Abstract
Background
An estimated 1.5 million persons in Germany are intellectually disabled. Persons with intellectual disability (ID) are especially vulnerable to somatic and mental illnesses.
Methods
This review is based on pertinent literature retrieved by selective searches in PubMed and the Cochrane Library.
Results
Genetic abnormalities are a frequent cause of diseases that affect multiple organs and need interdisciplinary treatment. A number of somatic diseases are more common in persons with ID than in the general population, including epilepsy (30–50% in persons with severe or very severe ID, vs. 0.5% in the general population) and dementia (five times more common than in the general population). Patients with Down syndrome are 20 times more likely than the general population to develop acute lymphoblastic leukemia. Some mental illnesses, too, are more common in persons with ID, e.g., autism spectrum disorders (7.5–15% vs. 1% in the general population). The history and the findings of the physical and psychiatric examination are assessed in accordance with the biopsychosocial model of disease, and in the light of the patient’s mental developmental age. Structured instruments for behavioral evaluation and diagnosis are an important additional component of the diagnostic assessment. A holistic approach is required that takes multiple life areas into account and involves the patient’s familial and social environment, while obeying the rules of simple language. Psychotherapeutic and psychosocial measures must be adapted to the patient’s cognitive abilities and mental developmental age.
Conclusion
Intellectually disabled persons can be treated in a multimodal, multiprofessional approach. As of early 2019, there were 38 medical centers for adults with intellectual disability or severe multiple disabilities in Germany (Medizinische Behandlungszentren für Erwachsene mit geistiger Behinderung oder schweren Mehrfachbehinderungen, MZEB), where they can be cared for with due attention to their special needs.
Intellectual disability (ID) is defined as the result of a disturbance of intellectual development (1) and, therefore, must begin before the patient becomes an adult. Common synonyms for ID include cognitive impairment, mental impairment, intellectual disability. These persons’ IQ is significantly below the mean in the general population (more than 2 standard deviations below the norm, 1–2% of the population, ca. 1.5 million affected persons); they thus have difficulty in learning new and complex information or skills and in living independently (etable 1).
eTable 1. Grades of severity of intellectual disability (ID): definition, features, and frequency among persons with ID.
| Severity of ID | IQ | ICD-10 | Cognitive reference age | Features | Prevalence rates among people with ID |
| Learning disturbance | 70–85 | F81.9 | >12 years | Learning disturbance that is not severe enough to be considered an intellectual disability | |
| Mild | 50–69 | F70.x | 9–12 years | Slow learning performance, often delayed speech development, cultural techniques can be learned, independent living is possible, occupational traning is possible | About 80% |
| Moderate | 35–49 | F71.x | 6–9 years | Delayed language development, often with a reduced vocabulary, often delayed motor development, indepenent living may be possible with support as needed, work in a protected workplace or on a simple task is posible, cultural techniques can be learned with certain limitations | About 12% |
| Severe | 20–34 | F72.x | 3–6 years | Marked impairment of language comprehension, has no active language or can only produce individual words, needs comprehensive support in the activities of daily life | About 7% |
| Very severe | <20 | F73.x | 0–3 years | Verbal communication impossible or nearly so, needs comprehensive support in self-care and in the activities of daily life, often incontinent, somatic comorbidities (e.g., epilepsy) are common | About 1% |
IQ, intelligence quotient
The German Federal Statistical Office reported that, in 2017, 9.4% of the population (7.8 million persons) suffered from a severe disability of some kind, i.e., a degree of disability above 50%. In approximately one million persons, a disturbance of intellectual development or organic brain dysfunction was the sole or main type of disability present (2).
Methods
This review is based on pertinent publications retrieved by selective searches in the PubMed and Cochrane Library databases. The following search terms were used, among others: “intellectual (developmental) disability,” “somatic disorder,” “mental disorder,” “therapy,” and “diagnostics.”
Common genetic causes
Impaired intellectual development may be due to exogenous factors such as alcohol consumption (fetal alcohol spectrum disorder) or malnutrition during gestation, intrauterine or perinatal infection, obstetric complications, or metabolic disease, e.g., hypothyroidism. Learning impairment (IQ: 70–84) can also be caused, in part, by a lack of educational opportunities or attention from the individual’s social environment.
Chromosomal anomalies (mainly, new microdeletions) are found in some 20% of cases. Alongside monogenetic disturbances of dominant or recessive inheritance (ca. 30–40%), polygenetic disturbances have been described as well (3, 4). There are now 1222 known primary genes for ID that have been definitely clinically associated with a developmental disorder, and a further 1127 candidate genes with a possible association (5).
Increased morbidity and mortality
Mortality is three to four times higher than in the general population (6– 8). In a study in Germany, ID was found to lower life expectancy by 6 to 12 years compared to the general population: 65 to 71 vs. 77 years for men, 70–73 vs. 82.5 years for women (9). The most common causes of death are respiratory diseases (especially pneumonia), cardiovascular diseases, and cancer (7, 8, 10). Aside from unpreventable conditions such as multimorbidity or neurodegenerative diseases, the preventable contributory causes of death include aspiration pneumonia (in persons with unrecognized dysphagia), avoidable falls and injuries, insufficient vaccination, lack of preventive care, and polypharmacy (6, 11– 14).
The mental developmental age must be considered within the biopsychosocial model of disease
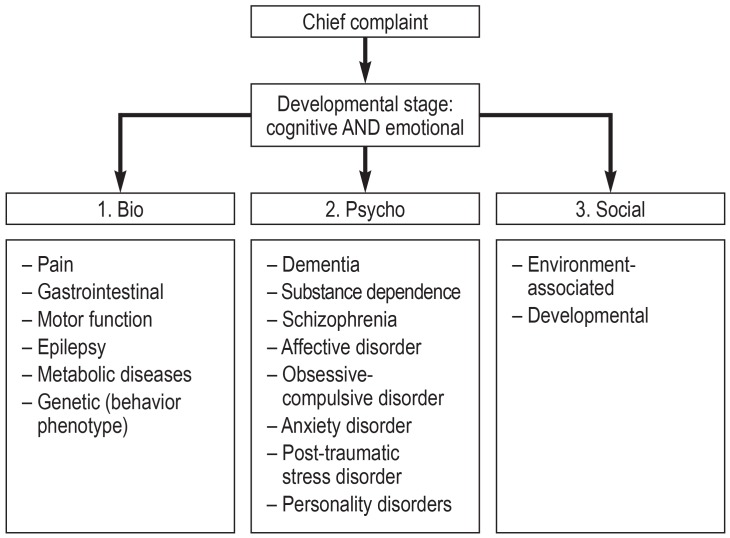
The history and the findings of the physical and psychiatric examination are supplemented with historical information from the main persons that interact with the patient in the major areas of his or her life. The basis of the evaluation is the biopsychosocial model of disease (figure), extended by consideration of the patient’s emotional development. This model provides insight into the individual’s mental developmental age, which may be very different from his or her biological age, and which can be determined using a scale of emotional development (15– 20). In the light of the individual’s emotional and cognitive stage of development, modes of behavior become intelligible and diagnostic systems in common international use can be applied (efigure). For example, in a person with a mental reference age of about three years, oppositional defiant behavior may be developmentally appropriate and of no pathological significance.
Figure.
