Abstract
Purpose of Review
This review will outline scapular function in throwing, discuss scapular dyskinesis as an impairment of function that can be associated with throwing injuries and altered performance, and present an algorithm that encompasses guidelines for evaluation and can serve as a basis for treatment.
Recent Findings
Optimal scapular function is integral to optimal shoulder function. Multiple roles of the scapula in arm function and throwing have been identified while scapular dysfunction continues to be associated with various shoulder pathologies. Although scapular motion alterations may be common in overhead athletes, various reports have shown that identification and management of the alterations can result in improved rehabilitation and performance outcomes.
Summary
Baseball throwing occurs as the result of integrated, multisegmented, sequential joint motion, and muscle activation within the kinetic chain. The scapula is a key component link within the chain through its function to maximize the scapulohumeral rhythm and efficient throwing mechanics. Evaluation and management beginning with the scapula can produce improved outcomes related to shoulder pathology in overhead athletes.
Keywords: Scapula, Scapular dyskinesis, Kinetic chain, Overhead athlete
Scapular Position and Motion in Shoulder Function and Shoulder Injury
The scapula plays several key roles to optimize the function of the shoulder, providing a position of support and a motion for stability. Its position facilitates optimal muscle activation and strength development, and force and energy transfer through the kinetic chain, while its dynamic motion maximizes glenohumeral (G-H) concavity/compression kinematics and G-H stability, maximizes G-H range of motion, and minimizes humeral impingement. Studies have accurately documented the composite 3-dimensional scapular motions necessary to optimize the roles. The most effective scapular position to achieve these goals is retraction and the most effective motion is retraction in cocking and controlled protraction in ball release and follow through.
Scapular Dyskinesis
Most scapular-related problems in throwing athletes can be traced to loss of control of normal resting scapular position and dynamic scapular motion, which will produce scapular protraction, a combination of anterior tilt, increased internal rotation, and decreased upward rotation. Protraction is not an injury and has not been directly linked with an injury. A consensus conference review classified the protracted position and motion as an impairment, creating possible increased loads, altered motions, and decreased muscle activations that can be associated with decreased performance and increased injury risk [1].
The observational finding of protraction has been termed scapular dyskinesis, reflecting the alteration (dys) of motion (kinesis) [2]. Various studies have determined that it is frequently found (67–100%) in association with all types of shoulder pathology [3, 4]. Scapular dyskinesis has multiple effects that may alter optimal shoulder function. They include increasing the G-H angle in horizontal abduction, which increases anterior capsular tension and shear with simultaneous increases in posterior labral compression [5, 6], decreasing maximal rotator cuff strength for compression stability [7], decreasing maximal subacromial space to minimize impingement [8], and decreasing optimal G-H abduction external rotation necessary for overhead function.
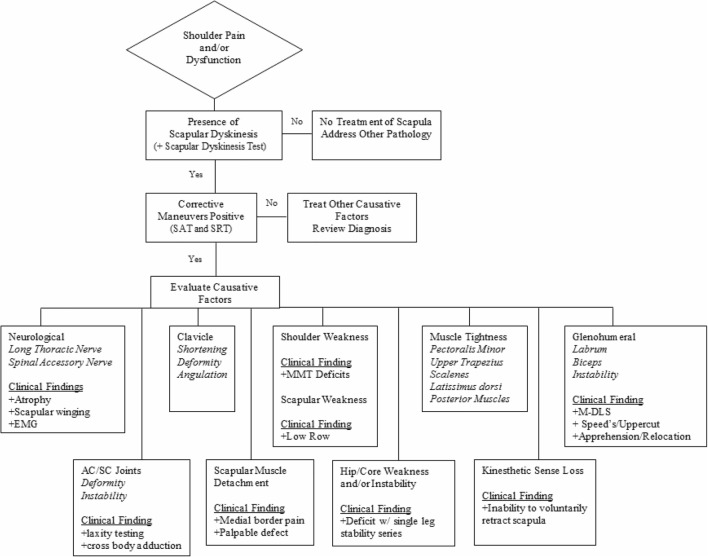
Dyskinesis has multiple causative factors, which can be discovered by history, physical examination, imaging, and special testing utilizing a specific algorithm. Not all observed dyskinesis is associated with shoulder symptoms and dysfunction. This algorithm can help highlight clinically significant dyskinesis and its causative factors (Fig. 1). It creates steps that progressively (1) establish the presence or absence of observational dyskinesis, (2) determine the clinical relationship of the dyskinesis to the symptoms and dysfunction by employing specific corrective maneuvers, and (3) assesses the possible causative factors. Treatment can then be directed based on the findings (Fig. 2).
Fig. 1.
Diagnostic algorithm
Fig. 2.
Decision-making process based on algorithm findings
The first step, identifying the presence or absence of the physical impairment of scapular dyskinesis, is best accomplished by observation of static position at rest or dynamic motion upon arm motion using the scapular dyskinesis test [9–11]. The exam is conducted by having the patients raise the arms in forward flexion to maximum elevation, and then lower them 3–5 times, with a 3-–5-pound weight in each hand [9, 10]. Prominence of any aspect of the medial scapular border on the symptomatic side is recorded as “yes” (prominence detected) or “no” (prominence not detected) [12] (Fig. 3).
Fig. 3.

Example of scapular dyskinesis showing medial border and inferior angle prominence
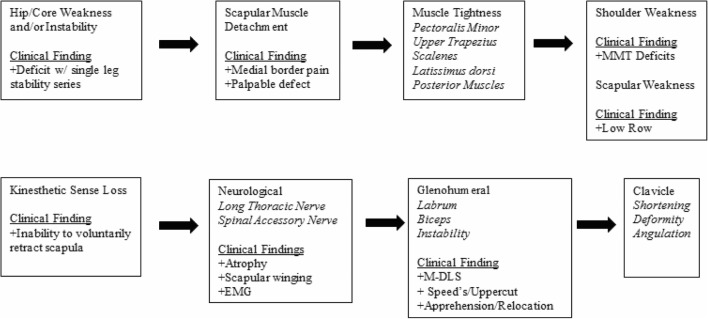
The next step is determining the relation of the observed dyskinesis to clinical symptoms. The scapular assistance test (SAT) and scapular retraction test (SRT) are corrective maneuvers that can alter the injury symptoms and provide information about the role of scapular dyskinesis in the total picture of the dysfunction [11, 13]. In the SAT, the examiner applies gentle pressure to assist scapular upward rotation and posterior tilt as the patient elevates the arm (Fig. 4). A positive result occurs when the painful arc of impingement symptoms is relieved and the arc of motion is increased. In the SRT, the examiner first grades the strength in forward flexion following standard manual muscle testing procedures (Fig. 5a) or evaluates the labrum by the modified dynamic labral shear (M-DLS) test [14]. The examiner then places and manually stabilizes the scapula in a retracted position (Fig. 5b). A positive test occurs when the demonstrated strength is increased or the symptoms of internal impingement in the labral injury are relieved in the retracted position.
