Abstract
Background
The standard diagnostic work-up for hand and wrist fractures consists of history taking, physical examination and imaging if needed, but the supporting evidence for this work-up is limited. The purpose of this study was to systematically examine the diagnostic accuracy of tests for hand and wrist fractures.
Methods
A systematic search for relevant studies was performed. Methodological quality was assessed and sensitivity (Se), specificity (Sp), accuracy, positive predictive value (PPV) and negative predictive value (NPV) were extracted from the eligible studies.
Results
Of the 35 eligible studies, two described the diagnostic accuracy of history taking for hand and wrist fractures. Physical examination with or without radiological examination for diagnosing scaphoid fractures (five studies) showed Se, Sp, accuracy, PPV and NPV ranging from 15 to 100%, 13–98%, 55–73%, 14–73% and 75–100%, respectively. Physical examination with radiological examination for diagnosing other carpal bone fractures (one study) showed a Se of 100%, with the exception of the triquetrum (75%). Physical examination for diagnosing phalangeal and metacarpal fractures (one study) showed Se, Sp, accuracy, PPV and NPV ranging from 26 to 55%, 13–89%, 45–76%, 41–77% and 63–75%, respectively.
Imaging modalities of scaphoid fractures showed predominantly low values for PPV and the highest values for Sp and NPV (24 studies). Magnetic Resonance Imaging (MRI), Computed Tomography (CT), Ultrasonography (US) and Bone Scintigraphy (BS) were comparable in diagnostic accuracy for diagnosing a scaphoid fracture, with an accuracy ranging from 85 to 100%, 79–100%, 49–100% and 86–97%, respectively. Imaging for metacarpal and finger fractures showed Se, Sp, accuracy, PPV and NPV ranging from 73 to 100%, 78–100%, 70–100%, 79–100% and 70–100%, respectively.
Conclusions
Only two studies were found on the diagnostic accuracy of history taking for hand and wrist fractures in the current review. Physical examination was of moderate use for diagnosing a scaphoid fracture and of limited use for diagnosing phalangeal, metacarpal and remaining carpal fractures. MRI, CT and BS were found to be moderately accurate for the definitive diagnosis of clinically suspected carpal fractures.
Keywords: Diagnostic tests, Finger, Fracture, Hand, Wrist
Background
Hand and wrist injuries are among the most common traumatic presentations to the emergency department [1, 2], and commonly affect young people of working age [3, 4]. Scaphoid fractures are the most frequently injured carpal bones, accounting for 61–90% of fractures [4–6]. The diagnosis of a scaphoid fracture may however be difficult to establish on a conventional radiograph [7, 8]. Previous research has shown that 10–35% of scaphoid fractures are missed on primary radiographs [4, 9–12]. Metacarpal fractures are detected in 30–40% of all hand fractures in all emergency department admissions [4, 9, 10].
Hand and wrist injuries represent a considerable economic burden, with high health-care and productivity costs [13]. The total costs have been estimated at US $410 million per year, with US $307 million in productivity costs [14].
If not treated properly, patients with hand and wrist injuries may experience lifelong pain and lose their job, which also has major effects on their quality of life [15]. Accurate diagnosis and early treatment of hand and wrist fractures are important because missed diagnosis and delayed initiation of therapy increase the risk of complications and subsequent functional impairment [16–22].
In recent decades, research has predominantly focused on imaging modalities for the diagnosis of wrist fractures. However, the standard diagnostic work-up for wrist complaints that are suspected fractures should also include detailed patient history taking, a conscientious physical examination and, only if needed, imaging [23]. It has been shown that different provocative tests are somewhat useful for diagnosing wrist fractures [24–27], but there is no consensus on imaging protocols due to limited evidence regarding the diagnostic performance of these advanced imaging techniques [28]. Therefore, diagnosing wrist pathologies remain complex and challenging and there is increasing demand for evidence for accurate diagnostic tools [29].
Diagnostic studies performed in hospital care cannot automatically be translated into guidelines for non-institutionalized general practitioner care [30]. The clinical utility of diagnostic tests for hand and wrist fractures is hindered by the low prevalence of true fractures, approximately 7% on average [31].
Currently, there are several systematic reviews available on the diagnostic accuracy of tests for the diagnosis of hand and wrist fractures, as presented in Table 1 [32–39]. Of these, only the review by Carpenter et al. used ‘history’ as a keyword in their search terms, but they could not find studies assessing the diagnostic accuracy of history for scaphoid fractures [32]. All the available systematic reviews only examined diagnostic tests for scaphoid fractures [32–39], while in practice it is often not quite clear during the diagnostic process which hand or wrist anatomical structure or tissue (soft tissue or bone) is affected. Moreover, these reviews focused predominantly on imaging as a diagnostic tool, while in clinical practice a diagnosis is mainly made on history taking and physical examination.
Table 1.
Characteristics of the Currently Available Systematic Reviews on the Diagnostic Accuracy of Tests
| Author(s) | Population in eligible studies as described by the review authors | Fracture | Number of studies included | Diagnostic test | Pooled Se (95% CI) |
Pooled Sp (95% CI) |
Positive LR | Conclusion |
|---|---|---|---|---|---|---|---|---|
| HISTORY TAKING | ||||||||
| Carpenter (2014) [32] | Emergency Department. | Scaphoid | 0 | History examination alone is inadequate to rule in or rule out scaphoid fracture. | ||||
| PHYSICAL EXAMINATION | ||||||||
| Carpenter (2014) [32] | Emergency Department. | Scaphoid | 6 | ASB tenderness | 0.96 (0.92–0.98) | 0.39 (0.36–0.43) | Except for the absence of snuffbox tenderness, which can significantly reduce the probability of scaphoid fracture, physical examination alone is inadequate to rule in or rule out scaphoid fracture. | |
| 6 | LTC | 0.82 (0.77–0.87) | 0.58 (0.54–0.62) | |||||
| 7 | Ultrasound fibration pain | 0.67 (0.59–0.75) | 0.57 (0.51–0.62) | |||||
| 3 | Clamp sign | 0.73 (0.67–0.78) | 0.92 (0.89–0.95) | |||||
| 3 | Painfull ulnar deviation | 0.77 (0.68–0.83) | 0.42 (0.34–0.49) | |||||
| 3 | STT | 0.92 (0.86–0.96) | 0.47 (0.43–0.52) | |||||
| 2 | Resisted supination pain | 0.94 (0.85–0.98) | 0.74 (0.63–0.84) | |||||
| Burrows (2014) [33] | Not specified | Scaphoid | 5 | ASB tenderness | 1.52 (1.12–2.06) | Three clinical tests with statistically significant diagnostic validity were identified. In isolation, the clinical significance of each is questionable. | ||
| 7 | Scaphoid compression test | 2.37 (1.27–4.41) | ||||||
| 3 | STT | 1.67 (1.33–2.09) | ||||||
| Mallee (2015) [34] | Patients presenting to the emergency department or outpatient clinic | Scaphoid | 8 | ASB tenderness | 0.87–1.00 a | 0.03–0.98 b | Anatomical snuff box tenderness was the most sensitive clinical test. The low specificity of the clinical tests may result in a considerable number of over-treated patients. Combining tests improved the post-test fracture probability. | |
| 8 | LTC | 0.48–1.00 a | 0.22–0.97 b | |||||
| 4 | STT | 0.82–1.00 a | 0.17–0.57 b | |||||
| 4 | Painfull ulnar deviation | 0.67–1.00 a | 0.17–0.60 b | |||||
| 4 | ASB swelling | 0.67–0.77 a | 0.37–0.72 b | |||||
| IMAGING | ||||||||
| Carpenter (2014) [32] | Emergency Department. | Scaphoid | 5 | X-ray fat pad | 0.82 (0.76–0.86) | 0.72 (0.68–0.75) | MRI is the most accurate imaging test to diagnose scaphoid fractures in ED patients with no evidence of fracture on initial x-rays. If MRI is unavailable, CT is adequate to rule in scaphoid fractures, but inadequate for ruling out scaphoid fractures. | |
| 18 | BS | 0.91 (0.87–0.94) | 0.86 (0.83–0.88) | |||||
| 6 | US | 0.80 (0.67–0.90) | 0.87 (0.81–0.91) | |||||
| 8 | CT | 0.83 (0.83–0.89) | 0.97 (0.94–0.98) | |||||
| 13 | MRI | 0.96 (0.92–0.99) | 0.98 (0.96–0.99) | |||||
| Yin (2012) [35] | Not specified | Scaphoid | 28 | Follow-up radiographs | 0.91 (0.81–0.98) | 1.00 (0.99–1.00) | If we acknowledge the lack of a reference standard for diagnosing suspected scaphoid fractures, MRI is the most accurate test; follow-up radiographs and CT may be less sensitive, and bone scintigraphy less specific. | |
| 18 | BS | 0.98 (0.96–0.99) | 0.94 (0.91–0.95) | |||||
| 15 | MRI | 0.98 (0.95–0.99) | 1.00 (0.99–1.00) | |||||
| 9 | CT | 0.85 (0.74–0.94) | 1.00 (0.98–1.00) | |||||
| Yin (2010) [36] | Not specified | Scaphoid | 15 | BS | 0.97 (0.93–0.99) | 0.89 (0.83–0.94) | Bone scintigraphy and MRI have equally high sensitivity and high diagnostic value for excluding scaphoid fracture; however, MRI is more specific and better for confirming scaphoid fracture. | |
| 10 | MRI | 0.96 (0.91–0.99) | 0.99 (0.96–1.00) | |||||
| 6 | CT | 0.93 (0.83–0.98) | 0.99 (0.96–1.00) | |||||
| Mallee (2014) [34] | People of all ages who presented at hospital or clinic | Scaphoid | 6 | BS | 0.99 (0.69–1.00) | 0.86 (0.73–0.94) | Bone scintigraphy is statistically the best diagnostic modality to establish a definitive diagnosis in clinically suspected fractures when radiographs appear normal. The number of overtreated patients is substantially lower with CT and MRI. | |
| 4 | CT | 0.72 (0.36–0.92) | 0.99 (0.71–1.00) | |||||
| 5 | MRI | 0.88 (0.64–0.97) | 1.00 (0.38–1.00) | |||||
| Kwee (2018) [37] | Not specified | Scaphoid | 7 | US | 0.86 (0.74–0.93) | 0.84 (0.72–0.91) | Ultrasound can diagnose radiographically occult scaphoid fracture with a fairly high degree of accuracy. | |
| Ali (2018) [38] | Not specified | Scaphoid | 6 | US | 0.94 (0.78–1.00) | 0.89 (0.78–1.00) | US reveals high sensitivity and specificity in scaphoid fracture diagnosis. | |
ASB Anatomic snuff-box, LTC Longitudinal (thumb) compression test, STT Scaphoid tubercle tenderness, BS Bone Scintigraphy, US Ultrasound, CT Computed TomographyMRI: Magnetic Resonance Imaging
aSensitivity range described, because of the high heterogeneity Mallee et al. [34] refrained from calculating pooled estimate points
bSpecificity Range described, because of the high heterogeneity Mallee et al. [34] refrained from calculating pooled estimate points
Therefore, the purpose of this literature review is to provide an up-to-date systematic overview of the diagnostic accuracy of history taking, physical examination and imaging for phalangeal, metacarpal and carpal fractures and to distinguishing between studies in hospital and non-institutionalized general practitioner care settings, as test properties may differ between settings. Compared to previously published reviews, in this systematic review we also included studies that examined history taking and physical examination for phalangeal, metacarpal or carpal fractures.
Methods
Data sources and searches
A review protocol was drafted, but central registration was not completed. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement was used to guide the conduct and reporting of the study [40]. A Biomedical Information specialist (Wichor M. Bramer) performed a search for studies in Medline, Embase, Cochrane Library, Web of Science, Google Scholar ProQuest and Cinahl from 2000 up to 6 February 2019. This starting point was used since multiple reviews are available that already cover the period up to the year 2000 (Table 1). Search terms included phalangeal, metacarpal and carpal injuries, anamnestic assessment, provocative test(s), diagnostic test(s) and imaging tests. The full electronic search strategy for the Embase database is presented in Table 2 (the others are available upon request).
Table 2.