The biopsychosocial model of disease
* Autism-spectrum disorders, attention-deficit/hyperactivity disorder, emotional developmental disorders, developmental trauma disorders, attachment disorders (modified from [e60]: Sappok T (ed.): Psychische Gesundheit bei intellektueller Entwicklungsstörung. Stuttgart: Kohlhammer 2018; reprinted with the kind permission of Kohlhammer Verlag)
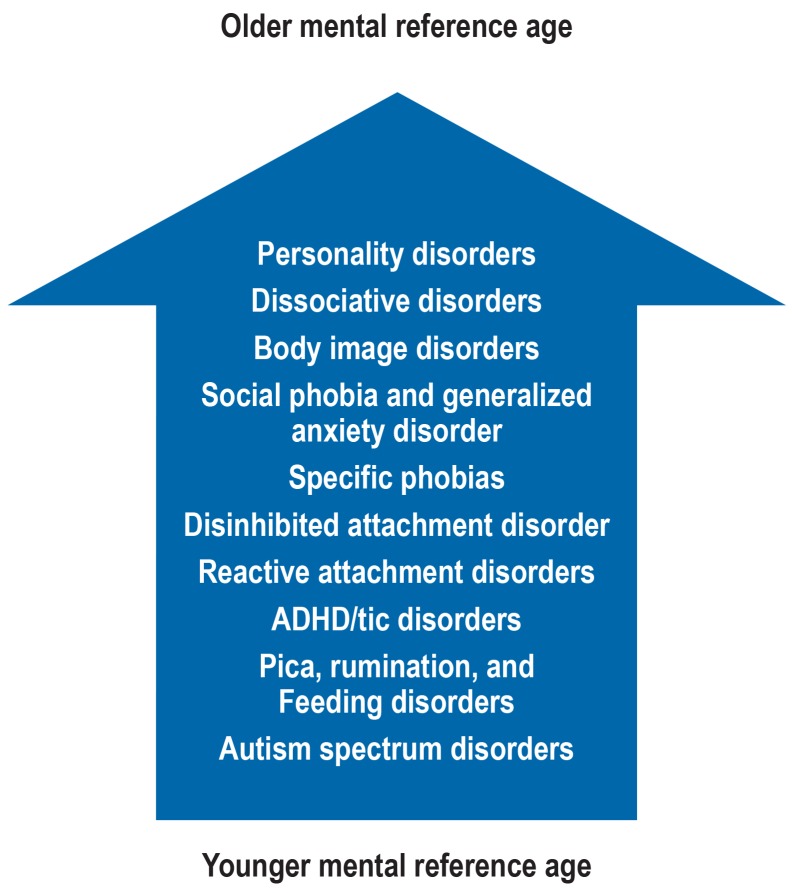
eFigure.
The link between psychiatric disturbances and mental developmental age
The frequency of certain mental illnesses depends, among other things, on mental developmental age. The arrow symbolizes increasing mental developmental age. Certain disorders are more common in persons with a low mental developmental age (e.g., autism) or may occur only in such persons (e.g., pica, rumination, feeding disorders); while, for other disorders, a minimal developmental age appears to be a prerequisite. For example, the development of a socal phobia or of a body-image disorder requires the prior development of mentalizing capacity (theory of mind). Other types of mental illness, e.g., affective disorders, post-traumatic stress disorder, and dementia, can arise independently of mental developmental age and can be found at all stages of development.
ADHD, attention-deficit/hyperactivity disorder
Adaptation of the diagnostic assessment
Patients with ID can often give no more than a limited account of their own symptoms and may express their distress or pain in unusual ways (box 1) (21). In general, any sudden change in the pattern of behavior should prompt suspicion of, and diagnostic evaluation for, an underlying somatic disease (table 1) (22). Somatic distress, and pain in particular, often leads to aggression against others, or against the patient him- or herself (22); this can complicate the clinical assessment. In such cases, an imaging study under analgesia/sedation, or even under general anesthesia, may be needed and, if so, must be undertaken despite the additional cost and labor involved. Knowledge of the patient’s emotional reference age can be helpful in the interpretation and diagnostic classification of observed behavior patterns (23). Communication between the physician and the patient should obey the rules of simple language (24), and the physician should give the patient sufficient time to answer questions (the “6-second rule”) (box 2) (25).
BOX 1. Case illustration.
Mr. Walter is 57 years old and has lived for many years in a living facility with round-the-clock assistance. He has previously been given the diagnoses of deafness, severe intellectual disability, and recurrent depression. He is referred to the psychiatric service because of suspected agitated depression. On psychiatric examination of the mute patient, he is seen to be happy when playing clapping games, which he is known to like. He makes good contact with the examiner, laughs, and seems relaxed. He initiates multiple further rounds of play. His mood abruptly transforms into loud complaints when he is asked to stand up and walk. Physical examination reveals internal rotation and shortening of the left leg. A hip x-ray confirms the clinical suspicion of a left femur fracture.
Because of limitations in history-taking (in this case, the absent history of a fall) and in physical and psychiatric examination (the patient cannot follow instructions or speak), the diagnostic assessment of a new (in this case: plaintive) type of behavior is more difficult than usual. It is all the more important, therefore, that the potential somatic causes be thoroughly investigated, and that persons from the patient’s near social environment be called in to assist in the medical evaluation and treatment of persons with cognitive impairment.
Table 1. Potential attribution of behaviors to different underlying causes of pain.
| Behavior | Possible causes | Diagnostic test or empirical treatment |
| Rolling and throwing self on the ground, “like a seizure” | Colic | Upper abdominal ultrasoundInternal medical diagnostic work-up |
| Striking self in the face, spitting | Toothache, sinusitis, herpes zoster | Medical and dental examination |
| Agitation, self-inflicted injury | Pruritic skin disease | Inspection of the unclothed patient, physical examination of the entire body |
| Rubbing the ear | Otitis, tubal ventilation disturbance | Otoscopy, nose drops against swelling |
| Refusal of food | Neck pain, toothachepharyngitis, ulcer | Oral inspectionGastroscopy as indicated |
| Manipulation in the genital area | Urinary tract infection or other infection | Urinalysis; inspection and examination of the genital region |
| Regurgitation, rumination | Reflux, achalasia, gastrointestinal disease | Physical examination H2-blockers, gastroscopy as indicated |
| Moor agitation, aggression against others or self, shouting | Urinary retention, fractures, other acute and severe pain (e.g., testicular torsion!) | Whole-body physical examination including digital rectal examination, CT/MRI under general anesthesia |
| Shouting, antalgic posture | Fracture, other injury | Physical examination, x-rays, CT |
CT, computed tomography; MRI, magnetic resonance imaging
BOX 2. Recommendations for effective physician–patient communication.
Use short sentences without subordinate clauses.
Use words and formulations that are used by the patient.
Make use of persons in the patient’s near social environment as “translators.”
Avoid foreign words, metaphors, irony, and negatives (say, e.g., “Speak softly” rather than “Don’t shout“).
Check whether you have been understood by asking the patient to repeat what you said in his or her own words.
Work with pictures or objects to illustrate what you mean.
Demonstrate how you will be examining the patient.
Involve the patient (e.g., the patient can be “doctor” to a stuffed animal or listen to his/her own heart via stethoscope).
Let diagnostic tests be prepared and practiced in advance with persons whom the patient trusts, e.g., blood drawing, blood-pressure measurement, electrocardiography, or encephalography, letting the patient become acquainted with the necessary materials and procedures ahead of time in his or her own familiar living environment.
The operationalized diagnostic systems (DSM-5, ICD-10) are often of limited utility for persons with ID, because the disease manifestations must be interpreted against the background of their emotional and intellectual stage of development (figure). The Royal College of Psychiatrists has adapted the ICD-10 criteria in its Diagnostic Criteria for Learning Disabilities (26). An overview of standardized examining techniques is given in eTable 2. These diagnostic instruments can be used to screen for certain suspected diagnoses and modes of behavior (e1– e23). Definitively establishing a diagnosis is the physician’s task; in complex situations involving, e.g., autism or dementia, the diagnosis may need to be determined in a multiprofessional case conference (27).
Common somatic diseases
Many of the genetically based disorders are mutiorgan diseases requiring treatment by specialists from multiple medical disciplines (table 2). Pediatricians and pediatric neurologists have broad training, but adult patients generally need to be treated by multiple specialists, with the primary care physician coordinating the specialized consultations. For this purpose, specialized outpatient clinics are well-established in academic hospitals. In Germany, these patients can also be cared for in the newly founded medical centers for adults with disabilities (Medizinische Zentren für Erwachsene mit Behinderung, MZEB). Care requirements are highly disease-specific (e24, e25): adult Down syndrome patients suffer mainly from neurologic disturbances (e26), while those with tuberous sclerosis have neoplasias and epilepsy (e27), those with fragile X syndrome have mental abnormalities, and those with Curschmann–Steinert syndrome have sociomedical difficulties, respiratory disturbances, and cardiological problems (e28, e29). In general, the more severe the intellectual disability, the more intense the patient’s medical care needs to be.
