Abstract
Introduction
Kidney injury molecule-1 (KIM-1) is an important diagnostic and prognostic marker in acute kidney injury and chronic kidney disease of various aetiologies. The aim of the study was to evaluate the usefulness of serum KIM-1 (sKIM-1) and urine KIM-1 (uKIM-1) for predicting febrile and non-febrile urinary tract infection (UTI) in infants.
Material and methods
A prospective study included 101 children divided into three groups: febrile UTI 49 children, non-febrile UTI 22 children, and healthy controls 30 children. The following laboratory tests were performed: sKIM-1, uKIM-1, white blood count (WBC), C-reactive protein (CRP), and procalcitonin (PCT).
Results
Median levels of sKIM-1 were significantly higher in the febrile and non-febrile UTI group compared to the healthy controls (both p < 0.05). Mean levels of uKIM-1 were significantly lower in the febrile UTI group compared to the non-febrile UTI group and healthy controls (p < 0.001 and p < 0.0001, respectively). Univariate logistic regression analysis has demonstrated a positive association of sKIM-1 with febrile and non-febrile UTI (both p < 0.05), and negative association uKIM-1 with febrile UTI (p < 0.0001). Receiver operating curve (ROC) analysis showed good diagnostic profiles of uKIM-1 with a best cut-off value of 2.4 ng/ml and sKIM-1 with a best cut-off value of 3.88 ng/ml for predicting febrile UTI (area under the curve [AUC] 0.82 and 0.67, sensitivity 73% and 63%, specificity 86% and 80%, respectively).
Conclusions
sKIM-1 can be useful for predicting febrile UTI. We do not recommended use of uKIM-1 as a marker of febrile UTI because of its negative association with febrile UTI. Both markers are not useful for predicting non-febrile UTI.
Keywords: children, biomarkers, acute kidney injury, urinary tract infection, kidney injury molecule-1
Introduction
Urinary tract infection (UTI) is one of the most common bacterial infections in infants [1]. It occurs in 5.7-8.3% of girls presenting with fever in the first year of life and varies from 8.7% in febrile boys aged < 3 months to 1.7% in febrile boys aged 6 months to 1 year [2]. The diagnosis of UTI in infants is challenging due to non-specific UTI symptoms in this age [3, 4]. Moreover, difficulty in specimen collection, non-infection pyuria, and the high risk of contamination of urine may contribute to its misdiagnosis in infants [5, 6]. The waiting time required for urine culture results poses another problem [3, 7]. Paediatricians may be confused as to whether antibiotic treatment should be started before obtaining the results of urine culture [5]. Febrile UTI may cause acute pyelonephritis (APN) and subsequent renal scarring. Therefore, it is important to diagnose and treat UTI as soon as possible [3, 8]. Other markers of UTI, besides urinalysis and urine culture, are needed for quick identification of cases of UTI in infants [5].
Several studies have suggested potential biomarkers for this purpose, e.g. interleukin (IL)-6, IL-8, neutrophil gelatinase-associated lipocalin (NGAL), kidney injury molecule (KIM-1), retinol binding protein (RBP), and YKL-40 glycoprotein [6, 7, 9, 10]. KIM-1, a type I cell membrane glycoprotein, was discovered by Ichimura et al. in 1998 [11]. It is expressed at low level in healthy kidney but is highly upregulated in injured proximal tubule epithelial cells [3, 12]. KIM-1 is an important diagnostic and prognostic marker in acute kidney injury (AKI) and chronic kidney disease (CKD) of various aetiologies [12]. It was also investigated in UTI in children and adults. However, the data about its role in UTI are still limited and contentious [6, 7, 13, 14]. The aim of the study was to evaluate the usefulness of serum KIM-1 (sKIM-1) and urine KIM-1 (uKIM-1) for predicting febrile and non-febrile UTI in infants.
