Abstract
Background
Continuous low-intensity ultrasound (cLIUS) facilitates the chondrogenic differentiation of human mesenchymal stromal cells (MSCs) in the absence of exogenously added transforming growth factor-beta (TGFβ) by upregulating the expression of transcription factor SOX9, a master regulator of chondrogenesis. The present study evaluated the molecular events associated with the signaling pathways impacting SOX9 gene and protein expression under cLIUS.
Methods
Human bone marrow-derived MSCs were exposed to cLIUS stimulation at 14 kPa (5 MHz, 2.5 Vpp) for 5 min. The gene and protein expression of SOX9 was evaluated. The specificity of SOX9 upregulation under cLIUS was determined by treating the MSCs with small molecule inhibitors of select signaling molecules, followed by cLIUS treatment. Signaling events regulating SOX9 expression under cLIUS were analyzed by gene expression, immunofluorescence staining, and western blotting.
Results
cLIUS upregulated the gene expression of SOX9 and enhanced the nuclear localization of SOX9 protein when compared to non-cLIUS-stimulated control. cLIUS was noted to enhance the phosphorylation of the signaling molecule ERK1/2. Inhibition of MEK/ERK1/2 by PD98059 resulted in the effective abrogation of cLIUS-induced SOX9 expression, indicating that cLIUS-induced SOX9 upregulation was dependent on the phosphorylation of ERK1/2. Inhibition of integrin and TRPV4, the upstream cell-surface effectors of ERK1/2, did not inhibit the phosphorylation of ERK1/2 and therefore did not abrogate cLIUS-induced SOX9 expression, thereby suggesting the involvement of other mechanoreceptors. Consequently, the effect of cLIUS on the actin cytoskeleton, a mechanosensitive receptor regulating SOX9, was evaluated. Diffused and disrupted actin fibers observed in MSCs under cLIUS closely resembled actin disruption by treatment with cytoskeletal drug Y27632, which is known to increase the gene expression of SOX9. The upregulation of SOX9 under cLIUS was, therefore, related to cLIUS-induced actin reorganization. SOX9 upregulation induced by actin reorganization was also found to be dependent on the phosphorylation of ERK1/2.
Conclusions
Collectively, preconditioning of MSCs by cLIUS resulted in the nuclear localization of SOX9, phosphorylation of ERK1/2 and disruption of actin filaments, and the expression of SOX9 was dependent on the phosphorylation of ERK1/2 under cLIUS.
Electronic supplementary material
The online version of this article (10.1186/s13287-019-1532-2) contains supplementary material, which is available to authorized users.
Background
As cartilage does not have the innate potential to regenerate, lesions frequently result in large-scale degenerative changes and osteoarthritis (OA) [1, 2]. The clinical outcomes of current strategies of cartilage repair autologous chondrocyte implantation (ACI) or matrix-assisted autologous chondrocyte implantation (MACI) are compromised by the phenotypic instability of expanded autologous chondrocytes ex vivo [3, 4] that leads to graft hypertrophy [5] and the formation of a mechanically inferior tissue in vivo. Therefore, regenerative approaches that employ progenitor cells such as mesenchymal stromal cells (MSCs) to improve cartilage repair outcomes are of interest.
Taking cues from the in vivo regulation of MSC chondrogenesis, current in vitro protocols include select growth factors (i.e., TGFβ) for differentiation of MSCs [6]. However, long-term conditioning of MSCs with TGFβ induces hypertrophy [5, 7] and calcification [8] upon terminal differentiation, leading to endochondral ossification instead of hyaline cartilage formation. Thus, chondroinductive protocols that do not rely on growth factors are of interest for the eventual development of ex vivo differentiation protocols for ACI and in situ repair strategies like microfracture.
Previously, a variety of biophysical stimuli, including mechanical stimulation, have been extensively studied in directing the differentiation of MSCs both in the absence and presence of growth factors [9–15]. Synergistic application of TGFβ with biomechanical forces yielded superior chondrogenic differentiation of MSCs in vitro, as evidenced by elevated expression of chondrocyte markers (Collagen II, SOX9, and aggrecan) [13, 14, 16]. However, as the mechanical stimulus was applied concurrently with TGFβ, the chondroinductive potential of the mechanical stimulus alone becomes indiscernible. Therefore, studies that critically examine MSC chondrogenesis in the absence of exogenously added growth factors are of significance.
In that regard, electrical stimulation and dynamic compressive loading have been documented to induce in vitro MSC chondrogenesis without the assistance of growth factors, as measured by the increased expression of chondrocyte markers, biochemical content, and mechanical stiffness over controls [12, 17–19], albeit the outcomes were inferior when compared to TGFβ-preconditioning [20–22]. Therefore, alternative methods of mechanical stimulation, including low-intensity ultrasound (LIUS), were explored for preconditioning MSCs toward a chondrogenic phenotype [23–25].
Low-intensity ultrasound (0.8 to 1.5 MHz, < 200 mW/cm2), applied as pulsed (pLIUS) or continuous (cLIUS) wave, has been documented to enhance the chondrocyte phenotype [26–28], improve cartilage repair [29, 30], and induce MSC chondrogenesis in vitro [25, 31] and in vivo [32], notably in the absence of exogenous chondroinductive biochemical factors [24, 33–35]. However, the growth factor-independent chondrogenic effect of pLIUS and cLIUS was either non-existent [31] or modest as evidenced by marginal increases in GAG and collagen content in 3D cultures of differentiated MSCs [34]. Differently from previous studies employing pLIUS or cLIUS at empirically derived frequencies (~ 1 MHz), theoretical modeling and experimental investigations conducted in our laboratory established that cLIUS couples more energy than pLIUS and cellular bioeffects are maximized at the cell resonant frequency of 5 MHz [36, 37]. For example, the long-term culture of MSC constructs receiving pLIUS stimulation at 1.5 MHz, a frequency outside the resonant bandwidth [36, 37], produced a substantially lower chondrogenic effect as evidenced by decreased biochemical content (GAG and collagen II) when compared to cLIUS stimulation at 5 MHz [34]. Additionally, the exposure of MSC constructs to cLIUS (5 MHz) for 8 weeks prevented the hypertrophic differentiation of MSCs by downregulating the expression of collagen X, a hypertrophic marker while sustaining the elevated expression of hyaline cartilage markers (SOX9 and collagen II) [38]. Taken together, cLIUS at 5 MHz was noted to be chondroinductive by acting as a stable inducer of chondrogenic differentiation in MSCs. Enhanced expression of the transcription factor SOX9, the master regulator of chondrogenesis [39–42], was observed in MSCs under pLIUS or cLIUS stimulation [24, 35, 38]; however, the underlying signaling events governing the upregulation of SOX9 are poorly understood.
In chondrocytes, a variety of signaling molecules are involved in the regulation of SOX9 [39, 41–45]. TGFβ induces chondrogenesis by regulating the phosphorylation of SOX9 through the SMAD (canonical) and p38 MAPK pathway (non-canonical) [43, 46, 47]. Mechanical stimulation by compressive loading was also reported to regulate the phosphorylation of SOX9 during MSC chondrogenesis by PKA [48] or by the autocrine TGFβ/SMAD [16] pathways. Despite the evidence of MSC chondrogenesis under mechanical stimulation in the absence of exogenously added TGFβ [20, 34, 49], the involvement of signaling cascades that regulate the gene expression of SOX9 is limited.
Long-term culture of scaffold-seeded with MSCs under cLIUS at 5 MHz, yielded a sustained and elevated expression of collagen II and glycosaminoglycan (GAG), notably in the absence of exogenously added growth factor TGFβ [38]. Our collective data indicated that cLIUS was chondroinductive as evidenced by the expression of cartilage-specific markers, notably SOX9 [41, 40, 58, 73]. Thus, gaining a better understanding of the molecular events involved in the regulation of the expression of SOX9 in MSCs under cLIUS can help develop preconditioning protocols based on cLIUS. We postulate that cell-surface receptors (integrin, TRPV4), key intracellular signaling molecules (ERK1/2, PKA), and the actin cytoskeleton are involved in transducing cLIUS stimulus leading to the expression of SOX9 in MSCs and are schematically illustrated in Fig. 1. To our knowledge, this is the first study that seeks to elucidate the underlying signaling events that regulate SOX9 upon cLIUS stimulation in MSCs. Thus, the assessment of select signaling molecules that are involved in regulating SOX9 under cLIUS was undertaken. Specificity was established using small molecule inhibitors of select signaling molecules. The study was motivated by the potential of cLIUS, a clinically translatable mode of stimulation in cartilage regeneration and rehabilitation.
Fig. 1.
Schematic representation of the possible SOX9-directed pathways under cLIUS stimulation. The diagram shows putative signaling pathways that may be activated upon cLIUS stimulation in MSCs leading to the gene expression of SOX9 and its target gene COL2A1. Select intracellular signaling molecules (ERK1/2 and PKA), upstream effectors (integrin and TRPV4), and the actin cytoskeleton were targeted by pharmacological inhibition to investigate the involvement of integrin-MAPK or calcium signaling through TRPV4 pathways leading to SOX9 upregulation under cLIUS in MSCs
Methods
2D culture of MSCs
Human MSCs were purchased from Lonza (PT-2501, Walkersville, MD, USA) and expanded in alpha-Minimum Essential Medium (α-MEM) supplemented with 10% MSC-qualified fetal bovine serum (FBS) (Gibco, USA), 1× Glutamax (Gibco, USA), and 1× antibiotic-antimycotic solution (Gibco, USA) in a CO2 incubator at 37 °C, 5% carbon dioxide, and 99% humidity. MSCs harvested from passage 4–5 were employed in all experiments. MSCs were plated in 12-well TCP at following seeding densities: 1 × 105 cells/well (RNA and protein extractions following treatment with inhibitors and non-treated controls), 1 × 104 cells/well (for immunofluorescence studies following treatment with inhibitors and non-treated controls), 2 × 104 cells/well (for RNA decay assay). All treatments with inhibitors and/or cLIUS were conducted after 24 h of initial seeding of MSCs in TCP.