Example electronic search strategy
| Database | Search terms |
|---|---|
| Embase | (‘hand injury’/exp. OR ‘wrist injury’/exp. OR ‘wrist fracture’/exp. OR ((‘hand bone’/exp. OR wrist/exp. OR hand/exp. OR ‘wrist pain’/exp. OR ‘hand pain’/exp) AND (‘bone injury’/exp. OR fracture/de OR ‘ligament injury’/exp. OR ‘ligament rupture’/exp)) OR (((hand OR hands OR wrist* OR finger* OR carpal* OR carpus OR phalanx* OR metacarp* OR capitate* OR hamat* OR lunat* OR pisiform* OR scaphoid* OR trapezium* OR trapezoid* OR triquetr* OR navicular* OR lunar OR semilunar* OR multangulum* OR pyramid* OR metacarpophalang* OR thumb* OR ‘distal radius’ OR ‘distal ulna’ OR ‘distal radial’ OR ‘distal ulnar’ OR scapholunate* OR lunotriquetral* OR ‘triangular fibrocartilaginous’ OR SLIL OR LTIL OR tfcc OR ‘ulnar collateral ligament’ OR ‘ulnar collateral ligaments’ OR ucl) NEAR/3 (injur* OR trauma* OR wound* OR lesion* OR dislocate* OR fracture* OR damage* OR tear* OR sprain* OR displace* OR rupture*))):ab,ti) AND (‘diagnostic test’/de OR ‘function test’/exp. OR ‘diagnostic error’/exp. OR ‘diagnostic accuracy’/exp. OR ‘diagnostic value’/exp. OR ‘differential diagnosis’/exp. OR ‘delayed diagnosis’/exp. OR ‘sensitivity and specificity’/exp. OR (((diagnos* OR detect* OR differen* OR strength* OR motion*) NEAR/3 (test* OR accura* OR error* OR false OR fail* OR value* OR impact* OR effective* OR earl* OR missed OR correct* OR incorrect* OR delay* OR difficult* OR negative* OR positive* OR sensitivit* OR specificit* OR confirm* OR abilit*)) OR (diagnos* NEAR/3 differen*) OR misdiagnos* OR underdiagnos* OR undetect* OR (predict* NEAR/3 value*) OR (function* NEAR/3 test*) OR (false NEAR/3 (negative* OR positive*))):ab,ti) NOT ([Conference Abstract]/lim OR [Letter]/lim OR [Note]/lim OR [Editorial]/lim) AND [english]/lim NOT ([animals]/lim NOT [humans]/lim) |
Search terms for the other databases are available upon request
Study selection
Studies describing diagnostic accuracy of history taking, physical examination or imaging in adult patients (age ≥ 16 years) with phalangeal, metacarpal and/or carpal fractures were included. No language restriction was applied. Case reports, reviews and conference proceedings were excluded. Distal radius and ulna injuries were also excluded, as they can be diagnosed accurately with plane X-ray or computer tomography imaging.
Two reviewers (PK, YA) read all titles and abstracts independently. Articles that could not be excluded on the basis of the title and/or abstract were retrieved in full text and were read and checked for inclusion by the two reviewers independently. If there was no agreement, a third reviewer (JR) made the final decision. In addition, the reference lists of all included studies were reviewed to check for additional relevant studies.
Data extraction and methodological quality assessment
Two reviewers (PK, JR) independently extracted the data. Data were extracted describing the study design, characteristics of the study population, test characteristics, study population setting (hospital care or non-institutionalized general practitioner care) and diagnostic parameters. Methodological quality was assessed by two independent reviewers (PK, JR), using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) checklist [41]. Disagreements were resolved by discussion.
Heterogeneity
Key factors in a meta-analysis are the number and the methodological quality of the included studies and the degree of heterogeneity in their estimates of diagnostic accuracy [42]. Heterogeneity in diagnostic test accuracy reviews is expected and the possibilities of performing meta-regression analyses will depend on the number of studies available for a specific index test that provide sufficient information [39]. The data from the included studies were combined when studies showed no limitations according to QUADAS-2 and had no other forms of bias (e.g. incorporation bias).
Data synthesis and analysis
The following values were extracted, if documented: sensitivity (Se), specificity (Sp), accuracy, positive predictive value (PPV), negative predictive value (NPV) and likelihood ratio (LR). If these diagnostic outcomes were not reported, they were calculated using published data. If an included study presented results from multiple independent observers, the measures of Se, Sp, accuracy, PPV and NPV were averaged over the observers.
Index test
Diagnostic tools such as history taking, physical examination or imaging were accepted as index tests.
Reference standard
There is no consensus about the reference test for the diagnosis of a true fracture of the phalangeal, metacarpal or carpal bones [35]. Therefore, in this systematic review clinical outcome (physical examination or additional treatment) and/or various (combined) imaging modalities during follow-up were used as the reference standard for confirming diagnosis of phalangeal, metacarpal or carpal fractures.
Results
The flow diagram is presented in Fig. 1. A total of 35 diagnostic studies were identified, assessed and interpreted. The characteristics of these studies are presented in Table 3. 20 studies were performed in an emergency department, four studies in a traumatology setting and three other studies in a radiology department. The patients in the studies by Mallee et al. [56–58] were derived from one prospective study; therefore the setting was the same for each study: patients were initially seen by the emergency physicians and in follow-up by the orthopaedic department and/or trauma surgery department, depending on who was on call. In five studies the setting was not specified. To our knowledge, all first authors of those five studies were working in a hospital care setting, so we assume all to have been done in hospital care. History taking, physical examination and imaging as index tests were investigated in 0, 20% (7/35) [48, 53, 62, 64, 67, 73, 77] and 86% (30/35) [43–47, 49–51, 53–61, 63, 65, 66, 68–77] of the studies, respectively.
Fig. 1.
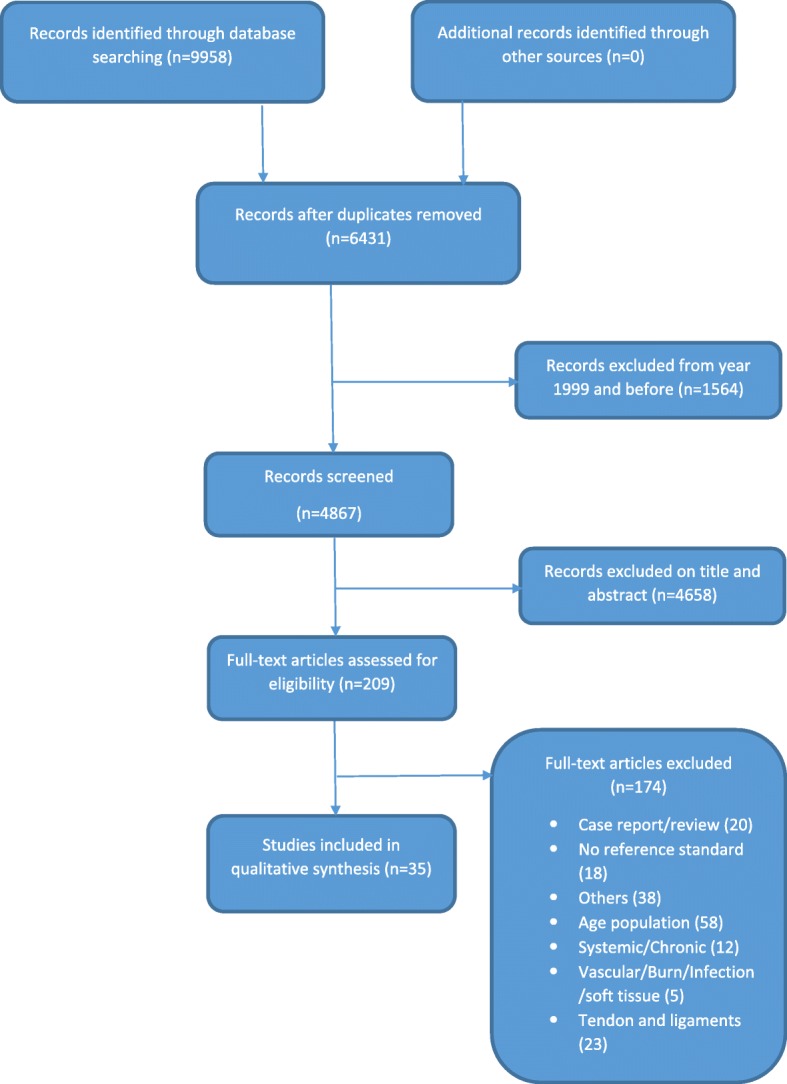
Flow chart study selection
Table 3.
Characteristics of the Eligible Studies (N = 35)
| Author(s) | Participants | Design | Department of patient presentation (Country) | Fracture | Index test | Reference test |
|---|---|---|---|---|---|---|
| SCAPHOID AND OTHER CARPAL BONES FRACTURES | ||||||
| Adey (2007) [43] | 30 | Retrospective | Not described (USA) | Scaphoid | CT | Radiographs 6 weeks after injury |
| Annamalai (2003) [44] | 50 | Retrospective | Not described (Scotland) | Scaphoid | Radiology (scaphoid and pronator fat stripe) | MRI 0,2 T (12-72 h) |
| Behzadi (2015) [45] | 124 | Retrospective | Emergency department (Germany) | Scaphoid | Radiographs (anterior-posterior, lateral and oblique projections) | MDCT (within 10 days) |
| Beeres (2007) [46] | 50 | Prospective | Emergency department (Netherlands) | Scaphoid and other carpal bones | Bone scintigraphy (3–7 days after injury) |
Clinical outcome: physical examination at fixed intervals No fracture, with a normal physical examination at 2 or 6 weeks, BS was considered correct. However, if there were clinical signs of a fracture after 2 and 6 weeks, BS was considered false negative. Another fracture in the carpal region and physical examination after 2 weeks (during change of cast) matched with such a fracture, BS was considered correct. But, when physical examination after 2 weeks showed no signs of fracture, BS was considered false positive. A scaphoid fracture, confirmed on physical examination after 2 weeks (during change of cast), BS was considered correct. If however, neither physical examination after 2 weeks, nor consecutive physical examinations showed evidence of a scaphoid fracture, there was no scaphoid fracture. BS was then considered false positive. |
| Beeres (2008) [47] | 100 | Prospective | Emergency department (Netherlands) | Scaphoid | MRI 1.5 T (< 24 h) and Bone scintigraphy (between 3 and 5 days) | Absence or presence of a fracture on both MRI and bone scintigraphy, or in the case of discrepancy, clinical and/or radiological evidence of a fracture. |
| Bergh (2014) [48] | 154 | Prospective | Emergency department, outpatient clinic (Norway) | Scaphoid | Clinical Scaphoid Score (CSS): tenderness in the anatomical snuffbox with the wrist in ulnar deviation (3 points) + tenderness over the scaphoid tubercle (2 points) + pain upon longitudinal compression of the thumb (1 point) | MRI 1.5 T |
| Breederveld (2004) [49] | 29 | Prospective | Emergency department (Netherlands) | Scaphoid | BS (three-fase) and CT | Clinical follow-up (including CT and Bone scintigraphy) |
| Cruickshank (2007) [50] | 47 | Prospective | Teaching emergency department (Australia) | Scaphoid and other carpal bones | CT (same or next day) | The diagnosis on Day 10 with clinical examination and X-rays, with MRI performed in patients with persistent tenderness but normal X-rays. |
| Fusetti (2005) [51] | 24 | Prospective | Not described (Switzerland) | Scaphoid | HSR-S (< 24 h of the clinical examination) | CT (immediately after HSR-S performed) |
| Gabler (2001) [52] | 121 | Prospective | Department of traumatology: fracture clinics (Austria) | Scaphoid | Repeated clinical examination (tenderness over the anatomical snuff box or the carpus as well as a positive scaphoid compression test) and radiological examinations (scaphoid views) | MRI 1.0 T |
| Herneth (2001) [53] | 15 | Prospective | Not described (Austria) | Scaphoid | Clinical examination, radiography and High-spatial resolution ultrasonography | MRI 1,0 T (< 72 h) |
| Ilica (2011) [54] | 54 | Prospective | Emergency department (Turkey) | Scaphoid | MDCT | MRI 1.5 T |
| Kumar (2005) [55] | 22 | Prospective | Collaboration between the Department of Emergency Medicine and Medical Imaging (New Zealand) | Scaphoid | MRI 1.5 T (< 24 h) | MRI in those without fracture at MRI < 24 h or no clinical signs of fracture |
| Mallee (2011) [56] | 34 | Prospective | Initially emergency physicians and in follow-up by the Orthopedic department and/or Trauma surgery department, depending on who was on call. (Netherlands) | Scaphoid | CT and MRI 1.0 T (within 10 days) | Radiographs, after 6 weeks follow-up |
| Mallee (2016) [57] | 34 | Prospective | Initially emergency physicians and in follow-up by the Orthopedic department and/or Trauma surgery department, depending on who was on call. (Netherlands) | Scaphoid | 6-weeks radiographs in JPEG- and DICOM- view | CT, MRI, or CT and MRI |
