Abstract
Background:
Urinary tract infections are considered as one of the most frequent bacterial infections in the community and hospital settings. In this era of increasing antimicrobial resistance, antimicrobial stewardship has become highly important in the struggle to preserve the effectiveness of available drugs. One the main causes of antibiotic resistance is the inappropriate prescribing of antibiotics; which evidence show that community pharmacists contribute to.
Objective:
This study aims to evaluate antibiotic prescribing rate and responses of the contact persons in community pharmacies and to assess the conformity of the prescribed antibiotics with international guidelines. It also aims to evaluate the responses with sociodemographic characteristics.
Methods:
A cross-sectional, nationwide study conducted between February and May 2017 using a simulated patient case of acute uncomplicated cystitis. Two hundred fifty pharmacies were included. Descriptive data was reported for the medications prescribed, conformity, questions asked and counseling. Bivariate analysis using the Pearson chi-squared, Fisher’s exact and Student’s t-tests were used to identify possible factors affecting the prescribing rates and responses in community pharmacies.
Results:
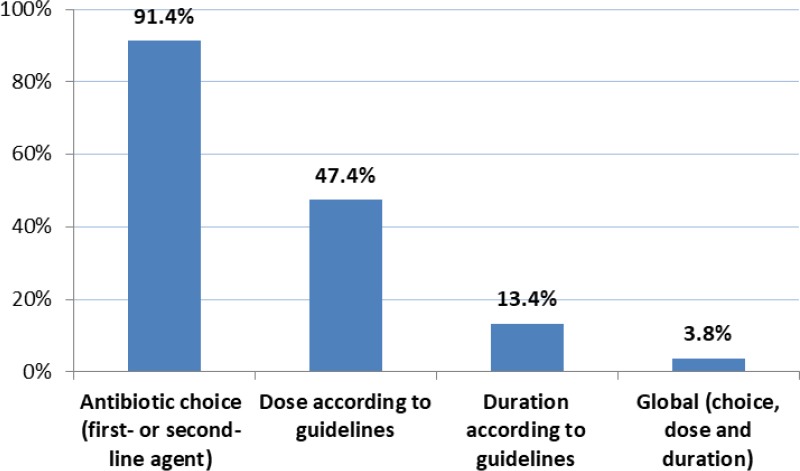
The prescribing rate of antibiotics was 83.6% (n=209) with ciprofloxacin being the most prescribed (50.2%, n=105). The global conformity to international guidelines was 3.8% (n=8) with the highest conformity rate for the antibiotic choice (91.4%, n=191). Counseling about what to do in case symptoms persist was 12.8% (n=32) and that of non-pharmacological management was 53.6% (n=134). Male participants (88.1%) had a higher prescribing rate than female participants (77.6%) (p<0.05). The number of questions asked was higher in pharmacists and in female participants (p<0.05). Other results showed non-significant differences in diagnosis, antibiotic prescribing, conformity rates, referral rates and counseling points between the pharmacists and assistants.
Conclusions:
The high antibiotic prescribing rate in Lebanese community pharmacies is alarming and calls for action. This should be tackled by legislative bodies, which should enforce laws that restrict such practices.
Keywords: Anti-Bacterial Agents, Urinary Tract Infections, Inappropriate Prescribing, Prescription Drug Overuse, Antimicrobial Stewardship, Drug Resistance, Bacterial, Professional Practice, Pharmacies, Pharmacists, Counseling, Referral and Consultation, Patient Simulation, Cross-Sectional Studies, Lebanon
INTRODUCTION
Urinary tract infections (UTIs) are considered one of the most frequent bacterial infections in the community and hospital settings.1 The responsible bacteria for these infections are gaining greater resistance, particularly the extended spectrum beta-lactamase (ESBL) producing bacteria and the fluoroquinolone-resistant Enterobacteriaceae.2,3 According to the World Health Organization (WHO), antimicrobial resistance forms a major public threat since it is evolving throughout the years.4 The Centers for Disease Control and Prevention (CDC) stated that at least 2 million people become infected each year in the United States with bacteria that are resistant to antibiotics, with at least 23,000 deaths each year.5,6 Similarly, the WHO stated that a post-antibiotic era would result in frequent infections leading to death if we fail to act against the resistance.7
Evidence shows that inappropriate prescribing of antibiotics is the main cause of antibiotic resistance and it includes inappropriate indication or posology by physicians, self-medicating by patients and prescribing antibiotics by community pharmacists.8,9 It is well-documented that community pharmacists contribute to antibiotic misuse in many countries for common infections.10 Thus, practice of pharmacists in antibiotic dispensing and prescribing is of main concern, noting that pharmacists are not prescribers of antibiotics according to the CDC.11
Although there are laws in many countries that prohibit dispensing of antibiotics without medical prescriptions, alarming results were reported when evaluating the rate of antibiotic prescribing by community pharmacists. One of the most common infections in women is acute uncomplicated cystitis.11 Using a simulated case of acute uncomplicated cystitis in Saudi Arabia, Jordan and Spain, antibiotics were dispensed without a medical prescription.12-14 There is a similar law in Lebanon, however its implementation is questionable. The rates of antibiotic prescribing in community pharmacies reported in Lebanon were evaluated using surveys, a subjective method. However, no studies, to date, have evaluated the true antibiotic prescribing rate in acute uncomplicated cystitis in Lebanese community pharmacies. The primary objectives of this study are to evaluate the rate of antibiotic prescribing, determine the type of antibiotics prescribed and assess the global and specific conformity of the antibiotics prescribed with international guidelines in Lebanese community pharmacies. The secondary objectives are to assess the questions asked and counseling of the contact persons (participants) and to study the association between the participants’ responses and their socio-demographic characteristics.