Treatment with inhibitors
MSCs were cultured in 12-well TCPs at 1 × 105 seeding density per well (for RNA and protein extraction) with α-MEM medium supplemented with 10% MSC-qualified FBS, 1× Glutamax (Gibco, USA), and 1× antibiotic-antimycotic solution. For immunofluorescence staining, the 1 × 104 cells per well were seeded onto sterilized 15-mm coverslips placed at the bottom of each well of a 12-well TCP. The MSCs were serum-starved prior to treatment with inhibitors by removing the growth medium containing 10% MSC-qualified FBS and replacing it with low serum medium containing 1% MSC-qualified FBS overnight. The serum-starved cells were incubated for 4 h in medium containing inhibitors solubilized in DMSO: 100 μg/ml GRGDSP (Sigma, USA), 50 μM PD98059 (Cell Signaling Technology, USA), 30 μM RN1738 (Tocris, USA), and 10 μM Y-27632 (Cell Signaling Technology, USA) separately for the inhibition of integrin, MEK/ERK1/2, and ROCK respectively prior to cLIUS stimulation. Non-cLIUS-treated MSCs incubated in medium containing DMSO (0.125% v/v) served as controls.
cLIUS treatment regimen of 2D MSC cultures
Non-focused immersion transducers (Panametrics V300, 12.7 mm diameters, Panametrix, Waltham, MA, USA) were used to apply cLIUS (< 30 mW/cm2) to MSCs plated in 12-well TCP. The volume of medium per well was maintained at 4 ml to ensure complete immersion of ultrasound transducers in the well for effective propagation of ultrasound waves. Care was taken to avoid contact of the transducer surface to the cell layer at the bottom of the TCP. For cLIUS frequency study, cLIUS was applied at 5 MHz (2.5 Vpp), 2 MHz (6 Vpp), or 8 MHz (9.5 Vpp) at constant pressure amplitude of 14 kPa one time for 5 min. For inhibitor studies and RNA decay assay, cLIUS was applied one time for 5 min at 5 MHz (2.5 Vpp) with constant pressure amplitude of 14 kPa and subjected to qRT-PCR. For inhibitor studies, western blotting and immunofluorescence staining were conducted in addition to qRT-PCR following cLIUS stimulation.
Quantitative RT-PCR (qRT-PCR)
Total RNA was isolated after 1 h upon cLIUS stimulation of MSCs in 2D. MSCs that received no cLIUS stimulation served as controls. Briefly, the medium was removed and cells were washed with HBSS (Gibco, USA). Cells were then lysed by adding 100 μl of Trizol (Invitrogen, USA) per well. RNA was then extracted from the homogenized cell lysates using the RNeasy Mini Kit (Qiagen, USA) as per manufacturer’s protocol. Cell lysates pooled from two wells served as one replicate. Three such replicates from three independent experiments were used for analysis (n = 3). qRT-PCR was carried out in Realplex™ real-time PCR system (Eppendorf, USA) using TaqMan® RNA-to-CT™ 1-Step Kit (Life Technologies, USA) as per the manufacturer’s guidelines. TaqMan® probes (Life Technologies, USA) for SOX9 (Hs00165814_m1) was used to quantify mRNA expression of SOX9. The expression of mRNA transcripts was normalized to the housekeeping gene, GAPDH (Hs02786624_g1); expression and relative expression levels were calculated using the 2−ΔΔCt method.
Protein isolation and western blotting
Following treatment with inhibitors and/or cLIUS stimulation in 2D MSC cultures, total protein was isolated within 15 min of cLIUS stimulation (n = 3 biological replicates per group) as phosphorylation events are transient in nature. MSCs that received no cLIUS stimulation in the presence or absence of inhibitors served as respective controls. Briefly, the medium was removed, and cells were rinsed thoroughly in HBSS (Gibco, USA). The cells were lysed by adding 100 μl of Pierce IP lysis buffer (Thermo Scientific, Rockford, IL, USA) supplemented with 1× Halt protease and phosphatase inhibitor cocktail and 1X EDTA (Thermo Scientific, Rockford, IL, USA) per well. The cell lysates were centrifuged at 13,000g for 15 min, and the supernatant was used for protein quantification by standard BCA assay (QuantiPro™ BCA Assay Kit, Sigma-Aldrich, USA) as per the manufacturer’s guidelines. SDS-PAGE was conducted using NuPAGE gels (Invitrogen, USA) per the manufacturer’s instructions. Briefly, 20 μg protein in NuPAGE 4X lithium dodecyl sulfate sample buffer and NuPAGE 10× sample reducing agent was denatured at 75 °C for 15 min and loaded onto wells of 4–12% NuPAGE bis-tris gels, and electrophoresis was carried out. Proteins separated by SDS-PAGE were then transferred onto the PVDF membrane. Membranes were then blocked with 2% goat serum in 1× TBST (tris buffer saline with 0.1% tween20) for 2 h and incubated separately with primary antibodies: rabbit anti-phospho-p44/42 MAPK (ERK1/2) and p44/42 MAPK (ERK1/2) (catalog numbers 4377 and 4695, Cell Signaling Technology, USA) at a dilution of 1:1000 overnight at 4 °C. β-actin (catalog number 8H10D10, Cell Signaling Technology) or α-tubulin (catalog number 2144S, Cell Signaling Technology) was used as a loading control at a dilution of 1:5000. Following copious washing in TBST, the blots were incubated with HRP conjugated anti-rabbit IgG (1:5000 dilution, catalog number A0525, Sigma-Aldrich, USA) or anti-mouse IgG (1:10000 dilution, catalog number 12-349, Millipore-Sigma) for 2 h at room temperature. The blots were washed in TBST and then visualized by incubating with Clarity™ western ECL kit (Bio-Rad, USA) as per manufacturer’s instructions, finally captured with hyperfilm™ ECL (GE Healthcare Amersham™, USA). The blots were quantified by ImageJ™ software.
Immunofluorescence staining
MSCs were seeded at a density of 1 × 104 cells per coverslip per well in 12-well TCP. Immediately after treatment with inhibitors with or without cLIUS stimulation (5 min), MSCs were fixed in 4% paraformaldehyde for 20 min (n = 3). The cells were then rinsed in PBS and blocked with 2% goat serum in 1× TBST for 2 h. The blocking solution was removed, and the cells were incubated with a primary monoclonal antibody raised in rabbit against SOX9 (1:200 dilution, Catalog number 82630, Cell Signaling Technology, USA) at 4 °C overnight. After primary antibody incubation, the cells were washed with 1× TBST and incubated for 2 h at room temperature with goat anti-rabbit IgG conjugated with Alexa Fluor 488 (1:50 dilution, catalog number ab150077, Abcam, USA) followed by incubation with phalloidin-Alexa Fluor 594 (1:50 dilution, catalog number A12381, Molecular Probes, USA) for 30 min and staining with 300 nM DAPI (D1306, Molecular Probes, USA) for 5 min. The coverslips were rinsed and mounted onto glass slides with Prolong™ Gold antifade mountant (Invitrogen, USA) and viewed under a confocal microscope (Olympus IX81) at a magnification of ×60 (z step size = 5 μm). The fluorescence staining intensity in the images (n = 10–20 per group) from three independent experiments was quantified by measuring the integrated density of the cells using ImageJ software (NIH, Bethesda, USA). Quantification of actin filament number and length were measured by FilaQuant software (the University of Rostock, Institute of Mathematics, Mathematical Optimization) per user guidelines.
Intracellular Ca++staining
MSCs were plated at an initial seeding density of 2 × 105 cells/well. MSCs were pre-treated with the Fluo-4-AM probe (Catalog number F14201, Thermo Fisher Scientific, USA) at a concentration of 3 μM/ml in recording medium (20 mM HEPES, 115 mM NaCl, 5.4 mM KCl, 0.8 mM MgCl2, 1.8 mM CaCl2, 13.8 mM glucose) for 20 min, after which the medium was replaced with recording medium without Fluo-4-AM. Intracellular calcium was visualized 5 min after cLIUS stimulation (5 MHz. 2.5 Vpp, 5 min) under a fluorescence microscope at × 5 magnification (n = 3). Non-cLIUS-stimulated MSCs served as controls (n = 3).
RNA decay assay
MSCs were cultured in 12-well TCP at a seeding density of 2 × 104 cells per well in DMEM supplemented with 10% FBS, 1× antibiotic-antimycotic solution, and 25 μg/ml ascorbic acid. For RNA decay study, medium containing FBS was removed and replaced with a serum-free medium. cLIUS was then applied to the wells at 5 MHz and 2.5 Vpp for 15 min (n = 3). After cLIUS stimulation, the medium was immediately removed and replaced with serum-free DMEM containing 5 μg/ml actinomycin D (Cell Signaling Technology, USA). At each time point of 0 h, 0.5 h, 1 h, and 2 h post-actinomycin D treatment, the medium was removed and followed by total RNA extraction and qRT-PCR. Non-cLIUS-treated samples served as controls. Parallelly, MSCs were stimulated with cLIUS at 5 MHz and 2.5 Vpp for 15 min without subsequent actinomycin D treatment, and RNA was extracted at the aforementioned time points and subjected to qRT-PCR for measuring the relative amount of SOX9 mRNA transcripts in the presence and absence of actinomycin D.