Material and methods
This prospective observational study was performed in infants with a first episode of UTI, who were diagnosed and treated in the Department of Paediatrics and Nephrology of Warsaw Medical University. The study was conducted from May 2016 to February 2019. The research was approved by the Local Bioethics Committee. Written, informed consent was obtained from all parents. We enrolled 101 children aged between one month and 12 months: 71 infants who presented with a first episode of UTI and 30 healthy infants as a control group. Children with other infectious disease, previous UTI, and known congenital urinary tract anomalies were excluded. The control group included healthy infants without any infection, history of UTI, or renal disease. Based on the clinical manifestation and laboratory tests, children were categorised into three groups: febrile UTI, non-febrile UTI, and healthy controls. Fever was defined as the presence of body temperature > 38.0°C. Urinalysis, urine culture, white blood cell count (WBC), C-reactive protein (CRP), procalcitonin (PCT), and serum creatinine (Cr) were performed on admission. Urine samples were collected by bladder catheterisation or midstream urine. Pyuria was defined as > 10 WBC per high-power field (HPF; 400×) in the urine sediment. Significant bacteriuria was defined as growth of a single pathogen with bacterial concentration in urine ≥ 105/colony-forming units (CFU)/ml. UTI was diagnosed on the basis of the presence of both pyuria and significant bacteriuria. Antibacterial treatment was started immediately after urinalysis and urine culture was collected. Normal values of evaluated indices were as follows: CRP ≤ 1.0 mg/dl, PCT < 0.05 mg/dl, Cr ≤ 0.4 mg/dl, and WBC count according to age. Serum and urine samples for measurement of sKIM-1 and uKIM-1 were collected prior to antibiotic treatment. They were immediately centrifuged and stored at –80°C until further evaluation. The levels of sKIM-1 and uKIM-1 were determined using commercially available enzyme-linked immunosorbent assay (ELISA) kit (Human Kim-1; cat. no: 201-12-1100; SunRed, Shanghai, China), following the manufacturer instructions. Serum samples for KIM-1 were diluted 1 : 2; urine samples for KIM-1 were not diluted. The detection range for sKIM-1 was 0.1-20 ng/ml and for uKIM-1 was 0.1-10 ng/ml. Kidney and urinary tract ultrasound (US) was performed after admission, and voiding cystourethrography (VCUG) was performed 2-3 weeks after treatment of UTI for children with any abnormal finding on US or atypical UTI.
Statistical methods
Statistical analysis was performed with the use of the Statistica package version 11.0 for Windows. The distribution of continuous variables was checked for normality using Shapiro-Wilk test. Continuous data were presented as the mean ±standard deviation (SD) or median with interquartile range (IQR). Variables with normal distribution (age, WBC, and uKIM-1) were checked for homogeneity of variances using Bartlett test. Parametric ANOVA test or non-parametric Kruskal-Wallis test were used to compare continuous variables between three groups. Parametric Student’s t-test and non-parametric Mann-Whitney test were used to compare variables between two groups. Categorical data (gender) were presented as numbers and percentiles. Tests for probability were used to compare the gender distribution between three groups. Correlations between variables were evaluated by Sperman’s rank correlation. The coefficient of univariate logistic regression (β1) and odds ratio (OR) including 95% confidence interval (CI) were calculated to identify the association of sKIM-1 and uKIM-1 with the presence of febrile and non-febrile UTI. Receiver operating curves (ROC) were performed and areas under the curves (AUC) were calculated, including 95% CI, to determine the sensitivity, specificity, and optimal cut-off values of sKIM-1 and uKIM-1 to predict febrile and non-febrile UTI. The statistical significance level was established at p < 0.05.
Results
Febrile UTI was diagnosed in 49 (69%) infants, non-febrile UTI in 22 (31%). The control group consisted of 30 infants. Escherichia coli was isolated in 68 (96%) infants with UTI, and other bacteria in three (4%) children (Klebsiella pneumoniae in one, Proteus mirabilis in one, Enterococcus faecalis in one). Based on US and VCUG, CAKUT was diagnosed in 13 (12.9%) children: in six with febrile UTI (five – VUR grade 2, one – mild pyelectasis), in three with non-febrile UTI (two – mild pyelectasis, one – duplicated collecting system), and in four healthy controls (four – mild pyelectasis). There were no significant differences in frequency of CAKUT in the groups of children (data not shown).