METHODS
It is an observational cross-sectional study using the simulated patient method of a case of acute uncomplicated cystitis. We evaluated the rate of antibiotic prescribing in Lebanese community pharmacies and we assessed the prescribing practices for conformity with international guidelines. At the time of data collection, no national guidelines were available. The guidelines used as reference were the Infectious Diseases Society of America (IDSA) in collaboration with European Society for Microbiology and Infectious Diseases (ESCMID) (2011), European Association of Urology (EAU) (2015) and American Association of Family Physicians (AAFP) guidelines for the treatment of acute uncomplicated cystitis (2011).15-17 We defined the global conformity of the antibiotic prescribed to the aforementioned international guidelines as meeting the three types of conformity simultaneously: choice, dose and duration. Choice conformity was met whether the prescribed antibiotic belonged to the first-line or second-line agents.
Sampling and data collection
We obtained a list of all Lebanese community pharmacies from the Order of Pharmacists of Lebanon. We obtained a random sample through stratifying Lebanon into its six distinct provinces (Beirut, Mount Lebanon, North Lebanon, South Lebanon, Bekaa and Nabatiyeh), followed by a proportional systematic random sampling in each province. The distribution of community pharmacies in Lebanon is previously reported in a similar study (18). We included 250 community pharmacies, assuming that the expected rate of dispensing was 75%.12 We set the acceptable margin of error to 5% and the confidence level 95%.
We collected data from February 2017 to late May 2017. There were two investigators (who are among the authors and are pharmacists) responsible for data collection. Each investigator had an exclusive and defined role. They presented to each of the sampled community pharmacies with a standardized case of uncomplicated cystitis. The main investigator claimed to have a female relative with urinary symptoms and the other investigator only observed. The latter’s main role was to help with the recall of data once the encounter was done, to minimize the recall bias. Both investigators were aware of the actual objective of this study. The main investigator would ask for the pharmacist, if he/she was not available, the encounter proceeded with the assistant. The investigator would then ask for advice for the female relative.
The encounter went as follows: “hello, are you the pharmacist?”, once the participant was identified to be the pharmacist or assistant, the investigator proceeded: “my cousin has a burning sensation upon urination, what do I get her?”. The standardized case was the following:
Patient characteristics: 27-year-old, non-pregnant, sexually inactive woman with no known allergies
Present illness: painful urination, frequency and urgency, which started 2 days ago. No fever, flank pain or vaginal discharge is present
Past medical history: no urologic abnormalities (stones, stents, indwelling catheters, neurogenic bladder, polycystic kidney disease), comorbidities (immunocompromised, metabolic disorder or childhood urinary tract infections) or previous urinary tract infections
Medications: no current chronic medications
Management at home: acetaminophen for pain management
If referral to a physician was directly suggested by the participant, the investigator would not insist on getting advice. If antibiotics were suggested and no information was provided about use, the investigator would question about them. Following each encounter, the investigators filled one data collection form. It included three major parts: Pharmacy Demographics, Questions Asked by the contact person (Online appendix), and Treatment and Counseling.
Data analysis
We performed all the data analyses using IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA). We reported the descriptive data as percentages and means with standard deviations (SD). We conducted bivariate analyses to evaluate antibiotic prescribing rate with each sociodemographic characteristic such as the participant, gender and province of the pharmacy. We conducted the same analyses for the number of questions asked. We studied the differences between pharmacists and assistants in the diagnosis, counseling points, referral and conformity rates. We used the Pearson chi-squared test for the qualitative dichotomous variables and Fisher’s exact test when the expected values within cells were less than 5. For the quantitative variables, we used the Student’s t-test. We set a p<0.05 for statistical significance. Non-disclosure to participants was considered ethically acceptable by the Lebanese University ethics committee, since we kept the data anonymous and did not record any of the encounters.
RESULTS
We visited a total of 250 pharmacies distributed across the six provinces of Lebanon (Beirut, Mount Lebanon, North Lebanon, South Lebanon, Bekaa, Nabatiyeh). The distribution of the contact persons and the pharmacies across the provinces of Lebanon are detailed in Table 1. Mainly, not all the participants were pharmacists (71%) and almost 60% were male participants.