The ΔΔCt method is used for calculations. Ct values were first normalized to GAPDH and then normalized to the respective samples before the addition of actinomycin D, which were set to 1 [50]. This gives the decay of SOX9 mRNA over time. To calculate the amount of SOX9 mRNA transcripts at each time point, the Ct values (normalized to GAPDH first) of samples in the presence of actinomycin D were normalized to the Ct value of the sample in the absence of actinomycin D at respective time points.
3D encapsulation and culture of MSCs
MSCs were encapsulated in hyaluronan-based hydrogel using the HyStem-C hydrogel kit purchased from ESI-BIO (CA, USA) as per manufacturer’s instructions with slight modifications. Briefly, the hydrogel was prepared by mixing 2% Glycosil, 1% Gelin-S, and 4% Extralink solution supplied in the kit. Passage 4 MSCs were then harvested and resuspended in the hydrogel solution at an encapsulation density of 5 × 106 cells/ml hydrogel. MSC-laden hydrogels were cast in sterile cylindrical inserts (4 mm height, 3 mm diameter) by pipetting 300 μl of the hydrogel-MSC mixture into the inserts. The inserts were then carefully removed after the solidification of MSC-laden hydrogels which typically ensued within (two constructs per well) were cultured in six-well tissue culture plates (TCP) in DMEM-high glucose medium supplemented with 10% fetal bovine serum (FBS) (Gibco, USA), 100 nM dexamethasone, 50 μg/ml ascorbic acid, and 1× antibiotic-antimycotic solution (Gibco, USA) at 37 °C and 5% CO2 with or without cLIUS for 6 weeks.
cLIUS treatment regimen of 3D MSC constructs
Six-well TCPs containing MSC-hydrogel constructs were placed in plate holders of a cLIUS-assisted incubator developed at the Department of Chemical Engineering, University of Nebraska-Lincoln (UNL), USA, with operating procedures detailed elsewhere [51]. cLIUS was applied to the plates at 5 MHz frequency and 2.5 Vpp (14 kPa) for 20 min per application at four applications/day for a period of 6 weeks. At the end of 6 weeks, the constructs (n = 3) were fixed in 10% neutral buffered saline prior to immunohistochemistry. Non-cLIUS-treated constructs served as controls and were cultured in a CO2 incubator (37 °C and 5% CO2).
Statistical analyses
The data are expressed as average ± standard deviation where the average is calculated from three independent experiments conducted in triplicate (n = 3). For qRT-PCR, ImageJ™, and FilaQuant data, Welch’s test was used for pair-wise comparisons of cLIUS-stimulated and non-cLIUS-stimulated control groups. For western blotting data and RNA decay assay, one-way analysis of variance (ANOVA) followed by post hoc Tukey’s test was employed for pair-wise comparisons. Statistically significant data (α = 0.5) was indicated by p values.
Results
cLIUS upregulates load-inducible genes
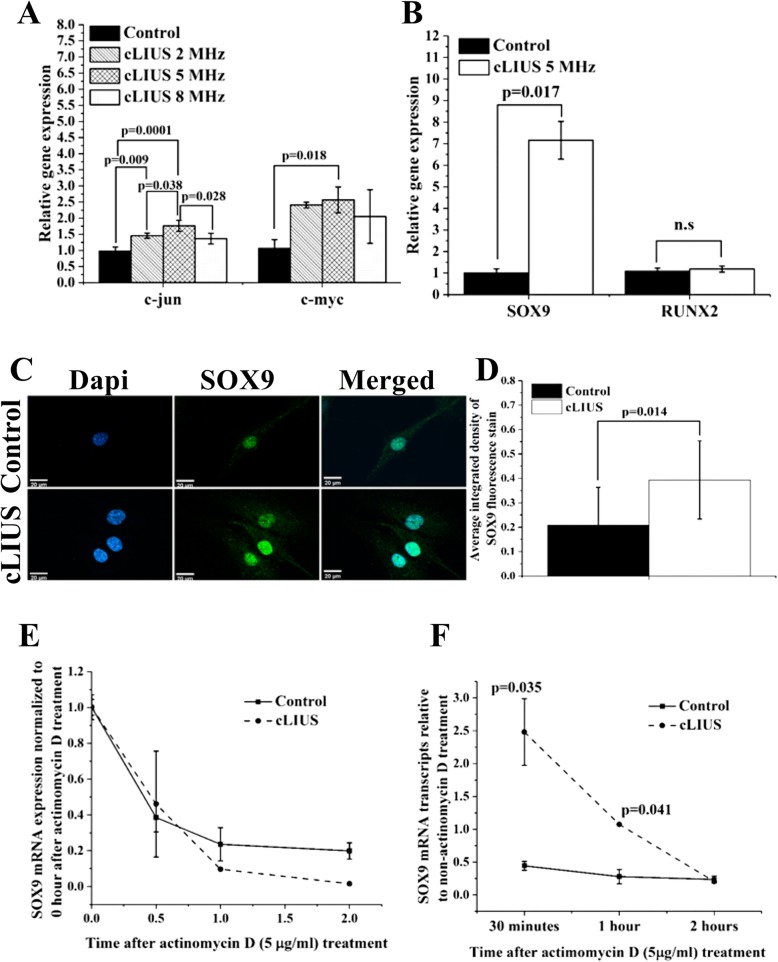
To establish the frequency dependence of MSCs under cLIUS, the expression of load-inducible genes c-MYC and c-JUN that are independent of new protein synthesis [52], was evaluated using methods as detailed elsewhere [37] and shown in Fig. 2a. The gene expression of c-MYC and c-JUN were maximized at 5 MHz. Thus, in the current study, cLIUS at 5 MHz was employed in all experiments.
Fig. 2.
Effect of cLIUS on select genes, SOX9 localization, and SOX9 mRNA stability. Gene expression of a c-MYC and c-JUN and b SOX9 and RUNX2 in MSCs exposed to cLIUS at indicated frequencies were estimated by qRT-PCR (n = 3). MSCs plated at 1 × 105 cells/well were exposed to cLIUS (14 kPa) at frequencies: 5 MHz (2.5 Vpp), 2 MHz (6 Vpp), or 8 MHz (9.5 Vpp) at constant pressure amplitude of 14 kPa one time for 5 min. Non-cLIUS-stimulated MSCs served as controls (n = 3). Data are shown as the mean ± standard deviation (Welch’s t-test). c MSCs in coverslips (n = 3) at an initial seeding density of 1 × 105 cells/well were stimulated with cLIUS application at 14 kPa (5 MHz, 2.5 Vpp) for 5 min and fixed in 4% PFA. Confocal micrographs (× 60 magnification) of immunofluorescent staining of SOX9 (green) shows the localization of SOX9 in the MSCs under cLIUS (Scale bar = 20 μm). Nucleus was stained by Dapi (blue) and d quantified by ImageJ (n = 10–20). Data are shown as the mean ± standard deviation. e MSCs (2 × 104 cells per well) were treated with 5 μg/ml actinomycin D, followed by stimulation with cLIUS at 14 kPa (5 MHz, 2.5 Vpp), for 15 min (n = 3). Total RNA was collected after 0 min, 30 min, 1 h, and 2 h of actinomycin D treatment, and the fold change in mRNA transcripts of SOX9 were quantified by qRT-PCR. In a parallel experiment without actinomycin D treatment, total RNA was collected at indicated time points following cLIUS stimulation, and the fold change in SOX9 mRNA transcripts was quantified by qRT-PCR (n = 3). Non-cLIUS-stimulated samples served as controls at respective time points (n = 3). Data represent the average ± standard deviation of fold change in SOX9 mRNA levels normalized to time point 0. f Graphical representation of the amount of SOX9 mRNA transcripts in actinomycin D-treated MSCs with or without cLIUS stimulation normalized to non-actinomycin D-treated samples at respective time points
To first establish the chondroinductive potential of cLIUS at 5 MHz, the gene expression of the chondrogenic marker SOX9 and osteogenic marker RUNX2 were evaluated in MSCs and shown in Fig. 2b. Under cLIUS, a sevenfold increase in the gene expression of SOX9 was observed whereas the gene expression of RUNX2 remained unaffected when compared to non-cLIUS-stimulated control. In a separate study, no significant difference in the expression of osteogenic markers (RUNX2, COL1A1) and adipogenic markers (CEBPA, PPARγ) in MSCs was observed following 10 days of cLIUS (5 MHz) stimulation whereas chondrogenic markers (SOX9 and COL2A1) remained significantly elevated under cLIUS stimulation when compared to non-cLIUS-stimulated controls (Additional file 1: Figure S1).
The transcriptional activity of SOX9 is contingent upon its subsequent nuclear translocation [53]. Thus, to further corroborate the gene expression results, the effect of cLIUS on the protein expression of SOX9 in cultures of MSCs was evaluated by immunofluorescence staining and is shown in Fig. 2c, d. The fluorescence intensity of SOX9 stain was significantly elevated (p = 0.014) in cLIUS-stimulated MSCs when compared to non-cLIUS-stimulated controls (Fig. 2d) and was highly concentrated in the nuclear region (Fig. 2c). Our collective data show that cLIUS increases the expression of the SOX9 gene and protein in MSCs.
cLIUS enhances the biosynthesis of SOX9 without affecting SOX9 mRNA stability
To ascertain the impact of cLIUS on the biosynthesis of SOX9 or its mRNA stability, RNA decay assay in the presence of actinomycin D was performed in 2D cultures of MSCs and shown in Fig. 2e, f. The degradation profile of SOX9 mRNA under cLIUS and non-cLIUS-stimulated control were similar (Fig. 2e), thus indicating that cLIUS had no discernible effect on the stability of SOX9 mRNA. In contrast, with respect to appropriate controls, higher levels of SOX9 mRNA transcripts were noted under cLIUS (Fig. 2f). The results demonstrated that cLIUS promoted the biosynthesis of SOX9 mRNA without affecting its stability.