| Mallee (2014) [58] | 34 | Prospective | Initially emergency physicians and in follow-up by the Orthopedic department and/or Trauma surgery department, depending on who was on call. (Netherlands) | Scaphoid |
CT-scaphoid: reformations in planes defined by the long axis of the scaphoid. CT-wrist: reformations made in the anatomic planes of the wrist. CT performed within 10 days. |
Radiographs in four standard scaphoid views after 6 weeks follow-up. |
| Memarsadeghi (2006) [59] | 29 | Prospective | Not described (Austria) | Scaphoid | MDCT and MRI 1,0 T | Radiographs obtained 6 weeks after trauma. View: posteroanterior with the wrist in neutral position, lateral, semipronated oblique scaphoid, and radial oblique scaphoid. |
| Ottenin (2012) [60] | 100 | Retrospective | Radiology department of the emergency unit (France) | Scaphoid and other carpal bones | Tomosynthesis (frontal and lateral), MDCT (within 7 days) and radiographs (posteroanterior view, lateral view, anteroposterior oblique view, scaphoid view with ulnar deviation, and posteroanterior view with clenched fist) | The reference standard for each case was determined after completion of all examinations; analysis of MRI (n = 13; performed in cases of doubt after completion of diagnostic standard radiography, tomosynthesis, and CT); and follow-up information obtained by physical examination or, in case of no clinical follow-up, by telephone recalls. |
| Platon (2011) [61] | 62 | Prospective | Emergency department (Switzerland) | Scaphoid | US within 3 days (presence of a cortical interruption of the scaphoid along with a radio-carpal or scaphotrapezium-trapezoid effusion) | CT (immediately after US) |
| Rhemrev (2010) [62] | 100 | Prospective | Emergency department (Netherlands) | Scaphoid | MDCT (< 24 h) and Bone scintigraphy (3–5 days) |
Final diagnosis after final discharge, according to the following standard: If CT and bone scintigraphy showed a fracture, the final diagnosis was fracture. If CT and bone scintigraphy showed no fracture, the final diagnosis was no fracture. In case of discrepancy between CT and bone scintigraphy, both radiographic (6 weeks after injury) and physical reevaluation during follow-up were used to make a final diagnosis. In case of radiographic evidence of a scaphoid fracture 6 weeks after injury, the final diagnosis was fracture. In case of no radiographic evidence of a scaphoid fracture 6 weeks after injury but there were persistent clinical signs of a scaphoid fracture after 2 weeks, the final diagnosis was fracture. If there was no radiographic evidence of a scaphoid fracture 6 weeks after injury and there were no longer clinical signs of a scaphoid fractures throughout follow-up, the final diagnosis was no fracture. |
| Rhemrev (2010) [63] | 78 | Prospective | Emergency department (Netherlands) | Scaphoid |
Three clinical exams: 1) inspection of the snuffbox for the presence of ecchymosis or edema, 2) flexion and extension of the wrist, 3) Supination and pronation strength, 4) Grip strength. |
MRI 1,5 T, bone scintigraphy, radiography and physical re-evaluation during 6 weeks clinical follow-up. |
| Steenvoorde (2006) [64] | 31 | Not described | Emergency department (Netherlands): request for radiograph of the scaphoid by general practitioners were excluded | Scaphoid and other carpal bones | Five or more positive clinical tests out of seven tests: 1) loss of concavity of the anatomic snuff box, 2) snuffbox tenderness, 3) the clamp sign, 4) palmar tenderness of the scaphoid, 5) axial compression of the thumb along its longitudinal axis, 6) site of pain on resisted supination, 7) site of pain on ulnar deviation. | Clinical follow-up |
| Yildirim (2013) [65] | 63 | Prospective | Emergency department (Turkey) | Scaphoid | BUS (presence of a cortical interruption of the scaphoid along with a radiocarpal or scaphotrapezium trapezoid effusion) | MRI (< 24 h) |
| de Zwart (2016) [66] | 33 | Prospective | Emergency department (Netherlands) | Scaphoid | MRI (< 72 h), CT(< 72 h) and Bone Scintigraphy (between 3 and 5 days) |
If MRI, CT and BS all showed a fracture, the final diagnosis was: fracture. If MRI, CT and BS all showed no fracture, the final diagnosis was: no fracture. In case of discrepancy between MRI, CT and BS, the final diagnosis was established based on specific clinical signs of a fracture after 6 weeks (tender anatomic snuffbox and pain in the snuffbox when applying axial pressure on the first or second digit) combined with the radiographic evidence of a fracture after 6 weeks. If these signs were absent and no radiographic evidence, the final diagnosis was: no fracture. |
| Sharifi (2015) [67] | 175 | Prospective | Emergency department (Iran) | Scaphoid fractures | VAS pain score (anatomical snuff box tenderness) | MRI |
| Brink (2014) [68] | 98 | Prospective | Department of Radiology (Netherlands) | Fractures carpus and metacarpal | CT or radiography | Clinical follow-up |
| Neubauer (2018) [69] | 102 | Retrospective | Orthopedics and Trauma/Hand Surgery (Germany) | Scaphoid fractures | CBCT or radiography | Clinical follow-up (including images) |
| Borel (2017) [70] | 49 | Prospective | Orthopedics and Trauma Surgery (France) | Scaphoid or wrist fractures | CBCT | MRI |
| SCAPHOID, OTHER CARPAL AND METACARPAL BONES FRACTURES | ||||||
| Balci (2015) [71] | 455 | Retrospective | Emergency department (Turkey) | Carpal and metacarpal | Radiographs | MDCT |
| Jorgsholm (2013) [72] | 296 | Prospective | Emergency department (Sweden) | Scaphoid, other carpal and metacarpal bones | Radiographs (dorsovolar and lateral projections with an additional 4 views of the scaphoid.) and CT | MRI 0.23 T (within 3 days) |
| Nikken (2005) [73] | 87 | Prospective | Radiology department referred by traumatologist, orthopedic surgeon or emergency physician (Netherlands) | Scaphoid and other carpal bones. Metacarpal bones II–IV | Anatomic snuffbox tenderness, radiographs (posteroanterior and lateral projection) and MRI 0,2 T (short procedure) | Additional treatment |
| CARPAL AND METACARPAL BONES AND PHALANGEAL FRACTURES | ||||||
| Javadzadeh (2014) [74] | 260 | Not described | Emergency department (Iran) | Carpal, metacarpal, and phalangeal | BUS and WBT ultrasonography | Radiographs (not described when performed) |
| METACARPAL BONES AND/OR PHALANGEAL FRACTURES | ||||||
| Faccioli (2010) [75] | 57 | Prospective | Traumatology department (Italy) | Phalangeal | CBCT | MSCT |
| Kocaoglu (2016) [76] | 96 | Prospective | Emergency department (Turkey) | Metacarpal | US | Radiographs (anteroposterior and oblique) |
| Tayal (2007) [77] | 78 | Prospective | Emergency department (USA) | Metacarpal and phalangeal | US and physical examination | Radiographs and when operated, surgical findings |
MRI Magnetic resonance imaging, CT Computed Tomography, CBCT Cone Beam Computed Tomography, MSCT Multi-slice Computed Tomography, HSR-S High Spatial Resolution sonography, BUS Bedside ultrasonography, WBT Water bath technique ROM Range of motion
Quality assessment
There was considerable underreporting of important quality domains in 23 of the 35 studies (see Table 4). In 13 of the 35 studies [43, 44, 48, 50, 54, 55, 59, 64, 67, 72, 74, 76, 77], patient selection was not well documented. Furthermore, the risk of bias was predominantly due to the absence of a proper description of the index test (9/35) [43, 45, 49, 53, 55, 64, 65, 72, 77] or the reference standard (13/35) [45, 49, 55, 62, 64–68, 71–73, 75]. Twelve of the studies (34%) demonstrated no limitations when risk of bias was assessed, according to QUADAS-2 [46, 47, 51, 52, 56–58, 60, 61, 63, 69, 70]. Eight showed incorporation bias [46, 47, 49, 55, 60, 62, 66, 69].
Table 4.
Summary of Methodological Quality according to Quality Assessment of Diagnostic Accuracy Studies-2
| Author(s) | Risk of Bias | Applicability Concerns | |||||
|---|---|---|---|---|---|---|---|
| Patient Selection | Index Test | Reference standard | Flow and Timing | Patient Selection | Index Test | Reference standard | |
| Adey (2007) [43] | HR | UR | LR | LR | LR | LR | LR |
| Annamalai (2003) [44] | HR | LR | LR | LR | LR | LR | LR |
| Balci (2015) [71] | LR | LR | HR | LR | LR | LR | LR |
| Beeres (2007) [46] | LR | LR | LR | LR | LR | LR | LR |
| Beeres (2008) [47] | LR | LR | LR | LR | LR | LR | LR |
| Behzadi (2015) [45] | LR | HR | HR | LR | LR | LR | LR |
| Bergh (2014) [48] | UR | LR | LR | LR | LR | LR | LR |
| Borel (2017) [70] | LR | LR | LR | LR | LR | LR | LR |
| Breederveld (2004) [49] | LR | UR | UR | LR | LR | LR | LR |
| Brink (2019) [68] | LR | LR | HR | LR | LR | LR | LR |
| Cruickshank (2007) [50] | UR | LR | LR | LR | LR | LR | LR |
| Faccioli (2010) [75] | LR | HR | HR | LR | LR | LR | LR |
| Fusetti (2005) [51] | LR | LR | LR | LR | LR | LR | LR |
| Gabler (2001) [52] | LR | LR | LR | LR | LR | LR | LR |
| Herneth (2001) [53] | LR | UR | LR | LR | LR | LR | LR |
| Ilica (2011) [54] | UR | LR | LR | LR | LR | LR | LR |
| Javadzadeh (2014) [74] | UR | LR | LR | LR | LR | LR | LR |
| Jorgsholm (2013) [72] | UR | HR | HR | LR | LR | LR | LR |
| Kocaoglu (2016) [76] | UR | LR | LR | LR | LR | LR | LR |
| Kumar (2005) [55] | UR | HR | HR | HR | LR | LR | LR |
| Mallee (2011) [56] | LR | LR | LR | LR | LR | LR | LR |
| Mallee (2016) [57] | LR | LR | LR | LR | LR | LR | LR |
| Mallee (2014) [58] | LR | LR | LR | LR | LR | LR | LR |
| Memarsadeghi (2006) [59] | UR | LR | LR | LR | LR | LR | LR |
| Neubauer (2018) [69] | LR | LR | LR | LR | LR | LR | LR |
| Nikken (2005) [73] | LR | LR | HR | LR | LR | LR | LR |
| Ottenin (2012) [60] | LR | LR | LR | LR | LR | LR | LR |
| Platon (2011) [61] | LR | LR | LR | LR | LR | LR | LR |
| Rhemrev (2010) [62] | LR | LR | HR | LR | LR | LR | LR |
| Rhemrev (2010) [63] | LR | LR | LR | LR | LR | LR | LR |
| Sharifi (2015) [67] | UR | LR | UR | LR | LR | LR | LR |
| Steenvoorde (2006) [64] | UR | HR | HR | LR | LR | LR | LR |
| Tayal (2007) [77] | UR | LR | LR | LR | LR | LR | LR |
| Yildirim (2013) [65] | LR | HR | HR | HR | LR | LR | LR |
| de Zwart (2016) [66] | LR | LR | HR | LR | LR | LR | LR |
Abbreviations: LR Low Risk, HR High Risk, UR Unclear Risk
Diagnosing carpal fractures in hospital care
Table 5 presents the accuracy of the diagnostic tests of all the carpal fractures. Two studies described the diagnostic accuracy of history taking [62, 67]. Physical examination [48, 53, 62, 64] and combined physical and radiological examination [52] for diagnosing scaphoid fractures showed Se, Sp, accuracy, PPV and NPV ranging from 15 to 100%, 13–98%, 55–73%, 14–73% and 75–100%, respectively.