Fig. 4.

Scapular assistance test
Fig. 5.
Scapular retraction test. Muscle testing without (a) and with (b) scapular retraction
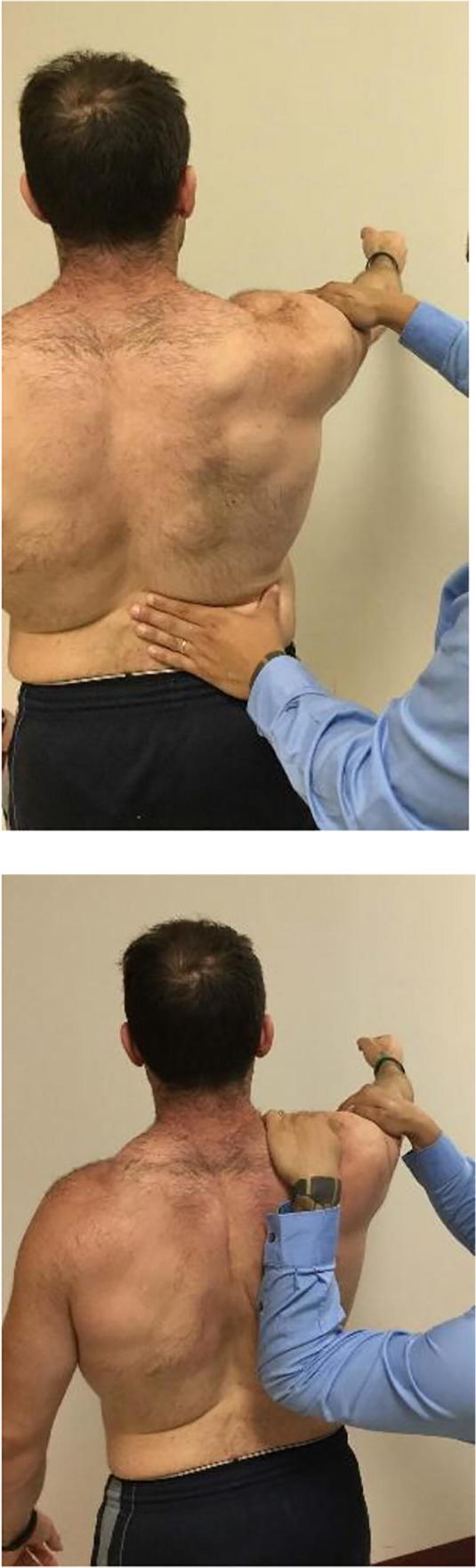
The final step is to employ a check off list to evaluate the causative factors (Fig. 2). The check off list can be used as a guide when performing the comprehensive evaluation. The check off list includes all of the known possible causative factors such as core weakness, with altered facilitation of muscle activation [15–17]; altered periscapular muscle activation due to pain-derived muscle inhibition [18, 19]; muscle stiffness or strength imbalances; G-H or acromioclavicular (A-C) joint injury with pain, instability, or mechanical compensations [20–23]; altered G-H joint motion especially internal rotation (GIRD) and total arc of motion (TAMD) [24–31]; bony injury to the clavicle or A-C joint with disruption of the strut stability [32–35]; or neurologic injury such as cervical radiculopathy, long thoracic nerve, or spinal accessory nerve injury [36, 37]. A linear evaluation program would include (1) evaluation of core stability and strength, through a screening exam for one leg stance and knee bend stability; (2) strength testing for the periscapular muscles, especially in retraction, using standard clinical tests; (3) testing for inflexibility of commonly tight muscles, such as the upper trapezius, pectoralis minor, scalenes, and latissimus dorsi; (4) G-H joint evaluation for altered rotation (internal, external, total motion, and horizontal adduction), instability, labral injury, bicep tendinopathy, and rotator cuff disease, using standard G-H exam techniques; (5) clavicle and A-C joint evaluation for stability, angulation, shortening, or malrotation; and (6) neurological evaluation for cervical radiculopathy and long thoracic and accessory nerve injury.
Specific Problems in the Throwing Athlete
Scapular dyskinesis has been found in association with almost every pathologic injury in the shoulder and arm in the throwing athlete. The incidence varies, but dyskinesis can be identified in between 50 and 100% of throwers with injuries.
Labral Injury
Scapular dyskinesis has a high association with labral injury with up to 94% of injured athletes demonstrating dyskinesis [30, 38]. The altered position and motion of internal rotation and anterior tilt plus loss of upward rotation changes G-H alignment, placing increased tensile strain on the anterior ligaments [5], increases “peel-back” of the biceps/labral complex on the glenoid [24], increases posterior humeral head translation against the posterior labrum, and creates pathological internal impingement resulting in labral compression, tearing, and insubstance shearing [29, 30]. Only a 10-degree loss of upward rotation increases the area and amount of compressive impingement, while a 10-degree increase in internal rotation increases the amount of compressive impingement [7]. These effects are magnified in the presence of GIRD, which creates increased protraction due to “windup” of the tight posterior structures in follow through. In addition, correction of the symptoms of pain found in the modified dynamic labral shear (M-DLS) test can be frequently demonstrated by the scapular retraction test (SRT). This indicates the presence of dyskinesis as part of the pathophysiology and the need for scapular rehabilitation to improve scapular retraction. A scapular-based rehabilitation program has been found to be successful to modify symptoms and improve performance so that surgery is not required in 41% of professional athletes [39] and 50–60% of nonprofessional but recreationally active athletes [40].
Glenohumeral Instability
The type of instability will usually determine how to address the dyskinesis. Traumatic anterior or posterior instability results in dyskinesis due to pain, muscle alteration(s), or altered joint mechanics, but dyskinesis can rarely be completely resolved in the presence of the anatomic lesion.
Symptoms in multidirectional and microtraumatic posterior instability are more related to alterations of the muscle function, which then create dyskinesis, and treatment of dyskinesis has been shown to have a more central effect on symptom resolution and functional restoration [41–43].
Impingement
Impingement is frequently seen in throwing athletes but is rarely a primary or isolated diagnosis. Altered muscle activations, muscle tightness, and G-H joint injury produce the dyskinetic protracted position and motion characterized by decreased scapular posterior tilt, increased internal rotation, and decreased upward rotation. The impairment decreases the height of the subacromial space, increases rotator cuff contact on the acromion and glenoid, and decreases demonstrated rotator cuff strength.
Altered muscle activations include increased upper trapezius activation, altered activation sequencing of the upper trapezius and lower trapezius, and decreased lower trapezius and serratus anterior activation. These weaknesses create a lack of scapular external rotation and upward rotation as the arm elevates.
