Abstract
Background
over 50% of older people in hospital are prescribed a pre-admission medicine that is potentially inappropriate; however, deprescribing by geriatricians and pharmacists is limited. This study aimed to characterise geriatricians’ and pharmacists’ barriers and enablers to deprescribing in hospital. It also intended to develop a framework of intervention components to facilitate implementation of hospital deprescribing.
Methods
fifty-four geriatricians and pharmacists representing four UK hospitals attended eight focus groups. We designed a topic guide to invite discussions about barriers and enablers to deprescribing. After thematic analysis, themes were mapped to the theoretical domains framework (TDF), enabling prioritisation of domains for behaviour change. We then identified evidence-based intervention components for changing behaviour within prioritised TDF domains.
Results
geriatricians and pharmacists described several deprescribing enablers in the hospital setting including alignment with their role and generalist knowledge, and routine patient monitoring. Five prioritised TDF domains represent the key barriers and enabler: patient and caregiver attachment to medication (social influence); perceptions that deprescribing is riskier than continuing to prescribe (beliefs about consequences); pharmacists’ working patterns limiting capacity to support deprescribing (environmental context and resources); deprescribing being a low hospital priority (goals) and incentives to deprescribe (reinforcement). Prioritised TDF domains aligned with 44 evidence-based intervention components to address the barriers and enabler to hospital deprescribing.
Conclusion
the behavioural determinants and their associated intervention components provide a hospital deprescribing implementation framework (hDIF). Intervention components should be selected from the hDIF to provide a theory and evidence-based intervention tailored to hospital contexts.
Keywords: inappropriate medication, deprescriptions, behaviour change, secondary care, qualitative, older people
Key points
Barriers and enablers to deprescribing are context-specific; interventions targeting deprescribing behaviour should reflect this.
This study provides a hospital deprescribing implementation framework of 44 intervention components.
Intervention components may be selected from the implementation framework according to individual hospital contexts.
Background
Over 50% of older people in hospital are prescribed a pre-admission medicine that is potentially inappropriate, predisposing them to adverse outcomes including morbidity, rehospitalisation and mortality [1]. This has led to calls for deprescribing of potentially inappropriate medicines (PIMs) in hospital [2]. A 2018 evaluation of hospital deprescribing reported only 4% of patients had a pre-admission medicine deprescribed [3], suggesting a need to change practitioner behaviour to facilitate routine deprescribing in hospital.
An understanding of whose behaviour needs changing and their barriers and enablers to this behaviour is key to behaviour change [4]. Primary care barriers to deprescribing include limited skills and knowledge to deprescribe and perceived resistance of patients and carers [5]. Emerging guidelines regarding when and how to deprescribe medicine groups may address knowledge and skill barriers [6–9]. Theory-informed interventions to encourage patient participation in deprescribing may address the barrier of their resistance [10]. Access to geriatricians and pharmacists working in hospitals is a primary care enabler to deprescribing [5].
Geriatricians and pharmacists may be the most appropriate practitioners to deprescribe in hospitals; however, their barriers and enablers to deprescribing are yet to be fully understood [5]. This may explain the failure of hospital deprescribing interventions to achieve clinically significant reductions in PIMs [11]. Some primary care barriers and enablers may be relevant to geriatricians and pharmacists in hospital [5]. However, others that are specific to the hospital context may remain unknown and also vary between hospitals [12].
The importance of applying theory to understand the processes of behaviour change is widely recognised [13]. The theoretical domains framework (TDF) is an integrative framework of behaviour change theories for developing interventions [14]. It comprises 14 domains representing determinants of behaviour, for example the “Knowledge” domain refers to “an awareness of the existence of something” and “Environmental context and resources” refers to “circumstance of a person’s situation or environment that discourages or encourages the desired behaviour” [14]. Identifying the important domains for the target behaviour provides the theoretical understanding required to develop an intervention [14]. The 14 TDF domains are linked to a taxonomy of behaviour change techniques (BCTs) [15], which are the “building blocks” of behaviour change interventions. The TDF has been applied extensively to develop interventions targeting practitioners’ behaviours including promoting uptake of a screening tool in geriatric oncology [16].
In the present qualitative study, we used the TDF to understand geriatricians’ and pharmacists’ barriers and enablers to deprescribing in hospital. We explored whether these barriers and enablers differed between hospital contexts. Additionally, for the TDF domains identified as important for deprescribing, we identified relevant BCTs for selecting to develop a theory and evidence-based hospital deprescribing intervention for older people.