Table 5.
Diagnostic Accuracy of the Diagnostic Tests of the Carpal, Metacarpal and Phalangeal Fractures (N=35)
| Author(s) | Index test | Reference test | Fracture | Se % (95% CI) | Sp % (95% CI) | Accuracy % (95% CI) | PPV % (95% CI) | NPV % (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Scaphoid and other carpal bones fractures | ||||||||
| History taking | ||||||||
| Sharifi (2015) [74] | VAS pain score cutt of: 3,0 | MRI | Scaphoid | 100 | 100 | |||
| 4,5 | MRI | Scaphoid | 94 | 92 | ||||
| 5,5 | MRI | Scaphoid | 94 | 82 | ||||
| 6,5 | MRI | Scaphoid | 94 | 72 | ||||
| 7,5 | MRI | Scaphoid | 88 | 43 | ||||
| 8,5 | MRI | Scaphoid | 75 | 28 | ||||
| 9,5 | MRI | Scaphoid | 31 | 13 | ||||
| Physical examination | ||||||||
| Bergh (2014) [44] | Clinical Scaphoid Score ≥4 | MRI 1,5T | Scaphoid | 77 | 56 | 58 | 14 | 96 |
| Gabler (2001) [45] | Repeated clinical and radiological examinations (after 10 days) | MRI 1,0T | Scaphoid | 82 | ||||
| Repeated clinical and radiological examinations (after 38 days) | MRI 1,0T | Scaphoid | 100 | 100 | 100 | 100 | 100 | |
| Repeated clinical and radiological examinations (after 38 days) | MRI 1,0T | Capitate | 100 | |||||
| Repeated clinical and radiological examinations (after 38 days) | MRI 1,0T | Triquetrum | 75 | |||||
| Repeated clinical and radiological examinations (after 38 days) | MRI 1,0T | Hamate | 100 | |||||
| Repeated clinical and radiological examinations (after 38 days) | MRI 1,0T | Lunate | 100 | |||||
| Repeated clinical and radiological examinations (after 38 days) | MRI 1,0T | Trapezoid | 100 | |||||
| Herneth (2001) [47] | Clinical examination | MRI | Scaphoid | 89 | 50 | 73 | 73 | 75 |
| Rhemrev (2010) [63] | Pronation strength ≤10% | Clinical follow-up | Scaphoid | 69 | 65 | |||
| Extension < 50% | Clinical follow-up | Scaphoid | 85 | 59 | ||||
| Supination strength ≤10% | Clinical follow-up | Scaphoid | 85 | 77 | ||||
| Grip strength ≤25% | Clinical follow-up | Scaphoid | 92 | 34 | ||||
| extension <50%, supination strength <10% and presence of a previous fracture of either the involved or uninvolved hand or wrist. | Clinical follow-up | Scaphoid | 15 | 98 | 61 | 85 | ||
| extension <50%, supination strength <10% and presence of a previous fracture of either the involved or uninvolved hand or wrist. | Clinical follow-up | No scaphoid fracture | 46 | 92 | 54 | 89 | ||
| Steenvoorde (2006) [64] | Seven clinical tests (≥ 5 positive tests) | Clinical follow-up | Scaphoid | 100 | 13 | 55 | 52 | 100 |
| Imaging: Radiographs | ||||||||
| Annamalai (2003) [44] | Scaphoid fat stripe on radiography | MRI 0,2T (12-72h) | Scaphoid | 50 | 50 | 50 | 50 | 50 |
| Pronator fat stripe on radiography | Scaphoid | 26 | 70 | 48 | 46 | 49 | ||
| Balci (2015) [71] | Radiographs | MDCT | Scaphoid | 66 | 98 | 77 | 96 | |
| Radiographs | MDCT | Lunate | 20 | 100 | 100 | 97 | ||
| Radiographs | MDCT | Triquetrum | 29 | 100 | 100 | 96 | ||
| Radiographs | MDCT | Pisiform | 0 | 100 | 0 | 99 | ||
| Radiographs | MDCT | Trapezium | 18 | 99 | 33 | 98 | ||
| Radiographs | MDCT | Trapezoid | 0 | 100 | 0 | 99 | ||
| Radiographs | MDCT | Capitate | 8 | 100 | 50 | 98 | ||
| Radiographs | MDCT | Hamata | 41 | 100 | 78 | 98 | ||
| Behzadi (2015) [45] | Radiographs (anterior-posterior, lateral and oblique projections) | MDCT (within 10 days) | Scaphoid | 43 | 81 | 60 | 53 | 73 |
| Herneth (2001) [53] | Radiographs | MRI | Scaphoid | 56 | 100 | 73 | 100 | 60 |
| Jorgsholm (2013) [72] | Radiographs | MRI 0.23T (within 3 days) | Scaphoid | 70 (61-78) | 98 (95-100) | 87 | 97 | 82 |
| Radiographs 6-week: DICOM viewer | MRI 0.23T (within 3 days) | Triquetrum | 59 (33-82) | |||||
| Radiographs 6-week: DICOM viewer | MRI 0.23T (within 3 days) | Lunate | 25 (1-81) | |||||
| Radiographs 6-week: DICOM viewer | MRI 0.23T (within 3 days) | Capitate | 7 (0-34) | |||||
| Radiographs 6-week: DICOM viewer | MRI 0.23T (within 3 days) | Hamata | 0 (0-46) | |||||
| Mallee (2016) [57] | Radiographs 6-week: JPEG | MRI | Scaphoid | 42 (37-47) | 56 (54-59) | 53 (51-56) | 20 (17-23) | 79 (76-81) |
| Radiographs 6-week: JPEG | MRI | Scaphoid | 64 (57-71) | 53 (50-57) | 56 (52-59) | 26 (22-30) | 85 (82-88) | |
| Mallee (2016) [57] | Radiographs 6-week: JPEG | CT | Scaphoid | 56 (50-62) | 59 (56-61) | 58 (56-61) | 19 (16-22) | 89 (87-90) |
| Mallee (2016) [57] | Radiographs 6-week: DICOM viewer | CT | Scaphoid | 79 (72-85) | 55 (51-58) | 58 (55-61) | 23 (19-27) | 94 (91-96) |
| Mallee (2016) [57] | Radiographs 6-week: JPEG | MRI + CT | Scaphoid | 52 (45-59) | 58 (55-60) | 57 (55-59) | 14 (12-17) | 90 (88-92) |
| Mallee (2016) [57] | Radiographs 6-week: DICOM viewer | MRI + CT | Scaphoid | 75 (67-83) | 53 (50-56) | 56 (52-59) | 18 (14-21) | 94 (92-96) |
| Ottenin 2012 [60] | Radiographs | Clinical follow-up | Scaphoid | 67ɸ | 93ɸ | 88ɸ | 68ɸ | 92ɸ |
| Ottenin 2012 [60] | Radiographs | Clinical follow-up | Other carpal bones | 40ɸ | 94ɸ | 88ɸ | 44ɸ | 93ɸ |
| Brink (2019) [68] | X-ray | 1-year clinical follow-up | Scaphoid | 25 | 97 | |||
| X-ray | 1-year clinical follow-up | Triquetral | 18 | 100 | ||||
| X-ray | 1-year clinical follow-up | Lunate | 0 | 100 | ||||
| X-ray | 1-year clinical follow-up | Trapezium | 0 | 100 | ||||
| X-ray | 1-year clinical follow-up | Trapezoid | 0 | 100 | ||||
| X-ray | 1-year clinical follow-up | Hamate | 100 | 100 | ||||
| X-ray | 1-year clinical follow-up | Capitate | 100 | 100 | ||||
| Neubauer (2018) [69] | Radiography | Clinical follow-up | Scaphoid | 87 (83-92) | 77 (71-83) | 82 | 80 (75-86) | 84 (80-90) |
| Imaging: MRI | ||||||||
| Beeres (2008) [47] | MRI 1,5T (<24h) | A combination of MRI, bone scintigraphy and when not in agreement, clinical follow-up | Scaphoid | 80 (56-94) | 100 (96-100) | 96 | 100 (74-100) | 95 (88-99) |
| Kumar (2005) [55] | MRI 1,5T (<24h) | MRI in those without fracture at MRI <24h or no clinical signs of fracture | Scaphoid | 100b | 100b | 100b | 100b | 100b |
| Mallee (2011) [56] | MRI 1.0T | Radiographs | Scaphoid | 67 | 89 | 85 |
57 54c |
93 93d |
| Memarsadeghi (2006) [59] | MRI 1,0T | Radiographs obtained 6 weeks after trauma. | All scaphoid | 100 (82-100) | 100 (87-100) | 100 | 100 | 100 |
| Memarsadeghi (2006) [59] | MRI 1,0T | Radiographs obtained 6 weeks after trauma. | Cortical scaphoid fractures | 38 (16-65) | 100 (52-100) | 55 (24-85) | 100 | 27 |
| Memarsadeghi (2006) [59] | MRI 1,0T | Radiographs obtained 6 weeks after trauma. | Other carpal fractures | 85 | 100 | 84 | ||
| de Zwart (2016) [66] | MRI (<72h) | Final diagnosis after MRI, CT, BS and 6-weeks clinical signs | Scaphoid | 67 | 100 (88-100) | 94 | 67 | 97 |
| Imaging: (Multi detector) computed tomography | ||||||||
| Adey (2007) [43] | CT (first round interpretation) | Radiographs 6 weeks after injury | Scaphoid | 89 (84-92) | 91 (86-94) | 89 (89-92) | 28 (23-32) | 99 (97-99) |
| CT (second round interpretation) | Radiographs 6 weeks after injury | Scaphoid | 97 (93-99) | 85 (77-89) | 88 (82-91) | |||
| Breederveld (2004) [49] | CT | Clinical follow-up | Scaphoid | 100 | 100 | 100 | 100 | 100 |
| Cruickshank (2007) [50] | CT (same or next day) | The diagnosis on Day 10 with clinical examination and X-rays, with MRI performed in patients with persistent tenderness but normal X-rays. | Scaphoid and other fractures (Triquetral, Trapezium, Capitate and Lunate) | 94 (72-100) | 100 (87-100) | 98 | 100 (78-100) | 97 (82-100) |
| Ilica (2011) [54] | MDCT | MRI 1,5T | Scaphoid | 86 | 100 | 95 | 100 | 91 |
| Jorgsholm (2013) [72] | CT | MRI 0.23T (within 3 days) | Scaphoid | 95 (91-97) | ||||
| CT | MRI 0.23T (within 3 days) | Capitate | 75 (35-97) | |||||
| CT | MRI 0.23T (within 3 days) | Hamata | 100 (40-100) | |||||
| Mallee (2011) [56] | CT | Radiographs | Scaphoid | 67 | 96 | 91 |
80 76c |
93 94d |
| Mallee (2014) [58] | CT-scaphoid: reformations in planes defined by the long axis of the scaphoid | Radiographs | Scaphoid | 67 | 96 | 91 |
80 76c |
93 94d |
| CT-wrist: reformations made in the anatomic planes of the wrist | Radiographs | Scaphoid | 33 | 89 | 79 |
40 36c |
86 87d |
|
| Memarsadeghi (2006) [59] | MDCT | Radiographs obtained 6 weeks after trauma. | All scaphoid | 73 (48-89) | 100 (87-100) | 89 (78-100) | 100 | 86 |
| Memarsadeghi (2006) [59] | MDCT | Radiographs obtained 6 weeks after trauma. | Cortical scaphoid fractures | 100 (75-100) | 100 (52-100) | 100 | 100 | 100 |
| Ottenin (2012) [60] | MDCT | Clinical follow-up | Scaphoid | 77ɸ | 94ɸ | 91ɸ | 76ɸ | 95ɸ |
| Ottenin (2012) [60] | MDCT | Clinical follow-up | Other carpal bones | 60ɸ | 95ɸ | 91ɸ | 56ɸ | 96ɸ |
| Rhemrev (2007) [63] | MDCT (<24h) | Final diagnosis after CT, BS and, both radiographic (6 weeks after injury) and physical reevaluation. | Scaphoid | 64 | 99 | 94 | 90 | 94 |
| de Zwart (2016) [66] | CT(<72h) | Final diagnosis after MRI, CT, BS and 6-weeks clinical signs | Scaphoid | 33 | 100 (88-100) | 94 | 100 | 94 |
| Brink (2019) [68] | CT | 1-year clinical follow-up | Scaphoid | 100 | 100 | |||
| CT | 1-year clinical follow-up | Triquetral | 100 | 100 | ||||