Table 2. Complications of common genetic syndromes with intellectual disability in adulthood that are of significance for the primary care physician.
| Syndrome | Genetic background/frequency | Organ(s) involved | Clinical manifestations | Tasks for the primary care physician |
| Down syndrome | Trisomy of chromosome 21 with various genetic variants: free trisomy (95%), translocational trisomy, mosaic trisomy 1/600 newborns |
Thyroid | Hypothyroidism | Annual TSH checks |
| Heart | Mitral/aortic valve disease, ASD, ASVD |
Cardiac ultrasound, care by a cardiologist; risk of endocarditis! | ||
| Blood | Acute myeloid leukemia (1/100) | If nonspecific symptoms are present, differential blood count | ||
| Metabolism | Obesity | Proper nutrition and exercise | ||
| Brain | Alzheimer dementia Gait disturbance Epilepsy (10%, especially myoclonic epilepsy) |
Neurological consultation in case of a cognitive decline, behavioral change, or impairment of consciousness | ||
| Skeleton | Atlantoaxial dislocation Hip dysplasia |
Orthopedic examination, cervical spine x-ray | ||
| Respiration | Sleep apnea | Polygraphy as indicated | ||
| Sensory organs | Impaired hearing Visual disturbance (70%), cataract |
Otological and/or ophthalmological consultation if there appears to be a disturbance (behavior!) | ||
| Fragile X syndrome | Trinucleotide expansion in the FRM1 gene (fragile X mental retardation 1) on the X chromosome Males: 1/1200 Females: 1/2500 |
Brain | Autism Behavioral disturbance ID Epilepsy (20%) |
Psychiatric care Special needs education Neurologic care, EEG |
| Skeleton | Scoliosis Ankle deformity |
Orthopedic care / concomitant orthopedic care | ||
| Heart | Mitral valve prolapse | Cardiologist, cardiac ultrasound | ||
| Respiration | Sleep apnea | If symptomatic, polygraphy | ||
| Tuberous sclerosis (TS) | Autosomal dominant mutation in the TSC1 or TSC2 gene on chromosome 9q34 or 16q13, repsectively, causing overactivation of mTOR 1/5800; 60% new mutations |
Brain | Tubers, developmental disorder, ID, epilepsy, tumors (giant-cell astrocytoma), hydrocephalus | Concomitant neurological careAnticonvulsants Periodic follow-up head CT or MRI (on an individual basis) |
| Skin | Adenoma sebaceum | Concomitant dermatological care | ||
| Kidneys | Angiomyolipoma | Renal ultrasound, abdominal MRI, GFR | ||
| Lung | Lymphangioleiomyomatosis (interstitial lung disease) | Pulmonary function tests,chest CT as indicated | ||
| Heart, skin, teeth, eyes | Non-cancerous tumors | Referral to a TS center (treatment with an mTOR inhibitor?) |
||
| MD-1 (myotonic dystrophy type 1, Curschmann–Steinert disease) | Autosomal-dominant trinucleotide expansion in the untranslated 3´ region of the dystrophia myotonica protein kinase (DMPK) gene onchromosome 19 1/10 000 |
Muscles | Progressive, mainly distal myotonia | Physiotherapy, physical aids |
| Brain | Tetraparesis ID only with juvenile onset and in congenital forms Organic personality change |
Concomitant psychiatric care as indicated Psychosocial assistance |
||
| Respiration | Respiratory muscle paralysis Respiratory drive (80%) |
Pulmonary function teststcCO 2 in sleep (inpatient sleep study), indication for non-invasive ventilation | ||
| Pancreas | Diabetes mellitus (20%) | HbA1c, glucose | ||
| Heart | RLS (arrhythmia, sudden cardiac death) | Concomitant care by a cardiologist Long-term ECG Check indication for pacemaker |
||
| Sensory organs | Cataract, hearing impairment | Concomitant opthalmological care | ||
| Rett syndrome | Dominant mutation of the MECP2 gene on chromosome Xp28, 90% new mutations 1/10 000 in girls, very rare in boys |
Brain | Severe, progressive developmental disorder, epilepsy, spasticity | Concomitant care by a neurologist (always) and a psychiatrist (in case of behavioral disturbances (epilepsy center) |
| Skeleton | Scoliosis Microcephaly |
Corset, positional aids, walking aids Pediatric (neuro-)orthopedic care | ||
| Teeth | Bruxism with destruction of the teeth | Dentist, orthodontist | ||
| Deletion syndrome 22q11.2 (DiGeorge syndrome, velocardiofacial syndrome) | The most common chromosomal microdeletion (1/3000), generally due to a new mutation | Immune system | Immune deficiency | Primary care physician, immunologist |
| Endocrine system | Hypoparathyroidism | Endocrinologist | ||
| Heart | Congenital cardiac anomalies Aortic stenosis Multiple organ malformations |
Cardiologist, cardiac surgeon, pediatric surgeon | ||
| Mental health | ID, schizophrenic psychoses | Concomitant psychiatric treatment | ||
| Prader–Willi syndrome | Multiple mechanisms: 1. deletion 15q11q13 of paternal origin (70%) 2. maternal uniparental disomy (15%) 3. imprinting center defect: the corresponding genes on the paternal chromosome are turned off. Frequency: 1/10 000 |
Metabolism | Obesity, diabetes mellitus, metabolic synrome | Dietary counseling Diabetes therapy Behavioral therapy |
| Endocrine system | Hypogonadism Short stature |
Serial endocrinological testing | ||
| CNS | Sleep apnea syndrome ID |
Polygraphy/polysomnography |
ASD, autism spectrum disorders; ASVD, atrioventricular septal defect; CNS, central nervous system; CT, computed tomography; ECG, electrocardiogram; GFR, glomerular filtration rate; EEG, electroencephalography; HbA1c, hemoglobin A1c; ID, intellectual disability; MECP2, methyl-CpG binding protein 2; MRI, magnetic resonance imaging; mTOR, mechanistic target of rapamycin; RLS, restless legs syndrome; tcCO2,transcutaneously measured carbon dioxide; TSC, tuberous sclerosis complex; TSH thyroid-stimulating hormone; TS- center, tuberous sclerosis center
Epilepsy
The prevalence of epilepsy is 0.5% in the general population, 15% in persons with mild intellectual disability, and 30–50% in persons with severe to very severe intellectual disability (28). Mortality is elevated because of sudden death in epilepsy (SUDEP), seizure-related injuries, and an increased tendency to fall in persons taking antiepileptic drugs (28).
Pain
Persons with ID often suffer from pain of various causes that may go unrecognized, or is recognized only after a delay, because of the unusual presentation. Pain adversely affects sleep and quality of life in general (29, e30, e31). table 1 contains information on a number of characteristic pain-related behavior patterns and their association with organ diseases (21, 30).
Chronic pain is a feature, for example, of Rett syndrome (table 2) and of cerebral palsy (e30– e32).
Gastrointestinal disturbances
Chronic constipation is common in persons with ID and can take a severe course, e.g., with overflow coprostasis and pseudodiarrhea, potentially even resulting in death (31, e33). Meticulous rectal digital examination and laxative treatment can spare the patient an unnecessary diagnostic evaluation (31).
Gastro-esophageal reflux is more common with more severe disability (>50% in persons with IQ <35); risk factors include cerebral palsy, scoliosis, and anticonvulsive drugs. Sleep impairment, depressive mood disturbance, rumination, inappetence, and agitation are potential manifestations (32).
Cardiovascular diseases
Cardiovascular disease is no more common among persons with ID than in the general population but is less commonly diagnosed and treated. The cardiovascular risk is elevated by the increased prevalence of obesity and diabetes mellitus (13, e34).
Cancerous and non-cancerous tumors
Persons with ID have a different profile of cancers than the general population (7). Some cancers are more common in certain genetic syndromes, e.g., acute lymphoblastic leukemia is 20 times more common in persons with Down syndrome, because of a CRLF2 rearrangement (table 2) (e35). Increased mortality from certain cancers, e.g. colorectal cancer, and shortened median survival times are attributed to delayed diagnosis, relative lack of preventive care, and poor treatment adherence (6, 14). Patients with tuberous sclerosis, the most common phakomatosis associated with ID, can develop giant-cell astrocytoma, possibly leading to hydrocephalus, as well as renal angiomyolipoma (table 2) (e27).
Movement disorders
The syndrome called cerebral palsy is the most common sequela of brain damage in early childhood (e32); there are also dystonic, athetoid, and ballistic syndromes. These patients need lifelong interdisciplinary neuro-orthopedic and neurological care, with individually tailored operations, physical aids, and drugs to improve their motor function (33).