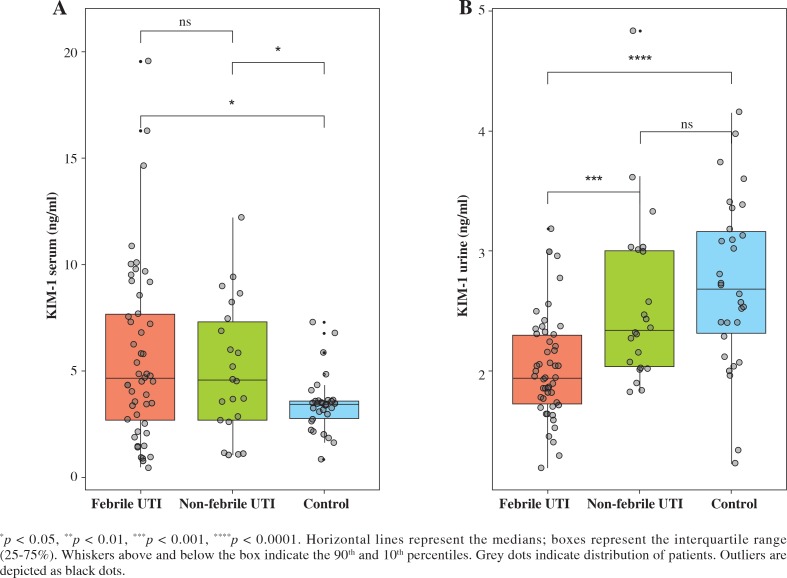
Demographic and laboratory data for each group are summarised in Table 1. The age distribution did not differ between the groups. There were significantly more boys in the febrile UTI group than in the healthy control group. Median levels of sKIM-1 were significantly higher in the febrile and non-febrile UTI group compared to the heathy controls. There was no significant difference in sKIM-1 levels between the febrile and non-febrile UTI group (Table 1, Fig. 1A). Mean levels of uKIM-1 were significantly lower in the febrile UTI group compared to the non-febrile UTI group and healthy controls. There was no significant difference in uKIM-1 levels between non-febrile UTI and healthy controls (Table 1, Fig. 1B). Mean levels of WBC and median levels of CRP and PCT were significantly higher in the febrile UTI group than in the non-febrile UTI group. No significant differences in urine WBC count and proteinuria were documented between patients with febrile and non-febrile UTI (data not shown). sCr levels were normal in all children evaluated in the study (data not shown).
Table 1.
Demographic and laboratory findings of children with febrile urinary tract infection (UTI), non-febrile UTI, and healthy controls
| Variable | Group | p | ||||
|---|---|---|---|---|---|---|
| Febrile (1) (n = 49) |
Non-febrile (2) (n = 22) |
Control (3) (n = 30) |
1 vs. 2 | 1 vs. 3 | 2 vs. 3 | |
| Age (months) | 5.3 ±3.15 | 3.84 ±2.3 | 4.63 ±2.9 | NS | NS | NS |
| Boys, n (%) | 30 (61.2) | 14 (63.3) | 11 (36.7) | NS | < 0.05 | NS |
| sKIM-1 (ng/ml) IQR |
4.66 4.96 |
4.54 4.8 |
3.43 0.9 |
NS | < 0.05 | < 0.05 |
| uKIM-1 (ng/ml) | 2.02 ±0.43 | 2.57 ±0.72 | 2.73 ±0.71 | < 0.001 | < 0.0001 | NS |
| WBC (mm3) | 20.2 ±6.85 | 15.24 ±3.71 | – | < 0.05 | – | – |
| CRP (mg/dl) IQR |
8.2 10.7 |
1.25 2.2 |
– | < 0.0001 | – | – |
| PCT (ng/ml) IQR |
0.87 4.28 |
0.08 0.03 |
– | < 0.0001 | – | – |
Normally distributed variables are presented as mean ±SD, non-normally distributed variables are presented as median and IQR; sKIM-1 – serum kidney injury molecule-1, uKIM-1 – urine kidney injury molecule-1, WBC – white blood cell count, CRP – C-reactive protein, PCT – procalcitonin
Fig. 1.
Values of serum and urine kidney injury molecule-1 in children with febrile urinary tract infection (UTI), non-febrile UTI, and healthy controls
Correlations between sKIM-1 and uKIM-1, one side and age, and inflammatory markers on the other side are presented in Table 2. There was negative correlation of uKIM-1 with age WBC, CRP, and PCT. Univariate logistic regression analysis demonstrated a positive association of sKIM-1 with febrile and non-febrile UTI and negative association of uKIM-1 with febrile UTI (Table 3). ROC analysis demonstrated that sKIM-1 and uKIM-1 have high specificity and lower sensitivity for prediction of febrile UTI and that these markers are not useful for prediction of non-febrile UTI (Table 4).
Table 2.
Correlations between biomarkers, age, and inflammatory markers of urinary tract infection (UTI)
| Variable | sKIM-1 | uKIM-1 | ||
|---|---|---|---|---|
| r | p | r | p | |
| Age | –0.02 | NS | –0.24 | < 0.05 |
| sKIM-1 | – | – | 0.07 | NS |
| uKIM-1 | 0.07 | NS | – | – |
| WBC | 0.17 | NS | –0.29 | < 0.05 |
| CRP | 0.07 | NS | –0.39 | < 0.05 |
| PCT | 0.16 | NS | –0.33 | < 0.05 |
sKIM-1 – serum kidney injury molecule-1, uKIM-1 – urine kidney injury molecule-1, WBC – white blood cell count, CRP – C-reactive protein, PCT – procalcitonin
Table 3.