A tight pectoralis minor muscle creates a position of scapular protraction at rest and does not allow scapular posterior tilt or external rotation upon arm motion, predisposing patients to impingement symptoms [44]. In this population of throwing athletes, even in the presence of positive impingement signs and impingement tests, most cases of impingement symptoms not associated with G-H injury can be resolved by including restoration of scapular kinematics in the rehabilitation program [45].
Rotator Cuff Injury
Shoulder dysfunction associated with rotator cuff injury can be created but most frequently may be exacerbated by dyskinesis. Causative factors for dyskinesis include G-H joint injury, pectoralis minor tightness, lower trapezius and serratus anterior muscle weakness, and upper trapezius tightness. The protracted position increases compression loads on the bursal side of the rotator cuff and increases internal impingement/torsional twisting on the articular side of the rotator cuff.
Rehabilitation programs that address restoration of scapular mechanics have been shown to decrease rotator cuff symptoms and decrease the requests for surgery, both in partial thickness and full thickness tears [46]. In both nonoperative and postoperative cases, early rehabilitation protocols should avoid exercises or arm positions that create protraction. These positions increase the compressive load on the tendon repair and can impair or delay optimum healing [23, 47].
Clavicle Fractures and Acromioclavicular Joint Injuries
The A-C joint creates a stable articulation that allows efficient 3-dimensional claviculo-scapulo-humeral rhythm to optimize arm motion and position. The clavicle is the only bony strut for this mechanism [35, 48]. Clavicle fractures or A-C joint injuries can create dyskinesis by disruption of the anatomy and biomechanics of normal scapular motion. In A-C joint injuries, the loss of the suspension of the scapula on the clavicle, unbalanced muscle pull, and gravity produce the dyskinetic protraction [32]. In clavicle fractures, muscle pull, gravity, and torque transmitted through the coracoclavicular ligaments produce the dyskinetic protraction [33]. The observed dyskinesis is an indication of altered scapular kinematics that may have important clinical implications for anatomic bony or joint healing and for optimal shoulder function in the face of chronic protraction. Treatment should be directed at restoring the anatomic disruption that will restore scapular kinematics [33, 49].
Scapula and the Elbow
The elbow is a downstream joint in the kinetic chain of overhead athletes [50]. Position and motion of the joint, resulting forces and loads, and injury occurrence can be significantly impacted by scapular and shoulder function [51–55]. Scapular muscle fatigue from repetitive overhead motions can produce dyskinetic protraction, mainly with altered internal/external rotation and anterior/posterior tilt [52, 53]. Compensatory elbow motions and inconsistency in reproduction of the elbow positions and motions increase elbow loads [51]. Compensatory arm motions can alter G-H angulation, producing increased humeral horizontal abduction which can increase elbow centripetal forces and can alter arm abduction, creating the “dropped elbow,” which has been associated with increased elbow valgus loads [55–57].
Rehabilitation
Three types of rehabilitation scenarios exits for throwing athletes: no activity with formal rehabilitation, limited/modified activity with supplemental rehabilitation, and full activity with supplemental conditioning. The key points for each level are described below.
No Activity with Formal Rehabilitation
Removing the high load activity can help re-establish the normal activations that create scapulohumeral rhythm. This phase concentrates on addressing the causative factors for the dyskinesis and also re-establishes the proximal to distal kinetic chain activations that allow rehabilitation of the body to function as a unit in order to perform a multitude of tasks [17, 38, 58–60].
A kinetic chain rehabilitation framework focuses on three critical characteristics [15]. First, patients are upright during exercise performance rather than be positioned supine or prone when possible to simulate functional demands [15]. Second, the lever arm on the shoulder and trunk is shortened to reduce the load on the injured arm. Finally, arm motions should be initiated using the legs and trunk to facilitate activation of the scapula and shoulder muscles, which is a typical neurological pattern of motion [61, 62]. This framework was later expanded to include a set of progressive goals [58]: (1) establish proper postural alignment, (2) establish proper motion at all involved segments, (3) facilitation of scapular motion via exaggeration of lower extremity/trunk movement, (4) exaggeration of scapular retraction in controlling excessive protraction, (5) utilize the closed chain exercise early, and (6) work in multiple planes.
Posture and Motion
Proper posture and motion can be achieved by restoring skeletal segmental stability and mobility through muscle re-education, soft tissue mobility, and spinal/rib mobilization. Muscle re-education and strengthening of the core muscles should begin early in rehabilitation, targeting both local and global muscles [17]. In this first stage of the kinetic chain approach, soft tissue deficits of both upper and lower extremities should also be addressed. Segmental mobility of the thoracic spine and rib cage mobility is necessary for the scapula to synchronously move during arm motion.
Scapular Motion Facilitation
Primary stabilization and motion of the scapula on the thorax involves the coupling of the upper and lower fibers of the trapezius muscle with the serratus anterior and rhomboid muscles. Arm function overhead requires that the scapula obtains a position of posterior tilt and external rotation, which allows optimal shoulder muscle activation that is synergistic with the trunk and hip musculature. This kinetic chain pattern of activation then facilitates maximal activation of the muscles attached to the scapula [15]. This integrated sequencing allows the retracted scapula to serve as a stable base for the origin of all the rotator cuff muscles, allowing optimal concavity compression to occur [63, 64].
