Simple behavioral nudges with risk-enhancing education can alter parents’ opioid-disposal beliefs and behaviors.
Abstract
Video Abstract
OBJECTIVES:
Leftover prescription opioids pose risks to children and adolescents, yet many parents keep these medications in the home. Our objective in this study was to determine if providing a behavioral disposal method (ie, Nudge) with or without a Scenario-Tailored Opioid Messaging Program (STOMP) (risk-enhancement education) improves parents’ opioid-disposal behavior after their children’s use.
METHODS:
Parents whose children were prescribed a short course of opioids were recruited and randomly assigned to the Nudge or control groups with or without STOMP. Parents completed surveys at baseline and 7 and 14 days. Main outcomes were (1) prompt disposal (ie, immediate disposal of leftovers after use) and (2) planned retention (intention to keep leftovers).
RESULTS:
There were 517 parents who took part, and 93% had leftovers after use. Prompt disposal behavior was higher for parents who received both the STOMP and Nudge interventions (38.5%), Nudge alone (33.3%), or STOMP alone (31%) compared with controls (19.2%; P ≤ .02). Furthermore, the STOMP intervention independently decreased planned retention rates (5.6% vs 12.5% no STOMP; adjusted odds ratio [aOR] 0.40 [95% confidence interval (CI) 0.19–0.85]). Higher risk perception lowered the odds of planned retention (aOR 0.87 [95% CI 0.79–0.96]), whereas parental past opioid misuse increased those odds (aOR 4.44 [95% CI 1.67–11.79]).
CONCLUSIONS:
Providing a disposal method nudged parents to dispose of their children’s leftover opioids promptly after use, whereas STOMP boosted prompt disposal and reduced planned retention. Such strategies can reduce the presence of risky leftover medications in the home and decrease the risks posed to children and adolescents.
What’s Known on This Subject:
Leftover prescription opioids pose significant risks of morbidity and mortality to children and adolescents, yet many parents keep these and other leftover medications in the home.
What This Study Adds:
In this randomized trial, we showed that providing scenario-tailored risk information improved parents’ prompt disposal of their children’s leftover opioids and reduced their planned retention rates. Providing a disposal method enhanced prompt disposal but did not affect planned retention.
Over the course of 2 decades, opioid-related emergency department, hospital, and ICU admission rates doubled and opioid-related mortality nearly tripled for children and adolescents.1–3 Exposure to prescribed opioids accounted for large majorities of these opioid-related pediatric hospital and critical care admissions3 and deaths,2 and 96% of exposures occurred in private residences.4 Therapeutic error (ie, unintentionally given a wrong dose or someone else’s medication) was found to account for only 1 in 5 pediatric exposures in 1 report, leaving the majority due to accidental or intentional access by children and adolescents.4 Retention and easy access to leftover prescription opioids is considered to be a major source of accidental and intentional pediatric exposures, posing significant risks of morbidity and mortality. Half to 90% of prescribed opioid doses are left over after acute pain treatment in children,5–9 and 3 out of 4 middle school children have reported unsupervised access to risky medications in the home.10 Moreover, up to 40% of adolescents who reported opioid misuse accessed their own past prescription, and more than half accessed that of a friend or family member.11–13 Importantly, most parents have admitted to keeping their children’s leftover opioids,14 and 10% to 20% of adults report sharing their children’s or their own leftovers between family and friends.14–16
Interventions such as providing disposal information, giving store credit, and expanded availability of community take-back programs have increased opioid disposal to some degree, but up to two-thirds of those with leftovers retain them despite intervention.6,8,17 Indeed, a majority of adults who acknowledge the hazard and who have been given disposal information have reported an intention to retain their own or their children’s leftover opioids.6,14,15 Thus, lack of knowledge about safe disposal may not fully explain drug retention. Instead, there may be real or perceived barriers to disposal that factor into behavior. Recent data support this notion, showing that perceived barriers were associated with parents’ poor opioid storage and retention practices.9 Additionally, drug take-back programs have been estimated to remove only a tiny portion of what is known to be leftover, suggesting barriers to action.8
Behavioral theorists recognize that people often fail to change behavior in a way that reduces risk even when they have relevant information about risks.18 They emphasize the importance of shaping the choice architecture to make preferred risk-reduction actions more salient and easier to perform and the implied default or expected behavior.19,20 Nudges are designed tactics meant to shape the choice architecture to prompt better decisions.18 Providing a disposal method at the time of prescribing is a type of nudge strategy that could prompt or motivate disposal rates over and above what other, less convenient methods have achieved because it minimizes the steps needed and enhances the perception that disposal is the expected behavior (subjective norm).
Another solution is to provide enhanced education about the real risks that leftover opioids pose to children and adolescents. Data suggest that to best reduce risky decision-making, educational interventions must enhance the perceived riskiness of the behavior rather than inform risk awareness alone.21 We previously showed how our Scenario-Tailored Opioid Messaging Program (STOMP) enhanced parents’ opioid risk perceptions, shifted their preferences toward risk avoidance, and improved safe analgesic decision-making.22 To date, there are limited data about whether behavioral or educational strategies are most effective and efficient in prodding early and safe disposal of leftover prescribed opioids.