Dementia
Persons with ID, independently of their degree of cognitive impairment, develop dementia five times more often than the general population; the frequency of dementia is particularly elevated in persons with Down syndrome (34, e36). Characteristic features include memory impairment, loss of practical abilities in everyday life, and the early appearance of behavioral abnormalities (e37– e39). The two-step diagnostic assessment consists of neuropsychological evaluation and history-taking from persons in the patient’s near social environment (etable 2) (e22, e23). Laboratory and imaging studies are essential to rule out treatable causes, such as hypothyroidism (e26). Dementia is treated with acetylcholinesterase (AChE) inhibitors in accordance with current guidelines; patients with ID, however, are more vulnerable to side effects (e.g., epileptic seizures), and thus non-pharmacological measures, e.g., adapting the patient’s physical environment to dementia, should receive due attention (35, e40).
eTable 2. Diagnostic instruments in intellectual disability (ID).
| Technique | Study | Remarks | Source |
| Genetic diagnostic tests | |||
| Chromosomal analysis | Chromosomal changes | E.g., in Down syndrome | Zweier 2018 (e1) |
| Sanger sequencing | Monogenetic changes | Identification of only 5% of the genetic causes | |
| Next-generation sequencing | Sequencing of the entire exome | Identification of ca. 40% of the genetic causes | |
| Severity of ID | |||
| Disability Assessment Scale (DAS) | 16 ordinally scaled questions for assessing the severity of ID ([ICD] F70/F71/F72/F73) | The assessment is based on competencies in everday life in the areas of continence, self-assistance (eating, washing, dressing), communication, and skills (reading, writing, money, household). | Holmes et al. 1982 (e2), Meins and Süssmann 1993 (e3) |
| Cognitive performance tests | |||
| Basic Intelligence Test Scale 2 – Revision (CFT-20-R) | Performance test for persons aged 8.5 to 60 years | Weiss 2006 (e4) | |
| Colored Progressive Matrices Test (CPM) | Logical abstract thinking and problem-solving ability | For mute or deaf persons; 4–11 years | Raven et al. 2006 (e5) |
| Kaufmann Assessment Battery (K-ABC) | Intellectual performance | Language-free version available; 3 to 12 years | Melchers and Preuss 2009 (e6); Kaufman and Kaufman 2015 (e7) |
| Snijders-Omen Nonverbal Intelligence Test | Abstract, concrete, and spatial thinking ability and perceptual performance | Language-free; 2.5 to 40 years | Snijders et al. 2005 (e8); Tellegen et al. 2012 (e9) |
| Wechsler Adult Intelligence Scale-IV (WAIS-IV) | Overall IQ and index values for language comprehension, logical thinking, working memory, and processing speed | Normed for persons with ID; 16 to 90 years | Petermann 2012 (e10) |
| Tests of emotional development | |||
| Skala der emotionalen Entwicklung – Diagnostik (SEED)[Scale of Emotional Development: Diagnostic Evaluation] | Assessment of the emotional developmental level overall and in each of 8 developmental domains | Semi-structured interview with persons near to the patient, by an expert in developmental psychology; 5-point scale:1. Adaptation: up to 6 months; 2. Socialization: 7th to 18th month; 3. Individuation: 19th to 36th month; 4. Identification: 4th to 7th year 5. Reality awareness; 8th to 12th year | Sappok et al. 2018 (20) |
| Behavioral tests | |||
| ABC Analysis | Functional contexts of modes of behavior | Structured behavioral observation and context analysis with protocol forms, with the following components: (A) Antecedent = situation before the behavior arose(B) Behavior = the behavior itself, and (C) Consequence = the immediate reaction of persons around the patient to the behavior | Bienstein and Werner 2018 (e11) |
| Target symptom analysis | Appearance and severity of types of behavior over the course of time | structured behavioral observation with protocol forms: persons near the patient document the appearance and severity of the target manifestations, e.g., over the course of one month | |
| Aberrant Behavior Checklist (ABC) | Problematic behaviors in the areas of irrtability, lethargy, stereotypy, hyperactivity, and language impairment | 4-point scale, to be filled out by persons who are near to the patient | Aman and Sing 1994 (e12) |
| Verhaltensfragebogen bei Entwicklungsstörungen (VFE)[Behavior Problem Inventory (BPI)] | Behavioral abnormalities on five scales: 1. disruptive/antisocial, 2. self-absorbed, 3. communication disturbance, 4. fear, 5. social relationship disorder | 3-point scale, to be filled out by persons who are near to the patient | Steinhausen and Winkler-Metzke 2011 (e13) |
| Modified Overt Aggression Scale (MOAS) | Severity of aggressive behaviors (verbal aggression, damage to property, injury to oneself and others) | 5-point scale, to be filled out by persons who are near to the patient | Knoedler 1989 (e14); Yudofsky 1986 (e15) |
| Inventar zur funktionellen Erfassung selbstverletzenden Verhaltens (IfES) [Inventory of self-harm behaviors] | The function of self-injurious behavior | Bienstein and Nussbeck 2010 (e16) | |
| Psychiatric tests | |||
| Diagnostic Assessment for the Severly Handicapped (DASH-II) | Psychopathology in adults with severe and very severe ID | Semistructured interview of persons near to the patient; provides evidence of mental illness | Matson et al. 1991 (e17) |
| Psychiatric Assessment Schedule for Adults with Developmental Disabilities (PAS-ADD) | Organic or mental disease in persons with ID | Provides evidence of an organic, affective, or psychotic disorder | Moss et al. 1998 (e18) |
| Psychiatric Instrument for the Intellectually Disabled Adult (SPAID) | Psychiatric diagnoses in persons with ID | Currently available only in Italian; translation into German, and validation, are planned (Cooperation: Bertelli/Sappok) | Bertelli et al. 2012 (e19) |
| Tests for autism | |||
| diagnostischer Beobachtungs-bogen für Autismus-Spektrum-Störungen – revidiert (DiBAS-R)[questionnaire on behavior] | Suspected autism | To be filled out by persons near to the patient; 4-point scale; based on the ICD-10/DSM-5 creiteria for autism | Sappok et al. 2015 (e20) |
| Autismus Check-List (ACL) | Suspected autism; assessment of early childhood or atypical autism | Based on the ICD-10 research criteria; supports structured history-taking and physical examination in patients suspected of being autistic; for physicians and psychologists | Sappok et al. 2015 (e20) |
| Pain evaluation | |||
| Evaluation of Pain in Adults and Adolescents with Multiple Handicaps (EDAAP) | Behaviors relevant to pain | Screening questionnaire for pain on the basis of 11 criteria, on a 5-point scale, for persons near to the patient | Belot 2009 (e21) |
| Dementia | |||
| Checkliste zur Erfassung von demenziellen Entwicklungen bei Menschen mit Intelligenzminderung (CEDIM) | Dementia screening | Consists of seven questions for persons near to the patient | Schanze 2012 (e22) |
| Demenztest für Menschen mit Intelligenzminderung (DTIM) [Dementia Checklist, resp. Dementia Test, for Persons with Intellectual disability] | If dementia is suspected | The test consists of two parts: a neuropsychological part (orientation, language, attention, memory, planning and acting, abstract logical thinking, and perception/communication) and an assessment by another person | Müller and Kuske 2019, in press (e23) |
Common mental illnesses
According to population-based studies from the United Kingdom, the point prevalence of mental illness in persons with ID is approximately 20% (36, 37). In addition to mental illness in the narrow sense, some 25% of persons with ID have severe behavioral disturbances that are not attributable to a somatic or mental illness (36– 38). Behavioral disturbances have been defined as culturally inappropriate behavior of such intensity, frequency, and duration that it either threatens the physical integrity of the patient or others or else renders the patient’s use of public facilities difficult or impossible (38).
Substance dependence
Persons with mild ID have similar living situations to the general population and also have a similar point prevalence of substance dependence (1.8%). On the other hand, persons with severe or very severe ID suffer less commonly from substance dependence (0.5%); the cases that do arise are often iatrogenic (36). Substance dependence in persons with ID is treated with a combination of withdrawal, dishabituation, psychotherapy, and environmental adaptation.
Schizophrenia
The point prevalence of schizophrenic psychosis is elevated in persons with mild ID (6%) and lower in persons with more severe ID (36). In circumscribed syndromes, such as velocardiofacial syndrome (Table 2, the prevalence is increased (persistent in about 30%) (e41). Schizophrenia may go unrecognized in persons with ID because of “diagnostic overshadowing,” i.e., misinterpretation of schizophrenic manifestations as part of the disability (e.g., movement disturbances, negative manifestations). Hallucinations may not be reported by the patient, and thought disorders may not be interpretable. The following aspects may point to the presence of schizophrenia:
Age of onset (young adulthood)
Positive family history
Talking with persons who are not there; covering or hitting the ears
Paroxysmal aggression and anxiety.