Univariate logistic regression analysis of serum and urine kidney injury molecule-1 for prediction of febrile and non-febrile urinary tract infection (UTI)
| Variable | β1 | p | OR (95% CI) |
|---|---|---|---|
| Febrile UTI | |||
| sKIM-1 | 0.273 | < 0.05 | 1.31 (1.07-1.62) |
| uKIM-1 | –2.242 | < 0.0001 | 0.11 (0.04-0.32) |
| Non-febrile UTI | |||
| sKIM-1 | 0.318 | < 0.05 | 1.37 (1.04-1.82) |
| uKIM-1 | –0.340 | NS | 0.71 (0.32-1.6) |
β1 – coefficient of logistic regression, OR – odds ratio, CI – confidence interval, sKIM-1 – serum kidney injury molecule-1, uKIM-1 – urine kidney injury molecule-1
Table 4.
Diagnostic value of serum and urine kidney injury molecule-1 for diagnosing febrile and non-febrile urinary tract infection (UTI)
| Variable | AUC | p | Cut off (ng/ml) | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|
| Febrile UTI | |||||
| sKIM-1 | 0.67 (0.55-0.79) | < 0.01 | 3.88 | 63.3 | 80.0 |
| uKIM-1 | 0.82 (0.72-0.92) | < 0.0001 | 2.4 | 73.3 | 85.7 |
| Non-febrile UTI | |||||
| sKIM-1 | 0.66 (0.49-0.83) | NS = 0.06 | 3.66 | 63.6 | 80.0 |
| uKIM-1 | 0.38 (0.23-0.54) | NS | – | – | – |
sKIM-1 – serum kidney injury molecule-1, uKIM-1 – urine kidney injury molecule-1
Discussion
KIM-1 is emerging as a sensitive and specific biomarker for kidney proximal tubule injury, which increases earlier than any of the conventional biomarkers, e.g. sCr and blood urea nitrogen (BUN) [15]. It is one of the most effective biomarkers for early diagnosis of AKI and its clinical outcomes [12, 16-18]. KIM-1 demonstrates prognostic potency in CKD patients with primary inflammatory renal disease, such as glomerulonephritis and vasculitis [19], in diabetic kidney disease (DKD) [12, 20], allograft nephropathy, and renal cell carcinoma [20]. Additionally, it has been approved by the US Food and Drug Administration (FDA) and European Medicines Agency (EMA) as a urinary biomarker for monitoring drug-induced AKI in preclinical studies and clinical trials [21]. KIM-1 has been evaluated in UTI, but the findings of experimental and clinical studies are contentious [3, 6, 14].
Young children with UTI may develop prerenal type of AKI due to dehydration and renal hypoperfusion as a result of fever, reduced appetite, and vomiting [4, 8]. Significantly less often, severe forms of APN may provide the renal type of AKI [8, 22]. Skowron et al. in an experimental study performed in rats, found significantly higher uKIM-1 levels in the APN group with AKI developing secondarily to the UTI, as well in the APN group with AKI and urosepsis, than in the isolated APN group. The authors suggested that uKIM-1 can be used as a marker of AKI associated with UTI [22]. Petrovic et al. also reported significantly higher uKIM-1 levels in APN children complicated with AKI than in APN children without AKI [8]. Han et al. demonstrated in adults significantly higher levels of uKIM-1/uCr in patients with AKI than in patients with UTI, and no difference between UTI patients and healthy controls [14]. Urbschat et al. found in adults no differences in levels of uKIM-1 in patients with uncomplicated upper and lower UTI compared to healthy controls [13]. In our study children with UTI had no signs of AKI. We demonstrated no differences in uKIM-1 levels between children with non-febrile UTI and healthy controls. We even found significantly lower uKIM-1 levels in the febrile UTI group compared to the non-febrile UTI group and healthy controls. APN involves tubule-interstitial region in the kidney. In APN the distal part of nephron is affected more than the proximal tubule. Therefore, the low levels of KIM-1 in patients with APN without AKI and in patients with lower UTI are not unexpected [13].
Contradictory reports have demonstrated that uKIM-1 is also effective for diagnosis of UTI in children without AKI. Yim et al. reported significantly elevated levels of uKIM-1 and uKIM-1/uCr in febrile UTI children compared to healthy controls. However, they found relatively low sensitivity (50% and 45%, respectively) of both markers for predicting febrile UTI [6]. Also, Lee et al. described significantly elevated uKIM-1/uCr levels in febrile UTI children compared to febrile and non-febrile controls. They noted higher sensitivity (76%) of uKIM-1/uCr for detecting febrile UTI [3]. Valdimarsson et al. presented in UTI infants significantly higher uKIM-1 levels than in healthy controls and significantly higher uKIM-1/uCr levels than in febrile and healthy controls [7]. The authors revealed nearly the same sensitivity of both markers (74% and 75%, respectively) as did Lee et al. for diagnosing UTI [3].