Our purpose in this randomized, controlled trial was to examine whether provision of a disposal method with or without enhanced risk information at the time of prescribing would improve parents’ leftover disposal behavior after short-term use. Specifically, we hypothesized that when controlled for child and parent pain-related factors in a factorial design, the following would occur.
Providing a take-home disposal packet at the time of prescribing (ie, Nudge) would independently increase parents’ timely disposal behavior compared with parents who were randomly assigned to the no packet group (control).
STOMP risk information will increase timely disposal rates and lower planned retention of leftover opioids compared with routine information.
Methods
Interventions
Nudge is a cost-efficient disposal kit with illustrated instructions (ie, Ziploc of coffee grounds, a US Food and Drug Administration–sanctioned method for leftover drug disposal).23 The Nudge intervention provides a how-to-dispose kit that eliminates uncertainty, makes the required steps concrete, and creates an injunctive norm that use of the kit is expected behavior. The Nudge intervention was meant to boost response efficacy by putting the risk-reduction behavior within parents’ immediate control.
STOMP is an interactive Web-based program that presents descriptive, clinically relevant pain and risk situations in which parents consider common scenarios and make intentional analgesic use and handling decisions.21,24,25 Each decision prompts immediate feedback about the risk portrayed along with behavioral advice about what to do to reduce the risk. Parsimonious messages serve to heighten risk perception and build behavioral response efficacy.26 Similar feedback strategies have been shown to enhance health behaviors and outcomes compared with provider interactions alone.27 We hypothesized that STOMP information would improve disposal behavior and intentions by enhancing parents’ risk perceptions.
Main Outcome Measure
The main outcomes were prompt disposal (parents’ self-reported disposal immediately after the children’s course of treatment) and intention to retain (parents will keep after use). Self-report is the primary method used to ascertain opioid storage and disposal behavior.9,28,29 Meta-analyses show that health intentions correlate moderately with actual behavior and that this association increases when the risk behavior is within the control of the subject and when expected behavior change is <5 weeks postintervention.30 We used recent recommendations to optimize the validity of self-report,31 including computer survey of outcomes (instead of face-to-face assessment, which could increase social desirability), brief recall period, and inclusion of nonjudgmental wording (eg, “people often keep their leftover medications for various reasons”). We also asked parents to submit a photograph of the disposal as a secondary validation of the self-report.
Other Measures
The Parents’ Postoperative Pain Measure–Short Form32 measured the children’s pain (scored 0–10; 10 = most pain interference). This tool has excellent internal consistency (α = .85)32 and agreement with self-reported pain intensity in children.33
Risk perception was measured by several questions derived from a validated survey assessing parental concerns about prescription opioid storage in the home.9 Scores on the composite measure ranged from −6 to +6, where lower scores indicate strong disagreement and higher scores indicate strong agreement about the riskiness of opioid retention and misuse in the home.
Procedure
With approval from the institutional review board (Institutional Review Board, Medicine Human Subjects No. 127009), we consecutively recruited and consented parents whose children (aged 5–17 years) were scheduled to undergo a short-stay surgical procedure with a typical need for prescribed opioids. All recruitment occurred between October 2017 and December 2018, and follow-up was completed by January 31, 2019. We excluded non–English-speaking parents and those whose children were undergoing emergency procedures, those who could not self-report their pain, and those who had chronic pain or opioid use (≥3 months in the past year).
Trained assistants used computer-generated randomization to assign parents a priori to either the control group (no disposal Ziploc) versus the Nudge group (ie, received the disposal Ziploc) and to the STOMP versus routine information. Parents (blinded to assignment) completed baseline surveys using a Qualtrics link via iPad for consistency, completeness, and privacy. Parents entered their assigned, unique identification number and recorded their demographics, their own and their children’s past pain and opioid use, analgesics stored in the home, and whether they had ever taken a prescribed opioid in greater amounts or more frequently than prescribed, taken someone else’s prescribed opioid, or shared their opioid with a friend or family member (together coded as past opioid misuse). Parents’ health literacy was assessed by using the Rapid Estimate of Adult Literacy in Medicine–Short Form, which has established reliability and validity in adults (score range 0–7; scores <3 indicate less than a sixth-grade reading level).34 Parents assigned to the STOMP feedback received this information (embedded into the Qualtrics survey platform) immediately after the baseline survey.