Methods
Ethical approval
Ethical and governance approvals were obtained from the Faculty of Medicine and Health Sciences Research Ethics Committee, University of East Anglia (Reference: 2017/2018—59) and the United Kingdom Health Research Authority (IRAS project ID: 231262), respectively.
Design
We adopted an exploratory qualitative approach to understand the barriers and enablers to deprescribing experienced and perceived by geriatricians and pharmacists. We selected a focus group study design and employed thematic analysis to explore barriers and enablers inductively. We used the TDF as a framework to identify BCTs to address barriers and enablers [4]. We used the consolidated criteria for reporting qualitative research checklist to guide reporting (Appendix 1, Supplementary data are available in Age and Ageing online).
Setting
We selected four hospitals across three English counties, two of which were 1,000 and 1,200 bed teaching hospitals with four and six geriatric wards, respectively, and two were 450 and 550 bed district general hospitals each with three geriatric wards. These were used to explore barriers and enablers of deprescribing for older people and capture any variation arising from differing resources and patient populations associated with these different sample settings.
Sample
We included senior geriatricians and pharmacists from the four hospitals based on practice experience (minimum 6 and 4 years respectively). We invited pharmacists from all clinical specialities in recognition of the range of responsibilities often adopted despite speciality.
We planned eight focus groups to explore similarities and differences in attitudes between geriatricians and pharmacists, and identify hospital characteristics that might influence deprescribing. Each hospital site hosted two focus groups: one with geriatricians and one with pharmacists, with five to eight participants each (n = 40 to 64 in total).
We followed the principles for deciding saturation in theory-based qualitative studies outlined by Francis et al. [17]. However, as a study objective was to explore any differences between district general and teaching hospital contexts, an a priori decision was made to convene all eight planned focus groups irrespective of whether data saturation was achieved.
Recruitment
We invited all eligible potential participants by email via a gatekeeper. The email comprised an information leaflet (including study aims) and focus group scheduling arrangements. Potential participants completed an online expression of interest survey requesting: professional group, gender, hospital seniority grade and prescribing authority status (pharmacists only). We purposively sampled potential participants to maximise variation in demographics. We sought a mixture of prescribing and non-prescribing pharmacists to explore differences in attitudes arising from the acquisition of additional prescribing competencies. We remunerated employing hospitals for participants’ time commitment to the research.
Data collection
Researchers, geriatricians, pharmacists and patient and caregiver representatives developed a semi-structured topic guide (Appendix 2, Supplementary data are available in Age and Ageing online) informed by the deprescribing literature. Guiding questions were designed to elicit views regarding the following:
Perception of existing deprescribing practice
Barriers to increasing deprescribing practice
Enablers of increasing deprescribing practice
We adapted standard questions to elicit barriers and enablers to deprescribing within all 14 TDF domains and used them as probes to ensure full coverage of the TDF in discussions. We piloted the topic guide with geriatrician and pharmacist collaborators (n = 3) who were representative of the target focus group population; they did not participate in the study. The purpose of the piloting was to check understanding of questions, ascertain the depth of data generated from the guide and assess the feasibility of covering all TDF domains in the allotted time.
We collected focus group data between February and May 2018. We obtained consent at the beginning of each focus group and convened them in meeting rooms at the hospitals. Two academic pharmacist researchers (SS and DB) facilitated, made field notes during the discussions and audio recorded the events. SS completed training in qualitative research methodology and the principles and practice of behaviour change research prior to the study. DB has extensive experience of conducting qualitative research underpinned by behaviour change theory.
Analysis
A research administrator transcribed verbatim focus group recordings that were then anonymised and checked for accuracy by a researcher (SS). We imported data into NVivo 11 (QSR International, Melbourne, Australia) to facilitate the following three phases of analysis: (i) thematic analysis to identify determinants of deprescribing in hospital, (ii) mapping of all identified determinants of deprescribing to the TDF and (iii) prioritising TDF domains for targeting in a deprescribing intervention and identify the BCTs linked to these domains. We shared all processes of the analysis with the study management group, which included geriatricians, clinical pharmacists and patient and caregiver representatives, to enhance transparency and validity of interpretation.