The reasons for the heterogenicity of the results above outlines remain unclear. There are two possible explanations for these findings. The first possibility is that elevated levels of uKIM-1 in UTI children were associated with unrecognised subclinical AKI. This is supported by the study by Moledina et al., who found that 49% of deceased kidney donors with severe histological acute tubular injury (ATI) in kidney biopsy did not have sCr-based AKI [23]. Currently AKI is defined as a rise in sCr. However, sCr is not a sensitive and specific marker for early AKI detection because its concentration may not change until 25-50% of the kidney function has been lost [24]. An alternative explanation is that proteinuria detected in UTI children could affect the uKIM-1 concentration in the absence of injury. Nadkarni et al. reported that several factors available through urine dipstick, including proteinuria, haematuria, leukocyte esterase, and nitrites were associated with increased uKIM-1 concentration, which was independent of clinical kidney injury [25]. On one hand, it is well known that proteinuria may be an early symptom of ATI [15]. On the other hand, most UTI patients demonstrate proteinuria in urinalysis, which is associated with inflammation in the urinary tract and pyuria rather than with subclinical AKI. In the present work sCr levels were normal in all children evaluated in the study and no significant differences in proteinuria levels were documented between patients with febrile and non-febrile UTI.
KIM-1 is not an inflammatory marker, and its increase is independent of infection, such as UTI [22]. This was confirmed by studies, which demonstrated elevated uKIM-1 levels only in individuals with AKI or with APN complicated by AKI [8, 14, 22]. However, Yim et al. and Petrovic et al. reported significantly lower uKIM-1 levels after treatment UTI than before [6, 8], and Lee et al. reported positive correlation of uKIM-1/uCr with CRP [3]. In the current study we found significantly higher levels of WBC, CRP, and PCT in the febrile UTI group than in the non-febrile UTI group, but we noted negative correlation of uKIM-1 with WBC, CRP, and PCT. The biological role of KIM-1 in kidney injury remains unknown. It has been suggested that KIM-1 expression is associated with both kidney injury and recovery processes [12, 16]. KIM-1 induces re-epithelisation and reduces apoptosis. It transforms proximal epithelial cells into semi-professional phagocytes, mediates phagocytosis of apoptotic cells, and down-regulates the proinflammatory immune response in acute ischaemic and toxic injury [8, 12]. Probably, the decrease of uKIM-1 levels after treatment UTI in the studies by Petrovic et al. and Yim et al. were associated with subclinical AKI and regeneration process after tubule injury.
To date, nothing is known about the value of blood KIM-1 for predicting UTI. Several studies have documented that after proximal tubule injury KIM-1 could also be released into the bloodstream [21]. Blood elevation of KIM-1 is associated with lost polarity of tubule epithelial cells and increased trans-epithelial and microvascular permeability [26]. Experimental studies found significantly higher plasma KIM-1 (pKIM-1) levels in acute and chronic kidney injury [26, 27]. In humans, the usefulness of blood (serum/plasma) KIM-1 was documented in AKI and CKD [21, 26, 28]. Circulating KIM-1 strongly predicted progression of CKD in patients with type 1 and type 2 diabetes [26, 29, 30] and was useful in allograft nephropathy [31]. A recent study by Schultz et al. has also shown that pKIM-1 may predict the future decline of estimated glomerular filtration rate (eGFR) and risk of CKD in healthy middle-aged participants [32]. Our study demonstrated significantly higher sKIM-1 levels in febrile and non-febrile UTI groups compared to the heathy controls. However, children with UTI had normal values of serum Cr; it is possible that some of the UTI children could have not recognised subclinical AKI. We can speculate that blood elevation of KIM-1 in UTI patients could be detected earlier than urine elevation of KIM-1. Therefore, we found in infants with UTI high levels of sKIM-1 and low levels of uKIM-1. Most of the children with febrile UTI were admitted to the hospital in the early phase of UTI, after a few hours of fever.
Studies performed in children with UTI have demonstrated lower sensitivity of uKIM-1 for detecting UTI than uNGAL, which was investigated in this purpose [3, 6, 7]. In our previous research conducted in a smaller cohort of children, we found that sNGAL was a good diagnostic marker of febrile UTI with higher sensitivity than uNGAL. In non-febrile children the diagnostic value of sNGAL was smaller, and uNGAL was not useful at all [10]. The present work demonstrated better diagnostic profile for uKIM-1 than sKIM-1 for predicting febrile UTI (AUC 0.82 vs. 0.67, respectively; sensitivity 73% vs. 63%, respectively). sKIM-1 and uKIM-1 were not useful for predicting non-febrile UTI.