Controlling Protraction and Exaggerating Retraction
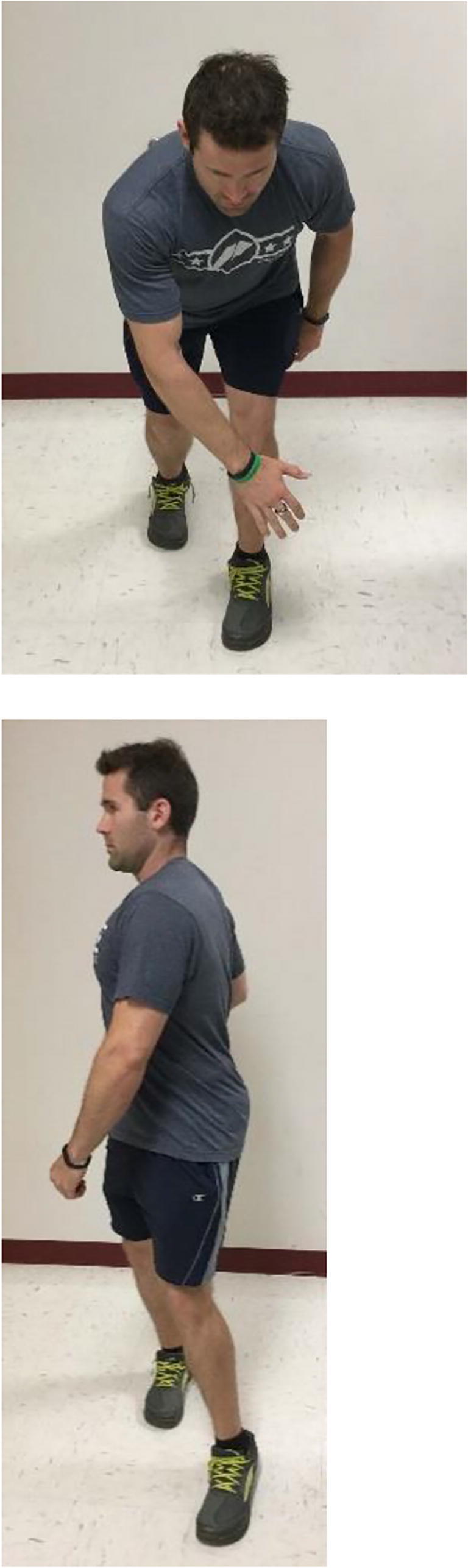
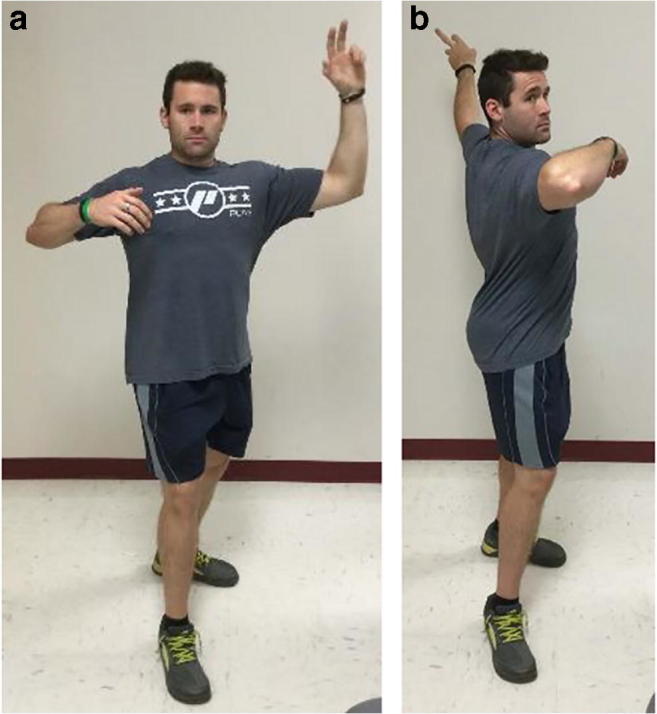
Although scapular protraction is a necessary kinematic translation which occurs during the ball release through follow-through phases of the throwing motion, excessive scapular protraction does not allow optimal rotator cuff activation to occur [65–68]. The muscles responsible for performing scapular retraction can help control scapular protraction through eccentric control. When optimized, these muscles can properly maintain scapular stability thus decreasing excessive protraction with arm movement. For this reason, the early phases of training should focus on scapular strengthening, especially in eccentric activation, in an attempt to restore normal scapular kinematics rather than placing an early emphasis on rotator cuff strengthening as performed in more traditional rehabilitation protocols. A basic exercise to utilize in this phase would be conscious correction of the scapula using visual feedback [69] (Fig. 6a, b).
Fig. 6.

Conscious correction of the scapula requires the patient to actively position the scapulae from a relaxed position (a) to a retracted position (b) prior to moving the arm
Early Closed Chain Implementation
Kinetic chain-based rehabilitation activities have been grouped into open and closed chain [70, 71]. Typically, closed chain exercises are implemented early in the rehabilitation process. These types of exercises are best suited for re-establishing the proximal stability and control in the links of the kinetic chain such as the pelvis and trunk. Open chain exercises, which generate greater loads in comparison with closed chain activities, should be utilized later in rehabilitation programs due to the longer lever arm these exercises require which causes increased demand on the soft tissue.
The rationale behind the closed-chain framework is to maximize the ability of the inhibited muscles to activate. This involves placing the extremity in a closed-chain position, emphasizing normal activation patterns and focusing on the muscle of interest by deemphasizing compensatory muscle activation. A closed chain exercise such as the low row (Fig. 7a, b) should be utilized because the short lever positioning in conjunction with the pelvis and trunk acting as the driver facilitates lower trapezius and serratus anterior co-activation which decreases the activation of the upper trapezius [72]. Once the normal activation pattern of retraction and depression has been restored; then, more challenging exercises can be employed.
Fig. 7.

Low row exercise: the patient is positioned standing with the hand of the involved arm against the side of a firm surface and legs slightly flexed (a). The patient should be instructed to extend the hips and trunk to facilitate scapular retraction and hold the contraction for 5 s (b)
Working in Multiple Planes
During the functional phase in the latter stages of the rehabilitation process, general G-H strengthening would be introduced. Open chain exercises attempt to isolate the rotator cuff muscles through long lever arms performed in single plane ranges of motion which could potentially create shear force across the joint and cause muscular irritation. The patient should be positioned in standing positions in order to effectively use all segments within the kinetic chain [73]. This will simulate normal function and limit attempts at trying to treat muscles in isolation [73]. Since, most activities occur in the transverse plane, the transverse plane should be exploited particularly in the early phases of rehabilitation, using diagonal and rotation exercises (Figs. 8a, b and 9a, b).
Fig. 8.
Lawnmower exercise: the lawnmower begins with the hips and trunk flexed and the arm slightly forward elevated (a). The patient is instructed to extend the hips and trunk, followed by rotation of the trunk to facilitate scapular retraction (b)
Fig. 9.