On days 7 and 14 postdischarge, parents received follow-up Qualtrics survey links via e-mail to record pain interference scores, analgesic use, discontinuation, leftover opioid amounts, and disposal behavior and retention intentions. Parents who intended to retain leftovers were asked to provide reasons for retention (semistructured and open-ended options). Those who indicated disposal intention were asked how they disposed or planned to dispose and to e-mail or text a picture of the disposal process if possible. Parents recorded all opioid doses administered in diaries, which they returned in a prestamped envelope after analgesic discontinuation. These data were used to check the reliability of parental reports of leftover opioid amounts. Parents received $50 for completion of all surveys and diaries. We obtained prescription and surgical procedure data from the children’s electronic medical record. All surveys and child data were linked by using the parents’ unique identifier to maintain privacy and enhance honest disclosure.
Statistical Analyses
Data were analyzed by using SPSS (version 24; IBM SPSS Statistics, IBM Corporation) and are presented as n (%) and mean ± SD with odds ratios (ORs) or mean differences and 95% confidence intervals (CIs) when appropriate. No missing data were imputed. Univariate comparisons of group characteristics were conducted by using χ2 with Fisher’s exact tests or unpaired t tests with Levene’s tests for equality of variance. Logistic regression models assessed the effects of our interventions on the outcomes (1) prompt disposal and (2) intention to retain. In both models, we included our interventions and controlled for relevant pain and analgesic factors, including child procedure, pain interference, past opioid (parent and child), parental opioid misuse, and opioid storage in the home at baseline. We report adjusted odds ratios (aORs) for all factors and accepted significance at P < .05.
Sample Size Determination
We based our sample size on an expected disposal rate of 30% in our control group.14 To detect a small effect of the Nudge on disposal behavior (OR 1.5) with 95% confidence and a relative precision of 50%, we needed 196 parents in the Nudge and control groups. We recruited 640 parents to account for potential loss to follow-up and missing data (30%) and to ensure a sufficient sample to detect small effects of the interventions in a factorial model with up to 10 covariates (sample needed = 333).
Results
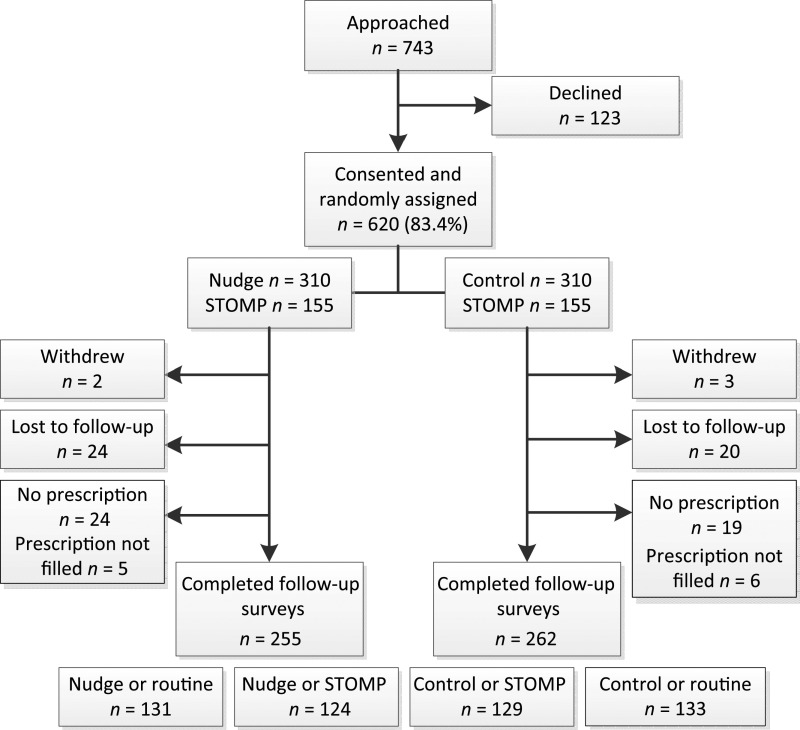
Our analytical sample derivation (n = 517) is depicted in Fig 1. There were no significant differences in baseline characteristics between the study groups at baseline (Table 1). Of note, 61 parents (11.8%) reported past prescription opioid misuse (31% for pain relief, 11% for sleep, and 5% to relax or for another effect), and the balance provided no motivation.
FIGURE 1.
Consolidated Standards of Reporting Trials diagram depicting sample derivation: prompt disposal.
TABLE 1.