In the healthy population KIM-1 is released in very low or undetectable levels from renal proximal tubules and liver [19, 26]. The baseline value of uKIM-1 may differ and be related to the degree of prematurity, age, and gender. Askenazi et al. reported that uKIM-1 levels were higher in the most premature infants and decreased with increasing gestational age [24]. Kamianowska et al. found in healthy full-term newborns positive correlation of uKIM-1 and inverse correlation of sKIM-1 with gestational age [33]. Zwiers et al. revealed in children aged one day to one year no relation of uKIM-1 with age [34]. Studies performed in older children presented increase of uKIM-1 levels with age [35, 36]. Pennemans et al. also demonstrated in a healthy population higher uKIM-1 levels in males than in females [37]. Reference intervals for sKIM-1 are lacking for healthy individuals. McWiliams et al. reported also diurnal variation of uKIM-1 levels, with higher values in the morning than in the evening [30]. In contrast, we found negative correlation of uKIM-1 with age. In our study serum and urine samples were collected at various times of day. It could affect results of serum and urine KIM-1. We analysed only absolute values of uKIM-1. Normalisation of the tubular marker to uCr is controversial [12]. uKIM-1 is released from injured tubular cells, whereas uCr is dependent on the glomerular filtration rate. A study by Schley et al. demonstrated that normalisation of urine biomarkers is required in patients with the need for high fluid resuscitation, e.g. sepsis, to account for variations of urinary flow rate [38]. Urine Cr excretion demonstrates age-related changes and may vary for different reasons; therefore, urine Cr would not be useful as a normalisation tool [35, 36].
There are some limitations of this study. It was a single-centre study with a small number of patients in each group. The small sample size could affect to the results of our study, and the statistical results could be improved after recruiting more patients. Serum and urine samples for KIM-1 were collected at varying times of day. This could also affect the results.
Conclusions
This study was performed to evaluate the potential value of serum and urine KIM-1 for the prediction of febrile and non-febrile UTI. The results of this prospective study show that high levels of sKIM-1 can be useful for predicting febrile UTI. The role of uKIM-1 for detecting febrile UTI is not clear because of the negative association of uKIM-1 with febrile UTI. Therefore, we do not recommend the use of uKIM-1 as a marker of febrile UTI. Serum and urine KIM-1 were not useful for predicting non-febrile UTI.
Footnotes
The authors declare no conflict of interest.
References
- 1.Hansson S, Bollgren I, Esbjörner E, et al. Urinary tract infection in children below two years of age: a quality assurance oriject in Sweden. Acta Paediatr. 1999;88:270–274. doi: 10.1080/08035259950170015. [DOI] [PubMed] [Google Scholar]
- 2.Shaikh N, Morone NE, Bost JE, et al. Prevalence of urinary tract infection in childhood: a meta-analysis. Pediatr Infect Dis J. 2008;27:302–308. doi: 10.1097/INF.0b013e31815e4122. [DOI] [PubMed] [Google Scholar]
- 3.Lee H-E, Kim DK, Kang HK, et al. The diagnosis of febrile urinary tract infection in children may be facilitated by urinary biomarkers. Pediatr Nephrol. 2015;30:123–130. doi: 10.1007/s00467-014-2905-5. [DOI] [PubMed] [Google Scholar]
- 4.Wang P-Y, Chang H-C, Lei R-L, et al. Personal history and physical examination in judgment of urinary tract infection in children aged 3 months to 2 year. Pediatr Neonatol. 2016;57:274–279. doi: 10.1016/j.pedneo.2015.09.011. [DOI] [PubMed] [Google Scholar]
- 5.Kim HH, Chung MH, Bin JH, et al. Urinary YKL-40 as a candidate biomarker for febrile urinary tract infection in young children. Ann Lab Med. 2018;38:39–45. doi: 10.3343/alm.2018.38.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yim HE, Yim H, Bae ES, et al. Predictive value of urinary and serum biomarkers in young children with febrile urinary tract infections. Pediatr Nephrol. 2014;29:2181–2189. doi: 10.1007/s00467-014-2845-0. [DOI] [PubMed] [Google Scholar]