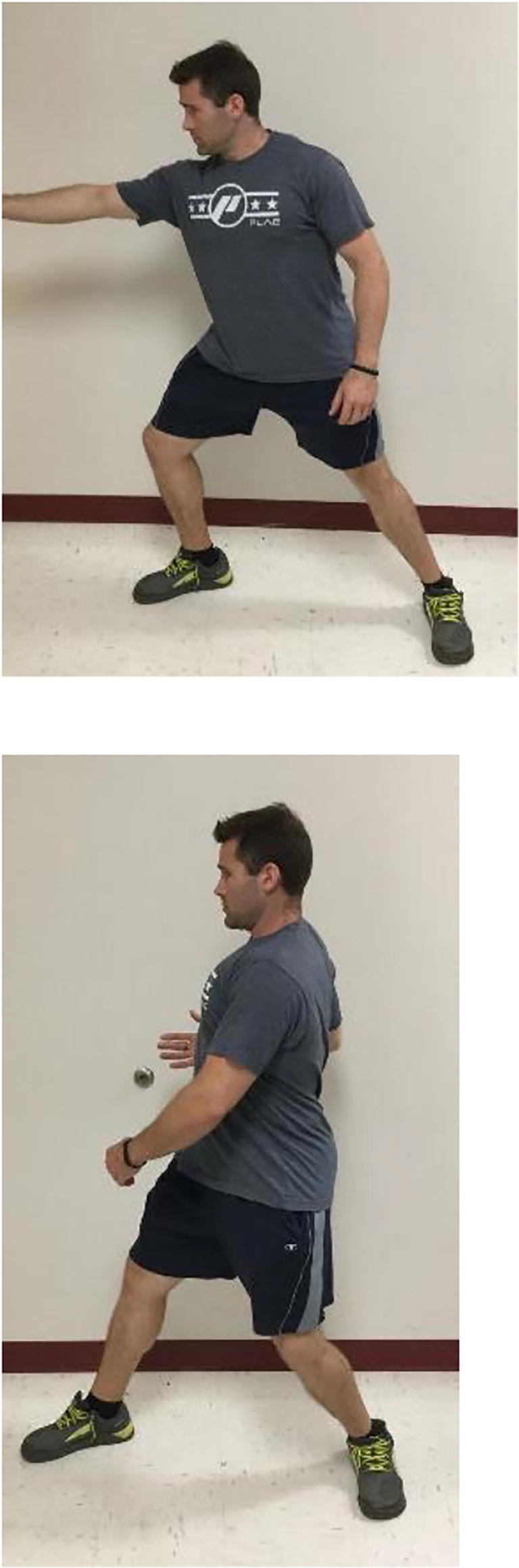
Fencing: this maneuver begins in a standing position with the patient grasping resistance bands or tubing (a). It utilizes multiple kinetic chain segments to enhance proper muscle scapular muscle activation through activation of the legs, trunk, scapula, and arm (b)
Limited Activity with Supplemental Rehabilitation
At this level, the athlete would likely present similar to the athlete at the “no activity” level; however, the symptoms may be more general or vague suggesting something deleterious is beginning rather than fully existing. Additionally, chronic injury such as long standing labral pathology or tendinopathy of the long head of the biceps brachii or rotator cuff may be detected but may not grossly affect function. Because of this less severe presentation, allowing the athlete to participate in some team activities is permissible and often tolerable. The activity modifications would include limited throwing volume, participation in field drills that only require gathering a ball and batting.
Supplemental rehabilitation involves supervised exercises and/or stretches that target specific muscles or tissues directly affecting scapular function and the treatment plan would likely serve as an adjunct to strength training and conditioning. Similar to the exercise progression described for the “no activity with formal rehabilitation” level, the kinetic chain-based approach would be implemented to address scapular control and integration of all kinetic chain links. Examples would include reverse throwing (Fig. 10a, b) and power position (Fig. 11a, b). The strength training program would also be modified so the athlete receives the training benefit but the injured or irritated tissue would not be overly stress or taxed. Examples would include modifying arm maneuvers to avoid hyperextension, horizontal abduction, or overhead positions. At this level, clinicians tend to address underlying kinetic chain concerns and inflexibilities of local muscles (i.e., scapular stabilizers) while strength and conditioning specialists target muscle endurance of larger global muscles (i.e., prime movers). It is important to note that communication between the clinician and strength specialist is important in order to avoid overlap in training programs that could be deleterious to recovery.
Fig. 10.
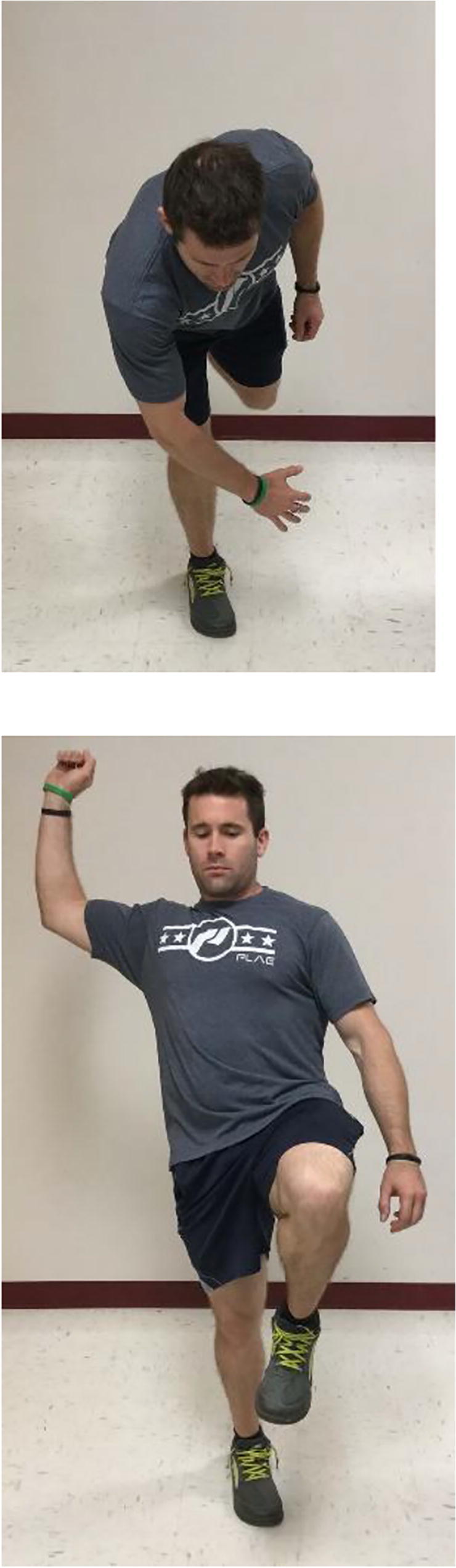
Reverse throw: the patient begins with the trunk and hip flexed and standing on a single leg (a) and then actively extends the trunk and hip in order to bring the arm into a position of 90° abduction and 90° of elbow flexion
Fig. 11.
Power position: the athlete is positioned standing with dominant arm in 90/90 position and forearm pronated (a). The athlete is instructed to rotate the trunk without moving the feet while maintaining the 90/90 position of the arm (b). The forearm should be allowed to supinate to imitate the act of the overhead throwing
Full Activity with Supplemental Conditioning
In most cases, basic preexercise regimens and postexercise maintenance are effective at staving off soreness and injury. However, it is possible for baseball athletes to have 1 or 2 underlying deficiencies ranging from soft tissue inflexibility to muscle weakness or imbalance, all of which can contribute to habitual soreness. In these cases, clinicians should diligently assess all aspects of the athlete’s regimen—mechanics during throwing, fielding, and hitting; technique during strength and conditioning maneuvers; volume and frequency of sporting drills; and off-season programming—to determine if an adjustment to current training should be employed. Furthermore, an assessment of the athlete’s prethrowing regimen should occur. The adjustments could be a modification of training interventions (more endurance-focused exercises rather than power-focused exercises), an addition of exercises not currently being performed, or a change in mechanics during drills or throwing. Pre- and postactivity measurements of G-H rotation and scapular position should be obtained because a significant percentage of throwing athletes will demonstrate large changes that can have implications for shoulder and arm kinematics [26, 28, 74].