Description of Baseline Characteristics of the Groups
| Control | Nudge | |||
|---|---|---|---|---|
| STOMP (n = 129) | Routine (n = 133) | STOMP (n = 124) | Routine (n = 131) | |
| Female parent, n (%) | 111 (86) | 103 (77) | 105 (85) | 106 (81) |
| High school diploma or less, n (%) | 18 (14) | 14 (11) | 16 (13) | 10 (8) |
| Parent health literacy,a mean ± SD | 6.95 ± 0.21 | 6.83 ± 0.69 | 6.89 ± 0.37 | 6.86 ± 0.59 |
| White race, n (%) | 116 (90) | 115 (87) | 105 (85) | 116 (89) |
| Hispanic, n (%) | 2 (2) | 6 (5) | 5 (4) | 3 (2) |
| Child previous surgery, n (%) | 85 (66) | 81 (61) | 84 (68) | 78 (60) |
| Female child, n (%) | 47 (36) | 59 (44) | 50 (40) | 60 (46) |
| Child age, mean ± SD | 12.76 ± 3.72 | 12.79 ± 3.86 | 13.52 ± 3.40 | 12.36 ± 3.72 |
| Child procedure type, n (%) | ||||
| Orthopedic or sports medicine | 79 (61) | 78 (59) | 69 (56) | 74 (57) |
| General surgery or urology | 25 (19) | 26 (20) | 21 (17) | 28 (21) |
| Otology | 11 (9) | 16 (12) | 13 (11) | 20 (15) |
| Other | 14 (11) | 13 (10) | 21 (17) | 9 (7) |
| Child past opioid use, n (%) | 30 (23) | 35 (26) | 40 (32) | 34 (26) |
| Parent past opioid use, n (%) | 78 (61) | 50 (38) | 60 (48) | 72 (55) |
| Opioid kept in home, n (%) | 28 (22) | 22 (17) | 24 (19) | 36 (27) |
| Past opioid misuse, any, n (%) | 18 (14) | 8 (6) | 11 (9) | 24 (18) |
| Took more | 8 (6) | 3 (2) | 7 (6) | 12 (9) |
| Shared their opioid | 10 (8) | 4 (3) | 3 (2) | 14 (11) |
| Took someone else’s | 7 (5) | 3 (2) | 8 (7) | 17 (13) |
Measured by using Rapid Estimate of Adult Literacy in Medicine–Brief, scored 0 to 7.
There were no differences between the groups in the children’s opioid and analgesic prescriptions or their use after hospital discharge (Table 2). Overall, 59% of children took opioids for ≤2 days, and 84% took them for <6 days. Most parents reported leftover opioids; 99 (19%) estimated that >50% to 100% of doses remained, 146 (28%) had one-quarter to half of the doses left, and 101 (20%) had only a few doses leftover. Comparisons between parents’ diary dose recordings and dispensed volume validated parental leftover estimates.
TABLE 2.
Details of Prescribed Analgesics, Use After Discharge, and Opioid Leftovers in the Groups
| Control | Nudge | |||
|---|---|---|---|---|
| STOMP (n = 129) | Routine (n = 133) | STOMP (n = 124) | Routine (n = 131) | |
| Oxycodone prescription, n (%) | 112 (87) | 120 (90) | 113 (91) | 126 (96) |
| Hydrocodone prescription, n (%) | 17 (13) | 13 (10) | 15 (12) | 7 (5) |
| Doses dispensed, n (median [IQR]) | 27.91 (24.39 [23.07–32.74]) | 25.59 (21.43 [21.77–29.41]) | 23.09 (20.00 [19.55–26.64]) | 22.77 (20.00 [19.47–26.06]) |
| Other analgesics ordered, n (%) | ||||
| Acetaminophen | 92 (74) | 95 (74) | 92 (76) | 93 (71) |
| Ibuprofen | 61 (50) | 66 (51) | 55 (45) | 67 (54) |
| Diazepam | 10 (8) | 7 (5) | 11 (9) | 7 (5) |
| Gabapentin | 4 (3) | 6 (5) | 6 (5) | 5 (4) |
| Magnesium | 17 (13) | 12 (9) | 16 (13) | 16 (12) |
| Opioid given after discharge | 106 (82) | 109 (83) | 101 (82) | 103 (79) |
| Total opioid doses given after discharge, range (median [IQR]) | 0–41 (5 [1–11]) | 0–36 (5 [1–10]) | 0–61 (4 [1–9.25]) | 0–39 (6 [1–10]) |
| Nonopioid given after discharge, n (%) | 122 (95) | 126 (98) | 115 (94) | 124 (97) |
| Ongoing nonopioid use (d 14), n (%) | 35 (27) | 31 (23) | 45 (36) | 29 (22) |
| Ongoing opioid use (d 14), n (%) | 8 (6) | 2 (2) | 4 (3) | 3 (2) |
| Pain interference score (d 14), mean ± SD | 1.14 ± 2.18 | 0.80 ± 1.43 | 1.05 ± 1.83 | 1.00 ± 2.03 |
| Leftover opioids, n (%) | 120 (93) | 122 (92) | 113 (91) | 126 (96) |
IQR, interquartile range.