- 7.Valdimarsson S, Jodal U, Barregård L, et al. Urine neutrophil gelatinase-associated lipocalin and other biomarkers in infants with urinary tract infection and in febrile controls. Pediatr Nephrol. 2017;32:2079–2087. doi: 10.1007/s00467-017-3709-1. [DOI] [PubMed] [Google Scholar]
- 8.Petrovic S, Bogavac-Stanojevic N, Peco-Antic A, et al. Clinical application neutrophil gelatinase-associated lipocalin and kidney injury molecule-1 as indicators of inflammation persistence and acute kidney injury in children with urinary tract infection. Biomed Res Int. 2013;2013:947157. doi: 10.1155/2013/947157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krzemień G, Szmigielska A, Turczyn A, et al. Urine interleukin-6, interleukin-8 and transforming growth factor β1 in infants with urinary tract infection and asymptomatic bacteriuria. Centr Eur J Immunol. 2016;41:260–267. doi: 10.5114/ceji.2016.63125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krzemień G, Pańczyk-Tomaszewska, Adamczuk D, et al. Neutrophil gelatinase-associatedl lipocalIn: a biomarker for early diagnosis of urinary tract infections in infants. Advs Exp Med Biol. 2018;38:71–80. doi: 10.1007/5584_2017_107. [DOI] [PubMed] [Google Scholar]
- 11.Ichimura T, Bonventre JV, Bailly JV, et al. Kidney injury molecule-1 (KIM-1), a putative epithelial cell adhesion molecule containing a novel immunoglobulin domain, is up-regulated in renal cell after injury. J Biol Chem. 1998;273:4135–4142. doi: 10.1074/jbc.273.7.4135. [DOI] [PubMed] [Google Scholar]
- 12.Moresco RN, Bochi GV, Stein CS, et al. Urinary kidney injury molecule-1 in renal disease. Clin Chim Acta. 2018;487:15–21. doi: 10.1016/j.cca.2018.09.011. [DOI] [PubMed] [Google Scholar]
- 13.Urbschat A, Obermüller N, Paulus P, et al. Upper and lower urinary tract infections can be detected early but not be discriminated by urinary NGAL in adults. Int Urol Nephrol. 2014;46:2243–2249. doi: 10.1007/s11255-014-0831-x. [DOI] [PubMed] [Google Scholar]
- 14.Han WK, Waikar SS, Johnson A, et al. Urinary biomarkers in the early diagnosis of acute kidney injury. Kidney Int. 2008;73:863–869. doi: 10.1038/sj.ki.5002715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waikar SS, Bonventre JV. Biomarkers for the diagnosis of acute kidney injury. Nephron Clin Pract. 2008;109:c192–c197. doi: 10.1159/000142928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang J-J, Chi N-H, Huang T-M, et al. Urinary biomarkers predict advanced acute kidney injury after cardiovascular surgery. Crit Care. 2018;22:108. doi: 10.1186/s13054-018-2035-8. 1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fan H, Zhao Y, Sun M, et al. Urinary neutrophil gelatinase-associated lipocalin, kidney injury molecule-1, N-acetyl-β-D-glucosaminidasw levels and mortality risk in septic patients with acute kidney injury. Arch Med Sci. 2018;14:1381–1386. doi: 10.5114/aoms.2018.79006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Westhoff JH, Seibert FS, Waldherr S, et al. Urinary calprotectin, kidney injury molecule-1, and neutrophil gelatinase-associated lipocalin for the prediction of adverse outcome in pediatric acute kidney injury. Eur J Pediatr. 2017;176:745–755. doi: 10.1007/s00431-017-2907-y. [DOI] [PubMed] [Google Scholar]
- 19.Seibert FS, Sitz M, Passfall J, et al. Prognostic value of urinary calprotectin, NGAL and KIM-1 in chronic kidney disease. Kidney Blood Press Res. 2018;43:1255–1262. doi: 10.1159/000492407. [DOI] [PubMed] [Google Scholar]
- 20.Yin C, Wang N. Kidney injury molecule-1 in kidney disease. Ren Fail. 2016;38:1567–1573. doi: 10.1080/0886022X.2016.1193816. [DOI] [PubMed] [Google Scholar]
- 21.Li Z, Shen C, Wang Y, et al. Circulating kidney injury molecule-1 is a novel diagnostic biomarker for renal dysfunction during long-term adefovir therapy in chronic hepatitis B. Medicine (Baltimore) 2016;95:e5264. doi: 10.1097/MD.0000000000005264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skowron B, Baranowska A, Dobrek L, et al. Urinary neutrophil gelatinase-associated lipocalin, kidney injury molecule-1, uromodulin, and cystatin C concentrations in an experimental rat model of ascending acute kidney injury induced by pyelonephritis. J Physiol Pharmacol. 2018;69:625–637. doi: 10.26402/jpp.2018.4.13. [DOI] [PubMed] [Google Scholar]