| CT | 1-year clinical follow-up | Lunate | 100 | 100 | ||||
| CT | 1-year clinical follow-up | Trapezium | 100 | 100 | ||||
| CT | 1-year clinical follow-up | Trapezoid | 100 | 100 | ||||
| CT | 1-year clinical follow-up | Hamate | 100 | 100 | ||||
| CT | 1-year clinical follow-up | Capitate | 100 | 0 | ||||
| Neubauer (2018) [69] | CBCT | Clinical follow-up | Scaphoid | 93 (89-96) | 96 (93-99) | 94 | 96 (93-99) | 92 (89-96) |
| Borel (2017) [70] | CBCT | MRI | Scaphoid cortical fracture | 100 (75-100) | 97 (83-100) | 94 (68-100) | 100 (87-100) | |
| CBCT | MRI | All scaphoid fractures | 94 (68-100) | 97 (83-100) | 94 (68-100) | 97 (82-100) | ||
| CBCT | MRI | Wrist cortical fracture | 100 (83-100) | 95 (75-100) | 96 (78-100) | 100 (83-100) | ||
| CBCT | MRI | All wrist fractures | 89 (70-97) | 95 (75-100) | 96 (78-100) | 88 (67-97) | ||
| Imaging: Bone scintigraphy | ||||||||
| Beeres (2007) [46] | Bone scintigraphy (3-7 days after injury) | Clinical outcome | Scaphoid | 92 | 87 | 88a | 69a | 97 |
| Bone scintigraphy (3-7 days after injury) | Clinical outcome | Scaphoid and other carpal bones | 96 | 59a | 80a | 75 | 93a | |
| Beeres (2008) [47] | Bone scintigraphy (between 3 and 5 days) | A combination of MRI, bone scintigraphy and when not in agreement, clinical follow-up | Scaphoid | 100 (83-100) | 90 (81-96) | 92 | 71 (52-87) | 100 (95-100) |
| Breederveld (2004) [49] | Bone scintigraphy (three-fase) | Clinical follow-up | Scaphoid | 78 | 90 | 86 | 78 | 90 |
| Rhemrev (2010) [62] | Bone scintigraphy (3-5 days) | Final diagnosis after CT, BS and, both radiographic (6 weeks after injury) and physical reevaluation. | Scaphoid | 93 | 91 | 91 | 62 | 99 |
| de Zwart (2016) [66] | Bone Scintigraphy (between 3 and5 days) | l diagnosis after MRI, CT, BS and 6-weeks clinical signs | Scaphoid | 100 | 97 (83-100) | 97 | 75 | 100 |
| Imaging: Ultrasonography | ||||||||
| Fusetti (2005) [51] | HSR-S global evaluation | CT (immediately after HSR-S performed) | Scaphoid | 100 | 79 | 83 | 56 | 100 |
| HSR-S scaphoid cortical disruption | CT (immediately after HSR-S performed) | Scaphoid | 100 | 95 | 96 | 83 | 100 | |
| HSR-S radioarpal (RS) effusion | CT (immediately after HSR-S performed) | Scaphoid | 100 | 42 | 54 | 31 | 100 | |
| HSR-S scapho-trapezium-trapezoid (STT) effusion | CT (immediately after HSR-S performed) | Scaphoid | 100 | 84 | 88 | 62 | 100 | |
| HSR-S cortical disruption with RS and STT effusion (high index of suspicion) | CT (immediately after HSR-S performed) | Scaphoid | 100 | 100 | 100 | 100 | 100 | |
| Herneth (2001) [53] | US | MRI | Scaphoid | 78 | 100 | 87 | 100 | 75 |
| Javadzadeh (2014) [74] | BUS | Radiographs | Carpal bones | 42 (23-64) | 87 (74-94) | 74 (62-83) | 57 (33-79) | 78 (65-88) |
| Javadzadeh (2014) [74] | WBT ultrasonography | Radiographs | Carpal bones | 47 (27-68) | 87 (74-94) | 75 (64-84) | 60 (36-80) | 80 (67-89) |
| Platon (2011) [61] | US | CT | Scaphoid | 92 | 71 | 76 | 46 | 97 |
| US | CT | Scaphoid fracture with a high potential of complication | 100 | 67 | 71 | 30 | 100 | |
| Yildirim (2013) [65] | BUS | MRI (<24h) | Scaphoid | 100 (69-100) | 34 (19-52) | 49 | 30 (16-49) | 100 (74-100) |
| Imaging: Tomosynthesis | ||||||||
| Ottenin (2012) [60] | Tomosynthesis | Clinical follow-up | Scaphoid | 91ɸ | 98ɸ | 96ɸ | 90ɸ | 98ɸ |
| Ottenin (2012) [60] | Tomosynthesis | Clinical follow-up | Other carpal bones | 80ɸ | 98ɸ | 96ɸ | 83ɸ | 98ɸ |
| Scaphoid, other carpal bones and/or metacarpal fractures | ||||||||
| Physical examination | ||||||||
| Nikken (2005) [73] | Anatomic snuffbox tenderness | Additional treatment need | Scaphoid and other carpal bones. Metacarpal bones II–IV | 39 | 78 | 62 | 56 | 65 |
| Imaging: Radiographs | ||||||||
| Balci (2015) [71] | Radiographs | MDCT | Metacarpal | 67 | 99 | 82 | 98 | |
| Jorgsholm (2013) [72] | Radiographs | MRI 0.23T (within 3 days) | Metacarpal | 30 (7-65) | ||||
| Nikken (2005) [73] | Radiographs | Additional treatment need | Scaphoid and other carpal bones. Metacarpal bones II–IV | 72 | 92 | 84 | 87 | 82 |
| Brink (2019) [68] | X-ray | 1-year clinical follow-up | Metacarpal | 67 | 100 | |||
| Imaging: MRI | ||||||||
| Nikken (2005) [73] | MRI | Additional treatment need | Scaphoid and other carpal bones. Metacarpal bones II–IV | 67 | 76 | 73 | 63 | 79 |
| Imaging: CT | ||||||||
| Brink (2019) [68] | CT | 1-year clinical follow-up | Metacarpal | 100 | 100 | |||
| Metacarpal bones and finger fractures | ||||||||
| Physical examination | ||||||||
| Tayal (2007) [77] | Physical examination: deformity | Radiographs and surgical findings | Metacarpal bones and phalanx | 55 (44-66) | 89 (83-96) | 76 | 77 (68-87) | 75 (65-85) |
| Physical examination: swelling | Radiographs and surgical findings | Metacarpal bones and phalanx | 94 (88-99) | 13 (5-20) | 45 | 41 (30-52) | 75 (65-85) | |
| Physical examination: erythema | Radiographs and surgical findings | Metacarpal bones and phalanx | 26 (16-36) | 85 (77-93) | 62 | 53 (42-54) | 63 (53-74) | |
| Imaging: Ultrasonography | ||||||||
| Tayal (2007) [77] | US | Radiographs and surgical findings | Metacarpal bones and phalanx | 90 (74-97) | 98 (95-100) | 95 | 97 (93-100) | 94 (89-99) |
| Javadzadeh (2014) [74] | BUS | Radiographs | Metacarpal bones | 73 (43-90) | 78 (45-94) | 70 (48-85) | 80 (49-94) | 70 (40-89) |
| BUS | Radiographs | Phalanx | 83 (61-94) | 90 (78-96) | 88 (78-94) | 79 (57-91) | 93 (81-97) | |
| WBT ultrasonography | Radiographs | Metacarpal bones | 82 (52-95) | 89 (57-98) | 70 (48-85) | 90 (60-98) | 80 (49-94) | |
| WBT ultrasonography | Radiographs | Phalanx | 94 (74-99) | 95 (84-99) | 95 (86-98) | 89 (87-100) | 98 (87-100) | |
| Kocaoglu (2016) [76] | US | Radiographs | Metacarpal bones | 93 (79-98) | 98 (90-100) | 96 | 97 (85-100) | 95 (85-98) |
| Imaging: CBCT | ||||||||
| Faccioli (2010) [75] | CBCT | MSCT | Articular involvement of the phalanx | 100 | 100 | 100 | 100 | 100 |
| CBCT | MSCT | Phalangeal bone fragments | 87 | 100 | 92 | 100 | 82 | |
BUS Bedside Ultra Sonography, CBCT Cone Beam Computed tomography arthrography, MDCT Multidetector Computed tomography, MRI Magnetic resonance imaging, T Tesla, US Ultra Sonography, HSR-S High Spatial Resolution sonography, VAS Visual Analogue Scale, Se Sensitivity, Sp Specificity, PPV Positive predictive value, NPV Negative predictive value, LR Likelihood ratio
aOne patient had a physical examination matching with another carpal fracture instead of a scaphoid fracture at both 2 and 6 weeks after injury
bFour patient did not receive MRI during follow-up (reference standard)
cPositive predictive value accounting for prevalence and incidence
dNegative predictive value accounting for prevalence and incidence
c/dThe positive predictive value and negative predictive value were determined with use of the Bayes theorem, which requires an a priori estimate of the prevalence (pretest probability) of the presence of scaphoid fractures. The positive predictive value is the patient’s probability of having a scaphoid fracture when the test is positive, and the negative predictive value is the probability of a patient not having a scaphoid fracture when the test is negative. The predictive values of any imaging modality depend critically on the prevalence of the characteristic in the patients being tested; hence the use of the appropriate Bayesian analysis is important. For the determination of positive and negative predictive values, we estimated an average prevalence of scaphoid fractures of 16% on the basis of the best available data. The positive predictive value was calculated as sensitivity · prevalence/(sensitivity · prevalence) 1 [(1 – specificity) · (1 – prevalence)], and the negative predictive value was calculated as specificity · (1 – prevalence)/[(1 – sensitivity) · prevalence] 1 [specificity · (1 – prevalence)].54,60
ɸ Average between presented individual values of three readers (junior radiologist, junior orthopedic surgeon and senior radiologist)
Repeated physical examination with radiological examination after 38 days [52] for diagnosing other carpal bone fractures showed a Se of 100% with the exception of the triquetrum (75%).
Radiographs used as an index test for diagnosing scaphoid fractures showed Se, Sp, accuracy, PPV and NPV ranging from 25 to 87%, 50–100%, 48–88%, 14–100% and 49–94%, respectively. For diagnosing scaphoid fractures, Magnetic Resonance Imaging (MRI) as an imaging modality showed Se, Sp, accuracy, PPV and NPV ranging from 67 to 100%, 89–100%, 85–100%, 54–100% and 93–100%, respectively. Multi Detector Computed Tomography (MDCT) showed Se, Sp, accuracy, PPV and NPV ranging from 33 to 100%, 85–100%, 79–100%, 28–100% and 86–100%, respectively. Bone Scintigraphy (BS) as an index test for diagnosing scaphoid fractures showed Se, Sp, accuracy, PPV and NPV ranging from 78 to 100%, 87–97%, 86–97%, 62–78% and 90–100%, respectively. For diagnosing scaphoid fractures, Ultrasonography (US) as an imaging modality showed Se, Sp, accuracy, PPV and NPV ranging from 78 to 100%, 34–100%, 49–100%, 30–100% and 75–100%, respectively.