Table 1. Sociodemographic characteristics of the sampled pharmacies (N=250).
| Sociodemographic characteristic | n (%) |
|---|---|
| Participant (contact person) | |
| Pharmacist | 179 (71.6) |
| Assistant | 71 (28.4) |
| Gender | |
| Male | 143 (57.2) |
| Female | 107 (42.8) |
| Province of the Pharmacy | |
| Beirut | 20 (8.0) |
| Mount Lebanon | 109 (43.6) |
| North Lebanon | 36 (14.4) |
| South Lebanon | 29 (11.6) |
| Bekaa | 39 (15.6) |
| Nabatiyeh | 17 (6.8) |
In response to the presentation of the investigator with a case of acute uncomplicated cystitis, the diagnoses of the 250 participants was as follows: 180 participants (72%) diagnosed the patient with a UTI, two (0.8%) diagnosed the patient with lithiasis and 68 (27.2%) gave no diagnosis. None of the participants who diagnosed the patient with a UTI specified the type.
The global antibiotic prescribing rate was 83.6%. The most prescribed antibiotic was ciprofloxacin (50.2%) whereas the least prescribed ones were trimethoprim/sulfamethoxazole (TMP/SMX) 600/180mg and amoxicillin/clavulanic acid 500/125mg with a prescribing rate of 0.5% for each. The most prescribed antibiotic family was the fluoroquinolones with the highest rate of 86.6%. The antibiotics prescribed are presented in Table 2.
Table 2. Antibiotics prescribed by participants (N=209).
| Antibiotics prescribed | n (%) |
|---|---|
| Nitrofuran | 3 (1.4) |
| Nitrofurantoin 100mg | 3 (1.4) |
| Sulfonamide | 1 (0.5) |
| TMP/SMX 160/800mg | 1 (0.5) |
| Phosphonic Acid | 5 (2.4) |
| Fosfomycin | 5 (2.4) |
| Fluoroquinolones | 181 (86.6) |
| Ciprofloxacin 500mg | 105 (50.2) |
| Norfloxacin 400mg | 71 (34) |
| Levofloxacin 500mg | 4 (1.9) |
| Ofloxacin 200mg | 1 (5) |
| Beta-Lactams | 19 (9.1) |
| Amoxicillin Clavulanate 500/125mg | 1 (0.5) |
| Cefixime 400mg | 18 (8.6) |
Out of the 250 participants, 76 (30.4%) prescribed medications other than antibiotics. The medications are divided into four classes. The most prescribed class was the supplements (cranberry) (18.4%), followed by disintegrating agents (including concrement solvents and pH modifiers) (5.6%), antispasmodics (4.8%) and lastly anti-inflammatory (1.6%).
The global conformity rate of the prescribed antibiotic to one of the international guidelines was 3.8% (n=8). Conformity to the antibiotic type was the highest with a choice conformity rate of 91.4% (n=191), followed by dose and duration conformity as shown in Figure 1.
Figure 1. Conformity rates to international guidelines based on antibiotic choice, dose and duration (N=209).
The questions asked by the 250 participants after the presentation of the simulated patient case by the investigator were grouped into four categories: UTI Symptoms, Differential Symptoms, Risk Factors and Other Questions. The total frequency of each category of questions (where at least one question was asked in the category) was 54.4%, 41.6%, 66.8% and 37.6%, respectively. The most asked questions in each category were frequency of urination (44%), vaginal symptoms (20%), age (61.2%) and onset (28%). The mean number of questions asked was 3.1 (SD=2.27) questions, ranging between no questions asked to 10 questions asked. None of the contact persons asked all five questions relating to the symptoms of cystitis. In addition, two participants asked three questions that differentiate between cystitis and other medical conditions. Out of the 250 participants, two asked about the use of concomitant medications, seven asked about pregnancy and 11 asked about allergies.
In response to the case of acute uncomplicated cystitis, the participants’ referral rate to directly seek a physician was 15.2%. In addition, 18% of the participants suggested a urine test. Out of the 209 participants who prescribed an antibiotic, 87.1% explained the expected action of the medication prescribed, and none counseled about side effects, interactions or actions to be taken in case a dose is missed. Regarding the counseling points if symptoms persist, 32 participants mentioned at least one of the suggestions: seek a physician (4%), do urine tests (7.2%), take antibiotic course (3.6%) or take cranberry (0.4%). Moreover, 134 participants (53.6%) counseled about the non-pharmacological management of acute uncomplicated cystitis. The suggestions included at least one of the following: increasing water intake (46.8%), using a vaginal wash (4.8%), voiding frequently (0.4%), or taking cranberry supplements (1.6%).
The prescribing rate of antibiotics was compared against the sociodemographic characteristics. The results are presented in Table 3. For the gender, the antibiotic prescribing rate of male participants was significantly higher (88.1%) than that of the female participants (77.6%) (p=0.026). On the other hand, the prescribing rate did not differ between pharmacists and assistants, or between provinces. There was no statistically significant difference between any of the sociodemographic characteristics and the choice of antibiotic prescribed. Similarly, happened for the global conformity rate. It was not statistically different between the pharmacists and the assistants; 3.4% (n=5) and 5% (n=3), respectively (p>0.05) or the other sociodemographic characteristics. Likewise, for the diagnosis, referral rate, and counseling points, if symptoms persist. When comparing the number of questions asked, statistically significant results were obtained for the participants and gender, as presented in Table 4. The pharmacists had a higher mean of questions asked than the assistants’ (3.45; SD=2.36 versus 2.24; SD=1.76) (p<0.001). Similarly, for the male participants versus the female participants (2.81; SD=2.19 versus 3.49; SD=2.32) (p=0.018). In addition, there was no significant difference in the mean number of questions asked between those who prescribed an antibiotic (3.19; SD=2.2) and those who did not (2.65; SD=2.5) (p=0.765).