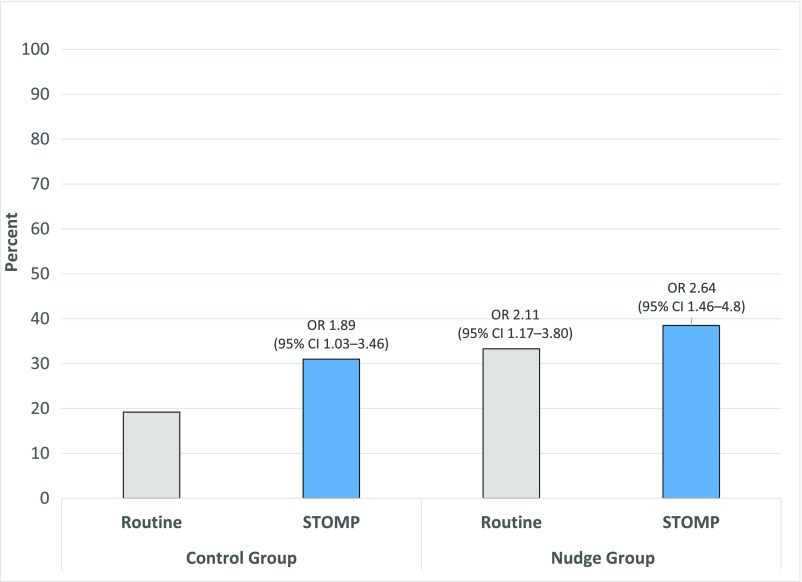
At the final survey, disposal rates were significantly higher for all intervention groups (Fig 2). Prompt disposal was highest for the STOMP and Nudge group (38.5%) and lowest for the control and routine information group (19.2%; OR 2.64 [95% CI 1.46–4.80]). Disposal confirmation by e-mailed image validated 56 (40%) early disposal cases.
FIGURE 2.
Prompt leftover prescription opioid-disposal rates between the study groups. Presented are ORs (95% CIs) versus control (no nudge) without the STOMP (routine) group.
Most parents reported an intention to eventually dispose of leftover opioids, but 44 (9%) intended to retain them. Planned retention was significantly lower for parents who received the STOMP intervention (5.6% vs 12.5% for parents without STOMP; OR 0.41 [95% CI 0.21–0.81]). Reasons for planned retention included concern for future child need (n = 34 [77%]), future family need (n = 3 [7%]), paid for the drug (n = 5 [11%]), and do not know how to dispose or not easy to get rid of (n = 6 [14%]). There was no association between intention to retain and doses administered at home or number of doses dispensed (ρ 0.071 and −0.004, respectively). Of those planning retention, 7 parents (64%) who had received STOMP planned to store the retained opioid in a locked cabinet or drawer compared with 11 (38%) who received standard information (P = .17).
Our hypotheses were supported by logistic regression analyses, showing that both the Nudge and STOMP interventions had significant effects on prompt disposal behavior when controlled for child and parent factors (Table 3). The STOMP significantly reduced parents’ intention to retain, whereas the Nudge had no independent effect on planned retention (Table 3). Importantly, higher parental risk perception lowered the odds of planned retention, whereas their past prescription opioid misuse behavior increased the odds of planned retention.
TABLE 3.
Results of Hypotheses Tests: Effects of Nudge and STOMP on Parental Disposal Behavior and Planned Retention
| Factor | aOR (95% CI) |
|---|---|
| Outcome: prompt opioid disposal (children with ongoing opioid use at final survey excluded); model χ2 28.54 (df 11); P = .003; Hosmer-Lemeshow test 0.447 | |
| Child age | 0.95 (0.90–1.01) |
| Child past opioid use | 1.29 (0.76–2.18) |
| Pain interference score | 0.92 (0.80–1.06) |
| Orthopedic or SM procedure | 0.66 (0.43–1.02) |
| Opioid kept in home baseline | 0.82 (0.47–1.45) |
| Parent past opioid use | 0.78 (0.49–1.23) |
| Parent misused opioid | 1.06 (0.51–2.19) |
| Total opioid doses dispensed | 0.99 (0.98–1.01) |
| Nudge intervention | 1.78 (1.16–2.73) |
| STOMP intervention | 1.68 (1.10–2.58) |
| Perceived opioid risk | 1.02 (0.96–1.10) |
| Outcome: parental intention to retain leftover opioid (included all parents); model χ2 43.96 (df 11); P < .001; Hosmer-Lemeshow test 0.815 | |
| Child age | 1.02 (0.92–1.12) |
| Child past opioid use | 1.03 (0.44–2.39) |
| Pain interference score | 0.96 (0.79–1.17) |
| Orthopedic or SM procedure | 2.45 (1.09–5.51) |
| Opioid kept in home baseline | 2.13 (0.96–4.71) |
| Parent past opioid use | 0.63 (0.27–1.50) |
| Parent misused opioid | 4.44 (1.67–11.79) |
| Total opioid doses dispensed | 1.00 (0.99–1.02) |
| Nudge intervention | 1.04 (0.51–2.12) |
| STOMP intervention | 0.40 (0.19–0.85) |
| Perceived opioid risk | 0.87 (0.79–0.96) |
df, degrees of freedom; SM, sports medicine.