Diagnosing phalangeal and metacarpal fractures in hospital care
Table 5 also presents the accuracy of the diagnostic tests for metacarpal and/or phalangeal fractures, as described in six studies [71, 73–77]. Physical examination [77] for diagnosing phalangeal and metacarpal fractures showed Se, Sp, accuracy, PPV and NPV ranging from 26 to 55%, 13–89%, 45–76%, 41–77% and 63–75%, respectively. Imaging for metacarpal and finger fractures showed Se, Sp, accuracy, PPV and NPV ranging from 73 to 100%, 78–100%, 70–100%, 79–100% and 70–100%, respectively. The reported diagnostic accuracy measures of phalangeal and metacarpal fractures were characterized by markedly heterogeneous results among the eligible studies.
Combined diagnostic accuracy of the studies with no limitations and no incorporation Bias
Table 6 shows combined diagnostic accuracy measures of the studies that had no limitations and no incorporation bias. A wide range of results were found for the specificity, accuracy and NPV of MRI, US, CT and BS. The sensitivity of BS and US showed similar, acceptable results. US and MRI are imaging tools that have similar PPV, but with large confidence intervals.
Table 6.
Combined Diagnostic Accuracy of the Studies with no Limitations on QUADAS-2 and No Incorporation Bias (N = 7)
| Author(s) | Diagnostic test | Scaphoid fracture | Se % | Sp % | Accuracy % | PPV % | NPV % |
|---|---|---|---|---|---|---|---|
| Gabler (2001) [52] | Repeated clinical and radiological examinationsa | Scaphoid | 82–100 | 100 | 100 | 100 | 100 |
| Mallee (2016) [57] | Radiographs b | Scaphoid | 42–79 | 53–59 | 53–58 | 14–26 | 79–94 |
| Fusetti (2005) [51] and Platon (2011) [61] | Ultrasonography | Scaphoid | 92–100 | 42–100 | 54–100 | 30–100 | 97–100 |
| Mallee (2011) [56] | MRI | Scaphoid | 67 | 8 | 85 | 57 | 93 |
| Mallee (2011) [56] and Mallee (2014 [58] | (MD)CTc | Scaphoid | 33–67 | 89–96 | 79–91 | 40–80 | 86–93 |
| Borel (2017) [70] | CBCT | Scaphoid | 94 | 97 | 94 | 97 | |
| Author | Diagnostic test | Other carpal fracture | Sensitivity % | Specificity % | Accuracy % | PPV % | NPV % |
| Mallee (2014) [58] | Repeated clinical and radiological examinations | Other carpal bones | 75–100 |
aRepeated clinical and radiological examinations after 10 and 38 days
bRadiographs after 6 weeks evaluated with JPEG or DICOM files
cCT-scaphoid: reformations in planes defined by the long axis of the scaphoid versus CT-wrist: reformations made in the anatomic planes of the wrist
Discussion
In previous reviews, no studies were identified on the diagnostic accuracy of history taking for phalangeal, metacarpal or carpal fractures. In the current systematic review, only two such studies were identified. This update included one extra study on physical examinations for diagnosing scaphoid fractures in hospital care, which was not included in previous reviews [48]. Based on these results and those presented in the previous reviews, physical examination is of moderate use for diagnosing a scaphoid fracture. Physicians should be aware that tenderness in the anatomical snuff box (ASB), tenderness over the scaphoid tubercle and pain on longitudinal compression of the thumb have limited added value in a diagnostic process for a scaphoid fracture.
The present systematic review identified eight supplementary imaging studies [58, 61, 65, 66, 68–70, 74], subdivided into MRI [66], CT [58, 66, 68–70], BS [66] and US [61, 65, 74]. The overall conclusion is that imaging tests were found to be moderately accurate for a definitive diagnosis. However, the standard diagnostic work-up for wrist complaints suspected of being a fracture should also include detailed patient history taking, a conscientious physical examination and, only if needed, imaging [23]. Diagnostic studies focusing on history taking and physical examination of patients with suspected phalangeal, metacarpal and carpal fractures are therefore desired.
Compared with previous reviews, the current systematic review attempted to distinguish between studies based on their setting. Remarkably, no studies examined the diagnostic accuracy of any diagnostic test for phalangeal, metacarpal and carpal fractures in a non-institutionalized general practitioner care setting. It is known that results from hospital care cannot automatically be translated into guidelines for non-institutionalized general practitioner care. For that reason, it is not possible to advise general practitioners properly on the diagnosis of carpal, metacarpal and phalangeal fractures based on the currently available literature. Given the burden of finger, hand and wrist fractures on non-institutionalized care and the importance of proper diagnoses, diagnostic studies focusing on phalangeal, metacarpal and carpal fractures in non-institutionalized general practitioner care are urgently needed [2].
Methodological quality assessment
The methodological quality of the eligible studies included in this update was limited, which might affect the estimates of diagnostic accuracy. Many of the included studies had methodological flaws and lacked the necessary details to replicate the studies. There was considerable underreporting of important domains in most of the included studies. The studies in this and previous systematic reviews also had the inherent risk of publication bias. As the mechanisms of publication bias are not yet well understood for diagnostic accuracy studies, there are currently no assessment tools available to investigate this risk other than graphical interpretation. Furthermore, several studies demonstrate incorporation bias, with the risk of overestimation of the diagnostic accuracy [78].
Diagnostic accuracy of the diagnostic tests for phalangeal and metacarpal fractures
The identified studies evaluated a variety of metacarpal and phalangeal pathologies. US may be an option for detecting metacarpal fractures and prevent unnecessary X-ray imaging examinations in patients presenting to the Emergency Department (ED) with hand trauma. Some advantages of US have increased its utilization in emergency departments; these include a short procedure time, a non-invasive and nonionizing radiation involving nature, availability for use in nonhospital settings or bedside settings, repeatability, and a higher safety in children and pregnant patients [79].
None of the previous reviews included studies showing evidence on the diagnostic accuracy for diagnosing metacarpal and phalangeal fractures. Therefore, this is the first study to systematically summarize the diagnostic accuracy of diagnostic tests for phalangeal and metacarpal fractures. This study concludes that physical examination was of limited use for diagnosing phalangeal and metacarpal fractures.
Diagnostic accuracy of history taking and physical examination of carpal fractures
History taking and physical examination are important tools in a diagnostic process of diagnosing patients with wrist pain [23]. Although common practice in hospital care, only two studies were found on the diagnostic accuracy of history taking for carpal fractures in the previous reviews and current review.
Previous reviews reported that tenderness in the anatomical snuff box demonstrated an Se and Sp for scaphoid fractures ranging from 87 to 100% and 3–98%, respectively [32, 34]. Tenderness over the scaphoid tubercle (ST) demonstrated a Se and Sp ranging from 82 to 100% and 17–57%, respectively [32, 34]. The Longitudinal Thumb Compression test (LTC) demonstrated a Se and Sp ranging from 48 to 100% and 22–97%, respectively [32, 34].
The current systematic update included three extra studies on physical examinations for diagnosing scaphoid fractures in hospital care [48, 52, 53]. Based on these results and those presented in the previous reviews, combining provocative tests improved the accuracy of the post-test fracture probability, and physical examination alone was not sufficient to rule in or rule out scaphoid fracture, which may lead to unnecessary out-patient reviews and/or overtreatment. If a patient with wrist pain and normal X-rays has a combination of tenderness in the anatomical snuff box, tenderness over the scaphoid tubercle and longitudinal compression (LC) tenderness towards the scaphoid, supplementary imaging is still recommended. At present, in a patient with a strong suspicion of a scaphoid fracture based on history taking and physical examination despite no deviation on imaging, the wrist will be temporarily immobilized until repeated evaluation of the physical examination and imaging has taken place later [80].
Diagnostic accuracy of imaging of carpal fractures
In this and previous systematic reviews, the reported diagnostic accuracy measures for imaging modalities were characterized by markedly heterogeneous results among the eligible studies. Plain radiography remained the commonest modality for diagnosing carpal fractures [81–83]. Its advantages include its wide availability, easy accessibility and low costs. Most studies describe diagnostic tests of scaphoid fractures and only a few studies concern other carpal fractures. At present, there is still insufficient scientific evidence regarding the ideal imaging technique for scaphoid fractures [23]. Repeated radiographs seems to have limited value for evaluating suspected scaphoid fractures. The irregular contour, the three-dimensional location in the wrist of the scaphoid and the overlap of the carpal bones render interpretation of scaphoid radiographs difficult, especially in the absence of fracture dislocation [81–83].
The best diagnostic modality for confirmation of the diagnosis of a carpal fracture that is not visible on the initial radiograph is still the subject of debate. As found in previous reviews (Table 1), MRI, CT and BS have been shown to have better diagnostic performance than isolated repeated scaphoid radiographs. Previous reviews by Yin et al. concluded that BS and MRI have equally high pooled sensitivity and high diagnostic value for excluding scaphoid fracture, when the lack of a reference standard is acknowledged [35, 36]. However, MRI is more specific and better for confirming scaphoid fractures when compared to BS. According to the Cochrane review of Mallee et al., statistically BS is the best diagnostic modality for establishing a definitive diagnosis in clinically suspected fractures when radiographs appear normal, but the number of overtreated patients is substantially lower with CT and MRI [39]. Moreover, physicians must keep in mind that BS is more invasive than the other modalities. Previous reviews by Kwee et al. and Ali et al. concluded that US can diagnose occult scaphoid fracture with a fairly high degree of accuracy and Kwee et al. stated that US may be used when CT and MRI are not readily available [37, 38]. Nonetheless, one needs to keep in mind that, although scaphoid fractures are the most frequently injured carpal bones, the consequences of fractures of other carpal bones should not be underestimated. All previously available systematic reviews only examined diagnostic tests for scaphoid fractures [32–39], while in practice it is often not quite clear during the diagnostic process which hand or wrist anatomical structure or tissue (soft tissue or bone) is affected.
Conclusion
As no studies in non-institutionalized general practitioner care were identified, general practitioners who examine patients with a suspected hand or wrist fracture have limited instruments for providing adequate diagnostics. A general practitioner could decide to refer such patients to a hospital for specialized care, but one could question what assessments a specialist can use to come to an accurate diagnosis. In hospital care, two studies of the diagnostic accuracy of history taking for phalangeal, metacarpal and carpal fractures were found and physical examination was of moderate use for diagnosing a scaphoid fracture and of limited use for diagnosing phalangeal, metacarpal and remaining carpal fractures. Based on the best evidence synthesis, imaging tests (conventional radiograph, MRI, CT and BS) were only found to be moderately accurate for definitive diagnosis in hospital care.
Acknowledgements
The authors thank Wichor Bramer (Biomedical information specialist of Erasmus MC University Medical Center Rotterdam, Medical Library) for help with the electronic search strategies and Yassine Aaboubout (MSc) for helping with study selection and extracting the data.
Abbreviations
- ASB
Anatomic snuff-box
- BS
Bone scintigraphy
- BUS
Bedside ultra sonography
- CBCT:
Cone beam computer tomography
- CT
Computed tomography
- HR
High risk
- HSR-S
High spatial resolution-sonography
- LR
Likelihood ratio
- LTC
Longitudinal (thumb) compression test
- MDCT
Multi detector computed tomography
- MRI
Magnetic resonance imaging
- MSCT
Multi-slice computer tomography
- NPV
Negative predictive value
- PPV
Positive predictive value
- QUADAS
Quality Assessment of diagnostic accuracy studies
- ROM
Range of motion
- Se
Sensitivity
- Sp
Specificity
- STT
Scaphoid tubercle tenderness
- T
Tesla
- UR
Unclear Risk
- US
Ultra sonography
- VAS
Visual analogue scale
- WBT
Water bath technique
Authors’ contributions
PK, NM, SB, GK and JR all contributed to the design of the study. PK and JR were responsible for article selection and analysed the data. All authors contributed to writing and revision of the manuscript. All authors have given approval of the submitted version of the manuscript and agree to be accountable for all aspects of the work.
Funding
No funding.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Patrick Krastman, Email: wetenschap@dezorghoek.nl.
Nina M. Mathijssen, Email: N.Mathijssen@rdgg.nl
Sita M. A. Bierma-Zeinstra, Email: s.bierma-zeinstra@erasmusmc.nl
Gerald Kraan, Email: KraanG@rdgg.nl.
Jos Runhaar, Email: j.runhaar@erasmusmc.nl.