Assessing the role of select signaling molecules in regulating SOX9 under cLIUS
Studies have shown that key intracellular signaling molecules ERK1/2 [54] and PKA [48] are involved in the phosphorylation of SOX9. Upstream cell-surface effectors of ERK1/2 and PKA such as integrin and ion channel TRPV4 are known to be activated by mechanical stimuli [55–57]. Under cLIUS stimulation of MSCs, increased intracellular calcium ion levels were observed as measured by Fluo-4-AM assay as compared to non-cLIUS-stimulated control (Additional file 2: Figure S2). Therefore, the involvement of ion channel TRPV4 in the transduction of cLIUS signals to SOX9 gene expression was examined. To establish the specificity of cLIUS-induced upregulation of the SOX9 gene, the gene expression and the nuclear localization of SOX9 under cLIUS were examined by qRT-PCR and immunofluorescence staining respectively, in the absence and presence of inhibitors of select signaling molecules in cultures of MSCs depicted in Fig. 1 and shown in Figs. 3 and 4.
Fig. 3.
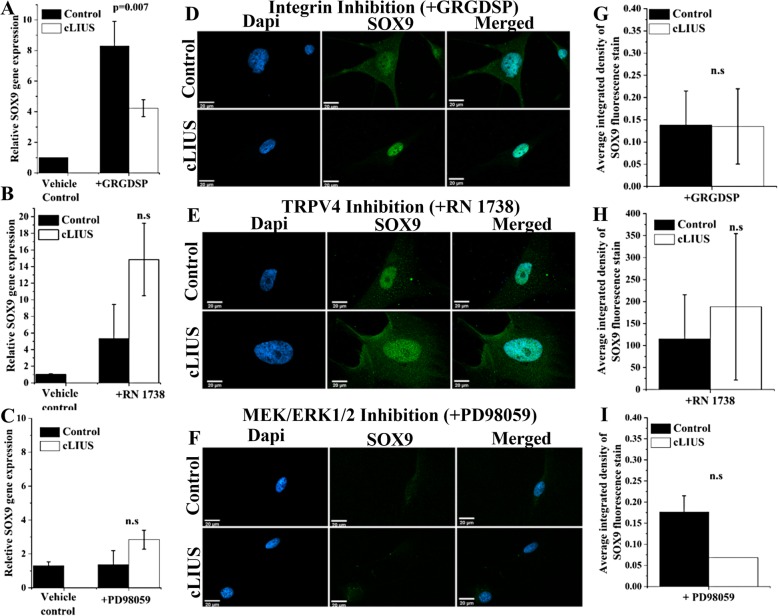
cLIUS-induced SOX9 regulation under integrin, TRPV4, and MEK/ERK1/2 inhibition. SOX9 gene expression in MSCs under a integrin inhibition by GRGDSP, b TRPV4 inhibition by RN 1738 (n = 3), and c MEK/ERK1/2 inhibition by PD98059 is shown. Serum-starved 2D cultures of MSCs were treated with inhibitors: 100 μg/ml GRGDSP (integrin inhibitor) or 30 μM RN1738 (TRPV4 inhibitor) for 4 h. Total RNA was collected 1 h after cLIUS stimulation at 14 kPa (5 MHz, 2.5 Vpp) for 5 min and the gene expression of SOX9 was quantified by qRT-PCR. Non-cLIUS-stimulated MSCs incubated in DMSO served as vehicle controls (n = 3). Data represented as a mean ± standard deviation. d–f MSCs were grown in coverslips (n = 4–6 per treatment condition) at an initial seeding density of 1 × 105 cells/well and were treated with inhibitors followed by the cLIUS application at 14 kPa (5 MHz, 2.5 Vpp) for 5 min and fixed in 4% PFA. Confocal micrographs (× 60 magnification) of immunofluorescent staining of SOX9 (green) shows the localization of SOX9 in the MSCs under d integrin inhibition by GRGDSP, e TRPV4 inhibition by RN1738, and f MEK/ERK1/2 inhibition by PD98059. The nucleus was stained with Dapi (blue). Scale bar represents 20 μm. g–i Quantification of SOX9 immunofluorescence intensity in control and cLIUS samples in the presence or absence of inhibitors by ImageJ (n = 10–20). Data are shown as the mean ± standard deviation of samples in triplicate. The p value represents the statistical significance, and n.s represents the non-significant difference as analyzed by Welch’s t-test
Fig. 4.
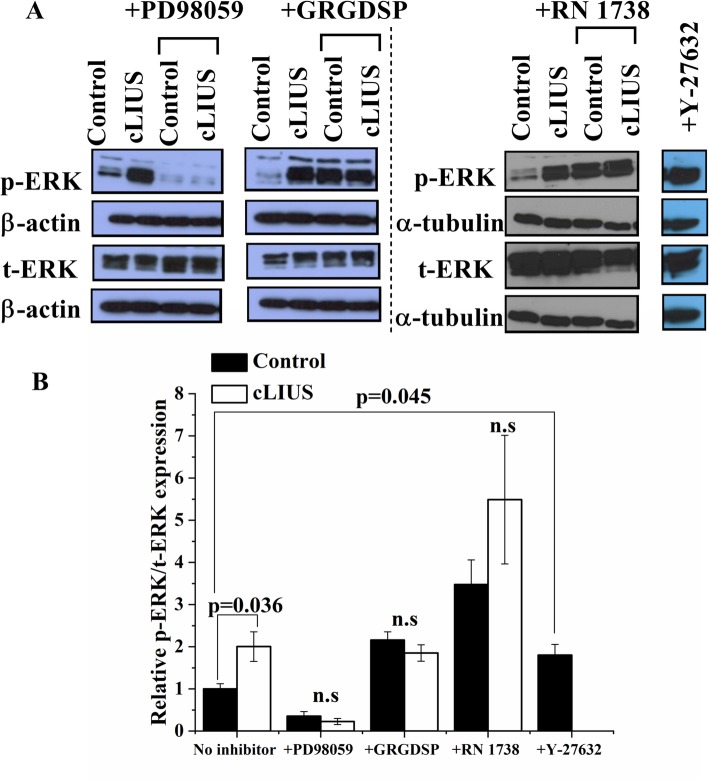
Effect of actin disruption on SOX9 upregulation. a–l Immunofluorescence staining of SOX9 (green) and F-actin filaments (red) in cLIUS-stimulated (5 MHz, 2.5 Vpp, 5 min, 1×) and Y-27632-treated MSCs grown on coverslips (n = 3) at an initial seeding density of 1 × 104 cells/well (n = 3). Non-cLIUS-stimulated MSCs served as control (n = 3). Confocal micrographs were imaged at × 60 magnification. Scale bar represents 20 μm. m The gene expression of SOX9 was evaluated by qRT-PCR in MSCs treated with Y-27632 or stimulated with cLIUS at 14 kPa (5 MHz, 2.5 Vpp) for 5 min (n = 3). Non-cLIUS-stimulated MSCs without Y-27632 treatment served as controls (n = 3). Data are shown as the mean ± standard deviation. Statistical significance was tested by Welch’s test. n Quantification of the actin filament number and length in non-cLIUS-stimulated control, cLIUS-, and Y-27632-treated cells (n = 10) by FilaQuant software
Inhibition of integrin or TRPV4 does not abrogate cLIUS-induced SOX9 upregulation
In the absence of inhibitors, a sevenfold increase in the gene expression of SOX9 was observed under cLIUS stimulation (p = 0.017) when compared to non-cLIUS-stimulated control (Fig. 2b). Upon inhibition of the cell-surface receptor integrin by GRGDSP, the gene expression of SOX9 was significantly reduced but not completely abrogated when exposed to cLIUS (Fig. 3a). In the presence of RN 1738, an inhibitor of TRPV4, the gene expression of SOX9 was upregulated; however, no difference in the expression levels was noted between cLIUS- and non-cLIUS-stimulated MSCs (Fig. 3b). Additionally, in the presence of inhibitors of integrin and TRPV4, no significant difference in the fluorescence intensity of SOX9 was noticed between cLIUS-stimulated and non-cLIUS-stimulated controls (Fig. 3d, e, g, h).
Pharmacological inhibition shows that ERK-1/2 and not PKA transduces cLIUS signal
Prevention of the phosphorylation of the intracellular signaling molecule, ERK1/2, by the inhibition of its immediate upstream effector MEK1/2 by PD98059, abrogated the gene expression of SOX9 (Fig. 3c). In the presence of H-89, an inhibitor of PKA, the gene expression of SOX9 was upregulated in both cLIUS-stimulated MSCs and non-cLIUS-stimulated controls; however, no significant difference was observed between the groups (Additional file 2: Figure S2). Under MEK/ERK1/2 inhibition by PD98059, no nuclear localization of SOX9 was observed upon immunofluorescence staining in cLIUS-stimulated MSCs and non-cLIUS-stimulated controls (Fig. 3f, i). This result correlates with the previous finding that the gene expression of SOX9 was abrogated upon MEK/ERK1/2 inhibition (Fig. 3c), thus confirming that the cLIUS-induced SOX9 expression was dependent on the phosphorylation of ERK1/2.
