996;22:277–88. [DOI] [PubMed] [Google Scholar]
- 52.Schneider A. How quality improvement in health care can help to achieve the millennium development goals. Sao Paulo, Brazil: SciELO Public Health; 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP. The improvement guide: a practical approach to enhancing organizational performance. New Jersey, NJ: John Wiley & Sons; 2009. [Google Scholar]
- 54.Wandersman A, Imm P, Chinman M, Kaftarian S. Getting to outcomes: A results-based approach to accountability. Eval Program Plann. 2000;23(3):389–95. doi: 10.1016/S0149-7189(00)00028-8. [DOI] [Google Scholar]
- 55.Eccles M, Grimshaw J, Campbell M, Ramsay C. Research designs for studies evaluating the effectiveness of change and improvement strategies. BMJ Qual Saf. 2003;12(1):47–52. doi: 10.1136/qhc.12.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shadish W, Cook TD, Campbell DT Experimental and quasi-experimental designs for generalized causal inference. Boston, MA: Houghton Mifflin; 2002. [Google Scholar]
- 57.Patsopoulos NA. A pragmatic view on pragmatic trials. Dialogues Clin Neurosci. 2011;13:217–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Roland M, Torgerson DJ. Understanding controlled trials: what are pragmatic trials?. Bmj. 1998;316:285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care. 2012;50(3):217–26. doi: 10.1097/MLR.0b013e3182408812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Brown P, Brunnhuber K, Chalkidou K, Chalmers I, Clarke M, Fenton M, Forbes C, Glanville J, Hicks NJ, Moody J, et al. How to formulate research recommendations. Bmj. 2006;333(7572):804–06. doi: 10.1136/bmj.38987.492014.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. J Continuing Educ Nurs. 2015;46(11):501–07. doi: 10.3928/00220124-20151020-02. [DOI] [PubMed] [Google Scholar]
- 62.Levac D, Colquhoun H, O‘Brien KK. Scoping studies: advancing the methodology. Implementation Sci. 2010;5(1):69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gough D, Thomas J, Oliver S. Clarifying differences between review designs and methods. Syst Rev. 2012;1(1):28. doi: 10.1186/2046-4053-1-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tricco AC, Tetzlaff J, Moher D. The art and science of knowledge synthesis. J Clin Epidemiol. 2011;64(1):11–20. doi: 10.1016/j.jclinepi.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 65.Colquhoun HL, Levac D, O‘Brien KK, Straus S, Tricco AC, Perrier L, Kastner M, Moher D. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–94. doi: 10.1016/j.jclinepi.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 66.World Health Organization Summary of WHO position papers - Recommended routine immunizations for children Geneva, Switzerland: World Health Organization; 2018. [accessed 2018 July 12 at 2:38PM] http://www.who.int/immunization/policy/Immunization_routine_table2.pdf?ua=1. [Google Scholar]
- 67.Effective Practice and Organization of Care (EPOC) EPOC Taxonomy; 2015. [accessed 2017] http://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/2015%20EPOC%20Taxonomy%20FINAL.pdf.
- 68.Ripple AS. Expert Googling: best practices and advanced strategies for using Google in health sciences libraries. Med Ref Serv Q. 2006;25(2):97–107. doi: 10.1300/J115v25n02_08. [DOI] [PubMed] [Google Scholar]
- 69.Freeman MK, Lauderdale SA, Kendrach MG, Woolley TW. Google Scholar versus PubMed in locating primary literature to answer drug-related questions. Ann Pharmacother. 2009;43(3):478–84. doi: 10.1345/aph.1L223. [DOI] [PubMed] [Google Scholar]
- 70.American Academy of Paediatrics Quality improvement; 2018. [accessed 2018 July 14 at 2:48pm] https://www.aap.org/en-us/professional-resources/quality-improvement/Pages/default.aspx.
- 71.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–69. [DOI] [PubMed] [Google Scholar]
- 72.Pawson R. Evidence-based policy: in search of a method. Evaluation. 2002;8(2):157–81. doi: 10.1177/1358902002008002512. [DOI] [Google Scholar]
- 73.Heidi Gurov (2018). Assessment-Feedback-Incentives-Exchange. Wyoming Immunization Conference. Wyoming, United States, Wyoming Department of Health. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Effective Practice and Organization of Care (EPOC) EPOC Taxonomy; 2015. [accessed 2017] http://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/2015%20EPOC%20Taxonomy%20FINAL.pdf.