Phase 1: thematic analysis
We initially analysed data through the customary steps of thematic analysis to ensure resultant themes were not restricted to the pre-defined TDF domains [18]. After data familiarisation (step 1), SS coded inductively for barriers and enablers to deprescribing (step 2). Two researchers experienced in qualitative (MJT) and behaviour change (DB) research reviewed codes and refined through discussion. Three researchers (SS, MJT and DB) then categorised the inductive coding and subsequent themes were extracted, reviewed and defined (steps 3–5). Inductive coding and thematic analysis were undertaken concurrently after each focus group. Geriatrician and pharmacist transcripts were initially coded separately and grouped into categories as appropriate. Categories for both professional groups were then combined to form overarching themes. At all times of data abstraction, constant referral back to transcripts, hospital contexts and codes was undertaken to unsure that the analysis remained true to, and reflected appropriately, the developing themes.
We considered emergent themes in the context of the existing literature; we comprehensively reported and described themes representing novel concepts and briefly described any themes overlapping with the literature [5].
Phase 2: mapping of all determinants of deprescribing to the TDF
SS and DB re-read the transcripts and mapped inductive codes from phase 1 to the relevant TDF domain(s). We used the TDF domain definitions to guide this mapping and organised coded data within each domain into barriers and enablers to deprescribing [14]. We compared our mapping and resolved any disagreements through discussion and referral to a third researcher experienced in health psychology and qualitative research (JT).
Phase 3: prioritising TDF domains for targeting in a deprescribing intervention and identifying the BCTs linked to these domains
The phase 1 thematic analysis provided a contextualised understanding of the barriers and enablers most important to participants for effecting deprescribing behaviour change. We used this information to prioritise the TDF domains most relevant for a deprescribing intervention. We identified the relevant domains through consensus discussion between three researchers (SS, MJT and DB) and confirmed by a health psychologist (JT).
For each theme, we collated all barriers and enablers expressed by the collective as exerting a strong impact on deprescribing behaviour and no significant conflicting views. We prioritised the mapped domain for each of the barriers. For the enablers, if participants expressed that a change in the status quo was required, then we prioritised whilst those enablers already present by virtue of implementing the intervention in the hospital setting were not prioritised.
For each of the prioritised TDF domains, we identified all potentially effective BCTs for developing a deprescribing intervention for older people in hospital. We used the mapping table developed by Cane et al. [15], which links BCTs to TDF domains to inform this process.
Results
Sample
All geriatricians and pharmacists who were purposively sampled participated in the focus groups. Fifty-four participants; 28 geriatricians and 26 pharmacists, participated across the eight focus groups. Table 1 provides participant characteristics. The mean (standard deviation) focus group duration was 55 (5) minutes.
Table 1.
Focus group participant characteristics
| Hospital | Professional group | Number of participants | Number with prescribing authority |
|---|---|---|---|
| Hospital 1a | Pharmacists | 8 (4 female 4 male) | 3 |
| Hospital 1a | Geriatricians | 7 (5 female 2 male) | 7 |
| Hospital 2a | Pharmacists | 7 (7 female) | 1 |
| Hospital 2a | Geriatricians | 8 (3 female 5 male) | 8 |
| Hospital 3b | Pharmacists | 6 (3 female 3 male) | 1 |
| Hospital 3b | Geriatricians | 7 (4 female 3 male) | 7 |
| Hospital 4b | Pharmacists | 5 (2 female 3 male) | 1 |
| Hospital 4b | Geriatricians | 6 (1 female 5 male) | 6 |
aTeaching hospital.
bDistrict general hospital.
Phase 1: thematic analysis
We identified four themes: (i) role of different professionals; (ii) the inpatient environment; (iii) consideration of outcomes and (iv) attitudes towards medicines. Themes were recurring after the third focus group and no new themes emerged after the sixth focus group.
In accordance with the planned analysis, themes 1 and 2 represented novel concepts and are therefore comprehensively reported with illustrative quotations for contextualisation provided. Themes 3 and 4 are briefly described because they overlap extensively with the existing primary care literature, therefore only divergences are highlighted. There were no discernible differences between participants from teaching and district general hospitals or prescribing and non-prescribing pharmacists.
Role of different professionals
There was high motivation to increase deprescribing in hospital; geriatricians and pharmacists recognised that existing practice was limited and reactive to harms, rather than proactive to avoid harms.