The actin cytoskeleton is reorganized under cLIUS
Actin reorganization has been connected to SOX9 upregulation [42, 45] where actin depolymerization correlated with the elevated gene expression of SOX9 in cells treated Y-27632, an actin-depolymerizing compound [45]. Reorganization of actin in chondrocytes exposed to a similar cLIUS regimen has been previously reported [58]. Therefore, the actin cytoskeleton was examined in cultures of MSCs under cLIUS and in the presence of Y-27632 and shown in Fig. 4. Actin-phalloidin staining of MSCs depicted intact actin stress fibers in non-cLIUS-stimulated controls (Fig. 4c) while diffused or disrupted actin fibers were observed in MSCs exposed to cLIUS (Fig. 4g). Quantification of the number of actin fibers as measured by FilaQuant software (Fig. 4n) revealed a significant decrease (p = 0.002) in the number of actin filaments per cell from 283.64 ± 190.75 in non-cLIUS-stimulated controls to 52.00 ± 28.18 under cLIUS in MSCs. Similarly, diffused actin fibers were observed in Y-27632-treated MSCs (Fig. 4k) with a significant reduction in the actin filament number and length (Fig. 4n). The cLIUS-induced changes in the actin cytoskeleton were reversed within 24 h of withdrawal of cLIUS stimulus (data not included). In MSCs treated with Y-27632, increased expression of the SOX9 gene (Fig. 4m) and the nuclear localization of the SOX9 protein (Fig. 4i, j) was noted. Similar trends were observed in MSCs exposed to cLIUS, which also exhibited actin disruption (Fig. 4j, e–h).
ERK1/2 is phosphorylated under cLIUS
Given the abolition of cLIUS-induced expression of SOX9 by inhibition of MEK/ERK1/2, the phosphorylation of ERK1/2 under cLIUS was investigated. The protein expression of phosphorylated ERK1/2 (p-ERK) and total ERK1/2 (t-ERK) under cLIUS in cultures of MSCs was analyzed by western blotting and shown in Fig. 5a. A twofold higher p-ERK/t-ERK ratio was noted under cLIUS stimulation as compared to non-cLIUS-stimulated control (Fig. 5b). Inhibition of MEK/ERK1/2 by PD98059 abrogated the phosphorylation of ERK1/2 in non-cLIUS-stimulated control as well as cLIUS-stimulated MSCs.
Fig. 5.
Phosphorylation of ERK1/2 under cLIUS. a Western blots depicting protein expression of phosphorylated ERK1/2 (p-ERK) and total ERK1/2 (t-ERK). 2D cultures of MSCs were grown in the presence or absence of inhibitors of MEK/ERK1/2 (PD98059), integrin (GRGDSP), or TRPV4 (RN1734) separately (n = 3), followed by exposure to cLIUS at 14 kPa (5 MHz, 2.5 Vpp) for 5 min. MSCs were lysed, total protein was extracted, and western blots were developed after SDS-PAGE. Non-cLIUS-stimulated MSCs served as respective controls (n = 3). b Quantification of bands observed in western blot by ImageJ (n = 3). Data are shown as the mean ± standard deviation of samples in triplicate. The p value represents a statistical significance and n.s. represents the non-significant difference (Welch’s test). Western blots were cropped for clarity and to exclude redundant adjacent lanes. Uncropped western blots are provided in supplementary files
In contrast, inhibition of integrin and TRPV4 by GRGDSP and RN 1738, respectively, displayed increased levels of p-ERK/t-ERK ratio in both non-cLIUS-stimulated control and in cLIUS-stimulated MSCs. Thus, inhibition of the cell-surface receptors, integrin, and TRPV4, did not reduce the levels of p-ERK1/2, implying that other receptors of mechanical stimuli may be activated leading to the phosphorylation of ERK1/2 under cLIUS.
In MSCs treated with Y-27632 that promotes actin disruption, elevated levels of p-ERK were noted. Similar trends were observed in MSCs exposed to cLIUS which exhibited actin disruption (Fig. 4g) in concert with an increased p-ERK (Fig. 5a) and SOX9 expression (Fig. 4e, f, m). Taken together, these results indicate a possible relationship between p-ERK and increased SOX9 gene expression under cLIUS stimulation in MSCs.
Chondrogenesis under cLIUS
To examine the ability of cLIUS to induce a chondrogenic phenotype in MSCs in the absence of exogenously added TGFβ, MSC-laden-HyStem-C hydrogel constructs (3D) were cultured under cLIUS stimulation for 6 weeks and shown in Fig. 6. Immunohistochemical staining of HyStem-C hydrogel constructs displayed a higher deposition of collagen II and chondroitin sulfate in cLIUS-stimulated constructs as compared to non-cLIUS-stimulated constructs.
Fig. 6.
The culture of MSC-laden HyStem-C constructs under cLIUS stimulation. MSCs were encapsulated at a density of 5 × 106 cells/ml of HyStem-C hydrogel and grown in DMEM medium supplemented with 10% FBS, 100 nM dexamethasone, and 50 μg/ml l-ascorbic acid for 6 weeks under cLIUS at 14 kPa (5 MHz, 2.5 Vpp), 20 min/application, and 4 applications/day (n = 3). Non-cLIUS-stimulated 3D constructs served as controls (n = 3). Representative images of 4-μm sections of the constructs stained immunohistochemically for collagen II and chondroitin sulfate is shown. Scale bar represents 100 μm
Discussion
Chondrogenic differentiation of MSCs is predicated on the transcriptional activity SOX9, which is initiated by the direct binding of phosphorylated SOX9 to the target genes such as collagen type II, IX, XI, aggrecan, link protein; consequently, inducing their transcription [59, 60]. Therefore, priming of MSCs toward a chondrogenic lineage, by growth factors or mechanical stimuli, centers on the upregulation of SOX9. Given the increased levels of SOX9 protein and mRNA in MSCs under cLIUS stimulation [24, 38], the aim of the present study was to evaluate the underlying molecular events that regulate the cLIUS-induced expression of SOX9. Our results indicated that nuclear localization of the SOX9 protein, phosphorylated ERK1/2, and disrupted actin filaments were differentially regulated under cLIUS and play a role in transducing cLIUS signals to induce SOX9 expression in MSCs.
The nuclear import of the transcription factor is related to its subsequent transcriptional activity [61]. For SOX9 to be transcriptionally active, nuclear localization of SOX9 is vital for its target DNA binding [61–63]. Indeed, the most prominent inducer of chondrogenesis, TGFβ, operates by essentially increasing the transcriptional activity of the SOX9 protein through its stabilization and binding to the COL2A1 gene via canonical or non-canonical pathways [43, 64]. In the present study, enhanced nuclear accumulation of SOX9 under cLIUS in MSCs (Fig. 2c) was indicative of its increased transcriptional activity as evidenced by elevated COL2A1 and SOX9 gene expression in MSCs (Additional file 1: Figure S1).
Mechanical stimuli including cLIUS have been previously documented to increase p-ERK1/2 and SOX9 [11, 65, 66] in both chondrocytes and MSCs [54]. However, a relationship between elevated levels of p-ERK and the gene expression of SOX9 was not established. Our results demonstrate that under cLIUS, SOX9 upregulation in MSCs was dependent on the phosphorylation of ERK1/2 and the specificity was established using MEK/ERK1/2 inhibitor. Similar results were observed in FGF-2 treated immortalized ADTC5 cell lines [67]. The exact molecular mechanism of p-ERK1/2 directed regulation of SOX9 expression remains to be investigated.
In the present study, cLIUS was shown to disrupt actin filaments in MSCs and a correlation between the perturbed actin cytoskeleton and SOX9 upregulation under cLIUS was inferred. Interestingly, reorganization of the actin cytoskeleton was noted as a precondition to differentiation [68]. Previous work alludes to the role of actin disrupted by the cytoskeletal drug, Y-27632, in inducing chondrogenesis in limb mesenchymal cultures by elevating the gene expression of SOX9 [44, 45]. In our study, cLIUS-induced disruption of the actin filaments was concomitant with increased SOX9 gene expression in MSCs (Fig. 4). To establish specificity, actin stabilizer jasplakinolide was added; however, the results were inconclusive. In our study, the gene expression of SOX9 was dependent on ERK1/2 phosphorylation. We postulate that increases in SOX9 observed under cLIUS or Y-27632 as a result of actin disruption was influenced by the increased levels of p-ERK (Fig. 5). The treatment of non-stimulated MSCs by the MEK/ERK1/2 inhibitor, which prevented the phosphorylation of ERK1/2, disrupted actin but did not result in the upregulation of SOX9 as expected (Fig. 3, Additional file 3: Figure S3). Thus, our present study indicated that the phosphorylation of ERK1/2 was the key molecular event impacting the expression of SOX9.
As the phosphorylation of ERK1/2 was pivotal in the upregulation of SOX9 under cLIUS, the role of upstream effectors of ERK1/2 was evaluated to understand the pathways through which cLIUS signals were transduced to ERK1/2, ultimately leading to the gene expression of SOX9 in MSCs. The involvement of the integrin-mediated MAPK pathway in transducing cLIUS signals to ERK1/2 in chondrocytes has been reported [65, 69]. In another study, pLIUS was shown to immediately elevate levels of p-ERK1/2 [27] through the activation of TRPV4-mediated calcium signaling pathway in chondrocytes. In the current study, individual blockage of either integrin or TRPV4 failed to abrogate p-ERK1/2 under cLIUS stimulation in MSCs, and hence, SOX9 remained elevated. Thus, other sensors of mechanical signals that also regulate the phosphorylation of ERK1/2 could play a role in the ERK1/2-mediated SOX9 upregulation under cLIUS in MSCs.