References
- 1.Owen RA, Melton LJ, III, Johnson KA, Ilstrup DM, Riggs BL. Incidence of Colles fracture in a north American community. Am J Public Health. 1982;72:605–607. doi: 10.2105/AJPH.72.6.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Larsen CF, Mulder S, Johansen AM, Stam C. The epidemiology of hand injuries in The Netherlands and Denmark. Eur J Epidemiol. 2004;19(4):323–327. doi: 10.1023/B:EJEP.0000024662.32024.e3. [DOI] [PubMed] [Google Scholar]
- 3.McCullough NP, Smith FW, Cooper JG. Early MRI in the management of the clinical scaphoid fracture. Eur J Emerg Med. 2011;18(3):133–136. doi: 10.1097/MEJ.0b013e32833edb59. [DOI] [PubMed] [Google Scholar]
- 4.van der Molen AB, Groothoff JW, Visser GJ, Robinson PH, Eisma WH. Time off work due to scaphoid fractures and other carpal injuries in the Netherlands in the period 1990 to 1993. J Hand Surg Br. 1999;24(2):193–198. doi: 10.1054/JHSB.1998.0109. [DOI] [PubMed] [Google Scholar]
- 5.Hey HWD, Chong AKS, Murphy D. Prevalence of carpal fracture in Singapore. J Hand Surg Am. 2011;36(2):278–283. doi: 10.1016/j.jhsa.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 6.Van Onselen EB, Karim RB, Hage JJ, Ritt MJ. Prevalence and distribution of hand fractures. J Hand Surg Br. 2003;28(5):491–495. doi: 10.1016/S0266-7681(03)00103-7. [DOI] [PubMed] [Google Scholar]
- 7.Cooney WP., III Scaphoid fractures: current treatments and techniques. Instr Course Lect. 2003;52:197–208. [PubMed] [Google Scholar]
- 8.Krasin E, Goldwirth M, Gold A, Goodwin DR. Review of the current methods in the diagnosis and treatment of scaphoid fractures. Postgrad Med J. 2001;77:235–237. doi: 10.1136/pmj.77.906.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frazier WH, Miller M, Fox RS, Brand D, Finseth F. Hand injuries: incidence and epidemiology in an emergency service. JACEP. 1978;7:265–268. doi: 10.1016/S0361-1124(78)80336-0. [DOI] [PubMed] [Google Scholar]
- 10.Aitken S, Court-Brown CM. The epidemiology of sports-related fractures of the hand. Injury. 2008;39:1377–1383. doi: 10.1016/j.injury.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 11.Van der Linden MW, Westert GP, de Bakker DH, Schellevis FG. Tweede Nationale Studie naar ziekten en verrichtingen in de huisartspraktijk. NIVEL/RIVM: Klachten en aandoeningen in de bevolking en in de huisartspraktijk. Utrecht/Bilthoven; 2004. [Google Scholar]
- 12.Roolker W, Maas M, Broekhuizen AH. Diagnosis and treatment of scaphoid fractures, can non union be prevented? Arch Orthop Trauma Surg. 1999;119:428–431. doi: 10.1007/s004020050014. [DOI] [PubMed] [Google Scholar]
- 13.Schaub TA, Chung KC. Systems of provision and delivery of hand care, and its impact on the community. Injury. 2006;37(11):1066–1070. doi: 10.1016/j.injury.2006.07.021. [DOI] [PubMed] [Google Scholar]
- 14.de Putter CE, van Beeck EF, Polinder S, Panneman MJ, Burdorf A, Hovius SE, Selles RW. Healthcare costs and productivity costs of hand and wrist injuries by external cause: a population-based study in working-age adults in the period 2008-2012. Injury. 2016;47(7):1478–1482. doi: 10.1016/j.injury.2016.04.041. [DOI] [PubMed] [Google Scholar]
- 15.Greene WB. Essentials of musculoskeletal care. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2001.
- 16.Langhoff O, Andersen JL. Consequences of late immobilization of scaphoid fractures. J Hand Surg Br. 1988;13:77–79. doi: 10.1016/0266-7681(88)90058-7. [DOI] [PubMed] [Google Scholar]
- 17.Eddeland A, Eiken O, Hellgren E, Ohlsson NM. Fractures of the scaphoid. Scand J Plast Reconstr Surg. 1975;9:234–239. doi: 10.3109/02844317509022872. [DOI] [PubMed] [Google Scholar]
- 18.Taleisnik J. Clinical and technologic evaluation of ulnar wrist pain. J Hand Surg [Am] 1988;13:801–802. doi: 10.1016/0363-5023(88)90250-X. [DOI] [PubMed] [Google Scholar]
- 19.Steenvoorde P, Jacobi C, van der Lecq A, van Doorn L, Kievit J, Oskam J. Development of a clinical decision tool for suspected scaphoid fractures. Acta Orthop Belg. 2006;72(4):404–410. [PubMed] [Google Scholar]
- 20.Phillips TG, Reibach AM, Slomiany WP. Diagnosis and management of scaphoid fractures. Am Fam Physician. 2004;70:879–884. [PubMed] [Google Scholar]
- 21.Freeland P. Scaphoid tubercle tenderness: a better indicator of scaphoid fractures? Arch Emerg Med. 1989;6:46–50. doi: 10.1136/emj.6.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Grover R. Clinical assessment of scaphoid injuries and the detection of fractures. J Hand Surg Br. 1996;21:341–343. doi: 10.1016/S0266-7681(05)80197-4. [DOI] [PubMed] [Google Scholar]
- 23.Groves AM, Kayani I, Syed R, Hutton BF, Bearcroft PP, Dixon AK, Ell PJ. An international survey of hospital practice in the imaging of acute scaphoid trauma. AJR Am J Roentgenol. 2006;187(6):1453–1456. doi: 10.2214/AJR.05.0686. [DOI] [PubMed] [Google Scholar]
- 24.Hobby JL, Tom BD, Bearcroft PW, Dixon AK. Magnetic resonance imaging of the wrist: diagnostic performance statistics. Clin Radiol. 2001;56(1):50–57. doi: 10.1053/crad.2000.0571. [DOI] [PubMed] [Google Scholar]
- 25.Tiel-van Buul MM, van Beek EJ, Borm JJ, Gubler FM, Broekhuizen AH, van Royen EA. The value of radiographs and bone scintigraphy in suspected scaphoid fracture. A statistical analysis. J Hand Surg Br. 1993;18:403–406. doi: 10.1016/0266-7681(93)90074-P. [DOI] [PubMed] [Google Scholar]
- 26.Hunter JC, Escobedo EM, Wilson AJ, Hanel DP, Zink-Brody GC, Mann FA. MR imaging of clinically suspected scaphoid fractures. AJR Am J Roentgenol. 1997;168:1287–1293. doi: 10.2214/ajr.168.5.9129428. [DOI] [PubMed] [Google Scholar]
- 27.Furunes H, Vandvik PO. Cast immobilisation for suspected scaphoid fractures. Tidsskr Nor Laegeforen. 2009;129:177–179. doi: 10.4045/tidsskr.09.34096. [DOI] [PubMed] [Google Scholar]
- 28.Cheung GC, Lever CJ, Morris AD. X-ray diagnosis of acute scaphoid. J Hand Surg Br. 2006;31:104–109. doi: 10.1016/J.JHSB.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 29.Lozano-Calderon S, Blazar P, Zurakowski D, Lee SG, Ring D. Diagnosis of scaphoid fracture displacement with radiography and computed tomography. J Bone Joint Surg Am. 2006;88:2695–2703. doi: 10.2106/JBJS.E.01211. [DOI] [PubMed] [Google Scholar]
- 30.Steel N, Abdelhamid A, Stokes T, Edwards H, Fleetcroft R, Howe A, Qureshi N. A review of clinical practice guidelines found that they were often based on evidence of uncertain relevance to primary care patients. J Clin Epidemiol. 2014;67(11):1251–1257. doi: 10.1016/j.jclinepi.2014.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ring D, Lozano-Calderon S. Imaging for suspected scaphoid fracture. J Hand Surg Am. 2008;33(6):954–957. doi: 10.1016/j.jhsa.2008.04.016. [DOI] [PubMed] [Google Scholar]
- 32.Carpenter CR, Pines JM, Schuur JD, Muir M, Calfee RP, Raja AS. Adult scaphoid fracture. Acad Emerg Med. 2014;21(2):101–121. doi: 10.1111/acem.12317. [DOI] [PubMed] [Google Scholar]
- 33.Burrows B, Moreira P, Murphy C, Sadi J, Walton DM. Scaphoid fractures: a higher order analysis of clinical tests and application of clinical reasoning strategies. Man Ther. 2014;19(5):372–378. doi: 10.1016/j.math.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 34.Mallee WH, Henny EP, van Dijk CN, Kamminga SP, van Enst WA, Kloen P. Clinical diagnostic evaluation for scaphoid fractures: a systematic review and meta-analysis. J Hand Surg Am. 2014;39(9):1683–1691. doi: 10.1016/j.jhsa.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 35.Yin ZG, Zhang JB, Kan SL, Wang XG. Diagnostic accuracy of imaging modalities for suspected scaphoid fractures: meta-analysis combined with latent class analysis. J Bone Joint Surg Br. 2012;94(8):1077–1085. doi: 10.1302/0301-620X.94B8.28998. [DOI] [PubMed] [Google Scholar]
- 36.Yin ZG, Zhang JB, Kan SL, Wang XG. Diagnosing suspected scaphoid fractures: a systematic review and meta-analysis. Clin Orthop Relat Res. 2010;468(3):723–734. doi: 10.1007/s11999-009-1081-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kwee RM, Kwee TC. Ultrasound for diagnosing radiographically occult scaphoid fracture. Skelet Radiol. 2018;47(9):1205–1212. doi: 10.1007/s00256-018-2931-7. [DOI] [PubMed] [Google Scholar]
- 38.Ali M, Ali M, Mohamed A, Mannan S, Fallahi F. The role of ultrasonography in the diagnosis of occult scaphoid fractures. J Ultrason. 2018;18(75):325–331. doi: 10.15557/JoU.2018.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mallee WH, Wang J, Poolman RW, Kloen P, Maas M, de Vet HCW, Doornberg JN. Computed tomography versus magnetic resonance imaging versus bone scintigraphy for clinically suspected scaphoid fractures in patients with negative plain radiographs. Cochrane Database of Systematic Reviews 2015, Issue 6. Art. No.: CD010023. [DOI] [PMC free article] [PubMed]
- 40.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement BMJ 2009; 339: b2535. [PMC free article] [PubMed]
- 41.Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. QUADAS-2 group. Ann Intern Med. 2011;155(8):529–536. doi: 10.7326/0003-4819-155-8-201110180-00009. [DOI] [PubMed] [Google Scholar]
- 42.Devillé WL, Buntinx F, Bouter LM, Montori VM, de Vet HC, van der Windt DA, Bezemer PD. Conducting systematic reviews of diagnostic studies: didactic guidelines. BMC Med Res Methodol. 2002;2:9. doi: 10.1186/1471-2288-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Adey L, Souer JS, Lozano-Calderon S, Palmer W, Lee SG, Ring D. Computed tomography of suspected scaphoid fractures. J Hand Surg Am. 2007;32(1):61–66. doi: 10.1016/j.jhsa.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 44.Annamalai G, Raby N. Scaphoid and pronator fat stripes are unreliable soft tissue signs in the detection of radiographically occult fractures. Clin Radiol. 2003;58(10):798–800. doi: 10.1016/S0009-9260(03)00230-7. [DOI] [PubMed] [Google Scholar]