Table 3. Antibiotic prescribing rate according to the participant, gender and province (N=250).
| Antibiotic prescribed N=209 | Antibiotic prescribed N=41 | p-value | |
|---|---|---|---|
| Participant † | 0.807 | ||
| Pharmacist | 149 (83.2%) | 30 (16.8%) | |
| Assistant | 60 (84.5%) | 11 (15.5%) | |
| Gender † | 0.026* | ||
| Male | 126 (88.1%) | 17 (11.9%) | |
| Female | 83 (77.6%) | 24 (22.4%) | |
| Province of the Pharmacy ‡ | 0.271 | ||
| Beirut | 15 (75.0%) | 5 (25.0%) | |
| Mount Lebanon | 90 (82.6%) | 19 (17.4%) | |
| North Lebanon | 30 (83.3%) | 6 (16.7%) | |
| South Lebanon | 27 (93.1%) | 2 (6.9%) | |
| Bekaa | 35 (89.7%) | 4 (10.3%) | |
| Nabatiyeh | 12 (70.6%) | 5 (29.4%) |
†The statistical test used was the Pearson Chi-Squared
‡The statistical test used was Fisher’s Exact
statistically significant
Table 4. The mean number of questions asked according to the participant, gender and province (N=250).
| questions Mean (SD) | p-value | |
|---|---|---|
| Participant † | <0.001* | |
| Pharmacist | 3.45 (2.36) | |
| Assistant | 2.24 (1.76) | |
| Gender † | 0.018* | |
| Male | 2.81 (2.19) | |
| Female | 3.49 (2.32) | |
| Province of the Pharmacy † | 0.765 | |
| Beirut | 3.09 (2.31) | |
| Outside Beirut | 3.25 (1.8) |
†Student’s t-test.
statistically significant
SD: standard deviation
DISCUSSION
To our knowledge, this study is the first to assess the true rate of antibiotic prescription for UTIs in a representative sample of 250 Lebanese community pharmacies distributed across the six provinces of the country. The standardized patient method unifies the presentation of acute uncomplicated cystitis and hence the results it provides are reliable, valid, and comparable across pharmacies. The results of the present study show that the prescribing rate of antibiotics in Lebanon following a simulated case of acute uncomplicated cystitis is 83.6%. This prescribing rate is high, especially that such practice is restricted by laws and regulations and that the investigators neither requested antibiotics nor insisted on having them. The results from a study using a self-administered questionnaire filled by the pharmacists report that 61% of them would dispense antibiotics without a medical prescription for cases of urinary symptoms without fever, flank pain or vaginal symptoms.19 However, our study shows a much higher rate of antibiotic prescribing than that self-reported by the pharmacists. The latter rate was evaluated using a subjective method, which probably underestimated the true rate of antibiotic dispensing without a prescription, since many pharmacists might have not admitted their actual practices, a great limitation to that study. Unlike Zimbabwe, where the study conducted to compare the rate of self-reported antibiotic prescribing by pharmacists and the actual prescribing in real life setting were similar.20 Given that the two most prescribed antibiotics were ciprofloxacin and norfloxacin, fluroquinolones were the most prescribed antibiotic family. Fluoroquinolones are second-line antibiotics which can be used depending on the susceptibility patterns, tolerance, availability and cost. The third most prescribed antibiotic, cefixime, a third generation cephalosporin.
These results concord with previous studies done in Lebanon that tackle antibiotic misuse. A study to assess self-medication in Lebanon report that 42% of the participants were buying antibiotics without a prescription with the pharmacists being the main helpers (18.8 %).21 Although there are no previous studies conducted in Lebanon using the simulated patient method for UTIs, the antibiotic prescribing rate was found to be comparable to that in other countries. A study in Riyadh reported the antibiotic prescribing rate to be 77.6%, of which 95% were dispensed without the patient’s request, and in cases of UTI to be 75% with ciprofloxacin being the most prescribed (86%).12 In a similar study also conducted in Riyadh, the prescribing rate was 82% for the simulated-UTI-patient with fluoroquinolones being the most prescribed (69%).22 In Jordan, the prescribing rate was reported to be 74.3% in general and 83.3% for UTI cases with fluoroquinolones being the most prescribed family (80%).23 Similar results were reported in Spain, where the prescribing rate of antibiotics in a simulated case of UTI was 79.7%.14 Generally, the antibiotic prescribing rate of a simulated case of UTI are comparable to that of Lebanon’s and ciprofloxacin and the fluoroquinolones family were the most prescribed in all of the mentioned studies.