The main purpose of the study was to evaluate the chondroinductive ability of cLIUS by monitoring the gene and protein expression of SOX9, transcription factor that controls the expression of collagen II (COL2A1). Thus, the focus was on the molecular consequences following cLIUS, which are best evaluated upon a single exposure to LIUS. To offer proof of the relevance of these molecular events to chondrogenesis, MSC constructs were cultured in Hystem-C™ hydrogels under cLIUS (note no exogenous growth factors were added) for 6 weeks (Fig. 6). Increased deposition of collagen II and chondroitin sulfate at the end of the culture period demonstrated MSC chondrogenesis upon extended exposure to cLIUS. Previously, the long-term 3D culture of MSCs in scaffolds under cLIUS stimulation, notably in the absence of TGFβ, also yielded an elevated expression of collagen II and SOX9 protein [38]. Further, the biochemical, as well as mechanical properties (compressive strength and aggregate modulus), were significantly higher in MSC-laden scaffold constructs exposed to cLIUS stimulation for 8 weeks as opposed to non-cLIUS-stimulated controls [38]. Collectively, our results demonstrated the chondroinductive ability of cLIUS in 3D cultures of MSCs in the absence of TGFβ.
Conclusions
In summary, our study identified the phosphorylation of ERK1/2, increased nuclear localization of the SOX9 protein, and disrupted actin as the events mediating increased SOX9 gene expression under cLIUS. Most notably, cLIUS-induced upregulation of SOX9 was dependent on the phosphorylation of ERK1/2, signifying the involvement of ERK1/2 signaling on the SOX9 gene and protein expression. The involvement of endogenously secreted TGFβs in MSCs in response to cLIUS was excluded, as the current study focused on the immediate molecular events following one dose of cLIUS stimulation. However, the role of intrinsic TGFβ signaling in concert with cLIUS in MSCs will be investigated in future studies. The role of additional physical perturbations such as nuclear deformation and chromatin reorganization on MSCs in response to cLIUS will also be undertaken in future investigations. Additionally, the results presented in the current study remain to be verified in 3D cultures and in cartilage explants.
Supplementary information
Figure S1. Gene expression of select osteogenic, chondrogenic and adipogenic markers under cLIUS. MSCs were grown at an initial seeding density of 2 x 105 cells/ml in 12-well TCP. MSCs were exposed to cLIUS at 14 kPa (5.0 MHz, 2.5 Vpp), 5 min/application, 4X/day for a period of 10. MSCs (n=3) were treated with Trizol and total RNA was extracted using RNeasy Mini Kit (Qiagen, USA) as per manufacturer’s protocol. Non-cLIUS-stimulated MSCs served as control (n=3). qRT-PCR was carried out in Realplex™ real-time PCR system (Eppendorf, USA) using TaqMan® RNA-to-CT™ 1-Step Kit (Life Technologies, USA) as per manufacturer’s guidelines. The gene expression of select osteogenic (Runx2, SPP-1, and COL1A1), chondrogenic (SOX9 and COL2A1) and adipogenic (CEBPA and PPARγ) was evaluated. Data represent mean ± standard deviation. *p-value <0.05 & compared with control.
Figure S2. Intracellular Ca++ influx under cLIUS and SOX9 gene expression under PKA inhibition: a MSCs were plated at an initial seeding density of 2 X 105 cells/well on 12-well TCP. MSCs were pre-treated with the Fluo-4-AM probe (3 μM) in a recording medium (20 mM HEPES, 115 mM NaCl, 5.4 mM KCl, 0.8 mM MgCl2, 1.8 mM CaCl2, 13.8mM glucose) for 20 minutes, after which the medium was replaced with recording medium without Fluo-4-AM. Intracellular calcium was visualized 5 minutes after cLIUS stimulation (5 MHz. 2.5 Vpp, 5 minutes) under a fluorescence microscope at 5X magnification(n=3). Non-cLIUS-stimulated MSCs served as controls (n=3). Phase-contrast images (5X magnification) depict the general morphology of the stained cells. b The gene expression of SOX9 in non-cLIUS-stimulated and cLIUS-stimulated MSCs in the presence of H-89, an inhibitor of PKA (20μg/ml). Total RNA was collected 1 hour after cLIUS treatment in MSCs treated with H-89 and subjected to qRT-PCR. Non-cLIUS stimulated MSCs served as control. Data represented as a mean ± standard deviation and normalized to vehicle control.
Figure S3. Figure. Actin staining in MSCs under ERK1/2 inhibition. MSCs were treated with MEK/ERK1/2 inhibitor PD98059 for 4 h and fixed in 4% paraformaldehyde. Immunofluorescence staining for F-actin (red) by phalloidin-Alexa Fluor 594 was carried out and the representative confocal image is presented (n = 3). Scale bar represents 20 μm.
Acknowledgements
We are thankful to Teresa Fangman of Morrison Microscopy Core Research Facility at UNL, for assistance with microscopy and Melissa Holzapfel of Tissue Sciences Facility at the University of Nebraska Medical Center for assistance with histology.
Abbreviations
- 2D
2-Dimensional
- 3D
3-Dimensional
- ACI
Autologous chondrocyte implantation
- cLIUS
Continuous low-intensity ultrasound
- DMSO
Dimethyl sulfoxide
- ERK1/2
Extracellular signal-regulated kinase 1 and 2
- FBS
Fetal bovine serum
- GAG
Glycosaminoglycans
- MACI
Matrix-assisted autologous chondrocyte implantation
- MAPK
Mitogen-activated protein kinase
- MSC
Mesenchymal stromal cell
- PKA
Protein kinase A
- ROCK
Rho kinase
- SOX9
Sex determining region Y-box 9
- TGFβ
Transforming growth factor β
- TRPV4
Transient receptor potential vanilloids 4
- α-MEM
α-Minimal essential medium
Authors’ contributions
AS conceived the study. NS, GB, and AS designed the experiments. NS carried out experiments, analyzed and interpreted data. GB contributed to Additional file 1: Figure S1. NS and AS drafted the manuscript. All authors revised and approved the final version of the manuscript.
Funding
We are grateful to the Nebraska Research Initiative for funding and support.
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13287-019-1532-2.
References
- 1.Thelin N, Holmberg S, Thelin A. Knee injuries account for the sports-related increased risk of knee osteoarthritis. Scand J Med Sci Sports. 2006;16(5):329–333. doi: 10.1111/j.1600-0838.2005.00497.x. [DOI] [PubMed] [Google Scholar]
- 2.Little CB, Hunter DJ. Post-traumatic osteoarthritis: from mouse models to clinical trials. Nat Rev Rheumatol. 2013;9(8):485–497. doi: 10.1038/nrrheum.2013.72. [DOI] [PubMed] [Google Scholar]
- 3.Darling EM, Athanasiou KA. Rapid phenotypic changes in passaged articular chondrocyte subpopulations. J Orthop Res. 2005;23(2):425–432. doi: 10.1016/j.orthres.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Dell'Accio F, De Bari C, Luyten FP. Molecular markers predictive of the capacity of expanded human articular chondrocytes to form stable cartilage in vivo. Arthritis Rheum. 2001;44(7):1608–1619. doi: 10.1002/1529-0131(200107)44:7<1608::AID-ART284>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 5.Pelttari K, Winter A, Steck E, Goetzke K, et al. Premature induction of hypertrophy during in vitro chondrogenesis of human mesenchymal stem cells correlates with calcification and vascular invasion after ectopic transplantation in SCID mice. Arthritis Rheum. 2006;54(10):3254–3266. doi: 10.1002/art.22136. [DOI] [PubMed] [Google Scholar]
- 6.Augello A, De Bari C. The regulation of differentiation in mesenchymal stem cells. Hum Gene Ther. 2010;21(10):1226–1238. doi: 10.1089/hum.2010.173. [DOI] [PubMed] [Google Scholar]
- 7.Mueller MB, Fischer M, Zellner J, Berner A, et al. Hypertrophy in mesenchymal stem cell chondrogenesis: effect of TGF-beta isoforms and chondrogenic conditioning. Cells Tissues Organs. 2010;192(3):158–166. doi: 10.1159/000313399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bian L, Zhai DY, Tous E, Rai R, et al. Enhanced MSC Chondrogenesis following delivery of TGF-β3 from alginate microspheres within hyaluronic acid hydrogels in vitro and in vivo. Biomaterials. 2011;32(27):6425–6434. doi: 10.1016/j.biomaterials.2011.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Delaine-Smith RM, Reilly GC. Mesenchymal stem cell responses to mechanical stimuli. Muscles Ligaments Tendons J. 2012;2(3):169–180. [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C, Dai J, Zhang XA. Environmental physical cues determine the lineage specification of mesenchymal stem cells. Biochim Biophys Acta. 2015;1850(6):1261–1266. doi: 10.1016/j.bbagen.2015.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simmons CA, Matlis S, Thornton AJ, Chen S, et al. Cyclic strain enhances matrix mineralization by adult human mesenchymal stem cells via the extracellular signal-regulated kinase (ERK1/2) signaling pathway. J Biomech. 2003;36(8):1087–1096. doi: 10.1016/S0021-9290(03)00110-6. [DOI] [PubMed] [Google Scholar]