Discussion
In this randomized controlled study, the Nudge intervention significantly enhanced parents’ timely disposal of leftover prescribed opioids after their children’s short-term use. Despite this important finding, the Nudge intervention had no effect on planned retention rates. In contrast, the STOMP intervention had significant effects on both prompt disposal behavior and planned retention. These findings suggest that provision of a handy disposal method can nudge immediate risk-reduction behavior but has little effect on future planning. To further reduce parents’ retention of leftover opioids, clear messaging about the risks posed to children and adolescents in the home is required.
We considered prompt disposal to be the best risk-reduction behavior because storage in the home, even for short periods, poses increased risk to family members and others. Good intentions to dispose, which the majority of our parents reported, may wane over time as parents get busy with other more pressing family activities. Furthermore, several parents in our study anecdotally described barriers in finding appropriate take-back programs, particularly for liquid medications. Many parents with disposal intentions planned to take their children’s leftover opioids back to a pharmacy or to their children’s clinic where appropriate disposal capability was unclear.
Our findings have important implications for promoting parental disposal of leftover prescription opioids. Nudge interventions aim to enhance behavior at the time of decision-making. In contrast, our STOMP intervention is meant to enhance opioid risk perceptions in addition to guiding risk-reduction behavior. STOMP provides parents with simple but blunt risk messages (eg, “Younger children have been poisoned, and some have died. ... Overdose and death have occurred in teenagers who took leftover opioids”) paired with recommended behaviors (eg, “...get rid of all leftovers right away by 1 of these approved ways. ...Getting rid of all leftover prescribed pain relievers is the only way to keep children and teenagers from potentially causing themselves harm”). That STOMP improved the rates of timely disposal and also reduced retention intentions supports this strategy. Notably, our messages have not, to date, diminished parents’ pain management behavior. That is, parents who receive scenario-tailored risk information have been found to make better decisions about when it is safe to use opioids to manage their children’s pain and when it is unsafe to do so.22 Thus, scenario-tailored messaging achieves a more balanced risk/benefit understanding that can improve pain outcomes while reducing risk. A balanced approach to education is imperative because parents’ primary motivation for retaining opioids is the anticipated future pain relief needs of their children.
Importantly, parents’ past prescription opioid misuse behavior quadrupled the risk of planned retention. Parents who have misused a prescribed opioid are likely to perceive the risks to be low, particularly if they or their families experienced no adverse problems. Assessing parents’ past behaviors and enhancing their perceptions of the real risks posed to children are important targets for risk reduction. This is particularly germane given new data showing that maternal prescription opioid misuse increases the risk for adolescent misuse (aOR 1.62 [95% CI 1.28–2.05]), whereas higher parental risk perceptions decrease this risk (aOR 0.93 [95% CI 0.87–1.00]).35 Additionally, mothers have been found to strongly influence their teenagers’ analgesic use and information.36,37 To interrupt the modeled pattern of medication misuse, assessments and interventions must first target parents.
Despite our rigorous randomized controlled trial design, our ability to generalize findings is somewhat limited. Firstly, we cannot reject the possibility of a social desirability bias because parents may want to appear to be doing the right thing for their children and household. We minimized the potential for social desirability bias by including nonjudgmental statements in our survey and using computerized surveys (versus face to face). Although use of self-reported outcomes may have overestimated disposal behavior, evidence from adherence studies suggests their correlation with other observational methods and their good predictive validity.31 Next, our sample consisted of mostly white, well-educated parents in a state and community that has been heavily impacted by the opioid epidemic and related deaths. Thus, parents’ baseline opioid risk perceptions may be higher than those in other less-impacted communities. Finally, our intervention was particularly low cost, thus meeting the definition of a nudge intervention. Although commercially available drug disposal pouches are available, it is unclear how their cost would impact use and implementation across settings. Even if policies mandated their distribution with scheduled drugs, it is likely that the cost would be passed along to consumers, thus creating a potential barrier to use. Despite these limitations, our findings have relevance to inform future interventions aimed at reducing the retention of leftover, high-risk prescription medications.
Conclusions
In summary, we found that providing a disposal method at the time of opioid prescribing effectively nudged more parents to do the right thing and promptly dispose of their children’s leftovers after short-term use. Heightening risk perceptions with tailored risk information had an additive effect on parental behavior and reduced their intention to retain prescription opioid leftovers. It will be important to determine if such interventions have longer-lasting impacts on opioid misuse and adverse events among children, teenagers, families, and communities.
Acknowledgments
We acknowledge the work of the research team who recruited and surveyed subjects and managed data collection and entry: Elizabeth Loescher, Trevor de Sibour, Emily Currier, Sarah Dwyer, and Hannah Hamilton.
Glossary
- aOR
adjusted odds ratio
- CI
confidence interval
- OR
odds ratio
- STOMP
Scenario-Tailored Opioid Messaging Program
Footnotes
Deidentified individual participant data will not be made available at this time.