“I think we do a lot more reactive deprescribing probably and a lot less proactive deprescribing than we should.” (Pharmacist 2, Hospital 2)
Both professional groups acknowledged that increasing deprescribing aligned with the generalist nature of their respective roles and responsibilities. However, the role of practitioners with a restricted focus, such as therapeutic area specialists (e.g. cardiology, infectious diseases and surgery), was described as potentially incompatible with deprescribing for older people.
Participants indicated that junior healthcare practitioners, including junior geriatricians and pharmacists, lacked the required competencies to lead deprescribing. This was a recognised consequence of insufficient trainee healthcare practitioner experience and limited education regarding deprescribing within training programmes.
Whilst the scope for several professional groups working in hospital to contribute to deprescribing was recognised, there was consensus that overall responsibility should rest with one professional group. There was agreement across the focus groups that geriatricians should assume this overall responsibility. Furthermore, in the geriatrician focus groups, many participants expressed confidence in their ability to weigh up the risks and benefits of deprescribing PIMs to inform decision-making. For geriatricians therefore, the main barriers to deprescribing were environmental and resource factors.
“It’s interesting how all of the barriers to deprescribing are practical rather than I just don’t know whether I should stop it. So we’re extremely confident in our ability to decide this is why this is what we should do.” (Geriatrician 5, Hospital 2)
Pharmacists suggested that their skill set aligns with identifying PIMs and advising on deprescribing, which was also endorsed by geriatricians. Pharmacists were reluctant to assume overall responsibility for deprescribing because of an expressed lack of confidence in decision-making.
“And then it’s just the difficulty of clinical relevance of these medications and the context of the patient that maybe pharmacists wouldn’t be happy with. It would have to be somebody who’s feeling happy enough to do it.” (Pharmacist 2, Hospital 3)
However, existing working patterns and priorities in hospital were reported to limit pharmacists’ capacity to assume any substantial role in deprescribing and was a significant barrier to them supporting deprescribing in hospital.
“The time that we have on the ward as pharmacists is for discharges, missed doses if you can do a medication reconciliation great and that’s about it. The actual clinical review of medicines is squeezed.” (Pharmacist 5, Hospital 4)
The inpatient environment
The patient’s clinical picture, communication and access to resources were perceived influencers of deprescribing. Both geriatricians and pharmacists acknowledged that there was scope to increase deprescribing in hospital. This was complemented by the necessary resources and capacity available in hospital to safely trial deprescribing and monitor patients.
“If they’re in hospital they can be monitored more closely when you do stop the riskier medication and if they’re in for a length of time … then there’s the time to stop medication.” (Pharmacist 5, Hospital 3)
Challenges to deprescribing in the hospital setting were also acknowledged. Limited information available to hospital practitioners regarding patients’ medications was raised as a barrier. Strength, dose and formulation of pre-admission medications were routinely ascertained by pharmacists by discussing with patients and accessing electronic medication records. However, key information required to determine whether deprescribing is appropriate, such as the reason why the medication was prescribed and for how long, were reportedly rarely known.
“You don’t always have all the information in hospital... it’s very difficult to make that decision. There’s always the risk you might end up stopping something they really do need. And it might not be obvious that they really do need it from the information you’ve got in front of you.” (Pharmacist 7, Hospital 1)
A further barrier to deprescribing was the acute nature of a hospital admission requiring prioritisation of the patient’s problems for immediate action. This was confounded by the patient’s artificial lifestyle whilst in hospital, including immobility, scheduled meals and medications being managed by healthcare practitioners. These factors were perceived to distort the assessments undertaken in hospital to inform long-term deprescribing decisions.
“Things might change so dramatically when they leave hospital, either they’ve recovered from their sepsis and they need their antihypertensives or they’ve started eating again and they need more of their gliclazide.” (Geriatrician 5, Hospital 2)
Participants asserted a clear need to establish a safety net through sharing information with primary care providers responsible for ongoing care after patients are discharged from hospital. It was suggested that such correspondence could include directions for monitoring for changes that may indicate re-prescribing was necessary. However, participants agreed that the existing transfer of information between care settings was poor and may undermine deprescribing efforts.
“I think we’re very bad at relaying changes to the GPs [primary care practitioners]. I get a lot of letters from GPs saying this person was discharged and you stopped this list of medications and then you look at the discharge letter and there’s no reason why, or sometimes it doesn’t mention it was stopped at all.” (Geriatrician 5, Hospital 4)
Similarly, pharmacist participants voiced concerns regarding communicating medication changes with patients in hospital. Barriers identified included patients being unable to participate in decision-making because of ill health and deprescribing being regarded by patients as a low priority relative to the acute condition responsible for the admission. However, the availability of carers as both sources of medication information and participants in decision-making were facilitators.