Conclusion
Baseball throwing occurs as the result of integrated, multisegmented, sequential joint motion, and muscle activation within the kinetic chain. The scapula is a key component link within the chain through its function to maximize scapulohumeral rhythm and efficient throwing mechanics. Multiple roles of the scapula in arm function and throwing have been identified while scapular dysfunction continues to be associated with various shoulder pathologies. Evaluation and management beginning with the scapula can produce improved outcomes related to shoulder pathology in overhead athletes.
Compliance with Ethical Standards
Conflict of Interest
W. Ben Kibler and Aaron Sciascia receive royalties from Springer Publishing for co-editing 2 textbooks.
Footnotes
This article is part of the Topical Collection on Injuries in Overhead Athletes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
W. Ben Kibler, Email: wkibler@aol.com.
Aaron Sciascia, Email: aaron.sciascia@eku.edu.
References
- 1.Hickey D, Solvig V, Cavalheri V, Harrold M, Mckenna L. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: a systematic review and meta-analysis. Br J Sports Med. 2018;52:102–110. doi: 10.1136/bjsports-2017-097559. [DOI] [PubMed] [Google Scholar]
- 2.Kibler WB, Ludewig PM, McClure PW, Uhl TL, Sciascia AD. Scapula summit 2009. J Orthop Sports Phys Ther. 2009;39(11):A1–A13. doi: 10.2519/jospt.2009.030. [DOI] [PubMed] [Google Scholar]
- 3.Warner JJP, Micheli LJ, Arslanian LE, Kennedy J, Kennedy R. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome. Clin Orthop Relat Res. 1992;285(191):199. [PubMed] [Google Scholar]
- 4.Paletta GA, Warner JJP, Warren RF, Deutsch A, Altchek DW. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tears. J Shoulder Elb Surg. 1997;6:516–527. doi: 10.1016/S1058-2746(97)90084-7. [DOI] [PubMed] [Google Scholar]
- 5.Weiser WM, Lee TQ, McQuade KJ. Effects of simulated scapular protraction on anterior glenohumeral stability. Am J Sports Med. 1999;27:801–805. doi: 10.1177/03635465990270061901. [DOI] [PubMed] [Google Scholar]
- 6.Kibler WB, Uhl TL, Maddux JWQ, Brooks PV, Zeller B, McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elb Surg. 2002;11:550–556. doi: 10.1067/mse.2002.126766. [DOI] [PubMed] [Google Scholar]
- 7.Mihata T, Jun BJ, Bui CN, Hwang J, McGarry MH, Kinoshita M, et al. Effect of scapular orientation on shoulder internal impingement in a cadaveric model of the cocking phase of throwing. J Bone Joint Surg Am. 2012;94(17):1576–1583. doi: 10.2106/JBJS.J.01972. [DOI] [PubMed] [Google Scholar]
- 8.Sarkar S, Seeley S, Beranek K, Blom K, Braman JP, Ludewig PM, editors. Rotator cuff proximity to potential impinging structures during clinical impingement tests. IXth Conference of the International Shoulder Group; 2012; Wales, UK: Aberystwyth University.
- 9.McClure PW, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis: part 1: reliability. J Athl Train. 2009;44(2):160–164. doi: 10.4085/1062-6050-44.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tate AR, McClure PW, Kareha S, Irwin D, Barbe MF. A clinical method for identifying scapular dyskinesis: part 2: validity. J Athl Train. 2009;44(2):165–173. doi: 10.4085/1062-6050-44.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the "scapula summit". Br J Sports Med. 2013;47:877–885. doi: 10.1136/bjsports-2013-092425. [DOI] [PubMed] [Google Scholar]
- 12.Uhl TL, Kibler WB, Gecewich B, Tripp BL. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy. 2009;25(11):1240–1248. doi: 10.1016/j.arthro.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 13.Kibler WB. The role of the scapula in athletic function. Am J Sports Med. 1998;26:325–337. doi: 10.1177/03635465980260022801. [DOI] [PubMed] [Google Scholar]
- 14.Kibler WB, Sciascia AD, Dome DC, Hester PW, Jacobs C. Clinical utility of new and traditional exam tests for biceps and superior glenoid labral injuries. Am J Sports Med. 2009;37(9):1840–1847. doi: 10.1177/0363546509332505. [DOI] [PubMed] [Google Scholar]
- 15.McMullen J, Uhl TL. A kinetic chain approach for shoulder rehabilitation. J Athl Train. 2000;35(3):329–337. [PMC free article] [PubMed] [Google Scholar]
- 16.Crossley KM, Zhang WJ, Schache AG, Bryant A, Cowan SM. Performance on the single-leg squat task indicates hip abductor muscle function. Am J Sports Med. 2011;39(4):866–873. doi: 10.1177/0363546510395456. [DOI] [PubMed] [Google Scholar]
- 17.Kibler WB, Press J, Sciascia AD. The role of core stability in athletic function. Sports Med. 2006;36(3):189–198. doi: 10.2165/00007256-200636030-00001. [DOI] [PubMed] [Google Scholar]
- 18.Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther. 2000;80(3):276–291. doi: 10.1093/ptj/80.3.276. [DOI] [PubMed] [Google Scholar]
- 19.Ludewig PM, Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009;39(2):90–104. doi: 10.2519/jospt.2009.2808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ogston JB, Ludewig PM. Differences in 3-dimensional shoulder kinematics between persons with multidirectional instability and asymptomatic controls. Am J Sports Med. 2007;35:1361–1370. doi: 10.1177/0363546507300820. [DOI] [PubMed] [Google Scholar]
- 21.Timmons MK, Thigpen CA, Seitz AL, Karduna AR, Michener LA. Scapular kinematics and subacromial impingement syndrome: a meta-analysis. J Sport Rehabil. 2012;21(4):354–370. doi: 10.1123/jsr.21.4.354. [DOI] [PubMed] [Google Scholar]
- 22.Green RA, Taylor NF, Watson L, Ardern C. Altered scapular position in elite young cricketers with shoulder problems. J Sci Med Sport. 2013;16(1):22–27. doi: 10.1016/j.jsams.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 23.Reuther KE, Thomas SJ, Tucker JJ, Yannascoli SM, Caro AC, Vafa RP, Liu SS, Gordon JA, Bhatt PR, Kuntz AF, Soslowsky LJ. Scapular dyskinesis is detrimental to shoulder tendon properties and joint mechanics in a rat model. J Orthop Res. 2014;32(11):1436–1443. doi: 10.1002/jor.22693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology part I: pathoanatomy and biomechanics. Arthroscopy. 2003;19(4):404–420. doi: 10.1053/jars.2003.50128. [DOI] [PubMed] [Google Scholar]