Some of the reasons that might explain this high antibiotic prescribing rate can be explained by the reasons that were reported by Lebanese pharmacists for dispensing antibiotics without a prescription. These include the inability of many patients to afford a medical visit.19 We believe that this is very common in Lebanon for patients to consider community pharmacists as the ‘go-to’ healthcare professionals for clinical advice, given the cost of medical consultation. This is also highlighted in a study done in Colombia where participants report that pharmacy storekeepers are more trusted than other health-care professionals.24 In addition, it is reported that the pharmacist’s choice of antibiotic is profit-driven where it is based on the sales offers and discounts by pharmaceutical companies and distributors.19 We suggest that this very applicable here where many incentives are provided by the pharmaceutical industry for medication prescribers to affect their choice of medication. The high competition between community pharmacies also plays a role, thus, pharmacists treat their patients in order not to “lose them” to neighboring community pharmacies. Another reason is the affordability of the antibiotics, along with the recent major drop in their prices. In addition, the participants might have considered this infection as simple and common, specifically because the case is a young adult. The rate might have been lower if the case was an older adult or a child. All these reasons affect the ethics and professionalism of the pharmacists’ (and their assistants’) practice. However, the rate would have been higher if the data collection was done in the summer, when UTIs occurrence peak as reported in a study to assess the seasonality of UTIs.25 Moreover, a study done in Saudi Arabia summarizes the contributing factors to this practice that can be applicable to Lebanon which include economic hardship, patient’s age, emotional factors, and self-confidence of many pharmacists in diagnosing and prescribing medications, specifically antibiotics.26 Although considered illegal, the law that prohibits antibiotic dispensing without a prescription, nonetheless antibiotic prescribing, is not being enforced by the authorities, which can contribute to this practice.
Medications that were prescribed other than antibiotics were not recommended by any of the guidelines. Most of the medications prescribed help in symptomatic relief like the anti- inflammatory and anti-spasmodic classes. The disintegrating agents, concrement solvents and urinary pH modifiers are mainly used in cases of lithiasis and stones. These classes are no indicated in cases of acute uncomplicated cystitis. Finally, cranberry has no proven efficacy in the treatment of cystitis. We suggest that such medications were prescribed due to a doubtful diagnosis of the participants (whether it is a UTI, lithiasis, both or none). What might have also played a role is that some of the medications are classified as over-the-counter medications. We also suggest that this practice might be profit-driven, similar to the antibiotic prescribing.
As for the conformity to one of the mentioned guidelines, the highest rate of conformity was the antibiotic choice (91.4%) where the participants either prescribed a first or a second line antibiotic. This rate cannot precisely describe whether the condition was well-treated or not, since fluoroquinolones may be prescribed due to their vast availability on the market or to misdiagnosis of the condition. On the other hand, it can reflect a correct choice of antibiotic since fosfomycin and nitrofurantoin were out of stock and difficult to acquire by community pharmacies during the time of data collection, pivmecillinam is not available in Lebanon and TMP/SMX’s resistance rate in Lebanon is higher than 20%. Cefixime is not recommended by any of the reference guidelines which recommend cephalexin, cefaclor, cefdinir or cefpodoxime.17 The use of cefixime, considering that the recommended cephalosporins are available in the Lebanese market, reflects troubling prescribing practices and raises questions about the determinants of the choice of the antibiotic.
The global conformity to all three criteria (choice, dose and duration) was as low as 3.8%, which reflects an issue of obvious antibiotic misuse with the low conformity rates of dose and of duration. This misuse of antibiotics, including bypassing standard acceptable dosage limits, is a great contributor to microbial resistance and increased morbidity.27 It can also lead to serious adverse effects including skin problems, hypersensitivity and others (28). We suspect that the participants recommended the dose and duration of the antibiotic based on the number of tablets in the antibiotic box. Thus, the recommendation of ‘finishing the full course of antibiotic’ was translated into finishing the full ‘box’ of antibiotic in practice, leading to antibiotic overdosing.
The participants were mainly interested in questioning about the age of the patient. If the patient was of extreme age, child or older adult, we suspect that they might have not been this assured to prescribe antibiotics. Only a few participants inquired about using other drugs, having allergies or being pregnant which would minimize the risk of side effects. The latter is especially alarming considering that fluoroquinolones are pregnancy category C and can only be prescribed after weighing the risks versus the benefits due to the difficult extrapolation of the animal toxicity and mutagenicity to humans.29 We believe that the participants did not ask clinically important questions, due to the lack of knowledge and underestimation of the adverse events of antibiotics. Also, due to the lack of time to properly evaluate the patient case. Another reason is the assumption that patients would alert them (or voluntarily announce) if they were pregnant or have allergies. A study in Spain showed similar results for asking about allergies and possible pregnancy while prescribing antibiotics. Pharmacists did not ask about allergies in 73.9% of cases and never asked about possible pregnancy.30 Similarly, in India, none of the participants queried about potential drug allergies.31
The referral of the case to a physician was only 15.2%. This is very low considering that acute uncomplicated cystitis is an infection that needs a physician’s evaluation to prescribe an appropriate antibiotic regimen and that might get complicated if left untreated or treated inappropriately.32 A study done in Spain reported that pharmacists prefer to diagnose and treat the patients rather than referring them to physicians, especially that they underestimate the physician’s qualifications and overestimate their own knowledge.33 This raises questions about what cases the pharmacists and assistants consider themselves to be incapable of managing in which they need to refer the patient to a physician. In addition, the rate of suggesting a urine test was low considering that a urine dipstick confirms the diagnosis of cystitis. Thus, resulted in the assumption of cystitis, rather than in an evidence-based diagnosis. This was reflected by the unspecified ‘UTI’ diagnosis and misdiagnosis. The participants may not have suggested a urine test in order not to lose a “client” that would buy the antibiotic recommended. In addition, the counseling of the participants mostly targeted the expected action of the medication and did not include possible side effects, interactions or what to do in case of a missed dose which consequences may range between minor and life-threatening. The lack of counseling might be attributed to the lack of knowledge and/or time of the participants. Neither of which should be reasons to not counsel patients, especially that counseling on drug utilization is one of the major responsibilities of pharmacists.