Dr Voepel-Lewis developed the interventions, designed the study and methods, supervised the recruitment and data collection, ensured the ethical conduct of the study, guided the analyses, interpreted data, and drafted the manuscript; Drs Farley and Grant contributed to the risk education intervention and research design, facilitated the recruitment of the surgical population, interpreted the data, and edited the final manuscript; Dr Tait assisted with the research design and methods, conducted the statistical analyses, assisted with data interpretation, and edited the final manuscript; Drs Boyd and McCabe assisted with the research methods and surveys, interpreted data, and edited the final manuscript; Ms Weber assisted with survey methodology, supervised all subject recruitment, data collection, and database management, and edited the final manuscript; Dr Harbagh assisted with editing; Dr Zikmund-Fisher helped to develop the educational and behavioral interventions, designed the study and survey methodology, guided statistical analyses and interpretation of data, and helped to draft the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
This trial has been registered at www.clinicaltrials.gov (identifier NCT03287622).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by the National Institute on Drug Abuse (R01DA044245). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Gaither JR, Leventhal JM, Ryan SA, Camenga DR. National trends in hospitalizations for opioid poisonings among children and adolescents, 1997 to 2012. JAMA Pediatr. 2016;170(12):1195–1201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaither JR, Shabanova V, Leventhal JM. US national trends in pediatric deaths from prescription and illicit opioids, 1999-2016. JAMA Netw Open. 2018;1(8):e186558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kane JM, Colvin JD, Bartlett AH, Hall M. Opioid-related critical care resource use in US children’s hospitals. Pediatrics. 2018;141(4):e20173335. [DOI] [PubMed] [Google Scholar]
- 4.Allen J, Casavant M, Spiller H, Chounthirath T, Hodges N, Smith G. Prescription opioid exposures among children and adolescents in the US: 2000-2015. Pediatrics. 2017;139(4):e20163382. [DOI] [PubMed] [Google Scholar]
- 5.Abou-Karam M, Dubé S, Kvann HS, et al. . Parental report of morphine use at home after pediatric surgery. J Pediatr. 2015;167(3):599–604–2 [DOI] [PubMed] [Google Scholar]
- 6.Maughan BC, Hersh EV, Shofer FS, et al. . Unused opioid analgesics and drug disposal following outpatient dental surgery: a randomized controlled trial. Drug Alcohol Depend. 2016;168:328–334 [DOI] [PubMed] [Google Scholar]
- 7.Voepel-Lewis T, Wagner D, Tait AR. Leftover prescription opioids after minor procedures: an unwitting source for accidental overdose in children. JAMA Pediatr. 2015;169(5):497–498 [DOI] [PubMed] [Google Scholar]
- 8.Egan KL, Gregory E, Sparks M, Wolfson M. From dispensed to disposed: evaluating the effectiveness of disposal programs through a comparison with prescription drug monitoring program data. Am J Drug Alcohol Abuse. 2017;43(1):69–77 [DOI] [PubMed] [Google Scholar]
- 9.McDonald EM, Kennedy-Hendricks A, McGinty EE, Shields WC, Barry CL, Gielen AC. Safe storage of opioid pain relievers among adults living in households with children. Pediatrics. 2017;139(3):e20162161. [DOI] [PubMed] [Google Scholar]
- 10.Ross-Durow PL, McCabe SE, Boyd CJ. Adolescents’ access to their own prescription medications in the home. J Adolesc Health. 2013;53(2):260–264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manchikanti L, Fellows B, Ailinani H, Pampati V. Therapeutic use, abuse, and nonmedical use of opioids: a ten-year perspective. Pain Physician. 2010;13(5):401–435 [PubMed] [Google Scholar]
- 12.McCabe SE, West BT, Boyd CJ. Leftover prescription opioids and nonmedical use among high school seniors: a multi-cohort national study. J Adolesc Health. 2013;52(4):480–485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miech R, Johnston LD, O’Malley P, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the Future National Survey Results on Drug Use, 1975–2017. Ann Arbor, MI: Institute for Social Research; 2018 [Google Scholar]
- 14.Clark S, Singer D, Matos-Moreno A, Kauffman A, Schultz S, Davis M. Narcotics in the Medicine Cabinet: Provider Talk Is Key to Lower Risk, vol. Vol 26 Ann Arbor, MI: C.S. Mott Children’s Hospital, University of Michigan; 2016 [Google Scholar]
- 15.McCauley JL, Back SE, Brady KT. Pilot of a brief, web-based educational intervention targeting safe storage and disposal of prescription opioids. Addict Behav. 2013;38(6):2230–2235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kennedy-Hendricks A, Gielen A, McDonald E, McGinty EE, Shields W, Barry CL. Medication sharing, storage, and disposal practices for opioid medications among US adults. JAMA Intern Med. 2016;176(7):1027–1029 [DOI] [PubMed] [Google Scholar]