Affective disorders
The prevalence of affective disorders is the same across all degrees of severity of ID. The point prevalence is 6–7 %, similar to that in the general population (9.3%) (36, e42). The risk of depression is elevated in certain syndromes, such as fetal alcohol spectrum disorder (FASD), Prader–Willi syndrome, phenylketonuria, and Down syndrome, while bipolar affective disorder is more common in velocardiofacial syndrome, fragile X syndrome, Klinefelter syndrome, Rubenstein–Taybi syndrome, and FASD (e43). Depressed mood is often less obvious in intellectually disabled persons. It may manifest itself as:
Self-injury and aggression
Irritability
Psychomotor agitation, screaming
Regressive behavior
Sleeping and eating disturbances.
Antidepressants and mood stabilizers are prescribed; tricyclic antidepressants should be avoided, because persons with ID are more vulnerable to their side effects (e44). Adapted psychotherapeutic methods can also be used, particularly cognitive behavioral therapy (e45).
Anxiety disorders
Anxiety disorders can be seen in patients with a mental developmental age of at least six months (“first socialization” on the German emotional development scale, Skala der emotionalen Entwicklung—Diagnostik [SEED]-2). Social phobia and generalized anxiety disorder can only arise in the presence of mentalization ability and are thus seen only in persons with an emotional reference age of at least four years. The exact prevalence of anxiety disorders in unclear; their point prevalence is inversely related to the severity of ID (International Statistical Classification of Diseases and Related Health Problems [ICD] F70, ca. 6%; F71–73, ca. 2.4%) (36). Specific phobias, e.g., of dogs or elevators, are often seen. Exposure therapy and other treatments are often effective, but the procedure must be adapted to the intellectual and emotional developmental age of the patient (e46).
Disorders due to emotional trauma
Disabled persons often experience violence (39). In a meta-analysis, the risk of experiencing violence among disabled adults was found to be 6%, corresponding to an odds ratio [OR] of 1.5 compared to the general population (e47). Disabled children, in fact, reportedly have even higher prevalences of combined violent experiences (27%, OR: 3.68), physical violence (20%; OR: 3.56), and sexual violence (14%; OR: 2.88) (e48). Institutionalization, dependence on others, lessened coping capacity, and lack of social support make the intellectually disabled more vulnerable to the experience of an emotionally traumatizing event, and about 10% of those affected develop post-traumatic stress disorder (e49). The diagnostic assessment can be performed with trauma-biographical scales as well as structured instruments for the evaluation of disorders due to emotional trauma (e49). As for treatment, there have been individual case series on the efficacy of Eye Movement Desensitization and Reprocessing (EMDR) (39, e50).
Autism spectrum disorders
In persons with ID, the prevalence of autism spectrum disorders is 7.5–15%, much higher than the estimated 1% in the general population (36, 37, e51, e52). Suspected autism should be evaluated in a multistep procedure; various screening scales and structured behavioral observations can be used to support the diagnostic process (etable 2) (e20). Even if autism cannot now be cured, special needs education in qualified hands can improve both the level of social functioning (effect size [ES]: 0.65) and maladaptive behavior (ES: –0.92) (e53). Patients with severe behavioral abnormalities can be treated, for a limited time, with low doses of risperidone or aripiprazole (evidence level Ia) (e54, e55). Methylphenidate, atomoxetine, and alpha-2 agonists are effective in attention-deficit/hyperactivity disorder (ADHD) (e56), and melatonin is beneficial in sleep disorders (e57). There is no evidence for the efficacy of serotoninergic drugs or antiepileptic drugs in the treatment of autism (e58, e59).
Therapeutic procedure
Somatic and mental illnesses are treated by the same principles as in non-disabled persons. The need-based, goal-oriented overall treatment plan should take all levels of disturbance (bio-psycho-socio-emotional) and all persons in the patient’s near environment into account. Psychoactive drugs should be used only for strict indications, and as monotherapy wherever possible (16– 19, 40), in patient-centered fashion, with regular reassessment of the indication, drug holidays, and drug monitoring as matters of routine. Psychoactive drugs for the treatment of behavioral problems should be avoided if possible and given only in rare cases, transiently, and at low doses. All drugs should be started at a low dose, with slow escalation up to the lowest possbile target dose (“start low, go slow”). Polypharmacy and off-label use should be avoided, and reserve drugs should be used only in clearly defined situations (11, 16– 19, 40). Non-drug treatments are usually the treatment of first choice in patients with mild ID; simple language is used, learning speed is adapted to the patient’s situation, and more experiential and body-oriented exercises are done (24). In severe or very severe ID, special needs education and developmentally based approaches are the main elements of treatment (23).
Medical care
The medical care of persons with ID is complex, requiring thinking across disciplinary boundaries and, sometimes, special knowledge and skills. In order to teach the latter, specialty societies such as the German Society for Persons with Intellectual and Multiple Disability (Deutsche Gesellschaft für Medizin für Menschen mit geistiger und mehrfacher Behinderung, DGMGB; www.dgmgb.de) and the German Society for Mental Health in Persons with Intellectual Disability (Deutsche Gesellschaft für seelische Gesundheit bei Menschen mit geistiger Behinderung, DGSGB; www.dgsgb.de) host regular contining medical education events and issue specialized publications, such as the journal “Inklusive Medizin” or the DGSGB materials collection. A number of providers of continuing medical education offer a certificate of training in medicine for persons with intellectual or multiple disability that is recognized by the German Medical Association. The organizational challenges of this compex work were taken into account in the founding, in 2016, of medical treatment centers for adults with intellectual disability or severe multiple disabilities (Medizinische Behandlungszentren für Erwachsene mit geistiger Behinderung oder schweren Mehrfachbehinderungen, (MZEB; www.bagmzeb.de) of which there have been 38 in Germany since early 2019.
Key Messages.
Persons with intellectual disability (ID) have elevated morbidity and mortality.
The medical assessment of ID is performed according to the biopsychosocial model of disease and includes an estimation of the patient’s developmental age.
The patient’s modes of behavior and complaints must be interpreted in the light of his or her cognitive and emotional stage of development.
In the care of the patient, simple language should be used, and an appropriate physician–patient relationship should be established.
In Germany, specialized medical centers (MZEB) are available for help with unusually complex clinical situations.
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
Dr. Sappok has received royalities for authoring or co-authoring publications on the topic of this article. She has received third-party funding for an SEO project from the Bodelschwinghsche Stiftungen Bethel.
Dr. Winterholler serves on the board of the BAG-MZEB. He has received lecture honoraria from Merz Pharma, Ipsen Pharma, Allergan Deutschland, and UCB Pharma.
Prof. Diefenbacher has received lecture honoraria and reimbursement of travel expenses from FomF GmbH.