In studying the association between the participants’ practice and socio-demographic characteristics, it was evident that male participants had a higher antibiotic prescribing rate than female participants did. The differences in antibiotic prescribing rate between genders cannot be explained by the number of questions asked, even if female participants asked more questions (and prescribed less) than male participants did. A reason for the higher number of questions might be the one that is reflected in a study that assesses the knowledge of Lebanese pharmacists towards antibiotic prescribing in the pediatric population, where female pharmacists had a significantly higher knowledge index compared to male pharmacists.34 According to Safaeian et al. findings, which may be applicable here, there are unclear reasons why differences in the treatment approaches exist between male and female physicians.35 In addition, not all encounters were with a pharmacist. Pharmacists and assistants had similar responses reflected in the similar diagnosis, counseling, referral, antibiotic prescribing and conformity rates. The assistants assessed a patient case, provided clinical recommendations, and prescribed antibiotics. This shows dangerous practices occurring in the Lebanese community, where under-qualified personnel can exercise clinical judgement to treat a patient. This can be attributed to the absence of pharmacists in the community pharmacy, the freedom of practice given to the assistants by the pharmacists and the lack of law enforcement that prohibits such practices.
Some of the strengths of this study is that we used the simulated patient method which allowed us to objectively determine the true antibiotic prescribing rate in community pharmacies. It also allowed us to identify the different practices for participants of various sociodemographic characteristics. In addition, we took a sample using appropriate random sampling methods that represents the community pharmacies across all the provinces of Lebanon. Moreover, the case scenario written was based on the case scenario of similar studies, which was derived from the definition, symptoms, and risk factors of acute uncomplicated cystitis. Finally, in order to eliminate heterogeneity and minimize the recall bias, two investigators collected the data with the same investigator presenting the case and the other one observing.
A limitation of the study is the absence of published national treatment guidelines of uncomplicated cystitis at the time of data collection and analyses, which may have created some underestimation of the conformity although the newly published Lebanese guidelines are very similar to the international ones.36 Another limitation is the unavailability or difficulty of obtaining the first line antibiotics (fosfomycin and nitrofurantoin) in the Lebanese market, which may have resulted in bias in the choice of antibiotic. Furthermore, it was not possible to verify the sincerity of the participants when stating whether they are pharmacists or assistants, nor was it possible to study the socio-demographic characteristics (age, education, position, experience) of the participants.
CONCLUSIONS
The irrational use of antibiotics remains a major health problem for the entire public. The high rate of antibiotic prescribing is alarming, especially that only few antibiotics prescribed conform to guidelines. The practices documented should urge the concerned legislative authorities to enforce the laws for ensuring the presence of a pharmacist in each community pharmacy and the prohibition of unauthorized antibiotic dispensing. In addition, the Ministry of Public Health should raise awareness on the accessibility of physician care in much lower costs in primary healthcare centers and dispensaries situated across Lebanon. In addition, national guidelines for the treatment of UTIs should be generalized and communicated with all healthcare professionals in order to optimize patient treatment. Finally, healthcare professionals and the public should be alerted about the proper use of antibiotics, whether it is prescribing, dispensing, counseling or using. This could be done with the organization of education programs, workshops, seminars and awareness campaigns. In conclusion, definitive measures should be undertaken in order to tackle the misuse of antibiotics in Lebanese community pharmacies.
ACKNOWLEDGEMENTS
No assistance in the preparation of this article is to be declared. We acknowledge the Lebanese community pharmacists.
Footnotes
CONFLICT OF INTEREST
No potential conflict of interest was reported by the authors.
FUNDING
This research did not receive any specific grant from funding or sponsorship.
Contributor Information
Sally G. Yaacoub, Faculty of Public Health, Lebanese University. Fanar (Lebanon). sally.yaacoub@gmail.com.
Valerie Koyess, Faculty of Public Health, Lebanese University. Fanar (Lebanon). valerienkoyess@gmail.com.
Nathalie Lahoud, Clinical Epidemiology and Toxicology, National Institute of Public Health (INSPECT-LB); & Faculty of Pharmacy, Lebanese University. Hadat (Lebanon). nathalie.lahoud@hotmail.com.
Deema Rahme, Department of Pharmacy Practice, Faculty of Pharmacy, Beirut Arab University. Beirut (Lebanon). deemarahme@yahoo.com.
Nicole Francis, Faculty of Public Health, Lebanese University. Fanar (Lebanon). nicole.francis@lau.edu.