- 23.Moledina DG, Hall IE, Thiessen-Philbrook H, et al. Performance of serum creatinine and kidney injury biomarkers for diagnosing histologic acute tubular injury. Am J Kidney Dis. 2017;70:807–816. doi: 10.1053/j.ajkd.2017.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Askenazi DJ, Koralkar R, Levitan EB, et al. Baseline values of Candidate Urine Acute Kidney Injury (AKI) Biomarkers Vary by Gestational Age in Premature Infants. Pediatr Res. 2011;70:302–306. doi: 10.1203/PDR.0b013e3182275164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nadkarni GN, Coca SG, Meisner A, et al. Urinalysis findings and urinary kidney injury biomarker concentrations. BMC Nephrol. 2017;18:218. doi: 10.1186/s12882-017-0629-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sabbisetti VS, Waikar SS, Antoine DJ, et al. Blood Kidney Injury Molecule-1 is a biomarker of acute and chronic kidney injury and predicts progression to ESRD in type I diabetes. J Am Soc Nephrol. 2014;25:2177–2186. doi: 10.1681/ASN.2013070758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuwata K, Nakamura I, Ide M, et al. Comparison of changes in urinary and blood levels of biomarkers associated with proximal tubular injury in rat models. J Toxicol Pathol. 2015;28:151–164. doi: 10.1293/tox.2014-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ibrahim NE, McCarthy CP, Shrestha S, et al. Blood kidney injury molecule-1 predicts short and longer term kidney outcomes in patients undergoing diagnostic coronary and/ or peripheral angiography-results from the Catheter Sampled Blood Archive in Cardiovascular Diseases (CASABLANCA) study. Am Heart J. 2018;209:36–46. doi: 10.1016/j.ahj.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 29.Nowak N, Skupien J, Niewczas MA, et al. Increased plasma kidney injury molecule-1 suggests early progressive renal decline in non-proteinuric patients with type 1 diabetes. Kidney Int. 2016;89:459–467. doi: 10.1038/ki.2015.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Colombo M, Looker HC, Farran B, et al. Serum kidney injury molecule 1 and β2-microglobulin perform as well as larger biomarkers panels for prediction of rapid decline in renal function in type 2 diabetes. Diabetologia. 2019;62:156–168. doi: 10.1007/s00125-018-4741-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shahbaz SK, Pourrezagholi F, Barabadi M, et al. High expression of TIM-3 and KIM-1 in blood and urine of renal allograft rejection patients. Transpl Immunol. 2017;43-44:11–20. doi: 10.1016/j.trim.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 32.Schultz CA, Engström G, Nilsson J, et al. Plasma kidney injury molecule-1 (KIM-1) levels and deterioration of kidney function over 16 years. Nephrol Dial Transplant. 2019 doi: 10.1093/ndt/gfy382. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kamianowska M, Szczepański M, Kulikowska EE, et al. Do serum and urinary concentration of kidney injury molecule-1 in healthy newborns depend on birth weight, gestational age or gender ? J Perinatol. 2017;37:73–76. doi: 10.1038/jp.2016.169. [DOI] [PubMed] [Google Scholar]
- 34.Zwiers AJ, deWildt SN, de Rijke YB, et al. Reference intervals for renal injury biomarkers neutrophil gelatinase-associated lipocalin and kidney injury molecule-1 in young infants. Clin Chem Lab Med. 2015;53:1279–1289. doi: 10.1515/cclm-2014-1020. [DOI] [PubMed] [Google Scholar]
- 35.Bennett MR, Nehus E, Haffner C, et al. Pediatric reference ranges for acute kidney injury biomarkers. Pediatr Nephrol. 2015;30:677–685. doi: 10.1007/s00467-014-2989-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McWilliam SJ, Antoine DJ, Sabbisetti V, et al. Reference intervals for urinary renal injury biomarkers KIM-1 and NGAL in healthy children. Biomark Med. 2014;8:1189–1197. doi: 10.2217/bmm.14.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pennemans V, Rigo JM, Faes C, et al. Estabilishment of reference values for novel urinary biomarkers for renal damage in the healthy population: are age and gender an issue? Clin Chem Lab Med. 2013;51:1795–1802. doi: 10.1515/cclm-2013-0157. [DOI] [PubMed] [Google Scholar]
- 38.Schley G, Köberle C, Manuilova E, et al. Comparison of plasma and urine biomarker performance in acute kidney injury. PLoS One. 2015;10:e0145042. doi: 10.1371/journal.pone.0145042. [DOI] [PMC free article] [PubMed] [Google Scholar]