- 45.Behzadi C, Karul M, Henes FO, Laqmani A, Catala-Lehnen P, Lehmann W, Nagel HD, Adam G, Regier M. Comparison of conventional radiography and MDCT in suspected scaphoid fractures. World J Radiol. 2015;7(1):22–27. doi: 10.4329/wjr.v7.i1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Beeres FJ, Hogervorst M, Rhemrev SJ, den Hollander P, Jukema GN. A prospective comparison for suspected scaphoid fractures: bone scintigraphy versus clinical outcome. Injury. 2007;38(7):769–774. doi: 10.1016/j.injury.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 47.Beeres FJ, Rhemrev SJ, den Hollander P, Kingma LM, Meylaerts SA, le Cessie S, Bartlema KA, Hamming JF, Hogervorst M. Early magnetic resonance imaging compared with bone scintigraphy in suspected scaphoid fractures. J Bone Joint Surg Br. 2008;90(9):1205–1209. doi: 10.1302/0301-620X.90B9.20341. [DOI] [PubMed] [Google Scholar]
- 48.Bergh TH, Lindau T, Soldal LA, Bernardshaw SV, Behzadi M, Steen K, Brudvik C. Clinical scaphoid score (CSS) to identify scaphoid fracture with MRI in patients with normal x-ray after a wrist trauma. Emerg Med J. 2014;31(8):659–664. doi: 10.1136/emermed-2012-202219. [DOI] [PubMed] [Google Scholar]
- 49.Breederveld RS, Tuinebreijer WE. Investigation of computed tomographic scan concurrent criterion validity in doubtful scaphoid fracture of the wrist. J Trauma. 2004;57(4):851–854. doi: 10.1097/01.TA.0000124278.29127.42. [DOI] [PubMed] [Google Scholar]
- 50.Cruickshank Jaycen, Meakin Alex, Breadmore Ross, Mitchell David, Pincus Steven, Hughes Thomas, Bently Bronwyn, Harris Mark, Vo Austin. Early computerized tomography accurately determines the presence or absence of scaphoid and other fractures. Emergency Medicine Australasia. 2007;19(3):223–228. doi: 10.1111/j.1742-6723.2007.00959.x. [DOI] [PubMed] [Google Scholar]
- 51.Fusetti C, Poletti PA, Pradel PH, Garavaglia G, Platon A, Della Santa DR, Bianchi S. Diagnosis of occult scaphoid fracture with high-spatial-resolution sonography: a prospective blind study. J Trauma. 2005;59(3):677–681. [PubMed] [Google Scholar]
- 52.Gäbler C, Kukla C, Breitenseher MJ, Trattnig S, Vécsei V. Diagnosis of occult scaphoid fractures and other wrist injuries. Are repeated clinical examinations and plain radiographs still state of the art? Langenbeck's Arch Surg. 2001;386(2):150–154. doi: 10.1007/s004230000195. [DOI] [PubMed] [Google Scholar]
- 53.Herneth AM, Siegmeth A, Bader TR, Ba-Ssalamah A, Lechner G, Metz VM, Grabenwoeger F. Scaphoid fractures: evaluation with high-spatial-resolution US initial results. Radiol. 2001;220(1):231–235. doi: 10.1148/radiology.220.1.r01jl15231. [DOI] [PubMed] [Google Scholar]
- 54.Ilica AT, Ozyurek S, Kose O, Durusu M. Diagnostic accuracy of multidetector computed tomography for patients with suspected scaphoid fractures and negative radiographic examinations. Jpn J Radiol. 2011;29(2):98–103. doi: 10.1007/s11604-010-0520-3. [DOI] [PubMed] [Google Scholar]
- 55.Kumar S, O'Connor A, Despois M, Galloway H. Use of early magnetic resonance imaging in the diagnosis of occult scaphoid fractures: the CAST Study (Canberra Area Scaphoid Trial) N Z Med J. 2005;118(1209):U1296. [PubMed] [Google Scholar]
- 56.Mallee W, Doornberg JN, Ring D, van Dijk CN, Maas M, Goslings JC. Comparison of CT and MRI for diagnosis of suspected scaphoid fractures. J Bone Joint Surg Am. 2011;93(1):20–28. doi: 10.2106/JBJS.I.01523. [DOI] [PubMed] [Google Scholar]
- 57.Mallee WH, Mellema JJ, Guitton TG, Goslings JC, Ring D. Doornberg JN; science of variation group. 6-week radiographs unsuitable for diagnosis of suspected scaphoid fractures. Arch Orthop Trauma Surg. 2016;136(6):771–778. doi: 10.1007/s00402-016-2438-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mallee WH, Doornberg JN, Ring D, Maas M, Muhl M, van Dijk CN, Goslings JC. Computed tomography for suspected scaphoid fractures: comparison of reformations in the plane of the wrist versus the long axis of the scaphoid. Hand (NY) 2014;9(1):117–121. doi: 10.1007/s11552-013-9556-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Memarsadeghi M, Breitenseher MJ, Schaefer-Prokop C, Weber M, Aldrian S, Gäbler C, Prokop M. Occult scaphoid fractures: comparison of multidetector CT and MR imaging-initial experience. Radiol. 2006;240(1):169–176. doi: 10.1148/radiol.2401050412. [DOI] [PubMed] [Google Scholar]
- 60.Ottenin MA, Jacquot A, Grospretre O, Noël A, Lecocq S, Louis M, Blum A. Evaluation of the diagnostic performance of tomosynthesis in fractures of the wrist. AJR Am J Roentgenol. 2012;198(1):180–186. doi: 10.2214/AJR.11.6374. [DOI] [PubMed] [Google Scholar]
- 61.Platon A, Poletti PA, Van Aaken J, Fusetti C, Della Santa D, Beaulieu JY, Becker CD. Occult fractures of the scaphoid: the role of ultrasonography in the emergency department. Skelet Radiol. 2011;40(7):869–875. doi: 10.1007/s00256-010-1086-y. [DOI] [PubMed] [Google Scholar]
- 62.Rhemrev SJ, Beeres FJ, van Leerdam RH, Hogervorst M, Ring D. Clinical prediction rule for suspected scaphoid fractures: A prospective cohort study. Injury. 2010;41(10):1026–1030. doi: 10.1016/j.injury.2010.03.029. [DOI] [PubMed] [Google Scholar]
- 63.Rhemrev SJ, de Zwart AD, Kingma LM, Meylaerts SA, Arndt JW, Schipper IB, Beeres FJ. Early computed tomography compared with bone scintigraphy in suspected scaphoid fractures. Clin Nucl Med. 2010;35(12):931–934. doi: 10.1097/RLU.0b013e3181f9de26. [DOI] [PubMed] [Google Scholar]
- 64.Steenvoorde P, Jacobi C, van Doorn L, Oskam J. Pilot study evaluating a clinical decision tool on suspected scaphoid fractures. Acta Orthop Belg. 2006;72(4):411–414. [PubMed] [Google Scholar]
- 65.Yıldırım A, Unlüer EE, Vandenberk N, Karagöz A. The role of bedside ultrasonography for occult scaphoid fractures in the emergency department. Ulus Travma Acil Cerrahi Derg. 2013;19(3):241–245. doi: 10.5505/tjtes.2013.64927. [DOI] [PubMed] [Google Scholar]
- 66.de Zwart AD, Beeres FJ, Rhemrev SJ, Bartlema K, Schipper IB. Comparison of MRI, CT and bone scintigraphy for suspected scaphoid fractures. Eur J Trauma Emerg Surg. 2016;42(6):725–731. doi: 10.1007/s00068-015-0594-9. [DOI] [PubMed] [Google Scholar]
- 67.Sharifi MD, Moghaddam HZ, Zakeri H, Ebrahimi M, Saeedian H, Hashemian AM. The accuracy of pain measurement in diagnosis of scaphoid bone fractures in patients with magnetic resonance imaging: report of 175 cases. Med Arch. 2015;69(3):161–164. doi: 10.5455/medarh.2015.69.161-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Brink M, Steenbakkers A, Holla M, de Rooy J, Cornelisse S, Edwards MJ, Prokop M. Single-shot CT after wrist trauma: impact on detection accuracy and treatment of fractures. Skelet Radiol. 2019;48(6):949–957. doi: 10.1007/s00256-018-3097-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Neubauer J, Benndorf M, Ehritt-Braun C, Reising K, Yilmaz T, Klein C, Zajonc H, Kotter E, Langer M, Goerke SM. Comparison of the diagnostic accuracy of cone beam computed tomography and radiography for scaphoid fractures. Sci Rep. 2018;8(1):3906. doi: 10.1038/s41598-018-22331-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Borel C, Larbi A, Delclaux S, Lapegue F, Chiavassa-Gandois H, Sans N, Faruch-Bilfeld M. Diagnostic value of cone beam computed tomography (CBCT) in occult scaphoid and wrist fractures. Eur J Radiol. 2017;97:59–64. doi: 10.1016/j.ejrad.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 71.Balci A, Basara I, Çekdemir EY, Tetik F, Aktaş G, Acarer A, Özaksoy D. Wrist fractures: sensitivity of radiography, prevalence, and patterns in MDCT. Emerg Radiol. 2015;22(3):251–256. doi: 10.1007/s10140-014-1278-1. [DOI] [PubMed] [Google Scholar]
- 72.Jørgsholm P, Thomsen NO, Besjakov J, Abrahamsson SO, Björkman A. The benefit of magnetic resonance imaging for patients with posttraumatic radial wrist tenderness. J Hand Surg Am. 2013;38(1):29–33. doi: 10.1016/j.jhsa.2012.09.034. [DOI] [PubMed] [Google Scholar]
- 73.Nikken JJ, Oei EH, Ginai AZ, Krestin GP, Verhaar JA, van Vugt AB, Hunink MG. Acute wrist trauma: value of a short dedicated extremity MR imaging examination in prediction of need for treatment. Radiol. 2005;234(1):116–124. doi: 10.1148/radiol.2341031067. [DOI] [PubMed] [Google Scholar]
- 74.Javadzadeh HR, Davoudi A, Davoudi F, Ghane MR, Khajepoor H, Goodarzi H, Faraji M, Mahmoudi S, Shariat SS, Emami MK. Diagnostic value of "bedside ultrasonography" and the "water bath technique" in distal forearm, wrist, and hand bone fractures. Emerg Radiol. 2014;21(1):1–4. doi: 10.1007/s10140-013-1161-5. [DOI] [PubMed] [Google Scholar]
- 75.Faccioli N, Foti G, Barillari M, Atzei A, Mucelli RP. Finger fractures imaging: accuracy of cone-beam computed tomography and multislice computed tomography. Skelet Radiol. 2010;39(11):1087–1095. doi: 10.1007/s00256-010-0911-7. [DOI] [PubMed] [Google Scholar]
- 76.Kocaoğlu S, Özhasenekler A, İçme F, Pamukçu Günaydın G, Şener A, Gökhan Ş. The role of ultrasonography in the diagnosis of metacarpal fractures. Am J Emerg Med. 2016;34(9):1868–1871. doi: 10.1016/j.ajem.2016.06.083. [DOI] [PubMed] [Google Scholar]
- 77.Tayal VS, Antoniazzi J, Pariyadath M, Norton HJ. Prospective use of ultrasound imaging to detect bony hand injuries in adults. J Ultrasound Med. 2007;26(9):1143–1148. doi: 10.7863/jum.2007.26.9.1143. [DOI] [PubMed] [Google Scholar]
- 78.Worster A, Carpenter C. Incorporation bias in studies of diagnostic tests: how to avoid being biased about bias. CJEM. 2008;10(2):174–175. doi: 10.1017/S1481803500009891. [DOI] [PubMed] [Google Scholar]
- 79.William DM, Kurtz BK, Hertzberg BS. In: Yımaz C, editor. Bilinmesi Gerekenler-Ultrason. Çev. Ed. 2. Baskı. İzmir: Güven Bilimsel; 2008:3–4.
- 80.Dias J, Kantharuban S. Treatment of scaphoid fractures: European approaches. Hand Clin. 2017;33(3):501–509. doi: 10.1016/j.hcl.2017.04.003. [DOI] [PubMed] [Google Scholar]
- 81.Low G, Raby N. Can follow-up radiography for acute scaphoid fracture still be considered a valid investigation? Clin Radiol. 2005;60:1106–1110. doi: 10.1016/j.crad.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 82.Munk B, Frokjaer J, Larsen CF, Johannsen HG, Rasmussen LL, Edal A, Rasmussen LD. Diagnosis of scaphoid fractures. A prospective multicenter study of 1,052 patients with 160 fractures. Acta OrthopScand. 1995;66:359–360. doi: 10.3109/17453679508995561. [DOI] [PubMed] [Google Scholar]
- 83.Tiel-van Buul MM, van Beek EJ, Broekhuizen AH, Nooitgedacht EA, Davids PH, Bakker AJ. Diagnosing scaphoid fractures: radiographs cannot be used as a gold standard! Injury. 1992;23:77–79. doi: 10.1016/0020-1383(92)90035-Q. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