Nadine Saleh, Clinical Epidemiology and Toxicology, National Institute of Public Health (INSPECT-LB); & Faculty of Pharmacy, Lebanese University. Hadat (Lebanon). nadeensh@gmail.com.
Patrick Maison, Paris-Est Health-Work Institute (IST-PE), Créteil Intercommunal Hospital Center (CHIC). Créteil (France). patrick.maison@ansm.sante.fr.
References
- 1.IDSA. [[cited 2019 Oct 1], (accessed Oct 1, 2019];Uncomplicated Cystitis and Pyelonephritis (UTI) [Internet] Available at: http://www.idsociety.org/Guidelines/Patient_Care/IDSA_Practice_Guidelines/Infections_by_Organ_System/Genitourinary/Uncomplicated_Cystitis_and_Pyelonephritis_(UTI)/
- 2.Khawcharoenporn T, Vasoo S, Singh K. Urinary tract infections due to multidrug-resistant enterobacteriaceae:prevalence and risk factors in a Chicago emergency department. Emerg Med Int. 2013;2013:258517. doi: 10.1155/2013/258517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Picozzi SCM, Casellato S, Rossini M, Paola G, Tejada M, Costa E, Carmignani L. Extended-spectrum beta-lactamase-positive Escherichia coli causing complicated upper urinary tract infection:Urologist should act in time. Urol Ann. 2014;6(2):107–112. doi: 10.4103/0974-7796.130536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO. [accessed Apr 12, 2019];Antibiotic resistance. Available at: http://www.who.int/mediacentre/factsheets/antibiotic-resistance/en/
- 5.Aminov RI, Mackie RI. Evolution and ecology of antibiotic resistance genes. FEMS Microbiol Lett. 2007;271(2):147–161. doi: 10.1111/j.1574-6968.2007.00757.x. [DOI] [PubMed] [Google Scholar]
- 6.Freire-Moran L, Aronsson B, Manz C, Gyssens IC, So AD, Monnet DL, Cars O ECDC-EMA Working Group. Critical shortage of new antibiotics in development against multidrug-resistant bacteria-Time to react is now. Drug Resist Updat. 2011;14(2):118–124. doi: 10.1016/j.drup.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 7.WHO. [accessed Apr 12, 2019];WHO's first global report on antibiotic resistance reveals serious, worldwide threat to public health. WHO. Available at: http://www.who.int/mediacentre/news/releases/2014/amr-report/en/
- 8.The antibiotic alarm. Nature. 2013;495(7440):141. doi: 10.1038/495141a. [DOI] [PubMed] [Google Scholar]
- 9.Al-Azzam SI, Al-Husein BA, Alzoubi F, Masadeh MM, Al-Horani MAS. Self-medication with antibiotics in Jordanian population. Int J Occup Med Environ Health. 2007;20(4):373–380. doi: 10.2478/v10001-007-0038-9. [DOI] [PubMed] [Google Scholar]
- 10.Ventola CL. The antibiotic resistance crisis:part 1:causes and threats. P T. 2015;40(4):277–283. [PMC free article] [PubMed] [Google Scholar]
- 11. [accessed Apr 12, 2019];Get Smart About Antibiotics |Print Materials for Everyone |CDC. Available at: https://www.cdc.gov/getsmart/community/materials-references/print-materials/everyone/index.html .
- 12.Bin Abdulhak AA, Altannir MA, Almansor MA, Almohaya MS, Onazi AS, Marei MA, Aldossary OF, Obeidat SA, Obeidat MA, Riaz MS, Tleyjeh IM. Non prescribed sale of antibiotics in Riyadh, Saudi Arabia:a cross sectional study. BMC Public Health. 2011;11:538. doi: 10.1186/1471-2458-11-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Almaaytah A, Mukattash TL, Hajaj J. Dispensing of non-prescribed antibiotics in Jordan. Patient Prefer Adherence. 2015;9:1389–1395. doi: 10.2147/PPA.S91649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Llor C, Cots JM. The sale of antibiotics without prescription in pharmacies in Catalonia, Spain. Clin Infect Dis. 2009;48(10):1345–1349. doi: 10.1086/598183. [DOI] [PubMed] [Google Scholar]
- 15.Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, Moran GJ, Nicolle LE, Raz R, Schaeffer AJ, Soper DE Infectious Diseases Society of America;European Society for Microbiology and Infectious Diseases. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women:A 2010 Update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011;52(5):e103–e120. doi: 10.1093/cid/ciq257. [DOI] [PubMed] [Google Scholar]
- 16.Grabe M. Guidelines on Urological Infections [Internet] [accessed Oct 1, 2019];European Association of Urology. 2015 Available at: http://uroweb.org/wp-content/uploads/19-Urological-infections_LR2.pdf .