References
- 1.WHO. ICD-11 for mortality and morbidity statistics (ICD-11 MMS) 2018 version. https://icd.who.int/browse11/l-m/en (last accessed on 26 February 2019) 2017 [Google Scholar]
- 2.Statistisches Bundesamt. Statistik der schwerbehinderten Menschen, Kurzbericht. www.destatis.de (last accessed on 12 August 2019) [Google Scholar]
- 3.Zweier C. Genetische Störungen Psychische Gesundheit bei intellektueller Entwicklungsstörung. Ein Lehrbuch für die Praxis. In: Sappok T, editor. Kohlhammer Verlag. Stuttgart: 2018. pp. 81–87. [Google Scholar]
- 4.Vissers LE, Gilissen C, Veltman JA. Genetic studies in intellectual disability and related disorders. Nat Rev Genet. 2016;17:9–18. doi: 10.1038/nrg3999. [DOI] [PubMed] [Google Scholar]
- 5.Kochinke K, Zweier C, Nijhof B, et al. Systematic phenomics analysis deconvolutes genes mutated in intellectual disability into biologically coherent modules. Am J Hum Genet. 2016;98:149–164. doi: 10.1016/j.ajhg.2015.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glover G, Williams R, Heslop P, Oyinlola J, Grey J. Mortality in people with intellectual disabilities in England. J Intellect Disabil Res. 2017;61:62–74. doi: 10.1111/jir.12314. [DOI] [PubMed] [Google Scholar]
- 7.O‘Leary L, Cooper SA, Hughes-McCormack L. Early death and causes of death of people with intellectual disabilities: a systematic review. J Appl Res Intellect Disabil. 2018;31:325–342. doi: 10.1111/jar.12417. [DOI] [PubMed] [Google Scholar]
- 8.Ng N, Flygare Wallén E, Ahlström G. Mortality patterns and risk among older men and women with intellectual disability: a Swedish national retrospective cohort study. BMC Geriatr. 2017;17 doi: 10.1186/s12877-017-0665-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dieckmann F. Alter erleben. Lebensqualität und Lebenserwartung von Menschen mit geistiger Behinderung im Alter. In: Metzler H, editor. Kommunalverband für Jugend und Soziales. Stuttgart: 2013. [Google Scholar]
- 10.Oppewal A, Schoufour JD, van der Maarl HJK, Evenhuis HM, Hilgenkamp TIM, Festen DA. Causes of mortality in older people with intellectual disability: results from the HA-ID study. Am J Intellect Dev Disabil. 2018;123:61–71. doi: 10.1352/1944-7558-123.1.61. [DOI] [PubMed] [Google Scholar]
- 11.Schoufour JD, Oppewal A, van der Maarl HJK, et al. Multimorbidity and polypharmacy are independently associated with mortality in older people with intellectual disabilities: a 5-year follow-up from the HA-ID study. Am J Intellect Dev Disabil. 2018;123:72–82. doi: 10.1352/1944-7558-123.1.72. [DOI] [PubMed] [Google Scholar]
- 12.Robertson J, Chadwick D, Baines S, Emerson E, Hatton C. Prevalence of dysphagia in people with intellectual disability: a systematic review. Intellect Dev Disabil. 2017;55:377–391. doi: 10.1352/1934-9556-55.6.377. [DOI] [PubMed] [Google Scholar]
- 13.Cooper SA, Hughes-McCormack L, Greenlaw N, et al. Management and prevalence of long-term conditions in primary health care for adults with intellectual disabilities compared with the general population: a population-based cohort study. J Appl Res Intellect Disabil. 2018;31(Suppl 1):68–81. doi: 10.1111/jar.12386. [DOI] [PubMed] [Google Scholar]
- 14.Wallace RA. National disability insurance scheme, health, hospitals and adults with intellectual disability. Intern Med J. 2018;48:351–359. doi: 10.1111/imj.13671. [DOI] [PubMed] [Google Scholar]
- 15.Sappok T. Diefenbacher A, editor. Die 4. Dimension: Erweiterung des bio-psycho-sozialen Krankheitsmodells um die emotionale Entwicklungskomponente bei Menschen mit geistiger Behinderung. Bielefeld: Bethel Verlag. 2017 [Google Scholar]
- 16.Gardner WI, Dosen A, Griffiths DM. NADD Press. New York: 2006. Practice guidelines for diagnostic, treatment and related support services for people with developmental disabilities and serious behavioral problems. [Google Scholar]
- 17.NICE. Guideline: Challenging behavior and learning disabilities: prevention and interventions for people with learning disabilities whose behavior challenges. www.nice.org.uk/guidance/ng11. (last accessed on 2 March 2019) 2015 [PubMed] [Google Scholar]
- 18.AWMF. Leitlinie: Autismus-Spektrum-Störungen im Kindes-, Jugend- und Erwachsenenalter. www.awmf.org (last accessed on 23 February 2019) 2016 [Google Scholar]
- 19.Canadian Consensus Guidelines. Primary care of adults with developmental disabilities. Can Fam Physician. 2011;57:541–553. [PMC free article] [PubMed] [Google Scholar]
- 20.Sappok T, Zepperitz S, Barrett BF, Došen A. Skala der emotionalen Entwicklung - Diagnostik (SEED) Bern: Hogrefe. 2018 [Google Scholar]
- 21.Sappok T, Sinzig J, Lehmkuhl G, Diefenbacher A. Berger M, editor. Kapitel 24: Intelligenzminderung Psychische Erkrankungen, Klinik und Therapie, München. Elsevier Urban & Fischer. (6) 2018 [Google Scholar]
- 22.de Winter CF, Jansen AA, Evenhuis HM. Physical conditions and challenging behaviour in people with intellectual disability: a systematic review. J Intellect Disabil Res. 2011;55:675–698. doi: 10.1111/j.1365-2788.2011.01390.x. [DOI] [PubMed] [Google Scholar]
- 23.Sappok T, Zepperitz S. Hogrefe 2nd edition. Bern: 2019. Das Alter der Gefühle - über die Bedeutung der emotionalen Entwicklung bei geistiger Behinderung. [Google Scholar]
- 24.Mensch zuerst - Netzwerk People First Deutschland e. V. Das neue Wörterbuch für Leichte Sprache. Kassel. Nordlicht Digitaldruck. 2008 [Google Scholar]
- 25.Vogel M, Feuerherd C. Die Erhebung des psychopathologischen Befundes Psychische Gesundheit bei intellektueller Entwicklungsstörung. Ein Lehrbuch für die Praxis. In: Sappok T, editor. Kohlhammer Verlag. Stuttgart: 2018. pp. 281–289. [Google Scholar]
- 26.The Royal College of Psychiatrists. Gaskell. London: 2001. DC-LD: Diagnostic criteria for psychiatric disorders for use with adults with learning disabilities/mental retardation. [Google Scholar]
- 27.Bergmann T, Diefenbacher A, Heinrich M, Riedel A, Sappok T. Perspektivenverschränkung: Multiprofessionelle Autismusdiagnostik bei erwachsenen Menschen mit Intelligenzminderung. Z Psychiatr Psych Ps. 2016;64:257–267. [Google Scholar]
- 28.Robertson J, Hatton C, Emerson E, Baines S. Prevalence of epilepsy among people with intellectual disabilities: a systematic review. Seizure. 2015;29:46–62. doi: 10.1016/j.seizure.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 29.Walsh M, Morrison TG, McGuire BE. Chronic pain in adults with an intellectual disability: prevalence, impact, and health service use based on caregiver report. Pain. 2011;152:1951–1957. doi: 10.1016/j.pain.2011.02.031. [DOI] [PubMed] [Google Scholar]
- 30.Elstner S, Salzmann E. Angst-, Zwangstörungen, Belastungs-, dissoziative und somatoforme Störungen Psychiatrische Diagnostik und Therapie bei Menschen mit Intelligenzminderung. In: Schanze C, editor. Schattauer Verlag. 2. Stuttgart: 2014. pp. 129–146. [Google Scholar]
- 31.Robertson J, Baines S, Emerson E, Hatton C. Constipation management in people with intellectual disability: a systematic review. J Appl Res Intellect Disabil. 2018;31:709–724. doi: 10.1111/jar.12426. [DOI] [PubMed] [Google Scholar]
- 32.de Veer AJ, Bos JT, Niezen-de Boer RC, Böhmer CJ, Francke AL. Symptoms of gastroesophageal reflux disease in severely mentally retarded people: a systematic review. BMC Gastroenterol. 2008;11:8–23. doi: 10.1186/1471-230X-8-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Timmeren EA, van der Schans CP, van der Putten AA, et al. Physical health issues in adults with severe or profound intellectual and motor disabilities: a systematic review of cross-sectional studies. J Intellect Disabil Res. 2017;61:30–49. doi: 10.1111/jir.12296. [DOI] [PubMed] [Google Scholar]
- 34.Strydom A, Chan T, King M, Hassiotis A, Livingston G. Incidence of dementia in older adults with intellectual disabilities. ResDev Disabil. 2013;34:1881–1885. doi: 10.1016/j.ridd.2013.02.021. [DOI] [PubMed] [Google Scholar]