Participants expressed disappointment about not receiving feedback on positive outcomes resulting from hospital-initiated deprescribing once patients were discharged. Both professional groups recognised the successes of schemes to incentivise changes in antimicrobial prescribing practice in the UK hospital setting. This led to suggestions that similar approaches may also be enablers of deprescribing.
Consideration of outcomes
The perceived risks and potential benefits of deprescribing versus continuing to prescribe were identified as key influencers of deprescribing behaviour. Potential patient orientated positive outcomes were a reduction in medication burden and incidence of adverse drug events, leading to improved quality of life. A reduction in unnecessary medication expenditure, reduced treatment costs associated with adverse drug events and rationalising use of health resources were proposed healthcare system benefits. In turn, patient and health system benefits were perceived to result in individual practitioner benefits, with geriatricians and pharmacists suggesting that deprescribing may lead to reduced workloads.
There was divergence in views between geriatrician and pharmacist participants regarding whether deprescribing was perceived to carry greater risk than continuing to prescribe. Pharmacist participants felt that on balance, passively continuing to prescribe a medicine in the absence of immediate harm was safer than proactively deprescribing. Conversely, geriatricians felt that both deprescribing and continuing to prescribe were active decisions, with no inherent differences in risk providing both are carefully considered.
Attitudes towards medicines
Geriatricians and pharmacists described patients’, families’, other healthcare practitioners’ and wider societies’ attitudes towards medicines as influencers on their own deprescribing behaviour. Patient and carer attachment to medication was described as a difficult barrier to overcome. However, both professional groups acknowledged that a significant proportion of older people dislike taking medication and are therefore likely to be amenable to deprescribing.
Healthcare culture’s attitude towards medication use was acknowledged as changing in favour of deprescribing, with the burden of inappropriate medication use now increasingly recognised. Nevertheless, participants felt that this attitude was not reflected in treatment guidelines, which were described as overemphasising prescribing medication without considering opportunities for deprescribing.
Phase 2: mapping of all determinants of deprescribing to the TDF
All of the inductive codes from the four themes, organised into the nine mapped TDF domains, according to whether they were barriers or enablers to deprescribing (i.e. influencers of deprescribing behaviours) are provided in Appendix 3, Supplementary data are available in Age and Ageing online. Codes in the theme “Attitudes towards medicines” were only mapped to one TDF domain whilst the remaining three themes incorporated multiple domains. A summary of barriers and enablers derived from the inductive codes within each theme, mapped to nine TDF domains, is provided in Table 2.
Table 2.
Summary of barriers and enablers to deprescribing mapped to nine TDF domains
| Barrier | Enabler | TDF domain |
|---|---|---|
| Theme: attitudes towards medicines | ||
| Patient and carer attachment to medicationa,b | Patient dislike of medicationa,b | 6. Social influence |
| Treatment guidelinesa | Primary care respecting hospital decision-makingb | |
| Societal labelling of medicines as “always good”a | Deprescribing awarenessb | |
| Theme: consideration of outcomes | ||
| Adverse outcomes for patients, practitioners and hospitalsa,b | Improved outcomes for patients, practitioners and hospitalsa,b | 10. Beliefs about consequences |
| Continuing to prescribe is less risky than deprescribingb | No difference in risk between prescribing and deprescribinga | |
| Fear of consequences and assuming responsibilitya | 14. Emotion | |
| Theme: role of different healthcare professionals | ||
| Pharmacists lack confidence to make decisionsa,b | Confidence in decision makingb | 8. Beliefs about capabilities |
| Deprescribing education is poora,b | Generalist knowledge and broad experiencea,b | 1. Knowledge |
| Hospitals primary role is acute carea | Role includes deprescribinga,b | 7. Social/professional role and identity |
| Pharmacists’ existing working patternsa,b | Changing working patterns to support deprescribinga,b | 5. Environmental context and resources |
| Theme: the inpatient environment | ||
| Deprescribing is not a hospital’s prioritya,b | Setting deprescribing goalsa,b | 12. Goals |
| Limited feedback on deprescribing outcomesa | Deprescribing incentivea,b | 13. Reinforcement |
| Artificial patient status in hospitala,b | Hospitals are well resourced to deprescribea,b | 5. Environmental context and resources |
| Incomplete medication historya,b | Opportunity to trial deprescribinga,b | |
aGeriatrician expressed barrier or enabler.
bPharmacist expressed barrier or enabler.