- 12.Kwon HJ, Lee GS, Chun H. Electrical stimulation drives chondrogenesis of mesenchymal stem cells in the absence of exogenous growth factors. Sci Rep. 2016;6:39302. doi: 10.1038/srep39302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ogawa R, Mizuno S, Murphy GF, Orgill DP. The effect of hydrostatic pressure on three-dimensional chondroinduction of human adipose-derived stem cells. Tissue Eng Part A. 2009;15(10):2937–2945. doi: 10.1089/ten.tea.2008.0672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo T, Yu L, Lim CG, Goodley AS, et al. Effect of dynamic culture and periodic compression on human mesenchymal stem cell proliferation and chondrogenesis. Ann Biomed Eng. 2016;44(7):2103–2113. doi: 10.1007/s10439-015-1510-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tigli RS, Cannizaro C, Gumusderelioglu M, Kaplan DL. Chondrogenesis in perfusion bioreactors using porous silk scaffolds and hESC-derived MSCs. J Biomed Mater Res A. 2011;96(1):21–28. doi: 10.1002/jbm.a.32949. [DOI] [PubMed] [Google Scholar]
- 16.Li Z, Yao SJ, Alini M, Stoddart MJ. Chondrogenesis of human bone marrow mesenchymal stem cells in fibrin-polyurethane composites is modulated by frequency and amplitude of dynamic compression and shear stress. Tissue Eng Part A. 2010;16(2):575–584. doi: 10.1089/ten.tea.2009.0262. [DOI] [PubMed] [Google Scholar]
- 17.Huang CY, Hagar KL, Frost LE, Sun Y, et al. Effects of cyclic compressive loading on chondrogenesis of rabbit bone-marrow derived mesenchymal stem cells. Stem Cells. 2004;22(3):313–323. doi: 10.1634/stemcells.22-3-313. [DOI] [PubMed] [Google Scholar]
- 18.Puetzer J, Williams J, Gillies A, Bernacki S, et al. The effects of cyclic hydrostatic pressure on chondrogenesis and viability of human adipose- and bone marrow-derived mesenchymal stem cells in three-dimensional agarose constructs. Tissue Eng Part A. 2013;19(1–2):299–306. doi: 10.1089/ten.tea.2012.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fahy N, Alini M, Stoddart MJ. Mechanical stimulation of mesenchymal stem cells: implications for cartilage tissue engineering. J Orthop Res. 2018;36(1):52–63. doi: 10.1002/jor.23670. [DOI] [PubMed] [Google Scholar]
- 20.Kisiday JD, Frisbie DD, McIlwraith CW, Grodzinsky AJ. Dynamic compression stimulates proteoglycan synthesis by mesenchymal stem cells in the absence of chondrogenic cytokines. Tissue Eng Part A. 2009;15(10):2817–2824. doi: 10.1089/ten.tea.2008.0357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mauck RL, Byers BA, Yuan X, Tuan RS. Regulation of cartilaginous ECM gene transcription by chondrocytes and MSCs in 3D culture in response to dynamic loading. Biomech Model Mechanobiol. 2007;6(1–2):113–125. doi: 10.1007/s10237-006-0042-1. [DOI] [PubMed] [Google Scholar]
- 22.Huang AH, Farrell MJ, Kim M, Mauck RL. Long-term dynamic loading improves the mechanical properties of chondrogenic mesenchymal stem cell-laden hydrogel. Eur Cell Mater. 2010;19:72–85. doi: 10.22203/eCM.v019a08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cui JH, Park K, Park SR, Min BH. Effects of low-intensity ultrasound on chondrogenic differentiation of mesenchymal stem cells embedded in polyglycolic acid: an in vivo study. Tissue Eng. 2006;12(1):75–82. doi: 10.1089/ten.2006.12.75. [DOI] [PubMed] [Google Scholar]
- 24.Lee HJ, Choi BH, Min BH, Son YS, et al. Low-intensity ultrasound stimulation enhances chondrogenic differentiation in alginate culture of mesenchymal stem cells. Artif Organs. 2006;30(9):707–715. doi: 10.1111/j.1525-1594.2006.00288.x. [DOI] [PubMed] [Google Scholar]
- 25.Schumann D, Kujat R, Zellner J, Angele MK, et al. Treatment of human mesenchymal stem cells with pulsed low intensity ultrasound enhances the chondrogenic phenotype in vitro. Biorheology. 2006;43(3,4):431–443. [PubMed] [Google Scholar]
- 26.Zhang ZJ, Huckle J, Francomano CA, Spencer RG. The effects of pulsed low-intensity ultrasound on chondrocyte viability, proliferation, gene expression and matrix production. Ultrasound Med Biol. 2003;29(11):1645–1651. doi: 10.1016/j.ultrasmedbio.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 27.Nishida T, Kubota S, Aoyama E, Yamanaka N, et al. Low-intensity pulsed ultrasound (LIPUS) treatment of cultured chondrocytes stimulates production of CCN family protein 2 (CCN2), a protein involved in the regeneration of articular cartilage: mechanism underlying this stimulation. Osteoarthr Cartil. 2017;25(5):759–769. doi: 10.1016/j.joca.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 28.Hsu H-C, Fong Y-C, Chang C-S, Hsu C-J, et al. Ultrasound induces cyclooxygenase-2 expression through integrin, integrin-linked kinase, Akt, NF-κB and p300 pathway in human chondrocytes. Cell Signal. 2007;19(11):2317–2328. doi: 10.1016/j.cellsig.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 29.Cook SD, Salkeld SL, Popich-Patron LS, Ryaby JP, et al. Improved cartilage repair after treatment with low-intensity pulsed ultrasound. Clin Orthop Relat Res. 2001;391:S231–SS43. doi: 10.1097/00003086-200110001-00022. [DOI] [PubMed] [Google Scholar]
- 30.Cook SD, Salkeld SL, Patron LP, Doughty ES, et al. The effect of low-intensity pulsed ultrasound on autologous osteochondral plugs in a canine model. Am J Sports Med. 2008;36(9):1733–1741. doi: 10.1177/0363546508316766. [DOI] [PubMed] [Google Scholar]
- 31.Ebisawa K, Hata K, Okada K, Kimata K, et al. Ultrasound enhances transforming growth factor beta-mediated chondrocyte differentiation of human mesenchymal stem cells. Tissue Eng. 2004;10(5–6):921–929. doi: 10.1089/1076327041348437. [DOI] [PubMed] [Google Scholar]
- 32.Yamaguchi S, Aoyama T, Ito A, Nagai M, et al. Effect of low-intensity pulsed ultrasound after mesenchymal stromal cell injection to treat osteochondral defects: an in vivo study. Ultrasound Med Biol. 2016;42(12):2903–2913. doi: 10.1016/j.ultrasmedbio.2016.07.021. [DOI] [PubMed] [Google Scholar]
- 33.Lee HJ, Choi BH, Min BH, Park SR. Low-intensity ultrasound inhibits apoptosis and enhances viability of human mesenchymal stem cells in three-dimensional alginate culture during chondrogenic differentiation. Tissue Eng. 2007;13(5):1049–1057. doi: 10.1089/ten.2006.0346. [DOI] [PubMed] [Google Scholar]
- 34.Choi JW, Choi BH, Park SH, Pai KS, et al. Mechanical stimulation by ultrasound enhances chondrogenic differentiation of mesenchymal stem cells in a fibrin-hyaluronic acid hydrogel. Artif Organs. 2013;37(7):648–655. doi: 10.1111/aor.12041. [DOI] [PubMed] [Google Scholar]
- 35.Cui JH, Park SR, Park K, Choi BH, et al. Preconditioning of mesenchymal stem cells with low-intensity ultrasound for cartilage formation in vivo. Tissue Eng. 2007;13(2):351–360. doi: 10.1089/ten.2006.0080. [DOI] [PubMed] [Google Scholar]
- 36.Miller AD, Chama A, Louw TM, Subramanian A, et al. Frequency sensitive mechanism in low-intensity ultrasound enhanced bioeffects. PLoS One. 2017;12(8):e0181717. doi: 10.1371/journal.pone.0181717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Louw TM, Budhiraja G, Viljoen HJ, Subramanian A. Mechanotransduction of ultrasound is frequency dependent below the cavitation threshold. Ultrasound Med Biol. 2013;39(7):1303–1319. doi: 10.1016/j.ultrasmedbio.2013.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sanjukta Guha T, Neety S, April M, Gaurav B, et al. Long-term culture of human mesenchymal stem cell-seeded constructs under ultrasound stimulation: evaluation of chondrogenesis. Biomed Phys Eng Express. 2016;2(5):055016. doi: 10.1088/2057-1976/2/5/055016. [DOI] [Google Scholar]
- 39.Lefebvre V, Huang W, Harley VR, Goodfellow PN, et al. SOX9 is a potent activator of the chondrocyte-specific enhancer of the pro alpha1(II) collagen gene. Mol Cell Biol. 1997;17(4):2336–2346. doi: 10.1128/MCB.17.4.2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang B, Guo H, Zhang Y, Chen L, et al. MicroRNA-145 regulates chondrogenic differentiation of mesenchymal stem cells by targeting Sox9. PLoS One. 2011;6(7):e21679. doi: 10.1371/journal.pone.0021679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Huang W, Chung UI, Kronenberg HM, de Crombrugghe B. The chondrogenic transcription factor Sox9 is a target of signaling by the parathyroid hormone-related peptide in the growth plate of endochondral bones. Proc Natl Acad Sci U S A. 2001;98(1):160–165. doi: 10.1073/pnas.98.1.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Haudenschild DR, Chen J, Pang N, Lotz MK, et al. Rho kinase-dependent Sox9 activation in chondrocytes. Arthritis Rheum. 2010;62(1):191–200. doi: 10.1002/art.25051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Coricor G, Serra R. TGF-β regulates phosphorylation and stabilization of Sox9 protein in chondrocytes through p38 and Smad dependent mechanisms. Sci Rep. 2016;6:38616. doi: 10.1038/srep38616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Woods A, Beier F. RhoA/ROCK signaling regulates chondrogenesis in a context-dependent manner. J Biol Chem. 2006;281(19):13134–13140. doi: 10.1074/jbc.M509433200. [DOI] [PubMed] [Google Scholar]