- 35.Livingstone N, Hanratty J, McShane R, Macdonald G. Pharmacological interventions for cognitive decline in people with Down syndrome. Cochrane Database Syst Rev. 2015;10 doi: 10.1002/14651858.CD011546.pub2. doi: 10.1002/14651858.CD011546.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cooper SA, Smiley E, Morrison J, Williamson A, Allan L. Mental ill-health in adults with intellectual disabilities: prevalence and associated factors. Br J Psychiatry. 2007;190:27–35. doi: 10.1192/bjp.bp.106.022483. [DOI] [PubMed] [Google Scholar]
- 37.Sheehan R, Hassiotis A, Walters K. Mental illness, challenging behaviour, and psychotropic drug prescribing in people with intellectual disability: UK population based cohort study. BMJ. 2015;351 doi: 10.1136/bmj.h4326. h4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Emerson E, Bromley J. The form and functioning of challenging behavior. J Intellect Disabil Res. 1995;39:388–398. doi: 10.1111/j.1365-2788.1995.tb00543.x. [DOI] [PubMed] [Google Scholar]
- 39.Rittmannsberger D, Lueger-Schuster B, Weber G. Traumafolgestörungen Psychische Gesundheit bei intellektueller Entwicklungsstörung. Ein Lehrbuch für die Praxis. In: Sappok T, editor. Kohlhammer Verlag. Stuttgart: 2018. pp. 331–37. [Google Scholar]
- 40.NICE. Guideline: Mental health problems in people with learning disabilities: prevention, assessment and management. www.nice.org.uk/guidance/ng54. (last accessed on 26 February 2019) [PubMed] [Google Scholar]
- E1.Zweier C. Kohlhammer Verlag 2018b. Stuttgart: Genetische Diagnostik In: Sappok T (eds.): Psychische Gesundheit bei intellektueller Entwicklungsstörung. Ein Lehrbuch für die Praxis; pp. 275–280. [Google Scholar]
- E2.Holmes N, Shah A, Wing L. The disability assessment schedule: a brief screening device for use with mentally retarded. Psychol Med. 1982;12:879–890. doi: 10.1017/s0033291700049175. [DOI] [PubMed] [Google Scholar]
- E3.Meins W, Süssmann D. Evaluation of an adaptive behaviour classification for mentally retarded adults. Soc Psychiatry Psychiatr Epidemiol. 1993;28:201–205. doi: 10.1007/BF00797324. [DOI] [PubMed] [Google Scholar]
- E4.Weiß R. Hogrefe Verlag. Bern: 2006. Grundintelligenztest Skala 2 - Revision (CFT 20-R) mit Wortschatztest und Zahlenfolgentest - Revision (WS/ZF-R) [Google Scholar]
- E5.Raven JC, Raven J, Court JH. Harcourt. Frankfurt am Main: 2006. Coloured progressive matrices (CPM) Deutsche Bearbeitung und Normierung. [Google Scholar]
- E6.Melchers P, Preuss U. Pearson Assessment. 8. Frankfurt: 2009. Kaufman assessment battery for children Deutschsprachige Fassung (KABC) [Google Scholar]
- E7.Kaufman AS, Kaufman NL. Hogrefe. 2. Göttingen: 2015. Kaufman assessment battery for children (KABC-2) [Google Scholar]
- E8.Snijders JTH, Tellegen PJ, Laros JA. Hogrefe. 3. Göttingen: 2005. Snijders-Oomen Non-verbaler Intelligenztest: SON-R 5½ - 17. [Google Scholar]
- E9.Tellegen PJ, Laros JA, Petermann F. Hogrefe. 1. Göttingen: 2012. Snijders-Oomen non-verbaler Intelligenztest: SON-R 6-40. [Google Scholar]
- E10.Petermann F. Pearson Assessment. 2. Frankfurt: 2012. Wechsler adults intelligence scale. [Google Scholar]
- E11.Bienstein P, Werner N. Verhaltensanalyse Psychische Gesundheit bei intellektueller Entwicklungsstörung. Ein Lehrbuch für die Praxis. In: Sappok T, editor. Kohlhammer Verlag. Stuttgart: 2018. pp. 290–296. [Google Scholar]
- E12.Aman MG, Sing NN. East Aurora, Slosson Educational Publications. New York: 1994. Aberrant behavior checklist: community supplementary manual. [Google Scholar]
- E13.Steinhausen HC, Winkler-Metzke C. Der Verhaltensfragebogen bei Entwicklungsstörungen im Erwachsenenalter (VFE-ER), Psychometrische Kennwerte und Normierung. Z Klein Psych Psychother. 2011;40:160–171. [Google Scholar]
- E14.Knoedler DW. The modified overt aggression scale. Am J Psychiatry. 1989;146:1081–1082. doi: 10.1176/ajp.146.8.1081b. [DOI] [PubMed] [Google Scholar]
- E15.Yudofsky SC, Silver JM, Jackson W, Endicott J, Williams D. The overt aggression scale for the objective rating of verbal and physical aggression. Am J Psychiatry. 1986;143:35–39. doi: 10.1176/ajp.143.1.35. [DOI] [PubMed] [Google Scholar]
- E16.Bienstein P, Nussbeck S. Hogrefe. Göttingen: 2010. Inventar zur funktionellen Erfassung selbstverletzenden Verhaltens. [Google Scholar]
- E17.Matson JL, Gardner WI, Coe DA, Sovner R. A scale for evaluating emotional disorder in severely and profound mentally retarded persons Development of the Diagnostic Assessment for the Severly Handicapped (DASH) scale. Br J Psychiatry. 1991;159:404–409. doi: 10.1192/bjp.159.3.404. [DOI] [PubMed] [Google Scholar]
- E18.Moss S, Prosser H, Costello H, et al. Reliability and validity of the PAS-ADD checklist for detecting psychiatric disorders in adults with intellectual disability. J Intellect Disabil Res. 1998;42:173–183. doi: 10.1046/j.1365-2788.1998.00116.x. [DOI] [PubMed] [Google Scholar]
- E19.Bertelli M, Scuticchio D, Ferrandi A, et al. Reliability and validity of the SPAID-G checklist for detecting psychiatric disorders in adults with intellectual disability. Res Dev Disabil. 2012;33:382–390. doi: 10.1016/j.ridd.2011.08.020. [DOI] [PubMed] [Google Scholar]
- E20.Sappok T, Diefenbacher A, Bergmann T, et al. Huber. Bern: 2015. Der Diagnostische Beobachtungsbogen für Autismus-Spektrum-Störungen - Revidiert (DiBAS-R) Ein Screening-Instrument für Erwachsene mit Intelligenzminderung. [Google Scholar]
- E21.Belot M. Der Ausdruck von Schmerz bei mehrfachbehinderten Personen: Evaluation der Schmerzzeichen bei Jugendlichen und Erwachsenen mit Mehrfachbehinderung In: Maier-Michalitsch NJ (eds.): Leben pur - Schmerz bei Menschen mit schweren und mehrfachen Behinderungen. Düsseldorf: verlag selbstbestimmtes leben. 2009 [Google Scholar]
- E22.Schanze C. Checkliste zur Erfassung von demenziellen Entwicklungen bei Menschen mit Intelligenzminderung. www.demenz-service-westliches-ruhrgebiet.de/tl_files/westliches_ruhrgebiet/Meldungen/edbMed0211_SA_SchanzeChecklisten.pdf (last accessed on 2 March 2019) 2009 [Google Scholar]
- E23.Müller SV, Kuske B. Hogrefe Verlag. Bern: 2019. Demenztest für Menschen mit Intelligenzminderung. [Google Scholar]
- E24.Duis J, van Wattum PJ, Scheimann A, et al. A multidisciplinary approach to the clinical management of Prader-Willi syndrome. Mol Genet Genomic Med. 2019 doi: 10.1002/mgg3.514. 7(3): e514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E25.McDonald-McGinn DM, Sullivan KE, Marino B, et al. 22q112 deletion syndrome. Nat Rev Dis Primers. 2015;19 doi: 10.1038/nrdp.2015.71. 1:15071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E26.Capone GT, Chicoine B, Bulova P, et al. Down Syndrome Medical Interest Group DSMIG-USA Adult Health Care Workgroup: Co-occurring medical conditions in adults with Down syndrome: a systematic review toward the development of health care guidelines. Am J Med Genet A. 2018;176:116–133. doi: 10.1002/ajmg.a.38512. [DOI] [PubMed] [Google Scholar]
- E27.Yates JR, Maclean C, Higgins JN, et al. The Tuberous Sclerosis 2000 Study: presentation, initial assessments and implications for diagnosis and management. Arch Dis Child. 2011;961:020–025. doi: 10.1136/adc.2011.211995. [DOI] [PubMed] [Google Scholar]
- E28.Erickson CA, Kaufmann WE, Budimirovic DB, et al. Best practices in fragile X syndrome treatment development. Brain Sci. 2018;15 doi: 10.3390/brainsci8120224. pii: E224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E29.Spiesshoefer J, Runte M, Heidbreder A, et al. Sleep-disordered breathing and effects of non-invasive ventilation on objective sleep and nocturnal respiration in patients with myotonic dystrophy type I. Neuromuscul Disord. 2019;29:302–309. doi: 10.1016/j.nmd.2019.02.006. [DOI] [PubMed] [Google Scholar]