Phase 3: prioritising TDF domains for targeting in a deprescribing intervention and identifying the BCTs linked to these domains
Figure 1 provides the hospital deprescribing implementation framework (hDIF) of TDF domains prioritised for targeting in a novel hospital deprescribing intervention for older people. For the prioritised domains, the 44 linked BCTs are listed [15]. The process of selecting from this list of 44 BCTs according to local contexts is also illustrated in Figure 1, and examples are provided for five hypothetically selected BCTs that have been characterised by the research team.
Figure 1.
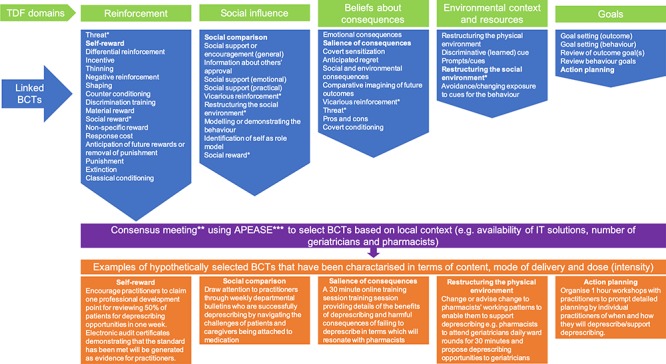
A hospital deprescribing implementation framework (hDIF) of prioritised TDF domains and linked BCT for developing a deprescribing intervention targeting the behaviours of geriatricians and pharmacists according to local hospital contexts. *BCT is linked to multiple prioritised TDF domains. **e.g. Nominal group and Delphi techniques [19]. ***Affordable, practical, effective/cost-effective, acceptable, safe and equitable [20]
“Social professional role and identity” and “Knowledge” are not prioritised because whilst these represented strong enablers, both geriatricians and pharmacists asserted that deprescribing aligns with existing perceptions of their complementary roles and knowledge. Similarly, “Beliefs about capabilities” are not represented because both professions had confidence in their ability to undertake their defined roles. It can be seen that the “Emotion” domain, which was exclusively expressed with barriers by pharmacists being fearful of assuming responsibility for any negative consequences of deprescribing, is not represented. This is in recognition of participants across both professions agreeing that geriatricians should assume overall responsibility for deprescribing in hospital.
The three TDF domains of “Social influence”, “Environmental Context and Resources” and “Goals” represented strong barriers to both geriatricians and pharmacists deprescribing behaviour and therefore are prioritised for targeting. Additionally, for pharmacists, the “Beliefs about consequences” domain is prioritised in recognition of their perception that continuing to prescribe a medication presents less risk than deprescribing.
The “Reinforcement” domain is prioritised because participants expressed a desire for feedback on patient outcomes and an incentive in order to facilitate deprescribing.
Discussion
Key drivers for implementing hospital deprescribing for older people are that both geriatricians and pharmacists perceive it to align with their (Social/professional role and identity). They are also confident in their existing “Knowledge” and “Beliefs about capabilities” to undertake their identified roles. This contrasts the ambivalence and perceived additional training needs of primary care physicians to undertaking this role [5].
A hospital deprescribing intervention for older people led by geriatricians and supported by pharmacists was the preferred configuration. For pharmacists to adopt this supportive role, the “Environmental context and resources” domain needs targeting to facilitate pharmacists’ working patterns aligning with active participation in core clinical team activity [21, 22].
The evidence suggests that deprescribing is widely acceptable to patients and carers [23–25], yet geriatricians and pharmacists believe there to be resistance. An intervention should therefore target “Social influences” to address this misalignment between the evidence and practitioners’ beliefs.
The enablers to deprescribing offered by the inpatient environment such as routine monitoring provide a safe opportunity to trial deprescribing. Pharmacists were still concerned that the risks may outweigh the potential benefits of deprescribing. An intervention should therefore target pharmacists’ “Beliefs about consequences” to recalibrate their perceptions of the relative risks and benefits of deprescribing.
The inpatient environment presented the barrier of prioritising acute problems over deprescribing. Targeting the “Goals” domain to raise the priority of deprescribing in hospital may be an appropriate solution. Encouragingly, participants acknowledged the scope to increase deprescribing in hospital [3]. The proposed enabler of incentivisation mapped to the “Reinforcement” domain may be an appropriate intervention component given that it has previously demonstrated efficacy in influencing hospital antimicrobial prescribing behaviours [26].