- 25.Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy. 2003;19(6):641–661. doi: 10.1016/S0749-8063(03)00389-X. [DOI] [PubMed] [Google Scholar]
- 26.Reinold MM, Wilk KE, Macrina LC, Sheheane C, Dun S, Fleisig GS, et al. Changes in shoulder and elbow passive range of motion after pitching in professional baseball players. Am J Sports Med. 2008;36(3):523–527. doi: 10.1177/0363546507308935. [DOI] [PubMed] [Google Scholar]
- 27.Kibler WB, Sciascia AD, Thomas SJ. Glenohumeral internal rotation deficit: pathogenesis and response to acute throwing. Sports Med Arthrosc Rev. 2012;20(1):34–38. doi: 10.1097/JSA.0b013e318244853e. [DOI] [PubMed] [Google Scholar]
- 28.Kibler WB, Sciascia AD, Moore SD. An acute throwing episode decreases shoulder internal rotation. Clin Orthop Relat Res. 2012;470:1545–1551. doi: 10.1007/s11999-011-2217-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Myers JB, Laudner KG, Pasquale MR, Bradley JP, Lephart SM. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2006;34:385–391. doi: 10.1177/0363546505281804. [DOI] [PubMed] [Google Scholar]
- 30.Laudner KG, Myers JB, Pasquale MR, Bradley JP, Lephart SM. Scapular dysfunction in throwers with pathologic internal impingement. J Orthop Sports Phys Ther. 2006;36(7):485–494. doi: 10.2519/jospt.2006.2146. [DOI] [PubMed] [Google Scholar]
- 31.Laudner KG, Stanek JM, Meister K. Differences in scapular upward rotation between baseball pitchers and position players. Am J Sports Med. 2007;35:2091–2095. doi: 10.1177/0363546507305098. [DOI] [PubMed] [Google Scholar]
- 32.Gumina S, Carbone S, Postacchini F. Scapular dyskinesis and SICK scapula syndrome in patients with chronic type III acromioclavicular dislocation. Arthroscopy. 2009;25(1):40–45. doi: 10.1016/j.arthro.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 33.Shields E, Behrend C, Beiswenger T, Strong B, English C, Maloney M, Voloshin I. Scapular dyskinesis following displaced fractures of the middle clavicle. J Shoulder Elb Surg. 2015;24(12):e331–e336. doi: 10.1016/j.jse.2015.05.047. [DOI] [PubMed] [Google Scholar]
- 34.McKee MD, Pedersen EM, Jones C, Stephen DJG, Kreder HJ, Schemitsch EH, Wild LM, Potter J. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg Am. 2006;88:35–40. doi: 10.2106/JBJS.D.02795. [DOI] [PubMed] [Google Scholar]
- 35.Oki S, Matsumura N, Iwamoto W, Ikegami H, Kiriyama Y, Nakamura T, Toyama Y, Nagura T. Acromioclavicular joint ligamentous system contributing to clavicular strut function: a cadaveric study. J Shoulder Elb Surg. 2013;22(10):1433–1439. doi: 10.1016/j.jse.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 36.Kuhn J, Plancher K, Hawkins R. Scapular winging. J Am Acad Orthop Surg. 1995;3:319–325. doi: 10.5435/00124635-199511000-00002. [DOI] [PubMed] [Google Scholar]
- 37.Kibler WB, Sciascia A, Wilkes T. Scapular dyskinesis and its relation to shoulder injury. J Am Acad Orthop Surg. 2012;20(6):364–372. doi: 10.5435/JAAOS-20-06-364. [DOI] [PubMed] [Google Scholar]
- 38.Kibler WB, Kuhn JE, Wilk KE, Sciascia AD, Moore SD, Laudner KG, Ellenbecker T, Thigpen C, Uhl T. The disabled throwing shoulder - spectrum of pathology: 10 year update. Arthroscopy. 2013;29(1):141–161. doi: 10.1016/j.arthro.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 39.Fedoriw WW, Ramkumar P, McCulloch PC, Lintner DM. Return to play after treatment of superior Labral tears in professional baseball players. Am J Sports Med. 2014;42(5):1155–1160. doi: 10.1177/0363546514528096. [DOI] [PubMed] [Google Scholar]
- 40.Edwards SL, Lee JA, Bell JE, Packer JD, Ahmad CS, Levine W, et al. Nonoperative treatment of superior labrum anterior posterior tears: improvements in pain, function, and quality of life. Am J Sports Med. 2010;38(7):1456–1461. doi: 10.1177/0363546510370937. [DOI] [PubMed] [Google Scholar]
- 41.Kibler WB. Management of the scapula in glenohumeral instability. Tech Should Elbow Surg. 2003;4(3):89–98. doi: 10.1097/00132589-200309000-00001. [DOI] [Google Scholar]
- 42.Burkhead WZ, Rockwood CA. Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am. 1992;74-A(6):890–896. doi: 10.2106/00004623-199274060-00010. [DOI] [PubMed] [Google Scholar]
- 43.Wilk KE, Macrina LC, Reinold MM. Non-operative rehabilitation for traumatic and atraumatic glenohumeral instability. N Am J Sports Phys Ther. 2006;1(1):16–31. [PMC free article] [PubMed] [Google Scholar]
- 44.Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35(4):227–238. doi: 10.2519/jospt.2005.35.4.227. [DOI] [PubMed] [Google Scholar]
- 45.Ellenbecker TS, Cools A. Rehabilitation of shoulder impingement syndrome and rotator cuff injuries: an evidence-based review. Br J Sports Med. 2010;44:319–327. doi: 10.1136/bjsm.2009.058875. [DOI] [PubMed] [Google Scholar]
- 46.Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elb Surg. 2009;18:138–160. doi: 10.1016/j.jse.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 47.Sciascia A, Karolich D. A comprehensive approach for non-operative treatment of the rotator cuff. Curr Phys Med Rehabil Rep. 2013;1(1):29–37. doi: 10.1007/s40141-012-0002-x. [DOI] [Google Scholar]
- 48.Sahara W, Sugamoto K, Murai M, Yoshikawa H. Three-dimensional clavicular and acromioclavicular rotations during arm abduction using vertically open MRI. J Orthop Res. 2007;25:1243–1249. doi: 10.1002/jor. [DOI] [PubMed] [Google Scholar]
- 49.Kibler WB, Sciascia AD, Morris BJ, Dome DC. Treatment of symptomatic acromioclavicular joint instability by a docking technique: clinical indications, surgical technique, and outcomes. Arthroscopy. 2017;33:696–708. doi: 10.1016/j.arthro.2016.08.023. [DOI] [PubMed] [Google Scholar]