- E30.Martin P. Pain in Rett syndrome: peculiarities in pain processing and expression, liability to pain causing disorders and diseases, and specific aspects of pain assessment. Adv Autism. 2017;3:163–182. [Google Scholar]
- E31.Walter-Fränkel S. Schmerzdiagnostik Psychische Gesundheit bei intellektueller Entwicklungsstörung. Ein Lehrbuch für die Praxis. In: Sappok T, editor. Kohlhammer Verlag. Stuttgart: 2018. pp. 265–274. [Google Scholar]
- E32.Schwartz L, Engel JM, Jensen MP. Pain in persons with cerebral palsy. Arch Phys Med Rehabil. 1999;80:1243–1246. doi: 10.1016/s0003-9993(99)90023-0. [DOI] [PubMed] [Google Scholar]
- E33.Andresen V, Enck P, Frieling T, et al. S2 Leitlinie chronische Obstipation. www.awmf.org/uploads/tx_szleitlinien/021-019l_S2k_Chronische_Obstipation_2013-06-abgelaufen.pdf (last accessed on 12 August 2019) [Google Scholar]
- E34.Franke ML, Heinrich M, Adam M, Sünkel U, Diefenbacher A, Sappok T. Körpergewicht und psychische Erkrankungen - Ergebnisse einer klinisch-psychiatrischen Querschnittsanalyse bei Menschen mit Intelligenzminderung. Nervenarzt. 2017;89:552–558. doi: 10.1007/s00115-017-0411-2. [DOI] [PubMed] [Google Scholar]
- E35.Brown AL, de Smith AJ, Gant VU, et al. Inherited genetic susceptibility of acute lymphoblastic leukemia in Down syndrome. Blood. 2019;26 doi: 10.1182/blood.2018890764. pii: blood.2018890764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E36.Holland AJ, Hon J, Huppert FA, Stevens F, Watson P. Population-based study of the prevalence and presentation of dementia in adults with Down‘s syndrome. Br J Psychiatry. 1998;172:493–498. doi: 10.1192/bjp.172.6.493. [DOI] [PubMed] [Google Scholar]
- E37.Dekker AD, Sacco S, Carfi A, et al. The behavioral and psychological symptoms of dementia in Down Syndrome (BPSD-DS) Scale: comprehensive assessment of psychopathology in down syndrome. J Alzheimers Dis. 2018;63:797–819. doi: 10.3233/JAD-170920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E38.Devshi R, Shaw S, Elliott-King J, et al. Prevalence of behavioural and psychological symptoms of dementia in individuals with learning Disabilities. Diagnostics (Basel) 2015;5:564–576. doi: 10.3390/diagnostics5040564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E39.Axmon A, Björne P, Nylander L, Ahlström G. Psychiatric diagnoses in relation to severity of intellectual disability and challenging behaviors: a register study among older people. Aging Ment Health. 2018;22:1344–1350. doi: 10.1080/13607863.2017.1348483. [DOI] [PubMed] [Google Scholar]
- E40.Fonseca LM, Navatta AC, Bottino CM, Miotto EC. Cognitive rehabilitation of dementia in adults with Down Syndrome: a review of non-pharmacological interventions. Dement Geriatr Cogn Dis Extra. 2015;5:330–340. doi: 10.1159/000438858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E41.Tang SX, Moore TM, Calkins ME, et al. Emergent, remitted and persistent psychosis-spectrum symptoms in 22q112. deletion syndrome. Transl Psychiatry. 2017;25 doi: 10.1038/tp.2017.157. 7: e1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E42.Jacobi F, Höfler M, Strehle J, et al. Psychische Störungen in der Allgemeinbevölkerung. Nervenarzt. 2014;85:77–87. doi: 10.1007/s00115-013-3961-y. [DOI] [PubMed] [Google Scholar]
- E43.Fletcher R, Barnhill J, Cooper SA. Diagnostic manual-intellectual disability: a textbook of diagnosis of mental disorders in persons with intellectual disability. Kingston. NADD Press/ National Association for the Dually Diagnosed. (2) 2016 [Google Scholar]
- E44.Hiremath A, Gangavati S, Gumber R, Barrett M. Bhaumik S, Branford D, Barret M, Gangadharan SK, editors. Depression The frith prescribing guidelines for people with intellectual disability. Chichester: John Wiley & Sons. (3) 2015:169–178. [Google Scholar]
- E45.Hamers PCM, Festen DAM, Hermans H. Non-pharmacological interventions for adults with intellectual disabilities and depression: a systematic review. J Intellect Disabil Res. 2018;62:684–700. doi: 10.1111/jir.12502. [DOI] [PubMed] [Google Scholar]
- E46.Sappok T, Voß T, Millauer E, Schade C, Diefenbacher A. Psychotherapie bei Menschen mit IM: Theoretischer Hintergrund und praktische Umsetzung. Der Nervenarzt. 2010;81:827–836. doi: 10.1007/s00115-009-2917-8. [DOI] [PubMed] [Google Scholar]
- E47.Hughes K, Bellis MA, Jones L, et al. Prevalence and risk of violence against adults with disabilities: a systematic review and meta-analysis of observational studies. The Lancet. 2012;379:1621–1629. doi: 10.1016/S0140-6736(11)61851-5. [DOI] [PubMed] [Google Scholar]
- E48.Jones L, Bellis MA, Wood S, et al. Prevalence and risk of violence against children with disabilities: A systematic review and meta-analysis of observational studies. Lancet. 2012;380:899–907. doi: 10.1016/S0140-6736(12)60692-8. [DOI] [PubMed] [Google Scholar]
- E49.Daveneyn J, Hassiotis A, Katona C, Matcham F, Sen P. Ascertainment and prevalence of post-traumatic stress disorder (PTSD) in people with intellectual disabilities. J Ment Health Res Intellect Disabil. 2019 DOI: 10.1080/19315864.2019.1637979. [Google Scholar]
- E50.Gilderthorp RC. Is EMDR an effective treatment for people diagnosed with both intellectual disability and post-traumatic stress disorder? J Intellect Disabil. 20151;9:58–68. doi: 10.1177/1744629514560638. [DOI] [PubMed] [Google Scholar]
- E51.Baio J, Wiggins L, Christensen DL, et al. Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network,11 Sites, United States, 2014. MMWR Surveill Summ. 2018;67:1–23. doi: 10.15585/mmwr.ss6706a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E52.Brugha TS, Spiers N, Bankart J, et al. Epidemiology of autism in adults across age groups and ability levels. Brit J Psychiat. 2016;209:498–503. doi: 10.1192/bjp.bp.115.174649. [DOI] [PubMed] [Google Scholar]
- E53.Virues-Ortega J, Julio FM, Pastor-Barriuso R. The TEACCH program for children and adults with autism: a meta-analysis of intervention studies. Clin Psychol Rev. 2013;33:940–953. doi: 10.1016/j.cpr.2013.07.005. [DOI] [PubMed] [Google Scholar]
- E54.Jesner OS, Aref-Adib M, Coren E. Risperidone for autism spectrum disorder. Cochrane Database Syst Rev. 2007;24 doi: 10.1002/14651858.CD005040.pub2. CD005040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E55.Hirsch LE, Pringsheim T. Aripiprazole for autism spectrum disorders (ASD) Cochrane Database Syst Rev. 2016;26 doi: 10.1002/14651858.CD009043.pub3. CD009043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E56.Reichow B, Volkmar FM, Bloch MH. Systematic review and meta-analysis of pharmacological treatment of the symptoms of attention-deficit/hyperactivity disorder in children with pervasive developmental disorders. J Autism Dev Disord. 2013;43:2435–2441. doi: 10.1007/s10803-013-1793-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E57.Cuomo BM, Vaz S, Lee EAL, Thompson C, Rogerson JM, Falkmer T. Effectiveness of sleep-based: interventions for children with autism spectrum disorder: a meta-synthesis. Pharmacotherapy. 2017;37:555–578. doi: 10.1002/phar.1920. [DOI] [PubMed] [Google Scholar]
- E58.Williams K, Brignell A, Randall M, Silove N, Hazell P. Selective serotonin reuptake inhibitors (SSRIs) for autism spectrum disorders (ASD) Cochrane Database Syst Rev. 2013;8 doi: 10.1002/14651858.CD004677.pub3. CD004677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E59.Hirota T, Veenstra-Vanderweele J, Hollander E, Kishi T. Antiepileptic medications in autism spectrum disorder: a systematic review and meta-analysis. J Autism Dev Disord. 2014;44:948–957. doi: 10.1007/s10803-013-1952-2. [DOI] [PubMed] [Google Scholar]
- E60.Sappok T. Kohlhammer Verlag. Stuttgart: 2018. Psychische Gesundheit bei intellektueller Entwicklungsstörung Ein Lehrbuch für die Praxis. [Google Scholar]