Sufficient medication information needs to be available to facilitate deprescribing decision-making, including when and why a medication was originally prescribed [27]. The barrier of incomprehensive medication histories extends across all healthcare settings, prompting calls for routine documentation of indications and an intended duration at initial prescribing [28]. Targeting the “Environmental context and resources” domain through restructuring the environment may ameliorate some of these effects and additionally address the barrier of patients being acutely unwell during periods of the admission. This may take the form of an outpatient clinic, which provides time to both gather medication information and for the patients to recover from their acute illness.
The influencers of whether geriatricians and pharmacists deprescribe in the hospital setting that requires addressing are mapped to 44 BCTs. This provides a theory-informed hospital deprescribing implementation framework (hDIF) for developing an intervention targeting geriatricians’ and pharmacists’ behaviour. Patient focussed interventions such as the EMPOWER educational brochure may complement this approach through encouraging patient engagement in deprescribing [10].
Data triangulation from intra and inter-professional convergence around the key issues was frequently observed, affording confidence in the reliability of findings [29]. The transferability of barriers and enablers between district general and teaching hospitals indicates that the BCTs identified may be applicable to other hospital contexts [30].
Confining the study to the UK hospital population may limit the international transferability of findings, particularly where roles and resource factors differ from this sample. The required specificity when developing behaviour change interventions focussed this study on geriatricians and pharmacists, and therefore the views of other potentially relevant professionals were not captured. This approach could be duplicated in other countries and other professional groups where the deprescribing role is less likely to be assumed by geriatricians and pharmacists.
The deprescribing research agenda should recognise the five TDF domains of “Social influence”, “Beliefs about consequences”, “Environmental context and resources”, “Goals” and “Reinforcement”. The hDIF developed in this study provides a range of BCTs for developing a hospital deprescribing intervention. Future work to select BCTs from the hDIF according to local contexts may be achieved through consensus methods structured according to affordability, practicability, effectiveness/cost-effectiveness, acceptability, side effects/safety and equity [20].
Supplementary Material
Acknowledgements
We thank participating geriatricians, pharmacists and gatekeepers for their contribution to this study. The authors also thank the National Institute for Health Research Clinical Research Network for assisting with recruitment.
Declaration of Conflict of Interest
None.
Declaration of Funding
The research was funded by Pharmacy Research UK (Personal Research Award number: PRUK-2017-PA2-A).
Sponsor’s role
The sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data and preparation, review, or approval of the manuscript.
References
- 1. Gallagher P, Lang PO, Cherubini A et al. . Prevalence of potentially inappropriate prescribing in an acutely ill population of older patients admitted to six European hospitals. Eur J Clin Pharmacol 2011; 67: 1175–88. [DOI] [PubMed] [Google Scholar]
- 2. Avery AJ, Coleman JJ. Tackling potentially inappropriate prescribing. BMJ 2018; 363: k4688. [DOI] [PubMed] [Google Scholar]
- 3. Scott S, Clark A, Farrow C et al. . Deprescribing admission medication at a UK teaching hospital; a report on quantity and nature of activity. Int J Clin Pharmacol 2018. Oct 1; 40: 991–6. [DOI] [PubMed] [Google Scholar]
- 4. Atkins L, Francis J, Islam R et al. . A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci 2017; 12: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Anderson K, Stowasser D, Freeman C, Scott I. Prescriber barriers and enablers to minimising potentially inappropriate medications in adults: a systematic review and thematic synthesis. BMJ Open 2014; 4: e006544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Farrell B, Black C, Thompson W et al. . Deprescribing antihyperglycemic agents in older persons: evidence-based clinical practice guideline. Can Fam Physician 2017; Nov. 1, 63: 832–43. [PMC free article] [PubMed] [Google Scholar]