- 50.Kibler WB, Sciascia AD. Kinetic chain contributions to elbow function and dysfunction in sports. Clin Sports Med. 2004;23(4):545–552. doi: 10.1016/j.csm.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 51.Tripp BL, Boswell LL, Gansneder BM, Shultz SJ. Functional fatigue decreases three-dimensional multi-joint position reproduction acuity in the overhead throwing athlete. J Athl Train. 2004;39(4):316–320. [PMC free article] [PubMed] [Google Scholar]
- 52.Tripp B, Uhl TL, Mattacola CG, Srinivasan C, Shapiro R. Functional multijoint position reproduction acuity in overhead athletes. J Athl Train. 2006;41(2):146–153. [PMC free article] [PubMed] [Google Scholar]
- 53.Ebaugh DD, McClure PW, Karduna AR. Effects of shoulder muscle fatigue caused by repetitive overhead activities on scapulothoracic and glenohumeral kinematics. J Electromyogr Kinesiol. 2006;16:224–235. doi: 10.1016/j.jelekin.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 54.Wilk KE, Macrina LC, Fleisig GS, Aune KT, Porterfield RA, Harker P, et al. Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers: a prospective study. Am J Sports Med. 2014;42:2075–2081. doi: 10.1177/0363546514538391. [DOI] [PubMed] [Google Scholar]
- 55.Itami Y, Mihata T, McGarry MH, Lin CC, Patel NA, Kantor A, Neo M, Lee TQ. Effect of increased scapular internal rotation on glenohumeral external rotation and elbow valgus load in the late cocking phase of throwing motion. Am J Sports Med. 2018;46:3182–3188. doi: 10.1177/0363546518800267. [DOI] [PubMed] [Google Scholar]
- 56.Hirashima M, Kudo K, Watarai K, Ohtsuki T. Control of 3D limb dynamics in unconstrained overarm throws of different speeds performed by skilled baseball players. J Neurophysiol. 2007;97(1):680–691. doi: 10.1152/jn.00348.2006. [DOI] [PubMed] [Google Scholar]
- 57.Hirashima M, Yamane K, Nakamura Y, Ohtsuki T. Kinetic chain of overarm throwing in terms of joint rotations revealed by induced acceleration analysis. J Biomech. 2008;41:2874–2883. doi: 10.1016/j.jbiomech.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 58.Sciascia A, Cromwell R. Kinetic chain rehabilitation: a theoretical framework. Rehabil Res Pract. 2012;2012:1–9. doi: 10.1155/2012/853037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sciascia Aaron, Monaco Michele. Elite Techniques in Shoulder Arthroscopy. Cham: Springer International Publishing; 2015. When Is the Patient Truly “Ready to Return,” a.k.a. Kinetic Chain Homeostasis; pp. 317–327. [Google Scholar]
- 60.Sciascia AD, Thigpen CA, Namdari S, Baldwin K. Kinetic chain abnormalities in the athletic shoulder. Sports Med Arthrosc Rev. 2012;20(1):16–21. doi: 10.1097/JSA.0b013e31823a021f. [DOI] [PubMed] [Google Scholar]
- 61.Bouisset S, Zattara M. A sequence of postural movements precedes voluntary movement. Neurosci Lett. 1981;22:263–270. doi: 10.1016/0304-3940(81)90117-8. [DOI] [Google Scholar]
- 62.Hodges PW, Richardson CA. Feedforward contraction of transversus abdominus is not influenced by the direction of arm movement. Exp Brain Res. 1997;114:362–370. doi: 10.1007/PL00005644. [DOI] [PubMed] [Google Scholar]
- 63.Lippitt S, Matsen Iii FA. Mechanisms of glenohumeral joint stability. Clin Orthop Relat Res. 1993;291:20–28. [PubMed] [Google Scholar]
- 64.Lippitt S, Vanderhooft JE, Harris SL, Sidles JA, Harryman Ii DT, Matsen Iii FA. Glenohumeral stability from concavity-compression: a quantitative analysis. J Shoulder Elb Surg. 1993;2(1):27–35. doi: 10.1016/S1058-2746(09)80134-1. [DOI] [PubMed] [Google Scholar]
- 65.Smith J, Kotajarvi BR, Padgett DJ, Eischen JJ. Effect of scapular protraction and retraction on isometric shoulder elevation strength. Arch Phys Med Rehabil. 2002;83:367–370. doi: 10.1053/apmr.2002.29666. [DOI] [PubMed] [Google Scholar]
- 66.Smith J, Dietrich CT, Kotajarvi BR, Kaufman KR. The effect of scapular protraction on isometric shoulder rotation strength in normal subjects. J Shoulder Elb Surg. 2006;15:339–343. doi: 10.1016/j.jse.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 67.Kibler WB, Sciascia AD, Dome DC. Evaluation of apparent and absolute supraspinatus strength in patients with shoulder injury using the scapular retraction test. Am J Sports Med. 2006;34(10):1643–1647. doi: 10.1177/0363546506288728. [DOI] [PubMed] [Google Scholar]
- 68.Tate AR, McClure P, Kareha S, Irwin D. Effect of the scapula reposition test on shoulder impingement symptoms and elevation strength in overhead athletes. J Orthop Sports Phys Ther. 2008;38(1):4–11. doi: 10.2519/jospt.2008.2616. [DOI] [PubMed] [Google Scholar]
- 69.De May K, Danneels L, Cagnie B, Huyghe L, Seyns E, Cools AM. Conscious correction of scapular orientation in overhead athletes performing selected shoulder rehabilitation exercises: the effect on trapezius muscle activation measured by surface electromyography. J Orthop Sports Phys Ther. 2013;43(1):3–10. doi: 10.2519/jospt.2013.4283. [DOI] [PubMed] [Google Scholar]
- 70.Ellenbecker TS, Manske R, Davies GJ. Closed kinetic chain techniques of the upper extremities. Orthop Phys Ther Clin N Am. 2000;9(2):219–229. [Google Scholar]
- 71.Kibler WB, Livingston B. Closed-chain rehabilitation for upper and lower extremities. J Am Acad Orthop Surg. 2001;9(6):412–421. doi: 10.5435/00124635-200111000-00006. [DOI] [PubMed] [Google Scholar]
- 72.Kibler WB, Sciascia AD, Uhl TL, Tambay N, Cunningham T. Electromyographic analysis of specific exercises for scapular control in early phases of shoulder rehabilitation. Am J Sports Med. 2008;36(9):1789–1798. doi: 10.1177/0363546508316281. [DOI] [PubMed] [Google Scholar]
- 73.De May K, Danneels L, Cagnie B, Cools A. Are kinetic chain rowing exercises relevant in shoulder and trunk injury prevention training? Br J Sports Med. 2011;45(4):320. [Google Scholar]
- 74.Wilk KE, Macrina LC, Fleisig GS, Porterfield R, Simpson Ii CD, Harker P, et al. Loss of internal rotation and the correlation to shoulder injuries in professional baseball pitchers. Am J Sports Med. 2011;39(2):329–335. doi: 10.1177/0363546510384223. [DOI] [PubMed] [Google Scholar]