- 45.Woods A, Wang G, Beier F. RhoA/ROCK signaling regulates Sox9 expression and actin organization during chondrogenesis. J Biol Chem. 2005;280(12):11626–11634. doi: 10.1074/jbc.M409158200. [DOI] [PubMed] [Google Scholar]
- 46.Furumatsu T, Matsumoto E, Kanazawa T, Fujii M, et al. Tensile strain increases expression of CCN2 and COL2A1 by activating TGF-beta-Smad2/3 pathway in chondrocytic cells. J Biomech. 2013;46(9):1508–1515. doi: 10.1016/j.jbiomech.2013.03.028. [DOI] [PubMed] [Google Scholar]
- 47.Li J, Zhao Z, Liu J, Huang N, et al. MEK/ERK and p38 MAPK regulate chondrogenesis of rat bone marrow mesenchymal stem cells through delicate interaction with TGF-beta1/Smads pathway. Cell Prolif. 2010;43(4):333–343. doi: 10.1111/j.1365-2184.2010.00682.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Juhasz T, Matta C, Somogyi C, Katona E, et al. Mechanical loading stimulates chondrogenesis via the PKA/CREB-Sox9 and PP2A pathways in chicken micromass cultures. Cell Signal. 2014;26(3):468–482. doi: 10.1016/j.cellsig.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 49.O’Conor CJ, Leddy HA, Benefield HC, Liedtke WB, et al. TRPV4-mediated mechanotransduction regulates the metabolic response of chondrocytes to dynamic loading. Proc Natl Acad Sci. 2014;111(4):1316–1321. doi: 10.1073/pnas.1319569111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Qiu LQ, Lai WS, Stumpo DJ, Blackshear PJ. Measurement of mRNA Decay in Mouse Embryonic Fibroblasts. Bio protoc. 2016;6(13):e1858. 10.21769/BioProtoc.1858. [DOI] [PMC free article] [PubMed]
- 51.Noriega S, Mamedov T, Turner JA, Subramanian A. Intermittent applications of continuous ultrasound on the viability, proliferation, morphology, and matrix production of chondrocytes in 3D matrices. Tissue Eng. 2007;13(3):611–618. doi: 10.1089/ten.2006.0130. [DOI] [PubMed] [Google Scholar]
- 52.Sng JC, Taniura H, Yoneda Y. A tale of early response genes. Biol Pharm Bull. 2004;27(5):606–612. doi: 10.1248/bpb.27.606. [DOI] [PubMed] [Google Scholar]
- 53.Sim H, Argentaro A, Harley VR. Boys, girls and shuttling of SRY and SOX9. Trends Endocrinol Metab. 2008;19(6):213–222. doi: 10.1016/j.tem.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 54.Ling Li, Wei Tianqin, He Lianli, Wang Yaping, Wang Yan, Feng Xiushan, Zhang Wenqian, Xiong Zhengai. Low-intensity pulsed ultrasound activates ERK1/2 and PI3K-Akt signalling pathways and promotes the proliferation of human amnion-derived mesenchymal stem cells. Cell Proliferation. 2017;50(6):e12383. doi: 10.1111/cpr.12383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Katsumi A, Orr AW, Tzima E, Schwartz MA. Integrins in Mechanotransduction. J Biol Chem. 2004;279(13):12001–12004. doi: 10.1074/jbc.R300038200. [DOI] [PubMed] [Google Scholar]
- 56.Corrigan MA, Johnson GP, Stavenschi E, Riffault M, et al. TRPV4-mediates oscillatory fluid shear mechanotransduction in mesenchymal stem cells in part via the primary cilium. Sci Rep. 2018;8(1):3824. doi: 10.1038/s41598-018-22174-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Matta C, Zakany R. Calcium signalling in chondrogenesis: implications for cartilage repair. Front Biosci (Schol Ed) 2013;5:305–324. doi: 10.2741/S374. [DOI] [PubMed] [Google Scholar]
- 58.Noriega S, Budhiraja G, Subramanian A. Remodeling of chromatin under low intensity diffuse ultrasound. Int J Biochem Cell Biol. 2012;44(8):1331–1336. doi: 10.1016/j.biocel.2012.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lefebvre V, Dvir-Ginzberg M. SOX9 and the many facets of its regulation in the chondrocyte lineage. Connect Tissue Res. 2017;58(1):2–14. doi: 10.1080/03008207.2016.1183667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ng LJ, Wheatley S, Muscat GE, Conway-Campbell J, et al. SOX9 binds DNA, activates transcription, and coexpresses with type II collagen during chondrogenesis in the mouse. Dev Biol. 1997;183(1):108–121. doi: 10.1006/dbio.1996.8487. [DOI] [PubMed] [Google Scholar]
- 61.Huang W, Zhou X, Lefebvre V, de Crombrugghe B. Phosphorylation of SOX9 by cyclic AMP-dependent protein kinase a enhances SOX9’s ability to transactivate a Col2a1 chondrocyte-specific enhancer. Mol Cell Biol. 2000;20(11):4149–4158. doi: 10.1128/MCB.20.11.4149-4158.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ito T, Sawada R, Fujiwara Y, Tsuchiya T. FGF-2 increases osteogenic and chondrogenic differentiation potentials of human mesenchymal stem cells by inactivation of TGF-β signaling. Cytotechnology. 2008;56(1):1–7. doi: 10.1007/s10616-007-9092-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Argentaro A, Sim H, Kelly S, Preiss S, et al. A SOX9 defect of calmodulin-dependent nuclear import in campomelic dysplasia/autosomal sex reversal. J Biol Chem. 2003;278(36):33839–33847. doi: 10.1074/jbc.M302078200. [DOI] [PubMed] [Google Scholar]
- 64.Tsuda M, Takahashi S, Takahashi Y, Asahara H. Transcriptional co-activators CREB-binding protein and p300 regulate chondrocyte-specific gene expression via association with Sox9. J Biol Chem. 2003;278(29):27224–27229. doi: 10.1074/jbc.M303471200. [DOI] [PubMed] [Google Scholar]
- 65.Whitney NP, Lamb AC, Louw TM, Subramanian A. Integrin-mediated mechanotransduction pathway of low-intensity continuous ultrasound in human chondrocytes. Ultrasound Med Biol. 2012;38(10):1734–1743. doi: 10.1016/j.ultrasmedbio.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Shakibaei M, Seifarth C, John T, Rahmanzadeh M, et al. Igf-I extends the chondrogenic potential of human articular chondrocytes in vitro: molecular association between Sox9 and Erk1/2. Biochem Pharmacol. 2006;72(11):1382–1395. doi: 10.1016/j.bcp.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 67.Murakami S, Kan M, McKeehan WL, de Crombrugghe B. Up-regulation of the chondrogenic Sox9 gene by fibroblast growth factors is mediated by the mitogen-activated protein kinase pathway. Proc Natl Acad Sci U S A. 2000;97(3):1113–1118. doi: 10.1073/pnas.97.3.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Müller P, Langenbach A, Kaminski A, Rychly J. Modulating the actin cytoskeleton affects mechanically induced signal transduction and differentiation in mesenchymal stem cells. PLoS One. 2013;8(7):e71283. doi: 10.1371/journal.pone.0071283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Choi BH, Choi MH, Kwak MG, Min BH, et al. Mechanotransduction pathways of low-intensity ultrasound in C-28/I2 human chondrocyte cell line. Proc Inst Mech Eng H. 2007;221(5):527–535. doi: 10.1243/09544119JEIM201. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Gene expression of select osteogenic, chondrogenic and adipogenic markers under cLIUS. MSCs were grown at an initial seeding density of 2 x 105 cells/ml in 12-well TCP. MSCs were exposed to cLIUS at 14 kPa (5.0 MHz, 2.5 Vpp), 5 min/application, 4X/day for a period of 10. MSCs (n=3) were treated with Trizol and total RNA was extracted using RNeasy Mini Kit (Qiagen, USA) as per manufacturer’s protocol. Non-cLIUS-stimulated MSCs served as control (n=3). qRT-PCR was carried out in Realplex™ real-time PCR system (Eppendorf, USA) using TaqMan® RNA-to-CT™ 1-Step Kit (Life Technologies, USA) as per manufacturer’s guidelines. The gene expression of select osteogenic (Runx2, SPP-1, and COL1A1), chondrogenic (SOX9 and COL2A1) and adipogenic (CEBPA and PPARγ) was evaluated. Data represent mean ± standard deviation. *p-value <0.05 & compared with control.
Figure S2. Intracellular Ca++ influx under cLIUS and SOX9 gene expression under PKA inhibition: a MSCs were plated at an initial seeding density of 2 X 105 cells/well on 12-well TCP. MSCs were pre-treated with the Fluo-4-AM probe (3 μM) in a recording medium (20 mM HEPES, 115 mM NaCl, 5.4 mM KCl, 0.8 mM MgCl2, 1.8 mM CaCl2, 13.8mM glucose) for 20 minutes, after which the medium was replaced with recording medium without Fluo-4-AM. Intracellular calcium was visualized 5 minutes after cLIUS stimulation (5 MHz. 2.5 Vpp, 5 minutes) under a fluorescence microscope at 5X magnification(n=3). Non-cLIUS-stimulated MSCs served as controls (n=3). Phase-contrast images (5X magnification) depict the general morphology of the stained cells. b The gene expression of SOX9 in non-cLIUS-stimulated and cLIUS-stimulated MSCs in the presence of H-89, an inhibitor of PKA (20μg/ml). Total RNA was collected 1 hour after cLIUS treatment in MSCs treated with H-89 and subjected to qRT-PCR. Non-cLIUS stimulated MSCs served as control. Data represented as a mean ± standard deviation and normalized to vehicle control.
Figure S3. Figure. Actin staining in MSCs under ERK1/2 inhibition. MSCs were treated with MEK/ERK1/2 inhibitor PD98059 for 4 h and fixed in 4% paraformaldehyde. Immunofluorescence staining for F-actin (red) by phalloidin-Alexa Fluor 594 was carried out and the representative confocal image is presented (n = 3). Scale bar represents 20 μm.
Data Availability Statement
All data generated or analyzed during this study are included in this published article [and its supplementary information files].