- 7. Farrell B, Pottie K, Thompson W et al. . Deprescribing proton pump inhibitors: evidence-based clinical practice guideline. Can Fam Physician 2017; 63: 354–64. [PMC free article] [PubMed] [Google Scholar]
- 8. Pottie K, Thompson W, Davies S et al. . Deprescribing benzodiazepine receptor agonists: evidence-based clinical practice guideline. Can Fam Physician 2018; 64: 339–51. [PMC free article] [PubMed] [Google Scholar]
- 9. Bjerre LM, Farrell B, Hogel M et al. . Deprescribing antipsychotics for behavioural and psychological symptoms of dementia and insomnia: evidence-based clinical practice guideline. Can Fam Physician 2018; 64: 17–27. [PMC free article] [PubMed] [Google Scholar]
- 10. Martin P, Tannenbaum C. Use of the EMPOWER brochure to deprescribe sedative-hypnotic drugs in older adults with mild cognitive impairment. BMC Geriatr 2017; 17: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thillainadesan J, Gnjidic D, Green S, Hilmer SN. Impact of deprescribing interventions in older hospitalised patients on prescribing and clinical outcomes: a systematic review of randomised trials. Drugs Aging 2018; 35: 303–19. [DOI] [PubMed] [Google Scholar]
- 12. Papanikolaou PN, Christidi GD, Ioannidis JPA. Patient outcomes with teaching versus nonteaching healthcare: a systematic review. PLoS Med 2006; 3: e341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ 2008; Sep 29; 337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci 2012; 7: 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cane J, Richardson M, Johnston M, Ladha R, Michie S. From lists of behaviour change techniques (BCTs) to structured hierarchies: comparison of two methods of developing a hierarchy of BCTs. Br J Health Psychol 2015; 20: 130–50. [DOI] [PubMed] [Google Scholar]
- 16. Gulasingam P, Haq R, Mascarenhas Johnson A et al. . Using implementation science to promote the use of the G8 screening tool in geriatric oncology. J Am Geriatr Soc 2019. doi: 10.1111/jgs.15920. [DOI] [PubMed] [Google Scholar]
- 17. Francis JJ, Johnston M, Robertson C et al. . What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health 2010; 25: 1229–45. [DOI] [PubMed] [Google Scholar]
- 18. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 19. McMillan SS, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharmacol 2016; 38: 655–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Michie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. 1st edition. Great Britain:Silverback Publishing, 2014. [Google Scholar]
- 21. Béchet C, Pichon R, Giordan A, Bonnabry P. Hospital pharmacists seen through the eyes of physicians: qualitative semi-structured interviews. Int J Clin Pharmacol 2016; 38: 1483–96. [DOI] [PubMed] [Google Scholar]
- 22. Makowsky MJ, Schindel TJ, Rosenthal M, Campbell K, Tsuyuki RT, Madill HM. Collaboration between pharmacists, physicians and nurse practitioners: a qualitative investigation of working relationships in the inpatient medical setting. J Interprof Care 2009; 23: 169–84. [DOI] [PubMed] [Google Scholar]
- 23. Okeowo D, Patterson A, Boyd C, Reeve E, Gnjidic D, Todd A. Clinical practice guidelines for older people with multimorbidity and life-limiting illness: what are the implications for deprescribing? Ther Adv Drug Saf 2018; 9: 619–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Reeve E, Anthony AC, Kouladjian O’Donnell L et al. . Development and pilot testing of the revised patients’ attitudes towards deprescribing questionnaire for people with cognitive impairment. Australas J Ageing 2018; 37: E150–4. [DOI] [PubMed] [Google Scholar]
- 25. Sirois C, Ouellet N, Reeve E. Community-dwelling older people’s attitudes towards deprescribing in Canada. Res Soc Adm Pharm 2017; 13: 864–70. [DOI] [PubMed] [Google Scholar]
- 26. Islam J, Ashiru-Oredope D, Budd E et al. . A national quality incentive scheme to reduce antibiotic overuse in hospitals: evaluation of perceptions and impact. J Antimicrob Chemother 2018; 73: 1708–13. [DOI] [PubMed] [Google Scholar]
- 27. Woodward MC. Deprescribing: achieving better health outcomes for older people through reducing medications. J Pharm Pract Res 2003; 33: 323–8. [Google Scholar]
- 28. Pike H. Deprescribing: the fightback against polypharmacy has begun. Pharm J 2018; 301: 11. [Google Scholar]
- 29. Farmer T, Robinson K, Elliott SJ, Eyles J. Developing and implementing a triangulation protocol for qualitative health research. Qual Health Res 2006; 16: 377–94. [DOI] [PubMed] [Google Scholar]
- 30. Smith B. Generalizability in qualitative research: misunderstandings, opportunities and recommendations for the sport and exercise sciences. Qual Res Sport Exerc Heal 2018; 10: 137–49. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