- 17. [accessed Feb 7, 2019];Diagnosis and Treatment of Acute Uncomplicated Cystitis - American Family Physician. Available at: http://www.aafp.org/afp/2011/1001/p771.html . [PubMed]
- 18.Yaacoub SG, Lahoud NA, Francis NJ, Rahme DW, Murr TH, Maison PF, Saleh NG. Antibiotic Prescribing Rate in Lebanese Community Pharmacies:A Nationwide Patient-Simulated Study of Acute Bacterial Rhinosinusitis. J Epidemiol Glob Health. 2019;9(1):44–49. doi: 10.2991/jegh.k.190305.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Farah R, Lahoud N, Salameh P, Saleh N. Antibiotic dispensation by Lebanese pharmacists:a comparison of higher and lower socio-economic levels. J Infect Public Health. 2015;8(1):37–46. doi: 10.1016/j.jiph.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Nyazema N, Viberg N, Khoza S, Vyas S, Kumaranayake L, Tomson G, Lundborg CS. Low sale of antibiotics without prescription:a cross-sectional study in Zimbabwean private pharmacies. J Antimicrob Chemother. 2007;59(4):718–726. doi: 10.1093/jac/dkm013. [DOI] [PubMed] [Google Scholar]
- 21.Cheaito L, Azizi S, Saleh N, Salameh P. Assessment of self-medication in population buying antibiotics in pharmacies:a pilot study from Beirut and its suburbs. Int J Public Health. 2014;59(2):319–327. doi: 10.1007/s00038-013-0493-y. [DOI] [PubMed] [Google Scholar]
- 22.Al-Ghamdi MS. Empirical treatment of uncomplicated urinary tract infection by community pharmacist in the Eastern province of Saudi Arabia. Saudi Med J. 2001;22(12):1105–1108. [PubMed] [Google Scholar]
- 23.Almaaytah A, Mukattash TL, Hajaj J. Dispensing of non-prescribed antibiotics in Jordan. Patient Prefer Adherence. 2015;9:1389–1395. doi: 10.2147/PPA.S91649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aponte-González J, González-Acuña A, Lopez J, Brown P, Eslava-Schmalbach J. Perceptions in the community about the use of antibiotics without a prescription:Exploring ideas behind this practice. Pharm Pract (Granada) 2019;17(1):1394. doi: 10.18549/PharmPract.2019.1.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rossignol L, Pelat C, Lambert B, Flahault A, Chartier-Kastler E, Hanslik T. A method to assess seasonality of urinary tract infections based on medication sales and google trends. PLoS One. 2013;8(10):e76020. doi: 10.1371/journal.pone.0076020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bahnassi A. Pharmacists Views and Practices in Regard to Sales of Antibiotics Without a Prescription in Madinah, Saudi Arabia. J Patient Saf. 2016;12(3):159–164. doi: 10.1097/PTS.0000000000000087. [DOI] [PubMed] [Google Scholar]
- 27.Michael CA, Dominey-Howes D, Labbate M. The antimicrobial resistance crisis:causes, consequences, and management. Front Public Health. 2014;2:145. doi: 10.3389/fpubh.2014.00145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bennadi D. Self-medication:A current challenge. J Basic Clin Pharm. 2013;5(1):19–23. doi: 10.4103/0976-0105.128253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sádel Fiol F, Gerenutti M, Groppo FC. Antibiotics and pregnancy. Pharmazie. 2005;60(7):483–493. [PubMed] [Google Scholar]
- 30.Guinovart MC, Figueras A, Llor C. Selling antimicrobials without prescription –Far beyond an administrative problem. Enferm Infecc Microbiol Clin. 2018;36(5):290–292. doi: 10.1016/j.eimc.2016.10.006. [DOI] [PubMed] [Google Scholar]
- 31.Shet A, Sundaresan S, Forsberg BC. Pharmacy-based dispensing of antimicrobial agents without prescription in India:appropriateness and cost burden in the private sector. Antimicrob Resist Infect Control. 2015;4:55. doi: 10.1186/s13756-015-0098-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. [accessed Apr 12, 2019];Acute uncomplicated cystitis in women - UpToDate. Available at: https://www.uptodate.com/contents/acute-uncomplicated-cystitis-in-women .
- 33.Caamaño F, Tomé-Otero M, Takkouche B, Gestal-Otero JJ. Influence of pharmacists'opinions on their dispensing medicines without requirement of a doctor's prescription. Gac Sanit. 2005;19(1):9–14. doi: 10.1157/13071811. [DOI] [PubMed] [Google Scholar]
- 34.Zahreddine L, Hallit S, Shakaroun S, Al-Hajje A, Awada S, Lahoud N. Knowledge of pharmacists and parents towards antibiotic use in pediatrics:a cross-sectional study in Lebanon. Pharm Pract (Granada) 2018;16(3):1194. doi: 10.18549/PharmPract.2018.03.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Safaeian L, Mahdanian AR, Salami S, Pakmehr F, Mansourian M. Seasonality and Physician-related Factors Associated with Antibiotic Prescribing:A Cross-sectional Study in Isfahan, Iran. Int J Prev Med. 2015;6:1. doi: 10.4103/2008-7802.151431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. [accessed Apr 12, 2019];The Lebanese Society of Infectious Diseases and Clinical Microbiology Guidelines for the treatment of urinary tract infections –JML / LM. Available at: http://www.lebanesemedicaljournal.org/lmj/2017/12/23/the-lebanese-society-of-infectious-diseases-and-clinical-microbiology-guidelines-for-the-treatment-of-urinary-tract-infections/