- 17.Rose P, Sakai J, Argue R, Froehlich K, Tang R. Opioid information pamphlet increases postoperative opioid disposal rates: a before versus after quality improvement study. Can J Anaesth. 2016;63(1):31–37 [DOI] [PubMed] [Google Scholar]
- 18.Kosters M, Van der Heijden J. From mechanism to virtue: evaluating nudge theory. Evaluation. 2015;21(3):276–291 [Google Scholar]
- 19.Thayler R, Sunstein C. Nudge: Improving Decisions about Health, Wealth, and Happiness. New York, NY: Penguin Group; 2009 [Google Scholar]
- 20.Janz NK, Becker MH. The Health Belief Model: a decade later. Health Educ Q. 1984;11(1):1–47 [DOI] [PubMed] [Google Scholar]
- 21.Voepel-Lewis T, Zikmund-Fisher BJ, Smith EL, Redman RW, Zyzanski S, Tait AR. Parents’ analgesic trade-off dilemmas: how analgesic knowledge influences their decisions to give opioids. Clin J Pain. 2016;32(3):187–195 [DOI] [PubMed] [Google Scholar]
- 22.Voepel-Lewis T, Zikmund-Fisher BJ, Boyd CJ, et al. . Effect of a scenario-tailored opioid messaging program on parents’ risk perceptions and opioid decision-making. Clin J Pain. 2018;34(6):497–504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.US Food and Drug Administration. Where and how to dispose of unused medicines. 2015. Available at: www.fda.gov/ForConsumers/ConsumerUpdates/ucm101653.htm. Accessed August 31, 2016
- 24.Voepel-Lewis T, Zikmund-Fisher B, Smith EL, Zyzanski S, Tait AR. Opioid-related adverse drug events: do parents recognize the signals? Clin J Pain. 2015;31(3):198–205 [DOI] [PubMed] [Google Scholar]
- 25.Voepel-Lewis T, Zikmund-Fisher BJ, Smith EL, Zyzanski S, Tait AR. Parents’ preferences strongly influence their decisions to withhold prescribed opioids when faced with analgesic trade-off dilemmas for children: a prospective observational study. Int J Nurs Stud. 2015;52(8):1343–1353 [DOI] [PubMed] [Google Scholar]
- 26.Luszczynska A, Tryburcy M, Schwarzer R. Improving fruit and vegetable consumption: a self-efficacy intervention compared with a combined self-efficacy and planning intervention. Health Educ Res. 2007;22(5):630–638 [DOI] [PubMed] [Google Scholar]
- 27.Riiser K, Løndal K, Ommundsen Y, Småstuen MC, Misvær N, Helseth S. The outcomes of a 12-week Internet intervention aimed at improving fitness and health-related quality of life in overweight adolescents: the Young & Active controlled trial. PLoS One. 2014;9(12):e114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wieczorkiewicz SM, Kassamali Z, Danziger LH. Behind closed doors: medication storage and disposal in the home. Ann Pharmacother. 2013;47(4):482–489 [DOI] [PubMed] [Google Scholar]
- 29.Bartels K, Mayes LM, Dingmann C, Bullard KJ, Hopfer CJ, Binswanger IA. Opioid use and storage patterns by patients after hospital discharge following surgery. PLoS One. 2016;11(1):e0147972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McEachan R, Conner M, Taylor N, Lawton R. Prospective prediction of health-related behaviours with the Theory of Planned Behaviour: a meta-analysis. Health Psychol Rev. 2011;5:97–144 [Google Scholar]
- 31.Stirratt MJ, Dunbar-Jacob J, Crane HM, et al. . Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med. 2015;5(4):470–482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.von Baeyer CL, Chambers CT, Eakins DM. Development of a 10-item short form of the parents’ postoperative pain measure: the PPPM-SF. J Pain. 2011;12(3):401–406 [DOI] [PubMed] [Google Scholar]
- 33.Walther-Larsen S, Aagaard GB, Friis SM, Petersen T, Møller-Sonnergaard J, Rømsing J. Structured intervention for management of pain following day surgery in children. Paediatr Anaesth. 2016;26(2):151–157 [DOI] [PubMed] [Google Scholar]
- 34.Haun J, Luther S, Dodd V, Donaldson P. Measurement variation across health literacy assessments: implications for assessment selection in research and practice. J Health Commun. 2012;17(suppl 3):141–159 [DOI] [PubMed] [Google Scholar]
- 35.Griesler PC, Hu MC, Wall MM, Kandel DB. Nonmedical prescription opioid use by parents and adolescents in the US. Pediatrics. 2019;143(3):e20182354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shehnaz SI, Khan N, Sreedharan J, Arifulla M. Drug knowledge of expatriate adolescents in the United Arab Emirates and their attitudes towards self-medication. Int J Adolesc Med Health. 2014;26(3):423–431 [DOI] [PubMed] [Google Scholar]
- 37.Skarstein S, Lagerløv P, Helseth S, Leegaard M. How do parents influence their adolescents’ use of over-the-counter analgesics: a review of the current literature. J Clin Nurs. 2019;28(9–10):1451–1464 [DOI] [PubMed] [Google Scholar]